Abstract
Background
There is increasing evidence regarding the association between endotoxemia and the pathogenesis of atherosclerosis and myocardial infarction (MI). During the acute phase of MI, endotoxemia might increase inflammation and drive adverse cardiovascular (CV) outcomes. We aimed to explore the risk factors and prognostic value of endotoxemia in patients admitted for acute MI.
Methods
Patients admitted to the coronary care unit of Dijon University Hospital for type 1 acute MI between 2013 and 2015 were included. Endotoxemia, assessed by plasma lipopolysaccharide (LPS) concentration, was measured by mass spectrometry. Major adverse CV events were recorded in the year following hospital admission.
Results
Data from 245 consecutive MI patients were analyzed. LPS concentration at admission markedly increased with age and diabetes. High LPS concentration was correlated with metabolic biomarkers (glycemia, triglyceride, and total cholesterol) but not with CV (troponin Ic peak and N-terminal pro-brain natriuretic peptide) or inflammatory biomarkers (C-reactive protein, IL6, IL8, and TNFα). LPS concentration was not associated with in-hospital or 1-year outcomes.
Conclusions
In patients admitted for MI, higher levels of endotoxins were related to pre-existing conditions rather than acute clinical severity. Therefore, endotoxins measured on the day of MI could reflect metabolic chronic endotoxemia rather than MI-related acute gut translocation.
Keywords: endotoxemia, lipopolysaccharide, acute myocardial infarction, inflammation, diabetes, lipoprotein
Introduction
Myocardial infarction (MI) is a frequent event that carries high morbidity and mortality worldwide. Bacterial endotoxins (lipopolysaccharides, LPSs) are pathogen-associated molecular patterns (PAMPs) that are part of the outer membrane of Gram-negative bacteria. LPSs have been described as exerting a noxious effect by triggering inflammation (TLR-4 recognition and NF-kB transcription) (1).
There is increasing evidence that endotoxemia is associated with MI through multiple underlying mechanisms. First, chronic low-grade endotoxemia has been reported in metabolic disorders (2, 3), defining the concept of metabolic endotoxemia (4). In addition, LPSs are closely linked to lipoprotein metabolism by reverse LPS transport (5, 6). These conditions are risk factors for MI, and emerging concepts suggest that endotoxemia has a role in coronary artery disease (CAD) and the genesis of MI (7, 8). Second, several studies have suggested an alteration of the gut barrier function at the acute phase of MI, resulting in acute endotoxemia (9, 10). Because endotoxins reduce cardiac performance (11) and cause vasoplegia (12), they might increase the risk of heart failure after MI and worsen short-term patient outcomes. Finally, inflammation is thought to extend myocardial injury (13) and promote recurrent cardiovascular (CV) events (14), so endotoxemia might also have negative effects on long-term recovery. Despite these potentially harmful effects, data regarding acute endotoxemia and MI are scarce and further evidence is needed (15).
The primary objective of the present study was to explore factors associated with endotoxemia at hospital admission in patients with MI and to determine whether endotoxemia at hospital admission was related to metabolic conditions (thus chronic low-grade translocation promoting atherosclerosis) or to acute gut barrier failure in the context of MI. The secondary objective was to determine the association of endotoxemia with inflammation, initial MI severity, and short-term and long-term outcomes.
Methods
Patients
This study is an ancillary analysis of a prospectively acquired database (RICO survey) (16). All consecutive patients admitted to the coronary intensive care unit (ICU) of the Dijon University Hospital (France) from January 2013 to April 2015 for type 1 MI were prospectively included. Patients with prior coronary arterial disease [MI, transluminal angioplasty, unstable angina, or coronary artery bypass graft (CABG) surgery] or chronic kidney disease were excluded. The present study agrees with the ethical guidelines of the Declaration of Helsinki. Informed consent was obtained from the participants before their inclusion in the study, and the Ethics Committee of the University Hospital of Dijon approved the protocol (BIOCARDIS-2016–9205AAO034S02117).
Data collection
Patient characteristics, including age and gender, were obtained at hospital admission, along with medical history (hypertension, diabetes, smoking, and family history of coronary artery disease, main treatments [antiplatelets, angiotensin 2 receptor blockers (ARB), angiotensin 2 converting enzyme (ACE) inhibitors, statins, and beta-blockers], and clinical data [left ventricular ejection fraction, heart rate (HR), blood pressure, catecholamine administration, and infarction location]. Shock index was defined as the heart rate divided by systolic blood pressure (SBP). Coronary artery disease burden at coronary angiography through multivessel disease and the SYNTAX (17) score were also collected. The Global Registry of Acute Coronary Events (GRACE) risk score (18), a robust prognosis tool following MI, was also calculated.
Determination of blood markers
Blood samples were taken on admission. N-terminal pro-brain natriuretic peptide (Nt-ProBNP, normal value <125 pg/ml), blood lipids [normal range 1.20–2.4 g/L for cholesterol, 0.4–0.6 g/L for HDL cholesterol, and 0.4–1.5 g/L for triglycerides (TG)], glucose (normal range 4.3–6.4 mmol/L), glycated hemoglobin (HbA1c, normal value <6%), and C-reactive protein (CRP) (normal value <4 mg/L) were measured. The troponin Ic peak (normal value <0.1 µg/L) was obtained from three blood samples within 24 h following admission. The estimated glomerular filtration rate (eGFR) was calculated using the chronic kidney disease-epidemiology collaboration formula (CKD-EPI).
Plasma was taken upon ICU admission in an EDTA (ethylenediaminetetraacetic acid) blood collection tube. Blood was centrifugated (2,000×g for 10 min at 4 °C), and plasma was stored at −80 °C. LPS, lipid transfer protein activities [phospholipid transfer protein (PLTP) and cholesteryl ester transfer protein (CETP)], and cytokines were retrospectively measured from this plasma collection.
