Abstract
The detailed changes in disc properties after intradiscal injection of condoliase remain controversial. At 3 and 9 months after administration, radiographic changes in discs were investigated. A total of 41 patients (men, 25; median age, 46 years) who underwent regular follow-up magnetic resonance imaging at 3 and 9 months after administration without additional invasive therapy were retrospectively investigated. The intensity changes of the nucleus pulposus based on the Pfirrmann disc grading system, midsagittal disc height, and maximum protrusion length of herniation were assessed. In addition, disc height changes were compared between 24 patients aged <50 years (young group) and 17 patients aged ≥50 years (over 50s group). The overall mean disc heights were 9.1, 7.5, and 7.6 mm preoperatively, at 3 months, and at 9 months, respectively, with a significant reduction at 3 months (P < 0.001) and no significant changes thereafter. The mean maximum protrusion length of herniation significantly and gradually decreased. The overall proportions of Pfirrmann disc grades after administration were equivalent between 3 and 9 months. However, the recovery from Pfirrmann disc grades IV to III was confirmed in 8 of 17 cases (47.1%) between 3 and 9 months, whereas 6 of 20 cases (30.0%) showed a decline from III to IV. Patients in the young group with pretreatment disc height >11 mm had the greatest reduction in disc height than the over 50s group. In conclusion, the clinical outcomes in the over 50s group were comparable to those in the young group after injection of condoliase, whereas young patients with higher disc were more susceptible to disc height reduction.
Keywords: chemonucleolysis, condoliase, chondroitin sulfate ABC endolyase, lumbar disc herniation, degeneration
Introduction
Percutaneous chemonucleolysis with condoliase has been available in Japan since 2018 as a less invasive treatment for painful lumbar disc herniation. This treatment relieves pain in the buttocks and lower limbs caused by lumbar disc herniation with indirect decompression by reducing the water content of proteoglycan as the main component of the nucleus pulposus with the percutaneous intradiscal administration of condoliase. The effective clinical rates of chemonucleolysis with condoliase ≤6 months after the administration have been reported to be 70.2%-85.4%.1-6) A few studies also reported effective clinical rates of 76.1%-85% in the further long term ≤2 years.7-9)
Contrarily, regarding radiographic assessments, a few studies have reported changes in disc properties >6 months after condoliase administration, but the interpretation of the results remains controversial.3,8,9) Therefore, this study aimed to show detailed radiographic changes in the intervertebral disc with clinical outcomes at 3 and 9 months after condoliase administration, further dividing patients into the young and over 50s groups for the analysis of disc height reduction.
Materials and Methods
Patients
We retrospectively investigated 41 consecutive patients (men, 25; women, 16; median age, 46.0 years; interquartile range [IQR], 33.0-57.5 years) who underwent intradiscal injection of condoliase between October 2020 and September 2022 as well as regular follow-up magnetic resonance imaging (MRI) at 3 and 9 months after administration without additional invasive therapy. During the same period, four patients underwent removal of herniation 3 months or later after administration due to a lack of pain relief, and five patients refused to undergo MRI at 9 months after administration, claiming that their pain had been relieved and that no further examinations were necessary. The indications for intradiscal injection of condoliase were as follows: unilateral leg pain with or without low back pain, no improvement after conservative treatment for 6 weeks and more, and distribution of leg pain corresponding to probable subligamentous herniation on MRI. Conversely, the following conditions were listed as contraindications: herniation of apparent transligamentous or sequestration type, cauda equina syndrome, and motor weakness manual muscle test ≤4-. This study was approved by the institutional review board of our institution (registration number: 230) and was therefore conducted in accordance with the principles of the 1964 Declaration of Helsinki and its later amendments. Written informed consent was obtained from all patients before chemonucleolysis. However, due to the retrospective nature of the study, informed consent was not required for patients to participate in this study. Table 1 presents the demographic and baseline characteristics of the 41 patients.
Table 1.
