Abstract
Introduction:
Rheumatic heart disease (RHD) poses a substantial global health challenge, especially impacting resource-limited nations, with over 40.5 million cases reported in 2019. The crucial role of Benzathine penicillin G in both primary and secondary prevention, particularly the latter, emphasizes its significance.
Method:
Following PRISMA guidelines, our systematic review explored Medline, Scopus, Google Scholar, and Embase databases from 1990 to 2022. Registered with PROSPERO ), the review utilized quality appraisal tools, including the PRISMA checklist, Cochrane bias tool and Newcastle–Ottawa scale. The objective was to identify and stratify the impact of socio-economic factors on adherence to secondary prophylaxis in RHD.
Results and discussion:
The impact of education on adherence has been found to be significant. Socially disadvantaged environments significantly influenced adherence, shaped by education, socio-economic status, and geographical location and access to healthcare. Surprisingly, lower education levels were associated with better adherence in certain cases. Factors contributing to decreased adherence included forgetfulness, injection-related fears, and healthcare provider-related issues. Conversely, higher adherence correlated with younger age, latent disease onset, increased healthcare resources, and easy access.
Conclusion:
Patient education and awareness were crucial for improving adherence. Structured frameworks, community initiatives, and outreach healthcare programs were identified as essential in overcoming barriers to secondary prophylaxis. Taking active steps to address obstacles like long-distance commute, waiting time, injection fears, and financial issues has the potential to greatly improve adherence. This, in turn, can lead to a more effective prevention of complications associated with RHD.
Keyword: RHD, rheumatic heart disease, secondary prophylaxis
Introduction
Highlights
Rheumatic heart disease (RHD), a global health challenge, underscores the vital role of Benzathine penicillin. In 2019, over 40.50 million cases emphasized its significance in prevention.
Secondary prophylaxis, delivered through intramuscular Benzathine Penicillin, is essential for managing RHD and preventing recurrence.
Adherence to secondary prophylaxis is notably influenced by socio-economic factors, including income, education, geographical location and access to healthcare.
Education plays a crucial role in adherence to secondary prophylaxis in RHD, with varying impacts noted.
Enhancing adherence requires addressing socio-economic conditions. Patient education, community initiatives, and overcoming barriers, like long-distance commutes and injection fears, are crucial for preventing RHD complications effectively.
Rheumatic heart disease (RHD) is a chronic condition primarily affecting the heart valves, occurring as a complication of repetitive episodes of acute rheumatic fever (ARF), caused by an infection with group A β-haemolytic streptococcus (GAS). It most commonly affects children and young adults in resource-limited countries. In 2019, more than 40.5 million cases of RHD were reported worldwide, including almost 0.3 million RHD‐related deaths and 10.7 million years of healthy life lost to RHD1. Administering Benzathine Penicillin G (BPG) has been the cornerstone for the primary and secondary prevention of RHD2. While primary prevention focuses on reducing the incidence of ARF due to GAS infection, secondary prevention emphasized on mitigation of the devastating effect recurrent infection can have on the heart valves, by the provision of long-term medication. Secondary antibiotic prophylaxis with intramuscular benzathine penicillin is the mainstay of the management of RHD2.
With the global use of penicillin as primary as well as secondary prophylaxis, developed countries have gotten rid of the burden of RHD. However, it still ranks high as the leading cause of morbidity and mortality in developing countries3. A significant risk factor for the recurrences of acute rheumatic fever and the possibility of its progression to RHD, and the resultant morbidity and mortality, is low adherence to secondary prophylaxis4.
Lack of knowledge, ease of access to health care, and cost of medicine have been reported as the key factors to low compliance to secondary prophylaxis of RHD by several studies in the past, but these studies have failed to provide a direct comparison between the different strata of the socio-economic determinants4,5. Thus, to address this scenario, this study was conducted to identify and stratify some of the common socio-economic factors influencing adherence to secondary prophylaxis in rheumatic heart disease.
