Abstract
Background:
Calcaneal avulsion fractures (CAvFs) at the Achilles tendon insertion are among the more challenging fractures to treat. Although rare, they often require reoperation. The optimal treatment, including nonsurgical procedures and better implants for surgical procedures in the treatment of CAvFs, remains to be established. Therefore, our study aimed to (1) perform a descriptive evaluation of CAvFs, including cases managed nonsurgically, and (2) assess surgical procedures, including the incidence of complications and reoperation for surgically treated CAvFs.
Methods:
In this multicenter retrospective study, we collected data of patients with CAvFs treated at 9 hospitals from 2012 to 2022. We performed a descriptive study of CAvFs and compared postoperative complications and reoperation rates for multiple surgical techniques and implants. The size of the bone fragments was quantified.
Results:
The data of 70 patients with CAvFs were analyzed; 20 patients were treated nonsurgically, and 50 were treated surgically. The mean age of patients was 68.5 years; 67% of the patients were female. Nineteen percent of the patients had diabetes, and 19% had osteoporosis. The incidence of postoperative complications was 30%, with infection in 14%, necrosis in 26%, and loss of reduction in 18%. The reoperation rate was 22%. Surgical techniques with use of cannulated cancellous screws were performed in 80% of the surgical cases. Cannulated cancellous screw (CCS) fixation alone resulted in a reoperation rate of 35%, whereas additional augmentation, including washers with CCS fixation, resulted in a reoperation rate of 10%. CCS fixation was successfully performed, although suture anchors were used in some cases with smaller fragments.
Conclusions:
CAvFs occurred more frequently in older women and had a high rate of postoperative complications. A combination of CCS with augmentation was more effective at reducing postoperative complications than CCS fixation alone, even when the bone fragment size was small.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Calcaneal fractures constitute about 1.2% of all fractures. Among these, calcaneal avulsion fractures (CAvFs) specifically at the Achilles tendon insertion, which do not extend into the subtalar joint, account for 1.3% to 2.7% of calcaneal fractures1. CAvFs are distinct from other calcaneal avulsion injuries such as those involving the anterior process or the calcaneocuboid ligament.
CAvFs are more common in older women with osteoporosis or diabetes mellitus1-12. Early repair and fixation are recommended for CAvFs to minimize damage to soft tissues and improve the function of the gastrocnemius-soleus complex4,9. Various surgical methods exist, including methods using cannulated cancellous screws, suture anchors, tension-band wiring, and plates. Cannulated cancellous screw (CCS) fixation is the most common method of surgical treatment8. However, bone fragility and preexisting comorbidities often result in treatment failure that requires reoperation, and these fractures are considered challenging to repair1-12. A previous study reported the occurrence of soft-tissue compromise and fixation failure in a substantial number of CAvFs treated at 2 Level-I trauma centers. The study reported that implant failure or fracture displacement was noted in 28.2% of patients, postoperative wound complications requiring local wound care affected 17.9% of patients, and reoperation was necessary in 35.9% of patients10. The optimal implants and surgical procedures for CAvFs have not yet been established because CAvFs are relatively rare; thus, it is difficult to report a large number of treated cases6,10-12.
In this multicenter retrospective analysis, we aimed to (1) perform a descriptive evaluation of CAvFs, including nonsurgically treated cases, and (2) assess surgical procedures, including the incidence of complications and reoperation for surgically treated CAvFs.
Materials and Methods
Since 2012, the Trauma Research Group of Nagoya (TRON) has maintained a database of orthopaedic trauma cases at its 9 member hospitals that are affiliated with the Department of Orthopaedic Surgery at our university. All eligible patients were registered using an opt-out consent process. The registry received ethical approval from all participating institutions, and this study received institutional ethical approval (2020-564). For the present study, we extracted patient information from the TRON database for 72 patients with CAvFs treated from 2012 to 2022. The details (such as patient demographics) were extracted from the medical records of each facility and reviewed retrospectively. CAvFs are characterized by an extra-articular fracture line extending from the tuberosity to a point posterior to the subtalar joint and involving the osseous insertion of the Achilles tendon13.
