Abstract
The incidence of autoimmune liver diseases (ALDs) and research on their pathogenesis are increasing annually. However, except for autoimmune hepatitis, which responds well to immunosuppression, primary biliary cholangitis and primary sclerosing cholangitis are insensitive to immunosuppressive therapy. Besides the known effects of the environment, genetics, and immunity on ALDs, the heterogeneity of target cells provides new insights into their pathogenesis. This review started by exploring the heterogeneity in the development, structures, and functions of hepatocytes and epithelial cells of the small and large bile ducts. For example, cytokeratin (CK) 8 and CK18 are primarily expressed in hepatocytes, while CK7 and CK19 are primarily expressed in intrahepatic cholangiocytes. Additionally, emerging technologies of single-cell RNA sequencing and spatial transcriptomic are being applied to study ALDs. This review offered a new perspective on understanding the pathogenic mechanisms and potential treatment strategies for ALDs.
Keywords: Autoimmune hepatitis, Primary biliary cholangitis, Primary sclerosing cholangitis, Disease heterogeneity, Single-cell RNA sequencing, Pathogenesis
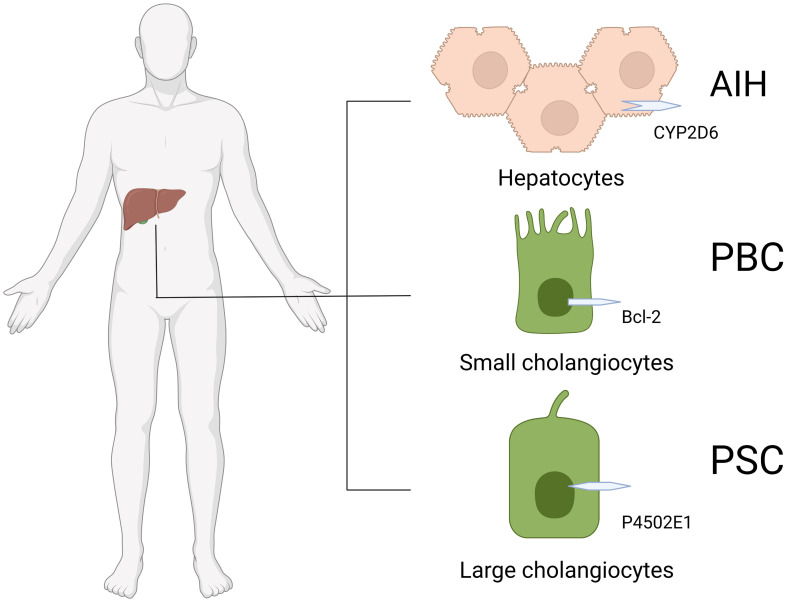
Graphical abstract
Introduction
The prevalence of autoimmune liver diseases (ALDs), including autoimmune hepatitis (AIH), primary biliary cholangitis (PBC), and primary sclerosing cholangitis (PSC), is increasing.1 The pathogenesis of these diseases remains unclear, but they are believed to involve a complex interaction of environmental, genetic, and immune factors. In genetically predisposed individuals, environmental factors may provoke autoimmune responses in the liver. ALDs are significant contributors to the spectrum of noncommunicable liver diseases, leading to severe outcomes, including cirrhosis, liver failure, and hepatocellular carcinoma.2
AIH is characterized by autoimmune-mediated damage to hepatic cells, as indicated by elevated serum aminotransferase levels, increased levels of immunoglobulin (Ig) G, presence of serum autoantibodies, and liver histology showing moderate-to-severe interface hepatitis. Treatment typically involves glucocorticoid administration and immunosuppressive therapy. PBC, an autoimmune disorder resulting in chronic intrahepatic cholestasis, predominantly affects epithelial cells of bile ducts and is more prevalent in middle-aged women. Symptoms include fatigue and pruritus, and diagnostic markers comprise elevated levels of alkaline phosphatase (ALP) and/or γ-glutamyl transpeptidase (GGT), elevated IgM, and the presence of anti-mitochondrial antibodies (AMAs) or PBC-specific antinuclear antibodies (ANAs). PBC pathology is characterized by ongoing non-suppurative and destructive cholangitis, with ursodeoxycholic acid as the primary therapeutic agent. PSC is characterized by chronic inflammation and fibrosis of intra- and extrahepatic bile ducts, leading to stenosis.3 Currently, there is no specific medication or therapeutic regimen for PSC, and the efficacies of glucocorticoids and immunosuppressants are unclear.
Although ALDs share common etiological factors, they affect different types of liver cells. Furthermore, there is considerable variability in affected populations, clinical manifestations, treatment approaches, and disease prognoses. This review aimed to examine the fundamental causes of these disparities and explore the potential for overlapping syndromes to affect liver and bile duct cells. We aimed to examine the pathogenesis of ALDs through cellular heterogeneity and identify precise therapeutic interventions. The novelty of this review stems from its comprehensive longitudinal and cross-sectional comparative analysis of target cell characteristics in ALDs. By focusing on heterogeneity, we aimed to elucidate previously unknown pathogenic mechanisms underlying autoimmune liver disorders and identify functional targets within the implicated cell populations. We anticipate that the insights gained will generate new avenues for clinical investigation.
Heterogeneity in the growth and development of hepatocytes and bile duct epithelial cells
Embryologically, hepatocytes and intrahepatic bile duct cells are derived from hepatoblasts,4 whereas extrahepatic bile duct cells share developmental origins with the pancreas and duodenum.5 Hepatocytes exhibit heterogeneity along the central vein-to-portal axis,6 displaying a zonal distribution of key liver-gene expression.7 Near the central vein, liver cells express various cytochrome enzymes and proliferate under homeostatic conditions,8 influenced by WNT and RSPO3 signaling from cells of the central vein endothelium.9
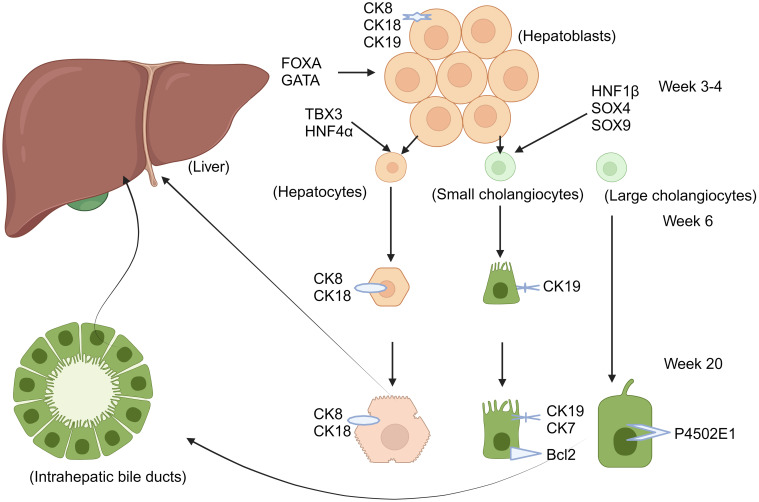
During embryogenesis, bipotent hypoblasts give rise to hepatocytes and bile duct cells.10 The transcription factors FOXA and GATA open chromatin, facilitating the transcription of serum albumin and HNF4α, which are essential for liver development.11,12 TBX3 and HNF4α further specify hypoblasts, while bile duct specificity is governed by HNF1β, SOX4, SOX9, ONECUT1, and ONECUT2.13,14 ONECUT2 inhibits CEBPα and HNF4α in bile duct cells, with SOX9 and CEBPα triggering epigenomic changes.15,16 By the 6th week of gestation, hypoblasts near the portal region form ductal plates, which are precursor structures to bile ducts.17 The expression of cytokeratins, including cytokeratin (CK) 8, CK18, and CK19 varies with portal vein proximity, indicative of differentiation status.18,19 CK7 expression emerges by the 20th week, primarily in cells of the intrahepatic bile duct.20 Postnatally, hepatocytes express CK8 and CK18, while CK7 and CK19 are characteristic of cells of the intrahepatic bile duct, which also exhibit hematopoietic stem cell markers, including c-kit, CD34, and CD33.21 Organoids from these bile duct cells express KRT19, underscoring their lineage.22 Liver development is a multicellular process,23 with hepatocytes maturing embryonically,24 unlike bile duct cells, which require additional transcription factors and activation of distinct signaling pathways.
