Abstract
Background
This study was exclusively focused on the documentation and cross-cultural evaluation of ethnomedicinal knowledge (EMK) within the diverse linguistic groups of Kohistan situated between the Himalayan and Hindukush Mountain ranges in the north Pakistan.
Methods
Data were gathered during the field survey (May 2022 to July 2023) through group conversations, semi-structured interviews, and on-site observation. Venn diagrams were employed to illustrate the comparative assessment of EMK, and different ethnobotanical indices were utilized to examine the data.
Results
A total of 96 wild medicinal plant species (MPs) belonging to 74 genera and 52 botanical families were documented. The most reported MPs belong to the family Polygonaceae (11 species), followed by Asteraceae (9 species) and Lamiaceae (8 species). The ethnomedicinal uses of Leontopodium himalayanum, Pedicularis oederi, Plocama brevifolia, Polypodium sibiricum, Pteridium esculentum, Sambucus wightiana, Solanum cinereum, Teucrium royleanum, Rhodiola integrifolia, Aconitum chasmanthum were reported for the first time in this region. Among the reported taxa herbaceous species were dominated (72%), followed by trees and shrubs (17% and 10%, respectively). Digestive problems (40 taxa and 114 use reports) and skin disorders (19 taxa and 549 use reports) were the most cited disease categories, whereas M. communis, M. longifolia, Ajuga integrifolia, Ziziphus jujuba, and Clematis grata exhibited the highest percentage fidelity levels. Out of 109 documented medicinal uses, a mere 12 were shared across all linguistic groups, and Bateri emerges as a notable outlier with the highest number of medicinal uses. In addition, a significant homogeneity was noted in the reported botanical taxa (61 species) among different linguistic groups. However, since the last decade biocultural heritage of Kohistan is facing multifaceted risks that need urgent attention.
Conclusion
Our findings could be valuable addition to the existing stock of ethnomedicinal knowledge and may provide ethnopharmacological basis to novel drug discovery for preexisting and emerging diseases prioritizing detailed phytochemical profiling and the evaluation of bioactive potential.
Keywords: Wild medicinal plants, Cross-culture, Fidelity level, Venn diagram: linguistics, Kohistan
Introduction
Kohistan region is an important hotspot of biocultural diversity and could be thus declared a biocultural refugium. The region has been a crossroad for the exchange of biocultural knowledge between South, Southwestern Asia, and Central Asia. The close sociocultural interactions among the different ethnic communities within the region and then the invasion of modernization and infrastructural developments pose a clear challenge to local ecological knowledge within each community. In the face of sociocultural as well as environmental change, the local ethnobotanies are changing and in some case the cultural dominancy has driven a change to make the local knowledge blended with exotic knowledge and this phenomenon is well understood in ethnobiology. The multiculturality and multilingualism of the region make the area a viable place to study human–plant interactions. It is worth mentioning that the remoteness of the area has stood out a reason for scientific research in the study area that may have potentially allowed the local communities to retain cultural practices alive and distinct around the local flora.
Our research on food ethnobotany recorded substantial body of local plant knowledge among the different ethnolinguistic groups living across the Kohistan region [1]. The current ethnobotanical survey has primarily been guided by our food ethnobotanical research work in the region. Our research has indicated significant level of idiosyncrasy or heterogeneity in local knowledge on food plants among the studied communities and considering these specific patterns of knowledge retention or mobilization within the different groups. We have hypothesized that some important debates especially related to human ecology could be constructed and could come with more concrete results on the pattern of local knowledge mobilization which we might have missed to derive from the results of our previous food ethnobotanical studies. Additionally, it may also give rise to new and more stimulating debate related to context-based social anthropology while discussing the local knowledge systems on medicinal plants within these specific communities.
North Pakistan has been extensively researched in ethnobotanical literature; however, the Kohistan region is still underexplored in the existing literature. The literature indicates specific trends in sharing local plant knowledge among the various ethnic groups. We believe that the medical ethnobotany and its related dynamics are a different subject area then food ethnobotany, and therefore, studies on the medical ethnobotany could provide new insights to enrich the anthropological discussion around the use of local medicinal plants. Moreover, culturally guided uses of plants are an important subject in medical anthropology and therefore the intertwining of medical anthropology and medical ethnobotany plays a pivotal role in understanding the dynamics how the local knowledge systems persist and evolve within modern societies.
In Kohistan, the traditional ecological knowledge including the plant knowledge is highly challenged by the new developing infrastructure that impact the local subsistence and ecological practices, and this in turn has negatively impacted the local knowledge systems. For instance, the ongoing mega projects such as Dassu and Basha Hydropower Projects and several small projects in different valleys of Kohistan are affecting the lifestyle of the young generation significantly. Slowly but surely, allopathic medicines are also integrating with traditional healthcare in this region. Specifically, recent developments under the China–Pakistan Economic Corridor (CPEC) project are one of the key factors diverting the attention of the young generation, thus recording the ethnomedicinal knowledge in Kohistan essential. Specifically, documenting the medical ethnobotany of the region will have a crucial role in understanding how different cultures use plants, and how these uses are guided by social, environmental, and economic factors in shaping human–plant relationship. The aim of the current study is that the medical ethnobotany of the ethnolinguistic groups in Kohistan would provide a holistic view; how human interact with their natural environment? The study will preserve new knowledge on scientific background and will give new directions to the already existing literature as we have seen that many Pakistani ethnobotanical studies have been conducted but lacking the best and standard practices to reach the minimum level of scientific integrity. Our study undertakes clear methodological approach—has been conducted with specific objective to address the proposed research questions. We have documented and compared the ethnomedicinal knowledge on wild medicinal plant species among different linguistic groups of Kohistan region in the north Pakistan.
The specific objectives of the study were:
Documentation of the local names and medicinal use of wild plants!
Cross-cultural analysis and comparison of the quoted plants used in traditional health care system among the different ethnic groups.
Methodology
Description of the study area
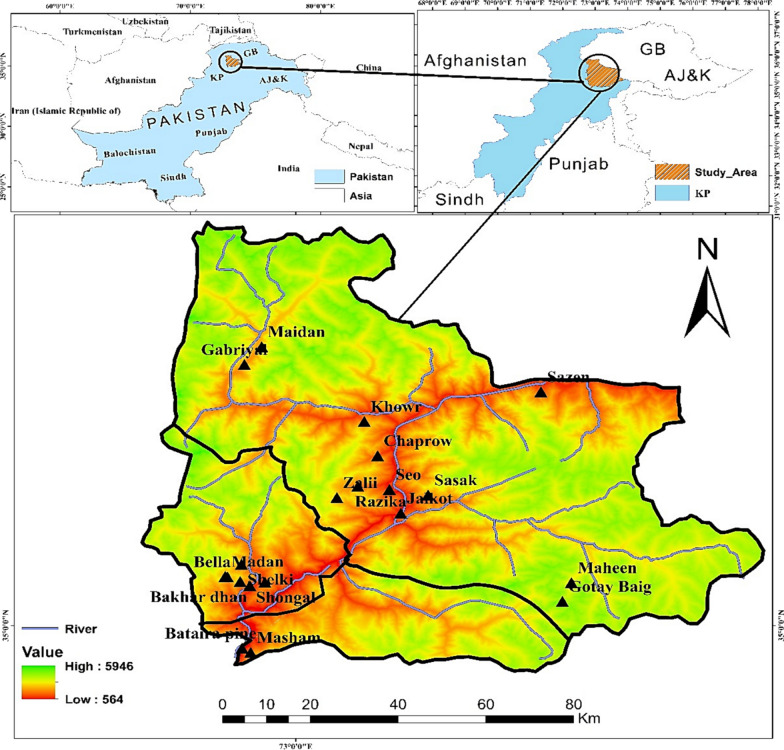
Kohistan region lies between 35° 16′ 16′′ N latitude and 73° 13′ 24′′ E longitude in the sub-humid eastern and wet mountain zones of north Pakistan [2]. Kohistan is subdivided into three districts, namely Kohistan Upper, Lower Kohistan, and Kolai Pallas Kohistan, as dissected by the Indus River (Fig. 1). Characterized by their geographical location, these districts are richly endowed with natural beauty, including majestic mountain vistas, fertile valleys, and vast expanses of biodiversity. Kohistan is distinguished by a dry and cold climate in the winter and a hot and dry climate in the summer. In the valleys, rainfall is prevalent during the winter, while snowfall is observed in alpine pastures and hilly areas [3].
Fig. 1.
Map illustrating study area and survey sites
The vegetation of Kohistan falls into dry and moist temperate forests areas [4, 5]. The primary objective of the present study was to conduct a comprehensive investigation on medicinal uses of wild plant species among different linguistic groups, including Kohistani, Shinaki, Bateri, Pashtoon, and Gujjars, residing in three districts of Kohistan. These linguistic groups, despite their unique dialects and varying lifestyles, do share certain commonalities in religious belief systems and dialect similarities, thus contributing to the diverse cultural mosaic of Kohistan. Additionally, we have discussed in detail the history and ethnolinguistic diversity of Kohistan in our previous article [1]. Agriculture, livestock rearing, and weaving constitute the primary economic activities of the inhabitants of Kohistan, significantly contributing to the region’s economic vitality [2]. Kohistan is the most remote region of Pakistan and lacks modern health facilities. Even in the contemporary era, this region lacks hospitals, necessitating inhabitants to travel over 150 km and endure a journey of at least seven hours to reach the nearest health facility in Abbottabad. Consequently, the inhabitants of this region rely mainly on plants and animals in their environment for sustenance and as components of their indigenous healing practices [6].
Valleys and linguistic groups in Kohistan
The Indus River splits Kohistan into eastern and western parts. Seo, Kandia, and Dubair are three major valleys on the western side, while Jalkot, Palas, and Kolai valleys lie on the eastern side (Fig. 2). In western part of Kohistan, local communities which are known as “Kohiste” speak Kohistani language in different dialects like Shuthun, Maiya, Indus Kohistani, and Abasin Kohistani. The history of Kohistani people and their language is controversial, as different people assume diverse ancestors of Kohistani. It has been documented that Kohistani language belongs to the Dardic group of Indo-Aryan languages [7–11]. According to Rensch [7], Kohistani language linking with the Torwali language is spoken in Swat valley. However, there is lack of further details on the origin of Indus Kohistani language.
Fig. 2.

Panoramic view of different valleys in Kohistan
Local inhabitants in Jalkot, Palas, and Kolai on the eastern side of Kohistan are known as “Shinaki” and they speak Shina language. Shina belongs to the Dardic language family which is a subgroup of the Indo-Aryan linguatuliasis. Phylogenetically, Shina has strong associations with Indo-Aryan, Dravidian, Austro Asiatic, and Tibeto Burman and is written in the “Persio-Arabic script.” Some researchers believe that Shina is Brahmi script which was originally used in the era of Ashok in 3rd BC [12]. Shina language has different dialects which are spoken in different valleys of Kohistan. It is the most spoken language in different valleys of Gilgit-Baltistan, Jammu and Kashmir, Ladakh regions of Pakistan, India, and China [9, 13, 14]. The different dialects of Shina language, for instance, Kohistani, Astori, Chilasi, Gilgiti, Hunzai, and Diameri, are mainly based on local influence, geography, and topography of valleys [13–15].
Bateri, Pushto, and Gujjari linguistic groups are minorities in Kohistan and live in specific areas. Bateri community live in Batera Pain and Batera Bala villages on the east bank of the Indus River in Kolai Pallas Kohistan. Bateri language also known as Bateri Kohistani and Batarwal language belongs to the Dardic language branch of Indo-European family. Beside Kohistan, Bateri is also spoken in Jammu and Kashmir region of India [7]. Pushto language belongs to the eastern Iranian language, a subgroup of Aryan linguistics family, and is further divided into Iranian and Indian branches. In Pakistan, the Pushto speaker has different accents and dialects [7, 16, 17]. Although Pushto linguistic group is limited in the Indus Kohistan region, Pashtuns (Pushto speakers) spread almost in all parts of Pakistan, and specifically in the north province “Khyber Pakhtunkhwa.” In Indus Kohistan, Pashtuns are common at Shongal and Jag villages in Dubair valley. The nomadic Gujjars live in the most remote area of each valley on both sides of Kohistan. It has been reported that Gujjars came to this region from Mongolia at the time of Mongol incursion on India in the fifth century [10]. These tribes speak Gujjari, which accounts for 10.5% compared to other Kohistani and Shina languages [7, 8].
Field survey
Twenty study sites/villages were selected to conduct field survey from May 2022 to July 2023. Study sites’ selection was based on their ethnicity, linguistic groups, vegetation or forest types, and elevation zones. While conducting the field survey, we meticulously observed the ethical guidelines as recommended by “International Society of Ethnobiology” [18]. These guidelines emphasize the importance of maintaining respect for different cultures, acknowledging local knowledge, and preserving biodiversity. Verbal consent of the participants as reported previously [19, 20] was taken for data collection, photography, and sharing their knowledge and picture with the public. As demonstrated earlier [21], informants between 20 and 80 years of age were selected using the snowball approach. The study participants chosen for the survey have a long-lasting relationship with the natural environment and the local flora and were recognized as experienced in local medicinal plant knowledge. Male field researchers co-authoring this article recruited male study participants in the interviews (Fig. 3) since female informants could not be approached due to cultural/religious issues; therefore, the first author interviewed only those women who were his relatives. Moreover, it is also important to note that our respondents were not traditional healers or doctors but laypeople, i.e., experts in local plant knowledge who gained it orally from their elders. In the particular social and cultural context of the study area, women participants could be taken for the interviews if they local communities are guided better and explain the purpose of the study with the help of a local guide.
Fig. 3.

Authors collecting information during filed survey in different areas of Kohistan
From each linguistic group, 15–20 informants including male and female were selected based on their age, gender, linguistic group, experience, and knowledge (Table 1). In Kohistan, open communication between male and female is strictly restricted, except close family members. With the help of female members or relatives from his family, the first author collected information from female respondents who reside in Kohistan. Data were collected by using field observation, semi-structured interviews, and group discussions as explained earlier [22]. The interviews as well as the group discussions were conducted in the local languages (Kohistani, Shina, Bateri, Pushto, and Gujjari). To ensure comprehension, native speakers of these languages and interpreters were engaged. The gathered information was subsequently translated into English, thus facilitating comparative analysis and interpretation.
Table 1.
