Since it was first introduced three decades ago, computed tomography has become an important investigative tool. Conall Garvey and Rebecca Hanlon explain different types of scanners and what they are used for
Computed tomography was first introduced 30 years ago and has since become an integral part of clinical practice.1 Because of rapid advances in technology few clinicians are aware of the scope and limitations of the different types of scanners. This review describes the three main types of computed tomographic scanner that are used in routine clinical practice and discusses their use in the investigation of a wide range of different conditions. It also flags up differing views on the relative merits of computed tomography versus magnetic resonance imaging.
Summary points
The role of “conventional” computed tomography is declining and has been superseded by spiral scanning
Multislice scanning is faster and more versatile than spiral scanning and facilitates newer applications, particularly in vascular, cardiac, and colonic imaging
Multislice computed tomography is expensive and has implications for workload and data storage
Concern has been raised about the increasing radiation dose from examinations by computed tomography
As magnetic resonance scanners become faster and availability increases, considerations of dose may relegate computed tomography to a secondary role for many applications
Methods
The information contained in this review was gathered from several sources. These include many years of personal experience using computed tomography and magnetic resonance imaging, discussions with manufacturers of equipment, and knowledge of radiation dosimetry issues, supported by a search of Medline and the Cochrane databases for systematic reviews comparing computed tomography and magnetic resonance imaging.
Evolution of computed tomographic scanners
By today's standards early computed tomographic scanners were extremely slow and required enormous computer facilities to generate comparatively crude scans. Improvements in tube technology and computer hardware and software have shortened scan times and improved the resolution of scans. The incorporation of slip ring technology into scanners in the late 1980s resulted in the development of spiral (helical) scanners. More recently, multislice scanners with scan times of less than a second have become widely available. These important technological changes have been linked to newer and faster computers to provide the systems that are currently available.
Conventional computed tomographic scanners
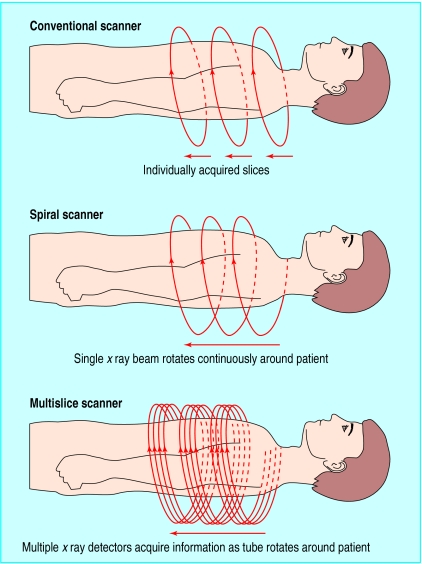
In first generation (conventional) scanners, the tube produces a narrow beam of x rays that passes through the patient and is picked up by a row of detectors on the other side (fig 1). The tube and detectors are positioned on opposite sides of a ring that rotates around the patient. The physical linkages between the power cables and the tube mean that the tube is unable to rotate continuously. After each rotation the scanner must stop and rotate in the opposite direction. Each rotation acquires an axial image, typically with a slice thickness of 1 cm, taking approximately 1 second per rotation. The table moves the patient a set distance through the scanner between each slice.
Figure 1.
Three different types of computed tomographic scanners and how they work
Conventional scanners have some limitations. The scan time is slow, and scans are prone to artefact caused by movement or breathing. Scanners have a poor ability to reformat in different planes, studies of dynamic contrast are impossible, and small lesions between slices may be missed.
Many departments are now acquiring spiral scanners, and it is anticipated that over the next few years half the scanners in the United Kingdom will be multislice scanners.2 Often a conventional scanner is retained alongside a new scanner. Conventional scanners still have a role, mainly in non-contrast examinations that do not require fast scanning for optimal vascular enhancement. A large bulk of the computed tomography workload of many large radiology departments consists of routine examinations of the head by unenhanced computed tomography—for example, for cerebral infarcts or haemorrhage. These can still be performed satisfactorily on an existing conventional scanner, thus freeing time on the spiral scanner.
