Abstract
The movements of syringes and medications during an anesthetic case have yet to be systematically documented. We examine how syringes and medication move through the anesthesia work area during a case. We conducted a video-based observational study of 14 laparoscopic surgeries. We defined ‘syringe events’ as when syringe was picked up and moved. Medications were administered to the patient in only 48 (23.6%) of the 203 medication or syringe events. On average, 14.5 syringe movements occurred in each case. We estimate approximately 4.2 syringe movements for each medication administration. When a medication was administered to the patient (either through the IV pump or the patient port), it was picked up from one of 8 locations in the work area. Our study suggests that the syringe storage locations vary and include irregular locations (e.g., patient bed or provider’s pockets). Our study contributes to understanding the complexity in the anesthesia work practices.
Keywords: Anesthesia providers, Work system, Medication preparation and storage
1. Introduction
Medication administration in anesthesia is a complex process that involves multitasking tasks that include clinical decisions, diagnosis, and medication preparation. This occurs within a complex sociotechnical system that involves a number of system risk factors for patient safety events (Sonoda et al., 2018). As many as 1 in 20 perioperative medication administrations result in errors that may lead to patient harm (Nanji et al., 2016). Rather than attributing these events to people alone, it has become increasingly valuable to find causes within the clinical sociotechnical system (Sonoda et al., 2018). Anesthesia providers need to prepare, maintain, and administer multiple medications at the same time (Munoz-Price et al., 2019), while monitoring, communicating, and making decisions (Göras et al., 2019; McDowell et al., 2009), often within environments not designed to support the work (Jurewicz, et al., 2021), and under the conditions of time pressure and uncertainty.
Observing how medication preparation and anesthesia care is actually performed (i.e., work as done) can provide insights into the interactions between people, tasks, tools, and the working environment. A rich understanding of the anesthesia work system can create opportunities to mitigate harm through the design and implementation of informed and integrating interventions. Direct observational studies of medication administration have found that around 4%–10% of medication administrations may contain errors (Samost-Williams and Nanji, 2020). The physical patterns of movement and organization associated with the preparation and administration of medications during an anesthetic case have yet to be systematically documented.
Interventions used to address medication administration adverse events and potential patient harm have yielded a number of innovative and technologically complex solutions (Berdot et al., 2016). While these interventions may work well within one sociotechnical system or for specific case types, few interventions have broadly addressed issues related to medication administration adverse events. An additional issue is how these interventions are evaluated in terms of their success in preventing errors or shaping provider behaviors. This is often done by counting errors and patient safety events, but organizations, units, and individuals may define (and thus report) errors differently (Biro et al., 2022), which can lead to systematic errors in multi-institution evaluations of interventions.
In this study, we explore how anesthesia medication syringes are used, stored, and moved within an operating room (OR), in order to understand more about the processes, variability, efficiency, and risks associated with the anesthetic workspace and physical work environment. Specifically, if we understand where syringes are placed during the medication delivery process within a surgical case and how they are moved through the workspace, then we can better design interventions to reduce the risks of medication-related patient harm events. This supports efforts to examine system vulnerabilities and potential patient safety risks associated with those tools, supplies, and equipment. Using a traditional “time and motion” approach, this work examined the number of times syringes and medications move through the environment, the number of times multiple drugs were handled simultaneously, the anesthesia work areas that are used to store medication within anesthesiology delivery, and the phases of the surgery in which syringe movements occurred.
2. Materials and methods
Video recordings of operating room cases were captured as a part of a prior investigation of operating room systems. Videos consist of 4 camera views of the operating room with one camera focused specifically on the anesthesia work area. (Joseph et al., 2019; Mousavi et al., 2018; Neyens et al., 2019; Wingler et al., 2018, 2020). Our approach included an observational analysis of existing video data to examine the detailed movement of syringes and medications by anesthesia providers. This study was approved by the Medical University of South Carolina’s Institutional Review Board IRB# Pro00048787. All individuals who were recorded in these videos consented to be recorded in the study (including both providers and patients). For this analysis, videos of 14 laparoscopic surgeries were examined that occurred in the same operating room and included five cholecystectomy procedures, six gastric bypasses and/or band removals, one hernia repair, and two gastrectomy procedures. All of the anesthetics were general anesthesia with an endotracheal tube. Anesthesia care was provided in a care-team model with an anesthesiologist supervising a certified registered nurse anesthetist (CRNA) or anesthesia resident. Each surgical case may have involved multiple anesthesia providers providing patient care during the case due to staff breaks and lunches. Syringe motion analysis was limited to the time between the patient entering the OR and leaving the OR, and thus any medication preparation done before the patient entered the room was not included in the analysis.