Characteristics of the targeted localities and study participants
| Sites | Forest types | Ethnic group | AH | SA | EnR./ExR | Linguistic group | Villages | El. (m,a,s,l.) | NH | NI (M/F) | Age |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Seo valley | Himalayan dry and moist temperate forests | Seowos (96%) | Sixteenth–seventeenth century | Pastoralism, animal husbandry and farming | Endogamic, rarely exogamic | Kohistani | Seo | 878 | 320 | 13/5 | 15–60 years |
| Razika | 1830 | 275 | 15/3 | ||||||||
| Chaprow | 1316 | 35 | 10/4 | ||||||||
| Gujjars/Guzar (4%) | NR | Pastoralism and animal husbandry | Exogamic | Gujjari | Zalii | 3093 | 37 | 12/3 | |||
| Jalkot valley | Himalayan dry and moist temperate forest, and alpine pastures | Shinaki/Jalkoti (90%) | Sixteenth–seventeenth century | Pastoralism, animal husbandry, farming, and mining | Endogamic, rarely exogamic | Shina | Maheen | 3503 | 25 | 15/0 | 20–80 years |
| Sasak | 2001 | 120 | 13/1 | ||||||||
| Sazen | 1415 | 154 | 14/0 | ||||||||
| Jalkot | 892 | 250 | 15/2 | ||||||||
| Gujjars/Guzar (10%) | NR | Pastoralism and animal husbandry | Exogamic | Gujjari | Gotay Baig | 4741 | 25 | 9/0 | |||
| Kandia valley | Himalayan dry and moist temperate forests | Kheloos (85%) | Sixteenth–seventeenth century | Pastoralism, animal husbandry and farming | Endogamic, rarely exogamic | Kohistani | Khowr | 1633 | 75 | 11/1 | 20–80 years |
| Gabriyal | 2113 | 286 | 12/2 | ||||||||
| Gujar/Guzar (15%) | NR | Pastoralism and animal husbandry | Exogamic | Gujjari | Maidan | 2655 | 85 | 11/0 | |||
| Kolai valley | Himalayan dry and moist temperate forest, and alpine pastures | Kulooj (95%) | Sixteenth–seventeenth century | Pastoralism, animal husbandry and farming | Exogamic | Shina | Bella | 2232 | 45 | 10/3 | 20–70 years |
| Madan | 2226 | 250 | 14/1 | ||||||||
| Bahtooj (5%) | NR | Pastoralism, animal husbandry and farming | Endogamic, rarely exogamic | Bateri | Bateri pine | 625 | 230 | 13/4 | |||
| Masham | 1810 | 170 | 9/3 | ||||||||
| Dubair valley | Himalayan dry and moist temperate forest, and alpine pastures | Shongali (5%) | NR | Pastoralism, animal husbandry and farming | Exogamic | Pushto | Shongal | 1612 | 120 | 12/2 | 20–60 years |
| Jaagi (5%) | NR | Jaag Kali | 1548 | 160 | 11/3 | ||||||
| Dubairi (90%) | Sixteenth–seventeenth century | Pastoralism, animal husbandry and farming | Endogamic | Kohistani | Bakhar dhan | 2286 | 95 | 13/1 | |||
| Shelki | 2036 | 65 | 9/2 |
AH arrival history in the area, SA subsistence activities, EnR endogamic rules, ExR exogamic rules, El elevation, NH number of households, NI number of informants, M male, F female, AG age groups, NR no record
We adopted a mixed approach for selecting the informants. The survey started with participants selected through random sampling, and then, once we became familiar with the study area, we adopted the snowball technique. The duration of the interviews varied, i.e., in some cases, it ended after 20 min, while in others, it lasted for hours. The participants with long experience of nature and who remained in the study area for decades were preferred. Interviews were conducted in public gathering places, local shops, and fields, mainly after prayer near mosques where the local population used to gather and interact. Some people were also interviewed while working in the fields. The information collected from the interviewees focused on the local names of medicinal taxa, parts used, diseases treated, and modes of preparation and application. Free listing was used to obtain a thorough knowledge of the therapeutic uses of the quoted plants. Initial free listing was attempted, but it was usually short and rarely succeeded.
Plant specimen collection and processing
Medicinal plant species enlisted in Table 2, used by the inhabitants of the study area, were collected during the field survey. The plant specimen were identified by expert taxonomists and with the help of Flora of Pakistan [23]. Botanical nomenclature and family name of the identified specimen were further confirmed with the help of international data base of plant species “The World Flora Online” https://www.worldfloraonline.org/. All specimens were properly dried, poisoned, and mounted on herbarium sheets, and the voucher specimens were deposited in the herbarium at COMSATS University Islamabad, Abbottabad Campus, for future records.
Table 2.
Ethnomedicinal application of wild plants of Kohistan
| S. # | Scientific name/ Family/Local name/ voucher number | Habit | Part(s) use | Preparation | Application | Diseases treated | Disease categories | FC | RFC | PRMUP | PRMUN |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 |
Ajuga integrifolia Buch. -Ham Lamiaceae BhutiK,S,G CUHA-06 |
Herb | Lvs./Stm | Powder, Decoction | Oral | Fever, skin infection, to purify blood | General and unspecified, Skin, Cardiovascular | 14 | 0.05 | 24 | 24 |
| 2 |
Aconitum chasmanthum Stapf ex Holmes Ranunculaceae Sakhat MorilS CUHA-405 |
Herb | Rt | Powder mixed in maize flour | Oral | Anti-rodents | Others | 15 | 0.05 | 25 | |
| 3 |
Artemisia gmelinii Weber ex Stechm Asteraceae Tanda TarkhaP CUHA-237 |
Herb | Lvs | Paste and fresh leaves | Topical | Wounds healing, injuries | Skin | 14 | 0.05 | 26 | |
| 4 |
Artemisia stechmanniana Besser Asteraceae Dada TarkhaP CUHA-239 |
Herb | Lvs, | Tea | Oral | Fever, flue, cough, corona symptoms | General and Unspecified, Respiratory | 14 | 0.05 | 27 | |
| 5 |
Astragalus anisacanthus Boiss Leguminosae MuskandaK, ChokandaG CUHA-13 |
Herb | Rt | Toothbrush, Paste | Topical | To clean teeth and mouth gums | Digestive | 18 | 0.06 | 28 | |
| 6 |
Berberis lycium Royle Berberidaceae ShoonglooK,S, ShugloB, KoarayP CUHA-204 |
Shrub | Rt | Powder with egg white | Topical and Oral | Wounds healing and Backache | Skin, Musculoskeletal | 12 | 0.04 | 29 | |
| 7 |
Bergenia stracheyi (Hook.f. & Thomson) Saxifragaceae Kala parK, KuratS, RechowooG CUHA-187 |
Herb | Rt | Powder | Oral | Chest infection, stomach disorder, and backache | Respiratory, Digestive, Musculoskeletal | 9 | 0.03 | 30 | |
| 8 |
Bergenia ciliata (Haw.) Sternb Saxifragaceae Kala parK, KuratS, RechowooG CUHA-14 |
Herb | Rt | Powder | Oral | Chest infection, stomach disorder, and backache | Respiratory, Digestive, Musculoskeletal | 15 | 0.05 | 29 | |
| 9 |
Buxus wallichiana Baill Buxaceae NeekB CUHA-250 |
Shrub | Lvs | Paste | Oral | Constipation | Digestive | 12 | 0.04 | 31 | |
| 10 |
Caltha palustris L Ranunculaceae PataraG CUHA-251 |
Herb | Lvs | Powder with butter | Oral | Intestinal wounds | Digestive | 9 | 0.03 | 32 | |
| 11 |
Cannabis sativa L Cannabaceae Bhang S,G, Fat kandaB CUHA-16 |
Herb | Lvs | Paste with maize flour | Topical | Body weakness and indigestion | Digestive | 15 | 0.05 | 33 | |
| 12 |
Cedrus deodara (Roxb. ex D.Don) Pinaceae BeechK, PlolzS, Low G CUHA-17 |
Tree | Rt./Stm./Rn | Oil | Topical | Skin infection, against pests/insects, as anti-hair fall, mouth gums, stomach disorders | Skin, Digestive, Others | 14 | 0.05 | 30 | |
| 13 |
Celtis caucasica Willd Cannabaceae MeyoonK,S, DodooB CUHA-401 |
Tree | Fr | Powder | Oral | Allergy | Others | 14 | 0.05 | 31 | |
| 14 |
Chrysojasminum humile (L.) Banfi Oleaceae TobkioS, Naltah B CUHA-277 |
Herb | Rt | Powder | Oral | Ringworms | Digestive | 15 | 0.05 | 36 | |
| 15 |
Cirsium arvense (L.) Scop Asteraceae HoralG CUHA-27 |
Herb | Ap./Rt | Decoction and Powder | Oral | Typhoid fever, and to heal wounds | General and Unspecified, Skin | 15 | 0.05 | 37 | |
| 16 |
Cirsium verutum Spreng Asteraceae ZachK, JaachaS, ZheheeaB, KenareG CUHA-254 |
Herb | Lvs | Fresh Part/Powder | Oral | Fever | General and Unspecified | 11 | 0.04 | 38 | |
| 17 |
Clematis grata Wall Ranunculaceae ZultoK CUHA-26 |
Climber | Lvs | Powder | Oral | Urinary disorder and bladder infection | Urological | 12 | 0.04 | 32 | |
| 18 |
Clinopodium vulgare L Lamiaceae Shakbar butiK CUHA-255 |
Herb | Lvs | Powder | Oral | Internal wounds | Digestive | 14 | 0.05 | 39 | |
| 19 |
Daphne mucronata Royle Thymelaeaceae Laatar B CUHA-259 |
Shrub | Fr | Paste | Topical | Face stains | Digestive, Skin | 12 | 0.04 | 40 | |
| 20 |
Datisca cannabina L Datiscaceae KarayeeK, KalbeerS, BarsatraB, KurkoronG CUHA-30 |
Herb | Rt | Paste | Topical | Joint swelling | Musculoskeletal | 14 | 0.05 | 41 | |
| 21 |
Dodonaea viscosa Jacq Sapindaceae ShonthK, AshadB, GoodniG CUHA-33 |
Shrub | Lvs | Extract | Orally | Throat infection | Respiratory | 13 | 0.05 | 42 | |
| 22 |
Duchesnea indica (Andrews) Teschem Rosaceae BhangrosK, MagrosS, MuabrosB, Dharti MianG, BhangrusP CUHA-263 |
Herb | Fr | Fresh Part | Oral | Indigestion | Digestive | 12 | 0.04 | 43 | |
| 23 |
Dysphania botrys (L.) Mosyakin & Clemants Amaranthaceae JamamaB CUHA-253 |
Herb | Lvs | Powder | Oral | Abdominal warm | Digestive | 17 | 0.06 | 32 | |
| 24 |
Erigeron canadensis L Asteraceae LindiK, KasarS CUHA-28 |
Herb | Ap | Paste | Topical | Toothache | Digestive | 14 | 0.05 | 42 | |
| 25 |
Ficus palmata Forssk Moraceae PhahK,B, PagoyeS, CameraG CUHA-37 |
Tree | Lvs./Milk | Paste | Topical | spots or stain on face, to heal wounds | Skin | 12 | 0.04 | 34 | |
| 26 |
Geranium himalayense Klotzsch Geraniaceae Rathan JokG,S CUHA-267 |
Herb | Ap | Powder | Oral | stomach pain | Digestive | 11 | 0.04 | 45 | |
| 27 |
Hypericum oblongifolium Choisy Hypericaceae Khan kawaB CUHA-271 |
Herb | Lvs | Powder | Oral | Backache | Musculoskeletal | 12 | 0.04 | 45 | |
| 28 |
Hypericum perforatum L Hypericaceae Chai thigoK, EsperkayeG CUHA-41 |
Herb | Lvs |
Decoction and Powder |
Oral | Backache | Musculoskeletal | 11 | 0.04 | 46 | |
| 29 |
Indigofera tinctoria L Fabaceae Kayth K, KastiS, Khati B, KheentheyG CUHA-43 |
Shrub | Stm./Lvs | Toothbrush, Decoction | Oral | To strengthen teeth, paralysis | Digestive, Neurological, | 12 | 0.04 | 47 | |
| 30 |
Juglans regia L Juglandaceae ChooK, AchoyeS, AkhoryG CUHA-45 |
Tree | Brk | Fresh | Topical | To clean teeth, mouth gums | Digestive | 14 | 0.05 | 48 | |
| 31 |
Juniperus excelsa M.Bieb Cupressaceae CheliS CUHA-279 |
Tree | Fr | Powder | Oral | Kidney inflation | Urological | 15 | 0.05 | 49 | |
| 32 |
Justicia adhatoda L Acanthaceae BhekarS, BasheeB CUHA-190 |
Shrub | Lvs | Paste | Topical | Wounds healing | Skin | 13 | 0.05 | 50 | |
| 33 |
Leontopodium himalayanum DC. Compositae Taliban kaleelS CUHA-280 |
Herb | Lvs | Fresh Part | Oral | Abdominal pain | Digestive | 15 | 0.05 | ||
| 34 |
Lepidium sativum L Brassicaceae TumeraS,, GulpechaB CUHA-46 |
Herb | Ap | Decoction | Oral | Asthma | Respiratory | 15 | 0.05 | 42 | |
| 35 |
Mallotus philippensis (Lam.) Müll.Arg Euphorbiaceae KamlaS, KambilaB CUHA-284 |
Tree | Fr | Powder | Oral | Abdominal warms | Digestive | 17 | 0.06 | 34 | |
| 36 |
Melia azedarach L Meliaceae Kamsal laghaK, LagandS, Tora bekarP CUHA-47 |
Tree | Lvs | Powder | Oral | Allergy | General and Unspecified | 14 | 0.05 | 41 | |
| 37 |
Mentha arvensis L Lamiaceae PhepeelS, PodinaG CUHA-287 |
Herb | Ap | Powder | Oral | Diarrhea | Digestive | 15 | 0.05 | 51 | |
| 38 |
Mentha longifolia (L.) L Lamiaceae PhemilK, PhepeelS, ZoonB, PodinaG, veliniP CUHA-48 |
Herb | Lvs | Powder and Tea | Oral | Diarrhea and indigestion | Digestive | 14 | 0.05 | 40 | |
| 39 |
Mentha spicata L Lamiaceae PhemilK, PodinaG CUHA-288 |
Herb | Lvs | Decoction | Oral | Diarrhea and indigestion | Digestive | 14 | 0.05 | 40 | |
