Abstract
Mental fitness is a construct that goes beyond a simple focus on subjective emotional wellbeing to encompass more broadly our ability to think, feel, and act to achieve what we want in our daily lives. The measurement and monitoring of multiple (often interacting) domains is crucial to gain a holistic and complete insight into an individual’s mental fitness. We aimed to demonstrate the capability of a new mobile app to characterise the mental fitness of a general population of Australians and to quantify the interrelationships among different domains of mental fitness. Cross-sectional data were collected from 4901 adults from the general population of Australians engaged in work or education who used a mobile app (Innowell) between September 2021 and November 2022. Individuals completed a baseline questionnaire comprised of 26 questions across seven domains of mental fitness (i.e., physical activity, sleep and circadian rhythms, nutrition, substance use, daily activities, social connection, psychological distress). Network analysis was applied at both a domain-level (e.g., 7 nodes representing each cluster of items) and an individual item-level (i.e., 26 nodes representing all questionnaire items). Only 612 people (12%) were functioning well across all domains. One quarter (n = 1204, 25%) had only one problem domain and most (n = 3085, 63%) had multiple problem domains. The two most problematic domains were physical activity (n = 2631, 54%) and social connection (n = 2151, 44%), followed closely by daily activity (n = 1914, 39%). At the domain-level, the strongest association emerged between psychological distress and daily activity (r = 0.301). Psychological distress was the most central node in the network (as measured by strength and expected influence), followed closely by daily activity, sleep and circadian rhythms and then social connection. The item-level network revealed that the nodes with the highest centrality in the network were: hopelessness, depression, functional impairment, effortfulness, subjective energy, worthlessness, and social connectedness. Social connection, sleep and circadian rhythms, and daily activities may be critical targets for intervention due to their widespread associations in the overall network. While psychological distress was not among the most common problems, its centrality may indicate its importance for indicated prevention and early intervention. We showcase the capability of a new mobile app to monitor mental fitness and identify the interrelationships among multiple domains, which may help people develop more personalised insights and approaches.
Subject terms: Disease prevention, Public health, Quality of life, Risk factors
Introduction
Mental health is a fundamental part of our overall health and wellbeing, and it is commonly recognised that there is “no health without mental health”1. This sentiment reflects how mental health is not just isolated to cognitions and emotions (how we think and feel), but instead it connects to many social and biological components of what it means to be human. This broad view of mental health encapsulates the related but distinct concepts of mental illness and mental fitness.
Mental fitness is a continuum that encompasses personal autonomy alongside social connection and participation. It goes beyond a simple focus on ‘mood’ or subjective emotional wellbeing to encompass more broadly our ability to think, feel, and act to achieve what we want in our daily lives. It is not a new concept and many versions of it have been presented over the past few decades which includes concepts of positive psychology, wellbeing, and flourishing2,3. The pursuit of a mental fitness concept largely reflects the need for a construct that is measurable, improvable (like physical fitness), and distinct from mental illness in that it focuses on the positive aspects of human cognition, emotion, and behaviour4. By contrast, mental illness (or disorder), which has a distinct focus on distressing experiences and symptoms, has its own continuum of illness stages and severity that have differential risks of progression and recurrence5,6,7.
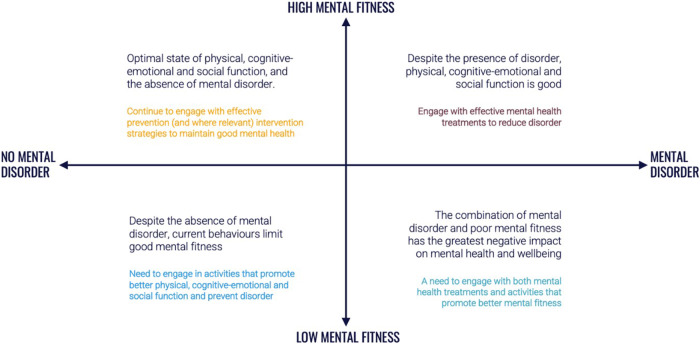
Globally, it is estimated that almost one in three people will experience a mental disorder in their lifetime, and that approximately one in five people have experienced a major disorder within the past 12-months8. Many people may never experience a mental illness, though all of us will move up and down the related but distinct continuum of mental fitness over the course of our lives (Fig. 1). For some, these oscillations may be more frequent or severe, and increase the risk of more serious mental health problems and illness. For others, the distinction between illness and fitness reflects how functioning and mental health may not always be directly correlated, particularly for those self-managing an illness (e.g., those in the top right quadrant of Fig. 1). Much like we do for our physical health, using evidence-based strategies to monitor and enhance mental fitness, alongside regular checks of our mental health, is important to promote to the widest possible population groups.
Fig. 1.
The continuums of mental fitness and the mental disorder.
