Abstract
Background and purpose
The etiological distribution of oculomotor nerve palsy has varied amongst the studies. This study aimed to define the clinical features and underlying etiologies of isolated oculomotor nerve palsy by recruiting patients from all departments in a referral‐based university hospital.
Methods
The medical records of 672 patients who had a confirmed diagnosis of isolated oculomotor nerve palsy at all departments of Seoul National University Bundang Hospital, Seongnam, South Korea, from 2003 to 2020 were reviewed. A proportion of the etiology of isolated oculomotor nerve palsy was also compared with that of patients pooled from the previous studies that were searched on PubMed in May 2022.
Results
The most common etiology was microvascular (n = 168, 26.5%), followed by vascular anomalies (n = 110, 17.4%), neoplastic (n = 86, 13.6%), inflammatory (n = 79, 12.5%), idiopathic (n = 60, 9.5%) and traumatic (n = 53, 8.4%). Neurologists were mainly involved in the management of microvascular and inflammatory oculomotor nerve palsies whilst ophthalmologists mainly participated in the care of idiopathic, neoplastic and traumatic palsies. Neurosurgeons mostly took care of oculomotor nerve palsy due to vascular anomalies.
Conclusions
The proportion of etiologies of isolated oculomotor nerve palsy may differ according to the specialties involved in the management. The results of previous studies on the etiological distribution of isolated oculomotor nerve palsy should be interpreted with this consideration.
Keywords: diplopia, double vision, etiology, oculomotor nerve palsy
INTRODUCTION
Third cranial nerve (oculomotor nerve) palsy is one of the most common causes of ophthalmoplegia and may indicate benign to life‐threatening causes [1, 2, 3]. The incidence of acquired oculomotor nerve palsy increases with age and peaks in the 70s and 90s age groups with an annual incidence at 3.71–4.0 per 100,000 [3, 4]. Even though microvascular, traumatic and intracranial aneurysms are the most common causes of oculomotor nerve palsy [3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16], the proportion of etiology has been different amongst studies depending on the study population and the department where the recruitment of patients was performed [3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16]. Previous studies were primarily undertaken in referral‐based neuro‐ophthalmological clinics run exclusively by ophthalmologists or neurologists, which would have resulted in a referral bias. Even though our hospital has neuro‐ophthalmological clinics run by ophthalmologists and neurologists independently but in close cooperation and consultation, it was previously found that only 37.9% of the patients with binocular diplopia as the primary symptom were managed by both neurologists and ophthalmologists in our institution [17]. Furthermore, the etiological proportion of diplopia, trochlear palsy and abducens nerve palsy significantly differed between the clinics [17, 18, 19].
This study aimed to establish the clinical features and underlying etiologies of isolated oculomotor nerve palsy by recruiting patients from all departments for an 18‐year period in a referral‐based university hospital in the Republic of Korea. The etiological distribution of isolated oculomotor palsy in the current study was also compared with that of pooled results from previous reports.
METHODS
Subjects
This study was based on 672 consecutive patients who had a confirmed diagnosis of isolated oculomotor nerve palsy in Seoul National University Bundang Hospital, Seongnam, Republic of Korea, from 2003 to 2020 (Figure 1). The data on diagnoses and clinical features were acquired using electronic medical records. The search terms adopted for screening of oculomotor nerve palsy on the electronic medical records included diplopia, strabismus, oculomotor nerve palsy, third cranial nerve palsy, oculomotor nerve aplasia, third cranial nerve aplasia, injury of oculomotor nerve and injury of third cranial nerve.
FIGURE 1.
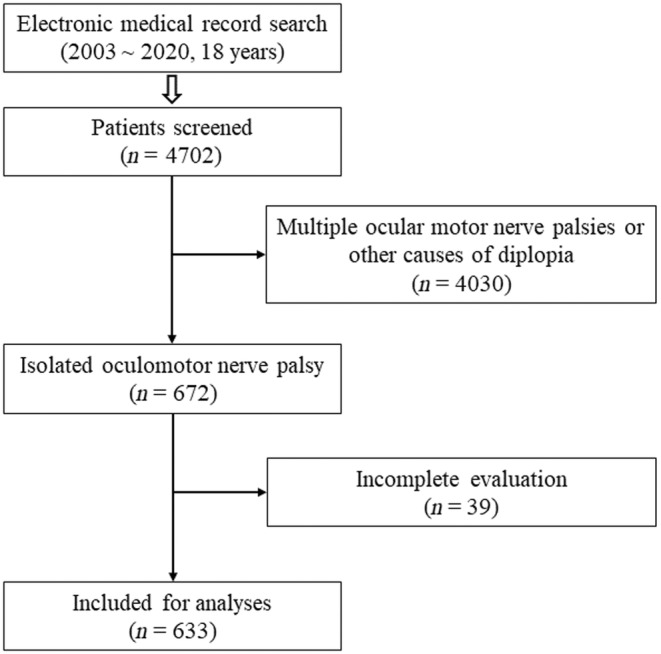
The flow diagram for subjects of the study.
