Abstract
Objective
Evidence on the efficacy of social skills training for adolescents with Level 1 Autism Spectrum Disorder (ASD) is unclear.
Method
We searched Pubmed, Scopus, and Web of Science until July 27th, 2023, for randomized controlled trials (RCTs) of social skills training for pre-adolescents and adolescents (aged 9-18) with Level 1 ASD. We then pooled data on efficacy from individual RCTs by conducting multivariate mixed-effects meta-analyses in R. We estimated possible bias in the retained RCTs using the RoB2 tool.
Results
We retained 36 RCTs (encompassing 2796 participants), including 18 RCTs comparing an experimental treatment to a waiting list, and 18 RCTs comparing it to standard care/control treatment. Meta-analyses showed that experimental treatments were significantly more efficacious than waiting list or standard care/ control treatments in improving social skills (SMD = 0.3745; 95%CI = [0.2396; 0.5093]), as well as reducing behavioral symptoms (0.3154;0.1783, 0.4525) and anxious/depressive symptoms (0.2780; 0.0432, 0.5128). However, for some outcomes there was significant heterogeneity across studies and evidence of publication bias. Subgroup analyses and meta-regressions did not identify any specific clinical or demographic factors as significant predictors of outcome. The most common risk of bias across studies was related to deviations from intended interventions and measurement of the outcomes.
Conclusions
At the group level, social skills training for adolescents with Level 1 ASD is efficacious, with small-to-moderate effect size. Future research should focus on personalized medicine approaches, aimed at tailoring interventions to specific characteristics of adolescents with Level 1 ASD.
Keywords: autism spectrum disorders, adolescence, social skills training, RCT design, meta-analysis
Introduction
Level 1 Autism Spectrum Disorder (ASD) is characterized by challenges in social communication, limited and repetitive behaviors, and focused interests, while maintaining typical cognitive and linguistic abilities (APA, 2022). Adolescents with Level 1 ASD often exhibit weaknesses in social skills, which can significantly impact their daily lives and emotional well-being (Rosello et al., 2023). These weaknesses may include difficulties recognizing differences from peers, feelings of loneliness, and experiences of rejection (Mirzaei et al., 2020), as well as trouble understanding non-verbal social cues (Ames & Jarrold, 2009), initiating and maintaining conversations (Koegel et al., 2021), sensory sensitivity (Narzisi et al., 2022), interpreting others' emotions, and navigating complex social dynamics (Ma et al., 2023).
Several reasons necessitate specific interventions and support for these weaknesses. Firstly, social skills are crucial for social, academic, and professional achievement (Lord et al., 2022). Without these skills, adolescents with Level 1 ASD may feel isolated, frustrated, and struggle to build meaningful relationships with their peers. They often encounter difficulties such as depression and anxiety, which contribute to increased isolation stemming from their peers. Consequently, their withdrawal from social interactions exacerbates their already existing social skill weaknesses (Bifulco et al., 2014; Flynn & Healy, 2012; Narzisi & Stavropoulos, 2022). Secondly, social difficulties can lead to behavioral problems (Lupi et al., 2023). Adolescents with Level 1 ASD may exhibit inappropriate behaviors or isolate themselves from their peers due to their lack of understanding of implicitly accepted social rules (Oh et al., 2021). This can lead to a cycle of isolation and low self-esteem, which can be difficult to break without targeted interventions (van der Cruijsen et al., 2024).
While understanding the causes behind these social skills deficiencies is crucial, it is equally important to delve into the nuanced consequences they entail (Frye, 2018). Social withdrawal, rejection, exclusion, bullying, anxiety, and depression are among the multifaceted repercussions of social skills weaknesses in individuals with ASD (Mazefsky et al., 2013; White et al., 2007). However, these consequences are not isolated phenomena but they are intricately intertwined with underlying mechanisms and coping strategies employed by individuals with ASD within their social environments. For instance, social withdrawal may manifest as a protective mechanism in response to overwhelming social stimuli, allowing individuals with ASD to seek solace in familiar and predictable environments (Bellini, 2006). Rejection and exclusion, often fueled by misinterpretations of social cues and non-conformity to social norms, can trigger feelings of alienation and inadequacy (Bauminger-Zviely et al., 2013). Bullies may exploit these vulnerabilities, targeting individuals with ASD for their perceived differences (Sterzing et al., 2012). Consequently, anxiety and depression may ensue as individuals grapple with the emotional toll of navigating a social landscape fraught with uncertainty and misunderstanding (White et al., 2013). Understanding these connections between social skills weaknesses, underlying mechanisms, and coping strategies is essential for tailoring effective interventions and support systems for adolescents with Level 1 ASD.
Moreover, it is important to provide functional support rather than following just a treatment protocol because each adolescent with Level 1 ASD is a unique individual with specific needs and challenges. A personalized approach allows interventions to be tailored to the specific needs of the adolescent, considering their interests, strengths, and areas of development (Gabis et al., 2021).
Furthermore, the support environment, which may involve family, school, and community, plays a fundamental role in providing a supportive context for the development of social skills (Rispoli et al., 2019). For example, teachers and educators can adopt differentiated teaching strategies and create opportunities for practicing social skills within the school environment (Rispoli et al., 2019). Family can play an important role in supporting and reinforcing learned skills in everyday situations (Tomaszewski et al., 2020).
Supporting social skills in adolescents with Level 1 ASD could be crucial for their long-term success and well-being (Lord et al., 2021). A personalized and functional approach that considers their individual needs and the implementation of social skills development programs could help them improve their developmental trajectories and reach their full potential (Roberts et al., 2018).
The studies on interventions has predominantly focused on childhood and early childhood, neglecting the adolescent period (Crasta et al., 2023; Narzisi, 2015). This is unfortunate as it is becoming increasingly apparent that social skill deficits manifest more prominently during adolescence (Dean et al., 2020). The social skills issues are compounded by the multifaceted upheaval in physical, emotional, cognitive, and social realms that adolescents with ASD and their families are faced with, each transition posing unique obstacles (Cresswell & Cage, 2019). To address these challenges, adolescents with Level 1 ASD can engage in group-based SSTs (Social Skills Trainings). SSTs could be an effective intervention for individuals with Level 1 ASD for several reasons (Laugeson et al., 2012). SST provides a structured and supported environment to acquire and practice social skills through direct instruction, modelling and role-playing (Soares et al., 2021). They provide a safe and controlled context in which they can experience and learn social dynamics without the pressure or anxiety they might experience in natural social situations (Adams et al., 2023). This can help adolescents build confidence in their social skills and feel more comfortable engaging with others (You et al., 2024).
In addition, the group provides opportunities for social feedback and sharing similar experiences, which can foster a sense of belonging and mutual learning (Hotton & Coles, 2016). In addition, being part of a group during SST can help individuals with Level 1 ASD develop skills of collaboration, empathy and understanding the perspectives of others, skills that are essential for positive and meaningful social relationships (Afsharnejad et al., 2024).
Social Skills Training (SST) programs exhibit considerable variability in terms of content, teaching methodologies, delivery modes, and therapeutic intensity. Standardized SST programs often involve behavioral modeling of specific social skills, role-playing to practice these skills, and personalized feedback on performance. Some programs adopt didactic approaches with structured lessons, while others utilize play-based interventions to elicit social skills (Kaat & Lecavalier, 2015). The effect sizes (from small to large) and the way in which SST is delivered also varies across studies, with involvement from parents, peers, or teachers, either individually or in tandem (Wolstencroft et al., 2018; Gates et al., 2017).
As pointed out by the systematic reviews and meta-analyses, despite the widespread adoption of Social Skills Training (SST), the evidence regarding its goodness remains limited and primarily relies on studies with methodological weaknesses (Afsharnejad et al., 2024; Cappadocia & Weiss, 2011; Ferraioli & Harris, 2011; Gilmore et al., 2022; Gosling et al., 2022; McMahon et al., 2013; Rao et al., 2008; Reichow & Volkmar, 2010; White et al., 2007).
Recent large-scale evidence synthesis efforts have addressed the efficacy of interventions for ASD, including SST. In 2022, Gosling et al., published an umbrella review examining outcomes from a total of 128 meta-analyses. These analyses synthesized evidence from over 190 unique controlled clinical trials investigating the effectiveness (i.e. the degree to which something is successful in producing a desired result) of psychosocial interventions on core ASD symptoms and related issues. Gosling et al. found that a considerable portion of these meta-analyses demonstrated a moderate to large combined effect size (i.e., SMD ≥ 0.50; 41% of the meta-analyses) and/or statistically significant findings (53% of the meta-analyses) favoring psychosocial interventions. According to the algorithmic criteria established for this umbrella review, researchers concluded that the efficacy of many of these psychosocial interventions was supported by highly suggestive or suggestive evidence, depending on the age of the participants and the specific outcomes evaluated. For late school-aged children and adolescents, suggestive evidence was identified for the goodness of social skills groups (SSGs) in improving social communication and overall Level 1 ASD symptoms. However, Gosling et al.'s review, unlike what we proposed in our study did not solely examine RCTs (Gosling et al., 2022).
In 2024, Afsharnejad et al., published a systematic review and meta-analysis examining social skills group programs (SSGPs) designed to aid autistic adolescents in navigating social environments. The study assessed the programs' methodological quality, fidelity, and efficacy. Through an analysis of 18 studies, it revealed a moderate overall efficacy (g=0.60, p<.001) in supporting socialization among autistic adolescents. Despite generally good methodological quality, most studies displayed moderate to low program fidelity. However, Afsharnejad' et al. (2024) specifically excluded school-based programs and those focusing on parent or family outcomes. Additionally, Afsharnejad et al.'s study did not encompass the outcomes arising from social skills enhancement programs implemented within educational settings, nor did it consider assessments by teachers and/ or parents before and after the interventions. However, to gain insight into the external validity of social skills interventions in real-world scenarios (Laugeson et al., 2009), it is fundamental to assess also the efficacy of social skills programs, including evaluations from teachers and parents.