Spiral (helical) computed tomographic scanners
The incorporation of slip ring technology into the design of scanners in the late 1980s removed the need for a rigid mechanical linkage between the power cables and the x ray tube. This “simple” development, by enabling the tube to rotate in one direction indefinitely, has re-established computed tomography at the forefront of imaging. While the tube is rotating, the table supporting the patient also moves continuously so that a volume of tissue rather than individual slices is scanned. The data are then reformatted automatically to display the images as axial slices. High quality reconstructed (reformatted) images in coronal, sagittal, and oblique planes can be readily acquired on a workstation.
Spiral scanning has several advantages. The scan time is much shorter than that of conventional computed tomography. Closely spaced scans are readily obtained, allowing good quality reconstructions in different planes. Lesions can be evaluated during different phases of contrast enhancement. Computed tomographic angiography is possible, and the likelihood that a small lesion may be overlooked is less/smaller. Spiral computed tomography is a powerful diagnostic tool. A spiral scanner is not as fast as a multislice scanner but is considerably cheaper (typically one third to one half the cost of a multislice scanner (GE Medical Systems, personal communication)).
Multislice computed tomographic scanners
A multislice (multidetector) computed tomographic scanner can be considered as a “turbocharged” spiral scanner. Conventional and spiral scanners use a single row of detectors to pick up the x ray beam after it has passed through the patient. Multislice scanners currently have up to eight active rows of detectors, and scanners under development will use direct direct digital detectors on flat panels (GE Medical Systems, personal communication). The increased number of detectors and tube rotation times that take a fraction of a second combine to give faster coverage of a given volume of tissue. Newer multislice scanners also come with faster computer software, offering increased reconstruction and postprocessing capabilities (see figs 2–4, for example).
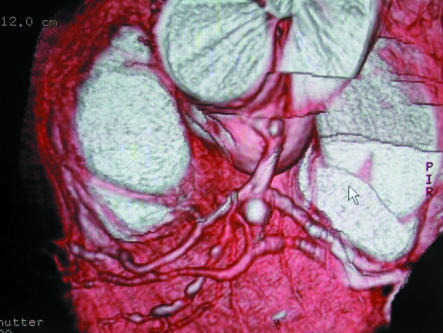
Figure 2.
Multislice computed tomography for vascular imaging (volume rendered image showing liver and kidneys). Multislice technology may show from the renal arteries to the ankle with a single injection.7,8 As magnetic resonance angiography develops, the lack of radiation and use of non-toxic magnetic resonance contrast agents may render computed tomographic angiography obsolete (courtesy of GE Medical Systems)
Figure 4.
Spiral computed tomography for colonography (this coronal reconstruction shows a sawtooth edge to the abdominal wall produced by breathing artefact). This study was performed on a spiral scanner. This artefact should be less common with multislice scanning.13 Computed tomographic colonography (virtual colonoscopy) was first introduced in the mid-1990s as a non-invasive technique to image the colon.14 Thin axial slices through the abdomen are obtained in supine and prone positions. These may be reconstructed into three dimensional (surface rendered) images giving the impression of viewing the large bowel via an endoscope. This technique will expand with further improvements in imaging technology and experience of observers.15
The use of a four row scanner offers various options to the radiologist. A large volume of the patient can be scanned during a single breath hold (for example, thorax, abdomen, and pelvis in a trauma patient in 20 seconds). Alternatively, a normal volume can be examined by using much finer slices (for example, acquisition of 1 mm sections through the chest in 20 seconds, improving detail and facilitating reformatted images of better quality). In theory, the time taken to perform a scan with a multislice scanner with four detectors would be a quarter of that of a single slice spiral scanner. In practice, a multislice scanner acquires images two to three times faster than a single slice scanner.3
Use of a multislice scanner will considerably increase throughput of patients compared with a conventional scanner, but the throughput will be similar to that achieved with a modern spiral scanner. Multislice scanners generate an increased amount of data compared with single slice scanners, and in practice the throughput of patients is limited by the time taken to image and reconstruct these data. For institutions with a picture archive and communication system (PACS, the “filmless hospital”), the volume of data resulting from studies of multislice computed tomography can pose considerable strain on storage systems. If more patients are scanned and more information acquired during each examination the radiologist's workload will significantly increase.
