Abstract
BACKGROUND
Breast cancer is among the most common malignancies worldwide. With progress in treatment methods and levels, the overall survival period has been prolonged, and the demand for quality care has increased.
AIM
To investigate the effect of individualized and continuous care intervention in patients with breast cancer.
METHODS
Two hundred patients with breast cancer who received systemic therapy at The First Affiliated Hospital of Hebei North University (January 2021 to July 2023) were retrospectively selected as research participants. Among them, 134 received routine care intervention (routing group) and 66 received personalized and continuous care (intervention group). Self-rating anxiety scale (SAS), self-rating depression scale (SDS), and Functional Assessment of Cancer Therapy-Breast (FACT-B) scores, including limb shoulder joint activity, complication rate, and care satisfaction, were compared between both groups after care.
RESULTS
SAS and SDS scores were lower in the intervention group than in the routing group at one and three months after care. The total FACT-B scores and five dimensions in the intervention group were higher than those in the routing group at three months of care. The range of motion of shoulder anteflexion, posterior extension, abduction, internal rotation, and external rotation in the intervention group was higher than that in the routing group one month after care. The incidence of postoperative complications was 18.18% lower in the intervention group than in the routing group (34.33%; P <0.05). Satisfaction with care was 90.91% higher in the intervention group than in the routing group (78.36%; P <0.05).
CONCLUSION
Personalized and continuous care can alleviate negative emotions in patients with breast cancer, quicken rehabilitation of limb function, decrease the incidence of complications, and improve living quality and care satisfaction.
Keywords: Breast cancer, Personalized care, Continuous care, Negative emotions, Living quality, Rehabilitation effect
Core Tip: Surgery is currently the treatment of choice for breast cancer. Long-term rehabilitation exercises are necessary after surgery due to surgical trauma. At the same time, surgery alters breast structure, increases the patient's psychological stress response, and makes them prone to negative emotions, affecting quality of life and adherence to recovery. Therefore, there is a need to find a care model that improves the negative emotions and quality of life of patients and promotes their recovery.
INTRODUCTION
According to 2020 data from the International Cancer Research Center, there are approximately 2.3 million new cases of breast cancer, making it the most common cancer in the world[1]. Currently, breast cancer therapy is mostly based on surgery supplemented with radiotherapy and chemotherapy[2]. Long-term treatment remains a significant challenge for patients with breast cancer. They not only suffer from physical pain, including fatigue, lack of physical function, and side effects of treatment, but also bear a variety of psychological pressures, such as uncertainty in disease prognosis, lack of family role function, and economic burden, which often lead to negative emotions, decreased quality of life, and serious adverse effects on rehabilitation[3,4]. The key issue in clinical nursing is alleviating negative emotions in patients with breast cancer, improving their quality of life, and encouraging them to gradually return to society. In recent years, personalized and continuous care has received increasing attention in the field of oncology. Personalized care is patient-centered, focuses on meeting the individual needs of patients, and provides better services[5]. Continuous care provides patients with medical, nursing, and rehabilitation guidance services after discharge, which is conducive to them receiving reliable and complete rehabilitation guidance[6]. Therefore, this study applied personalized and continuous care to the management of breast cancer and aims to serve as a reference for nursing work.
MATERIALS AND METHODS
Patient characteristics
Two hundred patients with breast cancer who received systemic therapy at The First Affiliated Hospital of Hebei North University from January 2021 to July 2023 were retrospectively selected as research participants. The inclusion criteria were as follows: (1) Pathological examination that diagnosed breast cancer for the first time; (2) female patients; (3) patients aged between 30 and 60 years; (4) a treatment plan that included surgery combined with chemotherapy and radiotherapy; and (5) routine or personalized and continuous care received during treatment. The exclusion criteria were as follows: (1) Suffering from heart, brain, liver, or other major organ diseases; (2) combination of malignant tumors and immune, blood system, and infectious diseases; (3) observed mental and cognitive disorders; (4) patients with a previous history of chest surgery; (5) patient loss for follow-up and to death; (6) pregnant or lactating women; and (7) incomplete clinical data.