The diagnosis of oculomotor palsy was based on the weakness of the extraocular muscles innervated by the oculomotor nerve with or without a pupillary involvement [2]. Isolated oculomotor nerve palsy was diagnosed when the patients had no other neurological symptoms and signs except headache or periorbital pain associated with the diplopia. Particular attention was paid to exclude disorders that may mimic oculomotor nerve palsy, such as exotropia, blepharoptosis, congenital ptosis, anisocoria of other causes (e.g., physiological anisocoria, Horner's syndrome, Adie's tonic pupil), thyroid‐associated orbitopathy, orbital wall fracture, orbital myositis, myasthenia gravis, childhood exotropia, congenital exotropia and Duane syndrome. The investigation was subjected to the clinical features and suspected etiology of isolated oculomotor nerve palsy even though most patients had complete blood counts with erythrocyte sedimentation rate, routine chemistry and serology for inflammation (C‐reactive protein, rheumatoid factor, antinuclear antibody, anti‐double‐stranded deoxyribonucleic acid antibody and antineutrophil cytoplasmic antibody) in addition to routine physical and neuro‐ophthalmological examination. The magnetic resonance imaging (MRI) protocol included T1‐ and T2‐weighted gradient echo axial imaging, T1‐weighted sagittal imaging and gadolinium‐enhanced T1‐axial imaging with or without diffusion‐weighted MRI, high‐resolution cranial nerve imaging of the brainstem and orbit, and MR angiography.
Standard protocol approvals and patient consents
All experiments followed the tenets of the Declaration of Helsinki and this study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B‐2308‐844‐103). All patients gave an informed and written consent to participate in this study.
Classification of the etiologies
The etiologies of the oculomotor nerve palsy were classified into microvascular, vascular anomalies, neoplastic, inflammatory, traumatic, congenital, vascular, infectious, recurrent painful ophthalmoplegic neuropathy, iatrogenic, central demyelination, Fisher syndrome and idiopathic. Microvascular oculomotor nerve palsy was diagnosed when the ophthalmoplegia was of an acute onset with a spontaneous recovery within 1 year in adults (≥20 years) with at least one vascular risk factor (hypertension, diabetes mellitus, dyslipidemia or smoking), and when there were no lesions that may explain the oculomotor nerve palsy on MRIs and no other disorders that may explain the oculomotor nerve palsy better. Vascular anomalies were diagnosed when the oculomotor nucleus, fascicle or nerve was affected by vascular malformation (e.g., intracranial aneurysm, dural arteriovenous fistula, cavernous malformation or arteriovenous malformation). Inflammatory etiology was presumed when MRIs demonstrated T2 hyperintense and gadolinium‐enhanced lesions affecting the oculomotor nucleus, fascicle or nerve (e.g., Tolosa–Hunt syndrome) and the symptoms responded to steroid treatments [20]. A traumatic cause was defined when there was a documented onset of oculomotor nerve palsy following head trauma and no other disorders to explain the oculomotor nerve palsy better. Congenital oculomotor nerve palsy was diagnosed when the patients had an infantile onset of ophthalmoplegia after excluding congenital cranial dysinnervation disorders, such as Duane syndrome and congenital Horner syndrome [21, 22]. Vascular etiology included ischaemic and hemorrhagic strokes not related to vascular anomalies. Infectious etiology was diagnosed when the clinical features and results of serology and cerebrospinal fluid analyses were consistent with a specific pathogen affecting the oculomotor nerve. Recurrent painful ophthalmoplegic neuropathy was diagnosed according to the criteria proposed in the third edition of the International Classification of Headache Disorders [23]. Central demyelination was defined as inflammatory demyelinating diseases of the central nervous system (CNS), including multiple sclerosis and neuromyelitis optica spectrum disorder [24]. Fisher syndrome was diagnosed when the patients had a positive serum ganglioside antibody without a lesion on MRIs that may explain the ophthalmoplegia, and the ophthalmoplegia was not better accounted for by other etiologies. Finally, the oculomotor nerve palsy was classified as idiopathic when the etiology could not be determined even with appropriate evaluation for the etiology of oculomotor nerve palsy. Myasthenic or neuromuscular causes of ophthalmoplegia were excluded. The etiology assigned to each patient by the primary physician was reviewed by the authors (HJK and JSK) and was finally accepted when considered appropriate.
Literature review
A literature search was conducted on PubMed in May 2022 using the combination of terms “cause(s) or etiology” and “oculomotor (nerve) palsy”. Fourteen articles that included more than 50 patients with a clear classification of the etiology of isolated oculomotor nerve palsy were found.
Comparison with isolated trochlear and abducens nerve palsy
The results of this study were compared with those of our previous reports on isolated trochlear palsy and isolated abducens nerve palsy performed in the same institution with the same methods during the same period [18, 19].
Statistical analyses
The Mann–Whitney U test was used to compare the age between men and women and the preferential involvement of each eye. The chi‐squared test was adopted to compare the proportion of etiologies between men and women and between the current study and pooled data, the proportion of involved specialists according to age and etiology, the proportion of involved specialists amongst oculomotor, trochlear and abducens nerve palsies in our institution, the proportion of patients who visited the emergency department first according to clinical features, and the proportion of patients who visited the emergency department first amongst oculomotor, trochlear and abducens nerve palsies in our institution. All these tests were performed using SPSS (version 25) and p < 0.05 was considered significant. The Bonferroni correction was applied for post hoc analyses and multiple comparisons, and p < 0.05 was considered significant.
RESULTS
From the 4702 patients initially recruited with the search terms it was possible to find isolated oculomotor nerve palsy in 672 patients. After excluding 39 patients with incomplete evaluation, 633 patients with isolated oculomotor nerve palsy were finally included for this study (Figure 1).
