Abstract
Background and purpose
Neurological disorders constitute a significant portion of the global disease burden, affecting >30% of the world's population. This prevalence poses a substantial threat to global health in the foreseeable future. A lack of awareness regarding this high burden of neurological diseases has led to their underrecognition, underappreciation, and insufficient funding. Establishing a strategic and comprehensive research agenda for brain‐related studies is a crucial step towards aligning research objectives among all pertinent stakeholders and fostering greater societal awareness.
Methods
A scoping literature review was undertaken by a working group from the European Academy of Neurology (EAN) to identify any existing research agendas relevant to neurology. Additionally, a specialized survey was conducted among all EAN scientific panels, including neurologists and patients, inquiring about their perspectives on the current research priorities and gaps in neurology.
Results
The review revealed the absence of a unified, overarching brain research agenda. Existing research agendas predominantly focus on specialized topics within neurology, resulting in an imbalance in the number of agendas across subspecialties. The survey indicated a prioritization of neurological disorders and research gaps.
Conclusions
Building upon the findings from the review and survey, key components for a strategic and comprehensive neurological research agenda in Europe were delineated. This research agenda serves as a valuable prioritization tool for neuroscientific researchers, as well as for clinicians, donors, and funding agencies in the field of neurology. It offers essential guidance for creating a roadmap for research and clinical advancement, ultimately leading to heightened awareness and reduced burden of neurological disorders.
Keywords: Europe, neurological disorders, research agenda, research gaps, research priorities
INTRODUCTION
Neurological disorders contribute massively and increasingly to the global burden of disease, with at least one in three people worldwide being diagnosed with a neurological disease, and this burden is increasing following the COVID‐19 pandemic [1]. The impact of neurological disorders on patients is staggering also in terms of years lost in disability (showing an increase of 15% in the past 30 years), premature death (increasing 39% in past 30 years) and high levels of stigma and discrimination [2]. Moreover, the costs of neurological disorders to health care systems and society are immense. In 2012, the total cost of disorders of the brain in Europe was estimated at €798 billion (equivalent to €1.037 billion in 2023), including direct costs (37% direct health care costs and 23% direct nonmedical costs) and indirect costs associated with production losses (40%) [3]. This equals the sum of the costs of all cardiovascular and oncological diseases taken together [4]. The level of awareness of this high burden of neurological diseases is still insufficient among health care professionals, academics, researchers, politicians, civil servants (in particular, ministries of health), industry, and the general public, which results in neurological care, neurological education, and the need for brain research being greatly undervalued and underfunded. Whereas the burden of neurological disorders is >30% of all disorders, the estimated funding level for neurological research is only 10% of the overall funding [5]. As a fundamental outcome of different national, international, and global awareness campaigns, neurological disorders have been identified as a global health imperative in a resolution of the World Health Assembly approved in 2022 by all the World Health Organization (WHO) Member States (WHO Intersectoral Global Action Plan for Epilepsy and Other Neurological Disorders [IGAP]) [6]. It is in the context of a well‐known lack of health professionals, of health structures, of the existing underfunding and the current momentum for increased attention to neurological disorders that there is a high need for a sharp research agenda for neurological and brain research. There are increasing efforts by many recognized institutions to set up research agendas, and this reflects their multifaceted importance. The aim of a research agenda is to identify research priorities to catalyse funds to support scientific efforts to eventually improve diagnosis and treatment for people with neurological disorders, improve their quality of life, and consequently reduce the burden of neurological disorders. Creating a research agenda also allows us to reflect on the past research, to detect the current gaps, and to define the most highly prioritized future research goals. It is known that research agendas can sometimes be biased by researcher or commercial interests, leading to a mismatch between the priorities of donors, of researchers, and of people with neurological disorders and their caregivers [7, 8]. As such, there is a growing acknowledgment of the need to engage patients with neurological disorders as partners in research and to direct funding of those areas deemed most essential by end users. By asking not only experts such as neurologists and basic/translational/clinical neuroscientists, but also people affected by neurological disorders and their family and caregivers about the most urgent research needs, patient involvement can be acquired, resulting in a truly patient‐centred vision on research priorities [9].
Research agendas often highlight the need for interdisciplinary research, broadening research possibilities. In addition, these agendas provide evidence for the necessity of increased funding and investments to maximize neuroscientific research and of developing new technologies for the realization of brain and neurological research in the context of identified priorities and epidemiological needs. Hence, in addition to providing research priorities, research agendas also serve as a framework to guide research funding agencies and sponsors in developing funding programmes [8].
In October 2022, the Shared Brain Research Agenda (SEBRA) was launched and made available to researchers and policymakers[9]. SEBRA was developed as a key deliverable of the European Brain Research Area (EBRA) project, funded under the European Union’s Horizon 2020 research and innovation framework programme (Grant Agreement number: 825348). The project was undertaken by a consortium of key organizations and EU‐ funded initiatives such as the EU Joint Programme on Neurodegenerative Diseases (JPND), ERA‐NET NEURON, and the Human Brain Project (HBP) and the European Brain Council. Its primary aim was to accelerate collaboration and coordination in brain research to support both brain health and scientific progress.
The SEBRA document covers preclinical to basic and translational neuroscience as well as psychiatry, child neurology and pharmacology and serves as a good starting point to establish a general brain research agenda. The document provides a detailed description of preclinical research needs to better understand how the healthy and pathological brain functions, but it is less detailed on means to fight the burden and improve the diagnosis and treatment of neurological disorders as well as on public health impact of neurological disorders. It therefore does not focus enough on prioritization of vitally important and necessary translational neurological advances.
