Abstract
Objective:
Traumatic brain injuries (TBIs) are increasingly common and a major cause of death and long-term disability. Many individuals experience chronic stressors and adverse health outcomes, emphasizing the importance of cultivating resilience, (defined herein as individual, social, and systemic components engaged in response to the stressors that allow individuals to “bounce back,” or move forward adaptively after TBI). Patients’ perceptions of factors influencing resilience are critical to guide interventions that meet their needs. Here we offer the first meta-synthesis of factors influencing resilience after TBI using a Social Ecological model framework.
Research Methods/Design:
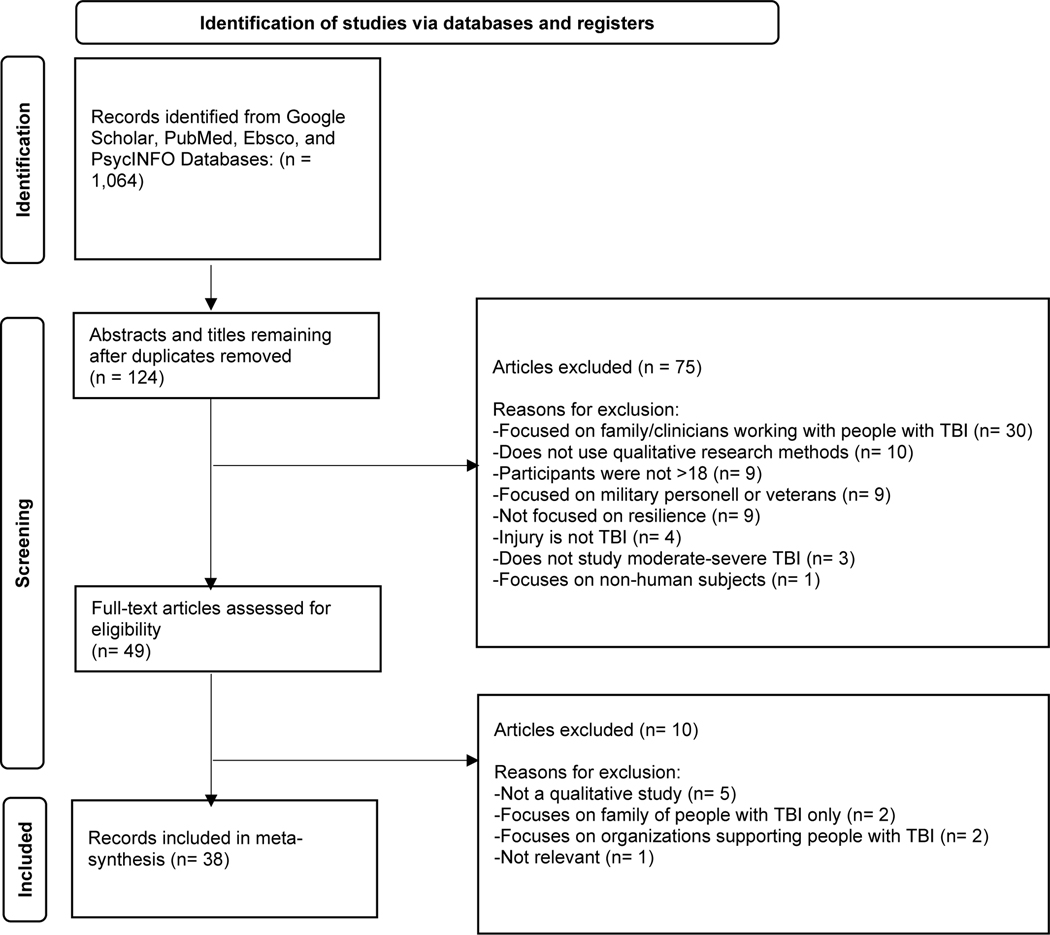
We preregistered our meta-synthesis on PROSPERO (CRD42021233975) and followed PRISMA guidelines. We searched four electronic databases for qualitative studies from inception up until June 2021. We included qualitative studies detailing perspectives of individuals with a history of moderate-severe TBI. We excluded case studies and systematic reviews. After removal of duplicates, we identified 124 articles for screening. We reviewed 49 articles for full text eligibility, and included 38 studies. We extracted study characteristics and data (e.g., author interpretations and relevant quotes) relating to factors influencing resilience.
Results:
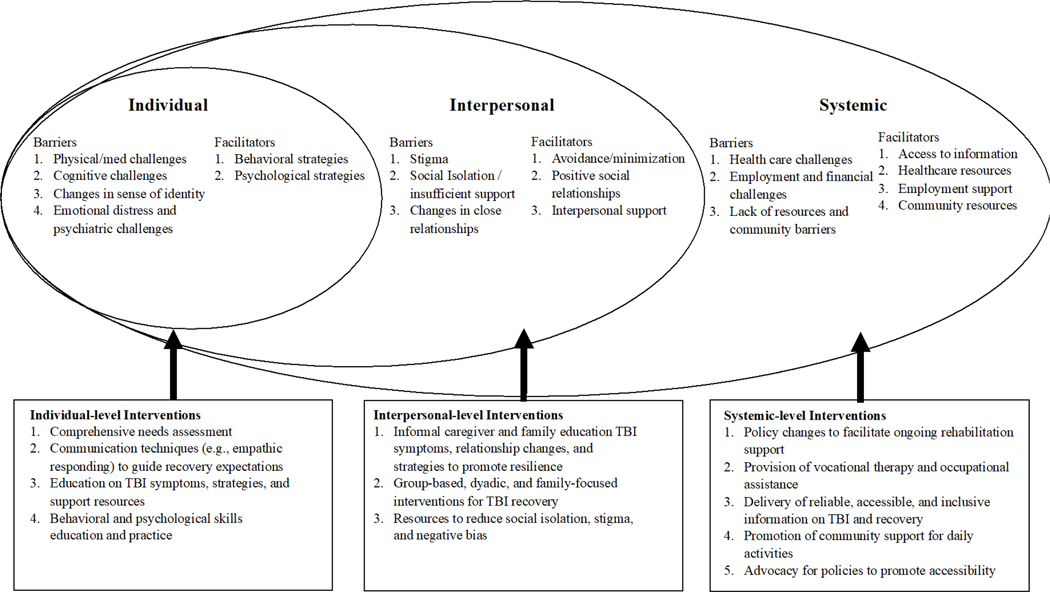
We synthesized findings using a Social Ecological Model framework to guide thematic analysis. Persons with TBI identified barriers and facilitators to resilience at individual (e.g., physical and cognitive challenges, coping behaviors), interpersonal, (e.g., stigma and isolation) and systemic (e.g., access to resources, rehabilitation support) levels.
Conclusions/Implications:
Considering multifaceted factors at individual, interpersonal and systemic levels in clinical, research, and policy-setting contexts is important for cultivating resilience and optimizing recovery after TBI.
Introduction
Traumatic brain injury (TBI) is a public health concern that impacts 12% of adults worldwide (Frost, Farrer, Primosch, & Hedges, 2013) and is a major cause of death, disability, and a host of negative physical and mental health outcomes (Faul, Wald, Xu, & Coronado, 2010; Frost et al., 2013; Nelson et al., 2019). TBI is largely considered a chronic illness rather than a single event due to the substantial secondary medical concerns stemming from injury that often require lifelong observation, management, and medical care (Masel & DeWitt, 2010). These concerns include persistent declines in functioning and an increased likelihood for re-injury, TBI-related health complications (e.g., stroke), and chronic illnesses (e.g., chronic pain, neurodegenerative diseases) (Bannon et al., 2021; Stocchetti & Zanier, 2016; Zaloshnja, Miller, Langlois, & Selassie, 2008) emphasizing the importance of cultivating protective factors to improve recovery after TBI.
