Abstract
HIV-related stigma remains a significant barrier to implementing effective HIV treatment and prevention strategies in Nigeria. Despite the high uptake of peer support groups among people living with HIV (PLHIV) in Nigeria, the potential role of such peer support on the burden of internalized stigma remains understudied. To address this gap, we conducted a secondary analysis of the PLHIV Stigma Index 2.0, a socio-behavioral survey implemented by PLHIV led-organizations to assess the relationship between group membership and internalized stigma. Internalized stigma was measured using the Internalized AIDS-related Stigma Scale. Multinomial logistic regression was used to measure the association between self-reported engagement in peer support groups and internalized stigma adjusting for age, education, duration since HIV diagnosis, employment, disclosure status, and sex-work engagement. Of the 1,244 respondents in this study, 75.1% were engaged in HIV peer support groups. Over half (55.5%) and about one-fourth (27.3%) demonstrated low/moderate and high levels of internalized stigma, respectively. PLHIV engaged in HIV peer support groups were less likely to report both low/moderate (versus no) (adjusted odds ratio (aOR): 0.47 [95% CI: 0.27 to 0.81]; p = 0.006) and high (versus no) (aOR: 0.30 [95% CI: 0.17 to 0.53]; p < 0.001) levels of internalized stigma compared to those not engaged. In this study, the burden of internalized stigma is high among PLHIV in Nigeria. However, engagement in peer support groups appears to mitigate these stigmas. Stigma mitigation strategies to increase peer support may represent a critical tool in decreasing sustained HIV treatment gaps among PLHIV in Nigeria.
Keywords: HIV, Stigma, Peer Support, Social Capital, Nigeria, sub-Saharan Africa
Introduction
HIV-related stigma remains a major barrier to testing, treatment, and adherence for people living with HIV (PLHIV) in Nigeria [1, 2]. A secondary analysis of the 2013 Nigerian National Demographic Health Survey found that about half the men and women aged 15–49 years discriminated against PLHIV [1]. Additionally, HIV-related stigma has been shown to be a significant barrier to developing an effective national response to HIV [2, 3]. With the fourth highest number of PLHIV worldwide, there are unmet treatment needs among PLHIV in Nigeria [4]. As of December 2020, an estimated 92% of all PLHIV in Nigeria were aware of their status, 90% were on HIV treatment, and only 59% were virally suppressed [4].
HIV stigmas manifest in various forms, including internalized, anticipated, perceived, experienced or enacted, and intersectional [5]. These stigmas have consistently been shown to interfere with the prevention, care, and treatment of HIV [5]. Internalized stigma related to HIV is defined as the acceptance, acknowledgement and application of negative labels, stereotypes, and societal perceptions of PLHIV to the self [6]. It encompasses self-blame, perceptions of being less than others, and deserving of negative or adverse outcomes [6]. Consistent data suggests that internalized stigma is driven by wider social and structural factors that affect health [7]. Further, evidence has shown that internalized stigma occurs at an intersection of social categorizations based on sociodemographic and other distinguishing characteristics that are mutually reinforcing and contribute to the marginalization of individuals [7–9]. Characterizing the intersectional mechanisms of stigma on adverse health outcomes has been shown to be important for the development of system-wide interventions to address internalized stigma [7].
Leveraging social capital has been suggested as a system-wide approach that can ameliorate the effects of stigma and improve the health outcomes of PLHIV [10]. The World Bank defines social capital as norms and networks that allow groups within a society to achieve a common objective. Social capital includes the institutions and relationships that shape social interactions within a society [11] and has been found to influence health across various levels within the socioecological model [12]. In a framework by Nahapiet and Ghoshal, three different but interrelated constructs of social capital were proposed, namely structural, cognitive, and relational. They defined structural social capital as all the resources available to an individual through a social network that can be measured by their membership or activity [13]. The relationships and networks formed through peer support have been leveraged as a strategy to build social capital and support program goals [14].
The data demonstrating effectiveness of HIV peer support groups in improving clinical outcomes for PLHIV remains inconsistent [15]. A PLHIV peer support group has been defined as a community-level, peer driven HIV intervention where PLHIV come together to share lived experiences without fear of criticism, judgement, stigmatization, or social isolation [16]. Incorporating peers into HIV interventions has been shown to improve linkage to HIV care, medication adherence, retention, and quality of life [17] thereby making it an increasingly popular intervention in sub-Saharan Africa [15, 18]. A study among female sex workers in Zimbabwe also found that strong peer support networks improved familiarity and trust with HIV programs and increased willingness to engage in interventions [19]. In contrast, a recent scoping review on peer support for PLHIV globally demonstrated mixed impacts of peer interventions on HIV-related outcomes [20]. Notwithstanding the variability on the direct effectiveness of peer support groups on clinical outcomes, these groups have been demonstrated as a common and widely acceptable component of HIV service delivery in sub-Saharan Africa [15].
As of 2022, the potential role of HIV peer support groups in addressing internalized stigma among PLHIV remains understudied. In response, this study aimed to characterize the relationship between engagement in peer support groups and internalized stigma among PLHIV in Nigeria. As a secondary aim, we examined whether anticipated or experienced stigma modified the observed relationship between peer support groups and internalized stigma.
