Abstract
Problem
Delay in starting thrombolytic treatment in patients arriving at hospital with chest pain who are diagnosed as having acute myocardial infarction.
Design
Audit of “door to needle times” for patients presenting with chest pain and an electrocardiogram on admission that confirmed acute myocardial infarction. A one year period in each of three phases of development was studied.
Background and setting
The goal of the national service framework for coronary heart disease is that by April 2002, 75% of eligible patients should receive thrombolysis within 30 minutes of arriving at hospital. A district general hospital introduced a strategy to improve door to needle times. In phase 1 (1989-95), patients with suspected acute myocardial infarction, referred by general practitioners, were assessed in the coronary care unit; all other patients were seen first in the accident and emergency department. In phase 2 (1995-7), all patients with suspected acute myocardial infarction were transferred directly to a fast track area within the coronary care unit, where nurses assess patients and doctors started treatment.
Key measures for improvement
Median door to needle time in phase 1 of 45 minutes (range 5-300 minutes), with 38% of patients treated within 30 minutes. Median door to needle time in phase 2 of 40 minutes (range 5-180 minutes), with 47% treated within 30 minutes
Strategies for change
In phase 3 (1997-2001), all patients with suspected acute myocardial infarction were transferred directly to the fast track area and assessed by a “coronary care thrombolysis nurse.” If electrocardiography confirmed the diagnosis of acute myocardial infarction, the nurse could initiate thrombolytic therapy (subject to guidelines and exclusions determined by the consultant cardiologists).
Effects of change
Median door to needle time in phase 3 of 15 minutes (range 5-70 minutes), with 80% of patients treated within 30 minutes. Systematic clinical review showed no cases in which a nurse initiated inappropriate thrombolysis.
Lessons learnt
Thrombolysis started by nurses is safe and effective in patients with acute myocardial infarction. It may provide a way by which the national service framework's targets for door to needle times can be achieved.
Introduction
Prompt thrombolytic treatment is well established in the management of acute myocardial infarction, and mortality is reduced and clinical outcome improved if treatment is started in the first hour after the onset of ischaemic chest pain.1–3 The management of patients with acute myocardial infarction will be most effective when the interval between onset of pain and initiation of thrombolysis—the “pain to needle time”—is as short as possible. To achieve this objective, healthcare providers are looking at systems that give rapid and efficient transfer to hospital of patients with suspected acute myocardial infarction.
Education of patients and the public is crucial to ensure that patients whose symptoms may be due to acute myocardial infarction seek medical attention and that paramedical services are able to attend soon after the onset of pain. One major concern for doctors is the length of time between patients arriving at hospital and those diagnosed with acute myocardial infarction being given thrombolytic therapy—the “door to needle time.” In the United Kingdom, the Department of Health produced the national service framework for the delivery of coronary heart disease services,4 which sets targets for the management of acute myocardial infarction and for door to needle times (box).
Targets of the national service framework for coronary heart disease for the in hospital management of acute myocardial infarction
April 2001—Agree protocol for whole hospital for management of suspected and confirmed acute myocardial infarction and other acute coronary syndromes
April 2002—75% of eligible patients should receive thrombolysis within 30 minutes of arrival at hospital
April 2003—75% of eligible patients should receive thrombolysis within 20 minutes of arrival at hospital
We developed a strategy for the initial diagnosis and treatment of patients presenting with chest pain and suspected acute myocardial infarction at the Princess Royal Hospital in Telford—a district general hospital with 350 beds, serving a population of 220 000 in east Shropshire. The cardiology department has a coronary care unit with five beds staffed by 14 nurses. During phase 1 (1989-95), patients with suspected acute myocardial infarction referred by general practitioners were transferred directly to the coronary care unit; all other patients were assessed in the accident and emergency department.
The hospital was one of six district general hospitals observed in an audit of thrombolysis by the Royal College of Physicians and the British Cardiac Society, which recommended that fast track assessment areas be developed.5–7 The development of such areas formed phase 2 (1995-7) of our strategy. All patients with suspected acute myocardial infarction were transferred directly to a fast track area in the coronary care unit. Initial assessment was by a nurse, and treatment was prescribed and started by a doctor.