A focus on multiple (often interacting) domains is important to gain a holistic and complete insight into an individual’s mental fitness. Current holistic measures tend to focus on subjective positive well-being states and quality of life based on positive psychology concepts, though few measures capture a broader set of behaviours important for mental fitness9,10, including those that emphasize physiological and not just psychological domains. The domains most relevant for this include aspects of our physical health related to physical activity, sleep and circadian rhythms, nutrition and substance use; our cognitive-emotional health (e.g., mood, anxiety, stress); and our social health, which includes functioning in daily roles and social connections11–21. Problems in any one of these domains may be indicative of an increased risk for poorer health outcomes that may be due to dysfunction (or sub-optimal function) in one or more underlying systems which govern most of our behaviour, cognition, and emotion. For example, poor cognitive-emotional health could reflect prolonged activation of the stress response system22, which regulates our hormonal response to stress; or poor sleep quality or energy during the day may suggest dysfunction of the circadian system, which orchestrates the daily rhythmic timing of almost all physiological processes and behaviours23.
The rise of digital technologies provides the opportunity for monitoring and managing various aspects of our mental fitness. While there are numerous health apps available24, there is a growing need for more comprehensive tools that can assess and address the interconnected nature of these social, physical and cognitive-emotional dimensions. By identifying the patterns and relationships between these dimensions, people can develop more personalised insights and recommendations to enhance their unique mental fitness and reduce future risks. The objective of this paper is to demonstrate the capability of a new mobile app (‘Innowell’) to characterise the mental fitness of a general population of Australians and to quantify the interrelationships among the social, physical, and cognitive-emotional domains of mental fitness.
Results
Domain Ratings
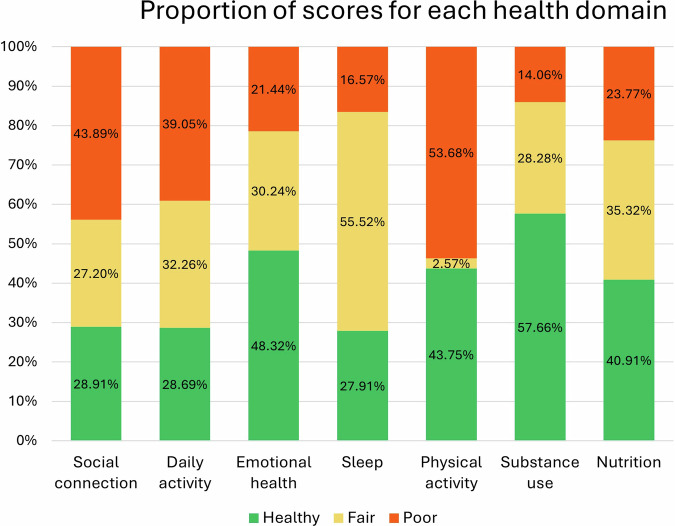
A total of 4901 individuals completed the initial questionnaire and were eligible for analyses, though socio-demographics were not available for this study. Only 612 people (12%) of the population had scores that were ‘healthy’ or ‘fair’ across all domains. About a quarter (n = 1204, 25%) had only one ‘poor’ domain, and the majority (n = 3085, 62%) had multiple ‘poor’ domain. The two most problematic domains were physical activity (n = 2631, 54%) and social connection (n = 2151, 44%), followed closely by daily activity (n = 1914, 39%) (Fig. 2).
Fig. 2.
Proportion of scores for each health domain. Total completions n = 4901.
Domain-level Network
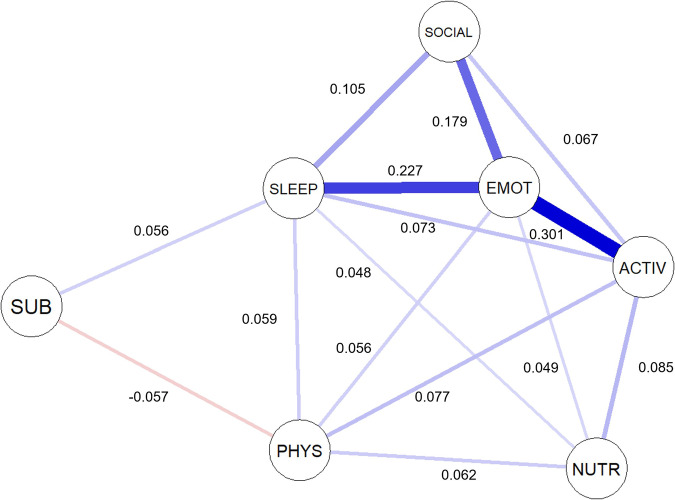
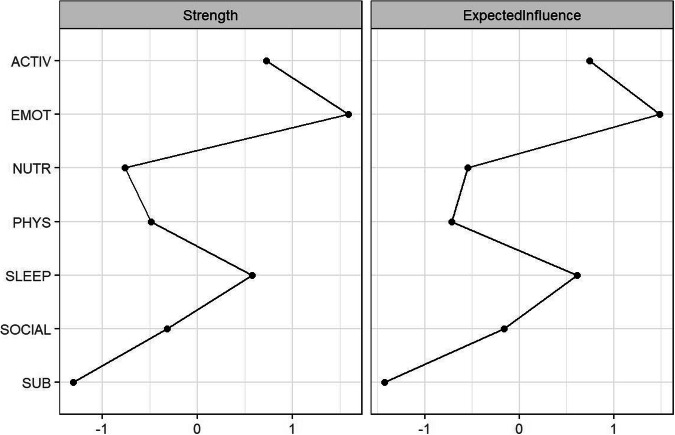
The domain-level network is presented in Fig. 3. Each domain was connected either directly or indirectly via other domains in the network. The strongest association emerged between psychological distress and daily activity (r = 0.301), while the weakest non-zero association was between nutrition and sleep and circadian rhythms (r = 0.048). Of the possible 21 associations across all domains, 71.43% (n = 15) were nonzero with only one negative relationship identified, between substance use and physical activity (r = −0.057). Psychological distress was the most central node in the network (as measured by strength and expected influence) (Fig. 4), followed closely by daily activity and sleep and circadian rhythms.
