Abstract
Background
Identification of latent tuberculosis infection (LTBI) is a critical step of tuberculosis surveillance, especially in low-incidence countries. However, it is limited to situations with a higher probability of developing active disease, e.g., patients with hematological malignancies. According to guidelines, in TB non-endemic countries, no clear screening program is established at diagnosis for patients with acute leukemia (AL). The primary endpoint of this study was to establish the prevalence of LTBI in patients with a diagnosis of AL using QuantiFERON (QFT)-TB. Secondarily, radiological and clinical features driving the increased risk of LTBI were evaluated.
Methods
QFT-TB screening was performed before induction or consolidation in all patients with AL (myeloid and lymphoid) treated at our Institution between October 2019 and August 2023.
Results
We accrued 62 patients, of whom 7 (11,3%) tested positive, without any symptoms or signs of active TB, and 2 (3,2%) resulted as indeterminate. All positive patients started prophylaxis with isoniazid 300 mg daily, while patients whose test was indeterminate did not receive any prophylaxis. Active TB was excluded by imaging, as well as microscopic, cultural, and molecular examination on bronchoalveolar lavage if signs of any infection were detected. During the 46 months of observation, no patients developed TB reactivation.
Conclusions
Despite the low sample size, 1/10 of our patients had prior TB exposure, hinting that LTBI could be more common than expected in Italy. This finding suggests implementing TB screening in the pre-treatment setting, particularly at a time when more active treatments are becoming available also for patients ineligible for intensive chemotherapy.
Keywords: Acute Leukemia, Tuberculosis, Latent tuberculosis infection, Prophylaxis, Acute Myeloid Leukemia, Acute Lymphoblastic Leukemia
Introduction
According to data from the 2023 report published by the World Health Organization and the European Centre for Disease Prevention and Control, Italy is a low tuberculosis (TB) incidence country, with < 20 new cases/100.000 inhabitants.1 Latent tuberculosis infection (LTBI) is defined as the presence of Mycobacterium tuberculosis in individuals without any symptoms or signs of active disease.2
While most individuals with LTBI rarely develop active disease, up to 15% of such cases with concurrent high-risk factors, such as Human Immunodeficiency Virus (HIV) infection, malnutrition, active cancer, solid organ transplant, or hematopoietic stem cell transplantation and immunodepression, may progress to active TB.3–6 Moreover, a variety of environmental situations, workplace, and personal habits concur with increasing the risk of developing active TB.7
Patients with hematologic malignancies and LTBI have a 40 times higher risk of progression to fully-blown disease,4,8 with studies showing the prevalence of up to 30% of LTBI in patients with hematological malignancies, even in those countries that are not TB-endemic.9
According to current guidelines, in non-endemic TB countries, no clear TB screening program is established at diagnosis for patients with acute leukemia (AL), while it is imperative prior to hematopoietic stem cell transplantation. Information about the efficacy and safety of TB preventive treatment in patients with newly diagnosed AL is very limited, and there is a very high heterogeneity in TB screening approaches across Centers of Care for hematological patients at diagnosis. Search for LTBI at diagnosis of AL could provide an opportunity to prompt recognition and subsequent treatment or prophylaxis, thereby lowering morbidity and mortality associated with TB.10
Considering our Italian peninsula, only a few monocentric studies analyzed LTBI prevalence and efficacy of prophylaxis in similar hematological populations, underlining the unmet need to establish further evaluations to confront data from different Centers and geographic areas. According to Bettelli et al., 7,7% of patients with AL or aplastic anemia tested positive for QuantiFERON (QFT)-TB test, concluding that LTBI is not uncommon as expected in low-incidence countries.11 For this reason, it is of great utility to expand current evidence with experiences and data from as many centers as possible to establish a more solid picture of epidemiology in this category of patients and attempt to develop common strategies of intervention. Herein, we aim to study the prevalence of LTBI in our patients with AL.
Material and Methods
Study design and endpoints
This is a retrospective, observational, monocentric study focused on consecutive patients admitted to the Department of Hematology at Policlinico Tor Vergata with a diagnosis of AL (myeloid, lymphoblastic, promyelocytic) who underwent a QFT-TB test from October 2019 to August 2023, with a follow-up period of 1 to 46 months.
The primary endpoint was to establish the LTBI prevalence in patients with a diagnosis of AL using QFT-TB as screening.
Secondary endpoints included the evaluation of any possible correlations between radiological findings and the QFT-TB results.
Setting
Policlinico Tor Vergata, Rome, Italy.
