General clinicians and junior paediatricians may have little experience of interpreting paediatric electrocardiograms. Although the basic principles of cardiac conduction and depolarisation are the same as for adults, age related changes in the anatomy and physiology of infants and children produce normal ranges for electrocardiographic features that differ from adults and vary with age. Awareness of these differences is the key to correct interpretation of paediatric electrocardiograms.
Successful use of paediatric electrocardiography
Be aware of age related differences in the indications for performing electrocardiography, the normal ranges for electrocardiographic variables, and the typical abnormalities in infants and children
Genuine abnormality is unusual; if abnormality is suspected, seek a specialist opinion
Indications for paediatric electrocardiography
| • Syncope or seizure | • Electrolyte disturbance |
| • Exertional symptoms | • Kawasaki disease |
| • Drug ingestion | • Rheumatic fever |
| • Tachyarrhythmia | • Myocarditis |
| • Bradyarrhythmia | • Myocardial contusion |
| • Cyanotic episodes | • Pericarditis |
| • Heart failure | • Post cardiac surgery |
| • Hypothermia | • Congenital heart defects |
Recording the electrocardiogram
To obtain a satisfactory recording in young children requires patience, and the parents may be helpful in providing a source of distraction. Limb electrodes may be placed in a more proximal position to reduce movement artefacts. Standard adult electrode positions are used but with the addition of either lead V3R or lead V4R to detect right ventricular or atrial hypertrophy. Standard paper speed (25 mm/s) and deflection (10 mm/mV) are used, although occasionally large QRS complexes may require the gain to be halved.
Paediatric electrocardiographic findings that may be normal
Heart rate >100 beats/min
QRS axis >90°
Right precordial T wave inversion
Dominant right precordial R waves
Short PR and QT intervals
Short P wave and short duration of QRS complexes
Inferior and lateral Q waves
Indications for electrocardiography
Chest pain in children is rarely cardiac in origin and is often associated with tenderness in the chest wall. Electrocardiography is not usually helpful in making a diagnosis, although a normal trace can be very reassuring to the family. Typical indications for paediatric electrocardiography include syncope, exertional symptoms, tachyarrhythmias, bradyarrhythmias, and drug ingestion. Use of electrocardiography to evaluate congenital heart defects is a specialist interest and will not be discussed here.
Age related changes in normal electrocardiograms
Features that would be diagnosed as abnormal in an adult's electrocardiogram may be normal, age related changes in a paediatric trace. The explanation for why this is so lies in how the heart develops during infancy and childhood.
At birth the right ventricle is larger than the left. Changes in systemic vascular resistance result in the left ventricle increasing in size until it is larger than the right ventricle by age 1 month. By age 6 months, the ratio of the right ventricle to the left ventricle is similar to that of an adult. Right axis deviation, large precordial R waves, and upright T waves are therefore normal in the neonate. The T wave in lead V1 inverts by 7 days and typically remains inverted until at least age 7 years. Upright T waves in the right precordial leads (V1 to V3) between ages 7 days and 7 years are a potentially important abnormality and usually indicate right ventricular hypertrophy.
The QRS complex also reflects these changes. At birth, the mean QRS axis lies between +60° and +160°, R waves are prominent in the right precordium, and S waves are prominent in the left precordium. By age 1 year, the axis changes gradually to lie between +10° and +100°.
The resting heart rate decreases from about 140 beats/min at birth to 120 beats/min at age 1 year, 100 at 5 years, and adult values by 10 years. The PR interval decreases from birth to age 1 year and then gradually increases throughout childhood. The P wave duration and the QRS duration also increase with age. The QT interval depends on heart rate and age, increasing with age while decreasing with heart rate. Q waves are normally seen in the inferior or lateral leads but signify disease if present in other leads.
Abnormal paediatric electrocardiograms
Diagnosis of abnormality on a paediatric electrocardiogram will require knowledge of normal age related values, particularly for criteria relating to right or left ventricular hypertrophy.
P wave amplitude varies little with age and is best evaluated from lead II, V1, or V4R. Wide P waves indicate left atrial hypertrophy, and P waves taller than 2.5 mm in lead II indicate right atrial hypertrophy. P waves showing an abnormal pattern, such as inversion in leads II or aVF, indicate atrial activation from a site other than the sinoatrial node.
Prolongation of the QRS complex may be due to bundle branch block, ventricular hypertrophy, metabolic disturbances, or drugs.
Diagnosis of ventricular hypertrophy by “voltage criteria” will depend on age adjusted values for R wave and S wave amplitudes. However, several electrocardiographic features may be useful in making a diagnosis. A qR complex or an rSR′ pattern in lead V1, upright T waves in the right precordial leads between ages 7 days and 7 years, marked right axis deviation (particularly associated with right atrial enlargement), and complete reversal of the adult precordial pattern of R and S waves will all suggest right ventricular hypertrophy. Left ventricular hypertrophy may be indicated by deep Q waves in the left precordial leads or the typical adult changes of lateral ST depression and T wave inversion.