Method
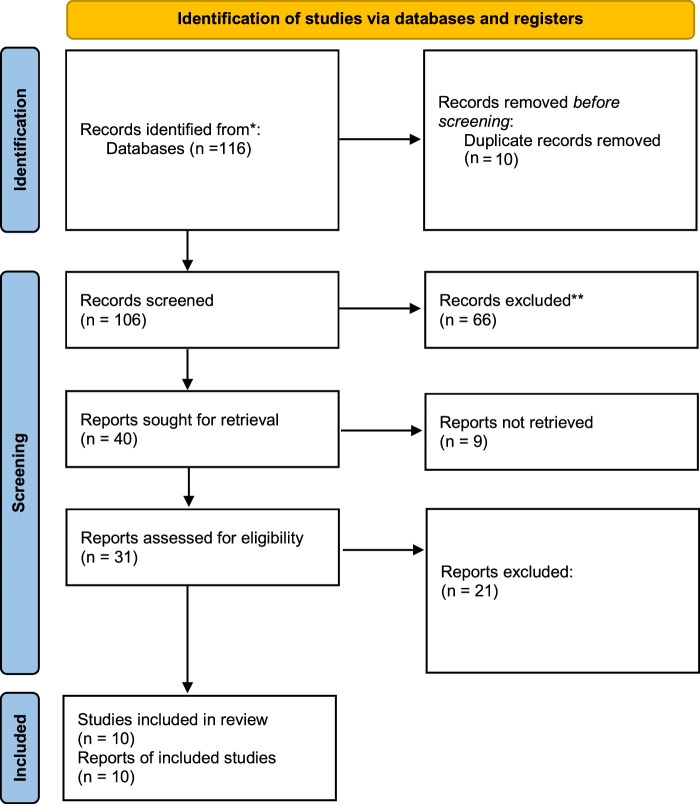
We conducted a systematic review of literature reporting the socio-economic factors influencing adherence to secondary prophylaxis in RHD according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement6 (Fig. 1). This review has been registered with PROSPERO (International Prospective Register of Systematic Reviews).
Figure 1.
PRISMA flow diagram illustrating the search strategy and study selection process. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses. PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers only. *Consider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers). **If automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools. From: Page, et al. 20216 For more information, visit: http://www.prisma-statement.org/.
A comprehensive search strategy was applied and relevant studies from 1990 to 2022 from Medline, Scopus, Google Scholar, and Embase databases were extracted. We used Zotero to store the studies that were considered eligible, with limitations only to publications in the English. Original randomized control trials (RCTs), observational cohort studies, and cross-sectional and case-controlled studies on secondary prophylaxis of rheumatic heart disease were included. Articles were screened for inclusion in a two-step process by two independent reviewers. In cases of dissonance between the two reviewers, a third reviewer was consulted. When studies couldn’t be retrieved, their authors were contacted to request a copy of the publication.
In this study to measure the adherence to secondary prophylaxis among individuals diagnosed with rheumatic heart diseases, the outcomes include: (1). Quantitative adherence rates, including the percentage of patients adhering to secondary prophylaxis (2). Qualitative factors influencing adherence include patient perceptions, beliefs, and attitudes related to socio-economic determinants (3). Identify barriers to adherence (i.e. economic constraints, educational limitations, employment-related issues, and healthcare access obstacles) (4). Identify specific facilitators that enhance adherence, including socio-economic factors that positively influence adherence behaviour (5). Exploration of any disparities in adherence based on different levels of socio-economic determinants, allowing for a nuanced analysis of how these factors impact adherence to secondary prophylaxis in RHD patients.
Search techniques
Using the population, intervention, comparison, and outcome (PICO) criteria, a thorough review of the literature was carried out. Rheumatic heart disease, RHD, adherence, medication adherence, treatment adherence, secondary prophylaxis, secondary prevention, antibiotic prophylaxis, rheumatic fever prevention, socio-economic factors, income, education, employment, occupation and socio-economic determinants as appropriate keywords in the search on databases like PubMed (including MEDLINE and PubMed Central) and Google Scholar.