LPS was quantified by measuring one of its components [3-hydroxy myristate (3HM)] using liquid chromatography coupled with tandem mass spectrometry, as previously described (19). Briefly, samples were hydrolyzed for 3 h at 90 °C in the presence of hydrochloric acid to release free fatty acids, which were subsequently extracted with water and ethane/ethyl acetate (3/2 v/v). Dried extracts were dissolved in ethanol and injected onto an SBC18 2.1 mm × 50 mm, 1.8 µm column, connected to an Infinity 1290 HPLC system (Agilent Technologies). Separation of hydroxylated fatty acids was achieved at 45 °C at a flow rate of 0.4 ml/min using ammonium formate (5 mM/0.1% formic acid) as eluent A (55% for 0.5 min) and 95% acetonitrile as eluent B (100% reached in 2.5 min and maintained for 5 min). MS/MS detection was performed in negative mode using a QqQ 6490 triple quadrupole mass spectrometer equipped with a JetStream ESI source to quantify the selected ions as follows: for 3HM, precursor ion 243.2 Da and product ion 59 Da; for 3-hydroxytridecanoic acid (IS), which was used as the internal standard, precursor ion 229.2 Da and product ion 59 Da.
PLTP and CETP activities were measured in undiluted plasma using commercially available fluorescence activity assays (Roar Biomedical), according to the manufacturer's instructions. Incubations were performed at 37 °C for 30 min (for PLTP) or 3 h (for CETP), with fluorescence monitoring (excitation, 465 nm; emission, 535 nm) throughout the incubation period with a Victor2 multilabel counter (PerkinElmer, Waltham, United States). Transfer activities were calculated from the slope of fluorescence increase between 1 and 30 min (for PLTP) or between 1 min and 1 h (for CETP) and expressed as arbitrary fluorescence units (AU).
Cytokines were measured using a Luminex® Human Magnetic assay (R&D Systems, Minneapolis, USA). The assays were performed according to the manufacturer's instructions (including for sample collection and preparation). Plasma was not diluted for this analysis. Standards and samples were analyzed on a Luminex® apparatus (BioPlex 200, Bio-Rad, Munich, Germany) using BioPlex Manager Software (Version 5, Bio-Rad, Hercules, CA, USA). For all cytokines, standard curves ranged from 3.2 to 10,000 pg/ml.
Outcomes
Plasma markers included endotoxin plasma concentration, cytokine plasma concentration, and CRP.
Clinical outcomes included in-hospital major adverse CV events (MACEs), such as CV death, heart failure (defined as Killip class >1), and recurrent myocardial infarction, ventricular and supraventricular arrhythmia, and ICU length of stay. A follow-up at 1 year with the patient, next of kin, or the treating physician was conducted by mail or telephone. Occurrences of MACEs, defined as CV death, recurrent myocardial infarction, hospitalization for heart failure, unscheduled percutaneous coronary intervention (PCI), coronary artery bypass surgery, unstable angina or angina pectoris, were collected.
Statistical analysis
No sample size calculation was performed for this study. All the patients included in the cohort were analyzed. Dichotomous variables are expressed as n (%), and continuous variables are expressed as means ± standard deviations or medians [interquartile ranges (IQR)]. A Kolmogorov–Smirnov test was performed to assess the normality of continuous variables. Non-normally distributed variables were log-transformed when needed. The Mann–Whitney test or Student's t-test was used to compare continuous data, as appropriate. Pearson correlation analyses (for normally distributed variables) or Spearman correlation analyses (one or two non-Gaussian variables) were performed. The threshold for significance was set at p < 0.05. Multivariate linear regression models were built to estimate LPS levels based on significant variables in univariate analysis, with an inclusion threshold of p < 0.10. Variable selection was stepwise. The normality of residuals and homoscedasticity were checked graphically; the model was also checked for autocorrelations of residuals (Durbin–Watson test) and multicollinearity (variance inflation factor). Missing data were considered at random and were omitted. SPSS version 12.0.1 (IBM Inc., Armonk, NY, USA) was used for all analyses.
Results
Baseline characteristics
Two hundred and forty-five patients were analyzed. Baseline characteristics are presented in Table 1. The mean age was 62 ± 13 years, most patients were men (72%), and the median body mass index (BMI) was 27 (25–29). We identified 92 patients (37.6%) with hypercholesterolemia and 34 (14%) with diabetes. Most patients had ST-segment elevation (Table 2).
Table 1.
Association between LPS plasma concentration and patient's characteristics.
| Variable |
n (%), mean ± SD or median (IQR) N = 245 |
Total LPS or r | p | |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age, years | 62 ± 13 | 0.173 | 0.007 | |
| Female | No | 176 (71.8%) | 106.36 (82.45–131.16) | 0.946 |
| Yes | 69 (28.2%) | 106.18 (84.47–129.99) | ||
| BMI, kg/m2 | 27 (25–29) | 0.192 | 0.003 | |
| Medical history | ||||
| Hypertension | No | 139 (56.7%) | 104.78 (83.16–127.42) | 0.521 |
| Yes | 106 (43.3%) | 108.23 (86.14–133.28) | ||
| Diabetes | No | 211 (86.1%) | 103.03 (82.45–124.74) | <0.001 |
| Yes | 34 (13.9%) | 139.60 (113.86–230.62) | ||
| Family history of CAD | No | 168 (68.6%) | 108.98 (83.49–133.13) | 0.141 |
| Yes | 77 (31.4%) | 102.95 (83.11–125.39) | ||
| Current smoking | No | 137 (55.9%) | 110.44 (91.60–132.65) | 0.022 |
| Yes | 108 (44.1%) | 102.06 (79.58–121.80) | ||
| Chronic treatments | ||||
| Antiplatelet | No | 241 (98.4%) | 106.32 (83.30–131.00) | 0.938 |
| Yes | 4 (1.6%) | 107.04 (77.49–133.89) | ||
| Aspirin | No | 223 (91.0%) | 106.13 (83.44–129.14) | 0.570 |
| Yes | 22 (9.0%) | 115.68 (74.40–139.42) | ||
| ARB | No | 209 (85.3%) | 106.07 (82.75–128.84) | 0.191 |
| Yes | 36 (14.7%) | 115.28 (95.36–136.59) | ||
| ACE inhibitors | No | 219 (89.4%) | 106.32 (83.06–130.28) | 0.572 |
| Yes | 26 (10.6%) | 107.20 (88.77–144.31) | ||
| Statin | No | 214 (87.3%) | 107.88 (83.72–131.71) | 0.173 |
| Yes | 31 (12.7%) | 98.82 (75.14–121.03) | ||
| Beta-blockers | No | 210 (85.7%) | 106.36 (83.06–130.38) | 0.961 |
| Yes | 35 (14.3%) | 104.61 (90.90–133.92) | ||
Data are expressed as n (%), mean ± standard deviation (SD), or median (IQR).