TBI researchers have recently focused on understanding resilience following TBI to promote positive outcomes. Recently, TBI researchers have defined resilience as a multifaceted construct encompassing individual, social, and systemic (i.e., environmental or external) components engaged in response to the stressors experienced after injury that allow individuals to “bounce back,” or move forward adaptively (Boulton, Horne, & Todd, 2018; Holt-Lunstad, 2018; Partelow, 2018). This definition is consistent with a recent movement to use a Social Ecological Model to understand how TBI and other health conditions impact individuals differently based on differences in their broader environment (Boulton et al., 2018; Fleury & Lee, 2006; Meints, Cortes, Morais, & Edwards, 2019; Partelow, 2018; Saadi, Bannon, Watson, & Vranceanu, 2021). Social Ecological Models characterize the ways in which individual, interpersonal, and systemic factors dynamically influence physical and mental health over time (Partelow, 2018). Such approaches can be useful for explaining the myriad factors that serve as barriers (i.e., inhibiting factors) and facilitators (i.e., enhancing factors) to resilience after TBI (Atallah, Bacigalupe, & Repetto, 2021; Brodsky & Cattaneo, 2013; Levack, Kayes, & Fadyl, 2010; Nalder, Hartman, Hunt, & King, 2019; Villa, Causer, & Riley, 2020). Indeed, there is some quantitative evidence that resilience after TBI is impacted by individual (e.g., healthy lifestyle behaviors, personal outlook), interpersonal (e.g., family functioning, social support), and systemic (e.g., available rehabilitation resources, financial stability) factors (Braaf et al., 2020; Holland & Schmidt, 2015; Lefkovits, Hicks, Downing, & Ponsford, 2020; Levack et al., 2010). However, there has been no systematic investigation or comprehensive synthesis of micro- and macro-level factors impacting resilience after TBI. Gaining insight into the perceptions of individuals with TBI and their impressions on factors linked to their resilience is key for guiding feasible and efficatious interventions for this population. (Fleury & Lee, 2006; Kanavaki et al., 2017)
Qualitative methods are increasingly used by TBI researchers (Dijkers, 2004), and are particularly useful for characterizing understudied or overlooked populations’ perspectives, such as those with TBI (George & Apter, 2004). Meta-syntheses (i.e., qualitative systematic reviews) are useful for identifying themes across studies and informing the design of intervention approaches and policies “from the ground up” (Jesus & Silva, 2016; McCulloch et al., 2016). Though prior meta-syntheses have comprehensively characterized individuals’ perceptions of factors influencing their own recovery and outcomes following TBI, existing work has largely adopted a disability-focused lens to characterize barriers to recovery (Levack, Kayes, & Fadyl, 2010). Synthesizing the perspectives of individuals with TBI using a Social Ecological Model lens can contribute to more equitable model of resilience in that findings illustrate how the larger infrastructure can promote or inhibit individuals’ resilience (Doorn, Gardoni, & Murphy, 2019). In the present study, we sought to comprehensively review and synthesize available literature and identify factors that facilitate or inhibit resilience after TBI using a Social Ecological Model framework (Fleury & Lee, 2006; Partelow, 2018). Our broader goal was to generate recommendations for researchers, clinicians, and policymakers as a first step towards implementing interventions, resources, and policies that optimize recovery.
Methods
Tranparency and openness
We pre-registered our meta-synthesis on PROSPERO (CRD42021233975) and was consistent with both PRISMA and JARS guidelines for meta-syntheses (Moher, Liberati, Tetzlaff, Altman, & Group, 2009). All data, analysis codes and taxonomies, and other research materials are available by reasonable request through email to the corresponding author. The study’s aims and analysis plan were registered on PROSPERO.
Study Selection Criteria and Search Strategy
We performed key word searches in five electronic data bases (Google Scholar, PubMed, PsycINFO, and EBSCOhost) from inception until June 2021. Our search comprised three sets of terms consistent with our overarching aims, including TBI, qualitative research, and resilience (Supplemental Table 1). Table 1 describes eligibility criteria. We selected studies that met the following criteria: (1) included civilian adults with history of at least 1 moderate to severe TBI; (2) included information on psychosocial stressors, coping strategies, and/or resources related to adjustment after TBI; (3) used any type of qualitative method; (4) were not a systematic review; (5) were written in English. Two reviewers (NSF, KW) separately screened article titles and abstracts to select those that fit the inclusion and exclusion criteria. We chose to focus on civilian populations given the documented differences in factors impacting clinical characteristics and outcomes between civlilian and military contexts (Loignon, Ouellet, & Belleville, 2020; Trudel, Nidiffer, & Barth, 2007). The reviewers met weekly to discuss and identify articles for inclusion. The reviewers performed full text screening for potentially eligible articles, and disagreements were resolved through discussion with the research team.
Table 1:
Inclusion and Exclusion Criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| 1. Article is written in English | 1. Article does not include primary data collection (e.g., literature review, opinion or perspective article) |
| 2. Published in a peer-reviewed academic journal | 2. Used only quantitative methodology for data collection and analysis |
| 3. Concerns original research and primary data collection | 3. Concerns perspectives of informal caregivers (e.g., spouses, family, friends) or healthcare providers (e.g., physicians, nurses, rehabilitation therapists) |
| 4. Used any type of qualitative methods for data collection or analysis of data (including mixed methods) | 4. Not relevant to the recovery experiences of persons with TBI in the period after injury |
| 5. Concerns perspectives of adult (ages 18 and older) persons with TBI | 5. Characterizes military populations of individuals with TBI |
| 6. Relevant to the recovery experiences of persons with TBI in the period after injury | |
| 7. Characterizes civilian populations of individuals with TBI |
Study Quality Appraisal
We used the 9-item quality appraisal tool developed by Hawker and colleagues to assess the methodological and reporting quality of all included studies (Hawker, Payne, Kerr, Hardey, & Powell, 2002). The criteria used to evaluate articles was based on the extent that: (a) the abstract and title provided a clear description of the study, (b) the introduction included a good background and clear statement of the aims of the research, (c) the methods were appropriate and clearly explained, (d) the sampling strategy was appropriate to address the aims, (e) the authors included a rigorous description of the data analytic strategy, (f) the authors described the ways that ethical issues and researcher bias were addressed, (g) there was a clear description of findings, (h) the findings were transferabe to a wider audience, and (i) the findings were useful for policy and/or practice. These criteria were evaluated on a four-point scale of very poor (1 point), poor (2 points), fair (3 points), and good (4 points). The results were summed to compile overall quality scores for each article (range= 9–36). Two independent reviewers assessed each article and met to discuss findings and resolve disagreements. Overall, included studies were of good quality (Table 2; M=34.55 out of a possible 36; range 31–36). Articles received the lowest ratings on criterion (f) due to insufficient descriptions ethical considerations and researcher bias, with 16% of articles (n=6) receiving a rating of “poor” or “very poor.” In addition, articles received lower scores on criterion (h) describing transferability of findings, with 8% (n=3) of articles receiving a “poor” rating due to their lack of discussions of their findings in connection to the broader TBI literature.
Table 2:
Results of the quality assessment for included qualitative studies (N=38)
| Criteria | Good | Fair | Poor | Very Poor |
|---|---|---|---|---|
| (4) | (3) | (2) | (1) | |
|
| ||||
| 1. Abstract/ title | 34 | 4 | 0 | 0 |
| 2. Introduction/ aims | 36 | 2 | 0 | 0 |
| 3. Data collection | 38 | 0 | 0 | 0 |
| 4. Sampling | 30 | 8 | 0 | 0 |
| 5. Analysis | 38 | 0 | 0 | 0 |
| 6. Ethics/ bias | 28 | 4 | 2 | 4 |
| 7. Results | 38 | 0 | 0 | 0 |
| 8. Transferability | 29 | 7 | 3 | 0 |
| 9. Implications | 35 | 0 | 3 | 0 |
Note: Hawker et al (2002) quality assessment tool
Data Extraction
Two members of the team independently reviewed each full-text article and extracted findings. We then inserted extracted findings into a standardized form that included following information: author(s), publication year, study location, sample size, study population, participant characteristics (i.e., age, gender, etc.), time since TBI, research question, data collection method, data analysis method, psychosocial stressors and challenges faced after TBI. The two reviewers for each article resolved discrepancies through discussions and consolidated findings.
