Abstract
Background:
Surgical training traditionally took place at academic centres, but changed to incorporate community and rural hospitals. As little data exist comparing resident case volumes between these locations, the objective of this study was to determine variations in these volumes for routine general surgery procedures.
Methods:
We analyzed senior resident case logs from 2009 to 2019 from a general surgery residency program. We classified training centres as academic, community, and rural. Cases included appendectomy, cholecystectomy, hernia repair, bowel resection, adhesiolysis, and stoma formation or reversal. We matched procedures to blocks based on date of case and compared groups using a Poisson mixed-methods model and 95% confidence intervals (CIs).
Results:
We included 85 residents and 28 532 cases. Postgraduate year (PGY) 3 residents at academic sites performed 10.9 (95% CI 10.1–11.6) cases per block, which was fewer than 14.7 (95% CI 13.6–15.9) at community and 15.3 (95% CI 14.2–16.5) at rural sites. Fourth-year residents (PGY4) showed a greater difference, with academic residents performing 8.7 (95% CI 8.0–9.3) cases per block compared with 23.7 (95% CI 22.1–25.4) in the community and 25.6 (95% CI 23.6–27.9) at rural sites. This difference continued in PGY5, with academic residents performing 8.3 (95% CI 7.3–9.3) cases per block, compared with 18.9 (95% CI 16.8–21.0) in the community and 14.5 (95% CI 7.0–21.9) at rural sites.
Conclusion:
Senior residents performed fewer routine cases at academic sites than in community and rural centres. Programs can use these data to optimize scheduling for struggling residents who require exposure to routine cases, and help residents complete the requirements of a Competence by Design curriculum.
Abstract
Contexte:
On a de tout temps donné la formation en chirurgie dans des établissements universitaires, mais désormais, les centres ruraux et communautaires sont également mis à contribution. Étant donné qu’on dispose de peu de données comparatives sur le volume de cas pris en charge par les résidentes et les résidents entre les différents types d’établissements, nous avons mené cette étude afin d’observer les différences quant aux volumes des interventions en chirurgie générale.
Méthodes:
Nous avons analysé les registres de cas pris en charge par les résidentes et résidents séniors d’un programme de résidence en chirurgie générale de 2009 à 2019. Nous avons classé les centres de formation selon qu’il s’agissait d’établissements universitaires, communautaires, ou ruraux. Les cas incluaient appendicectomie, cholécystectomie, cure de hernie, résection intestinale, adhésiolyse, et création ou fermeture de stomie. Nous avons assorti les interventions par blocs en fonction des dates et comparé les blocs à l’aide d’un modèle de Poisson mixte et d’intervalles de confiance (IC) de 95 %.
Résultats:
Nous avons inclus 85 résidentes et résidents et 28 532 cas. Les résidentes et résidents de 3e année des centres universitaires ont effectué 10,9 (IC de 95 % 10,1–11,6) cas par bloc, ce qui s’est révélé inférieur à 14,7 (IC de 95 % 13,6–15,9) dans les établissements communautaires et à 15,3 (IC de 95 % 14,2–16,5) dans les établissements ruraux. Les résidentes et résidents de 4e année se sont nettement démarqués : ceux des établissements universitaires ont réalisé 8,7 (IC de 95 % 8,0–9,3) cas par bloc, contre 23,7 (IC de 95 % 22,1–25,4) dans les établissements communautaires et 25,6 (IC de 95 % 23,6–27,9) dans les établissements ruraux. La différence s’est maintenue chez les résidentes et résidents de 5e année : ceux des établissements universitaires ont réalisé 8,3 (IC de 95 % 7,3–9,3) cas par bloc, contre 18,9 (IC de 95 % 16,8–21,0) dans les établissements communautaires et 14,5 (IC de 95 % 7,0–21,9) dans les établissements ruraux.
Conclusion:
Les résidentes et résidents séniors ont pris en charge un moins grand nombre de cas de routine dans les établissements universitaires que dans les établissements communautaires et ruraux. Les programmes pourraient utiliser ces données pour améliorer la formation des résidentes et résidents qui doivent être exposés à des cas de routine en chirurgie générale et les aider à obtenir les acquis nécessaires pour tout programme de Compétence par conception.