LPS is expressed as 3HM (pmol/L). p-values are given for the association between each variable and LPS plasma concentration.
Table 2.
Association between LPS plasma concentration and clinical data on admission.
| Variable |
n (%), mean ± SD, or median (IQR) N = 245 |
Total LPS or r | p | |
|---|---|---|---|---|
| Clinical data | ||||
| LVEF, % | 55 (45–60) | −0.069 | 0.283 | |
| LVEF <40% | No | 219 (89.8%) | 106.18 (83.06–128.54) | 0.203 |
| Yes | 25 (10.2%) | 113.98 (90.45–155.10) | ||
| HR, bpm | 76 (67–88) | 0.191 | 0.003 | |
| SBP, mmHg | 141 ± 27 | 0.131 | 0.043 | |
| DBP, mmHg | 83 ± 19 | 0.100 | 0.123 | |
| Catecholamine | No | 230 (93.9%) | 106.15 (83.37–130.54) | 0.827 |
| Yes | 15 (6.1%) | 113.98 (83.06–131.83) | ||
| Shock index ≥ 0.7 | No | 191 (80.3%) | 104.78 (82.22–125.75) | 0.034 |
| Yes | 47 (19.7%) | 117.01 (90.64–163.53) | ||
| STEMI | No | 97 (39.6%) | 103.87 (79.72–125.67) | 0.181 |
| Yes | 148 (60.4%) | 108.99 (85.24–133.56) | ||
| Anterior wall location | No | 150 (61.2%) | 106.10 (82.91–128.31) | 0.396 |
| Yes | 95 (38.8%) | 110.24 (85.18–133.51) | ||
| Heart failure | No | 201 (82.0%) | 108.51 (83.69–131.75) | 0.162 |
| Yes | 44 (18.0%) | 96.28 (79.71–122.72) | ||
| Time to admission, min | 160 (101–338) | 0.038 | 0.549 | |
| GRACE risk score | 137 ± 36, n = 238 | 0.110 | 0.089 | |
| Angiographical data | ||||
| Coronary angiography | No | 2 (0.8%) | 94.60 (83.06-x) | 0.515 |
| Yes | 243 (99.2%) | 106.40 (83.44–131.32) | ||
| SYNTAX score | 8 (5–14), n = 238 | 0.071 | 0.275 | |
| Multivessel disease | No | 137 (55.9%) | 106.18 (84.49–129.29) | 0.811 |
| Yes | 108 (44.1%) | 107.33 (81.79–131.58) | ||
| PCI | No | 45 (18.4%) | 105.62 (84.78–123.27) | 0.641 |
| Yes | 200 (81.6%) | 108.23 (83.08–132.14) | ||
| Plasma markers | ||||
| Creatinine, µmol/L | 77 ± 15 | −0.054 | 0.400 | |
| Troponin Ic peak, ng/ml | 26.0 (5.3–93.5) | 0.077 | 0.228 | |
| Nt-ProBNP, pg/ml | 400 (103–1,247) | 0.000 | 0.996 | |
DBP, diastolic blood pressure; STEMI, ST-elevation myocardial infarction.
Data are expressed as n (%), mean ± standard deviation (SD), or median (IQR). LPS is expressed as 3HM (pmol/L). The shock index was calculated as the ratio of heart rate to systolic blood pressure. p-values are given for the association between each variable and LPS plasma concentration. p-values presented are not corrected for multiple comparisons.