Fig. 3. A network model to infer cross-sectional relationships between social, cognitive-emotional, and physical health areas for a general population (n = 4901).
The network plot was developed in accordance with the Fruchterman-Reingold algorithm60, which places edges with greater absolute coefficient values closer together. The blue edges represent positive partial correlations, whereas the red edges represent negative partial correlations. Social = social connection; activ = daily activities; emot = psychological distress; sleep = sleep and circadian rhythms; phys = physical activity; sub = substance use; and nutr = nutrition.
Fig. 4.
Domain-level centrality plots. Social = social connection; activ = daily activities; emot = psychological distress; sleep = sleep and circadian rhythms; phys = physical activity; sub = substance use; and nutr = nutrition.
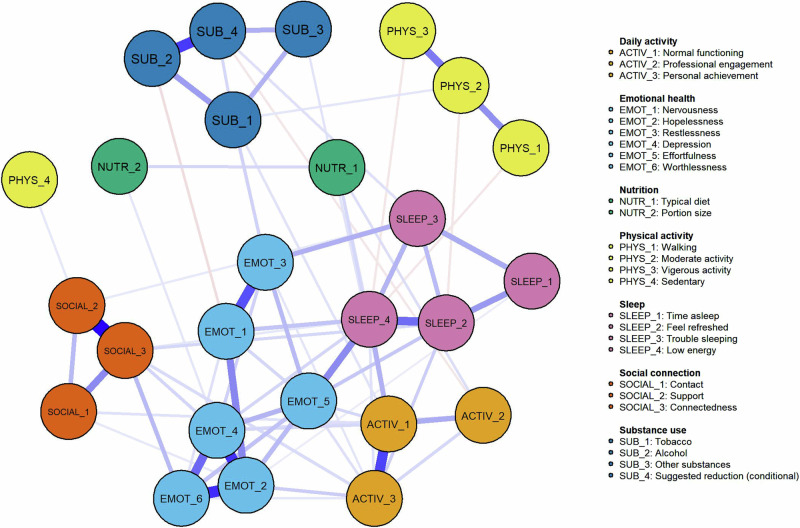
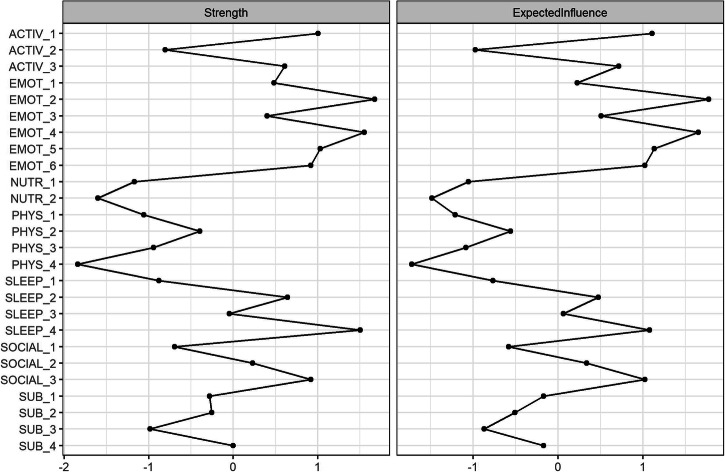
Item-level Network
For the item-level network, all items were connected either directly or indirectly via other symptoms in the network (Fig. 5). The nodes with the highest expected influence centrality in the network were (Fig. 6); Emot_2 (Hopelessness), Emot_4 (Depression), Activ_1 (Normal functioning), Emot_5 (Effortfulness), Sleep_4 (Subjective energy), Emot_6 (Worthlessness), and Social_3 (Connectedness).