Methods
Study Setting, Sample, and Recruitment
PLHIV Stigma Index 2.0
In 2008, the Global Network of People Living with HIV (GNP+), the International Community of Women Living with HIV (ICW), the Joint United Nations Programme on HIV/AIDS, and the International Planned Parenthood Federation developed the first PLHIV Stigma Index [21]. This tool was developed by and for PLHIV to document their experiences of HIV-related stigma, including intersectional stigma due to high-risk behavior and discrimination, in line with the Greater Involvement of People living with HIV and AIDS (GIPA) principle [22]. The GIPA principle aims to uphold the rights of PLHIV to be involved in decision-making processes that impact their lives [23]. However, in 2018, to align with a shift in the response to the HIV epidemic globally, the Stigma Index was modified and re-launched as the PLHIV Stigma Index 2.0. This modification focused on better measuring the experiences of a diverse population of PLHIV to more clearly understand the impact of stigma on healthcare access and health outcomes across the HIV continuum of care [24].
This study is a secondary analysis of quantitative data from the PLHIV Stigma Index 2.0 – a cross-sectional survey that was implemented by PLHIV-led organizations across 16 states and the Federal Capital Territory in Nigeria. The PLHIV Stigma Index 2.0 in Nigeria was designed through a consultative process led by the Network of People Living with HIV in Nigeria, GNP+, ICW, and supported by other stakeholders. Details of the survey methodology have been previously described [25]. The research team recruited 1,244 PLHIV in Nigeria using venue-based (antiretroviral therapy clinics, HIV community-based organizations, One Stop Shops, and HIV support groups) and snowball sampling. These sampling strategies were adopted to capture a diverse range of populations living with HIV, including key populations. Participants were eligible for the study if they were 18 years old or older, living with HIV, and aware of their HIV status for at least one year.
Data Collection
Eligible participants completed an interviewer-administered PLHIV Stigma Index 2.0 questionnaire via the RED-Cap (Research Electronic Data Capture) online survey platform. Interviewers self-identified as PLHIV and were trained in survey administration. Written informed consent was obtained from all participants before recruitment in the study. Survey data was collected from May to June 2021. Primary data collection was approved by the National Health Research Ethics Committee Nigeria, while the Johns Hopkins School of Public Health approved the secondary data analysis presented here.
Measures
Outcome
The Internalized AIDS-related Stigma Scale (IA-RSS) was used to assess internalized stigma [26, 27]. Developed by Kalichman and colleagues, this tool reflects Goffman’s dimensions of stigma and focuses on self-blame and concealment of HIV status, and has been validated in settings across eSwatini, South Africa, and the United States [25–28]. This tool was used to assess internalized stigma because of its established content validity and adequate internal consistency, as reported in prior studies with a Cronbach’s α coefficient that ranges between 0.73 and 0.76 [26]. The IA-RSS was also found to be brief and straightforward to administer [26, 29]. The IA-RSS used a six (6) item scale composed of two (2) items related to disclosure and four (4) items related to feelings of shame. Participants were asked the following questions: “It is difficult to tell people about my HIV infection,” “Being HIV positive makes me feel dirty,” “I feel guilty that I am HIV positive,” “I am ashamed that I am HIV positive,” “I sometimes feel worthless because I am HIV positive” and “I hide my HIV status from others.” Responses were recorded as a binary outcome (agree vs. disagree), which was summed to provide a score for each participant. We categorized respondents on a scale of zero (0), described as having no internalized stigma, to a full scale of six (6), with the highest level of internalized stigma. For this analysis, we further categorized the IA-RSS scores into three categories – score 0 (no internalized stigma), 1–3 (low/moderate internalized stigma) and 4–6 (high internalized stigma).
Exposure
The primary exposure of interest was engagement in HIV peer support groups measured as a dichotomous variable. The study had identified respondents as being engaged in a support group if they selected “yes” on the questionnaire item “Are you a member of a network or support group of people living with HIV?”
Covariates
Other covariates were chosen based on their hypothesized association with engagement in HIV peer support groups and internalized stigma from the literature [30]. These variables were self-reported and included participants’ sociodemographic, behavioral, and structural characteristics. Demographic characteristics reported included age, gender (male, female, and transgender), educational level, employment status (employed full-time, employed part-time, retired/on a pension, unemployed). Gender identity was assessed using a two-step instrument where sex assigned at birth and current gender were used to determine respondents’ gender identity. The behavioral level determinants assessed included engagement in sex work. Two main stigma types – anticipated or experienced stigma related to HIV status were used as proxy measures for structural level factors. While these measures don’t directly capture structural level factors that may affect PLHIV, it does reflect the perceived impact of structural factors on PLHIV and can provide insights into how broader societal attitudes and policies impact PLHIV. Anticipated or experienced stigma was measured based on self-reported experiences of discrimination in healthcare settings and the workplace, social exclusion, and avoidance of seeking healthcare due to fear of stigma and discrimination. Participants who self-reported at least one of the above experiences were categorized under these two stigma types. The hypothesized relationship of these variables with engagement in HIV support groups and internalized stigma are shown in the conceptual model (Fig. 1).
Fig. 1.
