Abstract
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) belongs to the genus Beta coronavirus and the family of Coronaviridae. It is a positive-sense, non-segmented single-strand RNA virus. Four common types of human coronaviruses circulate globally, particularly in the fall and winter seasons. They are responsible for 10%-30% of all mild upper respiratory tract infections in adults. These are 229E, NL63 of the Alfacoronaviridae family, OC43, and HKU1 of the Betacoronaviridae family. However, there are three highly pathogenic human coronaviruses: SARS-CoV-2, Middle East respiratory syndrome coronavirus, and the latest pandemic caused by the SARS-CoV-2 infection. All viruses, including SARS-CoV-2, have the inherent tendency to evolve. SARS-CoV-2 is still evolving in humans. Additionally, due to the development of herd immunity, prior infection, use of medication, vaccination, and antibodies, the viruses are facing immune pressure. During the replication process and due to immune pressure, the virus may undergo mutations. Several SARS-CoV-2 variants, including the variants of concern (VOCs), such as B.1.1.7 (Alpha), B.1.351 (Beta), B.1.617/B.1.617.2 (Delta), P.1 (Gamma), and B.1.1.529 (Omicron) have been reported from various parts of the world. These VOCs contain several important mutations; some of them are on the spike proteins. These mutations may lead to enhanced infectivity, transmissibility, and decreased neutralization efficacy by monoclonal antibodies, convalescent sera, or vaccines. Mutations may also lead to a failure of detection by molecular diagnostic tests, leading to a delayed diagnosis, increased community spread, and delayed treatment. We searched PubMed, EMBASE, Covariant, the Stanford variant Database, and the CINAHL from December 2019 to February 2023 using the following search terms: VOC, SARS-CoV-2, Omicron, mutations in SARS-CoV-2, etc. This review discusses the various mutations and their impact on infectivity, transmissibility, and neutralization efficacy.
Keywords: Variant of concern, SARS-CoV-2, Omicron, N501Y mutation, E484K mutation
Core Tip: The severe acute respiratory syndrome coronavirus-2 virus is constantly evolving because to natural immunity and vaccine-induced immunity which exert continual immunological pressure, resulting in the generation of newer variants and numerous new mutations. This study detailed the many variants of concern (VOCs), including their transmissibility, severity, and immune-evasion capacities. We have also discussed several key mutations and their consequences. The tables summarized the major points of the paper and provided a full discussion of the important mutations found in these VOCs. Readers will benefit from our article's concise overview of these areas.
INTRODUCTION
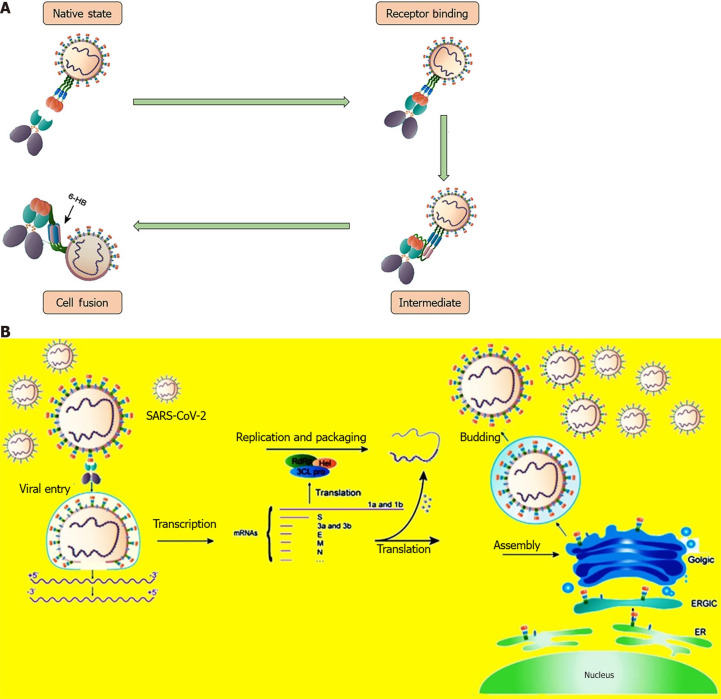
Variants are coronaviruses that have the same inherited set of very distinctive mutations[1]. It is worth noting that RNA viruses tend to have higher mutation rates than DNA viruses, and single-stranded viruses mutate quicker than double-stranded viruses[2]. However, the rate of mutations among the coronaviruses is lower than that of most RNA viruses. The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) acquires 2-3 single-nucleotide (nt) mutations in its genome per month. This is half the rate of influenza (4 nt/month) and one-fourth the rate of human immunodeficiency virus (8 nt/month) mutations[3,4]. The slow rate of mutation may be explained by the existence of a novel 3′-to-5′ exoribonuclease (ExoN) in nsp14, which serves as a proofreader and corrects some replication errors[5]. Genetic inactivation of this ExoN function causes a 15- to 20-fold rise in mutation rates[6]. When variants with various mutations infect the same host, they accumulate mutations and create diversity via recombination[7-9]. Human hosts may also contribute to the diversity via host-mediated RNA editing[10,11]. It is important to know that not every mutation will have a long-lasting effect on the virus. Typically, synonymous mutations are neutral, whereas non-synonymous mutations are persistent[12]. Wang et al[13] observed that in SARS-CoV-2, non-synonymous mutations are 14 times less likely to persist as weak deleterious mutations are slowly eliminated[13]. Mutations may increase infectivity, transmissibility, disease severity, and decreased neutralization efficacy by monoclonal antibodies (mAbs) and convalescent sera, as well as lower vaccine efficacy (VE). Moreover, a few variants may be responsible for negative results on the diagnostic tests. For example, with the Alpha and Omicron variants, there could be “S” gene target failure (SGTF)[14-16]. Delay in diagnosis increases the likelihood of viral transmission. The surface transmembrane spike (S) protein consists of S1 and S2 subunits. The S1 subunit has the N-terminal domain (NTD) and a receptor-binding domain (RBD) and it mediates the critical step of viral entry into the cell via interacting with the angiotensin-converting enzyme 2 (ACE2) receptor of the host cell[17]. The S1 subunit is also the primary target of neutralizing antibodies upon infection and various therapeutic and vaccines[18]. S2 mediates fusion of the viral and cellular membranes[19]. The RBD must be in an upright position to bind with ACE2 receptors and initiate the viral entry process. It is followed by the cleavage of S1/S2, which helps in membrane fusion (Figure 1A). The SARS-CoV-2 also enters in the cell by endosomal/lysosomal pathway. Inside the cell, the virus undergoes replication, translation, assembly, and exocytosis followed by viral release (Figure 1B). The most common site of mutation in SARS-CoV-2 is the spike protein, but it may involve other proteins as well. The diagnostic assays for SARS-CoV-2 are based on the two most abundant and immunogenic viral proteins, such as spike or nucleocapsid (N) proteins[20]. The spike protein contains sequences that are unique to the SARS-CoV-2 virus, thereby reducing the risk of cross-reactivity. However, spike protein has the highest potential to undergo mutation, and it has the potential to cause false-negative tests on immunoassays that are based only on detecting spike protein. Since N protein is less susceptible to mutations, it is the best target for developing diagnostic assays[20]. Recently, several variants of concern (VOCs) have been de-escalated. It will provide updated knowledge on the de-escalated status of various VOCs, subcategories, and VE. A detailed evaluation of the existing mutations and emerging mutations has been of immense help in studying their impact on transmissibility, severity, neutralization potency, and VE. This narrative review will provide an updated version of SARS-CoV-2 VOCs, associated mutations, the effect of mutations, and the present status of the VOCs in detail. Understanding the biological characteristics of the mutations will guide us in the surveillance, prevention, and control of coronavirus disease 2019 (COVID-19) infection.
Figure 1.
Showing the S protein mediated binding, fusion and various steps of severe acute respiratory syndrome coronavirus-2 infection cycle in the humans. A: Showing the S protein mediated binding and fusion with human cell; B: Showing the various steps in the severe acute respiratory syndrome coronavirus-2 infection cycle in human. It includes viral cellular entry, transcription, replication and packaging, translation, assembly within cellular organelle. SARS-CoV-2: Severe acute respiratory syndrome coronavirus-2; ER: Endoplasmic reticulum; ERCIC: ER-to-Golgi intermediate compartment; RdRP: RNA-dependent RNA polymerase; 3CLpro: 3C-like proteinase; Hel: Helicase.
SARSCOV2 VARIANT’S NOMENCLATURE SYSTEM
The SARS-CoV-2 interagency group (SIG) of the United States Department of Health and Human Services has classified the newly developing variations of SARS-CoV-2 into many groups. The SIG is responsible for better coordination among various United States departments and agencies, rapid characterization of emerging variants, and actively monitoring their potential impact on vaccines, therapeutics, and diagnostics[21]. Due to the lack of a standardized system, various nomenclature systems are in use. The Global Initiative on Sharing Avian Influenza Data, Nextstrain, and Phylogenetic Assignment of Named Global Outbreak (PANGO) are the most commonly used nomenclature systems by the scientific community worldwide[22]. The PANGO lineage system contains an alphabetical prefix and a suffix containing up to three numbers separated by periods indicating sub-lineages (such as B.1.1.7). Starting from high impact to low impact, SARS-CoV-2 variants may be classified as variants of high consequence, VOCs, variants of interest, and alerts for further monitoring. The VOC is characterized by increased transmissibility, a severe disease associated with an increased rate of hospitalizations or deaths, a significant reduction in neutralization by antibodies generated during previous infection or vaccination, reduced effectiveness of treatments or vaccines, or diagnostic detection failures[23].
TRANSLATIONAL SCIENCE
The COVID-19 pandemic has demonstrated the importance of translational research in pandemic control. Translational research encompasses a wide range of disciplines, including diagnostics, newer drug development, pathogenesis, epidemiology, and vaccine development. The COVID-19 pandemic has changed the traditional approach to clinical research[24].
NATURAL SELECTION AND IMMUNE IMPRINTING
Two phenomena play a significant role in the natural history of SARS-CoV-2 virus evolution. These include natural selection and immune imprinting. Animal experiments have confirmed the existence of natural selection. Lei et al[25] investigated the composition and codon use of the SARS-CoV-2 virus in infected humans and animals[25]. They reported the maximum mutations in mink. SARS-CoV-2 in mink showed that substitutions of cytidine contributed to approximately 50% of substitutions. The corresponding figure for other animals was 30%. However, the incidence of adenine transversion in SARS-CoV-2 in other animals is three times higher than in mink. They also found lower adaptability than humans in all other animals except for mink. Furthermore, a binding affinity analysis revealed that the spike protein of the SARS-CoV-2 variant in mink had a greater preference for binding with the mink receptor ACE2 than the human receptor, particularly with the mutations Y453F and F486L in mink SARS-CoV-2, which improved the binding affinity for the mink receptor. This study demonstrates that SARS-CoV-2's natural history in mink includes both natural selection and host adaptation. Similarly, Fu et al[26] showed that natural selection had a stronger influence on some SARS-CoV-2 sequences than mutational pressure[26]. The Y453F and N501T mutations in mink SARS-CoV-2 increased viral spike binding to the mink receptor. It confirmed the role of these mutations in natural selection and viral fitness. Natural selection favors the strains with beneficial mutations and reduces the number of strains with deleterious mutations[27]. However, it is still unclear whether natural selection occurred first in an animal host before zoonotic transfer or whether natural selection occurred in humans after zoonotic transfer[28]. Rubio-Casillas et al[29] coined the term “intermittent virulence”, which is basically an evolutionary equilibrium between transmissibility and virulence[29]. They considered this phenomenon to be due to natural selection. Habib et al[30] scanned the RBD of the Omicron spike protein for adaptive evolution based on a public database in Bangladesh[30]. It was reported that the adaptive mutations in the RBD domain were characterized by a non-synonymous to synonymous nt substitution rate of more than one. This indicates a positive selection. Some of the adaptive sites mediate increased viral fitness. Immune imprinting is the mechanism by which memory B lymphocytes induced by an initial viral infection prevent the development of B cells in response to a subsequent infection with a novel but related virus[31]. Chemaitelly et al[32] conducted a retrospective cohort study in Qatar to compare the incidence of SARS-CoV-2 reinfection in persons who had received primary-series (two-dose) vaccination, no vaccination, or booster (three-dose) vaccinations[32]. They found that a history of primary-series immunization enhanced immune protection against omicron reinfection, whereas a history of booster vaccination compromised protection against omicron reinfection. In the future, a study elucidating the pathogenetic mechanism behind the phenomenon of immune imprinting may provide useful insights for creating a more effective vaccine against the SARS-CoV-2 virus. In addition, we should not forget the short-term public health benefits of vaccination.