Fig. 5.
Item-level network model to infer cross-sectional relationships between 26 items from the Innowell Questionnaire.
Fig. 6.
Item-level centrality plots.
Discussion
This study presents cross-sectional data about the mental fitness of a general population of adult Australians and quantifies the relationship between these domains. Very few people were healthy across all domains, with most of the population having two or more areas that could be improved. Physical activity, social connection and daily activity were the three most common problem areas. Centrality analyses indicated that psychological distress, daily activity, and sleep and circadian rhythms had the highest influence in the network. This work highlights which domains may be particularly important for mental fitness, however longitudinal studies of these relationships would offer further insights about indicated prevention and early intervention approaches.
The psychological distress domain asks people about common symptoms of depression, anxiety, and stress. Four individual items from this domain (hopelessness, depression, effortfulness, and worthlessness) were part of the top five most central nodes in the item-level network. In conjunction with psychological distress being the most central node in the domain-level network, this finding demonstrates how cognitive-emotional health is strongly linked to both social and physical health. While psychological distress is increasingly common in Australia’s general population25, it is positively associated with mental ill-health18,19.
In this cohort, only 21% were identified as having ‘poor’ psychological distress, yet its strong connections with common problem areas (social connection, sleep and circadian rhythms, and daily activity) emphasise the need for indicated prevention and early intervention in these areas to avoid the development of vicious cycles of worsening outcomes. The strongest domain-level association was between psychological distress and daily activity. Daily activity specifically measures whether a person can ‘carry out daily tasks’ and ‘achieve the things you want to’ in daily roles, and so its widespread impact to other areas is significant. Functional impairment is common among those with mental illness and changes in functioning are often an early sign of mental ill-health18,26–29. Major functional impairment is associated with worse mental health outcomes30, future suicidality31, and is positively correlated with the severity of mental illness7. This reinforces the need for regular monitoring of daily activities and functioning, so that early changes or problems in this area can be promptly detected and proactively responded to before these problems get worse or exacerbate problems in other areas.
Social connection was one of the most commonly reported problems with high centrality, which is concerning given its known widespread effects on health and wellbeing. Social isolation and disconnection are associated with higher rates of mental disorders32, and associated with poor long-term outcomes (including increased mortality risk)33. We identified a strong association between social connection and psychological distress, specifically feelings of depression and worthlessness, which reiterates the increased vulnerability among socially isolated individuals. Growing evidence points to common mechanisms involving elevated activity to the sympathetic nervous system and hypothalamus-pituitary-adrenal axis, as well as chronic inflammation, which may link social isolation and disconnection to deteriorating mental health and other poor health outcomes34,35. Altogether, this work suggests that indicated prevention and early intervention strategies that help people develop and maintain quality social relationships with friends and family and foster deeper connection to their communities may be critical to enhance mental fitness and prevent further health problems in other areas36.
The centrality of sleep and circadian rhythms in the domain-network is particularly important given that it was identified as 'poor' or 'fair' for over two-thirds of the population and had the second strongest domain-level association (psychological distress and sleep and circadian rhythms, r = 0.227). The relationship between sleep and circadian rhythms and mental health is well established, with many people reporting a range of sleep and circadian disturbances (e.g. trouble falling asleep, insomnia, fatigue, etc)12,37 that are typically associated with increased stress, depression, and state anxiety, and usually worsen with more severe illness7,38. We identified that subjective energy had strong connections in the network, particularly with being able to ‘carry out daily tasks’ and ‘effortfulness’. This is consistent with evidence which indicates that subjective energy may be an effective intervention target for mood, as some targeted sleep and circadian interventions have been shown to also improve energy and mood39,40. Taking steps to improve the 24-hour sleep-wake cycle may contribute to better mood, cognitive-emotional regulation, help reduce symptoms of mental illnesses39,41–43, and may reduce the likelihood of developing a mental disorder12,30.
Despite the strong relationship between sleep and circadian rhythms with both social and cognitive-emotional health, the remaining areas of physical health (nutrition, physical activity, and substance use) had relatively weak associations with other domains in the network. Each of these domains tended to be quite independent. This may reflect that their emergence is dependent on other factors not measured by the current physical, social, and cognitive-emotional domains, and/or that their relationship with other domains is more specific to certain subgroups within this population, and therefore unable to be detected by the current analyses. Nonetheless, their independence could reflect that these physical health areas require more specific preventative and intervention strategies since they may be less amendable to cascading effects from improvements in other domains of social and cognitive-emotional health.