x Ray tubes are expensive. In the United Kingdom in 2002, a typical spiral scanner can expect to have one tube replaced per year at a cost of £30 000-40 000. The life of the tube for a multislice scanner should be the same as the tube for a single slice scanner if the same techniques are used. Since many patients examined on a multislice scanner will have multiphase and fine slice studies, the tube life may be shorter, requiring more regular replacement.
Advantages of multislice scanning
Faster acquisition compared with spiral scanner
Better for uncooperative, breathless, and trauma patients
A larger area can be covered during a single acquisition
Less movement artefact
Lifelike multiplanar reformats
Improved vascular and cardiac imaging
Potential for faster throughput of patients
Disadvantages of multislice scanning
Increased capital cost
Increased costs for replacement tubes and data storage
More time required to analyse data
Increased radiological workload
Potential for higher radiation dose
Effect of computed tomography on radiation dose
Computed tomography accounts for 40% of medical diagnostic radiation but represents only 4% of radiology examinations.4 Any expansion in the use of computed tomography will need to be balanced against the radiation dose. Readers are referred to the guidelines published and regularly upgraded by the Royal College of Radiologists.5
The views whether multislice scanners will lead to an increase or decrease in population dose from examinations by computed tomography differ. Generally the dose from a multislice spiral scanner is slightly greater than from a single slice spiral scanner. Because multislice scanners are faster, more slices tend to be performed and more images acquired in different phases of enhancement, which results in an increased dose of radiation. In 1992, the National Radiological Protection Board pointed out the potential for high doses to patient from inappropriate examinations by computed tomography.6 More recently, the US Food and Drug Administration raised the alarm about the dangers of unnecessary scans and excessive radiation. Particular concerns were raised about the use of computed tomography in children and patients of small stature and the increasing use of the technique for screening for lung cancer and cardiac artery disease (see web link in patient information).
Computed tomography is a highly useful tool for solving problems. It should, however, never be allowed to replace proper history taking and clinical examination. Radiologists must use their knowledge to ensure that requests for computed tomography are appropriate and use low dose protocols targeted at the clinical problem.
Magnetic resonance or computed tomography?
The lack of systematic reviews comparing magnetic resonance imaging and computed tomography is notable. A search of the Cochrane database found no complete reviews and only a small number of quality assessed systematic reviews. In our view, many radiologists practising the two techniques are rivals. On the positive side, this rivalry has been responsible for many innovations, but it may encourage proponents to advocate their particular technique in a biased fashion. This, combined with a dearth of high quality systematic reviews, could lead to confusion among clinicians when trying to determine which investigation is most appropriate for a given condition.
In general, magnetic resonance is excellent for imaging soft tissue and bone marrow. It is not generally used in patients with acute trauma, in the evaluation of the lungs, or in the assessment of cortical bone. Currently, most studies by magnetic resonance imaging take much longer than a spiral or multislice scan of the same area. Computed tomography is generally better for examinations of areas prone to motion, such as the lungs and the bowel. Availability of scanner time and cost are the major limiting factors for magnetic resonance imaging, whereas radiation dose and potential nephrotoxicity from iodinated contrast agents are the limiting factors for computed tomography.