Inclusion and exclusion criteria
To accomplish our research objectives, we defined precise inclusion and exclusion criteria. Table 1 provides an overview of our criteria.
Table 1.
The criteria adopted for the inclusion of studies.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Individuals of all ages with a confirmed diagnosis of rheumatic heart disease (RHD) | Studies focus solely on primary prophylaxis (preventing initial streptococcal infections) or non-pharmacological interventions |
| Studies reporting on adherence to secondary prophylaxis among RHD patients | Studies that do not provide information on adherence to secondary prophylaxis |
| Studies reporting socio-economic determinants, specifically income, education, employment status, and access to healthcare services | Studies with insufficient data to analyze the influence of socio-economic determinants on adherence |
| Observational, RCTs | Studies that focus solely on other interventions unrelated to socio-economic determinants |
| Studies published in the English language | Review articles, animal studies, case reports, editorials, and commentaries |
RCT, randomised controlled trial.
Quality appraisal
We made use of a variety of quality assessment tools to ensure the validity of the papers we chose. For systematic reviews and meta-analyses, we used the PRISMA checklist and Cochrane bias tool assessment for randomized clinical trials. The Newcastle–Ottawa tool scale was used to evaluate clinical studies that were not randomized. Using the Critical Appraisal Skills Program (CASP) checklist, we evaluated the calibre of the qualitative investigations, as shown in Table 2.
Table 2.
Quality appraisal tools used.
| Quality appraisal tool | Types of studies |
|---|---|
| Cochrane bias tool assessment | Randomized control trials |
| Newcastle–Ottawa tool | Non-RCT and observational studies |
| PRISMA checklist | Systematic reviews |
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; RCT, randomised controlled trial.
Results
After selecting databases such as PubMed, MEDLINE, and Google Scholar, we retrieved 116 articles. Out of these articles, 13 were eliminated due to inadequate titles or abstracts. We evaluated the remaining 18 papers and disqualified 12 articles as they did not meet our inclusion criteria. Finally, we conducted a thorough quality check on the remaining 6 papers, which all fulfilled our criteria. Our systematic review includes these 6 articles and Table 3 provides comprehensive descriptions of each paper.
Table 3.
Summary of the selected papers.
| Author | Country | Study design | Participants | Adherence rate | Conclusion |
|---|---|---|---|---|---|
| Kang et al., 20177 | Australia | Observational Study multivariate analysis |
686 | 24.9% | Adherence of rural patients [median (IQR): 48% (25–62) >urban: 38% (19–53), P=0.0001] No difference in adherence between Indigenous and non-Indigenous patients Those with good adherence were from more disadvantaged areas i.e. SEIFA inversely associated with adherence (Spearman’s rho =−0.13, P=0.002) |
| Kevat et al., 20168 | Australia | Retrospective analysis multi-level mixed model logistic regression |
277 | 12% (for children receiving >80% injection within 35 days); 0% received >80% within 28 days interval | Adherence was not affected by IRSAD, education and occupation, number of people per household and rural or remote setting (ARIA). Increasing age was associated with delayed injection delivery when injection interval > 35 days; OR: 1.46 (1.24–1.71) P value: 0.000004; however, this association was non-significant for injection delivery >28 days |
| Mekonen et al., 20209 | Ethiopia | Cross-sectional study multivariate regression analysis |
145 | 80.6% | Adherence was not influenced by education level. (P >0.05) Adherence was higher in patients who were not admitted to the hospital (AOR: 26.22; CI: 2.55–269.70; P=0.006) and once admitted patients (AOR: 50.08; CI: 2.87–873.77; P=0.007) compared to those admitted twice or more. Factors that decreased adherence: Forgetting to go to health facilities, stocking out of BPG, the unwillingness of HCPs to administer BPG. Half of the participants did not know the purpose of receiving BPG injection. 11.7% of the population had some fear of side effects of BPG injection that decreased adherence |
