Abstract
Objective
The objective was to estimate the rural–urban differences in the receipt of prepregnancy, prenatal, and postpartum services.
Methods
The authors conducted a cross-sectional data analysis using data from the Pregnancy Risk Assessment and Monitoring System from 2016 to 2018 to analyze rural–urban differences in the receipt of medical visits and care content delivery during the prepregnancy year, as well as the prenatal and postpartum periods among birthing people in the US, using survey-weighted multivariable logistic regression models.
Results
Rural-dwelling birthing people were significantly less likely to attend a medical visit in the prepregnancy year or postpartum period, even when controlled for sociodemographic and clinical characteristics. Compared to their urban counterparts, they were also less likely to receive comprehensive screening and counseling in the prepregnancy and postpartum maternity phases.
Conclusion
Efforts to ameliorate rural–urban differences in maternal care access and quality should explicitly adopt multilevel, systemic approaches to policy and program implementation and evaluation. Policymakers and practitioners should consider telehealth as a potential complementary tool to minimize gaps in quality of care which disproportionately impact rural-dwelling birthing people.
Keywords: Urban, prepregnancy, postpartum, Rural, Differences, birthings
Introduction
Rural-dwelling birthing people in the US face alarming gaps in maternal health care beyond labor and delivery. 1,2 Exacerbated by a shortage of maternal health care practitioners and by rural hospital closures, the provision of high-quality, comprehensive maternal health care in rural communities is currently insufficient. 3–8 High-quality, comprehensive maternal health care refers to guideline-concordant care before, during, and after pregnancy that allows practitioners to identify and treat medical and behavioral health needs and provides essential counseling to new parents to plan for a healthy pregnancy and birth. In addition to efficient, risk-appropriate medical visits from prepregnancy to postpartum, other examples of guideline-concordant maternal care include counseling, with topics ranging from controlling medical conditions and health maintenance, family planning, smoking, and testing for sexually transmitted infections. 9–12 Not only are these care components recommended by national quality standards, they are the basis of practitioner reimbursement and are connected with additional financial incentives for practitioners and health systems. 13,14
Without high-quality, comprehensive maternal care, rural-dwelling birthing people face greater likelihood of worse health outcomes. Rural-dwelling birthing people have a 9% greater probability of severe maternal morbidity and mortality than those living in urban areas during childbirth hospitalization, even after controlling for sociodemographic characteristics and clinical conditions. 15
Poor maternal morbidity and mortality outcomes for rural-dwelling birthing people may point to subpar maternal health care delivery and access throughout prepregnancy, pregnancy, and after childbirth. Recent evidence has found that rural communities who experience a Labor and Delivery unit closure are less likely to achieve an overall adequate number of prenatal care visits compared to similar communities in counties that maintained their Labor & Delivery units. 16 One study found that > 50% of rural US counties have no hospital obstetric services. 17 Rural-dwelling birthing people are also more likely to be transferred from one hospital to another both prior to and after childbirth, which indicates an inability of the original hospital to provide the level of care needed for the mother and/or infant. 18 Patient-related factors further complicate access to high-quality, comprehensive maternal health care for rural birthing people. Rural residents aged 18–64 years reported the highest rates of delayed care or no medical care due to cost (18.6%) and no health insurance coverage (23.1%). 19 Less than 50% of rural women have access to maternal services within a 30-mile drive from their home, and > 10% of rural women drive ≥ 100 miles for these services. 20–22 Many rural residents face work challenges during pregnancy and returning to work following childbirth, which may hinder their ability to seek needed medical services. 23
Telehealth has been heralded as a promising method of expanding and sustaining local access to maternal health services. 24 Prior studies have recommended that clinical and policy efforts to address poor maternal and infant outcomes include telehealth for practitioner-to-practitioner consultations. 25–27 Telehealth can be used for various services, including prenatal care, maternal–fetal medicine consultation, fetal echocardiography, fetal heart rate monitoring, genetic counseling, and monitoring chronic illnesses. 28 Telehealth may benefit patients by reducing travel burdens to see a practitioner, which can reduce the time burden for rural residents from pregnancy through postpartum. Telehealth also may increase access to subspecialists not available in a patient’s community. 29,30 Benefits of telehealth for practitioners and health care systems include reduced travel by practitioners to different clinic locations. 31–33 Local practitioners may also benefit from having better access to subspecialty practitioners, which allows them to manage their patients locally instead of referring to tertiary centers. 28,34 Despite calls for increasing use of telehealth in rural communities, little is known about where telehealth may be best targeted to address gaps in maternal health services.
The objective of this study was to examine rural–urban differences in current trends in the receipt of guideline-concordant prepregnancy, prenatal, and postpartum maternal health care and counseling. Such evidence is urgently needed to focus efforts to eliminate rural–urban disparities in maternal health delivery and, subsequently, in outcomes. This study used a nationally representative data set to identify gaps in service delivery to rural birthing people compared to their urban counterparts.
Materials and Methods
The authors used the Pregnancy Risk Assessment Monitoring System (PRAMS) surveillance survey data collected in 40 states, New York City, and Puerto Rico from 2016 to 2018, available through the Centers for Disease Control and Prevention (CDC). 1 From birth certificate data, participating states select a stratified random sample of all birthing people who delivered a liveborn, oversampling to ensure sufficient data are available in smaller subpopulations. The survey collects data using a standardized mail and telephone survey of recently postpartum people, including demographic characteristics, insurance status, health care utilization, and health outcomes before, during, and after pregnancy. The CDC upholds a minimum overall response rate threshold policy for each survey year, which ranged between 50% and 55% for this study’s data; response rates by site and year are publicly available online.