2.1. System for video coding
The videos were manually coded using a data collection sheet with specific events defined. As this study aimed to examine the medication-related tasks and the position of syringes and medications throughout the anesthesia work area, only medication events were coded. These codes were created based on previous observations in the operating rooms, interviews, and the literature related to medication errors in anesthesia. All of the events that were coded started with a trigger event that had one of two types: a syringe trigger or a storage cabinet trigger. A syringe event was triggered when an anesthesia provider picked up a syringe. Even if a vial was picked up right before a syringe event, the event did not begin until the syringe was picked up. A storage cabinet event was triggered when an anesthesia provider opened the door or a drawer and reached into the medication storage cabinets.
When an event occurred, several variables were coded for the event as outlined in Table 1. The variables coded in this study were determined by the research team with the collaborating clinicians to identify meaningful and identifiable variables in the videos of the anesthesia delivery. These variables were used to describe the tasks associated with the medication management and locations. If a provider’s actions were not visible from any of 4 camera angles, the view was coded as obstructed. Two members of the research team coded the videos and all coding elements were in agreement between the two coders. After the first few videos were coded, the research team and the clinical collaborators reviewed the coding and the videos to verify that the events and the variables were correctly identified in the videos.
Table 1.
Variable definitions used for all events in the data coding.
| Variable | Definition |
|---|---|
| Trigger type | A storage cabinet triggered event, or a syringe triggered event. |
| Pick up location of vial or syringe | Initial location of the vial or syringe being described in the event. The options for the initial location included: the storage cabinet drawer, storage cabinet bottom, work surface, work surface drawer, top of the anesthesia machine, the boom, or a provider’s pockets. |
| Syringe involved | This variable was used to determine if a syringe was picked up and used at any time during the event [Yes] or not [No]. |
| Medication or vial involved | This variable was used to determine if a medication or vial was involved in the event [Yes] or not [No]. |
| More than one medication or syringe at a time | Indicate if multiple medications or syringes were being picked up and moved at the same time [Yes] or only a single item was picked up and moved [No]. |
| Administer medication | The administered medications variable was used to indicate if and how a medication was administered. Options were IV pump, direct, and not administered. |
| Final location of vial or syringe | The final location of vial or syringe at the end of the event. The options for the final location were storage cabinet drawer, work surface drawer, work surface, anesthesia machine, pockets, storage cabinet bottom, boom, garbage, bed, and nothing removed. |
| Phases of surgery | The phases of surgery variable were used to indicate the corresponding phase of the surgery when an event was triggered. Options of this variable include patient preparation phase, intraoperative phase (anesthesia maintenance), or postoperative phase (including emergence). |
2.2. Analysis approach
As this was a descriptive study, descriptive statistics were used to evaluate and summarize the video coding data. The movement of the syringe was then mapped on the architectural drawings of the anesthesia work area layout.
3. Results
The total procedure duration for the 14 surgical cases was on average 75.6 min (standard deviation = 44.8 min). In total, there were 203 medication-related events that involved a syringe. These syringe events mainly occurred during the intraoperative phase (65%), followed by pre-operative phase (31%) and post-operative phase (3.9%). On average, 14.5 syringe movements occurred in each case. For the cases included within this study, interactions with a syringe (the syringe movements) occurred about 7.7 times per hour on average.
3.1. Multitasking
We documented the instances in which an anesthesia provider interacted with more than one medication during one of the events. The data shows that anesthesia providers removed more than one medication from the storage cabinet in 35.3% (41) of the storage cabinet triggered events and in 16.6% (24) of the syringe triggered events. In our study, administrating more than one medication typically occurred more frequently in the intraoperative phase (58.5%) of the surgery, followed by the patient preparation phase (39%), and postoperative phase (2.4%).
3.2. Locations of syringes and medications during syringe involved events
The initial pickup locations of syringes or medication (that is, where the syringes or medication was picked up from) in all the syringe involved events is coded in Table 2 below. The most common initial locations of syringes or vials were work surface (33.0%), storage cabinet drawer (25.6%) and anesthesia machine (23.7%).
Table 2.
Pathways of initial location and put-down location of syringe or vials in syringe involved events.