Study Population
We enrolled consecutive patients aged ≥ 18 years, diagnosed with AL according to the 2016 revision to the World Health Organization (WHO) classification12 and risk-stratified according to the European Leukemia Net (ELN) 201713 for patients diagnosed before the updated versions, and then according to the WHO 2022 classification14 and the ELN 2022,15 when available. We selected patients undergoing induction or consolidation treatment, both fit and unfit for intensive treatment. Patients who were candidates for best supportive care were also enrolled in the study. Indeed, the vast majority (n=58/62, 94%) of our patients were tested before induction therapy and only 4 (6%) before consolidation. However, we then focused (as detailed by patient characteristics) on those naïve to treatment.
We collected data on cases that underwent the QFT-TB test (using the QuantiFERON-TB Gold Plus method) from October 2019 to August 2023. The test assessed patients’ TB status: positive, indeterminate, or negative (see below).
QuantiFERON-TB test
QFT-TB Gold Plus from peripheral blood was used to detect M. tuberculosis infection. Briefly, the test evaluated the presence of Interferon Gamma, a cytokine produced after T-cell stimulation by two highly specific M. tuberculosis antigens (ESAT-6 and CFP-10). Moreover, this test was able to differentiate CD4+ and CD8+ -specific cellular responses.
Results could be positive, negative, or indeterminate. A patient was considered positive for M. tuberculosis infection if the IFN-γ response to TB antigens was deemed above the test cutoff. A positive result may result in either latent or active tuberculosis based on radiological imaging and/or microbiological studies as per established guidelines.1
The QFT-TB test in our institute is used in clinical practice for patients with hematological malignancies before the start of treatment.
Statistical Analysis
Patients’ characteristics have been described by frequency tables for qualitative variables and location indicators for quantitative variables. For the univariate analysis, Chi-square or Fisher’s exact test for qualitative variables and Mann-Whitney test for quantitative variables have been used. Confidence intervals have been calculated at 95%, and differences with p < 0.05 have been considered statistically significant. All analyses were performed using IBM SPSS Statistics 25 software.
Data Collection
Data were retrieved and tabulated by revision of patients’ medical records. Variables of major interest included the following: gender, age at diagnosis of AL and at QFT-TB test, type of diagnosis and characteristics (molecular biology and cytogenetic alterations) according to WHO 2016 and 2022 classification, risk according to ELN 2017 and 2022 classification, specific antineoplastic treatments, QFT-TB test results, information on TB preventive treatment, adverse events and possible pharmacological interactions were evaluated according to Common Terminology Criteria for Adverse Events (CTCAE v5.0). Additional epidemiologic data were collected, such as place of birth and living at the moment of diagnosis, work occupation, smoking habits, comorbidities, blood cell count at diagnosis and QFT-TB test, microbiology studies (direct microscopy, blood, and bronchoalveolar lavage cultures, galactomannan assay in serum or bronchoalveolar lavage), and imaging. Data from regular follow-up were collected: date of allogeneic stem cell transplantation (alloHSCT) and date of death.
Computed Tomography (CT) scan was performed using a 256-slice scanner (GE Medical System, Revolution CT) with the following parameters: slice acquisition 2.5 mm, reconstructed to 1.25 with soft tissue windows for mediastinal revision and lung windows for parenchymal revision, pitch 0.5, rotation time 0.7 s, tube voltage 120 kVp, with adaptive mA. Two experienced radiologists reviewed the chest CT scans to assess whether the positivity of the QFT-TB test had a radiological counterpart consistent with a diagnosis of typical or atypical tuberculosis. All patients, regardless of the results of the QFT-TB test, underwent chest CT before starting treatment as part of the initial staging of the disease or due to respiratory symptoms.
Ethics Approval and Consent to Participate
The review and collection of clinical and molecular data were performed in accordance with the protocols and written consent approved by our institution’s Institutional Review Board (number of Ethical Committee approval: 105.23 CET2 PTV) and the guidelines set forth by the Declaration of Helsinki.
Results
From October 2019 to August 2023, a total of 62 consecutive patients (36 male/26 female) were included in the study, of whom 47 (76%) had Acute Myeloid Leukemia (AML), 12 (19%) with Acute Lymphoblastic Leukemia (ALL) and 3 (5%) with Acute Promyelocytic Leukemia (APL). The median age at AL diagnosis was 64 years (range 18–83). Charlson Comorbidity Index (CCI) was used to evaluate comorbidity burden, and the median CCI was 4 (range 2–7).15 Of all patients, 34 (55%) underwent intensive treatment, and 3 proceeded to alloHSCT.
QFT-TB test was performed before induction therapy in 58 (94%) patients and before consolidation in 4 (6%) patients. In our cohort, 7 cases (11,3%) tested positive: 6 (9,6%) before induction chemotherapy and 1 (1,6%) before first consolidation, without any symptoms or signs of active TB. Four patients tested indeterminate: 2 of them (both with a diagnosis of AML) tested negative in a subsequent evaluation, while the remaining 2 (one diagnosed with ALL and the other one with AML) were confirmed as indeterminate.
