Abstract
Introduction:
Gastric cancer has been reported to occur with mild to moderate mucosal atrophy, particularly after the eradication of Helicobacter pylori (HP) more than 10 years previously. However, no conclusion has been reached on how many years of esophagogastroduodenoscopy should be performed after HP eradication.
Presentation of case:
This was a case of gastric carcinoma of the fundic gland type (GCFGT) 32 years after the eradication of HP, which is the longest posteradication period reported. A 62-year-old male patient was diagnosed with GCFGT after HP eradication and regular esophagogastroduodenoscopy, which revealed a white raised lesion on the anterior wall of the upper part of the body. Endoscopic submucosal dissection was performed for GCFGT, and the vertical and horizontal margins were negative.
Clinical discussion:
In this case, HP was eradicated in 1990, and GCFGT developed 32 years later. To the best of our knowledge, this is the longest case in which gastric cancer appeared after HP eradication. HP eradication therapy for a duodenal ulcer was first reported in 1990, supporting that this is the longest case.
Conclusions:
This is the first case of gastric cancer more than 20 years after the eradication of HP. The endoscopic findings of this case are typical of GCFGT and may be useful when encountering such cases in the future. Therefore, the risk of gastric cancer should be considered for an extended period even after the eradication of HP, and regular esophagogastroduodenoscopy is recommended even after the eradication of HP.
Keywords: case report, duodenal ulcer, endoscopic submucosal dissection, eradication of Helicobacter pylori, esophagogastroduodenoscopy, gastric carcinoma of the fundic gland type
Introduction
Highlights
The patient developed gastric carcinoma of fundic gland type 32 years after eradication of Helicobacter pylori for a duodenal ulcer.
Gastric carcinoma of fundic gland type is a differential diagnosis for white elevated lesions of the stomach.
The possibility of gastric cancer should be considered for long time after HP eradication.
Helicobacter pylori (HP) infection is a major carcinogenic factor of gastric cancer1. HP eradication therapy reduces the risk of gastric cancer occurring in relation to atrophic gastritis2. Additionally, HP eradication therapy for chronic gastritis was approved for coverage by the Japanese national health insurance scheme in February 20133. Although a 30–40% reduction in the risk of gastric cancer has been reported4, gastric cancer is reported to occur at an annual rate of 0.2% even after HP eradication5. Kamada et al.6 reported that gastric cancer can still occur more than 10 years after HP eradication.
No conclusion has been reached on the duration for which esophagogastroduodenoscopy should be performed after HP eradication, although the incidence of gastric cancer in patients with a history of duodenal ulcers is low7. The occurrence of gastric carcinoma of the fundic gland type (GCFGT) has been reported after HP eradication8.
Considering the increase in HP eradication, gastric cancer after HP eradication is expected to increase in the future. We report a case of GCFGT discovered 32 years after HP eradication for a duodenal ulcer that was treated using endoscopic submucosal dissection (ESD).
Presentation of case
This case was approved by the Ethics Committee of the International University of Health and Welfare Hospital (approval number: 23-B-21) and adhered to the principles outlined in the Declaration of Helsinki. Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. This case report has been described in accordance with Surgical CAse REport (SCARE) Criteria9.
A male patient in his early 60s underwent regular esophagogastroduodenoscopy after the eradication of HP. He underwent HP eradication therapy 32 years previously for a duodenal ulcer. The patient has a history of hyperuricemia and hyperlipidemia. His lifestyle includes consuming two shots of alcohol daily and not smoking cigarettes, and he has no family history of any special significance.