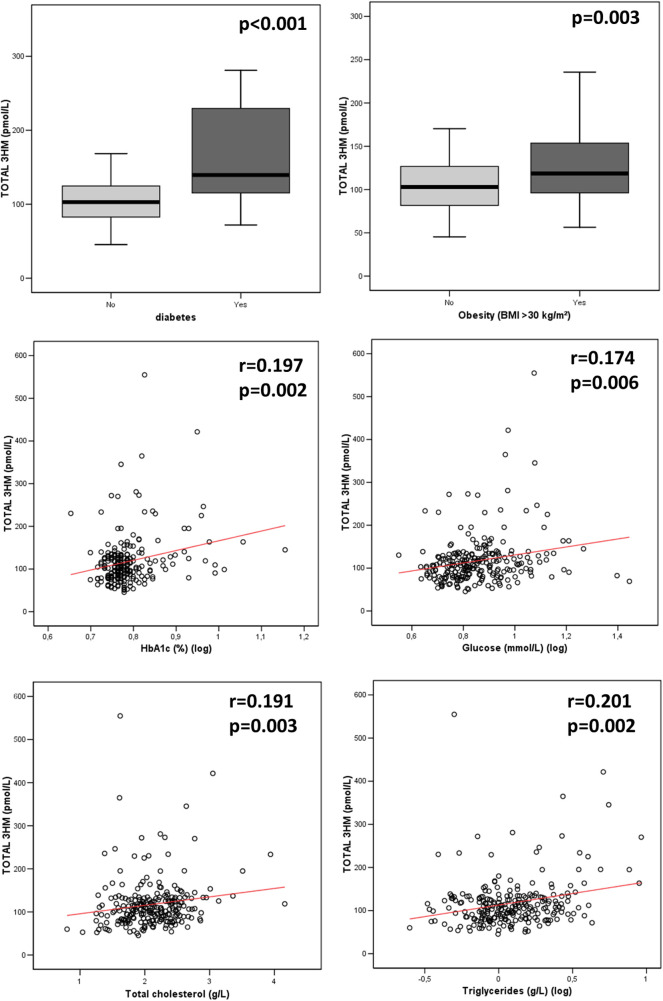
Variables associated with endotoxemia
The median LPS concentration was 106 (83–131) pmol/L of 3HM. The distribution of LPS concentration in our population is illustrated in Figure 1. Endotoxemia was associated with age, diabetes, and obesity (Table 1, Figure 2), as well as with total cholesterol (r = 0.191, p = 0.003), triglyceridemia (r = 0.201, p = 0.002), and glucose metabolism parameters (blood glucose, HbA1c) (Table 3). LPS was lower in smokers (102.06 pmol/L of 3HM (79.58–121.80) vs. 110.44 pmol/L of 3HM (91.60–132.65), p = 0.22). PLTP activity was positively correlated with LPS concentrations (r = 0.146, p = 0.022). At admission, patients with high endotoxemia had a faster heart rate (r = 0.19, p < 0.01), and a higher shock index (≥0.7) was associated with higher LPS concentrations. In multivariate analysis, triglycerides, total cholesterol, history of diabetes, and age were independently associated with LPS concentration (Table 4).
Figure 1.
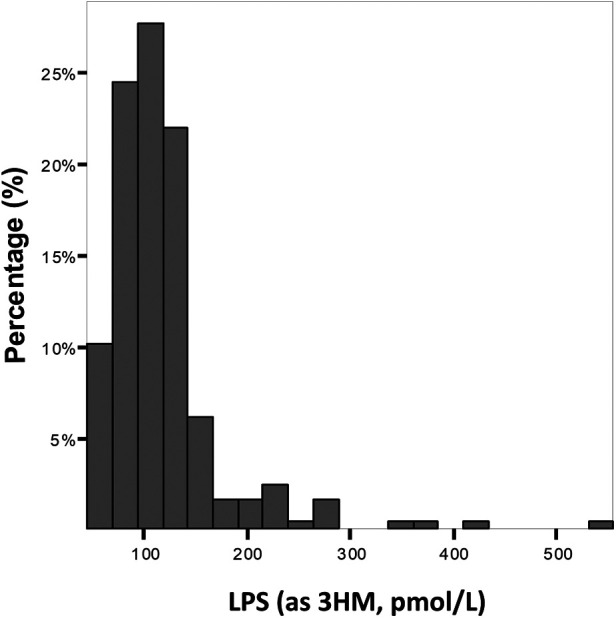
Distribution of the population according to LPS concentration at admission. Results are expressed as % of the population for each range of LPS concentration.
Figure 2.
Association between LPS concentration and metabolic parameters at admission. p-values were computed using the Spearman test for correlation and the Mann–Whitney test for group comparisons. n = 235 for HbA1c, 245 for glycemia, 245 for diabetes, and 244 for total cholesterol, triglyceridemia, and obesity. 3HM, 3-hydroxy myristate.
Table 3.
Association between LPS plasma concentration and lipid and glucose metabolism.
| Variable |
n (%) or median (IQR) N = 245 |
Total LPS or r | p | |
|---|---|---|---|---|
| LDL cholesterol, g/L | 1.32 (1.09–1.60) | 0.099 | 0.124 | |
| HDL cholesterol, g/L | 0.47 (0.38–0.56) | 0.095 | 0.138 | |
| Total cholesterol, g/L | 2.09 (1.80–2.40) | 0.191 | 0.003 | |
| Triglycerides, g/L | 1.16 (0.81–1.80) | 0.201 | 0.002 | |
| PLTP, AU | 186.7 ± 33.0 | 0.146 | 0.022 | |
| CETP, AU | 31.3 ± 11.3 | −0.051 | 0.424 | |
| LBP, µg/ml | 26.1 ± 10.2 | −0.132 | 0.040 | |
| HbA1c, % | 5.9 (5.7–6.3) | 0.197 | 0.002 | |
| Hyperglycemia (>11 mmol/L) | No | 219 (89%) | 105.62 (83.05–127.42) | 0.010 |
| Yes | 26 (11%) | 126.58 (94.85–171.39) |
LDL, low-density lipoprotein; HDL, high-density lipoprotein; LBP, lipopolysaccharide-binding protein.
Data are expressed as n (%), mean ± standard deviation (SD), or median (IQR). LPS is expressed as 3HM (pmol/L). p-values are given for the association between each variable and LPS plasma concentration. p-values presented are not corrected for multiple comparisons.
Table 4.