Several variables were analyzed in an attempt to establish a correlation with QFT-TB test results, but no significant differences were observed, as shown in Table 1.
Table 1.
Variables in the study population according to QFT-TB test results.
| QFT + (n=7) | QFT – (n=53) | p | ||
|---|---|---|---|---|
| Age | Median (range) | 61 (50–83) | 64 (18–83) | 0.3 |
| Sex | Male, n (%) | 3 (43) | 31 (58) | 0.6 |
| Female, n (%) | 4 (57) | 22 (42) | ||
| Foreign born | n (%) | 1 (14) | 6 (11) | 0.9 |
| Smoking habit | n (%) | 4 (57) | 22 (42) | 0.4 |
| Diagnosis | AML, n (%) | 6 (86) | 40 (75) | 0.7 |
| ALL ph+, n (%) | 0 | 3 (6) | ||
| ALL, ph−, n (%) | 1 (14) | 7 (13) | ||
| APL, n (%) | 0 | 3 (6) | ||
| Intensive treatment * | n (%) | 4 (57) | 29 (55) | 0.9 |
| Treatment phase | Induction, n (%) | 6 (86) | 50 (95) | 0.6 |
| Consolidation, n (%) | 1 (14) | 3 (5) | ||
| Neutrophils ** (x10 9 /L) | Median (range) | 0,950 (0,32–3,44) | 650 (20–23.600) | 0.5 |
| Lymphocytes ** (x10 9 /L) | Median (range) | 1,48 (0,74–7,43) | 0,92 (0,16–145,75) | 0.2 |
| Monocytes ** (x10 9 /L) | Median (range) | 0,88 (0,25–5,62) | 0,20 (0–51,07) | 0.1 |
| Bronchoalveolar lavage (BAL) positivity *** | n (%) | 2 (40) | 4 (7) | 0.1 |
| Not performed, n (%) | 2 (28.5) | 25 (47) | ||
| Pulmonary lesion at RX | n (%) | 6 (86) | 23 (42) | 0.2 |
| Not detected, n (%) | 4 (57) | 32 (58) | ||
| Pneumonia of other origin | n (%) | 4 (57) | 25 (47) | 0.8 |
| Comorbidities | HIV infection, n (%) | 0 (0) | 0 (0) | |
| Diabetes, n (%) | 1 (14) | 5 (9) | ||
| COPD, n (%) | 0 (0) | 0 (0) | ||
| Previous cancer, n (%) | 0 (0) | 5 (9) |
Two patients (in the Quantiferon – group) were tested in an off-treatment setting (post-transplant).
A blood test was performed at Quantiferon’s time.
BAL was performed to investigate the direct or indirect presence of bacterial or fungal infection. The 2 Quantiferon + patients were also positive for Pneumocystis jirovecii and Enterococcus faecalis in BAL. Among the 3 Quantiferon – patients, one resulted positive for Pneumocystis jirovecii, one for Enterobacter kobei, and two for Galactomannan.
Abbreviations: AML, Acute Myeloid Leukemia; ALL, Acute Lymphoblastic Leukemia; APL, Acute Promyelocytic Leukemia; QFT, QuantiFERON-TB test; HIV, Human Immunodeficiency Virus; COPD, Chronic Obstructive Pulmonary Disease.
We then focused on potential epidemiological indicators of the 7 patients who tested positive. Three patients (4.8%) had occupational-related risk, but all tested negative for the QFT-TB test, while 22 (35,5%) patients had a smoking habit: Four (57%) of the 7 QFT-positive patients were in this subgroup.
6 (9,6%) of 62 patients were foreign born: 2 patients from Peru, 2 from Romania, 1 from Albania, and 1 from Uganda. Of these, only Uganda and Peru are listed by the World Health Organization as having high TB burden profiles. None of the 62 patients were living in foreign countries. Of the 6 foreign-born patients, just one (1 of the 2 from Romania) tested positive for the QFT-TB test. None of the 62 patients had ever been tested before for tuberculosis, and only 1 (1,6%) of 62 patients referred previous exposure to a relative with active tuberculosis and tested positive for the QFT-TB test. All 62 patients were tested for HIV serology, all resulting negative. Relevant comorbidities are listed in Table 1. None of the 62 patients was undergoing immunomodulatory or steroid therapy at the time of the QFT-TB test.