Magnetic resonance imaging was performed in almost all the patients (608/633, 96.1%), all in microvascular, vascular anomalies, neoplastic, inflammatory, idiopathic, vascular, infectious, recurrent painful ophthalmoplegic neuropathy, iatrogenic, central demyelination and Fisher syndrome, 66.0% in traumatic and 73.1% in congenital causes, using a 3.0‐T or 1.5‐T unit (Intera; Philips Medical Systems, Best, The Netherlands).
Demographic characteristics
Patients included 353 (55.8%) men and 280 (44.2%) women with a men‐to‐women ratio of 1.3:1 (p < 0.001) (Table 1). Age ranged from 2 months to 85.0 years (median 59.0, interquartile range 44.0–69.0) without a difference between men and women (median 60.0, interquartile range 45.0–69.0 vs. 58.0, interquartile range 42.5–69.0; p = 0.400). The first peak of incidence appeared before the age of 10 years, and the second peak occurred in the 60s (Figure 2). Unilateral involvement was found in 628 (99.2%) patients whilst bilateral palsies were observed in only five (0.8%) patients. In unilateral oculomotor nerve palsy, there was no predilection for each eye (right eye vs. left eye 332 [52.9%] vs. 296 [47.1%]; p = 0.118).
TABLE 1.
Demographic characteristics and proportion of management.
| Classification | No. | Age (years), median (IQR) | Men, n (%) | Management, n (%) | ||||
|---|---|---|---|---|---|---|---|---|
| OPH | NEUR | ER | NS | Other | ||||
| Microvascular | 168 | 66.0 (58.0–73.3) | 122 (72.6) | 114 (67.9) | 134 (79.8) | 101 (60.1) | 8 (4.8) | 7 (4.2) |
| Vascular anomalies | 110 | 58.5 (49.0–68.0) | 34 (30.9) | 82 (74.5) | 51 (46.4) | 67 (60.9) | 99 (90.0) | 1 (0.9) |
| Neoplasm | 86 | 56.0 (39.0–67.0) | 43 (50.0) | 78 (90.7) | 34 (39.5) | 25 (29.1) | 62 (72.1) | 19 (22.1) |
| Inflammatory | 79 | 56.0 (36.0–64.5) | 55 (69.6) | 49 (62.0) | 75 (94.9) | 54 (68.4) | 7 (8.9) | 3 (3.8) |
| Idiopathic | 60 | 63.0 (50.8–69.0) | 34 (56.7) | 43 (71.7) | 40 (66.7) | 26 (43.3) | 4 (6.7) | 1 (1.7) |
| Trauma | 53 | 47.0 (25.0–59.0) | 22 (41.5) | 48 (90.6) | 16 (30.2) | 16 (30.2) | 17 (32.1) | 6 (11.3) |
| Vascular | 28 | 66.5 (55.8–75.0) | 17 (60.7) | 16 (57.1) | 26 (92.9) | 18 (64.3) | 2 (7.1) | 2 (7.1) |
| Congenital | 26 | 0.9 (0.1–2.8) | 16 (61.5) | 26 (100.0) | 1 (3.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Infectious | 12 | 64.5 (33.5–69.0) | 6 (50.0) | 11 (91.7) | 8 (66.7) | 9 (75.0) | 2 (16.7) | 5 (41.7) |
| Recurrent painful ophthalmoplegic neuropathy | 5 | 45.0 (34.0–46.0) | 3 (60.0) | 2 (40.0) | 3 (60.0) | 1 (20.0) | 1 (20.0) | 0 (0.0) |
| Iatrogenic | 4 | 45.5 (30.3–61.5) | 0 (0.0) | 4 (100.0) | 2 (50.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) |
| Central demyelination | 1 | 19 | 0 (0.0) | 1 (100.0) | 1 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Fisher syndrome | 1 | 48 | 1 (100.0) | 1 (100.0) | 1 (100.0) | 1 (100.0) | 0 (0.0) | 0 (0.0) |
| Total | 633 | 59.0 (44.0–69.0) | 353 (55.8) | 475 (75.0) | 392 (61.9) | 319 (50.4) | 202 (31.9) | 44 (7.0) |
Abbreviations: ER, emergency physician; IQR, interquartile range; NEUR, neurologist; NS, neurosurgeon; OPH, ophthalmologist.
FIGURE 2.
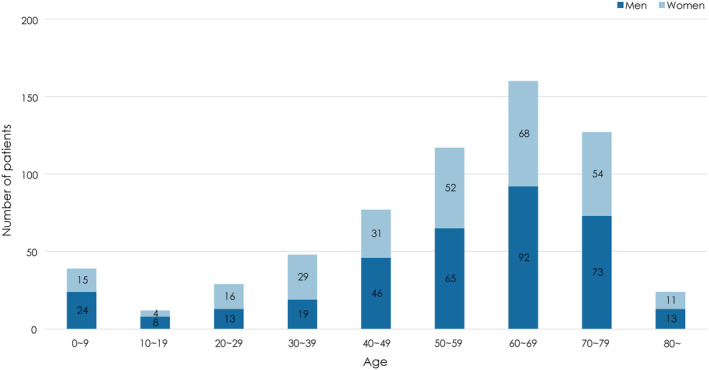
Distribution of isolated oculomotor nerve palsy according to age and sex. The incidence of isolated oculomotor nerve palsy shows double peaks, the first in the first decade and the second in the seventh decade. Men were more frequently affected with a men‐to‐women ratio of 1.3:1.