Data Collection
Data were collected from patients’ medical charts at each facility. We obtained demographic data, including patient age, sex, body mass index, smoking status, diabetes mellitus, corticosteroid use, osteoporosis, Fracture Mobility Score, mechanism of injury (low or high-energy trauma, traffic injury), and closed or open fracture. The Fracture Mobility Score classifies the patient’s mobility as 1 of the following 5 categories: (0) freely mobile without aids, (1) mobile outdoors with 1 aid, (2) mobile outdoors with 2 aids or a walker, (3) some indoor mobility but never going outside without help, and (4) no functional mobility (no use of lower limbs)14. Soft-tissue injuries were classified according to the Tscherne classification15. For surgical cases, we also obtained the time to operation (number of days), operative time, and surgical fixation method (use of CCS alone; use of CCS with augmentation by a washer, suture anchor, tension-band wiring, or Steinmann pin; use of a washer, suture anchor, tension-band wiring, or Steinmann pin alone; or debridement). We investigated the following conditions as postoperative complications: surgical site infection, skin necrosis, loss of reduction, and reoperation. Surgical site infection was defined as an infection that occurred within 3 months after surgery, and it was classified as superficial or deep infection according to the presence or absence of surgical intervention16. Skin necrosis was identified by the appearance of dark, thick, leathery tissue or yellow, tan, green, or brown and moist, loose, and stringy tissue17. Loss of reduction was defined as fragment displacement of >10 mm or failure of the implant that required revision surgery because of soft-tissue complication or the prospect of nonunion10.
Radiographic Evaluation
Radiographic data were obtained by reading the radiographic computerized images in medical records. The radiographic evaluation included an analysis of conventional radiographs, including lateral and axial views preoperatively, immediately postoperatively, and at 3, 6, and 12 months postoperatively, with additional radiographs that may have been obtained as needed during the course of treatment.
The axial view was made with the patient in the supine position, with the plantar surface of the foot at 90° to the table in the frontal and sagittal planes, and the x-ray tube was tilted 40° cranially and directed at the mid-heel18. CAvFs were classified as Type I: sleeve fractures, Type II: beak fractures, or Type III: infrabursal avulsion fractures, as described by Beavis et al.1 (see Appendix Supplemental Table 1).
On a lateral view radiograph, the length of the fracture line of the bone fragment was defined as the base. A perpendicular line was drawn from the base to the calcaneal tuberosity, and its length was defined as the height. The “fragment index” was calculated using the following formula: (height × base)/2 (Fig. 1). Each measurement was made twice by 1 orthopaedic surgeon (Y. Takahashi) at intervals of 2 weeks.
Fig. 1.
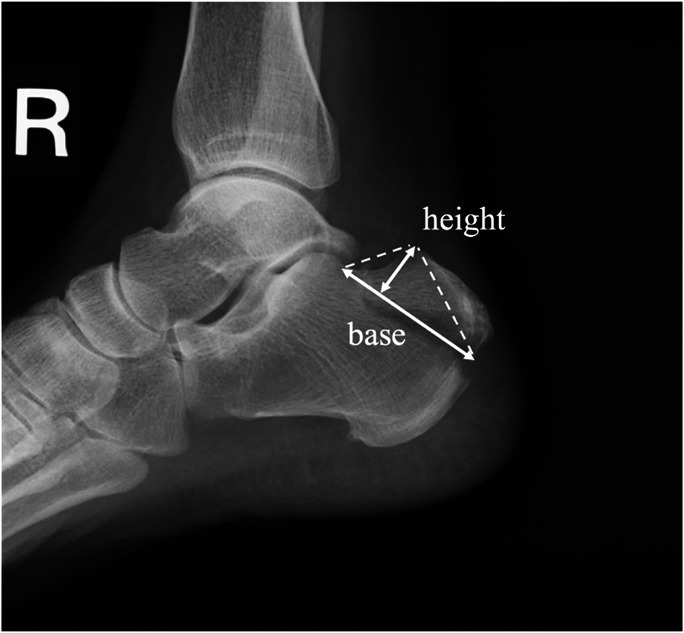
The “fragment index” was calculated as (height × base)/2 on a lateral view radiograph.
Nonsurgical Treatment
Nonsurgical treatment was selected in cases in which a physician determined that the bone-fragment displacement was minor and the soft-tissue condition was relatively good; functional demands were low; the risk of surgery was high; or the patient refused surgery. The method consisted of 6 to 8 weeks of cast immobilization in a mild equinus position, followed by weekly radiographs and soft-tissue evaluation. Physical therapy was then initiated, and the patient’s weight-bearing was gradually increased4,9.
Surgical Technique and Postoperative Management
In the emergency department, protocols are established to elevate the injured limb. When the patient is in bed, a Thomas splint or suitable padding is used to elevate the limb, maintaining this position during the period of waiting for surgery. The median waiting time from injury to surgery was 3 days (range, 0 to 19 days).
Typically, nondisplaced fractures do not necessitate surgical intervention. In our multicenter retrospective study, the criteria for surgical treatment were determined at the discretion of the attending surgeons. The prognostic outcomes of CAvFs are not comprehensively understood. Patients were indicated for surgery even in some cases without displacement or permanent impaired function, if there were concerns about complications from nonsurgical treatment, such as secondary displacement, skin necrosis, and loss of plantar flexion strength19. Some institutions elected to pursue surgical fixation, with objectives including facilitating early mobilization and preempting potential displacement, in cases in which stabilization of the fracture site was deemed practical.
