For complex reasons, society seems to accept a lower standard of safety from road use compared with other forms of transport. Road traffic crashes cause some 320 000 injuries, 40 000 serious injuries, and 3400 deaths a year in the United Kingdom.1 This is equivalent to the Lockerbie air crash happening every four weeks or the Paddington rail crash happening every other day throughout the year. As road traffic crashes are so common, many doctors will give roadside treatment at some time during their career. A third of prehospital deaths may be preventable,2 so doctors have a duty to offer assistance at a crash scene, but this can be a frightening and distressing experience for those not trained to work in the prehospital environment.
Summary points
At some time in their career many doctors will have to deal with a road traffic crash
Safety for yourself at the incident scene is the first priority
Doctors untrained in prehospital care should concentrate on giving good first aid, working under the direction of ambulance service staff
Providing excellent medical treatment at a road crash requires specific training and experience
Patients with airway and breathing problems may need immediate (prehospital) advanced medical intervention
Treatment should be aimed at promoting oxygenation and preserving clot, with rapid patient movement to a hospital with the appropriate facilities to provide definitivecare
Methods
This article was written from the authors' personal experience of working in prehospital care with the London Helicopter Emergency Medical Service, a review of articles in the Cochrane Library, a literature review, participation in internet discussion groups on prehospital care, and aggregated experience of colleagues from the Ambulance Service and the British Association of Immediate Care Schemes (BASICS).
The evidence
This article is based on our synthesis of best practice, but there is often controversy about optimal prehospital care because good evidence is lacking. A recent survey of the prehospital literature on behalf of the World Health Organization found only 24 randomised controlled trials and concluded there was insufficient data to provide a secure evidence base for many of the common prehospital interventions.3
Ethical and practical difficulties (such as lack of informed consent) make it difficult and expensive to perform good prehospital research. None of the UK research funding bodies has a strategy for prehospital care research. Few good quality studies have been carried out, so practice is often based on experience and consensus, leading to a large variation in the configuration of medical services for road traffic casualties.
Prehospital care systems
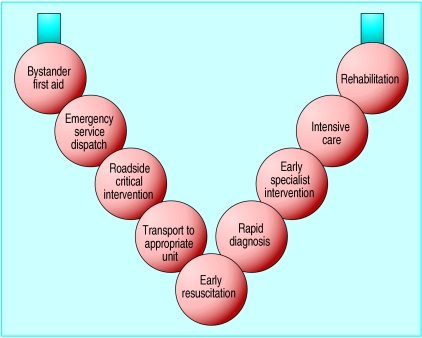
It is easy to underestimate how long it takes to move a patient to hospital. Even for efficient emergency medical services there is a 30-45 minute interval between the time of the crash and arrival at hospital.4 The “golden hour”5 is therefore a prehospital event. The way in which a trauma care system is organised seems to influence the number of deaths after injury.6 Considering prehospital care separately from the rest of the trauma treatment system for road traffic casualties is an artificial distinction; the prehospital phase should be viewed as the start of a continuum of care that forms a “trauma chain” (fig 1). Each link must work well for a patient to attain optimal outcome. Several reports have suggested that trauma systems should be developed in Britain, but little progress has been made.7
Figure 1.
The trauma chain that forms a continuum of care for road traffic casualties
Action at a crash scene by doctors untrained in prehospital care
A road traffic crash scene is a disorientating environment. Your senses will be overloaded by the sights (flashing lights and wreckage), sounds (noise of generators and engines), and smells (fuel and exhaust). Your “patients” will be fully clothed, limiting examination. Lighting may be poor at night, and the weather conditions may be adverse. You will probably have little equipment of your own, and ambulance service equipment may be unfamiliar. With all these factors, it is unreasonable to expect an untrained doctor to provide advanced medical care. However, most doctors feel that they should be giving the same level of care that they would in a resuscitation room. Such unrealistic expectations add to the stress.
When you stop to offer assistance at a crash scene your own safety is the first priority. Make sure that you park in a safe place off the road and that, as you approach the scene, you will not be hit by another vehicle and that the wreckage itself will not be hit. Stop and look for hazards. Telephone the emergency services if they are not already present: either 999 or 112 (the European Union standard emergency number) can be used to activate the emergency services anywhere in Britain. The precise location of the incident is the most important piece of information to give (by street name and intersection or junction, with the direction of travel on a dual carriageway or motorway). Remember that “on the A1” could be anywhere from London to Newcastle. Turn off the ignition of vehicles and put the handbrakes on. Make sure that the walking wounded do not “wander”; move them to a safe place away from other traffic. Do all of this before starting to assess any casualties.
