Saturday, June 29, 2024
Ageing and dementia 1
EPO‐001
Development of small molecules promoting tau clearance in Alzheimer disease
L. Wang1; R. Kumar1,2; P. Pavlov1; B. Winblad 1,3
1Division of Neurogeriatrics, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Solna, Sweden; 2Department of Pharmaceutical Engineering and Technology, Indian Institute of Technology (BHU), Varanasi, India; 3Theme Inflammation and Aging, Karolinska University Hospital, Huddinge, Sweden
Background and Aims: A major pathological hallmark of Alzheimer disease (AD) is the intracellular accumulations of neurofibrillary tangles composed of paired helical filaments (PHFs) of tau protein. Lowered efficiency of degradation pathways, such as ubiquitin proteasome system, further exacerbates the aggregated tau accumulation. Proteolysis‐Targeting Chimeras (PROTACs) are hetero‐bifunctional molecules that can bring E3 ligase into the vicinity of protein of interest, leading to protein ubiquitination, followed by proteasomal degradation. Since 2016, PROTACs have been applied to resolve tau pathologies. Most of these PROTACs have only been evaluated in cell models and the exploration is still at the early stage. In this study, we aim to perform intensive research to develop novel small‐molecule PROTACs to initiate tau degradation for AD treatment.
Methods: We screened a library of tau binders from a public database (bindingdb.org) by performing global molecular docking into the 3D structure of PHFs. The top ranked compounds were selected to design new PROTACs, with different linkers connected to the ligands binding to E3 ligase, for instance cereblon and carboxyl terminus of Hsp70 interacting protein (CHIP). We are performing modeling of the ternary complex (tau‐PROTACs‐E3 ligase) and the highly scored PROTACs will be synthesised. Their protein binding affinities and tau‐reducing effects will be evaluated in cell models.
Results: We perform the development of small‐molecule PROTACs according to the methods listed above. We selected the top ranked tau binders and designed new PROTACs.
Conclusion: The hit PROTACs will move on to in vivo study and provide pre‐clinical evidence for novel treatment of AD tauopathies.
Disclosure: The authors declare no conflict of interest.
EPO‐002
Functional connectivity as biomarker of neurodegenerative disease
A. Medvedeva
First Moscow State Medical University, Russia
Background and Aims: Alzheimer's disease (AD) selectively involves cerebral neuronal networks. The aim was to correlate fMRI patterns and EEG‐coherence in Alzheimer's disease (AD), amnestic Mild cognitive impairment (aMCI), non amnestic Mild cognitive impairment (nMCI), Frontotemporal Dementia (FTG) and controls.
Methods: 90 patients with AD, 90 aMCI, 85 nMCI, 60 FTD patients and 90 age‐matched controls underwent fMRI (3 Tesla, TRIO, Siemens) and resting EEG‐recordings (NeuroScan Synamps System). EEGs were recorded using a standard protocol and montage. Coherences between regions of interest, based on fMRI activation patterns were calculated.
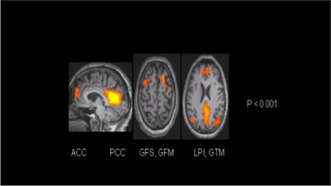
Comparison of controls vs. AD patients. fMRI activations (p < 0.001)
Results: There were significant differences between AD and aMCI for theta coherences between anterior cingulate gyrus (ACC) and left temporal gyrus (LTG) (AD < aMCI, p < 0.05) Fig.2; between AD and controls for theta between ACC and right temporal gyrus, between ACC and left hippocampus, and between ACC and right parietal gyrus (AD < controls, p < 0.01) Fig. 1. aMCI‐subjects showed reduced coherence compared with controls between ACC and left frontal superior gyrus within delta, theta and alpha1‐band. Theta coherence was significantly between anterior and posterior cingulate gyrus, between right and LTG (aMCI < controls, p < 0.05) Fig. 3. There were significant differences between FTG and controls, between ACC and left temporal gyrus in delta and theta (FTG < controls, p < 0.05). There were not found significant differences between AD, FTD and nMCI.
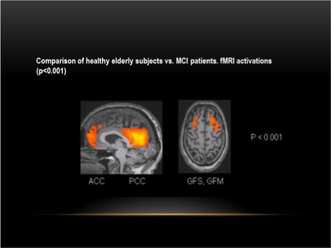
Comparison of controls vs. aMCI patients. fMRI activations (p < 0.001)
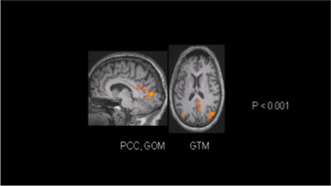
Comparison of aMCI vs. AD patients. fMRI activations (p < 0.001)
Conclusion: EEG coherence seems to be a useful approach, which helps to detect the early stage of cognitive decline.
Disclosure: Nothing to disclose.
EPO‐003
Improving FTD diagnosis with NODDI metrics and machine learning integration
S. Basaia 1; S. Pisano2; C. Cividini1; F. Facente1; E. Spinelli3; E. Canu1; V. Castelnovo1; G. Cecchetti4; A. Ghirelli3; F. Caso5; G. Magnani5; P. Caroppo6; S. Prioni6; C. Villa6; L. Tremolizzo7; I. Appollonio7; F. Verde8; N. Ticozzi9; V. Silani9; M. Filippi10; F. Agosta3
1Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; and Neurology Department, Istituto Clinico S. Anna Hospital, Brescia, Italy; 3Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 4Neurophysiology Service, Neurology Unit, and Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute Milan, Italy; 5Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; 6Fondazione IRCCS Istituto Neurologico Carlo Besta, Unit of Neurology, Milan, Italy; 7Neurology Unit, "San Gerardo" Hospital and University of Milano‐Bicocca, Monza, Italy; 8Department of Neurology and Laboratory of Neuroscience, IRCCS Istituto Auxologico Italiano, Milano, Italy; 9Department of Neurology and Laboratory of Neuroscience, IRCCS Istituto Auxologico Italiano, and "Dino Ferrari" Center, Department of Pathophysiology and Transplantation, Università degli Studi di Milano, Milan, Italy, 10Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: To investigate microstructural gray matter (GM) and white matter (WM) alterations in FTLD patients and to develop machine learning (ML) algorithm that classifies patients according to NODDI metrics and neuropsychological data.
Methods: Thirty‐five behavioral‐variant frontotemporal dementia (bvFTD), 20 semantic‐variant primary progressive aphasia (svPPA), 14 nonfluent‐variant primary progressive aphasia (nfvPPA), 9 semantic‐bvFTD (sbvFTD) and 48 controls performed multi‐shell diffusion‐brain MRI. Fractional anisotropy (FA), Intra‐cellular Volume Fraction (ICVF) and Orientation Dispersion Index (ODI) maps were estimated. GM and WM comparisons between FTLD groups were performed. ML algorithm was trained on (i) mean GM/WM values of FA, ICVF and ODI maps subdivided in brain lobes and (ii) neuropsychological data.
Results: FA maps showed widespread WM damage in FTLD patients relative to controls. ICVF maps showed damage in FTLD patients relative to controls in frontotemporal for bvFTD, left temporal‐frontal for svPPA and nfvPPA, right temporal for sbvFTD. ODI maps showed a GM reduction with a similar ICVF‐GM pattern. WM alterations in patients relative to controls was observed: (i) WM reduction in corpus callosum and corona radiata (bvFTD, svPPA, nfvPPA) and right corona radiata (sbvFTD); (ii) WM increase in temporo‐occipital WM bundles (bvFTD) and stria‐terminalis (svPPA). ML model (ICVF + ODI + neuropsychological data) showed a 95.9% accuracy in the classification of each patient syndrome.
Conclusion: NODDI and ML algorithm hold potential for advancing our understanding of FTLD pathology and facilitating diagnosis, personalized treatment strategies at individual‐level. Funding: European Research Council (StG‐2016_714388_NeuroTRACK); Foundation Research on Alzheimer Disease; Next Generation EU/National Recovery and Resilience Plan, Investment PE8‐Project Age‐It.
Disclosure: S Basaia research support from Italian Ministry of Health (IMH). S Pisano, C Cividini, F Facente, EG Spinelli, V Castelnovo, A Ghirelli, F Caso, G Magnani, P Caroppo, S Prioni, C Villa, L Tremolizzo, I Appollonio, F Verde nothing to disclose. E Canu research support from Italian Ministry of Health. G Cecchetti speaker honoraria from Neopharmed Gentili. N Ticozzi consulting services for Amylyx Pharmaceuticals, Zambon Biotech SA and lectures for Italfarmaco; funding from IMH and AriSLA. V Silani consulting services and/or speaking activities for AveXis, Cytokinetics, Italfarmaco; and research support from IMH, AriSLA, and E‐Rare Joint Transnational Call. M Filippi consulting or speaking activities or advisory boards for Alexion, Almirall, Biogen, Bayer, Bristol‐Myers Squibb,Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA; scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol‐Myers Squibb, Lilly, Novartis, Sanofi‐Genzyme; research support from Biogen Idec, Merck‐Serono, Novartis, Roche, IMH, Italian Ministry of University and Research, and FISM. F Agosta received speaker honoraria from Biogen Idec, Italfarmaco, Roche, Zambon and Eli Lilly, and has received research supports from IMH, Italian Ministry of University and Research, ARiSLA, ERC, EU Joint Programme – Neurodegenerative Disease Research, and Foundation Research on Alzheimer Disease.
EPO‐004
Aging features through connectome analysis and advanced diffusion‐weighted metrics with a machine learning approach
S. Basaia 1; S. Pisano2; E. Sibilla1; E. Spinelli3; E. Canu1; M. Filippi4; F. Agosta3
1Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; and Neurology Department, Istituto Clinico S. Anna Hospital, Brescia, Italy; 3Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 4Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: To develop machine learning algorithm combining connectome analysis and advanced diffusion‐weighted metrics to classify different features underlying aging process.
Methods: Forty‐eight young‐controls (YC), 20–31 years, 21 middle‐aged [MC] and 44 elderly‐controls [EC], 41–85 years, underwent brain multi‐shell diffusion‐MRI and cognitive evaluation. Fractional anisotropy (FA), Intra‐cellular Volume Fraction (ICVF) and Orientation Dispersion Index (ODI) maps were estimated. TBSS and connectomics were performed. Support‐vector‐machine (SVM) model trained on FA, ICVF and ODI values of all connections resulted different in TBSS and connectomics, was used for the identification of features (TBSS‐ or connectome‐related) of aging process. Features that better distinguished three groups were used as variables in a multivariate polynomial regression to predict subject's age. Correlation coefficient between the predicted age by the model and the age of the subjects.
Results: SVM models showed 99.7% and 100% accuracy in the classification of YC relative to MC/EC, ODI values of TBSS‐related connections as best selected feature. SVM models demonstrated 83.4% accuracy between MC‐EC groups, identifying FA connections values as the most informative feature for classification. Mean ODI of TBSS‐ and FA of connectome‐related connections were inserted in the multivariate polynomial regression to predict subject's age. Correlation analysis indicated relationship between age‐predicted and actual age of subjects (r = 0.93; p < 0.001).
Conclusion: Combination of SVM and neuroimaging achieved high accuracy in group classification and age prediction, highlighting the potential for understanding brain connectivity patterns and age‐related changes. Funding. European‐Research‐Council (StG‐2016_714388_NeuroTRACK); Foundation Research on Alzheimer's disease; Next Generation EU/National Recovery and Resilience Plan, Investment PE8‐Project Age‐It.
Disclosure: S Basaia research support from Italian Ministry of Health (IMH). S Pisano, E Sibilla and EG Spinelli have nothing to disclose. E Canu research support from Italian Ministry of Health. M Filippi consulting or speaking activities or advisory boards for Alexion, Almirall, Biogen, Bayer, Bristol‐Myers Squibb,Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA; scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol‐Myers Squibb, Lilly, Novartis, Sanofi‐Genzyme; research support from Biogen Idec, Merck‐Serono, Novartis, Roche, IMH, Italian Ministry of University and Research, and FISM. F Agosta received speaker honoraria from Biogen Idec, Italfarmaco, Roche, Zambon and Eli Lilly, and has received research supports from IMH, Italian Ministry of University and Research, ARiSLA, ERC, EU Joint Programme – Neurodegenerative Disease Research, and Foundation Research on Alzheimer Disease.
