Abstract
Background and purpose
Neurology residency programmes, which were first established at the beginning of the 20th century, have become mandatory all over Europe in the last 40–50 years. The first European Training Requirements in Neurology (ETRN) were published in 2005 and first updated in 2016. This paper reports the most recent revisions of the ETRN.
Methods
Members of the EAN board performed an in depth revision of the ETNR 2016‐version, which was reviewed by members of the European Board and Section of Neurology of the UEMS, the Education and Scientific Panels, the Resident and Research Fellow Section and the Board of the EAN, as well as the presidents of the 47 European National Societies.
Results
The new (2022) ETRN suggest a 5‐year training subdivided in three phases: a first phase (2 years) of general neurology training, a second phase (2 years) of training in neurophysiology/neurological subspecialties and a third phase (1 year) to expand clinical training (e.g., in other neurodisciplines) or for research (path for clinical neuroscientist). The necessary theoretical and clinical competences as well as learning objectives in diagnostic tests have been updated, are newly organized in four levels and include 19 neurological subspecialties. Finally, the new ETRN require, in addition to a programme director, a team of clinician‐educators who regularly review the resident's progress.
The 2022 update of the ETRN reflects emerging requirements for the practice of neurology and contributes to the international standardization of training necessary for the increasing needs of residents and specialists across Europe.
Keywords: EAN, education, European, neurology, residents, standardization, training
INTRODUCTION
Neurology arose as a new medical specialty first in France, the UK and Germany and then in North and South America in the second half of the 19th century [1]. The first chair of neurology was created in 1882 in Paris for J.M. Charcot (chairs with other denomination and broader responsibility had been established for neurologists in other countries such as Germany, the United States and Russia) [2, 3]. By the end of the century chairs of neurology had been established in several countries including Argentina, the Netherlands and Switzerland [1, 4].
The first national neurological societies were founded in the United States (1875) and Belgium (1896) [2]. The German (1907), Italian (1907) and Swiss (1908) neurological societies were founded a few years later [4]. In many countries neurological societies were founded only after the Second World War (e.g., in 1948 in Canada). First clinics, wards, divisions and departments of neurology were established in Europe, the United States and South America at the turn of the 20th century [1, 4, 5].
The recognition of neurology as an independent medical specialty in Europe remained slow, however, taking place rarely before (e.g., Germany in 1919, the Netherlands in 1931, Switzerland in 1932) and most commonly after the Second World War (e.g., 1945 in the UK, 1965 in Canada, 1968 in France, 1976 in Slovenia, 1977 in Italy, 1991 in Belgium, 1994 in Austria [2, 6, 7]). It is noteworthy that in several countries, including Austria, Canada, France, Germany, Japan, Italy, the United States and Switzerland, joint neurology‐psychiatry or neurology‐neurosurgery training programmes (and certifications) persisted for a long time and were separated only in the second half of the late 20th century [2, 8].
EUROPEAN PREGRADUATE PROGRAMMES (MEDICAL SCHOOL TEACHING) IN NEUROLOGY
In 1911 there was no independent medical school teaching (pregraduate programmes) in neurology in most countries [9]. At the time of the first World Neurology Meeting in Bern in 1931, neurology was recognized in Europe as a mandatory field of the pregraduate medical curriculum only in Bulgaria, Estonia, Romania, Russia and Norway [4].
In a few other countries pregraduate programmes were established shortly thereafter (e.g., in 1913 in the Netherlands, in 1935 in Switzerland, in the 1930s in Belgium, in 1945 in Slovenia) [10]. In a survey published in 2011 a pregraduate curriculum in neurology was found to be present in all 31 participating European countries with a mean number of hours of training ranging from 20 (Spain) to 240 h (Hungary) [11, 12].
In the United States, most medical schools offer rotations for students that average 4 weeks in length and are typically placed in the third year [13]. In several European countries clinical rotations are placed in the last 2 years of the master training.