| Prasad et al., 202010 | India | Cross-sectional study - questionnaire-based | 42 | 53% | Adherence was not affected by education level: (OR 3.5, P value 0.15). Adherence was not affected by income level: (OR 5.29, 95% CI 0.55–50.08, P 0.11) Factors associated with non-compliance: misinformation, cost, injection pain, non-availability of injection and allergy to BPG. Many noncompliant patients had no specific reason to discontinue medication indicating high ignorance of disease. 81% of participants had poor awareness of RHD |
| Longenecker et al., 201711 | Uganda | Multivariable logistic regression model | 1504 | 91.40% | Adherence greater in Employed or employed caregiver (vs. unemployed): 1.42 (1.03–1.96)* P value: 0.030 Limited education was associated with better adherence. Limited education (vs. more advanced education) - 1.70 (1.06–2.74), P value: 0.028 Living farther from health service is a barrier to adherence=Distance to the nearest health centre (per km): .94 (0.91–0.98)* P value: 0.001 Household size had an inverse relation with adherence: 0.96 (0.93–0.99) P value: 0.038 Patient factors associated with increased adherence: Younger age, latent (vs. symptomatic) disease. Health service factors that increased adherence: more staff, funding, resources dedicated to tracking patients and access to health care. Factors that decreased adherence: distance from the health care centre, increasing age |
| Gasse et al., 201312 | New Caledonia | Retrospective cohort | 70 | 77% | Adequate healthcare coverage increased adherence: (OR, 0.21; 95% CI 0.06–0.72), P value: 0.0013 Household with more than 5 people was protective against poor adherence: OR: 0.25 (0.08–0.75) P value: 0.0014 Income and distance from the health centre did not influence adherence. Factors that were protective against poor adherence: a household with more than five people, a previous medical history of symptomatic ARF and adequate healthcare coverage |
AOR, adjusted odds ratio; ARF, acute rheumatic fever; BPG, Benzathine Penicillin G; HCP, Health Care Provider; IQR, interquartile range; IRSAD, Index of Relative Socio-economic Advantage and disadvantage; OR, odds ratio; RHD, rheumatic heart disease; SEIFA, Socio-Economic Indexes for Areas.
Discussion
RHD is the morbidly important sequel of ARF. Patients with a prior history of RHD have a greater risk of recurrence of ARF. It has been established that each recurrence worsens the prior RHD13. The risk of recurrence in the pre-antibiotic era was 50–75% with the highest risk being in the first 5 years following the initial disease process13. Meta-analysis studies from the United States between 1939 and 1960 have shown a strong association with the role of penicillin in preventing recurrences13.
Prevention of rheumatic fever is crucial for decreasing the incidence of RHD, which may be primary prevention—prevention of the initial attack or Secondary prevention—prevention of recurrent attacks14. It has been established that true primary prevention of rheumatic fever depends more on the improvement of socio-economic factors and education directed at the public and health workers than the provision of antibiotics15. Secondary prevention is equally important since even an asymptomatic or optimally treated GAS throat infection can still trigger rheumatic fever recurrence. Theoretically, there are two options for secondary prevention which are the use of a vaccine against GAS or antibiotic chemoprophylaxis. Unfortunately, the availability of a vaccine is currently under development, and antibiotic chemoprophylaxis is the only option available at present14.
Randomised controlled trials have shown that secondary prophylaxis reduces the severity of RHD by preventing disease progression and the recurrences of ARF. It is the single most important step in the management of ARF16. Administration of Penicillin compared to doing nothing confers a 55% relative reduction in risk of RF17. Injectable (intramuscular benzathin penicillin) penicillin is considered superior to Oral formulations2,16. Suboptimal adherence or Non-adherence to penicillin can be associated with increased recurrences, heart failure and mortality over 1 year11. Administering regular penicillin injections every 3 or 4 weeks as secondary prophylaxis is a cost-effective strategy for controlling ARF and RHD18.