| Initial pickup location* | Final location | Frequency | Percent |
|---|---|---|---|
| Work surface | Work surface | 27 | 13.3% |
| Storage cabinet drawer | Work surface | 18 | 8.9% |
| Anesthesia machine | Anesthesia machine | 18 | 8.9% |
| Storage cabinet drawer | Anesthesia machine | 13 | 6.4% |
| Anesthesia machine | Patient port | 11 | 5.4% |
| Work surface | Anesthesia machine | 10 | 4.9% |
| Another provider | Anesthesia machine | 6 | 3.0% |
| Work surface | Another provider | 6 | 3.0% |
| Work surface drawer | Work surface | 5 | 2.5% |
| Anesthesia machine | Garbage | 4 | 2.0% |
| Storage cabinet drawer | Patient port | 4 | 2.0% |
| Work surface | Patient port | 4 | 2.0% |
| Work surface drawer | Patient port | 4 | 2.0% |
| Work surface | Storage cabinet drawer | 4 | 2.0% |
| Work surface | Garbage | 3 | 1.5% |
| Work surface drawer | Anesthesia machine | 2 | 1% |
| Anesthesia machine | Another provider | 2 | 1% |
| Work surface drawer | Garbage | 2 | 1% |
| Storage cabinet drawer | Pockets | 2 | 1% |
| Work surface | Pockets | 2 | 1% |
| Anesthesia machine | Storage cabinet drawer | 2 | 1% |
| Storage cabinet drawer | Storage cabinet drawer | 2 | 1% |
| Storage cabinet bottom | Anesthesia machine | 1 | 1% |
| Storage cabinet drawer | Boom | 1 | 1% |
| Pockets | Garbage | 1 | 1% |
| Another provider | Patient port | 1 | 1% |
| IV pump | Patient port | 1 | 1% |
| Anesthesia machine | Pockets | 1 | 1% |
| Work surface drawer unit | Pockets | 1 | 1% |
| Work surface drawer unit | Storage cabinet drawer | 1 | 1% |
| Anesthesia machine | Work surface | 1 | 1% |
| Another provider | Work surface | 1 | 1% |
| Patient bed | Work surface | 1 | 1% |
NOTE:
any event with obstructed views for either the initial location or final location has been omitted from this table n = 41.
We mapped the initial pickup location and the final location for each syringe event. These pathways are shown in Tables 2 and are graphically shown on a layout of the physical environment of the specific OR (Fig. 1). Within Fig. 1, the thickness of the line pathway, the initial and put-down location pathways, represent the frequency of that location pair. More frequent pairings are presented with a thicker line. We observed 33 different pathways of the picked-up and put-down locations of syringes. The most frequently occurred pathways were work surface to work surface (13.3%), storage cabinet drawer to work surface (8.9%) and anesthesia machine to anesthesia machine (8.9%). Approximately 3.5% of the pathways either started or ended with something stored in the providers’ pocket, including storage cabinet drawer to pockets (n = 2), work surface to pockets (n = 2), pockets to garbage (n = 1), anesthesia machine to pockets (n = 1) and work surface of drawer unit to pockets (n = 1).
Fig. 1.
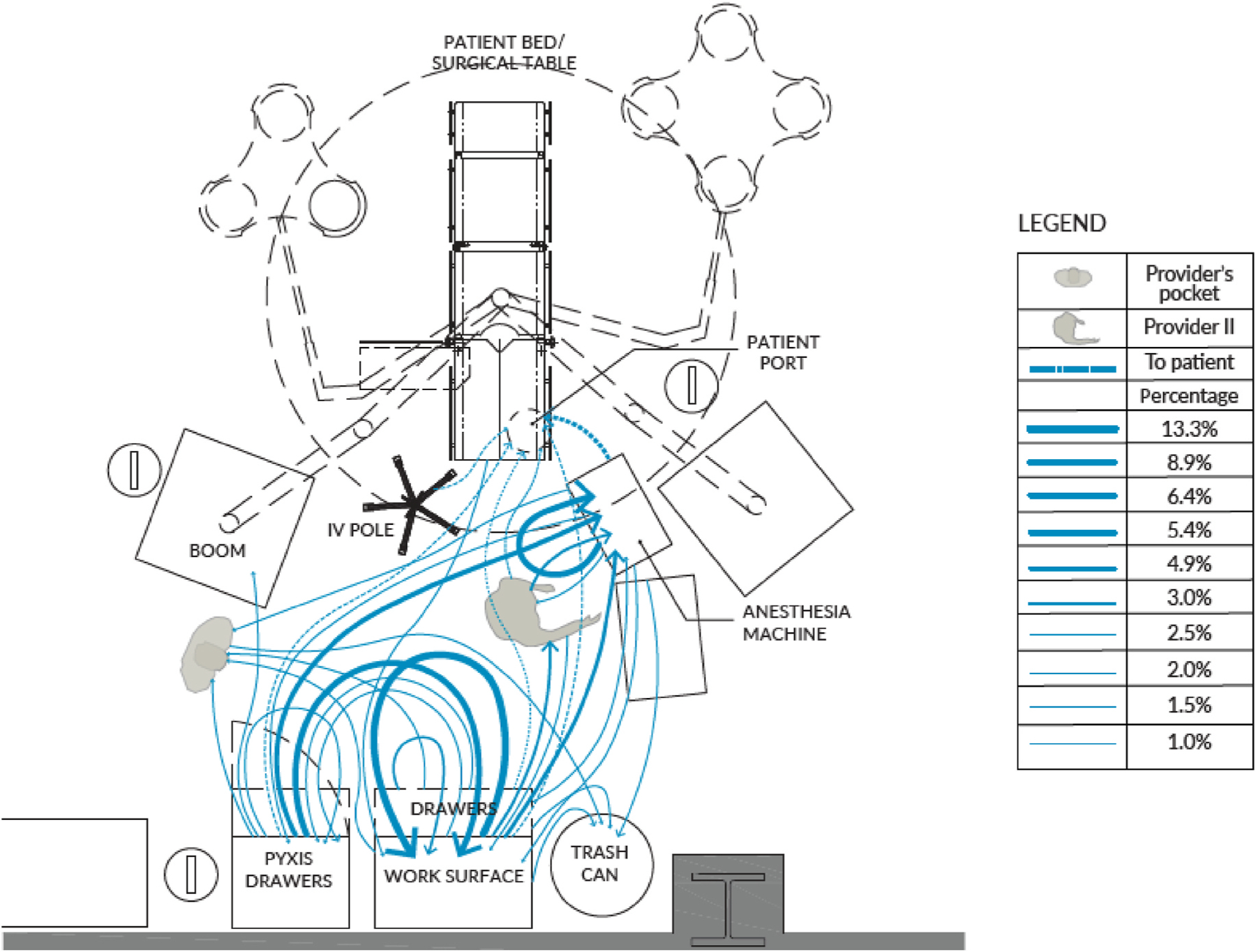
Movement of initial pickup locations and final locations of syringes in syringe involved events across all 14 cases mapped on the room layout. Note: Dotted lines indicate that the medication was administered to the patient.