EUROPEAN POSTGRADUATE (RESIDENCY) PROGRAMMES IN NEUROLOGY
Postgraduate training in neurology started to be available in some European countries and the United States already in the 19th century. Neurology residency programmes were established in the first decades of the 20th century in the United States (e.g., in 1919 at Mayo Clinic) and Europe (e.g., in 1931 in the Netherlands, in 1939 in Switzerland) [10, 14].
In most European countries, South America and Asia independent neurology curricula were established only after the Second World War (e.g., 1945 in the UK and Slovenia, 1967 in Argentina, 1970 in Australia, 1990 in Belgium, 1991 in Italy [7, 15]). The result of this delay was a very limited number of neurologists in most countries (e.g., two in Australia at the eve of the Second World War, 57 in in the UK in 1954 compared to 166 in 1956 in Switzerland) [6, 10, 15, 16]. In the USA residency review committees were introduced in the 1950s and only 19 Americans became board‐certified neurologists in 1960 [2, 14, 17]. The introduction of the National Health Service in the UK (1945) and of Medicare in the United States (1965) had a major impact on the creation (UK) and expansion (United States) of neurological residency programmes in these two countries [6, 15, 17].
The European Union of Medical Specialists (UEMS) was created in 1958 to oversee and promote the highest level of training and the development of European standards in the different medical disciplines. The UEMS, Section of Neurology/European Board of Neurology (UEMS‐SN/EBN) oversees the qualification in neurology.
The first European Training Requirements in Neurology (ETRN) were published in 2005 by the European Federation of Neurological Societies (EFNS) and the UEMS Section of Neurology and were first updated in 2016 [18].
The first European Board examination organized by the UEMS‐SN/EBN took place in 2009. Currently the yearly examination is organized under the supervision of the Examination Board with support from the Joint Educational Board (JEB), which was created in 2019. The JEB consists of representatives from both the European Academy of Neurology (EAN) and UEMS‐SN/EBN. Passing the examination is considered as proof of excellence of a neurologist. Still, it is without legal value unless national authorities adopt it as equivalent to or instead of their national examination (e.g., Flanders in Belgium) or accept it as an exit examination if no national equivalent exists. If no national examination exists, health authorities still must ratify the EBN examination. Slovenia, for example, recently shortened the residency programme from 6 to 5 years and recognized the EBN examination as equivalent to the national exit examination [19].
Today, postgraduate specialty training in neurology is defined in every European country. However, as expected, there is considerable heterogeneity in the access systems, duration, types of training, formal curriculum, international opportunities and assessment methods [20, 21]. For instance, not all countries have an examination to enter or at the end of postgraduate training (typically regulated by national rules), the duration ranges from 2 to 3 (Russia, Moldavia) to 6 (The Netherlands, Denmark) years (most commonly 4 or 5 years), and the balance between theoretical and clinical parts is highly variable [20]. Simultaneously, training centres have their accreditation and exceptionally also visitation from their national authorities but the process tends to vary significantly between countries.
THE NEW EUROPEAN POSTGRADUATE (RESIDENCY) PROGRAMME
European Training Requirements for Neurology (ETRN)
In 2021 the President of the EAN (CB) and four members of the EAN board (CB, RS, DV, PB) started an in‐depth revision of the ETRN 2016 version motivated by several considerations. First, knowledge in basic and clinical neurosciences is increasing exponentially. Secondly, the subspecialization in neurology is increasing. For example, in 2012 there were 25 neurological subspecialties recognized in the United States [22]. Thirdly, different surveys have shown shortcomings in current residency programmes concerning diagnostic and therapeutic procedures, practical skills and specialized contents such as sleep medicine [23, 24]. Fourthly, there is a growing need for international standardization of teaching due to the increased mobility of European students, residents and specialists.
The draft document was first reviewed by members of the Joint EAN‐SN/EBN (European Board and Section of Neurology of the UEMS, RS, BS, JBMK, MR, PC) and subsequently by the Education and Scientific Panels, the Resident and Research Fellow Section and the Board of the EAN. The 47 European National Societies were also given the possibility to provide their input. Finally, the UEMS council provided the final review and approval of the document.