VOC
Several VOCs have been identified, and they differ from one another in terms of infectivity, transmissibility, severity, therapeutic efficacy, and neutralization efficacy by mAbs, convalescent sera, or vaccines. These are B.1.1.7 (Alpha), B.1.351 (Beta), B.1.617/B.1.617.2 (Delta), P.1 (Gamma), and B.1.1.529 (Omicron). The European Center for Disease Prevention and Control declared a new category in July 2021 as de-escalated variants. These VOCs have been de-escalated because they are either not circulating or, if they are, have no epidemiological impact. Moreover, they are not associated with any concerning properties[33].
Alpha (B.1.1.7 lineage) VOC
The B.1.1.7 variant was the first VOC to be detected in southeast England in September 2020. It eventually became the dominant variant in the United Kingdom and many other countries due to its increased transmissibility[33]. The B.1.1.7 variant was found to be 50%-75% more transmissible than the origin lineage, with a R0 value that was 1.75 times higher[34]. Another feature is the increased disease severity compared to the pre-existing SARS-CoV-2 variants of that time. Davies et al[35] had shown that the hazard of death with SGTF was 55% (95%CI: 39%–72%) higher than that in cases without SGTF after adjustment for age, sex, ethnicity, deprivation, care home residence, local authority of residence, and test date[35]. The B.1.1.7 variant's higher transmissibility is due to the presence of the N501Y mutation and Deletion69/Deletion70, which increase binding affinity to ACE2[36,37]. Other characteristics include SGTF due to mutations in the S gene and no change in susceptibility to monoclonal antibody therapy such as Bamlanivimab-etesevimab, casirivimab-imdevimab, and sotrovimab[38-40]. However, E484K and/or other NTD mutations (especially deletions) may result in a considerable reduction in neutralizing efficacy[41]. The ChAdOx1 nCoV-19 (AstraZeneca) vaccine showed an efficacy of 70.4%[42]. The first and second doses of the BNT162b2 vaccine (Pfizer–BioNTech) reported 48.7% and 93.7% effectiveness, respectively[43]. The reported efficacy of two doses of the mRNA-1273 (Moderna) vaccine was 98.4%[44].This variant has been de-escalated[33].
Beta (B.1.351) VOC
Tegally et al[45] detected this variant, also known as 501Y.V2, in late 2020 in the Eastern Cape, South Africa[45]. The beta variants also show increased transmissibility, similar to the B.1.1.7 variants. In comparison to the alpha and gamma versions, this variant increased the likelihood of hospitalization, intensive care unit (ICU) admission, and mortality. However, it causes less severe disease than the delta variant[46]. These variants also show immune-evasion properties. There was a 45-fold decrease in susceptibility to Bamlanivimab-etesevimab therapy; however, casirivimab-imdevimab and sotrovimab retained susceptibility[38-40]. Furthermore, beta versions demonstrate lower neutralization by convalescent and post-vaccination sera[47]. In a systematic review and meta-analysis, Zeng et al[48] assessed 11 COVID-19 vaccines (BNT162b2, mRNA-1273, ChAdOx1, Ad26.COV2.S, BBV152, CoronaVac, NVX-CoV2373, BBIBP-CorV, CVnCoV, SCB-2019, and HB02) and reported full vaccination efficacy against Alpha, Beta, Gamma, Delta, and Omicron variants of 88.0% (95%CI: 83.0%–91.5%), 73.0% (95%CI: 64.3%–79.5%), 63.0% (95%CI: 47.9%–73.7%), 77.8% (95%CI: 72.7%–82.0%), and 55.9% (95%CI: 40.9%–67.0%), respectively[48]. The efficacy of booster vaccination was higher against Delta and Omicron variants, 95.5% (95%CI: 94.2%–96.5%) and 80.8% (95%CI: 58.6%–91.1%), respectively. They also reported a higher efficacy of mRNA vaccines (mRNA-1273/BNT162b2) against VOC over others.
Gamma (P.1; GR/501Y.V3)
The P.1 variant was first reported from Japan on January 6, 2021, by four people who had arrived in Tokyo after visiting Amazonas, Brazil[49]. Faria et al[50] further published the genomic and epidemiological analysis of this Brazilian variant from Manaus[50]. They reported 17 mutations in the P.1 variants, including three in the spike protein RBDs (K417T, E484K, and N501Y). These mutations caused enhanced binding to the human ACE2 receptor. The P.1 variant is 1.7 to 2.4 times more transmissible than the previous (non-P.1) infection. Infection with P.1 is also 1.2 to 1.9 times more likely to cause mortality than previous lineages[50]. This variant also possesses immune evasion properties. Although the P.1 variant retained susceptibility to Casirivimab-imdevimab and Sotrovimab, there was a 511-fold decrease in susceptibility to Bamlanivimab-etesevimab[38-40]. This variant has been deescalated. Full vaccination efficacy against the gamma variants was 63.0%[48].
Delta (G/478 K.V1; B.1.617.2)
The B.1.617.2 variant was first identified in India in October 2020 and quickly became the dominant variant in India and globally until the emergence of the Omicron variant. This variant was 40%-60% more transmissible than the B.1.1.7 variant and almost twice as transmissible as the original Wuhan strain[51]. The B.1.617 variant has three sublineages: B.1.617.1, B.1.617.2, and B.1.617.3. The B.1.617.2 variants show increased transmissibility and replication advantages. This variant shows 1260-fold higher viral loads than those for the 2020 infections with clade 19A/19B viruses. It makes the person more infectious[52]. Compared to the B.1.1.7 cases, the B.1.617 variant is associated with an increased severity of the disease[53,54] and an increased risk of hospitalization[54,55]. The common signature mutations located in the spike protein are D111D, G142D, L452R, E484Q, D614G, and P681R. The L452R, E484Q, and P681R mutations contribute to increased transmissibility, and the E484Q and P681R mutations influence antibody binding. Neutralization by mAbs is affected minimally. Although there is a moderate reduction in VE against symptomatic COVID-19 infection, efficacy against severe disease and hospitalization showed no significant impact[47]. The 2-dose mRNA-1273 vaccine showed 86.7% (95%CI: 84.3%- 88.7%) efficacy against infection and 97.5% (95%CI: 92.7%-99.2%) efficacy against hospital admission with the B.1.617.2 variant[44]. However, VE decreased from 94.1% at 14-60 d after immunization to 80.0% at 151-180 d following vaccination. The efficacy of 2-doses of BNT162b2 and ChAdOx1 nCoV-19 vaccines was 88.0% (95%CI: 85.3%-90.1%) and 67.0% (95%CI: 61.3%-71.8%) among those with the delta variant, respectively[43]. Effectiveness after one dose of vaccine with both BNT162b2 and ChAdOx1 nCoV-19 vaccine was notably lower among persons with the delta variant (30.7%; 95%CI: 25.2%- 35.7%).
Omicron (B.1.1.529 lineage) variant
The Omicron variant was initially reported from Botswana and then from South Africa. Very soon, it became the dominant variant globally. The World Health Organization classified it as VOC on November 26 and named it Omicron[56]. Subsequently; several sublineages of the SARS-CoV-2 variant were identified. These are BA.1, BA.2, BA.4/BA.5, BA.4.6 (BA.4), BA.2.75.2 (BA.2), BQ.1/BQ.1.1 (BA.5), and XBB/XBB.1/XBB.1.5 (BA.2.10.1 and BA.2.75 recombinant) sublineages[47]. TheBA.4 and BA.5 sublineages have identical spike proteins similar to BA.2 except for the addition of 69-70 deletions, L452R, F486V, and the wild-type amino acid at Q493[57]. However, other sublineages differ from the others by at least one spike protein mutation[58]. Typical features of Omicron variants are high transmissibility, increased risk of reinfection or breakthrough infection, less severe disease compared to delta variants, and reduced or absent neutralization efficacy by vaccines and monoclonal antibody therapies. The Omicron variant is heavily mutated, as it contains up to 59 mutations in its genome, including 36 occurring within the spike protein and more than 30 involving the RBD[58,59]. The Omicron variant has a replication advantage over the B.1.617.2 variant, with the basic reproduction number (R0) exceeding 3[60,61]. The high R0 is the result of both higher transmissibility and immunological evasion. Compared to the earlier surge, hospitalized patients with the B.1.1.529 variant in Tshwane, Gauteng Province, South Africa, showed lower rates of ICU admissions (1% vs 4.3%, P < 0.00001), in-hospital death (4.5% vs 21.3%, P < 0.00001), and length of hospital stay (4.0 d vs 8.8 d)[62]. Omicron sublineages show immune evasion properties. Yue et al[62] reported that Omicron subvariant XBB.1.5 was more transmissible than other XBB sublineages[62]. This subvariant XBB.1.5 has an additional Ser486Pro substitution. The authors demonstrated a higher ACE2-receptor binding affinity and significant immune evasion in convalescent plasma. Moreover, Bebtelovimab showed no neutralization effect against the XBB.1/XBB.1.5 subvariant[63]. Similarly, Sotrovimab, Tixagevimab-cilgavimab, and Casirivimab-imdevimab remain inactive against the XBB/XBB.1/XBB.1.5 sublineages[47]. The mAbs resistant in B.1.1.529 variants may be explained by the presence of the following mutations: K417N, N440K, G446S, S477N, T478K, E484A, Q493R, G496S, Q498R, N501Y, S371L, and Y505H, which are located within or close to the epitopes targeted by these antibodies. The Omicron variety (B.1.1.529 lineage) also has SGTF, which causes a delay in diagnosis and increases the risk of infection transmission. However, the BA.2 lineage does not show SGTF due to a lack of deletions in positions 69-70[64]. The above-mentioned monoclonal antibody cocktails should not be used against the B.1.1.529 variants[65]. Mass vaccination is a crucial public health intervention that lowers COVID-19-related hospitalization and mortality. However, the duration of protection wanes over time. Wu et al[66] in a meta-analysis, studied the long-term efficacy of COVID-19 vaccinations against infection, hospitalization, and mortality up to 307 d after completion of the primary vaccination series and 139 d after a first booster vaccination[66]. They reported a vaccine effectiveness of 83% against infection, 92% against hospitalization, and 91% against mortality after the primary COVID-19 vaccination. However, the efficacy decreased over time. The VE against the omicron sublineages was 61% and 71% against infection and hospitalization, respectively. However, a booster dose increased the vaccine effectiveness against the omicron variant to 67% against infection and 89% against hospitalization. Andrews et al[67] reported a decreased efficacy of the vaccine against the omicron variant compared to the delta variant[67]. The two doses of ChAdOx1 nCoV-19 (AstraZeneca) showed no efficacy against the symptomatic disease caused by the Omicron. The VE of 2-dose BNT162b2 doses and the mRNA-1273 vaccine were 65.5% (95%CI: 63.9%-67.0%) and 75.1% (95%CI: 70.8%-78.7%), respectively. However, efficacy decreases over time. Among patients who received ChAdOx1 nCoV-19 as the primary vaccine, a BNT162b2 and mRNA-1273 booster dose increased the efficacy to 62.4% (95%CI: 61.8%-63.0%) and 70.1% (95%CI: 69.5%-70.7%), respectively. Booster doses are required to mount a more appropriate immune response against omicron infection[46]. Among patients who received BNT162b2 as primary vaccine, a BNT162b2 booster dose increased the efficacy to 67.2% (95%CI: 66.5%-67.8%). The BNT162b2 vaccine showed an efficacy of 70% against hospitalization[68]. Table 1 shows the characteristic features of various VOCs.
Table 1.