To corroborate the findings of Afsharnejad et al. (2024), we conducted the present systematic review and meta-analysis to estimate the efficacy of Social Skills interventions for Adolescents with Level 1 ASD including not only the assessments of clinicians but also those of parents and teachers. We also tested for specific moderators of response to treatment, including treatment duration, cognitive functioning, specific psychiatric comorbidities, and concurrent use of psychotropic medications, as well as age and gender, which have all been to affect the outcomes of specific rehabilitation programs (Bent et al., 2023; Linstead et al., 2017; Kedar & Bauminger-Zviely, 2023; Storch et al., 2022).
Methods
The reporting of this systematic review with meta-analysis followed the most recent PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Page et al., 2021) (see PRISMA Checklist in supplemental materials – table S1). The protocol was preregistered on PROSPERO (CRD42022309132).
Search Strategy and Selection Criteria
We systematically searched Pubmed, Scopus, and Web of Science from their date of inception to 27 July 2023, with a restriction to articles published in English (we had no funding to professionally translate articles into languages other than English). The search strategy and syntax were as follows: (therap* OR treatment OR intervention) AND (autis*) AND (child* OR adolescen*) AND social skill* AND random* (the full search strategies applied for each database are available in supplemental materials – table S2). Studies were considered eligible for inclusion when they met the following criteria: (1) RCT; (2) including youths aged 9-18; (3) meeting DSM or ICD diagnostic criteria (any version) for Level 1 ASD or equivalent; (4) focusing on interventions explicitly aimed at improving social skills; (5) using control group represented by (a) waiting list or (b) services as usual/or not primarily focused on the implementation of social skills (Not Focused on Social Skills - NFSS); (7) using standardized clinical measures of Social Skills (SS), Social Skills + Restrictive and Repetitive Behaviors (SS+RRB), Behavioral Symptoms (BEH), and/or Anxious/Depressive Symptoms (ANX/DEP).
Data Selection, Extraction and Coding
First, the titles and abstracts of the studies were independently screened by three authors (A.N., R.M. and S.S.) to identify potential studies that met the inclusion criteria. Any disagreements that arose were resolved through discussion among the authors. Subsequently, the full texts of selected articles were independently evaluated by three authors (A.N., R.M. and S.S) to confirm their eligibility for inclusion. During the data extraction phase, three authors utilized standardized forms to extract information from each third of the retrieved studies. To ensure accuracy and completeness, the extracted data were then double-checked by the remaining two extractors.
The clinical scales used in the included studies were classified according to the type of outcome they assessed, as follows: Social Skills (SS), Social Skills + Restrictive and Repetitive Behaviors (SS+RRB), Behavioral Symptoms (BEH) and Anxious/Depressive Symptoms (ANX/DEP). In cases where data were unavailable in the published reports, attempts were made to gather the missing information by reaching out the corresponding, first, or senior authors via e-mail (see Appendix 1 for more details).
Data Synthesis and Analysis
Initially, a descriptive synthesis was conducted for all studies included in the systematic review. Subsequently, meta-analyses were performed in RStudio 4.0® (R-Core-Team, 2020) to estimate the pooled effect size across studies for each type of outcome (i.e., SS, SS+RRB, BEH and ANX/DEP) and for each type of comparison (i.e., experimental treatment versus waiting list, experimental treatment versus control treatment, experimental treatment versus waiting list + control treatment). Meta-analyses were conducted whenever there were at least two studies reporting on the same outcome for each comparison.
For studies that reported means and standard deviations of outcome measures, pre-to-post raw mean differences were calculated by subtracting the raw scores obtained before treatment from those obtained after treatment, with scale scores reversed when necessary. The standard deviations of pre-to-post treatment changes were computed using the formula: SD = √ (SDpre)2 + (SDpost)2 – 2 × r × SDpre × SDpost, where r represents the correlation coefficient. In this study, a conservative estimate of r = 0.4 was chosen based on previous literature (Bucher et al., 1997; Gu et al., 2015; Van de Laar et al., 2005). The between-group standardized mean differences (SMD) and related variances were estimated using the package metafor in RStudio® and used as a measures of effect size in the meta-analyses.
For each type of outcome variable and comparison, a multivariate mixed-effects meta-analytic model was fitted to the data using metafor package in RStudio® (Viechtbauer, 2010). This model accounted for the non-independence of data by nesting effect sizes within studies that reported multiple effect sizes for the same component. The Restricted Maximum-Likelihood (REML) estimator was employed, and the Knapp-Hartung confidence interval adjustment (Langan et al., 2019) was applied. Heterogeneity across studies was assessed using the Cochran Q test (p-value < 0.05 indicates significant heterogeneity). Publication bias was assessed visually using funnel plots for small studies and quantitatively with the rank correlation test for funnel plot asymmetry (Begg & Mazumdar, 1994) – a modified version of the Egger’s test (Egger et al., 1997) suitable for multivariate meta-analytic models – by computing Kendall’s tau.
In the presence of significant heterogeneity across studies, exploratory subgroup analyses and meta-regressions were conducted to investigate potential factors that might have affected the pooled effect size in studies assessing Social Skills as outcome variable. The explored moderators for subgroup analysis included the presence of psychiatric comorbidities (specifically, Attention-Deficit/Hyperactivity Disorder (ADHD), Oppositional Defiant Disorder (ODD) and Anxiety Disorder (AD)), and concurrent use of psychotropic medications. Meta-regressions were conducted using age, sex assigned at birth (hereafter, “gender”), treatment duration, percent use of medication and full-scale intelligence quotient as regressors of interest.
Study Quality Rating
Two authors (A.N. and S.S.) used the most recent version of the Cochrane Risk-of-Bias scale for randomized trials (RoB-2 scale; Sterne et al., 2019). The RoB-2 scale comprises a fixed set of bias domains that encompass various potential sources of bias, including (D1) bias from randomization, (D2) deviations from intended interventions, (D3) missing outcome data, (D4) measurement bias, and (D5) bias in selection of reported results. Each domain includes a series of "signaling questions" that aim to gather information relevant to the risk of bias in the trial. These domains are mandatory and cover all potential biases in randomized trials. The judgment for each domain was classified as ‘Low’ or ‘High’ risk of bias, or ‘Some Concerns’.
Results
Study Selection
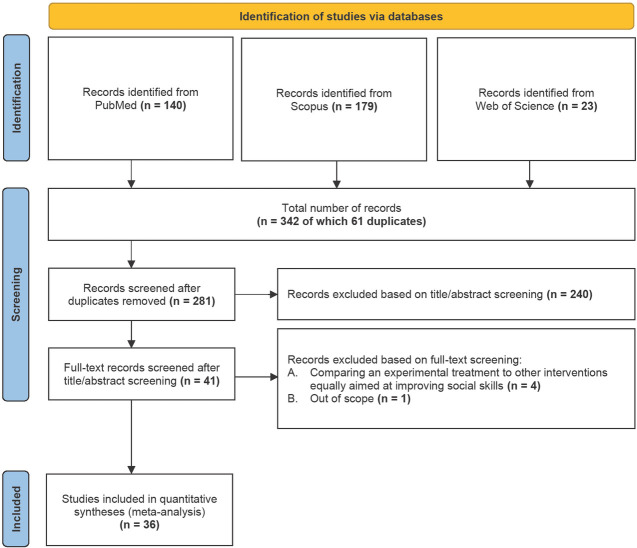
As shown in the PRISMA flowchart (figure 1) after screening 281 possibly relevant references, 36 studies were included in the meta-analyses (2794 participants in total; 1435 undergoing an experimental treatment and 1359 in the control group). Among the included studies, 18 compared an experimental treatment (489 participants) to a waiting list (471 participants), whereas another 18 compared an experimental treatment (946 participants) to a service as usual/or not primarily focused on the implementation of social skills (Not Focused on Social Skills - NFSS) (888 participants). In the next sections we present the findings from the meta-analyses according to the type of outcome variable assessed, as well as to the type of comparison (see Appendix 1 for more details).
Figure 1.
PRISMA flowchart
From: Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., McGuinness, L. A., … Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Systematic reviews, 10(1), 89. https://doi.org/10.1186/s13643-021-01626-4
Meta-Analyses
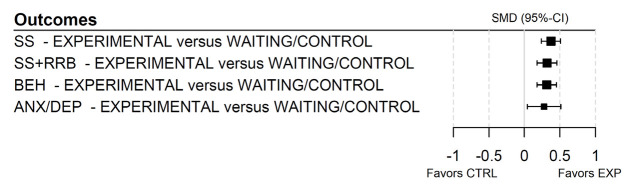
Our study included 36 RCTs that evaluated the eficacy of 18 Social Skills Trainings (SST) (see tables S3, S4, S5 and Appendix 1 for more details). Figure 2 presents a summary forest plot illustrating the results of the four meta-analyses encompassing all outcome variables.
Figure 2.
Forest plot of the four meta-analyses across all outcome variables
Abbreviations: 95%-CI = confidence interval at 95%; ANX/DEP = anxious/depressive symptoms; BEH = behavioral symptoms; CTRL = waiting list/control treatment; EXP = experimental intervention; RRB = restrictive and repetitive behaviors; SMD = standardized mean difference; SS = social skills.
Furthermore, we fitted eight additional multivariate mixed-efects meta-analytic models according to the type of comparison (experimental treatment versus waiting list and experimental treatment versus control treatment) for each type of outcome variable. A summary forest plot of the eight additional meta-analyses, considering all types of comparison and outcome variables, can be found in supplemental materials – figure S1.
