Abstract
Objective
This meta-analysis study aims to determine the efficacy and safety of surgical and conservative treatments for distal radius fractures (DRFs) in adults.
Methods
Reports of randomized controlled trials were retrieved from the Web of Science, Pubmed, Google Scholar, EMBASE, Cochrane Library, Medline, Ovid, and BIOSIS for studies that met the eligibility criteria. The search was limited to human subjects and had no language limits. The search strategy was check by two independent reviewers. If there was any dispute, a third reviewer was consulted. Primary outcomes were: (1) the active wrist range of motion including flexion, extension, pronation, supination, radial, and ulnar deviation; (2) the Disabilities of the Arm, Shoulder, and Hand (DASH) score; and (3) radiological outcomes including radial inclination and ulnar variance. Secondary outcomes were the number of complications including non-infectious and infectious. Quality assessment was performed using the Cochrane Risk of Bias Tool provided by the Cochrane Review Manager 5.3.
Results
A total of 10 randomized controlled trials were included. The meta-analysis detected no statistically significant difference in pooled data for complications not included infection (MD 0.64, CI: 0.33 to 1.23, Z=1.34, p=0.18). Surgical treatment achieved a better range of motion (MD 3.76, CI: 1.58 to 5.95, Z=3.37, p=0.0007), DASH score (MD −6.57, CI: −9.08 to −4.06, Z=5.12, p<0.00001), and radiographic outcomes (MD 3.75, CI: 2.75 to 4.74, Z=7.37, p<0.00001) compared with conservative treatment. In contrast, the conservative treatment achieved less infection rate compared with surgical treatment (MD 4.09, CI: 1.18 to 14.21, Z=2.21, p=0.03).
Conclusion
Findings of this study reveal that when compared with conservative treatment, surgical treatment can ensure better clinical and radiological results for the treatment of DRFs in adults. Although similar complication rates can be encountered with both treatment modalities, it should be taken into account that the rate of infection may be higher in surgical treatment.
Level of Evidence
Level I, Therapeutic Study
Keywords: Distal radius fractures, Surgical treatment, Conservative treatment, Randomized controlled trials
Introduction
Distal radius fractures (DRFs) are one of the most frequent fractures among the elderly and pediatric population. The absolute number of pediatric DRFs decreased from 2002 to 2017, whereas the incidence of hospitalization among DRF patients increased, indicating a trend towards operative treatment (1). The age-adjusted incidence ranges from 73 to 767 per 100000 in men and women in large population-based studies (2). DRFs are more common in osteoporosis patients (2). At the age of 60 years, the risk of a DRF is approximately 2% for men and 15% for women in their residual lifetime (3).
There are two main options for the treatment of DRFs, conservative treatment and surgical treatment. Elderly patients whose bone substance cannot sustain an operation tend to be treated with conservative treatment, which includes closed reduction and plaster immobilization. In addition, conservative treatment is suitable for nondisplaced fractures. However, young patients demand better joint function while recovery, and they have good bone substance. Hence, operational treatment is a better choice for them. In particular, when encountered with comminuted fractures, the bone fragments may be too small, making it impossible to use conservative treatment to fix the fragments or joint cartilage, which will lead to the malalignment of bone fragments after the patient is healed. The exact indications of conservative and surgical treatment methods are as follows: dorsal angulation >20° at presentation, dorsal comminution, intra-articular fractures, associated ulnar fracture, and age over 60 years. If 3 of these 5 predictors exist, the fracture is considered to be potentially unstable, and therefore, surgical treatment is advisable (4).
With improvements in the surgical techniques over the years, surgical treatment such as Kirschner-wire stabilization, external fixation, open reduction, and internal fixation with volar locked plating (ORIF) are developing rapidly. There is a trend of using surgical treatment rather than conservative treatment to heal DRFs (5–11). But there is no clear to answer the question of whether, in treatment of DRFs, the benefits of anatomical reconstruction of the wrist joint by surgical treatment, coupled with swift attainment functional stability, outweigh the disadvantage of greater risk of complications and higher costs (7, 11, 12).
Thus, as the optimal treatment for DRFs remains unknown, we perform a meta-analysis of randomized controlled trials (RCTs) to establish the optimal management of DRF.
Materials and Methods
Literature search strategy
Reports of RCTs were retrieved from Web of Science, Pubmed, Google Scholar, EMBASE, Cochrane Library, and BIOSIS. Studies from the earliest records available to those dated December 11, 2019 were retrieved. The following search terms were used: “distal radius fracture” “distal radius fractures”, “fractures of distal radius” “fractures of radius” “Colles fractures” “surgical treatment” “surgical option” “Kirschner-wire stabilization” “K-wire stabilization” “external fixation” “open reduction” “internal fixation” “volar locked plating” “nonsurgical treatment” “nonsurgical option” “conservative treatment” “conservative option” “closed reduction” “plaster casting” “plaster immobilization or casting”. The search was limited to human subjects and had no language limits. The combination of the following terms was used: “(distal radius fracture or distal radius fractures or fractures of distal radius or fractures of radius or Colles fractures) and (surgical treatment or surgical option) and (Kirschner-wire stabilization or K-wire stabilization or external fixation or open reduction or internal fixation or volar locked plating or nonsurgical treatment or nonsurgical option or conservative treatment or conservative option or closed reduction or plaster casting or plaster immobilization or casting)”. The search strategy was check by two independent reviewers. If there was any dispute, a third reviewer was consulted.
Inclusion and Exclusion
Inclusion criteria
Studies were included if they met the following criteria: [1] studies comparing the outcomes of surgical and conservative treatments of DRF patients; [2] were RCTs; [3] patients suffering from fractures of radius; [4] no others therapies were adopted for the patients before surgical or conservative treatment; and [5] outcome measures included the active ranges of motion of the wrist or DASH scores or radiological outcomes or complications or infections.