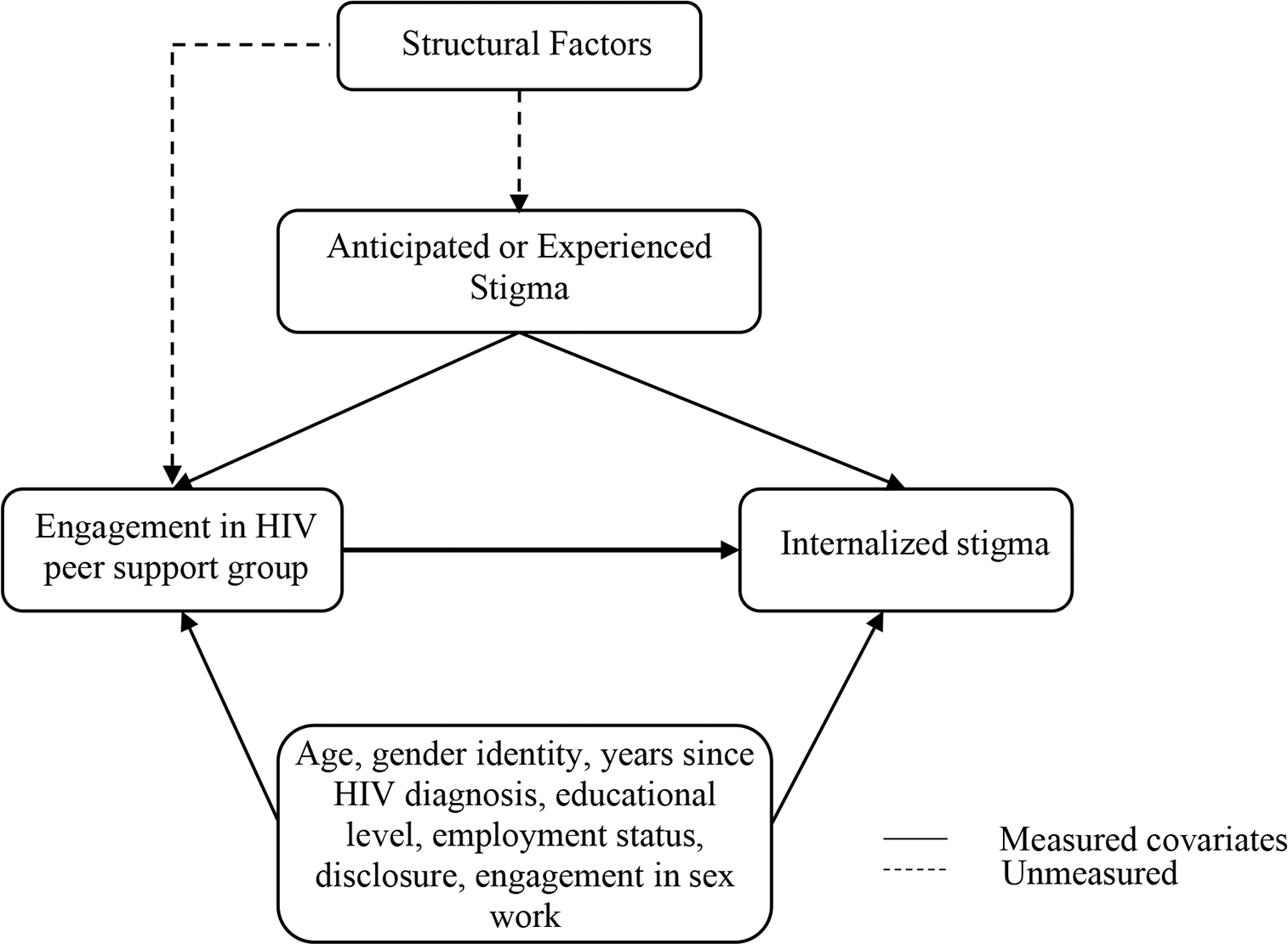
Conceptual model illustrating the hypothesized relationship between engagement in HIV peer support group and internalized stigma
Statistical Analyses
Participants’ sociodemographic and behavioral characteristics were stratified by engagement in HIV peer support groups and presented as frequencies and proportions. Multinomial logistic regression was used to model the association between primary exposure of interest and internalized stigma in univariate analysis. A multivariable multinomial logistic regression model adjusted for potential confounders of the relationship between engagement in HIV peer support groups and internalized stigma. Covariates included in the final model were age, educational level, duration since HIV diagnosis, employment status, disclosure status, and engagement in sex work.
To assess the presence of effect measure modification on the multiplicative scale, an interaction term was constructed between engagement in peer support and anticipated/experienced stigma and included in our final adjusted model. A likelihood ratio test was used to confirm if the added covariates (anticipated or experienced stigma and interaction term) in the extended model were required to explain the hypothesized relationship between engagement in peer support groups and internalized stigma. Effect measure modification by anticipated or experienced stigma was further examined in stratified analyses, comparing point estimates and 95% confidence intervals (95%CI) for the association between peer support and internalized stigma among participants who did and did not report anticipated/experienced stigma. Stata/BE version 17.0 (StataCorp LLC, College Station, TX) was used for all analyses.
Results
Participant Characteristics
There were 1,244 participants in this study (Table 1). Respondents had a median age of 38 years (Interquartile range; 30–45), with women making up more than half of the sample (63.3%; 788/1,244). The mean duration since HIV diagnosis was 8.6 years (standard deviation [SD] = 5.5). Most (81.4%; 1,012/1,244) of the study respondents reported having an educational level at or above secondary/high school. Over two-thirds (77.2%; 960/1,244) reported having part-time or full-time employment. One-fifth (20.5%; 255/1,244) reported engagement in sex work. More than half (66.5%; 827/1,244) had disclosed their HIV status to a family member, partners, or other community members. The majority (75.1%; 934/1,244) of respondents were engaged in HIV peer support groups. Over half (55.5%; 690/1244) and about one-fourth (27.3%; 343/1,244) demonstrated low/moderate and high levels of internalized stigma respectively, with a mean internalized stigma score of 2.44 (SD = 1.88).