Social Skills
Twenty-three studies (Afsharnejad et al., 2021; Beaumont et al., 2021; Begeer et al., 2015; Corbett et al., 2019; Corbett et al., 2023; Dekker et al., 2018; Dolan et al., 2016; Frankel et al., 2010; Hopkins et al., 2011; Idris et al., 2022; Ko et al., 2018; Locke, Rotheram-Fuller & Kasari, 2012; Lopata et al., 2010; Lopata et al., 2019; Owens et al., 2008; Platos et al., 2022; Rabin et al., 2018; Schohl et al., 2014; Shum et al., 2019; Thomeer et al., 2019; Vernon et al., 2018; Wright et al., 2023; Yoo et al., 2014) reported clinical measures of SS as outcome variable with suficient information for efects sizes to be computed and were thus included in the meta-analysis. A meta-analysis conducted on 103 efect sizes showed that experimental treatments were significantly more eficacious on SS than waiting list/ control treatment (SMD = 0.3745; SE = 0.0681; 95%-CI = [0.2396; 0.5093]; t = 5.5015; p < 0.0001). Between-study heterogeneity was significant (Q = 292.1041; p < 0.0001) and publication bias was also detected (τ = 0.3472; p < 0.0001). Forest and funnel plots are depicted in supplemental materials – figure S2A – B.
Since significant heterogeneity was detected, two further meta-analyses were conducted to investigate whether the type of comparison afected findings of the main meta-analysis. A meta-analysis on 54 efect sizes reported by 12 studies showed that experimental treatments were significantly more eficacious on SS than waiting list (SMD = 0.5385; SE = 0.0816; 95%-CI = [0.3752; 0.7017]; t = 6.6004; p < 0.0001), though both between-study heterogeneity (Q = 148.0237; p < 0.0001) and publication bias (τ = 0.4324; p < 0.0001) were still significant. Similarly, a meta-analysis on 49 efect sizes reported by nine studies showed that experimental treatments were significantly more eficacious on SS than control treatments (SMD = 0.1762; SE = 0.0743; 95%-CI = [0.0273; 0.3252]; t = 2.3733; p = 0.0213), though both between-study heterogeneity (Q = 82.8690; p = 0.0054) and publication bias (τ = 0.1880; p = 0.0452) were still significant.
Social Skills and Restricted Repetitive Behaviors
Fourteen studies (Begeer et al., 2015; de Korte et al., 2021; Idris et al., 2022; Lopata et al., 2010; Lopata et al., 2015; Luckardt et al., 2018; Platos et al., 2022; Rabin et al., 2018; Schohl et al., 2014; Shum et al., 2019; Thomeer et al., 2016; Thomeer et al., 2019; Vernon et al., 2018; White et al., 2013) reported clinical measures of SS+RRB as outcome variable with suficient information for efects sizes to be computed and were thus included in the meta-analysis. A meta-analysis conducted on 20 efect sizes showed that experimental treatments were significantly more eficacious on SS+RRB than waiting list/control treatment (SMD = 0.3193; SE = 0.0668; 95%-CI = [0.1800; 0.4585]; t = 4.7827; p = 0.0001). Between-study heterogeneity was not significant (Q = 30.9873; p = 0.0554) and publication bias was not detected (τ = 0.3333; p = 0.0360). Forest and funnel plots are depicted in supplemental materials – figure S3A – B.
The meta-analysis of 12 efect sizes reported by nine studies showed that experimental treatments were significantly more efective on SS+RRB than waiting list (SMD = 0.3122; SE = 0.0729; 95%-CI = [0.1534; 0.4710]; t = 4.2834; p = 0.0011), as well as a meta-analysis on eight efect sizes reported by five studies showing that experimental treatments were significantly more eficacious on SS+RRB than control treatments (SMD = 0.3172; SE = 0.1253; 95%-CI = [0.0209; 0.6134]; t = 2.5312; p = 0.0392).
Behavioral Symptoms
Twelve studies (Beaumont et al., 2021; de Korte et al., 2021; Frankel et al., 2010; Lopata et al., 2010; Owens et al., 2008; Rabin et al., 2018; Schohl et al., 2014; Shum et al., 2019; Thomeer et al., 2016; Thomeer et al., 2019; White et al., 2013; Yoo et al., 2014) reported clinical measures of BEH as outcome variable with suficient information for efects sizes to be computed and were thus included in the meta-analysis. A meta-analysis conducted on 21 efect sizes showed that experimental treatments were significantly more eficacious on BEH than waiting list/control treatment (SMD = 0.3154; SE = 0.0657; 95%-CI = [0.1783; 0.4525]; t = 4.7989; p = 0.0001). Between-study heterogeneity was not significant (Q = 11.0250; p = 0.9456), whereas publication bias was detected (τ = 0.5238; p = 0.0006). Forest and funnel plots are depicted in supplemental materials – figure S4A – B.
Coherently, a meta-analysis of 16 efect sizes reported in eight studies showed that experimental treatments were significantly more eficacious on BEH than waiting list (SMD = 0.2908; SE = 0.0814; 95%-CI = [0.1173; 0.4643]; t = 3.5729; p = 0.0028). A meta-analysis of five efect sizes reported by four studies showing that experimental treatments were significantly more efective on BEH than control treatments (SMD = 0.4048; SE = 0.1290; 95%-CI = [0.0466; 0.7629]; t = 3.1380; p = 0.0349).
Anxious/Depressive Symptoms
Nine studies (Beaumont et al., 2021; de Korte et al., 2021; Frankel et al., 2010; Locke et al., 2012; Schiltz et al., 2018; Schohl et al., 2014; Vernon et al., 2018; White et al., 2013; Yoo et al., 2014) reported clinical measures of ANX/DEP as outcome with suficient information for efects sizes to be computed and were thus included in the meta-analysis. A meta-analysis conducted on 21 efect sizes showed that experimental treatments were significantly more eficacious on ANX/DEP than waiting list/control treatment (SMD = 0.2780; SE = 0.1126; 95%-CI = [0.0432; 0.5128]; t = 2.4694; p = 0.0227). Between-study heterogeneity was significant (Q = 34.3435; p = 0.0239) and publication bias was also detected (τ = 0.3905; p = 0.0131). Forest and funnel plots are depicted in supplemental materials – figure S5A – B.
Since significant heterogeneity was detected, two further meta-analyses were conducted to investigate whether the type of comparison afected findings of the main meta-analysis. A meta-analysis on 16 efect sizes reported by 6 studies showed that experimental treatments were significantly more efective on ANX/DEP than waiting list (SMD = 0.4459; SE = 0.0754; 95%-CI = [0.2852; 0.6066]; t = 5.9149; p < 0.0001), and neither between-study heterogeneity (Q = 11.5404; p = 0.7134) nor publication bias (τ = 0.3000; p = 0.1160) were significant anymore. By contrast, a meta-analysis of five efect sizes reported in three studies found no significant diferences between experimental and control treatments in the eficacy on ANX/DEP (SMD = –0.1080; SE = 0.1560; 95%-CI = [–0.5410; 0.3250]; t = –0.6924; p = 0.5268); neither between-study heterogeneity (Q = 4.3316; p = 0.3630) nor publication bias (τ = –0.2000; p = 0.8167) were significant anymore.
Subgroup Analyses and Meta-Regressions
None of the explored moderators in the subgroup analyses significantly affected the results related to the efficacy of all interventions combined (see table S6). Additionally, five meta-regressions were conducted on a priori selected variables, including age, gender, treatment duration, percent use of medication and full-scale intelligence quotient (FSIQ), but none of them were found to significantly moderate the pooled efect size (see table S7).
Risk of Bias Assessment
For D1 (Bias from randomization), 26 out of 36 studies (72%) exhibited a low risk, 10 studies (28%) showed some concerns, and none showed a high risk. Regarding D2 (Deviations from intended interventions), 12 studies (33%) showed low risk, 22 studies (61%) showed some concerns and 2 studies (6%) showed high risk. Concerning D3 (Missing outcome data), 34 studies (94%) displayed a low risk, 2 studies (6%) showed some concerns, and none had a high risk. For D4 (Measurement bias), 7 studies (19%) showed low risk, 22 studies (61%) showed some concerns, and seven studies (19%) showed high risk. Finally, regarding D5 (Bias in selection of reported results), 32 studies (97%) reported low risk, four studies (11%) had some concern, and none reported high risk (see figure 3).
Figure 3.
