Abstract
Introduction
Cardiopulmonary resuscitation training in Malaysia has evolved from traditional to modern approaches, embracing technology for better outcomes. Smartphone-based training apps offer interactive learning with simulations and real-time feedback, improving cardiopulmonary resuscitation skills anytime, anywhere. This study evaluates the effectiveness of the smart-cardiopulmonary resuscitation application for healthcare practitioners.
Methods
This randomized controlled pilot study was conducted with 30 healthcare practitioners at the University of Malaysia Sabah. Participants underwent a Cardiopulmonary Resuscitation Practical formal educational training program, and data were collected using a Basic Life Support questionnaire and skills assessment checklist sourced from the American Heart Association (2020). Data analysis was conducted utilizing repeated analysis of variance and the Cochran ‘Q’ test supported by Statistical Package for the Social Sciences statistical software.
Result
The control and intervention groups showed improved knowledge and skills from pre-to post-cardiopulmonary resuscitation courses; a significant increase was observed in the intervention group compared to the control group. The F-test indicated a significant time-group effect (F-stat (df) = 16.14 (2), p = 0.01). Cochran’s ‘Q’ test also revealed significant changes in the proportion of healthcare practitioners passing their skills assessments over time (2 = 14.90, control 01).
Conclusion
The smart-cardiopulmonary resuscitation application is convenient for refreshing cardiopulmonary resuscitation skills and maintaining proficiency. While it doesn’t replace formal cardiopulmonary resuscitation courses, it saves healthcare practitioners and the community time and money. Both groups showed improved cardiopulmonary resuscitation knowledge and skills, with the intervention group using the smart-cardiopulmonary resuscitation application showing higher success rates after two months. Adopting smartphone-based cardiopulmonary resuscitation training with comprehensive content is recommended.
Keywords: Smart-cardiopulmonary resuscitation application, Technology-driven cardiopulmonary resuscitation training, Smartphones, Randomized controlled pilot study, Healthcare practitioners
1. Introduction
CPR training is vital in emergency medical care, especially during cardiac arrests. In Malaysia, like many places, CPR training has shifted from traditional to modern methods due to technological advancements and improved understanding of best practices [1] (Lim et al., 2022). Historically, Malaysian CPR training, like global practices, relied on classroom sessions with lectures and basic hands-on exercises [2] (KKM, 2014). However, this approach had limitations such as instructor availability and difficulty fully simulating real-life scenarios. However, studies have also reported poor retention of CPR knowledge and skills among healthcare professionals and laypersons following conventional training methods [3] (Fariduddin & Jaafar, 2021). As a result, there has been a growing demand for more engaging and interactive training methods. Contemporary CPR training techniques have emerged, leveraging technology to transform the learning process [1] (Lim et al., 2022). Using advanced manikins and immersive scenarios, simulation-based training enhances practitioners’ critical thinking, decision-making, and confidence in CPR skills [4] (Hill et al., 2023). Moreover, integrating multimedia resources and e-learning platforms has diversified training approaches, allowing for flexible, self-paced learning. Additionally, mobile applications and virtual reality (VR) have broadened CPR training opportunities, offering accessible tools for knowledge dissemination and skills evaluation [5] (Ali et al., 2021). Smartphone-based CPR training revolutionizes resuscitation education, offering convenient, comprehensive instruction and interactive simulations to enhance CPR proficiency. It provides immediate feedback, accessible anytime, anywhere, with engaging multimedia content. Smartphone sensors enable performance evaluation, democratizing high-quality CPR education and empowering healthcare professionals to respond effectively to cardiac emergencies [6,7] (Lins et al., 2022; Mccaw et al., 2023). Therefore, this study aims to evaluate the feasibility and effectiveness of the SCPR application and the entire training program, using smartphones as the primary training tool among the targeted audience, which includes healthcare practitioners (HCPs).
2. Materials and methods
2.1. Study design
The research employed the randomized controlled pilot study approach, commencing in December 2023 and concluding in January 2024 in the Faculty of Medicine and Health Science and a teaching hospital at Universiti Malaysia Sabah. This training aimed to see if the SCPR application and the whole technology-based CPR training program worked.