Normal values in paediatric electrocardiograms
| Age | PR interval (ms) | QRS duration (ms) | R wave (S wave) amplitude (mm) | |
|---|---|---|---|---|
| Lead V1 | Lead V6 | |||
| Birth | 80-160 | <75 | 5-26 (1-23) | 0-12 (0-10) |
| 6 months | 70-150 | <75 | 3-20 (1-17) | 6-22 (0-10) |
| 1 year | 70-150 | <75 | 2-20 (1-20) | 6-23 (0-7) |
| 5 years | 80-160 | <80 | 1-16 (2-22) | 8-25 (0-5) |
| 10 years | 90-170 | <85 | 1-12 (3-25) | 9-26 (0-4) |
The QT interval must be corrected for heart rate by dividing its value by the square root of the R-R interval. A corrected QT interval exceeding 0.45 s should be considered prolonged, but it should be noted that the QT interval is highly variable in the first three days of life. QT prolongation may be seen in association with hypokalaemia, hypocalcaemia, hypothermia, drug treatment, cerebral injury, and the congenital long QT syndrome. Other features of the long QT syndrome include notching of the T waves, abnormal U waves, relative bradycardia for age, and T wave alternans. These children may be at risk of ventricular arrhythmia and sudden cardiac death.
Q waves are normally present in leads II, III, aVF, V5, and V6. Q waves in other leads are rare and associated with disease—for example, an anomalous left coronary artery, or myocardial infarction secondary to Kawasaki syndrome,.
ST segment elevation may be a normal finding in teenagers as a result of early repolarisation. It may also be seen in myocardial infarction, myocarditis, or pericarditis.
In addition to the changes seen in ventricular hypertrophy, T waves may be inverted as a result of myocardial disease (inflammation, infarction, or contusion). Flat T waves are seen in association with hypothyroidism. Abnormally tall T waves occur with hyperkalaemia.
Abnormalities of rate and rhythm
The wide variation in children's heart rate with age and activity may lead to misinterpretation by those more used to adult electrocardiography. Systemic illness must be considered in any child presenting with an abnormal cardiac rate or rhythm. Sinus tachycardia in babies and infants can result in rates of up to 240 beats/min, and hypoxia, sepsis, acidosis, or intracranial lesions may cause bradycardia. Sinus arrhythmia is a common feature in children's electrocardiograms and is often quite marked. Its relation to breathing—slowing on expiration and speeding up on inspiration—allows diagnosis.
The approach to electrocardiographic diagnosis of tachyarrhythmias in children is similar to that used in adults. Most narrow complex tachycardias in children are due to atrioventricular re-entrant tachycardia secondary to an accessory pathway. If the pathway conducts only retrogradely, the electrocardiogram in sinus rhythm will be normal and the pathway is said to be “concealed.” If the pathway conducts anterogradely in sinus rhythm, then the trace will show the typical features of the Wolff-Parkinson-White syndrome. AV nodal re-entrant tachycardia is rare in infants but may be seen in later childhood and adolescence.
Extrasystoles
Atrial extrasystoles are very common and rarely associated with disease
Ventricular extrasystoles are also common and, in the context of the structurally normal heart, are almost always benign
Typically, atrial and ventricular extrasystoles are abolished by exercise
Atrial flutter and fibrillation are rare in childhood and are usually associated with underlying structural heart disease or previous cardiac surgery. Atrial flutter can present as an uncommon arrhythmia in neonates with apparently otherwise normal hearts.
Aids for diagnosing tachycardias, such as atrioventricular dissociation and capture and fusion beats, are less common in children than in adults
Although all forms of ventricular tachycardia are rare, broad complex tachycardia should be considered to be ventricular tachycardia until proved otherwise. Bundle branch block (usually right bundle) often occurs after cardiac surgery, and a previous electrocardiogram can be helpful. Monomorphic ventricular tachycardia may occur secondary to surgery for congenital heart disease. Polymorphic ventricular tachycardia, or torsades de pointes, is associated with the long QT syndrome.
Complete atrioventricular block
Complete atrioventricular block may be congenital or secondary to surgery
An association exists between congenital complete atrioventricular block and maternal anti-La and anti-Ro antibodies, which are believed to cross the placenta and damage conduction tissue
Classification of atrioventricular block into first, second, and third degree follows the same principles as for adults, although a diagnosis of first degree heart block should take into account the variation of the PR interval with age. First degree heart block and the Wenckebach phenomenon may be a normal finding in otherwise healthy children. First or second degree block, however, can occur with rheumatic carditis, diphtheria, digoxin overdose, and congenital heart defects.