Data Synthesis
We chose to adopt meta-synthesis framework to data analysis to integrate findings across studies and produce novel interpretations of the data (Walsh & Downe, 2005). As facilitated by the standardization of our data extraction process, we performed a taxonomic analysis on our a-priori determined themes of interest: barriers and facilitators of resilience (i.e., recovery and positive adaptation to the stressors experienced following TBI). We extracted findings into 2 taxonomies—one for barriers of resilience and another for facilitators of resilience, consistent with empirical models of resilience following TBI (Hanks, Rapport, Waldron Perrine, & Millis, 2016; Holland & Schmidt, 2015). We utilized a Social Ecological Model (Fleury & Lee, 2006; Partelow, 2018) framework to organize findings within each taxonomy into individual, interpersonal, and systemic levels. Two reviewers iteratively analyzed the taxonomies to minimize redundancy and promote clear and succinct wording. Additional details on the process of refining findings taxonomies is presented in Supplemental Table 2.
Results
Study Characteristics
See Figure 1 for a PRISMA flow chart depicting our article search and selection process. After full-text screening, we identified 38 articles that were eligible for inclusion in our meta-synthesis. Supplemental Table 3 displays the study and participant characteristics of included articles. Included studies were primarily conducted in Australia (n=9), the United States (n=8), New Zealand (n=3), and South Africa (n=3), and had sample sizes that ranged from N=2–150. Studies predominantly utilized semistructured interviews (n=34) or focus groups (n=4). To analyze qualitative data, studies primarily utilized thematic analysis (n=29) or grounded theory (n=8). Most studies reported on the time elapsed since TBI using approximate ranges (in years). Most studies did not report on the type of injury (e.g., motor vehicle accident) linked to the index TBI. A small (n=4) number of studies examined findings with longitudinal designs.
Figure 1:
PRISMA flow diagram
Synthesized Findings
We used a Social Ecological Model framework (Partelow, 2018) to identify factors serving as barriers and facilitators of resilience. Specifically, we identified findings within 3 levels: (1) individual, (2) interpersonal, and (3) systemic. Supplemental Tables 3–5 present findings at the individual, interpersonal, and systemic levels.
Level 1: Individual Factors
Our review identified 4 subthemes pertaining to the individual-level barriers to resilience reported by individuals following TBI: (a) physical or medical challenges, (b) cognitive challenges, (c) changes in identity, and (d) emotional distress and psychiatric challenges. In the weeks, months, and years following injury, individuals across studies described experiencing common symptoms (e.g., new-onset pain, headaches, fatigue, sleep disturbance) (Mumbower et al., 2019; Nalder, Fleming, Cornwell, Shields, & Foster, 2013; Simpson, Mohr, & Redman, 2000) and changes in their abilities and functioning (e.g., sensory abilities, attentional capacity, executive functioning) (Dixon, Thornton, & Young, 2007; Dubuc et al., 2019; Graff, Christensen, Poulsen, & Egerod, 2018; Herrmann & Deatrick, 2019; Mbakile-Mahlanza, Manderson, & Ponsford, 2015; Nalder et al., 2013) that made it difficult to maintain their participation in daily activities, work, and interpersonal relationships. These challenges often resulted in changes in persons’ identity, and participants across studies described a loss of their former self and a negative perception of their current abilities and identity (Anne Jones & Curtin, 2011; Godwin, Chappell, & Kreutzer, 2014; Keegan, Togher, Murdock, & Hendry, 2017; Levack et al., 2010; Liddle et al., 2012; Mealings, Douglas, & Olver, 2019; Muenchberger, Kendall, & Neal, 2008; Mumbower et al., 2019). Individuals also described finding it difficult to live a “normal life” in the midst of these challenges and experiencing multiple perceived losses. As a consequence, complex and overwhelming emotions (e.g., anger, frustration, fear, grief, shame) were common in the months and years following injury (Muenchberger et al., 2008; Soeker et al., 2012). Individuals with TBI also described coping with these emotions in ways that inhibited their recovery, including with drugs/ alcohol that resulted in new-onset addiction, and a reduced ability to adhere to medical regimens (Self, Driver, Stevens, & Warren, 2013; Stenberg, Stålnacke, & Saveman, 2020) .
Our review also identified 2 subthemes surrounding individual-level facilitators of resilience reported by individuals with TBI, (a) behavioral strategies, and (b) psychological strategies. They described behavioral strategies such as seeking TBI-related information on common symptoms, prognosis, and strategies to promote positive recovery, as well as working to develop new strategies (e.g., breaking down tasks into steps, allowing more time to complete tasks, keeping a memory notebook, and reducing stimuli) to minimize the impact of TBI symptoms (Mumbower et al., 2019; Nalder et al., 2013; Nochi, 2000; Soeker & Pape, 2019). Individuals with TBI also utilized psychological coping strategies that helped them manage emotional distress and promote balanced thinking. These strategies included adopting a present moment focus and cultivating mindful awareness of daily activities (Douglas, 2013; Kruithof et al., 2018), as well as a number of strategies to promote positive mood (e.g., cultivating gratitude and optimism) (Mumbower et al., 2019; Nalder et al., 2013) and a positive framing of their current challenges and identity (e.g., focusing on values, cultivating acceptance, adopting a growth mindset) (McPherson et al., 2018; Salas et al., 2018). For example, participants described viewing the TBI as a “new beginning” linked to a renewed desire to pursue goals as well as a chance to modify their health behaviors (e.g., sleep, exercise, substance use) to optimize recovery.
Level 2: Interpersonal Factors
We identified interpersonal barriers to recovery, which we organized into 3 subthemes: (a) stigma, (b) social isolation and insufficient support, and (c) changes in close relationships. Perceptions of being treated differently were commonly reported by individuals with TBI, particularly being underestimated or ignored by family, friends, and coworkers (Soeker & Pape, 2019). Individuals with TBI also described a fear of burdening others, which led to their withdrawal from social activities and increased loneliness and social isolation (Mumbower et al., 2019). Over time, they noticed that people in their lives were less invested in their relationship (McPherson et al., 2018) and had negative reactions to the symptoms they experienced after TBI (e.g., irritability, memory deficits, physical impairments) (McPherson et al., 2018; Stenberg et al., 2020). In addition to challenges with established relationships, individuals with TBI described having difficulties forming new friendships (Salas et al., 2018) They attributed this challenge to their TBI symptoms and a lack of access to social activities and peer groups with similar experiences (Herrmann & Deatrick, 2019). Finally, they described challenges surrounding changes in their identity regarding relationships with others (e.g., changes in social or familial roles and familiar relationship dynamics, difficulty communicating with others) that lead to a loss of intimacy and increased relationship strain with spouses, family members, and friends (Adams & Dahdah, 2016; Dubuc et al., 2019; Stenberg et al., 2020) .