2.2. Sample
The training sessions occurred at the Faculty of Medicine and Health Sciences (FMHS) and HUMS. Eligible participants were healthcare providers (HCPs) from FMHS and HUMS who had received formal CPR certification and were not pregnant. Pregnant individuals and those unwilling to participate were excluded. Participants were selected using the systematic random sampling approach where those participants who meet the eligible criteria will pick a number (1: controlled group, 2: intervention group) to determine their group assignment. This choice aligns with what [8] Whitehead et al. (2016) said should be done. They used the non-central t-distribution (NCT) method to determine the sample size for randomized controlled pilot studies. The NCT approach was selected with a confidence level of 90% and a margin of error set at 5% significance. The NCT method is particularly advantageous for calculating sample sizes in studies aiming to detect small to moderate effect sizes, as it provides more accurate power estimates, especially when the effect size is non-zero. Additionally, the NCT method is beneficial for complex study designs involving multiple comparisons or factor interactions, offering a robust framework for sample size calculations in these scenarios [9] (Flight & Julious, 2016).
2.3. Study instrument
Smart Cardiopulmonary Resuscitation (SCPR) training is a smartphone-based CPR training app. It is designed to help healthcare practitioners learn and maintain CPR skills. The app’s structured approach aims to improve users’ CPR proficiency, making them better prepared for cardiac emergencies. To perform CPR practical training, users can practice it either on a manikin or other do-it-yourself manikin, such as a pillow. The developer acknowledges this potential limitation in practicing practical skills. The rescue breathing component was omitted from the application to focus on high-quality chest compressions, which are more feasible for non-medical personnel to perform. This decision aligns with the recommendations of the [10] American Heart Association (AHA, 2020), demonstrating that the training app is also suitable for community use.
2.4. Knowledge measurement
In this pilot study, participants answered 50 multiple-choice questions (MCQs). Each correct answer earned 1 point, with a maximum score of 50. To pass, participants needed a score of 43 or higher. Scores over 43 (86% or more) were considered “satisfactory,” scores between 35 and 42 (70–84%) were “fair,” and scores below 34 (less than 68%) were “poor.” The questions came from the Basic Life Support (BLS) question bank at Universiti Malaysia Sabah’s teaching hospital.
2.5. Skills measurement
Practical skills were evaluated using four parameters: rate, depth, and ventilation techniques [10]. The American Heart Association (AHA) 2020 skills assessment checklist was used, covering the recognition of sudden cardiac arrest (SCA), activating the Emergency Response Team (ERT), and performing high-quality chest compressions. This included maintaining a rate of 100–120 compressions per minute, a depth of at least 5 cm, minimizing interruptions, avoiding excessive ventilation, ensuring complete chest recoil, and using the head tilt chin lift technique. Certified trainers graded participants as pass or fail based on expert judgment of the correct sequence of actions.
2.6. Data collection
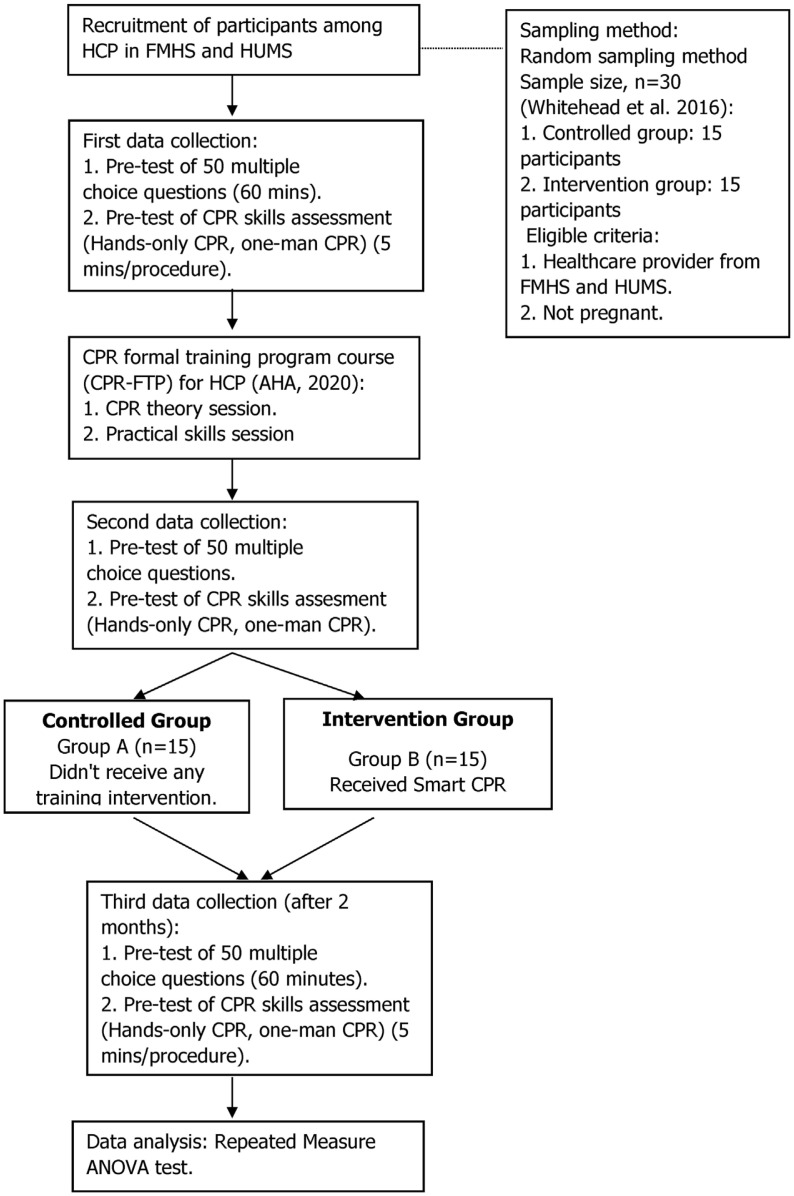
The study assessed improved CPR knowledge and skills, focusing on chest compression proficiency. Primary and secondary outcomes were evaluated before and after participants completed a formal CPR training program (CPR-FTP), with a follow-up assessment two months later to gauge retention. Initial data were collected through pre-tests with multiple-choice questions (MCQs) and skills assessments. Post-tests were administered after completing the CPR-FTP. Participants were then randomly assigned to Group A (control, no further intervention) or Group B (intervention, using the Cardiac Resuscitation Simulation Training Program (CRSTP) app to enhance CPR knowledge and skills). Fig. 1 offers a comprehensive and detailed representation of the data collection process.
Fig. 1.
The workflow of data collection.
2.7. Data analysis
The outcomes of both the theoretical examination and the practical skills assessment were recorded on data collection forms, then reviewed and transferred to an Excel spreadsheet. The Statistical Package for the Social Sciences (SPSS version 29) was employed to analyze the collected data.
3. Result
In this pilot study, 30 participants were recruited and evenly divided between the control group (n = 15) and the intervention group (n = 15). In the intervention group, 2 (13.3%) participants were male and 13 (86.7%) were female, representing diverse disciplines such as the Infection Control Unit (26.7%), Emergency and Trauma Department (20%), Primary Care Centre Department (20%), Internal Medicine Department (13.3%), Intensive Care Unit, Rehabilitation Department, and Haemodialysis Unit (6.7% each). The majority were registered nurses (86.7%), with assistant medical officers and medical officers making up 6.7% each. Educationally, 86.7% held diplomas and 13.3% held degrees. In terms of clinical experience, 46.7% had 4–6 years, 26.7% had 7–9 years, 20% had over 10 years, and 6.7% had 1–3 years. All intervention group participants had completed formal CPR training, with 46.7% having completed the Basic Life Support (BLS) course 3–4 years ago, 26.7% 1–2 years ago, and 6.7% over seven years ago.
The control group consisted of 11 (73.3%) female and 4 (26.7%) male participants from various departments including Obstetrics and Gynaecology (20%), General Surgery (13.3%), Orthopaedics (13.3%), Otorhinolaryngology (13.3%), Ophthalmology (13.3%), Cardiology (6.7%), Psychiatry (6.7%), Dental (6.7%), and Forensic Unit (6.7%). Most were registered nurses (66.7%), followed by medical officers (20%) and assistant medical officers (13.3%). Regarding educational qualifications, 53.3% held diplomas and 46.7% held bachelor’s degrees. All had clinical work experience, with 53.3% having 7–9 years, 26.7% having 4–6 years, 13.3% having over ten years, and 6.7% having 1–3 years. Concerning the last formal CPR training, 46.7% received it 1–2 years ago, 40% 3–4 years ago, and 6.7% each 5–6 years ago and over seven years ago. The demographic distribution of participants is detailed in Table 1.
Table 1.
Distribution of sample based on demographic data (n = 30).
| Variable | Intervention group, n (%) | Controlled group, n (%) |
|---|---|---|
| Gender | ||
| Male | 2 (13.3) | 4 (26.7) |
| Female | 13 (86.7) | 11 (73.3) |
| Department | ||
| Obstetric and Gynaecology | 3 (20) | |
| General Surgery | 2 (13.3) | |
| Orthopaedic | 2 (13.3) | |
| Otorhinolaryngology | 2 (13.3) | |
| Cardiology | 1 (6.7) | |
| Ophthalmology | 2 (13.3) | |
| Psychiatric | 1 (6.7) | |
| Dental | 1 (6.7) | |
| Forensic | 1 (6.7) | |
| Primary Care Centre | 3 (20) | |
| Emergency and Trauma | 3 (20) | |
| Internal Medicine | 2 (13.3) | |
| Infection Control | 4 (26.7) | |
| Intensive Care Unit | 1 (6.7) | |
| Rehabilitation | 1 (6.7) | |
| Haemodialysis | 1 (6.7) | |
| Designation | ||
| Registered Nurse | 13 (86.7) | 10 (66.7) |
| Assistant Medical Officer | 1 (6.7) | 2 (13.3) |
| Medical Officer | 1 (6.7) | 3 (20) |
| Level of education | ||
| Diploma | 13 (86.7) | 8 (53.3) |
| Bachelors | 2 (13.3) | 7 (46.7) |
| Clinical work experience | ||
| 1–3 years | 1 (6.7) | 1 (6.7) |
| 4–6 years | 7 (46.7) | 4 (26.7) |
| 7–9 years | 4 (26.7) | 8 (53.3) |
| >10 years | 3 (20) | 2 (13.3) |
| Last CPR training | ||
| 1–2 years | 4 (26.7) | 7 (46.7) |
| 3–4 years | 7 (46.7) | 6 (40) |
| 5–6 years | 4 (26.7) | 1 (6.7) |
| >7 years | 1 (6.7) | 1 (6.7) |
A repeated-measures analysis of variance (ANOVA) was conducted to assess the impact of time on scores from multiple-choice questions (MCQs) for both the control and intervention groups. Both groups demonstrated an enhancement in their knowledge levels from the pre-CPR course (Control Group: M = 37.4, SD = 5.75; Intervention Group: M = 38.20, SD = 6.01) to the post-CPR course (Control Group: M = 43.53, SD = 2.50; Intervention Group: M = 42.73, SD = 3.22). However, while the knowledge score decreased in the control group (M = 39.27, SD = 3.83), there was a significant improvement among participants in the intervention group (M = 43.60, SD = 0.83). Table 2 displays the means (M) and standard deviations (SD) for both groups concerning the effect of time.
Table 2.
Comparison of the mean score for multiple-choice questions score between intervention and control groups based on time (Time*Group effect).
| Time | Groups | Mean score (SE) | Mean difference (95% CI) | F (df) | p-value |
|---|---|---|---|---|---|
| Pre-CPR Course | Control | 37.4 (1.49) | 0.8 (35.64, 39.96) | 0.14 (1) | 0.71 |
| Intervention | 38.2 (1.55) | ||||
| Post-CPR Course | Control | 43.5 (0.65) | −0.8 (42.06,44.20) | 0.58 (1) | 0.45 |
| Intervention | 42.7 (0.83) | ||||
| Post-2 months of CPR Course | Control | 39.27 (0.99) | 4.33 (40.13, 42.74) | 18.38 (1) | <0.001 |
| Intervention | 43.6 (0.21) |
The multivariate test statistics showed a significant interaction between time and group (Time-Group effect), supported by both Pillai’s Trace [F-stat (df) = 16.14 (2), p-value = 0.01] and Wilk’s Lambda [F-stat (df) = 16.14 (2), p-value = 0.01], with significant p-values. As shown in Table 2, there were no significant changes in MCQ knowledge scores for either group during the pre-CPR course (p = 0.71) or post-CPR course (p = 0.45). However, a significant score improvement was seen post-2 months after the initial CPR course (p =<0.001).
Cochran’s test explored differences in CPR skills retention among 30 participants in control and intervention groups across three assessment points: before, immediately after, and two months post the CPR course. The test revealed a significant variation in the proportion of healthcare providers passing and failing their skills assessments over time, with a chi-square value of x2 (2) = 14.90, p < 0.001. To mitigate type 1 error, a Bonferroni post hoc test adjusted the alpha value to 0.016.
Table 3 demonstrates a notable difference in the frequency of CPR skills assessments regarding time, notably between pre- and post-CPR courses (p < 0.001). Conversely, there were no significant changes in skills assessment between post-CPR and post-2 months (p = 0.727). However, a significant alteration in frequency value was evident between pre-CPR and post-2 months (p = 0.002). Descriptive data in Table 3 indicates that 33.33% of the control group and 40% of the intervention group passed before the CPR course. Following the course, both groups exhibited improved performance, with 86.67% in the control and intervention groups passing. However, two months later, only 60% of the control group passed, while all intervention group participants succeeded, suggesting that using the CRSTP aids in CPR competency retention.
Table 3.
Represents the overall comparison of CPR skills performance result and the time effect.
| Time | Control Group, N (%) | Intervention Group N (%) | p-value | ||
|---|---|---|---|---|---|
|
|
|
||||
| Pass | Failed | Pass | Failed | ||
| Pre-CPR course | 5 (33.33) | 10 (66.7) | 6 (40) | 9 (60) | <0.001 |
| Post-CPR course | 13 (86.67) | 2 (13.33) | 13 (86.67) | 2 (13.333) | 0.727 |
| Post-2 months of CPR course | 9 (60) | 6 (40) | 15 (100) | 0 | 0.002 |
4. Discussion
In this study, Smart CPR Training (SCPR) is a technology-based tool delivered through Android smartphones. Its main aim is to teach and maintain CPR skills and knowledge for healthcare providers (HCPs) [11] (Taherdoost & Madanchian, 2022). Technology-based education is considered advanced, and the American Heart Association (AHA) supports hybrid learning [10] (AHA, 2020). Therefore, the CRSTP application has been developed into a comprehensive CPR training program based on evidence-based modules. SCPR focuses on skill development, even without real CPR events. It uses audio and visual aids to improve personalized learning outcomes, aligning with research indicating higher satisfaction with video-based learning [12] AbuFarha et al. (2020). In this study, both Group A and Group B participants showed significantly enhanced CPR knowledge and skills post-CPR Formal Training Programme (CPRFTP) compared to before training. Notably, while scores improved, demographic data and variables remained unchanged. Prior research by [13] Lee et al. (2023) and [1] Lim et al. (2022) suggests smartphone and technology-based training, like the SCPR app, may be more effective than traditional methods, highlighting its potential as a viable alternative. This underscores SCPR’s capacity to enhance competency, especially in scenarios with limited formal training opportunities. Considering CPRFTP and SCPR’s effectiveness in improving skills and knowledge, both methods are recommended for healthcare providers (HCP) and potentially for the community [14] (Ahmad et al., 2023).
CPR training is crucial for healthcare providers (HCPs) to maintain skills. The CPRFTP program effectively boosted CPR knowledge and skills immediately post-training, but skills declined in the control group after two months. To address this, integrating advanced technology-based CPR training like the SCPR app is recommended, aligning with research advocating for combining traditional and advanced methods [15] Karnjus et al. (2023). Developed during the COVID-19 pandemic, SCPR addresses the need for continuous education despite movement restrictions [16] (Siripipatthanakul et al., 2023). Both groups showed a decline in CPR proficiency after two months, with the intervention group maintaining higher skills. SCPR enhances and sustains CPR knowledge and skills, supporting participants in maintaining proficiency. Further development, including bilingual support, is needed for optimal outcomes. This study identified several limitations in data collection during the two-month post-training period, particularly the inability to track user progress. This gap made it challenging for researchers to determine if users were consistently practicing CPR with the SCPR application. To address this and maintain the integrity of the randomized controlled pilot study, participants were asked to send video recordings of their CPR performance via WhatsApp and to provide pre- and post-training scores. This ensured adherence to study protocols despite the application’s lack of direct monitoring features. Additionally, researchers acknowledged potential confounding factors, such as education or work experience, which could influence knowledge and skills, and used methods like randomization and data adjustment to mitigate their impact.
5. Conclusion
The SCPR application serves as an effective tool for individuals aiming to refresh their CPR skills and maintain proficiency, enabling users to train and review at their own pace and convenience. While it does not replace formal CPR certification courses, SCPR offers substantial time and cost benefits for healthcare providers and the community. Both study groups demonstrated improvement in CPR knowledge and skills, with the intervention group using SCPR showing higher success rates after two months. Thus, a larger-scale study is recommended to evaluate the effectiveness of technology-based CPR training via smartphones.
Abbreviations
- CPR
Cardiopulmonary resuscitation
- VR
virtual reality
- HCP
healthcare practitioner
- MCQ
multiple-choice questions
- AHA
American Heart Association
- FMHS
Faculty of Medicine and Health Sciences
- HUMS
Hospital Universiti Malaysia Sabah
- NCT
non-central t-distribution
- SCPR
Smart Cardiopulmonary resuscitation
- CPRTM
Cardiopulmonary Resuscitation Theory Module
- CPRPM
Cardiopulmonary resuscitation Practical Module
- CPRFTP
Cardiopulmonary Resuscitation Practical formal educational training program
- DRSCAB
Danger, Respond, Shout for help, Chest compression, Airway, Breathing
- SCA
sudden cardiac arrest
- ERT
Emergency Response Team
- CRSTP
Cardiac Resuscitation Simulation Training Program
- SPSS
Statistical Package for the Social Sciences
- ANOVA
Analysis of Variance
Footnotes
Ethical approval: Ethical approval to conduct the study was obtained from the Faculty of Medicine and Health Sciences Research Ethics Committee at UMS [JKE-tika 4/23 (8)], and the trial was conducted at Hospital Universiti Malaysia Sabah (HUMS) with participants providing written consent beforehand.
Conflict of interest: The authors declare that there are no conflicts of interest associated with this research study.
Author contributions: Conception and design of Study: NA, MM. Literature review: NA, AH. Acquisition of data: FK, SS. Analysis and interpretation of data: FK, SS. Research investigation and analysis: NA, MM. Data collection: HH, RM. Drafting of manuscript: HH, RM. Revising and editing the manuscript critically for important intellectual contents: AH, RM. Data preparation and presentation: FK, SS. Supervision of the research: MM, AH. Research coordination and management: NA, AH. Funding for the research: NA, HH.
Disclosure of funding: This study is self-funded. The authors declare that no funding was received for this research study.
References
- 1. Lim XMA, Liao WA, Wang W, Seah B. The effectiveness of technology-based cardiopulmonary resuscitation training on the skills and knowledge of adolescents: systematic review and meta-analysis. J Med Internet Res. 2022;24(12) doi: 10.2196/36423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.KKM. Guidelines for resuscitation training in ministry of Health Malaysia hospitals & healthcare facilities. Ncort. 2014. 2014. https://www.moh.gov.my/moh/resources/Polisi/GUIDELINES_FOR_RESUSCITATION_TRAINING.pdf .
- 3. Fariduddin MN, Jaafar MJ. Retention of cardiopulmonary resuscitation (CPR) knowledge among undergraduate teacher student in Malaysian university. Malaysian J Med Health Sci. 2021;17(1):3–9. [Google Scholar]
- 4. Hill K, Schumann M, Farren L, Clerkin R. An evaluation of the use of low-fidelity and high-fidelity Mannequins in clinical simulations in a module preparing final year children’s and general nursing students for internship placement. Compr Child Adolesc Nurs. 2023;46(4):295–308. doi: 10.1080/24694193.2023.2232456. [DOI] [PubMed] [Google Scholar]
- 5. Ali DM, Hisam B, Shaukat N, Baig N, Ong MEH, Epstein JL, et al. Cardiopulmonary resuscitation (CPR) training strategies in the times of COVID-19: a systematic literature review comparing different training methodologies. Scand J Trauma Resuscitation Emerg Med. 2021;29(1) doi: 10.1186/s13049-021-00869-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lins C, Friedrich B, Hein A, Fudickar S. An evolutionary approach to continuously estimate CPR quality parameters from a wrist - worn inertial sensor. Health Technol. 2022:161–73. doi: 10.1007/s12553-021-00618-7. [DOI] [Google Scholar]
- 7.Mccaw JM, Yelton SEG, Tackett SA, Rapal RMLL, Gamalinda AN, Reyles AA, et al. Effect of repeat refresher courses on neonatal resuscitation skill decay: an experimental comparative study of in - person and video - based simulation training. 2023. pp. 1–8. [DOI] [PMC free article] [PubMed]
- 8. Whitehead AL, Julious SA, Cooper CL, Campbell MJ. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res. 2016;25(3):1057–73. doi: 10.1177/0962280215588241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Flight L, Julious SA. Practical guide to sample size calculations: superiority trials. Pharmaceut Stat. 2016;15(1):75–9. doi: 10.1002/pst.1718. [DOI] [PubMed] [Google Scholar]
- 10. American Heart Association. Highlights of the 2020 American Heart association guidelines for CPR and ECC. Am J Heart Assoc. 2020;9:32. [Google Scholar]
- 11.Hamed Taherdoost, Madanchian M.Employment of technological-based approaches for creative E-learning; teaching management information systems. 2022. pp. 802–8. [DOI]
- 12. Farha ARK, Rashad M, Hasen E, Mukattash TL, Al-Hashar A, Basheti IA. Evaluation of the effect of video tutorial training on improving pharmacy students’ knowledge and skills about medication reconciliation. Pharm Pract. 2020;18(1):1711. doi: 10.18549/PharmPract.2020.1.1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lee SGW, Hong KJ, Lee SY, Do Shin S, Song KJ, Park JH, et al. Efficacy of distance training program for cardiopulmonary resuscitation utilizing smartphone application and home delivery system. AJEM (Am J Emerg Med) 2023;66:67–72. doi: 10.1016/j.ajem.2023.01.026. [DOI] [PubMed] [Google Scholar]
- 14. Ahmad N, Wider W, Kadir F, Hidrus A, Hassan H. The effectiveness of modified conventional CPR training among North Borneo University Hospital healthcare providers. 2023;18(2):124–30. doi: 10.20473/jn.v18i2.44667. [DOI] [Google Scholar]
- 15.Karnjuš I, Simčič D, Žvanut B.Knowledge retention when using e-learning to supplement face-to face training of first responders. 2023. [DOI]
- 16.Siripipatthanakul S, Muthmainnah M, Asrifan A, Siripipattanakul S, Kaewpuang P, Sriboonruang P, et al. Blended learning and online learning during the COVID-19 pandemic. Vol. 1. Island Publishers; 2023. pp. 44–54. Retrieved from SSRN: https://ssrn.com/abstract=4375583. [Google Scholar]