In this paper, we outline the limited improvements in door to needle times achieved during phase 2 of the strategy. We describe the development of phase 3 (1997-2001) in which nurse initiated thrombolysis was introduced.
Problem
Significant delays in the assessment and treatment of patients with suspected acute myocardial infarction after admission to hospital. Increased door to needle times lead to reduced efficacy of thrombolytic therapy.
Process of gathering information
We collected data about all admissions with suspected acute myocardial infarction to the hospital up to 1999. We audited the data for one period of 12 months for each phase of development (table). We looked at the door to needle times and electrocardiograms that confirmed acute myocardial infarction for all patients presenting with chest pain who received thrombolytic therapy. Patients who presented with an acute coronary syndrome but whose electrocardiogram at the time of admission did not fulfil electrocardiogram criteria for thrombolysis were excluded. Inpatients who had an acute myocardial infarction after admission were also excluded.
Analysis and interpretation
Phase 1: 1989-95
During phase 1, patients with possible acute myocardial infarction seen in the community by general practitioners were referred to the on-call general medical registrar. The patients were then admitted directly to the coronary care unit, where they were assessed by the on-call medical registrar or senior house officer. All other patients with suspected acute myocardial infarction were admitted through the accident and emergency department. If thrombolysis was indicated, patients were transferred to the coronary care unit. The local policy was not to initiate thrombolytic therapy in the accident and emergency department but to wait until the patient arrived in the coronary care unit.
During the audit period in phase 1 (1 July 1994 to 30 June 1995), 160 patients received thrombolytic therapy for acute myocardial infarction. The median door to needle time was 45 minutes, and 38% of patients (60) were treated within 30 minutes of arrival.
The two main reasons for the long door to needle time were delays in patients being assessed in and referred from the accident and emergency department and delays in patients being assessed by the general medical team after patients arrived at the coronary care unit. Four patients who presented with chest pain and an electrocardiogram confirming acute myocardial infarction waited over 180 minutes for thrombolysis because their treatment was delayed by both of these factors. The difference in door to needle times between patients assessed in the accident and emergency department before being transferred to coronary care and those transferred directly to coronary care was mentioned in the audit of the Royal College of Physicians and British Cardiac Society.5
Phase 2: 1995-7
The guidelines that resulted from the audit recommended a “fast track” system of assessment for patients with suspected acute myocardial infarction.5–7 Phase 2, therefore, involved transferring all patients with suspected acute myocardial infarction who presented to general practitioners, the accident and emergency department, or paramedics directly to the coronary care unit. They were assessed initially by a coronary care nurse, who took a brief history, baseline observations, and an electrocardiogram. The on-call medical team was informed of the patient's arrival and decided whether to initiate thrombolysis.
The median door to needle time in the audit period (1 November 1995 to 31 October 1996) in phase 2 was 40 minutes. Treatment was started within 30 minutes of the patient arriving at hospital in 74/157 (47%) patients.
Strategies for change
The audit during phase 2 showed a considerable improvement in door to needle times over those in phase 1. Initiation of thrombolytic drugs was delayed in a number of patients who had clear evidence of acute myocardial infarction at presentation because a doctor was not available to attend them immediately. In uncomplicated cases, this led to a straightforward delay in the diagnosis being confirmed and thrombolysis prescribed. In complicated cases—for example, where the patient needed to be treated for hypertension before thrombolysis began—the delay was even greater.
Phase 3: 1997-2001
In phase 3, we introduced a system in which nurses assessed and initiated thrombolysis in patients presenting with symptoms suggestive of acute myocardial infarction. This meant that the nurses' role in the fast track area was expanded. We developed a protocol through collaboration between the consultant cardiologist and senior coronary care nurses, and this was strongly supported by the nursing director. At this time, only one other hospital in the United Kingdom allowed nurses to initiate thrombolysis, and we felt that we needed formal approval from the trust's board. After the board had considered the audit data from phase 2, the proposed protocol, and assurances from the consultant cardiologist that the proposed system was safe, the board approved the move for nurses to initiate thrombolysis.
