Prolapse (from the Latin prolapsus, a slipping forth) refers to the falling or slipping out of place of a part or viscus. Pelvic organ prolapse is descent of the pelvic organs into the vagina, often accompanied by urinary, bowel, sexual, or local pelvic symptoms. The incidence of genital prolapse is difficult to determine, as many women do not seek medical advice. It has been estimated that a half of parous women lose pelvic floor support, resulting in some degree of prolapse, and that of these women 10-20% seek medical care.1 In the United Kingdom genital prolapse accounts for 20% of women on the waiting list for major gynaecological surgery.2 The incidence of prolapse requiring surgical correction in women who have had a hysterectomy is 3.6 per 1000 person years of risk; the cumulative risk is 1% at 3 years and 5% at 17 years after a hysterectomy.3 The chance of a woman having a prolapse increases with age.4 Therefore, the incidence of prolapse will rise as life expectancy increases. This article deals with the management in primary care of women with genital prolapse and the options in secondary care.
Summary points
Doctors should consider the patient's history of rectal prolapse, bladder and bowel function, and sexual activity
It is important to treat predisposing factors such as obesity, obstructive airway disease, constipation, and pelvic masses
Although prolapse can occur in the anterior, middle, or posterior compartments, the pelvic floor should be considered as a single unit in the treatment of prolapse
When surgery is needed, doctors should check for potential stress incontinence
There is a lack of good data on the prevention and treatment of prolapse, and in particular more research is needed on the role of pelvic floor exercises and on the pros and cons of vaginal, abdominal, and laparoscopic routes of surgery
Methods
We searched Medline (1966 to 2001), using the key words “genital prolapse,” “prevention,” and “treatment.” We then hand searched the results for further citations. We also referred to textbooks and drew from personal experience.
Symptoms and signs
Prolapse is often asymptomatic and an incidental finding, and clinical examination may not necessarily correlate with symptoms.5 Prolapses can occur in the anterior, middle, or posterior compartment of the pelvis:
Anterior compartment—prolapse into the vagina of the urethra (urethrocele) or bladder (cystocele) or both (cystourethrocele)
Middle compartment—uterine or vault descent and enterocele (herniation of the pouch of Douglas)
Posterior compartment—prolapse of the rectum into the vagina (rectocele).
Enteroceles may contain small bowel and omentum. Cystourethrocele is the most common type of prolapse, followed by uterine descent and then rectocele. Urethroceles are rare. Traditionally uterine descent is graded as 1st degree (within the vagina), 2nd degree (descent to the introitus), or 3rd degree (descent outside the introitus).
Symptoms are often related to the site and type of prolapse (box B1). Symptoms common to all types of prolapse are a feeling of dragging, or a lump in the vagina, or something coming down. (See boxes B2 and B3 for a summary of the evidence on the causes and prevention of genital prolapse.)
Box 1.
Symptoms associated with genital prolapse
Box 2.
Causes and contributing factors
Box 3.
Prevention
- Few large prospective trials have assessed the prevention of prolapse
- The role of obstetric risk factors is unclear—reduced duration of the second stage of labour, decreased use of instrumental deliveries, and episiotomies may help prevent prolapse in the long term
- Treatment of conditions that increase intra-abdominal pressure such as constipation, obstructive airway disease, chronic cough, and obesity are primary and secondary prevention strategies
- The role of hormone replacement therapy in preventing prolapse is uncertain
- Pelvic floor exercises after childbirth may help, though this has not been proved
- Concomitant procedures at the time of hysterectomy, such as closure of the pouch of Douglas with a Moschcowitz's procedure or uterosacral plication, may reduce the incidence of prolapse
Doctors or clinicians should examine the patient—who should be in the left lateral or standing position—with a Sims' speculum, inserting it along the posterior vaginal wall to assess the anterior wall and vault and vice versa. Uterine descent can be assessed by traction with a single toothed vulsellum. A cervix that protrudes outside the vagina may be ulcerated and hypertrophied.
Investigations
When urinary symptoms are present, a mid-stream specimen of urine must be sent for culture and sensitivity analysis before any investigations.
Urodynamic studies
Cystometry and uroflowmetry are recommended in women with genital prolapse to evaluate potential stress incontinence, other overt urinary incontinence, and emptying phase dysfunction. Potential stress incontinence may be masked by prolapse, so urodynamic studies should occur before any surgery. If the studies show stress incontinence, a continence procedure can be combined with pelvic floor reconstruction. However, opinions vary—some doctors counsel women before the operation for prolapse and perform a continence procedure later.6
Imaging
When the symptoms and signs of prolapse do not correlate—for example, when the patient complains of sensation of prolapse but a prolapse is not discernible on examination—pelvic fluoroscopy with barium contrast in the vagina, bladder, small bowel, and rectum may help.7
Treatment
Conservative treatment
Conservative treatment should always be offered before referral to hospital.