Demographic and baseline characteristics of patients
| Variables | Data (n = 41) |
|---|---|
| Age, years; median (IQR) | 46.0 (33.0-57.5) |
| 10s | 5 (12.2%) |
| 20s | 4 (9.8%) |
| 30s | 6 (14.6%) |
| 40s | 9 (22.0%) |
| 50s | 9 (22.0%) |
| 60s | 3 (7.3%) |
| 70s | 3 (7.3%) |
| 80s | 2 (4.9%) |
| Men, n | 25 (61.0%) |
| Follow-up periods, days; median (IQR) | 274.0 (266.0-285.0) |
| Herniation level | |
| L2/3 | 3 (7.3%) |
| L3/4 | 1 (2.4%) |
| L4/5 | 21 (51.2%) |
| L5/S1 | 16 (39.0%) |
| Laterality, n (%) | |
| Left | 22 (53.7%) |
| Right | 19 (46.3%) |
| MRI T2WI signal of nucleus pulposus, n | |
| Pfirrmann disc grade II | 3 (7.3%) |
| Pfirrmann disc grade III | 37 (90.2%) |
| Pfirrmann disc grade IV | 1 (2.4%) |
T2WI, T2-weighted image
Intervention
The patient was placed in the prone position on a radiolucent bed. After local disinfection and anesthesia, a 21-gauge disc puncture needle was inserted into the intervertebral disc from 5-10 cm lateral to the midline under fluoroscopic guidance. The needle tip was positioned in the dorsal 1/3 of the intervertebral disc near the herniation with the laterality from the herniation dominant side; the positions were rigorously confirmed via cone beam computed tomography in all cases.1) Condoliase (1.25 U) was dissolved in 1.2-mL saline and injected into the intervertebral disc. The patients were allowed to move freely immediately after administration and were discharged the following day.
Clinical and radiographic evaluations
Clinical outcomes were evaluated at baseline, 3 months, and 9 months after administration using the Japanese Orthopaedic Association Back Pain Questionnaire (JOABPEQ),10) a visual analogue scale (VAS) score for low back pain, and VAS scores for pain and numbness in the buttocks and lower limbs. The JOABPEQ includes functional scores for each of the five domains (pain-related disorders, lumbar spine dysfunction, gait disturbance, social life dysfunction, and psychological disorders) based on the patient's subjective judgment. The score for each domain is in the range of 0-100, with higher scores indicating better condition. The therapeutic effects for individual patients were judged “effective” if either of the following conditions were met: 1) posttreatment score ≥20 points higher than the pretreatment score and 2) pretreatment score <90 points and posttreatment score ≥90 points. The effectiveness rate based on each pre- and postoperative domain (low back pain, lumbar function, walking ability, social life function, and mental health) in each group was calculated using the following formula: (number of patients judged “effective”)/[(total number of patients in the group) − (number of patients with pre and posttreatment scores both ≥90)] × 100 (%). The recovery of VAS scores ≥ 2 points was defined as “effective” and with ≥50% as “satisfactory” based on the concept of minimum clinically important difference.11)
For radiographic assessment, MRI was performed pre- and postoperatively in conjunction with the clinical examination. In all 41 patients, the following MRI parameters were used to compare pre- and postoperative radiographic data: mid-sagittal disc height, maximum protrusion length of herniation from the posterior line of the adjacent vertebral bodies, and Pfirrmann disc grade of the nucleus pulposus on MRI T2-weighted image (T2WI).12) The Pfirrmann disc grading system is defined as follows: grade I, homogeneous with a bright hyperintense white signal intensity and a normal disc height; grade II, inhomogeneous with a hyperintense white signal, clear distinction between the nucleus and the annulus, and normal disc height; grade III, inhomogeneous with an intermediate gray signal intensity, unclear distinction between the nucleus and annulus, and normal or slightly decreased height; and grade IV, inhomogeneous with an hypointense dark gray signal intensity, lost distinction between the nucleus and the annulus, and normal or moderately decreased disc height. Furthermore, comparisons of the clinical outcomes and changes in disc height between 24 patients in the young group (<50 years, Y group) and 17 patients in the over 50s group (≥50 years, O group) were performed using five effective rates in JOABPEQ, VAS score for low back pain, and VAS scores for pain and numbness in the buttocks and lower limbs. Each value of the radiographic parameter was carefully fixed after a few measurements to avoid an error by T.O.
Statistical analysis
Continuous variables in clinical parameters were expressed as median (IQR), and differences between the groups were compared using the chi-squared test, Wilcoxon signed rank test, or Mann-Whitney U test. Contrarily, for the analysis of changes in intervertebral disc properties, continuous variables in radiographic parameters were expressed as mean ± standard deviation using the repeated measures analysis of variance test. Two-sided P < 0.05 was considered to indicate statistical significance. All statistical analyses were conducted using IBM SPSS Statistics for Windows, version 28.0 (IBM Corp., Armonk, NY, USA).