Coronary care unit nurses can reliably identify electrocardiographic criteria for the diagnosis of acute myocardial infarction.8,9 During phase 2, when patients in the fast track area were assessed by nurses who then called the doctor to prescribe thrombolysis, nurses' assessment of a clear indication for thromboloysis was always correct. In some cases, their assessment was more accurate than that of inexperienced junior doctors.
After the protocol for nurses initiating thrombolysis had been approved by the board, coronary care nurses at grades F and G were assessed formally by the consultant cardiologist to test their knowledge of the protocol. The assessment examined their ability to identify electrocardiographic criteria for thrombolysis and absolute and relative contraindications. Once a nurse satisfactorily completed the assessment, a certificate formally extending that nurse's role to include initiation of thrombolysis was signed by the nurse, the consultant cardiologist, and the nursing director.
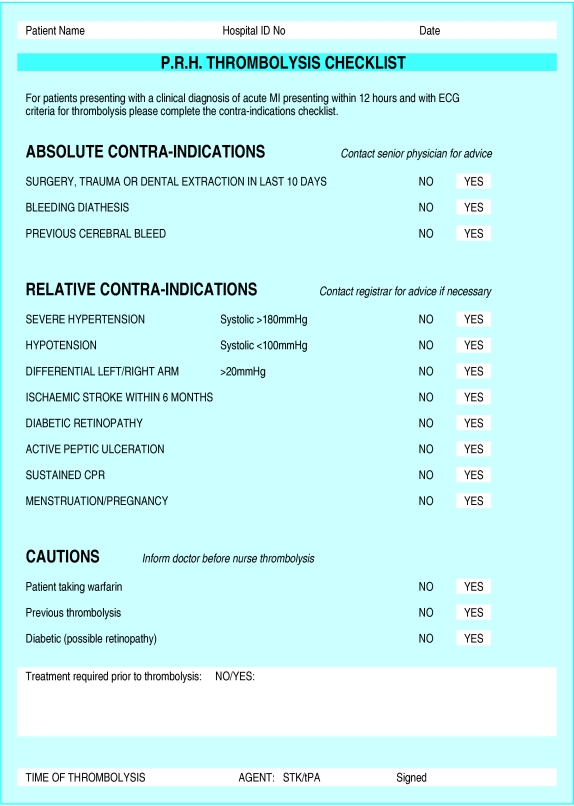
All patients with suspected acute myocardial infarction were transferred to the fast track area, where they were assessed by a coronary care thrombolysis nurse according to guidelines established by the consultant cardiologists. A brief history, baseline observations, and a 12 lead electrocardiogram were taken, and soluble aspirin was given (if not already given). When a patient's history was compatible with thrombolysis and their electrocardiogram confirmed acute myocardial infarction, the nurse completed a contraindication checklist (fig 1). If there were no contraindications, thrombolysis with streptokinase was started. The on-call general medical team was notified, took a formal history and examined the patient, and decided on further management.
Figure 1.
Checklist of contraindications to thrombolysis
In cases where there were absolute or relative contraindications to thrombolysis, the on-call team was asked to review the patient as a matter of urgency. If a thrombolysis nurse was not on duty, the usual fast track system—in which a nurse assesses the patient and the doctor initiates thrombolysis—operated.
Effects of change
In phase 3 (1 January 1999 to 31 December 1999), the median door to needle time was 15 minutes, and 74/93 (80%) patients received thrombolysis within 30 minutes of arriving at the hospital. All of the 24 patients in whom thrombolysis was initiated by a nurse received thrombolytic drugs within 30 minutes of arrival. Systematic clinical review showed no cases in which a nurse started thrombolysis inappropriately.