General surgery training has long followed a template in which residents spend most of their time at large academic centres in order to experience a wide breadth of surgical cases and provide the necessary clinical service for quaternary surgical services to run effectively.1 Over time, community and rural resident training sites have become part of training paradigms to provide residents with real-world experience and can provide a fresh environment for training. These sites are high volume in common, routine general surgery procedures that all general surgeons are required to perform, but perhaps lack in overall complexity.2 Additionally, these experiences often do not have the same service requirements, which would allow for a more focused, technical educational experience.
In Canada, general surgery residency training programs tend to be varied with regard to the location of training and the case mix. At the University of British Columbia (UBC), the residency program has evolved and is integrated within the province to create a distributed training model. Residents now spend large portions of their time as senior trainees away from academic centres. As the UBC training program is the only one in the province, and given the very large geographic area it covers, trainees have opportunities to visit many different locations, including those in urban community sites and in rural areas.
Comparison of general surgery resident case volumes in academic versus community versus rural sites is lacking in the medical education literature. Some evidence exists that community programs have high operative volumes with ample time for junior residents to operate.3 The relatively unique structure of the UBC training program provides an opportunity to investigate whether there is a difference in case volume for residents among these 3 types of sites. Although complex procedures performed at academic centres are important for resident education, routine procedures — such as hernia repairs, cholecystectomies, and bowel resections — are expected to be performed by any general surgeon and are fundamental to master before completion of training. These are also very appropriate cases for senior residents. If there are differences between various training sites, general surgery training programs could use these findings to tailor education to resident and population needs and goals.
Methods
We carried out a retrospective review of resident case logs through the T-Res logging system used at UBC for cases performed by residents from July 1, 2009, to June 30, 2019. We included cases deemed to be routine procedures (Box 1). We derived these from the provincial privileging dictionary based on procedures that any surgeon in the province should be proficient in, that fit into a category in our logging system, and that are routinely performed by senior residents. We included both minimally invasive surgery and open cases. We included cases for senior residents only, defined as residents in postgraduate year (PGY) 3 to 5, who were listed as the primary operator. We excluded junior residents as they do not rotate away from academic centres. We excluded residents who logged fewer than 100 cases in a year and excluded cases with data-logging errors. Finally, we also excluded out-of-province elective cases. We based site classification of academic, urban community, and rural according to long-standing designations by the local health authorities and the residency program (Appendix 1, Fig. A.1, available at www.canjsurg.ca/lookup/doi/10.1503/cjs.005323/tab-related-content). Although no rigid criteria were in place for these designations, academic sites were generally quaternary centres with a substantial number of research faculty, and ready access to ancillary services such as complex critical care and interventional radiology. Community sites were usually tertiary hospitals with access to most ancillary services and minimal research faculty. Rural sites usually comprised primary and secondary hospitals with basic operative capabilities, but lacked many ancillary services. Resident rotations followed a standard rotation matrix, although mild variations in this were possible at the request of residents based on career objectives (Appendix 1, Fig. A.2).
Box 1.
Routine general surgery procedures
Appendectomy
Bowel resection*
Cholecystectomy
Hernia repair†
Lysis of adhesions
Stoma creation or reversal
Small and large bowel resections including rectal procedures such as abdominoperineal resection and low anterior resection.
Included several categories, such as inguinal, incisional, umbilical, and epigastric.
The primary outcome for this study examines case volume per PGY per site per block. Given the variations in how long residents spend at certain sites, standardizing cases per block allows direct comparisons between resident volumes and will increase the applicability of the results.
We calculated summary statistics and used a mixed-effect Poisson regression model to estimate the mean number of procedures performed by PGY and practice setting. The mixed-effect Poisson regression model included resident ID as a random effect and both PGY and practice setting as interacting fixed effects. We estimated mean rate of procedures per block and associated 95% confidence intervals (CIs) for each combination of PGY and practice setting. We considered estimates with nonoverlapping 95% CIs to be statistically significant. Academic years 2009–2011 had 12 blocks per year instead of 13 in 2011 onward, so we repeated modelling for sensitivity analysis using procedures standardized to 13 blocks instead of 12. For these sensitivity analyses, we multiplied number of procedures in each block in academic years 2009–2011 by a factor of 12 or 13 and rounded them down to the nearest integer. We performed all statistical tests and modelling using R version 4.2.2. This study was approved by the UBC Research Ethics Board.