EPO‐005
Clinical characteristics and biomarker profile in early and late‐onset Alzheimer's disease: The Shanghai Memory Study
J. Wu; Z. Xiao; X. Ma; X. Zhou; D. Ding; Q. Zhao
Institute of Neurology, Huashan Hospital, Fudan University, Shanghai, China
Background and Aims: Early‐onset Alzheimer's disease (EOAD) constitutes approximately 5%–10% of Alzheimer's disease (AD). Its difference with Late‐onset Alzheimer's disease (LOAD) was not well documented. The current study explored their characteristics covering clinical, neuropsychological and biomarker profiles.
Methods: Ninety‐ninety patients with LOAD and 104 with EOAD were enrolled from a Chinese hospital‐based cohort, the Shanghai Memory Study. Clinical features, cognitive performance, and full‐panel of plasma biomarker were compared cross‐sectionally. Disease progression and longitudinal cognition change were analyzed as well.
Results: Results: Patients with EOAD presented more severe impairment in global cognition, attention, and language function (all p < 0.05). Levels of plasma Aβ40, Aβ42, Aβ42/Aβ40, and neurofilament light (NfL) were higher in the LOAD group, while plasma p‐tau181 concentration was higher in the EOAD group (all p < 0.05). After adjusting for age, gender, disease severity, and comorbid disease, younger age at onset (AAO) was associated with lower levels of plasma Aβ40 (B = 1.827, 95% CI 1.205 to 2.450, p < 0.001), Aβ42 (B = 0.106, 95% CI 0.064 to 0.147, p < 0.001), and NfL (B = 0.280, 95% CI 0.145 to 0.415, p < 0.001), while with higher concentrations of p‐tau181 (B = −0.040, 95% CI −0.069 to −0.012, p = 0.006). The level of plasma p‐tau181 was significantly correlated with global cognition, memory, attention, and visuospatial function in patients with EOAD, but not in LOAD.
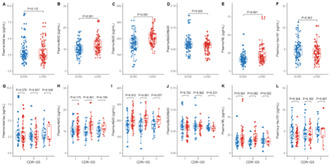
FIGURE 1 Concentrations of plasma biomarkers among patients with different age‐at onset and disease severity.
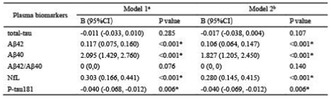
TABLE 2 multiple linear regression of plasma biomarkers and age at onset Note: a mode 1, data were adjusted for CDR‐global score, gender, education duration, and APOE genotype; b in model 2, data were adjusted for gender, education duration, CDR‐glo.

FIGURE 2 correlations between plasma biomarker concentrations and cognitive domains. Note: The plasma biomarkers concentrations were log transformed. A, correlations between plasma biomarker concentrations and cognitive domains in all participants; B, co.
Conclusion: Conclusion: Patients with EOAD differed from LOAD in cognitive performance and biomarker profile. Plasma p‐tau181 level showed more tremendous change in EOAD.
Disclosure: Nothing to disclose.
EPO‐006
Sleep disturbances and the impact in neuropsychiatric symptoms in Alzheimer's disease
C. Fernandes 1; D. Valente2; I. Carvalho1; F. Gomes1; F. Barros1; C. Bernardes1; P. Faustino1; J. Durães3; M. Lima4; I. Baldeiras4; M. Tábuas‐Pereira3; I. Santana3
1Neurology Department, Hospitalar and University Center Coimbra, Coimbra, Portugal; 2Neurology Department, Hospitalar and University Center os Algarve, Faro, Portugal; 3Neurology Department, Hospitalar and University Center Coimbra, Coimbra, Portugal; CIBB – Center for Innovative Biomedicine and Biotechnology, University of Coimbra, Coimbra, Portugal; Faculty of Medicine, University of Coimbra, Coimbra, Portugal; 4Neurology Department, Hospitalar and University Center Coimbra, Coimbra, Portugal and CIBB – Center for Innovative Biomedicine and Biotechnology, University of Coimbra, Coimbra, Portugal
Background and Aims: Sleep disturbances are common in Alzheimer's disease (AD), contributing to accelerate cognitive deterioration and progression of neuropsychiatric symptoms (NPS). Understanding the sleep disturbances in AD can expand our knowledge and improve treatment of NPS. Evaluate the association between sleep disturbances and NPS in patients with AD.
Methods: We performed a cross‐sectional study, including patients with the diagnosis of AD supported by biomarkers. NPS were assessed with Frontal Behavioral Inventory (FBI) and Neuropsychiatric Inventory (NPI). Sleep disturbances were evaluated with Pittsburgh Sleep Quality Index (PSQI), STOP‐BANG score, Epworth scale (ES) and REM Behavior Disorder screening questionnaire (RBDSQ). Statistical analysis comprised univariate analysis and statistical significance was set at p < 0.05.
Results: We included 61 patients (68.9% female) with average age of onset of 64.2(±6.8) years. The median education was 4.0 (IQR = 5.0) and MMSE of 20 (IQR = 8). According to the STOP‐BANG score, 11 patients (21.2%) were at intermediate or higher risk of obstructive sleep apnea (OSA) and 18 patients (29.5%) reported sleep disturbances in PSQI (score >5). Total PSQI scores were correlated with FBI indifference (r = 0.031; p = 0.012), inattention (r = 0.380; p = 0.006), aphasia (r = 0.429; p = 0.002) and perseveration (r = 0.294; p = 0.038). STOP‐BANG score was correlated with FBI indifference (r = 0.290; p = 0.043), logopenia (r = 0.358; p = 0.012), aphasia (r = 0.513; p < 0.001), perseveration (r = 0.440; p = 0.002), comprehension deficit (r = 0.316; p = 0.027), hyperorality (r = 0.498; p < 0.001) and utilization behaviors (r = 0.295; p = 0.038). No correlation was found between NPS symptoms and ES and RBDSQ.
Conclusion: Sleep disturbances were associated with NPS frontal dysfunction showing that sleep quality influences the diurnal function of AD patients. Interestingly, patients at higher risk of OSA presented with more prominent frontal features suggesting a possible pattern of AD phenotype related to hypoxia, meriting further studies.
Disclosure: Nothing to disclose.
EPO‐007
Effect of Aβ on Alzheimer's disease tau spreading
F. Nabizadeh
School of Medicine, Iran University of Medical Sciences, Tehran, Iran
Background and Aims: Alzheimer's disease (AD) is characterized by the accumulation of Amyloid‐beta (Aβ) plaques initiated approximately two decades before the symptom onset followed by buildup and spreading of neurofibrillary tau aggregates. Although it has been suggested that the Aβ amplifies tau spreading the observed spatial disparity called it into question. Yet it is unclear how neocortical Aβ remotely affects early pathological tau, triggering it to leave the early formation area, and how Aβ facilitates tau aggregate spreading throughout cortical regions. I aimed to investigate how Aβ can facilitate tau spreading through neuronal connections in the AD pathological process by combining fMRI normative connectomes and longitudinal in vivo molecular imaging data.
Methods: In total, the imaging data of 317 participants including, 173 Aβ‐negative non‐demented and 144 Aβ‐positive non‐demented participants have entered the study from ADNI. Furthermore, normative resting‐state fMRI connectomes were used to model tau spreading through functional connections.
Results: It was observed that the Aβ in regions with the highest deposition (Aβ epicenter) is remotely associated with connectivity‐based spreading of tau pathology. Moreover, Aβ in regions that exhibit the highest tau pathology (tau epicenter) is associated with increased connectivity‐based tau spreading to non‐epicenter regions.
Conclusion: The findings provide a further explanation for a long‐standing question of how Aβ can affect tau aggregate spreading through neuronal connections despite spatial incongruity. The results suggest that Aβ pathology can remotely and locally facilitate connectivity‐based spreading of tau aggregates.
Disclosure: Nothing to disclose.
EPO‐008
Solanezumab treatment for Alzheimer disease: Meta analysis for non expedition trials
A. Al Wssawi; H. Talib Hashim
University of Warith Al‐Anbiyaa, College of Medicine
Background and Aims: Solanezumab, a monoclonal antibody, has shown promise in treating Alzheimer's disease by targeting beta‐amyloid plaques, potentially slowing cognitive decline. Despite mixed initial trials, ongoing research indicates potential benefits.
Methods: It is a systematic review and meta‐analysis. We included only RCTs for Non‐EXPEDITION Trials. 1202 records were screened based on our search strategy on main database (Pubmed, Scopus, WOS, Cochrane). Continuous Outcomes were pooled using Random Effects, Inverse Variance and Mean Difference.

Flow chart of study selection and included study based on PRISMA

ROB for included study
Results: 6 RCTs, 4956 participant used Solanezumab. 5 RCTs included, outcome of (ADAS‐Cog14, ADAS‐Cog11, MMSE, CDR‐SB Score), intervention number in each Trial (n1 = 578, n2 = 102, n3 = 50, n4 = 1057, n5 = 659). Improvements in cognitive subscale of the Alzheimer's Disease Assessment Scale (ADAS‐cog14) were observed by 5 studies. The overall pooled results showed that Solanezumab is associated with a significant reduction in ADAS‐ Cog 14 scores as compared to placebo. (MD −1.18, 95% CI (−1.96, −0.40); p = 0.003, I 2 = 0%). Improvements in cognitive subscale of the Alzheimer's Disease Assessment Scale (ADAS‐cog11) were observed by 2 studies. Pooled analysis showed that Solanezumab is associated with a significant reduction in ADAS‐ Cog 11 scores as compared to placebo. (MD −1.68, 95% CI (−2.80, −0.55); p = 0.003, I 2 = 0%).

Baseline characteristic of included study
Conclusion: Solanezumab treatment for Alzheimer's disease presents a promising avenue in the quest for effective interventions. While its ability to halt or reverse the disease remains uncertain, it offers hope by targeting the underlying amyloid plaques, a key hallmark of Alzheimer's.
Disclosure: Nothing to disclose.
EPO‐009
Gender disparities in down syndrome‐associated Alzheimer's disease and related pathologies
M. Altuna 1; A. Estanga1; J. Saldias1; M. Cañada1; A. Garrido2; M. Echeverria2; J. Larrea3; M. García‐Sebastián1
1Cita Alzheimer Foundation, Donostia, Spain; 2Osakidetza Basque Health Service, Donostialdea Integrated Health Organisation, Clinical Biochemistry Department, Donostia, Spain; 3Osakidetza Basque Health Service, Donostialdea Integrated Health Organisation, Radiology Department, Donostia, Spain
Background and Aims: Down syndrome (DS) constitutes a genetically determined form of Alzheimer's disease (DSAD). While gender differences in risk factors and the clinical course of Alzheimer's have been identified in the general population, this aspect remains unexplored in DS. Our primary aim is to investigate gender influences on DSAD diagnosis and related comorbidities in DS.
Methods: Observational cross‐sectional study in a population‐based cohort of adults with DS, regardless of intellectual disability (ID) and cognitive status, with dual purposes (clinical and research), from January to December 2023. Conducted adapted neurological‐neuropsychological evaluations to determine ID and cognitive status in relation to DSAD. Optional procedures included brain MRI, lumbar puncture for AT(N) biomarker study, and blood analysis, addressing both clinical and research objectives.

Protocol of baseline visit of clinical and research cohort of adults with DS
Results: Recruited 115 participants, 46.9% women, average age 46.32 years (25–65). No gender differences in ID (89.9% mild to moderate) or cognitive status for DSAD (35.6% symptomatic). Similarly, no distinctions in age of cognitive symptom onset (51.1 ± 5.4 years), prodromal (51.4 ± 4.7 years), and DSAD dementia (53.6 ± 5.7 years) diagnosis; and or global cognition, episodic memory, neuropsychiatric inventory, functional autonomy scales, and quantitative neurological assessment (balance, gait scales, and screening for rigid‐akinetic syndrome) scores. No differences observed in epilepsy and obstructive sleep apnea prevalence. The only comorbidities with statistically significant differences (more prevalent in women) were hypothyroidism and vitamin D deficiency.
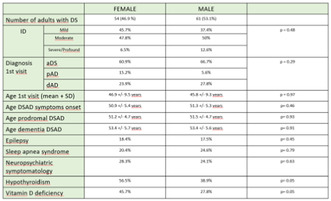
Down syndrome population data
Conclusion: The influence of gender on the clinical course of symptomatic Alzheimer's and more frequent comorbidities may be lesser, possibly not significant, in genetically determined forms, or at least in DSAD.