Typical AIH is characterized by interfacial hepatitis and inflammation around the portal and periportal veins.25 Heterogeneity in cell surface marker distribution could influence the preference of AIH for specific hepatic sites. Therefore, exploring the differential expression of these markers and their impact on targets related to ALDs is a critical area of research (Fig. 1).
Fig. 1. Hepatoblasts begin to differentiate under the action of FOXA and GATA.
Hepatoblasts differentiate into hepatocytes, large and small cholangiocytes. CK8, CK18, and CK19 are expressed in hepatoblasts. CK8 and CK18 are expressed in hepatocytes at week 6. CK19 is expressed in intrahepatic cholangiocytes. CK7 is expressed in intrahepatic cholangiocytes at week 20. Bcl2 is expressed in small cholangiocytes after final differentiation. P4502E1 is expressed in large cholangiocytes. CK, cytokeratin; Bcl2, B-cell lymphoma 2; HNF, hepatocyte nuclear factor.
Heterogeneity in morphology and structure of hepatocytes and bile duct epithelial cells
Hepatocytes and bile duct cells exhibit cellular polarity, with liver cells arranged in a specialized polarized manner. Two adjacent hepatocytes contribute to the apical plasma membrane, forming bile canaliculi.26 This polarization is energy-dependent and crucial for maintaining liver function, while its disruption can lead to liver pathologies.27
Bile duct cells can be classified into six categories based on size, with the cytoplasm-to-nucleus ratio increasing with increasing bile duct diameter. Epithelial diversity is observed from the luminal surface to the deeper layers of the bile duct wall in peribiliary glands. As bile duct cells increase in size, they become more responsive to hormones and play a greater role in bile modification.28 Typically, these cells exhibit a columnar morphology, promoting apical-basal polarity and increasing the luminal surface area for efficient bile transport.29
Bile duct epithelial cells have distinct parietal luminal and basolateral plasma membrane domains, with primary cilia on the apical surface involved in homeostatic regulation. These cells facilitate communication and transport through endocytosis and exocytosis, while the actin cytoskeleton preserves the distribution and function of plasma membrane proteins. The cilia also serve as a protective barrier, shielding hepatocytes from exposure to bile.30,31
Functional heterogeneity of hepatocytes and epithelial cells of the bile duct
The liver serves as a pivotal metabolic regulator and performs essential functions, including the regulation of metabolism, protein synthesis, and bile production. Parenchymal and non-parenchymal liver cells exhibit unique properties in antigen presentation. Intestinal microbes, endogenous lipids, metabolites, and polypeptides can be presented via conventional and non-traditional pathways to activate intrahepatic immune cells. The glycosylation of antigens with N-acetylgalactosamine or N-acetylglucosamine enhances their uptake by hepatic antigen-presenting cells and induces immune tolerance. Hepatocytes maintain a threshold of antigen presentation that balances immune tolerance and immune responses, while disruptions to these thresholds may lead to ALDs.32,33 A low initial antigen load in hepatocytes triggers an effector CD8+ T cell response, whereas high antigen levels result in CD8+ T cell depletion and anergy,34 offering new insights for future ALD research. Bile duct epithelial cells are engaged in bile secretion. Contrary to earlier beliefs that only large bile duct cells secrete bile, current studies indicate that bile acid transporters are present in large and small duct cells. These cells exhibit functional heterogeneity, with small bile duct cells expressing blood group antigens and the anti-apoptotic protein Bcl-2, while large bile duct cells produce cytochrome P450 enzymes.30 Secretin stimulates the secretion of HCO3− and Cl− into the bile lumen, with receptors predominantly on cells of large bile ducts.35 The cilia on bile duct cells are crucial for mechanical, osmotic, and chemosensory functions, and their dysfunction is implicated in certain cholangiopathies.30
Heterogeneity of hepatocyte and bile duct epithelial cell damage in ALDs
In AIH, hepatocytes are the primary targets of damage, marked by inflammation extending from the portal tract into adjacent lobules. At the portal-lobule junction, progressive damage and necrosis occur in hepatocytes, resulting in interface hepatitis where cells necrose and desquamate at the boundary plate.36 Within lobules, hepatocyte edema, degeneration, and necrosis occur, ranging from focal (punctate) necrosis to confluent (bridging) necrosis. Additionally, regenerating hepatocytes form pseudo-glandular, rosette-like structures. Severe interfacial hepatitis can progress into lobules, presenting as zone 3 necrosis or bridging necrosis. The interaction of lymphocytes with hepatocytes leads to a halo-like structure, inducing apoptosis, known as the penetration phenomenon, with apoptotic bodies often observed. Severe portal inflammation and interface hepatitis may coincide with bile duct reactions, characterized by ductular reactions at the portal-parenchymal interface, lined by CK7-positive cells indicative of regenerative processes. Bile duct injury occurs in ≤ 83% of patients with AIH, at times resembling PBC, even without overlapping syndromes. However, the bile duct is not the primary target of AIH, and bile duct destruction or loss is not characteristic of the disease. The amelioration of bile duct injury following immunosuppressive treatment suggests that it may result from collateral damage during severe inflammation.37
PBC is characterized by chronic, nonsuppurative, and destructive cholangitis of the interlobular and septal bile ducts. The hallmark lesion, termed the florid duct lesion, includes lymphocytic infiltration and formation of epithelioid granulomas.38 Bile duct cells may exhibit edema, vacuolization, eosinophilic transformation, and necrosis, sometimes with proliferative cholangiopathy. Ductopenia, defined when <50% of portal tracts contain bile ducts, is also a feature.39 Mild interface hepatitis, characterized by portal inflammation, can occur in PBC along with parenchymal necro-inflammatory changes that are typically mild.40 Advanced stages of PBC may show feathery degeneration of hepatocytes due to the cytotoxic effects of hydrophobic bile acids.38
PSC is characterized by inflammation and fibrosis of the bile duct system, involving both intrahepatic and extrahepatic bile ducts. The characteristic onion-skin-like fibrosis encircles affected bile ducts, leading to atrophy, stenosis, and occlusion. Small-duct PSC a variant predominantly observed in children, affects only small intrahepatic bile ducts.38 It is an important feature of PSC, often accompanied by a reduction in interlobular bile ducts (Table 1).41
Table 1. Heterogeneity of hepatocyte and cholangiocyte damage in ALDs.