Table 1.
Participant characteristics and engagement in HIV peer support groups
| Participant characteristicsa | Total (n = 1244) | HIV Peer Support Group |
|
|---|---|---|---|
| Not engaged (n = 310) | Engaged (n = 934) | ||
|
| |||
| Age, years (median [IQR]) | 38 (30–45) | 35 (28–43) | 39 (31–46) |
| Educational level | |||
| No Formal Education | 48 (3.9%) | 15 (4.8%) | 33 (3.5%) |
| Primary/Elementary | 140 (11.3%) | 35 (11.3%) | 105 (11.2%) |
| Secondary/High School | 563 (45.3%) | 152 (49.0%) | 411 (44.0%) |
| University/Tertiary | 449 (36.1%) | 97 (31.3%) | 352 (37.7%) |
| Trade/Vocational | 43 (3.5%) | 11 (3.5%) | 32 (3.4%) |
| Gender identity | |||
| Women | 788 (63.3%) | 186 (60.0%) | 602 (64.5%) |
| Men | 415 (33.4%) | 111 (35.8%) | 304 (32.5%) |
| Transgender | 19 (1.5%) | 6 (1.9%) | 13 (1.4%) |
| Other | 18 (1.4%) | 7 (2.3%) | 11 (1.2%) |
| Employment status | |||
| Employed Full-time | 444 (35.7%) | 121 (39.0%) | 323 (34.6%) |
| Employed Part-time | 516 (41.5%) | 100 (32.3%) | 416 (44.5%) |
| Retired/Pension | 20 (1.6%) | 7 (2.3%) | 13 (1.4%) |
| Unemployed | 265 (21.2%) | 82 (26.5%) | 182 (19.5%) |
| Years since HIV diagnosis (mean [SD]) | 8.6 (5.5%) | 6.1 (4.2%) | 9.4 (5.7%) |
| Engaged in sex work | 255 (20.5%) | 87 (28.1%) | 168 (18.0%) |
| Anticipated/Experienced stigma | 472 (37.9%) | 124 (40.0%) | 348 (37.3%) |
| Disclosure | 827 (66.5%) | 185 (59.7%) | 642 (68.7%) |
Variable distributions are reported as n (%) unless otherwise specified
Abbreviations: IQR, interquartile range; SD, standard deviations Categorical variables with missing values include gender identity (4/1244; 0.3%), educational level (1/1244; 0.1%), engagement in sex work (38/1244; 3%), disclosure (11/1244; 1%)
Among participants engaged in peer support groups, 65.9% (614/934) were women while 61.0% (192/318) were women among those not engaged. Men made up 34.1% (318/934) of those engaged in support groups and 39.0% (123/310) of those not engaged. Transgender people made up less than 1% of those engaged (0.6%; 6/934) and (1.0%; 3/310) of those not. About half of the PLHIV in support groups (44.5%; 416/934) reported having part-time employment. More than one third (39.0%; 121/310) of the PLHIV not engaged in a peer support group reported full-time employment. Educational levels did not differ greatly between PLHIV engaged in support groups and those who were not engaged. About one-third (28.1%; 87/310) of those engaged in sex work were not engaged in peer support groups and one-fifth (18.0%; 168/934) of sex workers were engaged in peer support groups.
Engagement in HIV peer Support Groups and Internalized Stigma
Engagement in HIV support groups was associated with internalized stigma in unadjusted analysis, with PLHIV who engaged in support groups less likely to report either low/moderate (odds ratio (OR): 0.45 [95% CI: 0.28 to 0.71]; p = 0.001) or high (OR: 0.26 [95% CI: 0.16 to 0.42]; p < 0.001) levels of internalized stigma relative to no stigma. Adjusted multivariable multinomial logistic regression revealed that PLHIV engaged in HIV support groups were less likely to report low/moderate (adjusted odds ratios (aOR): 0.47 [95% CI: 0.27 to 0.81]; p = 0.006) levels of internalized stigma than no stigma compared to those not engaged in peer support groups. Additionally, PLHIV engaged in HIV support groups were less likely to report high (aOR: 0.30 [95% CI: 0.17 to 0.53]; p < 0.001) levels of internalized stigma than no stigma compared to those not engaged in peer support groups (Table 2).
Table 2.
Adjusted odds ratios (aOR) comparing engagement in HIV support groups and internalized stigma scaled categories
| Low/moderate internalized stigma vs None |
High internalized stigma vs None |
|||||||
|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI | p-value | aOR | 95% CI | p-value | |||
|
| ||||||||
| HIV Peer Support Groups | Not engaged | Reference | - | Reference | - | |||
| Engaged | 0.47 | 0.27–0.81 | 0.006* | 0.30 | 0.17–0.53 | < 0.001* | ||
Odds ratios adjusted for age, educational level, duration of HIV diagnosis, gender identity, employment status, disclosure status, and engagement in sex work;
Significant p-values are < 0.05
Effect Measure Modification by Anticipated or Experienced Stigma
Engagement in HIV support groups was associated with low/moderate internalized stigma (aOR: 0.65 [95% CI: 0.26 to 1.67]; p = 0.359) and high internalized stigma (aOR: 0.35 [95% CI: 0.14 to 0.89]; p = 0.026) in the context of anticipated or experienced stigma. Overall, stratum specific estimates suggested that effect measure modification by anticipated or experienced stigma was not present (Table 3).