All patients underwent surgery in the prone position under local anesthesia. A 5 to 7-cm vertical skin incision was made directly above the fracture site in every case. Bone fragments of adequate size were fixed by CCS, and for small bone fragments for which CCS insertion was difficult, a suture anchor was used alone1,4,11,12,20. All screws used were partially threaded and ranged from 3.5 to 6.5 mm in diameter. All screws utilized the plantar cortex for fixation3,4,8,11,12,20-22. A washer, suture anchor, tension-band wiring, or Steinmann pin was also used for augmentation. The optimal implants have not yet been established, and the adaptation of the fixation method depends on the surgeon’s preference and the fracture pattern. For use of a suture anchor alone, 2 screw anchors were inserted into the fracture site, and each was sutured to the Achilles tendon with a double Krackow suture weave technique9,23. Tension-band wiring was through a figure-of-8 tension-band wire into the CCS and fixed at the posterior wall of the calcaneus. It was also performed using a Kirschner wire without CCS3,4,10,24. The Steinmann pin was inserted from the bone fragments into the cubital bone and penetrated through the calcaneus.
After surgery, all patients were made non-weight-bearing with immobilization by a cast in the equinus position for 2 to 6 weeks. Physical therapy was then initiated, and the patient’s weight-bearing was gradually increased3,4,22,24.
Clinical Evaluation
American Orthopaedic Foot & Ankle Society (AOFAS) scores were used to evaluate pain and functional outcomes during the follow-up period. We assessed the AOFAS score at 3, 6, and 12 months after surgery25.
Statistical Analysis
A chi-square test and Student t test were performed as univariate analyses to analyze the difference in the incidence of complications. We performed a multiple logistic regression analysis for the failure of CCS fixation. We selected age, sex, smoking status, diabetes mellitus, degree of displacement, and use of augmentation as explanatory factors. We defined p values of <0.05 as significant. All statistical analyses were performed using the EZR software program (version 1.40; Jichi Medical University.)
Results
Demographic Analysis
The data of 70 patients with CAvFs over a period of 11 years were analyzed; 20 patients were treated nonsurgically, and 50 were treated surgically. The mean follow-up period was 10.1 months (range, 3 to 59 months). The mean age was 68.5 years. The study population included 23 male and 47 female patients. Table I shows a comparison of the nonsurgical and surgical cases. The nonsurgical cases tended to have less displacement and lower AOFAS scores (see Appendix Supplemental Table 2).
TABLE I.
Demographic Comparison of Nonsurgical and Surgical Cases
| Nonsurgical Cases | Surgical Cases | P Value | |
|---|---|---|---|
| No. | 20 | 50 | |
| Age* (yr) | 68.6 ± 15.3 | 67.3 ± 16.4 | 0.769 |
| No. male/female | 8/12 | 15/35 | 0.574 |
| Body mass index† (kg/m2) | 21.2 (16.7-27.6) | 22.3 (16.2-29.9) | 0.876 |
| Smoking (no. [%]) | 5 (25.0) | 7 (14.0) | 0.499 |
| Diabetes mellitus (no. [%]) | 5 (25.0) | 8 (16.0) | 0.498 |
| Corticosteroids (no. [%]) | 2 (10.0) | 3 (6.0) | 0.619 |
| Osteoporosis (no. [%]) | 5 (25.0) | 8 (16.0) | 0.498 |
| Fracture Mobility Score (no. [%]) | 0.293 | ||
| 0 | 12 (60.0) | 34 (68.0) | |
| 1 | 5 (25.0) | 14 (28.0) | |
| 2 | 2 (10.0) | 2 (4.0) | |
| 3 | 1 (5.0) | 0 (0.0) | |
| Beavis classification (no. [%]) | 0.047 | ||
| Type I | 13 (65.0) | 16 (32.0) | |
| Type II | 7 (35.0) | 31 (62.0) | |
| Type III | 0 (0.0) | 3 (6.0) | |
| Closed fracture: Tscherne classification (no. [%]) | 0.53 | ||
| Grade 0 | 17 (85.0) | 35 (70.0) | |
| Grade 1 | 3 (15.0) | 12 (24.0) | |
| Grade 3 | 0 (0.0) | 3 (6.0) | |
| Open fracture: Tscherne classification (no. [%]) | — | ||
| Grade 2 | 0 (0.0) | 1 (100.0) | |
| Displacement† (mm) | 7.25 (0.0-57.0) | 20.8 (1.0-56.5) | 0.001 |
The values are given as the mean and standard deviation.
The values are given as the mean, with the range in parentheses.