3.3. Syringe movement during medication administration
Within our coding of the initial trigger and then set down of the syringes, we also documented when a medication was administered to the patient. Of the 203 syringe movements, the medication was retrieved from one location and administered to the patient in 48 (23.6%) of these events. In aggregate, we estimate that there were 4.2 syringe movements for each medication administration. When a syringe was used to administer medication to the patient, it was retrieved from one of 8 locations in the work area (see Table 3). The locations of syringes, immediately preceding medication administration, are shown in Fig. 2.
Table 3.
Syringe location immediately preceding medication administration.
| Initial pickup location | Frequency | Percent |
|---|---|---|
| Anesthesia machine | 20 | 41.7% |
| Work surface | 9 | 18.8% |
| Storage cabinet drawer | 7 | 14.6% |
| Work surface drawer | 6 | 12.5% |
| Another provider | 3 | 6.3% |
| IV pump | 1 | 2.1% |
| Patient bed | 1 | 2.1% |
| Pockets | 1 | 2.1% |
Fig. 2.
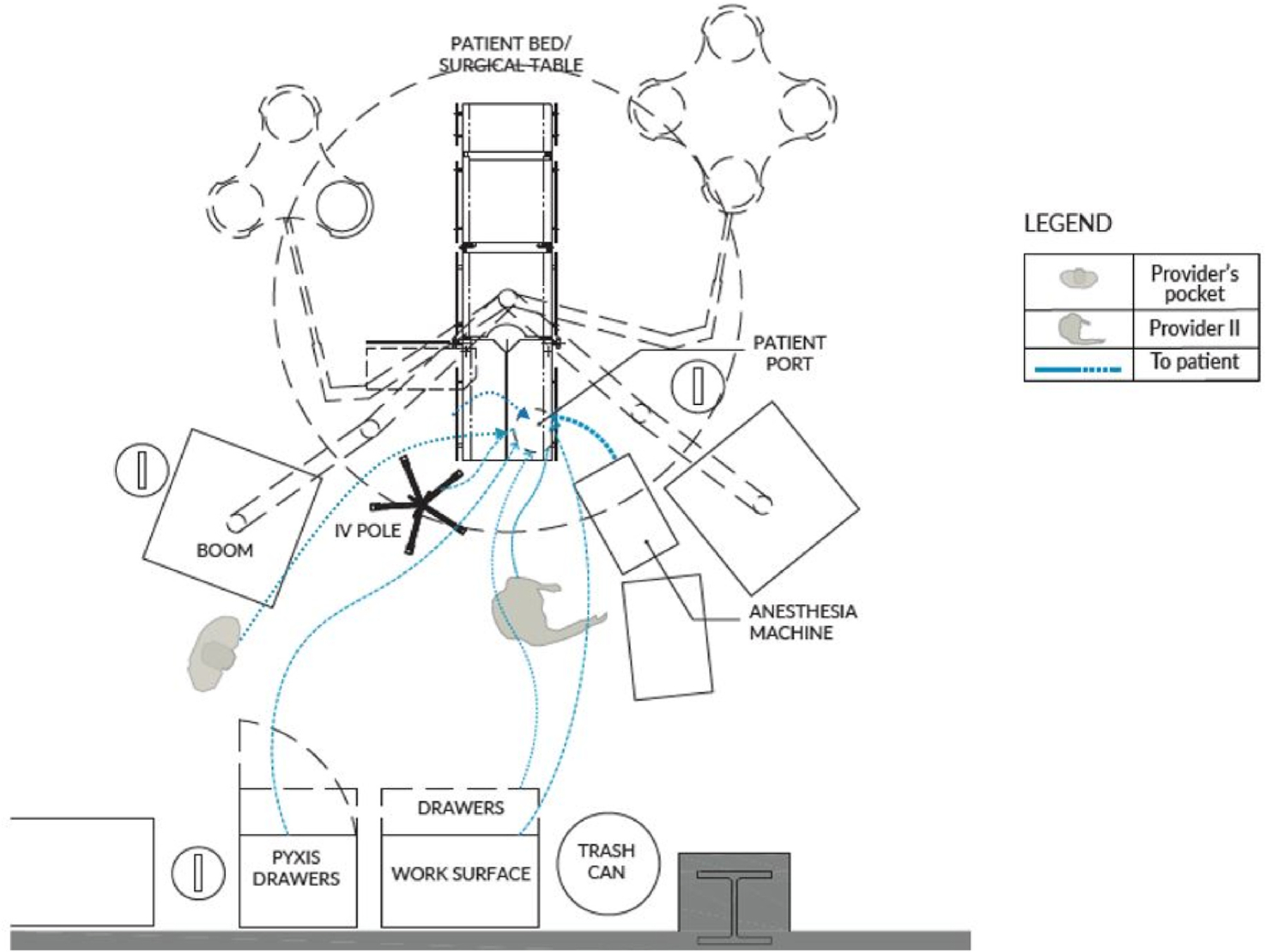
Movement of initial pickup locations and the administration of the medications to the patient across all 14 cases mapped on the room layout.
3.4. Events with syringes being filled with medications
About 31% of events were related to filling syringes with medication. The frequency of filling syringes varied across the phases of the surgical cases. Filling syringes occurred mostly in the intra-operative phase (82%). Filling syringes only occurred 12.5% and 4.7% in the preoperative phase and postoperative phase, respectively. Additionally, when a syringe was labeled, it was frequently not directly administered to the patient, with 76.5% of the syringes that were labeled being set aside for later use.
4. Discussion
The objective of this study was to examine how syringes and medication move through the anesthesia work environment and the anesthesia workstation during laparoscopic surgical cases, and how they are used for medication administration within anesthesiology delivery. Across the cases in this study, there are 8 different areas where medications were picked up and then immediately administered to the patient: storage cabinet drawer, work surface and work surface drawer, IV pump, and the anesthesia machine. Across the surgical cases evaluated, there were approximately 14.5 syringe movements per case which correspond to an average of 4.2 syringe movements for each medication administration across these cases. The different work surfaces and the locations used, in combinations with the frequent movements of the syringes, suggests that there are opportunities for reducing the complexity associated with the task of medication administration during the intraoperative period.
