Abstract
Calcific tendinitis, classified as enthesopathy, is a self-limiting disease that rarely involves the tendons of the gluteus maximus. We discuss a 52-year-old woman with a 1-year history of localized, reproducible posterolateral pain of her left hip, which was previously treated with steroid injection to her left greater trochanteric bursa without significant pain relief. Plain radiography and magnetic resonance imaging of the left hip revealed abnormal edema and calcifications at the insertion of the gluteus maximus tendon to the gluteal tuberosity, corresponding to the area of maximal tenderness on examination. This case report contributes to the growing medical literature for the rare presentation of calcific tendinitis of gluteus maximus insertion and reinforces the importance of the patient history, focused physical examination with special testing, and pertinent imaging for proper diagnosis and management.
Keywords: Calcific tendinitis, Calcium deposition, Gluteus maximus, Musculoskeletal, Sports medicine, Orthopedic surgery
Introduction
Calcific tendinitis of the gluteus maximus, characterized by calcium deposits within the tendon of gluteal muscles, is not commonly reported in medical literature. Patients typically present with sharp, localized pain as a consequence of local tendon inflammation. Plain radiography, computed tomography, magnetic resonance imaging, and ultrasonography are diagnostic imaging modalities that can be utilized to identify calcium deposits near the gluteus maximus tendinous insertion. Conservative management includes NSAIDs, physical therapy, and ultrasound-guided steroid injection [1] to reduce local inflammation. Minimally invasive percutaneous needle tenotomy [2] or surgical debridement of the calcific deposit, with or without tendon repair, may be required in refractory cases [3]. Understanding the nuances of calcific tendinitis of the gluteus maximus is important for proper diagnosis and management.
Case report
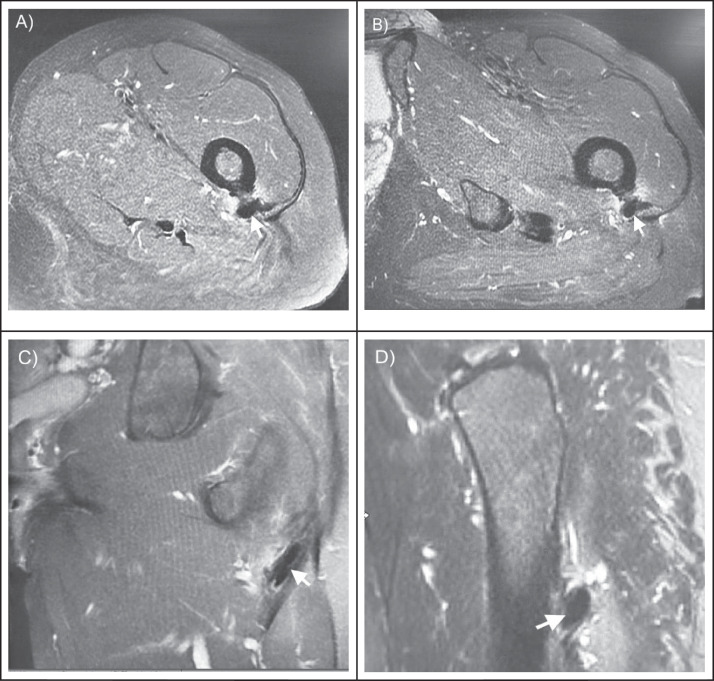
A 52-year-old woman who presented to an outpatient Sports Medicine clinic with gradual onset of left posterolateral hip pain of 1-year duration. The pain was exacerbated by walking, climbing stairs, and sit-to-stand repositioning. There was no history of trauma, fever, or unintentional weight loss. The patient was previously treated with steroid injection for suspected greater trochanteric bursitis without significant pain relief. On focused examination of the left hip, the patient had full range of motion and there were no obvious signs of deformity. She noted reproduction of her localized pain with active hip extension and thigh abduction. The pain was also reproduced upon passive hip flexion with thigh adduction and knee extension. She was exquisitely tender to palpation at the posterolateral aspect of her left thigh, distal to the greater trochanter. Special testing: FABER, FADIR, Hip Quadrant Scour, Stinchfield, and Straight Leg Raise (SLR) did not reproduce her pain. Plain radiography and magnetic resonance imaging of the left hip revealed abnormal edema and calcifications at the insertion of the gluteus maximus tendon to the gluteal tuberosity (Fig. 1, Fig. 2), corresponding to the area of maximal tenderness on examination. The focused physical exam and imaging findings were diagnostic for calcific tendinitis of the gluteus maximus insertion. The patient was offered an ultrasound-guided steroid injection and referral to Orthopedic Surgery. She preferred to discuss her case with Orthopedic Surgery prior to any intervention.
Fig. 1.
MRI of the left hip with foci of globular signal void near the posterior subtrochanteric region of the proximal femur at the insertion of the gluteus maximus (white arrows). Proton density-weighted, fat suppressed, A) axial view, B) axial-oblique view, and C) coronal view, and D) T2-weighted, fat suppressed, sagittal view.
Fig. 2.
Radiographs of the left hip, A) anteroposterior view and B) lateral view, showing calcified deposit (white arrows) near the proximal femoral subtrochanteric region at the insertion of the gluteus maximus.