We also identified interpersonal-level facilitators to resilience, organized into 3 subthemes: (a) preserving identity by minimizing challenges, (b) positive social relationships, and (c) interpersonal support to promote TBI recovery. Participants in several studies described engaging in social strategies surrounding their reluctance to discuss or focus on TBI-related challenges in order to reduce potential stigma or changes in their relationships with others (Jumisko, Lexell, & Söderberg, 2009; McPherson et al., 2018). This strategy preserved normalcy and helped individuals reduce potential stigmatizing reactions from others, but was difficult to maintain long-term. Participants also provided several examples of the ways in which social relationships facilitated their recovery. Specifically, they reported that maintaining close connections despite changes in functioning was critical to mitigate social isolation and negative self-identity after injury (Anne Jones & Curtin, 2011; Jumisko et al., 2009; Salas, Casassus, Rowlands, Pimm, & Flanagan, 2018) . In addition, preserved relationships provided a context for individuals with TBI to practice acceptance of changes in roles and functioning and engage in positive re-appraisal of their challenges (Anne Jones & Curtin, 2011; Fadyl et al., 2017). Finally, they described ways in which caregiving and social support were of critical importance to promote resilience (Lefebvre & Levert, 2012).They noted the benefits of support with a variety of individuals: informal caregivers, friends, healthcare providers, and TBI survivors with similar experiences. Participants in support groups and online forums also expressed the value of forming new friendships and relationshps with others with TBI to minimize stigma and social isolation and to normalize their experiences after injury (Hux et al., 2010; Jumisko et al., 2009; Lefebvre et al., 2008; Levack et al., 2010).
Level 3: Systemic Factors
We identified barriers at the systemic level that we organized into 3 subthemes: (a) healthcare system and formal caregiving support, (b) employment and financial challenges, and (c) lack of community resources. Regarding their healthcare and formal caregiving support, persons with TBI identified a variety of barriers to resilience. Many described the negative impact of others’ perceptions of their ability to independently complete tasks (e.g., walking, completing household tasks) and the optimal level of support for such tasks to cultivate resilience (Dixon, Thornton, & Young, 2007; Dubuc et al., 2019; Self et al., 2013). They also described challenges finding and accessing reliable information on the strategies and support resources that would enhance their resilience, help them prepare for the future, and navigate life transitions (Adams & Dahdah, 2016; Chouliara & Lincoln, 2016; Herrmann & Deatrick, 2019). While psychosocial support was cited as critical to promote resilience, those that had access to psychosocial resources were dissatisfied with existing services and cited unmet needs to address their specific challenges (e.g., identity issues for younger participants; return to school) (Graff, Christensen, Poulsen, & Egerod, 2018; Mbakile-Mahlanza, Manderson, & Ponsford, 2015; Stenberg et al., 2020). Participants across studies experienced limits of ongoing rehabilitation support. Specifically, many reported that they were no longer deemed eligible for certain healthcare resources beyond 1-year post-injury (e.g., rehabilitation therapies) despite having persistent needs, and reported dissatisfaction with the timing of psychosocial and rehabilitative interventions (e.g., delivered too early or too late) (Dubuc et al., 2019; Lefebvre et al., 2008). Several studies acknowledged cultural variations impacting TBI recovery and rehabilitation services acknowledged the lack of tailoring of services for those from different cultural backgrounds (e.g., different understandings of the rehabilitation process and recovery expectations, lack of services in individuals’ native language) (Simpson et al., 2000; Soeker, Van Rensburg, & Travill, 2012).
Persons with TBI also experienced a host of employment and financial challenges that served as barriers to resilience, including loss of employment, limited financial resources, and challenges finding suitable employment due to TBI-related challenges (Douglas, 2013; Nalder et al., 2013; Oppermann, 2004; Self et al., 2013). For those who remained employed, they experienced challenges completing work tasks due to persistent TBI symptoms (e.g., attention deficits, headaches, fatigue, inability to drive), with inadequate accomodations to work successfully in the midst of their TBI symptoms (Herrmann & Deatrick, 2019; Soeker & Pape, 2019). Finally, individuals with TBI described barriers surrounding community resources, including challenges with transportation due to changes in their ability to drive as well as geographic barriers to accessing rehabilitation services (Liddle et al., 2012; Self et al., 2013; Soeker & Pape, 2019). The financial impact of TBI also led many to experience financial instability, impacting their ability to afford food and pay for medical services (Lefebvre, Cloutier, & Josée Levert, 2008).
In addition, we identified systemic facilitators of resilience organized into 4 subthemes: (a) availability of TBI-related information, (b) healthcare resources, (c) employment and financial resources, and (d) community resources. Individuals with TBI benefitted from the availability of reliable information on the consequences of TBI, ways of accessing support resources, and education on strategies to minimize TBI-related changes in functioning (Anne Jones & Curtin, 2011; Fadyl, Theadom, Channon, & McPherson, 2017; McPherson et al., 2018). Consistent with the common impression that TBI could provide a “fresh start,” many also valued educational resources on healthy lifestyle behaviors (e.g., diet, exercise, stress management) (Douglas, Driver, Callender, & Woolsey, 2019). In addition, the availability of continued support from heathcare providers and healthcare settings were viewed as a crucial resource to promote resilience (Fadyl et al., 2017; Hux et al., 2010). Specifically, persons with TBI benefitted from ongoing rehabilitation support and providers’ willingness to educate informal caregivers on appropriate ways of helping promote recovery after their injury (Fadyl et al., 2017; Mumbower et al., 2019). In recognition of the many financial and employment-related barriers that individuals with TBI experienced, they noted the benefits of programs that aided individuals’ resuming employment, either through specialized training (e.g., co-worker models, therapist shadowing) or vocational training to find positions suitable for their current skill level (Muenchberger et al., 2008; Oppermann, 2004; Soeker et al., 2012; Stenberg et al., 2020). Participants across studies also underscored the benefits of volunteering to add structure to their day, promote positive self-esteem and gratitude, and allow them to maintain a sense of purpose (Anne Jones & Curtin, 2011; Jumisko et al., 2009). Finally, aspects of individuals’ community and environment also promoted resilience, including living in an environment that was accessible given their current abilities (e.g., the availability of sidewalks, public transportation, and ride services) (Jumisko et al., 2009) and having access to information, programs, and activities that promoted their engagement in healthy lifestyle behaviors, routines, and social connections (Godwin et al., 2014; Mumbower et al., 2019; Soeker & Pape, 2019; Soeker, 2016). Examples described by participants included meal preparation programs that accounted for their current abilities, brain injury support groups, and ongoing wellness activities (e.g., yoga, meditation, walking) (Soeker & Pape, 2019).
Discussion
We conducted the first meta-synthesis (N=38 qualitative studies) comprehensively characterizing barriers and facilitators to resilience for persons with TBI. We utilized a Social Ecological Framework (Partelow, 2018) to guide the extraction and multifaceted synthesis of findings across studies. Results illustrated numerous barriers and facilitators to resilience experienced by persons with TBI at individual, interpersonal, and systemic levels. Below, we describe findings at each level and recommendations for providers, advocates, and healthcare systems (see Figure 2 for a summary).
Figure 2:
Social Ecological Model of Factors Impacting Resilience after TBI
At the individual level, individuals described barriers to resilience related to their TBI symptoms (physical, cognitive, emotional) and the impact of such symptoms on their identity. They further described behavioral and psychological coping strategies that mitigated the impact of TBI symptoms and promoted resilience in connection to their life roles and responsibilities. These findings are consistent with prior quantitative and qualitative systematic reviews (Dijkers, 2004; Holland & Schmidt, 2015; Levack et al., 2010; Villa et al., 2020), and suggest that TBI survivors would benefit from interventions that offer education on TBI symptoms and expected challenges, as well as resources and skills to target cognitive, emotional, and identity-related challenges. Consistent with Social Ecological Models describing TBI and other chronic health concerns (e.g., chronic pain; (Bannon, Greenberg, Goldson, O’Leary, & Vranceanu, 2020; Meints et al., 2019; Nalder et al., 2019)); clinicians should use therapeutic communication techniques (e.g., empathic responding) to guide expectations surrounding patients’ engagement in medical treatment and promote shared decision making. Providers should use their needs assessment to inform their treatment approach, and consider offering corresponding referrals to appropriate resources to enhance individual resilience through education and skills practice surrounding positive coping strategies (Godwin & Kreutzer, 2013). Evidence-based psychosocial interventions (e.g., mindfulness and acceptance-based approaches, Cognitive behavioral Therapy, Dialectical Behavior Therapy, Cognitive Remediation training) have growing support in addressing such challenges among individuals with TBI (Doering & Exner, 2011; Fann et al., 2015; Vranceanu et al., 2020). These interventions can be delivered alongside ongoing rehabilitation services, and have the potential to be delivered via telehealth approaches (e.g., phone-based, live video) early after injury and in the months and years after hospital discharge (Fann et al., 2015; Vranceanu et al., 2020).