Care intervention methods
The routing group received routine care, including condition monitoring, health education, and follow-up, as well as medication, psychological, perioperative, and rehabilitation care, and so on. The intervention group received individualized and continuous care based on the routine care. This involved the following: (1) Establishment of a care group composed of head nurses and multiple nursing staff. After admission, the patient's condition and family situation were recorded in a case file through data collection. The group collectively evaluated the patient's condition and potential risk factors and then developed a personalized care plan in line with the actual situation through discussions; (2) Health education and psychological care: Combined with the patient's cultural level, knowledge of health education on breast cancer surgery, perioperative precautions, and possible adverse reactions after surgery were provided through oral presentations, handbooks, videos, and other means to deepen their understanding. The psychological changes in patients were closely observed, care given when considering speech and physical behavior, and questions regarding any of their doubts were answered patiently. Targeted psychological education should be carried out by psychologists when necessary; (3) Life care: Encouraged patients to express their inner needs and strove to create a comfortable sickroom environment. Based on the patient's personal preferences and overall condition, personalized recipes were developed to ensure nutritional intake; (4) Perioperative care: Postoperative changes in patients were closely monitored to ensure early treatment of complications. After the patient's postoperative condition stabilized, the responsible nurse provided one-on-one functional exercise guidance, and the exercise intensity was based on the patient’s tolerance. After the patients and their families mastered the exercise methods, the exercise situation was registered daily to provide continuous and periodic functional exercise guidance; and (5) Out-hospital care: Through the “intelligent health education system” to achieve continuous care for patients, the nursing staff dynamically tracked the patient's condition after discharge on the platform and used a questionnaire survey to grasp information on the medication, diet, and exercise in detail. According to feedback information from the platform, the nursing team developed a new management plan for patients every two weeks and set up a punch card to urge them to implement it.
Index measurements
Negative emotions: Before and one and three months after care, the self-rating anxiety scale (SAS) and the self-rating depression scale (SDS)[7] were used to assess the negative emotions of patients. Both the SAS and SDS include 20 items, each of which can be rated on a scale of 1-4, with a total score of 20-80. The SAS is bounded by 50 scores: 50-59, mild anxiety; 60-69, moderate anxiety; and >69, severe anxiety. The SDS is bounded by 53 scores: 53-62, mild depression; 63-72, moderate depression; and 72, severe depression. In this study, the total score of the two scales multiplied by 1.25 was converted into a percentage system to present its integer part, with a final full score of 100 points.
Living quality: Before and three months after care, the Functional Assessment of Cancer Therapy-Breast (FACT-B)[8] was used to assess the quality of life of patients. FACT-B includes five subscales and 36 items, namely, physiological (seven items), emotional (six items), social (seven items), and functional well-being (seven items), as well as a specific breast cancer subscale (nine items). Each item can be rated on a scale of 0-4, with a total score ranging from 0-144. A higher score indicates a better living quality.
Limb shoulder joint activity: Before and one month after care, the angles of shoulder anteflexion, posterior extension, abduction, internal rotation, and external rotation were measured using a protractor.
Complications: Postoperative complications in the two patient groups were compared, such as flap necrosis, upper limb lymphedema, wound infection, and subcutaneous effusion.
Care satisfaction: A self-made care satisfaction questionnaire was used to assess patient satisfaction with nursing work. There are 20 items in the questionnaire, each of which can be rated on a scale of 1-5, with a total score of 20-100. A total questionnaire score of ≤ 59 indicates unsatisfied, between 60 and 89 indicates satisfied, and ≥ 90 indicates greatly satisfied. Care satisfaction = (satisfied + greatly satisfied) / total number of cases.