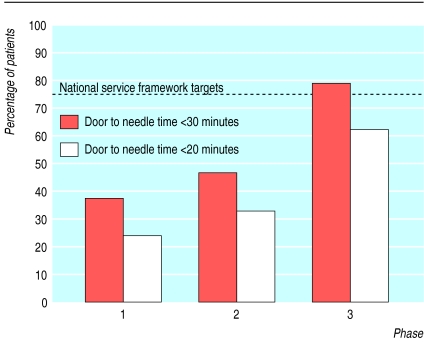
The strategy in which nurses started thrombolysis in patients before they were assessed by a doctor was a safe and effective way to reduce door to needle times in patients with acute myocardial infarction. As a result of this strategy, the Princess Royal Hospital already meets the national service framework's April 2002 target for door to needle times (75% of patients to receive thrombolysis within 30 minutes), and is approaching the April 2003 target (75% within 20 minutes) (fig 2).
Figure 2.
Percentage of door to needle times within 20 and 30 minutes for the one year audit periods from each of the three phases of development at Princess Royal Hospital. National service framework targets: 75% within 30 minutes by April 2002 and 75% within 20 minutes by April 2003
Audit showed that door to needle times for thrombolysis started by doctors also have been reduced compared with those in phase 2. This was partly because the medical team was more aware of the importance of promptly attending the fast track area to assess patients with suspected acute myocardial infarction. The nature and quality of the liaison between medical and nursing staff have improved considerably, with patients presenting to the fast track area receiving more efficient treatment whether a thrombolysis nurse was on duty or not. The longer door to needle times for thrombolysis started by doctors rather than nurses to some extent reflect the fact that patients reviewed by a doctor before receiving thrombolytic therapy (after assessment by a thrombolysis nurse) generally have unusual presentations or relative contraindications to thrombolysis.
Our nurse led approach introduced questions as to whether junior doctors would lose out by having less experience in diagnosing and treating acute myocardial infarction. The senior coronary care nursing staff were invaluable in preventing this loss of experience—sharing their knowledge of interpretation of electrocardiograms for patients with acute coronary syndromes and rhythm disturbances with junior medical staff by means of formal and informal teaching as well as advanced life support training. The guidelines and checklists used by nurses approved to initiate thrombolysis also act as educational tools. Thorough formal history taking and examination by on-call doctors remain crucial parts of the admission and assessment process, and it is the medical team that determines the patient's management after thrombolysis has been started.
Next steps
Currently, four of our 14 coronary care nursing staff are approved to initiate thrombolysis. Other senior staff in the coronary care unit are being trained and assessed as part of phase 4. We plan to have at least seven thrombolysis nurses; this will allow us to always have a thrombolysis nurse on duty in the coronary care department. We are also introducing documents to describe the coronary care pathways for the management of patients with acute myocardial infarction and unstable angina as part of phase 4. These will combine documents used by nurses and medical staff with the checklists for nurses approved to initiate thrombolysis. They will provide a structured route for the assessment, management, and audit of patients with suspected acute myocardial infarction and unstable angina.
The system in which nurses initiate thrombolysis was a natural development from the fast track assessments by nurses, and it is a model that could be adopted in most coronary care units. The national service framework's April 2003 target of door to needle times of less than 20 minutes in 75% of cases is attainable using this system. However, such targets must not lead to rushed or inaccurate assessments or to thrombolysis being administered inappropriately.
Public education about the symptoms of acute myocardial infarction will help to reduce the time between onset of ischaemic pain and the emergency services being called, and the national service framework has set target times for paramedics and ambulances to reach patients with suspected acute myocardial infarction. The overall aim is to reduce the interval between onset of pain and the initiation of thrombolytic drugs—the pain to needle time.
The proposed phase 5 of the Princess Royal Hospital's programme is thrombolysis started by paramedics before the patient reaches the hospital. A number of methods have been attempted—including mobile coronary care units and drugs administered by general practitioners10,11—but no comprehensive system of prehospital thrombolysis exists in the United Kingdom.12 Paramedics currently spend some time training in the coronary care unit and in the cardiology department, and we feel that further training for experienced paramedics would allow a safe system of prehospital thrombolysis and considerable reductions in pain to needle times. A pilot study to assess the safety and feasibility of this approach is planned.
Key learning points
Prompt thrombolytic therapy reduces morbidity and mortality of patients with acute myocardial infarction
Fast track assessment of patients with suspected acute myocardial infarction has improved door to needle times
Nurse inititated thrombolysis is a safe and effective way to gain further reductions in door to needle times
This model may provide a route to attaining the national service framework targets for door to needle times
Table.