Analysis of Surgical Treatment, Including Complications and Reoperation
The fixation methods used to treat the fractures were as follows: CCS alone (n = 20), CCS and washer (n = 11), CCS and suture anchor (n = 5), CCS and tension-band wiring (n = 3), CCS and Steinmann pin (n = 1), suture anchor alone (n = 5), tension-band wiring alone (n = 3), and Steinmann pin alone (n = 1). One additional patient received debridement alone (Fig. 2). The average duration of immobilization was 20.6 days (range, 2 to 40 days).
Fig. 2.
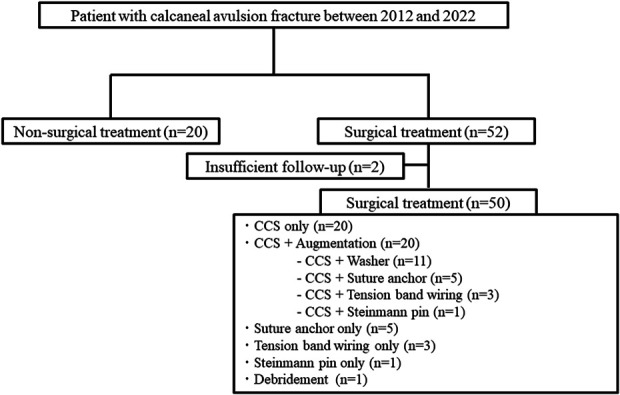
Flow diagram of the participants included in the study. CCS = cannulated cancellous screw.
Postoperative complications occurred in 15 (30%) of the 50 surgical patients and included soft-tissue complications (infection, n = 7 [14%] and necrosis, n = 13 [26%]) and loss of reduction (n= 9; 18%). In the cases of loss of reduction, 7 cases underwent reoperation while 2 cases were observed without reoperation. Many patients had multiple complications, and the details of the 11 cases that resulted in reoperation, excluding implant removal after bone union, are shown in Table II. The reoperation rate was 22%. The average displacement of the fragment in reoperation cases was 23.2 mm (range, 5.4 to 37 mm). Treatment with Steinmann pins caused loss of reduction and soft-tissue complications in 2 of 2 patients. In the group with fixation with CCS, excluding the Steinmann pins, there were complications in 8 of 39 cases.
TABLE II.
Characteristics of the 11 Patients with Reoperation*
| Patient No. | Sex | Age (yr) | Comorbidity, Smoking Status | Beavis Type | Closed Fracture: Tscherne Grade | FI (mm2) | Displacement (mm) | Waiting Time Until Initial Surgery (days) | Surgical Procedure | Complications | Surgical Procedure of Reoperation |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 48 | None | II | 0 | 462 | 24 | 0 | 2 CCS (4 mm) | LOR, necrosis | 2 CCS (4 mm) + washer |
| 2 | F | 66 | DM, smoker | II | 0 | 210.3 | 24.7 | 11 | 2 CCS (3.5 mm) + washer | Infection (deep), necrosis | Debridement, skin grafting |
| 3 | F | 86 | Osteoporosis | II | 1 | 185.6 | 13.5 | 8 | 2 CCS (3.5 mm) | LOR | 2 CCS (4 mm) + washer, suture anchor |
| 4 | F | 85 | None | II | 0 | 132 | 22 | 3 | 2 CCS (4.0 mm) | Necrosis | Debridement, skin grafting |
| 5 | M | 59 | Smoker | I | 0 | 148.5 | 37 | 4 | 2 CCS (3.5 mm) | LOR, necrosis | Debridement, skin grafting, 2 CCS (3.5 mm) + washer, suture anchor |
| 6 | F | 79 | Smoker | II | 0 | 108 | 29 | 0 | 1 CCS (3.5 mm) | LOR | 1 suture anchor added |
| 7 | M | 33 | None | II | 3 | 145.2 | 5.4 | 12 | 2 CCS (4 mm) | Nonunion | Autogenous bone grafting, 2 CCS (4 mm) + washer |
| 8 | F | 65 | DM | I | 1 | 123.5 | 28 | 15 | 2 CCS (4 mm) | Infection (deep), necrosis | Debridement, implant removal |
| 9 | M | 73 | None | III | 0 | 80.5 | 22 | 6 | Suture anchor | LOR, infection (deep), necrosis | Debridement, implant removal, plastic reconstructive surgery |
| 10 | M | 66 | None | II | 0 | 376 | 21 | 1 | 2 Steinmann pins (4 mm) | LOR, infection (deep), necrosis | Debridement, implant removal |
| 11 | M | 34 | None | II | 0 | 568 | 28.5 | 1 | 1 CCS (4.5 mm) + 1 Steinmann pin (4 mm) | LOR, necrosis | Debridement, and 1 more CCS (4.5 mm) added |
FI = fragment index, CCS = cannulated cancellous screw(s), LOR = loss of reduction, and DM = diabetes mellitus.