The primary aim of the ETRN remains the definition of the basic educational requirements in the different domains of neurology to enable specialists to move across European country borders for professional purposes.
The aim of ETRN is the acquisition of broad (general) neurological knowledge and skills for competent diagnosis and management of both common and rare neurological diseases. Such training may be followed by the acquisition of a particular competence in one or more subspecialties of neurology, and by neurological research.
The residency programme should consist of a minimum of 4 years, subdivided into a phase of basic (general neurology) clinical training (years 1 and 2) and a phase of advanced clinical training in neurophysiology/neurological subspecialties (years 3 and 4) (Figure 1). At least one additional year of training is recommended to expand the advanced clinical training.
FIGURE 1.
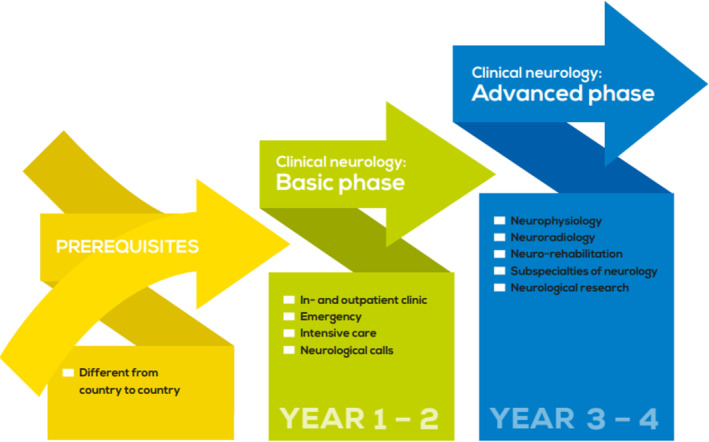
Different phases of the residency training in neurology. From European Training Requirements for Neurology, version 2021.
Additional requirements to the specific training in neurology are requested in some countries (e.g., a 3–4 year rotation in general and internal medicine in Australia and New Zealand, a 4‐year rotation in general and internal medicine in the UK, a 1‐year rotation in internal medicine in the United States and Switzerland, a 6‐month rotation in emergency medicine in Slovenia).
The first phase (years 1 and 2) allows the acquisition of the basic (general neurology) neurological skills (including the art of detailed history taking and clinical examination) through the exposure to neurological calls/emergencies and intensive care neurology and the management of both inpatients and outpatients with a balanced proportion of a broad spectrum of neurological diseases, as well as the opportunity to follow up patients.
The second phase (years 3 and 4) should include rotations in neurophysiology (electroencephalography, electromyography, evoked potentials, cerebrovascular neurosonography, sleep–wake tests), neuroradiology (standard and advanced neuroimaging techniques), neurorehabilitation and work in units specializing in the complex care of neurological diseases (epilepsy, stroke, movement disorders, neuroimmunology/multiple sclerosis, sleep–wake disorders, neuro‐oncology, neuromuscular diseases, dementia, neurorehabilitation, paediatric neurology etc.). A minimum of two subspecialized fields should be covered.
In parallel, the possibility of a combined clinical‐research appointment over a limited period (e.g., 6–12 months) should be made available to promote a career as clinical neuroscientist with exposure to patient‐oriented/clinical neurological research.
Optional rotation in general or internal medicine, neurosurgery, psychiatry, neuro‐paediatrics, neuroradiology and neuropathology should be offered, preferably in the recommended additional year of training.
A precise list of competences to be acquired by trainees to be a European neurologist at the start of unsupervised practice has been defined. In some countries, a system of entrustable professional activities (EPA) has been defined so that residents can be followed more closely with regard to clinical skills. The current ETRN does not refer to EPA, but their implementation is being considered within the EAN and UEMS‐SN/EBN in the future.
A certified trainer should supervise a trainee's clinical work during every particular training period, and every trainee should have a mentor for the whole duration of training.