Results
All five domains in the JOABPEQ, VAS score for low back pain, and VAS scores for pain and numbness in the buttocks and lower limbs at 3 and 9 months after administrations significantly improved compared with baseline (Table 2). These five effectiveness rates in the JOABPEQ at 3 and 9 months after administrations compared with baseline were as follows: 82.5% and 82.5% for low back pain, 65.9% and 90.2% for lumbar function, 69.4% and 86.1% for walking ability, 63.4% and 70.7% for social life function, and 36.6% and 51.2% for mental health. The proportions of VAS score recoveries ≥2 points for low back pain, pain in the buttocks and lower limbs, and numbness in the buttocks and lower limbs at 3 and 9 months postoperatively from baseline were 75.6% and 75.6%, 87.8% and 90.2%, and 70.7% and 82.9%, respectively. Furthermore, the proportion of VAS score recoveries ≥50% for low back pain, pain in the buttocks and lower limbs, and numbness in the buttocks and lower limbs at 3 and 9 months after administration compared with baseline were 58.5% and 70.7%, 68.3% and 87.8%, and 65.9% and 78.0%, respectively, with satisfactory proportions, particularly in the recovery of VAS score for pain in the buttocks and lower limbs. In general, allergic reaction is considered to be a concern with chemonucleolysis with condoliase, but even mild allergic reaction such as skin rash was not confirmed in our cohort.
Table 2.
JOABPEQ and VAS scores at baseline, 3 months, and 9 months after administration
| Baseline | 3 months | P | 9 months |
P (VS baseline) |
|
|---|---|---|---|---|---|
| JOABPEQ; median (IQR) | |||||
| Pain-related disorders | 29 (14-43) | 100 (57-100) | <0.001* | 100 (71-100) | <0.001* |
| Lumbar spine dysfunction | 42 (29-58) | 75 (58-100) | <0.001* | 83 (79-100) | <0.001* |
| Gait disturbance | 43 (14-71) | 93 (64-100) | <0.001* | 100 (86-100) | <0.001* |
| Social life dysfunction | 43 (19-57) | 73 (51-78) | <0.001* | 78 (59-100) | <0.001* |
| Psychological disorders | 48 (39-54) | 59 (51-74) | <0.001* | 66 (49-78) | <0.001* |
| VAS, median (IQR) | |||||
| Low back pain | 5.0 (3.5-7.5) | 2.0 (1.0-3.0) | <0.001* | 1.0 (0.8-3.0) | <0.001* |
| Pain in the buttocks and lower limb | 7.0 (5.0-8.5) | 2.0 (1.0-4.0) | <0.001* | 1.0 (0-2.0) | <0.001* |
| Numbness in the buttocks and lower limb | 6.0 (3.0-8.0) | 1.0 (0-2.5) | <0.001* | 0 (0-1.5) | <0.001* |
Wilcoxon signed rank test.
JOABPEQ, Japanese Orthopaedic Association Back Pain Evaluation Questionnaire; VAS, visual analogue scale; IQR, interquartile range
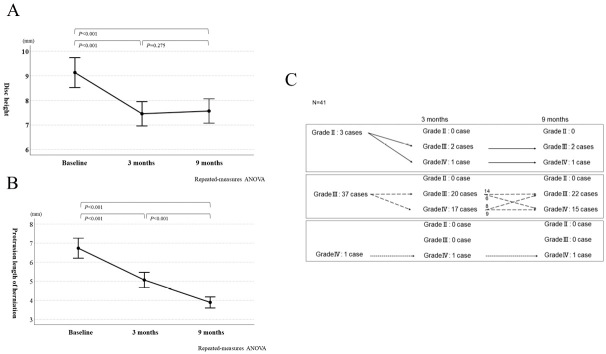
Regarding radiographic assessment, the mean mid-sagittal disc height on MRI significantly decreased from 9.1 ± 0.3 mm preoperatively to 7.5 ± 0.2 mm at 3 months (P < 0.001) and remained unchanged at 7.6 ± 0.2 mm at 9 months (Fig. 1A). The mean maximum protrusion lengths of herniation were 6.7 ± 0.3 mm preoperatively, 5.1 ± 0.2 mm at 3 months, and 3.9 ± 0.1 mm at 9 months, showing a significant gradual decrease (Fig. 1B). The Pfirrmann disc grade II, III, and IV proportions of the nucleus pulposus were 3 (7.3%), 37 (90.2%), and 1 (2.4%) case at baseline; 0 (0%), 22 (53.7%), and 19 (46.3%) at 3 months; and 0 (0%), 24 (58.5%), and 17 (41.5%) at 9 months, respectively, showing no apparent differences in the proportions of disc grades between 3 and 9 months in the overall patient population. However, when focusing on grades III and IV in the changes in each disc grade, the increased intensity of the nucleus pulposus from grades IV to III was confirmed in 8 of 17 cases (47.1%) between 3 and 9 months, whereas 6 of 20 cases (30.0%) presented with decreased intensity from grades III to IV during the same period (Fig. 1C).