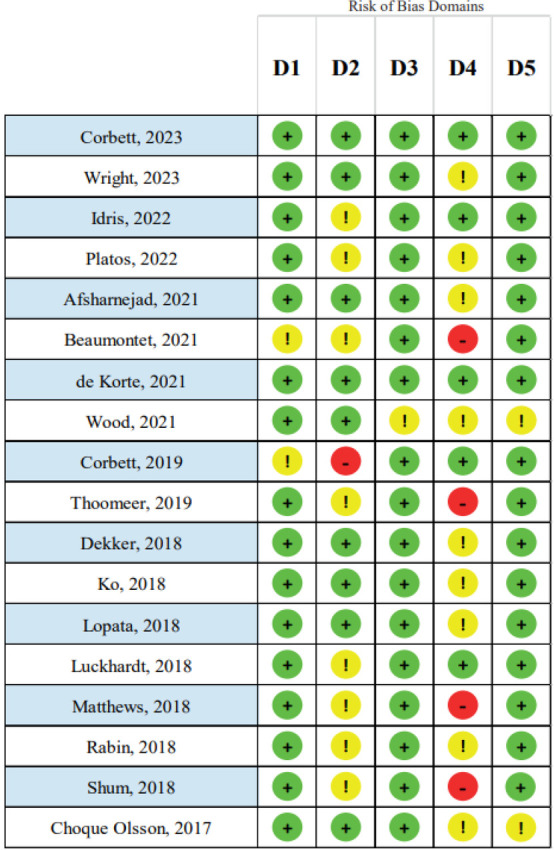
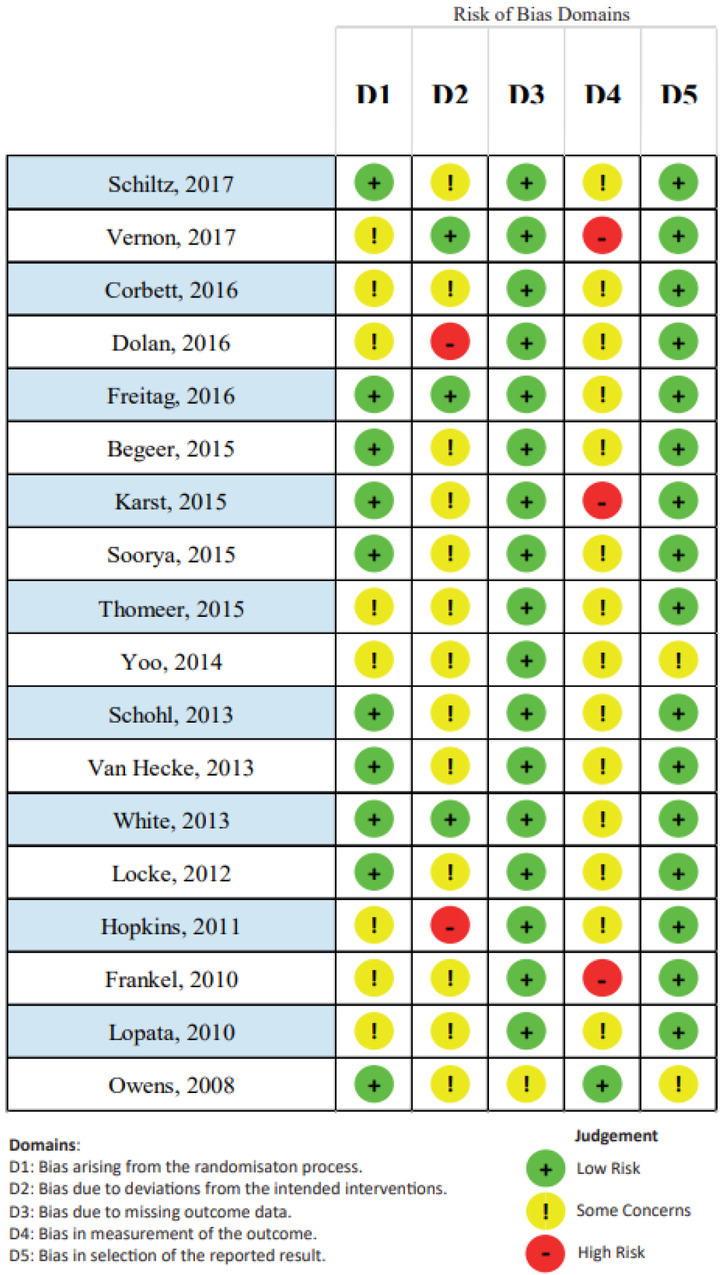
Risk of bias assessment according the RoB-2 scale domains
Discussion
This meta-analysis explored the eficacy of SST for adolescents with Level 1 ASD for four outcomes: Social Skills (SS), Social Skills plus Restricted Repetitive Behaviors (SS+RRB), Behavioral symptoms (BEH), and Anxious/Depressive symptoms (ANX/DEP). Findings showed that experimental treatments were significantly more eficacious, with small-to-moderate efect sizes in enhancing outcomes, than waiting list or control treatments in all four domains. Notably, significant heterogeneity and publication bias were detected. In detail, our study showed that experimental treatments were significantly more efective in improving social skills (SS) than waiting list or control treatments. However, it is important to note that significant heterogeneity was found among studies and the presence of publication bias. These factors could afect the overall reliability of the results. Heterogeneity could result from diferences in intervention protocols, study population or social skills assessment methods. Consequently, future research should focus on reducing this heterogeneity and identifying factors that might influence treatment outcomes. This could include analysis of variables such as age, level of cognitive functioning, severity of autistic symptoms, and type of intervention used. A better understanding of these factors could improve intervention design and optimize outcomes for individuals with ASD.
In the outcome Social Skills and Restricted Repetitive Behaviors (SS+RRB), experimental treatments were significantly more efective in improving social skills and reducing repetitive behaviors than waiting list or control treatments. The fact that no significant heterogeneity was found among the studies may indicate greater consistency in the results than in the domain of SS alone. This suggests that targeted intervention might have benefits not only on social skills but also on repetitive behaviors, which are often problematic for people with ASD.
Regarding the outcome Behavioral symptoms (BEH), our results showed that experimental treatments were significantly more effective in reducing behavioral symptoms than waiting list or control treatments. Again, the absence of significant heterogeneity among studies suggests greater consistency in results. This advice that targeted interventions can have a positive impact on behavioral symptoms associated with ASD, which is crucial to improving the quality of life for patients and their families.
Analysis of the outcome Anxious/Depressive symptoms (ANX/DEP) showed that experimental treatments are significantly more effective in reducing anxiety/depressive symptoms than waiting list or control treatments. However, it is important to note that significant heterogeneity was found among the studies and the presence of publication bias. Interestingly, the results Figure of the 3. subgroup Risk of bias analysis assessment suggest according that the efficacy 2 scale of experimental treatments might vary depending on sizes, with results ranging from large to small effects in social skills and no significant effect in behavioral/ emotional challenges and autistic-like features. In 2017, Gates et al.' study reported medium effect sizes instead. Regarding heterogeneity of outcome measures, our study found significant heterogeneity in all four outcome domains, while Afsharnejad’s et al. (2024) study observed significant heterogeneity only in the outcomes of autistic-like characteristics. From a prospective analysis, the results of our study showed a general consistency in the benefits of experimental treatment, although heterogeneity and publication bias may influence the confidence in the results. The presence of significant heterogeneity suggests that the results may be influenced by uncontrolled factors or variations domains in study design. On the other hand, Afsharnejad's et al. (2024) study showed more variable results, with the type of comparison used. This underscores the importance of carefully considering the study design and comparison used when interpreting the results related to anxiety/depressive symptoms.
The effects size ranged from moderate to small, with the largest effect observed in SS (SMD = 0.3745) and the smallest effect observed in ANX/DEP symptoms (SMD = 0.2780). On the other hand, the recent study by Afsharnejad et al. (2024) reported more varied effect a wider range of size effects and less heterogeneity in the overall results. Gates' et al. (2017) study contributed results of average size and non-significant heterogeneity. Comparing our study with those of Afsharnejad et al. (2024) and Gates et al. (2017) shows that our study provides a more specific and quantitative view of the effects of experimental interventions on a range of outcomes, while Afsharnejad's et al. (2024) study provides a more detailed perspective on how effects are measured and how they vary across outcome domains. Gates' et al. (2017) study adds further evidence on the average effects of interventions on social competence, providing a complementary perspective to the other two studies.
In our study, heterogeneity in outcome measures may significantly influence the interpretation of clinical response to the intervention (see table S8). The presence of significant differences in the outcome measures used in the various included studies may make direct comparison of the effects of different experimental interventions complicated. For example, if some studies use different instruments to measure the same constructs, it may be difficult to determine whether the observed differences in outcomes are due to the actual effectiveness of the interventions or to discrepancies in the measurements themselves. In addition, heterogeneity in outcome measures could impact the accuracy of estimates of the effects of interventions. Combining results in a consistent and reliable meta-analysis could be made more difficult by the presence of different outcome measures. This could lead to greater uncertainty in estimates of the effects of interventions and reduce confidence in the overall results.
Finally, the heterogeneity of outcome measures could limit the generalizability of our study results. The variability in outcome measures used in the various included studies could make it difficult to determine whether the observed effects would translate into clinically meaningful benefits for the entire population of patients with ASD. Therefore, it is important to carefully consider the heterogeneity of outcome measures when evaluating the effects of experimental interventions in order to interpret the results accurately and informatively.
In our study, psychiatric comorbidities (ADHD, ODD, AD) and the use of psychotropic medications did not significantly impact results. However, the prevalence of psychiatric comorbidity and the use of psychotropic medications among individuals with ASD highlights the need for further investigation into their specific influence on treatment outcomes (Frankel et al., 2007; Gates et al., 2017; Herbrecht et al., 2009). Indeed, the effects of comorbidities varied across studies, with some studies reporting improvements with comorbid anxiety disorder but not ADHD (Antshel, 2011) and reduced effects with comorbid anxiety (Pellecchia et al., 2015).
Age, gender, treatment duration and full-scale intelligence quotient (FSIQ) were not moderators of the pooled effect size included. Even though our findings indicate that evidence-based interventions exhibit a small-to-moderate effect size, it is possible that due to extreme phenotypic heterogeneity, some individuals respond significantly well to these interventions while others do not, resulting in an average effect size that appears small or moderate.