Trainees should keep a logbook to record their clinical activity and to document all structured assessments: Mini CEX (Mini Clinical Evaluation Exercise—observed clinical skills), DOPS (Direct Observation of Procedural Skills, e.g., lumbar puncture), case‐based discussions, multisource 360° feedback (from colleagues, nurses and other professionals), patient feedback from inpatients and outpatients, discussion of diagnostic/treatment errors, teaching observation, logbook assessment, qualifications experience and core competences for trainers and training centres are extensively detailed. In many training centres, the CanMeds model has been adopted for this purpose [25].
Theoretical knowledge of specific competences for trainees is summarized in Figure 2. Clinical knowledge of specific competences is articulated in four levels (Figure 3).
FIGURE 2.
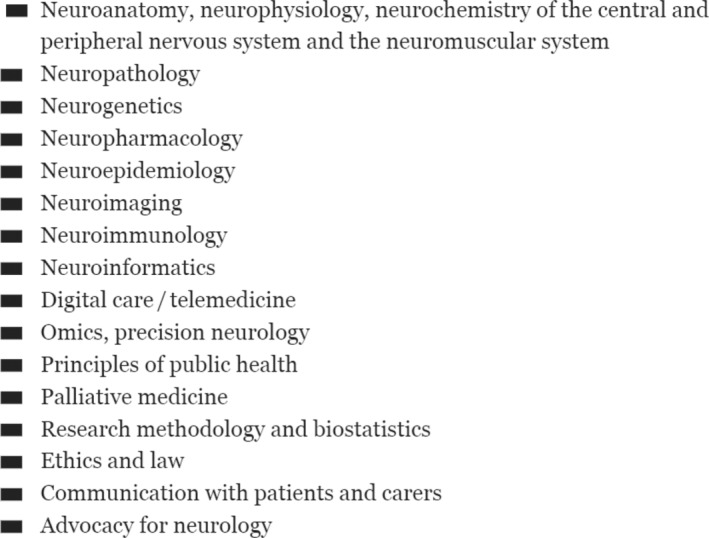
Specific competences: theoretical knowledge. From European Training Requirements for Neurology, version 2021.
FIGURE 3.
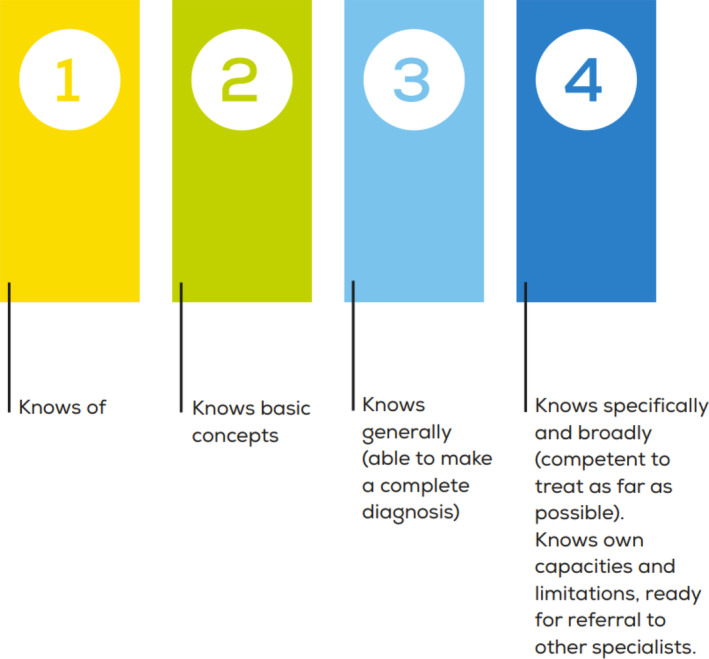
Specific competences: clinical knowledge. From European Training Requirements for Neurology, version 2021.