Detailed Examination of CCS as the Main Treatment Method
CCS was the main treatment method for 40 (80%) of the total 50 surgical cases. CCS fixation without augmentation was performed in 20 cases, while CCS fixation was augmented by different methods, including washer, suture anchor, tension-band wiring, and Steinmann pin augmentation, in 20 cases. The combination of CCS and washer was used in 11 of the 20 cases involving CCS with augmentation. The reoperation rate was 7 (35%) of 20 cases when CCS alone was used for fixation, but 2 (10%) of 20 cases when augmentation was added. We present representative cases illustrating both unsuccessful and successful outcomes in Figures 3 and 4.
Fig. 3.
A case of nonunion. Fig. 3-A A 59-year-old male patient presented with a calcaneal avulsion fracture classified as Beavis Type I. The fragment index was measured at 148 mm2, with displacement being 37 mm. Fig. 3-B A postoperative radiograph shows fracture fixation using 3 cannulated cancellous screws without augmentation. Fig. 3-C At 6 months postoperatively, the patient had experienced nonunion.
Fig. 4.
A successful case. Fig. 4-A An 81-year-old female patient presented with a calcaneal avulsion fracture classified as Beavis Type II. The fragment index was 104, and displacement measured 8 mm. Fig. 4-B A postoperative radiograph shows fixation using 2 cannulated cancellous screws augmented by a washer. Fig. 4-C At 6 months postoperatively, the fracture site had achieved union.
The logistic regression analysis suggested that current smoking, the extent of displacement, and the absence of augmentation were potentially associated with the failure of CCS fixation (see Appendix Supplemental Table 3).
Detailed Examination of Small Bone Fragments
Figure 5 shows the distribution of the fragment index according to the surgical procedure, divided into cases treated with 1 CCS + augmentation, suture anchor alone, and others (cases treated with >1 CCS with or without augmentation). Of the 10 cases with a fragment index of <100 mm2, 1 case that was fixed with a suture anchor alone was not successful. Despite the small fragment sizes, all 5 cases with additional CCS were successful. The remaining 4 cases achieved bone union with the suture anchor alone.
Fig. 5.
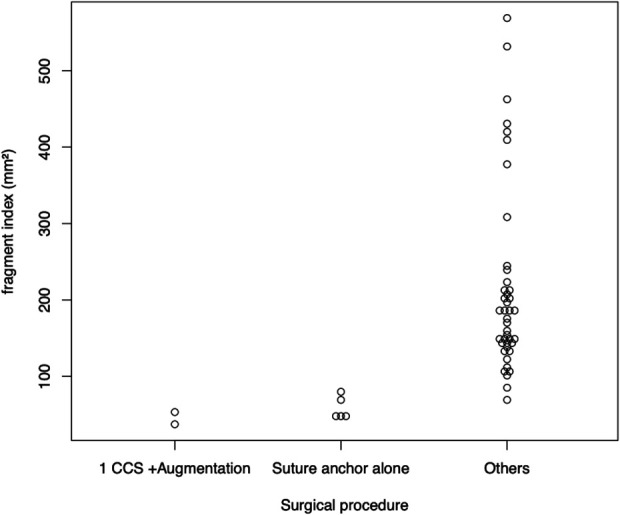
The distribution of the fragment index by surgical procedures. CCS = cannulated cancellous screw.
Discussion
In our multicenter retrospective study of CAvF, we demonstrated that most patients were older women, and the major treatment method was 2 cannulated cancellous screws with or without augmentation in surgical cases. The results showed that postoperative complications resulting in reoperation were still likely to occur, especially in cases with a large degree of initial displacement, current smoking, and CCS without augmentation.
The causes of postoperative complications are multifactorial, including osteoporosis, pressure on the skin by bone fragments, traction of bone fragments by the gastrocnemius-soleus complex, and poor fixation strength6,9-12,19,26. Carnero-Martín de Soto et al. reported that, in CAvFs with ≥20 mm of displacement, there was a 90% probability of complications, especially soft-tissue complications26. In the current study, the mean initial displacement of the fragment in patients with reoperation was 23 mm, which supports the findings reported by Carnero-Martín de Soto et al. Among the patients who underwent reoperation, there were 3 cases of infection and/or necrosis without loss of reduction. The initial displacement of the fragment was 22 to 28 mm, and the waiting time until initial operation was 3 to 15 days. Early intervention was desirable because one of the causes was thought to be persistent pressure on the skin by bone fragments2. In order to minimize the incidence of postoperative complications, it is necessary to pay attention to factors related to surgical interventions, such as early and minimally invasive surgery, assurance of the fixation strength, and prolonged immobilization in the equinus position4,8-12,19,20,22,26.
Overall, CCS fixation was performed in 80% of the surgically treated cases. We believe that CCS fixation is one of the most effective procedures for this type of fracture, associated with the minimization of soft-tissue problems because the CCS can be inserted easily and through a small incision8,20. Meanwhile, suture anchors were used in some cases when the bone fragments were small, because the bone fragments had to be of a certain size in order to insert a CCS; otherwise, it would cause the division of the bone fragment. When the bone fragment is small, using a suture anchor or tension-band wiring may be considered, although an additional skin incision would be necessary, and the fixation strength may be insufficient1,4,11,12. In the present study, the fragment index was used; a bone fragment index of <100 mm2 was considered to indicate a small fragment, and 1 case involving a fragment index of 80 mm2, which was fixed with an anchor alone, was unsuccessful. Since CCS fixation was successful in cases with a fragment index of <100 mm2, CCS fixation might still be the superior fixation technique and should be selected in combination with augmentation whenever possible, even in cases involving small bone fragments. In 2 cases, Steinmann pin fixation was performed alone or in combination with CCS fixation. In both cases, we found that Steinmann pin fixation was inadequate and therefore not indicated for CAvFs.
Augmentation is often used in combination with the treatment of CAvF4,7,9,11,12,21. In a biomechanical study investigating augmentation, Khazen et al. reported that CCS + suture anchor fixation significantly increased fixation strength compared with CCS alone, while Doany et al. and Mitchell et al. were unable to demonstrate a significant difference in the use of augmentation with CCS10,11,21. In the present study, the reoperation rate for CCS fixation alone was 35%. For CCS + augmentation, excluding the combination with a Steinmann pin, it was 5.3%, with the augmentation technique clearly contributing to improved results. CCS alone may cause the bone fragment to crack and lead to failure. Since there was no difference in the results among the different types of augmentation (although the study population was relatively small), a washer may be selected as the first choice because it involves small additional incisions12. In this study, 2 cannulated cancellous screws were inserted in 92.9% of the cases treated with CCS fixation, and, similar to the opinion of Doany et al.11, it is preferable to use multiple cannulated cancellous screws in cases in which the bone fragments are large enough4,10-12,20,22. A 1:2 screw-to-bone ratio was recommended for prevention of fragmentation of the fracture in a biomechanical study by Jordan et al.22. The present results suggest that 2 cannulated cancellous screws should be inserted if possible.
The study had several limitations, including the lack of a large number of cases and its retrospective nature. No formal statistical power analysis was performed in this study; power analysis is difficult for a condition with such a low incidence as CAvF. The results should be interpreted with caution, recognizing that there may not have been sufficient power to detect subtle differences or associations. Another limitation is that the small sample size did not allow statistical comparison of the various surgical techniques. Furthermore, we did not perform a 3-dimensional evaluation of the bone width and bone fragment cracking by computed tomography (CT). Certain treatments to reduce traction forces by the gastrocnemius-soleus complex, such as the Strayer procedure or botulinum toxin injection, were not considered. Although many patients with CAvFs have gastrocnemius tightness, which can be an inhibitor of repair, and such procedures are said to be effective, there is no certain opinion regarding the indications4,10. It has been shown that Ilizarov external fixation is useful for CAvF27,28. Another report demonstrated the usefulness of percutaneous fixation20. By using these other methods, it may be possible to reduce the complication rate. Macaulay et al. reported that AOFAS scores may reflect investigator bias in scoring the subjective sections. This highlights the high potential for bias29. Despite its widespread use, the lack of validation of the AOFAS score indicates that there may be a need for more accurate outcome measures, especially those that are patient-reported30. The Fracture Mobility Score has been shown to correlate well with the New Mobility Score in hip fractures14 but has not yet been validated for other fractures. The present study included some patients with a short follow-up period, although the inclusion of these patients did not seem to have a substantial impact on the primary end points of infection, necrosis, loss of reduction, and reoperation.
Conclusions
CAvFs occurred more frequently in older women and had a high rate of postoperative complications. To reduce postoperative complications, a combination of CCS with augmentation is more effective than CCS fixation alone, even when the bone fragment size is small.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A645).
Acknowledgments
Note: The authors thank the members of the research group (shown in alphabetical order of affiliation): Dr. Takeshi Oguchi (Anjo Kosei Hospital), Dr. Keigo Ito (Chubu Rosai Hospital), Dr. Masahiro Hanabayashi (Ichinomiya Municipal Hospital), Dr. Hiroaki Yoshida (Kamiiida Daiichi General Hospital), Dr. Hidenori Inoue (Japanese Red Cross Aichi Medical Center Nagoya Daiichi Hospital), Dr. Toshihiro Ando (Japanese Red Cross Aichi Medical Center Nagoya Daini Hospital), Dr. Koji Maruyama (Nakatsugawa Municipal General Hospital), Dr. Kenichi Yamauchi (Toyohashi Municipal Hospital); Dr. Yasuhide Kanayama (Toyota Kosei Hospital), Dr. Tadahiro Sakai (Toyota Memorial Hospital), and Dr. Nobuhiro Okui (Yokkaichi Municipal Hospital).
Footnotes
Investigation performed at Nagoya University, Nagoya, Japan
Disclosure: No external funding was received for this study. The Article Processing Charge for open access publication was funded by the authors. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A643).
Contributor Information
Yu Takahashi, Email: yuu.takahashi406@gmail.com.
Katsuhiro Tokutake, Email: k.tokutake@med.nagoya-u.ac.jp.
Yuta Asami, Email: yuta0862@yahoo.co.jp.
Hidetane Takahashi, Email: d12sm062@gmail.com.
Mihoko Kato, Email: mihoko.k0107@gmail.com.
Tokumi Kanemura, Email: spinesho@vmail.plala.or.jp.
Shiro Imagama, Email: imagama@med.nagoya-u.ac.jp.
References
- 1.Beavis RC, Rourke K, Court-Brown C. Avulsion fracture of the calcaneal tuberosity: a case report and literature review. Foot Ankle Int. 2008. Aug;29(8):863-6. [DOI] [PubMed] [Google Scholar]
- 2.Hess M, Booth B, Laughlin RT. Calcaneal avulsion fractures: complications from delayed treatment. Am J Emerg Med. 2008. Feb;26(2):254.e1-4. [DOI] [PubMed] [Google Scholar]
- 3.Banerjee R, Chao J, Sadeghi C, Taylor R, Nickisch F. Fractures of the calcaneal tuberosity treated with suture fixation through bone tunnels. J Orthop Trauma. 2011. Nov;25(11):685-90. [DOI] [PubMed] [Google Scholar]
- 4.Banerjee R, Chao JC, Taylor R, Siddiqui A. Management of calcaneal tuberosity fractures. J Am Acad Orthop Surg. 2012. Apr;20(4):253-8. [DOI] [PubMed] [Google Scholar]
- 5.Lee SM, Huh SW, Chung JW, Kim DW, Kim YJ, Rhee SK. Avulsion fracture of the calcaneal tuberosity: classification and its characteristics. Clin Orthop Surg. 2012. Jun;4(2):134-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gitajn IL, Abousayed M, Toussaint RJ, Vrahas M, Kwon JY. Calcaneal avulsion fractures: a case series of 33 patients describing prognostic factors and outcomes. Foot Ankle Spec. 2015. Feb;8(1):10-7. [DOI] [PubMed] [Google Scholar]
- 7.Yoshida K, Kasama K, Akahane T. Avulsion Fracture of the Calcaneus Treated With a Soft Anchor Bridge and Lag Screw Technique: A Report of Two Cases. J Foot Ankle Surg. 2016. Mar-Apr;55(2):310-3. [DOI] [PubMed] [Google Scholar]
- 8.Lui TH. Avulsion fracture of the posterosuperior tuberosity of the calcaneus managed with lag screw fixation. Foot Ankle Surg. 2018. Feb;24(1):45-8. [DOI] [PubMed] [Google Scholar]
- 9.Rauer T, Twerenbold R, Flückiger R, Neuhaus V. Avulsion Fracture of the Calcaneal Tuberosity: Case Report and Literature Review. J Foot Ankle Surg. 2018. Jan-Feb;57(1):191-5. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell PM, OʼNeill DE, Branch E, Mir HR, Sanders RW, Collinge CA. Calcaneal Avulsion Fractures: A Multicenter Analysis of Soft-Tissue Compromise and Early Fixation Failure. J Orthop Trauma. 2019. Nov;33(11):e422-6. [DOI] [PubMed] [Google Scholar]
- 11.Doany M, Garcia A, Komatsu D, Divaris N, Kottmeier S, Paulus M. Avulsion Fractures of the Calcaneal Tuberosity: A Single-Center Review of Outcomes and Complications. J Am Acad Orthop Surg Glob Res Rev. 2021. Dec 2;5(12). [DOI] [PubMed] [Google Scholar]
- 12.Hong CC, Lim JXY, Tan JH, Pearce CJ. Outcomes of operatively treated calcaneal tuberosity avulsion fractures. Injury. 2022. Mar;53(3):1276-82. [DOI] [PubMed] [Google Scholar]
- 13.Yu SM, Yu JS. Calcaneal Avulsion Fractures: An Often Forgotten Diagnosis. AJR Am J Roentgenol. 2015. Nov;205(5):1061-7. [DOI] [PubMed] [Google Scholar]
- 14.Voeten SC, Nijmeijer WS, Vermeer M, Schipper IB, Hegeman JH; DHFA Taskforce study group. Validation of the Fracture Mobility Score against the Parker Mobility Score in hip fracture patients. Injury. 2020. Feb;51(2):395-9. [DOI] [PubMed] [Google Scholar]