All 7 positive patients started prophylaxis with isoniazid 300 mg daily with pyridoxine supplementation without any side effects; 4 (57%) of them underwent intensive chemotherapy. No significant pharmacological interactions were recorded, and none of the patients required discontinuation of therapy due to side effects possibly registered with isoniazid (hepatotoxicity, peripheral neuropathy, neurological symptoms). In our QFT-indeterminate subgroup of patients, no prophylaxis was administered without any sign or symptom of subsequent active disease. One of the two QFT-indeterminate patients had more than 100.000/mmc lymphoid blasts at diagnosis of ALL, while the other patient, diagnosed with AML, had more than 10.000/mmc white blood cells at the QFT-TB test.
If lung infiltrates were detected, patients developing febrile neutropenia underwent a chest CT scan and bronchoalveolar lavage (BAL). Imaging, as well as microscopic, cultural, and molecular examination on BAL, excluded active TB when imaging showed suspicious findings of any possible infection. M. tuberculosis was not found on any microbiological or molecular examination performed in QFT-positive patients.
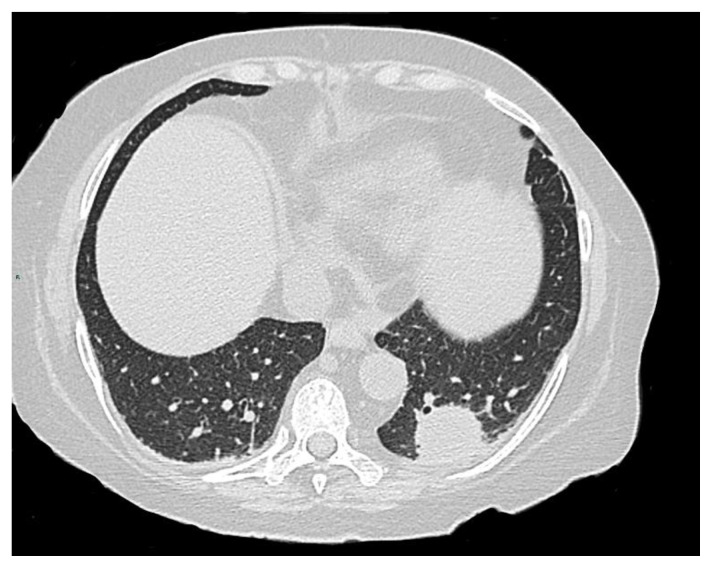
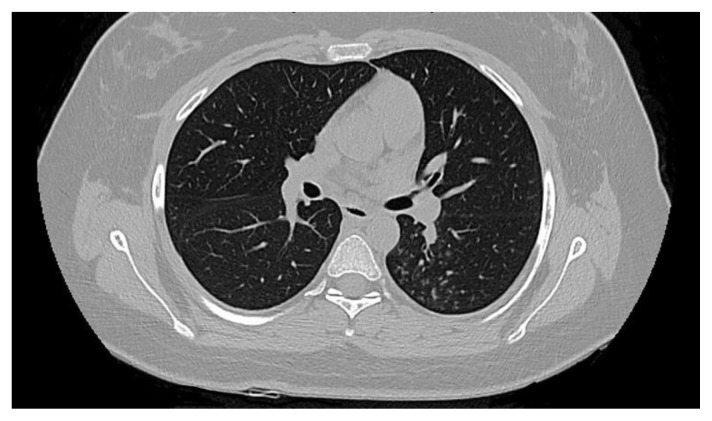
In accordance with the literature, radiologic signs such as cavitation, consolidation (Figure 1), unilateral pleural effusion, pericardial effusion, miliary nodules, centrilobular and tree-in-bud nodules (Figure 2), ground-glass opacity, bronchiectasis, and other more specific signs such as galaxy and marginal sign were sought. The imaging revision by two radiologists demonstrated an interobserver agreement of 100% in the interpretation of CT patterns: 5 of the seven patients with a positive QFT test and 5 of the total number of patients with a negative QFT test had radiological findings indicative of pulmonary infection (71% vs. 9%, respectively; p < 0.001) in the context of febrile neutropenia during induction. All patients with pulmonary infection, regardless of their previous QFT result, underwent BAL, and active TB was excluded through cultural and molecular examination. Given the peculiarity of patients, most of them being neutropenic, radiologic evaluation was challenging, and positive findings were generally interpreted as non-specific (e.g., consolidation, pleural effusion). In the 5 QFT-positive patients, the chest CT scan showed areas of consolidation with air bronchogram. Two of 5 showed a tree-in-bud pattern, 2 carried pleural effusions, and one had ground glass opacities type densitometric changes. Eventually, tree-in-bud patterns and ground-glass opacities were considered typical radiological signs of TB.
Figure 1.
A 76-year-old female patient with acute leukemia and negative QFT. Computed tomography (CT) of the chest shows pulmonary consolidation in the lower lobe of the left lung, a radiological finding similar to tuberculoma. (Courtesy of Dr. F. Di Giuliano and Dr. F. Chirico).
Figure 2.