In this regard 19 neurological diseases have been categorized and their sub‐items rated in terms of the required level of knowledge: cerebrovascular disorders, cognitive disorders/dementias, epilepsies and other paroxysmal disorders, headache and facial pain, immune‐mediated diseases, infections of the nervous system, movement disorders, neuro‐emergency and intensive care, neurological trauma, neurological manifestations and complications of non‐primary neurological diseases/conditions and intoxications, neuromuscular disorders, neuro‐oncology, neuro‐ophthalmology and neuro‐otology, neuropsychiatric and functional neurological disturbances, neurorehabilitation, pain and neurological pain syndromes, disturbances of circulation of cerebrospinal fluid, sleep–wake disorders, spinal cord and root disorders.
Advances in diagnostic technology have been extensive. Hence, the Learning Objectives section in Diagnostic Tests has been significantly updated (Figure 4).
FIGURE 4.
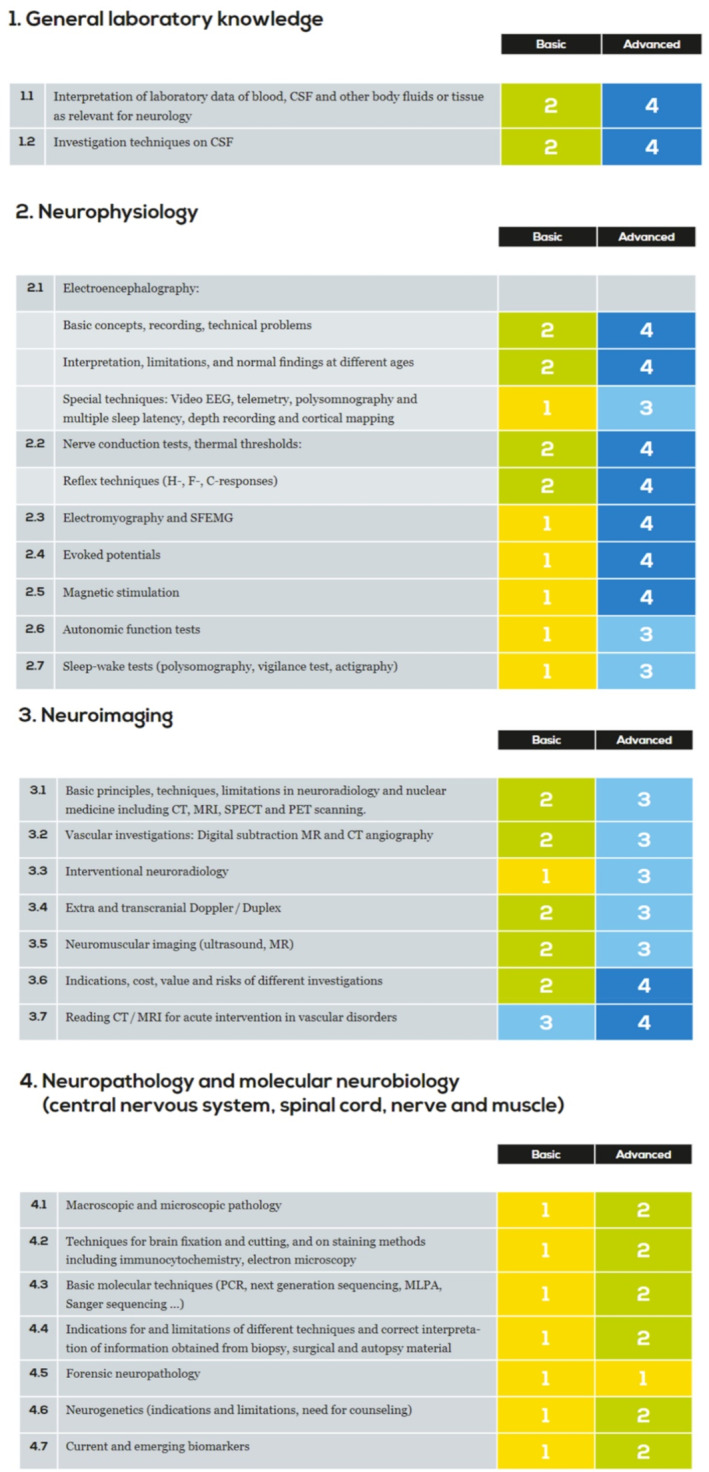
Learning objectives in diagnostic tests within ETRN. The table specifies four groups of diagnostic tests and the four levels of competence (basic 1–2, advanced 3–4, see Figure 2). From European Training Requirements for Neurology, version 2021.