Concerning age some studies have indicated comparatively superior gains in older participants (Herbrecht et al., 2009; Mathur et al., 1998), whereas others have suggested greater advantages for younger children using specific approaches (McMahon et al., 2013). However, the results of our exploratory subgroup analyses and meta-regressions, conducted to investigate potential sources of heterogeneity, indicated no significant moderation effect of age. The clinical explanation for this result could be that the effectiveness of interventions for ASD may vary with the age of the participants. It could be that younger people, being at a more susceptible and rapidly changing stage of development, benefit more from interventions than older individuals. This could be due to greater brain plasticity in younger children, which makes it easier for them to learn new social and behavioral skills. In addition, younger people might be less influenced by external or prior factors, such as accumulated experience over time, which could affect their response to interventions. This result suggests that interventions should be tailored according to the age of the patient and that early interventions might be particularly beneficial for improving social skills in children and adolescents with ASD. Moreover, individuals with higher cognitive abilities and improved verbal skills, as in our study, tend to derive more benefit from social skills training (Herbrecht et al., 2009; Solomon et al., 2004). From a clinical point of view, this could be because these people are better able to understand the concepts presented during the training and apply them in real social contexts. In addition, the more developed cognitive and verbal skills might facilitate communication and social interaction, reducing any barriers in active participation in the training and thus maximizing the results obtained. This suggests that intervention programs should be tailored to the individual's level of cognitive and verbal skills in order to maximize treatment effectiveness. Although our results are not significant the impact of sex on the effects of social skills training remains uncertain (Dean et al., 2023), further research with larger samples and more robust study designs may be needed to clarify the role of gender in response to social skills training and identify any significant differences that might exist between the sexes.
Regarding the duration of the intervention, which varied across studies, previous literature did not reach a consensus. Indeed, some studies found no correlation between intervention length and social improvement (Tyminski & Moore, 2008), while others observed greater increases in peer interactions with a greater number of intervention sessions (McMahon et al., 2013). Our meta-analysis did not establish a significant moderating effect on treatment outcome, although further research is needed to determine whether prolonged or more intensive interventions could yield more effects that are prominent. Guidance on this aspect is essential for service providers (Gates et al., 2017).
In summary, this meta-analysis demonstrated small-to-moderate effect size of experimental treatments over waiting list/control treatments across various outcomes, although caution is advised due to heterogeneity and publication bias in some analyses. Although interventions for ASD in children and adolescents have shown promise, further research should prioritize the development of Individual Participant Data (IPD) meta-analyses aimed at enhancing the personalized medicine approach, thereby customizing interventions to tackle the specific challenges encountered by adolescents with ASD (Cuijpers et al., 2022). In IPD meta-analyses, primary data from multiple trials are gathered, amalgamated into a comprehensive dataset, and subsequently collectively analyzed. This approach allows for an investigation into whether baseline patient characteristics are linked to therapy outcomes. Combining data from multiple trials significantly enhances statistical power, enabling a more thorough examination of outcome predictors and moderators.
Limitations
Our meta-analysis should be considered in light of some limitations of the included studies, as well as limitations of our own meta-analysis. In relation to the included studies, first, the significant heterogeneity in outcome instruments used across studies can pose challenges in directly comparing the results. Second, the presence of bias due to deviations of the included studies from intended interventions and outcome measurement can undermine the validity and interpretation of the results. It highlights the importance of adhering to rigorous study protocols and reporting guidelines to minimize these biases. Third, the limited adherence of most studies to reporting guidelines, such as CONSORT (Consolidated Standards of Reporting Trials), was a common issue in included studies. Reporting guidelines like CONSORT are designed to ensure transparency and completeness in the reporting of research studies, particularly clinical trials. When authors don't adhere to these guidelines, it can create several issues that affect both the quality and reliability of the research such as: Incomplete Information, Bias and Selective Reporting, Reproducibility and Replicability, Difficulty in Meta-Analysis and Ethical Considerations. In our work, the influence of this limitation may have been mainly in the interpretation and synthesis of the research results. Therefore, one has to be cautious about the potential impact of an incomplete report on the reliability and validity of the results. Furthermore, when drawing conclusions or making recommendations on the basis of the available evidence, it will be necessary to rely on additional sources or contexts to compensate for the shortcomings of the reports. Fourth, there was a lack of details on treatment fidelity and limited response from authors can limit the understanding of how interventions were implemented. Providing comprehensive details on treatment programs and ensuring treatment fidelity is crucial for evaluating the efficacy and replicability of interventions. Future studies should prioritize reporting on treatment fidelity and provide explicit information on the implementation process. Fifth, included studies relied mostly on waiting list control groups, which limits the ability to make direct comparisons between different interventions. Including control groups in future studies can provide valuable insights into the relative efficacy of different interventions. Sixth, the variability in terms of age of diagnosis and non-homogeneity of previous treatments may have influenced the outcome of subsequent treatments. Seventh, the potential impact of variability in the timing of diagnosis and initiation of social skills training on treatment outcomes was not consistently addressed in the original studies, warranting further consideration in future research discussions.
Finally, concerning our meta-analysis, due to budget issues we could not screen for studies in languages other than English. Moreover, even though we endeavored to gather unpublished information from study authors, this was not systematically provided.
Acknowledgments
We are deeply grateful to our colleagues for the ongoing discussions and invaluable contributions that have significantly influenced the development of this research. Our heartfelt thanks go to our patients and their families for their engaging in meaningful conversations about the importance of the interventions and their implementation. Their willingness to share their experiences and perspectives has been an inspiration for the realization of this study.
References
- Adams, D., Ambrose, K., Simpson, K., Malone, S., & Dargue, N. (2023). The relationshipbetween anxiety and social outcomes in autistic children and adolescents: A meta-analysis. Clinical child and family psychology review, 26(3), 706–720. 10.1007/s10567-023-00450-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). 10.1176/appi.books.9780890425787 [DOI]
- Ames, C. S., & Jarrold, C. (2009). Identifying symbolic relationships in autism spectrum disorders: a deficit in the identification of temporal co-occurrence?. Journal of autism and developmental disorders, 39(12), 1723–1734. 10.1007/s10803-009-0808-2 [DOI] [PubMed] [Google Scholar]
- Afsharnejad, B., Falkmer, M., Black, M. H., Alach, T., Lenhard, F., Fridell, A., Coco, C., Milne, K., Bölte, S., & Girdler, S. (2021). KONTAKT® social skills group training for Australian adolescents with autism spectrum disorder: a randomized controlled trial. European child & adolescent psychiatry, 31(11), 1695–1713. 10.1007/s00787-021-01814-6 [DOI] [PubMed] [Google Scholar]
- Afsharnejad, B., Black, M. H., Falkmer, M., Bölte, S., & Girdler, S. (2024). The Methodological Quality and Intervention Fidelity of Randomised Controlled Trials Evaluating Social Skills Group Programs in Autistic Adolescents: A Systematic Review and Meta-analysis. Journal of autism and developmental disorders, 54(4), 1281–1316. 10.1007/s10803-023-05893-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antshel, K. M., Polacek, C., McMahon, M., Dygert, K., Spenceley, L., Dygert, L., Miller, L., & Faisal, F. (2011). Comorbid ADHD and anxiety affect social skills group intervention treatment efficacy in children with autism spectrum disorders. Journal of developmental and behavioral pediatrics : JDBP, 32(6), 439–446. 10.1097/DBP.0b013e318222355d [DOI] [PubMed] [Google Scholar]
- Bauminger-Zviely, N., Eden, S., Zancanaro, M., Weiss, P. L., & Gal, E. (2013). Increasing social engagement in children with high-functioning autism spectrum disorder using collaborative technologies in the school environment. Autism : the international journal of research and practice, 17(3), 317–339. 10.1177/1362361312472989 [DOI] [PubMed] [Google Scholar]
