Extract
The primary determinant of clinical outcomes in pulmonary arterial hypertension (PAH) is the function of the right ventricle and regular evaluation for right ventricular dysfunction is increasingly recognised as a risk assessment tool [1]. Reducing right ventricular afterload through targeted therapy in PAH is associated with improved right ventricular function and clinical outcome.[2] Most commonly, transthoracic echocardiography is conducted to evaluate right ventricular structure and function in clinical practice, both at the time of diagnosis and during follow-up. Alongside echocardiographic measurements of area and volumes of the right ventricle, the ratio of tricuspid annular plane excursion (TAPSE) to pulmonary artery systolic pressure (PASP) was introduced as a prognostic and treatment-sensitive marker in current guidelines, reflecting the coupling between the right ventricle and the pulmonary artery [1].
Shareable abstract
The RVFWLS/PASP ratio, a novel surrogate for ventriculoarterial coupling, showed sensitivity to afterload-lowering treatment and the magnitude of change informed on long-term outcomes in PAH https://bit.ly/4cRtREC
To the Editor:
The primary determinant of clinical outcomes in pulmonary arterial hypertension (PAH) is the function of the right ventricle and regular evaluation for right ventricular dysfunction is increasingly recognised as a risk assessment tool [1]. Reducing right ventricular afterload through targeted therapy in PAH is associated with improved right ventricular function and clinical outcome.[2] Most commonly, transthoracic echocardiography is conducted to evaluate right ventricular structure and function in clinical practice, both at the time of diagnosis and during follow-up. Alongside echocardiographic measurements of area and volumes of the right ventricle, the ratio of tricuspid annular plane excursion (TAPSE) to pulmonary artery systolic pressure (PASP) was introduced as a prognostic and treatment-sensitive marker in current guidelines, reflecting the coupling between the right ventricle and the pulmonary artery [1]. However, the use of TAPSE has limitations due to its angle dependency and susceptibility to global heart motion [3]. Advances in echocardiographic application provide novel automated measurement tools including right ventricular strain analysis, which is independent of angulation and captures right ventricular segments differentially. The right ventricular free wall longitudinal strain (RVFWLS) specifically measures the longitudinal deformation of the free wall. Recently, Ünlü et al. [4] replaced TAPSE with RVFWLS and reported on the superior prognostic value of the RVFWLS/PASP ratio in 65 patients with precapillary pulmonary hypertension, with 52% classified as PAH. Since the RVFWLS/PASP ratio may also reflect the load-dependent length/force relationship of the right ventricle, Richter et al. [5] subsequently demonstrated that RVFWLS/PASP correlates with the pressure–volume loop-derived ratio of contractility (end-systolic elastance) to load (arterial elastance) in 29 patients with PAH. RVFWLS/PASP ratio may therefore capture clinically relevant aspects of right ventricular mechanics and could potentially inform on right ventricle-linked mortality risk in PAH. However, it is unknown whether RVFWSL/PASP ratio is sensitive to treatment in PAH and whether changes over time associate with clinical outcomes.
We performed a retrospective analysis of 48 treatment-naïve patients diagnosed with idiopathic or hereditable PAH between 2014 and 2019 at a single centre in Germany. PAH was diagnosed based on a mean pulmonary arterial pressure ≥25 mmHg and pulmonary arterial wedge pressure ≤15 mmHg. Patients were commenced on an (at the time) approved PAH targeted drug(s) and follow-up visits were scheduled every 3–6 months (or whenever clinically indicated). Composite outcome events were defined as all-cause mortality or lung transplantation (censored on 30 June 2023).
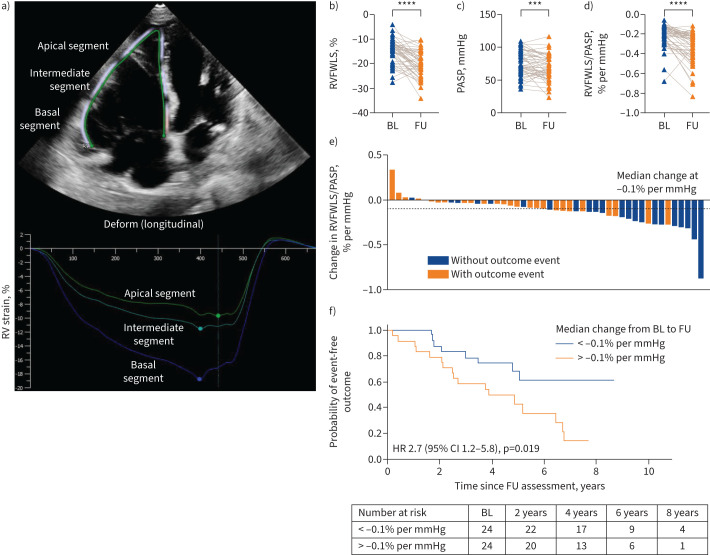
The Auto-Strain RV (IMAGE-COM, TOMTEC-ARENA; Tomtec Imaging System GmbH, Unterschleissheim, Germany) was used to automatically track the myocardium throughout the cardiac cycle on the apical four-chamber view and generate strain measurements. RVFWLS, as a percentage, was obtained by averaging strain values from the basal, intermediate and apical segments of the right ventricular free wall (figure 1a). TAPSE in millimetres was measured by placing the M-mode cursor through the lateral tricuspid annulus. PASP in millimetres of mercury was estimated based on the tricuspid regurgitation jet (simplified Bernoulli equation), as well as the collapse and diameter of the inferior vena cava.