Statistical analysis
SPSS 26.0n software was used for all data analyses. Quantitative data according to abnormal distribution were shown as the mean ± SD. A paired sample t-test was adopted for intragroup comparison, and an independent sample t-test for intergroup comparison. Qualitative data are shown as cases and percentages [n (%)], which were compared using the chi-square and Fisher's exact tests when more than 20% of the theoretical frequency was < 5, or when the theoretical frequency was < 1. Repeated measures analysis of variance was used to compare the data at different times between groups, which was then corrected using a Bonferroni test. Statistical significance was set at P < 0.05.
RESULTS
General data
In total, 134 patients who received routine care were included in the routing group, and 66 patients who received personalized and continuous care included in the intervention group. There were no statistically significant differences in the general data between the two groups (P > 0.05; Table 1).
Table 1.
Comparison of the general data between the routing and intervention groups
|
Data
|
Routing group (n = 134)
|
Intervention group (n = 66)
|
t/χ2/Z
|
P value
|
| Age (yr, mean ± SD) | 43.75 ± 7.15 | 45.39 ± 4.67 | 1.954 | 0.052 |
| BMI (kg/m2, mean ± SD) | 23.40 ± 1.23 | 23.59 ± 1.84 | 0.747 | 0.457 |
| Marital status [n (%)] | 0.186 | 0.918 | ||
| Spinsterhood | 7 (5.22) | 4 (6.06) | ||
| Married | 106 (79.11) | 53 (80.30) | ||
| Divorced/widowed | 21 (15.67) | 9 (13.64) | ||
| Cultural levels [n (%)] | 0.154 | 0.878 | ||
| Junior school or below | 25 (18.66) | 11 (16.67) | ||
| High school/technical secondary school | 76 (56.72) | 39 (59.09) | ||
| College or higher | 33 (24.62) | 16 (24.24) | ||
| Sources of treatment costs [n (%)] | 3.890 | 0.149 | ||
| Fee | 22 (16.42) | 8 (12.12) | ||
| Medical insurance | 96 (71.64) | 55 (83.33) | ||
| Private expense | 16 (11.94) | 3 (4.55) | ||
| Tumor diameter (cm, mean ± SD) | 4.16 ± 1.05 | 4.41 ± 0.98 | 1.623 | 0.104 |
| Lesion localization [n (%)] | 1.232 | 0.550 | ||
| Left side | 62 (46.27) | 29 (43.94) | ||
| Right side | 58 (43.28) | 32 (48.48) | ||
| Both sides | 14 (10.45) | 5 (7.58) | ||
| TNM [n (%)] | 1.763 | 0.078 | ||
| I | 29 (21.64) | 9 (13.64) | ||
| II | 82 (61.19) | 40 (60.61) | ||
| III | 23 (17.16) | 17 (25.76) | ||
| Pathological type [n (%)] | 1.140 | 0.802 | ||
| Early invasive cancer | 12 (8.96) | 5 (7.58) | ||
| Invasive nonspecific carcinoma | 110 (82.09) | 58 (87.88) | ||
| Specific invasive carcinoma | 7 (5.22) | 2 (3.03) | ||
| Else | 5 (3.73) | 1 (1.52) | ||
| Operation mode [n (%)] | 0.178 | 0.724 | ||
| Mastectomy surgery | 102 (98.51) | 52 (78.79) | ||
| Breast conservation | 32 (23.88) | 14 (21.21) |
BMI: Body mass index; TNM: Tumor node metastasis.