A 56-year-old male patient with acute leukemia and QFT positivity. CT shows a tree-in-bud radiological pattern in the left lung, a typical finding in post-primary TB. (Courtesy of Dr. F. Di Giuliano and Dr. F. Chirico).
Over the 46-month observation period (median time 6 months, range 1 – 46 months), none of the QFT-positive patients developed TB reactivation. Moreover, 3 (5%) of the 62 patients underwent alloHSCT; 2 with AML received stem cells from 10/10 HLA-identical sibling donors, 1 with ALL underwent alloHSCT from a haploidentical sibling donor after having received Chimeric Antigens Receptor Cells-T (CAR-T). All 3 of these patients were QFT-negative at diagnosis; in addition, the Tuberculin Skin Test performed during the pre-alloHSCT screening was negative in all 3 of them.
Discussion
It is estimated that M. tuberculosis infection affects approximately one-third of the world’s population. TB is especially concerning for individuals with compromised immune systems, such as patients with hematological malignancies. The increased risk in such a setting is due to both the underlying hematological disease and the specific antineoplastic therapies administered.17 Since anti-leukemia treatment could affect the outcome of the test, with possible indeterminate or false negative results, it seems of major utility to evaluate QFT-TB results in the pre-treatment setting. Moreover, LTBI patients with radiological pulmonary lesions suspected to be related to M. tuberculosis infection should be carefully observed during the treatment period, given the well-recognized risk of TB reactivation, even in a disseminated form.18 In our experience, 71% of patients positive for QFT also carried radiological abnormalities consistent with TB.
A relevant issue pertains to the site of M. tuberculosis dwelling during latent infection. It is assumed that latent bacilli primarily reside within fibrotic pulmonary granulomas.19 However, some studies demonstrated the presence of M. tuberculosis DNA not only in the macrophages of old granulomas but also in non-professional phagocytic cells found within histologically normal lung tissue specimens.20,21 This discovery suggests that latent mycobacteria may also exist within non-specialized phagocytic cells residing in other health tissues. This finding bears a critical significance as approximately 15% of TB reactivation cases manifest in extrapulmonary sites.22 Taking this into consideration, performing QFT-TB test in the pre-treatment setting and subsequent TB preventive therapy appears extremely important also for those patients without pulmonary lesions.
Patient-specific factors, such as diabetes, exposure to indoor air pollution, alcohol consumption, immunosuppressive drugs, and smoking, need to be considered possible contributors to the transition from LTBI to the development of active TB. These factors are in addition to widely acknowledged risk factors, e.g., HIV infection, malnutrition, and young age. Moreover, socioeconomic and behavioral habits have been shown to heighten susceptibility to TB infection.23
The diagnosis of LTBI is commonly achieved through two widely used methods: the Tuberculin Skin Test (TST) and Interferon Gamma Release Assays (IGRAs), including the QFT-TB test. In individuals with intact immune systems, the QFT-TB test displays sensitivity similar to the TST but offers improved specificity when it comes to LTBI diagnosis. QFT-TB offers several advantages: it provides numerical results, reduces the potential for bias in interpretation, and does not yield false-positive results due to prior Bacillus Calmette–Guérin (BCG) vaccination. Additionally, QFT-TB offers convenience, eliminating the need for a follow-up visit to interpret the results,24 resulting in more effective and less expensive than TST.25 Nonetheless, a notable drawback of the QFT-TB test is its inability to provide a clear interpretation of the response to TB-specific antigens when an indeterminate result occurs. Abnormalities in the number and differentials of white blood cells have been found to be possible predictors of indeterminate results.26
As regards preventive treatment, few studies have been carried out to evaluate toxicity, adherence to treatment, and possible pharmacological interactions.27 Notably, the latest guidelines on the management of M. tuberculosis infections in patients with hematological malignancies point out the possibility of administering TB preventive therapy in selected cases regardless of TST or IGRA status, considered at high risk of TB infection (e.g., patients with close and long-lasting contact with active pulmonary or laryngeal tuberculosis). On the other hand, they suggest evaluating the prognosis of the hematological malignancy and patients’ characteristics, especially age and therefore decide whether to omit LTBI treatment in individuals with poor prognosis.28
As regards which preventive therapy to use, international guidelines point out the non-inferiority of regimens containing rifamycin in terms of efficacy compared with isoniazid; nevertheless, shorter rifamycin-based treatment shows an improvement in adherence and completion rates.29,30 However, drug-to-drug interactions remain still a concern, not only considering the anti-leukemia specific drugs (e.g., daunorubicin) but also for the relative prophylaxis (e.g., posaconazole) due to the documented CYP450 induction by rifampin.31 Therefore, in our institution, we consider it more practical to administer isoniazid as a preventive treatment, given the non-inferiority in terms of efficacy, even though we are now evaluating the possible administration of rifamycin-based treatment in accordance with our infectious disease specialists.