Results
Demographic information is summarized in Table 1. During the study period, 85 unique general surgery residents had appropriate case logs. Of these, 73 had records during PGY3, 74 during PGY4, and 62 during PGY5. In total, 27 unique training sites were involved in training, comprising 5 academic centres, 13 community centres, and 9 rural centres. Residents logged 48 772 cases overall. Of these, 18 503 (37.9%) cases were performed at academic centres, 22 492 (46.1%) in community centres, and 7777 (16.0%) in rural centres. Out of these cases, 28 532 were routine general surgery cases (58.5% of total cases). Residents performed 9744 cases (34.1%) in academic centres, 14 001 (49.1%) in community centres, and 4787 (16.7%) in rural centres.
Table 1.
Cohort characteristics
| Characteristic | n |
|---|---|
| No. of residents | 85 |
| PGY3 | 73 |
| PGY4 | 74 |
| PGY5 | 62 |
| Total no. of cases | 28532 |
| Academic | 9744 |
| Urban community | 14001 |
| Rural | 4787 |
| Total no. of training sites | 27 |
| Academic | 5 |
| Urban community | 13 |
| Rural | 9 |
PGY = postgraduate year.
The average number of blocks spent during the calendar year in academic sites was 5.53 for PGY3, 4.16 in PGY4, and 4.98 during PGY5. For community sites, 3.02 blocks were spent in PGY3, 4.41 in PGY4, and 4.62 in PGY5. Finally, for rural sites, 3.30 blocks were spent in PGY3, 2.91 in PGY4, and 1.86 in PGY5.
With respect to overall case volumes per year and site (Table 2), PGY3 case volumes at academic versus community versus rural sites show no statistical difference, with 63.7 (54.3–73.2), 52.5 (40.9–64.1), and 52.4 (43.6–61.1) cases per year, respectively. There is a statistically significant difference in PGY4 at academic versus community and rural sites, with 38.6 (31.2–46.3) compared with 107.4 (89.3–125.3) and 76.1 (53.4–98.7) cases per year. The numbers in PGY5 are again significant, with academic and rural sites having 44.8 (36.9–52.7) and 30.0 (5.2–54.8) cases per year, respectively, compared with community sites, which had 89.4 (70.8–108.1) cases per year.
Table 2.
Cases per postgraduate year per site overall
| PGY | No. of cases per year, mean (95% CI) | ||
|---|---|---|---|
| Academic | Community | Rural | |
| PGY3 | 63.7 (54.3–73.2) | 52.5 (40.9–64.1) | 52.4 (43.6–61.1) |
| PGY4 | 38.6 (31.2–46.3) | 107.4 (89.3–125.3) | 76.1 (53.4–98.7) |
| PGY5 | 44.8 (36.9–52.7) | 89.4 (70.8–108.1) | 30.0 (5.2–54.8) |
CI = confidence interval; PGY = postgraduate year.
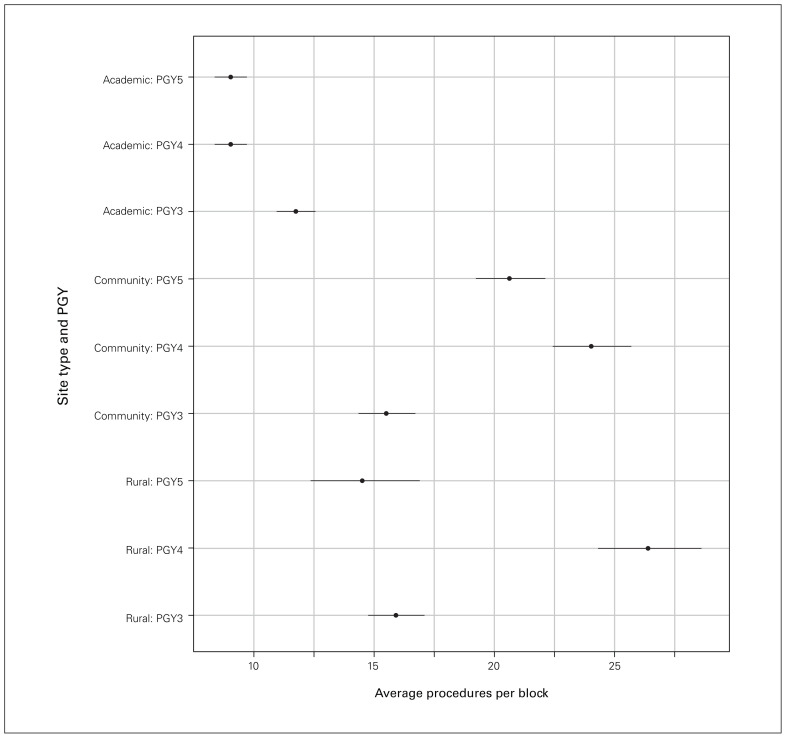
For cases per year per block per site (Table 3), community PGY3 residents performed more routine cases than those at academic sites, with 14.8 (13.7–16.0) versus 10.8 (10.0–11.6) cases per block. We saw the same trend when comparing rural and academic sites, with 15.3 (14.2–16.5) versus 10.8 (10.0–11.6) cases per block. In the PGY4 year, community residents performed more cases than those at academic sites, with 23.8 (22.2–25.5) versus 8.7 (8.0–9.3) cases per block. Again we noted this trend in a comparison of rural and academic sites, with 25.7 (23.6–27.9) versus 8.7 (8.0–9.3) cases per block. Finally, with respect to the PGY5 year, community residents again performed more cases than those at academic sites, with 20.1 (18.7–21.6) versus 8.7 (8.0–9.3) cases per block. We saw the same trend when comparing rural and academic sites with 15.1 (12.9–17.7) versus 8.7 (8.0–9.3) cases per block. Of note, case volumes per block between community and rural centres each year did not show any statistically significant difference. Overall relationships between sites and years are summarized in Figure 1.