This study has several limitations that should be considered alongside our findings. Firstly, we did not collect demographics for the current analyses. Therefore, the interpretation and generalisability of these results is limited as we are unable to determine the effect of age, gender, and other characteristics on the networks or say anything about who is more likely to use this app. While this is a major limitation, the focus of this work was on the interrelationships between these key domains and so future work should aim to include more detailed analyses of these characteristics. Secondly, the data were cross-sectional which does not allow conclusions about the longitudinal relationship between domains. The interactions among these domains over time may have the greatest influence on mental fitness and the emergence of illness. Their effects are probably not simply additive, but are likely part of a complex system characterised by non-linear relationships and feedback loops, which could lead to unexpected outcomes44. Thus, to achieve a holistic view of a person’s mental fitness, it is not sufficient to focus on single components alone, but important to monitor how these factors evolve and influence each other over time. Future studies with time-series data are needed to determine this. Finally, we relied on self-report measures. There is a growing need for passive data collection which can reduce burden on participants, increase the accuracy of data collected, and provide high frequency and valuable insights about individual patterns over time.
In conclusion, most people have areas of mental fitness that could be improved. Social connection, sleep and circadian rhythms and daily activities emerged as being potential targets for intervention due to their widespread associations in the overall network. While psychological distress was not among the most common problems, it was highly central in the network with connections to all domains (except for substance use), emphasising the key role of psychological distress in overall health and wellbeing. We showcase the use of digital technologies to monitor mental fitness and identify the interrelationships among multiple domains, which may help people develop more personalised insights and recommendations to enhance their mental fitness and reduce future risks.
Methods
Ethics
All data for this study was collected through a quality assurance process facilitated by the University of Sydney research team. All data is non-identifiable to protect the privacy of participants.
Innowell
Innowell is a mobile app that provides research validated, professional tools for people to monitor and reflect on their mental fitness. It includes (1) real-time assessments about each domain of a person’s mental fitness; (2) actionable insights about each domain of mental fitness; (3) personalised recommendations with evidence-based strategies and resources to understand and manage mental fitness; and (4) a goal setting and tracking tool which provide people with habit-forming activities designed to improve their mental fitness. The development of this tool involved a team of psychologists, psychiatrists, mental health research experts, and those with lived experience, who selected items that measure various components of mental fitness and collated evidence-based strategies and resources for mental fitness.
Dataset
The dataset is comprised of adults from a general population of Australians engaged in work or education who used Innowell between September 2021 and November 2022. The platform was offered to them as part of a mental health and wellbeing initiative, and so sign up and completion of the baseline questionnaire was self-directed. All data has been anonymised and shared for quality assurance with no identifying personal information available for reporting, in accordance with the privacy policy. The only measures reported here are individual responses to real-time assessments for each of the mental fitness domains to understand the interrelationships between them.
The measures used for these domains include; (i) social connection, three items from Schuster’s Social Support Scale45 which ask about social contact, support and wider family, cultural or community connectedness; (ii) daily activities, three items which ask about educational and employment engagement and participation, and personal achievement46,47; (iii) psychological distress, six items from the Kessler-6 which ask about common symptoms of depression, anxiety and stress48; (iv) sleep and circadian rhythms, four items which ask about time spent sleeping, feeling refreshed after sleep, trouble falling asleep and subjective energy49–51; (v) physical activity, four items from the International Physical Activity Questionnaire to measure of time spent engaged in walking, moderate exercise, vigorous exercise and sedentary behaviours52–55; (vi) substance use, four items about the use of tobacco, alcohol and other substances, and whether they should cut down56,57; and (vii) nutrition, two items about typical diet type and portion size58. See Supplementary Table 1 for further details.
Statistical analyses
All statistical analyses were performed in R version 4.2.159.
Statistical analyses were conducted in R. Frequency counts and proportions were obtained for scores across each mental fitness domain. We then applied network analysis to the data at both a domain-level (e.g., 7-nodes representing each cluster of items), and an individual item-level (i.e., 26-nodes representing all questionnaire items) to identify the dependency structure between domains and items measuring mental fitness. For this a partial correlation network was estimated using the graphical Least Absolute Shrinkage and Selection Operator (gLASSO) algorithm60. This algorithm estimates the partial correlation coefficients using a regularisation technique that limits the number of spurious edges. The regularisation parameter for the gLASSO algorithm was selected by minimising the Extended Bayesian Information Criteria (EBIC)61–64. As the dataset contains ordinal data, we used the polychoric correlation matrix as input for the network estimation algorithm61,63,64.
Accuracy and stability of edge-weights in the network were examined using nonparametric and case-dropping subset bootstrapping procedures62,64. Strength and expected influence were considered as the most reliable centrality measures and both measures gave similar results. The strength represents the sum of the absolute partial correlation coefficients. Expected Influence uses the summed partial correlation coefficients (i.e., including the sign) extending away from each node. These measures estimate how central a node is in the diagram, which assuming relationships are bidirectional can be thought of as a measure of influence that changing that node will have on the other nodes. We report these centrality measures, along with their bootstrapped 95% intervals.