Efforts to optimize compliance with penicillin and to ensure a safe and adequate supply of the drug are crucial components of secondary prophylaxis adherence can be significantly altered in socially disadvantaged environments where a multitude of interrelated factors exist. Education was an important theme in 5 studies, 4 involving logistic regression analysis and one involving questionnaire-based interviews. Kang et al. 7 reported that adherence was better in people from more disadvantaged areas that is with a low SEIFA score indicating that patients with limited education had better adherence than those who were more privileged. Similar findings were observed in the multivariate logistic regression model of Chris T. Longnecker et al.11, where limited education was associated with better adherence compared to those with more advanced education. It is worth noting that in the remaining three studies, education failed to produce any significant impact on adherence level8–10. This suggests that people who have limited education are less likely to resist the need for long-term compliance with secondary prophylaxis in RHD.
Two studies conducted in Australia compared adherence levels with their SEIFA/IRSAD score; a composite index where lower scores indicate more disadvantaged areas and higher scores indicate more advantaged areas. Kang and colleagues found an inverse relation with adherence that is those from a more “disadvantaged area” had better adherence while Kevat and colleagues found that IRSAD did not affect adherence7,8. Rural patients had better adherence compared to urban residents according to the study conducted by Kang et al. 7 and in the same study, it was found that there was no difference in the adherence between Indigenous and Non-indigenous populations. It's possible that improved disease recognition and enhanced service delivery in disadvantaged areas could be the reason behind this trend.
Assessment of the relation of adherence to ease of access to healthcare showed unclear findings. Mekonen et al. 9 demonstrated higher adherence in patients not admitted to the hospital than those admitted once or twice. While Longnecker et al. 11 found that living farther from the health services was a barrier to adherence. When analyzing the effect of income on the adherence of the population, three studies found no association between the two variables8,10,12. The study conducted in Australia by Kang et al. 7 showed that income level had an inverse relation with adherence since the SEIFA score was used to demonstrate the income level along with other variables. Kevat et al. 8 found that occupation had no relation to adherence in their study. Longneckter et al. 11 found in their study that those who were employed had better adherence than those unemployed.
The questionnaire-based study conducted by Prasad et al. 10 showed that many noncompliant patients had no specific reason to discontinue their medications, indicating a high ignorance of the disease and it was found that 81% of participants had poor awareness of the disease. The same study demonstrated several healthcare-related factors contributed to decreased adherence such as misinformation, fear of injection pain, cost, non-availability of injection and allergy to BPG10. Mekonen and colleagues highlighted that forgetting to go to health facilities, stocking out of BPG and the unwillingness of HCPs to administer BPG were the important healthcare-related factors creating a barrier to adherence in his study9,10. Longnecker et al. 11 showed that distance from the health centre, household size and increasing age had a negative impact on adherence. Another known factor leading to lower rates of BPG administration is the lack of BPG supply, but this is discussed only in one of the reviewed studies10. This is likely because BPG supply was ensured for the entire study population. Factors associated with higher adherence were also identified in the studies. The study by Longnecker and colleagues in Uganda showed patient factors and health service-related factors increasing adherence. Younger age and latent (vs. symptomatic) onset of the disease were associated with better adherence, and the important health service-related factors that increased adherence were increased number of staff, funding and resources dedicated to tracking patients, and ease of access to health care11. A retrospective cohort study conducted by Gasse et al. 12 highlighted that adequate healthcare coverage increased adherence, a previous history of symptomatic ARF, and a household with more than five people were also protective against poor adherence.