Thirty-two years after the eradication of HP, a 5 mm white-tone elevated lesion was found on the anterior wall of the upper part of the gastric body with dendritic vessels within the elevated area (Fig. 1A). Narrow-band imaging and weak magnification revealed surface microstructure, open gland orifices and interorbital spaces, and dendritic vessels (Fig. 1B). Atrophy of the gastric mucosa was C-1 according to the Kimura–Takemoto classification, indicating minimum atrophy. A biopsy of the elevated area showed an irregularly shaped glandular duct below the atypical epithelium, and a diagnosis of GCFGT consisting of atypical cells similar to the main cells was made. A whole-body computed tomography scan showed no evidence of distant or lymph node metastasis. Therefore, ESD was performed for GCFGT (Fig. 1C). The lesion was 8 mm, fading, and Type 0-IIa. The superficial layer was covered by non-neoplastic mucosa, and the number of tumor cells increased similar to the main cells, mainly in the deeper layers of the mucosa, with irregular branching structures, adhesions, and cyst-like dilatations (Fig. 1D). Furthermore, the final pathological diagnosis was U, Type 0-IIa, 8 mm, GCFGT, pT1a, UL0, Ly0, V0, HM0, and VM0 (Fig. 1D). Immunohistochemical staining was positive for pepsinogen 1 (Fig. 2A), MUC6 (Fig. 2B), H+/K+-ATPase (Fig. 2C), and negative for MUC5AC (Fig. 2D). The post-ESD course was uneventful, as shown by esophagogastroduodenoscopy performed 2 months, 8 months, and 1 year after ESD.
Figure 1.
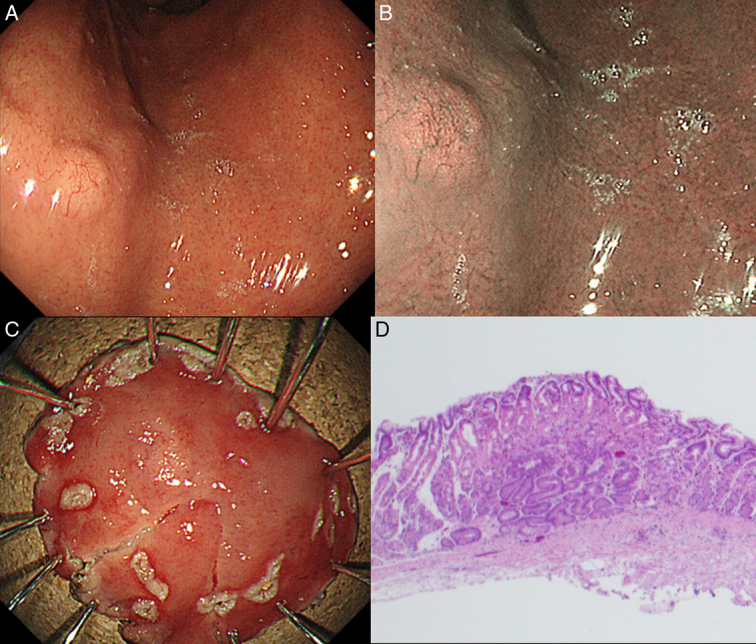
Endoscopic images of gastric carcinoma of the fundic gland type and hematoxylin and eosin (H&E) stained sections. (A) The lesion presents as a submucosal tumor-like white elevated lesion 5 mm in size. (B) Narrow band imaging observation shows dendritic vessels. (C) Endoscopic resection specimen. (D) Pathological examination of the resection specimen showed no vascular and lymphatic invasion (H&E staining, 4×).
Figure 2.
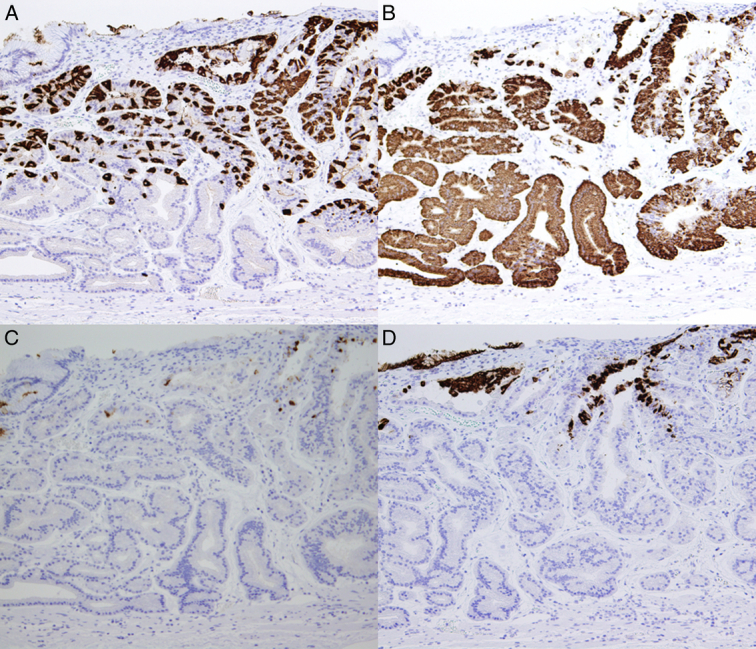
Immunohistochemistry specimen for gastric carcinoma of the fundic gland type. (A) Pathological examination of the specimen showed that pepsinogen 1 was localized in the mucosa. (B) Pathological examination of the resection specimen showed that MUC6 was confined to the mucosa. (C) Tumor cells were positive for H+/K+-ATPase immunostaining. (D) Tumor cells were negative for MUC5AC.