| 40 |
Myrtus communis L Myrtaceae AmboK, AobS CUHA-26 |
Herb | Fr./Lvs | Powder | Topical | Eczema | Skin | 18 | 0.06 | 48 | |
| 41 |
Nepeta podostachys Benth Lamiaceae JurpeK, PushmilyP CUHA-51 |
Herb | Lvs./Stm | Paste | Topical | Skin infections | Skin | 15 | 0.05 | 52 | |
| 42 |
Nerium oleander L Apocynaceae PhoolK,B CUHA-292 |
Shrub | Lvs | Decoction | Topical | To kill pests and fungus | Others | 17 | 0.06 | 31 | |
| 43 |
Oreoseris gossypina (Royle) X.D.Xu & V.A.Funk) Asteraceae KhoonP CUHA-402 |
Herb | Rt | Powder | Topical | Intestinal wounds | Digestive | 53 | |||
| 44 |
Oxalis corniculata L Oxalidaceae Cheko daroK, Chiki rangS CUHA-53 |
Herb | Lvs | Extract | Oral | Jaundice and hepatitis | Digestive | 14 | 0.05 | 31 | |
| 45 |
Oxyria digyna Hill Polygonaceae HuliS CUHA-294 |
Herb | Ap | Fresh Part/Powder | Oral | Constipation | Digestive | 15 | 0.05 | 54 | |
| 46 |
Pedicularis oederi Vahl Orobanchaceae Khana PhorS CUHA-296 |
Herb | Lvs | Powder | Oral | Indigestion and weakness | Digestive | 15 | 0.05 | ||
| 47 |
Persicaria amplexicaulis (D.Don) Ronse Decr Polygonaceae RoyK CUHA-57 |
Herb | Lvs | Powder | Oral | Backache | Others | 14 | 0.05 | 55 | |
| 48 |
Persicaria capitata (Buch. -Ham. ex D.Don) H.Gross Polygonaceae Maran KashK CUHA-58 |
Herb | Ap | Powder | Oral | Urinary tract infection and urinary bladder inflammation | Urological | 18 | 0.06 | 56 | |
| 49 |
Pistacia khinjuk Stocks Anacardiaceae KhakowK, KakohS CUHA-63 |
Tree | Lvs | Powder | Oral | Asthma and cough | Respiratory | 14 | 0.05 | 57 | |
| 50 |
Plantago lanceolata L Plantaginaceae CheelorK,S,G, JabayB CUHA-64 |
Herb | Lvs | Paste | Topical | Skin infections | Skin | 15 | 0.05 | 58 | |
| 51 |
Plantago major L Plantaginaceae CheelorK,G CUHA-65 |
Herb | Lvs | Decoction | Oral | Skin infection | Skin | 12 | 0.04 | 58 | |
| 52 |
Plocama brevifolia subsp. Brevifolia Rubiaceae ZoonrS, JhoorB CUHA-300 |
Herb | Ap | Paste | Topical | Blood clots and injuries | Blood | 15 | 0.05 | ||
| 53 |
Podophyllum hexandrum Royle Berberidaceae ShargoyeK, ShingoyS, KhakoriG CUHA-66 |
Herb | Rt | Paste | Oral | Warts and other skin infections | Skin | 14 | 0.05 | 59 | |
| 54 |
Polygonatum multiflorum (L.) All. Asparagaceae AschawagiK CUHA-67 |
Herb | Rt | Powder | Oral | Abdominal pain, dysentery | Digestive | 14 | 0.05 | 60 | |
| 55 |
Polygonum aviculare L Polygonaceae Zat GahK CUHA-68 |
Herb | Rt | Powder | Topical | External wounds | Skin | 18 | 0.06 | 61 | |
| 56 |
Polypodium sibiricum Sipliv Polypodiaceae ShaalK CUHA-70 |
Herb | Ap./Lvs | Decoction/Powder | Oral/ Topical | Intestinal ulcers, to heal wounds or injuries, stomach disorder | Digestive, Skin | 18 | 0.06 | ||
| 57 |
Primula elliptica Royle Primulaceae Kamzoor MorilS CUHA-302 |
Herb | Lvs | Ash | Topical | Mouth gums, diarrhea/ cough | Digestive, Others | 15 | 0.05 | 62 | |
| 58 |
Primula macrophylla D. Don Primulaceae MorilS CUHA-303 |
Herb | Lvs | Ash | Topical | Mouth gums | Others | 15 | 0.05 | 62 | |
| 59 |
Prunus persica (L.) Batsch Rosaceae AroK,G, AarS CUHA-74 |
Tree | Lvs | Infusion | Topical | Fungal and bacterial infections | Skin | 17 | 0.06 | 54 | |
| 60 |
Pteridium aquilinum L. Kuhn Dennstaedtiaceae Asbo mut K CUHA-75 |
Herb | Lvs | Powder | Oral | Chest pain | Respiratory | 14 | 0.05 | 63 | |
| 61 |
Pteridium esculentum (G.Forst.) Cockayne Dennstaedtiaceae KongiiG CUHA-76 |
Herb | Ap | Powder | Oral | External wounds, tumors, internal injuries | Skin, Cancer, Digestive, Blood | 12 | 0.04 | ||
| 62 |
Punica granatum L Lythraceae DangoK, DaroyeS, DeengoB, DarooG, AnogoraP CUHA-78 |
Tree | Rnd./Rt | Decoction/Powder | Oral | External wounds, tumors, internal injuries, intestinal worms | Skin, Digestive, Blood | 18 | 0.06 | 64 | |
| 63 |
Quercus semecarpifolia Sm Fagaceae BanK, BaniS, TarraB CUHA-81 |
Tree | Fr | Fresh Part | Oral | Stomach problem, to strengthen bones | Digestive, Musculoskeletal | 18 | 0.06 | 64 | |
| 64 |
Rheum australe D. Don Polygonaceae ChutiyalK,S CUHA-311 |
Herb | Rt | Powder | Oral | Constipation | Digestive, | 9 | 0.03 | 65 | |
| 65 |
Rheum webbianum Royle Polygonaceae Chutiyal KamzoorS,K CUHA-312 |
Herb | Rt | Fresh Part/Powder | Oral | Constipation | Digestive | 9 | 0.03 | 66 | |
| 66 |
Rhodiola integrifolia Raf Crassulaceae PechilS CUHA-313 |
Herb | Ap | Powder with maize flour | Oral | Vomiting and indigestion | Digestive | 9 | 0.03 | ||
| 67 |
Ricinus communis L Euphorbiaceae Jamal ghotaS CUHA-157 |
Tree | Lvs | Fresh leaves | Topical | External wounds | Skin | 11 | 0.04 | 42 | |
| 68 |
Rubus fruticosus Lour Rosaceae AnchaK CUHA-88 |
Shrub | Lvs | Decoction | Oral | Diarrhea, dysentery | Digestive | 12 | 0.04 | 32 | |
| 69 |
Rubus niveus var. micranthus (D.Don) H.Hara Rosaceae AnchaK, ZekeenyS CUHA-89 |
Shrub | Lvs | Powder | Oral | Cough and fever | Respiratory, General and Unspecified | 15 | 0.05 | 67 | |
| 70 |
Rumex acetosa L Polygonaceae ChukiS CUHA-318 |
Herb | Rt./Lvs | Extract | Oral | Jaundice and hepatitis | Digestive | 15 | 0.05 | 68 | |
| 71 |
Rumex hastatus D.Don Polygonaceae ChowkoS, HuliG CUHA-92 |
Herb | Ap | Extract | Oral | Skin rashes, jaundice, and hepatitis | Skin, Digestive | 15 | 0.05 | 42 | |
| 72 |
Rumex nepalensis Spreng Polygonaceae HububalS CUHA-319 |
Herb | Ap | Infusion and paste | Oral | Corona infection, constipation | Respiratory, Digestive | 14 | 0.05 | 42 | |
| 73 |
Rumex abyssinicus Jacq Polygonaceae MarkashK CUHA-90 |
Herb | Rt | Decoction | Oral | Jaundice and hepatitis | Digestive | 14 | 0.05 | 69 | |
| 74 |
Rumex dentatus L Polygonaceae BabalK, HububalS, HulowG CUHA-91 |
Herb | Rt | Paste with maize flour | Oral | Constipation | Digestive | 14 | 0.05 | 42 | |
| 75 |
Salix tetrasperma Roxb Salicaceae BeyoK,S, BatkorolS CUHA-94 |
Tree | Lvs | Decoction | Oral | Fever, common cold | General and Unspecified | 17 | 0.06 | ||
| 76 |
Sambucus wightiana Wall. Ex. Wight & Arn Adoxaceae KatoolK, GanalaS, KoohG CUHA-95 |
Herb | Stm | Fresh Part | Topical/ Smoke | Fever, sickness | General and Unspecified | 18 | 0.06 | ||
| 77 |
Selaginella. Sp Selaginellaceae CUHA-403 |
Herb | Ap | Fresh Part | Inhalation | Fever, sickness | General and Unspecified | 17 | 0.06 | 70 | |
| 78 |
Seriphidium maritimum subsp. Maritimum Asteraceae SalalK, JundS CUHA-404 |
Herb | Ap | Fresh Part | Inhalation | Mosquito repellent | Others | 14 | 0.05 | 71 | |
| 79 |
Silene conoidea L Caryophyllaceae BandakayB CUHA-324 |
Herb | Lvs | Fresh Part | Oral | Poultry diseases ailments | Others | 12 | 0.04 | 72 | |
| 80 |
Skimmia anquetilia N.P.Taylor & Airy Shaw Rutaceae NameerK,S CUHA-326 |
Herb | Lvs | Powder and paste | Oral | Smallpox, to kill worms, as an appetizer | General and Unspecified, Others | 11 | 0.04 | 73 | |
| 81 |
Solanum nigrum Acerbi ex Dunal Solanaceae KuchmachoK,G, KachmachS CUHA-97 |
Herb | Lvs | Extract/Powder | Oral | Urinary bladder inflammation and infection | Urological | 14 | 0.05 | 41 | |
| 82 |
Solanum villosum Mill Solanaceae Kuchmacho KG,KachmachS CUHA-330 |
Herb | Lvs | Extract/Powder | Oral | Urinary bladder inflammation and infection | Urological | 17 | 0.06 | 74 | |
| 83 |
Solanum virginianum L Solanaceae Kanr ShaB CUHA-331 |
Herb | Fr | Paste | Topical | Dandruff | Skin | 17 | 0.06 | 75 | |
| 84 |
Solanum miniatum Bernh. Ex. Wild Solanaceae Ker Ker K CUHA-96 |
Herb | Lvs | Fresh Part | Oral | Mouth gums and toothache | Digestive | 14 | 0.05 | 76 | |
| 85 |
Solanum cinereum R.Br Solanaceae Zacha rangoK, Kool ZachaS CUHA-406 |
Herb | Sd | Oil | Topical | Dandruff | Skin | 17 | 0.06 | ||
| 86 |
Sonchus arvensis L Asteraceae Cheer GandalB CUHA-332 |
Herb | Lvs | Extract | Topical | Mol | Skin | 12 | 0.04 | 32 | |
| 87 |
Tagetes minuta L Asteraceae MidiK, DoldooliS CUHA-101 |
Herb | Fl | Extract | Topical | Mosquito repellent | Others | 14 | 0.05 | 77 | |
| 88 |
Taraxacum campylodes G.E.Haglund Compositae HandhS CUHA-336 |
Herb | Lvs | Powder | Oral | Liver disorder | Digestive | 15 | 0.05 | 21 | |
| 89 |
Taxus wallichiana Zucc Taxaceae ThoonK, BarayP CUHA-102 |
Tree | Brk | Powder | Oral | Cough | Respiratory | 11 | 0.04 | 78 | |
| 90 |
Teucrium royleanum Wall Lamiaceae Plaki ThagoK, Satqa BotiP CUHA-338 |
Herb | Ap | Powder | Oral | Obesity | Digestive | 11 | 0.04 | ||
| 91 |
Thymus linearis Benth Lamiaceae Esperki K,P, Kalay de JaarS CUHA-339 |
Herb | Lvs | Infusion | Oral | Abdominal pain and intestinal worms | Digestive | 11 | 0.04 | 71 | |
| 92 |
Trifolium pratense L Leguminosae Kana EshpetK, ShotalS,G CUHA-103 |
Herb | Lvs | Powder | Oral | Cough, cold, and asthma | Respiratory | 14 | 0.05 | 64 | |
| 93 |
Valeriana jatamansi Jones Caprifoliaceae MushkebalaK,G CUHA-105 |
Herb | Ap | Powder | Oral | Fever and the common cold | General and Unspecified, respiratory | 15 | 0.05 | 79 | |
| 94 |
Verbascum thapsus L Scrophulariaceae Khardak K,B, Kuthay KumS, KhotikamG CUHA-106 |
Herb | Fl./Lvs | Powder | Oral | Cough, cold, and asthma, labor pain and wounds | Respiratory, Digestive | 12 | 0.04 | 34 | |
| 95 |
Zanthoxylum armatum DC Rutaceae TemberB CUHA-199 |
Shrub | Fr | Powder | Oral | Flue | Respiratory | 12 | 0.04 | 80 | |
| 96 |
Ziziphus jujuba Mill Rhamnaceae SageeK, SazenS, SageenG CUHA-112 |
Tree | Sd | Powder | Oral | Blood pressure, to purify blood | Cardiovascular, Blood | 13 | 0.05 | 81 |
K kohistani, S shina, B bateri, P pushto, G gujjari, PRTU previously reported as ethnobotanical use, PRMP previously reported as a medicinal plant, FC frequency of citation, RFC relative frequency of citation, UV used value, Ap aerial part, Lvs leaves, Rt roots, Stm stem, Fl flower, Fr fruit, Sd seed, Brk bark, Rn resin, Rnd rind
Data analysis
Filed data on ethnomedicinal uses of the reported botanical taxa were processed using MS Excel. Furthermore, different ethnobotanical indices, i.e., relative frequency citation (RFC), informant consent factor (ICF), and fidelity level (FL), were also computed. Data were presented in tabulated and graphical format with the help of Sigma Plot v12. Comparative assessment of data among different linguistic groups was presented as Venn diagrams drawn using free software available at http://bioinformatics.psb.ugent.be/webtools/Venn/[05 August 2023]. To find out novel uses of plant species, a comparison was made between the current ethnobotanical data and previously reported literature from Pakistan and neighboring countries [4, 21, 24–80], as given in Table 2.
Relative frequency citation (RFC)
The measured value of RFC demonstrates the importance of each plant species among the local inhabitants of an area. RFC is calculated based on the frequency of citation (FC) of each species, which indicates the number of informants citing the use of plant species for a specific purpose. We used the following equation to calculate RFC value of the reported plant species as described earlier [81].
| 1 |
FC indicates the frequency of citation of each species by respondents, and N is the total number of respondents participating in the survey.
Informant consensus factor (ICF)
The informant consensus factor is used to analyze the degree of agreement of the respondents about each use category. ICF of the reported species was computed by using below mentioned formula as reported earlier [81, 82].
| 4 |
Nur is the number of use reports in each use category, and Nt is the number of plant species used for that category.
