Abstract
Gastrointestinal bleeding due to hemobilia is a rare condition but can be very serious, even life-threatening. The main causes of biliary bleeding are invasive procedures in treatment, trauma, or malignant diseases. Chronic obstruction of the biliary tract can cause inflammation, erosion, and leakage of adjacent vascular structures and lead to pseudoaneurysm or hemorrhage, but this is very rare. In this article, we present a clinical case of upper gastrointestinal bleeding due to a pseudoaneurysm of the hepatic artery believed to have formed due to chronic cholangitis. An 81-year-old female patient with a medical history of chronic cholangitis was admitted to the hospital with recurrent inflammation accompanied by progressive upper gastrointestinal bleeding, potentially life-threatening. Ultrasound images and blood tests confirmed that the patient had anemia and cholangitis caused by stones. Gastrointestinal endoscopy showed bleeding suspected to be from the biliary tract. Hepatobiliary computed tomography confirmed that the common hepatic artery pseudoaneurysm located at the upper end of the common bile duct had active bleeding.
Keywords: Hemobilia, Chronic cholangitis, Gallstones, Computed tomography
Introduction
Hemobilia is defined as bleeding from or within the bile ducts. This is a rare but important cause of gastrointestinal bleeding that can be serious and even fatal [1]. The main causes of hemobilia are caused by diagnostic or treatment interventions, trauma, and cancer [2]. Chronic obstruction of the biliary tract can cause inflammation, erosion, and leakage of adjacent vascular structures and lead to pseudoaneurysm or hemorrhage [3]. Hepatic artery pseudoaneurysm due to chronic cholangitis causing hemobilia is a rare and underreported clinical condition [1,4]. Although the mechanism of pseudoaneurysm is still not clearly explained, some authors believe that pseudoaneurysm is caused by a severe inflammatory reaction in the biliary tracts that penetrates the liver parenchyma and can erode the layer of the hepatic artery wall [5]. In this article, we present a case of hepatic artery pseudoaneurysm due to chronic cholangitis causing life-threatening biliary bleeding.
Case presentation
A female patient, 81 years old, was admitted to the hospital because of upper abdominal pain, constant dull pain for 3 days, without attacks, accompanied by a fever of 39°C. In addition, the patient had symptoms of nausea, vomiting yellow fluid, and diarrhea in addition to dark liquid stools. On investigation, the patient had a clinical history of cholangitis caused by stones recurring many times. The patient was admitted to the hospital with an initial diagnosis of recurrent cholangitis.
Initial clinical examination found that the patient's abdomen was mildly distended, with tenderness in the epigastric area and negative guarding. The patient has a mild fever of 37.5°C, pale skin, and mucous membranes. Abdominal ultrasound showed dilated intra- and extra-hepatic bile ducts and stones in the left hepatic bile duct. Tests showed direct bilirubin 7.2 µmol/l, total bilirubin 19.7 µmol/l, and white blood cell 11 G/l in which the ratio of neutrophils was 87.7%. Besides, the patient has anemia with hemoglobin (Hb) 109 g/l. However, the patient has symptoms of increasing abdominal pain, accompanied by bloody stools. The complete blood count test was performed again and detected ongoing severe anemia, Hb level decreased to 58 g/l. Hepatobiliary magnetic resonance imaging shows thrombus filling the common bile duct (Fig. 1). Therefore, the patient was prescribed a stomach and colon endoscopy and abdominal computed tomography.
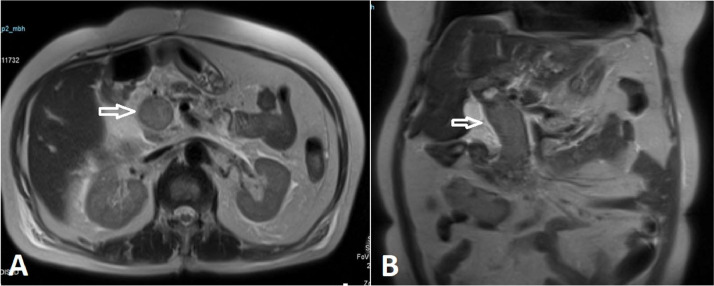
Fig. 1.
Hepatobiliary magnetic resonance image, on T2-weighted sequences shows a dilated common bile duct, containing extensive thrombus (arrows).
Endoscopy results showed that the duodenal bulb segment DII-DIII had a lot of blood. The Vater papilla increases in size, suspected of having a thrombosis inside, the surface of this papilla is covered with some large blood clots. On computed tomography images, thrombosis spread to the bile ducts inside and outside the liver (Fig. 2). She had a large pseudoaneurysm of the common hepatic artery protruding into the bile duct measuring 16 × 14 mm with an active bleeding. So the doctors have found the cause of the patient's acute anemia. Immediately, a consultation between gastroenterologists, surgeons, and interventionalists was organized. The best treatment direction for the patient was quickly given, which was endovascular embolization for pseudoaneurysm under the guidance for digital subtraction angiography (DSA) (Fig. 3). The intervention took place smoothly within 2 hours and there was no recurrent hemobilia after this procedure (Fig. 4).