Negative emotions
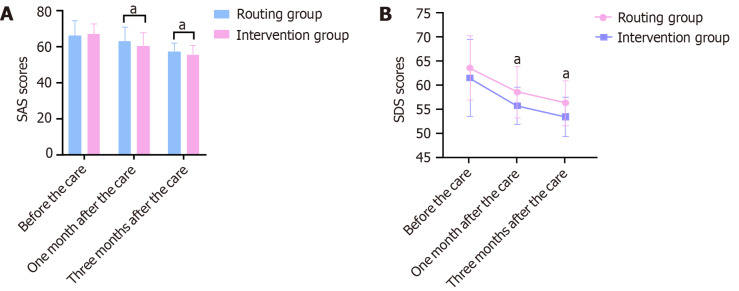
One month after care, the SAS total scores of the routing and intervention groups were 63.06 ± 8.02 and 60.64 ± 7.20, respectively. Three months after care, the SAS total scores of the routing and intervention groups were 57.44 ± 4.70 and 55.70 ± 5.19, respectively. The SAS scores in the intervention group were lower than those in the routing group at one and three months after care (P < 0.05; Figure 1A). Results of the repeated measures analysis of variance showed that the major effect of the number of measurements was significant (F = 98.041, P < 0.001), whereas the major effect of the group and the interaction effect were not (F = 3.341/2.808, P = 0.069/0.066).
Figure 1.
Comparison of the self-rating anxiety scale and self-rating depression scale scores between the routing and intervention groups. A: Self-rating anxiety scale scores; B: Self-rating depression scale scores. SAS: Self-rating anxiety scale; SDS: Self-rating depression scale. aP < 0.05.
One month after care, the SDS total scores of the routing and intervention groups were 58.45 ± 5.35 and 56.02 ± 5.85, respectively. Three months after care, the SDS total scores of the routing and interventions groups were 55.96 ± 4.71 and 53.33 ± 4.12, respectively. The SDS scores in the intervention group were lower than those in the routing group at one and three months after care (P < 0.05; Figure 1B). Results of repeated measures analysis of variance showed that the major effects of the group and number of measurements were significant (F = 18.406/93.001, P < 0.001), and there was no interaction effect between the grouping and number of measurements (F = 0.185, P = 0.831).
Living quality
Three months after care, total FACT-B scores and its five dimensions in both patient groups were greater than those before care intervention, where those recorded for the intervention group were higher than those in the routing group (Table 2).
Table 2.
Comparison of the Functional Assessment of Cancer Therapy-Breast scores between the routing and intervention groups (points, mean ± SD)
|
Time
|
Group
|
Case
|
Physiological well-being
|
Emotional well-being
|
Social well-being
|
Functional well-being
|
Specific breast cancer subscale
|
Total points
|
| T1 | ||||||||
| Routing group | 134 | 18.45 ± 3.39 | 16.09 ± 2.67 | 17.10 ± 3.64 | 15.06 ± 4.05 | 19.96 ± 4.35 | 86.65 ± 8.05 | |
| Intervention group | 66 | 17.82 ± 4.51 | 16.67 ± 3.55 | 17.53 ± 4.07 | 15.77 ± 2.47 | 21.08 ± 4.92 | 88.68 ± 8.46 | |
| t value | 1.002 | 1.169 | 0.761 | 1.538 | 1.639 | 1.799 | ||
| P value | 0.630 | 0.245 | 0.447 | 0.126 | 0.103 | 0.074 | ||
| T2 | ||||||||
| Routing group | 134 | 20.50 ± 3.34a | 18.60 ± 3.42a | 22.08 ± 3.13a | 19.37 ± 3.45a | 23.71 ± 3.33a | 104.27 ± 7.87a | |
| Intervention group | 66 | 22.27 ± 2.80a | 20.56 ± 1.72a | 23.68 ± 2.75a | 22.61 ± 2.40a | 26.29 ± 2.18a | 115.41 ± 5.85a | |
| t value | 3.940 | 5.382 | 3.532 | 7.697 | 6.556 | 11.249 | ||
| P value | < 0.001 | < 0.001 | 0.001 | < 0.001 | < 0.001 | < 0.001 |
P < 0.05, comparison of the same group before care.
T1: Before care intervention; T2: After three months of care intervention.