Treatment should follow simple first aid (ABC) principles, with basic airway manoeuvres and control of haemorrhage by pressure being the most important interventions. Patients should not be moved unless they are in danger of further injury. In-line manual immobilisation of the cervical spine should be maintained (this can easily be combined with a jaw thrust). Where possible stand back to supervise and instruct other bystanders in first aid.
When ambulance staff arrive remember that they are the experts at working in this environment. Priorities and procedures learnt in hospital may not apply, so do not feel that you have to take control—offer your help and support while the experts do what they are trained to do. If you have no identification proving your medical qualification your assistance will probably be declined. Do not give instructions to stop resuscitation unless you are experienced at patient assessment in this environment, as it is easy to overestimate injury severity among the chaos. If you have treated a patient you should write your own notes, and you must give your name and contact details to a police officer.
Training in prehospital care
Even if well trained in hospital trauma management a doctor will not be able to perform well at the roadside without considerable extra training. Countries with doctor based prehospital care systems often have extensive postgraduate medical training in prehospital care. There is an “alphabet soup” of emergency training courses available. The prehospital immediate care course (PHIC), prehospital trauma life support course (PHTLS), and basic trauma life support course (BTLS) are specifically aimed at prehospital care providers. The Faculty of Pre-Hospital Care at the Royal College of Surgeons of Edinburgh, in conjunction with the British Association of Immediate Care Schemes, has an examination leading to a diploma in immediate care.
Action at a road crash by a trained doctor
Several prehospital systems are set up to give prehospital medical treatment by a doctor. This is the standard pattern of prehospital care throughout Europe and Scandinavia, but in Britain doctors are not part of the normal ambulance service response. Instead, UK prehospital care doctors work for the British Association of Immediate Care Schemes (which has some 1850 members), London Helicopter Emergency Service, or one of the small number of hospital “flying squads.” These doctors are trained and equipped to provide a high level of medical care in the prehospital environment and are judged against a different set of standards from “good Samaritan” doctors. They should work within a defined clinical governance framework, with set standards, ongoing training, audit, and performance review.
A road crash scene is initially uncontrolled and chaotic (fig 2). The skill of a good prehospital care doctor lies in bringing order to the chaos and being able to deliver excellent medical care in difficult circumstances. Road crash scenes may look complex, but there are a relatively small number of types, each of which has a standard method for extricating casualties and a typical set of injuries (table). A system can therefore be developed to deal with each crash type, so the expectation of a high level of performance, with clinical audit against accepted treatment standards, is just as applicable to prehospital care as it is to hospital medicine.
Figure 2.
The initially chaotic situation at a road crash scene
Approach
On arrival at a crash scene, prehospital care doctors should introduce themselves to the ambulance staff and should liaise with the senior fire service and police officers on site. The scene of a road traffic crash is always dangerous. The drivers of passing vehicles will be distracted and may hit rescue workers or the wreckage. There is a risk of fire, vehicles may be unstable, and there are many sharp edges of metal and glass. Hazards need to be identified and the scene made safe, before emergency services start to deal with casualties. Changing car design gives new challenges. A recent example is the introduction of seat belt pre-tensioners and airbags, both of which contain explosives. If these have not been activated during the crash, they may be set off during extrication of vehicle occupants.
Initial patient assessment
The basic sequence of medical priorities is much the same as in hospital trauma care. A primary survey is carried out, and any critical interventions are performed. The emphasis is on finding conditions that might cause deterioration or death during extrication, such as airway obstruction, hypoxia, or tension pneumothorax. Prehospital care doctors place less importance on auscultation (often prevented by noise), full examination (as patients are left clothed to keep warm), and monitoring equipment (which is prone to producing artefacts under these conditions). More importance is placed on the mechanism of injury and clinical assessment of physiology. Oxygen is given, the cervical spine is stabilised, and basic monitoring (pulse rate and oxygen saturation) is applied. This initial patient assessment should be rapid so that extrication can proceed.