In order to provide more focus on the specific research needs within neurology and to add specific clinical neurology priorities to SEBRA, while tailoring to the wide societal needs and better serving the needs of neurological patients and their families, a European Academy of Neurology (EAN) working group conducted a scoping literature review in order to identify any existing research agenda applicable to neurology to highlight the current unaddressed research questions. [Correction added on 01 February 2024 after first online publication: The preceding paragraph has been revised in this version.] EAN is active in research at different levels, with a recent emphasis on supporting education, international research collaborations, and implementing in its national Neurological Societies, the WHO IGAP and its own detailed Brain Health Strategy [10]. Following the review, a dedicated survey among the members of all EAN scientific panels (SPs), including residents, early career neurologists, and patient representatives, was performed, asking neurologists and patients about their views and perspectives on the current research priorities in terms of neurological diseases and related research gaps. An additional review by all EAN board members yielded additional input for the EAN SP survey. The literature review, in combination with the survey, forms the fundament for setting up a first comprehensive and specific neurological research agenda in Europe. It is intended as a priority‐setting exercise and provides an opportunity for researchers, funding agencies, and sponsors to align their research goals in neurology with the values and needs of the patient community. However, it should be noted that this study focuses specifically on gaps within neurological care and on the impact of neurological disorders at the level of public health determined mainly by clinicians and scientists as well as patient organizations and their representatives. This study does not aim to determine the epidemiological scale of the burden and economic costs of neurological diseases, as these are the topic of other scientific studies supported by EAN [11].
METHODS
Scoping review
To gain insight into the current neurological research agendas, we searched for existing literature via the PubMed, James Lind Alliance, and Embase databases, covering the years 2018 to the date of search (1 January 2023). The following search terms were used: “neurology” and “research” and “agenda” or “research agenda”, using the MeSH (Medical Subject Headings) terms and corresponding options in all databases. Articles that were included had to at least report on research agendas developed by a predefined expert panel and on methodology, covering any specific or general neurology topic. Papers from both international and national organizations, worldwide, were considered eligible. Only papers published in the English language were considered. Opinion papers, conference abstracts, papers without clear methodology and without predefined expert panels, and research agendas covering topics other than neurology (e.g., neuroscience) were excluded.
The initial screening of publications was done by the two first authors (P.B. and E.L.) independently; in the case of inconsistency, the final decision of inclusion of a paper was done following a discussion with a third author (K.A.). The following data were extracted from the eligible studies: title, reference number (PMID or other), subspecialty, database in which it was identified, authors, year of publication, country (if national) or the name of organization, and the main priorities identified.
Survey of the SPs
Following the scoping review, a qualitative approach was adopted, and a survey questionnaire was developed and discussed among the EAN board members before submission to the EAN SP members (Table 1). To collect the opinions of as many leading neurologists in Europe as possible, all members of the EAN SPs were invited to participate in the survey. They were asked to list the first three research priorities for the common and rare neurological diseases within and outside their subspecialty areas, and the main research gaps.
TABLE 1.
List of EAN scientific panels.
|
|
Abbreviations: ALS, amyotrophic lateral sclerosis; NMJ, neuromuscular junction.
Follow‐up survey
Based on the results of the first survey, a follow‐up survey was set up with the purpose of obtaining more details on the subtypes of the seven most highly prioritized common and rare neurological diseases. More detailed questions were asked regarding the current research gaps specifically related to these diseases. The follow‐up survey was completed by the co‐chairs of the relevant SPs representing all panel members. An additional meeting was set up including all EAN board members to review the gathered data and adding relevant input regarding disease prioritization and identification of gaps. The follow‐up survey was also sent to all patient representatives in the different SPs of EAN.
Organization of data and data cleaning
For the first survey, blank responses were deleted, diseases were checked for their correspondence to common or rare categories (using the orpha.net classification of rare diseases), and responses were reclassified between the gap section and disease categories as appropriate.
Given that the participants were asked to concentrate on diseases specific to the SP to which they belong, and taking in consideration the practical research applications of the survey results, the answers that were too broad to provide specific insight were deleted, which included the following answers: “neurodegenerative diseases”, “stroke” (if reported by a member of the stroke SP), “epilepsy” (if reported by a member of the epilepsy SP), “diseases of cognitive disability”, “dementia” (if reported by a member of the dementia SP), and “multiple sclerosis” or “multiple sclerosis therapy” (if reported by a member of the multiple sclerosis [MS] SP). In addition, the diagnostic procedures were deleted from disease categories.
Analysis of data
Descriptive statistics were used to analyse the responses of the participants in the first survey. The three main categorical variables (common neurological diseases, rare neurological diseases, research gaps) were categorized and, based on the frequency for each of the three priorities, the weighted mean value was calculated. Subsequently, the disease categories were ranked according to the frequency they were voted for. A similar approach was used to rank the gap categories. To examine whether the number of experts who voted from the corresponding disease panels influenced the final disease ranking (response bias), the responses of those panels were summed and the number was ranked from the highest to the lowest number of members who responded. We compared this ranking with the ranking of the diseases, using the Kendall coefficient of concordance [12].
RESULTS
Scoping review
The flowchart of the literature search is shown in Figure 1. Using the search strategy described previously, we identified 275 published papers in total. After removal of duplicates, 207 articles were screened by title and abstract, and 29 full‐text articles were assessed for eligibility. From those, we identified a total of 21 eligible publications that could be considered research agendas related to a range of neurological items and subspecialties [12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33]. The main reasons for exclusion in the title and abstract stage were the following: nonneurological topics, conference abstracts, informal or nonsystematic reviews, and opinion papers. In the full‐text stage, papers were excluded because no research priorities were included, the paper was a review, or the paper lacked proper identification of research priorities.
FIGURE 1.