FIGURE 1.
Effect of afterload-lowering treatment on the right ventricular free wall longitudinal strain (RVFWLS) to pulmonary arterial systolic pressure (PASP) in pulmonary arterial hypertension (PAH). a) The apical four-chamber view and two-dimensional strain analysis of the right ventricle (RV) in a patient with idiopathic PAH, involving three segments of the RV free wall. The RV myocardium was automatically identified, segmented, and tracked, allowing visualisation of the RV strain to time curves. The reference point for image analysis was taken at the onset of the QRS complex (R-R gating). After automatic placement of the myocardial border at the end of diastole, the border accurately followed the cardiac motion throughout the cardiac cycle. The peak RV systolic strain of each segment was visually marked with a dot. The basal segment or RV free wall is represented by the lower curve (blue), the intermediate segment by the middle curve (turquoise) and the apical segment by the upper curve (green). The RVFWLS was then calculated by averaging strain values of the three segments. Targeted treatment for PAH decreased significantly b) RVFWLS, c) PASP and d) RVFWLS/PASP ratio from baseline to follow-up. e) Waterfall plot illustrates that the cumulative incidence of outcome events decreased in patients with more a distinct decrease of RVFWLS/PASP. f) Stratification of patients by the median change in RVFWLS/PASP (−0.1% per mmHg) significantly informed on long-term outcomes, as illustrated by the Kaplan–Meier plot. BL: baseline; FU: follow-up; HR: hazard ratio. ***: p≤0.001; ****: p≤0.0001.
Statistical analysis included the Wilcoxon matched pair test, log-rank test and receiver operating characteristic (ROC). Data are presented as mean±sd or as median (interquartile range). Data collection was approved by the local ethics committee and the study complied the Declaration of Helsinki.
Most patients were female (58%) and mean age at diagnosis was 60±19 years. Diagnostic right heart catheterisation revealed a mean pulmonary arterial pressure of 50±13 mmHg, pulmonary arterial wedge pressure of 10±3 mmHg and pulmonary vascular resistance of 10±6 Wood units. At baseline, 75% of the patients presented with World Health Organization functional class III–IV symptoms, with a 6-min walk distance averaging 329±130 m and N-terminal pro-B-type natriuretic peptide concentration of 3279±4865 ng·L−1. Upfront combination therapy was initiated in 56% of patients (dual in 46% and triple in 10%). The median time between treatment initiation and the follow-up visit was 5.2 (3.3–6.6) months. The median observational period, starting from the follow-up visit, was 4.5 (2.5–5.3) years, during which 23 outcome events occurred (22 deaths and one lung transplantation).
At baseline, RVFWLS was −14±4% and estimated PASP was 76±17 mmHg, both significantly decreasing during follow-up to −20±5% and 68±19 mmHg, respectively (figure 1b and c). The mean RVFWLS/PASP ratio was −0.2±0.1% per mmHg at baseline, decreasing during follow-up to −0.33±0.18% per mmHg (figure 1d). As the RVFWLS represents per cent change in myocardial length from the relaxed to the contractile state, improved right ventricular function is characterised by a more negative value. Similarly, a more negative value for the RVFWLS/PASP ratio indicates an improved length/force relationship. The cumulative incidence of outcome events decreased in patients with a more pronounced decrease of RVFWLS/PASP ratio from baseline to follow-up (figure 1e). Stratifying patients based on the median change in RVFWLS/PASP ratio (−0.1% per mmHg) significantly affected long-term outcomes (figure 1f). The area under the ROC curve was 0.67 (95% CI 0.51–0.83) for the ability of the absolute change to distinguish outcomes (p=0.031).
At baseline, the TAPSE/PASP ratio was 0.24±0.1 mm per mmHg, increasing during follow-up to 0.31±0.2 mm per mmHg (p=0.0001). The median change in the TAPSE/PASP ratio from baseline to follow-up (0.04 mm per mmHg) did not significantly correlate with survival (log-rank test p=0.54), and the absolute change did not clearly distinguish outcomes in this cohort (area under the ROC curve 0.57, 95% CI 0.4–0.74; p=0.41).
Our data add to the evaluation of the RVFWLS/PASP ratio as a prognostic noninvasive surrogate marker for ventriculoarterial coupling in PAH. We observed that this ratio was sensitive to afterload-lowering treatment and that the magnitude of change following treatment initiation informed on long-term outcomes, while changes in the TAPSE/PASP ratio did not differentiate among outcome events in this cohort.