Rural vs urban residency was determined by a dichotomized variable derived from the 6-level urban–rural classification developed by the National Center for Health Statistics in 2013 for 3141 US counties and county-equivalents.
For each respondent in the sample, the authors assessed the primary outcomes: 1) receipt of a health care visit in the 12 months prior to pregnancy, 2) receipt of a prenatal care visit, and 3) receipt of a postpartum care visit. Among patients who received any of these visits, the authors assessed the secondary outcomes of the receipt of (4–6) any of the counseling components at least once in that maternity phase, and (7–9) receipt of at least half of the counseling components during the prepregnancy, prenatal, and postpartum phases. These secondary outcomes were specifically selected as a proxy for quality of care delivered to birthing people, because the available evidence base supports the comprehensive delivery of these care components in primary and maternal care.
Prior research has shown that rural residents’ sociodemographic characteristics—including age, educational level, marital status, income, race/ethnicity, language, insurance, and parity—are associated with maternal care utilization. 10,35 Consistent with prior studies, the authors kept age, education level, and income as categorical variables, and marital status and language as dichotomous variables. Household income was calculated as a percentage of the Federal Poverty Level (FPL), and respondents with missing income data were retained by creating a missing data indicator that was incorporated into this study’s models. To classify race/ethnicity, the authors used self-reported variables provided in PRAMS derived from the birth certificate and added language as a proxy for nativity or acculturation in similar studies. 36,37 The authors followed methods that the CDC and other authors have previously used to characterize insurance coverage into Medicaid, private, and uninsured. 35 The Medicaid category included birthing people who reported enrollment in Medicaid or a state-named Medicaid program. The private category included those who reported private insurance alone or in combination with Medicaid and birthing people who reported TRICARE or other military insurance. The uninsured category included birthing people who reported no insurance. In line with the US Census, other national surveys, and previous PRAMS analyses, respondents reporting coverage from the Indian Health Service were also classified as uninsured. 35,38,39 Last, maternal chronic conditions, including self-reported diagnoses of gestational diabetes, hypertension, and depression, were included.
In this cross-sectional analysis with pooled 2016–2018 PRAMS data, the authors examined the association between rurality and birthing people’s self-report of whether they received medical visits and counseling components in the prepregnancy year, prenatal, and postpartum periods. First, descriptive statistics were used to describe the demographic characteristics of the sample. The authors calculated unadjusted, survey-weighted percentages of self-reported receipt of each associated medical visit, as well as each counseling component delivered to birthing people in the prepregnancy, prenatal, and postpartum periods (eg, with “unadjusted” denoting that the authors did not control for any covariates). The authors tested differences between rural and urban birthing people in the receipt of counseling components in the 3 phrases, with p < 0.05 considered significant.
To measure the association between rurality and receipt of any visits in the 3 periods, odds ratios (ORs) were estimated using survey-weighted multivariable logistic regression models, controlling for the sociodemographic and clinical characteristics listed in Table 1. The authors controlled for year of birth to account for temporal trends in the data.
Table 1:
Sample characteristics
| Sample characteristic | All birthing people in the sample | Urban | Rural | p Value |
|---|---|---|---|---|
| (N = 103,425) | (N = 83,542) | (N = 19,888) | ||
| Age, y | < 0.001 | |||
| < 20 | 5091 (4.9) | 3695 (4.1) | 1396 (6.6) | |
| 20–24 | 19,285 (18.7) | 14,402 (17.0) | 4883 (26.5) | |
| 25–29 | 30,373 (29.4) | 23,888 (28.5) | 6485 (33.1) | |
| 30–34 | 29,995 (29.0) | 25,364 (30.9) | 4631 (22.7) | |
| ≥35 | 18,679 (18.1) | 16,191 (19.4) | 2488 (11.1) | |
| Missing | 2 (0) | 2 (0) | 0 (0) | |
| Education level | < 0.001 | |||
| Less than high school | 13,559 (13.1) | 10,452 (11.9) | 3107 (14.7) | |
| High school | 25,164 (24.3) | 19,179 (22.9) | 5985 (32.2) | |
| More than high school | 63,595 (61.5) | 52,910 (64.2) | 10,685 (52.7) | |
| Missing | 1107 (1.1) | 1001 (0.99) | 106 (0.46) | |
| Marital status | < 0.001 | |||
| Married | 61,624 (59.6) | 50,654 (63.1) | 10,970 (57.6) | |
| Not married | 41,697 (40.3) | 32,815 (36.9) | 8882 (42.3) | |
| Missing | 104 (0.10) | 73 (0) | 31 (0.11) | |
| Income, % of the FPL | < 0.001 | |||
| < 100 | 33,286 (32.2) | 25,266 (28.8) | 8020 (38.2) | |
| 100–138 | 8802 (8.5) | 6899 (7.9) | 1903 (10.4) | |
| 139–199 | 5999 (5.8) | 4682 (5.3) | 1317 (6.7) | |
| ≥200 | 46,129 (44.6) | 39,046 (48.9) | 7083 (37.1) | |
| Missing | 9209 (8.9) | 7649 (9.2) | 1560 (7.6) | |
| Race/ethnicity | < 0.001 | |||
| White, non-Hispanic | 50,000 (48.3) | 38,035 (54.4) | 11,965 (75.7) | |
| Black, non-Hispanic | 19,222 (18.6) | 17,674 (15.5) | 1548 (7.5) | |
| Hispanic | 10,594 (10.2) | 9376 (12.9) | 1218 (5.9) | |
| Asian/Pacific-Islander | 7238 (7.0) | 6801 (6.7) | 437 (1.1) | |
| American Indian/Alaskan Native | 4530 (4.4) | 1767 (0.52) | 2763 (3.2) | |
| Other/mixed race | 10,779 (10.4) | 8935 (8.7) | 1844 (6.2) | |
| Missing | 1062 (1.0) | 954 (1.3) | 108 (0.48) | |
| Language | < 0.001 | |||
| English | 95,511 (92.4) | 76,488 (90.8) | 19,023 (96.1) | |
| Non-English | 7914 (7.7) | 7054 (9.2) | 860 (3.9) | |
| Insurance | < 0.001 | |||
| Medicaid | 45,215 (43.7) | 35,225 (39.2) | 9990 (48.6) | |
| Private | 51,943 (50.2) | 43,756 (54.9) | 8187 (42.9) | |
| Uninsured | 3638 (3.5) | 2632 (3.2) | 1006 (4.9) | |
| Other | 1778 (1.7) | 1314 (1.9) | 464 (2.4) | |
| Missing | 851 (0.82) | 615 (0.77) | 236 (1.1) | |
| Parity | < 0.001 | |||
| Nulliparous | 39,678 (38.4) | 32,645 (38.8) | 7033 (34.7) | |
| 1 previous live birth | 32,536 (31.5) | 26,544 (33.3) | 5992 (32.4) | |
| Multiparous | 30,987 (30.0) | 24,171 (27.7) | 6816 (32.7) | |
| Missing | 224 (0.22) | 182 (0.2) | 42 (0.17) | |
| Chronic conditions | ||||
| Gestational diabetes | 7314 (7.1) | 5959 (6.7) | 1355 (5.8) | 0.13 |
| Missing | 193 (0.19) | 132 (0.15) | 61 (0.21) | |
| Hypertension | 11,411 (11.0) | 9175 (8.6) | 2236 (8.9) | 0.26 |
| Missing | 194 (0.19) | 133 (0.15) | 61 (0.21) | |
| Depression | 14,565 (14.1) | 11,059 (12.1) | 3506 (18.1) | < 0.001 |
| Missing | 960 (0.93) | 822 (0.92) | 138 (0.62) |
Note: Data are presented as unweighted n, percentages in parentheses.
Authors’ analysis of data for 2016–2018 from the Pregnancy Risk Assessment Monitoring System (PRAMS) data set. The sample size (N = 103,425) and all numbers in the table are unweighted; percentages are survey-weighted to represent the US birthing population, representing 5,523,032 birthing people in 40 states, New York City, and Puerto Rico. Other/mixed race/ethnicity includes “other non-White” and “mixed race.” The authors further excluded Vermont from this study sample (ie, all analyses) due to the authors’ inability to standardize its race/ethnicity information to the rest of the available states in PRAMS for analyses. The authors show missing data for transparency purposes; a missing data indicator was incorporated for those in this study’s eligible sample who were missing only income data.
FPL, Federal Poverty Level.
Six additional outcome measures were then generated capturing whether respondents received any of the counseling components or at least half of the counseling and risk screening components associated with the prepregnancy, prenatal, and postpartum phases of maternal care that PRAMS asks respondents. The authors used survey-weighed multivariable logistic regression models with these outcomes. To improve interpretability, the authors calculated average marginal effects (AMEs) of rurality, which represented the difference in predicted probabilities of receiving any or half of counseling components if respondents were rural or urban, holding all other covariates constant at observed values for each observation.
All analyses applied survey weights provided by the CDC to account for the complex survey design, accounting for sampling, nonresponse, and noncoverage using overall birth certificate data from each participating state. A 2-sided p value of < 0.05 was considered statistically significant, and the authors conducted all analyses using Stata 16.1 SE. 40 However, the authors specifically took care to denote significant analysis findings in which rural and urban birthing people differed by at least 5 percentage points, a threshold the authors determined for spotlighting clinically significant differences. This study of deidentified survey data was exempt from the University of North Carolina at Chapel Hill institutional review board.
Results
This analysis was representative of 5,523,032 births (unweighted N = 103,425) in the period 2016–2018, including 4,722,060 (unweighted N = 83,542) births among urban residents and 800,972 (unweighted N = 19,883) births among rural residents (Table 1). Compared to urban residents who gave birth, higher proportions of rural residents were younger and had fewer years of education. Higher proportions of rural residents also had incomes that were < 100% of the FPL (38.2% vs 28.8%), identified as non-Hispanic White (75.7% vs 54.4%), were covered by Medicaid (48.6% vs 39.2%) and were more likely to have depression (18.1% vs 12.1%) than their urban counterparts. Rural residents were less likely than urban birthing people to be married (57.6% vs 63.1%), and speak a non-English language (3.9 vs 9.2%) than urban residents.
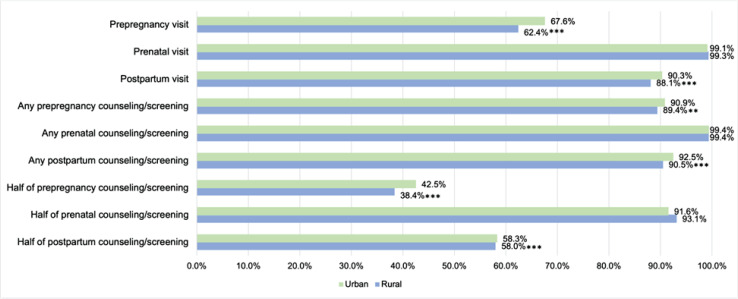
The proportion of rural residents who reported receiving a prepregnancy visit in the 12 months prior to pregnancy, those who reported receiving at least half of the 12 prepregnancy counseling and risk screening components, and those who reported at least half of the 10 postpartum counseling and risk screening components were statistically significantly lower than urban residents. Figure 1 displays the unadjusted, survey-weighted percentage of respondents who received prepregnancy, prenatal, and postpartum medical visits and associated counseling and risk screening components by rurality. However, only receipt of a prepregnancy visit differed by > 5 percentage points between rural and urban birthing people.
Figure 1:
Authors’ analysis of data for 2016–2018 from the Pregnancy Risk Assessment Monitoring System (PRAMS) data set of birthing people who reported receiving medical visits, any of the counseling they were asked about, and at least half of the counseling components associated with that maternity stage they were asked about. Percentages are survey-weighted proportions representing the US birthing population in participating PRAMS states. Other/mixed race/ethnicity includes “other non-White” and “mixed race.”
Furthermore, rural residents were statistically less likely than their urban counterparts to receive a postpartum visit or to receive any of the prepregnancy or postpartum care components about which they were asked. Across the maternity phases, there was wide variation in the self-reported receipt of the individual counseling and risk screening components (Supplemental Material 1). Among rural residents, the receipt of individual care components ranged from 13% to 79% in the prepregnancy period, 58% to 95% in the prenatal period, and 14% to 88% in the postpartum period. Overall, in the prepregnancy phase, managing conditions such as diabetes and blood pressure were rarely discussed (13%), and rural residents reported lower rates (defined as ≥ 5 percentage points of difference) than urban birthing people of being tested for HIV (25%), being counseled to take a vitamin with folic acid (32%), and being counseled on their desire to have or not have children (39%).
Although rural birthing people reported significantly lower rates of receiving 4 postpartum care components, rates between rural and urban birthing people did not exceed a 5 percentage point difference. However, rural birthing people were statistically significantly more likely to report receiving 8 of the 10 counseling and risk screening care components in the prenatal period and 1 in the postpartum period; only 1 (smoking assessment in postpartum) exceeded the 5 percentage point difference threshold between rural and urban birthing people.
Table 2 shows the adjusted ORs (aORs) from survey-weighted multivariable logistic regressions models for the likelihood of birthing people receiving any prepregnancy, prenatal, or postpartum medical visits. When controlling for sociodemographic and other clinical conditions, rural residents were found to have decreased odds of receiving a prepregnancy health visit in the 12 months prior to pregnancy (aOR = 0.867; p < 0.001) and increased odds of receiving a prenatal visit compared with urban residents (aOR = 1.437; p < 0.05).
Table 2:
Likelihood of receiving medical visits in the 12 months prior to pregnancy, during pregnancy, and postpartum
| Category | Likelihood of receiving any prepregnancy doctor visit in the 12 months prior to pregnancy | Likelihood of receiving any prenatal visit during pregnancy | Likelihood of receiving a postpartum check-up visit |
|---|---|---|---|
| aOR (95% CI) |
aOR (95% CI) |
aOR (95% CI) |
|
| Rurality | |||
| Urban | Ref | Ref | Ref |
| Rural | 0.867 (0.814–0.924)*** |
1.437 (1.026–2.014)* |
0.969 (0.883–1.064) |
| Age, y | |||
| < 20 | Ref | Ref | Ref |
| 20–24 | 0.780 (0.691–0.881)*** |
1.932 (1.254–2.979)** |
1.028 (0.877–1.205) |
| 25–29 | 0.974 (0.860–1.102) |
2.016 (1.279–3.179)** |
1.305 (1.105–1.542)** |
| 30–34 | 1.244 (1.092–1.417)** |
2.309 (1.362–3.915)** |
1.542 (1.288–1.846)*** |
| ≥ 35 | 1.460 (1.272–1.677)*** |
1.630 (0.940–2.825) |
1.357 (1.121–1.643)** |
| Education | |||
| Less than high school | Ref | Ref | Ref |
| High school | 1.087 (1.003–1.178)* |
1.712 (1.283–2.284)*** |
1.398 (1.263–1.547)*** |
| More than high school | 1.739 (1.602–1.889)*** |
2.982 (2.116–4.202)*** |
1.959 (1.756–2.186)*** |
| Marital status | |||
| Not married | Ref | Ref | Ref |
| Married | 1.192 (1.124–1.264)*** |
1.443 (1.102–1.890)** |
1.234 (1.132–1.346)*** |
| Income, % of the FPL | |||
| < 100 | Ref | Ref | Ref |
| 100–138 | 1.113 (1.021–1.213)* |
1.330 (0.867–2.039) |
1.378 (1.204–1.576)*** |
| 139–199 | 1.166 (1.051–1.295)** |
1.513 (0.861–2.659) |
1.264 (1.079–1.481)** |
| ≥ 200 | 1.862 (1.728–2.006)*** |
2.211 (1.486–3.288)*** |
1.885 (1.680–2.116)*** |
| Missing | 0.840 (0.773–0.914)*** |
1.515 (1.058–2.170)* |
1.046 (0.930–1.177) |
| Race/ethnicity | |||
| White, non-Hispanic | Ref | Ref | Ref |
| Black, non-Hispanic | 0.837 (0.779–0.899)*** |
0.694 (0.494–0.976)* |
0.869 (0.782–0.966)** |
| Hispanic | 0.724 (0.664–0.790)*** |
1.107 (0.688–1.780) |
0.933 (0.820–1.062) |
| Asian, Pacific-Islander | 0.393 (0.358–0.432)*** |
0.162 (0.118–0.223)*** |
0.706 (0.611–0.816)*** |
| American Indian/Alaskan Native | 0.795 (0.700–0.903)*** |
0.937 (0.648–1.355) |
0.704 (0.612–0.810)*** |
| Other/mixed race | 0.703 (0.644–0.767)*** |
1.250 (0.747–2.092) |
0.753 (0.660–0.858)*** |
| Language | |||
| English | Ref | Ref | Ref |
| Non-English | 0.773 (0.695–0.858)*** |
1.522 (0.889–2.604) |
1.127 (0.974–1.306) |
| Insurance | 0.773*** | 1.522 | 1.127 |
| Private | Ref | Ref | Ref |
| Medicaid | 0.599 (0.562–0.638)*** |
0.882 (0.650–1.196) |
0.734 (0.663–0.813)*** |
| Uninsured | 0.463 (0.401–0.534)*** |
0.243 (0.148–0.399)*** |
0.435 (0.362–0.522)*** |
| Other | 0.700 (0.576–0.850)*** |
0.811 (0.374–1.759) |
0.784 (0.592–1.040) |
| Parity | |||
| Nulliparous | Ref | Ref | Ref |
| 1 previous live birth | 0.883 (0.833–0.935)*** |
1.299 (0.950–1.776) |
0.758 (0.690–0.832)*** |
| Multiparous | 0.765 (0.717–0.817)*** |
1.038 (0.757–1.425) |
0.534 (0.482–0.591)*** |
| Chronic Conditions | |||
| Gestational diabetes | 0.977 (0.891–1.070) |
1.143 (0.717–1.823) |
1.099 (0.955–1.265) |
| Hypertension | 1.120 (1.034–1.212)** |
0.979 (0.660–1.453) |
1.082 (0.959–1.222) |
| Depression | 1.832 (1.706–1.968)*** |
0.818 (0.591–1.130) |
0.786 (0.716–0.863)*** |
| Year | |||
| 2016 | Ref | Ref | Ref |
| 2017 | 1.096 (1.037–1.158)** |
1.073 (0.811–1.419) |
1.124 (1.034–1.222)** |
| 2018 | 1.114 (1.052–1.180)*** |
1.052 (0.797–1.390) |
1.051 (0.964–1.146) |
| N | 98,341 | 97,194 | 97,645 |
Note: Data are presented as exponentiated coefficients, 95% confidence intervals in parentheses.
*p < 0.05, ** p < 0.01, *** p < 0.001 based on survey-weighed multivariable logistic regression results.
Authors’ analysis of data for 2016–2018 from the Pregnancy Risk Assessment Monitoring System (PRAMS) data set. The sample size for each model is unweighted; all other data are weighted to represent the US birthing population in participating PRAMS states. aORs controlled for maternal age, education, marital status, income, maternal race, spoken language, insurance, parity, chronic conditions, and birth year.
aOR, adjusted odds ratio; CI, confidence interval; FPL, Federal Poverty Level; Ref, reference.
Table 3 compares AMEs by rurality for the receipt of prepregnancy, prenatal, and postpartum counseling components. Being rural was associated with a 1.05 percentage point decrease in the probability of overall receipt of any prepregnancy counseling (p < 0.05) and with a 2.4 percentage point decrease in the probability of receipt of at least half of the recommended prepregnancy counseling components (p < 0.01). Being rural was also associated with a 0.7 percentage point decrease in the probability of receiving any postpartum counseling (p < 0.05). Conversely, being rural was associated with a 1.04 percentage point higher probability of receiving at least half of the prenatal counseling care components (p < 0.01).
Table 3:
Comparison of marginal effects by rurality for receipt of Prepregnancy, Prenatal, and Postpartum Counseling Components
| Rural/N | Prepregnancy counseling components | Prenatal counseling components | Postpartum counseling components | |||
|---|---|---|---|---|---|---|
| Receipt of any of the 12 | Receipt of at least half of the 12 | Receipt of any of the 10 | Receipt of at least half of the 10 | Receipt of any of the 12 | Receipt of at least half of the 12 | |
| Rural | −0.0105 (0.00508)* |
−0.0240 (0.00837)** |
0.00129 (0.000851) |
0.0104 (0.00381)** |
−0.00770 (0.00387)* |
0.00281 (0.00696) |
| N | 65,113 | 65,113 | 97,251 | 97,251 | 94,614 | 94,614 |
Note: Data are presented as average marginal effects, standard errors in parentheses.
** p < 0.01, * p < 0.05 based on predicted marginal effects based on survey-weighted multivariable regression results.
Authors’ analysis of data for 2016–2018 from the Pregnancy Risk Assessment Monitoring System (PRAMS) data set. The sample size for each model is unweighted; all other data are weighted to represent the US birthing population in participating PRAMS states. Adjusted models controlled for maternal age, education, marital status, income, maternal race, spoken language, insurance, parity, chronic conditions, and birth year. CI = confidence interval.
Discussion
The results of the present study show that rural-dwelling birthing people receive slightly different maternal care than their urban counterparts from the year before getting pregnant through pregnancy and postpartum. Rural-dwelling birthing people are less likely to receive any doctor visit in the 12 months before getting pregnant, and the counseling and screenings they receive in the year before pregnancy and in the postpartum period are less likely to be comprehensive. Conversely, rural-dwelling birthing people are more likely to have a visit with a health care practitioner in the prenatal period, and for that visit to incorporate more recommended counseling components than for urban counterparts, although these differences are within a few percentage points and are not likely to be very clinically significant. These findings suggest that the series of prenatal visits that progress in frequency throughout pregnancy likely increase the chances that rural-dwelling birthing people get more comprehensive care than they otherwise would and may explain this study’s findings that rural-dwelling birthing people receive more comprehensive prenatal care than their urban counterparts overall.
Considerable heterogeneity was found in the receipt of counseling components associated with the prepregnancy, prenatal, and postpartum periods; urban-dwelling birthing people were predicted to receive more substantive counseling than their rural counterparts, particularly in the prepregnancy and postpartum periods. These results suggest that although efforts to expand insurance and telehealth use among rural-dwelling communities have the potential to improve overall quality of care, such policies alone may not be sufficient to meet the needs of diverse, rural-dwelling patient populations.
Lower receipt and comprehensiveness of a health visit in the year before getting pregnant may present underlying health access challenges for rural-dwelling people (which may be further alleviated by access to telehealth), as well as unmet social and health needs, including maintaining continuous insurance coverage for birthing people through the postpartum year. Furthermore, a majority of maternal deaths occur in the postpartum period, which has traditionally consisted of one 6-week visit rather than a series of visits which comprise prenatal care. 41 Because rural-dwelling birthing people face a 9% greater probability of severe maternal morbidity and mortality overall than their urban counterparts, these findings suggest that clinical and policy approaches should address both individual- and system-related barriers to help narrow gaps in care for rural-dwelling birthing people. 15,18
These findings further suggest that important opportunities exist to inflect maternal care access and quality disparities for rural-dwelling birthing people in the year before getting pregnant and during the postpartum year. To improve care for rural-dwelling birthing people, the findings of this study support calls for rural-specific policy solutions and health system transformation, given the worsening rural maternity access and higher prevalence of potential risk factors among rural-dwelling birthing populations.
Additionally, some counseling components where the authors identified significant differences between rural and urban birthing people could readily be delivered via telehealth and do not need to be delivered by a physician. There is an opportunity for health systems to incorporate information about these service gaps for their rural populations when planning telehealth implementation and expansion to better meet care needs for birthing people in the year before they get pregnant and in the postpartum year. Future research should not only focus on evaluating the effectiveness of telehealth and how it modifies maternal care delivery in the long-term but should also assess the accessibility and use telehealth with an eye toward geographic equity across the maternal health continuum. Telehealth may have an important role to play in decreasing geographic disparities in access to care, and effective and thoughtful telehealth interventions for rural-dwelling birthing people are likely to look different from prepregnancy through the postpartum period.
Arguably, this study’s findings about the comprehensiveness of counseling and screening received by birthing people have the greatest clinical relevance, as they underline specific areas in the prepregnancy, prenatal, and postpartum phases where efforts or interventions may be helpful in narrowing quality gaps between rural and urban-dwelling birthing people. This may include innovative ways to deliver counseling and care to help rural-dwelling people manage any medical conditions such as diabetes and high blood pressure before pregnancy, for example, or offering birth control counseling for postpartum birthing people.
This study had several limitations. First, the dichotomous measure of urban vs rural residence does not fully capture the heterogeneity and variation of rural areas in the US. Second, the data did not allow us to adjust for area-level characteristics (such as the presence of maternity hospitals and other maternity practitioners) which differentially impact rural and urban-dwelling birthing people. Third, although these data captured a more comprehensive picture of the receipt of prepregnancy, prenatal, and postpartum visits and care content received by birthing people than is traditionally discernible in claims, these outcome variables were subject to measurement error. Respondents self-reported outcome variables of interest after they had given birth, which may subject them to reporting and recall bias. Additionally, the availability of data for this study’s primary outcome measures limited the study’s generalizability, given that only a subset of this study’s sample who had already received a prepregnancy, prenatal, or postpartum visit was subject to the corresponding counseling questions. Fourth, the present study’s sample included data from only 40 states. Although these included states represent a broad range of geographies and compositions of birthing people, the results are not generalizable to states that did not participate in the survey or states the authors excluded due to issues with data availability.
Implications for Practice and Policy
The findings of this study highlight the importance of addressing barriers to health care access within rural-dwelling communities to enable birthing people to utilize recommended care. Rural-dwelling birthing people face a myriad of health-care access challenges, including travel burden, 42,43 workforce shortages, and limited access to specialists. 44 In addition to added chronic disease burden and higher poverty rates among rural-dwelling communities, 45 these inequalities highlight the need for policy efforts that encompass systemic and multilevel approaches to eliminate disparities in maternal health care outcomes between rural and urban communities of birthing people.
Conclusion
Findings from this cross-sectional survey of birthing people suggest that rural-dwelling birthing people are less likely to receive any doctor visit in the 12 months before getting pregnant. Key opportunities exist to improve the quality of maternal care delivery to rural-dwelling people in the year before pregnancy and in the postpartum period, which should inform rural-specific policy solutions, as well as thoughtful deployment and evaluation of the use of telehealth across the maternal health continuum.
Supplementary Material
Supplemental Material
Acknowledgments
This study was supported by the Office for the Advancement of Telehealth (OAT), Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services (HHS).The information and conclusions in this presentation are those of the authors and no inferred endorsement by OAT, HRSA, or HHS, nor does mention of any department or agency names imply endorsement by the US government. The authors gratefully acknowledge the Pregnancy Risk Assessment Monitoring System Working Group and the Centers for Disease Control and Prevention for providing access to PRAMS data for this project.
Footnotes
Our analysis excluded Arizona, California, District of Columbia, Idaho, Indiana, Florida, Nevada, Ohio, Oregon, South Carolina, and Tennessee.
Author Contributions: Study conception and design: Christopher M Shea, PhD, MA, MPA, Burcu Bozkurt, PhD, and Saif Khairat, PhD, MPH; analysis and interpretation of results: Burcu Bozkurt, PhD, Christopher M Shea, PhD, MA, MPA, Joshua M Weinstein, PhD, MPP, Dorothy Cilenti, DrPH, MSW, Monisa Aijaz, MD, MPH, and Saif Khairat, PhD, MPH; draft manuscript preparation: Burcu Bozkurt, PhD, Christopher M Shea, PhD, MA, MPA, Monisa Aijaz, MD, MPH, Joshua M Weinstein, PhD, MPP, and Saif Khairat, PhD, MPH. All authors reviewed the results and approved the final version of the manuscript.
Conflicts of Interest: None declared
Funding: This study was supported by the Health Resources and Services Administration (HRSA; grant 6 U3GRH40003-01-01).
Data-Sharing Statement: Underlying data are not available.
References
- 1. Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611–620. 10.1016/j.puhe.2015.04.001 [DOI] [PubMed] [Google Scholar]
- 2. Maron DF. Maternal health care is disappearing in rural America. Scientific American; 2017. [Google Scholar]
- 3. Young RA. Maternity care services provided by family physicians in rural hospitals. J Am Board Fam Med. 2017;30(1):71–77. 10.3122/jabfm.2017.01.160072 [DOI] [PubMed] [Google Scholar]
- 4. Henning-Smith C, Almanza J, Kozhimannil KB. The maternity care nurse workforce in rural U.S. hospitals. J Obstet Gynecol Neonatal Nurs. 2017;46(3):411–422. 10.1016/j.jogn.2017.01.010 [DOI] [PubMed] [Google Scholar]
- 5. Rural Hospital Closures: NC Rural Health Research Program. The Cecil G. Sheps Center for Health Services Research. 2022. Accessed 1 March 2024. https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/
- 6. Rural Hospital Closures: Number and Characteristics of Affected Hospitals and Contributing Factors. GAO-18-634. U.S. Government Accountability Office. 2018. Accessed 1 March 2024. https://www.gao.gov/products/gao-18-634
- 7. Hung P, Kozhimannil K, Henning-Smith C, Casey M. Closure of Hospital Obstetric Services Disproportionately Affects Less-Populated Rural Counties. Minneapolis, Minnesota: University of Minnesota Rural Health Research Center; 2017. [Google Scholar]
- 8. Mental Health Care Health Professional Shortage Areas (HPSAs) . Kaiser Family Foundation. 2021. Accessed 1 March 2024. https://www.kff.org/other/state-indicator/mental-health-care-health-professional-shortage-areas-hpsas/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
- 9. STDs during Pregnancy Treatment and Care. Atlanta, GA: Centers for Disease Control and Prevention; 2015. Accessed https://www.cdc.gov/std/pregnancy/stdfact-pregnancy-detailed.htm [Google Scholar]
- 10. McKinney J, Keyser L, Clinton S, Pagliano C. ACOG Committee Opinion No. 736: Optimizing postpartum care. Obstet Gynecol. 2018;132(3):784–785. 10.1097/AOG.0000000000002849 [DOI] [PubMed] [Google Scholar]
- 11. Prepregnancy counseling: Committee Opinion No. 762. American Society for Reproductive Medicine, American College of Obstetricians and Gynecologists' Committe on Gynecologic Practice. Fertil Steril. 2019;111(1):32–42. 10.1016/j.fertnstert.2018.12.003 [DOI] [PubMed] [Google Scholar]
- 12. Guidelines for Perinatal Care: Eighth Edition. Elk Grove Village, IL: American Academy of Pediatrics; 2017. [Google Scholar]
- 13. Centers for Medicare & Medicaid Services . 2021 Core Set of Maternal and Perinatal Health Measures for Medicaid and CHIP (Maternity Core Set). 2021. Accessed 1 October 2023. https://www.medicaid.gov/medicaid/quality-of-care/downloads/2021-maternity-core-set.pdf
- 14. Prenatal Depression Screening and Follow-up (PND): National Committee of Quality Assurance. Accessed 1 October 2023. https://www.ncqa.org/hedis/measures/prenatal-depression-screening-and-followup/
- 15. Kozhimannil KB, Interrante JD, Henning-Smith C, Admon LK. Rural-urban differences in severe maternal morbidity and mortality in the US, 2007-15. Health Aff (Millwood). 2019;38(12):2077–2085. 10.1377/hlthaff.2019.00805 [DOI] [PubMed] [Google Scholar]
- 16. Radke SM, Smeins L, Ryckman KK, Gruca TS. Closure of Labor & Delivery units in rural counties is associated with reduced adequacy of prenatal care, even when prenatal care remains available. J Rural Health. 2023;39(4):746–755. 10.1111/jrh.12758 [DOI] [PubMed] [Google Scholar]
- 17. Hung P, Henning-Smith CE, Casey MM, Kozhimannil KB. Access to obstetric services in rural counties still declining, with 9 percent losing services, 2004–14. Health Aff (Millwood). 2017;36(9):1663–1671. 10.1377/hlthaff.2017.0338 [DOI] [PubMed] [Google Scholar]
- 18. Kozhimannil KJ, Kristensen-Cabrera A, Henning-Smith C, Theiler R. Severe Maternal Morbidity and Hospital Transfer Among Rural Residents. Minneapolis, MN: University of Minnesota Rural Health Research Center; 2019. [Google Scholar]
- 19. Health, United States, 2011 . With Special Feature on Socioeconomic Status and Health. National Center for Health Statistics, United States. Hyattsville, MD: United States Health; 2012. [PubMed] [Google Scholar]
- 20. Centers for M, Medicaid S. Improving Access to Maternal Health Care in Rural Communities, issue brief. Accessed 1 March 2024. https://www.cms.gov/About-CMS/Agency-Information/OMH/equity-initiatives/rural-health/09032019-Maternal-Health-Care-in-Rural-Communities.pdfLast
- 21. Rayburn WF, Richards ME, Elwell EC. Drive times to hospitals with perinatal care in the United States. Obstet Gynecol. 2012;119(3):611–616. 10.1097/AOG.0b013e318242b4cb [DOI] [PubMed] [Google Scholar]
- 22. American Congress of Obstetricians and Gynecologists . Workforce Studies and Planning Group. The Obstetrician-gynecologist Distribution Atlas. Washington, DC: American Congress Obstetricians and Gynecologists; 2013:132. [Google Scholar]
- 23. Corbett C, DeArruda Wharton K, Kozhimannil K. Challenges Related to Pregnancy and Returning to Work after Childbirth in a Rural, Tourism-Dependent Community. Minneapolis, MN: University of Minnesota Rural Health Research Center; 2018. [Google Scholar]
- 24. Williams RL, Meredith AH, Ott MA. Expanding adolescent access to hormonal contraception: An update on over-the-counter, pharmacist prescribing, and web-based telehealth approaches. Curr Opin Obstet Gynecol. 2018;30(6):458–464. 10.1097/GCO.0000000000000497 [DOI] [PubMed] [Google Scholar]
- 25. Mann S, McKay K, Brown H. The maternal health compact. N Engl J Med. 2017;376(14):1304–1305. 10.1056/NEJMp1700485 [DOI] [PubMed] [Google Scholar]
- 26. Magann EF, Bronstein J, McKelvey SS, Wendel P, Smith DM, Lowery CL. Evolving trends in maternal fetal medicine referrals in a rural state using telemedicine. Arch Gynecol Obstet. 2012;286(6):1383–1392. 10.1007/s00404-012-2465-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Implementing telehealth in practice. Obstet Gynecol. 2020;135(2):e73–e79. 10.1097/AOG.0000000000003671 [DOI] [PubMed] [Google Scholar]
- 28. Greiner AL. Telemedicine applications in obstetrics and gynecology. Clin Obstet Gynecol. 2017;60(4):853–866. 10.1097/GRF.0000000000000328 [DOI] [PubMed] [Google Scholar]
- 29. Khairat S, McDaniel P, Jansen M, Francis T, Edson B, Gianforcaro R. Analysis of social determinants and the utilization of pediatric tele-urgent care during the COVID-19 pandemic: Cross-sectional study. JMIR Pediatr Parent. 2021;4(3). 10.2196/25873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Khairat S, Haithcoat T, Liu S, et al. Advancing health equity and access using telemedicine: A geospatial assessment. J Am Med Inform Assoc. 2019;26(8–9):796–805. 10.1093/jamia/ocz108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Haleem A, Javaid M, Singh RP, Suman R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens Int. 2021;2:100117. 10.1016/j.sintl.2021.100117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Khairat S, Lin X, Liu S, et al. Evaluation of patient experience during virtual and in-person urgent care visits: Time and cost analysis. J Patient Exp. 2021;8:2374373520981487. 10.1177/2374373520981487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Khairat S, Tirtanadi K, Ottmar P, Sleath B, Obeid J. Evaluating the perceptions of teleconsent in urban and rural communities. Eur J Biomed Inform (Praha). 2019;15(2). [PMC free article] [PubMed] [Google Scholar]
- 34. Marcin JP, Shaikh U, Steinhorn RH. Addressing health disparities in rural communities using telehealth. Pediatr Res. 2016;79(1–2):169–176. 10.1038/pr.2015.192 [DOI] [PubMed] [Google Scholar]
- 35. Daw JR, Winkelman TNA, Dalton VK, Kozhimannil KB, Admon LK. Medicaid expansion improved perinatal insurance continuity for low-income women. Health Aff (Millwood). 2020;39(9):1531–1539. 10.1377/hlthaff.2019.01835 [DOI] [PubMed] [Google Scholar]
- 36. Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: A systematic review of public health studies with hispanic populations in the United States. Soc Sci Med. 2009;69(7):983–991. 10.1016/j.socscimed.2009.05.011 [DOI] [PubMed] [Google Scholar]
- 37. Carter-Pokras O, Zambrana RE, Yankelvich G, Estrada M, Castillo-Salgado C, Ortega AN. Health status of Mexican-origin persons: do proxy measures of acculturation advance our understanding of health disparities? J Immigr Minor Health. 2008;10(6):475–488. 10.1007/s10903-008-9146-2 [DOI] [PubMed] [Google Scholar]
- 38. Artiga S, Duckett P. Health coverage and care for American Indians and Alaska Natives. San Francisco, CA: Henry J. Kaiser Family Foundation; 2013. [Google Scholar]
- 39. Cohen R. Long-term trends in health insurance: estimates from the National Health Interview Survey, 1968–2018. Hyattsville, MD: National Center for Health Statistics; 2019. [Google Scholar]
- 40. StataCorp . Stata Statistical Software: Release 16. College Station, TX: StataCorp, LLC; 2019. [Google Scholar]
- 41. Li XF, Fortney JA, Kotelchuck M, Glover LH. The postpartum period: The key to maternal mortality. Int J Gynaecol Obstet. 1996;54(1):1–10. 10.1016/0020-7292(96)02667-7 [DOI] [PubMed] [Google Scholar]
- 42. Hung P, Casey MM, Kozhimannil KB, Karaca-Mandic P, Moscovice IS. Rural-urban differences in access to hospital obstetric and neonatal care: How far is the closest one? J Perinatol. 2018;38(6):645–652. 10.1038/s41372-018-0063-5 [DOI] [PubMed] [Google Scholar]
- 43. Sheets LR, Wallach E, Khairat S, Mutrux R, Edison K, Becevic M. Similarities and differences between rural and urban telemedicine utilization. Perspect Health Inf Manag. 2021;18(Winter). 10.1111/jrh.12112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kozhimannil KB, Casey MM, Hung P, Han X, Prasad S, Moscovice IS. The rural obstetric workforce in US hospitals: Challenges and opportunities. J Rural Health. 2015;31(4):365–372. 10.1111/jrh.12112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Centers for Disease Control and Prevention . About Rural Health. Atlanta, GA: Centers for Disease Control and Prevention; 2017. Accessed 1 March 2024. https://www.cdc.gov/ruralhealth/about.html [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material