The interdisciplinary aspects of several neurological disorders require that a resident in neurology will acquire knowledge and selected skills for managing issues related to neurosurgery, psychiatry, neuro‐paediatrics, neuro‐geriatrics and palliative medicine.
DISCUSSION
This paper presents the in‐depth revision of the ETRN, the European Postgraduate (Residency) Programme, which was created in 2005 and first revised in 2016. Overall, the structure of ETRN has been maintained. Still, the organization and content of the training have been modified in depth to reflect contemporary and emerging requirements for the practice of neurology and the resulting training needs.
The subdivision in the two (basic and advanced) phases over a period of 5 years is similar to the model of the Swiss neurology residency programme and to the 3‐year residency (always including a 1‐year rotation in internal medicine) and 1‐ to 2‐year fellowship programmes of the United States [10, 26]. The first 3 years are devoted to acquiring the skills in general neurology, whilst the remaining two include elective rotations in neurophysiology and different subspecialties and the option of rotations in research. In this revised version of the ETRN emerging subspecialties (e.g., sleep medicine, neurorehabilitation, palliative and preventive neurology/brain health [24, 27]) and novel approaches (e.g., neuroinformatics, teleneurology) are better represented.
The description of the neurology competences remains relatively short compared to those described in the recent document on the Standards of Accreditation for Residency Programmes in Adult and Paediatric Neurology from Canada [28]. In this document the training experience required or recommended or optional is articulated in phases, such as transition discipline, foundations of disciplines, core of discipline and transition to practice. It is interesting to note that in the competences of a neurologist the following specific roles were defined: medical expert, communicator, leader, scholar and professional with specific requirements for all roles. Overall, the skills required for managing neurological diseases of the ETRN are described similarly to those published by other continental specialty societies such as the European Society of Cardiology [29].
The worldwide movement towards competency‐based postgraduate medical education has shifted the paradigm of training with fixed length and variable competence to fixed competence (meeting standards) but variable length if needed, based on the individual progression of the resident [29]. This does not preclude that there is an average of 5 years of training with a minimum (‘experience in neurology’) of 4 years. Competent individuals or those with extensive experience before they start their neurology training might meet the standards in less than 5 years of neurology training, whilst some may need more than 5 years.
Another important advancement is that there should be a programme director and a team of clinician‐educators who regularly meet and review the resident's progress. In North America the so‐called Clinical Competency Committees are required by an Accreditation Council of General Medical Education and are becoming central in all postgraduate medical education programmes, with a minimum documented review of each resident every 6 months. Similar teams operate in the Netherlands and Belgium [30].
The ETRN has not specified the quantitative aspects of teaching (i.e., total hours of education per week or month) and leaves this quite open to national solutions.
Neurologists (as all other health professionals) should keep up with the advancements in knowledge and skills in their field of competence throughout their professional lives (clearly evident for patients and referring colleagues) by adhering to adequate continuing professional development and continuing medical education [31]. However, the regulation of this continuing medical education is still a matter of discussion in many European countries.
FUTURE
The EAN will keep track of all advances in neurology residency trainings throughout the European space and the rest of the world and continue to collaborate with the UEMS‐SN/EBN to ensure timely updates of the ETRN.
Future potential approaches may include modern teaching approaches (e.g., e‐learning, web‐based case repositories), the definition of academic programmes for ‘clinical neuroscientists’ (in which residency programmes are combined with research activities/PhD and clinical PhD programmes), a more systematic adoption and validation of EPA (to translate competences in clinical practice [32, 33]) and new tools to evaluate training programmes (e.g., involvement of patients, Delphi surveys). An important challenge will also be the format of the examination including clinical neurology skills tested in a practice‐based setting or in a virtual environment with real‐time simulated patient interactions.
FUNDING INFORMATION
No funding to disclose. In‐kind support has been provided by the European Academy of Neurology for producing graphic material and administrative support.