Coordination of physical and medical rescue
After the initial assessment, the medical team must speak to the senior fire officer. Extrication of trapped casualties needs close integration of physical and medical rescue (fig 3), which requires that prehospital care doctors understand fire service extrication procedures and terminology. This understanding is ideally based on combined training. Without this coordination, extrication becomes slow, frustrating, and may be dangerous for both patient and rescuers.
Figure 3.

Teamwork between emergency services to extricate casualties safely at a road crash scene
The usual pattern is initial assessment by the medical team, who then move away. The extrication team makes space (removal of car roof and sides) and then moves aside so that the medical team can reassess, followed by the medical team stepping back again so that definitive extrication can be performed. During extrication a doctor monitors the patient's condition and provides analgesia and further critical interventions as required, while keeping out of the way of the fire service staff as much as possible. A long backboard is used to slide the casualty up and out of the car.
Further patient assessment
After extrication, the patient is reassessed. Prehospital medical interventions should address each patient's needs, giving the right intervention at the right time. There is a major emphasis on airway and breathing interventions (such as anaesthesia and intubation). Intubation without anaesthesia is unlikely to be of benefit.8 Increasing importance is attached to preventing haemorrhage by preservation of the body's natural clotting mechanism (by minimising movement, splintage, and pressure). Intravenous infusion, although traditional, now has less priority because of the lack of evidence of benefit and the possibility of harm.9,10 Research and development is required to define the optimal use of prehospital health technologies.
Packaging
Patients should be “packaged” for transport with a hard cervical collar, head blocks, limb splints if required, and a body splint such as a scoop (bivalve) stretcher or a vacuum mattress. Spinal immobilisation is a standard procedure worldwide, although no appropriate trials have been carried out to show whether this is of benefit or harm.11
The appropriate hospital for definitive care
There are often several possible hospitals to which a patient could be taken. Time to definitive intervention (usually surgery) is an important determinant of outcome in some patients.12 Prehospital doctors need to know the specialties available at each of the local hospitals so that, wherever possible, a patient is triaged direct to a hospital that can provide definitive care, avoiding the long delays and increased mortality associated with an inter-hospital transfer. This is a complex multifactorial decision in which the patient's specialist needs, the patient's physiological condition, local knowledge about the quality of hospital response, and knowledge of the transport times to the possible destinations need to be carefully weighed.
Additional educational resources
Cochrane Injuries Group (www.cochrane-injuries.lshtm.ac.uk)
Trauma.org (www.trauma.org)
World Health Organization Department of Injuries and Violence Prevention (www.who.int/violence_injury_prevention/traumacare.htm)
Faculty of Pre-Hospital Care (www.rcsed.ac.uk/phc/)
Department for Transport, Local Government and the Regions. Transport statistics: road accidents (www.transtat.dtlr.gov.uk/roadsafe/)
Joint Royal Colleges Ambulance Liaison Committee (www.jrcalc.org.uk)
Ambulance Service Association (www.asa.uk.net)
BASICS (British Association for Immediate Care) (www.basics.org.uk)
Injury Control Resource Information Network (www.injurycontrol.com/icrin/)
RoSPA (Royal Society for the Prevention of Accidents) (www.rospa.co.uk/CMS/)
National Association of Air Ambulance Services (www.naaas.co.uk)
Patient information
Headway—the brain injury association (www.headway.org.uk/)
BRAKE—the organisation for safe road transport (www.brake.org.uk)
Patients UK. UK patient support groups: accidents/trauma (www.patient.co.uk/selfhelp/accidents.htm)
Transport
The transport of a patient from the crash scene to hospital accounts for a relatively small part of the total prehospital time in most urban and semirural areas. Monitoring and treatment need to continue throughout this time as deterioration is common during patient movement. Helicopter transport can be used to cover large distances (from remote areas), to avoid congested roads, or to increase the choice of hospital (and specialists) to which a patient can be transported. Most of Europe has a network of medical helicopters staffed by prehospital care doctors, although in Britain all but one are staffed by paramedics.13
Conclusion
Prehospital care has emerged as a specialist career in Europe, Scandinavia, and the United States, where it is the most popular subspecialty training for emergency physicians. In Britain the NHS has not made a commitment to providing prehospital care doctors, leading to ad hoc local arrangements with only a small proportion of road traffic victims receiving prehospital care from a specialist doctor. However, first aid and immediate care are increasingly part of undergraduate curricula, so that future doctors may be able to be better good Samaritans. All doctors ought to think about how they would cope with the victims of a road traffic crash, as it is likely that at some time they will suddenly be put into this situation.