Door to needle times for thrombolytic therapy for one year audit periods of three phases of development at Princess Royal Hospital
| Total no of patients | No (%) patients seen in ⩽20 minutes | No (%) patients seen in ⩽30 minutes | Median (range) door to needle time (minutes) | |
|---|---|---|---|---|
| Phase 1: | ||||
| All patients | 160 | 39 (24) | 60 (38) | 45 (5-300) |
| Patients direct to coronary care unit | 62 | 31 (50) | 40 (65) | 25 (5-300) |
| Patients first attending accident and emergency department | 98 | 9 (9) | 20 (20) | 60 (20-300) |
| Phase 2: | ||||
| All patients | 157 | 52 (33) | 74 (47) | 40 (5-180) |
| Phase 3: | ||||
| All patients | 93 | 58 (62) | 74 (80) | 15 (5-70) |
| Patients with thrombolysis initiated by nurse | 24 | 22 (92) | 24 (100) | 15 (5-30) |
| Patients with thrombolysis initiated by doctor | 69 | 36 (52) | 50 (73) | 20 (5-70) |
Footnotes
Funding: This study formed part of the structured audit within the cardiology department and received no additional or external funding.
Competing interests: None declared.
References
- 1.Fibrinolytic Therapy Trialists' Collaborative Group. Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Lancet. 1994;343:311–322. [PubMed] [Google Scholar]
- 2.Second International Study of Infarct Survival Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both or neither among 17,187 cases of suspected acute myocardial infarction. Lancet. 1988;ii:349–360. [PubMed] [Google Scholar]
- 3.Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardio. Effectiveness of intravenous thrombolytic therapy in acute myocardial infarction. Lancet. 1986;i:397–402. [PubMed] [Google Scholar]
- 4.Department of Health. National service framework for coronary heart disease. London: HMSO; 2000. [Google Scholar]
- 5.Birkhead JS.on behalf of the Joint Audit Committee of the British Cardiac Society and Cardiology Committee of the Royal College of Physicians of London. Time delays in provision of thrombolytic treatment in six district hospitals BMJ 1992305445–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weston CF, Penny WJ, Julian DG. Guidelines for the early management of patients with myocardial infarction. British Heart Foundation Working Group. BMJ. 1994;308:767–771. doi: 10.1136/bmj.308.6931.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pell ACH, Miller HC, Robertson CE, Fox KA. Effects of “fast track” admission for acute myocardial infarction on delay to thrombolysis. BMJ. 1992;304:83–87. doi: 10.1136/bmj.304.6819.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Somauroo JD, McCarten P, Appleton B, Amadi A, Rodrigues E. Effectiveness of a ‘thrombolysis nurse’ in shortening delay in acute myocardial infarction. J R Coll Phys Lond. 1999;33:46–50. [PMC free article] [PubMed] [Google Scholar]
- 9.Quinn T, MacDermott A, Caunt J. Determining patients' suitability for thrombolysis: coronary care nurses' agreement with an expert cardiological ‘gold standard’ as assessed by clinical and electrocardiographic ‘vignettes’. Intensive Crit Care Nurs. 1998;14:219–224. doi: 10.1016/s0964-3397(98)80614-9. [DOI] [PubMed] [Google Scholar]
- 10.Foster DB, Duchenbach JH, Barkdoll CM, Mitchell BK. Prehospital recognition of AMI using independent nurse/paramedic 12 lead ECG evaluation: impact on in-hospital times to thrombolysis in a rural community hospital. Am J Emerg Med. 1994;12:25–31. doi: 10.1016/0735-6757(94)90192-9. [DOI] [PubMed] [Google Scholar]
- 11.Grampian Region Early Antistreplase Trial Group. Feasibility, safety, and efficacy of domiciliary thrombolysis by general practitioners. BMJ. 1992;305:548–553. doi: 10.1136/bmj.305.6853.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weston C, Fox KA. Pre-hospital thrombolysis: current status and future prospects. J R Coll Phys Lond. 1991;25:312–320. [PMC free article] [PubMed] [Google Scholar]