Computed tomography remains the primary imaging technique for acute cranial trauma, but for most other cerebral applications magnetic resonance imaging has superseded computed tomography. In the abdomen, computed tomography is generally superior to magnetic resonance imaging for the hollow viscera. Examination of the solid organs is more contentious. State of the art computed tomography and magnetic resonance imaging are competitive for liver, spleen, kidneys, and possibly pancreas. Magnetic resonance imaging is superior for the pelvic organs. Which test to perform will be influenced by local expertise, availability of equipment, cost, and radiation dose.
Patient information
National Radiological Protection Board (www.nrpb.org.uk/Topics.htm). Explains in layman's terms the benefits and risks associated with medical x ray examinations.
Radiological Society of North America (www.rsna.org/enews/sepb.html). News bulletin highlighting the concerns expressed by the US Food and Drug Administration over the radiation risks of computed tomography.
General Electric (www.gemedicalsystems.co.uk). Website of one of the major manufacturers of radiography equipment. Access the radiology icon and follow the prompts for computed tomography to find out more.
Spiral scanning has enabled the development of computed tomographic fluoroscopy, providing real time imaging for intervention procedures guided by computed tomography.16,17 For example, when percutaneous lung biopsies are performed the needle can be guided in through the lung under direct vision. This means that the track of the needle can be constantly adjusted so that it is in line with the target area. In theory the number of punctures to the lung could be lowered appreciably, thus reducing the time of the procedure and the discomfort to the patient.18
Magnetic resonance imaging has a limited role in patients with major trauma and in patients on ventilators because of the challenge posed by the magnetic environment to anaesthetics and monitoring of patients. Contraindications for magnetic resonance imaging include pacemakers and certain metallic implants.
Most units that perform magnetic resonance imaging report a failure rate of 3-6% as a result of patients' claustrophobia or inability to keep still during the long scanning times, particularly in young or elderly patients. Primary care doctors often have to reassure patients who are anxious about undergoing magnetic resonance imaging (M Duffy, personal communication). As the technology improves, scanners are becoming faster and, with the introduction of “open” magnets and dedicated extremity magnets, claustrophobia may become a thing of the past.
Multislice computed tomography, with its speed and capability of multiplanar reformats, can be substituted for magnetic resonance imaging in several clinical situations. But if magnetic resonance imaging is indicated as the first line investigation then this is preferable because of the lack of ionising radiation.
Additional educational resources
Reisner MF, Takahashi M, Modic M, Bruening R. Multislice CT. Berlin: Springer, 2001.
Kearney SE, Garvey CJ. Unravelling the helix—a physician's guide to spiral computed tomography. Postgrad Med J 1998;74:96-100.
Fletcher JG, Johnson CD. Computed tomographic colonography: current and future status for colorectal cancer screening. Semin Roentgenol 2000;35:385-93.
Rydberg J, Buckwalter KA, Caldemeyer KS, Phillips MD, Conces DJ Jr, Aisen AM, et al. Multisection CT: scanning techniques and clinical applications. Radiographics 2000;20:1787-806.
Figure 3.
Multislice computed tomography for cardiac imaging (surface rendered 1 mm multislice acquisition showing coronary arteries). Imaging of the coronary arteries using electron beam scanning and single slice spiral scanning is established.9–12 With multislice scanning, thin slices of the whole heart can be obtained in a single breath hold, resulting in high quality images and lifelike three dimensional reconstructions (courtesy of GE Medical Systems)
Footnotes
Competing interests: None declared.