Exclusion criteria
Studies were excluded if: [1] they were protocols, abstracts, letters, or meeting proceedings, [2] were studies for pediatric, and [3] they did not specify the type of surgical treatment and nonsurgical treatment.
Data extraction
The following data were extracted from studies that met the inclusion criteria [1] first author’s name, methods of treatment, age, year of publication, number of patients; [2] clinical outcomes: flexion, extension, pronation, supination, radial deviation, ulnar deviation, and DASH score; and [3] radiological outcomes: radial inclination, ulnar variance, [4] number of complications, and [5] number of infections.
Quality assessment
Quality assessment was performed for the studies that were included by two independent reviewers using the Cochrane Risk of Bias Tool provided by the Cochrane Review Manager 5.3. If there were any inconsistencies, a third reviewer was consulted.
Outcome measures
The primary outcome measures were the active ranges of motion of the wrist of conservative and surgical groups, including flexion, extension, pronation, supination, radial deviation, ulnar deviation, DASH scores, and radiological outcomes (including radial inclination and ulnar variance). Secondary outcomes were the number of complications, including infectious and non-infectious.
Statistical analysis
Two authors entered the data into the Review Manager (RevMan) software (version 5.3; Cochrane Collaboration, London, UK) independently. The weighted mean difference was used for summary data for continuous outcomes, with 95% confidence interval (CI). Relative risk (RR) was used for dichotomous outcomes, with a 95% confidence interval (CI). Cochran Q and the I2 statistics were used to assess the heterogeneity of the studies. For Cochran Q, if p<0.10, it was considered that there was significant heterogeneity between the statistics (13). The percentage of the observed between-study variability due to heterogeneity was indicated by I2 statistic, which was based on the following ranges: 0–25%, no heterogeneity; 25–50%, moderate heterogeneity; 50–75%, large heterogeneity; and 75–100%, extreme heterogeneity13. Hence, the existence of heterogeneity between studies was indicated, if either p<0.1 or I2 >50%. Hence, if there was heterogeneity between studies, we used the random-effects model, else, a fixed-effects model was used, and the possible source of heterogeneity was explored. Two-sided tests were used for all analyses; the significance level was p<0.05.
Results
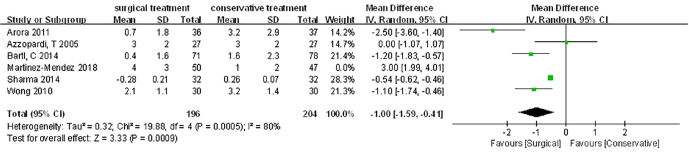
The details of search and exclusion criteria are displayed in the flow diagram (Figure 1).
Figure 1.
The graph shows a flow diagram of the detailed search and exclusion criteria
Included studies
Ten RCTs with a total of 784 patients were included (7, 14–23). All studies had a full publication (Table 1). In total, 4 articles compared percutaneous pin fixation with closed reduction with cast immobilization (14–17, 20), 5 articles compared open reduction and internal fixation with a volar locking plate with closed reduction with cast immobilization (7, 19, 21, 22), and 1 article compared external fixation using a Medium-C-Hoffman fixator with closed reduction with cast immobilization (18).
Table 1.
Characteristics of the 10 included studies
| Author (year) | Study Design | Surgical/Conservative (number of patients) | Age (years) Surgical/Conservative | Type of distal radial fracture | Surgical Treatment Details | Conservative Treatment | Outcome Measure | Follow-up Surgical/Conservative |