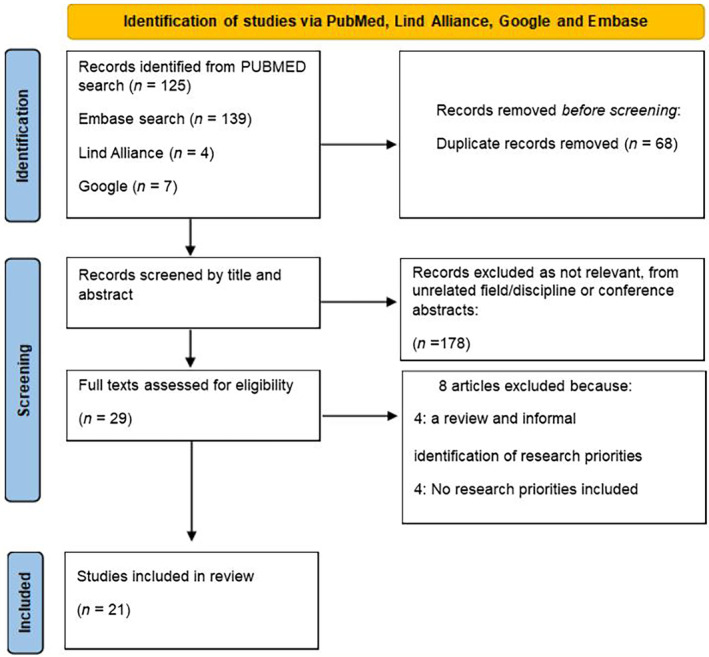
Prisma flowchart of the literature search results. PubMed example of the Medical Subject Headings (MeSH) terms used: (“neurology”[MeSH Terms] OR “neurology”[All Fields]) AND (((“research”[MeSH Terms] OR “research”[All Fields]) AND “agenda”[All Fields]) OR “research agenda”[All Fields]).
Not a single general, overarching research agenda covering different neurological diseases in different neurological subspecialties could be found in the literature search. In addition, the number of published agendas per subspecialty was highly variable. Stroke, MS, and neurodegenerative disorders are the subspecialties in which the highest number of articles outlining research agendas have been published. For other subspecialties such as headache, rare neurological disorders, and sleep disorders, no recent research agendas were found. Although there was a comprehensive sleep–wake disorder research agenda published in 2015 [13], this could not be included in the literature review, as it does not fulfil the inclusion criteria (years covered: 2018–2023), showing the importance of regularly updating research agendas. The currently available research agendas with their top three reported research priorities are summarized in Table 2. A more extensive version of this table can be found in the Supplementary Materials.
TABLE 2.
Currently available research agendas.
| Subspecialty | Publication | Country or (international) organization | Methods | Main findings |
|---|---|---|---|---|
| Stroke | Turner et al. [14] | United Kingdom | One‐day meeting with 11 stakeholders to gather and prioritize research gaps | Top 3 (out of 11) research priorities:
|
| Norrving et al. [15] |
Europe ESO in cooperation with the Stroke Alliance for Europe |
A steering committee guided 7 working groups (1 per domain). Per domain, 2 persons identified the research priorities. | Top 3 (out of 4) research goals:
|
|
| Stinear et al. [16] | Not specified | Literature review | Top 3 suggestions for stroke‐related clinical trial optimization:
|
|
| Hill et al. [17] |
United Kingdom Stroke Priority Setting Partnership Steering Group |
Two online surveys: 1 to identify research uncertainties, 1 to prioritize research uncertainties Online workshop |
Top 3 (out of 10) priorities related to prevention, diagnosis, and treatment:
Top 3 (out of 10) priorities related to rehabilitation and long‐term care:
|
|
| MS | Motl et al. [18] |
USA National Multiple Sclerosis Society |
Two 2‐day meetings on wellness in MS A focal literature review A wellness research group to set priorities |
Top 3 research questions related to:
Emotional wellness
Diet and nutrition
Exercise and physical activity
|
| Sumowski et al. [19] | US and European MS experts@ | Evaluation of the current state of the field by MS researchers and clinicians and identification of important practical and theoretical challenges |
Top 3 research priorities:
In understanding and measuring cognitive deficits
For neuroimaging investigations of cognitive deficits
For treatment and prevention of cognitive deficits
|
|
| Bebo et al. [20] | US National Multiple Sclerosis Society in collaboration with international MS organizations and committees |
Designing a roadmap together with the National Multiple Sclerosis Society's Scientific Advisory Committee, National Board of Directors, and the Pathways to Cures Task Force, composed of scientific thought leaders and people affected by MS A survey conducted in collaboration with the Accelerated Cure Project for Multiple Sclerosis |
Pathways to Cures Research Roadmap:
Stopping the MS disease process
Restoring lost function by reversing damage and symptoms
Ending MS through prevention
|
|
| Movement disorders | MacDuffie et al. [21] | USA | Online surveys | Top 3 research questions regarding stigma in FND:
|
| Gilbert et al. [22] |
USA Cerebral Palsy Research Network |
Development of a community‐drive research agenda together with clinicians, researchers, and the community | Top 3 (out of 10) priorities regarding dystonia in cerebral palsy:
|
|
| Neurodegenerative disorders | Schiess et al. [23] | Brain Health Unit at the World Health Organization | A multidisciplinary, sex‐balanced, international consultation workshop | Top 3 (out of 6) goals to address global disparities:
|
| De Miranda et al. [24] |
USA National Institute of Neurological Disorders and Stroke National Institute of Environmental Health Sciences |
Literature review |
Top 3 (out of 5) priorities related to PD prevention
Preclinical/basic
Clinical/translational
|
|
| Dams‐O'Connor et al. [25] |
USA National Institutes of Health |
An AD‐related dementias summit and follow‐up meetings | Top 3 (out of 4) research gaps related to TBI related to dementia:
|
|
| Martin et al. [26] | Europe | Literature review | Top 3 (out of 5) research gaps related to dementia:
|
|
| Epilepsy | Singh et al. [27] | Canada | Online surveys from stakeholders across Canada | Top 3 research priorities:
|
| Disorders of consciousness | Hocker et al. [28] | Neurocritical Care Research Network | In‐person meeting at the Fifth Neurocritical Care Research Network Conference | Top 3 research priorities regarding neurocritical care:
|
| Pain | Gatchel et al. [29] |
USA IPRCC and Office of Pain Policy at the National Institutes of Health |
Priority setting via interdisciplinary work groups | Top 3 research priorities:
|
| Child neurology | British Paediatric Neurology Association [30] |
United Kingdom British Paediatric Neurology Association |
Stakeholder questionnaire Information evaluation Second survey to rank priorities Stakeholder workshop to identify top 10 priorities |
Top 3 (out of 10) research priorities in child neurology:
|
| TBI | Hutchison et al. [31] |
Canada CTRC |
Development of a collaborative research group that integrated a multidisciplinary network of TBI researchers | Top 3 priorities:
|
| Neuroimaging in FND | Perez et al. [32] |
Worldwide International FND Neuroimaging Workgroup |
Literature review International FND Neuroimaging Workgroup meeting |
Top 3 (out of 10) research priorities:
|
| Aphasia | Ali et al. [33] |
Worldwide Collaboration of Aphasia Trialists |
Literature research Two‐day research agenda‐setting meeting |
Top 3 (out of 5) highly prioritized research themes in aphasia
|
| Myalgic encephalomyelitis/chronic fatigue syndrome | Tyson et al. [34] | United Kingdom | Online surveys and workshops | Top 3 (out of 10) research priorities:
|
Abbreviations: AD, Alzheimer disease; ADRD, AD and related dementias; CTRC, Canadian TBI Research Consortium; ESO, European Stroke Organization; FND, functional neurological disorder; IPRCC, Interagency Pain Research Coordinating Committee; MS, multiple sclerosis; PD, Parkinson disease; TBI, traumatic brain injury; TIA, transient ischaemic attack.