Early investigation and management can help prevent the progression of TB in this cohort of high-risk patients. This approach is even more relevant with the new emerging cellular therapies, e.g., bispecific antibodies and CAR-T cells, which impact the T-cell compartment even more, the major responsible for controlling LTBI when present.
Even though this study has limitations, such as its retrospective monocentric approach and the low sample size, it may contribute to highlighting that even in countries considered to have low TB burdens, such as Italy, LTBI could be not so uncommon as expected, also given the evolving characteristics and epidemiology of patients.
Considering the increasing globalization, immigration - also from TB-endemic countries - and the fact that patients with hematological malignancies are now receiving more active treatments (including those who may not be eligible for intensive chemotherapy or stem cell transplantation), enforcing TB screening in the pre-treatment setting becomes of critical importance. This approach not only could protect individual patients but may also help prevent the spread of TB in healthcare settings.
Conclusions
Our study adds to the current evidence regarding the prevalence of LTBI in hematological patients, emphasizing the importance of implementing pre-treatment screening approaches for LTBI in this setting, as well as the need to establish consensus guidelines. By doing so, clinicians can develop and share consistent and effective strategies to address the unique challenges presented by this high-risk population. Sharing data and experiences could help identify trends, common risk factors, and the most effective strategies for TB screening and prevention in this heterogeneous population.
Acknowledgments
We would like to thank all the patients who participated in this study; Doctor Stefano Di Carlo and Professor Sergio Bernardini, who provided the laboratory data.
Footnotes
Competing interests: The authors declare no conflict of Interest.
References
- 1.World Health Organization. Tuberculosis surveillance and monitoring in Europe 2023: 2021 data. 2023. [Accessed October 30, 2023]. Available at: https://www.ecdc.europa.eu/sites/default/files/documents/tuberculosissurveillance-monitoring-2023.pdf.
- 2.Getahun H, Matteelli A, Abubakar I, Aziz MA, Baddeley A, Barreira D, Den Boon S, Borroto Gutierrez SM, Bruchfeld J, Burhan E, Cavalcante S, Cedillos R, Chaisson R, Chee CB-E, Chesire L, Corbett E, Dara M, Denholm J, de Vries G, Raviglione M. Management of latent Mycobacterium tuberculosis infection: WHO guidelines for low tuberculosis burden countries. European Respiratory Journal. 2015;46(6):1563–1576. doi: 10.1183/13993003.01245-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Erkens CG, Kamphorst M, Abubakar I, Bothamley GH, Chemtob D, Haas W, Migliori GB, Rieder HL, Zellweger JP, Lange C. Tuberculosis contact investigation in low prevalence countries: a European consensus. Eur Respir J. 2010;36(4):925–49. doi: 10.1183/09031936.00201609. [DOI] [PubMed] [Google Scholar]
- 4.Compagno M, Navarra A, Campogiani L, Coppola L, Rossi B, Iannetta M, Malagnino V, Parisi SG, Mariotti B, Cerretti R, Arcese W, Goletti D, Andreoni M, Sarmati L. Latent Tuberculosis Infection in Haematopoietic Stem Cell Transplant Recipients: A Retrospective Italian Cohort Study in Tor Vergata University Hospital, Rome. Int J Environ Res Public Health. 2022;19(17):10693. doi: 10.3390/ijerph191710693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng MP, Kusztos AE, Bold TD, Ho VT, Glotzbecker BE, Hsieh C, Baker MA, Baden LR, Hammond SP, Marty FM. Risk of Latent Tuberculosis Reactivation After Hematopoietic cell Transplantation. Clin Infect Dis. 2019;69(5):869–72. doi: 10.1093/cid/ciz048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Litvoc MN, Leal FE, Ferreira DB, Ferreira Lopes MIB, Capuani L, Rocha VG, Costa SF. High tuberculosis density incidence rate in matched unrelated allogeneic stem cell transplantation recipients in the state of São Paulo, Brazil. Mediterr J Hematol Infect Dis. 2023;15(1):e2023037. doi: 10.4084/MJHID.2023.037. DOI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corradi M, Durando P, Lamberti M, Lodi V, Matteelli A, Nicosia V, Pagliaro G, Placidi D, Verso MG, Sotgiu G. Gestione e prevenzione della tubercolosi in ambito occupazionale in paesi a bassa incidenza. Giornale italiano di Medicina del Lavoro ed Ergonomia. 2018;2018;40:27–27. [Google Scholar]