Fig. 1.
The mean mid-sagittal disc height (A) and mean maximum protrusion length of herniation (B) on MRI at baseline, 3 months, and 9 months after intradiscal injection of condoliase are shown. The changes in Pfirrmann disc grades after administration are shown in detail, focusing on each grade at the baseline and each grade change at 3 and 9 months thereafter (C).
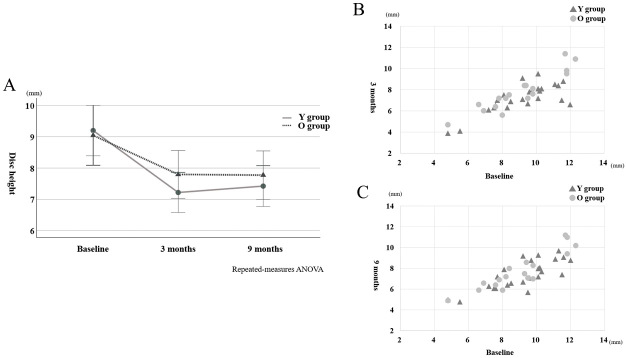
Comparisons of the clinical outcomes and changes in disc height between the Y and O groups showed a significant decrease in disc height at 3 months after administration in the Y group compared with the O group (P = 0.015) (Fig. 2A), showing no significant differences in all five effective rates in JOABPEQ, and the proportion of recovery of VAS scores ≥2 points and ≥50% for low back pain, pain in the buttocks and lower limbs, and numbness in the buttocks and lower limbs in both groups. However, the VAS score for low back pain at baseline was slightly higher in the Y group compared with the O group (P < 0.014) (Table 3). Particularly in disc height reduction, the patients in the Y group with pretreatment disc height >11 mm seemed to suffer the greatest reduction in disc height compared with the O group (Fig. 2B and C).
Fig. 2.
The changes in disc height after administration are shown, with patients divided into the young (Y) and over 50s (O) groups at age 50 (A). Note the trend toward great reductions in disc height at 3 and 9 months after administration in patients with baseline disc height > 11 mm in the Y group compared with the O group (B and C).
Table 3.
Characteristics at baseline and clinical outcomes at 9 months in the young and over 50s groups
| Y group | O group | P | |
|---|---|---|---|
| Number of cases | 24 | 17 | NA |
| Male, n | 16 (66.7%) | 9 (52.9%) | 0.375 |
| Age, years; median (IQR) | 36.5 (20.3-43.8) | 59.0 (54.0-70.0) | NA |
| JOABPEQ at baseline; median (IQR) | |||
| Pain-related disorders | 14.0 (0-43.0) | 43.0 (21.5-50.0) | 0.051 |
| Lumbar spine dysfunction | 37.5 (25.0-50.0) | 50.0 (33.0-70.5) | 0.131 |
| Gait disturbance | 60.5 (14.0-79.0) | 43.0 (10.5-64.0) | 0.129 |
| Social life dysfunction | 38.0 (8.8-51.0) | 51.0 (32.5-58.0) | 0.133 |
| Psychological disorders | 48.5 (36.8-55.5) | 46.0 (39.0-52.0) | 0.652 |
| VAS score at baseline; median (IQR) | |||
| Low back pain | 6.0 (4.3-8.0) | 5.0 (3.0-5.5) | 0.014* |
| Pain in the buttocks and lower limb | 7.0 (5.0-8.8) | 7.0 (5.0-8.5) | 0.452 |
| Numbness in the buttocks and lower limb | 6.0 (4.3-8.0) | 5.0 (2.5-8.0) | 0.699 |
| JOABPEQ; Effective rate | |||
| Low back pain | 20/24 (83.3%) | 13/16 (81.3%) | 1.000 |
| Lumbar function | 23/24 (95.8%) | 14/17 (82.4%) | 0.290 |
| Walking ability | 17/19 (89.5%) | 14/17 (82.4%) | 0.650 |
| Social life function | 19/24 (79.2%) | 10/17 (58.8%) | 0.184 |
| Mental health | 14/24 (58.3%) | 7/17 (41.2%) | 0.279 |
| Recovery of VAS score ≥ 2 points, n | |||
| Low back pain | 19 (79.2%) | 12 (70.6%) | 0.714 |
| Pain in the buttocks and lower limb | 22 (91.7%) | 15 (88.2%) | 1.000 |
| Numbness in the buttocks and lower limb | 21 (87.5%) | 13 (76.5%) | 0.421 |
| Recovery of VAS score ≥ 50%, n | |||
| Low back pain | 18 (75.0%) | 11 (64.7%) | 0.507 |
| Pain in the buttocks and lower limb | 22 (91.7%) | 14 (82.4%) | 0.633 |
| Numbness in the buttocks and lower limb | 20 (83.3%) | 12 (70.6%) | 0.450 |
χ2 test and Mann-Whitney U test.
Y group, young group; O group, over 50s group; NA, not applicable; JOABPEQ, Japanese Orthopaedic Association Back Pain Evaluation Questionnaire; VAS, visual analogue scale, IQR, interquartile range
Discussion