Discussion
Calcific tendinitis, classified as enthesopathy, is a self-limiting disease characterized by the deposition of calcium phosphate crystals in tendons, causing inflammation and pain. The most commonly affected site is the supraspinatus tendon of the shoulder [4], with rare cases involving the tendons of the gluteus medius and gluteus maximus reported in medical literature [[3], [4], [5], [6], [7], [8]]. The condition can present as acute or chronic hip pain and predominantly occurs in people over the age of 40 and is rare in those older than the age of 70 [3,9]. Although the exact etiology is unknown, suspected causes involve repetitive microtrauma, periarticular soft tissue degeneration, hypoxia-induced metaplasia with resultant calcification [3], and metabolic and autoimmune disorders [5]. In our case, the patient presented with localized posterolateral hip pain, which is similar to previously reported cases [3,10,11]. The absence of preceding trauma and lack of constitutional symptoms helped differentiate it from other conditions like myositis ossificans, infection, and malignancy. Reproducible pain with hip extension, tenderness to palpation near the site of gluteus maximus insertion, and negative special testing for lumbosacral radiculopathy targeted the subsequent imaging to the left hip. Plain radiographs of the affected hip were sufficient to demonstrate the presence of calcified deposit near the gluteus maximus insertion site. MRI is not necessary to diagnose calcific tendonitis but is helpful in detecting early tendon and bone marrow changes [3]. In our case, MRI of the left hip localized the inflammation to the gluteus maximus and ruled out other pathologies such as labral tears, infection, and malignancy. Conservative management options include NSAIDs and physical therapy, ultrasound-guided corticosteroid injection, needle lavage, and minimally invasive percutaneous needle tenotomy [1,7,9,12]. With diffuse calcific deposits, partial surgical excision and debridement is recommended if conservative measures fail.
Calcific tendinitis is diagnosed through patient history, physical examination, and imaging examination. Conservative management with NSAIDs and physical therapy is recommended, while minimally invasive percutaneous needle tenotomy or surgical excision and debridement are typically reserved for refractory cases with prolonged symptomatology and functional decline. This case report contributes to the growing medical literature for the rare presentation of calcific tendinitis of gluteus maximus insertion.
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Patient consent
Written informed consent was obtained from the patient for publication of their case.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Koen SM, Pecha F, Nilsson K. Ultrasound-guided needle lavage for calcific tendonitis of the gluteus medius tendon. Athletic Train Sports Health Care. 2017;9(5):238–240. [Google Scholar]
- 2.Hung CY, Chang KV. Ultrasound-guided percutaneous needle tenotomy with platelet-rich plasma injection for an uncommon case of proximal gluteus medius tendinopathy. J Med Ultrasound. 2019;27(2):111–112. doi: 10.4103/JMU.JMU_86_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar M, D′Silva DF, Shah M, Parekh G. Calcific tendonitis of the gluteus maximus tendon: A case report and review of the literature. J Mahatma Gandhi Institute Med Sci. 2016;21(1):65–68. doi: 10.4103/0971-9903.178111. [DOI] [Google Scholar]
- 4.Ellatif M, Razi F, Hogarth M, et al. Bilateral gluteus medius and minimus calcific tendonitis in a patient with previous bilateral calcific tendonitis of the shoulder: a case report. Radiol Case Rep. 2021;16(11):3222–3225. doi: 10.1016/j.radcr.2021.07.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kandemir U, Bharam S, Philippon MJ, Fu FH. Endoscopic treatment of calcific tendinitis of gluteus medius and minimus. Arthroscopy. 2003;19(1):E4. doi: 10.1053/jars.2003.50021. [DOI] [PubMed] [Google Scholar]
- 6.Park SM, Baek JH, Ko YB, et al. Management of acute calcific tendinitis around the hip joint. Am J Sports Med. 2014;42(11):2659–2665. doi: 10.1177/0363546514545857. [DOI] [PubMed] [Google Scholar]
- 7.Flemming DJ, Murphey MD, Shekitka KM, et al. Osseous involvement in calcific tendinitis: a retrospective review of 50 cases. AJR Am J Roentgenol. 2003;181:965–972. doi: 10.2214/ajr.181.4.1810965. [DOI] [PubMed] [Google Scholar]
- 8.Damme KV, Coster LD, Mermuys K, Van A, Walgraeve N, Geeter FD. Bone scan findings in calcific tendinitis at the gluteus maximus insertion: some illustrative cases. Radiol Case Reps. 2017;12(1):168–174. doi: 10.1016/j.radcr.2016.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim MS, Kim IW, Lee S, Shin SJ. Diagnosis and treatment of calcific tendinitis of the shoulder. Clin Shoulder Elb. 2020;23(4):210–216. doi: 10.5397/cise.2020.00318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Su CA, Ina JG, Raji Y, Strony J, Philippon M, Salata MJ. Endoscopic treatment of calcific tendinitis of the gluteus maximus: a case report. JBJS Case Connector. 2021;11(2):e20.00974–e20.00976. doi: 10.2106/JBJS.CC.20.00974. [DOI] [PubMed] [Google Scholar]
- 11.Huang K, Murphy D, Dehghan N. Calcific tendinitis of the gluteus maximus of a 53-year-old woman. CMAJ. 2017;189(50):E1561. doi: 10.1503/cmaj.171308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wen Qiang L, Gen Lin F, Chia ZY. A 57-year-old woman with calcific tendinitis of the gluteus medius presenting with right lateral hip pain managed by endoscopic debridement. Am J Case Rep. 2023;24 doi: 10.12659/AJCR.938661. [DOI] [PMC free article] [PubMed] [Google Scholar]