| AIH | PBC | PSC | |
|---|---|---|---|
| Main target cells | Hepatocytes. Severe chronic hepatitis with intense portal and lobular inflammation, severe interface hepatitis, and many damaged hepatocytes | Cholangiocytes (small interlobular and septal bile ducts). Non-suppurative destructive cholangitis. Cholangiocytes with swelling, vacuolated or eosinophilic cytoplasm, pyknotic nuclei, and proliferative changes with stratification | Cholangiocytes (large intra- and extra-hepatic bile ducts). Cholangiocytes with features of degeneration and atrophy, resulting in strictures and eventually occlusions |
| Inflammatory cells | Mainly lymphocytes, with a variable amount of plasma cells (especially the presence of plasma cell clusters). Some eosinophils and neutrophils may be seen | Mainly lymphocytes and often numerous plasma cells (especially a coronal arrangement of plasma cells around the bile duct). Eosinophils may also be numerous, particularly at earlier stages | In early disease, the changes are confined to portal tracts, with a mild mixed inflammatory cell infiltrate of lymphocytes, plasma cells, and neutrophils, usually more intense around bile ducts |
| Other parenchyma cells | Ductular reaction, collateral, and inconspicuous bile duct injury | Mild hepatocyte necrosis, acidophilic bodies, and even interface hepatitis. Feathery degeneration of hepatocytes in advanced disease stages | Small duct PSC (3–5% of PSC patients). In the late phase, periportal or diffuse hepatocyte metaplasia |
| Typical histopathology | Moderate-severe interface hepatitis, rosettes | Florid duct lesion | Onion skin fibrosis |
ALDs, autoimmune liver diseases; AIH, autoimmune hepatitis; PBC, primary biliary cholangitis; PSC, primary sclerosing cholangitis.
Heterogeneity in clinical manifestations of ALDs
The clinical presentation of ALDs typically begins insidiously, with patients often experiencing no symptoms or only nonspecific symptoms, such as fatigue. However, these conditions can progress to cirrhosis and liver failure. The following represent some notable distinctions among ALDs: First, AIH predominantly affects women and exhibits a significant incidence among adolescents, young children (0.23–0.4/100,000),42 and infants.43 Approximately one-third of AIH cases are acute. Generally, PBC and PSC have indistinct onsets. PBC is more prevalent in females aged >40 years, whereas PSC is more common in males, with an age range of 20–57 years, as well as some occurrences in children.44 Second, AIH is primarily characterized by hepatocyte damage, leading to a substantial increase in serum aminotransferase levels. In contrast, ALP and GGT levels remain normal or are only marginally elevated. However, patients with PBC or PSC exhibit significantly elevated ALP and/or GGT levels. Third, elevated serum IgG levels are observed in 90% of patients with AIH, while PBC is associated with increased IgM levels. Approximately half of patients with PSC exhibit mild-to-moderate elevations of IgG and/or IgM. Fourth, approximately one-third of patients with ALDs experience extrahepatic manifestations.45 AIH frequently coincides with autoimmune thyroid disease and celiac disease. Patients with PBC may develop Sjogren’s syndrome, autoimmune thyroid disease, and systemic sclerosis, among others.46 PSC is commonly associated with inflammatory bowel disease (IBD), including ulcerative colitis in 80% of cases, as well as Crohn’s disease and other unspecified forms of IBD.47 These comorbidities can influence the prognosis of the primary liver condition.48 Fifth, disease-specific autoantibodies vary among patients with ALDs. AIH involves ANAs, anti-smooth muscle antibodies, antibodies against liver/kidney microsomes, and/or liver cytosol antigens. PBC is characterized by AMAs, particularly AMA-M2, and PBC-specific ANAs targeting gp210 and p62 with a rim-like membranous pattern and a pattern of multiple nuclear dots recognizing sp100. Patients with PSC may exhibit nonspecific autoantibodies, including ANAs, anti-cardiolipin, anti-thyroperoxidase, rheumatoid factors, and anti-smooth muscle antibodies. Finally, therapeutic approaches differ; for instance, glucocorticoids and immunosuppressants are effective in AIH but are largely ineffective for PBC and PSC.49,50 Ursodeoxycholic acid is the first-line treatment for PBC but has no confirmed benefit in AIH or PSC. Prognostic models for PBC, PSC, and AIH can be developed based on demographic, clinical, complication-related, and serological characteristics.
Heterogeneity of target cells and the role of miRNAs in ALDs
AIH
Role of target cells
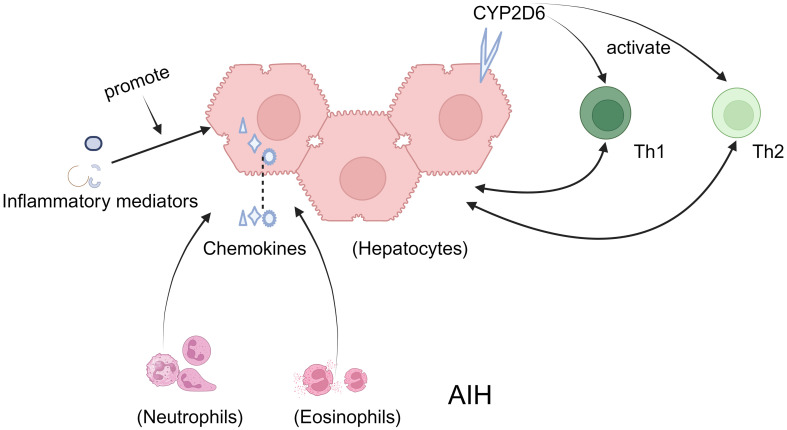
AIH is a chronic liver condition resulting from an autoimmune attack on hepatocytes.51 Serologically, AIH is characterized by elevated IgG levels and the presence of circulating autoantibodies, while histologically, interface hepatitis is evident.52 The autoimmune response in AIH may be initiated through molecular mimicry, wherein T cells mistakenly target host proteins.51 In AIH pathogenesis, the production of autoantibodies by plasma cells and the expression of antigen-specific cytotoxic T cells by hepatocytes significantly accelerate liver damage.53 Gatselis et al. found that decreased deoxyribonuclease I activity may be another important factor in the occurrence and development of AIH. When deoxyribonuclease activity decreases, the clearance of apoptotic cells is reduced, and the accumulation of nuclear antigen DNA aggravates the autoimmune reaction. Thus, in AIH, the persistence of liver damage is often self-perpetuating, driven by the apoptosis of infected liver cells.54 Interferon-gamma (IFN-γ) plays a pivotal role in mediating inflammation by inducing the expression of chemokine and adhesion molecules in hepatocytes, facilitating the chemotaxis of neutrophils and eosinophils.55 Furthermore, IFN-γ promotes the aberrant expression of HLA class II molecules in hepatocytes, allowing for antigen presentation and T-helper (Th) cell activation. Concurrently, increased expression of HLA class I molecules enables hepatocytes to present endogenous antigens to CD8+ T lymphocytes, which, upon activation, also secrete IFN-γ.
The enzyme cytochrome P450 2D6, a member of the cytochrome p450 family expressed by hepatocytes, is associated with anti-liver kidney microsomal antibodies in AIH.56 Cytochrome P450 2D6 is involved in Th1 and Th2 immune pathways.57 The involvement of epithelial cells of bile ducts in AIH is considered limited (Fig. 2).
Fig. 2. The role of hepatocytes in AIH.
1. In AIH, the expression of CYP2D6 in hepatocytes activates both Th1 and Th2 immune pathways. 2. Some inflammatory mediators induce the expression of chemokines and adhesion molecules in hepatocytes. AIH, autoimmune hepatitis; CYP2D6, Cytochrome P4502D6.