Table 3.
Effect measure modification by anticipated or experienced stigma
| Low/moderate internalized stigma vs. None |
High internalized stigma vs. None |
|||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | |||
|
| ||||||
| No anticipated or experienced stigma | HIV Peer Support Group | Not engaged | Reference | - | Reference | - |
| Engaged | 0.41* | 0.22–0.81 | 0.32* | 0.16–0.64 | ||
| Anticipated or experienced stigma present | HIV Peer Support Group | Not engaged | Reference | - | Reference | - |
| Engaged | 0.65 | 0.26–1.67 | 0.35* | 0.14–0.89 | ||
Measure of effect modification on multiplicative scale (interaction term): ratio of ORs (95% CI); low/moderate internalized stigma = 1.57 (0.50–4.95), p = 0.440; high internalized stigma = 1.13 (0.35–3.69), p = 0.835; Likelihood Ratio Test (LRT); Chi2 = 33.11; p = < 0.001;
Significant p-values are < 0.05
Discussion
This study explored the relationship of the engagement in peer support groups with internalized stigma among PLHIV in Nigeria. The findings from this study suggest that the majority of PLHIV are engaged in peer support groups, and that cisgender women make up a substantial proportion of those engaged. We also observed a high prevalence of internalized stigma and found that engagement in peer support groups was associated with lower levels of reported internalized stigma. The findings from this study further highlight that the association between peer support group engagement and internalized stigma may not vary based on whether an individual has also reported experienced or anticipated stigma.
Consistent with other studies from across sub-Saharan Africa, our study found a high prevalence of internalized stigma among PLHIV [23, 30, 31]. Specifically, the results of a systematic review reported a prevalence ranging between 26.9 and 66% using any indicator for internalized stigma across sub-Saharan Africa [26]. Prior studies across West Africa have also reported substantially higher prevalence of HIV-related stigma among key populations [32]. This finding may be attributed to the punitive legal landscape for people at substantial risk of HIV acquisition in this region. Importantly, the experiences of prejudice and discrimination among key populations in sub-Saharan Africa are often exacerbated by the stigma they face at the intersection of their HIV status and identities [31]. Moreover, various assessments have found that Nigeria’s current legislative landscape does not support a human rights-affirming HIV epidemic response [2]. This legal framework provides an enabling environment for increased marginalization and intersectional stigma among key populations. In recent years, there has been a decline in HIV-related stigma in Nigeria due to concerted efforts by various stakeholders through national policies [2]. Most programs developed as part of these national policies have focused on behavior change communication through mass media aimed at educating the populace about HIV. Notwithstanding the successes recorded, much still needs to be done to effectively address the high prevalence of internalized HIV-related stigma in Nigeria. The high prevalence of internalized stigma observed in our study possibly implies lack of effective multisectoral stigma mitigation efforts in Nigeria.
We characterized people in HIV support groups included in this study to determine better ways to improve support group engagement among all populations of PLHIV. Overall, there was a high proportion of PLHIV engaged in peer support groups, suggesting that peer-led interventions are acceptable among PLHIV. A majority of those engaged in peer support groups were middle-aged, female, and had been living with HIV longer than PLHIV who were not attending support groups. This finding supports existing data from sub-Saharan Africa showing older women have better engagement in HIV care compared to younger women [31–34]. Additionally, we found that disclosure of HIV status was significantly more common among those engaged in peer support groups compared to their counterparts. Individuals may be encouraged to disclose their status in part due to low rates of negative outcomes found in peer support groups [15, 35]. Furthermore, we saw that there was a lower proportion of sex workers engaged in peer support groups than those that were not engaged. This may be attributed to the intersectional stigmas that sex workers face, leading to distrust in health systems, thereby discouraging engagement with others [36]. Thus, understanding the role of peer support groups in determining disclosure of HIV status and the driving factors to engagement among middle-aged women with longer diagnosis may strengthen peer-led interventions. These findings also highlight the need to adapt peer-led interventions to accommodate the nuanced needs of the diverse populations of PLHIV in Nigeria, specifically among sex workers, younger women, and men newly diagnosed with HIV.
Maximizing social capital may prove to be a promising intervention considering scarce evidence-based system-level interventions to address internalized stigma among PLHIV [7, 37]. These analyses showed that PLHIV who are in an HIV support group had lower odds of internalized stigma compared to PLHIV who are not members of an HIV peer support group. As hypothesized, we expected that engagement in HIV peer support groups would improve social capital and consequently reduce the risk of internalized stigma among PLHIV. Using a reliable and validated measure of internalized stigma, we found that engagement in HIV peer support groups may have a potential role in reducing the risk of internalized HIV stigma among PLHIV in Nigeria. However, the role of peer support groups in stigma mitigation remains contentious in scientific literature. Although several studies have demonstrated the positive effects of peer support groups in stigma mitigation interventions, [37–42] contradicting evidence has also found no improvement in stigma observed among PLHIV because of their engagement in peer support groups [43]. The observed variability in the literature may be due to inconsistencies in tools used to measure HIV-related stigma. This conflicting evidence highlights the need for a universally acceptable, reliable, and valid measure of HIV-related stigma to enable policy advocates to accurately monitor progress made in HIV stigma elimination. The methods employed in this study attempt to address this by systematically measuring internalized HIV stigma and providing evidence that supports the potential role of peer support groups in reducing internalized stigma among PLHIV.