Pelvic floor exercises
Pelvic floor exercises may limit the progression of mild prolapse and alleviate mild prolapse symptoms such as low back ache and pelvic pressure.8 However, they are not useful if the prolapse extends to or beyond the vaginal introitus.9
Pessaries
For many years pessaries have been used to treat prolapse, although their use has decreased with advances in anaesthesia and surgical techniques. The main indications are:
Patients unfit for, awaiting, or who have declined surgery
Women who may yet bear children
In the management of prolapse in neonates, which can occur in conjunction with neural tube defects.10
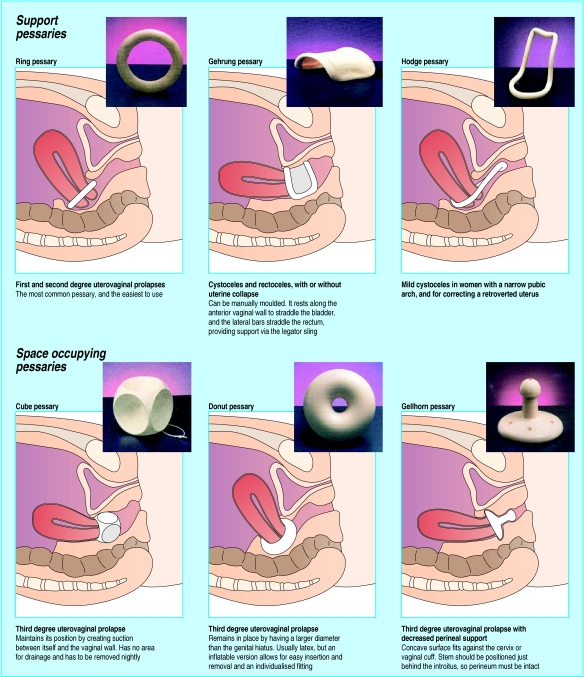
Pessaries are available in a variety of sizes and shapes to suit different patients and are of two main types: support pessaries, which rest under the symphysis and sacrum and elevate the vagina, and space occupying pessaries (fig 1).11
Figure 1.
Types of pessaries
Fitting and managing pessaries
Patients must be evaluated carefully before pessary placement. All treatment options should be discussed, and the patient should be an active participant in the treatment decision. Women must be capable of managing use of the pessary, either alone or with the help of a carer. Women with compromised eyesight or motor abilities may not be able to manage a pessary that requires self insertion and care.
Doctors do a bimanual examination and use the forefinger to estimate the size of the vagina. Sometimes trial and error may be the only way to determine which size of pessary should be used, and doctors should maintain a variety of sizes and styles. The pessary is placed in the vagina and the woman encouraged to walk around. If the woman reports pain or discomfort the pessary is likely to be too big, and a smaller one should be tried. She should be advised to return in a month's time for a check, but cautioned that if she experiences pain or difficulty in voiding she should return earlier.
If there are no adverse symptoms such as discharge, pain, or bleeding, the pessary can be changed every 9-12 months. If atrophy occurs, topical oestrogen cream should be applied twice a week and the pessary changed more often. Though uncommon, erosion or ulceration can occur with atrophic change in the vagina. The pessary should be removed and oestrogen cream applied until the ulcer has healed, when the pessary may be replaced. If the ulcer looks suspicious or does not heal, a biopsy may be indicated. Patients with a decubitus ulcer and a complete procidentia may need hospitalisation and vaginal packing with oestrogen cream.
When adequate follow up cannot be assured a pessary should not be used, as neglected pessaries can become impacted within the vagina and, rarely, ulcerate into the bladder or bowel. All patients should have a regular cervical smear test, according to the national programme.
There is a lack of good data on the indications for different types of pessary, who should change the pessary, how often pessaries should be changed, and whether pessaries should be used concurrently with hormone replacement therapy or pelvic floor exercises.12 Some women, particularly elderly women, find it less embarrassing and stressful to visit their general practitioner or practice nurse to change a pessary than return to the specialist. No data have been published on the effect of pessaries on sexual function. However, we would expect a space occupying pessary to produce some barrier to coitus.