At the interpersonal level, individuals described barriers related to stigma they experienced from family, friends, and other close relationships surrounding their TBI symptoms, since their injury was not visually apparent. They attempted to cope by minimizing or denying the extent of their symptoms, which had some impact on their resilience in preserving relationships but was difficult to maintain in the presence of severe symptoms. Over time, social isolation and declines in support were common. Participants further described the importance of preserved relationships and interpersonal support as facilitators of recovery. This is consistent with the extant quantitative literature on TBI recovery (Bannon et al., 2020), conceptual models of resilience after TBI, as well as the broader literature surrounding close relationships and health (Umberson & Karas Montez, 2010). Thus, interventions that promote positive interpersonal interactions and leverage caregiver support may foster resilience among individuals with TBI. These include the “dyadic” (i.e., treating patient and informal caregiver as a unit) resiliency interventions (Vranceanu et al., 2020) for acute TBI, group psychosocial interventions for TBI survivors (Neumann et al., 2017), and movement based interventions that include individuals with TBI and their informal caregivers (e.g., LoveYourBrain yoga) (Donnelly et al., 2021).
Healthcare systems should consider the robust impact of stigma and social isolation on TBI survivors’ coping strategies and resilience after injury and work to enact policies and programs that mitigate their impact. Specifically, they can enact anti-stigma initiatives for TBI that include narratives of TBI survivors experiences, “myth busting” information, and a discussion of the impact of stigma on prejudiced labeling and behaviors (Szeto & Dobson, 2010; Tsatsou, 2021; Werner & Scior, 2016). Sytems should consider implementing peer support or mentoring programs to reduce both isolation and stigma (Lau et al., 2021), as well as increase the presence of in-person and remote support groups, group-based interventions, and group-based community reintegration activities (e.g., walking group) (Chouliara & Lincoln, 2016; Neumann et al., 2017).
At the systemic level, we identified numerous barriers to resilience in healthcare, employment, and community contexts. Individuals with TBI described challenges accessing ongoing rehabilitation support, obtaining support to navigate financial and employment challenges, and barriers to navigating their local environment and community. Many also noted the poor fit of rehabilitation services due to the timing of delivery, lack of continued support, and poor fit of services for their cultural background. Indeed, reviews of the quantitative literature highlight the disparities that exist in outcomes across the continuum of TBI recovery based on race/ethnicity, SES, and other social determinants of health (Marcus, Burlie, Colantonio, Mann, & Chan, 2019; Saadi et al., 2021). At the systemic level, recommendations include both policylevel and clinical practice-level changes.
Policy-level changes include the expansion of the availability ongoing rehabilitation support and inclusions of vocational or occupational assistance as a part of routine rehabilitation care. In addition, health care systems should work to ensure that TBI survivors have access to reliable, accessible, and inclusive information on TBI symptoms, ways of engaging in professional and social supports, and behaviors to optimize recovery. Some states in the U.S. have made efforts to improve TBI-specific education and systemic support through a TBI Team Model consultation service to support students and families (Glang, Tyler, Pearson, Todis, & Morvant, 2004) as well as through the establishment of statewide clinical guidelines on the management of TBI for providers (Spaite et al., 2019). In addition, national organizations have enacted multilevel (e.g., local, state, national) initiatives to prevent secondary consequences of TBI (Sarmiento, Langlois, & Mitchko, 2008). Healthcare systems can also make education and training available to providers on sources of disparities in care and the negative impact of unconscious bias, with the goal of mitigating disparities in care (Saadi et al., 2021).
Our review also highlighted the role of aspects of community environments (e.g., access to sidewalks and public transportation) in connection to resilience following TBI, which is consistent with the broadeer recognition of the impact of land-use and transportation decisions on community health (Dannenberg et al., 2003). Communities can work to design more user-friendly transportation systems that best facilitate travel for work, shopping, social activities, and leisure of all persons—and include specific accomodations for persons with disabilities (Dannenberg et al., 2003).
In light of the systemic barriers to resilience such as lack of accessibility to services due to geographic, transportation, and financial barriers, healthcare systems should find ways of using telehealth technology to increase access to resources designed to increase individual resilience, including live-video interventions and web-based platforms.(Evans, 2019) Such approaches have been used to promote the delivery of individual, dyadic, and group based psychosocial interventions for TBI (Evans, 2019; Parrott & Ibarra, 2021; Vranceanu et al., 2020), and are supported by research demonstrating that patients have similar preferences to telehealth services relative to in-person care, with fewer barriers. Taken together, our findings highlight the importance of advocacy at multiple levels to promote adequate needs assessment, education, and resource provision.
Limitations and Future Directions
This meta-synthesis was limited to the available qualitative literature, and findings may not apply to diverse groups of individuals with experiences of TBI. Our review reflects themes identified from the available study samples, which were predominantly white, English-speaking, and recruited from prominent TBI clinical research and rehabilitation settings in Australia and the United States. Therefore, our findings may be less transferrable to individuals with TBI with racialized identities or cultural backgrounds not captured in the included studies, non-English speaking individuals, and individuals from other geographic regions in the world. Individuals with TBI who did not receive ongoing rehabilitation care were also seldom characterized by studies, and may report experiencing different barriers and facilitators to resilience. In addition, our quality appraisal of included studies revealed a pattern of researchers failing to include information surrounding ethical considerations and potential bias in their interpretation of results. Future qualitative studies of resilience following TBI should follow reporting guidelines to sufficiently examine and mitigate ethical concerns and thoroughly describe researcher reflexivity. (Johnson, Adkins, & Chauvin, 2020).
Most studies recruited individuals with varying time since their TBI, and few studies employed a longitudinal approach. It is therefore difficult to determine whether barriers and facilitators of resilience change over time in general, and in relation to each other across the levels characterized in our review. Researchers should work to incorporate social determinants of health into their exploration of TBI outcomes, and adopt approaches in quantitative studies (e.g., longitudinal growth curve modeling)(Hart et al., 2014; Kozlowski, Pretz, Dams-O’Connor, Kreider, & Whiteneck, 2013; Malec et al., 2019) that allow for a more nuanced and dynamic understanding of resilience after TBI (Marcus et al., 2019). Further, researchers studying TBI should consider ways of adopting a Social Ecological Model framework (Partelow, 2018) to their studies at the design, analysis, and interpretation phases to promote a more comprehensive understanding of the interplay between factors that influence resilience following injury.
Conclusions
This is the first meta-synthesis to comprehensively characterize factors influencing resilience among persons with TBI. A variety of factors contribute to and hinder resilience in this population, at individual, interpersonal, and systemic levels. Considering these multifaceted factors in clinical, research, and policy-setting contexts may help cultivate resilience and optimize recovery after TBI.
Supplementary Material
Impact.
Understanding factors contributing to resilience after Traumatic Brain Injury (TBI) can help improve outcomes and inform interventions for this population.
We offer the first meta-synthesis of factors influencing resilience after TBI using a Social Ecological model framework.
Resilience after TBI is multifaceted. Providers treating individuals with TBI should assess and address factors impacting resilience at individual, interpersonal, and systemic levels to help optimize recovery after TBI.
Funding:
This work was supported by grants from the SameYou Foundation and Heinz Family Foundation (#E7068) as part of a larger study on resilience after brain injury. In addition, this work was supported by grants from National Center for Complementary and Integrative Health awarded to Ana-Maria Vranceanu (1K24AT011760-01) and Jonathan Greenberg (1K23AT01065301A1).