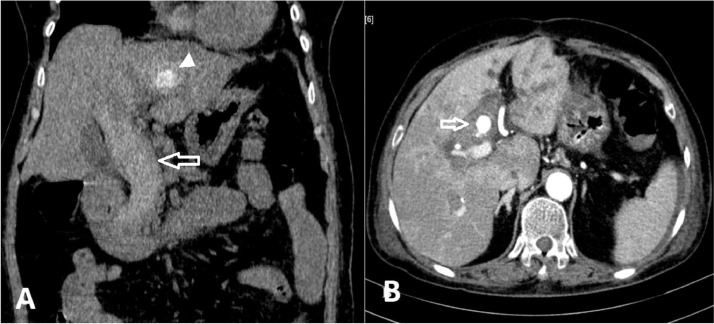
Fig. 2.
Computed tomography image. (A), On the precontrast image, the common bile duct is dilated and there is extensive thrombus with increased density (arrow), and intrahepatic biliary stones (arrow head). (B), On the postcontrast image, the arterial phase shows a pseudoaneurysm of the common hepatic artery protruding into the bile duct (arrow).
Fig. 3.
Digital subtraction angiography image. (A), Image of common hepatic artery pseudoaneurysm before intervention (arrow). (B), The postintervention image was rechecked and the aneurysm was no longer visible.
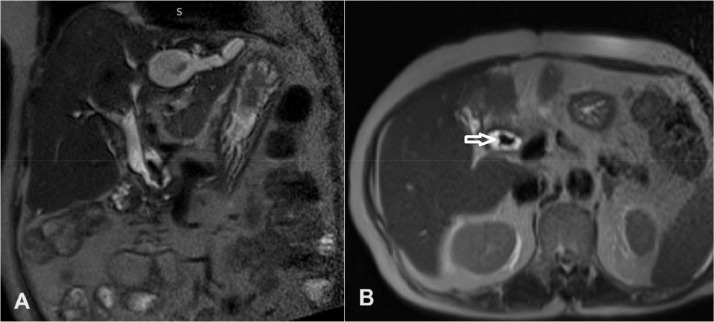
Fig. 4.
Hepatobiliary magnetic resonance image after treatment, the common bile duct is slightly dilated due to stones (arrow), and no thrombus is seen in the bile duct lumen.
Discussion
Gastrointestinal bleeding due to hemobilia is a rare condition but can be very serious, even life-threatening [1]. The main cause of hemobilia is recorded to be due to treatment interventions such as percutaneous cholangiography, endoscopic retrograde cholangiopancreatography, biliary tract surgery [3]. Besides, causes such as trauma and malignant diseases are also considered common causes of hemobilia [2]. Hemobilia due to chronic cholangitis or biliary obstruction is less common but is also mentioned. Chronic obstruction of the biliary tract can lead to inflammation, erosion, and leakage to adjacent vascular structures and lead to bleeding [3]. Severe inflammatory reactions in the biliary tract can penetrate the liver parenchyma and can erode the hepatic artery wall, thereby forming a pseudoaneurysm [5].
Hemobilia, although uncommon, is difficult to recognize because diagnosis and management are quite different from other causes of upper gastrointestinal bleeding [6]. Jaundice, right upper quadrant abdominal pain, and upper gastrointestinal bleeding are common symptoms of hemobilia—known as Quincke's triad, but all 3 symptoms at the same time only occur in 22%-35% of cases [7]. Therefore, in cases of unexplained gastrointestinal bleeding, especially in patients with hepatobiliary disease, hemobilia is one of the important differential diagnoses that should be considered [5]. Our patient had symptoms of abdominal pain and acute anemia suspected to be due to gastrointestinal bleeding. Combined with the patient's history of chronic cholangitis, hemobilia is a cause that doctors consider along with other causes of upper gastrointestinal bleeding. Immediately, gastrointestinal endoscopy and abdominal CT scan were ordered.