Surgical treatment
The lifetime risk of undergoing an operation for prolapse or incontinence by the age of 80 years is 11%,4 but this probably grossly underestimates the true figure. Reoperation is required in 29% of cases, and the time interval reduces between each successive operation.4
The indications for surgery are:
Failure of pessary
Patients who want definitive treatment
Prolapse combined with urethral sphincter incompetence or faecal incontinence.
The aims of surgical correction of prolapse are relief of symptoms, restoration of normal vaginal anatomy, and preservation of coitus and urinary and anal continence. Injury after childbirth usually involves all the pelvic floor and pelvic organ supports, although sometimes only one organ may prolapse. When more than one compartment is involved, a combination of procedures may be needed. Often urinary incontinence is overt, or it is potential and is masked by prolapse and may be precipitated by surgery, for example sacrocolpopexy. Some operations—for example, colposuspension for a cystourethrocele—may predispose to a prolapse in another compartment.13
Operations can be classified by compartment and by approach (table). It is important to enquire whether the woman is sexually active before considering vaginal surgery, as this may alter the choice of surgery. Other factors that influence choice of surgery are the fitness of the patient and surgeon's preference. There is a lack of data on pregnancy outcomes and childbirth after prolapse surgery. If the prolapse remains corrected and the patient conceives, an elective caesarean section may be advisable. Generally women should avoid heavy lifting after surgery and avoid sexual intercourse for 6-8 weeks.
Operations in the anterior compartment
Anterior colporrhaphy
This operation rectifies a cystourethrocele. Mesh may be placed in the anterior wall of the vagina for additional support when a previous repair has failed. The operation is no longer the first treatment of choice for major urethral sphincter incompetence; instead tension free vaginal tape (TVT) (Gynecare, Ethicon, Somerville, NJ) may be inserted with an anterior repair. Intraoperative complications are uncommon, though haemorrhage, haematoma, and cystotomy may occur. The main postoperative problems are difficulty in voiding and recurrence of the prolapse.14
Colposuspension
Colposuspension is indicated for urethral sphincter incontinence associated with a 2nd or 3rd degree cystourethrocele. The paravaginal fascia on either side of the bladder neck and the base of the bladder are approximated to the pelvic side wall by sutures placed through the ipsilateral iliopectineal ligament.
Operations in the middle compartment
Operations for uterine prolapse
Vaginal hysterectomy (rather than Manchester repair) is now the treatment of choice for uterine prolapse. This can be combined with an anterior or posterior repair (or both) if a cystocele or rectocele is present.
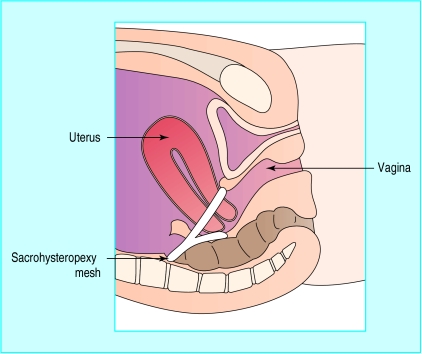
A sacrohysteropexy can be performed on women who wish to retain their uterus. Indications for sacrohysteropexy include failure of conservative treatment in a healthy, young nulliparous woman, a congenital anomaly (such as bladder exstrophy), women who wish to continue to bear children, and women who refuse a hysterectomy. It involves attaching the uterus to the anterior longitudinal ligament over the sacrum with a Y shaped graft (fig 2).15
Figure 2.
Sagittal section of the pelvis showing sacrohysteropexy mesh in place between the junction of the cervix and uterus and the anterior longitudinal ligament over the first sacral vertebra
Operations for vault prolapse and enterocele
Vaginal surgery has the advantage that no abdominal incision is needed, thereby reducing pain and hospital stay. The choice is between sacrospinous fixation, iliococcygeal hitch, and pubocervical rectovaginal fascia repair. Sacrospinous fixation involves unilateral or bilateral fixation of the vault to the sacrospinous ligament but can be complicated by injury to the pudendal nerve and vessels.16 In iliococcygeal hitch the vaginal vault is suspended bilaterally to the fascia of the iliococcygeus muscle, just anterior to the ischial spine.17
In abdominal or laparoscopic sacrocolpopexy the vaginal vault is attached by a mesh to the longitudinal ligament over the sacrum. The advantage of the laparoscopic approach is that hospitalisation is shorter. However, prospective randomised studies are lacking, and the role of the laparoscope needs to be defined.18 Abdominal sacrocolpopexy has a cure rate of 90%, and its main complications are intraoperative haemorrhage and a 3.3% risk of mesh erosion.19–21
Operations in the posterior compartment
A rectocele can be repaired by levator plication or by repair of discrete fascial defects. When surgery for prolapse has been done before, a mesh may be placed in the posterior vaginal wall for additional support. The main problem with levator plication is dyspareunia, which is attributed to atrophy of the muscle fibres and subsequent scarring.22 A retrospective analysis found that sexual dysfunction increased from 18% of patients preoperatively to 27% postoperatively.23 Recently there has been a renewed interest in the repair of isolated defects in the fascia. A prospective study found relief of dyspareunia in 92% of cases after rectovaginal reattachment for repair of rectocele.24
Additional educational resources
Selected texts
Bump RC, Cundiff GW. Pelvic organ prolapse. In: Stanton SL, Monga AK, eds. Clinical urogynaecology. London: Churchill Livingstone, 2001.