The role of patient education and awareness is of paramount importance in order to augment the secondary adherence rate and thereby prevent the malicious effects of RHD. The study by Tullu and colleagues, conducted in India, recorded a 90% adherence to prophylaxis among patients with RF by educating healthcare workers, teachers, and students to identify characteristic signs and symptoms of RF and direct the individual suspect of having RF to the nearest healthcare centre10. Studies have also proven that the generalized lack of awareness of secondary prophylaxis and, hence, lower adherence is independent of the educational status of the patient. Prasad et al. 10 showed that having educational qualifications below 10th grade did not pose as a significant risk in adherence ratio compared to those with higher educational qualifications.
Other proven factors associated with non-adherence to secondary prophylaxis include the long-distance commute, waiting time, fear of injections among both paediatric and adult patients, and the cost of injections. This reflects the absence of a structured framework to control, guide and monitor the RHD9,10. Some approaches to overcome the various barriers to secondary prophylaxis include introducing designated outreach healthcare programmes and thereby making the availability of benzathine penicillin more prevalent. Implementing community-driven initiatives that involve peer support groups and community health workers can raise awareness and make adherence a communal support.
Conclusion
Current literature has revealed a contrary or negligible association of education, income, and rural residence with adherence to secondary prophylaxis for RHD. Improved disease recognition and enhanced service delivery in disadvantaged areas could be the reason behind this trend. Socio-economic factors such as unemployment, advancing age, limited access to healthcare facilities, poor awareness about the disease, and inadequate availability of BPG emerged as barriers influencing adherence among RHD patients. Intervention focused on these specific barriers is necessary to improve the delivery of secondary prophylaxis. Moreover, a positive association between increased staffing, funding, and resources dedicated to tracking patients with improved adherence emphasizes the importance of healthcare-related infrastructure and adequate resources in treatment adherence. This literature elucidates the socio-economic factors associated with adherence to secondary prophylaxis of RHD. However, further studies in the field are crucial to keep track of these socio-economic factors and their temporal changes.
Ethical approval
None.
Consent
As this submission involves a systematic review and not a case report or study involving patients or volunteers, the requirement for obtaining written consent from individuals does not apply. Systematic reviews typically involve the analysis and synthesis of data from existing studies, and do not directly involve patients or volunteers. Therefore, there are no individuals whose consent needs to be obtained for publication.
Source of funding
All authors have declared that no financial support was received from any organization for the submitted work.
Author contribution
M.Y.: study concept and design, data collections, data analysis, writing the paper. N.A.S.: study concept and design, data collections, data analysis, writing the paper. K.B.: writing the paper, reviewed, edited the manuscript. A.G.I.: data collection, writing the paper. P.L.: reviewed and edited the article. A.J.: study concept and design, data collections, data analysis, writing the paper. D.Y.: reviwed the article. A.K.S.: data collection, writing the manuscript. N.S.: edited, revised the manuscript. S.Y.: writing the paper, edited the manuscript.
Conflicts of interest disclosure
The authors have no conflict of interest to declare.
Research registration unique identifying number (UIN)
PROSPERO - Systematic Review on Socioeconomic Determinants Influencing Adherence to Secondary Prophylaxis in Rheumatic Heart Disease [CRD42023456482] https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023456482.
Guarantor
Dr Newton Ashish Shah.
Data availability statement
All the required information is within the manuscript itself.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 17 May 2024
Contributor Information
Manish Yadav, Email: manishy486@gmail.com.
Newton Ashish Shah, Email: newtonashish@iom.edu.np;newtonashishnp@gmail.com.
Kritick Bhandari, Email: bhandarikritick@gmail.com.
Aksharaa G. Iyer, Email: gAksharaa@gmail.com.
Ashish Mishra, Email: ashishmishraiom9@gmail.com.
Pratik Lamichhane, Email: pratiklamichhane@iom.edu.np.
Amir Joshi, Email: amir.joshi95@gmail.com.
Digraj Yadav, Email: digraj1552@gmail.com.
Aanand K. Singh, Email: aanand9860426794@gmail.com.
Nischal Shah, Email: naz.nepali@gmail.com.
Samridhi Yadav, Email: Samridhiyadav2@gmail.com.