Addressing wider social and contextual factors that lead to anticipated and experienced stigma can be an important strategy in addressing internalized stigma among PLHIV [6]. In Nigeria, PLHIV experience sociocultural, economic, and structural barriers to care that often result from laws criminalizing same-sex practices and sex work. While we did not find statistical evidence of effect measure modification by anticipated or experienced stigma on the relationship between peer support group membership and internalized stigma, previous data have highlighted the importance of addressing social and structural factors when designing and developing stigma mitigation strategies [7]. We acknowledge that our findings may not reflect the complex nature of systemic issues faced by PLHIV in Nigeria as we did not directly capture the effects of structural factors in this study. However, if the barriers that exacerbate anticipated and experienced stigma are not addressed, internalized HIV stigma may not be eliminated.
There are key limitations to consider from our study. Firstly, causality cannot be ascertained between engagement in HIV peer support groups and internalized stigma from our cross-sectional study. Future research, such as longitudinal studies, may be needed to reinforce current evidence. Secondly, the recruitment methods used in the study were limited. Purposive and snowball sampling used in the study may have resulted in sampling bias that could have influenced our results. Thirdly, our study design was susceptible to recall bias and social desirability which may have affected the internal validity of our findings. Fourthly, we were limited by sample size to effectively assess effect measure modification which may explain why our association was not modified by anticipated or experienced stigma. Lastly, our measurement of peer support group engagement only involved membership in such groups. As such, key aspects related to engagement (e.g., frequency of engagement, length of membership, contents of peer group sessions) were not assessed. Previous studies have reported that membership alone may not be sufficient to mitigate stigma among PLHIV [41].
Conclusion
The findings from our study underscore the importance of adapting interventions to meet the needs of the diverse populations of PLHIV to ensure intervention engagement across all populations. Collectively, the results suggest that HIV-related stigma mitigation should be multilevel and multisectoral through the development and implementation of individual, community, and structural interventions.
HIV peer support groups have been shown to be an effective strategy used across HIV care programs to improve engagement in HIV care. Peer support groups can effectively increase social capital, reduce stigma, and promote healthy behavior change. Hence, these results suggest that promoting stigma mitigation strategies could enhance social capital as a means towards achieving the goal of universal treatment of people living with HIV in Nigeria.
Acknowledgements
We would like to extend our appreciation to the many stakeholders who provided critical oversight and were instrumental in the successful implementation of the Stigma Index 2.0 in Nigeria. Specifically, we would like to thank the Federal Ministry of Health in Nigeria, National Agency for the Control of AIDS, Family Health International 360 (FHI360), Society for Family Health, Global Network of People Living with HIV (GNP+), the International Community of Women Living with HIV (ICW), the US President’s Emergency Plan for AIDS Relief (PEPFAR), and the Joint United Nations Programme on HIV/AIDS (UNAIDS). We are incredibly grateful to the Network of People Living with HIV/AIDS in Nigeria (NEPWHAN) and KP secretariat – the principal investigators of the Stigma Index 2.0, for providing critical technical assistance in ensuring study coordination and implementation, including data collection. Above all, we want to thank the people living with HIV in Nigeria who informed this work by participating in the surveys, cognitive interviews, and focus group discussions. Finally, we would like to thank Lisa Lucas at the Johns Hopkins Center for Public Health and Human Right for her leadership in research coordination.
Funding
The PLHIV Stigma Index 2.0 in Nigeria was funded by the Global Fund to Fight AIDS, Tuberculosis, and Malaria, through the Global Fund-Nigeria HIV Grant to FHI360, also known as the National Aligned HIV/AIDS Initiative. KR was supported through the National Institute of Mental Health (NIMH) under award number K01MH129226. The research presented in this manuscript was made possible through a grant from NIMH under award number R01MH110358.
Footnotes
Competing Interests The authors declare that they have no conflicts of interest.
Ethical Approval Ethical review and approval were provided by the National Health Research Ethics Committee in Nigeria and the Johns Hopkins School of Public Health Institutional Review Board.
Consent to Participate Informed written consent was obtained from all individual participants included in the study.
Data Availability
The data that support the findings of this study are not publicly available. However, data from the PLHIV Stigma Index 2.0 may be made available upon reasonable request to GNP+.