The TAPSE/PASP ratio is a promising candidate for integrating right heart imaging into current risk stratification models [6, 7]. Compared to TAPSE alone, it was demonstrated in a large cohort of PAH patients that the presence of tricuspid regurgitation and dilation of the inferior vena cava adds prognostic value [8]. However, the measurement of TAPSE has limitations, and RVFWLS was found to provide prognostic information in patients with PAH and right ventricular dysfunction but with normal (or pseudonormal) TAPSE [9]. The RVFWLS/PASP ratio now serves as a combined measure of right ventricular function and afterload, considering the longitudinal shortening of the right ventricle along with its ability to generate pressure, which was found to be stronger predictor for clinical outcomes compared to TAPSE/PASP [4].
Our study has limitations, including its retrospective and single-centre design. We did not focus on the morphology of the right ventricular strain curve, which can be divided into certain patterns that themselves may carry prognostic information [10]. The cohort was not specifically selected for the analysis of the TAPSE/PASP ratio and statistical power was limited. Larger cohorts are warranted to assess differences between the RVFWLS/PASP and TAPSE/PASP ratios. Additionally, further investigation is needed to explore whether the integration of the RVFWLS/PASP ratio can improve clinical risk stratification tools.
In summary, our study adds data to the ongoing assessment of optimal noninvasive surrogates for right ventricular mechanics in PAH. Our findings support the RVFWLS/PASP ratio as a promising clinically relevant candidate and may contribute to a better understanding of how this surrogate can help to improve management of patients with PAH. Further research is warranted to explore these relationships prospectively.
Footnotes
Provenance: Submitted article, peer reviewed.
Ethics statement: Retrospective data collection was approved by the local ethics committee.
Conflict of interest: All authors have approved the current version of the manuscript prior to submission and declared that the submitted work is original and has not been published elsewhere (nor is it under consideration for publication) in any language, including English. No financial conflict of interest has arisen from any author that interferes with the study design, methods or results.
References
- 1.Humbert M, Kovacs G, Hoeper MM, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 2023; 61: 2200879. doi: 10.1183/13993003.00879-2022 [DOI] [PubMed] [Google Scholar]
- 2.Vizza CD, Lang IM, Badagliacca R, et al. Aggressive afterload lowering to improve the right ventricle: a new target for medical therapy in pulmonary arterial hypertension? Am J Respir Crit Care Med 2022; 205: 751–760. doi: 10.1164/rccm.202109-2079PP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tello K, Naeije R, de Man F, et al. Pathophysiology of the right ventricle in health and disease: an update. Cardiovasc Res 2023; 119: 1891–1904. doi: 10.1093/cvr/cvad108 [DOI] [PubMed] [Google Scholar]
- 4.Ünlü S, Bézy S, Cvijic M, et al. Right ventricular strain related to pulmonary artery pressure predicts clinical outcome in patients with pulmonary arterial hypertension. Eur Heart J Cardiovasc Imaging 2023; 24: 635–642. doi: 10.1093/ehjci/jeac136 [DOI] [PubMed] [Google Scholar]
- 5.Richter MJ, Rako ZA, Tello K. Ratio between right ventricular strain and systolic pulmonary artery pressure as a surrogate for right ventricular to pulmonary arterial coupling: validation against the gold standard. Eur Heart J Cardiovasc Imaging 2023; 24: e50–e52. doi: 10.1093/ehjci/jeac253 [DOI] [PubMed] [Google Scholar]
- 6.Fauvel C, Raitiere O, Boucly A, et al. Interest of TAPSE/sPAP ratio for noninvasive pulmonary arterial hypertension risk assessment. J Heart Lung Transplant 2022; 41: 1761–1772. doi: 10.1016/j.healun.2022.09.005 [DOI] [PubMed] [Google Scholar]
- 7.Ostermann J, Pott J, Hennigs JK, et al. Residual risk identified in routine noninvasive follow-up assessments in pulmonary arterial hypertension. ERJ Open Res 2023; 9: 00072-2023. doi: 10.1183/23120541.00072-2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghio S, Mercurio V, Fortuni F, et al. A comprehensive echocardiographic method for risk stratification in pulmonary arterial hypertension. Eur Respir J 2020; 56: 2000513. doi: 10.1183/13993003.00513-2020 [DOI] [PubMed] [Google Scholar]
- 9.van Kessel M, Seaton D, Chan J, et al. Prognostic value of right ventricular free wall strain in pulmonary hypertension patients with pseudo-normalized tricuspid annular plane systolic excursion values. Int J Cardiovasc Imaging 2016; 32: 905–912. doi: 10.1007/s10554-016-0862-8 [DOI] [PubMed] [Google Scholar]
- 10.Badagliacca R, Pezzuto B, Papa S, et al. Right ventricular strain curve morphology and outcome in idiopathic pulmonary arterial hypertension. JACC Cardiovasc Imaging 2021; 14: 162–172. doi: 10.1016/j.jcmg.2020.08.017 [DOI] [PubMed] [Google Scholar]