The present study demonstrates detailed radiographic changes in intervertebral disc with clinical outcomes after condoliase administration. First, the maximum protrusion length of herniation gradually decreased at 3 and 9 months after administration. Second, the mean mid-sagittal disc height decreased by approximately 1.6 mm at 3 months after administration and remained unchanged at 9 months. Third, the Pfirrmann disc grade deterioration was demonstrated in 20 of 41 patients (48.8%) at 3 months after administration, but no apparent differences in the proportions of disc grades were confirmed between 3 and 9 months in the overall patients. However, when focusing on grades III and IV in the changes in each disc grade, the intensity changes of the nucleus pulposus between grades IV and III were heterogeneous from 3 to 9 months. Fourth, a significant decrease in disc height at 3 months after administration was observed in the young group, whereas no significant difference was confirmed in all parameters related to clinical improvement in both groups. Overall satisfactory clinical results were achieved in patients after chemonucleolysis with condoliase. In particular, recovery rates ≥50% of the VAS scores for pain in the buttocks and lower limbs were 68.3% and 87.8% at 3 and 9 months, respectively.
Regarding the changes in intervertebral disc after injection of condoliase, Banno et al. reported the MRI findings in 35 patients at 2 years after administration. In this study, they reported the significant decrease in the mean disc height at 3 months after injection, the tendency of disc height recovery at 1 year without statistical significance, and maintenance of recovered disc height until two years. Progression in terms of Pfirrmann classification was also observed in 20 of 35 patients (57.1%) at 3 months; however, 6 patients (30.0%) showed recovery of nucleus pulposus intensity at 2 years. Furthermore, disc height recovery with a recovery rate > 50% at 2 years compared with baseline was observed in 15 of 35 patients (42.9%) and was significant in younger patients.9) Banno et al. also reported in another previous study that the disc height recovery rate > 50% at 1 year was 30.8%.7) This disc height recovery rate was calculated as follows: (disc height at the last follow-up − disc height at 3 months)/(disc height at baseline − disc height at 3 months) × 100 (%). Contrarily, in our cohort, Pfirrmann disc grade progression was detected in 20 of 41 patients (48.8%) at 3 months after administration, and Pfirrmann disc grade recovery was confirmed in 8 of 20 patients (40.0%) only with the recovery pattern from grades IV to III. In terms of disc height recovery, only 9 of 41 patients (22.0%) had a recovery rate > 50% at 9 months. Consequently, the gradual recovery of disc height would be expected to some extent and with a relatively high frequency, although the disc height temporally decreased in almost all cases during a few months after administration. Regarding the changes in Pfirrmann disc grades, we demonstrated the detailed changes in each grade after administration in the present study. The recovery of Pfirrmann disc grade was limited in the changes from grade IV at 3 months to III at 9 months, whereas one in three patients (33.3%) with grade II at baseline had an unfavorable progression to grade IV at 9 months. Therefore, condoliase should be administered to patients with near-normal nucleus pulposus after obtaining informed consent, which included information about the possibility of severe reduction in disc water-holding capacity. Animal studies in dogs or cynomolgus monkeys have demonstrated that the number of nucleus pulposus cells is significantly reduced after condoliase administration due to degeneration and necrosis, but from 4 weeks after administration, proteoglycan is produced by the regeneration of nucleus pulposus cells, suggesting that the water-holding capacity of nucleus pulposus tissue is restored over time.13,14) The mechanism by which Pfirrmann disc grade and disc height improve may involve the aforementioned actions.