- Beaumont, R., Walker, H., Weiss, J., & Sofronoff, K. (2021). Randomized Controlled Trial of a Video Gaming-Based Social Skills Program for Children on the Autism Spectrum. Journal of autism and developmental disorders, 51(10), 3637–3650. 10.1007/s10803-020-04801-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begeer, S., Howlin, P., Hoddenbach, E., Clauser, C., Lindauer, R., Clifford, P., Gevers, C., Boer, F., & Koot, H. M. (2015). Effects and Moderators of a Short Theory of Mind Intervention for Children with Autism Spectrum Disorder: A Randomized Controlled Trial. Autism research : official journal of the International Society for Autism Research, 8(6), 738–748. 10.1002/aur.1489 [DOI] [PubMed] [Google Scholar]
- Begg, C.B., & Mazumdar, M. (1994). Operating characteristics of a rank correlation test for publication bias. Biometrics, 50 4, 1088-101 . [PubMed] [Google Scholar]
- Bellini, S. (2006). Building social relationships: a systematic approach to teaching social interaction skills to children and adolescents with autism spectrum disorders and other social difficulties. Autism Asperger Publishing Company. [Google Scholar]
- Bent, C., Glencross, S., McKinnon, K., Hudry, K., Dissanayake, C., Victorian ASELCC Team, & Vivanti, G. (2023). Predictors of Developmental and Adaptive Behaviour Outcomes in Response to Early Intensive Behavioural Intervention and the Early Start Denver Model. Journal of autism and developmental disorders, 10.1007/s10803-023-05993-w. Advance online publication. 10.1007/s10803-023-05993-w [DOI] [PMC free article] [PubMed]
- Bifulco, A., Schimmenti, A., Jacobs, C., Bunn, A. and Rusu, A.C. (2014). Risk factors and psychological outcomes of bullying victimization: a community-based study. Child Indicators Research, 7, 633–648. 10.1007/s12187-014-9236-8. [DOI] [Google Scholar]
- Bucher, H. C., Guyatt, G. H., Griffith, L. E., & Walter, S. D. (1997). The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. Journal of clinical epidemiology, 50(6), 683–691. 10.1016/s0895-4356(97)00049-8 [DOI] [PubMed] [Google Scholar]
- Cappadocia, M.C., Weiss, J.A. (2011). Review of social skills training groups for youth with Asperger syndrome and high functioning autism. Research in Autism Spectrum Disorders, 5(1), 70–78. 10.1016/j.rasd.2010.04.001 [DOI] [Google Scholar]
- Choque Olsson, N., Flygare, O., Coco, C., Görling, A., Råde, A., Chen, Q., Lindstedt, K., Berggren, S., Serlachius, E., Jonsson, U., Tammimies, K., Kjellin, L., & Bölte, S. (2017). Social Skills Training for Children and Adolescents With Autism Spectrum Disorder: A Randomized Controlled Trial. Journal of the American Academy of Child and Adolescent Psychiatry, 56(7), 585–592. 10.1016/j.jaac.2017.05.001 [DOI] [PubMed] [Google Scholar]
- Corbett, B. A., Ioannou, S., Key, A. P., Coke, C., Muscatello, R., Vandekar, S., & Muse, I. (2019). Treatment Effects in Social Cognition and Behavior following a Theater-based Intervention for Youth with Autism. Developmental neuropsychology, 44(7), 481–494. 10.1080/87565641.2019.1676244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett, B. A., White, S., Lerner, M., Preacher, K. J., Klemencic, M. E., Simmons, G. L., Pilkington, J., Gable, P., Gioia, A., & Key, A. P. (2023). Peers, play, and performance to build social salience in autistic youth: A multisite randomized clinical trial. Journal of consulting and clinical psychology, 91(7), 411–425. 10.1037/ccp0000821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Côté, S. M., Larose, M. P., Geoffroy, M. C., Laurin, J., Vitaro, F., Tremblay, R. E., & Ouellet-Morin, I. (2017). Testing the impact of a social skill training versus waiting list control group for the reduction of disruptive behaviors and stress among preschool children in child care: the study protocol for a cluster randomized trial. BMC psychology, 5(1), 29. 10.1186/s40359-017-0197-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crasta, J. E., Green, O. J., Gavin, W. J., & Davies, P. L. (2023). The Relationship Between Attention, Sensory Processing, and Social Responsiveness Among Adults on the Autism Spectrum. Journal of autism and developmental disorders, 10.1007/s10803-023-06019-1. Advance online publication. 10.1007/s10803-023-06019-1 [DOI] [PubMed]
- Cresswell, L., & Cage, E. (2019). 'Who Am I?': An Exploratory Study of the Relationships Between Identity, Acculturation and Mental Health in Autistic Adolescents. Journal of autism and developmental disorders, 49(7), 2901–2912. 10.1007/s10803-019-04016-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers, P., Ciharova, M., Quero, S., Miguel, C., Driessen, E., Harrer, M., Purgato, M., Ebert, D., & Karyotaki, E. (2022). The Contribution of "Individual Participant Data" Meta-Analyses of Psychotherapies for Depression to the Development of Personalized Treatments: A Systematic Review. Journal of personalized medicine, 12(1), 93. 10.3390/jpm12010093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean, M., Williams, J., Orlich, F., & Kasari, C. (2020). Adolescents with autism spectrum disorder and social skills groups at school: A randomized trial comparing intervention environment and peer composition. School psychology review, 49(1), 60–73. 10.1080/2372966x.2020.1716636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean, M., Chang, Y. C., Shih, W., Orlich, F., & Kasari, C. (2023). Social engagement and loneliness in school-age autistic girls and boys. Women's health (London, England), 19, 17455057231170973. 10.1177/17455057231170973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Korte, M. W. P., van den Berk-Smeekens, I., Buitelaar, J. K., Staal, W. G., & van Dongen-Boomsma, M. (2021). Pivotal Response Treatment for School-Aged Children and Adolescents with Autism Spectrum Disorder: A Randomized Controlled Trial. Journal of autism and developmental disorders, 51(12), 4506–4519. 10.1007/s10803-021-04886-0 [DOI] [PubMed] [Google Scholar]
- Dekker, V., Nauta, M. H., Timmerman, M. E., Mulder, E. J., van der Veen-Mulders, L., van den Hoofdakker, B. J., van Warners, S., Vet, L. J. J., Hoekstra, P. J., & de Bildt, A. (2018). Social skills group training in children with autism spectrum disorder: a randomized controlled trial. European child & adolescent psychiatry, 28(3), 415–424. 10.1007/s00787-018-1205-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan, B. K., Van Hecke, A. V., Carson, A. M., Karst, J. S., Stevens, S., Schohl, K. A., Potts, S., Kahne, J., Linneman, N., Remmel, R., & Hummel, E. (2016). Brief Report: Assessment of Intervention Effects on In Vivo Peer Interactions in Adolescents with Autism Spectrum Disorder (ASD). Journal of autism and developmental disorders, 46(6), 2251–2259. 10.1007/s10803-016-2738-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger, M., Davey Smith, G., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed.), 315(7109), 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraioli, S. J., & Harris, S. L. (2011). Treatments to increase social awareness and social skills. Evidence-based practices and treatments for children with autism. Springer Science. [Google Scholar]
- Flynn, L., Healy, O. (2012). A review of treatments for deficits in social skills and self-help skills in autism spectrum disorder. Research in Autism Spectrum Disorders, 6, 431–441. 10.1016/j.rasd.2011.06.016 [DOI] [Google Scholar]
- Frankel, F., Myatt, R., & Feinberg, D. (2007). Parent-assisted friendship training for children with autism spectrum disorders: effects of psychotropic medication. Child psychiatry and human development, 37(4), 337–346. 10.1007/s10578-007-0053-x [DOI] [PubMed] [Google Scholar]
- Frankel, F., Myatt, R., Sugar, C., Whitham, C., Gorospe, C. M., & Laugeson, E. (2010). A randomized controlled study of parent-assisted Children's Friendship Training with children having autism spectrum disorders. Journal of autism and developmental disorders, 40(7), 827–842. 10.1007/s10803-009-0932-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye R. E. (2018). Social Skills Deficits in Autism Spectrum Disorder: Potential Biological Origins and Progress in Developing Therapeutic Agents. CNS drugs, 32(8), 713–734. 10.1007/s40263-018-0556-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabis, L. V., Gross, R., & Barbaro, J. (2021). Editorial: Personalized Precision Medicine in Autism Spectrum-Related Disorders. Frontiers in neurology, 12, 730852. 10.3389/fneur.2021.730852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates, J. A., Kang, E., & Lerner, M. D. (2017). Efficacy of group social skills interventions for youth with autism spectrum disorder: A systematic review and meta-analysis. Clinical psychology review, 52, 164–181. 10.1016/j.cpr.2017.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore, R., Ziviani, J., Chatfield, M. D., Goodman, S., & Sakzewski, L. (2022). Social skills group training in adolescents with disabilities: A systematic review. Research in developmental disabilities, 125, 104218. 10.1016/j.ridd.2022.104218 [DOI] [PubMed] [Google Scholar]
- Gosling, C. J., Cartigny, A., Mellier, B. C., Solanes, A., Radua, J., & Delorme, R. (2022). Efficacy of psychosocial interventions for Autism spectrum disorder: an umbrella review. Molecular psychiatry, 27(9), 3647–3656. 10.1038/s41380-022-01670-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu, S., Shi, J., Tang, Z., Sawhney, M., Hu, H., Shi, L., Fonseca, V., & Dong, H. (2015). Comparison of glucose lowering effect of metformin and acarbose in type 2 diabetes mellitus: a meta-analysis. PloS one, 10(5), e0126704. 10.1371/journal.pone.0126704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbrecht, E., Poustka, F., Birnkammer, S., Duketis, E., Schlitt, S., Schmötzer, G., & Bölte, S. (2009). Pilot evaluation of the Frankfurt Social Skills Training for children and adolescents with autism spectrum disorder. European child & adolescent psychiatry, 18(6), 327–335. 10.1007/s00787-008-0734-4 [DOI] [PubMed] [Google Scholar]
- Hopkins, I. M., Gower, M. W., Perez, T. A., Smith, D. S., Amthor, F. R., Wimsatt, F. C., & Biasini, F. J. (2011). Avatar assistant: improving social skills in students with an ASD through a computer-based intervention. Journal of autism and developmental disorders, 41(11), 1543–1555. 10.1007/s10803-011-1179-z [DOI] [PubMed] [Google Scholar]