Survey of the SPs
The survey was completed by members of the EAN SPs, all including representatives of patient organizations. Responses were obtained from all SPs with at least two and up to 12 responses from each SP. In total, 221 of 1969 SP members completed the survey (182 individual SP members, 21 members of the management groups, and 18 SP co‐chairs), after a reminder was sent. Responses were classified according to 19 common and 15 rare neurological disease categories, and according to 12 research gap categories (Table 3). Responses that could not be assigned to one of the categories were added to the "unclassified" category.
TABLE 3.
Overview of (common/rare) neurological disease and gap categories.
| Common neurological disease categories | Rare neurological disease categories | Research gap categories |
|---|---|---|
|
|
|
Abbreviation: TBI, traumatic brain injury.
Figure 2 shows the distribution of categorized common neurological disorders indicated by the EAN SP members with corresponding weighted percentages. The chart shows a top seven (weighted percentage ≥ 5%) highly prioritized common neurological disorder categories, with neuroinflammatory and neuroimmunology disorders being the first (16%), followed by headache and pain (13%), Alzheimer disease (12%), stroke (12%), movement disorders (10%), epilepsy (7%), and sleep/wake disorders (5%). The response bias analysis showed no correlation between the number of SP members who voted from the respective SP and the order of the top seven priorities (Kendall tau = 0.52, z = 0.13), indicating that there was no preference of the panels with the highest number of voters. Other common neurological disorders, amongst others neuro‐oncological disorders, coma and disorders of consciousness, autonomic disease, neuropathies, and traumatic brain diseases, had a weighted percentage of <5%. An overview showing a more detailed priority setting of all common neurological disease groups can be found in Table S1.
FIGURE 2.
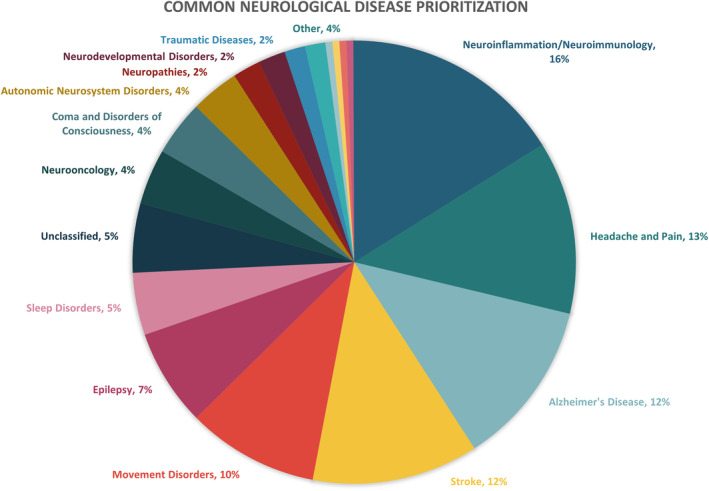
The distribution of categorized common neurological disorders.
Figure 3 shows the distribution of rare neurological disorder categories indicated by the EAN SP members with corresponding weighted percentages. The chart shows a top nine (weighted percentage ≥ 5%) highly prioritized rare neurological disorders, with rare neuroinflammatory/neuroimmunology disorders (25%) being the first, followed by rare movement disorders (14%), motor neuron diseases (10%), rare forms of dementia (9%), rare primary and secondary headaches (8%), rare vascular disorders (7%), rare developmental disorders with epilepsy as a major sign (6%), rare muscle disorders (5%), and rare neuropathies (5%). An overview showing a more detailed priority setting of all rare neurological disease groups can be found in Table S2. Again, the response bias analysis showed no correlation between the number of SP members who voted from the respective SP and the order of the top nine priorities (Kendall tau = 0.29, z = 0.45), indicating that there was no preference of the panels with the highest number of voters.
FIGURE 3.