Limb shoulder joint activity
One month after care, the range of motion of shoulder anteflexion, posterior extension, abduction, internal rotation, and external rotation in both groups was lower than that before care intervention, where that recorded in the intervention group was higher than that in the routing group (P < 0.05; Table 3).
Table 3.
Comparison of limb shoulder joint activity of the affected limb between the routing and the intervention groups (°, mean ± SD)
|
Time
|
Group
|
Case
|
Anteflexion
|
Posterior extension
|
Abduction
|
Internal rotation
|
External rotation
|
| T1 | |||||||
| Routing group | 134 | 150.39 ± 11.57 | 40.75 ± 3.25 | 161.97 ± 8.14 | 72.10 ± 5.63 | 77.26 ± 5.72 | |
| Intervention group | 66 | 148.97 ± 13.99 | 39.68 ± 5.24 | 163.03 ± 7.21 | 73.97 ± 7.67 | 75.70 ± 6.69 | |
| t value | 0.760 | 1.514 | 0.899 | 1.763 | 1.629 | ||
| P value | 0.448 | 0.134 | 0.370 | 0.081 | 0.106 | ||
| T2 | |||||||
| Routing group | 134 | 123.90 ± 14.14a | 28.49 ± 4.58a | 115.48 ± 7.37a | 60.00 ± 8.66a | 64.37 ± 5.29a | |
| Intervention group | 66 | 130.97 ± 17.07a | 32.83 ± 5.59a | 126.21 ± 9.40a | 64.65 ± 9.34a | 67.58 ± 8.44a | |
| t value | 3.102 | 5.470 | 8.131 | 3.481 | 2.822 | ||
| P value | 0.002 | < 0.001 | < 0.001 | 0.001 | 0.006 |
P < 0.05, comparison of the same group before care.
T1: Before care intervention; T2: After one month of care intervention.
Complications
The incidence of postoperative complications was 34.33% (46/134) and 18.18% (12/66) in the routing and intervention groups, respectively, with the intervention group showing the lowest incidence than the routing group (P < 0.05; Table 4).
Table 4.
Comparison of complications between the routing and intervention groups, n (%)
|
Group
|
Case
|
Skin flap necrosis
|
Upper limb lymphadendema
|
Scalp hydrops
|
Wound infection
|
Else
|
Total
|
| Routing group | 134 | 7 (5.22) | 17 (12.69) | 4 (2.99) | 12 (8.96) | 6 (4.48) | 46 (34.33) |
| Intervention group | 66 | 2 (3.03) | 6 (9.09) | 0 | 3 (4.55) | 1 (1.52) | 12 (18.18) |
| χ2 | 5.075 | ||||||
| P value | 0.024 |
Care satisfaction
Care satisfaction of the routing group was 78.36% (105/134) and that of the intervention group 90.91% (60/66). Thus, patients in the intervention group noted higher care satisfaction than those in the routing group (P < 0.05; Table 5).
Table 5.
Comparison of care satisfaction between the routing and intervention groups, n (%)
|
Group
|
Case
|
Not satisfied
|
Satisfied
|
Very satisfied
|
Total
|
| Routing group | 134 | 29 (21.64) | 69 (51.49) | 36 (26.87) | 105 (78.36) |
| Intervention group | 66 | 6 (9.09) | 34 (51.52) | 26 (39.39) | 60 (90.91) |
| χ2 | 4.825 | ||||
| P value | 0.028 |
DISCUSSION
Breast cancer results from a change in the biology of cancer cells in the epicenter of the breast gland owing to the role of multiple carcinogens, resulting in massive numbers of infantile cancer cells proliferating endlessly, crowding and destroying normal cellular organization, and damaging the structure of the breast[9,10]. The breast is not an organ that maintains vital motion in humans. However, because breast gland cells forfeit the specificity of normocytes, the connections between tissues are loose and easily detached. Once cancer cells are shed, they can spread throughout the body via the blood or lymph, resulting in potentially life-threatening metastases[11].