Footnotes
Conflict of interest: The Authors declare that there is no conflict of interest.
References
- Adams D, & Dahdah M. (2016). Coping and adaptive strategies of traumatic brain injury survivors and primary caregivers. NeuroRehabilitation, 39(2), 223–237. [DOI] [PubMed] [Google Scholar]
- Analytis P, McKay A, Hamilton M, Williams G, Warren N, & Ponsford J. (2018). Physical activity: perceptions of people with severe traumatic brain injury living in the community. Brain injury, 32(2), 209–217. [DOI] [PubMed] [Google Scholar]
- Anne Jones J, & Curtin M. (2011). Reformulating masculinity: Traumatic brain injury and the gendered nature of care and domestic roles. Disability and rehabilitation, 33(17–18), 1568–1578. [DOI] [PubMed] [Google Scholar]
- Atallah DG, Bacigalupe G, & Repetto P. (2021). Centering at the margins: Critical community resilience praxis. Journal of Humanistic Psychology, 61(6), 875–905. [Google Scholar]
- Bannon SM, Greenberg J, Goldson J, O’Leary D, & Vranceanu A-M (2020). A social blow: the role of interpersonal relationships in mild traumatic brain injury. Psychosomatics, 61(5), 518–526. [DOI] [PubMed] [Google Scholar]
- Bannon SM, Kumar RG, Bogner J, O’Neil-Pirozzi TM, Spielman L, Watson EM, & Dams-O’Connor K. (2021). Reinjury after moderate to severe TBI: rates and risk factors in the NIDILRR Traumatic Brain Injury Model Systems. The Journal of head trauma rehabilitation, 36(1), E50–E60. [DOI] [PubMed] [Google Scholar]
- Boulton ER, Horne M, & Todd C. (2018). Multiple influences on participating in physical activity in older age: Developing a social ecological approach. Health Expectations, 21(1), 239–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braaf S, Ameratunga S, Ponsford J, Cameron P, Collie A, Harrison J, … Gabbe B. (2020). Traumatic injury survivors’ perceptions of their future: a longitudinal qualitative study. Disability and rehabilitation, 42(19), 2707–2717. [DOI] [PubMed] [Google Scholar]
- Brodsky AE, & Cattaneo LB (2013). A transconceptual model of empowerment and resilience: Divergence, convergence and interactions in kindred community concepts. American journal of community psychology, 52(3), 333–346. [DOI] [PubMed] [Google Scholar]
- Chouliara N, & Lincoln NB (2016). Qualitative exploration of the benefits of group-based memory rehabilitation for people with neurological disabilities: implications for rehabilitation delivery and evaluation. BMJ open, 6(9), e011225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dannenberg AL, Jackson RJ, Frumkin H, Schieber RA, Pratt M, Kochtitzky C, & Tilson HH (2003). The impact of community design and land-use choices on public health: a scientific research agenda. American journal of public health, 93(9), 1500–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dijkers MP (2004). Quality of life after traumatic brain injury: a review of research approaches and findings. Archives of physical medicine and rehabilitation, 85, 21–35. [DOI] [PubMed] [Google Scholar]
- Dixon G, Thornton EW, & Young CA (2007). Perceptions of self-efficacy and rehabilitation among neurologically disabled adults. Clinical rehabilitation, 21(3), 230–240. [DOI] [PubMed] [Google Scholar]
- Doering B, & Exner C. (2011). Combining neuropsychological and cognitive–behavioral approaches for treating psychological sequelae of acquired brain injury. Current Opinion in Psychiatry, 24(2), 156–161. [DOI] [PubMed] [Google Scholar]
- Donnelly KZ, Baker K, Pierce R, St. Ivany AR, Barr PJ, & Bruce ML. (2021). A retrospective study on the acceptability, feasibility, and effectiveness of LoveYourBrain Yoga for people with traumatic brain injury and caregivers. Disability and rehabilitation, 43(12), 1764–1775. [DOI] [PubMed] [Google Scholar]
- Doorn N, Gardoni P, & Murphy C. (2019). A multidisciplinary definition and evaluation of resilience: The role of social justice in defining resilience. Sustainable and Resilient Infrastructure, 4(3), 112–123. [Google Scholar]
- Douglas JM (2013). Conceptualizing self and maintaining social connection following severe traumatic brain injury. Brain injury, 27(1), 60–74. [DOI] [PubMed] [Google Scholar]
- Douglas M, Driver S, Callender L, & Woolsey A. (2019). Evaluation of a 12-month lifestyle intervention by individuals with traumatic brain injury. Rehabilitation psychology, 64(1), 25. [DOI] [PubMed] [Google Scholar]
- Drummond M, Douglas J, & Olver J. (2013). ‘If I haven’t got any smell… I’m out of work’: consequences of olfactory impairment following traumatic brain injury. Brain injury, 27(3), 332–345. [DOI] [PubMed] [Google Scholar]
- Dubuc É, Gagnon‐Roy M, Couture M, Bier N, Giroux S, & Bottari C. (2019). Perceived needs and difficulties in meal preparation of people living with traumatic brain injury in a chronic phase: Supporting long‐term services and interventions. Australian occupational therapy journal, 66(6), 720–730. [DOI] [PubMed] [Google Scholar]
- Evans RM (2019). Telemedicine to treat traumatic brain injury in outlying and rural medical facilities: A review of current literature. Lynchburg Journal of Medical Science, 1(4), 16. [Google Scholar]
- Fadyl JK, Theadom A, Channon A, & McPherson KM (2017). Recovery and adaptation after traumatic brain injury in New Zealand: Longitudinal qualitative findings over the first two years. Neuropsychological rehabilitation. [DOI] [PubMed] [Google Scholar]
- Fann JR, Bombardier CH, Vannoy S, Dyer J, Ludman E, Dikmen S, … Temkin N. (2015). Telephone and in-person cognitive behavioral therapy for major depression after traumatic brain injury: a randomized controlled trial. Journal of neurotrauma, 32(1), 45–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul M, Wald MM, Xu L, & Coronado VG (2010). Traumatic brain injury in the United States; emergency department visits, hospitalizations, and deaths, 2002–2006. [Google Scholar]
- Fleury J, & Lee SM (2006). The social ecological model and physical activity in African American women. American journal of community psychology, 37(1), 129–140. [DOI] [PubMed] [Google Scholar]
- Frost RB, Farrer TJ, Primosch M, & Hedges DW (2013). Prevalence of traumatic brain injury in the general adult population: a meta-analysis. Neuroepidemiology, 40(3), 154–159. [DOI] [PubMed] [Google Scholar]
- George M, & Apter AJ (2004). Gaining insight into patients’ beliefs using qualitative research methodologies. Current opinion in allergy and clinical immunology, 4(3), 185–189. [DOI] [PubMed] [Google Scholar]
- Glang A, Tyler J, Pearson S, Todis B, & Morvant M. (2004). Improving educational services for students with TBI through statewide consulting teams. NeuroRehabilitation, 19(3), 219–231. [PubMed] [Google Scholar]
- Godwin E, Chappell B, & Kreutzer J. (2014). Relationships after TBI: A grounded research study. Brain injury, 28(4), 398–413. [DOI] [PubMed] [Google Scholar]
- Godwin EE, & Kreutzer JS (2013). Embracing a new path to emotional recovery: adopting resilience theory in post-TBI psychotherapy. Brain injury, 27(6), 637–639. [DOI] [PubMed] [Google Scholar]
- Graff HJ, Christensen U, Poulsen I, & Egerod I. (2018). Patient perspectives on navigating the field of traumatic brain injury rehabilitation: a qualitative thematic analysis. Disability and rehabilitation, 40(8), 926–934. [DOI] [PubMed] [Google Scholar]
- Hammond FM, Davis CS, Cook JR, Philbrick P, & Hirsch MA (2012). Relational dimension of irritability following traumatic brain injury: a qualitative analysis. Brain injury, 26(11), 1287–1296. [DOI] [PubMed] [Google Scholar]
- Hanks RA, Rapport LJ, Waldron Perrine B, & Millis SR (2016). Correlates of resilience in the first 5 years after traumatic brain injury. Rehabilitation psychology, 61(3), 269. [DOI] [PubMed] [Google Scholar]