Table.
Different types of road traffic crash
| Mechanism of crash | Injury pattern | Extrication required |
|---|---|---|
| Pedestrian knocked down—low speed | Knee and lower leg, pelvis, degloving | |
| Pedestrian knocked down—high speed | Head, chest, abdomen, pelvis | |
| “T bone” from right | Head, right side of chest, liver, right femur, pelvis | Roof removal, steering wheel removal, B post rip |
| “T bone” from left | Head, left chest, spleen, left femur, pelvis | Roof removal, B post rip |
| Frontal collision | Head, anterior chest, posterior dislocation of hip, knee, lower leg | Roof removal, steering wheel removal, B post rip, dashboard roll |
| Frontal oblique | Head, chest, thoracic spine, pelvis, femurs, lower legs | Roof removal, steering wheel removal, pedal pull, dashboard roll |
| Rollover | Head, cervical spine, chest | Stabilisation, making space |
| Rear end shunt | Cervical spine | Roof removal, possibly B post rip |
| Motorcyclist, high speed | All body areas, especially head, chest, thoracic spine, and brachial plexus | |
| Cyclist under lorry turning left | Head, lower body crush, degloving |
Footnotes
Competing interests: TJC and GD are members of BASICS and are closely associated with the London Helicopter Emergency Medical Service. TJC is an honorary adviser to BRAKE (a charity campaigning for road safety).
References
- 1.World Health Organization Department of Injuries and Violence Prevention. www.who.int/violence_injury_prevention/index.html (accessed 8 Apr 2002).
- 2.Hussain LM, Redmond AD. Are pre-hospital deaths from accidental injury preventable? BMJ 1994;3081077-80. [DOI] [PMC free article] [PubMed]
- 3.Bunn F, Kwan I, Roberts I, Wentz R. Effectiveness of pre-hospital trauma care. Report to the World Health Organization Pre-hospital Care Steering Committee. Geneva: WHO; 2001. [Google Scholar]
- 4.Nicholl JP, Brazier JE, Snooks HA. Effects of London helicopter emergency medical service on survival after trauma. BMJ. 1995;311:217–222. doi: 10.1136/bmj.311.6999.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trunkey DD. Trauma. Sci Am. 1983;249(2):28–35. [PubMed] [Google Scholar]
- 6.Mann NC, Mullins RJ, MacKenzie EJ, Jurkovich GJ, Mock CN. Systematic review of published evidence regarding trauma system effectiveness. J Trauma. 1999;47(suppl):S25–S33. doi: 10.1097/00005373-199909001-00007. [DOI] [PubMed] [Google Scholar]
- 7.Royal College of Surgeons of England and the British Orthopaedic Association. Better care for the severely injured. London: RCS; 2000. [Google Scholar]
- 8.Lockey D, Davies G, Coats TJ. Survival of trauma patients who have prehospital tracheal intubation without anaesthesia or muscle relaxants: observational study. BMJ. 2001;323:141. doi: 10.1136/bmj.323.7305.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kwan I, Bunn F, Roberts I. Timing and volume of fluid administration for patients with bleeding following trauma. Cochrane Database Syst Rev 2001;(1):CD002245. [DOI] [PubMed]
- 10.Roberts I, Evans P, Bunn F, Kwan I, Crowhurst E. Is the normalisation of blood pressure in bleeding trauma patients harmful? Lancet. 2001;357:385–387. doi: 10.1016/S0140-6736(00)03653-9. [DOI] [PubMed] [Google Scholar]
- 11.Kwan I, Bunn F, Roberts I. Spinal immobilisation for trauma patients. Cochrane Database Syst Rev 2001;(2):CD002803. [DOI] [PMC free article] [PubMed]
- 12.Chesnut RM, Marshall LF, Klauber MR, Blunt BA, Baldwin N, Eisenberg HM, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34:216–222. doi: 10.1097/00005373-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 13.National Association of Air Ambulance Services. www.naaas.co.uk (accessed 8 Apr 2002).