Role of microRNAs (miRNAs)
miRNAs, small RNA molecules critical for post-transcriptional gene regulation,58 have been implicated in various autoimmune conditions, including ALDs.59 Research on miRNAs in AIH has identified specific miRNAs, including miR-21, miR-122, and miR-155, which correlate with the severity of biochemical and histological abnormalities, as well as central pathogenic processes.60 Dysregulated miRNAs may act as biomarkers for disease activity and severity in AIH, and modulating their expression holds the potential to re-establish immune tolerance and reduce the autoimmune response.
PBC
Role of target cells
Bile duct cell dedifferentiation, senescence, stress, and DNA damage play key roles in the progression of PBC,61 which is histologically characterized by nonsuppurative destructive cholangitis and damage to the interlobular ducts.62 The disease features an immune-mediated inflammatory response, causing the degeneration, necrosis, and eventual disappearance of small-to-medium-sized intrahepatic bile ducts.63 Senescence of bile duct cells is increasingly recognized as a factor contributing to the progression of PBC and PSC.31 In PBC, continuous damage to bile duct epithelial cells causes senescence.64 This process begins with apoptosis, leading to the release of autoantigen epitopes that activate the immune system. When apoptosis of biliary epithelial cells (BECs) occurs in PBC, the E2 component of the mitochondrial pyruvate dehydrogenase complex in the formed apoptotic bodies retains immune activity, promoting immune activation.61 Disruptions to innate and adaptive immunity trigger disease onset.65 Additionally, aging BECs secrete chemokines and inflammatory mediators,66 contributing to the recruitment and activation of CD4+ Th cells.
Epithelial bile duct cells also serve as antigen-presenting cells, interacting with T cells,67 potentially causing bile duct damage. Among others, the chemokine C-X3-C motif chemokine ligand participates in this process.68 Furthermore, epithelial cells of bile ducts express molecules that recruit monocytes during disease, and these cells demonstrate significant proliferative activity to compensate for cell loss.69,70 When bile duct cells are damaged, they undergo a proliferative response as a protective mechanism. Specific liver injuries can trigger the proliferation of specific subsets of bile duct cells.71 Carpino et al. reported that SOX9+ cells from the peribiliary glands in PSC mice, induced by 3,5-diethoxycarbonyl-1,4-dihydrocollidine injury, proliferate and may be influenced by the activation of Wnt and Notch signaling pathways.72 Furthermore, bile duct cells in a damaged liver can differentiate into neuronal-like phenotypes, affecting disease progression.70
Role of miRNAs
In PBC, miR-122a and miR-26a are upregulated, while miR-328 and miR-299-5p are downregulated. These miRNAs and their target genes are implicated in biliary tract inflammation, apoptosis, and reactive oxidative stress.73 miR-506 has emerged as a unique contributor to the immunopathogenesis of PBC, with its chromosomal location on the X chromosome showing a female predominance, highlighting its potential role. MiR-506 decreases anion exchanger 2 (AE2) expression and activity in BECs, affecting bicarbonate secretion. Contemporary research has highlighted the role of miR-506 as a principal component of the immunopathogenesis of PBC. The correlation of miR-506’s position on the X chromosome with a higher disease prevalence in women highlights its likely importance in PBC pathophysiology.74 In vitro studies have shown that miR-506 may suppress AE2 expression, consequently hindering its function in BECs,75 and that applying miR-506 analogs can reduce bicarbonate secretion via AE2.76 Furthermore, increased concentrations of miR-122 and miR-378f, along with reduced levels of miR-4311 and miR-4714-3p in the serum of patients with treatment-resistant PBC, could provide valuable markers for evaluating therapeutic responses.77
PSC
PSC is a chronic cholestatic liver disease characterized by damage to the intrahepatic and/or extrahepatic bile ducts and is often associated with IBD.78 The distinct histological feature of PSC is onion-skin fibrosis, characterized by concentric layers of fibrotic tissue encasing bile duct epithelia. This fibrosis likely arises from interactions among bile duct cells, immune cells, hepatic stellate cells, and myofibroblasts in the portal areas, leading to ductal obstruction.79 Crosstalk between bile duct cells and T cells may facilitate the recruitment of inflammatory cells to portal tracts.80 In PSC, the biliary epithelium becomes highly reactive, exhibiting changes such as expansion of the peribiliary glandular system,81 yet precise pathogenic mechanisms remain elusive.
In managing ALDs, including AIH, PBC, and PSC, the application of immunosuppressive therapy faces numerous challenges.82 AIH is not merely an immune-mediated disease; various microenvironments may critically influence disease development.83
Application and updates of single-cell RNA sequencing and spatial transcriptomics in the heterogeneity of hepatocytes and cholangiocytes among ALDs
Single-cell RNA sequencing (scRNA-seq) is an emerging technology that characterizes the transcriptome of individual cells, identifying cell subpopulations within tissues with unprecedented resolution. Spatial transcriptomics complements this by capturing cell distribution using next-generation sequencing and imaging in spatially organized tissues.84 These technologies are increasingly used to explore disease pathogenesis. Researchers are developing two main approaches, deconvolution and mapping, to integrate them,85 enhancing our understanding of cell-type distribution and mechanisms of intercellular communication.
Recent studies have systematically compared transcriptomes from scRNA-seq and single-nucleus RNA sequencing, producing a high-resolution cellular atlas of the healthy human liver.86 Utilizing specific markers, researchers have spatially identified various cell subsets, including hepatocytes, cholangiocytes, and liver mesenchymal cells, demonstrating the physiological functions and pathological changes associated with ALDs.87 In a recent study using scRNA-seq in Oit3-CreERT2-tdTomato mice, Oit3 was identified as a key marker for tracing liver sinusoidal endothelial cells, offering a valuable model for investigating complexities in liver sinusoidal endothelial cells in relation to liver pathology.88
In the context of PBC, scRNA-seq and other methods have identified DUOX2+ACE2+ small cholangiocytes as pathogenic targets, with their reduction correlating with disease severity. Elevated levels of polymeric immunoglobulin receptor (pIgR) expression and serum anti-pIgR autoantibodies have been demonstrated in patients with PBC,89 suggesting a role in mediating IgA translocation and immune cell accumulation in the portal vein.90 Consequently, monoclonal antibodies targeting pIgR, DUOX2, and ACE2+ small cholangiocytes may serve as therapeutic options for PBC. Furthermore, spatial transcriptomics and multiplex immunofluorescence revealed an increase in the number of CD27+ memory B and plasma cells within the hepatic portal tracts of patients with PBC. scRNA-seq analysis of dnTGFbRII mice indicated that CD8+ T cells are pivotal in PBC pathogenesis, with distinct functions in terminally differentiated CD8aa T cells.91 Assessing these cell populations in liver biopsies or blood samples could assist in PBC diagnosis and staging, and personalized immunotherapy based on individual immune cell profiles may improve treatment efficacy.