- 8.Bumbacea D, Arend SM, Eyuboglu F, Fishman JA, Goletti D, Ison MG, Jones CE, Kampmann B, Kotton CN, Lange C, Ljungman P, Milburn H, Morris MI, Muller E, Muñoz P, Nellore A, Rieder HL, Sester U, Theodoropoulos N, Wagner D, Sester M. The risk of tuberculosis in transplant candidates and recipients: a TBNET consensus statement. Eur Respir J. 2012 Apr 10;40(4):990–1013. doi: 10.1183/09031936.00000712. [DOI] [PubMed] [Google Scholar]
- 9.Osorio-López EA, Vilar-Compte D, García-Tirado J, Martin-Onraet A. Prevalence of latent tuberculosis in patients with hematological neoplasms in a cancer referral hospital in Mexico City. BMC Infectious Diseases. 2021;21(1) doi: 10.1186/s12879-021-06236-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taha R, Kothari S, Foroutan F, Gitman M, Gupta V, Nguyen T, Rotstein C. Implementation of a Routine Screening Program for Latent Tuberculosis Infection among Patients with Acute Leukemia at a Canadian Cancer Center. Curr Oncol. 2022;29(12):9325–34. doi: 10.3390/curroncol29120731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bettelli F, Giusti D, Morselli M, Colaci E, Nasillo V, Pioli V, Gilioli A, Iotti S, Galassi L, Giubbolini R, Colasante C, Catellani H, Barozzi P, Lagreca I, Vallerini D, Maffei R, Franceschini E, Mussini C, Banchelli F, D’Amico R, Marasca R, Narni F, Potenza L, Comoli P, Luppi M, Forghieri F. Epidemiology and clinical outcomes of latent tuberculosis infection in adults affected with acute leukemia or aplastic anemia: a retrospective single-center study. Ann Hematol. 2020;99(9):2201–3. doi: 10.1007/s00277-020-04191-3. [DOI] [PubMed] [Google Scholar]
- 12.Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, Bloomfield CD, Cazzola M, Vardiman JW. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405. doi: 10.1182/blood-2016-03-643544. [DOI] [PubMed] [Google Scholar]
- 13.Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, Dombret H, Ebert BL, Fenaux P, Larson RA, Levine RL, Lo-Coco F, Naoe T, Niederwieser D, Ossenkoppele GJ, Sanz M, Sierra J, Tallman MS, Tien HF, Wei AH, Löwenberg B, Bloomfield CD. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017 Jan 26;129(4):424–47. doi: 10.1182/blood-2016-08-733196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khoury JD, Solary E, Abla O, Akkari Y, Alaggio R, Apperley JF, Bejar R, Berti E, Busque L, Chan JK, Chen W, Chen X, Chng WJ, Choi JK, Colmenero I, Coupland SE, Cross NC, De Jong D, Elghetany MT, Takahashi E, Emile JF, Ferry J, Fogelstrand L, Fontenay M, Germing U, Gujral S, Haferlach T, Harrison C, Hodge JC, Hu S, Jansen JH, Kanagal-Shamanna R, Kantarjian HM, Kratz CP, Li XQ, Lim MS, Loeb K, Loghavi S, Marcogliese A, Meshinchi S, Michaels P, Naresh KN, Natkunam Y, Nejati R, Ott G, Padron E, Patel KP, Patkar N, Picarsic J, Hochhaus A. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic Neoplasms. Leukemia. doi: 10.1038/s41375-022-01613-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Döhner H, Wei AH, Appelbaum FR, Craddock C, DiNardo CD, Dombret H, Ebert BL, Fenaux P, Godley LA, Hasserjian RP, Larson RA, Levine RL, Miyazaki Y, Niederwieser D, Ossenkoppele GJ, Röllig C, Sierra J, Stein EM, Tallman MS, Tien HF, Wang J, Wierzbowska A, Löwenberg B. Diagnosis and Management of AML in Adults: 2022 ELN Recommendations from an International Expert Panel. Blood. 2022 doi: 10.1182/blood.2022016867. [DOI] [PubMed] [Google Scholar]
- 16.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987 Jan;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 17.Anibarro L, Pena A. Tuberculosis in patients with hematological malignancies. Mediterr J Hematol Infect Dis. 2014;6(1) doi: 10.4084/mjhid.2014.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Anazi K, Al-Jasser A, Evans D. Infections caused by mycobacterium tuberculosis in patients with hematological disorders and in recipients of hematopoietic stem cell transplant, a twelve-year retrospective study. Annals of Clinical Microbiology and Antimicrobials. 2007;6(1):16. doi: 10.1186/1476-0711-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parrish NM, Dick JD, Bishai WR. Mechanisms of latency in Mycobacterium tuberculosis. Trends in Microbiology. 1998;6(3):107–112. doi: 10.1016/s0966-842x(98)01216-5. [DOI] [PubMed] [Google Scholar]