Discussion
In this case, HP was eradicated in 1990, and GCFGT developed 32 years later. To the best of our knowledge, this is the longest case in which gastric cancer appeared after HP eradication. HP eradication therapy for a duodenal ulcer was first reported in 199010, supporting that this is the longest case.
Take et al. monitored 2737 patients after the successful eradication of HP for up to 21.4 years and found 68 cases of gastric cancer during the observation period. Ten years or more after the eradication of HP, the incidence of subsequent gastric cancer was higher in the severe atrophy group (0.67%/year) than in the mild atrophy group (0.15%/year)11. In the present case, a patient with a history of duodenal ulcer and mild atrophy developed GCFGT 32 years after the eradication of HP.
A non-neoplastic epithelium covering cancerous tissue has been previously reported as a specific histological feature of gastric cancer after successful HP eradication12. Moreover, 50 and 5% of gastric cancers that develop >10 and <10 years after HP eradication, respectively, are reportedly covered by a non-neoplastic epithelium13. Kamada et al.5 reported that the characteristics of gastric cancer after successful HP eradication therapy are lesions <20 mm in size, located in the lower middle part of the stomach, microscopically depressed, and differentiated in histological type. In contrast, Take et al.11 reported that diffuse gastric carcinoma is a characteristic feature of gastric carcinoma that developed more than 10 years after HP eradication. In this case, the boundary of GCFGT was unclear, and diagnosing the extent of the carcinoma was difficult. It is necessary to consider the presence of diffuse gastric cancer and GCFGT and recognize that the surface of the cancerous tissue is covered by a non-neoplastic epithelium and presents a gastritis-like appearance when gastric cancer is detected more than 10 years after HP eradication.
GCFGT was first reported by Tohda et al. in 200714, and it presents on conventional esophagogastroduodenoscopy as a submucosal tumor-like raised lesion, with faded and white tone, dilated resinous vessels, and no atrophy of the background mucosa15. Differential diagnoses include gastric submucosal tumor, neuroendocrine tumor, and gastric fundic gland polyp.
Overall, 40% of GCFGT were HP-positive16. Therefore, the presence or absence of HP infection in the development of GCFGT remains unclear. The fact that this patient experienced GCFGT 32 years later indicates that GCFGT may not be directly related to HP infection.
Because this patient had a history of HP eradication, when esophagogastroduodenoscopy was performed for follow-up after HP eradication, regardless of the presence or absence of HP infection, it was necessary to examine the patient with a view to detect differentiated or diffuse-type early gastric cancer and GCFGT. In a report of GCFGT, acid secretion inhibitors were administered in seven of eight cases15; however, this present case has no history of long-term use of acid secretion inhibitors.
Conclusion
We report a case of GCFGT occurring 32 years after HP eradication for duodenal ulcers. Therefore, the risk of gastric cancer should be considered even in cases deemed to be at low risk of developing gastric cancer after HP eradication.
Ethical approval
This case was approved by the Ethics Committee of the International University of Health and Welfare Hospital (approval number: 23-B-21) and adhered to the principles outlined in the Declaration of Helsinki.
Consent
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Sources of funding
None.
Author contribution
D.S.: wrote the manuscript; K.S., M.Y., H.O., T.O., Y.O., Y.N., H.O., Y.S., and Y.K.: reviewed the literature and contributed to manuscript drafting; Y.K.: was responsible for the revision of the manuscript for important intellectual content. All authors approved the final version of the manuscript to be submitted.
Conflicts of interest disclosure
The authors declare no conflicts of interest.
Research registration unique identifying number
This paper is case report. The authors do not need to register this work.
Guarantor
Daisuke Suto and Kiichi Sato.