Showing characteristic features of various variants of concerns
|
VOCs
|
Transmissibility
|
Severity
|
Effect on neutralization by mABs
|
SGTF
|
Present status
|
Vaccine efficacy
|
|
| Alpha | Increased transmissibility (50%-100%) with R0 1.75-fold higher compared to original lineage[32] | Increased severity. Hazard of death of 55% (95%CI: 39%–72%) higher than in cases without SGTF after adjustment[33] | No impact on neutralization by mABs, and minimal impact by convalescent and/or post-vaccination sera[18]. E484K and/or various NTD mutations cause a significant fall in neutralization efficacy[39] | Presence | De-escalated | The ChAdOx1 nCoV-19 vaccine showed an efficacy of 70.4%[40]. The first and second dose of BNT162b2 vaccine (Pfizer–BioNTech) reported 48.7% and 93.7% effectiveness, respectively[41]. The reported efficacy of 2-doses of mRNA-1273 vaccine 98.4%[42] | |
| Beta | Increased transmissibility | Increased risk of hospitalization, ICU admission, and mortality in comparison to Alpha and Gamma variants, but less severe disease compared to Delta[44] | 45-fold decreased susceptibility to Bamlanivimab-etesevimab therapy. Casirivimab-imdevimab and sotrovimab retained susceptibility[38-40]. Moderate reduction in neutralization by convalescent and post-vaccination sera[45] | Absent | De-escalated | Full vaccination efficacy 73.0% (95%CI: 64.3%–79.5%)[46] | |
| Gamma | 1.7 to 2.4-fold higher transmissible than previous (non-P.1) infection[48]. Increased risk of reinfection | 1.2 to 1.9 times more likely to result in mortality compared with previous lineages[48] | > 511 fold decreased susceptibility to Bamlanivimab-etesevimab but no change in susceptibility with Casirivimab-imdevimab and Sotrovimab[38-40]. Reduced neutralization to convalescent and post-vaccination sera |
Absent | De-escalated | Full vaccination efficacy against Gamma variants 63.0% (95%CI: 47.9%–73.7%)[46] | |
| Delta | 40%-60% more transmissible than Alpha variant[49] | Increased severity of the disease[51,52] and increased risk of hospitalization[52,53].A shorter time interval between disease onset to hospitalization in comparison to the wild-type variant[44] | Neutralization is affected minimally | Absent | De-escalated | Moderate reduction in vaccine efficacy against symptomatic infection but retained efficacy against severe disease and hospitalization[45]. The 2-dose mRNA-1273 vaccine: 86.7% (95%CI: 84.3%-88.7%) efficacy against infection and 97.5% (92.7%-99.2%) efficacy against hospital admission. The 2-doses of BNT162b2 and ChAdOx1 nCoV-19 vaccine 88.0% (95%CI: 85.3%-90.1%) and 67.0% (95%CI: 61.3%-71.8%), respectively[41] | |
| Omicron | Increased risk of transmissibility, reinfection/breakthrough infection | Severity less compared to Delta variant | Reduced or absent neutralization efficacy by vaccines and mABs[56] | SGTF except BA.2 lineage[64] | Few sublineages de-escalated (BA.1, BA.2, BA.3, BA.4, BA.5 etc.) | Booster doses are needed to mount a more appropriate immune response against symptomatic or non-symptomatic infections, transmission, and serious manifestations[44] | |
VOCs: Variants of concerns; SGTF: “S” gene target failure; ICU: Intensive care unit; mAbs: Monoclonal antibodies; NTD: N-terminal domain.
COMMON MUTATIONS AND THEIR IMPACTS
D614G mutation
Genomic surveillance of SARS-CoV-2 during the first year of the COVID-19 pandemic revealed that the D614G mutation in the spike glycoprotein (Spike protein) was the predominant mutation in February 2020[69,70]. Later on, it spreads globally. The D614G mutation is caused by an aspartic acid-to-glycine substitution at position 614 of the spike glycoprotein. The D614G change is also associated with three other mutations: A, C-to-T mutation in the 5′ untranslated region (5’-UTR), a silent C-to-T mutation at position 3037, and a C-to-T mutation at position 14408, which causes an amino acid change in RNA-dependent RNA polymerase (RdRp)[70]. The D614G-mutated variants almost always carry these three mutations. Remdesivir targets the RdRp enzyme. Plante et al[71] examined the replication kinetics of the D614G variants in human lung epithelial cells (Calu-3 cells) and primary human airway tissues[71]. They found 2.4-fold more infectious virus at 36 hpi, indicating that the D614G mutation enhanced viral replication. Similarly, the golden Syrian hamster model infected with the D614G mutation produced higher infectious viral titers in the nasal washes and trachea but not in the lungs[71,72]. As a result, the D614G mutation may enhance viral loads in COVID-19 patients' upper respiratory tracts, increasing transmission. Korber et al[70] reported a lower real-time reverse transcription–polymerase chain reaction assay cycle threshold, which suggests higher viral loads and high infectivity[70]. However, the mechanism underlying improved replication fitness is unclear. Few studies have reported that increased cleavage efficiency of the spike protein into S1/S2 influences the SARS-CoV-2 infection[73,74]. However, Plante et al[71] observed no substantial differences in spike cleavage between the D614 and G614 virions, indicating that the enhanced infectivity is unlikely due to a D614G-mediated spike cleavage difference[71]. Another mechanism could be the disruption of the interprotomer latch between S1 and S2. Normally, the carboxyl groups in D614 form a hydrogen bond with the hydroxyl group in Thr859 across the S1/S2 interface[70]. The cryo-EM studies had shown that D614G disrupts the interprotomer latch between D614 in S1 and T859 in S2 and promotes the RDB domain to an “up” or open conformation and a higher chance of binding with the human ACE2 receptor. The ratio of closed and open conformation in D614 and G614 is 82% and 18%, and 42% and 58%, respectively[75]. Kannan et al[76] suggested that D614G alone would not be able to explain the high infectivity of the SARS-CoV-2 virus, and other coexistence mutations such as P323L (nsp12) and C241U (5’-UTR) and nsp mutations may also contribute to the infectivity[76]. D614G, by increasing the number of spike proteins per virion, may also be responsible for the increased infectivity[77,78]. However, since the 614 position lies outside the RBD, this mutation does not alter the affinity of spike protein to ACE2. Zhang et al[79] hypothesized that increased stability of the S-trimer in the presence of the D614G mutation may explain the enhanced infectivity as the S1 subunit dissociates more readily from the virus with an aspartic acid residue at position 614 than the virus having glycine at position 614[79]. The D614G mutation has been detected in B.1.1.7, B.1.351, P.1, and B.1.617.2 and B.1.1.529 lineages, indicating a transmission advantage of this mutation. However, it does not cause immune escape. Garcia-Beltran et al[80] had shown that the sera from convalescent individuals showed effective cross-neutralization of both wild type and D614G variants[80].
N501Y mutation
It includes replacing the amino acid asparagine (N) with tyrosine (Y) at position 501. The N501Y mutation has been identified in the B.1.1.7, B.1.351, P.1, and B.1.1.529 lineages. This mutation can alternatively be represented as S: N501Y, indicating that it occurs in the spike protein. The N501Y mutation is responsible for higher binding affinity to human ACE2 receptors, but has no impact on immune escape mechanisms[81]. Luan et al[82] in an in-silico study, had similarly shown that the N501Y mutation can increase the spike protein’s receptor binding affinity with the human ACE2 receptor[82]. The N501Y mutation on RBD may produce an aromatic ring-ring contact and an extra hydrogen bond with ACE2 receptors, increasing binding affinity by tenfold over the wild strain[83]. Moreover, the N501Y mutation decreases the polarity of critical residues located in RBD, thereby increasing the affinity between RBD and ACE2 receptors[84,85]. Zhu et al[86] reported that a higher number of ACE2 receptors bind with N501Y spikes as compared to N501[86]. Furthermore, using cryo-electron microscopy, the N501Y was placed into a cavity at the binding contact at Y41 of ACE2.This provides a structural basis for the N501Y mutant's higher ACE2 affinity, which is likely related to its greater infectivity. Teruel et al[87] in a modeling analysis demonstrated that D614G and N501Y mutations allow the RBD to remain in open conformation for a longer period of time[87]. However, large structural changes in the antibody-binding epitopes do not occur as the N501 is located outside the major neutralizing epitopes on the RBD[88]. Therefore, the N501Y mutation causes only minimal changes in the sensitivity to neutralizing antibodies. The N501Y mutation co-occurs with several other mutations, such as P681H and deletion of the amino acid at the 69th and 70th residues (Deletion69/Deletion70) on the spike protein. Leung et al[89] reported that the N501Y lineage with amino acid deletion Deletion69/Deletion70, detected among the United Kingdom strain, was 75% (70%–80%) more transmissible than the N501 lineage[89]. However, the N501Y mutation does not impact the binding and neutralization of most mAbs[90-95]. Similarly, it rarely shows reduced susceptibility to convalescent plasma[37,92-94].
E484K mutations
The E484K mutation is situated in the RBD and is critical for ACE2 receptor binding and antibody recognition. The E484K mutation has been detected in the B.1.1.7, B.1.351, P.1, and B.1.617.2 variants[53,95]. It involves the replacement of the amino acid glutamic acid (E) with lysine (K) at position 484 of the spike protein. The E484K mutation is an escape mutation, which permits the virus to slip past the body's immunological defenses[95]. Collier et al[96] observed that the B.1.1.7 variant carrying the E484K mutation increased the amount of serum antibody needed to prevent infection of cells substantially[96]. The E484K mutations reduce neutralization by antibodies and may cause breakthrough infections[41,95]. The E484 mutation with amino acid changes to K, Q, or P reduces neutralization by convalescent sera by more than an order of magnitude. Greaney et al[97] reported that the E484 mutation with K, Q, or P reduces the neutralization titer of the convalescent plasma collected from the subject on day 32 by 35 to 115-fold[97]. They also found that each of the four discovered mutations (E484A, E484D, E484G, and E484K) conferred resistance to all four convalescent sera tested. The E484 mutation is notable for causing the most significant decreases in neutralization titers. On the other hand, the K444E, G446V, L452R, and F490S mutations escaped three of the four sera tested. The G446V mutation caused approximately a 30-fold decrease in the neutralization titer. By co-incubating the pseudovirus with SARS-CoV-2 spike proteins and mAbs, Liu et al[98] demonstrated that that the E484 mutations resulted in considerably lower neutralization efficacy by both mAbs and convalescent sera[98]. Nelson et al[99] in a molecular dynamic simulation study, reported that the combination of E484K, K417N, and N501Y mutations resulted in the highest degree of conformational alterations of the RBD domain when bound to ACE2, compared to either E484K or N501Y alone[99]. These mutations favor ACE2 receptor binding. Zahradník et al[100] used an in vitro evolution model and found that S477N, E484K, and N501Y mutations were among the first to be selected[100]. Moreover, the E484K and N501Y mutations are the tightest binding mutations emerging from the B3 library. Wang et al[101] reported that E484K, N501Y individually, or K417N/E484K/N501Y mutations together showed a small but significant reduction in neutralization efficacy with Moderna and Pfizer-BioNTech vaccines[101].
L452R and E484Q mutations
Due to the presence of these two prominent mutations at the same location, it was initially called a “double mutant”. The L452R and E484Q are also the key mutations in the B.1.617.2 variants. The L452R and E484Q double mutants are the two-spike protein RBD mutations and have been detected in 15% to 20% of positive cases in the Maharashtra state of India on March 24, 2021, by the Indian SARSCoV-2 Consortium on Genomics[102]. The L452R and E484Q mutations are responsible for the overall stability of virus-host interaction[103]. They are also responsible for resistance to neutralization by monoclonal and polyclonal antibodies. In the pseudovirus-based study, the L452R mutation caused more cellular entry compared with that of the D614G mutation alone, but it was lower than the N501Y mutation[104]. The L452R mutation raised spike protein expression (0.32 times) and improved binding affinity to ACE2 receptors. It increases the virus's infectivity[84]. The L452R mutation also allows immune escape from human leukocyte antigen (HLA)-restricted cellular immunity[105].
P681R mutation
The furin cleavage site is located at the spike S1/S2 junction. The cleavage of this region is the key to host cell entry. This mutation is responsible for efficient furin cleavage, subsequent internalization, and better transmissibility. A unique feature of the B.1.617.2 variant is the P681R mutation in the spike protein, where proline is substituted by arginine. The P681R mutation is located adjacent to the furin cleavage site[106]. The P681R mutation makes the sequence less acidic and causes furin to function more effectively[51]. Increased furin cleavage will make more spike proteins primed to enter human cells. In the Delta variant, more than 75% of the spikes are primed to infect a human cell, whereas the values in the Alpha variant and original strain were 50% and 10%, respectively[107]. The P681R mutation is highly conserved in the B.1.617.2 variant and is responsible for the higher pathogenicity of the B.1.617.2 variant[108]. P681R mutation in the B.1.617.2 variant enhances SARS-CoV-2 fitness. In an experimental study, Liu et al[109] reported that the B.1.617.2 variants outnumbered other variants based on a replication competition assay done on human lung epithelial cells and primary human airway tissues[109]. The mechanism of increased infectivity was explained by the accumulation of the P681R mutation in the B.1.617.2 variant, which causes furin cleavage of the S1/S2 protein, leading to increased infectivity. Moreover, reverting the P681R mutation to wild-type P681 significantly reduced replication.