Disclosure: Nothing to disclose.
EPO‐010
MHC‐II receptor enrichment in locus coeruleus since Alzheimer's disease early stages
N. Rabaneda Lombarte 1; F. Pereira2; A. Ehrenberg2; V. Paes3; C. Suemoto4; R. Leite4; R. Rodriguez4; R. Ferretti‐Rebustini4; E. Ferrioli4; R. Nitrini4; W. Jacob‐Filho4; C. Pasqualucci4; W. Seeley5; S. Spina5; B. Miller6; L. Grinberg7
1Department of Neurosciences, Hospital Universitari Germans Trias i Pujol, Barcelona, Spain; 2Department of Neurology, Memory and Aging Center, Weill Institute for Neurosciences, University of California, San Francisco, California, USA; 3Department of Pathology, University of Sao Paulo Medical School, Sao Paulo, Brazil; 4Division of Geriatrics, University of Sao Paulo Medical School, Sao Paulo, Brazil; 5Department of Pathology and Global Brain Health Institute, University of California, San Francisco, California, USA; 6Department of Neurology, Memory and Aging Center, Weill Institute for Neurosciences, and Global Brain Health Institute, University of California, San Francisco, California, USA; 7Department of Pathology, University of Sao Paulo Medical School, Brazil. Department of Pathology and Neurology, Memory and Aging Center, Weill Institute for Neurosciences, and Global Brain Health Institute, University of California, San Francisco, USA
Background and Aims: The locus coeruleus (LC), a key noradrenergic nucleus for memory and arousal, is an early‐damaged region in Alzheimer's disease (AD) with tau vulnerability. The molecular mechanism for this remains unclear. We conducted RNA analysis on LC and substantia nigra (SN), a less vulnerable nucleus, in subjects at progressive AD stages, to explore the molecular basis of LC's selective vulnerability to AD‐tau.
Methods: RNA sequencing was conducted on RNA extracted from the LC and SN regions of postmortem brains belonging to healthy controls (HC; n = 11) and AD patients (n = 40) across distinct Braak stages (BB) (Fig. 1).
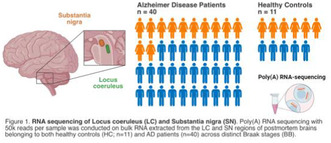
FIGURE 1
Results: Genes linked to the MHC‐II receptor ontology term showed upregulation from the initial BB in the LC (Fig. 2). Notably, the expression of HLA‐DQB1 gene, a key player in the immune system, exhibits a 1‐fold increase at BB 1 compared to BB 0. In BB 2 and BB 3 cases, an increase in the expression of CD4 and HLA‐DRA genes was observed compared to HC. In the advanced stages of the disease (BB 4–6), all MHC‐II genes exhibited higher RNA expression compared to HC. Notably, the SN showed none of these changes.
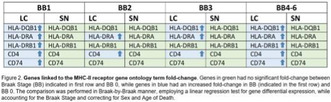
FIGURE 2
Conclusion: Multiple lines of evidence back MHC‐II involvement in AD. This study uniquely shows early MHC‐II activation, especially in the vulnerable human brain region. This suggests therapeutic potential in modulating this axis for AD treatment and offers insights into unknown disease origins. Further research is crucial to validate these findings and explore the earliest AD stages in subcortical nuclei.
Disclosure: NRL was a recipient of the “Rotación Externa de Formación en Neurología” grant from the Spanish Society of Neurology.
EPO‐011
Combined plasma biomarkers for the diagnosis of Alzheimer's Disease in clinical scenario
A. Pilotto 1; A. Galli1; C. Trasciatti1; V. Quaresima1; C. Tolassi1; M. Parigi2; A. Rizzardi1; S. Caratozzolo1; A. Benussi1; S. Giliani2; K. Blennov3; N. Ashton4; H. Zetterberg5; A. Padovani1
1Neurology Unit, University and ASST SPedali CIvili of Brescia, Brescia, Italy; 2Nocivelli Institute, ASST Spedali CIvili of Brescia, Brescia, italy; 3University of Gothenborg, GOthenborg, Sweden; 4University of Moelndal, Moelndal, Sweden; 5Wallenberg Institute, University of GOthenborg, Sweden
Background and Aims: The implementation of plasma biomarkers in clinical settings is pivotal for a rapid screening and diagnosis, as well as for tracking disease progression reducing the costs and burden of CSF assessments. Aim of the study was to evaluate the ability of plasma markers to discriminated Alzheimer's disease (AD) and both healthy controls (HC) and other neurodegenerative diseases (NDD).
Methods: The cross‐sectional study included patients with AD (A+T+N+), patients with non‐AD NDD, and healthy controls. Each patient underwent standard core‐standard CSF analyses, plasma p‐tau181, p‐tau 217, Aβ42, and Aβ40 were measured using single molecule arrays (SIMOA) analyses. The ability of blood‐based biomarkers to detect AD pathology was assessed by using ROC and linear regression analyses.
Results: two‐hundred eighty‐six individuals, namely 124 AD, 50 NDD, and 112 HC entered the study. P‐tau 181, p‐tau 217, p‐tau 181/Aβ42 ratio, and p‐tau 217/ Aβ42 ratio levels were elevated in AD compared to NDD and HC. P‐tau 217 biomarker showed the highest area under the receiver operating curve (AUC) for identifying AD from HC (AUC = 0.933), compared to p‐Tau 181 (AUC = 0.88) and other considered biomarkers. p‐tau 217/ Aβ42 ratio exhibited the highest AUC for identifying AD from NDD (AUC = 0.858).
Conclusion: plasma p‐tau 217 was the most accurate biomarker in ruling out AD individuals from HC, whereas its combination with Aβ42 was the best biomarker in identifying AD from other neurodegenerative diseases.
Disclosure: None.
EPO‐012
Primary progressive aphasia in Italian and English: A cross‐linguistic cohort study
S. Mazzeo 1; C. Hardy2; J. Jiang2; C. Morinelli3; V. Moschini3; J. Johnson2; A. Chokesuwattanaskul4; A. Volkmer5; J. Rohrer2; A. Ingannato6; S. Bagnoli6; S. Padiglioni3; B. Nacmias6; S. Sorbi6; V. Bessi6; J. Warren2
1Research and Innovation Centre for Dementia‐CRIDEM, Azienda Ospedaliero‐Universitaria Careggi, Florence, Italy; Vita‐Salute San Raffaele University, Milan, Italy; 2Dementia Research Centre, Department of Neurodegenerative Disease, UCL Queen Square Institute of Neurology, University College London, London, UK; 3Research and Innovation Centre for Dementia‐CRIDEM, Azienda Ospedaliero‐Universitaria Careggi, Florence, Italy; 4Division of Neurology, Department of Internal Medicine, King Chulalongkorn Memorial Hospital, Thai Red Cross Society, Bangkok, Thailand; 5Department of Psychology & Language Sciences, University College London, London, UK; 6Department of Neuroscience, Psychology, Drug Research and Child Health, University of Florence, Azienda Ospedaliera‐Universitaria Careggi, Florence, Italy
Background and Aims: Primary Progressive Aphasia (PPA) is a neurodegenerative disorder primarily affecting language abilities, with clinical variants (nonfluent/agrammatic variant [nfvPPA], semantic variant [svPPA], logopenic variant [lvPPA], and mixed‐PPA [mPPA]) categorized based on linguistic features. This study aims to compare PPA cohorts of native speakers of English and Italian.
Methods: We considered 166 English participants (70 nfvPPA, 45 svPPA, 42 lvPPA, 9 mPPA) and 106 Italian participants (14 nfvPPA, 20 svPPA, 42 lvPPA, 31 mPPA). Starting from the neuropsychological battery used to assess patients, we extracted one test for each cognitive and linguistic function that can be compared between cohorts. Comparisons were adjusted for symptom duration and Mini‐mental State Examination.
Results: The English cohort included a higher proportion of nfvPPA patients (42% vs. 13%, p < 0.001), while the Italian cohort showed higher proportions of lvPPA (25% vs. 38%, p = 0.019) and mPPA (5% vs. 29%, p < 0.001) (Fig. 1). English nfvPPA patients were more frequently impaired in single‐word comprehension (60% vs. 8%, p = 0.013), while Italian nfvPPA patients exhibited more agrammatism (46% vs. 93%, p = 0.015). English svPPA had a higher proportion of surface dyslexia (68% vs. 30%, p = 0.046) and spelling impairment (38% vs. 10%, p = 0.021). English lvPPA had broader impairments, including single‐word comprehension (89% vs. 29%, p < 0.001), repetition of words (61% vs. 26%, p = 0.03), nonverbal working memory (69% vs. 36%, p = 0.005), and visuospatial perception (89% vs. 25%, p < 0.001) (Fig. 2).
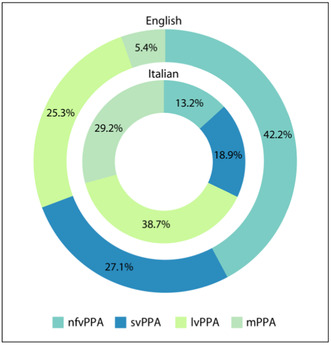
Donut plots showing proportion of PPA variants in English and Italian cohorts. Significant differences between cohorts are coded as follows: *p < 0.05 ***p < 0.001
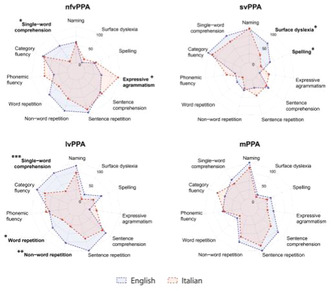
Profiles of neurolinguistic and general cognitive impairment in the Italian and English cohorts. Significant differences between cohorts are coded as follows: *p < 0.05; **p < 0.01; ***p < 0.001
Conclusion: Language‐specific characteristics impact the clinical presentation of PPA. Cultural and linguistic nuances should be considered in PPA diagnosis and management, calling for more tailored assessments and criteria.
Disclosure: Nothing to disclose.
EPO‐013
Distinctive longitudinal cortical atrophy progression patterns in clinical variants of frontotemporal dementia continuum
E. Spinelli 1; A. Ghirelli1; F. Orlandi2; E. Canu3; S. Basaia3; V. Castelnovo3; E. Sibilla3; G. Cecchetti4; F. Caso5; G. Magnani5; P. Caroppo6; S. Prioni6; C. Villa6; L. Tremolizzo7; I. Appollonio7; F. Verde8; N. Ticozzi9; V. Silani9; M. Filippi10; F. Agosta1
1Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 3Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 4Neurophysiology Service, Neurology Unit, and Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute Milan, Italy; 5Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; 6Fondazione IRCCS Istituto Neurologico Carlo Besta, Unit of Neurology 5‐Neuropathology, Milan, Italy; 7Neurology Unit, "San Gerardo" Hospital and University of Milano‐Bicocca, Monza, Italy; 8Department of Neurology and Laboratory of Neuroscience, IRCCS Istituto Auxologico Italiano, Milano, Italy; 9Department of Neurology and Laboratory of Neuroscience, IRCCS Istituto Auxologico Italiano, and "Dino Ferrari" Center, Department of Pathophysiology and Transplantation, Università degli Studi di Milano, Milan, Italy, 10Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: Recently, diagnostic criteria have been proposed for a variant of frontotemporal dementia (FTD) showing distinctive right temporal damage, named semantic behavioural variant FTD (sbvFTD). Our aim was to describe longitudinal patterns of disease progression for each FTD syndrome, with a particular focus on sbvFTD.
Methods: Our cohort included a total of 59 FTD patients with a diagnosis of behavioral variant of FTD (bvFTD, n = 38), sbvFTD (n = 8), or semantic variant of primary progressive aphasia (svPPA, n = 13), who underwent at least two MRI scans on a 3T scanner. Fifty‐two healthy controls underwent the same protocol. Cortical thickness analyses were performed at baseline and longitudinally to describe cortical atrophy progression.
Results: At baseline, patients with sbvFTD had an intermediate atrophy pattern between bvFTD and svPPA, with right‐predominant temporal pole involvement associated to significant right frontal atrophy. Longitudinally, bvFTD patients were found to progress widely bilaterally, while svPPA continued steady progression restricted to the temporal lobes, and sbvFTD showed progression only in the left temporal lobe with limited further volume loss in the right hemisphere.