When comparing the changes in disc height between the Y and O groups, as expected, a significant decrease in disc height at 3 months was observed in the Y group compared with the O group. Contrarily, no significant difference in disc height between the two groups was observed at 9 months because of the slight recovery in disc height from 3 to 9 months in the Y group. Despite such differences in changes in disc height after injection of condoliase in both groups, the parameters related to clinical improvement, such as five effective rates in JOABPEQ or the proportion of recovery of VAS scores ≥2 points and ≥50% for low back pain, pain in the buttocks and lower limbs, and numbness in the buttocks and lower limbs, were comparable in both groups. The VAS score for low back pain at baseline was significantly higher in the Y group than in the O group, but this was expected because the younger generations with lumbar disc herniations would generally have low back pain with the high proportions. Furthermore, the differences in VAS scores for low back pain between the generations would not be as significant because the primary indication for condoliase administration in Japan is unilateral leg pain with or without low back pain and the recovery of low back pain is a secondary effect. Future study should investigate the primary effect of intradiscal injection of condoliase for low back pain. In such point of view, patients should be informed of the possibility of severe reductions in disc height before administration, particularly young patients with near-normal disc height, but there is no need to hesitate in administering it to young patients who agree with such information. Contrarily, the therapeutic effect of condoliase on discs with some degree of advanced disc degeneration was also considered promising. McGirt reported that disc height losses of 18% at 3 months and 26% at 2 years were confirmed in 108 patients who underwent open discectomy in a prospective cohort study.15) Further studies are warranted to investigate the long-term risks of disc dehydration or disc height loss following discal injection of condoliase.
This study has some limitations. First, this was a retrospective study that included comparative analyses, and the sample size was small. A prospective randomized controlled trial in a larger population with a long study period is necessary. Second, the median follow-up period of 274 (IQR, 266-285) days after the administration is insufficient for the final evaluation of condoliase in lumbar disc herniation. However, the present study focused on the detailed radiographic changes at 3 and 9 months when the most active changes in intervertebral disc properties were expected after condoliase administration. Third, postoperative MRI was refused in five patients at 9 months after condoliase administration, although they did not want further examinations as their pain had improved. Finally, in the comparison of clinical outcomes and changes in disc properties between the Y and O groups, the separation of the cohort at age 50 may be insufficient for true intergenerational comparisons. In the future, analyses between more divided generations in a large population are mandatory.
In conclusion, the mean disc height after condoliase administration decreased by approximately 1.6 mm at 3 months but revealed no further reduction between 3 and 9 months. The proportions of Pfirrmann disc grades between 3 and 9 months after administration were equivalent in the overall patients, whereas heterogeneous changes between Pfirrmann disc grades III and IV were confirmed during the same period. Young patients with higher disc appeared to be more susceptible to disc height reduction after administration of condoliase, whereas no significant difference was confirmed between the two groups in all parameters related to clinical improvement. Chemonucleolysis with condoliase has the potential to be a first-line treatment instead of surgical removal for painful lumbar disc herniation owing to its less invasive nature if the rate of symptomatic problems due to disc degeneration is acceptable in the long term.
Portions of this work were presented in the afternoon seminar at the 38th Annual Meeting of the Neurospinal Society of Japan, Nagoya, Japan, June 16, 2023.
Abbreviations
MRI, magnetic resonance imaging; IQR, interquartile range; JOABPEQ, Japanese Orthopaedic Association Back Pain Questionnaire; VAS, visual analog scale; T2WI, T2-weighted image.