|---|---|---|---|---|---|---|---|---|
| Gupta 1999 | Single-center, prospective randomized controlled trail | 25/25 | 55.64 (22–80) | Colles' Fracture | Percutaneous Crossed-Pin Fixation | Plaster of Paris Cast Immobilization | Radiographic parameters, average loss of various movements, and complications. | 8 weeks/8 weeks |
| Rodriguez-Merchan 1997 | Single-center, prospective randomized controlled trail | 20/20 | 58(47–65)/ 56(46–63) | Unstable Frykman III–VIII distal radius fracture | Percutaneous transfixion with K-wires | Anatomic reduction and immobilized in a split below-elbow cast | Initial displacement, quality of reduction, carpal malalignment, articular step-off. Range of motion and grip strength. | 1 week, 3 weeks, 7 weeks, 1 year/ 1 week, 3 weeks, 7 weeks, 1 year |
| Wong 2010 | Single-center, prospective randomized controlled trail | 30/30 | 70(66–76)/ 71(65–76) | Unstable, dorsally angulated, extra-articular fracture of the distal radius | Percutaneous K-wires insertion | Plaster cast | The active ranges of motion of the wrist, the pain level, the grading of the activities of daily living, the subjective satisfaction score, the World Health Organization Quality of Life (WHOQoL) questionnaire and radiological assessment. | 1,2,4,6 weeks, 3 months, 6 months, 1 year/ 1,2,4,6 weeks, 3 months, 6 months, 1 year |
| Azzopardi 2005 | Single-center, prospective randomized controlled trail | 27/27 | 72(8)/ 71(9) | Unstable, dorsally angulated, extra-articular fracture of the distal radius(AO–A3 or Frykman I and Frykman II | Supplementary percutaneous pinning | Cast | The range of movement and grip strength, radiological evaluation, and implications. | Clinical and radiological reviews were performed at one, two, and five weeks, after four months and at one year. |
| Howard 1989 | Single-center, prospective randomized controlled trail | 25/25 | 45.3/ 49.2 | Several displaced comminuted Colles’ fractures, severe displacement was defined as either 30° of dorsal angulation or more than 1 cm of radial shortening as compared with the normal side. | External fixation using a Medium-C-Hoffman fixator | Conventional manipulation and plaster | Anatomical results, functional results, complications, and cosmetic result | 2 weeks, 3 months, 6 months |
| Bartl 2014 | Multi-center, prospective randomized controlled trail | 86/88 | 75.3(6.7)/ 74.4(7.1) | Colsed, unstable intra-articular fracture of the distal radius according to the AO criteria (fracture types 23-C1 to C3) | Open reduction with volar locking plate fixation | Closed reduction and cast immobilization | Short Form 36 (SF-36) questionnaire and Arm, Shoulder and Hand (DASH), EuroWol-5 Dimensions (EQ-5D) score, | 3 months, 12 months |
| Arora 2011 | Single-center, prospective randomized controlled trail | 36/37 | 75.9(65–88)/ 77.4(65–89) | Unstable dorsally displaced distal radial fractures | Open reduction and internal fixation with a volar locking plate | Closed reduction and cast immobilization | Patient-Rated Wrist Evaluation (PRWE) score, the Disabilities of the Arm, Shoulder and Hand (DASH) score, the level of pain, the range of wrist motion, and the rate of complications. | Clinical evaluation and radiographs at 1 week, 6 weeks, 12 weeks, 6 months, and 12 months |