Etiology
The most common etiology was microvascular (n = 168, 26.5%), followed by vascular anomalies (n = 110, 17.4%), neoplastic (n = 86, 13.6%), inflammatory (n = 79, 12.5%), idiopathic (n = 60, 9.5%) and traumatic (n = 53, 8.4%; Figure 3). Other miscellaneous causes were found in 12.2% and included vascular (n = 28, 4.4%), congenital (n = 26, 4.1%), infectious (n = 12, 1.9%), recurrent painful ophthalmoplegic neuropathy (n = 5, 0.8%), iatrogenic (n = 4, 0.6%), central demyelination (n = 1, 0.2%) and Fisher syndrome (n = 1, 0.2%). The etiology of bilateral oculomotor nerve palsy was neoplastic, traumatic, vascular, congenital and infectious in each patient.
FIGURE 3.

Etiological distribution of isolated oculomotor nerve palsy. The most common etiology was microvascular followed by vascular anomalies, neoplastic, inflammatory, idiopathic and traumatic. These six etiologies overall explained 87.8% of isolated oculomotor nerve palsy.
In the neoplasm, primary CNS neoplasms were more common than metastatic/invasive cancers (69 [80.2%] vs. 17 [19.8%]). Meningioma (n = 24, 34.8%) and pituitary adenoma (n = 24, 34.8%) were the most common causes of primary CNS tumors, followed by schwannoma (n = 6, 8.7%), glioma (n = 3, 4.3%) and others (n = 12, 17.4%). Vascular anomalies included intracranial aneurysm (n = 89, 80.9%), dural arteriovenous fistula (n = 10, 9.1%), cavernous malformation (n = 9, 8.2%) and arteriovenous malformation (n = 2, 1.8%).
Most patients were adults (91.9%), and the proportion of etiology largely depended on the patients' age (Table S1). Traumatic etiology was most common before the age of 10, second most common in the second and third decades, and its proportion decreased thereafter. Inflammation was the most common cause in the second (41.7%) and third decades (27.6%) and neoplasm was most common in the fourth decade (27.1%). Vascular anomalies were the most common cause in the fifth decade (26.0%). The proportion of microvascular etiology increased after the age of 30 and peaked in the 70s (41.7%). Microvascular was the most common etiology in adults (28.9%), and the leading cause in the sixth decade and thereafter. Idiopathic etiology was rather evenly distributed in adults.
The etiologies of isolated oculomotor nerve palsy differed significantly between men and women (p < 0.001, Figure 4). Microvascular was the most common cause in men (122/353, 34.6%) whilst vascular anomalies (76/280, 27.1%) was the most common cause in women. Microvascular (122/353, 34.6% vs. 46/280, 16.4%; p < 0.001) and inflammation (55/353, 15.6% vs. 24/280, 8.6%; p = 0.008) were more prevalent in men whilst vascular anomalies (34/353, 9.6% vs. 76/280, 27.1%; p < 0.001) and trauma (22/353, 6.2% vs. 31/280, 11.1%; p = 0.029) were more common in women.
FIGURE 4.
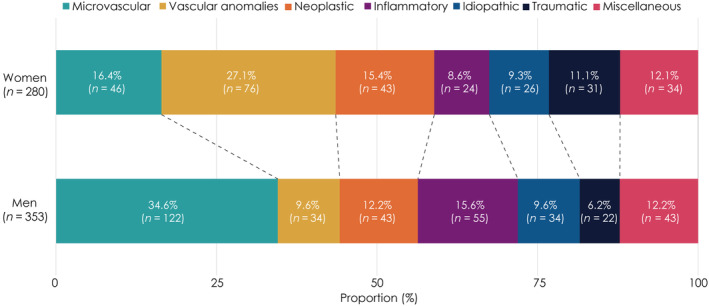
Etiological proportion of isolated oculomotor nerve palsy according to sex. Microvascular etiology was most common in men whilst vascular anomalies were most common in women.
Management
Patients with oculomotor nerve palsy visited the emergency department first in 42.5% of cases (n = 269) or were referred to the outpatient departments initially in 57.5% of cases (n = 364) (ophthalmology in 28.8% [n = 182], neurology in 16.7% [n = 106], neurosurgery in 8.8% [n = 56] and others in the remaining 3.2% [n = 20]). Patients with peri‐orbital pain or headache more frequently visited the emergency department first than those without (167/298, 56.0% vs. 102/335, 30.4%; p < 0.001).
Patients were mostly managed by ophthalmologists (475/633, 75.0%), followed by neurologists (392/633, 61.9%), emergency physicians (319/633, 50.4%), neurosurgeons (202/633, 31.9%) and others (44/633, 7.0%; Table 1, Figure 5). Either ophthalmologists or neurologists managed almost all the patients with isolated oculomotor nerve palsy (617/633, 97.5%). Of these, 36.5% (225/617) were managed by ophthalmologists only, 23.0% (142/617) by neurologists only and 40.5% (250/617) by both neurologists and ophthalmologists. The proportion of involved specialties also differed significantly according to the etiology of isolated oculomotor nerve palsy (p < 0.001). Neurologists were mainly involved in management of microvascular (134/168, 79.8%) and inflammatory oculomotor nerve palsies (75/79, 94.9%) whilst ophthalmologists mainly participated in the care of idiopathic (43/60, 71.7%), neoplastic (78/86, 90.7%) and traumatic (48/53, 90.6%) palsies. Neurosurgeons mostly took care of oculomotor nerve palsy due to vascular anomalies (99/110, 90.0%).
FIGURE 5.