Table 3.
Comparison of case volumes per postgraduate year per site per block
| PGY | Training site | Site 1, mean (95% CI) | Site 2, mean (95% CI) |
|---|---|---|---|
| PGY3 | Community v. academic | 14.7 (13.6–15.9) | 10.9 (10.1–11.6) |
| Rural v. academic | 15.3 (14.2–16.5) | 10.9 (10.1–11.6) | |
| Rural v. community | 15.3 (14.2–16.5) | 14.7 (13.6–15.9) | |
| PGY4 | Community v. academic | 23.7 (22.1–25.4) | 8.7 (8.0–9.3) |
| Rural v. academic | 25.6 (23.6–27.9) | 8.7 (8.0–9.3) | |
| Rural v. community | 25.6 (23.6–27.9) | 23.7 (22.1–25.4) | |
| PGY5 | Community v. academic | 18.9 (16.8–21.0) | 8.3 (7.3–9.3) |
| Rural v. academic | 14.5 (7.0–21.9) | 8.3 (7.3–9.3) | |
| Rural v. community | 14.5 (7.0–21.9) | 18.9 (16.8–21.0) |
CI = confidence interval; PGY = postgraduate year.
Fig. 1.
Forest plot of relationships between case volumes at different sites per year. PGY = postgraduate year.
Discussion
General surgery training requires residents to be exposed to and competent in several different procedures. Case volumes are an important factor in documenting and achieving proficiency.4 To our knowledge, this study is the first to compare 3 different types of resident training sites in a single program to see whether there are differences in case volumes for routine procedures.
Results from this study show that in training, differences exist in overall routine case volumes per training site that are significant in PGY4 and PGY5. There is no statistically significant difference for residents in PGY3. We also looked at routine case volume per block per site and found that residents were performing about 1.5–3 times the number of routine cases at nonacademic than academic sites, depending on the year. When we compared the community and rural volumes, however, these results showed there was no difference in case volumes. That said, it is important to note that the PGY5 rural case volumes are extremely low, which may limit results. This is likely a result of time off for exam preparation and required rotations at academic centres within the PGY5 year. Only residents who are interested in rural practice tend to request these rotations at this point in their training.
We did not see a significant difference in overall case volumes for PGY3 residents. Residents in the UBC program rarely have subspeciality rotations at academic centres in their third year, meaning their highest exposure to routine procedures at this site should occur during this time and offers the best direct comparison between groups. However, per block, PGY3 residents had about 1.5 times the number of cases away from academia. Although in 1 month this difference may not be clinically important (11 v. 15 cases), these numbers can add up, as residents are usually assigned to a rotation for several blocks. Further, in the third year of training, resident operative skill acquisition is exponential, and even small case volumes have a meaningful impact as this is when residents begin to perform operations more routinely. This effect is significantly compounded in PGY4, for example, where residents perform almost 3 times the number of cases away from academia.