Authors' Contributions
Tatsuya Ohtonari: Conceptualization, Data curation, Formal analysis, Investigation, Methodology. Kyohei Sakai: Data curation, Formal analysis. Yosuke Furukawa: Data curation. Yasushi Takeda: Data curation. The first draft of the manuscript was written by Tatsuya Ohtonari and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. Ohtonari, Sakai and Takeda who are members of the JNS registered online self-reported COI Disclosure Statement Forms through the website for JNS.
Acknowledgments
We are grateful to the radiologists of my hospital for their prompt preoperative radiological examinations and image processing work, and to Ms. Tomoko Fukushima for her advice on statistical analysis.
References
- 1). Ohtonari T, Torii R, Noguchi S, Kitagawa T, Nishihara N: Short-term clinical and radiographic outcomes of chemonucleolysis with condoliase for painful lumbar disc herniation and analysis regarding intradiscal injection area. Neurosurg Rev 46: 59, 2023 [DOI] [PubMed] [Google Scholar]
- 2). Banno T, Hasegawa T, Yamato Y, et al. : Clinical outcome of condoliase injection treatment for lumbar disc herniation: indications for condoliase therapy. J Orthop Sci 26: 79-85, 2021 [DOI] [PubMed] [Google Scholar]
- 3). Chiba K, Matsuyama Y, Seo T, Toyama Y: Condoliase for the treatment of lumbar disc herniation: a randomized controlled trial. Spine (Phila Pa 1976) 43: E869-E876, 2018 [DOI] [PubMed] [Google Scholar]
- 4). Hirai T, Takahashi T, Tanaka T, et al. : Intradiscal injection with condoliase (chondroitin sulfate ABC endolyase) for painful radiculopathy caused by lumbar disc herniation. Spine Surg Relat Res 6: 252-260, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Inoue M, Sainoh T, Kojima A, et al. : Efficacy and safety of condoliase disc administration as a new treatment for lumbar disc herniation. Spine Surg Relat Res 6: 31-37, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Nakajima H, Kubota A, Maezawa Y, et al. : Short-term outcome and predictors of therapeutic effects of intradiscal condoliase injection for patients with lumbar disc herniation. Spine Surg Relat Res 5: 264-271, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7). Banno T, Hasegawa T, Yamato Y, et al. : Disc degeneration could be recovered after chemonucleolysis with condoliase.-1 year clinical outcome of condoliase therapy. J Orthop Sci 27: 767-773, 2022 [DOI] [PubMed] [Google Scholar]
- 8). Okada E, Suzuki S, Nori S, et al. : The effectiveness of chemonucleolysis with condoliase for treatment of painful lumbar disc herniation. J Orthop Sci 26: 548-554, 2021 [DOI] [PubMed] [Google Scholar]
- 9). Banno T, Hasegawa T, Yamato Y, et al. : Condoliase therapy for lumbar disc herniation -2 year clinical outcome. J Orthop Sci 29: 64-70, 2024 [DOI] [PubMed] [Google Scholar]
- 10). Fukui M, Chiba K, Kawakami M, et al. : JOA Back Pain Evaluation Questionnaire (JOABPEQ)/JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ). The report on the development of revised versions. April 16, 2007. The Subcommittee of the Clinical Outcome Committee of the Japanese Orthopaedic Association on Low Back Pain and Cervical Myelopathy Evaluation. J Orthop Sci 14: 348-365, 2009 [DOI] [PubMed] [Google Scholar]
- 11). Dworkin RH, Turk DC, Wyrwich KW, et al. : Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain 9: 105-121, 2008 [DOI] [PubMed] [Google Scholar]
- 12). Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N: Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26: 1873-1878, 2001 [DOI] [PubMed] [Google Scholar]
- 13). Ono A, Harata S, Takagaki K, Endo M: Proteoglycans in the nucleus pulposus of canine intervertebral discs after chondroitinase ABC treatment. J Spinal Disord 11: 253-260, 1998 [PubMed] [Google Scholar]
- 14). Muramatsu D, Yamaguchi H, Minamisawa Y, Nii A: Selective chemonucleolysis with condoliase in cynomolgus monkeys. Toxicol Pathol 48: 656-668, 2020 [DOI] [PubMed] [Google Scholar]
- 15). McGirt MJ, Eustacchio S, Varga P, et al. : A prospective cohort study of close interval computed tomography and magnetic resonance imaging after primary lumbar discectomy: factors associated with recurrent disc herniation and disc height loss. Spine 34: 2044-2051, 2009 [DOI] [PubMed] [Google Scholar]