In studies of healthy individuals and those with PSC, scRNA-seq revealed a higher prevalence of intrahepatic naïve-like CD4+ T cells in patients with PSC, predisposed to Th-17 polarization.92 Overexpression of P4HA2 was observed in the livers of patients with PBC and PSC, suggesting its role in promoting cholangiocyte proliferation via the SAV1-mediated Hippo signaling pathway.93 Targeting P4HA2 may represent a viable therapeutic strategy, which may be useful in early diagnosis, disease monitoring, and evaluation of treatment responses.
scRNA-seq of murine models has determined the immunological landscape, demonstrating that activation of the aryl hydrocarbon receptor can mitigate concanavalin A-induced AIH by modulating pro- and anti-inflammatory cytokines. Tetrachlorodibenzo-p-dioxin has been identified as a potent therapeutic agent.94 Similarly, a comprehensive transcriptomic analysis of autoreactive CD4 T cells in AIH has been described using scRNA-seq.95 The continual advancement of scRNA-seq and spatial transcriptomics is exposing disease pathogenesis with previously unclear mechanisms, with high-resolution technologies poised to summarize ALDs.
Summary and perspectives
The underlying pathogenesis of ALDs, including AIH with hepatocyte lesions, and PBC and PSC with bile duct cell damage, remains unclear. A common theme among these diseases is the intricate interplay between genetic, environmental, and immunological factors. These similar etiological agents lead to diverse ALDs, each characterized by distinct target cells, pathological mechanisms, and principles of diagnosis and treatment. The heterogeneity of target cells is a crucial factor influencing aspects ranging from growth and development to morphological structure, function, pathological damage, clinical presentation, and, most importantly, pathogenesis; this topic warrants further investigation.
Environmental and genetic factors modulate the immune system. However, the determinants guiding the immune response toward hepatocytes or biliary epithelium are poorly understood. The potential for immune cells to interact with hepatocytes and the biliary epithelium raises questions regarding the identification of surface markers or serum metabolites that could serve as biomarkers for disease diagnosis, management, and evaluation of disease severity and prognosis.
Current therapeutic strategies for ALDs primarily target immune regulation and bile acid metabolism, underscoring the need for additional research on the specific target cells involved. For instance, cholangiocyte senescence has been implicated in PBC and PSC pathogenesis.63 Consequently, interventions aimed at decelerating cholangiocyte senescence might offer a viable approach to treating these conditions. Building on the foundations of this review, future work will leverage single-cell sequencing technologies to explore cellular heterogeneity in AIH, PBC, and PSC. We aimed to identify genes with unique expression patterns and validate our findings using relevant studies in animal models, thereby providing innovative conceptual pathways for clinical research.
References
- 1.Lamba M, Ngu JH, Stedman CAM. Trends in Incidence of Autoimmune Liver Diseases and Increasing Incidence of Autoimmune Hepatitis. Clin Gastroenterol Hepatol. 2021;19(3):573–579.e1. doi: 10.1016/j.cgh.2020.05.061. [DOI] [PubMed] [Google Scholar]
- 2.Shen ZX, Wu DD, Xia J, Wang XB, Zheng X, Huang Y, et al. Prevalence and clinical characteristics of autoimmune liver disease in hospitalized patients with cirrhosis and acute decompensation in China. World J Gastroenterol. 2022;28(31):4417–4430. doi: 10.3748/wjg.v28.i31.4417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heo NY, Kim H. Epidemiology and updated management for autoimmune liver disease. Clin Mol Hepatol. 2023;29(1):194–196. doi: 10.3350/cmh.2022.0387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vestentoft PS, Jelnes P, Hopkinson BM, Vainer B, Møllgård K, Quistorff B, et al. Three-dimensional reconstructions of intrahepatic bile duct tubulogenesis in human liver. BMC Dev Biol. 2011;11:56. doi: 10.1186/1471-213X-11-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tremblay KD, Zaret KS. Distinct populations of endoderm cells converge to generate the embryonic liver bud and ventral foregut tissues. Dev Biol. 2005;280(1):87–99. doi: 10.1016/j.ydbio.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Halpern KB, Shenhav R, Matcovitch-Natan O, Toth B, Lemze D, Golan M, et al. Single-cell spatial reconstruction reveals global division of labour in the mammalian liver. Nature. 2017;542(7641):352–356. doi: 10.1038/nature21065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gebhardt R. Metabolic zonation of the liver: regulation and implications for liver function. Pharmacol Ther. 1992;53(3):275–354. doi: 10.1016/0163-7258(92)90055-5. [DOI] [PubMed] [Google Scholar]
- 8.Wang B, Zhao L, Fish M, Logan CY, Nusse R. Self-renewing diploid Axin2(+) cells fuel homeostatic renewal of the liver. Nature. 2015;524(7564):180–185. doi: 10.1038/nature14863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peng WC, Logan CY, Fish M, Anbarchian T, Aguisanda F, Álvarez-Varela A, et al. Inflammatory Cytokine TNFα Promotes the Long-Term Expansion of Primary Hepatocytes in 3D Culture. Cell. 2018;175(6):1607–1619.e15. doi: 10.1016/j.cell.2018.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang X, Yang L, Wang YC, Xu ZR, Feng Y, Zhang J, et al. Comparative analysis of cell lineage differentiation during hepatogenesis in humans and mice at the single-cell transcriptome level. Cell Res. 2020;30(12):1109–1126. doi: 10.1038/s41422-020-0378-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bort R, Martinez-Barbera JP, Beddington RS, Zaret KS. Hex homeobox gene-dependent tissue positioning is required for organogenesis of the ventral pancreas. Development. 2004;131(4):797–806. doi: 10.1242/dev.00965. [DOI] [PubMed] [Google Scholar]
- 12.Bossard P, Zaret KS. GATA transcription factors as potentiators of gut endoderm differentiation. Development. 1998;125(24):4909–4917. doi: 10.1242/dev.125.24.4909. [DOI] [PubMed] [Google Scholar]
- 13.Yu C, Li X, Zhao Y, Hu Y. The role of FOXA family transcription factors in glucolipid metabolism and NAFLD. Front Endocrinol (Lausanne) 2023;14:1081500. doi: 10.3389/fendo.2023.1081500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alder O, Cullum R, Lee S, Kan AC, Wei W, Yi Y, et al. Hippo signaling influences HNF4A and FOXA2 enhancer switching during hepatocyte differentiation. Cell Rep. 2014;9(1):261–271. doi: 10.1016/j.celrep.2014.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lotto J, Stephan TL, Hoodless PA. Fetal liver development and implications for liver disease pathogenesis. Nat Rev Gastroenterol Hepatol. 2023;20(9):561–581. doi: 10.1038/s41575-023-00775-2. [DOI] [PubMed] [Google Scholar]