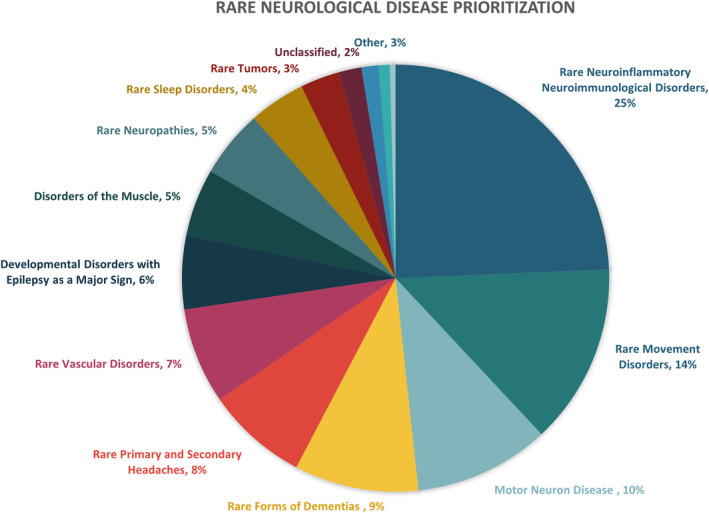
The distribution of rare neurological disorder categories.
Figure 4 shows the prioritization of current research gaps. The top six research gaps were the following: improving treatment (weighted mean = 31%), better understanding of underlying disease mechanisms (21%), improving diagnostic procedures (17%), improving outcome and prediction of outcome (8%), improving international collaboration and establishment of big datasets (6%), and prevention (5%). An overview showing a more detailed priority setting of all research gap categories can be found in Table S3.
FIGURE 4.
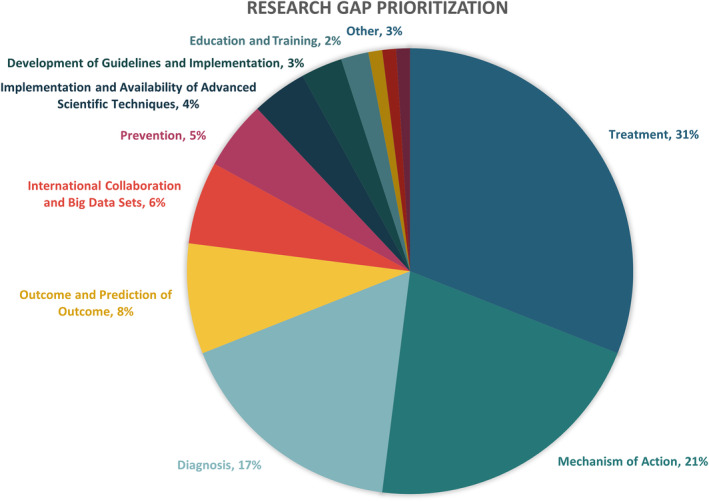
The prioritization of current research gaps.
Follow‐up survey of the panel co‐chairs, patient representatives, and board members
Based on the outcomes of the first survey, the following EAN SP chairs were asked to respond to the follow‐up survey: movement disorders, infectious diseases, amyotrophic lateral sclerosis and frontotemporal dementia, neuroimmunology, stroke, epilepsy, dementia and cognitive disorders, headache, MS, and sleep/wake disorders. This selection of SPs was based on their affinity with the top seven common neurological disorders identified in the first survey. Rare neurological disorders were identified as a separate priority category. Additionally, all EAN board members provided comments and input on their priorities regarding the different neurological disease groups and overarching research priorities not specifically associated with one particular disease group. To maximally include the patient voice, the follow‐up survey was also sent to all patient representatives in the EAN SPs.
Descriptive results of this follow‐up survey with responses of the co‐chairs are summarized in Table 4. Each panel indicated a top three prioritization of disease subtypes and research gaps related to the neurological disease relevant to their panel. A striking overlap between the indicated gap priorities of the first and second survey was found. In the second survey, nine of 24 (37.5%) gap priorities were related to investigating disease mechanisms, five of 24 (20.8%) to development of more targeted treatments, and four of 24 (16.7%) to improving diagnostic procedures. All three categories also belong to the top three identified gap priorities identified in the first survey (Figure 4), showing an alignment between the panel members and co‐chairs of the SPs. Additional research gaps and further details on previously mentioned gaps were provided by board members (Table 4). In Table 5, the responses of the patient representatives, including members of the European Federation of Neurological Associations, are summarized.
TABLE 4.
Top seven neurological disease groups, prioritization of subtypes of diseases, and research‐identified common NDs, according to the panel cochairs and board members.
| Disease group | Top 3 NDs | Top 3 research gaps | Detailed input given by the EAN board |
|---|---|---|---|
| Neuroinfections |
|
|
|
| Neuroimmunological diseases |
|
|
|
| MS |
|
|
|
| Headache/pain |
|
|
|
| AD and dementias |
|
|
|
| Stroke |
|
|
|
| Movement disorders |
|
|
|
| Epilepsy |
|
|
|
| SWDs |
|
|
|
| Rare NDs |
|
||
| Overarching research priorities, not specifically associated with disease groups |
|
Abbreviations: AD, Alzheimer disease; AIDS, acquired immunodeficiency syndrome; CNS, central nervous system; EAN, European Academy of Neurology; HIV, human immunodeficiency virus; MS, multiple sclerosis; ND, neurological disorders; NICU, neonatal intensive care unit; SWD, sleep–wake disorder.
TABLE 5.
Top three diseases and research gaps according to the patient representatives.
| Panel | Society | Top 3 diseases | Top 3 gaps |
|---|---|---|---|
| Movement disorders | Dystonia Europe |
|
|
| Parkinson's Europe |
|
|
|
| Headache | The migraine movement |
|
|
| Pain | EFNA |
|
|
| Sleep–wake disorders | EFNA |
|
|
| Palliative care | EFNA |
|
|
Abbreviation: EFNA, European Federation of Neurological Associations.
DISCUSSION AND CONCLUSIONS
The main aim of this paper was to design a research agenda tailored to the needs of neurologists, neurological patients, and relevant stakeholders. The paper is composed of a quantitative (literature review) and a qualitative part (surveys) able to provide clear indications and targets.