References
- 1.Dahlui M, Azahar N, Bulgiba A, et al. HIV/AIDS related stigma and discrimination against PLWHA in Nigerian Population. PLoS ONE. 2015;10(12):e0143749. 10.1371/journal.pone.0143749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Odimegwu CO, Akinyemi JO, Alabi OO. HIV-Stigma in Nigeria: Review of Research Studies, policies, and Programmes. AIDS Res Treat. 2017;2017:5812650. 10.1155/2017/5812650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):67–S79. 10.1097/01.aids.0000327438.13291.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.PEPFAR. Nigeria Country Operational Plan (COP) 2021 Strategic Direction Summary www.state.gov: PEPFAR. 2022. [Available from: https://www.state.gov/where-we-work-pepfar/
- 5.Blake Helms C, Turan JM, Atkins G, et al. Interpersonal mechanisms contributing to the Association between HIV-Related internalized Stigma and Medication Adherence. AIDS Behav. 2017;21:238–47. 10.1007/s10461-016-1320-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turan B, Budhwani H, Fazeli PL, et al. How does Stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV Stigma in the effects of Perceived Community Stigma on Health and Psychosocial outcomes. AIDS Behav. 2017;21:283–91. 10.1007/s10461-016-1451-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pantelic M, Sprague L, Stangl AL. It’s not “all in your head”: critical knowledge gaps on internalized HIV stigma and a call for integrating social and structural conceptualizations. BMC Infect Dis. 2019;19(1). 10.1186/s12879-019-3704-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kimberly Adams Tufts. An Intersectional Perspective on Stigma as a Barrier to Effective HIV Self-Management and Treatment for HIV-Infected African American Women. HSOA Journal of AIDS Clinical Research and STDs. 2015(2):139 – 50. 10.24966/ACRS-7370/100005 [DOI] [Google Scholar]
- 9.Sangaramoorthy T, Jamison A, Dyer T. Intersectional stigma among midlife and older black women living with HIV. Cult Health Sex. 2017;19(12):1329–43. 10.1080/13691058.2017.1312530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ransome Y, Thurber KA, Swen M, Crawford ND, German D, Dean LT. Social capital and HIV/AIDS in the United States: knowledge, gaps, and future directions. SSM - Population Health. 2018;5:73–85. 10.1016/j.ssmph.2018.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Bank. Overview: Social Capital [available from https://web.worldbank.org/archive/website01360/WEB/0__CON-2.HTM]. Accessed 30 September 2022.
- 12.Kawachi I Social capital and community effects on population and individual health. Ann N Y Acad Sci. 1999;896:120–30. 10.1111/j.1749-6632.1999.tb08110.x [DOI] [PubMed] [Google Scholar]
- 13.Nahapiet J, Ghoshal S, Social Capital. Intellectual Capital, and the organizational advantage. Acad Manage Rev. 1998;23. 10.2307/259373 [DOI] [Google Scholar]
- 14.Anita BG, Phillip WG, Laura E et al. Peer Support as a Social Capital Strategy for Programs Serving Individuals Reentering from Incarceration and Survivors of Intimate Partner Violence or Human Sex Trafficking. Office of the Assistant Secretary for Planning and Evaluation (ASPE). 2022. https://aspe.hhs.gov/reports/peer-support-social-capital-development. Accessed 30 July 2022. [Google Scholar]
- 15.Bateganya MH, Amanyeiwe U, Roxo U, Dong M. Impact of support groups for people living with HIV on clinical outcomes: a systematic review of the literature. J Acquir Immune Defic Syndr. 2015;68(Suppl 3):368. 10.1097/QAI.0000000000000519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fannel CW, Moyo RA. Guidelines for establishing and operating successful support groups for people living with HIV. Catholic Relief Services. 2009. https://www.crs.org/our-work-overseas/research-publications/guidelines-establishing-and-operating-successful-support [Google Scholar]
- 17.Genberg BL, Shangani S, Sabatino K, et al. Improving Engagement in the HIV Care Cascade: a Systematic Review of Interventions Involving People Living with HIV/AIDS as Peers. AIDS Behav. 2016;20(10):2452–63. 10.1007/s10461-016-1307-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tobin KE, Heidari O, Winiker A, et al. Peer approaches to improve HIV Care Cascade outcomes: a scoping review focused on peer behavioral mechanisms. Curr HIV/AIDS Rep. 2022;19(4):251–64. 10.1007/s11904-022-00611-3 [DOI] [PubMed] [Google Scholar]
- 19.Ndori-Mharadze T, Fearon E, Busza J, Dirawo J, Musemburi S, Davey C, et al. Changes in engagement in HIV prevention and care services among female sex workers during intensified community mobilization in 3 sites in Zimbabwe, 2011 to 2015. J Int AIDS Soc. 2018;21(S5):e25138. 10.1002/jia2.25138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Øgård-Repål A, Berg RC, Fossum M. Peer support for people living with HIV: a scoping review. Health Promot Pract. 2023;24(1):172–90. 10.1177/15248399211049824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.About the Stigma Index. People Living with HIV Stigma Index Web site. https://www.stigmaindex.org/about-the-stigma-index/. Accessed 22 August 2022.
- 22.UNAIDS, The Paris D, Geneva. UNAIDS. [available at http://data.unaids.org/pub/externaldocument/2007/theparisdeclaration_en.pdf]. Accessed 22 August 2022. [Google Scholar]
- 23.UNAIDS. UNAIDS acts to strengthen ‘GIPA’ with new policy. [available at https://www.unaids.org/en/resources/presscentre/featurestories/2007/march/20070330gipapolicybrief]. Accessed 19 October 2022.