Data availability statement
The datasets will be shared upon reasonable request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgements
None.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 20 May 2024
Contributor Information
Daisuke Suto, Email: daisuto@iuhw.ac.jp.
Kiichi Sato, Email: kiichi@iuhw.ac.jp.
Masashi Yoshida, Email: masashi@iuhw.ac.jp.
Hiroyoshi Ota, Email: hohta@shinshu-u.ac.jp.
Takaaki Otake, Email: totake@iuhw.ac.jp.
Yosuke Osawa, Email: yosawa@iuhw.ac.jp.
Yoshimasa Nakazato, Email: nakazato@iuhw.ac.jp.
Hironori Ohdaira, Email: hohdaira0428@gmail.com.
Yutaka Suzuki, Email: yutaka@iuhw.ac.jp.
Yutaka Kohgo, Email: ykohgo@iuhw.ac.jp.
References
- 1.Uemura N, Okamoto S, Yamamoto S, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med 2001;345:784–789. [DOI] [PubMed] [Google Scholar]
- 2.Sugano K. Effect of Helicobacter pylori eradication on the incidence of gastric cancer: a systematic review and meta-analysis. Gastric Cancer 2019;22:435–445. [DOI] [PubMed] [Google Scholar]
- 3.Tsuda M, Asaka M, Kato M, et al. Effect on Helicobacter pylori eradication therapy against gastric cancer in Japan. Helicobacter 2017;22:e12415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee YC, Chiang TH, Chou CK, et al. Association between Helicobacter pylori eradication and gastric cancer incidence: a systematic review and meta-analysis. Gastroenterology 2016;150:1113–1124.e5. [DOI] [PubMed] [Google Scholar]
- 5.Kamada T, Hata J, Sugiu K, et al. Clinical features of gastric cancer discovered after successful eradication of Helicobacter pylori: results from a 9-year prospective follow-up study in Japan. Aliment Pharmacol Ther 2005;21:1121–1126. [DOI] [PubMed] [Google Scholar]
- 6.Kamada T, Haruma K, Inoue K, et al. Clinical features of gastric cancer detected after H pylori eradication: comparison between gastric cancer detected in less than and more than 10 years after eradication. Stomach Intestine 2016;51:750–758. [Google Scholar]
- 7.Hansson LE, Nyrén O, Hsing AW, et al. The risk of stomach cancer in patients with gastric or duodenal ulcer disease. N Engl J Med 1996;335:242–249. [DOI] [PubMed] [Google Scholar]
- 8.Chiba T, Kato K, Masuda T, et al. Clinicopathological features of gastric adenocarcinoma of the fundic gland (chief cell predominant type) by retrospective and prospective analyses of endoscopic findings. Dig Endosc 2016;28:722–730. [DOI] [PubMed] [Google Scholar]
- 9.Sohrabi C, Mathew G, Maria N, et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl 2023;109:1136–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rauws EA, Tytgat GN. Cure of duodenal ulcer associated with eradication of Helicobacter pylori. Lancet 1990;335:1233–1235. [DOI] [PubMed] [Google Scholar]
- 11.Take S, Mizuno M, Ishiki K, et al. Risk of gastric cancer in the second decade of follow-up after Helicobacter pylori eradication. J Gastroenterol 2020;55:281–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saka A, Yagi K, Nimura S. Endoscopic and histological features of gastric cancers after successful Helicobacter pylori eradication therapy. Gastric Cancer 2016;19:524–530. [DOI] [PubMed] [Google Scholar]
- 13.Ueyama H, Matsumoto K, Nagahara A, et al. Gastric adenocarcinoma of the fundic gland type (chief cell predominant type). Endoscopy 2014;46:153–157. [DOI] [PubMed] [Google Scholar]
- 14.Tohda G, Osawa T, Asada Y, et al. Gastric adenocarcinoma of fundic gland type: endoscopic and clinicopathological features. World J Gastrointest Endosc 2016;8:244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan K, Brown IS, Kyle T, et al. Chief cell-predominant gastric polyps: a series of 12 cases with literature review. Histopathology 2016;68:825–833. [DOI] [PubMed] [Google Scholar]
- 16.Benedict MA, Lauwers GY, Jain D. Gastric adenocarcinoma of the fundic gland Type: update and literature review. Am J Clin Pathol 2018;149:461–473. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets will be shared upon reasonable request.