- 15.Ibrahim DA, Swenson A, Sassoon A, Fernando ND. Classifications In Brief: The Tscherne Classification of Soft Tissue Injury. Clin Orthop Relat Res. 2017. Feb;475(2):560-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sugimoto T, Tokutake K, Takegami Y, Okui N, Kanayama Y, Inoue H, Sugimoto R, Kagami Y, Imagama S. Plate fixation through the lateral extensile approach versus cannulated screw fixation through the sinus tarsi approach for calcaneal fracture: a multicenter, propensity score-matched TRON study. Eur J Orthop Surg Traumatol. 2022. Oct;32(7):1333-40. [DOI] [PubMed] [Google Scholar]
- 17.Keast DH, Bowering CK, Evans AW, Mackean GL, Burrows C, D’Souza L. MEASURE: A proposed assessment framework for developing best practice recommendations for wound assessment. Wound Repair Regen. 2004. May-Jun;12(3):S1-17. [DOI] [PubMed] [Google Scholar]
- 18.Harnroongroj T, Tangmanasakul A, Choursamran N, Sudjai N, Harnroongroj T. Measurement technique of calcaneal varus from axial view radiograph. Indian J Orthop. 2015. Mar-Apr;49(2):223-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gardner MJ, Nork SE, Barei DP, Kramer PA, Sangeorzan BJ, Benirschke SK. Secondary soft tissue compromise in tongue-type calcaneus fractures. J Orthop Trauma. 2008. Aug;22(7):439-45. [DOI] [PubMed] [Google Scholar]
- 20.Blum LE, Hundal R, Walton D, Hake ME. Percutaneous Fixation of Calcaneal Tuberosity Avulsion Fracture. J Orthop Trauma. 2019. Aug;33(Suppl 1):S44-5. [DOI] [PubMed] [Google Scholar]
- 21.Khazen GE, Wilson AN, Ashfaq S, Parks BG, Schon LC. Fixation of calcaneal avulsion fractures using screws with and without suture anchors: a biomechanical investigation. Foot Ankle Int. 2007. Nov;28(11):1183-6. [DOI] [PubMed] [Google Scholar]
- 22.Jordan MC, Hufnagel L, McDonogh M, Paul MM, Schmalzl J, Kupczyk E, Jansen H, Heilig P, Meffert RH, Hoelscher-Doht S. Surgical Fixation of Calcaneal Beak Fractures-Biomechanical Analysis of Different Osteosynthesis Techniques. Front Bioeng Biotechnol. 2022. Aug 4;10:896790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robb CA, Davies MB. A new technique for fixation of calcaneal tuberosity avulsion fractures. Foot Ankle Surg. 2003;9(4):221-4. [Google Scholar]
- 24.Squires B, Allen PE, Livingstone J, Atkins RM. Fractures of the tuberosity of the calcaneus. J Bone Joint Surg Br. 2001. Jan;83(1):55-61. [DOI] [PubMed] [Google Scholar]
- 25.Ibrahim T, Beiri A, Azzabi M, Best AJ, Taylor GJ, Menon DK. Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surg. 2007. Mar-Apr;46(2):65-74. [DOI] [PubMed] [Google Scholar]
- 26.Carnero-Martín de Soto P, Bautista-Enrique D, Gómez-Cáceres A, Rodríguez-León A, Bravo-Zurita MJ, Santos-Maraver MT. Avulsion Fractures of Posterior Calcaneal Tuberosity: Identification of Prognostic Factors and Classification. J Foot Ankle Surg. 2019. May;58(3):423-6. [DOI] [PubMed] [Google Scholar]
- 27.Takahashi M, Noda M, Saegusa Y. A new treatment for avulsion fracture of the calcaneus using an Ilizarov external fixator. Injury. 2013. Nov;44(11):1640-3. [DOI] [PubMed] [Google Scholar]
- 28.Ramanujam CL, Capobianco CM, Zgonis T. Ilizarov external fixation technique for repair of a calcaneal avulsion fracture and Achilles tendon rupture. Foot Ankle Spec. 2009. Dec;2(6):306-8. [DOI] [PubMed] [Google Scholar]
- 29.Macaulay A, Nandyala SV, Miller CP, Ghorbanhoseini M, Walley KC, Kwon JY. Potential for Bias and the American Orthopaedic Foot and Ankle Society Ankle-Hindfoot Scoring System. Foot Ankle Spec. 2018. Oct;11(5):416-9. [DOI] [PubMed] [Google Scholar]
- 30.Nguyen MQ, Dalen I, Iversen MM, Harboe K, Paulsen A. Ankle fractures: a systematic review of patient-reported outcome measures and their measurement properties. Qual Life Res. 2023. Jan;32(1):27-45. [DOI] [PMC free article] [PubMed] [Google Scholar]