The proportion of patients managed by each specialist according to the six main etiologies. The proportion of involved specialties differed according to the etiology of isolated oculomotor nerve palsy. Overall, the ophthalmologists were mostly frequently involved in the management of isolated oculomotor nerve palsy, but neurologists more frequently participated in the care of microvascular and inflammatory cases, and neurosurgeons in vascular anomalies. ER, emergency physician; NEUR, neurologist; NS, neurosurgeon; OPH, ophthalmologist.
Literature review
Microvascular was the most common etiology of isolated oculomotor nerve palsy in nine of the 14 papers, whilst trauma was the most common cause in one, aneurysm in one and idiopathic in the remaining three. Compared to the pooled data from the previous reports, the current study showed a higher prevalence of neoplastic (86/633, 13.6% vs. 231/2786, 8.3%; p < 0.001) but lower occurrence of microvascular (168/633, 26.5% vs. 885/2786, 31.8%; p = 0.010), idiopathic (60/633, 9.5% vs. 489/2786, 17.6%; p < 0.001) and traumatic (53/633, 8.4% vs. 387/2786, 13.9%; p < 0.001) causes. Overall, the etiological distribution of isolated oculomotor nerve palsy observed in the current study was different from that of 2786 patients pooled from the previous reports (p < 0.001, Table 2, Figure S1).
TABLE 2.
Previous studies on the etiology of isolated oculomotor nerve palsy.
| Country | Publication | Study duration | Age | No. of cases | Microvascular no. (%) | Idiopathic no. (%) | Aneurysm no. (%) | Trauma no. (%) | Neoplasm no. (%) | Miscellaneous no. (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Rucker [5] | USA | 1958 | 1945–1956 | 335 | 63 (18.8) | 95 (28.4) | 64 (19.1) | 51 (15.2) | 35 (10.4) | 27 (8.1) | |
| Goldstein and Cogan [6] | USA | 1960 | 61 | 28 (45.9) | 7 (11.5) | 11 (18.0) | 5 (8.2) | 6 (9.8) | 4 (6.6) | ||
| Green et al. [7] | USA | 1964 | 0–70 | 130 | 25 (19.2) | 31 (23.8) | 38 (29.2) | 14 (10.8) | 5 (3.8) | 17 (13.1) | |
| Rucker [8] | USA | 1966 | 1958–1964 | 274 | 47 (17.2) | 55 (20.1) | 50 (18.2) | 34 (12.4) | 50 (18.2) | 38 (13.9) | |
| Rush and Younge [9] | USA | 1981 | 1966–1978 | 0–91 | 290 | 60 (20.7) | 67 (23.1) | 40 (13.8) | 47 (16.2) | 34 (11.7) | 42 (14.5) |
| Berlit [10] | Germany | 1990 | 1966–1978 | 14–84 | 172 | 84 (48.8) | 17 (9.9) | 16 (9.3) | 10 (5.8) | 12 (7.0) | 33 (19.2) |
| Ing et al. [11] | Canada | 1992 | 1970–1991 | 0–17 | 54 | 1 (1.9) | 2 (3.7) | 0 (0.0) | 31 (57.4) | 2 (3.7) | 18 (33.3) |
| Richards et al. [12] | USA | 1992 | 1978–1988 | 0–93 | 231 | 55 (23.8) | 53 (22.9) | 25 (10.8) | 34 (14.7) | 22 (9.5) | 42 (18.2) |
| Akagi et al. [13] | Japan | 2008 | 1993–2001 | 63 | 22 (34.9) | 0 (0.0) | 10 (15.9) | 10 (15.9) | 5 (7.9) | 16 (25.4) | |
| Keane [14] | USA | 2010 | 1971–2007 | 3–89 | 500 | 151 (30.2) | 30 (6.0) | 101 (20.2) | 107 (21.4) | 11 (2.2) | 100 (20.0) |
| Kim et al. [15] | Korea | 2017 | 2004–2015 | 63 | 40 (63.5) | 17 (27.0) | 1 (1.6) | 3 (4.8) | 2 (3.2) | 0 (0.0) | |
| Fang et al. [3] | USA | 2017 | 1978–2014 | All | 145 | 61 (42.1) | 6 (4.1) | 9 (6.2) | 18 (12.4) | 16 (11.0) | 35 (24.1) |
| Choi et al. [16] | Korea | 2019 | 2015 | 9–88 | 81 | 44 (54.3) | 9 (11.1) | 2 (2.5) | 3 (3.7) | 1 (1.2) | 22 (27.2) |
| Jung et al. [4] | Korea | 2020 | 2002–2015 | All | 387 | 204 (52.7) | 100 (25.8) | 21 (5.4) | 20 (5.2) | 30 (7.8) | 12 (3.1) |
| Current study | Korea | 2023 | 2003–2020 | 0–85 | 638 | 168 (26.3) | 60 (9.4) | 89 (13.9) | 53 (8.3) | 86 (13.5) | 177 (27.7) |
Comparison with isolated trochlear and abducens nerve palsy
The etiological distribution of isolated oculomotor nerve palsy also differed from those isolated trochlear and abducens nerve palsies in our study cohort (p < 0.001, Figure 6a). The proportion of microvascular etiology was higher in isolated abducens nerve palsy (oculomotor vs. trochlear vs. abducens; 26.5% vs. 20.8% vs. 36.7%) whilst those of idiopathic (9.5% vs. 25.1% vs. 17.7%), congenital (4.1% vs. 32.4% vs. 1.2%) and traumatic (8.4% vs. 14.2% vs. 4.3%) etiology were higher in isolated trochlear palsy, and vascular anomalies (17.4% vs. 1.3% vs. 10.2%) were higher in isolated oculomotor nerve palsy. Patients with oculomotor nerve palsy more frequently visited the emergency department first than those with isolated trochlear or abducens nerve palsy (42.5% vs. 17.8% vs. 30.1%, p < 0.001; Figure 6b). The proportion of involved specialties also differed amongst the groups (p < 0.001, Figure 6c).