Variables independently associated with LPS plasma concentration.
| Variable | Standardized β | β | 95% CI | p | VIF |
|---|---|---|---|---|---|
| Age, per year | 0.192 | 0.835 | 0.347 to 1.322 | 0.001 | 1.179 |
| BMI > 30 kg/m2 | −0.018 | −2.667 | −20.081 to 14.747 | 0.763 | 1.162 |
| HR, per log unit | 0.053 | 29.479 | −33.226 to 92.184 | 0.355 | 1.088 |
| Diabetes | 0.375 | 63.484 | 43.470 to 83.497 | <0.001 | 1.196 |
| TG, per g/L | 0.235 | 11.427 | 5.653 to 17.201 | <0.001 | 1.209 |
| Total cholesterol, per g/L | 0.204 | 26.337 | 10.73 to 41.944 | 0.001 | 1.246 |
| Glycemia > 11 mmol/L | 0.100 | 19.148 | −3.246 to 41.542 | 0.093 | 1.179 |
n = 238 patients; R2 = 0.308; adjusted R2 = 0.287; Durbin–Watson test: 2.048; F-ratio = 14.650; p < 0.001. β values are regression coefficients.
Relationship between endotoxemia and inflammation
Interleukin (IL)-6 and CRP were below the detection threshold in most patients (74% and 84%, respectively). We found no association between the measured cytokines [IL-6, IL-8, tumor necrosis factor (TNF)-α] and LPS (p > 0.05). A level of CRP higher than 10 mg/L was not associated with LPS (Table 5).
Table 5.
Associations between LPS plasma concentration, inflammation, and short- and long-term outcomes.
| Variable |
n (%) or median (IQR) N = 245 |
Total LPS or r | p | |
|---|---|---|---|---|
| Inflammation | ||||
| IL-6 > 3.2 (pg/ml) | No | 181 (73.9%) | 106.59 (83.69–131.00) | 0.799 |
| Yes | 64 (26.1%) | 102.39 (82.00–132.47) | ||
| IL-8 > 3.2 (pg/ml) | No | 146 (59.6%) | 107.98 (86.70–133.62) | 0.144 |
| Yes | 99 (40.4%) | 104.51 (78.95–125.75) | ||
| TNF-α (pg/ml) | 9.31 (6.23–12.65) | −0.015 | 0.821 | |
| CRP > 10 mg/L | No | 204 (83.6%) | 106.50 (83.65–131.16) | 0.617 |
| Yes | 40 (16.4%) | 103.72 (81.99–130.83) | ||
| Short-term outcome (in-hospital)a | ||||
| Length of ICU stay, days | 3 (3–4) | 0.180 | 0.005 | |
| MACE | No | 180 (73%) | 108.37 (85.19–133.13) | 0.119 |
| Yes | 65 (27%) | 97.48 (79.80–126.24) | ||
| Death | No | 242 (98.8%) | 106.36 (83.37–130.84) | 0.380 |
| Yes | 3 (1.2%) | 89.12 (52.89–x) | ||
| Recurrent MI | No | 236 (96.3%) | 106.36 (83.65–131.58) | 0.413 |
| Yes | 9 (3.7%) | 97.48 (68.46–127.93) | ||
| Heart failure | No | 187 (76.3%) | 108.12 (83.62–132.69) | 0.329 |
| Yes | 58 (23.7%) | 100.41 (81.23–127.18) | ||
| Ventricular arrhythmia | No | 230 (93.9%) | 106.50 (83.72–131.71) | 0.305 |
| Yes | 15 (6.1%) | 94.89 (82.22–124.62) | ||
| Supraventricular arrhythmia | No | 230 (93.9%) | 106.25 (83.37–131.94) | 0.676 |
| Yes | 15 (6.1%) | 110.44 (82.22–125.33) | ||
| Long-term outcome (1-year)b | ||||
| MACE | No | 212 (86.5%) | 106.15 (83.09–130.58) | 0.636 |
| Yes | 33 (13.5%) | 111.42 (86.28–132.56) | ||
| Death | No | 231 (94.3%) | 106.32 (83.16–130.67) | 0.941 |
| Yes | 14 (5.7%) | 108.65 (83.35–133.21) | ||
| Recurrent MI | No | 241 (98.4%) | 106.18 (83.30–131.00) | 0.859 |
| Yes | 4 (1.6%) | 112.45 (83.75–132.93) | ||
| Heart failure | No | 238 (97.1%) | 106.25 (83.06–130.84) | 0.399 |
| Yes | 7 (2.9%) | 116.15 (91.88–246.44) | ||
| Unscheduled PCI | No | 228 (93.1%) | 106.15 (83.09–130.00) | 0.364 |
| Yes | 17 (6.9%) | 113.90 (95.74–134.16) | ||
| CABG | No | 237 (96.7%) | 106.40 (83.53–131.50) | 0.400 |
| Yes | 8 (3.3%) | 99.89 (76.80–121.32) | ||
| Unstable angina | No | 244 (99.6%) | 106.25 (83.23–131.16) | 0.865 |
| Yes | 1 (0.4%) | 112.45 | ||
| Angina pectoris | No | 243 (99.2%) | 106.32 (83.44–130.67) | 0.616 |
| Yes | 2 (0.8%) | 212.79 (80.26–x) | ||
LPS is expressed as 3HM (pmol/L). p-values are given for the association between each variable and LPS plasma concentration. p-values presented are not corrected for multiple comparisons.
In-hospital MACE: CV death, recurrent MI, and HF.
1-year MACE: CV death, recurrent MI, HF, unscheduled PCI, CABG, unstable angina, and angina pectoris.
Relationship between endotoxemia and short-term outcome
LPS blood concentration was not associated with initial severity (Table 2) nor with the occurrence of MACE (or any of its components) or all-cause mortality (p = 0.4) during hospital stay, as assessed by GRACE and SYNTAX scores. However, LPS was associated with a longer ICU stay (r = 0.18, p = 0.005) (Table 5).
Relationship between endotoxemia and long-term (1-year) outcome
LPS blood concentration was not associated with the occurrence of 1-year MACE (or any of its components) nor with all-cause mortality (p = 0.9, Table 5).