The aim of the literature review was to screen the current research agendas in the field of neurology and to summarize the reported gaps per subspecialty. This review showed that the currently available agendas are mostly focused on one specific subspecialty, and that no general and comprehensive neurological research agenda, covering different neurological diseases in different subspecialties, exists to date. The lack of such a general neurological research agenda hampers gaining consensus on priority‐setting across neurological disorders and related research gaps. Moreover, the absence of a generally shared and accepted neurological research agenda prevents providing effective guidance to research funding agencies, sponsors, and policymakers on how to better spend existing funding and possibly prioritize increased funding. Furthermore, a clear skewness in the number of published agendas across subspecialties has been detected. No agendas for rare neurological disorders were found. Even within the published agendas, there is a clear difference in number of agendas per subspecialty, with stroke and neurodegenerative disorders being the best covered subspecialties.
Subsequently, we endeavoured to set up a comprehensive neurological research agenda covering all subspecialties, adding a qualitative part to our research. To achieve this, a first survey was sent to all EAN SPs to identify the most highly prioritized neurological disorders and research gaps. Results showed that the top seven prioritized common neurological disorder categories are: neuroinflammatory/neuroimmunological disorders, headache and pain, Alzheimer disease, stroke, movement disorders, epilepsy, and sleep/wake disorders. According to all relevant stakeholders, ranging from experts in the field to patients, these neurological diseases are to be researched with the highest priority. According to the literature review, stroke, MS, and movement disorders have already received high levels of attention in the existing subspecialty literature. This suggests that headache and pain, Alzheimer disease, epilepsy, and sleep/wake disorders are neurological diseases that need to be researched with the highest priority. Equally important is to include rare neurological disorders in future research agendas and to identify prioritization among these disorders. This will increase the awareness of rare neurological diseases and the need to research underlying disease mechanisms to develop new treatments, as these diseases are often underrepresented in previous research agendas. A focus on investigating the nine main rare neurological disorders in this agenda is definitely an important first step, but the research focus should reach beyond these nine disorders.
Prioritizing research into specific neurological disorders, however, was not considered enough, as it is highly relevant to also identify the main research priorities beyond specific neurological diseases and to tackle existing research gaps. The survey revealed that the top six global research gap categories for neurology are, in ranking order: improving treatment options, improving the understanding of underlying disease mechanisms, improving diagnostic procedures, improving outcome and prediction of outcome, improving international collaboration and establishment of big datasets, and prevention. It is noteworthy that prevention is included in this list of top research priorities covering needs and gaps, as there is now rising interest in brain health and increased understanding of preventive measures for neurological disorders.
For the European neurological community, it seems clear that more research is needed to explore and develop new treatment options, especially for people suffering from the most highly prioritized diseases. Remarkably, investigating the underlying mechanism of neurological disorders was identified as the second most prioritized research need, showing that for neurologists, who mostly have a clinically oriented background and training, it is important to have a translational and multimodal approach to neurology. Our findings confirm that mechanistic and preclinical research is deemed relevant to understand the neurobiological and neurophysiological underpinnings of neurological disorders. The full understanding of these diseases from bench to bedside can lead to more precise and effective prevention, diagnosis, and treatment, in particular precision and personalized medicine.
To further examine the specific research questions related to the top seven common neurological disorders identified by this first survey, a follow‐up survey was sent to the EAN SP co‐chairs and patient representatives related to each category of this top seven. The results represent the most relevant subtypes of one of these top seven disorders and the corresponding gaps. Remarkably, there was a clear overlap between the top three gap categories identified by the first survey and the research gaps indicated by the SP co‐chairs. The validity of the top seven list was again confirmed by the members of the EAN board, and some additional research gaps and more detailed research topics (both disease‐specific and overarching) were listed, adding to a higher level of granularity of the present research agenda. Table 4 may serve as a formal shortlist of current clinically relevant research topics validated by a large number of representative clinicians, patients, clinical researchers, and leaders in European neurology. Table 5 shows in more detail patients organizations' research priorities that have been considered and listed so as to empower global results of the EAN research agenda. Remarkably, (lack of) education and training are the most frequently reported gaps by patient representatives, which is quite different from the results on gap prioritization of the first survey (Figure 4). This shows the importance of sharing and discussing research goals between all relevant stakeholders as well as incorporating patients' opinions, as this leads to new important insights.
The relevance of the present EAN strategic research agenda compared to SEBRA is clear‐cut. It truly is the first neurological research agenda to comprehensively cover all gaps and needs, to clearly suggest detailed research priorities, formulated and validated by a representative sample of the neurological community consisting of clinicians, clinical scientists, and patient representatives.
The present research agenda also has clear limitations. The methodology of administering surveys can only be expected to yield qualitative rather than quantitative outcomes. Although no response bias was detected and answers were obtained from all SPs, the surveys were only completed by part of all EAN SP members, which may limit the representativeness of our sample. Despite the inclusiveness of the panels in terms of age and gender and the representation of patients, we must be aware of bias that could be present due to the difference in response rate among different SPs. Societally relevant issues such as attention to sustainability and environmental factors relevant to neurological disorders were not specifically addressed in the present research agenda. It is noteworthy that non‐disease‐related gaps and needs have been considered but not listed by SP members, as questionnaires were mainly disease‐oriented; however, SP chairs and EAN board members, in line with recent publications, white papers, and roadmaps relevant to these issues [35, 36], have clearly labelled diversity, equity, and inclusion as well as environmental and climate change‐related research as high priorities.
It is also important to note that although patients are represented in most of the SPs, the majority of members of such panels and respondents to the survey were clinicians or clinician scientists. To counteract this and to maximally incorporate the patient voice in this agenda, the follow‐up survey was sent directly to all patient representatives of the EAN SPs, and a patient and advocate for patient inclusion in research co‐authored the manuscript. We truly believe that setting up a research agenda is an interactive process, in which this agenda can serve as a fundament. Additional steps will be needed to achieve an exclusively patient‐centred agenda in the future.