FIGURE 6.

Comparison of the characteristics with isolated trochlear and abducens nerve palsy. (a) The etiological distribution of isolated oculomotor nerve palsy differed from those of isolated trochlear and abducens nerve palsies in the same cohort reported previously (p < 0.001). (b) Patients with isolated oculomotor nerve palsy more frequently visited the emergency department first than trochlear or abducens nerve palsy (p < 0.001). (c) The proportion of involved specialties differed amongst the isolated ocular motor nerve palsies. For all three nerve palsies, the ophthalmologists were mostly involved in the management, especially for trochlear nerve palsy. In contrast, the neurologists were more frequently involved in the care of oculomotor and abducens nerve palsies than trochlear palsy.
DISCUSSION
This study determined the demographic features, etiologies and subspecialties involved in the management of isolated oculomotor nerve palsy in a large number of patients who had been recruited from all departments in a referral‐based university hospital from 2003 to 2020 when MRIs had been available for most of the patients. The main findings of this study may be summarized as follows. (i) Isolated oculomotor nerve palsy was more common in men than in women. (ii) Microvascular was overall the most common cause of isolated oculomotor nerve palsy, and was the leading cause in the sixth decades and thereafter. (iii) Vascular anomalies were the most common cause of isolated oculomotor nerve palsy in women. (iv) The proportions of microvascular and inflammatory etiologies were higher in men than in women whilst those of vascular anomalies, neoplasm and trauma were higher in women. (v) Ophthalmologists were involved in the management of isolated oculomotor nerve palsy in 75.0% and neurologists in 61.9% of the patients. (vi) Patients with oculomotor nerve palsy in association with peri‐orbital pain or headache more frequently visited the emergency department first. (vii) The etiological distribution of isolated oculomotor nerve palsy observed in the current study was different from that pooled from the previous reports.
In this study, isolated oculomotor nerve palsy was more common in men, but the men‐to‐women ratio varied from 0.7 to 1.7 in the previous studies [3, 4, 8, 11, 15, 16]. Of the 14 previous studies, six provided a men‐to‐women ratio with a male preponderance in three, female predominance in two and equal distribution in the remaining one [3, 4, 8, 11, 15, 16]. This variation in sex ratio may have been related to target population and have affected the proportion of etiologies, especially those with a strong sex predilection. However, the sex ratio did not appear to be related to the proportion of traumatic or microvascular etiologies that are known to be more common in men [3, 15].
As in most of the previous studies (23.8%–63.5%) [3, 4, 6, 10, 12, 13, 14, 15, 16], microvascular was the most common etiology of isolated oculomotor nerve palsy in this study (26.5%), especially in men (34.6%). In contrast, vascular anomalies were the most common in women (27.1%). In our previous study, however, microvascular was the most common etiology of isolated abducens nerve palsy in both men and women. The etiological distribution also differed significantly between men and women. This difference may be related to disparity in the prevalence of vascular risk factors between men and women. The predilection for men in microvascular etiology may be related to a higher prevalence of vascular risk factors such as diabetes, hypertension and smoking in men in the Republic of Korea [25, 26, 27]. The predilection for women in vascular anomalies may be related to the female predominance of intracranial aneurysm and cavernous sinus dural arteriovenous fistula that account for the large proportion of vascular anomalies (99/110, 90.0%) [28, 29]. The predilection for women in neoplastic etiology may be related to female predominance in meningioma (24/86, 27.9%; men‐to‐women ratio 6:18) that is 2.5 times more frequent in women [30].
The etiological distribution of isolated oculomotor nerve palsy observed in this study was significantly different from that of the data pooled from the previous reports with a higher prevalence of neoplastic etiology and lower prevalence of microvascular, idiopathic and traumatic etiologies. Our previous study also showed etiologies of isolated abducens nerve palsy that were different from those of the previous studies [19]. These findings seem to be related to a referral bias since our hospital is less frequently involved in the management of traumatic patients.
The etiological distribution differed amongst the groups of isolated ocular motor nerve palsy recruited from our institution over the same period [18, 19]. These differences may be due to the anatomical and physiological characteristics of each ocular motor nerve. The oculomotor nerve passes between the superior cerebellar and posterior cerebral arteries, and runs inferolateral to the posterior communicating artery to enter the roof of the cavernous sinus [31]. These characteristics may lead to a higher proportion of vascular anomalies amongst the etiologies. Each ocular motor nerve may have different vulnerabilities to microvascular ischaemia due to different blood supplies [32]. Since the trochlear nerve has the longest intracranial course and smallest diameter, and passes the free edge of the tentorium [33], it would be more susceptible to injuries associated with head trauma than other ocular motor nerves.