- 16.Mukherjee S, French DL, Gadue P. Loss of TBX3 enhances pancreatic progenitor generation from human pluripotent stem cells. Stem Cell Reports. 2021;16(11):2617–2627. doi: 10.1016/j.stemcr.2021.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Terada T, Nakanuma Y. Detection of apoptosis and expression of apoptosis-related proteins during human intrahepatic bile duct development. Am J Pathol. 1995;146(1):67–74. [PMC free article] [PubMed] [Google Scholar]
- 18.Shiojiri N. Development and differentiation of bile ducts in the mammalian liver. Microsc Res Tech. 1997;39(4):328–335. doi: 10.1002/(SICI)1097-0029(19971115)39:4<328::AID-JEMT3>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 19.Desmet VJ, Van Eyken P, Sciot R. Cytokeratins for probing cell lineage relationships in developing liver. Hepatology. 1990;12(5):1249–1251. doi: 10.1002/hep.1840120530. [DOI] [PubMed] [Google Scholar]
- 20.Cocjin J, Rosenthal P, Buslon V, Luk L, Jr, Barajas L, Geller SA, et al. Bile ductule formation in fetal, neonatal, and infant livers compared with extrahepatic biliary atresia. Hepatology. 1996;24(3):568–574. doi: 10.1002/hep.510240318. [DOI] [PubMed] [Google Scholar]
- 21.Blakolmer K, Jaskiewicz K, Dunsford HA, Robson SC. Hematopoietic stem cell markers are expressed by ductal plate and bile duct cells in developing human liver. Hepatology. 1995;21(6):1510–1516. [PubMed] [Google Scholar]
- 22.Wesley BT, Ross ADB, Muraro D, Miao Z, Saxton S, Tomaz RA, et al. Single-cell atlas of human liver development reveals pathways directing hepatic cell fates. Nat Cell Biol. 2022;24(10):1487–1498. doi: 10.1038/s41556-022-00989-7. [DOI] [PubMed] [Google Scholar]
- 23.Camp JG, Sekine K, Gerber T, Loeffler-Wirth H, Binder H, Gac M, et al. Multilineage communication regulates human liver bud development from pluripotency. Nature. 2017;546(7659):533–538. doi: 10.1038/nature22796. [DOI] [PubMed] [Google Scholar]
- 24.Collardeau-Frachon S, Scoazec JY. Vascular development and differentiation during human liver organogenesis. Anat Rec (Hoboken) 2008;291(6):614–627. doi: 10.1002/ar.20679. [DOI] [PubMed] [Google Scholar]
- 25.Lohse AW, Mieli-Vergani G. Autoimmune hepatitis. J Hepatol. 2011;55(1):171–182. doi: 10.1016/j.jhep.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 26.Slim CL, Lázaro-Diéguez F, Bijlard M, Toussaint MJ, de Bruin A, Du Q, et al. Par1b induces asymmetric inheritance of plasma membrane domains via LGN-dependent mitotic spindle orientation in proliferating hepatocytes. PLoS Biol. 2013;11(12):e1001739. doi: 10.1371/journal.pbio.1001739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gissen P, Arias IM. Structural and functional hepatocyte polarity and liver disease. J Hepatol. 2015;63(4):1023–1037. doi: 10.1016/j.jhep.2015.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Jong IEM, van den Heuvel MC, Wells RG, Porte RJ. The heterogeneity of the biliary tree. J Hepatol. 2021;75(5):1236–1238. doi: 10.1016/j.jhep.2021.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Treyer A, Müsch A. Hepatocyte polarity. Compr Physiol. 2013;3(1):243–287. doi: 10.1002/cphy.c120009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheung AC, Lorenzo Pisarello MJ, LaRusso NF. Pathobiology of biliary epithelia. Biochim Biophys Acta Mol Basis Dis. 2018;1864(4 Pt B):1220–1231. doi: 10.1016/j.bbadis.2017.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trussoni CE, O’Hara SP, LaRusso NF. Cellular senescence in the cholangiopathies: a driver of immunopathology and a novel therapeutic target. Semin Immunopathol. 2022;44(4):527–544. doi: 10.1007/s00281-022-00909-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Horst AK, Kumashie KG, Neumann K, Diehl L, Tiegs G. Antigen presentation, autoantibody production, and therapeutic targets in autoimmune liver disease. Cell Mol Immunol. 2021;18(1):92–111. doi: 10.1038/s41423-020-00568-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilson DS, Damo M, Hirosue S, Raczy MM, Brünggel K, Diaceri G, et al. Synthetically glycosylated antigens induce antigen-specific tolerance and prevent the onset of diabetes. Nat Biomed Eng. 2019;3(10):817–829. doi: 10.1038/s41551-019-0424-1. [DOI] [PubMed] [Google Scholar]
- 34.Horst AK, Neumann K, Diehl L, Tiegs G. Modulation of liver tolerance by conventional and nonconventional antigen-presenting cells and regulatory immune cells. Cell Mol Immunol. 2016;13(3):277–292. doi: 10.1038/cmi.2015.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alpini G, Glaser S, Robertson W, Rodgers RE, Phinizy JL, Lasater J, et al. Large but not small intrahepatic bile ducts are involved in secretin-regulated ductal bile secretion. Am J Physiol. 1997;272(5 Pt 1):G1064–G1074. doi: 10.1152/AJPGI.1997.272.5.G1064. [DOI] [PubMed] [Google Scholar]
- 36.Covelli C, Sacchi D, Sarcognato S, Cazzagon N, Grillo F, Baciorri F, et al. Pathology of autoimmune hepatitis. Pathologica. 2021;113(3):185–193. doi: 10.32074/1591-951X-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Verdonk RC, Lozano MF, van den Berg AP, Gouw AS. Bile ductal injury and ductular reaction are frequent phenomena with different significance in autoimmune hepatitis. Liver Int. 2016;36(9):1362–1369. doi: 10.1111/liv.13083. [DOI] [PubMed] [Google Scholar]
- 38.Sarcognato S, Sacchi D, Grillo F, Cazzagon N, Fabris L, Cadamuro M, et al. Autoimmune biliary diseases: primary biliary cholangitis and primary sclerosing cholangitis. Pathologica. 2021;113(3):170–184. doi: 10.32074/1591-951X-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.You H, Ma X, Efe C, Wang G, Jeong SH, Abe K, et al. APASL clinical practice guidance: the diagnosis and management of patients with primary biliary cholangitis. Hepatol Int. 2022;16(1):1–23. doi: 10.1007/s12072-021-10276-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.European Association for the Study of the Liver EASL Clinical Practice Guidelines: The diagnosis and management of patients with primary biliary cholangitis. J Hepatol. 2017;67(1):145–172. doi: 10.1016/j.jhep.2017.03.022. [DOI] [PubMed] [Google Scholar]
- 41.Deneau MR, El-Matary W, Valentino PL, Abdou R, Alqoaer K, Amin M, et al. The natural history of primary sclerosing cholangitis in 781 children: A multicenter, international collaboration. Hepatology. 2017;66(2):518–527. doi: 10.1002/hep.29204. [DOI] [PubMed] [Google Scholar]
- 42.Islek A, Tumgor G. Seronegative autoimmune hepatitis in childhood. World J Clin Pediatr. 2023;12(3):77–85. doi: 10.5409/wjcp.v12.i3.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mieli-Vergani G, Vergani D, Baumann U, Czubkowski P, Debray D, Dezsofi A, et al. Diagnosis and Management of Pediatric Autoimmune Liver Disease: ESPGHAN Hepatology Committee Position Statement. J Pediatr Gastroenterol Nutr. 2018;66(2):345–360. doi: 10.1097/MPG.0000000000001801. [DOI] [PubMed] [Google Scholar]