Conclusion: Our study has characterized structural neuroimaging hallmarks of each FTD variant and recognized variant‐specific patterns of disease progression. These findings could aid in the identification of imaging biomarkers able to improve FTD diagnosis and prognostic stratification. Moreover, our results singled out sbvFTD as a relatively distinct entity. Funding. Supported by European Research Council (StG‐2016_714388_NeuroTRACK); Foundation Research on Alzheimer Disease; Next Generation EU/National Recovery and Resilience Plan, Investment PE8‐Project Age‐It.
Disclosure: EG Spinelli, A Ghirelli, F Orlandi, V Castelnovo, E Sibilla, F Caso, G Magnani, P Caroppo, S Prioni, C Villa, L Tremolizzo, I Appollonio, F Verde have nothing to disclose. E Canu research support from Italian Ministry of Health (IMH). S Basaia research support from Italian Ministry of Health. G Cecchetti speaker honoraria from Neopharmed Gentili. N Ticozzi consulting services for Amylyx Pharmaceuticals, Zambon Biotech SA and lectures for Italfarmaco; funding from IMH and AriSLA. V Silani consulting services and/or speaking activities for AveXis, Cytokinetics, Italfarmaco; and research support from IMH, AriSLA, and E‐Rare Joint Transnational Call. M Filippi consulting or speaking activities or advisory boards for Alexion, Almirall, Biogen, Bayer, Bristol‐Myers Squibb,Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA; scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol‐Myers Squibb, Lilly, Novartis, Sanofi‐Genzyme; research support from Biogen Idec, Merck‐Serono, Novartis, Roche, IMH, Italian Ministry of University and Research, and FISM. F Agosta received speaker honoraria from Biogen Idec, Italfarmaco, Roche, Zambon and Eli Lilly, and has received research supports from IMH, Italian Ministry of University and Research, ARiSLA, ERC, EU Joint Programme – Neurodegenerative Disease Research, and Foundation Research on Alzheimer Disease.
EPO‐014
Clinical and neuroanatomical characterization of the semantic behavioural variant of frontotemporal dementia
E. Spinelli 1; A. Ghirelli1; E. Canu2; S. Basaia2; V. Castelnovo2; G. Cecchetti3; E. Sibilla2; G. Magnani4; F. Caso4; P. Caroppo5; S. Prioni5; C. Villa5; L. Tremolizzo6; I. Appollonio6; F. Verde7; N. Ticozzi8; V. Silani8; F. Agosta1; M. Filippi9
1Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 3Neurophysiology Service, Neurology Unit, and Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute Milan, Italy; 4Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; 5Fondazione IRCCS Istituto Neurologico Carlo Besta, Unit of Neurology 5 – Neuropathology, Milan, Italy; 6Neurology Unit, “San Gerardo” Hospital and University of Milano‐Bicocca, Monza, Italy; 7Department of Neurology and Laboratory of Neuroscience, IRCCS Istituto Auxologico Italiano, Milan, Italy; 8Department of Neurology and Laboratory of Neuroscience, IRCCS Istituto Auxologico Italiano, and “Dino Ferrari” Center, Department of Pathophysiology and Transplantation, Università degli Studi di Milano, Milan, Italy; 9Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: Semantic behavioral variant of frontotemporal dementia (sbvFTD) is a neurodegenerative condition presenting with specific behavioral and semantic derangements and predominant atrophy of the right anterior temporal lobe (rATL). Our objective was to evaluate clinical, neuropsychological, neuroimaging and genetic features of an Italian sbvFTD cohort, defined according to recently proposed guidelines, compared to semantic variant primary progressive aphasia (svPPA) and behavioral variant FTD (bvFTD) patients.
Methods: Fifteen sbvFTD, 63 bvFTD and 25 svPPA patients and 40 healthy controls were enrolled. Patients underwent clinical, cognitive evaluations and brain MRI. Emerging symptoms of sbvFTD patients were recorded. Grey matter atrophy was investigated using voxel‐based morphometry.
Results: sbvFTD patients developed early person‐specific semantic knowledge loss (67%), object semantic loss (67%), complex compulsions and rigid thought process (60%). Sequentially, additional behavioral symptoms emerged (apathy/inertia, loss of empathy, anxiety, suspiciousness). sbvFTD patients showed sparing of attentive and executive functions, especially compared to bvFTD, and better performance at language tests, compared to svPPA. sbvFTD had predominant rATL atrophy, almost specular to svPPA. Three sbvFTD patients showed pathogenic genetic variants.
Conclusion: We applied sbvFTD diagnostic guidelines to an Italian cohort, demonstrating that the presence of two out of three core diagnostic criteria (person‐specific semantic knowledge loss, mental rigidity and loss of empathy), along with the evidence of preserved executive functions and frontal lobes at MRI should prompt a diagnosis of sbvFTD. Funding. This study was supported by European Research Council (StG‐2016_714388_NeuroTRACK); Foundation Research on Alzheimer Disease; Next Generation EU/National Recovery and Resilience Plan, Investment PE8‐Project Age‐It.
Disclosure: EG Spinelli, A Ghirelli, V Castelnovo, E Sibilla, G Magnani, F Caso, P Caroppo, S Prioni, C Villa, L Tremolizzo, I Appollonio, F Verde have nothing to disclose. E Canu research support from Italian Ministry of Health (IMH). S Basaia research support from Italian Ministry of Health. G Cecchetti speaker honoraria from Neopharmed Gentili. N Ticozzi consulting services for Amylyx Pharmaceuticals, Zambon Biotech SA and lectures for Italfarmaco; funding from IMH and AriSLA. V Silani consulting services and/or speaking activities for AveXis, Cytokinetics, Italfarmaco; and research support from IMH, AriSLA, and E‐Rare Joint Transnational Call. F Agosta received speaker honoraria from Biogen Idec, Italfarmaco, Roche, Zambon and Eli Lilly, and has received research supports from IMH, Italian Ministry of University and Research, ARiSLA, ERC, EU Joint Programme – Neurodegenerative Disease Research, and Foundation Research on Alzheimer Disease. M Filippi consulting or speaking activities or advisory boards for Alexion, Almirall, Biogen, Bayer, Bristol‐Myers Squibb,Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA; scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol‐Myers Squibb, Lilly, Novartis, Sanofi‐Genzyme; research support from Biogen Idec, Merck‐Serono, Novartis, Roche, IMH, Italian Ministry of University and Research, and FISM.
EPO‐015
Gantenerumab for early Alzheimer's disease: A systematic review and meta‐analysis
A. Menegaz de Almeida1; M. G. H. S. J. Leite2; L. Moreira Lopes3; P. L. Gomes Lima4; M. L. Siegloch Barros4; S. L. Rocha Pinheiro5; Í. Barros Andrade 6; P. Viana7; V. Morbach8; R. de Oliveira9; A. C. Pinheiro10
1Federal University of Mato Grosso, Sinop, Brazil; 2Santa Marcelina University, São Paulo, Brazil; 3Sciences Medical School of Santos, Santos, Brazil; 4Federal University of Acre, Rio Branco, Brazil; 5Federal University of Bahia, Anísio Teixeira, Brazil; 6Faculdade de Saúde Santo Agostinho, Vitória da Conquista, Brazil; 7Extremo Sul University, Criciúma, Brazil; 8Feevale University, Novo Hamburgo, Brazil; 9Department of Medicine, Federal University of Mato Grosso, Sinop, Brazil, 10Department of Neurology, Massachusetts General Hospital, Brigham and Woman's Hospital, Harvard Medical School, Boston, MA
Background and Aims: Gantenerumab is a monoclonal antibody targeting amyloid β protein (Aβ) in early Alzheimer's disease (AD). Hence, we sought to evaluate gantenerumab safety and efficacy in early AD patients.
Methods: MEDLINE, Embase, and Cochrane databases were systematically searched until December 02, 2023. Data were examined using the Mantel‐Haenszel method and 95% confidence intervals (CIs). Heterogeneity was assessed using I 2 statistics. Meta‐regression analysis was conducted to evaluate a possible link between baseline Clinical Dementia Rating Scale – Sum of Boxes (CDR‐SB) and amyloid‐related imaging abnormalities (ARIA) at follow‐up. R, version 4.2.3, was used for statistical analysis.
Results: A total of 4 RCTs and 2848 patients were included, of whom 1580 (55%) received subcutaneous gantenerumab. Concerning clinical scores, the placebo group achieved better rates of change in the Disease Assessment Scale (ADAS‐Cog13) (SMD −0.1113; 95% CI −0.1942 to −0.0283; p = 0.009; I 2 = 0%). Gantenerumab was strongly associated with the occurrence of ARIA‐E and ARIA‐H: (19.67% vs. 2.31%; RR 9.46; 95% CI 5.55–16.11; p = < 0.000001; I 2 = 10%) and (21.95% vs. 12.38%; RR 1.79; 95% CI 1.50–2.13; p = < 0.000001; I 2 = 0%), respectively. Only injection site events showed a statistically significant difference between groups, tending towards the placebo group (17.64% vs. 7.53%; RR 2.23; 95% CI 1.81–2.73; p = < 0.000001; I 2 = 61%). The meta regression between baseline CDR‐SB and ARIA showed no significant link.
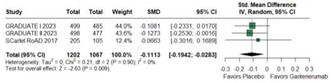
ADAS‐Cog 13
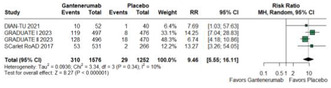
ARIA‐E
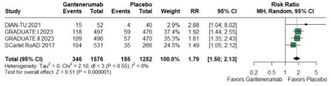
ARIA‐H
Conclusion: In this meta‐analysis, consistent results suggest that gantenerumab is not safe and efficient for early AD, showing no improvement in clinical scores for AD and being associated with the occurrence of ARIA‐E, ARIA‐H, and injection site events.
Disclosure: The authors declare that they have no disclosure.
Autonomic nervous system diseases 1
EPO‐016
Haemodynamic determinants of supine hypertension in patients with classical orthostatic hypotension
A. van der Stam 1; B. Gagaouzova2; F. Kerkhof2; I. van Rossum2; S. Shmuely1; R. Reijntjes2; M. van Houwelingen3; R. Thijs2; G. van Dijk2
1Department of Neurology, Donders Institute for Brain, Cognition and Behavior, Radboud University Medical Center, Nijmegen, The Netherlands; 2Department of Neurology, Leiden University Medical Center, Leiden, The Netherlands; 3Department of Experimental Cardiology, Erasmus Medical Center, Rotterdam, The Netherlands
Background and Aims: The underlying mechanisms of, and relation between supine hypertension (SH), classical orthostatic hypotension (cOH), and the severity of the orthostatic systolic blood pressure (SBP) fall are currently largely unknown. We investigated the relative importance of heart rate (HR), stroke volume (SV) and total peripheral resistance (TPR) to these issues.
Methods: Tilt table tests recorded with beat‐to‐beat BP recordings (Finapres NOVA and BMEye Nexfin) were assessed and divided in four groups: Controls without SH (SH−; i.e., supine SBP < 140 mmHg) (n = 19), controls/SH+ (n = 61), cOH/SH− (n = 30) and cOH/SH+ (n = 50). We used linear regression to relate cOH severity to supine SBP, and used the logratio method to analyse the relative contributions of hemodynamic parameters to upright BP. We used a p value of 0.003 after Bonferroni correction.
Results: In both patients and controls high supine SBP was caused by high TPR (Figure 1). The orthostatic SBP fall increased with supine SBP in patients (Figure 2). The main difference in the upright position between cOH/SH+ and cOH/SH− patients was TPRLR, which was higher in cOH/SH− than in cOH/SH+ (p < 0.002). A secondary difference was that SVLR decreased more in cOH/SH− than in cOH/SH+ (p < 0.003) (Figure 3). HRLR had similar relative contributions to orthostatic SBP (p = 0.028) (Figure 3).
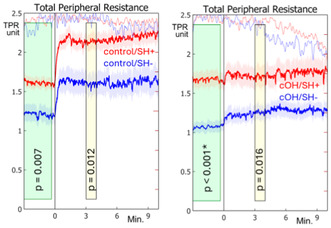
FIGURE 1 Measured total peripheral resistance (TPR) over time. The black line indicates completion of tilt. Both orthostatic hypotension (cOH) patients and controls are divided by the SBP>140 mmHg criterion for supine hypertension (SH). * = Significant.