- Hotton, M., & Coles, S. (2016). The Effectiveness of Social Skills Training Groups for Individuals with Autism Spectrum Disorder. Rev J Autism Dev Disord, 3, 68–81. 10.1007/s40489-015-0066-5 [DOI] [Google Scholar]
- Idris, S., van Pelt, B. J., Jagersma, G., Duvekot, J., Maras, A., van der Ende, J., van Haren, N., & Greaves-Lord, K. (2022). A randomized controlled trial to examine the effectiveness of the Dutch version of the Program for the Education and Enrichment of Relational Skills (PEERS®). BMC psychiatry, 22(1), 293. 10.1186/s12888-022-03913-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaat, A. J., & Lecavalier, L. (2015). Reliability and validity of parent- and child-rated anxiety measures in autism spectrum disorder. Journal of autism and developmental disorders, 45(10), 3219–3231. 10.1007/s10803-015-2481-y [DOI] [PubMed] [Google Scholar]
- Kasari, C., Rotheram-Fuller, E., Locke, J., & Gulsrud, A. (2012). Making the connection: randomized controlled trial of social skills at school for children with autism spectrum disorders. Journal of child psychology and psychiatry, and allied disciplines, 53(4), 431–439. 10.1111/j.1469-7610.2011.02493.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kedar, M., & Bauminger-Zviely, N. (2023). Predictors of individual differences in minimally verbal peer communication exchanges following peer-oriented social intervention. Autism research : official journal of the International Society for Autism Research, 16(1), 230–244. 10.1002/aur.2852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko, J. A., Miller, A. R., & Vernon, T. W. (2019). Social conversation skill improvements associated with the Social Tools And Rules for Teens program for adolescents with autism spectrum disorder: Results of a randomized controlled trial. Autism : the international journal of research and practice, 23(5), 1224–1235. 10.1177/1362361318808781 [DOI] [PubMed] [Google Scholar]
- Koegel, L. K., Koplen, Z., Koegel, B., & Koegel, R. L. (2021). Using a Question Bank Intervention to Improve Socially Initiated Questions in Adolescents and Adults With Autism. Journal of speech, language, and hearing research: JSLHR, 64(4), 1331–1339. 10.1044/2021_JSLHR-20-00534 [DOI] [PubMed] [Google Scholar]
- Langan, D., Higgins, J. P. T., Jackson, D., Bowden, J., Veroniki, A. A., Kontopantelis, E., Viechtbauer, W., & Simmonds, M. (2019). A comparison of heterogeneity variance estimators in simulated random-effects meta-analyses. Research synthesis methods, 10(1), 83–98. 10.1002/jrsm.1316 [DOI] [PubMed] [Google Scholar]
- Laugeson, E. A., Frankel, F., Mogil, C., & Dillon, A. R. (2009). Parent-assisted social skills training to improve friendships in teens with autism spectrum disorders. Journal of autism and developmental disorders, 39(4), 596–606. 10.1007/s10803-008-0664-5 [DOI] [PubMed] [Google Scholar]
- Laugeson, E. A., Frankel, F., Gantman, A., Dillon, A. R., & Mogil, C. (2012). Evidence-based social skills training for adolescents with autism spectrum disorders: the UCLA PEERS program. Journal of autism and developmental disorders, 42(6), 1025–1036. 10.1007/s10803-011-1339-1 [DOI] [PubMed] [Google Scholar]
- Linstead, E., Dixon, D. R., Hong, E., Burns, C. O., French, R., Novack, M. N., & Granpeesheh, D. (2017). An evaluation of the effects of intensity and duration on outcomes across treatment domains for children with autism spectrum disorder. Translational psychiatry, 7(9), e1234. 10.1038/tp.2017.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke, J., Rotheram-Fuller, E., & Kasari, C. (2012). Exploring the social impact of being a typical peer model for included children with autism spectrum disorder. Journal of autism and developmental disorders, 42(9), 1895–1905. 10.1007/s10803-011-1437-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopata, C., Thomeer, M. L., Volker, M. A., Toomey, J. A., Nida, R. E., Lee, G. K., Smerbeck, A. M., & Rodgers, J. D. (2010). RCT of a manualized social treatment for high-functioning autism spectrum disorders. Journal of autism and developmental disorders, 40(11), 1297–1310. 10.1007/s10803-010-0989-8 [DOI] [PubMed] [Google Scholar]
- Lopata, C., Thomeer, M. L., Rodgers, J. D., Donnelly, J. P., McDonald, C. A., Volker, M. A., Smith, T. H., & Wang, H. (2019). Cluster Randomized Trial of a School Intervention for Children with Autism Spectrum Disorder. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 48(6), 922–933. 10.1080/15374416.2018.1520121 [DOI] [PubMed] [Google Scholar]
- Lopata, C., Thomeer, M.L., Lipinski, A.M., Donnelly, J.P., Nelson, A.T., Smith, R.A., Booth, A.J., Rodgers, J.D., Volker, M.A. (2015). RCT examining the effect of treatment intensity for a psychosocial treatment for high-functioning children with ASD. Research in Autism Spectrum Disorders, 17, 52-63. 10.1016/j.rasd.2015.06.002 [DOI] [Google Scholar]
- Lord, C., Charman, T., Havdahl, A., Carbone, P., Anagnostou, E., Boyd, B., Carr, T., de Vries, P. J., Dissanayake, C., Divan, G., Freitag, C. M., Gotelli, M. M., Kasari, C., Knapp, M., Mundy, P., Plank, A., Scahill, L., Servili, C., Shattuck, P., Simonoff, E., … McCauley, J. B. (2022). The Lancet Commission on the future of care and clinical research in autism. Lancet (London, England), 399(10321), 271–334. 10.1016/S0140-6736(21)01541-5 [DOI] [PubMed] [Google Scholar]
- Luckhardt, C., Kröger, A., Elsuni, L., Cholemkery, H., Bender, S., & Freitag, C. M. (2018). Facilitation of biological motion processing by group-based autism specific social skills training. Autism research : official journal of the International Society for Autism Research, 11(10), 1376–1387. 10.1002/aur.2013 [DOI] [PubMed] [Google Scholar]
- Lupi, E., Tucci, F., Casula, L., Novello, R. L., Guerrera, S., Vicari, S., & Valeri, G. (2023). Early and stable difficulties of everyday executive functions predict autism symptoms and emotional/ behavioral problems in preschool age children with autism: a 2-year longitudinal study. Frontiers in psychology, 14, 1092164. 10.3389/fpsyg.2023.1092164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma, W., Mao, J., Xie, Y., Li, S., & Wang, M. (2023). Examining the Effects of Theory of Mind and Social Skills Training on Social Competence in Adolescents with Autism. Behavioral sciences (Basel, Switzerland), 13(10), 860. 10.3390/bs13100860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathur, S. R., Kavale, K. A., Quinn, M. M., Forness, S. R., & Rutherford, R. B. (1998). Social Skills Interventions with Students with Emotional and Behavioral Problems: A Quantitative Synthesis of Single-Subject Research. Behavioral Disorders, 23(3), 193–201. http://www.jstor.org/stable/23888718 [Google Scholar]
- McMahon, C. M., Lerner, M. D., & Britton, N. (2013). Group-based social skills interventions for adolescents with higher-functioning autism spectrum disorder: a review and looking to the future. Adolescent health, medicine and therapeutics, 2013(4), 23–28. 10.2147/AHMT.S25402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirzaei, S. S., Pakdaman, S., Alizadeh, E., & Pouretemad, H. (2020). A systematic review of program circumstances in training social skills to adolescents with high-functioning autism. International journal of developmental disabilities, 68(3), 237–246. 10.1080/20473869.2020.1748802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narzisi, A. (2015). Adults with Autism Spectrum Disorders: Research is the Future. Autism Open Access, 5, (3). 10.4172/2165-7890.1000149 [DOI] [Google Scholar]
- Narzisi, A., & Stavropoulos, K. K. M. (2022). Editorial: Enrichment of social skills in adolescent and young adults with high-functioning autism spectrum disorder. Frontiers in psychiatry, 13, 994914. 10.3389/fpsyt.2022.994914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narzisi, A., Fabbri-Destro, M., Crifaci, G., Scatigna, S., Maugeri, F., Berloffa, S., Fantozzi, P., Prato, A., Muccio, R., Valente, E., Viglione, V., Pecchini, E., Pelagatti, S., Rizzo, R., Milone, A., Barone, R., & Masi, G. (2022). Sensory Profiles in School-Aged Children with Autism Spectrum Disorder: A Descriptive Study Using the Sensory Processing Measure-2 (SPM-2). Journal of clinical medicine, 11(6), 1668. 10.3390/jcm11061668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh, M., Laugeson, E., Kim, J. H., Lee, K., Kim, J., Lee, S., Lim, B., Cha, S., Bong, G., Yoon, N. H., Bahn, G. H., & Yoo, H. J. (2021). A Randomized Controlled Trial of the Korean Version of the Program for the Education and Enrichment of Relational Skills for Young Adults (PEERS®-YA-K) With Autism Spectrum Disorder: A Pilot Study. Frontiers in psychiatry, 12, 730448. 10.3389/fpsyt.2021.730448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens, G., Granader, Y., Humphrey, A., & Baron-Cohen, S. (2008). LEGO therapy and the social use of language programme: an evaluation of two social skills interventions for children with high functioning autism and Asperger Syndrome. Journal of autism and developmental disorders, 38(10), 1944–1957. 10.1007/s10803-008-0590-6 [DOI] [PubMed] [Google Scholar]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., McGuinness, L. A., … Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical research ed.), 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellecchia, M., Connell, J. E., Kerns, C. M., Xie, M., Marcus, S. C., & Mandell, D. S. (2016). Child characteristics associated with outcome for children with autism in a school-based behavioral intervention. Autism : the international journal of research and practice, 20(3), 321–329. 10.1177/1362361315577518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Płatos, M., Wojaczek, K., & Laugeson, E. A. (2022). Effects of Social Skills Training for Adolescents on the Autism Spectrum: a Randomized Controlled Trial of the Polish Adaptation of the PEERS® Intervention via Hybrid and In-Person Delivery. Journal of autism and developmental disorders, 53(11), 4132–4146. 10.1007/s10803-022-05714-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabin, S. J., Israel-Yaacov, S., Laugeson, E. A., Mor-Snir, I., & Golan, O. (2018). A randomized controlled trial evaluating the Hebrew adaptation of the PEERS® intervention: Behavioral and questionnaire-based outcomes. Autism research : official journal of the International Society for Autism Research, 11(8), 1187–1200. 10.1002/aur.1974 [DOI] [PubMed] [Google Scholar]