P681H mutation
The P681H mutation involves the substitution of proline (P) with histidine (H) at position 681. The P681H mutation is also near the S1/S2 furin cleavage site that is responsible for efficient SARS-CoV-2 transmission and infection[85,110]. The P681H mutation may also reduce class 3 antibody recognition[111].
T478K mutation
The T478K mutation is found within the critical receptor binding motif of S gene[112]. It alters the virus's affinity for human cells, increasing viral infectivity. The T478K mutation is a shift in amino acid from polar, uncharged threonine (T) to basic, charged lysine. It may raise the electrostatic potential of spike protein, resulting in a more positive surface in an area that directly contacts ACE2. Furthermore, the longer side chain of lysine is expected to exacerbate the mutant's steric hindrance, perhaps altering the spike/ACE2 interaction[113]. The T478K mutation is frequently co-occurring with three other spike mutations located outside the canonical ACE2 interaction regions, such as D614G (99.83% co-occurrence), P681H, and T732A, with 93.8% and 88.7% co-occurrence with T478K, respectively[114].
N439K mutations
This mutation was identified in March 2020 in Scotland from lineage B.1 on the background of D614G. It has also appeared independently in multiple lineages. As of January 6, 2021, it was reported in 34 countries and was the second most commonly observed RBD mutation worldwide[115]. N439K enhances the binding affinity for the ACE2 receptor and is also responsible for immune evasion. The N439K mutation confers resistance against several neutralizing monoclonal and polyclonal antibodies[116]. The N439K mutation located in the RBD region creates a strong salt bridge with ACE2 receptors, which may enhance the electrostatic complementarity and binding affinity of spike proteins to ACE2[117].
Y453F mutations
The Y453F mutation is located on the RBD and has been detected in human and mink infections. The bidirectional transmission has been reported in the Netherlands[118,119]. Initially, in Denmark, one new lineage was identified and was known as “Cluster 5” and contained mutations in the spike protein[120]. Later on, the mutation was identified as a Y453F mutation located in the RBD domain[121]. The Y453F mutation enhances binding to ACE2. The Y453F mutations involve a tyrosine-to-phenylalanine substitution at amino acid 453 (Y453F). Y453F mutation significantly lowers susceptibility to casirivimab (74-fold), but not to other Food and Drug Administration/Emergency Use Authorisation approved mAbs[122,123]. The Y453F mutation is also found to escape from HLA-restricted cellular immunity[105].
N440K mutations
This mutation was detected in various parts of India in March and April 2021. The N440K mutation is also associated with the P323L substitution in the RdRP gene. The N440K variant can generate significantly higher viral loads within a short period, leading to its rapid spread. This variant has shown localized spread in the following four states: Karnataka, Maharashtra, Telangana, and Chhattisgarh. They together contributed to about 50% of these samples submitted for analysis[124]. The N440K mutation has also been reported to cause reinfection[125]. The frequency of the N440K variant was 2.1% in India and was particularly high in the state of Andhra Pradesh (33.8% of 272 genomes)[126]. The N440K variant is responsible for immune escape as it has shown resistance to class 3 mAbs and an enhanced binding affinity to the human ACE2 receptor[127].
AMINO-TERMINAL DOMAIN OR NTD MUTATIONS
NTD mutations in spike protein are often the neglected area in the SARS-CoV-2 genomic study. However, NTD mutations have been reported among the B.1.1.7 and B.1.351 lineages[128]. A significant transmission of a six-nt deletion in the S gene has been reported by Gupta et al[128] leading to a loss of two amino acids: H69 and V70[128].
Here we report recurrent emergence and significant onward transmission of a six-nt deletion in the S gene, which results in loss of two amino acids: H69 and V70. The H69/V70 variant also co-occurs with N501Y, N439K, and Y453F mutations on the RBD. The H69/V70 deletion increases infectivity twofold, and the effect on viral fitness is independent of the RBD changes. The H69/V70 mutations may also boost SARS-CoV-2’s ability to generate new variants, such as vaccine escape variants[129].
K417N/T mutations
The K417N/T mutation has been reported in the B.1.351 (as K417N), P.1 (as K417T), and B.1.1.529 variants (as K417N). Interestingly, the K417N/T mutation usually occurs in presence of other RBM mutations as these mutations may decrease the binding to ACE2 receptors[84,115]. The K417N/T mutation may cause immune evasion as well. The K417N mutation confers reduced susceptibility to etesevimab[130] and casirivimab[92] but retains susceptibility to bamlanivimab, imdevimab, and sotrovimab[124]. It also retains susceptibility to convalescent plasma or sera from patients vaccinated with the mRNA vaccine[92,123]. The K417N, E484K, or N501Y mutations showed a reduced or abolished neutralization by 14 of the 17 most potent mAbs tested[101]. Li et al[131] in a pseudovirus model, showed that the K417N mutation increases viral sensitivity to neutralization. Normally, the K417 variant allows a closed conformation, leading to reduced binding to ACE2 and reduced access to neutralization antibodies. The K417N mutation helps in an open conformation, resulting in the exposure of more epitopes to neutralizing antibodies and subsequently increased virus neutralization. Table 2 shows the five VOCs and their mutations.
Table 2.
Showing the five variants of concerns and their mutations
|
WHO label
|
Pango lineage
|
GISAID clade
|
Nextstrain clade
|
Spike protein substitutions
|
First detected
|
WHO date of designation
|
| Alpha | B.1.1.7 | GRY | 201(V1) | Deletion 69-70, Deletion 144, N501Y, A570D, D614G, P681H, T716I, S982A, D1118H | United Kingdom | 18th December 2020 |
| Beta | B.1.351 | GH/501Y.V2 | 20H(V2) | D80A, D215G, DeletionL242, DeletionA243, DeletionL244, K417N, E484K, N501Y, D614G, A701V | South Africa | 18th December 2020 |
| Delta | B.1.617.2 | G/478K.V1 | 21A | T19R, T95I, G142D, Deletion156, Deletion157, R158G, L452R, T478K, D614G, P681R and D950N | India | VOI: 4th April, 2021 VOC: 11th May, 2021 |
| Gamma | P.1 | GR/501Y.V3 | 20J(V3) | L18F, T20N, P26S, D138Y, R190S, K417T, E484K, N501Y, D614G, H655Y, T1027I | Brazil | 11th January 2021 |
| Omicron | B.1.1.529 lineage | GR/484A | 21K | A76V, T95I, Y145del, G339D, N440K, G446S, S477N, T478K, E484A, Q493R, G496S, Q498R, N501Y, Y505H, T547K, D614G, H655Y, N679K, P681H, N764K, D796Y, N856K, Q954H, N969K, L981F, L212I, S371L, S373P, S375F, K417N. ORF1a: K856R, ORF1a: L2084I, ORF1a: A2710T, ORF1a: T3255I, ORF1a: P3395H, ORF1a: I3758V, ORF1b: P314L, ORF1b: I1566V, and ORF9b: P10S | Botswana and South Africa | 26th November 2021 |
WHO: World health organization; GISAID: Global initiative on sharing all influenza data; VOI: Variants of interest; VOC: Variants of concern.
CONCLUSION
The emergence of SARS-CoV-2 variants is an important phenomenon in the natural history of SARS-CoV-2 infection because it poses a considerable public health risk. Currently, we have five VOCs. These variants are more transmissible than the Wuhan strain. Various mutations identified in these VOCs are located on the spike protein, especially in the RBD. These mutations influence virus-host cell interaction, binding affinity, furin cleavage, and neutralizing efficacy by antibodies and vaccines. The most recent VOC detected is the omicron variant; however, this will not be the last variant we encounter. We will also see newer variants in the future, too. Characterization of the genomic character of the VOCs will help in identifying newer mutations quickly and in exploring phenotypic effects on the virus. In this article, we looked at the characteristics of the five VOCs, as well as the associated mutations, and how they affect SARS-CoV-2 virus’s infectivity, transmissibility, and immune evasion. The best way to prevent the development of new variants is to vaccinate as many people as possible, closely adhere to infection prevention and control measures, and eliminate vaccine inequalities that limit future human transmission and acquisition.
Footnotes
Conflict-of-interest statement: Authors declare no conflicts of interest while publishing this research work.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medical laboratory technology
Country/Territory of origin: India
Peer-review report’s classification
Scientific Quality: Grade B
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Odhar HA, Iraq S-Editor: Liu H L-Editor: A P-Editor: Yu HG
Contributor Information
Malay Sarkar, Department of Pulmonary Medicine, Indira Gandhi Medical College, Shimla 171001, Himachal Pradesh, India.
Irappa Madabhavi, Department of Medical and Pediatric Oncology and Hematology, J N Medical College, and KAHER, Belagavi, Karnataka 590010, India; Department of Medical and Pediatric Oncology and Hematology, Kerudi Cancer Hospital, Bagalkot, Karnataka 587103, India. irappamadabhavi@gmail.com.
References
- 1. Coronavirus Mutations and Variants: What Does It Mean? Available from: https://srhd.org/news/2021/coronavirus-mutations-and-variants-what-does-it-mean .
- 2.Sanjuán R, Domingo-Calap P. Mechanisms of viral mutation. Cell Mol Life Sci. 2016;73:4433–4448. doi: 10.1007/s00018-016-2299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Callaway E. The coronavirus is mutating - does it matter? Nature. 2020;585:174–177. doi: 10.1038/d41586-020-02544-6. [DOI] [PubMed] [Google Scholar]
- 4.Ashley Hagen, M S. Is the Science Communications Specialist at the American Society for Microbiology. Available from: https://asm.org/Biographies/Ashley-Hagen .
- 5.Minskaia E, Hertzig T, Gorbalenya AE, Campanacci V, Cambillau C, Canard B, Ziebuhr J. Discovery of an RNA virus 3'->5' exoribonuclease that is critically involved in coronavirus RNA synthesis. Proc Natl Acad Sci U S A. 2006;103:5108–5113. doi: 10.1073/pnas.0508200103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Denison MR, Graham RL, Donaldson EF, Eckerle LD, Baric RS. Coronaviruses: an RNA proofreading machine regulates replication fidelity and diversity. RNA Biol. 2011;8:270–279. doi: 10.4161/rna.8.2.15013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Graham RL, Baric RS. Recombination, reservoirs, and the modular spike: mechanisms of coronavirus cross-species transmission. J Virol. 2010;84:3134–3146. doi: 10.1128/JVI.01394-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gribble J, Stevens LJ, Agostini ML, Anderson-Daniels J, Chappell JD, Lu X, Pruijssers AJ, Routh AL, Denison MR. The coronavirus proofreading exoribonuclease mediates extensive viral recombination. PLoS Pathog. 2021;17:e1009226. doi: 10.1371/journal.ppat.1009226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson B, Boni MF, Bull MJ, Colleran A, Colquhoun RM, Darby AC, Haldenby S, Hill V, Lucaci A, McCrone JT, Nicholls SM, O'Toole Á, Pacchiarini N, Poplawski R, Scher E, Todd F, Webster HJ, Whitehead M, Wierzbicki C COVID-19 Genomics UK (COG-UK) Consortium, Loman NJ, Connor TR, Robertson DL, Pybus OG, Rambaut A. Generation and transmission of interlineage recombinants in the SARS-CoV-2 pandemic. Cell. 2021;184:5179–5188.e8. doi: 10.1016/j.cell.2021.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simmonds P. Rampant C→U Hypermutation in the Genomes of SARS-CoV-2 and Other Coronaviruses: Causes and Consequences for Their Short- and Long-Term Evolutionary Trajectories. mSphere. 2020;5 doi: 10.1128/mSphere.00408-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Dorp L, Richard D, Tan CCS, Shaw LP, Acman M, Balloux F. No evidence for increased transmissibility from recurrent mutations in SARS-CoV-2. Nat Commun. 2020;11:5986. doi: 10.1038/s41467-020-19818-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Otto SP, Day T, Arino J, Colijn C, Dushoff J, Li M, Mechai S, Van Domselaar G, Wu J, Earn DJD, Ogden NH. The origins and potential future of SARS-CoV-2 variants of concern in the evolving COVID-19 pandemic. Curr Biol. 2021;31:R918–R929. doi: 10.1016/j.cub.2021.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang H, Pipes L, Nielsen R. Synonymous mutations and the molecular evolution of SARS-CoV-2 origins. Virus Evol. 2021;7:veaa098. doi: 10.1093/ve/veaa098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walker AS, Vihta KD, Gethings O, Pritchard E, Jones J, House T, Bell I, Bell JI, Newton JN, Farrar J, Diamond I, Studley R, Rourke E, Hay J, Hopkins S, Crook D, Peto T, Matthews PC, Eyre DW, Stoesser N, Pouwels KB Covid-19 Infection Survey Team. Tracking the Emergence of SARS-CoV-2 Alpha Variant in the United Kingdom. N Engl J Med. 2021;385:2582–2585. doi: 10.1056/NEJMc2103227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown KA, Gubbay J, Hopkins J, Patel S, Buchan SA, Daneman N, Goneau LW. S-Gene Target Failure as a Marker of Variant B.1.1.7 Among SARS-CoV-2 Isolates in the Greater Toronto Area, December 2020 to March 2021. JAMA. 2021;325:2115–2116. doi: 10.1001/jama.2021.5607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. SARS-CoV-2 Viral Mutations: Impact on COVID-19 Tests. Available from: https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/sars-cov-2-viral-mutations-impact-covid-19-tests .