- 20.Hernández-Pando R, Jeyanathan M, Mengistu G, Aguilar D, Orozco H, Harboe M, Rook G, Bjune G. Persistence of DNA from Mycobacterium tuberculosis in superficially normal lung tissue during latent infection. The Lancet. 2000;356(9248):2133–2138. doi: 10.1016/s0140-6736(00)03493-0. [DOI] [PubMed] [Google Scholar]
- 21.Arriaga AK, Orozco EH, Aguilar LD, Rook GAW, Pando RH. Immunological and pathological comparative analysis between experimental latent tuberculous infection and progressive pulmonary tuberculosis. Clinical & Experimental Immunology. 2002;128(2):229–237. doi: 10.1046/j.1365-2249.2002.01832.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barrios-Payán J, Saqui-Salces M, Jeyanathan M, Alcántara-Vazquez A, Castañon-Arreola M, Rook G, Hernandez-Pando R. Extrapulmonary Locations of Mycobacterium tuberculosis DNA During Latent Infection. The Journal of Infectious Diseases. 2012;206(8):1194–1205. doi: 10.1093/infdis/jis381. [DOI] [PubMed] [Google Scholar]
- 23.Narasimhan P, Wood J, MacIntyre CR, Mathai D. Risk Factors for Tuberculosis. Pulmonary Medicine. 20132013:1–11. doi: 10.1155/2013/828939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pai M, Denkinger CM, Kik SV, Rangaka MX, Zwerling A, Oxlade O, Metcalfe JZ, Cattamanchi A, Dowdy DW, Dheda K, Banaei N. Gamma Interferon Release Assays for Detection of Mycobacterium tuberculosis Infection. Clinical Microbiology Reviews. 2014;27(1):3–20. doi: 10.1128/cmr.00034-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deuffic-Burban S, Atsou K, Viget N, Melliez H, Bouvet E, Yazdanpanah Y. Cost-effectiveness of QuantiFERON®-TB test vs. tuberculin skin test in the diagnosis of latent tuberculosis infection. The International journal of tuberculosis and lung disease. 2010;14(4):471–481. [PubMed] [Google Scholar]
- 26.Huang C-C, Jerry Teng C-L, Wu M-F, Lee C-H, Chen H-C, Huang W-C. Features of indeterminate results of QuantiFERON-TB Gold In-Tube test in patients with haematological malignancies. Therapeutic Advances in Hematology. 2021;12:204062072110284. doi: 10.1177/20406207211028437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sánchez-García EM, Gamallo R, Blanco-Moure A, Viejo MA, Amador L, Anibarro L. Toxicity and adherence to treatment for latent tuberculosis infection in patients with hematologic malignancies. Infection. 2013;41(5):903–907. doi: 10.1007/s15010-013-0489-9. [DOI] [PubMed] [Google Scholar]
- 28.Bergeron A, Mikulska M, De Greef J, Bondeelle L, Franquet T, Herrmann JL, Lange C, Spriet I, Akova M, Donnelly JP, Maertens J, Maschmeyer G, Rovira M, Goletti D, de la Camara R, Greinix H, Maertens J, De Greef J, Slavin M, Spriet I, Hubacek P, Bergeron A, Cordonnier C, Kanerva J, Herbrecht R, Herrmann JL, Lanternier F, Bondeelle L, Robin C, Einsele H, Lehrnbecher T, Groll A, Maschmeyer G, Lange C, von Lilienfeld-Toal M, Pana D, Roilides E, Kassa C, Averbuch D, Engelhard D, Cesaro S, Mikulska M, Pagano L, Castagnola E, Compagno F, Goletti D, Mesini A, Donnelly PJ, Styczynski J, Chemaly R. Mycobacterial infections in adults with haematological malignancies and haematopoietic stem cell transplants: guidelines from the 8th European Conference on Infections in Leukaemia. Lancet Infect Dis. 2022 May; doi: 10.1016/s1473-3099(22)00227-4. [DOI] [PubMed] [Google Scholar]
- 29.Organizat WH. WHO consolidated guidelines on tuberculosis. Module 1: Prevention. Tuberculosis preventive treatment. Tuberc Lung Dis HIV Infect. (2):86–92. doi: 10.30978/tb2021-2-86. [DOI] [Google Scholar]
- 30.Krishnan S, Chaisson RE. US Guidelines Fall Short on Short-Course TB Preventive Therapy. Clin Infect Dis. 2023 doi: 10.1093/cid/ciad659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hohmann C, Kang EM, Jancel T. Rifampin and Posaconazole Coadministration Leads to Decreased Serum Posaconazole Concentrations. Clin Infect Dis. 50(6):939–40. doi: 10.1086/650740. [DOI] [PubMed] [Google Scholar]