References
- 1.Hounsfield GN. Computerized transverse axial scanning (tomography). 1. Description of system. Br J Radiol. 1973;46:1016–1022. doi: 10.1259/0007-1285-46-552-1016. [DOI] [PubMed] [Google Scholar]
- 2.Lewis MA. Multislice CT; opportunities and challenges. Br J Radiol. 2001;74:779–781. doi: 10.1259/bjr.74.885.740779. [DOI] [PubMed] [Google Scholar]
- 3.Dawson P, Lees WR. Multislice technology in computed tomography. Clin Radiol. 2001;56:302–309. doi: 10.1053/crad.2000.0651. [DOI] [PubMed] [Google Scholar]
- 4.Shrimpton PC, Edyvean S. CT scanner dosimetry. Br J Radiol. 1998;71:1–3. doi: 10.1259/bjr.71.841.9534691. [DOI] [PubMed] [Google Scholar]
- 5.Making the best use of a department of clinical radiology—guidelines for doctors. 4th ed. London: Royal College of Radiologists, London; 1998. [Google Scholar]
- 6.National Radiological Protection Board. Documents of the NRPB—patient dose reduction in diagnostic radiology. NRPB: Didcot; 1990. p. 1. (3). [Google Scholar]
- 7.Rubin GD, Shiau MC, Schmidt AJ. Computed tomographic angiography: historical perspective and new state of the art using multi detector row helical computed tomography. J Comput Assist Tomogr. 1999;23(suppl 1):83–90. [PubMed] [Google Scholar]
- 8.Rubin GD, Schmidt AJ, Logan LJ, Sofilos MC. Multi-detector row CT angiography of lower extremity arterial inflow and runoff: initial experience. Radiology. 2001;221:146–158. doi: 10.1148/radiol.2211001325. [DOI] [PubMed] [Google Scholar]
- 9.Budoff MJ, Brundage BH. Electron Beam computed tomography: screening for coronary artery disease. Clin Cardiol. 1999;22:554–558. doi: 10.1002/clc.4960220904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stanford W, Thompson BH. Imaging of coronary artery calcification. It's importance in assessing atherosclerotic disease. Radiol Clin North Am. 1999;37:257–272. doi: 10.1016/s0033-8389(05)70095-6. [DOI] [PubMed] [Google Scholar]
- 11.Rabin DN, Rabin S, Mintzer RA. A pictorial review of coronary artery anatomy on spiral CT. Chest. 2000;118:488–491. doi: 10.1378/chest.118.2.488. [DOI] [PubMed] [Google Scholar]
- 12.Ohnesorge B, Flohr T, Becker C, Kopp A, Knez A, Reiser MF, et al. Cardiac imaging by means of electrocardiographically gated multisection spiral CT: initial experience. Radiology. 2000;217:564–571. doi: 10.1148/radiology.217.2.r00nv30564. [DOI] [PubMed] [Google Scholar]
- 13.Hara AK, Johnson CD, MacCarty RL, Welch TJ, McCollough CH, Harmsen WS. CT colonography: single- versus multi-detector row imaging. Radiology. 2001;219:461–465. doi: 10.1148/radiology.219.2.r01ma28461. [DOI] [PubMed] [Google Scholar]
- 14.Vining DJ. Virtual colonoscopy. Gastrointest Endosc Clin N Amer. 1997;7:285–291. [PubMed] [Google Scholar]
- 15.Gluecker T, Jornod P, Proietti S, Keller W, Blum A, Dorta G, et al. CT colonography (virtual colonoscopy) with multi-detector computed tomography—preliminary results. In: Reisner MF, Takahashi M, Modic M, Bruening R, editors. Multi-slice CT. Berlin: Springer; 2001. pp. 77–82. [Google Scholar]
- 16.Carlson SK, Bender CE, Classic KL, Zink FE, Quam JP, Ward EM, et al. Benefits and safety of CT fluoroscopy in interventional procedures. Radiology. 2001;219:515–520. doi: 10.1148/radiology.219.2.r01ma41515. [DOI] [PubMed] [Google Scholar]
- 17.Wagner LK. CT fluoroscopy: another advancement with additional challenges in radiation management. Radiology. 2001;216:9–10. doi: 10.1148/radiology.216.1.r00jl489. [DOI] [PubMed] [Google Scholar]
- 18.Katada K, Kato R, Anno H, Ogura Y, Koga S, Ida Y, et al. Guidance with real-time CT fluoroscopy; early clinical experience. Radiology. 1996;200:851–856. doi: 10.1148/radiology.200.3.8756943. [DOI] [PubMed] [Google Scholar]