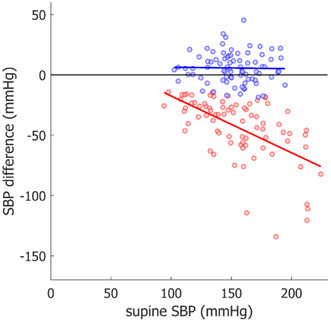
FIGURE 2 Relationship between the blood pressure fall three minutes after tilt and the supine blood pressure for controls (blue) and orthostatic hypotension patients (red).
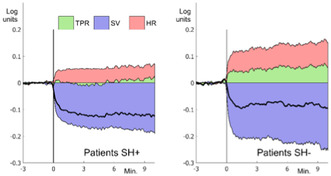
FIGURE 3 Relative contributions of the three hemodynamic parameters to orthostatic blood pressure. Orthostatic hypotension patients are divided by the SBP>140 mmHg criterion for supine hypertension (SH). The black line shows the mean arterial pressure.
Conclusion: High supine TPR explained SH; a failure to increase TPR explained the orthostatic SBP fall. The latter was likely due to autonomic failure, which can however not directly explain high supine TPR. Explaining this requires other mechanisms, such as residual sympathetic tone, denervation supersensitivity or humoral factors.
Disclosure: AvdS was supported by MJFF grant MJFF‐020200.
EPO‐017
Morphological and functional assessment of the vagus nerve in multiple sclerosis
A. Abicic 1; I. Adamec2; M. Krbot Skorić2; A. Junaković2; A. Karić2; M. Habek2
1Department of Neurology, General Hospital Zabok, Zabok, Croatia; 2Department of Neurology, University Hospital Centre Zagreb, Zagreb, Croatia
Background and Aims: Autonomic dysfunction (AD) has been linked to vagal nerve atrophy in some neurodegenerative diseases, but atrophy of the vagus nerve in multiple sclerosis (MS) and its association with AD has not been studied. The aim of this study was to determine the relationship between the cross‐sectional area (CSA) of the vagus nerve and parasympathetic function in people with MS (pwMS) and healthy controls (HC).
Methods: 40 pwMS (65.0% females, 36.03 ± 9.08 years) and 39 HC (79.5% females, 38.23 ± 7.19 years) were enrolled. The subjects underwent an ultrasound of the vagus nerve and testing of the parasympathetic nervous system was evaluated with the respiratory sinus arrhythmia (RSA), Valsalva ratio (VR) and heart rate variability (HRV).
Results: The mean vagal CSA in pwMS was 1.98 ± 0.44 mm2 on the right and 1.72 ± 0.39 mm2 on the left side. The mean vagal CSA in the HC group was 2.08 ± 0.53 mm2 on the right and 1.73 ± 0.36 mm2 on the left side. There was no significant difference between the two groups in right (p = 0.33) or left (p = 0.90) vagal CSA. In the HC, there was significant correlation between right vagal CSA and RSA (rp = 0.330, p = 0.040), and right‐left vagal CSA ratio and RSA (rp = 0.345, p = 0.031). The right‐left vagal CSA ratio correlated with the LF/HF (rp = 0.322, p = 0.049). No correlation was observed in pwMS.
Conclusion: The ultrasound characteristics of the vagal nerves correlate with the parasympathetic nervous system measures in HC. This correlation was not observed in pwMS.
Disclosure: Nothing to disclose.
EPO‐018
Peripheral visual exploration in postural tachycardia syndrome is reduced during standing: The cause of tunnel vision?
B. Rodriguez 1; L. Pantano1; T. Nef2; R. Müri2; W. Z'Graggen1
1Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland; 2Gerontechnology and Rehabilitation Group, ARTORG Center for Biomedical Engineering Research, University of Bern, Bern, Switzerland
Background and Aims: Patients with postural tachycardia syndrome (POTS) report strongly disturbing visual symptoms such as tunnel vision and focusing problems in everyday life, but this phenomenon has not yet received any attention from research. The aim of this study was to characterise visual symptoms in POTS and to investigate possible underlying pathophysiological mechanisms.
Methods: Fifteen patients with POTS and 15 healthy controls were included in this study. Hemodynamics, (visual) symptoms, eye movements and pupil diameter were measured in all participants during free exploration of images in the supine position and during 60° head‐up tilt using continuous cardiovascular monitoring, subjective symptom assessment and eye tracking.
Results: During head‐up tilt, patients with POTS showed a reduced number and duration of fixations as well as a reduced number, peak velocity and amplitude of saccades compared to their supine eye movements and to those of healthy subjects. This reduction in visual exploration occurred mainly in the peripheral two‐thirds of the visual field and paralleled the onset of subjective visual symptoms. There were no differences in the saccade main sequence between the two groups in either body position. The pupil diameter of patients increased excessively during head‐up tilt.
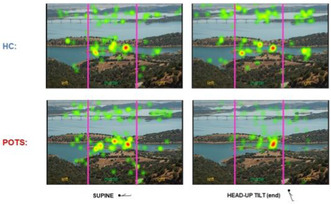
Illustration of fixations. The darker the marking, the more strongly the area was fixated. The image was divided into three areas of interest, whereby the values of the left and right areas were cumulated and used as "periphery" for further analysis.
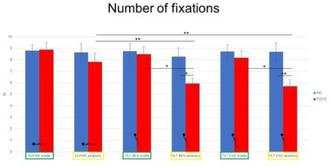
Bar graphs showing the number of fixations of POTS (red) and healthy controls (blue) in the supine position, during the first and last half of a ten‐minute 60° head‐up tilt. Values are given as means ± S.E.M. *p ≤ 0.05, **p ≤ 0.01.

Saccade main sequence (relationship of saccade peak velocity (degrees/second) and amplitude (degrees)) shown for POTS (red) and healthy controls (blue) in the supine position, during the first and last half of a ten‐minute 60° head‐up tilt.
Conclusion: Patients with POTS have a reduced exploration of the peripheral visual field exclusively in the upright body position, possibly leading to tunnel vision. Since the saccade main sequence was normal in patients in both body positions, the reduction of peripheral visual exploration is likely due to a position‐dependent dysfunction of the frontal eye field.
Disclosure: Nothing to disclose.
EPO‐019
Autonomic dysfunction in people with multiple sclerosis: A 6‐year longitudinal study
B. Ruška 1; L. Crnošija2; I. Adamec2; A. Junaković2; B. Barun2; T. Gabelić2; M. Krbot Skorić2; M. Habek3
1Department of Neurology, Sveti Duh University Hospital, Zagreb, Croatia; 2Department of Neurology, University Hospital Center Zagreb, Zagreb, Croatia; 3School of Medicine, University of Zagreb, Zagreb, Croatia
Background and Aims: The aim of this study was to investigate the evolution of autonomic dysfunction in pwMS over a six‐year follow‐up.
Methods: This was a prospective cohort study in which 121 consecutive pwMS (85 females, age at baseline 32.2 ± 8.7 years) were enrolled at the time of diagnosis and evaluated every two years for six years. ANS symptoms were evaluated with the Composite Autonomic Symptom Score (COMPASS‐31). Heart rate (HR) and blood pressure (BP) responses to the Valsalva maneuver, HR response to deep breathing (RSA), BP response to passive tilt and quantitative sudomotor axon reflex test (QSART) were performed with CNSystems Task Force® Monitor device. The severity and distribution of ANS function was quantified using adrenergic (AI), cardiovagal (CI) and sudomotor (SI) indices of the Composite Autonomic Severity Scale (CASS).
Results: There was no significant change in the frequency of autonomic symptoms measured with COMPASS‐31 over the years (p = 0.454). During the follow‐up, there was a significant progression of autonomic dysfunction (31% of pwMS experienced conversion of the CASS score from 0 at baseline to >0 at year 6, p = 0.038). This difference was mainly driven by progression of parasympathetic (19% of pwMS experienced conversion of the CI from 0 at baseline to >0 at year 6, p = 0.001) and sudomotor (32% of pwMS experienced conversion of the SI from 0 at baseline to >0 at year 6, p = 0.003) dysfunction. Increase in age was an independent predictor of progression of autonomic dysfunction (Exp(B) 1.107, 95% CI 1.038–1.180).
Conclusion: Substantial proportion of pwMS experience progression of autonomic dysfunction over time.
Disclosure: Nothing to disclose.
EPO‐020
Delayed orthostatic hypotension in Parkinson's disease and in the aging general population
B. Calió 1; F. Leys1; G. Matteucci2; N. Campese1; G. Rivasi2; G. Goebel1; G. Testa2; R. Granata1; S. Duerr1; J. Ndayisaba1; K. Radl1; M. Thurner1; K. Seppi1; W. Poewe1; S. Kiechl1; A. Ungar2; G. Wenning1; M. Rafanelli2; A. Fanciulli1
1Department of Neurology, Medical University of Innsbruck, Innsbruck, Austria; 2Department of Geriatrics, Careggi University Hospital, Florence, Italy
Background and Aims: Delayed orthostatic hypotension (dOH) is considered a prodromal form of classic OH (cOH), but its frequency and associated clinical features in Parkinson's disease (PD) and aging individuals are not well known.
Methods: We retrospectively studied individuals with PD and age‐matched aging individuals without parkinsonism referred to the Innsbruck and Florence dysautonomia centers for head‐up tilt‐test under continuous noninvasive blood pressure (BP) monitoring. In both study cohorts, we reviewed the medical records of the 6 months preceding and following the examination for history of syncope and falls.
Results: Two‐hundred thirteen individuals with PD [35% women; 73(69; 76) years of age; 6 (3; 10) years of disease duration] and 213 age‐matched aging individuals [45% women; 73(69; 77) years of age] were included. DOH occurred in 18% of patients with PD and 9% of the aging individuals, and was significantly associated with a diagnosis of PD [OR = 2.69 (95% C.I.: 1.3–5.7), p = 0.010]. Patients with PD had a more severe systolic BP fall during prolonged head‐up tilt with respect to aging individuals (p < 0.001). Syncope and syncope‐related falls history were more frequent in the aging individuals (p < 0.001).
Conclusion: Delayed OH is more common in PD than in aging individuals. In PD, the systolic BP fall drives dOH development and the slow onset of symptoms may reduce the occurrence of syncope‐related falls. Nonetheless, due to the frequency of dOH and its potential progression into cOH, a closer monitoring of the affected individuals should be considered.
Disclosure: Nothing to disclose.
EPO‐021
Long‐term efficacy of antihypotensive drugs for neurogenic OH: Real‐world data in patients with alpha‐synucleinopathies
S. Sajeev 1; G. Chiaro1; S. Johnstone1; G. Ingle1; V. Iodice2
1Autonomic Unit, The National Hospital for Neurology and Neurosurgery, UCLH NHS Trust, London, UK; 2Department of Brain Repair and Rehabilitation, UCL Queen Square Institute of Neurology, University College London, UK
Background and Aims: Treatment of neurogenic orthostatic‐hypotension (nOH) relies on consensus‐based approaches; real‐world data on long‐term efficacy and safety are lacking. We evaluated response to anti‐hypotensives in a longitudinal cohort of patients with synuclein‐related nOH (PAF, PD, DLB and MSA).
Methods: Severity of cardiovascular autonomic failure was assessed with autonomic function testing. Response to medications was measured with a semi‐composite questionnaire assessing the number of falls/month and hospitalizations/trimester, the burden of orthostatic symptoms, quality of life (OHQ, SF‐36, PGI scale) and BP monitoring (with structured diary and ambulatory monitoring). Demographic measures are reported as median + IQR, all other measures as mean ± SD.
Results: 101 patients completed the questionnaire (49‐PAF, 27‐PD, 21‐MSA and 4‐DLB). 61 patients were on long‐term treatment (26 on one, 35 on multiple anti‐hypotensives); 40 on non‐pharmacological measures, due to early‐stage disease, severe supine‐hypertension, immobilization, or medication unresponsiveness. Number of falls and hospital admission were 2 ± 12 and 0.3 ± 1 respectively. The OHQ composite score (range 1–10) was 7.24 ± 1.7. SF36 physical and mental composite scores (range: 0–100) were 33.2 ± 37.5 and 38.9 ± 37.8 respectively. PGI score (range: 1–7) was 4.7 ± 1.4. The magnitude of nOH was 56/27 (±34/19) mmHg in treated patients, compared to 29/6 (±22/11) mmHg in those untreated.