To our knowledge, this work is the first European global neurological research agenda identifying research priorities across neurological subspecialties. In addition to existing partial research agendas, the present EAN neurological research agenda can serve as a clinically and societally relevant roadmap for donors, funding agencies, researchers, and clinicians in the field of neurology. It will also help clinicians to align their research goals with the values and needs of the patient community. Researchers, clinicians, policymakers, patients, and other interested stakeholders should consider implementing this agenda when interacting with agencies involved in supporting brain and neurological research as well as when dealing with efforts to reduce the burden of neurological disorders in Europe. It is our firm belief that implementing this research agenda should eventually lead to closing the funding gap for neurological research and thus contributing to reduce the global burden of neurological disorders. Research has no borders.
AUTHOR CONTRIBUTIONS
Paul Boon: Conceptualization; investigation; writing – original draft; writing – review and editing; project administration; supervision; data curation; validation; resources; methodology. Emma Lescrauwaet: Project administration; methodology; writing – original draft; writing – review and editing; investigation; validation; resources; data curation; visualization; conceptualization; formal analysis. Katina Aleksovska: Investigation; visualization; writing – original draft; writing – review and editing; formal analysis; data curation; methodology; conceptualization. Maria Konti: Writing – original draft; visualization; formal analysis; data curation; methodology; investigation; writing – review and editing; conceptualization. Thomas Berger: Writing – review and editing; conceptualization. Matilde Leonardi: Writing – review and editing; conceptualization. Tony Marson: Writing – review and editing; conceptualization. Ulf Kallweit: Conceptualization; writing – review and editing. Elena Moro: Writing – review and editing; conceptualization. Antonio Toscano: Writing – review and editing; conceptualization. Irena Rektorova: Writing – review and editing; conceptualization. Michael Crean: Writing – review and editing; supervision; project administration; methodology; conceptualization; investigation; writing – original draft; validation; resources. Anja Sander: Writing – review and editing; conceptualization. Robert Joyce: Writing – review and editing. Claudio Bassetti: Conceptualization; writing – review and editing.
FUNDING INFORMATION
No external funding was acquired to support this study. The EAN and the EAN head office supported the practical management of this study.
CONFLICT OF INTEREST STATEMENT
All authors state explicitly that there is no conflict of interest to disclose in connection to this article.
Supporting information
DATA S1
TABLES S1–S3
TABLE S4
Boon P, Lescrauwaet E, Aleksovska K, et al. A strategic neurological research agenda for Europe: Towards clinically relevant and patient‐centred neurological research priorities. Eur J Neurol. 2024;31:e16171. doi: 10.1111/ene.16171
Paul Boon and Emma Lescrauwaet share first authorship; Paul Boon and Emma Lescrauwaet share contributed equally to the manuscript.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Xu E, Xie Y, Al‐Aly Z. Long‐term neurologic outcomes of COVID‐19. Nat Med. 2022;28(11):2406‐2415. doi: 10.1038/s41591-022-02001-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Feigin VL, Vos T, Nichols E, et al. The global burden of neurological disorders: translating evidence into policy. Lancet Neurol. 2020;19(3):255‐265. doi: 10.1016/S1474-4422(19)30411-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gustavsson A, Svensson M, Jacobi F, et al. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(10):718‐779. doi: 10.1016/j.euroneuro.2011.08.008 [DOI] [PubMed] [Google Scholar]
- 4. The Economist Impact . The value of action: mitigating the global impact of neurological disorders. 2022.
- 5. Chinthapilli K. Brain disorders cost the most overall but attract the least research funding. BMJ. 2013;347:f4766. [DOI] [PubMed] [Google Scholar]
- 6. World Health Assembly . Intersectoral global action plan on epilepsy and other neurological disorders. 2021.
- 7. Gudowsky N. Limits and benefits of participatory agenda setting for research and innovation. Eur J Futures Res. 2021;9(1):8. doi: 10.1186/s40309-021-00177-0 [DOI] [Google Scholar]
- 8. Crowe S, Fenton M, Hall M, Cowan K, Chalmers I. Patients', clinicians' and the research communities' priorities for treatment research: there is an important mismatch. Res Involv Engagem. 2015;1(1):2. doi: 10.1186/s40900-015-0003-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. The Shared European Brain Research Agenda . The European brain research area. https://www.ebra.eu/sebra/. Accessed June 1, 2023.