Fidelity level (FL)
The fidelity level specifies ratio among the number of respondents who mentioned use of a plant for a particular purpose and the total number of informants who mentioned the use of the plants for any purpose regardless of any use category. The FL values ≈ 100% are obtained for plants having almost all use-mentions refer to same purpose, whereas low FL is obtained for the plant species that have multipurpose uses [83, 84]. The fidelity level of the reported species was calculated using the formula as given here:
| 3 |
Ip is the number of respondents who reported the use of a plant species for a specific purpose, and Iu is the total number of respondents who mentioned that plant species for any purpose.
Results and discussion
Features of the targeted localities and respondents
Data were meticulously gathered for the current ethnomedical study from 20 villages dispersed across five distinct valleys in the captivating Kohistan region: Seo, Jalkot, Kandia, Kolai, and Dubair (Table 1). The survey spanned an altitudinal range from 625 m above sea level (m.a.s.l.) in Bateri pine village to 4741 m.a.s.l. in Gotay Baig village. The vegetation cover in the surveyed area exhibited a spectrum from dry temperate to moist temperate, and subalpine to alpine pastures, mirroring the altitudinal variations.
Kohistan’s entire population adheres to Sunni Muslims, with historical records indicating their settlement in the region from the sixteenth to seventeenth century and conversion to Islam occurred during the eighteenth century. According to Fredrik Bart (1956), the Chinese Pilgrims traveled through the Indus Kohistan region. Although the Chinese pilgrim reported about the difficult trains of the routes, it did not mention about the inhabitants of Kohistani [10, 85]. Notably, the Kohistani people differentiate themselves in terms of ethnicity, language, and culture from neighboring populations in the Swat, Dir, Gilgit, and Baltistan regions of Pakistan. Their beliefs underscore distinctions between both Pashtun and other local communities in Gilgit-Baltistan. Most of the local population in Kohistan faces literacy challenges and is engaging in subsistence activities such as pastoralism, animal husbandry, farming, and mining.
In the present study, data were collected from 281 informants of 20–80 years of age. Ethnically, these informants were classified into distinct groups, including Seowos, Gujjars, Shinaki, Jalkoti, Kheloos, Kulooj, Bahtooj, Shongali, Jaagi, and Dubairi. These groups communicate primarily in the Kohistani, Shina, Gujjari, Bateri, and Pushto languages. Each linguistic group exhibits a unique culture and predominantly resides in different valleys, except for the Gujjars, who are dispersed across all valleys. Most of these linguistic or ethnic groups practice endogamy, with rare instances of exogamy, except for the Gujjars and Bateri, who engage in exogamous relationships with other ethnic groups. Unfortunately, the latter two groups often experience marginalization within the Kohistan region. This intricate social fabric reflects the diversity and historical evolution of the Kohistani people.
Diversity of wild medicinal plant species
The wild medicinal plant species (WMPs) have played a significant role in the mountain communities’ healthcare practices for centuries and continue to do so today. The utilization of WMPs has been a longstanding tradition in the healthcare practices of the Kohistan region. This emphasizes the reliance of the mountain communities in this region on various plant species to meet their healthcare needs. Specifically, the WMPs play a crucial role in the local healthcare practices and are considered an integral part of the traditional medicine system of Kohistan.
According to the data presented in Table 2, the inhabitants of Kohistan use 96 WMPs, which belong to 74 distinct genera and 52 botanical families. Among the botanical families, Polygonaceae was the most prevalent, comprising 11 WMPs, followed closely by Asteraceae, Lamiaceae, Solanaceae, and Rosaceae, each contributing 10, 8, 5, and 4 WMPs, respectively. The extensive use of WMPs from the Polygonaceae family can be attributed to their diverse medicinal properties, such as anti-inflammatory, wound-healing, and antibacterial potential that make them effective in treating a wide range of ailments [86]. Interestingly, our findings align with previous studies conducted in the northern parts of Pakistan [22, 87]. These studies have also reported the dominance of Polygonaceae and Lamiaceae families in the Gilgit-Baltistan region, Kohistan, and surrounding areas is due to their widespread ecological distribution [60, 88, 89].
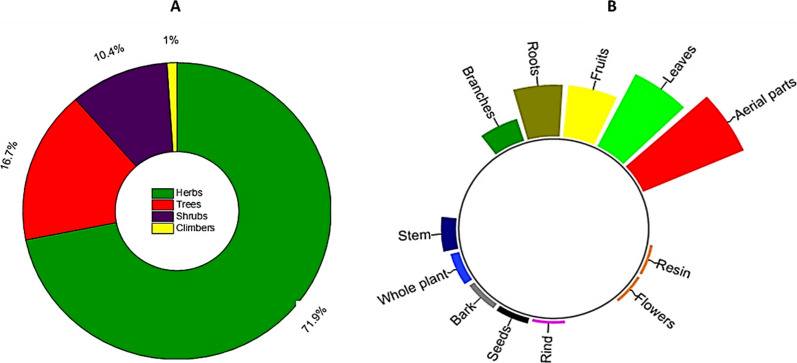
As depicted in Fig. 4A, the reported WMPs consist most of herbs (71.8%), followed by trees (16.6%) and shrubs (10.4%). These findings align with the geographical features of the Kohistan region, which predominantly consists of expansive pasture lands adorned with a variety of lush green herbs. Additionally, the local inhabitants of Kohistan exhibit a preference for collecting and utilizing herbaceous WMPs from their surroundings due to their accessibility and numerous health benefits, as compared to trees and shrubs. This observation corresponds to previous studies conducted in the other areas of Kohistan [79, 89].
Fig. 4.
A Different life forms B part(s) used of the reported WMPs
Part(s) used, modes of preparation and application
The inhabitants of Kohistan use different parts of the reported WMPs to treat various ailments (Fig. 4B). Among these, aerial parts of 36 herbaceous plant species are used in traditional therapies, followed by leaves of 28 species, fruits and roots of 18 species each, branches of 8 species, and stem of 5 species, whereas bark, seeds, rind, flowers, and resin of less than 5 WMPs are used in the primary health care system of Kohistan. Among these, leaves are the most utilized plant parts in traditional remedies for treating various diseases.
The use preference of leaves in traditional therapies could be attributed to their ease of collection compared to other parts of WMPs. Moreover, numerous studies have highlighted that leaves contain a rich concentration of secondary metabolites like polyphenolics, alkaloids, carotenoids, and vitamins, which have significant antimicrobial, antioxidant, anti-inflammatory, and other bioactive properties [89, 90]. Furthermore, the use of leaves instead of roots, flowers, seeds, and fruits in traditional medicines represents a more sustainable conservation approach that minimizes the risk of depleting valuable medicinal plant species [35].
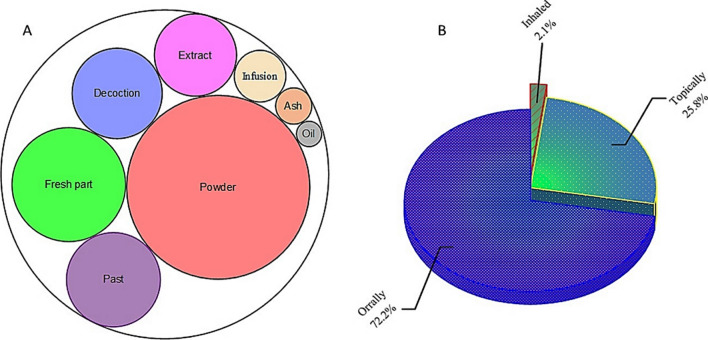
The array of methods employed in the preparation of herbal remedies includes everything from sun drying and grinding with mortars and pestles, to fermentation, distillation, and maceration, each having its unique advantages. As illustrated in Fig. 5A, local inhabitants of the study area utilize a total of eight different methods for preparing herbal remedies. Most of the reported WMPs (49 species) are shade dried and grinded using a mortar and pestle to make a fine powder that can be taken orally or applied topically to treat various diseases. According to the local respondents, the powdered crude drugs can be stored for extended periods of time in cotton sacks or pots made from mud or silver. Additionally, fresh plant parts (consisting of 19 species), pastes (13 species), decoctions (12 species), and extracts (10 species) are commonly employed modes of preparation in traditional recipes for the treatment of various ailments. These traditional recipes have their own unique preparations and applications. For instance, fresh leaf decoctions are commonly used as cleansing agents, while pastes made from powdered roots are often applied topically to treat skin infections.
Fig. 5.
A Preparation and B administration methods of traditional health care recipes
Among these recipes, approximately 72% (Fig. 5B) are taken orally in the form of decoctions, infusions, or extracts, while 25.8% are applied topically as pastes, powders, or oils, particularly for addressing skin infections. Water, milk, diluted curd (lassi), ghee, and butter are frequently used as mediums for consuming the powdered or fresh parts of wild medicinal plants. It is worth noting that similar methods of preparation and administration have been reported in previous studies conducted in this region, and neighboring areas [31, 32, 34, 57, 60, 67, 77, 91–94].
In accordance with the guidelines outlined by the international classification of primary care ICPC-2 [95], the recorded ailments among the inhabitants of Kohistan were classified into twelve distinct categories (Table 3). These include general and unspecified diseases (OTHA-A), digestive disorders (GAS-D), cardiovascular problems (CAR-K), conditions related to blood, blood-forming organs, and the immune system (Blood-B), musculoskeletal disorders (SKE-L), neurological disorders (NER-N), respiratory infections (RES-R), skin diseases (DER-S), urological disorders (URO-U), cancer (CAN-C), pregnancies, childbirth, family planning (PRE-W). For diseases that did not neatly fit into any specific category, minor modifications were made. Examples of such cases include fever, allergies, back pain, typhoid, and spiritual uses—these were categorized as general and unspecified.
Table 3.
Diseases category, informant consent factor, and fidelity level of the reported WMPs
| S. # | ICPC category | Ailments | Nbt | Nur | ICF | Botanical taxa | Disease(s) treated | FC | UM | FL |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | OTHA-A: General and unspecified | Fever, allergy, back pain, typhoid, and spiritual uses | 13 | 398 | 0.97 | Ajuga integrifolia | Fever | 14 | 11 | 78.57 |
| 2 | GAS-D: Digestive problems | Constipation, toothache, intestinal worms, diarrhea, jaundice, indigestion, stomachic pain, tooth gum, liver ailment, appetizer, abdominal warm, hepatitis, ulcer, and obesity | 40 | 114 | 0.65 | Mentha longifolia | Diarrhea and indigestion | 14 | 13 | 92.86 |
| 3 | CAR-K: Cardiovascular diseases | Blood pressure, and blood purifier | 2 | 73 | 0.99 | Ziziphus jujuba | Blood purifier | 13 | 10 | 76.92 |
| 4 | Blood-B: Blood, blood-forming organs, and immune mechanism | blood clots and injuries, to stop bleeding | 4 | 117 | 0.97 | Plocama brevifolia | Bleeding cuts or wounds | 15 | 7 | 46.67 |
| 5 | SKE-L: Musculoskeletal disorders | Joint swelling, and strengthening bones | 3 | 122 | 0.98 | Datisca cannabina | Joint swelling | 14 | 8 | 57.14 |
| 6 | NER-N: Neurological problems | Paralysis | 1 | 26 | 1.00 | Indigofera tinctoria | Paralysis | 12 | 5 | 41.67 |
| 7 | RES-R: Respiratory disorders | Flu, coughing, corona viral infection, chest pain, asthma, colds, bronchitis, throat infection, influenza, and chest pain | 17 | 479 | 0.97 | Lepidium sativum | Asthma | 14 | 9 | 64.29 |
| 8 | DER-S: Skin diseases | Wound healing, eczema, skin rash, skin patches, skin irritation, dandruff, warts, face stain, skin dryness, skin infection, and to remove mol | 19 | 549 | 0.97 | Myrtus communis | Eczema | 18 | 17 | 94.44 |
| 9 | URO-U: Urological disorders | Urinary disorder, bladder infection, kidney problem, urinary tract infection and urinary disorders | 5 | 119 | 0.97 | Clematis grata | Urinary disorder | 12 | 8 | 66.67 |
| 10 | CAN-C: Cancer | Tumor | 1 | 26 | 1.00 | Pteridium esculentum | Tumor | 12 | 5 | 41.67 |
| 11 | PRE-W: Pregnancy, childbearing, family planning | Labor pain | 1 | 26 | 1.00 | Verbascum thapsus | Labor pain, Respiratory disorders | 12 | 7 | 58.33 |
| 12 | OTH: Others | Anti-rodents, mosquito & mouse repellent, anti-insecticidal and fungicidal, livestock diseases, poultry ailments, and antimicrobial | 19 | 431 | 0.96 | Ambrosia artemisiifolia | Anti-rodents, mosquito repellent | 14 | 9 | 64.29 |
Nbt number of botanical taxa used, NUR number of use reports, PS prefer species, FC frequency of citation, UM use mention, FL fidelity level
Quantitative analysis of the reported WMPs
In total 281, respondents of five linguistic groups reported medicinal uses of 96 wild plant species, and total use reports were 3298 (Table 2). Among the reported botanical taxa, Myrtus communis had the highest RFC (0.34). This medicinal plant species is evergreen and local inhabitants of Kohistan use its leaves to treat eczema. In addition, M. communis is also used as tea, and flavoring agent in traditional cuisines of Kohistan (Amin et al. [1]) and has been reported as a medicinal plant in the neighboring regions [96, 97]. Beside this, Sambucus wightiana, Punica granatum, Quercus semecarpifolia, Astragalus anisacanthus, Persicaria capitata, Polygonum aviculare, and Polypodium sibiricum had maximum RFC.
The Informant Consent Factor (ICF) specifies consistency of understanding among respondents regarding ethnomedicinal application of specific plant species to cure diseases. The ICF values range from 0 to 1, and a disease category with highest ICF value exhibits maximum consensus of the respondents [98]. The ICF values for various disease categories as mentioned in Table 3 were calculated based on ethnomedicinal information provided by the respondents of different linguistic groups of Kohistan. The ICF values of reported disease categories ranged from 0.65 to 1. The highest number of WMPs were reported against GAS-D disease category, followed by DER-S, OTH, RES-R and OTHA-A (ranged from 13 to 40 botanical species). On the other hand, less than 10 species were documented for the remaining disease categories. Likewise, based on use reports major disease categories were in following order: DER-S ≥ RES-R ≥ OTH ≥ OTHA-A ≥ SKE-L ≥ URO-U ≥ Blood-B ≥ GAS-D ≥ CAR-K ≥ NER-N ≥ CAN-C ≥ PRE-W (Table 3). These findings provide valuable insights into the ethnomedicinal practices within different linguistic groups of Kohistan and highlight which diseases have received more attention in terms of herbal remedies. Overall, findings of this study demonstrate the consistency and agreement among respondents regarding the traditional therapeutic uses of specific plant species for various diseases. The results shed light on potential sources for further exploration and development in ethnobotanical research.