Supplementary information
Acknowledgements
This work was supported by the NHMRC Australia Fellowship (No. 511921 awarded to Prof Hickie). Frank Iorfino was supported by the Bill and Patricia Ritchie Foundation Fellowship and by an NHMRC Emerging Leadership Fellowship (GNT2018157). William Capon was supported by an Australian Government Research Training Program (RTP) Scholarship. Jacob Crouse was supported by an NHMRC Emerging Leadership Fellowship (GNT2008197).
Author contributions
F.I., M.V., W.C., and I.B.H. drafted the manuscript. M.V. & M.R. conducted the data analyses. All authors (F.I., M.V., W.C., M.R., J.J.C., H.M.L., S.H.P., S.P., Y.J.C.S., C.G., E.M.S., and I.B.H.) provided valuable interpretations of the data, made significant edits to the manuscript, and approved the final version of the manuscript for submission.
Data availability
The data presented in this manuscript is available upon reasonable request.
Competing interests
A/Prof Elizabeth Scott is Principal Research Fellow at the Brain and Mind Centre, The University of Sydney. She is Discipline Leader of Adult Mental Health, School of Medicine, University of Notre Dame, and a Consultant Psychiatrist. She was the Medical Director, Young Adult Mental Health Unit, St Vincent’s Hospital Darlinghurst until January 2021. She has received honoraria for educational seminars related to the clinical management of depressive disorders supported by Servier, Janssen and Eli-Lilly pharmaceuticals. She has participated in a national advisory board for the antidepressant compound Pristiq, manufactured by Pfizer. She was the National Coordinator of an antidepressant trial sponsored by Servier. Professor Ian Hickie is the Co-Director, Health and Policy at the Brain and Mind Centre (BMC) University of Sydney. The BMC operates an early-intervention youth services at Camperdown under contract to headspace. He is the Chief Scientific Advisor to, and a 3.2% equity shareholder in, InnoWell Pty Ltd. InnoWell was formed by the University of Sydney (45% equity) and PwC (Australia; 45% equity) to deliver the $30 M Australian Government-funded Project Synergy (2017-20; a three-year program for the transformation of mental health services) and to lead transformation of mental health services internationally through the use of innovative technologies.All other authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s44184-024-00078-7.
References
- 1.Prince M, et al. No health without mental health. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 2.Seligman ME, Csikszentmihalyi M. Positive psychology. An introduction. Am. Psychol. 2000;55:5–14. doi: 10.1037/0003-066X.55.1.5. [DOI] [PubMed] [Google Scholar]
- 3.Keyes CL. Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am. Psychol. 2007;62:95–108. doi: 10.1037/0003-066X.62.2.95. [DOI] [PubMed] [Google Scholar]
- 4.Robinson P., Oades L. & Caputi P. Conceptualising and Measuring Mental Fitness: A Delphi Study. Int. and J. Wellbeing. 5, 2015.
- 5.McGorry PD, Hickie IB, Yung AR, Pantelis C, Jackson HJ. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust. N. Z. J. Psychiatry. 2006;40:616–622. doi: 10.1080/j.1440-1614.2006.01860.x. [DOI] [PubMed] [Google Scholar]
- 6.Scott J., et al. Staging 2.0: refining transdiagnostic clinical staging frameworks to enhance reliability and utility for youth mental health. Lancet Psychiat. 2024. [DOI] [PubMed]
- 7.Iorfino F, et al. Clinical Stage Transitions in Persons Aged 12 to 25 Years Presenting to Early Intervention Mental Health Services With Anxiety, Mood, and Psychotic Disorders. JAMA Psychiatry. 2019;76:1167–1175. doi: 10.1001/jamapsychiatry.2019.2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steel Z, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int. J. Epidemiol. 2014;43:476–493. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sierk A, et al. A New Digital Assessment of Mental Health and Well-being in the Workplace: Development and Validation of the Unmind Index. JMIR Ment. Health. 2022;9:e34103. doi: 10.2196/34103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Su R, Tay L, Diener E. The development and validation of the Comprehensive Inventory of Thriving (CIT) and the Brief Inventory of Thriving (BIT) Appl Psychol. Health Well Being. 2014;6:251–279. doi: 10.1111/aphw.12027. [DOI] [PubMed] [Google Scholar]
- 11.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985;98:310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- 12.Freeman D, Sheaves B, Waite F, Harvey AG, Harrison PJ. Sleep disturbance and psychiatric disorders. Lancet Psychiatry. 2020;7:628–637. doi: 10.1016/S2215-0366(20)30136-X. [DOI] [PubMed] [Google Scholar]
- 13.Fusar-Poli P, et al. What is good mental health? A scoping review. Eur. Neuropsychopharmacol. 2020;31:33–46. doi: 10.1016/j.euroneuro.2019.12.105. [DOI] [PubMed] [Google Scholar]