- 17.Chi X, Yan R, Zhang J, Zhang G, Zhang Y, Hao M, Zhang Z, Fan P, Dong Y, Yang Y, Chen Z, Guo Y, Li Y, Song X, Chen Y, Xia L, Fu L, Hou L, Xu J, Yu C, Li J, Zhou Q, Chen W. A neutralizing human antibody binds to the N-terminal domain of the Spike protein of SARS-CoV-2. Science. 2020;369:650–655. doi: 10.1126/science.abc6952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020;181:281–292.e6. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tortorici MA, Veesler D. Structural insights into coronavirus entry. Adv Virus Res. 2019;105:93–116. doi: 10.1016/bs.aivir.2019.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ascoli CA. Could mutations of SARS-CoV-2 suppress diagnostic detection? Nat Biotechnol. 2021;39:274–275. doi: 10.1038/s41587-021-00845-3. [DOI] [PubMed] [Google Scholar]
- 21. SARS-CoV-2 variant classifications and definitions. Available from: https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html .
- 22.Cella E, Benedetti F, Fabris S, Borsetti A, Pezzuto A, Ciotti M, Pascarella S, Ceccarelli G, Zella D, Ciccozzi M, Giovanetti M. SARS-CoV-2 Lineages and Sub-Lineages Circulating Worldwide: A Dynamic Overview. Chemotherapy. 2021;66:3–7. doi: 10.1159/000515340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Global Consultation on a Decision Framework for Assessing the Impact of SARS-CoV-2 Variants of Concern on Public Health Interventions. Available from: https://www.who.int/news-room/events/detail/2021/03/29/default-calendar/global-consultation-on-a-decision-framework-for-assessing-the-impact-of-sars-cov-2-variants-of-concern-on-public-health-interventions .
- 24.Patel D, Venus B. Portable chest x-rays in the intensive care unit: importance of erect position. Crit Care Med. 1988;16:299. doi: 10.1097/00003246-198803000-00021. [DOI] [PubMed] [Google Scholar]
- 25.Lei Z, Zhang D, Yang RP, Li J, Du WX, Liu YQ, Tan HB, Liu ZX, Liu L. Substitutions and codon usage in SARS-CoV-2 in mammals indicate natural selection and host adaptation. 2021 Preprint. [Google Scholar]
- 26.Fu Y, Huang Y, Rao J, Zeng F, Yang R, Tan H, Liu Z, Du W, Liu L. Host adaptation of codon usage in SARS-CoV-2 from mammals indicates potential natural selection and viral fitness. Arch Virol. 2022;167:2677–2688. doi: 10.1007/s00705-022-05612-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. A Primer on Coronavirus, Variants, Mutation and Evolution. Available from: https://cals.ncsu.edu/applied-ecology/news/a-primer-on-coronavirus-variants-mutation-and-evolution/
- 28. Natural selection vs creation: a literature review on the origin of SARS-CoV-2. Available from: https://www.infezmed.it/media/journal/Vol_28_3_2020_3.pdf . [PubMed]
- 29.Rubio-Casillas A, Redwan EM, Uversky VN. SARS-CoV-2 Intermittent Virulence as a Result of Natural Selection. COVID. 2022;2:1089–1101. [Google Scholar]
- 30.Habib MT, Rahman S, Afrad MH, Howlader AM, Khan MH, Khanam F, Alam AN, Chowdhury EK, Rahman Z, Rahman M, Shirin T, Qadri F. Natural selection shapes the evolution of SARS-CoV-2 Omicron in Bangladesh. Front Genet. 2023;14:1220906. doi: 10.3389/fgene.2023.1220906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou Z, Barrett J, He X. Immune Imprinting and Implications for COVID-19. Vaccines (Basel) 2023;11 doi: 10.3390/vaccines11040875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chemaitelly H, Ayoub HH, Abu-Raddad LJ. COVID-19 Primary Series and Booster Vaccination and Potential for Immune Imprinting. Open Forum Infect Dis. 2023;10 Suppl 2:ofad500.1954. [Google Scholar]
- 33. SARS-CoV-2 variants of concern as of 15 March 2024. Available from: https://www.ecdc.europa.eu/en/covid-19/variants-concern .
- 34.Zárate S, Taboada B, Muñoz-Medina JE, Iša P, Sanchez-Flores A, Boukadida C, Herrera-Estrella A, Selem Mojica N, Rosales-Rivera M, Gómez-Gil B, Salas-Lais AG, Santacruz-Tinoco CE, Montoya-Fuentes H, Alvarado-Yaah JE, Molina-Salinas GM, Espinoza-Ayala GE, Enciso-Moreno JA, Gutiérrez-Ríos RM, Loza A, Moreno-Contreras J, García-López R, Rivera-Gutierrez X, Comas-García A, Wong-Chew RM, Jiménez-Corona ME, Del Angel RM, Vazquez-Perez JA, Matías-Florentino M, Pérez-García M, Ávila-Ríos S, Castelán-Sánchez HG, Delaye L, Martínez-Castilla LP, Escalera-Zamudio M, López S, Arias CF. The Alpha Variant (B.1.1.7) of SARS-CoV-2 Failed to Become Dominant in Mexico. Microbiol Spectr. 2022;10:e0224021. doi: 10.1128/spectrum.02240-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davies NG, Jarvis CI CMMID COVID-19 Working Group, Edmunds WJ, Jewell NP, Diaz-Ordaz K, Keogh RH. Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7. Nature. 2021;593:270–274. doi: 10.1038/s41586-021-03426-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Volz E, Mishra S, Chand M, Barrett JC, Johnson R, Geidelberg L, Hinsley WR, Laydon DJ, Dabrera G, O'Toole Á, Amato R, Ragonnet-Cronin M, Harrison I, Jackson B, Ariani CV, Boyd O, Loman NJ, McCrone JT, Gonçalves S, Jorgensen D, Myers R, Hill V, Jackson DK, Gaythorpe K, Groves N, Sillitoe J, Kwiatkowski DP COVID-19 Genomics UK (COG-UK) consortium, Flaxman S, Ratmann O, Bhatt S, Hopkins S, Gandy A, Rambaut A, Ferguson NM. Assessing transmissibility of SARS-CoV-2 lineage B.1.1.7 in England. Nature. 2021;593:266–269. doi: 10.1038/s41586-021-03470-x. [DOI] [PubMed] [Google Scholar]
- 37.Shen X, Tang H, McDanal C, Wagh K, Fischer W, Theiler J, Yoon H, Li D, Haynes BF, Sanders KO, Gnanakaran S, Hengartner N, Pajon R, Smith G, Glenn GM, Korber B, Montefiori DC. SARS-CoV-2 variant B.1.1.7 is susceptible to neutralizing antibodies elicited by ancestral spike vaccines. Cell Host Microbe. 2021;29:529–539.e3. doi: 10.1016/j.chom.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.U.S. Food and Drug Administration. Fact sheet for health careproviders emergency use authorization (EUA) of bamlanivimaband etesevimab. Available from: https://www.fda.gov/media/145802/download .
- 39.U.S. Food and Drug Administration. Fact sheet for health care providers emergency use authorization (EUA) of REGEN-COV (casirivimab with imdevimab). Available from: https://www.fda.gov/media/145611/download .
- 40.U.S. Food and Drug Administration. Fact sheet for health careproviders emergency use authorization (EUA) of sotrovimab. Available from: https://www.fda.gov/media/149534/download .
- 41.Jangra S, Ye C, Rathnasinghe R, Stadlbauer D Personalized Virology Initiative study group, Krammer F, Simon V, Martinez-Sobrido L, García-Sastre A, Schotsaert M. SARS-CoV-2 spike E484K mutation reduces antibody neutralisation. Lancet Microbe. 2021;2:e283–e284. doi: 10.1016/S2666-5247(21)00068-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Emary KRW, Golubchik T, Aley PK, Ariani CV, Angus B, Bibi S, Blane B, Bonsall D, Cicconi P, Charlton S, Clutterbuck EA, Collins AM, Cox T, Darton TC, Dold C, Douglas AD, Duncan CJA, Ewer KJ, Flaxman AL, Faust SN, Ferreira DM, Feng S, Finn A, Folegatti PM, Fuskova M, Galiza E, Goodman AL, Green CM, Green CA, Greenland M, Hallis B, Heath PT, Hay J, Hill HC, Jenkin D, Kerridge S, Lazarus R, Libri V, Lillie PJ, Ludden C, Marchevsky NG, Minassian AM, McGregor AC, Mujadidi YF, Phillips DJ, Plested E, Pollock KM, Robinson H, Smith A, Song R, Snape MD, Sutherland RK, Thomson EC, Toshner M, Turner DPJ, Vekemans J, Villafana TL, Williams CJ, Hill AVS, Lambe T, Gilbert SC, Voysey M, Ramasamy MN, Pollard AJ COVID-19 Genomics UK consortium; AMPHEUS Project; Oxford COVID-19 Vaccine Trial Group. Efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 variant of concern 202012/01 (B.1.1.7): an exploratory analysis of a randomised controlled trial. Lancet. 2021;397:1351–1362. doi: 10.1016/S0140-6736(21)00628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, Stowe J, Tessier E, Groves N, Dabrera G, Myers R, Campbell CNJ, Amirthalingam G, Edmunds M, Zambon M, Brown KE, Hopkins S, Chand M, Ramsay M. Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. N Engl J Med. 2021;385:585–594. doi: 10.1056/NEJMoa2108891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bruxvoort KJ, Sy LS, Qian L, Ackerson BK, Luo Y, Lee GS, Tian Y, Florea A, Aragones M, Tubert JE, Takhar HS, Ku JH, Paila YD, Talarico CA, Tseng HF. Effectiveness of mRNA-1273 against delta, mu, and other emerging variants of SARS-CoV-2: test negative case-control study. BMJ. 2021;375:e068848. doi: 10.1136/bmj-2021-068848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tegally H, Wilkinson E, Giovanetti M, Iranzadeh A, Fonseca V, Giandhari J, Doolabh D, Pillay S, San EJ, Msomi N, Mlisana K, von Gottberg A, Walaza S, Allam M, Ismail A, Mohale T, Glass AJ, Engelbrecht S, Van Zyl G, Preiser W, Petruccione F, Sigal A, Hardie D, Marais G, Hsiao NY, Korsman S, Davies MA, Tyers L, Mudau I, York D, Maslo C, Goedhals D, Abrahams S, Laguda-Akingba O, Alisoltani-Dehkordi A, Godzik A, Wibmer CK, Sewell BT, Lourenço J, Alcantara LCJ, Kosakovsky Pond SL, Weaver S, Martin D, Lessells RJ, Bhiman JN, Williamson C, de Oliveira T. Detection of a SARS-CoV-2 variant of concern in South Africa. Nature. 2021;592:438–443. doi: 10.1038/s41586-021-03402-9. [DOI] [PubMed] [Google Scholar]
- 46.Ortega MA, García-Montero C, Fraile-Martinez O, Colet P, Baizhaxynova A, Mukhtarova K, Alvarez-Mon M, Kanatova K, Asúnsolo A, Sarría-Santamera A. Recapping the Features of SARS-CoV-2 and Its Main Variants: Status and Future Paths. J Pers Med. 2022;12 doi: 10.3390/jpm12060995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. COVID-19: Epidemiology, virology, and prevention. Available from: https://www.uptodate.com/contents/covid-19-epidemiology-virology-and-prevention .