The patient's endoscopic image showed that the duodenum segment DII-DIII had a lot of blood. Vater papilla increases in size, suspected of thrombosis inside, large blood clots on the surface of this papilla. On computed tomography imaging, there was a common hepatic artery pseudoaneurysm with active bleeding. Diagnostic imaging techniques can be very helpful in making an initial diagnosis and directing subsequent treatment. However, findings may be nonspecific, in which case clinical, imaging, and laboratory correlations should be carefully considered [3]. For patients with upper gastrointestinal bleeding, endoscopy is the first step. If blood or clots are seen in the Vater papilla, hemobilia may be the cause of the bleeding [4]. However, in a small study of patients with hemobilia, endoscopy showed direct or indirect evidence in only 60% [7]. In addition, other techniques such as abdominal CT with angiography protocol, endoscopic retrograde cholangiopancreatography, angiography... are also used to diagnose hemobilia depending on each case [3,4]. Abdominal CT with angiography protocol is a means with many advantages in diagnosing biliary tract bleeding such as noninvasiveness and low radiation exposure compared to angiography, fast results, and high diagnostic specificity [3].
After determining the exact cause of bleeding, doctors choose to perform embolization under digital subtraction angiography guidance as the treatment method. This is a quick, appropriate, and effective solution for isolated pseudoaneurysms in elderly patients.
Hemostasis and reduction of biliary obstruction are the 2 main goals to be achieved in the treatment of hemobilia [4]. The management approach depends on several factors, including the suspected source of bleeding (arterial or venous bleeding), the degree of hemodynamic instability, and the causes [3]. Embolization is the main treatment option for patients with mild hemobilia that does not improve or with severe hemobilia requiring blood transfusion. The liver's dual blood supply (75% via the portal vein and 25% via the hepatic artery) allows embolization of hepatic artery branches without much concern for focal ischemia or infarction [7]. Placing a stent covers the vascular lesion is an alternative to embolization, often used in liver transplant patients. The majority of cases of hemobilia can be controlled with image-guided intervention so surgery is rarely necessary [3]. Surgical options include hepatic artery ligation, pseudoaneurysm resection, or hepatic segment/lobectomy possibly with concomitant cholecystectomy. Although surgery has a high success rate of over 90%, it also has a high mortality rate of up to 10% [7].
Conclusion
In conclusion, chronic cholangitis is one of the rare causes of hemobilia. However, severe inflammation in the biliary tract can penetrate the liver parenchyma and can erode the hepatic artery wall, thereby forming a pseudoaneurysm or hemorrhage. Therefore, in case of gastrointestinal bleeding of unknown cause, especially in patients with hepatobiliary disease, hemobilia is one of the important differential diagnoses that should be considered.
Patient consent
Informed consent for patient information to be published in this article was obtained.
Author's contributions
Tran QL and Nguyen MD: Case file retrieval and case summary preparation. Tran QL and Nguyen MD: preparation of manuscript and editing. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Our institution does not require ethical approval for reporting individual cases or case series. Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
Consent for publication
Not applicable.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments: None to declare.
References
- 1.Chang CW, Wu YH, Liu HL. Upper Gastrointestinal Bleeding With Hemobilia Caused by Gallstones. J Emerg Med. 2020;58(5):e227–e229. doi: 10.1016/j.jemermed.2020.03.035. [DOI] [PubMed] [Google Scholar]
- 2.Parvinian A, Fletcher JG, Storm AC, Venkatesh SK, Fidler JL, Khandelwal AR. Challenges in Diagnosis and Management of Hemobilia. Radiographics. 2021;41(3):802–813. doi: 10.1148/rg.2021200192. [DOI] [PubMed] [Google Scholar]
- 3.Berry R, Han JY, Kardashian AA, LaRusso NF, Tabibian JH. Hemobilia: Etiology, diagnosis, and treatment. Liver Res. 2018;2(4):200-208. 10.1016/j.livres.2018.09.007. [DOI] [PMC free article] [PubMed]
- 4.Liu TT, Hou MC, Lin HC, Chang FY, Lee SD. Life-threatening hemobilia caused by hepatic artery pseudoaneurysm: a rare complication of chronic cholangitis. World J Gastroenterol. 2003;9(12):2883–2884. doi: 10.3748/wjg.v9.i12.2883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akatsu T, Hayashi S, Egawa T, Doi M, Nagashima A, Kitano M, Yamane T, Yoshii H, Kitajima M. Hepatic artery pseudoaneurysm associated with cholecystitis that ruptured into the gallbladder. J Gastroenterol. 2004;39(9):900–903. doi: 10.1007/s00535-003-1408-0. [DOI] [PubMed] [Google Scholar]
- 6.Kim KH, Kim TN. Etiology, clinical features, and endoscopic management of hemobilia: a retrospective analysis of 37 cases. Korean J Gastroenterol. 2012;59(4):296–302. doi: 10.4166/kjg.2012.59.4.296. [DOI] [PubMed] [Google Scholar]
- 7.Murugesan SD, Sathyanesan J, Lakshmanan A, Ramaswami S, Perumal S, Perumal SU, et al. Massive hemobilia: a diagnostic and therapeutic challenge. World J Surg. 2014;38(7):1755–1762. doi: 10.1007/s00268-013-2435-5. [DOI] [PubMed] [Google Scholar]