- 14.Hermens D. F. et al. Frequent alcohol, nicotine or cannabis use is common in young persons presenting for mental healthcare: a cross-sectional study. BMJ Open. 2013;3. [DOI] [PMC free article] [PubMed]
- 15.Hosker DK, Elkins RM, Potter MP. Promoting Mental Health and Wellness in Youth Through Physical Activity, Nutrition, and Sleep. Child Adolesc. Psychiatr. Clin. N. Am. 2019;28:171–193. doi: 10.1016/j.chc.2018.11.010. [DOI] [PubMed] [Google Scholar]
- 16.Mikkelsen K, Stojanovska L, Polenakovic M, Bosevski M, Apostolopoulos V. Exercise and mental health. Maturitas. 2017;106:48–56. doi: 10.1016/j.maturitas.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Owen L, Corfe B. The role of diet and nutrition on mental health and wellbeing. Proc. Nutr. Soc. 2017;76:425–426. doi: 10.1017/S0029665117001057. [DOI] [PubMed] [Google Scholar]
- 18.Purcell R, et al. Demographic and clinical characteristics of young people seeking help at youth mental health services: baseline findings of the Transitions Study. Early Inter. Psychiatry. 2015;9:487–497. doi: 10.1111/eip.12133. [DOI] [PubMed] [Google Scholar]
- 19.Scott EM, et al. Targeted primary care-based mental health services for young Australians. Med. J. Aust. 2012;196:136–140. doi: 10.5694/mja11.10481. [DOI] [PubMed] [Google Scholar]
- 20.Shankar J, Barlow CA, Khalema E. Work, employment, and mental illness: expanding the domain of Canadian social work. J. Soc. Work Disabil. Rehabil. 2011;10:268–283. doi: 10.1080/1536710X.2011.622991. [DOI] [PubMed] [Google Scholar]
- 21.Umberson D, Montez JK. Social relationships and health: a flashpoint for health policy. J. Health Soc. Behav. 2010;51:S54–S66. doi: 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chu B., Marwaha K., Sanvictores T. & Ayers D. Physiology, Stress Reaction. StatPearls. Treasure Island (FL)2023. [PubMed]
- 23.Walker WH, 2nd, Walton JC, DeVries AC, Nelson RJ. Circadian rhythm disruption and mental health. Transl. Psychiatry. 2020;10:28. doi: 10.1038/s41398-020-0694-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neary M, Schueller SM. State of the Field of Mental Health Apps. Cogn. Behav. Pr. 2018;25:531–537. doi: 10.1016/j.cbpra.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Enticott J, et al. Mental Health in Australia: Psychological Distress Reported in Six Consecutive Cross-Sectional National Surveys From 2001 to 2018. Front Psychiatry. 2022;13:815904. doi: 10.3389/fpsyt.2022.815904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldstein TR, et al. Psychosocial functioning among bipolar youth. J. Affect Disord. 2009;114:174–183. doi: 10.1016/j.jad.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McIntyre RS, et al. Cognitive deficits and functional outcomes in major depressive disorder: determinants, substrates, and treatment interventions. Depress Anxiety. 2013;30:515–527. doi: 10.1002/da.22063. [DOI] [PubMed] [Google Scholar]
- 28.Romanowska S, et al. Social and role functioning in youth at risk of serious mental illness. Early Inter. Psychiatry. 2020;14:463–469. doi: 10.1111/eip.12872. [DOI] [PubMed] [Google Scholar]
- 29.O’Dea B, et al. A prospective cohort study of depression course, functional disability, and NEET status in help-seeking young adults. Soc. Psychiatry Psychiatr. Epidemiol. 2016;51:1395–1404. doi: 10.1007/s00127-016-1272-x. [DOI] [PubMed] [Google Scholar]
- 30.Iorfino F. et al. A Digital Platform Designed for Youth Mental Health Services to Deliver Personalized and Measurement-Based Care. Frontiers in Psychiatry. 2019;10. [DOI] [PMC free article] [PubMed]
- 31.Iorfino F, et al. Predicting self-harm within six months after initial presentation to youth mental health services: A machine learning study. PLoS One. 2020;15:e0243467. doi: 10.1371/journal.pone.0243467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wickramaratne PJ, et al. Social connectedness as a determinant of mental health: A scoping review. PLoS One. 2022;17:e0275004. doi: 10.1371/journal.pone.0275004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect. Psychol. Sci. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 34.Holt-Lunstad J. The Major Health Implications of Social Connection. Curr. Direct. Psychol. Sci. 2021;30:251–259. doi: 10.1177/0963721421999630. [DOI] [Google Scholar]
- 35.Lamblin M, Murawski C, Whittle S, Fornito A. Social connectedness, mental health and the adolescent brain. Neurosci. Biobehav Rev. 2017;80:57–68. doi: 10.1016/j.neubiorev.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 36.Killaspy H, et al. Community-based social interventions for people with severe mental illness: a systematic review and narrative synthesis of recent evidence. World Psychiatry. 2022;21:96–123. doi: 10.1002/wps.20940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Germain A, Kupfer DJ. Circadian rhythm disturbances in depression. Hum. Psychopharmacol. 2008;23:571–585. doi: 10.1002/hup.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Babson KA, Trainor CD, Feldner MT, Blumenthal H. A test of the effects of acute sleep deprivation on general and specific self-reported anxiety and depressive symptoms: an experimental extension. J. Behav. Ther. Exp. Psychiatry. 2010;41:297–303. doi: 10.1016/j.jbtep.2010.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Crouse JJ, et al. Circadian rhythm sleep-wake disturbances and depression in young people: implications for prevention and early intervention. Lancet Psychiatry. 2021;8:813–823. doi: 10.1016/S2215-0366(21)00034-1. [DOI] [PubMed] [Google Scholar]