The main principles of clinical treatment for breast cancer are early discovery, diagnosis, and therapy. At present, for most of the clinical procedures used in breast cancer radical surgery to further improve efficacy, the application of chemotherapy, radiotherapy, and other adjuvant therapies is critical[12]. With the continuous increase in treatment methods and levels, the survival rate of patients with breast cancer has increased, but the disease itself and treatment measures still cause unavoidable adverse effects in patients[13]. Statistically, patients with breast cancer have five- and ten-year survival rates of approximately 90% and 80%, respectively[14]. Therefore, improving a patient’s quality of life has become a key concern. Patients with breast cancer are prone to negative emotions during diagnosis and treatment. In a study of 2235 patients with breast cancer, 48.6% and 15% of them reported varying levels of anxiety and depression, respectively[15]. These emotions can seriously influence therapeutic effects and quality of life, increasing the risk of breast cancer recurrence and metastasis, shortening survival time, and increasing cancer mortality[16,17].
Routine care only attaches importance to the patient's condition and physical state, lacks targeted nursing measures to improve negative emotions and living quality, and the contract between the patient and the hospital ends after discharge; more services are provided to the patient through telephone follow-up and by other means, which make it difficult to effectively meet the needs of the patient[18]. Personalized care is based on scientific and humanized concepts. It generally requires doctors, patients, and family members to participate in the entire nursing process, including personalized evaluation, nursing plan formulation, efficient implementation, other aspects of nursing measures, is patient-centered, and requires improved nursing efficiency and quality[19]. Continuous care extends inpatient care services to families or communities to meet the health needs of discharged patients. It is an important nursing measure to accelerate the early rehabilitation of patients and is an indispensable part of deepening high-quality nursing[20].
In this study, personalized and continuous care was used for patients with breast cancer, and the results were as follows: (1) One and three months after care, the SAS and SDS scores in the intervention group were lower than those in the routing group; (2) Three months after care, the total FACT-B scores and the five associated dimensions in the intervention group were greater than those in the routing group; (3) One month after care, the range of motion of shoulder anteflexion, posterior extension, abduction, internal rotation, and external rotation in the intervention group was higher than that in the routing group; (4) Complications in the intervention group were less than those observed in the routing group; and (5) Care satisfaction of the intervention group was higher than that of the routing group. The reason is that, according to the theory of personalized and continuous care, nursing staff can provide targeted psychological counseling and catharsis; they can also develop appropriate cognitive intervention measures based on the patient's cultural level and acceptance. This helps to correct misconceptions and effectively reduce negative emotions. After breast cancer surgery, lifting the upper limb becomes challenging due to the need to remove the pectoralis major muscle and nerve. Additionally, dissection of axillary lymph nodes can block lymphatic reflux, leading to upper limb edema. Therefore, postoperative upper limb functional exercises are crucial for reducing scar traction and restoring limb function. After surgery, patients undergo guided early functional exercises with personalized plans tailored to their capabilities in terms of intensity, frequency, and duration. Following discharge, an online platform promptly provides patients with health-related information to address any difficulties. This enables patients to actively cooperate with treatment, while significantly reducing postoperative complications, promoting limb function recovery, and improving quality of life. Furthermore, personalized and continuous care focuses on establishing a strong ongoing connection with patients, while prioritizing their feelings and needs throughout the nursing process to improve acceptance and satisfaction.
There are some limitations to this study. Briefly, the number of samples included in this study was small and only used data from a single center. Therefore, the study conclusions need to be confirmed through future randomized controlled trials with larger sample sizes and involve multiple centers.
CONCLUSION
In summary, the application of personalized and continuous care in breast cancer therapy has a significant effect on alleviating negative emotions, accelerating the rehabilitation of limb function, decreasing the incidence of postoperative complications, and improving quality of life and care satisfaction. Overall, these findings are worthy of further extension and application.