Conclusion: Despite multiple anti‐hypotensive use, two‐thirds of patients were significantly symptomatic with nOH, as corroborated by falls rates and hospital admissions. These findings emphasized the critical nature of nOH, its current gaps in pharmacological management and its profound impact on patients' daily functioning.
Disclosure: Nothing to disclose.
EPO‐022
A systematic review of the effects of LCIG infusion on autonomic symptoms in advanced Parkinson's disease
S. Galli1; L. De Carolis1; E. Bianchini1; M. Alborghetti1; B. Caliò2; P. Pacilio1; A. Fanciulli2; F. Pontieri1; D. Rinaldi 1
1Department of Neuroscience, Mental Health and Sensory Organs (NESMOS), Sapienza University of Rome, Rome, Italy; 2Department of Neurology, Medical University of Innsbruck, Innsbruck, Austria
Background and Aims: Autonomic dysfunction significantly affects Parkinson's disease (PD) patients' quality of life, especially in the advanced stages. Levodopa/carbidopa intestinal gel (LCIG) infusion represents an established therapeutic approach for advanced PD characterized by severe motor complications and is considerably helpful in addressing some non‐motor symptoms (NMS). However, the impact of LCIG on autonomic symptoms remains less elucidated. We conducted a systematic review to investigate the influence of LCIG therapy on autonomic dysfunction in patients with PD.
Methods: Following the PRISMA guidelines, we systematically searched Pubmed for studies reporting autonomic outcome measures in LCIG‐treated PD patients published between January 2005 and June 2023 (Figure 1).
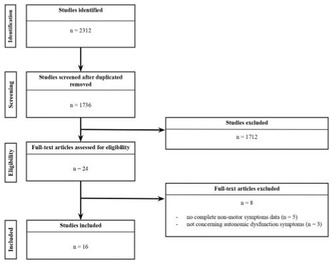
Flowchart of the systematic review process.
Results: Among the 2,312 studies identified, 16 met the inclusion criteria and underwent quality assessment and data extraction, encompassing a cohort of 1,361 patients with Parkinson's disease (PD) (Figure 2). Thirteen studies reported improvement or stability in gastrointestinal, urinary, and cardiovascular symptoms throughout the interventional period. Conversely, one study reported worsening cardiovascular symptoms, while two studies observed worsening urological symptoms. Regarding safety, seven studies reported gastrointestinal (8.4%), urinary (0.5%), cardiovascular (1.1%), and autonomic LCIG‐related AEs.
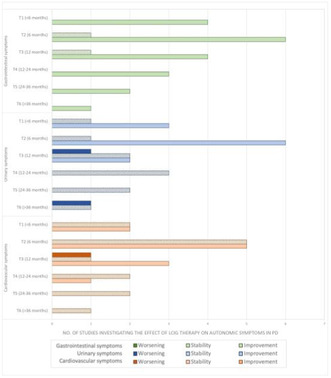
Number of studies reporting improvement, stability, or worsening of gastrointestinal, urinary, and cardiovascular symptoms at each timepoints.
Conclusion: LCIG infusion is relatively safe and may help reduce autonomic symptoms burden in advanced PD.

Proposed mechanisms for LCIG's beneficial effects on autonomic symptoms in PD.
Disclosure: Nothing to disclose.
EPO‐023
Characterize autonomic involvement and its correlation with electrophysiological parameters in various subtypes of GBS
P. Majumdar; A. Das
All India Institute of Medical Sciences, New Delhi
Background and Aims: GBS is an inflammatory demyelinating disorder of peripheral nerves. About 2/3 rd of patients of GBS have autonomic dysfunction. No studies have clearly mentioned type and severity of autonomic dysfunction in different types of GBS.
Methods: This was a prospective cohort study in which 68 patients of GBS underwent clinical workup along with autonomic function testing (heart rate variability with deep breathing, orthostatic blood pressure measurement, isometric handgrip test, cold pressor test and valsalva manoeuvre). The study was done in All India Institute of Medical Sciences, New Delhi. Autonomic function tests were done at two times, at admission and at 15th day. Primary outcome was to determine the predominant pattern of autonomic dysfunction in subtypes of GBS.
Results: 71 patients were screened for eligibility and 68 patients completed the study. At baseline, 79% of patient had dysfunction on laboratory autonomic function tests while only 25% had positive scores on Composite Autonomic Symptom Score (COMPASS‐31). Sympathetic dysfunction was the predominant abnormality accounting for 85.71% patients in AIDP group and 68.18% patients in axonal group (AMAN and AMSAN) combined. There was no correlation of any pattern of autonomic dysfunction with degree of axonal involvement (p = 0.681).
Conclusion: This study showed that sympathetic dysfunction is the predominant pattern of autonomic involvement in GBS patients. No correlation could be found out between types of autonomic dysfunction and variants of GBS/degree of axonal involvement in axonal variants.
Disclosure: Nothing to disclose.
EPO‐024
Nuclear imaging and autonomic biomarkers predict phenoconversion in pure autonomic failure
G. Chiaro 1; R. Alnasser Alsukhni1; G. Ingle1; K. Bhatia2; C. Mathias3; J. Bomanji4; V. Iodice1
1Autonomic Unit, National Hospital for Neurology and Neurosurgery, London, UK; 2Department of Clinical and Movement Neurosciences, UCL Queen Square Institute of Neurology, University College London, London, UK; 3UCL Queen Square Institute of Neurology, Faculty of Brain Sciences, University College London, London, UK; 4Institute of Nuclear Medicine, UCLH NHS Foundation Trust, London, UK
Background and Aims: Abnormal DaTSCAN is a potential biomarker of central nervous system involvement in pure autonomic failure (PAF) and can predict phenoconversion to more widespread alpha‐synucleinopathies. We aimed to describe whether combining DaTSCAN, MIBG cardiac scintigraphy and autonomic biomarkers can help assess likelihood of phenoconversion.
Methods: As part of our longitudinal program on alpha‐synucleinopathies, the Queen Square Autonomic Prodromal Project (QSA‐PRODROMAL), a subgroup of consecutive patients with an initial diagnosis of PAF underwent a multimodal assessment with cardiovascular autonomic function performed with Finapres NOVA, DaTSCAN and cardiac MIBG.
Results: 23 PAF patients with available DaTSCAN and cardiac MIBG were included. Within a median disease duration of 8 (IQR 6–12) years, 6 patients phenoconverted: 2 to Lewy body disorders ([LBD], 1 to Parkinson's disease and 1 to dementia with Lewy bodies), 1 to multiple system atrophy (MSA), and 2 met the research criteria for possible prodromal MSA. Nuclear imaging was abnormal up to 4 years prior to phenoconversion. Both LBD had abnormal DaTSCAN and cardiac MIBG with low supine plasma noradrenaline levels (<200 pg/ml). MSA had abnormal DaTSCAN, normal cardiac MIBG and normal supine plasma noradrenaline levels (>200 pg/mL). The 2 possible prodromal MSA had preserved cardiac innervation and either normal (cerebellar) or abnormal (parkinsonian) DaTSCAN, depending on their clinical phenotype.
Conclusion: The combination of DaTSCAN, cardiac MIBG and catecholamine profiles identified PAF patients at risk of developing other alpha‐synucleinopathies and helped predate their phenoconversion by up to 4 years.
Disclosure: The authors have nothing to disclose.
EPO‐025
Pain subtypes and sleep dysfunction in Parkinson's disease
I. Murasan 1; S. Diaconu1,2; D. Rusu1,2; B. Opritoiu1,2; L. Ungureanu1,2; B. Ciopleias1,2; C. Kakucs1,2; C. Falup‐Pecurariu1,2
1Department of Neurology, County Clinic Hospital, Brasov, Romania; 2Faculty of Medicine, Transilvania University, Brasov, Romania
Background and Aims: In Parkinson's disease (PD), sleep is often affected, pain being among the possible causes. This can lead to difficulties in initiating and maintaining sleep, one of the consequences being sleep fragmentation. We aimed to characterize the link between pain and sleep dysfunction in patients with Parkinson's disease.
Methods: 131 PD patients were enrolled in this case‐control study. Pain domains (according to the King's Parkinson's Disease Pain Scale‐KPPS) were analyzed according to the presence of sleep disturbances. Based on a Pittsburgh Sleep Quality Index (PSQI) score >5, patients with PD were considered "bad sleepers", and those with a score ≤5 were considered "good sleepers".
Results: 33 (25.19%) patients fell into the "good sleepers" category, and 98 (74.8%) into the "bad sleepers" category. "Bad sleepers" patients presented more significant pain than "good sleepers" for all the component domains of the KPPS scale, the results for the following domains being statistically significant: musculoskeletal pain (5.48 ± 3.50 vs. 2.70 ± 2.67, p < 0.001), chronic pain – respectively central pain (1.19 ± 2.01 vs. 0.15 ± 0.71, p = 0.004), nocturnal pain – respectively pain in relation to akinesia (2.26 ± 2.74 vs. 0.64 ± 1.22, p = 0.001) and radicular pain (4.35 ± 4.20 vs. 2.45 ± 3.55, p = 0.022).
Conclusion: The majority of the patients assessed have a diminished quality of sleep. In their case, pain is more prominent than in individuals with uninterrupted sleep. Focusing on treatment of pain would potentially improve the sleep of these PD patients.
Disclosure: Nothing to disclose.
EPO‐026
Circadian rhythm in patients with hereditary transthyretin amyloidosis and asymptomatic mutation carriers
L. Sander 1; G. Chiaro2; A. Torrente3; G. Ingle2; A. Carr4; C. Whelan5; J. Gillmore5; M. Reilly4; C. Mathias6; V. Iodice1
1Autonomic Unit, The National Hospital for Neurology and Neurosurgery, London, UK; Department of Brain, Repair and Rehabilitation, University College London Queen Square Institute of Neurology, London, UK; 2Autonomic Unit, The National Hospital for Neurology and Neurosurgery, London, UK; 3Autonomic Unit, The National Hospital for Neurology and Neurosurgery, London, UK; Department of Biomedicine, Neuroscience and Advanced Diagnostics (Bi.N.D.), University of Palermo, Palermo, Italy; 4Centre for Neuromuscular Diseases, Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology and the National Hospital of Neurology and Neurosurgery, London, UK; 5National Amyloidosis Centre, Division of Medicine, University College London, London, UK; 6Department of Brain, Repair and Rehabilitation, University College London Queen Square Institute of Neurology, London, UK
Background and Aims: Hereditary or variant transthyretin amyloidosis (ATTRv) is a life‐threatening disease with effective disease modifying treatments (DMT). Cardiovascular autonomic failure is a key feature. Abnormal circadian blood pressure (BP) rhythm might represent a risk factor for cardiovascular events. This study evaluates BP profile in ATTRv patients and carriers.
Methods: 97 patients with ATTRv and 12 TTR mutation carriers underwent ambulatory 24h BP measurements (ABPM; 29% females, mean age 58y, range 28–78 y, 43% T60A mutation). Dipping profile was defined according to the consensus criteria. Autonomic function testing (AFT) included tilt table/standing/pressor tests, heart rate responses to Valsalva Manoeuvre and deep breathing using Finapres NOVA.
Results: 54/97 patients were on treatment affecting BP (22 on pressor agents, 39 on antihypertensives), carriers had no treatments affecting BP. 74/109 subjects showed an abnormal dipping profile: 53 had reduced dipping, 21 were non‐ or reversed dippers. 4/74 subjects were carriers (all reduced dippers): three had mild AFT impairment, one was normal. 6/8 carriers with normal ABPM showed abnormal AFT. Only two carriers and two patients had unremarkable autonomic assessment throughout. No significant dipping profile difference was found at first assessment in patients with (12/97) or without DMT.
Conclusion: Pathologic BP profiles are common in ATTRv and may be an early feature in certain carriers. Both ABPM and AFT are needed to detect subtle autonomic impairment. ABPM might be a useful screening tool but does not allow for quantitative parasympathetic/sympathetic assessment requiring formal AFT. Longitudinal studies are needed to investigate changes in circadian rhythm and their response to DMT.