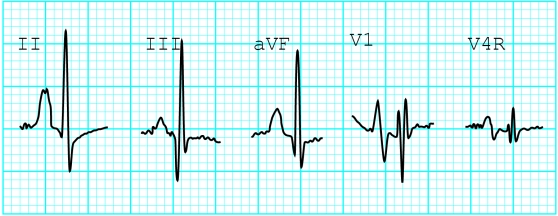
Figure.
Normal 12 lead electrocardiogram from 3 day old baby boy showing right axis deviation, dominant R wave in leads V4R and V1, and still predominantly upright T wave in V1. Persistence of upright T waves in right precordial leads beyond first week of life is sign of right ventricular hypertrophy
Figure.
Electrocardiogram from 12 year old (late childhood) (axis is now within normal “adult” range and R wave is no longer dominant in right precordial leads)
Figure.
Electrocardiogram from 3 year old with restrictive cardiomyopathy and severe right and left atrial enlargement. Tall (>2.5 mm), wide P waves are clearly seen in lead II, and P wave in V1 is markedly biphasic
Figure.
Electrocardiogram from 13 year old boy with transposition of great arteries and previous Mustard's procedure. The right ventricle is the systemic ventricle and the trace shows right ventricular hypertrophy with marked right axis deviation and a dominant R wave in the right precordial leads
Figure.
Electrocardiogram from 11 year old girl with left ventricular hypertrophy secondary to systemic hypertension. There are tall voltages in the left precordial and limb leads with secondary ST depression and T wave inversion
Figure.
Electrocardiogram from 3 year old girl with long QT syndrome
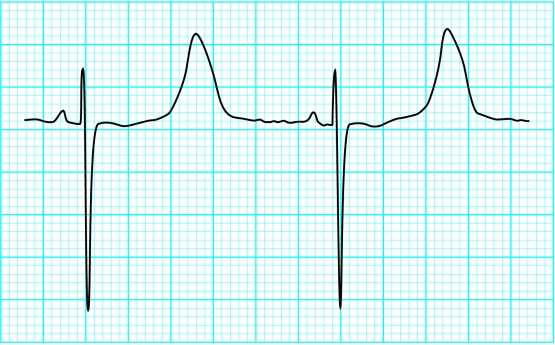
Figure.
Prolongation of QT interval in association with T wave alternans (note alternating upright and inverted T waves )
Figure.
Electrocardiogram from 9 year old boy showing marked sinus arrhythmia, a common finding in paediatric traces
Figure.
Electrocardiogram showing atrial “flutter” in 14 year old girl with congenital heart disease and previous atrial surgery (in neonates with atrial flutter, 1:1 atrioventricular conduction is more common, which may make P waves and diagnosis less evident)
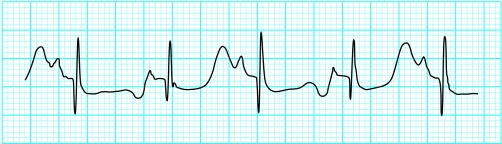
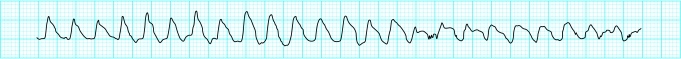
Figure.
Polymorphic ventricular tachycardia in 5 year old girl
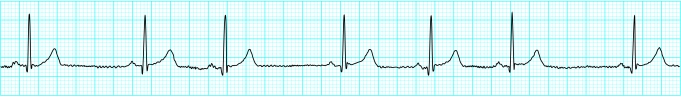
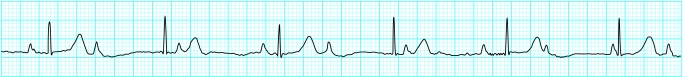
Figure.
Electrocardiogram from 6 year old girl with congenital heart block secondary to maternal antiphospholipid antibodies; there is complete atrioventricular dissociation, and the ventricular escape rate is about 50 beats/min
Footnotes
The ABC of clinical electrocardiography is edited by Francis Morris, consultant in emergency medicine at the Northern General Hospital, Sheffield; June Edhouse, consultant in emergency medicine, Stepping Hill Hospital, Stockport; William J Brady, associate professor, programme director, and vice chair, department of emergency medicine, University of Virginia, Charlottesville, VA, USA; and John Camm, professor of clinical cardiology, St George's Hospital Medical School, London. The series will be published as a book in the summer.
Steve Goodacre is health services research fellow in the accident and emergency department at the Northern General Hospital, Sheffield; and Karen McLeod is consultant paediatric cardiologist at the Royal Hospital for Sick Children, Glasgow.