- Hart T, Kozlowski AJ, Whyte J, Poulsen I, Kristensen K, Nordenbo A, & Heinemann AW (2014). Functional recovery after severe traumatic brain injury: an individual growth curve approach. Archives of Physical Medicine and Rehabilitation, 95(11), 2103–2110. [DOI] [PubMed] [Google Scholar]
- Hawker S, Payne S, Kerr C, Hardey M, & Powell J. (2002). Appraising the evidence: reviewing disparate data systematically. Qualitative health research, 12(9), 1284–1299. [DOI] [PubMed] [Google Scholar]
- Herrmann LL, & Deatrick JA (2019). Experiences and perceptions of hospitalization and recovery of older adults and their caregivers following traumatic brain injury:“Not Knowing”. Research in gerontological nursing, 12(5), 227–238. [DOI] [PubMed] [Google Scholar]
- Holland JN, & Schmidt AT (2015). Static and dynamic factors promoting resilience following traumatic brain injury: a brief review. Neural plasticity, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J. (2018). Why social relationships are important for physical health: A systems approach to understanding and modifying risk and protection. Annual review of psychology, 69, 437–458. [DOI] [PubMed] [Google Scholar]
- Hux K, Bush E, Zickefoose S, Holmberg M, Henderson A, & Simanek G. (2010). Exploring the study skills and accommodations used by college student survivors of traumatic brain injury. Brain injury, 24(1), 13–26. [DOI] [PubMed] [Google Scholar]
- Jesus TS, & Silva IL (2016). Toward an evidence-based patient-provider communication in rehabilitation: linking communication elements to better rehabilitation outcomes. Clinical rehabilitation, 30(4), 315–328. [DOI] [PubMed] [Google Scholar]
- Johnson JL, Adkins D, & Chauvin S. (2020). A review of the quality indicators of rigor in qualitative research. American Journal of Pharmaceutical Education, 84(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jumisko E, Lexell J, & Söderberg S. (2009). The meaning of feeling well in people with moderate or severe traumatic brain injury. Journal of Clinical Nursing, 18(16), 2273–2281. [DOI] [PubMed] [Google Scholar]
- Kanavaki AM, Rushton A, Efstathiou N, Alrushud A, Klocke R, Abhishek A, & Duda JL (2017). Barriers and facilitators of physical activity in knee and hip osteoarthritis: a systematic review of qualitative evidence. BMJ open, 7(12), e017042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keegan LC, Togher L, Murdock M, & Hendry E. (2017). Expression of masculine identity in individuals with a traumatic brain injury. Brain injury, 31(12), 1632–1641. [DOI] [PubMed] [Google Scholar]
- Kozlowski AJ, Pretz CR, Dams-O’Connor K, Kreider S, & Whiteneck G. (2013). An introduction to applying individual growth curve models to evaluate change in rehabilitation: a National Institute on Disability and Rehabilitation Research Traumatic Brain Injury Model Systems report. Archives of Physical Medicine and Rehabilitation, 94(3), 589–596. [DOI] [PubMed] [Google Scholar]
- Kruithof N, Traa MJ, Karabatzakis M, Polinder S, de Vries J, & de Jongh MAC (2018). Perceived changes in quality of life in trauma patients: A focus group study. Journal of Trauma Nursing| JTN, 25(3), 177–186. [DOI] [PubMed] [Google Scholar]
- Lau SK, Luong D, Sweet SN, Bayley M, Levy BB, Kastner M, … Shepherd J. (2021). Using an integrated knowledge translation approach to inform a pilot feasibility randomized controlled trial on peer support for individuals with traumatic brain injury: A qualitative descriptive study. PloS one, 16(8), e0256650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lefebvre H, Cloutier G, & Josée Levert M. (2008). Perspectives of survivors of traumatic brain injury and their caregivers on long-term social integration. Brain injury, 22(7–8), 535–543. [DOI] [PubMed] [Google Scholar]
- Lefebvre H, & Levert MJ (2012). The needs experienced by individuals and their loved ones following a traumatic brain injury. Journal of Trauma Nursing| JTN, 19(4), 197–207. [DOI] [PubMed] [Google Scholar]
- Lefkovits AM, Hicks AJ, Downing M, & Ponsford J. (2020). Surviving the “silent epidemic”: A qualitative exploration of the long-term journey after traumatic brain injury. Neuropsychological rehabilitation, 1–25. [DOI] [PubMed] [Google Scholar]
- Levack WM, Kayes NM, & Fadyl JK (2010). Experience of recovery and outcome following traumatic brain injury: a metasynthesis of qualitative research. Disability and rehabilitation, 32(12), 986–999. [DOI] [PubMed] [Google Scholar]
- Liddle J, Fleming J, McKenna K, Turpin M, Whitelaw P, & Allen S. (2012). Adjustment to loss of the driving role following traumatic brain injury: A qualitative exploration with key stakeholders. Australian occupational therapy journal, 59(1), 79–88. [DOI] [PubMed] [Google Scholar]
- Loignon A, Ouellet M-C, & Belleville G. (2020). A systematic review and meta-analysis on PTSD following TBI among military/veteran and civilian populations. The Journal of head trauma rehabilitation, 35(1), E21–E35. [DOI] [PubMed] [Google Scholar]
- Malec JF, Ketchum JM, Hammond FM, Corrigan JD, Dams-O’Connor K, Hart T, … Bogner J. (2019). Longitudinal Effects of Medical Comorbidities on Functional Outcome and Life Satisfaction after Traumatic Brain Injury: An Individual Growth Curve Analysis of NIDILIRR Traumatic Brain Injury Model System Data. The Journal of head trauma rehabilitation, 34(5), E24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus L, Burlie D, Colantonio A, Mann R, & Chan V. (2019). Social Determinants of Health and Psychological Distress Among Ontario Adults with Traumatic Brain Injury. Archives of Physical Medicine and Rehabilitation, 100(10), e121–e122. [Google Scholar]
- Masel BE, & DeWitt DS (2010). Traumatic brain injury: a disease process, not an event. Journal of neurotrauma, 27(8), 1529–1540. [DOI] [PubMed] [Google Scholar]
- Mbakile-Mahlanza L, Manderson L, & Ponsford J. (2015). The experience of traumatic brain injury in Botswana. Neuropsychological rehabilitation, 25(6), 936–958. [DOI] [PubMed] [Google Scholar]
- McCulloch KL, De Joya AL, Hays K, Donnelly E, Johnson TK, Nirider CD, … Ward I,. (2016). Outcome measures for persons with moderate to severe traumatic brain injury: recommendations from the American Physical Therapy Association Academy of Neurologic Physical Therapy TBI EDGE Task Force. Journal of Neurologic Physical Therapy, 40(4), 269–280. [DOI] [PubMed] [Google Scholar]
- McPherson K, Fadyl J, Theadom A, Channon A, Levack W, Starkey N, … Group, T. E. R. (2018). Living life after traumatic brain injury: phase 1 of a longitudinal qualitative study. Journal of head trauma rehabilitation, 33(1), E44–E52. [DOI] [PubMed] [Google Scholar]
- Mealings M, Douglas J, & Olver J. (2019). Is it me or the injury: Students’ perspectives on adjusting to life after traumatic brain injury through participation in study. Neuropsychological rehabilitation. [DOI] [PubMed] [Google Scholar]
- Meints SM, Cortes A, Morais CA, & Edwards RR (2019). Racial and ethnic differences in the experience and treatment of noncancer pain. Pain management, 9(3), 317–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & Group P. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine, 6(7), e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muenchberger H, Kendall E, & Neal R. (2008). Identity transition following traumatic brain injury: A dynamic process of contraction, expansion and tentative balance. Brain injury, 22(12), 979–992. [DOI] [PubMed] [Google Scholar]