The specialties involved in the management of isolated oculomotor nerve palsy differed markedly depending on the etiology. This finding is similar to that observed in our previous studies on isolated trochlear and abducens palsies [18, 19]. However, the proportion of involved specialists differed markedly amongst the isolated ocular motor nerve palsies (Figure 6c). Even though the ophthalmologists were mostly involved in the management of isolated oculomotor nerve palsy (75.0%), the proportion of involvement was lower than that in isolated trochlear palsy (82.5%) and higher than that in isolated abducens nerve palsy (71.4%, p < 0.001). This discrepancy seems also related to differences in the proportion of etiologies amongst the groups, especially the lower proportion of congenital etiology in isolated oculomotor and abducens nerve palsies.
Our patients with isolated oculomotor nerve palsy more frequently visited the emergency department first than those with isolated trochlear or abducens nerve palsy (42.5% vs. 17.8% vs. 30.1%, Figure 6b). This may be explained by a higher proportion of etiologies causing acute or subacute onset of diplopia such as vascular anomalies (17.4% vs. 1.3% vs. 10.2%) and inflammation (12.5% vs. 1.5% vs. 9.4%).
Limitation
In this study, the etiology in 5.8% (39/672) of the patients initially recruited could not be determined due to an incomplete evaluation. This may have affected the relative proportion of etiologies in our patients with isolated oculomotor nerve palsy. Even though the distribution of patients with incomplete evaluation was similar across the age groups, the men‐to‐women ratio was higher in these patients than in those finally included for analyses (1.8 vs. 1.3). This selection bias may have affected the overall distribution of etiology and the sex ratio. Since this is a retrospective study performed in a single referral‐based hospital, the results may have differed from those observed in the general population. Finally, the comorbidities, details of the treatments and prognosis were not analyzed, which should be the subjects of future studies.
CONCLUSION
This study, having recruited the largest number of patients from all departments in a referral‐based university hospital, showed that the proportion of etiologies of isolated oculomotor nerve palsy depended on the age of the patients and specialties involved in the management. Overall, microvascular was the most common cause of isolated oculomotor nerve palsy in men and the leading cause in the sixth decade and thereafter. In contrast, vascular anomalies were the most common cause in women and the leading cause in the fifth decade. Isolated oculomotor nerve palsy was more commonly managed by ophthalmologists than neurologists (75.0% vs. 61.9%) and was cared for by both ophthalmologists and neurologists only in 40.5% of patients.
AUTHOR CONTRIBUTIONS
Hyun‐Jae Kim: Conceptualization (supporting); data curation (lead); formal analysis (lead); investigation (lead); methodology (equal); software (lead); visualization (equal); writing—original draft (lead). Hyo‐Jung Kim: Formal analysis (supporting); visualization (equal); project administration (supporting). Jeong‐Yoon Choi: Validation (supporting); writing—review and editing (supporting). Hee Kyung Yang: Validation (supporting); writing—review and editing (supporting). Jeong‐Min Hwang: Validation (supporting); writing—review and editing (supporting). Ji‐Soo Kim: Conceptualization (lead); funding acquisition (lead); investigation (equal); methodology (equal); project administration (lead); resources (lead); supervision (lead); validation (lead); visualization (equal); writing—original draft (supporting); writing—review and editing (lead).
FUNDING INFORMATION
This study was supported by grant no. 06‐2023‐0267 from Seoul National University Bundang Hospital Research Fund.
ETHICS STATEMENT
This study followed the tenets of the Declaration of Helsinki and was performed according to the guidelines of the Institutional Review Board of Seoul National University Bundang Hospital (B‐2308‐844‐103).
Supporting information
Figure S1.
Table S1.
Text S1.
Kim H‐J, Kim H‐J, Choi J‐Y, Yang HK, Hwang J‐M, Kim J‐S. Etiological distribution of isolated oculomotor nerve palsy: analysis of 633 patients and literature review. Eur J Neurol. 2024;31:e16261. doi: 10.1111/ene.16261
DATA AVAILABILITY STATEMENT
Anonymized data will be shared by request from any qualified investigator.