Footnotes
Institutional review board statement: This study was reviewed and approved by the Institutional Ethics Committee of The First Affiliated Hospital of Hebei North University.
Informed consent statement: The Institutional Ethics Committee approved an exemption from informed consent.
Conflict-of-interest statement: Dr. Kong has nothing to disclose.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade B
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Kandasamy R S-Editor: Lin C L-Editor: A P-Editor: Che XX
Contributor Information
Ling-Xia Kong, Department of Breast Surgery, The First Affiliated Hospital of Hebei North University, Zhangjiakou 075000, Hebei Province, China. konglingxia1975@163.com.
Yan-Hong Zhao, Operating Room, The First Affiliated Hospital of Hebei North University, Zhangjiakou 075000, Hebei Province, China.
Zhi-Lin Feng, Department of Breast Surgery, The First Affiliated Hospital of Hebei North University, Zhangjiakou 075000, Hebei Province, China.
Ting-Ting Liu, Department of Breast Surgery, The First Affiliated Hospital of Hebei North University, Zhangjiakou 075000, Hebei Province, China.
Data sharing statement
The data used in this study can be obtained from the corresponding author upon request.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Storm-Dickerson T, Sigalove NM. The breast surgeons' approach to mastectomy and prepectoral breast reconstruction. Gland Surg. 2019;8:27–35. doi: 10.21037/gs.2018.11.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hashemi SM, Rafiemanesh H, Aghamohammadi T, Badakhsh M, Amirshahi M, Sari M, Behnamfar N, Roudini K. Prevalence of anxiety among breast cancer patients: a systematic review and meta-analysis. Breast Cancer. 2020;27:166–178. doi: 10.1007/s12282-019-01031-9. [DOI] [PubMed] [Google Scholar]
- 4.Getu MA, Chen C, Panpan W, Mboineki JF, Dhakal K, Du R. The effect of cognitive behavioral therapy on the quality of life of breast cancer patients: a systematic review and meta-analysis of randomized controlled trials. Qual Life Res. 2021;30:367–384. doi: 10.1007/s11136-020-02665-5. [DOI] [PubMed] [Google Scholar]
- 5.Le Boutillier C, Jeyasingh-Jacob J, Jones L, King A, Archer S, Urch C. Improving personalised care and support planning for people living with treatable-but-not-curable cancer. BMJ Open Qual. 2023;12 doi: 10.1136/bmjoq-2023-002322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kil WJ, Pham T, Kim K. Heart sparing breast cancer radiotherapy using continuous positive airway pressure (CPAP) and conventional supine tangential fields: an alternative method for patients with limited accessibility to advanced radiotherapy techniques. Acta Oncol. 2019;58:105–109. doi: 10.1080/0284186X.2018.1503711. [DOI] [PubMed] [Google Scholar]
- 7.Gao N, Li Y, Sang C, He J, Chen C. Effect of high-quality nursing on neurological function psychological moods quality of life of elderly patients with stroke. Front Neurol. 2023;14:1259737. doi: 10.3389/fneur.2023.1259737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang M, Gan C, Zhao J, Li W, Yu S, Yao S, Tang L, Xu J, Cheng H. Positive influence of managing cancer and living meaningfully (CALM) on fear of cancer recurrence in breast cancer survivors. Am J Cancer Res. 2023;13:3067–3079. [PMC free article] [PubMed] [Google Scholar]
- 9.Qaseem A, Lin JS, Mustafa RA, Horwitch CA, Wilt TJ Clinical Guidelines Committee of the American College of Physicians, Forciea MA, Fitterman N, Iorio A, Kansagara D, Maroto M, McLean RM, Tufte JE, Vijan S. Screening for Breast Cancer in Average-Risk Women: A Guidance Statement From the American College of Physicians. Ann Intern Med. 2019;170:547–560. doi: 10.7326/M18-2147. [DOI] [PubMed] [Google Scholar]