- 48.Zeng B, Gao L, Zhou Q, Yu K, Sun F. Effectiveness of COVID-19 vaccines against SARS-CoV-2 variants of concern: a systematic review and meta-analysis. BMC Med. 2022;20:200. doi: 10.1186/s12916-022-02397-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. SARS-CoV-2 Gamma variant. Available from: https://en.wikipedia.org/wiki/SARS-CoV-2_Gamma_variant .
- 50.Faria NR, Mellan TA, Whittaker C, Claro IM, Candido DDS, Mishra S, Crispim MAE, Sales FCS, Hawryluk I, McCrone JT, Hulswit RJG, Franco LAM, Ramundo MS, de Jesus JG, Andrade PS, Coletti TM, Ferreira GM, Silva CAM, Manuli ER, Pereira RHM, Peixoto PS, Kraemer MUG, Gaburo N Jr, Camilo CDC, Hoeltgebaum H, Souza WM, Rocha EC, de Souza LM, de Pinho MC, Araujo LJT, Malta FSV, de Lima AB, Silva JDP, Zauli DAG, Ferreira ACS, Schnekenberg RP, Laydon DJ, Walker PGT, Schlüter HM, Dos Santos ALP, Vidal MS, Del Caro VS, Filho RMF, Dos Santos HM, Aguiar RS, Proença-Modena JL, Nelson B, Hay JA, Monod M, Miscouridou X, Coupland H, Sonabend R, Vollmer M, Gandy A, Prete CA Jr, Nascimento VH, Suchard MA, Bowden TA, Pond SLK, Wu CH, Ratmann O, Ferguson NM, Dye C, Loman NJ, Lemey P, Rambaut A, Fraiji NA, Carvalho MDPSS, Pybus OG, Flaxman S, Bhatt S, Sabino EC. Genomics and epidemiology of the P.1 SARS-CoV-2 lineage in Manaus, Brazil. Science. 2021;372:815–821. doi: 10.1126/science.abh2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. How Dangerous Is the Delta Variant (B.1.617.2)? Available from: https://asm.org/Articles/2021/July/How-Dangerous-is-the-Delta-Variant-B-1-617-2#:~:text=Data%20indicate%20that%20Delta%20is%2040-60%25%20more%20transmissible,airways%20of%20patients%20infected%20with%20the%20Delta%20variant .
- 52.Li B, Deng A, Li K, Hu Y, Li Z, Shi Y, Xiong Q, Liu Z, Guo Q, Zou L, Zhang H, Zhang M, Ouyang F, Su J, Su W, Xu J, Lin H, Sun J, Peng J, Jiang H, Zhou P, Hu T, Luo M, Zhang Y, Zheng H, Xiao J, Liu T, Tan M, Che R, Zeng H, Zheng Z, Huang Y, Yu J, Yi L, Wu J, Chen J, Zhong H, Deng X, Kang M, Pybus OG, Hall M, Lythgoe KA, Li Y, Yuan J, He J, Lu J. Viral infection and transmission in a large, well-traced outbreak caused by the SARS-CoV-2 Delta variant. Nat Commun. 2022;13:460. doi: 10.1038/s41467-022-28089-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Public Health England. Investigation of novel SARS-CoV-2 variant: technical briefing. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/957504/Variant_of_Concern_VOC_202012_01_Technical_Briefing_5_England.pdf .
- 54.Sheikh A, McMenamin J, Taylor B, Robertson C Public Health Scotland and the EAVE II Collaborators. SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet. 2021;397:2461–2462. doi: 10.1016/S0140-6736(21)01358-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Risk assessment for SARS-CoV-2 variant: Delta (VOC-21APR-02, B.1.617.2) Public Health England. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/991135/3_June_2021_Risk_assessment_for_SARS-CoV-2_variant_DELTA.pdf .
- 56. Update on omicron-World Health Organization. 2021. Available from: https://www.who.int/news/item/28-11-2021-update-on-omicron .
- 57.Tegally H, Moir M, Everatt J, Giovanetti M, Scheepers C, Wilkinson E, Subramoney K, Makatini Z, Moyo S, Amoako DG, Baxter C, Althaus CL, Anyaneji UJ, Kekana D, Viana R, Giandhari J, Lessells RJ, Maponga T, Maruapula D, Choga W, Matshaba M, Mbulawa MB, Msomi N NGS-SA consortium, Naidoo Y, Pillay S, Sanko TJ, San JE, Scott L, Singh L, Magini NA, Smith-Lawrence P, Stevens W, Dor G, Tshiabuila D, Wolter N, Preiser W, Treurnicht FK, Venter M, Chiloane G, McIntyre C, O'Toole A, Ruis C, Peacock TP, Roemer C, Kosakovsky Pond SL, Williamson C, Pybus OG, Bhiman JN, Glass A, Martin DP, Jackson B, Rambaut A, Laguda-Akingba O, Gaseitsiwe S, von Gottberg A, de Oliveira T. Emergence of SARS-CoV-2 Omicron lineages BA.4 and BA.5 in South Africa. Nat Med. 2022;28:1785–1790. doi: 10.1038/s41591-022-01911-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Meo SA, Meo AS, Al-Jassir FF, Klonoff DC. Omicron SARS-CoV-2 new variant: global prevalence and biological and clinical characteristics. Eur Rev Med Pharmacol Sci. 2021;25:8012–8018. doi: 10.26355/eurrev_202112_27652. [DOI] [PubMed] [Google Scholar]
- 59.Garcia-Beltran WF, St Denis KJ, Hoelzemer A, Lam EC, Nitido AD, Sheehan ML, Berrios C, Ofoman O, Chang CC, Hauser BM, Feldman J, Roederer AL, Gregory DJ, Poznansky MC, Schmidt AG, Iafrate AJ, Naranbhai V, Balazs AB. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell. 2022;185:457–466.e4. doi: 10.1016/j.cell.2021.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Grabowski F, Kochańczyk M, Lipniacki T. The Spread of SARS-CoV-2 Variant Omicron with a Doubling Time of 2.0-3.3 Days Can Be Explained by Immune Evasion. Viruses. 2022;14 doi: 10.3390/v14020294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ferguson N, Ghani A, Cori A, Hogan A, Hinsley W, Volz E on behalf of the Imperial College COVID-19 response team. Imperial College London. Report 49 - Growth, population distribution and immune escape of the Omicron in England. Available from: https://www.imperial.ac.uk/media/imperial-college/medicine/mrc-gida/2021-12-16-COVID19-Report-49.pdf .
- 62.Abdullah F, Myers J, Basu D, Tintinger G, Ueckermann V, Mathebula M, Ramlall R, Spoor S, de Villiers T, Van der Walt Z, Cloete J, Soma-Pillay P, Rheeder P, Paruk F, Engelbrecht A, Lalloo V, Myburg M, Kistan J, van Hougenhouck-Tulleken W, Boswell MT, Gray G, Welch R, Blumberg L, Jassat W. Decreased severity of disease during the first global omicron variant covid-19 outbreak in a large hospital in tshwane, south africa. Int J Infect Dis. 2022;116:38–42. doi: 10.1016/j.ijid.2021.12.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yue C, Song W, Wang L, Jian F, Chen X, Gao F, Shen Z, Wang Y, Wang X, Cao Y. ACE2 binding and antibody evasion in enhanced transmissibility of XBB.1.5. Lancet Infect Dis. 2023;23:278–280. doi: 10.1016/S1473-3099(23)00010-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hoffmann M, Krüger N, Schulz S, Cossmann A, Rocha C, Kempf A, Nehlmeier I, Graichen L, Moldenhauer AS, Winkler MS, Lier M, Dopfer-Jablonka A, Jäck HM, Behrens GMN, Pöhlmann S. The Omicron variant is highly resistant against antibody-mediated neutralization: Implications for control of the COVID-19 pandemic. Cell. 2022;185:447–456.e11. doi: 10.1016/j.cell.2021.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Majumdar S, Sarkar R. Mutational and phylogenetic analyses of the two lineages of the Omicron variant. J Med Virol. 2022;94:1777–1779. doi: 10.1002/jmv.27558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wu N, Joyal-Desmarais K, Ribeiro PAB, Vieira AM, Stojanovic J, Sanuade C, Yip D, Bacon SL. Long-term effectiveness of COVID-19 vaccines against infections, hospitalisations, and mortality in adults: findings from a rapid living systematic evidence synthesis and meta-analysis up to December, 2022. Lancet Respir Med. 2023;11:439–452. doi: 10.1016/S2213-2600(23)00015-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Andrews N, Stowe J, Kirsebom F, Toffa S, Rickeard T, Gallagher E, Gower C, Kall M, Groves N, O'Connell AM, Simons D, Blomquist PB, Zaidi A, Nash S, Iwani Binti Abdul Aziz N, Thelwall S, Dabrera G, Myers R, Amirthalingam G, Gharbia S, Barrett JC, Elson R, Ladhani SN, Ferguson N, Zambon M, Campbell CNJ, Brown K, Hopkins S, Chand M, Ramsay M, Lopez Bernal J. Covid-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant. N Engl J Med. 2022;386:1532–1546. doi: 10.1056/NEJMoa2119451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Collie S, Champion J, Moultrie H, Bekker LG, Gray G. Effectiveness of BNT162b2 Vaccine against Omicron Variant in South Africa. N Engl J Med. 2022;386:494–496. doi: 10.1056/NEJMc2119270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shu Y, McCauley J. GISAID: Global initiative on sharing all influenza data - from vision to reality. Euro Surveill. 2017;22 doi: 10.2807/1560-7917.ES.2017.22.13.30494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Korber B, Fischer WM, Gnanakaran S, Yoon H, Theiler J, Abfalterer W, Hengartner N, Giorgi EE, Bhattacharya T, Foley B, Hastie KM, Parker MD, Partridge DG, Evans CM, Freeman TM, de Silva TI Sheffield COVID-19 Genomics Group, McDanal C, Perez LG, Tang H, Moon-Walker A, Whelan SP, LaBranche CC, Saphire EO, Montefiori DC. Tracking Changes in SARS-CoV-2 Spike: Evidence that D614G Increases Infectivity of the COVID-19 Virus. Cell. 2020;182:812–827.e19. doi: 10.1016/j.cell.2020.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Plante JA, Liu Y, Liu J, Xia H, Johnson BA, Lokugamage KG, Zhang X, Muruato AE, Zou J, Fontes-Garfias CR, Mirchandani D, Scharton D, Bilello JP, Ku Z, An Z, Kalveram B, Freiberg AN, Menachery VD, Xie X, Plante KS, Weaver SC, Shi PY. Spike mutation D614G alters SARS-CoV-2 fitness. Nature. 2021;592:116–121. doi: 10.1038/s41586-020-2895-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hou YJ, Chiba S, Halfmann P, Ehre C, Kuroda M, Dinnon KH 3rd, Leist SR, Schäfer A, Nakajima N, Takahashi K, Lee RE, Mascenik TM, Graham R, Edwards CE, Tse LV, Okuda K, Markmann AJ, Bartelt L, de Silva A, Margolis DM, Boucher RC, Randell SH, Suzuki T, Gralinski LE, Kawaoka Y, Baric RS. SARS-CoV-2 D614G variant exhibits efficient replication ex vivo and transmission in vivo. Science. 2020;370:1464–1468. doi: 10.1126/science.abe8499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hoffmann M, Kleine-Weber H, Pöhlmann S. A Multibasic Cleavage Site in the Spike Protein of SARS-CoV-2 Is Essential for Infection of Human Lung Cells. Mol Cell. 2020;78:779–784.e5. doi: 10.1016/j.molcel.