REFERENCES
- 1. Yanovitch T, Buckley E. Diagnosis and management of third nerve palsy. Curr Opin Ophthalmol. 2007;18:373‐378. [DOI] [PubMed] [Google Scholar]
- 2. Rucker JC, Rudich DS. Oculomotor nerve (cranial nerve III). In: Aminoff MJ, Daroff RB, eds. Encyclopedia of the Neurological Sciences. 2nd ed. Academic Press; 2014:633‐635. [Google Scholar]
- 3. Fang C, Leavitt JA, Hodge DO, Holmes JM, Mohney BG, Chen JJ. Incidence and etiologies of acquired third nerve palsy using a population‐based method. JAMA Ophthalmol. 2017;135:23‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jung EH, Kim SJ, Lee JY, Cho BJ. The incidence and etiologies of third cranial nerve palsy in Koreans: a 10‐year nationwide cohort study. Ophthalmic Epidemiol. 2020;27:460‐467. [DOI] [PubMed] [Google Scholar]
- 5. Rucker CW. Paralysis of the third, fourth and sixth cranial nerves. Am J Ophthalmol. 1958;46:787‐794. [DOI] [PubMed] [Google Scholar]
- 6. Goldstein JE, Cogan DG. Diabetic ophthalmoplegia with special reference to the pupil. Arch Ophthalmol. 1960;64:592‐600. [DOI] [PubMed] [Google Scholar]
- 7. Green WR, Hackett ER, Schlezinger NS. Neuro‐ophthalmologic evaluation of oculomotor nerve paralysis. Arch Ophthalmol. 1964;72:154‐167. [DOI] [PubMed] [Google Scholar]
- 8. Rucker CW. The causes of paralysis of the third, fourth and sixth cranial nerves. Am J Ophthalmol. 1966;61:1293‐1298. [DOI] [PubMed] [Google Scholar]
- 9. Rush JA, Younge BR. Paralysis of cranial nerves III, IV, and VI: cause and prognosis in 1,000 cases. Arch Ophthalmol. 1981;99:76‐79. [DOI] [PubMed] [Google Scholar]
- 10. Berlit P. Isolated and combined pareses of cranial nerves III, IV and VI: a retrospective study of 412 patients. J Neurol Sci. 1991;103:10‐15. [DOI] [PubMed] [Google Scholar]
- 11. Ing EB, Sullivan TJ, Clarke MP, Buncic JR. Oculomotor nerve palsies in children. J Pediatr Ophthalmol Strabismus. 1992;29:331‐336. [DOI] [PubMed] [Google Scholar]
- 12. Richards BW, Jones FR Jr, Younge BR. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am J Ophthalmol. 1992;113:489‐496. [DOI] [PubMed] [Google Scholar]
- 13. Akagi T, Miyamoto K, Kashii S, Yoshimura N. Cause and prognosis of neurologically isolated third, fourth, or sixth cranial nerve dysfunction in cases of oculomotor palsy. Jpn J Ophthalmol. 2008;52:32‐35. [DOI] [PubMed] [Google Scholar]
- 14. Keane JR. Third nerve palsy: analysis of 1400 personally‐examined inpatients. Can J Neurol Sci. 2010;37:662‐670. [DOI] [PubMed] [Google Scholar]
- 15. Kim K, Noh SR, Kang MS, Jin KH. Clinical course and prognostic factors of acquired third, fourth, and sixth cranial nerve palsy in Korean patients. Korean J Ophthalmol. 2018;32:221‐227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Choi KD, Choi SY, Kim JS, et al. Acquired ocular motor nerve palsy in neurology clinics: a prospective multicenter study. J Clin Neurol. 2019;15:221‐227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kim HJ, Kim HJ, Choi JY, Yang HK, Hwang JM, Kim JS. Diplopia: characteristics and etiologic distribution in a referral‐based university hospital. J Neurol. 2022;270:1067‐1075. [DOI] [PubMed] [Google Scholar]
- 18. Kim H‐J, Kim H‐J, Choi J‐Y, Yang HK, Hwang J‐M, Kim J‐S. Etiologic distribution of isolated trochlear palsy: analysis of 1020 patients and literature review. Eur J Neurol. 2022;29(12):3658‐3665. [DOI] [PubMed] [Google Scholar]
- 19. Kim HJ, Kim HJ, Choi JY, Yang HK, Hwang JM, Kim JS. Etiologic distribution of isolated abducens nerve palsy: analysis of 807 patients and literature review. Eur J Neurol. 2023;30:2471‐2480. [DOI] [PubMed] [Google Scholar]
- 20. Sánchez Vallejo R, Lopez‐Rueda A, Olarte AM, San RL. MRI findings in Tolosa–Hunt syndrome (THS). BMJ Case Rep. 2014;2014:bcr2014206629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Victor DI. The diagnosis of congenital unilateral third‐nerve palsy. Brain. 1976;99:711‐718. [DOI] [PubMed] [Google Scholar]
- 22. Kim JH, Hwang J‐M. Imaging of cranial nerves III, IV, VI in congenital cranial dysinnervation disorders. Korean J Ophthalmol. 2017;31:183‐193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Headache Classification Committee of the International Headache Society (IHS) the International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1‐211. [DOI] [PubMed] [Google Scholar]
- 24. Höftberger R, Lassmann H. Inflammatory demyelinating diseases of the central nervous system. Handb Clin Neurol. 2017;145:263‐283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011;35:303‐308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Choi KM, Park HS, Han JH, et al. Prevalence of prehypertension and hypertension in a Korean population: Korean National Health and Nutrition Survey 2001. J Hypertens. 2006;24:1515‐1521. [DOI] [PubMed] [Google Scholar]
- 27. Rim TH, Yoo TK, Kwak J, et al. Long‐term regular use of low‐dose aspirin and neovascular age‐related macular degeneration: National Sample Cohort 2010–2015. Ophthalmology. 2019;126:274‐282. [DOI] [PubMed] [Google Scholar]
- 28. Kim BS. Unruptured intracranial aneurysm: screening, prevalence and risk factors. Neurointervention. 2021;16:201‐203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tanaka M. Embryological consideration of dural arteriovenous fistulas. Neurol Med Chir (Tokyo). 2016;56:544‐551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sun T, Plutynski A, Ward S, Rubin JB. An integrative view on sex differences in brain tumors. Cell Mol Life Sci. 2015;72:3323‐3342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Park HK, Rha HK, Lee KJ, Chough CK, Joo W. Microsurgical anatomy of the oculomotor nerve. Clin Anat. 2017;30:21‐31. [DOI] [PubMed] [Google Scholar]
- 32. Galtrey CM, Schon F, Nitkunan A. Microvascular non‐arteritic ocular motor nerve palsies—what we know and how should we treat? Neuroophthalmology. 2015;39:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Joo W, Rhoton AL Jr. Microsurgical anatomy of the trochlear nerve. Clin Anat. 2015;28:857‐864. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1.
Table S1.
Text S1.
Data Availability Statement
Anonymized data will be shared by request from any qualified investigator.