Discussion
Lipopolysaccharide plasma concentration at hospital admission was associated with metabolic conditions (in particular cholesterol, triglyceride concentrations, and diabetes) and age rather than with MI severity. LPS concentrations were not associated with inflammatory biomarkers, coronary artery disease severity assessed by angiography, or short-term and long-term occurrence of MACE.
When compared with measurements obtained using the same method and in the same laboratory, the LPS plasma concentrations in our cohort were slightly higher than those reported in healthy volunteers [106 (83–131) vs. 96 (77–116)] but lower than in patients with septic shock [106 (83–131) vs. 134 (126–142)] (20). These findings are in line with previous studies that reported increased endotoxin concentrations in patients with coronary artery disease (10, 21), which led to a hypothesis about the role of LPS proinflammatory activity in atherosclerosis development (22, 23) and MI pathogenesis (7). However, whether low-grade endotoxemia in MI patients is related to pre-existing metabolic conditions or acute digestive translocation linked to an MI event remains to be determined. Moreover, as LPS is mostly inactive in human blood, the LPS burden is imperfectly captured by LPS activity measurement (i.e., an increase in activity could represent either higher translocation or a decreased host inactivation capacity) (24). Our findings, which suggest an increased LPS mass concentration, further suggest an increase in gut-derived absorption rather than a default in the inactivation process.
Endotoxemia has been shown to produce low-grade inflammation, which is involved in the pathogenesis of obesity (25). Lipid and carbohydrate metabolism are also associated with endotoxemia (26). In particular, LPS absorption might occur through chylomicron metabolism, which is closely related to triglyceride absorption (27). Obesity is associated with dysregulations in lipid (i.e., hypertriglyceridemia, low HDL cholesterol, high LDL cholesterol) (28) and carbohydrate (i.e., hyperglycemia, hyperinsulinemia, and insulin resistance) (29) metabolism, both of which were associated with endotoxemia in our cohort. Nevertheless, there was no association between obesity and endotoxemia after adjustment for these confounding conditions. Therefore, our results give new insight into the relationship between obesity and endotoxemia by suggesting that this association is driven by metabolic alterations. During the acute phase of gut barrier disruption, PLTP negatively correlates with LPS concentration, probably reflecting increased elimination capacity (30–32). In contrast, the positive association between PLTP activity and LPS reported here might be related to the increase in PLTP activity documented in patients with metabolic syndrome (33), further suggesting the presence of metabolic endotoxemia in our cohort. We did not observe associations between endotoxemia and inflammation in our cohort, probably due to the early measurement of inflammatory biomarkers (before the peak was reached). We observed lower LPS levels in smokers. Whereas smoking and endotoxemia have been described as increasing the risk of incident atherosclerosis (23), previous studies did not report an association between smoking and increased endotoxin activity (34).
In a previous study reporting on endotoxemia attributed to gut barrier failure in the acute phase of MI, the authors noted a peak value for LPS activity on day 2 and associations between LPS concentration (delta day 2 − day 1) and adverse post-MI CV events (9). In our cohort, LPS measured at admission was associated with heart rate and shock index, suggesting a link between LPS and hemodynamic changes in MI. LPS is known to trigger inflammation, and these hemodynamic changes might reflect inflammation-related vasoplegia. LPS was also correlated to longer cardiac ICU length of stay, suggesting the clinical consequences of acute translocation. Nevertheless, we found no association between LPS measured at admission and post-MI adverse events, thus suggesting that LPS concentration measured at admission has few clinical consequences.
Some limitations need to be underlined. This was a single-center study; therefore, our findings require external validation. There was no sample size calculation, and some analyses might lack power. The inflammation parameters were taken very early (at hospital admission), and many measurements were below the threshold for detection (probably measured before peak). As a consequence, the relationships between LPS, vascular tone, and acute inflammation warrant further evaluation. Repeated or daily measurements of LPS could have provided additional information on the translocation mechanisms in the acute phase of MI. A combination of LPS activity and LPS mass measurement may also have provided further insight. A comparison with patients undergoing percutaneous coronary intervention without evidenced atherosclerosis and with atherosclerosis but no myocardial infarction could have provided additional information on the respective roles of metabolic and acute endotoxemia. Describing the reasons for patients’ ICU length of stay duration could have provided additional interesting information. We measured the total 3HM; thus, it is possible that part of the 3HM measured might be derived from human metabolites. However, bacterial LPS is the major part of total 3HM, and total 3HM is highly associated with LPS concentration (19).
In conclusion, at admission, higher LPS levels were related to metabolic alterations (cholesterol, triglyceride, and diabetes) and age. They were also associated with hemodynamic modifications (higher heart rate and shock ratio) and longer cardiac ICU length of stay but were not associated with inflammation and short- or long-term MACEs. Altogether, endotoxins measured at admission in patients with MI seemed to reflect low-grade metabolic endotoxemia due to pre-existing conditions leading to myocardial infarction rather than acute clinical severity. Endotoxins, therefore, do not appear to be a relevant therapeutic target for treating acute MI, but targeting endotoxemia could represent a promising strategy to prevent metabolic disorders and subsequent coronary artery disease progression. However, these findings require further confirmation.
Acknowledgments
The authors thank Suzanne Rankin for the English revision of the manuscript and Morgane Laine for providing technical assistance.
Funding Statement
The authors declare financial support was received for the research, authorship, and/or publication of this article.