Although the NER-N, CAN-C, and PRE-W disease categories showed the highest ICF values (1 for each category), there was a noticeable lack of WMPs usage (1 species for each disease category) and minimal use reports (26 use reports for each disease category). This could be due to the rarity of neurological disorders (NER-N) and cancer (CAN-C) in the study area or a lack of awareness among the local population about these diseases. In the Kohistan region, neurological disorders such as epilepsy, stroke, and trauma are relatively uncommon. Similarly, cancer is also rare, which could be attributed to under-diagnosis or under-reporting. However, it is important to note that certain regions have a high incidence rate of neurological disorders like epilepsy, while globally there is an increasing trend in cancer cases. Even in developed countries, neurological disorders and cancers contribute significantly to morbidity rates. The difference in reported usage might be attributed to limited accessibility or availability of WMPs, cultural taboos, or a lack of recognition by local healers. Nonetheless, it is worth mentioning that despite being the less common ailments in this region, both CAN-C and PRE-W disease categories still showed high ICF values which indicate the perceived utility of WMPs in this region.
While digestive problems (GAS-D), skin diseases (DER-S), and respiratory system disorders (RES-R) have lower ICF values, they still hold significance in the study area. This is evident from the utilization of a high number of botanical taxa for the treatment of these diseases. For instance, 40 WMPs are used to treat digestive problems, 19 species to cure skin diseases, and 17 species for treating respiratory system disorders (Table 2). The largest number of botanical taxa against the above-mentioned diseases revealed prevalence of such heath disorders in the study area, and acceptability of WMPs among different linguistic groups of Kohistan. Our findings align with previous studies [99–102], reporting digestive disorders and skin infections as common health issues in high mountain regions. Similarly, the harsh climatic conditions, high altitude, exposure to UV radiation, and unhygienic practices at both individual and community levels may contribute to the prevalence of these diseases in Kohistan.
Female health issues, particularly during pregnancy and childbirth (PRE-W), are most prevalent in Kohistan. However, due to cultural barriers, collecting information on these diseases is challenging. In certain societies like Kohistani communities, there is a cultural taboo associated with discussing women’s health problems, making it even more difficult to gather data. These practices hinder our understanding of the true extent of female health issues in this region. Additionally, family planning issues are not common as having more children is preferred in Kohistan. Therefore, it is essential to address these challenges and find ways to gather accurate information on female health issues in this region. And that can be only possible by the active participation of female researchers from Kohistan and its allied areas. By doing so, we can develop effective interventions and provide appropriate healthcare services to improve the well-being of women in the Kohistan region.
According to Chen et al. [98], the fidelity level (FL) is an important measure for determining the effectiveness of a medicinal plant species in treating specific diseases compared to other plants used for the same purpose. High fidelity levels indicate that a particular plant species is consistently used by many individuals to treat a particular disease [102]. In our study, we found that 12 WMPs had fidelity levels ranging from 41.67% to 94.44%, demonstrating their significant medical applications within different linguistic groups of Kohistan (Table 3). The highest fidelity level of 94.44% was observed for Myrtus communis in treating skin diseases, specifically eczema, followed by Mentha longifolia with a fidelity level of 92.86% (Fig. 6), commonly used for digestive disorders such as diarrhea and indigestion (GAS-D). Interestingly, this finding aligns with Ahmad et al. [103] report on local communities in Madyan valley, Swat Pakistan, where similar species was utilized against gastrointestinal disorders. While it appears that M. communis has not been previously documented for its effectiveness in skin diseases. However, Haq [69] reported that inhabitants of Allai valley in the western Himalayan region of Pakistan use the same species to alleviate bronchial congestion. Likewise, Ajuga integrifolia, Ziziphus jujuba, Clematis grata, Lepidium sativum, Artemisia brevifolia, Verbascum thapsus, and Datisca cannabina have shown fidelity levels of ≥ 60% against various diseases (Table 3). The inhabitants of Kohistan utilize the leaves of A. integrifolia to alleviate fever, skin infections, and purify blood. Conversely, Ozturk et al. [24] stated that the same plant species is used to address hypertension in different regions of Turkey, Pakistan, and Malaysia. Similarly, Muhammad et al. [104] have reported a fidelity level of 100% for Z. jujuba from Malakand division KP, Pakistan in relation to lactation support and the treatment of skin disorders, gastrointestinal issues, urological conditions respiratory ailments diabetes and insomnia.
Fig. 6.
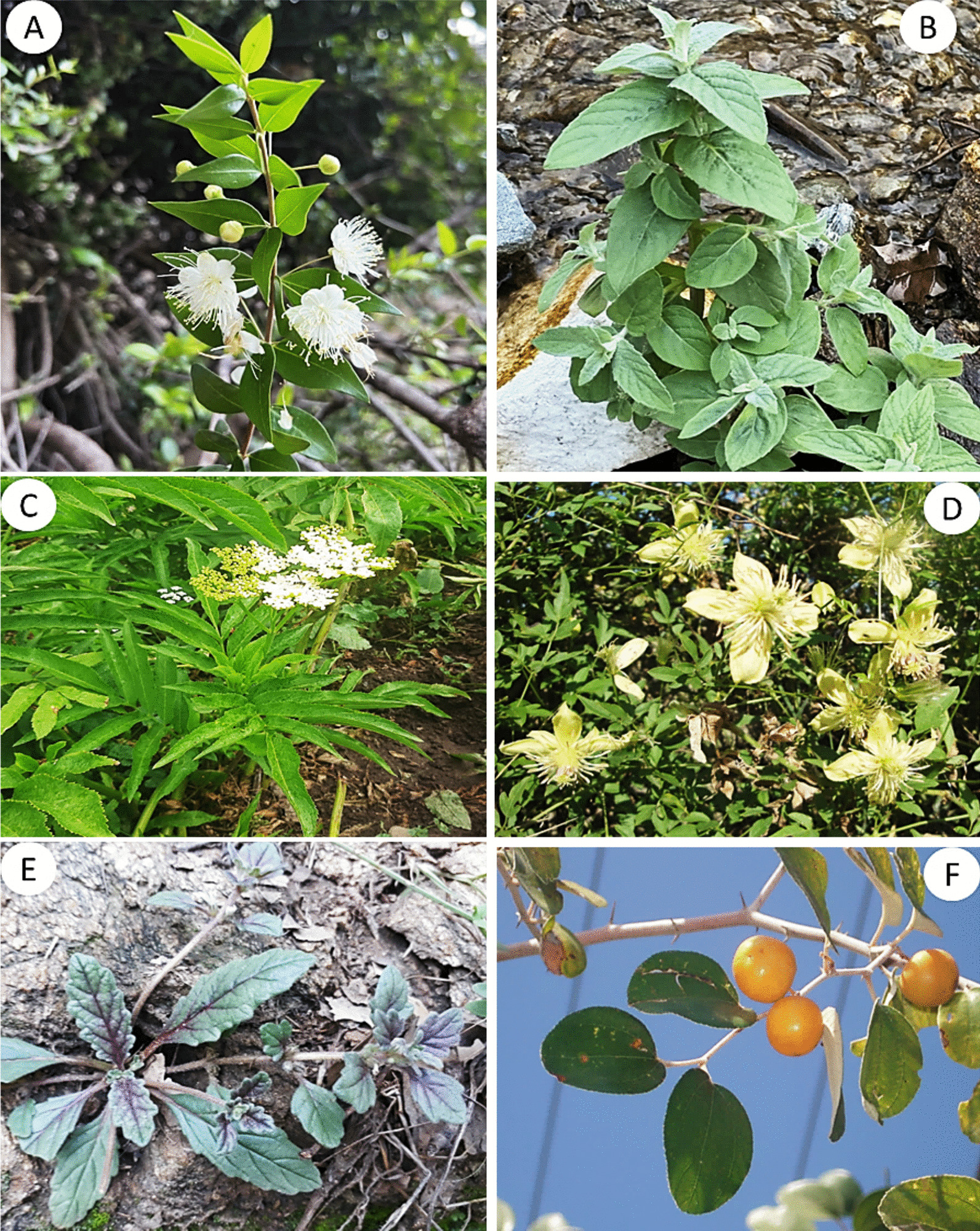
Some highly utilized medicinal plant species A Myrtus communis, B Mentha longifolia, C Sambucus wightiana, D Clematis grata, E Ajuga integrifolia F Ziziphus jujuba
Conversely, the local population in Kohistan employ powdered seeds from Z. jujuba to manage blood pressure levels and promote blood purification. Leaf powder from Clematis grata is orally administered for the treatment of urological disorders, but Rehman et al. [32] have highlighted that same species is used among tribal communities in the Buner region of Pakistan for managing skin infections. The efficacy of decoctions made from L. sativum leaves against asthma aligns with reports by Alamgeer et al. [50]. Inhabitants of Kohistan frequently utilize leaf powder derived from A. artemisiifolia as an anti-rodent and mosquito repellent, and its fidelity level is 64.29%. It should be noted that this utilization contradicted to the findings of Zhao et al. [25] who classify A. artemisiifolia as an invasive weed that poses harm to crops in Europe and Asia. Moreover, this species is also known to produce copious amounts of allergenic pollen grains that can adversely affect human health [105]. The fidelity level of V. thapsus in alleviating labor pain and respiratory disorders was found to be 58.33%, while D. cannabina demonstrated has FL 57.14% in reducing joint swelling. It is worth noting that Khan et al. [3] have documented the use of V. thapsus leaves for treating asthma and skin infections among the residents of Kashmir Himalayas, Pakistan. However, the application of this plant species against labor pain remains relatively unexplored in existing local and regional literature. Based on the high FL, we recommend further pharmacological investigations on these WMPs to explore their potential benefits and mechanisms of action.
Cross-culture analysis on the use of the botanical taxa
The cross-cultural analysis conducted among the five linguistic groups in Kohistan has unveiled a notable level of heterogeneity on the medical ethnobotany of the studied groups. Considering the number of plant taxa, the quoted botanical taxa among different linguistic groups are illustrated in Fig. 7. A total of 61 plant taxa (63%) were found to be commonly shared across all groups for the treatment of various health issues. However, a noteworthy exception was found in the Shina community, residing in the Himalayan sites of Kohistan, which reported the highest number of unique medicinal plant taxa. The unique taxa reported by the different groups are as follows: Shina: Aconitum chasmanthum, Juniperus excelsa, Leontopodium himalayanum, Oxyria digyna, Pedicularis oederi, Primula elliptica, P. macrophylla, Pteridium aquilinum, Rheum emodi, Rhodiola integrifolia, Ricinus communis, Rumex nepalensis, and Taraxacum campylodes (refer to Table 2 for detailed information). Bateri: Buxus wallichiana, Daphne mucronate, Dysphania botrys, Hypericum oblongifolium, Silene conoidea, Solanum virginianum, Sonchus arvensis, and Zanthoxylum armatum. Gujars: Caltha palustris and Cirsium arvense. Pushton: Artemisia gmelinii and A. stechmanniana. Kohistani: Clematis grata, Clinopodium vulgare, Persicaria capitata, Polygonatum multiflorum, Polygonum aviculare, Polypodium sibiricum, Rubus fruticosus, Rumex abyssinicus, Solanum miniatum, and Bistorta amplexicaulis.
Fig. 7.
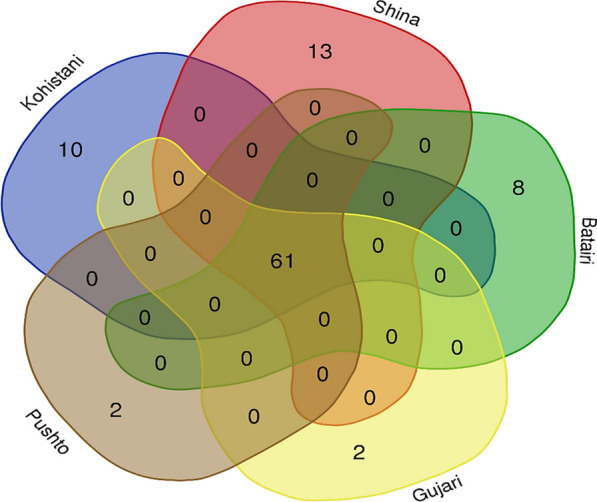
Medicinal plant taxa reported by all linguistic groups
The complex web of medicinal uses of the commonly used plants among the various groups is shown in Fig. 8. Venn diagram elucidates the intricate tapestry of medicinal plant utilization within these linguistic communities. Out of the total 109 documented medicinal uses, approximately 1.83% of the quoted uses were found to be shared across all linguistic groups. We have observed that 12.84% of the uses do overlap among the plant uses of Kohistani, Shina, and Gujjari. It is also important that close affinities (36 uses commonly along 33.02%) on the uses lie between Shina and Kohistani and this may be due their cultural and social dominancy and their social interactions might lead them to share and retain knowledge.
Fig. 8.
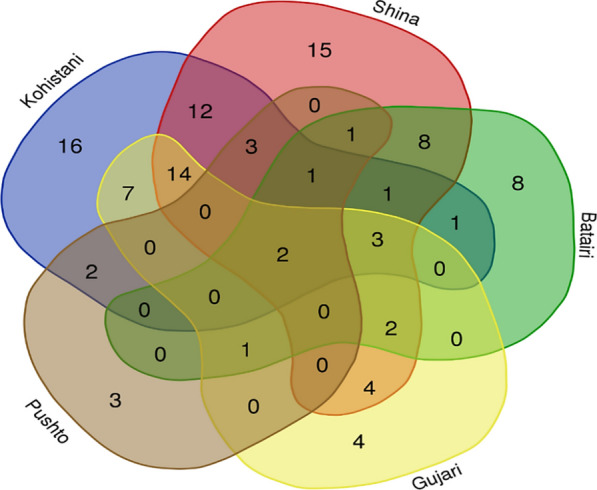
Comparison of medicinal uses mentioned by different linguistic groups
Most of the communal land is owned by these two groups in Kohistan and therefore is evident that these have been the original inhabitants of the study area for generations. The Kohistani and Shinaki people have shared sufficient idiosyncratic uses of plant species, while Bateri also emerged along with them. The Bateri linguistic group who claim to be autochthonous to the study area have some interactions with Kohistani, and we have observed the names of some plants who shared them with Shina although the fact is that their language is branch of Kohistani languages. Despite claiming indigenous roots in Kohistan, the Bateri population has diminish gradually in size over time and now only concentrated in the Bateri village, nestled within the Himalayan expanse of Kohistan-an area. Although Bateri is a linguistic minority in Kohistan, the distinctive wealth of traditional knowledge on idiosyncratic medicinal uses of wild plant species among them can be attributed to their ancestral knowledge, strong association with traditional health care system, historical marginalization, and to some extent due to intermarriage with Kohistani and Shinaki communities.