- 44.Kemme S, Mack CL. Pediatric Autoimmune Liver Diseases: Autoimmune Hepatitis and Primary Sclerosing Cholangitis. Pediatr Clin North Am. 2021;68(6):1293–1307. doi: 10.1016/j.pcl.2021.07.006. [DOI] [PubMed] [Google Scholar]
- 45.Floreani A, De Martin S, Secchi MF, Cazzagon N. Extrahepatic autoimmunity in autoimmune liver disease. Eur J Intern Med. 2019;59:1–7. doi: 10.1016/j.ejim.2018.10.014. [DOI] [PubMed] [Google Scholar]
- 46.Chalifoux SL, Konyn PG, Choi G, Saab S. Extrahepatic Manifestations of Primary Biliary Cholangitis. Gut Liver. 2017;11(6):771–780. doi: 10.5009/gnl16365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sohal A, Kayani S, Kowdley KV. Primary Sclerosing Cholangitis: Epidemiology, Diagnosis, and Presentation. Clin Liver Dis. 2024;28(1):129–141. doi: 10.1016/j.cld.2023.07.005. [DOI] [PubMed] [Google Scholar]
- 48.Jain V, Yachha SK, Bhatia E, Sarma MS, Srivastava A. Concurrent extrahepatic autoimmune disorders: unexplored dimension of autoimmune liver disease in children. Eur J Gastroenterol Hepatol. 2018;30(8):910–917. doi: 10.1097/MEG.0000000000001122. [DOI] [PubMed] [Google Scholar]
- 49.Wang ZL, Jin R, Hao M, Xie YD, Liu ZC, Wang XX, et al. Treatment of ursodeoxycholic acid with glucocorticoids and immunosuppressants may improve the long-term survival rate in primary biliary cholangitis patients. Medicine (Baltimore) 2022;101(46):e31395. doi: 10.1097/MD.0000000000031395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Engel B, Taubert R, Jaeckel E, Manns MP. The future of autoimmune liver diseases - Understanding pathogenesis and improving morbidity and mortality. Liver Int. 2020;40(Suppl 1):149–153. doi: 10.1111/liv.14378. [DOI] [PubMed] [Google Scholar]
- 51.Bhumi SA, Wu GY. Seronegative Autoimmune Hepatitis. J Clin Transl Hepatol. 2023;11(2):459–465. doi: 10.14218/JCTH.2022.00235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Terziroli Beretta-Piccoli B, Mieli-Vergani G, Vergani D. The clinical usage and definition of autoantibodies in immune-mediated liver disease: A comprehensive overview. J Autoimmun. 2018;95:144–158. doi: 10.1016/j.jaut.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 53.Lotfy A, Elgamal A, Burdzinska A, Swelum AA, Soliman R, Hassan AA, et al. Stem cell therapies for autoimmune hepatitis. Stem Cell Res Ther. 2021;12(1):386. doi: 10.1186/s13287-021-02464-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gatselis NK, Vakrakou AG, Zachou K, Androutsakos T, Azariadis K, Hatzis G, et al. Decreased serum DNase1-activity in patients with autoimmune liver diseases. Autoimmunity. 2017;50(2):125–132. doi: 10.1080/08916934.2017.1279610. [DOI] [PubMed] [Google Scholar]
- 55.Jaruga B, Hong F, Kim WH, Gao B. IFN-gamma/STAT1 acts as a proinflammatory signal in T cell-mediated hepatitis via induction of multiple chemokines and adhesion molecules: a critical role of IRF-1. Am J Physiol Gastrointest Liver Physiol. 2004;287(5):G1044–G1052. doi: 10.1152/ajpgi.00184.2004. [DOI] [PubMed] [Google Scholar]
- 56.Muratori L, Parola M, Ripalti A, Robino G, Muratori P, Bellomo G, et al. Liver/kidney microsomal antibody type 1 targets CYP2D6 on hepatocyte plasma membrane. Gut. 2000;46(4):553–561. doi: 10.1136/gut.46.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ma Y, Bogdanos DP, Hussain MJ, Underhill J, Bansal S, Longhi MS, et al. Polyclonal T-cell responses to cytochrome P450IID6 are associated with disease activity in autoimmune hepatitis type 2. Gastroenterology. 2006;130(3):868–882. doi: 10.1053/j.gastro.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 58.Qin B, Huang F, Liang Y, Yang Z, Zhong R. Analysis of altered microRNA expression profiles in peripheral blood mononuclear cells from patients with primary biliary cirrhosis. J Gastroenterol Hepatol. 2013;28(3):543–550. doi: 10.1111/jgh.12040. [DOI] [PubMed] [Google Scholar]
- 59.Szabo G, Bala S. MicroRNAs in liver disease. Nat Rev Gastroenterol Hepatol. 2013;10(9):542–552. doi: 10.1038/nrgastro.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Czaja AJ. Examining micro-ribonucleic acids as diagnostic and therapeutic prospects in autoimmune hepatitis. Expert Rev Clin Immunol. 2022;18(6):591–607. doi: 10.1080/1744666X.2022.2074839. [DOI] [PubMed] [Google Scholar]
- 61.Lleo A, Leung PSC, Hirschfield GM, Gershwin EM. The Pathogenesis of Primary Biliary Cholangitis: A Comprehensive Review. Semin Liver Dis. 2020;40(1):34–48. doi: 10.1055/s-0039-1697617. [DOI] [PubMed] [Google Scholar]
- 62.Lindor KD, Gershwin ME, Poupon R, Kaplan M, Bergasa NV, Heathcote EJ, et al. Primary biliary cirrhosis. Hepatology. 2009;50(1):291–308. doi: 10.1002/hep.22906. [DOI] [PubMed] [Google Scholar]
- 63.Tanaka A. Current understanding of primary biliary cholangitis. Clin Mol Hepatol. 2021;27(1):1–21. doi: 10.3350/cmh.2020.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brain JG, Robertson H, Thompson E, Humphreys EH, Gardner A, Booth TA, et al. Biliary epithelial senescence and plasticity in acute cellular rejection. Am J Transplant. 2013;13(7):1688–1702. doi: 10.1111/ajt.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li H, Guan Y, Han C, Zhang Y, Liu Q, Wei W, et al. The pathogenesis, models and therapeutic advances of primary biliary cholangitis. Biomed Pharmacother. 2021;140:111754. doi: 10.1016/j.biopha.2021.111754. [DOI] [PubMed] [Google Scholar]
- 66.Sasaki M, Ikeda H, Sato Y, Nakanuma Y. Proinflammatory cytokine-induced cellular senescence of biliary epithelial cells is mediated via oxidative stress and activation of ATM pathway: a culture study. Free Radic Res. 2008;42(7):625–632. doi: 10.1080/10715760802244768. [DOI] [PubMed] [Google Scholar]
- 67.Björkland A, Festin R, Mendel-Hartvig I, Nyberg A, Lööf L, Tötterman TH. Blood and liver-infiltrating lymphocytes in primary biliary cirrhosis: increase in activated T and natural killer cells and recruitment of primed memory T cells. Hepatology. 1991;13(6):1106–1111. doi: 10.1002/hep.1840130617. [DOI] [PubMed] [Google Scholar]
- 68.Isse K, Harada K, Zen Y, Kamihira T, Shimoda S, Harada M, et al. Fractalkine and CX3CR1 are involved in the recruitment of intraepithelial lymphocytes of intrahepatic bile ducts. Hepatology. 2005;41(3):506–516. doi: 10.1002/hep.20582. [DOI] [PubMed] [Google Scholar]
- 69.Imai T, Hieshima K, Haskell C, Baba M, Nagira M, Nishimura M, et al. Identification and molecular characterization of fractalkine receptor CX3CR1, which mediates both leukocyte migration and adhesion. Cell. 1997;91(4):521–530. doi: 10.1016/s0092-8674(00)80438-9. [DOI] [PubMed] [Google Scholar]