It is important that interventions designed to reduce the likelihood and severity of medication related patient safety events account for the work environment within which the tasks are conducted. Our results provide insights that reveal potential design considerations for interventions to reduce potential patient harm events. The complexity in the organization and the number of locations that syringes are stored is a critical component of intervention design. For example, interventions need to support the quantity of syringes used in anesthesia care and account for the number of locations that are used to store syringes during a case. Additionally, interventions need to account for the cognitive complexity associated with the layout and complexity of mental models associated with the work organization (Biro et al., 2022).
The results also present data that has not previously been well documented. The network of movements of syringes and medications in the anesthesia workstation illustrates that future research should build on the work being done with respect to how people, devices, and equipment are used and move throughout the areas within which anesthesia providers work. Thus, it is possible that interventions may also impact the efficiency and reduced complexity of the work and the work environment while also improving patient safety.
One particular patient safety-related event is a “syringe swap”, when an anesthesia provider picks up a prepared syringe that is not the one they intend to administer to the patient (Grissinger, 2018). Efforts to address syringe swaps and improve the organization of medications have resulted in different types of interventions [e.g., syringe holders (Long et al., 2019), mats (Grigg et al., 2017), and trays (Almghairbi et al., 2018; Wu et al., 2020)] but these events still present a safety risk (Degnan et al., 2020). Generally, studies have focused on standardization in processes or procedures to reduce patient safety risk (Leotsakos et al., 2014; Rozich et al., 2004; Salzwedel et al., 2016), and have not focused on the variability inherent in the process. Interventions for syringe swaps and other medication-related patient safety events need to account for the work environment, the tasks, and the tools used (Grigg et al., 2017; Jurewicz et al., 2021).