- 40.Merikangas KR, et al. Real-time Mobile Monitoring of the Dynamic Associations Among Motor Activity, Energy, Mood, and Sleep in Adults With Bipolar Disorder. JAMA Psychiatry. 2019;76:190–198. doi: 10.1001/jamapsychiatry.2018.3546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Freeman D, et al. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. 2017;4:749–758. doi: 10.1016/S2215-0366(17)30328-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Harvey AG, et al. Treating insomnia improves mood state, sleep, and functioning in bipolar disorder: a pilot randomized controlled trial. J. Consult Clin. Psychol. 2015;83:564–577. doi: 10.1037/a0038655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr. Opin. Psychiatry. 2005;18:189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 44.Fried EI. Theories and Models: What They Are, What They Are for, and What TheyAre About. Psychol. Inq. 2020;31:336–344. doi: 10.1080/1047840X.2020.1854011. [DOI] [Google Scholar]
- 45.Schuster TL, Kessler RC, Aseltine RH., Jr Supportive interactions, negative interactions, and depressed mood. Am. J. Community Psychol. 1990;18:423–438. doi: 10.1007/BF00938116. [DOI] [PubMed] [Google Scholar]
- 46.Office for National Statistics. UK Estimate of Young People Not in Education, Employment or Training (London, UK 2013).
- 47.World Health Organisation. Measuring health and disability: manual for WHO Disability Assessment Schedule (WHODAS 2.0). Ustun T. B., et al. editor. Geneva 2010. 88 p.
- 48.Kessler RC, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002;32:959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- 49.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 50.Vernon MK, Dugar A, Revicki D, Treglia M, Buysse D. Measurement of non-restorative sleep in insomnia: A review of the literature. Sleep. Med. Rev. 2010;14:205–212. doi: 10.1016/j.smrv.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 51.Zhang J, et al. Differentiating nonrestorative sleep from nocturnal insomnia symptoms: demographic, clinical, inflammatory, and functional correlates. Sleep. 2013;36:671–679. doi: 10.5665/sleep.2624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Craig CL, et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 53.Danquah IH, Petersen CB, Skov SS, Tolstrup JS. Validation of the NPAQ-short – a brief questionnaire to monitor physical activity and compliance with the WHO recommendations. BMC Public Health. 2018;18:601. doi: 10.1186/s12889-018-5538-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.World Health Organization. WHO guidelines on physical activity and sedentary behaviour. 2020. [PubMed]
- 55.Chaput J-P, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: summary of the evidence. Int. J. Behav. Nutr. Phys. Act. 2020;17:141. doi: 10.1186/s12966-020-01037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Newcombe DA, Humeniuk RE, Ali R. Validation of the world health organization alcohol, smoking and substance involvement screening test (ASSIST): report of results from the Australian site. Drug Alcohol Rev. 2005;24:217–226. doi: 10.1080/09595230500170266. [DOI] [PubMed] [Google Scholar]
- 57.Australian Government Department of Health and Aged Care. About drugs: Commonwealth of Australia; 2019.
- 58.Australian Government. Australian Dietary Guidelines Providing the scientific evidence for healthier Australian diets. 2013.
- 59.R Core Team. R: A Language and Environment for Statistical Computing. (Vienna, Austria: R Foundation for Statistical Computing; 2022).
- 60.Fruchterman TMJ, Reingold EM. Graph Drawing by Force-Directed Placement. Softw. Pract. Exp. 1991;21:1129–1164. doi: 10.1002/spe.4380211102. [DOI] [Google Scholar]
- 61.Foygel R. & Drton M. Extended Bayesian Information Criteria for Gaussian Graphical Models. Adv. Neural Inform. Proc. Syst. 2010;23.
- 62.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods. 2018;50:17. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Epskamp S, Cramer AO, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: Network Visualizations of Relationships in Psychometric Data. J. Stat. Softw. 2012;48:18. doi: 10.18637/jss.v048.i04. [DOI] [Google Scholar]
- 64.Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychol. Methods. 2018;23:617–634. doi: 10.1037/met0000167. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this manuscript is available upon reasonable request.