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yurkovetskiy L, Wang X, Pascal KE, Tomkins-Tinch C, Nyalile TP, Wang Y, Baum A, Diehl WE, Dauphin A, Carbone C, Veinotte K, Egri SB, Schaffner SF, Lemieux JE, Munro JB, Rafique A, Barve A, Sabeti PC, Kyratsous CA, Dudkina NV, Shen K, Luban J. Structural and Functional Analysis of the D614G SARS-CoV-2 Spike Protein Variant. Cell. 2020;183:739–751.e8. doi: 10.1016/j.cell.2020.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kannan SR, Spratt AN, Quinn TP, Heng X, Lorson CL, Sönnerborg A, Byrareddy SN, Singh K. Infectivity of SARS-CoV-2: there Is Something More than D614G? J Neuroimmune Pharmacol. 2020;15:574–577. doi: 10.1007/s11481-020-09954-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhang L, Jackson CB, Mou H, Ojha A, Peng H, Quinlan BD, Rangarajan ES, Pan A, Vanderheiden A, Suthar MS, Li W, Izard T, Rader C, Farzan M, Choe H. SARS-CoV-2 spike-protein D614G mutation increases virion spike density and infectivity. Nat Commun. 2020;11:6013. doi: 10.1038/s41467-020-19808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jackson CB, Zhang L, Farzan M, Choe H. Functional importance of the D614G mutation in the SARS-CoV-2 spike protein. Biochem Biophys Res Commun. 2021;538:108–115. doi: 10.1016/j.bbrc.2020.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhang J, Cai Y, Xiao T, Lu J, Peng H, Sterling SM, Walsh RM Jr, Rits-Volloch S, Zhu H, Woosley AN, Yang W, Sliz P, Chen B. Structural impact on SARS-CoV-2 spike protein by D614G substitution. Science. 2021;372:525–530. doi: 10.1126/science.abf2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Garcia-Beltran WF, Lam EC, Astudillo MG, Yang D, Miller TE, Feldman J, Hauser BM, Caradonna TM, Clayton KL, Nitido AD, Murali MR, Alter G, Charles RC, Dighe A, Branda JA, Lennerz JK, Lingwood D, Schmidt AG, Iafrate AJ, Balazs AB. COVID-19-neutralizing antibodies predict disease severity and survival. Cell. 2021;184:476–488.e11. doi: 10.1016/j.cell.2020.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lauring AS, Hodcroft EB. Genetic Variants of SARS-CoV-2-What Do They Mean? JAMA. 2021;325:529–531. doi: 10.1001/jama.2020.27124. [DOI] [PubMed] [Google Scholar]
- 82.Luan B, Wang H, Huynh T. Enhanced binding of the N501Y-mutated SARS-CoV-2 spike protein to the human ACE2 receptor: insights from molecular dynamics simulations. FEBS Lett. 2021;595:1454–1461. doi: 10.1002/1873-3468.14076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Liu H, Zhang Q, Wei P, Chen Z, Aviszus K, Yang J, Downing W, Jiang C, Liang B, Reynoso L, Downey GP, Frankel SK, Kappler J, Marrack P, Zhang G. The basis of a more contagious 501Y.V1 variant of SARS-CoV-2. Cell Res. 2021;31:720–722. doi: 10.1038/s41422-021-00496-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Starr TN, Greaney AJ, Stewart CM, Walls AC, Hannon WW, Veesler D, Bloom JD. Deep mutational scans for ACE2 binding, RBD expression, and antibody escape in the SARS-CoV-2 Omicron BA.1 and BA.2 receptor-binding domains. PLoS Pathog. 2022;18:e1010951. doi: 10.1371/journal.ppat.1010951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Laffeber C, de Koning K, Kanaar R, Lebbink JHG. Experimental Evidence for Enhanced Receptor Binding by Rapidly Spreading SARS-CoV-2 Variants. J Mol Biol. 2021;433:167058. doi: 10.1016/j.jmb.2021.167058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhu X, Mannar D, Srivastava SS, Berezuk AM, Demers JP, Saville JW, Leopold K, Li W, Dimitrov DS, Tuttle KS, Zhou S, Chittori S, Subramaniam S. Cryo-electron microscopy structures of the N501Y SARS-CoV-2 spike protein in complex with ACE2 and 2 potent neutralizing antibodies. PLoS Biol. 2021;19:e3001237. doi: 10.1371/journal.pbio.3001237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Teruel N, Mailhot O, Najmanovich RJ. Modelling conformational state dynamics and its role on infection for SARS-CoV-2 Spike protein variants. PLoS Comput Biol. 2021;17:e1009286. doi: 10.1371/journal.pcbi.1009286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cai Y, Zhang J, Xiao T, Lavine CL, Rawson S, Peng H, Zhu H, Anand K, Tong P, Gautam A, Lu S, Sterling SM, Walsh RM Jr, Rits-Volloch S, Lu J, Wesemann DR, Yang W, Seaman MS, Chen B. Structural basis for enhanced infectivity and immune evasion of SARS-CoV-2 variants. Science. 2021;373:642–648. doi: 10.1126/science.abi9745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Leung K, Shum MH, Leung GM, Lam TT, Wu JT. Early transmissibility assessment of the N501Y mutant strains of SARS-CoV-2 in the United Kingdom, October to November 2020. Euro Surveill. 2021;26 doi: 10.2807/1560-7917.ES.2020.26.1.2002106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Weisblum Y, Schmidt F, Zhang F, DaSilva J, Poston D, Lorenzi JC, Muecksch F, Rutkowska M, Hoffmann HH, Michailidis E, Gaebler C, Agudelo M, Cho A, Wang Z, Gazumyan A, Cipolla M, Luchsinger L, Hillyer CD, Caskey M, Robbiani DF, Rice CM, Nussenzweig MC, Hatziioannou T, Bieniasz PD. Escape from neutralizing antibodies by SARS-CoV-2 spike protein variants. Elife. 2020;9 doi: 10.7554/eLife.61312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Copin R, Baum A, Wloga E, Pascal KE, Giordano S, Fulton BO, Zhou A, Negron N, Lanza K, Chan N, Coppola A, Chiu J, Ni M, Wei Y, Atwal GS, Hernandez AR, Saotome K, Zhou Y, Franklin MC, Hooper AT, McCarthy S, Hamon S, Hamilton JD, Staples HM, Alfson K, Carrion R Jr, Ali S, Norton T, Somersan-Karakaya S, Sivapalasingam S, Herman GA, Weinreich DM, Lipsich L, Stahl N, Murphy AJ, Yancopoulos GD, Kyratsous CA. The monoclonal antibody combination REGEN-COV protects against SARS-CoV-2 mutational escape in preclinical and human studies. Cell. 2021;184:3949–3961.e11. doi: 10.1016/j.cell.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang P, Nair MS, Liu L, Iketani S, Luo Y, Guo Y, Wang M, Yu J, Zhang B, Kwong PD, Graham BS, Mascola JR, Chang JY, Yin MT, Sobieszczyk M, Kyratsous CA, Shapiro L, Sheng Z, Huang Y, Ho DD. Antibody resistance of SARS-CoV-2 variants B.1.351 and B.1.1.7. Nature. 2021;593:130–135. doi: 10.1038/s41586-021-03398-2. [DOI] [PubMed] [Google Scholar]
- 93.Rees-Spear C, Muir L, Griffith SA, Heaney J, Aldon Y, Snitselaar JL, Thomas P, Graham C, Seow J, Lee N, Rosa A, Roustan C, Houlihan CF, Sanders RW, Gupta RK, Cherepanov P, Stauss HJ, Nastouli E SAFER Investigators, Doores KJ, van Gils MJ, McCoy LE. The effect of spike mutations on SARS-CoV-2 neutralization. Cell Rep. 2021;34:108890. doi: 10.1016/j.celrep.2021.108890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Edara VV, Hudson WH, Xie X, Ahmed R, Suthar MS. Neutralizing Antibodies Against SARS-CoV-2 Variants After Infection and Vaccination. JAMA. 2021;325:1896–1898. doi: 10.1001/jama.2021.4388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wise J. Covid-19: The E484K mutation and the risks it poses. BMJ. 2021;372:n359. doi: 10.1136/bmj.n359. [DOI] [PubMed] [Google Scholar]
- 96.Collier DA, De Marco A, Ferreira IATM, Meng B, Datir RP, Walls AC, Kemp SA, Bassi J, Pinto D, Silacci-Fregni C, Bianchi S, Tortorici MA, Bowen J, Culap K, Jaconi S, Cameroni E, Snell G, Pizzuto MS, Pellanda AF, Garzoni C, Riva A CITIID-NIHR BioResource COVID-19 Collaboration, Elmer A, Kingston N, Graves B, McCoy LE, Smith KGC, Bradley JR, Temperton N, Ceron-Gutierrez L, Barcenas-Morales G; COVID-19 Genomics UK (COG-UK) Consortium, Harvey W, Virgin HW, Lanzavecchia A, Piccoli L, Doffinger R, Wills M, Veesler D, Corti D, Gupta RK. Sensitivity of SARS-CoV-2 B.1.1.7 to mRNA vaccine-elicited antibodies. Nature. 2021;593:136–141. doi: 10.1038/s41586-021-03412-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Greaney AJ, Loes AN, Crawford KHD, Starr TN, Malone KD, Chu HY, Bloom JD. Comprehensive mapping of mutations in the SARS-CoV-2 receptor-binding domain that affect recognition by polyclonal human plasma antibodies. Cell Host Microbe. 2021;29:463–476.e6. doi: 10.1016/j.chom.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Liu Z, VanBlargan LA, Bloyet LM, Rothlauf PW, Chen RE, Stumpf S, Zhao H, Errico JM, Theel ES, Liebeskind MJ, Alford B, Buchser WJ, Ellebedy AH, Fremont DH, Diamond MS, Whelan SPJ. Identification of SARS-CoV-2 spike mutations that attenuate monoclonal and serum antibody neutralization. Cell Host Microbe. 2021;29:477–488.e4. doi: 10.1016/j.chom.2021.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nelson G, BuzkoO, SpilmanP, Niazi K, Rabizadeh S, Soon-Shiong P. Molecular dynamic simulation reveals E484K mutation enhances spike RBD-ACE2 affinity and the combination of E484K, K417N and N501Y mutations (501Y.V2 variant) induces conformational change greater than N501Y mutant alone, potentially resulting in an escape mutant. 2021 Preprint. [Google Scholar]
- 100.Zahradník J, Marciano S, Shemesh M, Zoler E, Harari D, Chiaravalli J, Meyer B, Rudich Y, Li C, Marton I, Dym O, Elad N, Lewis MG, Andersen H, Gagne M, Seder RA, Douek DC, Schreiber G. SARS-CoV-2 variant prediction and antiviral drug design are enabled by RBD in vitro evolution. Nat Microbiol. 2021;6:1188–1198. doi: 10.1038/s41564-021-00954-4. [DOI] [PubMed] [Google Scholar]
- 101.Wang Z, Schmidt F, Weisblum Y, Muecksch F, Barnes CO, Finkin S, Schaefer-Babajew D, Cipolla M, Gaebler C, Lieberman JA, Oliveira TY, Yang Z, Abernathy ME, Huey-Tubman KE, Hurley A, Turroja M, West KA, Gordon K, Millard KG, Ramos V, Da Silva J, Xu J, Colbert RA, Patel R, Dizon J, Unson-O'Brien C, Shimeliovich I, Gazumyan A, Caskey M, Bjorkman PJ, Casellas R, Hatziioannou T, Bieniasz PD, Nussenzweig MC. mRNA vaccine-elicited antibodies to SARS-CoV-2 and circulating variants. Nature. 2021;592:616–622. doi: 10.1038/s41586-021-03324-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Genome Sequencing by INSACOG shows variants of concern and a Novel variant in India. Available from: https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1707177 .