- Rao, P. A., Beidel, D. C., & Murray, M. J. (2008). Social skills interventions for children with Asperger's syndrome or high-functioning autism: a review and recommendations. Journal of autism and developmental disorders, 38(2), 353–361. 10.1007/s10803-007-0402-4 [DOI] [PubMed] [Google Scholar]
- R Core Team (2020). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna. [Google Scholar]
- Reichow, B., & Volkmar, F. R. (2010). Social skills interventions for individuals with autism: evaluation for evidence-based practices within a best evidence synthesis framework. Journal of autism and developmental disorders, 40(2), 149–166. 10.1007/s10803-009-0842-0 [DOI] [PubMed] [Google Scholar]
- Rispoli, K. M., Lee, G. K., Nathanson, E. W., & Malcolm, A. L. (2019). The parent role in school-based teams for adolescents with autism spectrum disorder. School psychology (Washington, D.C.), 34(4), 458–467. 10.1037/spq0000289 [DOI] [PubMed] [Google Scholar]
- Roberts, J. M. A., Adams, D., Heussler, H., Keen, D., Paynter, J., Trembath, D., Westerveld, M., & Williams, K. (2018). Protocol for a prospective longitudinal study investigating the participation and educational trajectories of Australian students with autism. BMJ open, 8(1), e017082. 10.1136/bmjopen-2017-017082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosello, R., Martinez-Raga, J., Tomas, J. M., Rosello, B., Berenguer, C., & Cortese, S. (2023). Exploring developmental trajectories throughout adolescence of children with autism spectrum disorder without intellectual disability. Journal of neural transmission (Vienna, Austria : 1996), 130(3), 299–312. 10.1007/s00702-022-02554-w [DOI] [PubMed] [Google Scholar]
- Schiltz, H. K., McVey, A. J., Dolan, B. K., Willar, K. S., Pleiss, S., Karst, J. S., Carson, A. M., Caiozzo, C., Vogt, E. M., Yund, B. D., & Van Hecke, A. V. (2018). Changes in Depressive Symptoms Among Adolescents with ASD Completing the PEERS® Social Skills Intervention. Journal of autism and developmental disorders, 48(3), 834–843. 10.1007/s10803-017-3396-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schohl, K. A., Van Hecke, A. V., Carson, A. M., Dolan, B., Karst, J., & Stevens, S. (2014). A replication and extension of the PEERS intervention: examining effects on social skills and social anxiety in adolescents with autism spectrum disorders. Journal of autism and developmental disorders, 44(3), 532–545. 10.1007/s10803-013-1900-1 [DOI] [PubMed] [Google Scholar]
- Shum, K. K., Cho, W. K., Lam, L. M. O., Laugeson, E. A., Wong, W. S., & Law, L. S. K. (2019). Learning How to Make Friends for Chinese Adolescents with Autism Spectrum Disorder: A Randomized Controlled Trial of the Hong Kong Chinese Version of the PEERS® Intervention. Journal of autism and developmental disorders, 49(2), 527–541. 10.1007/s10803-018-3728-1 [DOI] [PubMed] [Google Scholar]
- Soares, E. E., Bausback, K., Beard, C. L., Higinbotham, M., Bunge, E. L., & Gengoux, G. W. (2021). Social Skills Training for Autism Spectrum Disorder: a Meta-analysis of In-person and Technological Interventions. Journal of technology in behavioral science, 6(1), 166–180. 10.1007/s41347-020-00177-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon, M., Goodlin-Jones, B. L., & Anders, T. F. (2004). A social adjustment enhancement intervention for high functioning autism, Asperger's syndrome, and pervasive developmental disorder NOS. Journal of autism and developmental disorders, 34(6), 649–668. 10.1007/s10803-004-5286-y [DOI] [PubMed] [Google Scholar]
- Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H. Y., Corbett, M. S., Eldridge, S. M., Emberson, J. R., Hernán, M. A., Hopewell, S., Hróbjartsson, A., Junqueira, D. R., Jüni, P., Kirkham, J. J., Lasserson, T., Li, T., McAleenan, A., … Higgins, J. P. T. (2019). RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed.), 366, l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- Storch, E. A., Wood, J. J., Guzick, A. G., Small, B. J., Kerns, C. M., Ordaz, D. L., Schneider, S. C., & Kendall, P. C. (2022). Moderators of Response to Personalized and Standard Care Cognitive-Behavioral Therapy for Youth with Autism Spectrum Disorder and Comorbid Anxiety. Journal of autism and developmental disorders, 52(2), 950–958. 10.1007/s10803-021-05000-0 [DOI] [PubMed] [Google Scholar]
- Storch, E. A., Ehrenreich May, J., Wood, J. J., Jones, A. M., De Nadai, A. S., Lewin, A. B., Arnold, E. B., & Murphy, T. K. (2012). Multiple informant agreement on the anxiety disorders interview schedule in youth with autism spectrum disorders. Journal of child and adolescent psychopharmacology, 22(4), 292–299. 10.1089/cap.2011.0114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strang, J. F., Kenworthy, L., Daniolos, P., Case, L., Wills, M. C., Martin, A., & Wallace, G. L. (2012). Depression and Anxiety Symptoms in Children and Adolescents with Autism Spectrum Disorders without Intellectual Disability. Research in autism spectrum disorders, 6(1), 406–412. 10.1016/j.rasd.2011.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomeer, M. L., Lopata, C., Donnelly, J. P., Booth, A., Shanahan, A., Federiconi, V., McDonald, C. A., & Rodgers, J. D. (2019). Community Effectiveness RCT of a Comprehensive Psychosocial Treatment for High-Functioning Children With ASD. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 48(sup1), S119–S130. 10.1080/15374416.2016.1247359 [DOI] [PubMed] [Google Scholar]
- Tomaszewski, B., Kraemer, B., Steinbrenner, J. R., Smith DaWalt, L., Hall, L. J., Hume, K., & Odom, S. (2020). Student, Educator, and Parent Perspectives of Self-Determination in High School Students with Autism Spectrum Disorder. Autism research : official journal of the International Society for Autism Research, 13(12), 2164–2176. 10.1002/aur.2337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyminski, R. F., & Moore, P. J. (2008). The impact of group psychotherapy on social development in children with pervasive developmental disorders. International journal of group psychotherapy, 58(3), 363–379. 10.1521/ijgp.2008.58.3.363 [DOI] [PubMed] [Google Scholar]
- Van de Laar, F. A., Lucassen, P. L., Akkermans, R. P., Van de Lisdonk, E. H., Rutten, G. E., & Van Weel, C. (2005). Alpha-glucosidase inhibitors for type 2 diabetes mellitus. The Cochrane database of systematic reviews, 2005(2), CD003639. 10.1002/14651858.CD003639.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Cruijsen, R., Begeer, S., & Crone, E. A. (2024). The role of autism and alexithymia traits in behavioral and neural indicators of self-concept and self-esteem in adolescence. Autism : the international journal of research and practice, 13623613241232860. Advance online publication. 10.1177/13623613241232860 [DOI] [PMC free article] [PubMed]
- Vernon, W.T., Miller, A.R., Ko, J.A., Barrett, A.C., & McGarry, E.S. (2018). A Randomized Controlled Trial of the Social Tools And Rules for Teens (START) Program: An Immersive Socialization Intervention for Adolescents with Autism Spectrum Disorder. Journal of autism and developmental disorders, 48(3), 892–904. 10.1007/s10803-017-3380-1 [DOI] [PubMed] [Google Scholar]
- Viechtbauer, W. (2010). Conducting Meta-Analyses in R with the metafor Package. Journal of Statistical Software, 36(3), 1–48. 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- White, S.W, Keonig, K., & Scahill, L. (2007). Social skills development in children with autism spectrum disorders: a review of the intervention research. Journal of autism and developmental disorders, 37(10), 1858–1868. 10.1007/s10803-006-0320-x [DOI] [PubMed] [Google Scholar]
- White, S. W., Ollendick, T., Albano, A. M., Oswald, D., Johnson, C., Southam-Gerow, M. A., Kim, I., & Scahill, L. (2013). Randomized controlled trial: Multimodal Anxiety and Social Skill Intervention for adolescents with autism spectrum disorder. Journal of autism and developmental disorders, 43(2), 382–394. 10.1007/s10803-012-1577-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolstencroft, J., Robinson, L., Srinivasan, R., Kerry, E., Mandy, W., & Skuse, D. (2018). A Systematic Review of Group Social Skills Interventions, and Meta-analysis of Outcomes, for Children with High Functioning ASD. Journal of autism and developmental disorders, 48(7), 2293–2307. 10.1007/s10803-018-3485-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, B., Kingsley, E., Cooper, C., Biggs, K., Bursnall, M., Wang, H. I., Chater, T., Coates, E., Teare, M. D., McKendrick, K., Gomez de la Cuesta, G., Barr, A., Solaiman, K., Packham, A., Marshall, D., Varley, D., Nekooi, R., Parrott, S., Ali, S., Gilbody, S., … Le Couteur, A. (2023). I-SOCIALISE: Results from a cluster randomised controlled trial investigating the social competence and isolation of children with autism taking part in LEGO® based therapy ('Play Brick Therapy') clubs in school environments. Autism: the international journal of research and practice, 27(8), 13623613231159699. Advance online publication. 10.1177/13623613231159699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo, H. J., Bahn, G., Cho, I. H., Kim, E. K., Kim, J. H., Min, J. W., Lee, W. H., Seo, J. S., Jun, S. S., Bong, G., Cho, S., Shin, M. S., Kim, B. N., Kim, J. W., Park, S., & Laugeson, E. A. (2014). A randomized controlled trial of the Korean version of the PEERS(®) parent-assisted social skills training program for teens with ASD. Autism research : official journal of the International Society for Autism Research, 7(1), 145–161. 10.1002/aur.1354 [DOI] [PubMed] [Google Scholar]
- You, X. R., Gong, X. R., Guo, M. R., & Ma, B. X. (2024). Cognitive behavioural therapy to improve social skills in children and adolescents with autism spectrum disorder: A meta-analysis of randomised controlled trials. Journal of affective disorders, 344, 8–17. 10.1016/j.jad.2023.10.008 [DOI] [PubMed] [Google Scholar]