CONFLICT OF INTEREST STATEMENT
No conflicts of interest to disclose.
ACKNOWLEDGMENTS
Open access funding provided by Inselspital Universitatsspital Bern.
Bassetti CLA, Soffietti R, Vodušek DB, et al. The 2022 European postgraduate (residency) programme in neurology in a historical and international perspective. Eur J Neurol. 2024;31:e15909. doi: 10.1111/ene.15909
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Allegri RF, Bartoloni L. The first steps of clinical neurology in South America. Neurology. 2013;80:1338‐1340. [DOI] [PubMed] [Google Scholar]
- 2. Freemon FR. American neurology. In: Finger S, Boller F, Tyler KL, eds. History of Neurology Handbook of Cliniical Neurology. Elsevier B.B.; 2010:606‐611. [Google Scholar]
- 3. Vein AA, van Emde Boas W. Kozhevnikov epilepsy: the disease and its eponym. Epilepsia. 2011;52:212‐218. [DOI] [PubMed] [Google Scholar]
- 4. Bassetti C, Valko PO. History of the Swiss Neurological Society in the context of the national and international development of neurology. Swiss Arch Neurol and Psychiatry. 2009;160:52‐65. [Google Scholar]
- 5. Naleym MA, Elkind MSB. Outpatient training in neurology. History and Future Challenges Neurology. 2006;66:E1‐E6. [DOI] [PubMed] [Google Scholar]
- 6. Shorvon S. How the coming of the NHS changed British neurology. Brain. 2018;141:1570‐1575. [DOI] [PubMed] [Google Scholar]
- 7. Facheris M, Mancuso M, Scaravilli T, Bonifati DM. Neurology residency training in Europe: an Italian perspective. Lancet Neurol. 2005;4:258‐262. [DOI] [PubMed] [Google Scholar]
- 8. Takahashi A. History of clinical neurology in Japan. In: Finger S, Boller F, Tyler KL, eds. History of Neurology Handbook of Clinical Neurology. Elsevier B.V; 2010:769‐779. [DOI] [PubMed] [Google Scholar]
- 9. Veraguth O. Der neurologische Unterrricht an den Schweizerischen Universitäten. Correspondenzblatt für Schweizer Aerzte. 1911;20:696‐708. [Google Scholar]
- 10. Bassetti CL, Galimanis A, Du Pasquier R. The new swiss postgraduate training (residency program) in neurology: making swiss neurologists more competitive. Clinical and Translational Neurosci. 2018;2:2514183X1879276. doi: 10.1177/2514183X18792760 [DOI] [Google Scholar]
- 11. Struhal W, Falup‐Pecurariu C, Sztriha LK, Grisold W, Sellner J. European Association of Young Neurologists and Trainees: position paper on teaching courses for generation Y. Eur J Neurol. 2011;18:e36‐e40. [DOI] [PubMed] [Google Scholar]
- 12. Struhal W, Sellner J, Lisnic V, Vécsei L, Müller E, Grisold W. Neurology residency training in Europe—the current situation. Eur J Neurol. 2011;18:e36‐e40. [DOI] [PubMed] [Google Scholar]
- 13. Gooch C. The state of academic neurology departments in the United States, 2016. Neurology. 2017;89:524‐525. [DOI] [PubMed] [Google Scholar]
- 14. Boes CJ, Burkholder DB, Coon EA, Cutsforth‐Gregory JK, Klaas JP, Jones LK Jr. Reciprocal development and progressive responsibility: the history of the Mayo Clinic Neurology Residency. Mayo Clin Proc. 2020;4:478‐498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Foley PB, Storey CE. History of neurology in Australia and New Zealand. In: Finger S, Boller F, Tyler KL, eds. History of Neurlogy Handbook of Clinical Neurology. Elsevier B.V.; 2010:781‐799. [DOI] [PubMed] [Google Scholar]
- 16. Hewer RL, Wood VA. Neurology in the United Kingdom. I: Historical development. J Neurol Neurosurg Psychiatry. 1992;55(Suppl):2‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Peltier WL. Core competencies in neurology resident education: a review and tips for implementation. Neurologist. 2004;10:97‐101. [DOI] [PubMed] [Google Scholar]