| Saving 2019 | Multi-center, prospective randomized controlled trail | 58/64 | 80(70–90)/ 78(70–98) | Dorsally displaced distal radial fractures | Volar locking plate fixation | Plaster | Patient-Rated Wrist Evaluation (PRWE) score, the Disabilities of the Arm, Shoulder and Hand (DASH) score, EuroWol-5 Dimensions (EQ-5D) score, range of motion, grip strength, radiographic outcomes, and complications | 3 months and 12 months |
| Sharma 2014 | Single-center, prospective randomized controlled trail | 32/32 | 52.39(9.05)/ 48.10(10.30) | Fractures of the distal radius (AO type B and C) | Volar locking plate fixation | Closed reduction and plaster cast application | The range of movement, grip strength, functional outcomes scores and radiological parameters. | 6 weeks |
| Martinez-Mendez 2018 | Single-center, prospective randomized controlled trail | 50/47 | 67(8)/70(7) | Displaced complex intra-articular distal radius fracture (AO type C) | Volar locking plate fixation | Closed reduction and plaster cast application | The range of movement, grip strength, functional outcomes scores (PRWE, DASH, VAS-pain), and radiological parameters. | 24 months |
DASH: disability arm shoulder hand score; EQ-5D: EuroWol-5 Dimensions; WHOQoL: Health Organization Quality of Life
Quality assessment
Quality assessment of the 10 included studies indicated that there was little bias in random sequence generation, but the high bias existed in performance bias. This is because the blinding of participants and personnel in the surgical treatment and conservative treatment is impossible (Figure 2 and 3).
Figure 2.
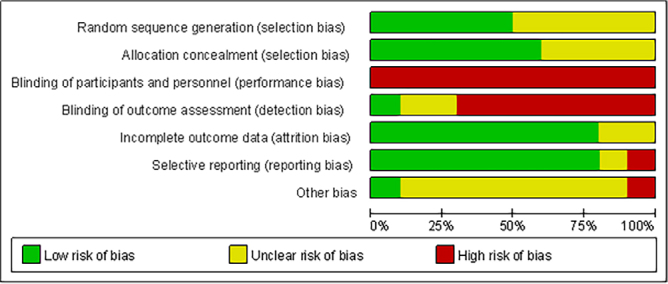
The graph shows the risk of bias graph
Figure 3.
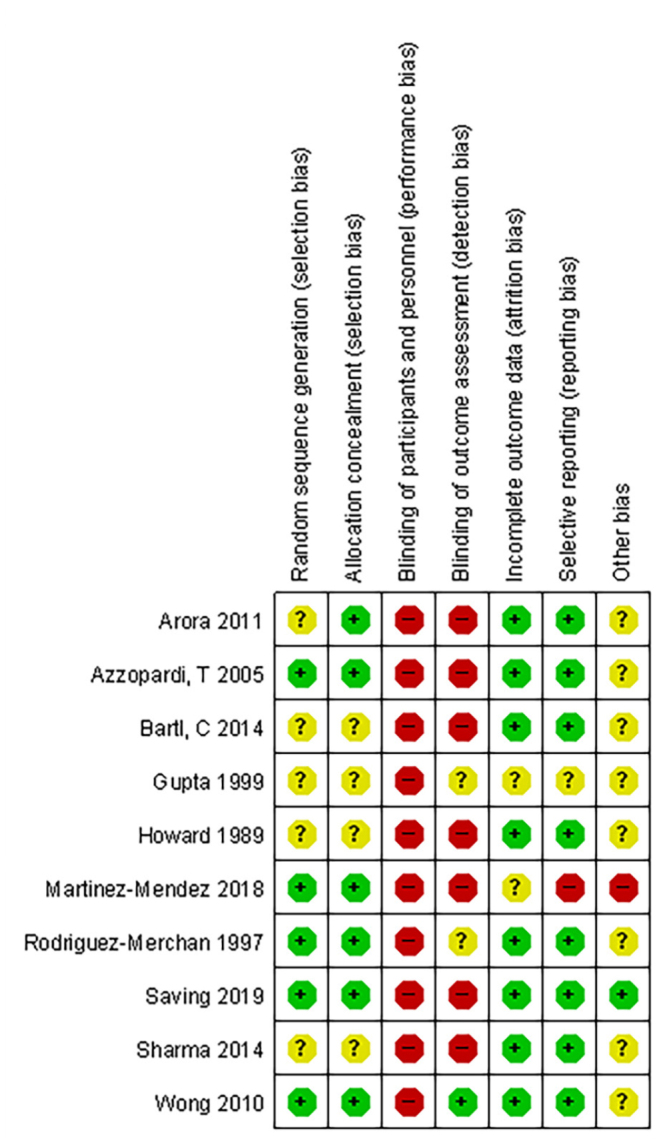
The graph shows the risk of bias summary
Effect of the Intervention
The primary outcome
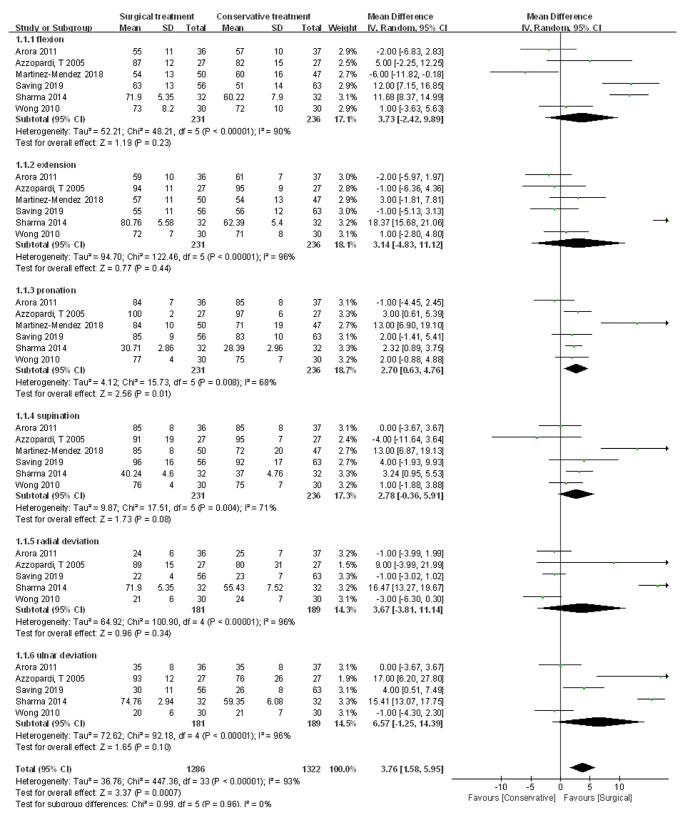
The mean range of movement
A total of 231 patients in the surgical treatment group and 236 patients in the conservative treatment group were available to compare the mean range of movement. Statistical heterogeneity was found between surgical treatment and conservative treatment in the mean range of movement, (I2=93%, Chi2=447.36, p<0.00001), and a random-effects model was used. Surgical treatment achieved a better range of movement compared with conservative treatment (MD 3.76, CI: 1.58 to 5.95, Z=3.37, p=0.0007) (Figure 4).
Figure 4.
The graph shows a forest plot of mean difference with a confidence interval for the active ranges of motion of the wrist
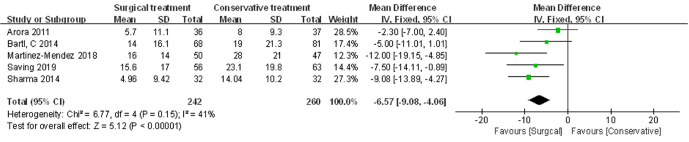
DASH score
A total of 242 patients in the surgical treatment group and 260 patients in the conservative treatment group were available to compare the DASH score. No statistical heterogeneity was found between surgical treatment and conservative treatment in the DASH score, (I2=41%, Chi2=6.77, p=0.15), and a fixed-effects model was used. Surgical treatment achieved better DASH scores as compared to conservative treatment (MD −6.57, CI: −9.08 to −4.06, Z=5.12, p<0.00001) (Figure 5).
Figure 5.
The graph shows a forest plot of mean difference with a confidence interval for DASH scores
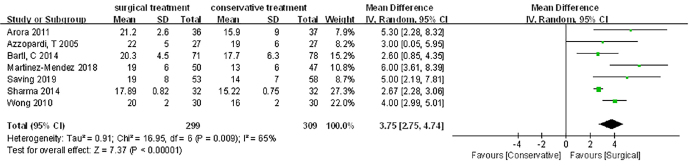
Radial inclination
A total of 299 patients in the surgical treatment group and 309 patients in the conservative treatment group were available to compare the radial inclination. Statistical heterogeneity was found between surgical treatment and conservative treatment in the radial inclination, (I2=65%, Chi2=16.95, p=0.009), and a random-effects model was used. The surgical treatment achieved better radial inclination as compared to conservative treatment (MD 3.75, CI: 2.75 to 4.74, Z=7.37, p<0.00001) (Figure 6).
Figure 6.
The graph shows a forest plot of mean difference with a confidence interval for radial inclination
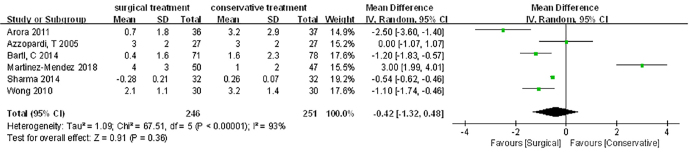
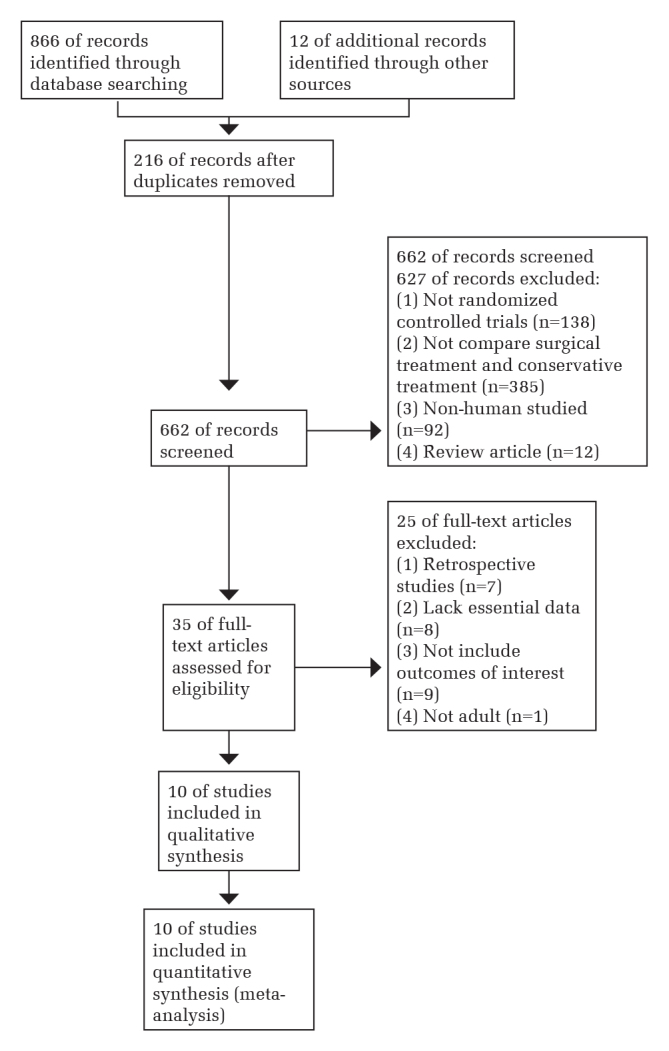
Ulnar deviation
A total of 246 patients in the surgical treatment group and 251 patients in the conservative treatment group were available to compare the ulnar deviation. Statistical heterogeneity was found between surgical treatment and conservative treatment in ulnar deviation, (I2=93%, Chi2=67.51, p<0.00001) (Figure 7), and a random-effects model was used. We found that the data of the Martinez-Mendez 2018 study were vastly different from other studies’ data. In figure 7, we can see that Martinez-Mendez 2018 study’s data are contrary to those of other studies. Therefore, we excluded the Martinez-Mendez 2018 study’s data. Surgical treatment achieved better ulnar deviation compared to conservative treatment (MD −1.00, CI: −1.59 to −0.41, Z=3.33, p=0.0009) (Figure 8).
Figure 7.
The graph shows a forest plot of mean difference with a confidence interval for ulnar deviation with random-effects including Martinez-Mendez 2018 study
Figure 8.
The graph shows a forest plot of mean difference with a confidence interval for ulnar deviation with random-effects excluding Martinez-Mendez 2018 study
The Secondary Outcome
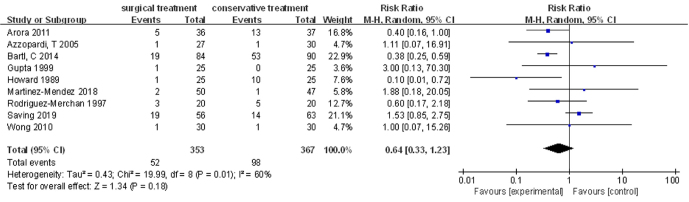
Complications did not include infections
A total of 353 patients in the surgical treatment group and 367 patients in the conservative treatment group were available to compare the complications like pain, angulated malunion, Sudeck’s atrophy, stiff joint, displacement, radial neuritis, median nerve compression, ulnar nerve compression, rupture of extensor pollicis longus, breakage of plates, extensor tenosynovitis, and flexor tendon rupture. However, this did not infection. Statistical heterogeneity was found between surgical treatment and conservative treatment in the complications, (I2=60%, Chi2=19.99, p=0.01), and a random-effects model was used. No significant difference was observed between surgical treatment and conservative treatment in complications. (MD 0.64, CI: 0.33 to 1.23, Z=1.34, p=0.18) (Figure 9).
Figure 9.
The graph shows a forest plot of relative risk with a confidence interval for complications
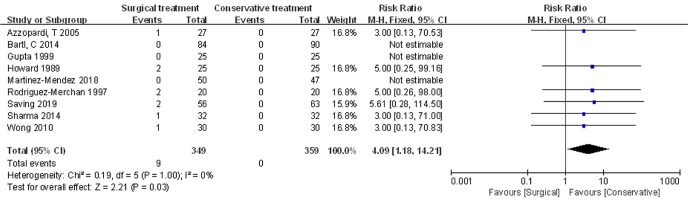
The infection
A total of 349 patients in the surgical treatment group and 359 patients in the conservative treatment group were available to compare the infection. No statistical heterogeneity was found between surgical treatment and conservative treatment in the infection, (I2=0%, Chi2=0.19, p=1.00), and a fixed-effects model was used. The conservative treatment achieved less infection compared to surgical treatment (MD 4.09, CI: 1.18 to 14.21, Z=2.21, p=0.03) (Figure 10). In terms of reducing infections, conservative treatment was superior to surgical treatment. In our meta-analysis, the infection included pin site infection, pin tract infection, and superficial wound infections. Most infections were superficial and responded to treatment by cleansing and antibiotics. One patient required the removal of K-wires after two weeks because of infection in the pin tracks in Azzopardi’s study.
Figure 10.
The graph shows a forest plot of relative risk with a confidence interval for infections
Discussion
In this study, the clinical functions and radiological parameters were better for surgical treatment compared with conservative treatment. The complications that did not include infection rates were similar. However, the infection rate is higher in surgical treatment.
Although there are 6 meta-analysis studies comparing surgical and nonsurgical treatments for DRFs, we find that there are new RCTs that they did not incorporate into their meta-analysis (24–27). Yu et al.’s meta-analysis found no significant difference between surgical and nonsurgical treatments in the wrist range of motion and radiographic parameters (27). In contrast, satisfactory radiographic outcomes were achieved with surgical treatment in Chen’s meta-analysis. Hence, Chen’s findings24 are different from theirs. Mellstrand Navarro et al. and Mulders et al. do not have the same endpoint as this meta-analysis (28, 29). Therefore, in order to establish whether surgical or conservative treatment is ideal for DRFs, we performed this meta-analysis.
For DRFs, closed reduction and cast immobilization treatment can be carried out nationwide without admission to the hospital at a low cost. Conservative treatment, such as an external support cast is a generally accepted treatment for extra-articular radial fracture, but the bone alignment may not be maintained. Surgical treatments like Kirschner-wire stabilization, external fixation, open reduction, and internal fixation with volar locked plating are common procedures that can be performed by orthopedic surgeons (30). In the study by Wang et al., they found that a volar locking plate could provide better results compared with external fixation (31). The use of volar locking plate appears to be associated with better DASH scores, ulnar variance, radial inclination, ulnar variance, ROM, and radiographic parameters. Although the meta-analysis of Yu et al. found no significant difference between surgical and nonsurgical treatments in the wrist range of motion and radiographic parameters, our findings are different from theirs (27). In our meta-analysis, we found that radiological results of surgical treatment are better than those of conservative treatment. Further, surgical treatment gained better functional outcomes in DASH score and radiographic parameters compared to conservative treatment. Surgical treatment allows patients to do gentle mobilization exercise without casting, and therefore, it is good for patients and may avoid later complications (32). The dislocated anatomical structure results in worse functional outcomes and DASH score of the conservative treatment group. Although patients who received conservative treatment slowly adapted to the new anatomical situations, the differences between surgical treatment and conservative treatment diminished during the long-term follow-up.
In our meta-analysis, we included adults. In children, a potential concern is the risk of physical injury, if pins must cross the growth plate to achieve stable fixation in pinning fractures of the distal radius (33). In the course of Miller’s investigation, they tried to establish an entry site proximal to the distal radial physis (20). In 2 children, this was not successful, and pins were fixed across the growth plate. However, there was no evidence of growth arrest at follow-up, and the fractures healed uneventfully (20). Although percutaneous K-wires have been widely used in children for the treatment of DRFs, their use in elderly population remains uncertain. Therefore, we did not include RCTs related to children.
Many studies support the opinion that K-wires do not gain sufficient purchase in elderly patients to maintain the anatomical reduction in osteopenic bone and to improve clinical functions (34). It has been suggested in many studies that there is a high correlation between the functional outcome and anatomical results in high-functioning and active young patients. Malunion of DRFs can result in unsatisfactory functional outcome and posttraumatic wrist arthrosis with a painful and deformed wrist. However, there are only few studies that support the goal of anatomical restoration of the articular surface and the radial length to achieve a satisfactory clinical functional outcome in an elderly population (35). However, volar locking plate fixation content surgical treatment has become the standard treatment. As clinical experience shows that elderly patients’ level of physical activity and perception of age have undergone a dramatic transformation in recent years, the treatment has to be oriented on the functional expectation of the individual patient. Egol et al. retrospectively compared the outcomes for elderly patients whose displaced DRFs were treated operatively with external fixation or plate fixation with those who underwent a conservative treatment (36). Open reduction and internal fixation with volar locked plating were associated with better radiographic results compared with plaster immobilization. There was a minor loss of reduction in the volar locking plate fixation group, and there were no malunions. Radial inclination, ulnar variance, and palmar tilt were significantly better in the volar locking plate fixation group compared to plaster immobilization group (36). The biomechanics of the volar locking plate fixation allows the oblique orientation of the distal screws to prevent collapse and displacement opposite the plate, provision of a buttress effect, and maintenance of anterior cortical continuity to prevent radius collapse.
We found that DASH scores were significantly better among patients who underwent surgical treatment. Chen et al.’s meta-analysis, which included retrospective studies, suggested that wrist function was better in the operative group, but the differences did not reach statistical significance (24). Hence, in our meta-analysis, surgical treatment seems to afford better functional outcomes and DASH scores.
Many surgeons doubt whether conservative treatment can even be recommended for complex intra-articular fractures. Most included studies permitted repeat reduction and continuation of conservative treatment when the position of the fragments was radiologically unfavorable, but this choice was rarely made. Many DRFs treated by conservative treatment show no relevant displacement and achieve good functional and life quality results. In our meta-analysis, although surgical treatment achieved better wrist joint mobility in general, no significant difference was observed between surgical treatment and conservative treatment in the extension, flexion, supination, radial deviation, and ulnar deviation in subgroup analysis. In addition, surgical treatment achieves better pronation, and conservative treatment achieves less infection. Although surgical treatment gained better radiological outcomes and DASH scores, currently, we cannot replace conservative treatment.
Most of the studies that we included followed up to 12 months; only 1 study followed up to 24 months. We look forward to seeing more RCTs follow up to 24 months for comparison of clinical functions of surgical treatment and conservative treatment in DRFs. As patients slowly adapt to the new anatomical situations in conservative treatment, the differences between surgical treatment and conservative treatment diminish in the long-term follow-up. As we only searched for published papers, we might have missed some unpublished papers.
In conclusion, the clinical functions and radiological parameters were better for surgical treatment compared with conservative treatment. Complications, other than infection rates, were similar. However, the infection rate was found to be higher in surgical treatment. Our results imply that surgical treatment is more efficient for DRF patients.
HIGHLIGHTS.
Different from other meta-analysis studies, our results imply a benefit for patients with a distal radial fracture to be treated with surgical treatment.
The clinical functions and radiological parameters were better for surgical treatment compared with conservative treatment.
The complication rates were similar. But the infection rate is higher in surgical treatment.
Footnotes
Ethics Committee Approval: N/A.
Informed Consent: N/A.
Author Contributions: Concept - Y.C.; Design - C.L., F.L., X.H.; Supervision - Y.C., C.L., X.L.; Materials - X.L., X.H.; Data Collection and/or Processing - C.L., X.H.; Analysis and/or Interpretation - X.H., Y.C.; Literature Review - F.L., C.L., X.H.; Writing - X.H.; Critical Review - Y.C., C.L., F.L., X.L.
Conflicts of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: This study was supported by Innovation Platform Projects of Science and Technology Program of Fuzhou (2019-S-wp3); Recipient: Fengfei Lin.
References
- 1. Körner D, Gonser CE, Bahrs C, Hemmann P. Change in paediatric upper extremity fracture incidences in German hospitals from 2002 to 2017: An epidemiological study. Arch Orthop Trauma Surg. 2020;140:887–94. doi: 10.1007/s00402-019-03321-5. [DOI] [PubMed] [Google Scholar]
- 2. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–7. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 3. Nguyen ND, Ahlborg HG, Center JR, Eisman JA, Nguyen TV. Residual lifetime risk of fractures in women and men. J Bone Miner Res. 2007;22:781–8. doi: 10.1359/jbmr.070315. [DOI] [PubMed] [Google Scholar]
- 4. Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989;20:208–10. doi: 10.1016/0020-1383(89)90113-7. [DOI] [PubMed] [Google Scholar]
- 5. Armstrong KA, von Schroeder HP, Baxter NN, Zhong T, Huang A, McCabe SJ. Stable rates of operative treatment of distal radius fractures in Ontario, Canada: a population-based retrospective cohort study (2004–2013) Can J Surg. 2019;62:386–92. doi: 10.1503/cjs.016218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Trevisan C, Klumpp R, Nava V, Riccardi D, Recalcati W. Surgical versus conservative treatment of distal radius fractures in elderly. Aging Clin Exp Res. 2013;25(Suppl 1):S83–4. doi: 10.1007/s40520-013-0075-0. [DOI] [PubMed] [Google Scholar]
- 7. Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A Prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011;93:2146–53. doi: 10.2106/JBJS.J.01597. [DOI] [PubMed] [Google Scholar]
- 8. Mattila VM, Huttunen TT, Sillanpää P, Niemi S, Pihlajamäki H, Kannus P. Significant change in the surgical treatment of distal radius fractures: A nationwide study between 1998 and 2008 in Finland. J Trauma. 2011;71:939–43. doi: 10.1097/TA.0b013e3182231af9. [DOI] [PubMed] [Google Scholar]
- 9. Wilcke MKT, Hammarberg H, Adolphson PY. Epidemiology and changed surgical treatment methods for fractures of the distal radius A registry analysis of 42,583 patients in Stockholm County, Sweden, 2004–2010. Acta Orthop. 2013;84:292–6. doi: 10.3109/17453674.2013.792035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mellstrand-Navarro C, Pettersson HJ, Tornqvist H, Ponzer S. The operative treatment of fractures of the distal radius is increasing results from a nationwide Swedish study. Bone Joint J. 2014;96-B:963–9. doi: 10.1302/0301-620X.96B7.33149. [DOI] [PubMed] [Google Scholar]
- 11. Schneppendahl J, Windolf J, Kaufmann RA. Distal Radius Fractures: Current Concepts. J Hand Surg Am. 2012;37:1718–25. doi: 10.1016/j.jhsa.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 12. Handoll HHG, Huntley JS, Madhok R. External fixation versus conservative treatment for distal radial fractures in adults. Cochrane Database Syst Rev. 2007;(3):CD006194. doi: 10.1002/14651858.CD006194.pub2. [DOI] [PubMed] [Google Scholar]
- 13. Hoaglin DC. Misunderstandings about Q and ‘Cochran’s Q test’ in meta-analysis. Stat Med. 2016;35:485–95. doi: 10.1002/sim.6632. [DOI] [PubMed] [Google Scholar]
- 14. Gupta R, Raheja A, Modi U. Colles’ fracture: Management by percutaneous crossed-pin fixation versus plaster of Paris cast immobilization. Orthopedics. 1999;22:680–2. [PubMed] [Google Scholar]
- 15. Rodriguez-Merchan EC. Plaster cast versus percutaneous pin fixation for comminuted fractures of the distal radius in patients between 46 and 65 years of age. J Orthop Trauma. 1997;11:212–7. doi: 10.1097/00005131-199704000-00013. [DOI] [PubMed] [Google Scholar]
- 16. Wong TC, Chiu Y, Tsang WL, Leung WY, Yam SK, Yeung SH. Casting versus percutaneous pinning for extra-articular fractures of the distal radius in an elderly Chinese population: a prospective randomised controlled trial. J Hand Surg Eur Vol. 2010;35:202–8. doi: 10.1177/1753193409339941. [DOI] [PubMed] [Google Scholar]