References
- 1.Ruan R, Liu X, Zhang Y, et al. Global, Regional, and National Advances toward the Management of Rheumatic Heart Disease Based on the Global Burden of Disease Study 2019. J Am Heart Assoc. 2023;12:e028921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beaton A, Okello E, Rwebembera J, et al. Secondary antibiotic prophylaxis for latent rheumatic heart disease. N Engl J Med 2022;386:230–240. [DOI] [PubMed] [Google Scholar]
- 3.Beaton A, Okello E, Rwebembera J, et al. ADHERENCE TO SECONDARY PROPHYLAXIS OF RHEUMATIC FEVER IN PATIENTS WITH RHEUMATIC HEART DISEASE IN RURAL AREAS. Pak Heart J 51(3). doi: 10.47144/phj.v51i3.1538 [DOI] [Google Scholar]
- 4.Nemani L, Maddury J, Barik R, et al. A Cross-sectional study to look at the determinants of poor adherence to secondary penicillin prophylaxis for rheumatic heart disease at a tertiary care center in South India. J Clin Prev Cardiol 2018;7:5. [Google Scholar]
- 5.Thompson SB, Brown CH, Edwards AM, et al. Low adherence to secondary prophylaxis among clients diagnosed with rheumatic fever, Jamaica. Pathog Glob Health. 2014;108:229–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kang K, Chau KWT, Howell E, et al. The temporospatial epidemiology of rheumatic heart disease in Far North Queensland, tropical Australia 1997–2017; impact of socioeconomic status on disease burden, severity and access to care. PLoS Negl Trop Dis 2021;15:e0008990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kevat PM, Gunnarsson R, Reeves BM, et al. Adherence rates and risk factors for suboptimal adherence to secondary prophylaxis for rheumatic fever. J Paediatr Child Health 2021;57:419–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mekonen KK, Yismaw MB, Abiye AA, et al. Adherence to Benzathine Penicillin G secondary prophylaxis and its determinants in patients with rheumatic heart disease at a cardiac center of an Ethiopian Tertiary Care Teaching Hospital. Patient Prefer Adherence 2020;14:343–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prasad A, Prasad A, Singh BK, et al. Compliance to the secondary prophylaxis and awareness of rheumatic heart disease: a cross-sectional study in low-income province of India. J Fam Med Prim Care 2020;9:1431–1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Longenecker CT, Morris SR, Aliku TO, et al. Rheumatic heart disease treatment cascade in Uganda. Circ Cardiovasc Qual Outcomes 2017;10:e004037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gasse B, Baroux N, Rouchon B, et al. Determinants of poor adherence to secondary antibiotic prophylaxis for rheumatic fever recurrence on Lifou, New Caledonia: a retrospective cohort study. BMC Public Health 2013;13:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iyengar SD, Grover A, Kumar R, et al. A rheumatic fever and rheumatic heart disease control programme in a rural community of north India. Natl Med J India 1991;4:268–271. [PubMed] [Google Scholar]
- 14.Manyemba J, Mayosi BM. Penicillin for secondary prevention of rheumatic fever. Cochrane Database Syst Rev 2002;2002:CD002227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bach JF, Chalons S, Forier E, et al. 10-year educational programme aimed at rheumatic fever in two French Caribbean islands. Lancet Lond Engl 1996;347:644–648. [DOI] [PubMed] [Google Scholar]
- 16.Carapetis JR, Beaton A, Cunningham MW, et al. Acute rheumatic fever and rheumatic heart disease. Nat Rev Dis Primer 2016;2:15084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watkins DA, Beaton AZ, Carapetis JR, et al. Rheumatic heart disease worldwide. J Am Coll Cardiol 2018;72:1397–1416. [DOI] [PubMed] [Google Scholar]
- 18.Günther G, Asmera J, Parry E. Death from rheumatic heart disease in rural Ethiopia. The Lancet 2006;367:391. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the required information is within the manuscript itself.