- 70.Alvaro D, Mancino MG, Glaser S, Gaudio E, Marzioni M, Francis H, et al. Proliferating cholangiocytes: a neuroendocrine compartment in the diseased liver. Gastroenterology. 2007;132(1):415–431. doi: 10.1053/j.gastro.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 71.Maroni L, Haibo B, Ray D, Zhou T, Wan Y, Meng F, et al. Functional and structural features of cholangiocytes in health and disease. Cell Mol Gastroenterol Hepatol. 2015;1(4):368–380. doi: 10.1016/J.JCMGH.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Carpino G, Nevi L, Overi D, Cardinale V, Lu WY, Di Matteo S, et al. Peribiliary Gland Niche Participates in Biliary Tree Regeneration in Mouse and in Human Primary Sclerosing Cholangitis. Hepatology. 2020;71(3):972–989. doi: 10.1002/hep.30871. [DOI] [PubMed] [Google Scholar]
- 73.Padgett KA, Lan RY, Leung PC, Lleo A, Dawson K, Pfeiff J, et al. Primary biliary cirrhosis is associated with altered hepatic microRNA expression. J Autoimmun. 2009;32(3-4):246–253. doi: 10.1016/j.jaut.2009.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rodrigues PM, Perugorria MJ, Santos-Laso A, Bujanda L, Beuers U, Banales JM. Primary biliary cholangitis: A tale of epigenetically-induced secretory failure? J Hepatol. 2018;69(6):1371–1383. doi: 10.1016/j.jhep.2018.08.020. [DOI] [PubMed] [Google Scholar]
- 75.Banales JM, Sáez E, Uriz M, Sarvide S, Urribarri AD, Splinter P, et al. Up-regulation of microRNA 506 leads to decreased Cl-/HCO3- anion exchanger 2 expression in biliary epithelium of patients with primary biliary cirrhosis. Hepatology. 2012;56(2):687–697. doi: 10.1002/hep.25691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ananthanarayanan M, Banales JM, Guerra MT, Spirli C, Munoz-Garrido P, Mitchell-Richards K, et al. Post-translational regulation of the type III inositol 1,4,5-trisphosphate receptor by miRNA-506. J Biol Chem. 2015;290(1):184–196. doi: 10.1074/jbc.M114.587030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Huang C, Xing X, Xiang X, Fan X, Men R, Ye T, et al. MicroRNAs in autoimmune liver diseases: from diagnosis to potential therapeutic targets. Biomed Pharmacother. 2020;130:110558. doi: 10.1016/j.biopha.2020.110558. [DOI] [PubMed] [Google Scholar]
- 78.Rabiee A, Silveira MG. Primary sclerosing cholangitis. Transl Gastroenterol Hepatol. 2021;6:29. doi: 10.21037/tgh-20-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Karlsen TH, Folseraas T, Thorburn D, Vesterhus M. Primary sclerosing cholangitis - a comprehensive review. J Hepatol. 2017;67(6):1298–1323. doi: 10.1016/j.jhep.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 80.Kamihira T, Shimoda S, Nakamura M, Yokoyama T, Takii Y, Kawano A, et al. Biliary epithelial cells regulate autoreactive T cells: implications for biliary-specific diseases. Hepatology. 2005;41(1):151–159. doi: 10.1002/hep.20494. [DOI] [PubMed] [Google Scholar]
- 81.Mederacke I, Hsu CC, Troeger JS, Huebener P, Mu X, Dapito DH, et al. Fate tracing reveals hepatic stellate cells as dominant contributors to liver fibrosis independent of its aetiology. Nat Commun. 2013;4:2823. doi: 10.1038/ncomms3823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhao Y, Wei S, Chen L, Zhou X, Ma X. Primary biliary cholangitis: molecular pathogenesis perspectives and therapeutic potential of natural products. Front Immunol. 2023;14:1164202. doi: 10.3389/fimmu.2023.1164202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ren X, Zhang L, Zhang Y, Li Z, Siemers N, Zhang Z. Insights Gained from Single-Cell Analysis of Immune Cells in the Tumor Microenvironment. Annu Rev Immunol. 2021;39:583–609. doi: 10.1146/annurev-immunol-110519-071134. [DOI] [PubMed] [Google Scholar]
- 84.Rao A, Barkley D, França GS, Yanai I. Exploring tissue architecture using spatial transcriptomics. Nature. 2021;596(7871):211–220. doi: 10.1038/s41586-021-03634-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Longo SK, Guo MG, Ji AL, Khavari PA. Integrating single-cell and spatial transcriptomics to elucidate intercellular tissue dynamics. Nat Rev Genet. 2021;22(10):627–644. doi: 10.1038/s41576-021-00370-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Andrews TS, Atif J, Liu JC, Perciani CT, Ma XZ, Thoeni C, et al. Single-Cell, Single-Nucleus, and Spatial RNA Sequencing of the Human Liver Identifies Cholangiocyte and Mesenchymal Heterogeneity. Hepatol Commun. 2022;6(4):821–840. doi: 10.1002/hep4.1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Saviano A, Henderson NC, Baumert TF. Single-cell genomics and spatial transcriptomics: Discovery of novel cell states and cellular interactions in liver physiology and disease biology. J Hepatol. 2020;73(5):1219–1230. doi: 10.1016/j.jhep.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Li ZW, Ruan B, Yang PJ, Liu JJ, Song P, Duan JL, et al. Oit3, a promising hallmark gene for targeting liver sinusoidal endothelial cells. Signal Transduct Target Ther. 2023;8(1):344. doi: 10.1038/s41392-023-01621-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Li X, Li Y, Xiao J, Wang H, Guo Y, Mao X, et al. Unique DUOX2(+)ACE2(+) small cholangiocytes are pathogenic targets for primary biliary cholangitis. Nat Commun. 2023;14(1):29. doi: 10.1038/s41467-022-34606-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Biswas S, Mandal G, Payne KK, Anadon CM, Gatenbee CD, Chaurio RA, et al. IgA transcytosis and antigen recognition govern ovarian cancer immunity. Nature. 2021;591(7850):464–470. doi: 10.1038/s41586-020-03144-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Han Y, Bian ZH, Yang SY, Wang CB, Li L, Yang YQ, et al. Single-Cell Characterization of Hepatic CD8(+) T Cells in a Murine Model of Primary Biliary Cholangitis. Front Immunol. 2022;13:860311. doi: 10.3389/fimmu.2022.860311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Poch T, Krause J, Casar C, Liwinski T, Glau L, Kaufmann M, et al. Single-cell atlas of hepatic T cells reveals expansion of liver-resident naive-like CD4(+) T cells in primary sclerosing cholangitis. J Hepatol. 2021;75(2):414–423. doi: 10.1016/j.jhep.2021.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhang J, Lyu Z, Li B, You Z, Cui N, Li Y, et al. P4HA2 induces hepatic ductular reaction and biliary fibrosis in chronic cholestatic liver diseases. Hepatology. 2023;78(1):10–25. doi: 10.1097/HEP.0000000000000317. [DOI] [PubMed] [Google Scholar]
- 94.Cannon AS, Holloman BL, Wilson K, Miranda K, Dopkins N, Nagarkatti P, et al. AhR Activation Leads to Attenuation of Murine Autoimmune Hepatitis: Single-Cell RNA-Seq Analysis Reveals Unique Immune Cell Phenotypes and Gene Expression Changes in the Liver. Front Immunol. 2022;13:899609. doi: 10.3389/fimmu.2022.899609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Renand A, Cervera-Marzal I, Gil L, Dong C, Garcia A, Kervagoret E, et al. Integrative molecular profiling of autoreactive CD4 T cells in autoimmune hepatitis. J Hepatol. 2020;73(6):1379–1390. doi: 10.1016/j.jhep.2020.05.053. [DOI] [PubMed] [Google Scholar]