- 17. Azzopardi T, Ehrendorfer S, Coulton T, Abela M. Unstable extra-articular fractures of the distal radius - A prospective, randomised study of immobilisation in a cast versus supplementary percutaneous pinning. J Bone Joint Surg Br. 2005;87:837–40. doi: 10.1302/0301-620X.87B6.15608. [DOI] [PubMed] [Google Scholar]
- 18. Howard PW, Stewart HD, Hind RE, Burke FD. External fixation or plaster for severely displaced comminuted Colles’ fractures? A prospective study of anatomical and functional results. J Bone Joint Surg Br. 1989;71:68–73. doi: 10.1302/0301-620X.71B1.2915010. [DOI] [PubMed] [Google Scholar]
- 19. Bartl C, Stengel D, Bruckner T, Gebhard F, Group OS. The treatment of displaced intra-articular distal radius fractures in elderly patients. Dtsch Arztebl Int. 2014;111:779–87. doi: 10.3238/arztebl.2014.0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Miller BS, Taylor B, Widmann RF, Bae DS, Snyder BD, Waters PM. Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: a prospective, randomized study. J Pediatr Orthop. 2005;25:490–4. doi: 10.1097/01.bpo.0000158780.52849.39. [DOI] [PubMed] [Google Scholar]
- 21. Saving J, Wahlgren SS, Olsson K, et al. Nonoperative treatment compared with volar locking plate fixation for dorsally displaced distal radial fractures in the elderly a randomized controlled trial. J Bone Joint Surg Am. 2019;101:961–9. doi: 10.2106/JBJS.18.00768. [DOI] [PubMed] [Google Scholar]
- 22. Sharma H, Khare GN, Singh S, Ramaswamy AG, Kumaraswamy V, Singh AK. Outcomes and complications of fractures of distal radius (AO type B and C): Volar plating versus nonoperative treatment. J Orthop Sci. 2014;19:537–44. doi: 10.1007/s00776-014-0560-0. [DOI] [PubMed] [Google Scholar]
- 23. Martinez-Mendez D, Lizaur-Utrilla A, de-Juan-Herrero J. Intra-articular distal radius fractures in elderly patients: a randomized prospective study of casting versus volar plating. J Hand Surg Eur Vol. 2018;43:142–7. doi: 10.1177/1753193417727139. [DOI] [PubMed] [Google Scholar]
- 24. Chen Y, Chen X, Li Z, Yan H, Zhou F, Gao W. Safety and efficacy of operative versus nonsurgical management of distal radius fractures in elderly patients: A systematic review and meta-analysis. J Hand Surg Am. 2016;41:404–13. doi: 10.1016/j.jhsa.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 25. Ju JH, Jin GZ, Li GX, Hu HY, Hou RX. Comparison of treatment outcomes between nonsurgical and surgical treatment of distal radius fracture in elderly: A systematic review and meta-analysis. Langenbecks Arch Surg. 2015;400:767–79. doi: 10.1007/s00423-015-1324-9. [DOI] [PubMed] [Google Scholar]
- 26. Song J, Yu AX, Li ZH. Comparison of conservative and operative treatment for distal radius fracture: A meta-analysis of randomized controlled trials. Int J Clin Exp Med. 2015;8:17023–35. [PMC free article] [PubMed] [Google Scholar]
- 27. Yu GS, Lin YB, Le LS, Zhan MF, Jiang XX. Internal fixation vs conservative treatment for displaced distal radius fractures: A meta-analysis of randomized controlled trials. Ulus Travma Acil Cerrahi Derg. 2016;22:233–41. doi: 10.5505/tjtes.2015.05995. [DOI] [PubMed] [Google Scholar]
- 28. Navarro CM, Brolund A, Ekholm C, et al. Treatment of radius or ulna fractures in the elderly: A systematic review covering effectiveness, safety, economic aspects and current practice. PLoS One. 2019;14:e0214362. doi: 10.1371/journal.pone.0214362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mulders MAM, Detering R, Rikli D, Rosenwasser MP, Goslings JC, Schep NWL. Association between radiological and patient-reported outcome in adults with a displaced distal radius fracture: A systematic review and meta-analysis. J Hand Surg Am. 2018;43:710–9. doi: 10.1016/j.jhsa.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 30. Boydstun S, Nash L, Rayan GM. Distal Radius Fracture Fixation Devices and Their Radiographs. J Hand Surg Asian Pac Vol. 2019;24:412–20. doi: 10.1142/S2424835519500528. [DOI] [PubMed] [Google Scholar]
- 31. Wang J, Lu Y, Cui Y, Wei X, Sun J. Is volar locking plate superior to external fixation for distal radius fractures? A comprehensive meta-analysis. Acta Orthop Traumatol Turc. 2018;52:334–42. doi: 10.1016/j.aott.2018.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wollstein R, Harel H, Lavi I, Allon R, Michael D. Postoperative treatment of distal radius fractures using sensorimotor rehabilitation. J Wrist Surg. 2019;8:2–9. doi: 10.1055/s-0038-1672151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pritchett JW. Does pinning cause distal radial growth plate arrest? Orthopedics. 1994;17:550–2. doi: 10.3928/0147-7447-19940601-10. [DOI] [PubMed] [Google Scholar]
- 34. Huard S, Blanchet N, Leclerc G, et al. [Fractures of the distal radius in patients over 70 years old: Volar plates or K-wires?]. Chir Main. 2010;29:236–41. doi: 10.1016/j.main.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 35. DeGeorge BR, Jr, Houten HKV, Mwangi R, Sangaralingham LR, Larson AN, Kakar S. Outcomes and complications in the management of distal radial fractures in the elderly. J Bone Joint Surg Am. 2020;102:37–44. doi: 10.2106/JBJS.18.00561. [DOI] [PubMed] [Google Scholar]
- 36. Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima N. Distal radial fractures in the elderly: Operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010;92:1851–7. doi: 10.2106/JBJS.I.00968. [DOI] [PubMed] [Google Scholar]