Disclosure: LS holds a grant from the University of Basel, Switzerland. GC, AT, GTI, CA, CJW, MMR, CJM: nothing to disclose. JDG provides consultancy for Alnylam, AstraZeneca, Bridgebio, Ionis, Intellia and ATTRalus. VI is supported by the National Institute for Health Research, University College London Hospitals Biomedical Research Centre.
EPO‐027
Sympathetic dysfunction as an early autonomic indicator in Parkinson's disease without orthostatic hypotension
J. Park 1; L. Okamoto2; I. Biaggioni2; B. Kim1
1Department of Neurology, Korea University Medicine, Seoul, Korea; 2Division of Clinical Pharmacology, Department of Medicine, Vanderbilt University Medical Center, Nashville, TN, USA
Background and Aims: This study aimed to evaluate the characteristics of autonomic dysfunction in drug‐naïve patients with early‐stage PD without orthostatic hypotension (OH) by analyzing Valsalva maneuver (VM) parameters.
Methods: Drug‐naïve patients without orthostatic hypotension (n = 61) and controls (n = 20) were retrospectively analyze. The patients were subcategorized into early‐PD (n = 35) and mid‐PD (n = 26) groups based on the Hoehn and Yahr staging. VM parameters driven by Finapres®, including changes in systolic blood pressure at late phase 2 (∆SBPVM2), ∆HRVM3, Valsalva ratio (VR), pressure recovery time, adrenergic baroreflex sensitivity, and vagal baroreflex sensitivity, were assessed.
Results: In the early‐PD group, ∆SBPVM2, a marker of sympathetic function, was significantly lower compared to that in controls (risk ratio = 0.95, p = 0.027). Receiver operating characteristic (ROC) curve analysis showed an optimal cutoff value of −10 mmHg for ∆SBPVM2 (p = 0.002, area under the curve [AUC]: 0.737) and 17 mmHg for ∆DBPVM2 (p = 0.002, AUC: 0.736). VR and age exhibited an inverse relationship with Unified Parkinson's Disease Rating Scale Part 3 scores (VR: p = 0.038, β = −28.61; age: p = 0.027, β = 0.35) in the multivariable regression analysis.
Conclusion: The ∆BPVM2 parameter of the VM may help detect autonomic nervous system involvement in early‐PD without OH. Our results suggest that sympathetic dysfunction is an early manifestation of autonomic dysfunction in patients with PD.
Disclosure: Nothing to disclose.
EPO‐028
Longitudinal assessment of sudomotor dysregulation in amyotrophic lateral sclerosis: A multimodal functional study
R. Dubbioso 1; V. Provitera2; M. Nolano2
1Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples Federico II, 2stituti Clinici Scientifici Maugeri IRCCS, Skin Biopsy Lab, Neurological Rehabilitation Unit of Telese Terme Institute
Background and Aims: Among autonomic complaints, sudomotor symptoms have been described in approximately one‐quarter of patients with amyotrophic lateral sclerosis (ALS). However, no study has systematically investigated their correlations with the onset and severity of the disease, as well as progression over time. Here we used a multimodal approach to answer these questions in a large cohort of ALS patients
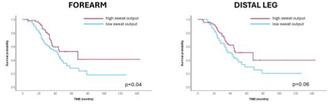
Methods: Patients underwent functional assessment of sudomotor dysfunction by clinical questionnaires and dedicated instruments, such as sympathetic‐skin‐response (SSR) and dynamic‐sweat‐test (DST) recorded at upper and lower limbs at recruitment, after 6 and 12 months.
Results: ALS patients (n = 125), compared with HC (n = 30), complained of more thermoregulatory symptoms (p = 0.001), with a significant reduction in sweat output at DST and SSR amplitude at upper and lower limbs (all p < 0.05). Across clinical stages, patients displayed a significant reduction in overall sweat output (all p < 0.02), a result confirmed by longitudinal study (p < 0.001). Bulbar onset patients showed more autonomic symptoms and thermoregulatory disturbances than spinal onset patients, interestingly functional study disclosed significant difference for SSR, but not for DST between the two groups, suggesting an impairment of central‐brainstem circuits underlying thermoregulatory dysfunction in the bulbar phenotype. Finally, survival analysis showed that reduction of total sweat output at upper limb was significantly associated with poor prognosis (p = 0.04).
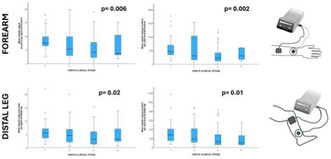
DYNAMIC SWEAT TEST ACROSS CLINICAL STAGES IN ALS PATIENTS
Kaplan‐Meier curves of survival probability of ALS patients stratified according to the total sweat output at the dynamic sweat test
Conclusion: Sudomotor disturbance is part of the non‐motor symptoms of ALS patients, worsening in parallel with motor disability and being more pronounced in bulbar phenotype. Functional assessment of sudomotor dysregulation could be considered as a potential biomarker of disease progression in ALS.
Disclosure: None.
EPO‐029
Association of fibromyalgia severity with patients' mood, sleep quality, quality of life and autonomic dysfunction
R. Singh 1; N. Rai2; J. Rai3; A. Pathak3
1Professor, Department of Physiology, AIIMS Bhopal; 2Visiting faculty, Department of Neurology, AIIMS Bhopal; 3JRF, Department of Physiology, AIIMS Bhopal
Background and Aims: Fibromyalgia syndrome is a musculoskeletal disorder characterized by widespread pain. Pain limits their daily activities, affecting their mood and quality of life. Autonomic derangements have also been shown to be associated with FMS. This study was done to explore the association of autonomic dysfunction, sleep quality and mood with increasing severity of fibromyalgia and its impact on their quality of life
Methods: Hundred adult fibromyalgia patients, as per ACR 2010 criteria, were evaluated for sleep quality, Quality of life, Pain, Mood, and FMS severity using validated questionnaires. They were also evaluated for autonomic functions using heart rate variability and Ewing's battery of tests.
Results: Pain scores on VAS were 6.80 ± 1.58 and 54.10 ± 14.33 on global pain scale. Mean FIQR score was 50.62 ± 13.68, poor sleep quality. Mean depression, anxiety, and stress scores as assessed by DASS‐21 were 10.04 ± 4.59, 8.33 ± 4.48, and 10.75 ± 4.66, respectively. Autonomic dysfunction was observed in less than 50% of patients, but no significant correlation was found between FMS severity and level of AD. An increasing trend of depression, anxiety, stress, was observed with increase in FMS severity. Sleep quality and quality of life deteriorated with increasing severity of FMS.
Conclusion: Pain increased with increasing severity of FMS but there is no association of FMS severity with autonomic dysfunction. There is a deterioration in mood, sleep quality as well as quality of life of patients with increasing severity. The causal association of autonomic dysfunction observed in a few of the patients needs further exploration in a follow‐up study.
Disclosure: Nothing to disclose.
EPO‐030
Autonomic function as predictor of cognitive impairment following deep brain stimulation in Parkinson's disease
V. Cabreira; M. Rosas; E. Azevedo; P. Castro
Neurology Department, Centro Hospitalar Universitario de Sao Joao, Porto, Portugal
Background and Aims: Parkinson's disease (PD) affects over 4 million people older than 50. While deep brain stimulation (DBS) is an established treatment for motor complications in PD, mechanisms explaining cognitive dysfunction post‐DBS remain incompletely understood. Our aim is to investigate whether baseline autonomic function is associated with cognitive impairment post‐DBS in PD.
Methods: Prospective cohort study. STN‐DBS surgery candidates were recruited between 2016 and 2019, and submitted to baseline neurological, autonomic (non‐invasive Finometer device (Finapres) and 3‐lead ECG), and comprehensive neuropsychological assessments. A follow‐up autonomic and cognitive assessment was conducted 6–12 months post‐surgery. An adaptation of the Ewing battery of autonomic tests was followed. The high frequency component of RRi variability (HFRR) (parasympathetic tone), the low frequency component of SAP variability (LFSAP) (sympathetic tone) and baroreceptor gain were used for analysis. Cognitive change scores (T1‐T2) were computed and assumed as dependent variable in a regression model, using baseline demographics and quantitative scores on autonomic non‐invasive tests as independent variables.
Results: 38 patients were included. Phonetic verbal fluency (p = 0.013), Frontal Assessment Battery (FAB) (p = 0.008) and Trail Making test part B (p = 0.035) deteriorated post‐DBS. LFSAP was associated with a worse FAB score post‐DBS, even after adjustment for age and disease duration (p = 0.022) (Figure 1). Both variables were correlated (r = 0.416; p = 0.035). This seems independent from a DBS effect on autonomic function.
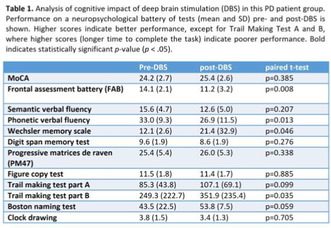
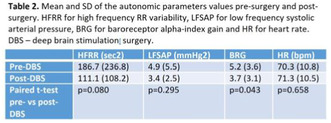
Conclusion: The identification of treatable targets and useful biomarkers of cognitive dysfunction after DBS helps identifying whose patients are specifically vulnerable for accelerated cognitive decline post‐DBS, allowing for better patient selection and prognostic information.
Disclosure: Nothing to disclose.
Cerebrovascular diseases 1
EPO‐031
Aetiology of index and recurrent ischemic events in patients treated with short‐term DAPT: Data from the READAPT study
F. De Santis1; R. Ornello1; E. De Matteis1; M. Foschi1; M. Romoli2; T. Tassinari3; V. Saia3; S. Cenciarelli4; C. Bedetti4; B. Censori5; V. Puglisi5; M. Guarino6; V. Barone6; M. Zedde7; I. Grisendi7; M. Diomedi8; M. Bagnato8; M. Petruzzellis9; V. Inchingolo10; M. Cappellari11; P. Candelaresi12; R. Giuseppe13; D. Toni14; S. Ricci4; S. Sacco1
1Department of Biotechnological and Applied Clinical Sciences, University of L'Aquila, L'Aquila, Italy; 2Department of Neuroscience, Maurizio Bufalini Hospital, AUSL Romagna, Cesena, Italy; 3Department of Neurology, Santa Corona Hospital, Pietra Ligure, Italy; 4Department of Neurology, Città di Castello Hospital, Città di Castello, Italy; 5Department of Neurology, ASST Cremona Hospital, Cremona, Italy; 6IRCCS Istituto delle Scienze Neurologiche di Bologna, Department of Neurology, Policlinico S.Orsola‐Malpighi, Bologna, Italy; 7Department of Neurology, AUSL‐IRCCS di Reggio Emilia, Reggio Emilia, Italy; 8Department of Systems Medicine, Tor Vergata University Hospital, Rome, Italy; 9Department of Neurology and Stroke Unit, "F. Puca" AOU Consorziale Policlinico, Bari, Italy, 10Department of Neurology, Casa sollievo della sofferenza, San Giovanni Rotondo, Italy; 11Department of Neuroscience, Azienda Ospedaliera Universitaria Integrata Verona, Verona, 12Department of Neurology and Stroke Unit, AORN Antonio Cardarelli, Naples, Italy, 13Department of Neurology, Di Venere Hospital, Bari, Italy, 14Department of Human neurosciences, University of Rome La Sapienza, Rome, Italy
Background and Aims: It is unclear whether the aetiology of minor stroke or TIA affects the effectiveness of short‐term dual antiplatelet treatment (DAPT). This study aims to analyse the aetiology of first and recurrent events and their predictive value in a real‐world population of patients treated with DAPT.
Methods: The real‐life study on short‐term DAPT in Patients with ischemic stroke or TIA (READAPT) prospectively included, from February 2021 to February 2023, patients with minor stroke or high‐risk TIA receiving DAPT. We determined the aetiology of index and recurrent cerebral ischemic events. Cox regression analysis identified predictors of ischaemic recurrence.
Results: Among 1920 patients with ischaemic stroke or TIA (65.4% male, median age 72 years) the index event was undetermined in 830 cases (43.2%), lacunar in 534 (27.8%), atherothrombotic in 452 (23.5%) and other determined cause in 104 (5.4%). Sixty‐four patients (3.3%) had a 90‐day recurrent ischaemic stroke or TIA. There were no differences among the different aetiologic groups in recurrent events. Among the 64 patients with recurrences, the distribution of aetiologies was different for the recurrent event as compared to the index events (undetermined 46.9% vs 34.4% large vessel 29.7% vs 21.8%; lacunar 18.8% vs 31.2%; other 4.7% vs 6.3%; cardioembolic 0 vs 6.3%; p = 0.001).