Cardozo L. Prolapse. In: Whitfield CR, ed. Dewhurst's textbook of obstetrics and gynaecology for postgraduates. Oxford: Blackwell Science, 1995.
Swift S, Theofrastous J. Aetiology and classification of pelvic organ prolapse. In: Cardozo L, Staskin D, eds. Textbook of urology and urogynaecology. London: Isis Medical Media, 2001.
BMJ archive
Jackson S, Smith P. Diagnosing and managing genitourinary prolapse. BMJ 1997;314:875-80.
Information for patients
Surgerydoor (www.surgerydoor.co.uk) Provides information on over 400 medical conditions, including vaginal prolapse.
Frequently Asked Questions on Women's Health (www.2womenshealth.co.uk) This illustrated e-book provides answers to frequently asked questions on women's health.
Continence Foundation (www.continence-foundation.org.uk) Provides information and advice, to patients and professionals, on bladder and bowel problems
The advantages of multidisciplinary care
For many years gynaecologists have been solely responsible for treating prolapse, but now the focus is on treating the pelvis as a whole rather than as three different compartments managed by urologists, gynaecologists, and colorectal surgeons. Thus patients with complex problems can be referred to a specialised clinic, run by surgeons experienced in all three fields, for a single examination and consultation. The advantage of this approach is shown by a recent audit of such a pelvic floor clinic, in which 20% of patients required combined procedures and avoided the anaesthetic risk and recuperative time of two procedures.25
Table.
Operations for prolapse
| Compartment | Vaginal route | Suprapubic route |
|---|---|---|
| Anterior | Anterior repair with or without mesh; paravaginal | Colposuspension; paravaginal |
| Middle | Vaginal hysterectomy; vault repair (fascia); sacrospinous fixation; bilateral iliococcygeal hitch | Sacrohysteropexy; sacrocolpopexy |
| Posterior | Levator plication; fascial repair with or without mesh; transanal repair | Mesh interposition;sacrocolpopexy with mesh interposition |
Footnotes
Competing interests: None declared.
References
- 1.Beck RP. Pelvic relaxation prolapse. In: Kase NG, Weingold AB, editors. Principles and practice of clinical gynecology. New York: John Wiley; 1983. pp. 677–685. [Google Scholar]
- 2.Cardozo L. Prolapse. In: Whitfield CR, editor. Dewhurst's textbook of obstetrics and gynaecology for postgraduates. Oxford: Blackwell Science; 1995. pp. 642–652. [Google Scholar]
- 3.Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. Br J Obstet Gynaecol. 1997;104:579–585. doi: 10.1111/j.1471-0528.1997.tb11536.x. [DOI] [PubMed] [Google Scholar]
- 4.Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–506. doi: 10.1016/S0029-7844(97)00058-6. [DOI] [PubMed] [Google Scholar]
- 5.Samuelsson EC, Arne V, Tibblin G, Svardsudd KF. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol. 1999;180:299–305. doi: 10.1016/s0002-9378(99)70203-6. [DOI] [PubMed] [Google Scholar]
- 6.Bump RC, Cundiff GW. Pelvic organ prolapse. In: Stanton SL, Monga AK, editors. Clinical urogynaecology. London: Churchill Livingstone; 2000. [Google Scholar]
- 7.Altringer WE, Saclarides TJ, Dominguez JM, Brubaker LT, Smith CS. Four-contrast defecography: pelvic “floor-oscopy.”. Dis Colon Rectum. 1995;38:695–699. doi: 10.1007/BF02048024. [DOI] [PubMed] [Google Scholar]