Within the broader context of Kohistan, Shina speakers (Shinaki) and Kohistani constitute the predominant linguistic groups, collectively spanning almost 80% of the region. The Shinaki groups assert dominance in the Himalayan regions, while the Kohistani communities prevail along the Hindu Kush Mountain range, flanking the right and left banks of the Indus River, respectively. Despite the abundant diversity of medicinal plants in both mountainous terrains, the Kohistani and Shina groups reported relatively fewer medicinal uses, documenting 27 and 26, respectively. As reported earlier [106, 107], discernible impact of modernization, encapsulating factors such as enhanced education, migration, and urbanization, is evident within Kohistan, and Shina linguistic groups is leading to a discernible decline in traditional knowledge. Adding a layer of complexity, the migratory patterns of the Shinaki people of Jalkot and allied areas offer insights into their traditional knowledge. During the summer, these communities typically migrate toward subalpine and alpine pastures where the above-mentioned botanical taxa are commonly found. As a result, the Shinaki people possess an intimate understanding of the medical applications of these unique plant species prevalent in the alpine and subalpine regions. The Pushton and Gujjari communities, often perceived as non-native in Kohistan, are confined to specific geographical areas. The Gujjari people, primarily nomadic, exhibit a preference for alpine and subalpine valleys and pastures. In contrast, a limited population of Pushto speakers resides in the lower regions of Kohistan along the River Indus. This limited dissemination of traditional knowledge is attributed to the tendency of Gujjari community to preserve such knowledge within the confines of their own family circles. The exploration of plant resource utilization among diverse ethnolinguistic groups unveils a fascinating tapestry of both homogeneity and heterogeneity [1, 108–110].
Novelty in reported WMPs
Comparative assessment of ethnomedicinal uses reported by different linguistic groups of Kohistan (as shown in Table 2) with previously reported literature revealed that out of ninety-six documented WMPs about 90% have already been reported from different areas of Pakistan and neighboring regions. However, to best of our knowledge, 10 botanical taxa, namely Leontopodium himalayanum, Pedicularis oederi, Plocama brevifolia, Polypodium sibiricum, Pteridium esculentum, Sambucus wightiana, Solanum cinereum, Teucrium royleanum, Rhodiola integrifolia, and Aconitum chasmanthum, have been reported for the first time (Fig. 9). In addition, although Artemisia stechmanniana, Cirsium verutum, Rubus niveus, Rumex abyssinicus, and Silene conoidea, are used in traditional health care systems of China, Nepal, Bangladesh, Ethiopia, and India [27, 36, 66, 68, 71], they never have been reported as medicinal plant species in Pakistan. Likewise, there were significant variations in plant part(s) used, mode of preparation, application, and types of diseases treated of the commonly reported medicinal plant species. For instance, the aerial parts of Primula elliptica and P. macrophylla are used in snuff by the inhabitants of Kohistan, but roots and flowers of the same species are used to heal wounds and against jaundice in Swat, Pakistan [61]. Likewise, inhabitants of Kohistan use seeds of Ziziphus jujuba as blood purifier; however, fruits and roots of same species were reported to treat diabetes and obesity [53, 79].
Fig. 9.
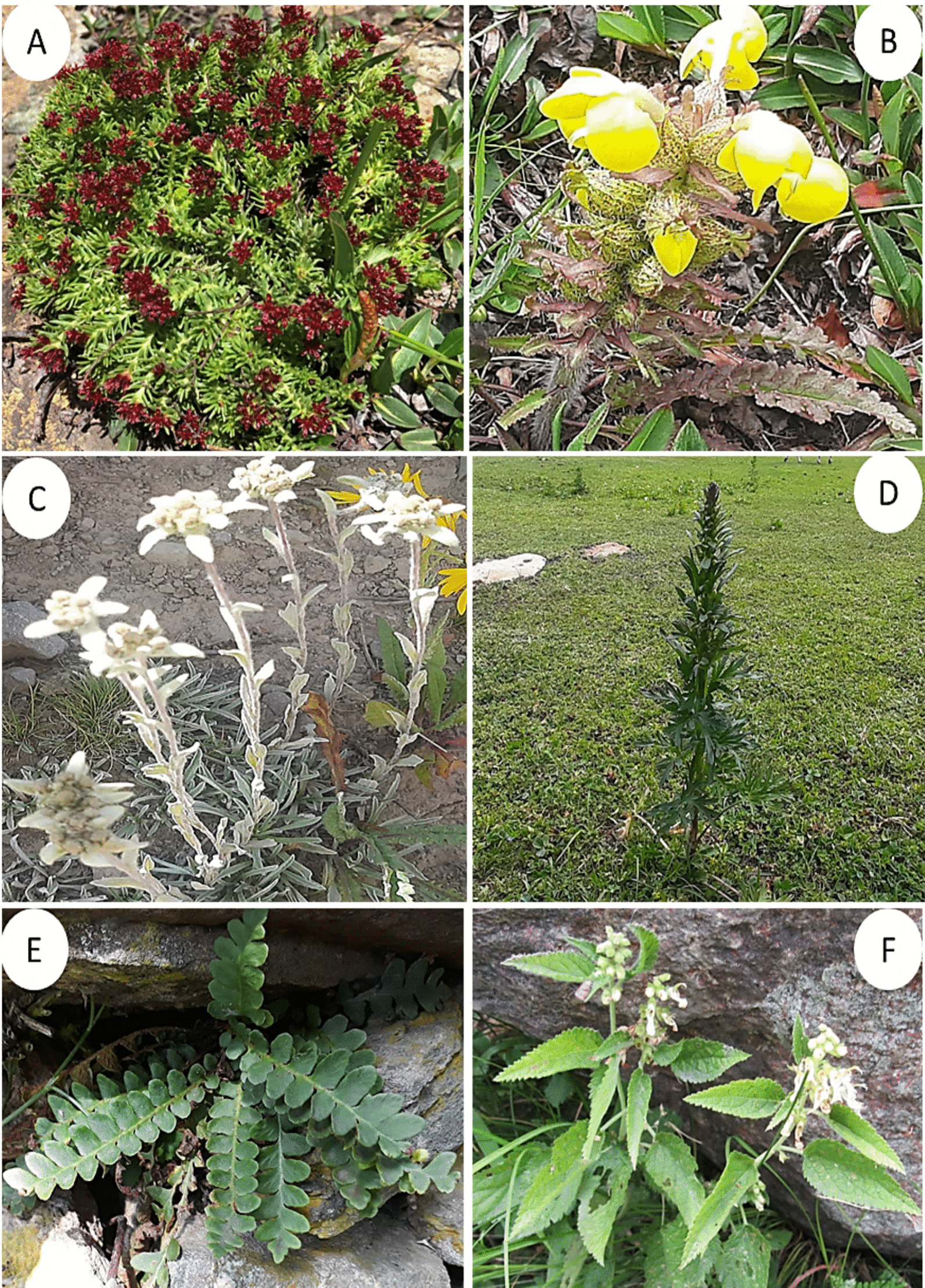
Some newly reported medicinal plants of Kohistan. A Rhodiola integrifolia, B Pedicularis oederi, C Leontopodium himalayanum, D Aconitum chasmanthum, E Pteridium esculentum, F Teucrium royleanum
Threats to ethnomedicinal knowledge of Kohistan
Ethnomedicinal knowledge among various linguistic groups reflects their beliefs, cultural practices, and bioresource management experience [111]. This knowledge, especially among minor groups in mountain regions like northern parts of Pakistan, is at risk of erosion due to challenges like globalization and urbanization [13, 99]. Our research found that the Bateri, a minor group, has significant botanical knowledge for public health, but it is fading due to younger generations’ disinterest and influence from dominant groups like Shina and Kohistani. This loss threatens traditional ethnomedicinal knowledge from this region.
In Kohistan, mega projects like the Dassu and Diamar Bhasha dams are changing lifestyles, leading to cultural erosion and loss of indigenous knowledge. It has also been seen that people migrate to other areas and the economic situation among many households is in transition. Because of this Kohistani people are losing connection to their local natural resources that in turn impact the core body of knowledge and its intergenerational transmission. Young people relocating for better job opportunities further disconnect them from their traditional roots. One of the most important things is that Shina and Kohistani who are the dominant groups in the study area are somehow going through the economic transition as the developmental infrastructures are affecting the localities of the two groups. Therefore, their plant knowledge transmission is more threatened than other groups. Overall, the practical use of local medicinal plants is sufficiently practiced as compared to other parts of the surrounding areas [21, 60, 88, 109, 112].
The absence of written documentation and inclusion in educational curricula exacerbates this loss. We can also use this to make people aware of the importance of natural resources, brochures should be periodically circulated. These brochures should be properly designed, and the relevant ethnobotanical knowledge should be the main material included in that. These brochures should be part of workshops that address the conservation of local flora in schools and colleges in the study area. Thus, preserving this knowledge requires a holistic approach involving government and educational authorities, focusing on conservation, natural resource management, and incorporating traditional knowledge into local education [99]. Moreover, engaging local communities and religious schools in Kohistan is crucial for the success of these conservation efforts, as these communities highly regard instructions from religious leaders. Cultural activities and educational programs can also aid in preserving this knowledge.
Conclusions
The present study was focused on the documentation of ethnomedicinal knowledge on wild plant species in Kohistan and its cross-linguistic comparison among different communities. Comparative assessment revealed some novel botanical taxa and medicinal uses which are valuable additions into the existing stock of ethnomedicinal knowledge and may provide ethnopharmacological basis for novel drug discovery and therapeutic opportunities for preexisting and emerging diseases. In the present study, a compelling observation of significant homogeneity emerged in the reported botanical taxa among different linguistic groups, and ≥ 63% of the plant species, possessing diverse therapeutic properties, were commonly employed across all groups for the treatment of various health disorders. Surprisingly, the Bateri linguistic group (a minority) emerges as a notable outlier, detailing the highest number of medicinal uses of the reported botanical taxa, and the distinctive wealth of traditional knowledge on idiosyncratic medicinal uses of wild plant species among them can be attributed to their ancestral knowledge, strong association with traditional health care system, historical marginalization, and to some extent due to intermarriage with Kohistani and Shinaki communities. Our findings revealed that in the era of modernization, Kohistan still holds a unique biocultural diversity thus proving our hypothesis on rich floristic and cultural diversity of Kohistan and significant ethnomedicinal knowledge of its inhabitants. However, changing live style, shifting socio-economic circumstances, cross-cultural interactions, migration due to remoteness, dominance of major linguistic groups, oral transmission, and lack of proper documented ethnomedicinal knowledge, and ignorance of government and local authorities are multifaceted risks to traditional knowledge and biocultural heritage of Kohistan. In this context, public awareness and education of young generation by the active involvement of education systems “formal and religious” may contribute significantly to the protection, and conservation of biocultural diversity, and ethnolinguistic knowledge in Kohistan. Women in the mountain regions are main custodians of ethnomedicinal knowledge and hence must be given priority in future studies in Kohistan region. Furthermore, phytochemical composition and pharmacological studies should consider wild medicinal plant species of Kohistan having highest RFC, ICF, and FL values.
Acknowledgements
The authors extend their appreciation to the Researchers Supporting Project Number (RSP2024R193), King Saud University, Riyadh, Saudi Arabia, for financial assistance.
Abbreviations
- EMK
Ethnomedicinal knowledge
- MPs
Medicinal plant species
- FDA
Food and drug administration
- KP
Khyber Pakhtunkhwa
- CPEC
China–Pakistan economic corridor
- RFC
Relative frequency citation
- ICF
Informant consent factor
- FL
Fidelity level
- WMPs
Wild medicinal plant species
Author contributions
MA contributed to data curation, formal analysis, methodology, and writing—original draft. MAA was involved in data analysis, writing–review and editing, validation, and visualization. AKM contributed to data curation, methodology, and visualization. AP was involved in conceptualization, writing—review and editing, validation, and visualization. J.A contributed to visualization, writing—review and editing, and funding acquisition. AN was involved in visualization and writing—review and editing. YG contributed to visualization and writing—review and editing. MRAG was involved in visualization, writing—review and editing, and funding acquisition. AMA contributed to conceptualization, project administration, resources, supervision, data analysis, validation, visualization, writing—review and editing, and funding acquisition.
Funding
This study is a part of PhD research work conducted by Mr. Amin “the first author,” and no funding was provided to conduct this research work.
Availability of data and materials
All data are available in this paper.
Declarations
Ethics approval and consent to participate
The research study proposal was approved by the Dean faculty of Science COMSATS University Islamabad, Pakistan, and was subsequently notified by Registrar Secretariat, Academic Unit (PS) COMSATS University Islamabad wide notification No: CUI-Reg/Notif-1671/21/1170 dated May 06, 2021. While conducting the field survey, we meticulously observed the ethical guidelines as recommended by the International Society of Ethnobiology. All the participants provided prior oral consent before the interviews for data collection, photography, and sharing their knowledge and pictures with the public.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Amin M, Aziz MA, Pieroni A, Nazir A, Al-Ghamdi AA, Kangal A, Abbasi AM. Edible wild plant species used by different linguistic groups of Kohistan Upper Khyber Pakhtunkhwa (KP) Pak J Ethnobiol Ethnomed. 2023;19(1):1–23. doi: 10.1186/s13002-023-00577-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan A, Ahmed M, Siddiqi MF, Shah M, Calixto ES, Khan A, Azeem M. Vegetation-environment relationship in conifer dominating forests of the mountainous range of Indus Kohistan in northern Pakistan. J Mt Sci. 2020;17(8):1989–2000. doi: 10.1007/s11629-019-5562-0. [DOI] [Google Scholar]
- 3.Khan A, Ahmed M, Siddiqui MF, Shah M, Hazrat A. Quantitative description, present status and future trend of conifer forests growing in the Indus Kohistan region of Khyber Pakhtunkhwa. Pak Pak J Bot. 2021;53(4):1343–1353. [Google Scholar]
- 4.Ismail I, Sohail M, Gilani H, Ali A, Hussain K, Hussain K, Kotru R. Forest inventory and analysis in Gilgit-Baltistan: a contribution towards developing a forest inventory for all Pakistan. Int J Clim Change Strateg Manag. 2018;10(4):616–631. doi: 10.1108/IJCCSM-05-2017-0100. [DOI] [Google Scholar]
- 5.Khan A, Ahmed M, Siddiqui MF, Iqbal J, Wahab M. Phytosociological analysis of Pine Forest at Indus Kohistan, KPK. Pak Pak J Bot. 2016;48(2):575–580. [Google Scholar]
- 6.Aati H, El-Gamal A, Shaheen H, Kayser O. Traditional use of ethnomedicinal native plants in the Kingdom of Saudi Arabia. J Ethnobiol Ethnomed. 2019;15(1):1–9. doi: 10.1186/s13002-018-0263-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rensch CR. Patterns of language use among the Kohistanis of the Swat valley. Sociolinguistic Surv Northern Pak. 1992;1:3–62. [Google Scholar]
- 8.Zoller CP. A grammar and dictionary of Indus Kohistani. Mouton de Gruyter: Walter de Gruyter; 2005. [Google Scholar]
- 9.Liljegren H. Gender typology and gender (in) stability in Hindu Kush Indo-Aryan languages. Gramm Gender Linguist Complex. 2019;1:279–328. [Google Scholar]
- 10.Frembgen JW. Indus kohistan an historical and ethnographie outline. Cent Asiat J. 1999;43(1):70–98. [Google Scholar]
- 11.Hallberg DG. The languages of Indus Kohistan. Languages of Kohistan. In SSNP-1 1992;83–141.