- 24.Friedland BA, Gottert A, Hows J, et al. The people living with HIV Stigma Index 2.0: generating critical evidence for change worldwide. AIDS. 2020;34. 10.1097/QAD.0000000000002602 [DOI] [PubMed] [Google Scholar]
- 25.Stigma Index. Country Reports. Nigeria People Living with HIV (PLHIV) Stigma Index 2.0 Report. 2021. [available at https://www.stigmaindex.org/wp-content/uploads/2022/04/Nigeria-SI-2.0-Report-2021.pdf] Accessed 25 October 2022. [Google Scholar]
- 26.Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the internalized AIDS-Related Stigma Scale. AIDS Care. 2009;21(1):87–93. 10.1080/09540120802032627 [DOI] [PubMed] [Google Scholar]
- 27.Geibel S, Gottert A, Friedland BA, et al. Internalized stigma among people living with HIV: assessing the internalized AIDS-Related Stigma Scale in four countries. AIDS. 2020;34:33. 10.1097/QAD.0000000000002649 [DOI] [PubMed] [Google Scholar]
- 28.DeFleur ML. Stigma: Notes on the Management of Spoiled Identity. By Erving Goffman. Englewood Cliffs, New Jersey: Prentice-Hall, 1963. 147 pp. Cloth, $4.50; paper, $1.95. Soc Forces. 1964;43(1):127–128. 10.1093/sf/43.1.127 [DOI] [Google Scholar]
- 29.Stevelink S, Wu IC, Voorend CGN, van Brakel WH. The psychometric assessment of internalised stigma instruments. Stigma Res Action. 2012;2(2):100–18. [Google Scholar]
- 30.Pantelic M, Shenderovich Y, Cluver L, Boyes M. Predictors of internalised HIV-related stigma: a systematic review of studies in sub-saharan Africa. Health Psychol Rev. 2015;9(4):469–90. 10.1080/17437199.2014.996243 [DOI] [PubMed] [Google Scholar]
- 31.Friedland BA, Sprague L, Nyblade L, Baral SD, Pulerwitz J, Gottert A, et al. Measuring intersecting stigma among key populations living with HIV: implementing the people living with HIV Stigma Index 2.0. J Int AIDS Soc. 2018;21(S5):e25131. 10.1002/jia2.25131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hodgson I, Plummer ML, Konopka SN, et al. A systematic review of individual and contextual factors affecting ART initiation, adherence, and retention for HIV-infected pregnant and postpartum women. PLoS ONE. 2014;9(11):e111421. 10.1371/journal.pone.0111421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chandy S, Heylen E, Ravikumar BN, Ekstrand ML. Examining engagement in care of women living with HIV in South India. Health Care Women Int. 2020;41(5):553–66. 10.1080/07399332.2019.1623799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rucinski KB, Schwartz SR, Mishra S, et al. J Acquir Immune Defic Syndr. 2020;85(2):148–55. 10.1097/QAI.0000000000002432. High HIV Prevalence and Low HIV-Service Engagement Among Young Women Who Sell Sex: A Pooled Analysis Across 9 Sub-Saharan African Countries. [DOI] [PubMed] [Google Scholar]
- 35.Maman S, Mbwambo JK, Hogan NM, Weiss E, Kilonzo GP, Sweat MD. High rates and positive outcomes of HIV-serostatus disclosure to sexual partners: reasons for cautious optimism from a voluntary counseling and testing clinic in Dar Es Salaam, Tanzania. AIDS Behav. 2003;7(4):373–82. 10.1023/B:AIBE.0000004729.89102.d4 [DOI] [PubMed] [Google Scholar]
- 36.Viswasam N, Schwartz S, Baral S. Characterizing the role of intersecting stigmas and sustained inequities in driving HIV syndemics across low-to-middle-income settings. Curr Opin HIV AIDS. 2020;15(4):243–9. 10.1097/COH.0000000000000630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16(3 Suppl 2):18734. 10.7448/IAS.16.3.18734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dunbar W, Labat A, Raccurt C, et al. A realist systematic review of stigma reduction interventions for HIV prevention and care continuum outcomes among men who have sex with men. Int J STD AIDS. 2020;31(8):712–23. 10.1177/0956462420924984 [DOI] [PubMed] [Google Scholar]
- 39.Garrido-Hernansaiz H, Alonso-Tapia J. Social Support in newly diagnosed people living with HIV: expectations and satisfaction along Time, Predictors, and Mental Health correlates. J Assoc Nurses AIDS Care. 2017;28(6):849–61. 10.1016/j.jana.2017.06.007 [DOI] [PubMed] [Google Scholar]
- 40.Neuman M, Obermeyer CM, MATCH Study Group. Experiences of stigma, discrimination, care and support among people living with HIV: a four country study. AIDS Behav. 2013;17(5):1796–808. 10.1007/s10461-013-0432-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mburu G, Ram M, Skovdal M, et al. Resisting and challenging stigma in Uganda: the role of support groups of people living with HIV. J Int AIDS Soc. 2013;16(3 Suppl 2):18636. 10.7448/IAS.16.3.18636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oosterhoff P, Anh NT, Yen PN, Wright P, Hardon A. Recreating kinship: coping options of HIV + AIDS widows in Vietnam. Health Care Women Int. 2010;31(1):17–36. 10.1080/07399330903133424 [DOI] [PubMed] [Google Scholar]
- 43.Van Tam V, Larsson M, Pharris A, et al. Peer support and improved quality of life among persons living with HIV on antiretroviral treatment: a randomised controlled trial from northeastern Vietnam. Health Qual Life Outcomes. 2012;10:53–3. 10.1186/1477-7525-10-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are not publicly available. However, data from the PLHIV Stigma Index 2.0 may be made available upon reasonable request to GNP+.