This work was supported by the Dijon University Hospital, French Federation of Cardiology, Association de Cardiologie de Bourgogne and by grants from the Agence Régionale de Santé (ARS) de Bourgogne-Franche-Comté and from the Regional Council of Burgundy-Franche-Comté. This work was supported by a French Government grant managed by the French National Research Agency (Agence nationale de la recherche) as part of the “Investissements d'Avenir” program, reference: ANR-11-LABX-0021-01- LipSTIC Labex. It is also part of an integrated project funded by the French government (Regional Council of Bourgogne-Franche-Comté).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the University Hospital of Dijon. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MN: Writing – review & editing, Writing – original draft. AP: Writing – review & editing, Writing – original draft, Methodology, Conceptualization. DM: Writing – review & editing, Writing – original draft, Supervision. YC: Writing – review & editing, Writing – original draft. TG: Supervision, Writing – review & editing, Writing – original draft. LT: Writing – review & editing, Writing – original draft. A-LR: Writing – review & editing, Writing – original draft. P-GG: Writing – review & editing, Writing – original draft. MM: Formal Analysis, Data curation, Writing – review & editing, Writing – original draft. J-PP: Writing – review & editing, Writing – original draft. VD: Writing – review & editing, Writing – original draft. MF: Writing – review & editing, Writing – original draft. LL: Writing – review & editing, Writing – original draft, Supervision. MZ: Writing – review & editing, Writing – original draft, Validation, Supervision, Methodology, Investigation, Conceptualization.
Conflict of interest
MF reports having received grants, consulting fees, and/or honoraria and delivering lectures for Abbott, Amarin, Amgen, AstraZeneca, Ajanta, Kowa, Merck and Co, Novartis, Organon, Pfizer, Recordati, Sanofi/Regeneron, Servier, SMB, Ultragenyx, and Viatris. YC reports receiving consultant or speaking fees for Bayer, BMS/Pfizer, Boehringer Ingelheim, Novartis, Sanofi, and Servier. MZ declares research grants from Amarin Corp and speaking fees from Organon. MN declares research grants and consulting fees from Baxter, educational fees from Fresenius, and congress fees from Pfizer. P-GG receive fees for lectures from Aguettant, AOP, Baxter, Medtronic, Edwards and Vygon. P-GG is a consultant for ABBOT.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Beutler B, Rietschel E. Innate immune sensing and its roots: the story of endotoxin. Nat Rev Immunol. (2003) 3:169–76. 10.1038/nri1004 [DOI] [PubMed] [Google Scholar]
- 2.Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. (2007) 56:1761–72. 10.2337/DB06-1491 [DOI] [PubMed] [Google Scholar]
- 3.Pussinen PJ, Havulinna AS, Lehto M, Sundvall J, Salomaa V. Endotoxemia is associated with an increased risk of incident diabetes. Diabetes Care. (2011) 34:392–7. 10.2337/DC10-1676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boutagy NE, McMillan RP, Frisard MI, Hulver MW. Metabolic endotoxemia with obesity: is it real and is it relevant? Biochimie. (2016) 124:11–20. 10.1016/j.biochi.2015.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gautier T, Deckert V, Nguyen M, Desrumaux C, Masson D, Lagrost L. New therapeutic horizons for plasma phospholipid transfer protein (PLTP): targeting endotoxemia, infection and sepsis. Pharmacol Ther. (2022) 236:108105. 10.1016/J.PHARMTHERA.2021.108105 [DOI] [PubMed] [Google Scholar]
- 6.Gautier T, Lagrost L. Plasma PLTP (phospholipid-transfer protein): an emerging role in “reverse lipopolysaccharide transport” and innate immunity. Biochem Soc Trans. (2011) 39:984–8. 10.1042/BST0390984 [DOI] [PubMed] [Google Scholar]
- 7.Carnevale R, Sciarretta S, Valenti V, di Nonno F, Calvieri C, Nocella C, et al. Low-grade endotoxaemia enhances artery thrombus growth via toll-like receptor 4: implication for myocardial infarction. Eur Heart J. (2020) 41:3156–65. 10.1093/EURHEARTJ/EHZ893 [DOI] [PubMed] [Google Scholar]
- 8.Asada M, Oishi E, Sakata S, Hata J, Yoshida D, Honda T, et al. Serum lipopolysaccharide-binding protein levels and the incidence of cardiovascular disease in a general Japanese population: the Hisayama study. JAHA. (2019) 8:e013628. 10.1161/JAHA.119.013628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou X, Li J, Guo J, Geng B, Ji W, Zhao Q, et al. Gut-dependent microbial translocation induces inflammation and cardiovascular events after ST-elevation myocardial infarction. Microbiome. (2018) 6:66. 10.1186/S40168-018-0441-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carrera-Bastos P, Picazo Ó, Fontes-Villalba M, Pareja-Galeano H, Lindeberg S, Martínez-Selles M, et al. Serum zonulin and endotoxin levels in exceptional longevity versus precocious myocardial infarction. Aging Dis. (2018) 9:317. 10.14336/AD.2017.0630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soraya H, Masoud WGT, Gandhi M, Garjani A, Clanachan AS. Myocardial mechanical dysfunction following endotoxemia: role of changes in energy substrate metabolism. Basic Res Cardiol. (2016) 111:24. 10.1007/s00395-016-0544-7 [DOI] [PubMed] [Google Scholar]
- 12.Suffredini AF, Fromm RE, Parker MM, Brenner M, Kovacs JA, Wesley RA, et al. The cardiovascular response of normal humans to the administration of endotoxin. N Engl J Med. (1989) 321:280–7. 10.1056/NEJM198908033210503 [DOI] [PubMed] [Google Scholar]
- 13.Frangogiannis NG, Smith CW, Entman ML. The inflammatory response in myocardial infarction. Cardiovasc Res. (2002) 53:31–47. 10.1016/S0008-6363(01)00434-5/2/53-1-31-GR3.GIF [DOI] [PubMed] [Google Scholar]