- 12.Schmidt RL, Zarin MM. The phonology and tonal system of Páalus/kohis' tyó~:/Shina. Münch Stud Sprachwiss. 1981;40:155–185. [Google Scholar]
- 13.Issa M, Khan HK, Hussain MS, Ali MA. Language erosion: an overview of declining status of indigenous languages of Gilgit-Baltistan. Pak Int J Multicult Educ. 2023;25(2):816–828. [Google Scholar]
- 14.Ali SS. Linguistic landscape and the public space: a case study of GilgitBaltistan. Kashmir J Lang Res. 2020;23(1):155–180. [Google Scholar]
- 15.Schmidt RL. A grammatical comparison of Shina dialects. Trends Linguist Stud Monogr. 2004;149:33–56. [Google Scholar]
- 16.Grierson GA. The ormuri or bargista language. Mem Asiat Soc Bengal 1918;7(1).
- 17.Oleary CF. Sociolinguistic survey of northern Pakistan (V1 to V5) Islamabad: National Institute of Pakistan Studies Islamabad Pakistan and Summer Institute of Linguistics; 1992. [Google Scholar]
- 18.ISE. International society of ethnobiology. Code of ethics. 2016. https://www.ethnobiology.net/what-we-do/core-programs/ise-ethics-program/code-of-ethics/. Accessed 1 Oct 2022
- 19.Delpero A, Volpato G. Integrated pond aquaculture and regional identity: ethnobiology of the golden humped tench of Poirino highlands, Northwest Italy. J Ethnobiol Ethnomed. 2022;18(1):1–14. doi: 10.1186/s13002-022-00529-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aziz MA, Ullah Z, Al-Fatimi M, De Chiara M, Sõukand R, Pieroni A. On the trail of an ancient Middle Eastern ethnobotany: traditional wild food plants gathered by Ormuri speakers in Kaniguram. NW Pak Biol. 2021;10(4):302. doi: 10.3390/biology10040302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aziz M, Abbasi AM, Ullah Z, Pieroni A. Shared but threatened: The heritage of wild food plant gathering among different linguistic and religious groups in the Ishkoman and Yasin Valleys, North Pakistan. Foods. 2020;9(5):601. doi: 10.3390/foods9050601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aziz MA, Ullah Z, Adnan M, Sõukand R, Pieroni A. Plant use adaptation in Pamir: Sarikoli foraging in the wakhan area. Northern Pak Biol. 2022;11(10):1543. doi: 10.3390/biology11101543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ali, S. I. and Qaiser, M. eds. Flora of Pakistan. Karachi: University of Karachi; 1993–2009.
- 24.Ozturk M, Altay V, Latiff A, Shareef S, Shaheen F, Iqbal CM. Potential medicinal plants used in the hypertension in Turkey, Pakistan, and Malaysia. Plant Hum Health Vol Ethnobot Physiol. 2018;1:595–618. doi: 10.1007/978-3-319-93997-1_16. [DOI] [Google Scholar]
- 25.Zhao W, Liu T, Sun M, Wang H, Liu X, Su P. Rapid monitoring of Ambrosia artemisiifolia in semi-arid regions based on ecological convergence and phylogenetic relationships. Front Ecol Evol. 2022;10:926990. doi: 10.3389/fevo.2022.926990. [DOI] [Google Scholar]
- 26.Khan SW, Khatoon S. Ethnobotanical studies in Haramosh and Bugrote valleys (Gilgit) Int J Biotechnol. 2004;1(4):584–589. [Google Scholar]
- 27.Kim WH, Jang HJ, Kim J, Jeong CH, Enebish G, Kim SY, Min H. Anti-inflammatory effects of Artemisia stechmanniana Besser extract on LPS-stimulated macrophages. Food Hydrocoll. 2021;32(1):679–692. [Google Scholar]
- 28.Abidin SZU, Munem A, Khan R, Batiha GES, Amhad M, Zafar M, Bhatti MZ. Ethnoveterinary botanical survey of medicinal plants used in Pashto, Punjabi and Saraiki communities of Southwest Pakistan. Vet Med Sci. 2021;7(5):2068–2085. doi: 10.1002/vms3.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ahmad M, Zafar M, Shahzadi N, Yaseen G, Murphey TM, Sultana S. Ethnobotanical importance of medicinal plants traded in Herbal markets of Rawalpindi-Pakistan. J Herbal Med. 2018;11:78–89. doi: 10.1016/j.hermed.2017.10.001. [DOI] [Google Scholar]
- 30.Rashid N, Gbedomon RC, Ahmad M, Salako VK, Zafar M, Malik K. Traditional knowledge on herbal drinks among indigenous communities in Azad Jammu and Kashmir. Pak J Ethnobiol Ethnomed. 2018;14(1):1–20. doi: 10.1186/s13002-018-0217-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sulaiman, Shah S, Khan S, Bussmann RW, Ali M, Hussain D, Hussain W. Quantitative ethnobotanical study of Indigenous knowledge on medicinal plants used by the tribal communities of Gokand Valley, District Buner, Khyber Pakhtunkhwa, Pakistan. Plants 2020;9(8):1001. [DOI] [PMC free article] [PubMed]
- 32.Rehman S, Iqbal Z, Qureshi R, Ur Rahman I, Khan MA, Elshaer M, Abu Bakr Elsaid NM. Ethnogynaecological knowledge of traditional medicinal plants used by the indigenous communities of north Waziristan, Pakistan. Evid-Based Complement Altern Med. 2022;2022(1):6528264. doi: 10.1155/2022/6528264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ayoub M, Saeed M, Saeed S, Saeed A, Ahmad M. Ethnobotanical survey and utilization of medicinal and food plants of Panjgur Balochistan, Pakistan. Asian J Ethnobiol 6(1).
- 34.Haq F, Ahmad H, Alam M. Traditional uses of medicinal plants of Nandiar Khuwarr catchment (District Battagram) Pak J Med Plants Res. 2011;5(1):39–48. [Google Scholar]
- 35.Umair M, Altaf M, Abbasi AM. An ethnobotanical survey of indigenous medicinal plants in Hafizabad district. Punjab-Pak PloS One. 2017;12(6):e0177912. doi: 10.1371/journal.pone.0177912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adhikari M, Thapa R, Kunwar RM, Devkota HP, Poudel P. Ethnomedicinal uses of plant resources in the Machhapuchchhre rural municipality of Kaski District, Nepal. Medicines. 2019;6(2):69. doi: 10.3390/medicines6020069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ajaib M, Ishtiaq M, Bhatti KH, Hussain I, Maqbool M, Hussain T, Bashir R. Inventorization of traditional ethnobotanical uses of wild plants of Dawarian and Ratti Gali areas of District Neelum, Azad Jammu and Kashmir Pakistan. PLoS ONE. 2021;16(7):e0255010. doi: 10.1371/journal.pone.0255010. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 38.Afzal S, Afzal N, Awan MR, Khan TS, Gilani A, Khanum R, Tariq S. Ethno-botanical studies from Northern Pakistan. J Ayub Med Coll Abbottabad. 2009;21(1):52–57. [PubMed] [Google Scholar]
- 39.Ahmed E, Arshad M, Saboor A, Qureshi R, Mustafa G, Sadiq S, Chaudhari SK. Ethnobotanical appraisal and medicinal use of plants in Patriata, New Murree, evidence from Pakistan. J Ethnobiol Ethnomed. 2013;9(1):1–10. doi: 10.1186/1746-4269-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sharif A, Asif H, Younis W, Riaz H, Bukhari IA, Assiri AM. Indigenous medicinal plants of Pakistan used to treat skin diseases: a review. Chin Med. 2018;13(1):1–26. doi: 10.1186/s13020-018-0210-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Younis W, Asif H, Sharif A, Riaz H, Bukhari IA, Assiri AM. Traditional medicinal plants used for respiratory disorders in Pakistan: a review of the ethno-medicinal and pharmacological evidence. Chin Med. 2018;13(1):1–29. doi: 10.1186/s13020-018-0204-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iqbal MS, Ahmad KS, Ali MA, Akbar M, Mehmood A, Nawaz F, Bussmann RW. An ethnobotanical study of wetland flora of Head Maralla Punjab Pakistan. PLoS ONE. 2021;16(10):e0258167. doi: 10.1371/journal.pone.0258167. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 43.Arshad M, Ahmad M. Ethnobotanical study of Galliyat for botanical demography and bioecological diversification. Ethnobotan Leafl. 2005;2004(1):4. [Google Scholar]
- 44.Hussain S, Hamid A, Ahmad KS, Mehmood A, Nawaz F, Ahmed H. Quantitative ethnopharmacological profiling of medicinal shrubs used by indigenous communities of Rawalakot, District Poonch, Azad Jammu and Kashmir, Pakistan. Rev Bras. 2019;29:665–676. [Google Scholar]
- 45.Ahsan AAMUH, Chaudhary UHHMA. Traditional medicines of plant origin used for the treatment of inflammatory disorders in Pakistan: a review. J Tradit Chin Med. 2018;38(4):636–656. doi: 10.1016/S0254-6272(18)30897-5. [DOI] [PubMed] [Google Scholar]
- 46.Amber R, Adnan M, Tariq A, Mussarat S. A review on antiviral activity of the Himalayan medicinal plants traditionally used to treat bronchitis and related symptoms. J Pharm Pharmacol. 2017;69(2):109–122. doi: 10.1111/jphp.12669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rahman IU, Ijaz F, Iqbal Z, Afzal A, Ali N, Afzal M, Asif M. A novel survey of the ethno medicinal knowledge of dental problems in Manoor Valley (Northern Himalaya), Pakistan. J Ethnopharmacol. 2016;194:877–894. doi: 10.1016/j.jep.2016.10.068. [DOI] [PubMed] [Google Scholar]
- 48.Nabi S, Al-Kahraman YM, Tahira B, Hajira B, Rasool A, Muhammad A, et al. A review on Juniperus Excelsa: description, distribution and ecology, ethnobotany, and biological activities. Indo Am J Pharm Sci. 2017;4(3):636–644. [Google Scholar]
- 49.Adnan M, Bibi R, Mussarat S, Tariq A, Shinwari ZK. Ethnomedicinal and phytochemical review of Pakistani medicinal plants used as antibacterial agents against Escherichia coli. Ann Clin Microbiol Antimicrob. 2014;13(1):1–18. doi: 10.1186/s12941-014-0040-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alamgeer Uttra AM, Ahsan H, Hasan UH, Chaudhary MA. Traditional medicines of plant origin used for the treatment of inflammatory disorders in Pakistan: a review. J Tradit Chin Med. 2018;38(4):636–656. doi: 10.1016/S0254-6272(18)30897-5. [DOI] [PubMed] [Google Scholar]
- 51.Rehman S, Iqbal Z, Qureshi R, Shah GM. Quantitative ethnobotanical study of medicinal plants used by the indigenous communities of Shawal Valley, District North Waziristan, Pakistan. Ethnobot Res Appl. 2023;25:1–24. [Google Scholar]
- 52.Dutta A, Sharma YP, Bikarma BS, Bussmann RW. Plant-based veterinary practices in Jammu and Kashmir: a review of the trends, transfer, and conservation of traditional ethnoveterinary knowledge. Ethnobot Res Appl. 2022;24:1–24. [Google Scholar]
- 53.Wali R, Khan MF, Mahmood A, Mahmood M, Qureshi R, Ahmad KS, Mashwani ZUR. Ethnomedicinal appraisal of plants used for the treatment of gastrointestinal complaints by tribal communities living in Diamir district, Western Himalayas. Pakistan Plos One. 2022;17(6):e0269445. doi: 10.1371/journal.pone.0269445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Batool S, Ahmed MS. Bistorta amplexicaulis: a brief insight to its ethnobotany. J Bioresour Manag. 2016;3(3):2. [Google Scholar]
- 55.Natarajan B, Paulsen BS, Korneliussen V. An ethnopharmacological study from Kulu District, Himachal Pradesh, India: traditional knowledge compared with modern biological science. Pharm Biol. 2000;38(2):129–138. doi: 10.1076/1388-0209(200004)3821-1FT129. [DOI] [PubMed] [Google Scholar]
- 56.Khan SW, Khatoon S. Ethnobotanical studies on useful trees and shrubs of Haramosh and Bugrote valleys in Gilgit northern areas of Pakistan. Pak J Bot. 2007;39(3):699–710. [Google Scholar]
- 57.Jan G, Khan MA, Gul F. Ethnomedicinal plants used against diarrhea and dysentery in Dir Kohistan valley (NWFP) Pak Ethnobot Leafl. 2008;2008(1):84. [Google Scholar]
- 58.Hamayun M. Traditional uses of some medicinal plants of Swat Valley, Pakistan. Ethnobotanical Leaflets. 2007;2007(1):1. [Google Scholar]
- 59.Sher H, Elyemeni M, Hussain K, Sher H. Ethnobotanical and economic observations of some plant resources from the northern parts of Pakistan. Ethnobot Res Appl. 2011;9:27–42. doi: 10.17348/era.9.0.27-41. [DOI] [Google Scholar]
- 60.Abbasi AM, Khan MA, Shah MH, Shah MM, Pervez A, Ahmad M. Ethnobotanical appraisal and cultural values of medicinally important wild edible vegetables of Lesser Himalayas-Pakistan. J Ethnobiol Ethnomed. 2013;9:1–13. doi: 10.1186/1746-4269-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Khan S, Shaheen H, Mehmood A, Nasar S, Khan T. Ethnobotanical and antibacterial study of Primula plants traditionally used in the indigenous communities of Western Himalaya. Pak Saudi J Biol Sci. 2022;29(5):3244–3254. doi: 10.1016/j.sjbs.2022.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Aziz MA, Adnan M, Khan AH, Rehman AU, Jan R, Khan J. Ethno-medicinal survey of important plants practiced by indigenous community at Ladha subdivision, South Waziristan agency, Pakistan. J Ethnobiol Ethnomed. 2016;12:1–14. doi: 10.1186/s13002-016-0126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hamayun M. Ethnobotany of some useful trees of Hindu-Kush Mountain region: a case study of Swat Kohistan, district Swat. Pak Ethnobot Leafl. 2005;2005(1):1. [Google Scholar]
- 64.Pandith SA, Dar RA, Lattoo SK, Shah MA, Reshi ZA. Rheum australe, an endangered high-value medicinal herb of Northwestern Himalayas: a review of its botany, ethnomedical uses, phytochemistry and pharmacology. Phytochem Rev. 2018;17:573–609. doi: 10.1007/s11101-018-9551-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Daniyal M, Tahir IM, Akram M, Zahid R, Zainab R, Riaz Z, Bin L. Pharmacological effects of Rheum emodi: a multiple purpose plant in health and disease. Pak J Med Biol Sci. 2019;2(1):68. [Google Scholar]
- 66.Uniyal SK, Singh KN, Jamwal P, Lal B. Traditional use of medicinal plants among the tribal communities of Chhota Bhangal, Western Himalaya. J Ethnobiol Ethnomed. 2006;2:1–8. doi: 10.1186/1746-4269-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jan G, Khan MA, Gul F. Ethnomedicinal plants used against jaundice in Dir Kohistan valleys (NWFP) Pak Ethnobot Leafl. 2009;2009(8):7. [Google Scholar]
- 68.Woldemariam G, Demissew S, Asfaw Z. An ethnobotanical study of traditional medicinal plants used for human ailments in Yem ethnic group, south Ethiopia. Ethnobot Res Appl. 2021;22:1–15. [Google Scholar]
- 69.Haq F. The ethno botanical uses of medicinal plants of Allai Valley, Western Himalaya Pakistan. Int J Plant Res. 2012;2(1):21–34. doi: 10.5923/j.plant.20120201.04. [DOI] [Google Scholar]
- 70.Abbas Z, Khan SM, Alam J, Khan SW, Abbasi AM. Medicinal plants used by inhabitants of the Shigar Valley, Baltistan region of Karakorum range-Pakistan. J Ethnobiol Ethnomed. 2017;13(1):1–15. doi: 10.1186/s13002-017-0172-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chandra S, Rawat DS. Medicinal plants of the family Caryophyllaceae: a review of ethno-medicinal uses and pharmacological properties. Integr Med Res. 2015;4(3):123–131. doi: 10.1016/j.imr.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nabi M, Tabassum N, Ganai BA. Skimmia anquetilia NP Taylor and airy shaw (rutaceae): A critical appraisal of its ethnobotanical and pharmacological activities. Front Plant Sci. 2022;13:930687. doi: 10.3389/fpls.2022.930687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Abdullah A, et al. A comprehensive appraisal of the wild food plants and food system of tribal cultures in the Hindu Kush Mountain Range; a way forward for balancing human nutrition and food security. Sustainability. 2021;13(9):5258. doi: 10.3390/su13095258. [DOI] [Google Scholar]
- 74.Aziz MA, Khan AH, Adnan M, Ullah H. Traditional uses of medicinal plants used by Indigenous communities for veterinary practices at Bajaur Agency. Pak J Ethnobiol Ethnomed. 2018;14(1):1–18. doi: 10.1186/s13002-018-0212-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Iqbal H, Sher Z. Medicinal plants from salt range Pind Dadan Khan, district Jhelum, Punjab. Pak J Med Plants Res. 2011;5(11):2157–2168. [Google Scholar]
- 76.Ata S, Farooq F, Javed S. Elemental profile of 24 common medicinal plants of Pakistan and its direct link with traditional uses. J Med Plant Res. 2011;5(26):6164–6168. [Google Scholar]
- 77.Malik K, Ahmad M, Zafar M, Ullah R, Mahmood HM, et al. An ethnobotanical study of medicinal plants used to treat skin diseases in northern Pakistan. BMC Complement Altern Med. 2019;19:1–38. doi: 10.1186/s12906-019-2605-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Iqbal I, Hamayun M. Studies on the traditional uses of plants of Malam Jabba valley, District Swat. Pak Ethnobot Leafl. 2004;2004(1):15. [Google Scholar]
- 79.Ahmad K, Ahmad M, Huber FK, Weckerle CS. Traditional medicinal knowledge and practices among the tribal communities of Thakht-e-Sulaiman Hills, Pakistan. BMC Complement Med Ther. 2021;21:1–21. doi: 10.1186/s12906-021-03403-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ishtiaq M, Maqbool M, Ajaib M, Ahmed M, Hussain I, Khanam H, Ghani A. Ethnomedicinal and folklore inventory of wild plants used by rural communities of valley Samahni, District Bhimber Azad Jammu and Kashmir. Pak Plos One. 2021;16(1):e0243151. doi: 10.1371/journal.pone.0243151. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 81.Vitalini S, Iriti M, Puricelli C, Ciuchi D, Segale A, Fico G. Traditional knowledge on medicinal and food plants used in Val San Giacomo (Sondrio, Italy)—An alpine ethnobotanical study. J Ethnopharmacol. 2013;145:517–529. doi: 10.1016/j.jep.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 82.Ong HG, Kim YD. Quantitative ethnobotanical study of the medicinal plants used by the Ati Negrito indigenous group in Guimaras island, Philippines. J Ethnopharmacol. 2014;157:228–242. doi: 10.1016/j.jep.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 83.Friedman J, Yaniv Z, Dafni A, Palewitch D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. J Ethnopharmacol. 1986;16:275–287. doi: 10.1016/0378-8741(86)90094-2. [DOI] [PubMed] [Google Scholar]
- 84.Idm'hand E, Msanda F, Cherifi K. Ethnobotanical study and biodiversity of medicinal plants used in the Tarfaya Province, Morocco. Acta Ecol Sin. 2020;40:134–144. doi: 10.1016/j.chnaes.2020.01.002. [DOI] [Google Scholar]
- 85.Barth F. Indus and swat kohistan-an ethnographic survey. Oslo: Forenede Trykkerier; 1956. [Google Scholar]
- 86.Gu XJ, Xiao PG. Phytochemical and biological research of Polygoneae medicinal resources. Med Plants. 2015 doi: 10.1016/B978-0-08-100085-4.00012-8. [DOI] [Google Scholar]
- 87.Noor A, Khatoon S, Ahmed M, Razaq A. Ethnobotanical study on some useful shrubs of Astore valley, Gilgit-Baltistan, Pakistan. Bangladesh J Bot. 2014;43(1):19–25. doi: 10.3329/bjb.v43i1.19741. [DOI] [Google Scholar]
- 88.Abbas Z, Kousar S, Aziz MA, Pieroni A, Aldosari AA, Bussmann RW, Abbasi AM. Comparative assessment of medicinal plant utilization among Balti and Shina communities in the periphery of Deosai National Park. Pak Biol. 2021;10(5):434. doi: 10.3390/biology10050434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Abbas Q, Khan SW, Khatoon S, Hussain SA, Hassan SN, Hussain A, Hussain I. Floristic biodiversity and traditional uses of medicinal plants of Haramosh valley Central Karakoram National Park of Gilgit district, Gilgit-Baltistan. Pakistan. J Biol Environ Sci. 2014;5:75–86. [Google Scholar]
- 90.Gang R, Matsabisa M, Okello D, Kang Y. Ethnomedicine and ethnopharmacology of medicinal plants used in the treatment of diabetes mellitus in Uganda. Appl Biol Chem. 2023;66(1):1–41. doi: 10.1186/s13765-023-00797-z. [DOI] [Google Scholar]
- 91.Hussain S, Hussain W, Nawaz A, Badshah L, Ali A, Ullah S, Bussmann RW. Quantitative ethnomedicinal study of indigenous knowledge on medicinal plants used by the tribal communities of Central Kurram, Khyber Pakhtunkhwa, Pakistan. Ethnobot Res Appl. 2022;23:1–31. [Google Scholar]
- 92.Birjees M, Ahmad M, Zafar M, Nawaz S, Jehanzeb S, Ullah F, Zaman W. Traditional knowledge of wild medicinal plants used by the inhabitants of Garam Chashma valley, district Chitral. Pak Acta Ecol Sin. 2022;42(2):19–33. doi: 10.1016/j.chnaes.2020.12.006. [DOI] [Google Scholar]
- 93.Afzal S, Ahmad HI, Jabbar A, Tolba MM, AbouZid S, Irm N, Aslam Z. Use of medicinal plants for respiratory diseases in Bahawalpur, Pakistan. BioMed Res Int. 2021;2021:5578914. doi: 10.1155/2021/5578914. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 94.Jan HA, Jana S, Walia S, Ahmad L, Sisto F, Bussmannd RW, Romman M. Ethnomedicinal study of medicinal plants used to cure dental diseases by the indigenous population of district Buner, Pakistan. Indian J Tradit Knowl. 2021;20(2):378–389. [Google Scholar]
- 95.Verbeke M, Schrans D, Deroose S, De Maeseneer J. The International Classification of Primary Care (ICPC-2): an essential tool in the EPR of the GP. Stud Health Technol Inf. 2006;124:809. [PubMed] [Google Scholar]
- 96.Dabbaghi MM, Fadaei MS, Soleimani Roudi H, Baradaran Rahimi V, Askari VR. A review of the biological effects of Myrtus communis. Physiol Rep. 2023;11(14):e15770. doi: 10.14814/phy2.15770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Medda S, Mulas M. Fruit quality characters of myrtle (Myrtus communis L.) selections: review of a domestication process. Sustainability. 2021;13(16):8785. doi: 10.3390/su13168785. [DOI] [Google Scholar]
- 98.Chen TX, Lia WZ, Hua CG, Chen YL, Zhao TT, Hu JZ, Tang J. Review article ethnobotanical study of miao nationality medicinal plants in Leishan County, Guizhou Province, China. J Herbal Med. 2023;41:100686. doi: 10.1016/j.hermed.2023.100686. [DOI] [Google Scholar]
- 99.Aziz MA, Hassan M, Ullah A, Ullah Z, Sõukand R, Pieroni A. Keeping their own and integrating the other: medicinal plant use among Ormurs and Pathans in South Waziristan. Pak J Ethnobiol Ethnomed. 2023;19(1):1–24. doi: 10.1186/s13002-023-00634-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bouafia M, Amamou F, Gherib M, Benaissa M, Azzi R, Nemmiche S. Ethnobotanical and ethnomedicinal analysis of wild medicinal plants traditionally used in Naâma, southwest Algeria. Vegetos. 2021;34:654–662. doi: 10.1007/s42535-021-00229-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Amjad MS, Zahoor U, Bussmann RW, Altaf M, Gardazi SMH, Abbasi AM. Ethnobotanical survey of the medicinal flora of Harighal, Azad Jammu & Kashmir, Pakistan. J Ethnobiol Ethnomed. 2020;16:1–28. doi: 10.1186/s13002-020-00417-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tamene S, Addisu D, Debela E. Ethno-medicinal study of plants in Boricha district: Use, preparation and application by traditional healers, Southern Ethiopia. J Med Plants Res. 2020;14(7):343–353. [Google Scholar]
- 103.Ahmad N, Anwar S, Fazal H, Abbasi BH. Medicinal plants used in indigenous therapy by people of Madyan Valley in district Swat, Pakistan. Int J Med Aromat Plants. 2013;3(1):47–54. [Google Scholar]
- 104.Muhammad N, Uddin N, Khan MKU, Mengjun L, Xuan Z, Ali N, Liu Z. Ethnomedicinal and cultural uses of Ziziphus species in flora of Malakand Division KP, Pakistan. Singapore J Sci Res. 2020;10(1):1–7. doi: 10.3923/sjsres.2020.1.7. [DOI] [Google Scholar]
- 105.Hamaoui-Laguel L, Vautard R, Liu LI, Solmon F, Viovy N, Khvorostyanov D, Epstein MM. Effects of climate change and seed dispersal on airborne ragweed pollen loads in Europe. Nat Clim Chang. 2015;5(8):766–771. doi: 10.1038/nclimate2652. [DOI] [Google Scholar]
- 106.Arjona-García C, Blancas J, Beltrán-Rodríguez L, López Binnqüist C, Colín Bahena H, Moreno-Calles AI, López-Medellín X. How does urbanization affect perceptions and traditional knowledge of medicinal plants? J Ethnobiol Ethnomed. 2021;17(1):1–26. doi: 10.1186/s13002-021-00473-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Saynes-Vásquez A, Caballero J, Meave AJ, Chiang F. Cultural change, and loss of ethnoecological knowledge among the Isthmus Zapotecs of Mexico. J Ethnobiol Ethnomed. 2013;9(40):1–5. doi: 10.1186/1746-4269-9-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yao R, He C, Xiao P. ‘Food and medicine continuum’in the East and West: old tradition and current regulation. Chin Herbal Med. 2023;15(1):6–14. doi: 10.1016/j.chmed.2022.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Haq SM, Hassan M, Bussmann RW, Calixto ES, Rahman IU, Sakhi S, Ali N. A cross-cultural analysis of plant resources among five ethnic groups in the Western Himalayan region of Jammu and Kashmir. Biology. 2022;11(4):491. doi: 10.3390/biology11040491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Majeed M, Bhatti KH, Pieroni A, Sõukand R, Bussmann RW, Khan AM, Amjad MS. Gathered wild food plants among diverse religious groups in Jhelum District, Punjab. Pak Foods. 2021;10(3):594. doi: 10.3390/foods10030594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Pieroni A, Vandebroek I. Traveling cultures and plants: the ethnobiology and ethnopharmacy of human migrations. 1. New York: Berghahn Books; 2009. [Google Scholar]
- 112.Ali A, Badshah L, Hussain F. Ethnobotanical appraisal and conservation status of medicinal plants in Hindukush Range, District Swat, Pakistan. J Herbs Spices Med Plants. 2018;24(4):332–355. doi: 10.1080/10496475.2018.1510456. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available in this paper.