- Mumbower R, Childs G, Vance DE, Dreer LE, Novack T, & Heaton K. (2019). Sleep following traumatic brain injury (TBI): experiences and influencing factors. Brain injury, 33(13–14), 1624–1632. [DOI] [PubMed] [Google Scholar]
- Nalder E, Fleming J, Cornwell P, Shields C, & Foster M. (2013). Reflections on life: Experiences of individuals with brain injury during the transition from hospital to home. Brain injury, 27(11), 1294–1303. [DOI] [PubMed] [Google Scholar]
- Nalder E, Hartman L, Hunt A, & King G. (2019). Traumatic brain injury resiliency model: a conceptual model to guide rehabilitation research and practice. Disability and rehabilitation, 41(22), 2708–2717. [DOI] [PubMed] [Google Scholar]
- Nelson L, Temkin N, Dikmen S, Barber J, Giacino J, & Yuh E. (2019). Recovery After Mild Traumatic Brain Injury in Patients Presenting to US Level I Trauma Centers: A Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI) Study. JAMA Neurol. 2019; 76: 1049–1059. In. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann D, Tsaousides T, Spielman L, Kajankova M, Guetta G, Gordon W, & Dams-O’Connor K. (2017). Improving emotion regulation following web-based group intervention for individuals with traumatic brain injury. Journal of head trauma rehabilitation, 32(5), 354–365. [DOI] [PubMed] [Google Scholar]
- Nochi M. (2000). Reconstructing self-narratives in coping with traumatic brain injury. Social Science & Medicine, 51(12), 1795–1804. [DOI] [PubMed] [Google Scholar]
- Oppermann JD (2004). Interpreting the meaning individuals ascribe to returning to work after traumatic brain injury: a qualitative approach. Brain injury, 18(9), 941–955. [DOI] [PubMed] [Google Scholar]
- Parrott D, & Ibarra S. (2021). Randomized Controlled Trial Comparing a Telemedicine Brain Injury Coping Skills (BICS) group intervention to traditional in-person BICS for Brain Injury Patients and Caregivers. Archives of Physical Medicine and Rehabilitation, 102(10), e15. [Google Scholar]
- Partelow S. (2018). A review of the social-ecological systems framework. Ecology and Society, 23(4). [Google Scholar]
- Saadi A, Bannon S, Watson E, & Vranceanu A-M (2021). Racial and ethnic disparities associated with traumatic brain injury across the continuum of care: a narrative review and directions for future research. Journal of racial and ethnic health disparities, 1–14. [DOI] [PubMed] [Google Scholar]
- Salas CE, Casassus M, Rowlands L, Pimm S, & Flanagan DA (2018). “Relating through sameness”: a qualitative study of friendship and social isolation in chronic traumatic brain injury. Neuropsychological rehabilitation, 28(7), 1161–1178. [DOI] [PubMed] [Google Scholar]
- Sarmiento K, Langlois JA, & Mitchko J. (2008). “Help seniors live better, longer: prevent brain injury”: an overview of CDC’s education initiative to prevent fall-related TBI among older adults. The Journal of head trauma rehabilitation, 23(3), 164–167. [DOI] [PubMed] [Google Scholar]
- Self M, Driver S, Stevens L, & Warren AM (2013). Physical activity experiences of individuals living with a traumatic brain injury: a qualitative research exploration. Adapted Physical Activity Quarterly, 30(1), 20–39. [DOI] [PubMed] [Google Scholar]
- Shorland J, & Douglas JM (2010). Understanding the role of communication in maintaining and forming friendships following traumatic brain injury. Brain injury, 24(4), 569–580. [DOI] [PubMed] [Google Scholar]
- Shotton L, Simpson J, & Smith M. (2007). The experience of appraisal, coping and adaptive psychosocial adjustment following traumatic brain injury: A qualitative investigation. Brain injury, 21(8), 857–869. [DOI] [PubMed] [Google Scholar]
- Simpson G, Mohr R, & Redman A. (2000). Cultural variations in the understanding of traumatic brain injury and brain injury rehabilitation. Brain injury, 14(2), 125–140. [DOI] [PubMed] [Google Scholar]
- Soeker MS, & Pape C. (2019). The use of the model of Occupational Self-Efficacy for work retraining: a multiple case study. Occupational Therapy International, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soeker MS, Van Rensburg V, & Travill A. (2012). Individuals with traumatic brain injuries perceptions and experiences of returning to work in South Africa. Work, 42(4), 589–600. [DOI] [PubMed] [Google Scholar]
- Soeker S. (2016). A pilot study on the operationalization of the Model of Occupational Self Efficacy: A model for the reintegration of persons with brain injuries to their worker roles. Work, 53(3), 523–534. [DOI] [PubMed] [Google Scholar]
- Spaite DW, Bobrow BJ, Keim SM, Barnhart B, Chikani V, Gaither JB, … Adelson PD (2019). Association of statewide implementation of the prehospital traumatic brain injury treatment guidelines with patient survival following traumatic brain injury: the excellence in prehospital injury care (EPIC) study. JAMA surgery, 154(7), e191152-e191152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenberg M, Stålnacke B-M, & Saveman B-I (2020). Family experiences up to seven years after a severe traumatic brain injury–family interviews. Disability and rehabilitation, 1–9. [DOI] [PubMed] [Google Scholar]
- Stocchetti N, & Zanier ER (2016). Chronic impact of traumatic brain injury on outcome and quality of life: a narrative review. Critical Care, 20(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szeto AC, & Dobson KS (2010). Reducing the stigma of mental disorders at work: a review of current workplace anti-stigma intervention programs. Applied and Preventive Psychology, 14(1–4), 41–56. [Google Scholar]
- Theadom A, Rowland V, Levack W, Starkey N, Wilkinson-Meyers L, & McPherson K. (2016). Exploring the experience of sleep and fatigue in male and female adults over the 2 years following traumatic brain injury: a qualitative descriptive study. BMJ open, 6(4), e010453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudel TM, Nidiffer FD, & Barth JT (2007). Community-integrated brain injury rehabilitation: Treatment models and challenges for civilian, military, and veteran populations. Journal of Rehabilitation Research & Development, 44(7). [DOI] [PubMed] [Google Scholar]
- Tsatsou P. (2021). Is digital inclusion fighting disability stigma? Opportunities, barriers, and recommendations. Disability & Society, 36(5), 702–729. [Google Scholar]
- Umberson D, & Karas Montez J. (2010). Social relationships and health: A flashpoint for health policy. Journal of health and social behavior, 51(1_suppl), S54–S66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villa D, Causer H, & Riley GA (2020). Experiences that challenge self-identity following traumatic brain injury: a meta-synthesis of qualitative research. Disability and rehabilitation, 1–17. [DOI] [PubMed] [Google Scholar]
- Vranceanu A-M, Bannon S, Mace R, Lester E, Meyers E, Gates M, … Tehan T. (2020). Feasibility and efficacy of a resiliency intervention for the prevention of chronic emotional distress among survivor-caregiver dyads admitted to the neuroscience intensive care unit: a randomized clinical trial. JAMA network open, 3(10), e2020807-e2020807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh D, & Downe S. (2005). Meta‐synthesis method for qualitative research: a literature review. Journal of advanced nursing, 50(2), 204–211. [DOI] [PubMed] [Google Scholar]
- Werner S, & Scior K. (2016). Interventions aimed at tackling intellectual disability stigma: What works and what still needs to be done. In Intellectual disability and stigma (pp. 129–147): Springer. [Google Scholar]
- Zaloshnja E, Miller T, Langlois JA, & Selassie AW (2008). Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. The Journal of head trauma rehabilitation, 23(6), 394–400. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.