- 8.Davilla GW, Bernier F. Multimodality pelvic physiotherapy treatment of urinary incontinence in adult women. Int Urogynecol J. 1995;6:187–194. [Google Scholar]
- 9.Davilla GW. Vaginal prolapse: management with nonsurgical techniques. Postgrad Med. 1996;99:171–185. [PubMed] [Google Scholar]
- 10.De Mola J, Carpenter S. Management of genital prolapse in neonates and young women. Obstet Gynecol Surv. 1996;51:253–260. doi: 10.1097/00006254-199604000-00022. [DOI] [PubMed] [Google Scholar]
- 11.Pott-Grinstein E, Newcomer JR. Gynecolgist's patterns of prescribing pessaries. J Reprod Med. 2001;46:205–208. [PubMed] [Google Scholar]
- 12.Cundiff GW, Weidner AC, Visco AG, Bump RC, Addison WA. A survey of pessary use by members of the American urogynecologic society. Obstet Gynecol. 2000;95:931–935. doi: 10.1016/s0029-7844(00)00788-2. [DOI] [PubMed] [Google Scholar]
- 13.Wiskind AK, Creighton SM, Stanton SL. The incidence of genital prolapse after the Burch colposuspension. Am J Obstet Gynecol. 1992;167:395–399. doi: 10.1016/s0002-9378(11)91419-7. [DOI] [PubMed] [Google Scholar]
- 14.Webber AW. Surgical correction of anterior vaginal wall prolapse. In: Walters MD, Karram MM, editors. Urogynecology and reconstructive surgery. 2nd ed. Toronto: Mosby; 2000. pp. 211–219. [Google Scholar]
- 15.Leron E, Stanton SL. Sacrohysteropexy with synthetic mesh for management of uterovaginal prolapse. Br J Obstet Gynaecol. 2001;108:629–630. doi: 10.1111/j.1471-0528.2001.00138.x. [DOI] [PubMed] [Google Scholar]
- 16.Nichols DH, Milley PS, Randall CL. Significance of restoration of normal vaginal depth and axis. Obstet Gynecol. 1970;36:251–256. [PubMed] [Google Scholar]
- 17.Shull BL, Capen CV, Riggs MW, Kuehl TJ. Bilateral attachment of the vaginal cuff to iliococcygeus fascia: an effective method of cuff suspension. Am J Obstet Gynecol. 1993;168:1669–1674. doi: 10.1016/0002-9378(93)90676-a. [DOI] [PubMed] [Google Scholar]
- 18.Jackson S, Smith P. Diagnosing and managing genitourinary prolapse. BMJ. 1997;314:875–880. doi: 10.1136/bmj.314.7084.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Timmons MC, Addison WA, Addison SB, Cavenar MG. Abdominal sacral colpopexy in 163 women with posthysterectomy vaginal vault prolapse and enterocele. Evolution of operative techniques. J Reprod Med. 1992;37:323–327. [PubMed] [Google Scholar]
- 20.Fox SD, Stanton SL. Vault prolapse and rectocele: assessment of repair using sacrocolpopexy with mesh interposition. Br J Obstet Gynaecol. 2000;107:1371–1375. doi: 10.1111/j.1471-0528.2000.tb11650.x. [DOI] [PubMed] [Google Scholar]
- 21.Timmons MC, Addison WA. Mesh erosion after abdominal sacral colpopexy. J Pelvic Surg. 1997;3:75–80. [Google Scholar]
- 22.Jeffcoate TNA. Posterior colpoperineorrhaphy. Am J Obstet Gynecol. 1959;77:490–502. doi: 10.1016/s0002-9378(16)36718-7. [DOI] [PubMed] [Google Scholar]
- 23.Kahn MA, Stanton SL. Posterior colporrhaphy: its effects on bowel and sexual function. Br J Obstet Gynaecol. 1997;104:82–86. doi: 10.1111/j.1471-0528.1997.tb10654.x. [DOI] [PubMed] [Google Scholar]
- 24.Kenton K, Shott S, Brubaker L. Outcome after rectovaginal fascia reattachment for rectocele repair. Am J Obstet Gynecol. 1999;181:1360–1364. doi: 10.1016/s0002-9378(99)70406-0. [DOI] [PubMed] [Google Scholar]
- 25.Nager CW, Kumar D, Kahn MA, Stanton SL. Management of pelvic floor dysfunction. Lancet. 1997;350:1751. doi: 10.1016/S0140-6736(05)63575-1. [DOI] [PubMed] [Google Scholar]