These results of academic versus nonacademic case volumes for routine procedures are similar to those in the literature, although the nonacademic sites are generally classified as “rural” in other studies.5–7 For example, a study from rural Tennessee reported residents performing about 35 cases per block, and all cases were essentially routine procedures.5 Another study from North Carolina reported about 10 cases per block for these cases when residents were at academic centres; however, they cited about 12 routine cases in rural sites, which differs from our results.8 The reason for this difference is not clear, but may reflect new training sites or local patient volumes.
These differences seen in our study’s volumes are also interesting, given that the total number of cases performed at each site excludes endoscopy, which in many programs, including the UBC program, is focused away from the academic centres.2 Endoscopy is a big component of practice for general surgeons away from academic centres and is an essential skill for general surgery overall.9 Hao and colleagues logged 68% of their cases during rural rotations as endoscopy.8 In the UBC program, the curriculum has a dedicated scoping rotation, usually at a community site, while nonacademic general surgery rotations are focused on operative exposure. Some endoscopy is still performed, but volume varies substantially between sites. If endoscopy had been included for this study, it is likely that the nonacademic case numbers would have been much higher.
Time and workload may be factors that contribute to decreased number of cases at academic sites. Senior residents at academic sites work concurrently with fellows and junior residents, who will take some of the case volume. Additionally, if more cases are performed by junior residents or some tasks are completed by medical students, this can increase the overall time for cases, leading to less opportunity for the senior resident to complete cases in a given day.10 Community and rural sites in this program have only a single resident working with the attending surgeons, and in many cases, attendings or experienced surgical assists may act as the assistant. Next, the case composition at academic centres is influenced by subspeciality services that perform nonroutine cases, which may not be applicable for this study because they are not appropriate for a senior resident to be the primary surgeon. Finally, cases at academic sites can also be more complex from both a technical standpoint (abdominal wall reconstruction v. small incisional hernia repair) and a patient standpoint, requiring more anesthesia support. From the technical standpoint, this leads to increased surgical time, as well as additional time for lines or neuraxial blocks, which will contribute to less overall daily volume. However, one must consider the complex interplay between volume, education, and complexity. Interestingly, the literature has not examined case complexity so far, and the topic is not classified in this study, but its effect is important in the development of expertise within residency and backed by educational theories.11,12 Cases with less complexity allow residents to learn the basics and limit cognitive overload, which is the goal in the PGY3 year. A high volume of simple cases can help with this. As a resident progresses, however, complexity should be sought, to improve educational value.
Given these findings, there is some evidence that residents are performing more routine cases as the primary operator away from academic training sites. This has implications for resident placement for rotations. For example, if a resident is struggling with skill development, an individualized educational plan might be required outside of the standard rotation matrix. Programs may consider sending this resident to a higher-volume site to improve and gain more exposure to routine cases before returning. This has further impact in the era of competency-based medical education, as program directors should have a keen sense of where to send residents, depending where they are in their clinical development.13 Our study may also be useful for the scheduling of an average resident. Although complex cases should be the focus of senior years, repeated exposure to routine cases is also essential, to maintain proficiency and develop mastery.14 Given the discrepancy of routine cases between sites, it may be beneficial for programs to spread out nonacademic rotations to avoid the concept of blocked practice and instead promote distributed practice, which is better for long-term skill retention and potentially more reflective of general surgery practice.15
Finally, these data provide a quality-control metric for this program to help decide whether improvements to operative volume are required, and provide a platform for other programs with multiple training sites to consider evaluation of their operative volumes to optimize learning.
Although this study was carried out in a Canadian program, its results could be used broadly. Many programs now follow a structure of academic hubs, with associated training locations in smaller centres. As long as training streams are not strictly academic versus nonacademic, case mixes should be similar, and the volumes seen here should be replicable, especially because we controlled for the number of blocks.
Limitations
Limitations of the study include its retrospective nature and the fact that all cases are self-logged by residents, which may not always be accurate.16,17 That said, self-logging is a required component for promotion during training, and therefore residents are generally careful in logging practices. Additionally, case classification is limited by the general description of cases. For example, the T-Res system lists a case category for ventral hernia repair, but this may be a simple hernia repair or a component separation, which is not a routine procedure in this study. Finally, definitions for community and rural general surgery centres are not clearly defined within this program or in the literature, and the studies that exist in this area are focused on rural surgical programs.
Conclusion
The results of this study show that residents perform routine general surgery procedures in higher numbers away from academic sites during senior residency. Future work in this area will look to understand overall case volumes of residents in terms of composition, location, and timing, to see how resident training can be further optimized. There is also opportunity for qualitative work to understand residents’ experiences at academic sites versus nonacademic sites for these routine cases and whether that may contribute to the differences seen here. Finally, studies should look at whether the difference in case volume truly affects the operative ability of residents or the quality of education.
Footnotes
This work was presented at the Canadian Surgery Forum, Sept. 15–17, 2022, Toronto, Ont.
Competing interests: None declared.
Contributors: Subin Punnen and Ahmer Karimuddin designed the study. All authors acquired the data, which Shayda Taheri, Leo Chen, and Tracy Scott analyzed. Subin Punnen and Ahmer Karimuddin wrote the manuscript, which Shayda Taheri, Leo Chen, and Tracy Scott revised critically for important intellectual content. All authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
References
- 1.Kerr B, O’Leary JP. The training of the surgeon: Dr. Halsted’s greatest legacy. Am Surg 1999;65:1101–2. [PubMed] [Google Scholar]
- 2.Milligan JL, Nelson HS, Mancini ML, et al. Rural surgery rotation during surgical residency. Am Surg 2009;75:743–5. [PubMed] [Google Scholar]
- 3.Vaughan A, Welling R, Boberg J. Surgical education in the new millennium: a community hospital perspective. Surg Clin North Am 2004;84:1441–51. [DOI] [PubMed] [Google Scholar]
- 4.Mattar SG, Alseidi AA, Jones DB, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg 2013;258:440–9. [DOI] [PubMed] [Google Scholar]
- 5.Giles WH, Arnold JD, Layman TS, et al. Education of the rural surgeon: experience from Tennessee. Surg Clin North Am 2009;89:1313–9. [DOI] [PubMed] [Google Scholar]
- 6.Moesinger R, Hill B. Establishing a Rural surgery training program: a large community hospital, expert subspecialty faculty, specific goals and objectives in each subspecialty, and an academic environment lay a foundation. J Surg Educ 2009; 66:106–12. [DOI] [PubMed] [Google Scholar]
- 7.Deveney K, Hunter J. Education for rural surgical practice: the Oregon Health & Science University model. Surg Clin North Am 2009;89:1303–8. [DOI] [PubMed] [Google Scholar]
- 8.Hao S, Johnson HM, Celio A, et al. Rural general surgery experience as a valuable adjunct to an academic based general surgery residency. J Surg Educ 2020;77:598–605. [DOI] [PubMed] [Google Scholar]
- 9.Sticca RP, Mullin BC, Harris JD, et al. Surgical specialty procedures in rural surgery practices: implications for rural surgery training. Am J Surg 2012;204:1007–12, discussion 12–3. [DOI] [PubMed] [Google Scholar]
- 10.Kauvar DS, Braswell A, Brown BD, et al. Influence of resident and attending surgeon seniority on operative performance in laparoscopic cholecystectomy. J Surg Res 2006;132:159–63. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt HG, Rikers RM. How expertise develops in medicine: knowledge encapsulation and illness script formation. Med Educ 2007;41:1133–9. [DOI] [PubMed] [Google Scholar]
- 12.Dreyfus SE. The five-stage model of adult skill acquisition. Bull Sci Technol Soc 2004;24:177–81. [Google Scholar]
- 13.Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach 2010;32:638–45. [DOI] [PubMed] [Google Scholar]
- 14.Ericsson KA, Harwell KW. Deliberate practice and proposed limits on the effects of practice on the acquisition of expert performance: why the original definition matters and recommendations for future research. Front Psychol 2019;10:2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moulton CA, Dubrowski A, Macrae H, et al. Teaching surgical skills: what kind of practice makes perfect?: A randomized, controlled trial. Ann Surg 2006;244:400–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collins C, Dudas L, Johnson M, et al. ACGME Operative case log accuracy varies among surgical programs. J Surg Educ 2020; 77:e78–85. [DOI] [PubMed] [Google Scholar]
- 17.Nygaard RM, Daly SR, Van Camp JM. General surgery resident case logs: do they accurately reflect resident experience? J Surg Educ 2015;72:e178–83. [DOI] [PubMed] [Google Scholar]