- 103.Cherian S, Potdar V, Jadhav S, Yadav P, Gupta N, Das M, Rakshit P, Singh S, Abraham P, Panda S, Team N. SARS-CoV-2 Spike Mutations, L452R, T478K, E484Q and P681R, in the Second Wave of COVID-19 in Maharashtra, India. Microorganisms. 2021;9 doi: 10.3390/microorganisms9071542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Deng X, Garcia-Knight MA, Khalid MM, Servellita V, Wang C, Morris MK, Sotomayor-González A, Glasner DR, Reyes KR, Gliwa AS, Reddy NP, Sanchez San Martin C, Federman S, Cheng J, Balcerek J, Taylor J, Streithorst JA, Miller S, Sreekumar B, Chen PY, Schulze-Gahmen U, Taha TY, Hayashi JM, Simoneau CR, Kumar GR, McMahon S, Lidsky PV, Xiao Y, Hemarajata P, Green NM, Espinosa A, Kath C, Haw M, Bell J, Hacker JK, Hanson C, Wadford DA, Anaya C, Ferguson D, Frankino PA, Shivram H, Lareau LF, Wyman SK, Ott M, Andino R, Chiu CY. Transmission, infectivity, and neutralization of a spike L452R SARS-CoV-2 variant. Cell. 2021;184:3426–3437.e8. doi: 10.1016/j.cell.2021.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Motozono C, Toyoda M, Zahradnik J, Saito A, Nasser H, Tan TS, Ngare I, Kimura I, Uriu K, Kosugi Y, Yue Y, Shimizu R, Ito J, Torii S, Yonekawa A, Shimono N, Nagasaki Y, Minami R, Toya T, Sekiya N, Fukuhara T, Matsuura Y, Schreiber G Genotype to Phenotype Japan (G2P-Japan) Consortium, Ikeda T, Nakagawa S, Ueno T, Sato K. SARS-CoV-2 spike L452R variant evades cellular immunity and increases infectivity. Cell Host Microbe. 2021;29:1124–1136.e11. doi: 10.1016/j.chom.2021.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tian D, Sun Y, Zhou J, Ye Q. The Global Epidemic of the SARS-CoV-2 Delta Variant, Key Spike Mutations and Immune Escape. Front Immunol. 2021;12:751778. doi: 10.3389/fimmu.2021.751778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. How the coronavirus infects cells — and why Delta is so dangerous. Scientists are unpicking the life cycle of SARS-CoV-2 and how the virus uses tricks to evade detection. By Megan Scudellari. Available from: https://www.nature.com/articles/d41586-021-02039-y . [DOI] [PubMed]
- 108.Saito A, Irie T, Suzuki R, Maemura T, Nasser H, Uriu K, Kosugi Y, Shirakawa K, Sadamasu K, Kimura I, Ito J, Wu J, Iwatsuki-Horimoto K, Ito M, Yamayoshi S, Loeber S, Tsuda M, Wang L, Ozono S, Butlertanaka EP, Tanaka YL, Shimizu R, Shimizu K, Yoshimatsu K, Kawabata R, Sakaguchi T, Tokunaga K, Yoshida I, Asakura H, Nagashima M, Kazuma Y, Nomura R, Horisawa Y, Yoshimura K, Takaori-Kondo A, Imai M Genotype to Phenotype Japan (G2P-Japan) Consortium, Tanaka S, Nakagawa S, Ikeda T, Fukuhara T, Kawaoka Y, Sato K. Enhanced fusogenicity and pathogenicity of SARS-CoV-2 Delta P681R mutation. Nature. 2022;602:300–306. doi: 10.1038/s41586-021-04266-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Liu Y, Liu J, Johnson BA, Xia H, Ku Z, Schindewolf C, Widen SG, An Z, Weaver SC, Menachery VD, Xie X, Shi PY. Delta spike P681R mutation enhances SARS-CoV-2 fitness over Alpha variant. bioRxiv. 2021 doi: 10.1016/j.celrep.2022.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. How the coronavirus infects cells — and why Delta is so dangerous? Available from: https://www.nature.com/articles/d41586-021-02039-y . [DOI] [PubMed]
- 111.Haynes WA, Kamath K, Lucas C, Shon J, Iwasaki A. Impact of B.1.1.7 variant mutations on antibody recognition of linear SARSCoV-2 epitopes. 2021 Preprint. [Google Scholar]
- 112.Lan J, Ge J, Yu J, Shan S, Zhou H, Fan S, Zhang Q, Shi X, Wang Q, Zhang L, Wang X. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 113.Pascarella S, Ciccozzi M, Zella D, Bianchi M, Benedetti F, Benvenuto D, Broccolo F, Cauda R, Caruso A, Angeletti S, Giovanetti M, Cassone A. SARS-CoV-2 B.1.617 Indian variants: Are electrostatic potential changes responsible for a higher transmission rate? J Med Virol. 2021;93:6551–6556. doi: 10.1002/jmv.27210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Di Giacomo S, Mercatelli D, Rakhimov A, Giorgi FM. Preliminary report on severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Spike mutation T478K. J Med Virol. 2021;93:5638–5643. doi: 10.1002/jmv.27062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Thomson EC, Rosen LE, Shepherd JG, Spreafico R, da Silva Filipe A, Wojcechowskyj JA, Davis C, Piccoli L, Pascall DJ, Dillen J, Lytras S, Czudnochowski N, Shah R, Meury M, Jesudason N, De Marco A, Li K, Bassi J, O'Toole A, Pinto D, Colquhoun RM, Culap K, Jackson B, Zatta F, Rambaut A, Jaconi S, Sreenu VB, Nix J, Zhang I, Jarrett RF, Glass WG, Beltramello M, Nomikou K, Pizzuto M, Tong L, Cameroni E, Croll TI, Johnson N, Di Iulio J, Wickenhagen A, Ceschi A, Harbison AM, Mair D, Ferrari P, Smollett K, Sallusto F, Carmichael S, Garzoni C, Nichols J, Galli M, Hughes J, Riva A, Ho A, Schiuma M, Semple MG, Openshaw PJM, Fadda E, Baillie JK, Chodera JD ISARIC4C Investigators; COVID-19 Genomics UK (COG-UK) Consortium, Rihn SJ, Lycett SJ, Virgin HW, Telenti A, Corti D, Robertson DL, Snell G. Circulating SARS-CoV-2 spike N439K variants maintain fitness while evading antibody-mediated immunity. Cell. 2021;184:1171–1187.e20. doi: 10.1016/j.cell.2021.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Harvey WT, Carabelli AM, Jackson B, Gupta RK, Thomson EC, Harrison EM, Ludden C, Reeve R, Rambaut A COVID-19 Genomics UK (COG-UK) Consortium, Peacock SJ, Robertson DL. SARS-CoV-2 variants, spike mutations and immune escape. Nat Rev Microbiol. 2021;19:409–424. doi: 10.1038/s41579-021-00573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zhou W, Xu C, Wang P, Luo M, Xu Z, Cheng R, Jin X, Guo Y, Xue G, Juan L, Anashkina AA, Nie H, Jiang Q. N439K Variant in Spike Protein Alter the Infection Efficiency and Antigenicity of SARS-CoV-2 Based on Molecular Dynamics Simulation. Front Cell Dev Biol. 2021;9:697035. doi: 10.3389/fcell.2021.697035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Oude Munnink BB, Sikkema RS, Nieuwenhuijse DF, Molenaar RJ, Munger E, Molenkamp R, van der Spek A, Tolsma P, Rietveld A, Brouwer M, Bouwmeester-Vincken N, Harders F, Hakze-van der Honing R, Wegdam-Blans MCA, Bouwstra RJ, GeurtsvanKessel C, van der Eijk AA, Velkers FC, Smit LAM, Stegeman A, van der Poel WHM, Koopmans MPG. Transmission of SARS-CoV-2 on mink farms between humans and mink and back to humans. Science. 2021;371:172–177. doi: 10.1126/science.abe5901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hammer AS, Quaade ML, Rasmussen TB, Fonager J, Rasmussen M, Mundbjerg K, Lohse L, Strandbygaard B, Jørgensen CS, Alfaro-Núñez A, Rosenstierne MW, Boklund A, Halasa T, Fomsgaard A, Belsham GJ, Bøtner A. SARS-CoV-2 Transmission between Mink (Neovison vison) and Humans, Denmark. Emerg Infect Dis. 2021;27:547–551. doi: 10.3201/eid2702.203794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Fonager J. Working paper on SARS-CoV-2 spike mutations arising in Danish mink, their spread to humans and neutralization data. Available from: https://files.ssi.dk/Mink-cluster-5-short-report_AFO2 .
- 121.Ren W, Lan J, Ju X, Gong M, Long Q, Zhu Z, Yu Y, Wu J, Zhong J, Zhang R, Fan S, Zhong G, Huang A, Wang X, Ding Q. Mutation Y453F in the spike protein of SARS-CoV-2 enhances interaction with the mink ACE2 receptor for host adaption. PLoS Pathog. 2021;17:e1010053. doi: 10.1371/journal.ppat.1010053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Baum A, Fulton BO, Wloga E, Copin R, Pascal KE, Russo V, Giordano S, Lanza K, Negron N, Ni M, Wei Y, Atwal GS, Murphy AJ, Stahl N, Yancopoulos GD, Kyratsous CA. Antibody cocktail to SARS-CoV-2 spike protein prevents rapid mutational escape seen with individual antibodies. Science. 2020;369:1014–1018. doi: 10.1126/science.abd0831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wang R, Zhang Q, Ge J, Ren W, Zhang R, Lan J, Ju B, Su B, Yu F, Chen P, Liao H, Feng Y, Li X, Shi X, Zhang Z, Zhang F, Ding Q, Zhang T, Wang X, Zhang L. Analysis of SARS-CoV-2 variant mutations reveals neutralization escape mechanisms and the ability to use ACE2 receptors from additional species. Immunity. 2021;54:1611–1621.e5. doi: 10.1016/j.immuni.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tandel D, Gupta D, Sah V, Harshan KH. N440K variant of SARS-CoV-2 has higher infectious ftness. 2021 Preprint. [Google Scholar]
- 125.Gupta V, Bhoyar RC, Jain A, Srivastava S, Upadhayay R, Imran M, Jolly B, Divakar MK, Sharma D, Sehgal P, Ranjan G, Gupta R, Scaria V, Sivasubbu S. Asymptomatic Reinfection in 2 Healthcare Workers From India With Genetically Distinct Severe Acute Respiratory Syndrome Coronavirus 2. Clin Infect Dis. 2021;73:e2823–e2825. doi: 10.1093/cid/ciaa1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Jolly B, Rophina M, Shamnath A, Imran M, Bhoyar RC, Divakar MK, Roja Rani P, Ranjan G, Sehgal P, Chandrasekhar P, Afsar S, Vijaya Lakshmi J, Surekha A, Sivasubbu S, Scaria V. Genetic epidemiology of variants associated with immune escape from global SARS-CoV-2 genomes. 2020 Preprint. [Google Scholar]
- 127.Barnes CO, Jette CA, Abernathy ME, Dam KA, Esswein SR, Gristick HB, Malyutin AG, Sharaf NG, Huey-Tubman KE, Lee YE, Robbiani DF, Nussenzweig MC, West AP Jr, Bjorkman PJ. SARS-CoV-2 neutralizing antibody structures inform therapeutic strategies. Nature. 2020;588:682–687. doi: 10.1038/s41586-020-2852-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gupta RK. Will SARS-CoV-2 variants of concern affect the promise of vaccines? Nat Rev Immunol. 2021;21:340–341. doi: 10.1038/s41577-021-00556-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Meng B, Kemp SA, Papa G, Datir R, Ferreira IATM, Marelli S, Harvey WT, Lytras S, Mohamed A, Gallo G, Thakur N, Collier DA, Mlcochova P COVID-19 Genomics UK (COG-UK) Consortium, Duncan LM, Carabelli AM, Kenyon JC, Lever AM, De Marco A, Saliba C, Culap K, Cameroni E, Matheson NJ, Piccoli L, Corti D, James LC, Robertson DL, Bailey D, Gupta RK. Recurrent emergence of SARS-CoV-2 spike deletion H69/V70 and its role in the Alpha variant B.1.1.7. Cell Rep. 2021;35:109292. doi: 10.1016/j.celrep.2021.109292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Starr TN, Greaney AJ, Addetia A, Hannon WW, Choudhary MC, Dingens AS, Li JZ, Bloom JD. Prospective mapping of viral mutations that escape antibodies used to treat COVID-19. Science. 2021;371:850–854. doi: 10.1126/science.abf9302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Li Q, Nie J, Wu J, Zhang L, Ding R, Wang H, Zhang Y, Li T, Liu S, Zhang M, Zhao C, Liu H, Nie L, Qin H, Wang M, Lu Q, Li X, Liu J, Liang H, Shi Y, Shen Y, Xie L, Qu X, Xu W, Huang W, Wang Y. SARS-CoV-2 501Y.V2 variants lack higher infectivity but do have immune escape. Cell. 2021;184:2362–2371.e9. doi: 10.1016/j.cell.2021.02.042. [DOI] [PMC free article] [PubMed] [Google Scholar]