- 18. Pontes CC, European Federation of Neurological Scoieties . Recommended core curriculum for a specialist training program in neurology. Eur J Neurol. 2005;12:743‐746. [DOI] [PubMed] [Google Scholar]
- 19. Rakusa M, Rot U. Toward a unified European curriculum—reforming national residency programme in Slovenia. Eur J Neurol. 2020;27:e80. doi: 10.1111/ene.14441 [DOI] [PubMed] [Google Scholar]
- 20. Kleineberg NN, van der Meulen M, Franke C, et al. Differences in neurology residency training programmes across Europe—a survey among the residents and research fellow section of the European Academy of Neurology national representatives. Eur J Neurol. 2020;27:1356‐1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sauerbier A, Macerollo A, Györfi O, et al. Insufficient global health education in European neurological post‐graduate training: a European Association of Young Neurologists and Trainees survey. Eur J Neurol. 2016;23:1680‐1683. [DOI] [PubMed] [Google Scholar]
- 22. Struhal W, Mellgren SI, Grisold W. Three important steps to European neurology harmonization: core curriculum, visitation program. European Board Examination Eur J Neurol. 2013;20:101‐104. [DOI] [PubMed] [Google Scholar]
- 23. Györfi O, Moarcas M, Balicza P, Macerollo A, Struhal W, Sellner J. European junior neurologists perceive various shortcomings in current residency curricula. Acta Neurol Scand. 2016;134:232‐237. [DOI] [PubMed] [Google Scholar]
- 24. Rakusa M, Sieminski M, Rakusa S, et al. Awakening to sleep disorders in Europe: survey on education, knowledge and treatment competence of European residents and neurologists. Eur J Neurol. 2021;28:2863‐2870. [DOI] [PubMed] [Google Scholar]
- 25. Frank JR. The CanMEDS 2005 Physician Competency Framework: Better Standards, Better Physicians, Better Care. Royal College of Physicians and Surgeons of Canada; 2005. [Google Scholar]
- 26. Bassetti CL, Hess CW, Steck A, Ludin HP. A 110‐year history of the Swiss Neurological Society (SNG) through the biosketches of its first 42 presidents. Clinical and Translational Neurosci. 2018;2:30. doi: 10.1177/2514183X18788797 [DOI] [Google Scholar]
- 27. Bassetti CLA, Endres M, Sander A, et al. The European Academy of Neurology Brain Health Strategy: One brain, one life, one approach. Eur J Neurol. 2022;29:2559‐2566. doi: 10.1111/ene.15391 [DOI] [PubMed] [Google Scholar]
- 28. Royal College of Physicians and Surgeons of Canada . Standards of Accreditation for Residency Programs in Adult and Paediatric Neurology; 2020:145A/145P. [Google Scholar]
- 29. Tanner FC, Brooks N, Fox KF, et al. ESC core curriculum for the cardiologist. Europ Heart J. 2020;41:3605‐3691. [DOI] [PubMed] [Google Scholar]
- 30. Smit MP, de Hoog M, Brackel HJL, Ten Cate O, Gemke RJBJ. A national process to enhance the validity of entrustment decisions for Dutch pediatric residents. Med Educ. 2019;11:158‐164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. ten Cate OT, Carraccio C. Envisioning a true continuum of competency‐based medical education, training, and practice. Acad Med. 2019;94:1283‐1288. [DOI] [PubMed] [Google Scholar]
- 32. ten Cate O. Nuts and bolts of entrustable professional activities. J Grad Med Educ. 2013;5:157‐158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lucey CR, Thibault GE, Ten Cate O. Competency‐based, time‐variable education in the health professions: crossroads. Acd Med. 2018;93 (3S Competency‐Based, Time‐Variable Education in the Health Professions):S1‐S5. doi: 10.1097/ACM.0000000000002080 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