- 10. Bassetti CLA, Endres M, Sander A, et al. The European Academy of Neurology Brain Health Strategy: one brain, one life, one approach. Eur J Neurol. 2022;29(9):2559‐2566. doi: 10.1111/ene.15391 [DOI] [PubMed] [Google Scholar]
- 11. Deuschl G, Beghi E, Fazekas F, et al. The burden of neurological diseases in Europe: an analysis for the Global Burden of Disease Study 2017. Lancet Public Health. 2020;5(10):e551‐e567. doi: 10.1016/S2468-2667(20)30190-0 [DOI] [PubMed] [Google Scholar]
- 12. Field AP. Kendall's coefficient of concordance. In: Balakrishnan N, Colton T, Everitt B, Piegorsch W, Ruggeri F, & Teugels J, eds. Wiley StatsRef: Statistics Reference Online. John Wiley & Sons, Ltd; 2014. doi: 10.1002/9781118445112.stat06537 [DOI] [Google Scholar]
- 13. Bassetti CL, Ferini‐Strambi L, Brown S, et al. Neurology and psychiatry: waking up to opportunities of sleep.: State of the art and clinical/research priorities for the next decade. Eur J Neurol. 2015;22(10):1337‐1354. doi: 10.1111/ene.12781 [DOI] [PubMed] [Google Scholar]
- 14. Turner GM, Backman R, McMullan C, Mathers J, Marshall T, Calvert M. Establishing research priorities relating to the long‐term impact of TIA and minor stroke through stakeholder‐centred consensus. Res Involv Engagem. 2018;4:2. doi: 10.1186/s40900-018-0089-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Norrving B, Barrick J, Davalos A, et al. Action plan for stroke in Europe 2018–2030. Eur Stroke J. 2018;3(4):309‐336. doi: 10.1177/2396987318808719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stinear CM, Lang CE, Zeiler S, Byblow WD. Advances and challenges in stroke rehabilitation. Lancet Neurol. 2020;19(4):348‐360. doi: 10.1016/S1474-4422(19)30415-6 [DOI] [PubMed] [Google Scholar]
- 17. Hill G, Regan S, Francis R, et al. Research priorities to improve stroke outcomes. Lancet Neurol. 2022;21(4):312‐313. doi: 10.1016/S1474-4422(22)00044-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Motl RW, Mowry EM, Ehde DM, et al. Wellness and multiple sclerosis: the National MS Society establishes a Wellness Research Working Group and research priorities. Mult Scler. 2018;24(3):262‐267. doi: 10.1177/1352458516687404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sumowski JF, Benedict R, Enzinger C, et al. Cognition in multiple sclerosis: state of the field and priorities for the future. Neurology. 2018;90(6):278‐288. doi: 10.1212/WNL.0000000000004977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bebo BF, Allegretta M, Landsman D, et al. Pathways to cures for multiple sclerosis: a research roadmap. Mult Scler. 2022;28(3):331‐345. doi: 10.1177/13524585221075990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. MacDuffie KE, Grubbs L, Best T, et al. Stigma and functional neurological disorder: a research agenda targeting the clinical encounter. CNS Spectr. 2020;1‐6. doi: 10.1017/S1092852920002084 [DOI] [PubMed] [Google Scholar]
- 22. Gilbert LA, Fehlings DL, Gross P, et al. Top 10 research themes for dystonia in cerebral palsy: a community‐driven research agenda. Neurology. 2022;99(6):237‐245. doi: 10.1212/WNL.0000000000200911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schiess N, Cataldi R, Okun MS, et al. Six action steps to address global disparities in Parkinson disease: a World Health Organization priority. JAMA Neurol. 2022;79(9):929‐936. doi: 10.1001/jamaneurol.2022.1783 [DOI] [PubMed] [Google Scholar]
- 24. De Miranda B, Goldman S, Miller G, Greenamyre J, Dorsey E. Preventing Parkinson's disease: an environmental agenda. J Parkinsons Dis. 2021;12:1‐24. doi: 10.3233/JPD-212922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dams‐O'Connor K, Bellgowan PSF, Corriveau R, et al. Alzheimer's disease‐related dementias summit 2019: National Research Priorities for the investigation of traumatic brain injury as a risk factor for Alzheimer's disease and related dementias. J Neurotrauma. 2021;38(23):3186‐3194. doi: 10.1089/neu.2021.0216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Martin A, O'Connor S, Jackson C. A scoping review of gaps and priorities in dementia care in Europe. Dementia. 2020;19(7):2135‐2151. doi: 10.1177/1471301218816250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Singh A, Woelfle R, Chepesiuk R, et al. Canadian epilepsy priority‐setting partnership: toward a new national research agenda. Epilepsy Behav. 2022;130:108673. doi: 10.1016/j.yebeh.2022.108673 [DOI] [PubMed] [Google Scholar]
- 28. Hocker S, Shah S, Vespa P, et al. The future of neurocritical care research: proceedings and recommendations from the Fifth Neurocritical Care Research Network Conference. Neurocrit Care. 2020;32(1):311‐316. doi: 10.1007/s12028-019-00767-8 [DOI] [PubMed] [Google Scholar]
- 29. Gatchel RJ, Reuben DB, Dagenais S, et al. Research agenda for the prevention of pain and its impact: report of the work group on the prevention of acute and chronic pain of the Federal Pain Research Strategy. J Pain. 2018;19(8):837‐851. doi: 10.1016/j.jpain.2018.02.015 [DOI] [PubMed] [Google Scholar]
- 30. British Paediatric Neurology Association . Childhood neurological conditions | James Lind Alliance. 2022. Accessed February 8, 2023. https://www.jla.nihr.ac.uk/priority‐setting‐partnerships/childhood‐neurological‐conditions/
- 31. Hutchison JS, Emery C, Gagnon I, et al. The Canadian Traumatic Brain Injury Research Consortium: epitomizing collaborative research in Canada. J Neurotrauma. 2018;35(16):1858‐1863. doi: 10.1089/neu.2018.5871 [DOI] [PubMed] [Google Scholar]
- 32. Perez DL, Nicholson TR, Asadi‐Pooya AA, et al. Neuroimaging in functional neurological disorder: state of the field and research agenda. Neuroimage Clin. 2021;30:102623. doi: 10.1016/j.nicl.2021.102623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ali M, Soroli E, Jesus LMT, et al. An aphasia research agenda – a consensus statement from the collaboration of aphasia trialists. Aphasiology. 2022;36(4):555‐574. doi: 10.1080/02687038.2021.1957081 [DOI] [Google Scholar]
- 34. Tyson S, Stanley K, Gronlund TA, et al. Research priorities for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): the results of a James Lind alliance priority setting exercise. Fatigue. 2022;10(4):200‐211. doi: 10.1080/21641846.2022.2124775 [DOI] [Google Scholar]
- 35. Sex, gender, and the cost of neurological disorders, towards an inclusive research agenda. Lancet Neurol. 2023;22:367. [DOI] [PubMed] [Google Scholar]
- 36. Rukovets O. A scoping review: what effects do climate change and air pollution have on neurologic disorders? Neurol Today. 2022;22(24):7. doi: 10.1097/01.nt.0000905788.76255.4d [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
DATA S1
TABLES S1–S3
TABLE S4
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