- 10.Shull JD, Dennison KL, Chack AC, Trentham-Dietz A. Rat models of 17β-estradiol-induced mammary cancer reveal novel insights into breast cancer etiology and prevention. Physiol Genomics. 2018;50:215–234. doi: 10.1152/physiolgenomics.00105.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yenmis G, Yaprak Sarac E, Besli N, Soydas T, Tastan C, Dilek Kancagi D, Yilanci M, Senol K, Karagulle OO, Ekmekci CG, Ovali E, Tuncdemir M, Ulutin T, Kanigur Sultuybek G. Anti-cancer effect of metformin on the metastasis and invasion of primary breast cancer cells through mediating NF-kB activity. Acta Histochem. 2021;123:151709. doi: 10.1016/j.acthis.2021.151709. [DOI] [PubMed] [Google Scholar]
- 12.Hu W, Xu D, Li N. Research Status of Systemic Adjuvant Therapy for Early Breast Cancer. Cancer Control. 2023;30:10732748231209193. doi: 10.1177/10732748231209193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Somashekhar SP, Sepúlveda MJ, Puglielli S, Norden AD, Shortliffe EH, Rohit Kumar C, Rauthan A, Arun Kumar N, Patil P, Rhee K, Ramya Y. Watson for Oncology and breast cancer treatment recommendations: agreement with an expert multidisciplinary tumor board. Ann Oncol. 2018;29:418–423. doi: 10.1093/annonc/mdx781. [DOI] [PubMed] [Google Scholar]
- 14.Nardin S, Mora E, Varughese FM, D'Avanzo F, Vachanaram AR, Rossi V, Saggia C, Rubinelli S, Gennari A. Breast Cancer Survivorship, Quality of Life, and Late Toxicities. Front Oncol. 2020;10:864. doi: 10.3389/fonc.2020.00864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Puigpinós-Riera R, Graells-Sans A, Serral G, Continente X, Bargalló X, Domènech M, Espinosa-Bravo M, Grau J, Macià F, Manzanera R, Pla M, Quintana MJ, Sala M, Vidal E. Anxiety and depression in women with breast cancer: Social and clinical determinants and influence of the social network and social support (DAMA cohort) Cancer Epidemiol. 2018;55:123–129. doi: 10.1016/j.canep.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Nakamura ZM, Deal AM, Nyrop KA, Chen YT, Quillen LJ, Brenizer T, Muss HB. Serial Assessment of Depression and Anxiety by Patients and Providers in Women Receiving Chemotherapy for Early Breast Cancer. Oncologist. 2021;26:147–156. doi: 10.1002/onco.13528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anuk D, Özkan M, Kizir A, Özkan S. The characteristics and risk factors for common psychiatric disorders in patients with cancer seeking help for mental health. BMC Psychiatry. 2019;19:269. doi: 10.1186/s12888-019-2251-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bartholomäus M, Zomorodbakhsch B, Micke O, Prott FJ, Rudolph I, Seilacher E, Hochhaus A, Huebner J. Cancer patients' needs for virtues and physicians' characteristics in physician-patient communication: a survey among patient representatives. Support Care Cancer. 2019;27:2783–2788. doi: 10.1007/s00520-018-4585-3. [DOI] [PubMed] [Google Scholar]
- 19.Parks RM, Cheung KL. Personalising Care in the Older Woman with Primary Breast Cancer. Ann Acad Med Singap. 2019;48:370–375. [PubMed] [Google Scholar]
- 20.Ding L, Ding S, He C, Zhang Q, An J. The efficacy of continuing nursing interventions on intraoperative pressure ulcer-related complications in breast cancer patients: systematic review and meta-analysis. Gland Surg. 2022;11:1078–1085. doi: 10.21037/gs-22-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this study can be obtained from the corresponding author upon request.