- 14.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. (2017) 377:1119–31. 10.1056/NEJMOA1707914 [DOI] [PubMed] [Google Scholar]
- 15.Nguyen M, Gautier T, Masson D, Bouhemad B, Guinot P-G. Endotoxemia in acute heart failure and cardiogenic shock: evidence, mechanisms and therapeutic options. J Clin Med. (2023) 12:2579. 10.3390/JCM12072579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zeller M, Steg PG, Ravisy J, Lorgis L, Laurent Y, Sicard P, et al. Relation between body mass index, waist circumference, and death after acute myocardial infarction. Circulation. (2008) 118:482–90. 10.1161/CIRCULATIONAHA.107.753483 [DOI] [PubMed] [Google Scholar]
- 17.Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, et al. Assessment of the SYNTAX score in the syntax study. EuroIntervention. (2009) 5:50–6. 10.4244/EIJV5I1A9 [DOI] [PubMed] [Google Scholar]
- 18.Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. (2003) 163:2345–53. 10.1001/ARCHINTE.163.19.2345 [DOI] [PubMed] [Google Scholar]
- 19.de Barros J-P P, Gautier T, Sali W, Adrie C, Choubley H, Charron E, et al. Quantitative lipopolysaccharide analysis using HPLC/MS/MS and its combination with the limulus amebocyte lysate assay. J Lipid Res. (2015) 56:1363–9. 10.1194/jlr.D059725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dargent A, De Barros J-P P, Ksiazek E, Fournel I, Dusuel A, Rerole AL, et al. Improved quantification of plasma lipopolysaccharide (LPS) burden in sepsis using 3-hydroxy myristate (3HM): a cohort study. Intensive Care Med. (2019) 45(11):1678–80. 10.1007/s00134-019-05749-0 [DOI] [PubMed] [Google Scholar]
- 21.Simonsen JR, Järvinen A, Harjutsalo V, Forsblom C, Groop P-H, Lehto M. The association between bacterial infections and the risk of coronary heart disease in type 1 diabetes. J Intern Med. (2020) 288:711–24. 10.1111/joim.13138 [DOI] [PubMed] [Google Scholar]
- 22.Westerterp M, Berbée JFP, Pires NMM, Van Mierlo GJD, Kleemann R, Romijn JA, et al. Apolipoprotein C-I is crucially involved in lipopolysaccharide-induced atherosclerosis development in apolipoprotein E–knockout mice. Circulation. (2007) 116:2173–81. 10.1161/CIRCULATIONAHA.107.693382 [DOI] [PubMed] [Google Scholar]
- 23.Wiedermann CJ, Kiechl S, Dunzendorfer S, Schratzberger P, Egger G, Oberhollenzer F, et al. Association of endotoxemia with carotid atherosclerosis and cardiovascular disease: prospective results from the Bruneck study. J Am Coll Cardiol. (1999) 34:1975–81. 10.1016/S0735-1097(99)00448-9 [DOI] [PubMed] [Google Scholar]
- 24.Nguyen M, Pallot G, Jalil A, Tavernier A, Dusuel A, Le Guern N, et al. Intra-abdominal lipopolysaccharide clearance and inactivation in peritonitis: key roles for lipoproteins and the phospholipid transfer protein. Front Immunol. (2021) 12:1641. 10.3389/FIMMU.2021.622935/BIBTEX [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dubinski P, Czarzasta K, Cudnoch-Jedrzejewska A. The influence of gut microbiota on the cardiovascular system under conditions of obesity and chronic stress. Curr Hypertens Rep. (2021) 23:31. 10.1007/S11906-021-01144-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Määttä AM, Salminen A, Pietiäinen M, Leskelä J, Palviainen T, Sattler W, et al. Endotoxemia is associated with an adverse metabolic profile. Innate Immun. (2021) 27:3. 10.1177/1753425920971702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghoshal S, Witta J, Zhong J, de Villiers W, Eckhardt E. Chylomicrons promote intestinal absorption of lipopolysaccharides. J Lipid Res. (2009) 50:90–7. 10.1194/jlr.M800156-JLR200 [DOI] [PubMed] [Google Scholar]
- 28.Klop B, Elte JWF, Cabezas MC. Dyslipidemia in obesity: mechanisms and potential targets. Nutrients. (2013) 5:1218–40. 10.3390/nu5041218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singla P, Bardoloi A, Parkash AA. Metabolic effects of obesity: a review. World J Diabetes. (2010) 1:76. 10.4239/WJD.V1.I3.76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nguyen M, Gautier T, Reocreux G, Pallot G, Maquart G, Bahr P-A, et al. Increased phospholipid transfer protein activity is associated with markers of enhanced lipopolysaccharide clearance in human during cardiopulmonary bypass. Front Cardiovasc Med. (2021) 8:756269. 10.3389/FCVM.2021.756269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deckert V, Lemaire S, Ripoll P-J, de Barros J-PP, Labbé J, Borgne CC-L, et al. Recombinant human plasma phospholipid transfer protein (PLTP) to prevent bacterial growth and to treat sepsis. Sci Rep. (2017) 7:3053. 10.1038/s41598-017-03285-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Payen D, Dupuis C, Deckert V, de Barros J-PP, Rérole A-L, Lukaszewicz A-C, et al. Endotoxin mass concentration in plasma is associated with mortality in a multicentric cohort of peritonitis-induced shock. Front Med (Lausanne). (2021) 8:749405. 10.3389/FMED.2021.749405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lebrun LJ, Pallot G, Nguyen M, Tavernier A, Dusuel A, Pilot T, et al. Increased weight gain and insulin resistance in HF-fed PLTP deficient mice is related to altered inflammatory response and plasma transport of gut-derived LPS. Int J Mol Sci. (2022) 23:13226. 10.3390/IJMS232113226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Erridge C, Attina T, Spickett CM, Webb DJ. A high-fat meal induces low-grade endotoxemia: evidence of a novel mechanism of postprandial inflammation. Am J Clin Nutr. (2007) 86:1286–92. 10.1093/AJCN/86.5.1286 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.