Conclusion: Our data suggest that there is no difference in the risk of recurrent events according to stroke aetiology of the index event in patients treated with short‐term DAPT. Recurrent events have a different aetiological distribution of index events.
Disclosure: Nothing to disclose.
EPO‐032
Exploring the prognostic role of fibrinogen in ischemic stroke
A. Maruccia 1; M. Pugliatti2; F. Colucci2
1Residency School of Neurology, Department of Neuroscience and Rehabilitation, University of Ferrara, Italy; 2Department of Neuroscience and Rehabilitation, University of Ferrara, Italy; S. Anna University Hospital, Ferrara, Italy
Background and Aims: Several biomarkers might play a prognostic role in stroke. We explored the prognostic role of plasma fibrinogen levels (PFL) at stroke onset on residual disability and risk of hemorrhagic infarction in incident patients with ischemic stroke (IS).
Methods: Historical cohort study design. Data on comorbidities, National Institutes of Health Stroke Scale (NIHSS) on admission, PFL at stroke onset (<300 mg/dL, >=300 mg/dL) and modified Rankin Scale (mRS) before and after 3 months were collected, as well as hemorrhagic conversion among patients treated with Intravenous Thrombolysis (IVT). ‘mRS difference’ was computed between mRS at 3‐months after stroke and onset. ANCOVA and logistic regression were used.
Results: 241 men and 203 women aged 66.9 ± 13.1 and 72.1 ± 14.2 years, respectively, were enrolled. PFL directly correlated with age at stroke onset (p = 0.043). No difference in the distribution of PFL by site of lesion, TOAST and Oxfordshire Community Stroke Project classification, indication to thromboarteriectomy and NIHSS were detected. Inverse association was found between PFL and IVT indication [aOR = 0.46 (95% CI: 0.30, 0.72, p = 0.001)]. In IVT treated patients, mean mRS difference was higher in subjects with high PFL after adjusting for age, onset NIHSS, diabetes mellitus, smoking habit (1.39 vs 1.33, p = 0.000013). No association of PFL with hemorrhagic infarct conversion was found.
Conclusion: In IS patients, high PFL are associated to reduced indication to IVT and increased disability at 3 months after stroke. The prognostic role of PFL at stroke onset may depend on age and NIHSS at onset. PFL was not associated with an increased risk of post‐treatment hemorrhagic infarction.
Disclosure: Nothing to disclose.
EPO‐033
Diagnostic utility of Vessel Wall MR Imaging in patients with Acute Ischemic Stroke
A. Mohan 1; M. Srivastava1; M. Salunkhe1; V. Goel2; R. Bhatia1; A. Garg2; L. Joseph2; S. Jain2; M. Singh1; A. Pandit1; V. VY1; R. Rajan1; A. Gupta1
1Department of Neurology, All India Institute of Medical Sciences, New Delhi, India; 2Department of Neuroimaging and Interventional Neuroradiology, All India Institute of Medical Sciences, New Delhi, India
Background and Aims: There is a need for better investigations to elucidate the etiology of stroke. High‐Resolution Vessel Wall MRI is emerging imaging technique used to help understand the etiopathogenesis of acute ischemic stroke (AIS). Studies describing various findings have not yet clarified the exact utility of VW‐MRI to subtype AIS. Current study was undertaken to evaluate the diagnostic utility of VW‐MRI in patients with AIS.
Methods: A single‐centre, prospective study recruited patients with AIS within 30 days. A team of stroke neurologists classified the etiology of AIS before and after VW‐MRI. Subsequent statistical analysis was done to look for the proportion of patients with a change in etiological classification before and after VW‐MRI and factors associated with the same.
Results: A total of 111 patients were recruited with a median age of 50.5 years (IQR: 38–60 years) and 72.4 % of the study population were males. The incorporation of VW‐MRI resulted in change in etiological classification in 38 out of 111 (34.3%) (p = 0.0001) patients. A baseline etiological classification of undetermined as per traditional luminal imaging modalities was found to be a strong predictor of change in etiological classification post VW‐MRI (OR: 38.7; 95% CI: 2.7–555.7)
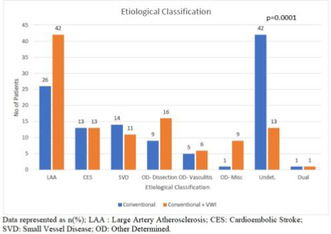
FIGURE Etiological Classification Before and After Vessel Wall MR Imaging
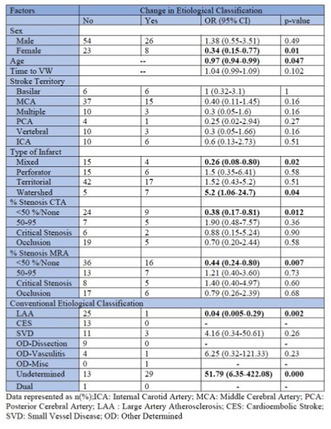
TABLE Univariate Logistic Regression for change in Etiological classification after VW‐ MRI
Conclusion: Vessel wall MRI can be an important additive investigation to help subtype AIS effectively, especially in the sub‐group of the “Undetermined” Category.
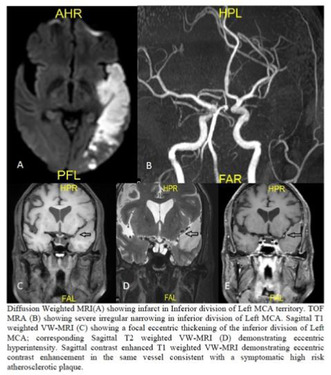
FIGURE Representative case with altered etiological classification post VW‐MRI.
Disclosure: Nothing to disclose.
EPO‐034
Perihematomal edema impact in the 3 years follow‐up of lobar intracerebral haemorrhage
B. Carvalho 1; C. Pisco2; L. Fonseca3; P. Castro1
1Department of Neurology, Centro Hospitalar Universitário de Sã João, Porto, Portugal; 2Department of Clinical Neurosciences and Mental Health, Faculty of Medicine, University of Porto, Porto, Portugal; 3Stroke Unit and Department of Internal Medicine, Centro Hospitalar Universitário de São João, Porto, Portugal
Background and Aims: Spontaneous intracerebral hemorrhage (ICH) is a leading cause of non‐ischemic strokes with substantial impact on morbidity and mortality. While perihematomal edema (PHE) is recognized as indicator of secondary brain injury and has been linked to increased neurological disability, there is a paucity of long‐term follow‐up studies exploring these associations. This study aims to address this gap and evaluate the enduring impact of PHE on the outcomes of ICH patients.
Methods: A retrospective cohort study at Centro Hospitalar Universitário São João, Porto, Portugal, included 87 lobar primary ICH patients from 2014 and 2020. We evaluated absolute (PHE), relative (rPHE) perihematomal edema, and edema extension distance (EED) measured at admission computer tomography (CT) scan and 24–72 hours post‐ICH. Primary outcomes were 3‐year survival and favorable functional outcome (FO) defined as modified Rankin Scale 0–3.
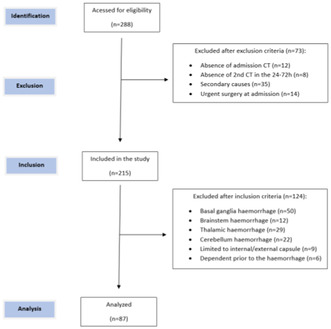
Patient selection flowchart
Results: Median age was 74.0 years (interquartile range 66–82), with 51.7% male. After 3 years, 40.2% were alive, 14.9% had a favorable FO. PHE at 24–72 h negatively correlated with survival in days (Cox regression hazard ratio 2.520, 95% CI 1.118–5.681, p = 0.026), but not rPHE or EED. An inverse correlation of EED at 24–72 hours to a better FO was also observed (OR 0.055, 95% CI 0.004–0.788, p = 0.033).

Demographic characteristics and follow‐up
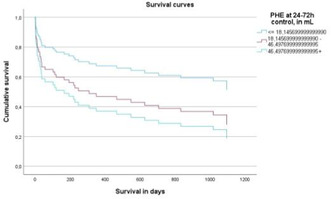
Survival curve for PHE at control
Conclusion: PHE appeared to predict early mortality in lobar ICH. Given the observed tendency towards better functional outcomes (FO) in patients with low EED, recognizing PHE as an early death predictor emphasizes the necessity for further research to understand its role in influencing patient outcomes.
Disclosure: Nothing to disclose.
EPO‐035
Clonal hematopoiesis of indeterminate potential (CHIP) in ischemic stroke etiology
C. Lázaro Hernández 1; P. Lozano Iragüen2; M. Montoro Gómez3; L. Palomo Sanchis3; J. Campos Zarraquiños3; Á. García‐Tornel García‐Camba1; J. Juega Mariño1; J. Pagola Pérez de la Blanca1; C. Molina Cateriano1; M. Rubiera del Fueyo1
1Neurology Department, Vall d'Hebron University Hospital, Barcelona, Spain; 2Neurology Department, Clínica Dávila, University of the Andes. Santiago, Chile; 3Hematology Department, Vall d'Hebron University Hospital, Barcelona, Spain
Background and Aims: Clonal Hematopoiesis of Indeterminate Potential (CHIP) is characterized by the presence of somatic mutations in peripheral blood cells without evidence of a hematological neoplasm. Recent research has associated CHIP with cardiovascular disease and stroke. The objective of our study is to evaluate the relationship of CHIP with the etiology of the ischemic stroke and how its measurement could contribute to the study of stroke causes.
Methods: Prospective observational study of consecutive patients who suffered an ischemic stroke between September 2021 and August 2022. After complete work‐up, patients were classified as cardioembolic (CE), atherothrombotic (AT) and cryptogenic (CRYP) stroke. Patients with double mechanism, incomplete study or active neoplasia were excluded. During hospital admission, 13 genes related to CHIP were analysed. A variant allele fraction of >1% was considered positive.
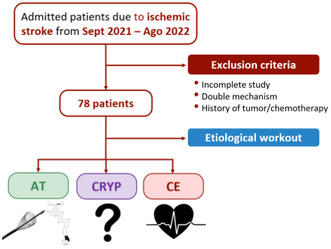
FIGURE 1 Methodology of the study with the corresponding exclusion criteria. AT = Atherothrombotic; CRYP = Cryptogenic; CE = Cardioembolic.
Results: Samples from 78 patients (50% women, mean age 73.4 years) were analysed and etiologically classified as: 37 CE (47.5%), 33 AT (42.3%) and 8 CRYP (10.3 %). Twenty‐eight patients had CHIP (35.9%), of which the predominating mutations were: DNMT3A (35.7%), TET2 (32.1%) and PPM1D (14.3%). Patients with CE stroke had a higher frequency of CHIP and less mutation heterogenicity (Figure 2). In the multivariate analysis, the TET2 mutation was associated with CE etiology after adjusting by age, coronary artery disease and classic cardiovascular risk factors (OR 20.9; p = 0.016) (Figure 3).
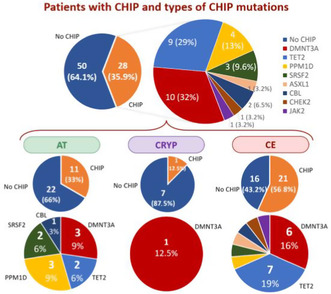
FIGURE 2 Frequency of CHIP and the different mutations according to the etiological diagnosis. It can be observed how patients with CE stroke had a higher frequency of CHIP and less mutation heterogenicity.
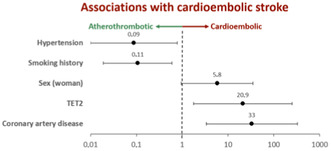
FIGURE 3 Forest plot of the multivariate analysis. In which it is shown the association between cardioembolic stroke and the presence of the TET2 mutation.
Conclusion: CHIP is frequently found in patients with ischemic stroke. The presence of the TET2 mutation was associated with CE stroke and could potentially facilitate the etiological diagnosis of stroke.
Disclosure: Nothing to disclose.
EPO‐036
Exploring sex disparities in ischemic stroke treatment and functional outcomes
A. Cabral 1; P. Almeida1; T. Gregório2; M. Rocha2; H. Costa2; L. