Abstract
Patients, often with underlying rheumatologic disease, may present with pericardial effusions in the setting of pulmonary hypertension (PHTN). Pericardial drainage in PHTN is associated with significant morbidity and mortality. We describe a patient with PHTN who developed cardiac tamponade that was managed safely and effectively with pulmonary artery catheter–guided pericardiocentesis.
Key Words: pericardial tamponade, pericardiocentesis, pulmonary artery catheter, pulmonary arterial hypertension
Graphical abstract
History of Presentation
A 33-year-old woman with a history of rheumatoid arthritis and systemic sclerosis overlap syndrome, pulmonary arterial hypertension (PAH), diabetes, obesity, and hypertension presented with 5 days of dyspnea, myalgias, and World Health Organization functional class III symptoms. Admission transthoracic echocardiography (TTE) showed a left ventricular ejection fraction of 55%, right ventricular (RV) dilation and hypertrophy, pulmonary artery systolic pressure of 68 mm Hg, and a moderate pericardial effusion without tamponade physiology. She underwent gentle diuresis with near resolution of her respiratory symptoms.
Learning Objectives
-
•
To recognize typical and atypical echocardiographic and hemodynamic features of cardiac tamponade in patients with pulmonary hypertension.
-
•
To describe the pathophysiology of hemodynamic failure following pericardial drainage in patients with pulmonary hypertension, and how real-time hemodynamics may detect early RV failure.
On hospital day 7, she had acute worsening of dyspnea, pleuritic chest pressure, nausea, and emesis. She was tachycardic to 150 beats/min, hypotensive to 74/48 mm Hg requiring vasopressor initiation, and hypoxic requiring 10 L supplemental oxygen. She had distended neck veins, distant heart rounds, and lower extremity edema.
Past Medical History
She was diagnosed with PAH 5 months prior, with right heart catheterization (RHC) demonstrating a mean pulmonary arterial pressure of 45 mm Hg, pulmonary capillary wedge pressure of 8 mm Hg, and pulmonary vascular resistance of 10.5 Wood units with negative vasoreactivity testing (Table 1). She was initiated on riociguat and macitentan, but macitentan was discontinued because of angioedema. Subsequently, because of rapid progression of her symptoms and progressive RV dysfunction, she was initiated on intravenous epoprostenol and maintained on this leading up to admission.
Table 1.
RHC Values Obtained 5 Months Before Presentation, on Hospital Day 1, on Hospital Day 7 Before Pericardiocentesis, and on Hospital Day 7 Immediately After Pericardiocentesis
| RHC |
||||
|---|---|---|---|---|
| 5 Months Prior | Hospital Day 1 | Hospital Day 7 Pre-Pericardiocentesis |
Hospital Day 7 Post-Pericardiocentesis |
|
| Relevant medications | None | Riociguat Epoprostenol |
Riociguat Epoprostenol Norepinephrine 0.2 μg/kg/min |
Riociguat Epoprostenol Norepinephrine Off |
| BP, mm Hg | 117/83 | 109/74 | 74/48 | 112/69 |
| Heart rate, beats/min | 98 | 181 | 133 | |
| RA, mm Hg | 17 | 17 | 28 | 17 |
| RV, mm Hg | 62/2 | 65/5 | 59/28 | |
| PASP, mm Hg | 65 | 68 | 62 | 63 |
| PADP, mm Hg | 29 | 23 | 35 | 44 |
| MPAP, mm Hg | 43 | 45 | 48 | 50 |
| PCWP, mm Hg | 8 | 15 | 24 | 39 |
| MvO2, % | 62 | 58 | 32 | 61 |
| Hgb, g/dL | 13.1 | 10.1 | 10.8 | 10.8 |
| Fick CO, L/min | 4.3 | 5.9 | 2.8 | 4.2 |
| Fick CI, L/min/m2 | 2.3 | 3.0 | 1.5 | 2.2 |
| PVR, WU | 8.1 | 5.1 | 8.6 | 2.6 |
| Pericardial opening pressure, mm Hg | 25 | 10 | ||
BP = blood pressure; CI = cardiac index; CO = cardiac output; Hgb = hemoglobin; MPAP = mean pulmonary artery pressure; MvO2 = mixed venous oxygen saturation; PADP = pulmonary artery diastolic pressure; PASP = pulmonary artery systolic pressure; PCWP = pulmonary capillary wedge pressure; PVR = pulmonary vascular resistance; RA = right atrium; RHC = right heart catheterization; RV = right ventricle.
Investigations
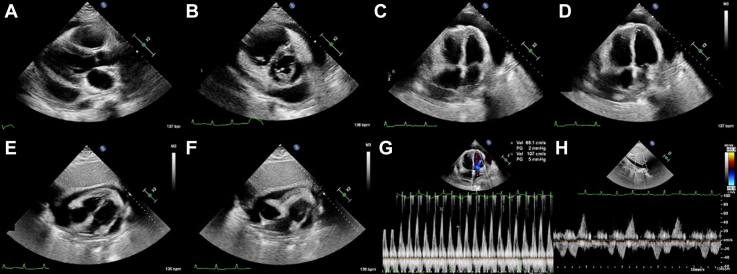
Emergent TTE on hospital day 7 demonstrated a large circumferential pericardial effusion with RV diastolic buckling and significant mitral respiratory inflow variation consistent with cardiac tamponade (Figure 1, Video 1). RHC demonstrated elevated biventricular filling pressures, diastolic equalization of pressures, and a Fick cardiac index of 1.3 L/min/m2 (Table 1).
Figure 1.
Transthoracic Echocardiogram Demonstrating Pericardial Tamponade in the Setting of Severe Pulmonary Hypertension
(A) The parasternal long-axis view demonstrating a large circumferential pericardial effusion with right ventricular (RV) outflow tract dilatation. (B) The parasternal short-axis view highlighting significant RV enlargement and a circumferential pericardial effusion. (C) The apical 4-chamber view in diastole demonstrating significant RV enlargement, a large circumferential pericardial effusion, and basal RV diastolic buckling. (D) The apical 4-chamber view at end-systole demonstrating left atrial systolic collapse. (E) The subcostal view in end-systole demonstrating large circumferential pericardial effusion, RV hypertrophy in this patient with known pulmonary hypertension, and left atrial systolic collapse. (F) The subcostal view in diastole demonstrating RV-free wall buckling consistent with tamponade physiology. (G) Mitral inflow velocities demonstrating significant respiratory variation (36%) consistent with pericardial tamponade. (H) Pulsed wave Doppler of the hepatic vein demonstrating respirophasic systolic flow reversal consistent with pericardial tamponade.
Management
Given the concerns for acute RV failure in patients with PAH who undergo pericardiocentesis, a multidisciplinary decision was made between cardiology, pulmonology, and rheumatology to perform an emergent pulmonary artery catheter (PAC) and intrapericardial pressure–guided pericardiocentesis for cardiac tamponade.
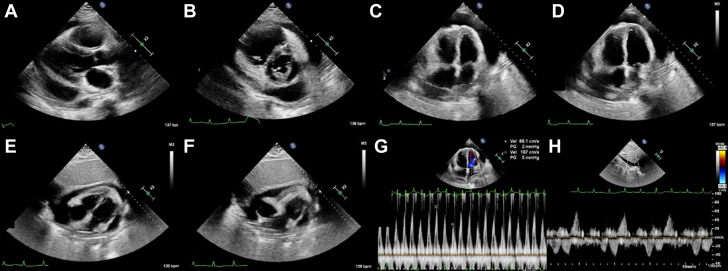
After emergent RHC, echocardiography-guided pericardiocentesis was performed via the subxiphoid approach with continuous monitoring of right atrial (RA) and pericardial pressures. Local anesthesia was administered without sedation given the patient’s tenuous hemodynamic status. The pericardial opening pressure was 23 mm Hg at an RA pressure of 34 mm Hg (Figure 2). After pericardiocentesis of 320 mL, pericardial pressure improved to 10 mm Hg with a Fick cardiac index of 2.2 L/min/m2 (Figure 2). Real-time hemodynamics demonstrated the patient tolerated pericardiocentesis well, with improved vital signs, discontinuation of vasopressors, and an improvement in cardiac output without an increase in RA pressure to suggest impeding RV failure (Table 1).
Figure 2.
Simultaneous Pressure Recordings Obtained From the Right Atrium and Pericardium Before, During, and After Pericardiocentesis
(A) Pressure recordings obtained from the right atrium (RA) and pericardium (P) before pericardiocentesis demonstrating right atrial (RA) pressure of 34 mm Hg and pericardial opening pressure of 23 mm Hg. (B) Pressure recordings obtained following pericardiocentesis of 200 mL serosanguinous pericardial effusion demonstrating RA pressure of 31 mm Hg and pericardial pressure of 16 mm Hg. (C) Pressure recordings immediately following pericardiocentesis of 320 mL serosanguinous pericardial effusion demonstrating RA pressure of 30 mm Hg and pericardial pressure of 12 mm Hg.
Discussion
Pericardial effusions may be seen in up to 25% of patients with PAH and are independently associated with increased mortality within this group.1,2 With elevated right-sided filling pressures, classic findings of tamponade may be absent because the right heart is relatively resistant to the effects of increased pericardial pressures. Accordingly, hemodynamic collapse may occur in the absence of RA and RV inversion or pulsus paradoxus.3,4 Atypical tamponade with isolated left atrial and ventricular collapse has been described in this population.3,4
In our case, emergent TTE demonstrated RV diastolic buckling without atrial collapse. Subsequent TTE demonstrated the presence of heterogeneous material adherent to the visceral pericardium, suspected inflammatory in etiology, which likely contributed to selective tamponade of the right ventricle. It is particularly interesting that the patient developed tamponade physiology several days into her admission and remains unclear whether this was caused by a progressive inflammatory process, diuresis decreasing RV transmural pressure (ie, RV diastolic pressure minus pericardial pressure), or a combination of the 2.
Management of pericardial effusions in patients with pulmonary hypertension remains particularly challenging and is associated with high morbidity and mortality. The expanding pericardial effusion limits RV transmural pressure. When relieved, a sudden increase in venous return in conjunction with rising transmural pressure may lead to hemodynamic collapse. Through parallel ventricular interdependence, acute RV dilatation in this setting compromises LV filling and may result in circulatory failure.2,5
A case series of 6 patients with PAH and large pericardial effusions found a mortality rate of 50% following either pericardiocentesis or surgical pericardial drainage.6 A more contemporary observational study described successful echocardiography-guided pericardiocentesis for 14 patients with PAH and pericardial effusions without evidence of RV failure immediately following pericardiocentesis or deaths within 48 hours of the procedure. Case reports have described gradual pericardial effusion drainage over several days to mitigate RV dysfunction following pericardiocentesis.7
Our patient underwent serial, low-volume pericardiocentesis over several days, during which time she was noted to intermittently reaccumulate pericardial fluid with rising RA and pulmonary artery diastolic pressures with diastolic equalization. We performed real-time invasive hemodynamic monitoring aimed at detecting any elevation in RA pressure as an index of RV failure with drainage. During gradual pericardial drainage, the presence of a PAC allowed for simultaneous monitoring of rising RA and PA diastolic pressures with or without equalization to discriminate between impending RV failure versus recurrent tamponade physiology, as well as serial monitoring of the cardiac output.
Data are even more limited with respect to pericardial windows for effusions in the setting of PAH. Two observational studies described pericardial windows for a total of 6 patients and did not address the role of pericardial windows for recurrent pericardial effusions in the setting of PAH and underlying rheumatologic illness. Although more data are needed to guide the management of patients with PAH and large pericardial effusions,8 we describe the case of a patient with obstructive shock from cardiac tamponade in the setting of PAH who was managed safely and effectively with serial PAC-guided pericardiocentesis.
Follow-Up
Over subsequent days, the patient underwent gradual PAC-guided pericardiocentesis with improvement in her hemodynamics. We drained small aliquots with the aim of rapidly detecting early evidence of RV failure as would be suggested by rising RA pressure. Simultaneously, pericardial pressure was transduced at bedside by connecting the pericardial drain to a standard arterial pressure transducer. The fall in pericardial pressure below that of the RA and PA diastolic pressure served as a stopping point, consistent with the absence of tamponade physiology.
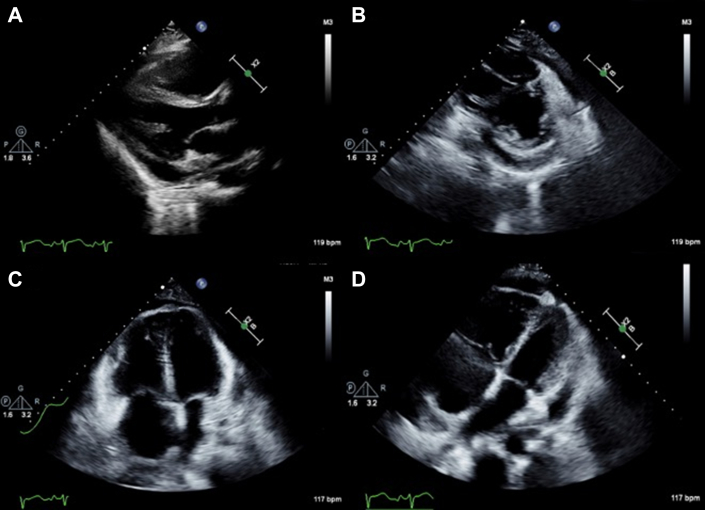
TTE following drain removal demonstrated RV dilation and a small pericardial effusion without tamponade (Figure 3, Video 2). She was maintained on maximally tolerated PAH therapy. It was believed that her underlying rheumatologic disease played a critical role in the pathogenesis of pericardial disease. Immunosuppressive therapy for her rheumatologic overlap syndrome was escalated, and she was discharged home 3 weeks after initial presentation.
Figure 3.
Transthoracic Echocardiogram Demonstrating a Small Residual Pericardial Effusion Following Pulmonary Artery Catheter–Guided Pericardiocentesis
(A) The parasternal long-axis view demonstrating a small circumferential pericardial effusion with posterior localization and right ventricular (RV) outflow tract dilatation. The (B) parasternal short-axis view and (C) apical 4-chamber view demonstrating significant RV enlargement with a small circumferential pericardial effusion. (D) The subcostal view in end-systole demonstrating small circumferential pericardial effusion with significant right heart dilatation.
Conclusions
The presence of pericardial effusions in patients with pulmonary hypertension is associated with significant morbidity and mortality. Although more data are needed to guide the management of the highly comorbid group of patients who present with PAH and pericardial effusions, we describe a safe and effective management strategy with serial PAC-guided pericardiocentesis.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Select Echocardiographic Views Demonstrating Pericardial Tamponade
Parasternal long-axis, parasternal short-axis, apical 4-chamber, and subxiphoid views demonstrating a large, circumferential pericardial effusion with right ventricular diastolic-free wall buckling and left atrial systolic collapse consistent with tamponade physiology.
Select Echocardiographic Views Following Pericardial Effusion Drainage
Parasternal long-axis, parasternal short-axis, and apical 4-chamber views demonstrating a small residual pericardial effusion following pericardiocentesis.
References
- 1.Benza R.L., Miller D.P., Gomberg-Maitland M., et al. Predicting survival in pulmonary arterial hypertension: insights from the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL) Circulation. 2010;122:164–172. doi: 10.1161/CIRCULATIONAHA.109.898122. [DOI] [PubMed] [Google Scholar]
- 2.Sahay S., Tonelli A.R. Pericardial effusion in pulmonary arterial hypertension. Pulm Circ. 2013;3:467–477. doi: 10.1086/674302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adams J.R., Tonelli A.R., Rokadia H.K., et al. Cardiac tamponade in severe pulmonary hypertension. A therapeutic challenge revisited. Ann Am Thorac Soc. 2015;12:455–460. doi: 10.1513/AnnalsATS.201410-453CC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruopp N.F., Schoenberg N.C., Farber H.W. Swan-Ganz and pericardial pressure-guided pericardiocentesis in pulmonary arterial hypertension-associated cardiac tamponade. Ann Am Thorac Soc. 2019;16:1189–1191. doi: 10.1513/AnnalsATS.201902-127CC. [DOI] [PubMed] [Google Scholar]
- 5.Yuriditsky E., Horowitz J.M. The physiology of cardiac tamponade and implications for patient management. J Crit Care. 2023;80 doi: 10.1016/j.jcrc.2023.154512. [DOI] [PubMed] [Google Scholar]
- 6.Hemnes A.R., Gaine S.P., Wiener C.M. Poor outcomes associated with drainage of pericardial effusions in patients with pulmonary arterial hypertension. South Med J. 2008;101:490–494. doi: 10.1097/SMJ.0b013e31816c0169. [DOI] [PubMed] [Google Scholar]
- 7.Vallabhajosyula S., Sundaragiri P.R. Atypical cardiac tamponade in severe pulmonary hypertension. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2014-209187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Honeycutt G.R., Safdar Z. Pulmonary hypertension complicated by pericardial effusion: a single center experience. Ther Adv Respir Dis. 2013;7:151–159. doi: 10.1177/1753465812471416. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Select Echocardiographic Views Demonstrating Pericardial Tamponade
Parasternal long-axis, parasternal short-axis, apical 4-chamber, and subxiphoid views demonstrating a large, circumferential pericardial effusion with right ventricular diastolic-free wall buckling and left atrial systolic collapse consistent with tamponade physiology.
Select Echocardiographic Views Following Pericardial Effusion Drainage
Parasternal long-axis, parasternal short-axis, and apical 4-chamber views demonstrating a small residual pericardial effusion following pericardiocentesis.