There are numerous studies that examine the frequency and propensity of medication events associated with the medication-related care provided in anesthesia delivery (Jones et al., 2018; Portuondo et al., 2019; Preckel et al., 2020) and there is work examining the tasks and the frequency of switching between tasks that occurs for anesthesia providers that are managing multiple sources of information and tasks simultaneously (Betza et al., 2016). Within a systems framework, it has been shown that the work environment (e.g., workspace, work surfaces and general environmental conditions) impacts the tools used, the way work is done, and the patient outcomes associated with that work (Braithwaite et al., 2017). Interventions designed to integrate into this system need to fit within the complex system and the work environments to support the people and tasks required to complete the work. In a review of 896 medication related incidents reported in anesthetic practice in Australia, half (50.4%) of the medication related incidents were related to syringe and medication preparation and 18.9% were syringe swap related (Abeysekera et al., 2005). As shown in our results, the number of locations that syringes and medications were placed represented opportunities for these syringe swaps and medication preparation related patient safety events. Within a systems view of this work, there appears to be a mismatch between the tasks, environment, and tools used to do the work. Thus, there is insufficient work surface area, or a lack of syringe storage tools or spaces for the medications to be set up and organized for use in a case. These are systemic factors that might contribute to the risk of medication related patient safety events.
Future research should examine what factors lead to the storage of syringes in a variety of locations during a case. That is, examining why so many locations are used, and if those locations have some cognitive structure that facilitates a mechanism for case management, or if it is due simply to not enough work surface area for proper medication storage. There may be tools that may assist with organizational strategies or case management that can represent ‘knowledge in the world’ in which information is displayed in such a way that an individual does not need to maintain progress cognitively (Nemeth et al., 2008). Examples of interventions that have been implemented include medication syringe holders and trays (Almghairbi et al., 2018; Wu et al., 2020) and mats (Grigg et al., 2017) with specific spaces allocated for the different syringes and organizes the syringes in meaningful ways that account for how the work is done and how the information can be organized in meaningful ways. The lack of widespread adoption of these tools may not indicate that the tools do not work, but rather that there is a mismatch between the environment, the tools, tasks, and the people within the systems view of this work.
4.1. Limitations
As this study is an analysis of existing videos of laparoscopic procedures, there are some obstructed views. The speed of movement and the tracking of locations may be quicker than a skilled, trained observer could record in real-time (via in-person observations), so video remains a primary means of extracting this type of data. We were not able to track a specific syringe or medication from trigger to administration or storage due to the number of syringes and medications stored in specific areas and the number of syringes and movements. Future work should track specific syringes and medications and their movements. Future studies may also consider adding additional video camera angles to minimize the likelihood of obstructed views. All of the surgery cases we examined occurred in the same OR and all were laparoscopic cases in an intentional effort to control for case complexity and room size and layout. The layout and work surfaces available to anesthesiology providers are not consistent across OR designs, the needs for surgical teams for the patient, and surgical table orientations (Joseph et al., 2021). Thus, these results may not translate to other ORs or surgical case types. Future work should examine if the same types of movement patterns occur in different ORs and with varying case complexity as well as tracking the specific medications and ampules.
4.2. Conclusions
Understanding the specific way syringes are stored, placed, and moved throughout the anesthesia work area can lead to a better understanding of the impact of workstation design and task organization on how medications are used in the delivery of anesthesia care. This can identify opportunities for interventions designed to support the workflow which may, in turn, reduce the risk of some medication related safety events (e.g., syringe swaps). The movement of syringes around the anesthesia work area represents an aspect of the delivery of anesthesia care that has not been well documented and thus is a potential opportunity for systems-based interventions. The complexity of syringe movements across cases may serve as motivation to help organize the medications in a way that helps the providers with organizational solutions that may lead to a reduced patient safety risk. While our study does not seek to link to medication errors or potential patient safety issues, understanding the complexity of the work processes and environment is critical to identifying how interventions will function in those complex environments. Future research should track specific medications, evaluate provider differences in syringe storage and movements, and investigate providers’ decision-making strategies to design interventions that reduce the risk of patient harm while supporting provider resilience in providing care. Additionally, future research should expand this study to other types of cases, and in different OR environments that may have impacts on the syringe storage and movements. Interventions specifically designed to assist with the storage and the handling of syringes may impact the movement of syringes, thus reducing the opportunities for syringe swap events as well as other potential patient harm events. Our results suggest that, in these cases, syringes are stored in multiple locations right before the medication is delivered to patients, including not only regular locations such as anesthesia machine, work surface, storage cabinet drawer, work surface drawer, and IV pumps, but also including irregular locations such as another provider, patient bed, and anesthesia provider’s pockets. Failing to account for the interaction between components of the work system (e.g., the tasks, equipment and tools, the people, and the environment) will continue to result in interventions or policies that do not address systems issues and the associated risks to patient safety.
Acknowledgements
We acknowledge Maya Rucks for her help in the video coding and initial data analysis and Joshua Biro provided edits to an earlier version of the paper. This project was funded under grant number HS026625-01 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services (HHS). The authors are solely responsible for this document’s contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this report as an official position of AHRQ or of HHS.
Footnotes
Prior presentations
A preliminary version of this work has been presented as: Yin, R., D. M. Neyens, C. Tobin, C. Jaruzel, J. Abernathy III, K. Catchpole (2022). Why do syringe swaps occur? Examining syringe movements within the anesthesia work area during surgical procedures. Institute of Industrial and Systems Engineers (IISE) 2022 Annual Conference & Expo, May 21–24, 2022. Seattle, WA.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Abeysekera A, Bergman IJ, Kluger MT, Short TG, 2005. Drug error in anaesthetic practice: a review of 896 reports from the Australian Incident Monitoring Study database. Anaesthesia 60 (3), 220–227. [DOI] [PubMed] [Google Scholar]
- Almghairbi DS, Sharp L, Griffiths R, Evley R, Gupta S, Moppett IK, 2018. An observational feasibility study of a new anaesthesia drug storage tray. Anaesthesia 73 (3), 356–364. 10.1111/ANAE.14187. [DOI] [PubMed] [Google Scholar]
- Berdot S, Roudot M, Schramm C, Katsahian S, Durieux P, Sabatier B, 2016. Interventions to reduce nurses’ medication administration errors in inpatient settings: a systematic review and meta-analysis. Int. J. Nurs. Stud 53, 342–350. [DOI] [PubMed] [Google Scholar]
- Betza SM, Jurewicz KA, Neyens DM, Riggs SL, Abernathy JH, Reeves ST, 2016. Anesthesia maintenance and vigilance: examining task switching. Proc. Hum. Factors Ergon. Soc. Annu. Meet 60 (1), 608–612. 10.1177/1541931213601139. [DOI] [Google Scholar]
- Biro J, Neyens DM, Jaruzel C, Tobin CD, Alfred M, Coppola S, Abernathy JH, Catchpole KR, 2022. “One size” doesn’t “fit all”: understanding variability in anesthesia work practices. Human Factors in Healthcare 2, 100026. 10.1016/J.HFH.2022.100026. [DOI] [Google Scholar]
- Braithwaite J, Herkes J, Ludlow K, Testa L, Lamprell G, 2017. Association between organisational and workplace cultures, and patient outcomes: systematic review. BMJ Open 7 (11), e017708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degnan DD, Bullard TN, Davis MBH, 2020. Risk of patient harm related to unnecessary dilution of ready-to-administer prefilled syringes: a literature review. J. Infusion Nurs 43 (3), 146–154. [DOI] [PubMed] [Google Scholar]
- Göras C, Olin K, Unbeck M, Pukk-Härenstam K, Ehrenberg A, Tessma MK, Nilsson U, Ekstedt M, 2019. Tasks, multitasking and interruptions among the surgical team in an operating room: a prospective observational study. BMJ Open 9 (5), e026410. 10.1136/bmjopen-2018-026410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigg EB, Martin LD, Ross FJ, Roesler A, Rampersad SE, Haberkern C, Low DKW, Carlin K, Martin LD, 2017. Assessing the impact of the anesthesia medication template on medication errors during anesthesia: a prospective study. Anesth. Analg 124 (5). [DOI] [PubMed] [Google Scholar]
- Grissinger M, 2018. Key vulnerabilities in the surgical environment: container mix-ups and syringe swaps. P T : A Peer-Reviewed Journal for Formulary Management 43 (3), 129–167. [PMC free article] [PubMed] [Google Scholar]
- Jones PM, Cherry RA, Allen BN, Jenkyn KMB, Shariff SZ, Flier S, Vogt KN, Wijeysundera DN, 2018. Association between handover of anesthesia care and adverse postoperative outcomes among patients undergoing major surgery. JAMA 319 (2), 143–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph A, Khoshkenar A, Taaffe KM, Catchpole K, Machry H, Bayramzadeh S, 2019. Minor flow disruptions, traffic-related factors and their effect on major flow disruptions in the operating room. BMJ Quality & Amp; Safety 28 (4), 276. 10.1136/bmjqs-2018-007957. LP – 283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph A, Neyens D, Mihandoust S, Taaffe K, Allison D, Prabhu V, Reeves S, 2021. Impact of surgical table orientation on flow disruptions and movement patterns during pediatric outpatient surgeries. Int. J. Environ. Res. Publ. Health 18 (Issue 15). 10.3390/ijerph18158114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jurewicz KA, Neyens DM, Catchpole K, Joseph A, Reeves ST, Abernathy JH, 2021. Observational study of anaesthesia workflow to evaluate physical workspace design and layout. Br. J. Anaesth 126 (3), 633–641. 10.1016/J.BJA.2020.08.063. [DOI] [PubMed] [Google Scholar]
- Leotsakos A, Zheng H, Croteau R, Loeb JM, Sherman H, Hoffman C, Morganstein L, O’Leary D, Bruneau C, Lee P, Duguid M, Thomeczek C, Schrieck, De Loos, van der E, Munier B, 2014. Standardization in patient safety: the WHO High 5s project. Int. J. Qual. Health Care 26 (2), 109–116. 10.1093/intqhc/mzu010. [DOI] [PubMed] [Google Scholar]
- Long DR, Doney A, Bartels DL, Tan CE, Sayal PK, Anderson TA, Agarwala AV, 2019. Anesthesia workspace cleanliness and safety: implementation of a novel syringe bracket using 3D printing techniques. Anesthesiology Research and Practice. 10.1155/2019/2673781, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell SE, Ferner HS, Ferner RE, 2009. The pathophysiology of medication errors: how and where they arise. Br. J. Clin. Pharmacol 67 (6), 605–613. 10.1111/j.1365-2125.2009.03416.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mousavi ES, Jafarifiroozabadi R, Bayramzadeh S, Joseph A, San D, 2018. An observational study of door motion in operating rooms. Build. Environ 144, 502–507. 10.1016/j.buildenv.2018.08.052. [DOI] [Google Scholar]
- Munoz-Price LS, Bowdle A, Johnston BL, Bearman G, Camins BC, Dellinger EP, Geisz-Everson MA, Holzmann-Pazgal G, Murthy R, Pegues D, 2019. Infection prevention in the operating room anesthesia work area. Infect. Control Hosp. Epidemiol 40 (1), 1–17. [DOI] [PubMed] [Google Scholar]
- Nanji KC, Patel A, Shaikh S, Seger DL, Bates DW, 2016. Evaluation of perioperative medication errors and adverse drug events. Anesthesiology 124 (1), 25–34. 10.1097/ALN.0000000000000904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemeth C, Wears R, Woods D, Hollnagel E, Cook R, 2008. Minding the gaps: creating resilience in Health care. In: Advances in Patient Safety. Agency for Healthcare Research and Quality (US), Rockville (MD). [PubMed] [Google Scholar]
- Neyens DM, Bayramzadeh S, Catchpole K, Joseph A, Taaffe K, Jurewicz K, Khoshkenar A, San D, Group RORS, 2019. Using a systems approach to evaluate a circulating nurse’s work patterns and workflow disruptions. Appl. Ergon 78, 293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portuondo JI, Shah SR, Singh H, Massarweh NN, 2019. Failure to rescue as a surgical quality indicator: current concepts and future directions for improving surgical outcomes. Anesthesiology 131 (2), 426–437. 10.1097/ALN.0000000000002602. [DOI] [PubMed] [Google Scholar]
- Preckel B, Staender S, Arnal D, Brattebø G, Feldman JM, Ffrench-O’Carroll R, Fuchs-Buder T, Goldhaber-Fiebert SN, Haller G, Haugen AS, Hendrickx JFA, Kalkman CJ, Meybohm P, Neuhaus C, Østergaard D, Plunkett A, Schüler HU, Smith AF, Struys MMRF, et al. , 2020. Ten years of the Helsinki Declaration on patient safety in anaesthesiology: an expert opinion on peri-operative safety aspects. European Journal of Anaesthesiology | EJA 37 (7). [DOI] [PubMed] [Google Scholar]
- Rozich JD, Howard RJ, Justeson JM, Macken PD, Lindsay ME, Resar RK, 2004. Standardization as a mechanism to improve safety in Health care. Joint Comm. J. Qual. Saf 30 (1), 5–14. 10.1016/S1549-3741(04)30001-8. [DOI] [PubMed] [Google Scholar]
- Salzwedel C, Mai V, Punke MA, Kluge S, Reuter DA, 2016. The effect of a checklist on the quality of patient handover from the operating room to the intensive care unit: a randomized controlled trial. J. Crit. Care 32, 170–174. [DOI] [PubMed] [Google Scholar]
- Samost-Williams A, Nanji KC, 2020. A systems theoretic process analysis of the medication use process in the operating room. Anesthesiology 133 (2), 332–341. [DOI] [PubMed] [Google Scholar]
- Sonoda Y, Onozuka D, Hagihara A, 2018. Factors related to teamwork performance and stress of operating room nurses. J. Nurs. Manag 26 (1), 66–73. [DOI] [PubMed] [Google Scholar]
- Wingler D, Joseph A, Bayramzadeh S, Robb A, 2020. Using virtual reality to compare design alternatives using subjective and objective evaluation methods. HERD: Health Environments Research & Design Journal 13 (1), 129–144. [DOI] [PubMed] [Google Scholar]
- Wingler D, Machry H, Bayramzadeh S, Joseph A, Allison D, 2018. Comparing the effectiveness of four different design media in communicating desired performance outcomes with clinical end users. HERD: Health Environments Research & Design Journal 12 (2), 87–99. 10.1177/1937586718796626. [DOI] [PubMed] [Google Scholar]
- Wu X, Ye G, Guo L, 2020. A novel device to prevent errors in medication dosing and dispensing. Transl. Pediatr 9 (2), 140–143. 10.21037/TP.2020.02.05. [DOI] [PMC free article] [PubMed] [Google Scholar]


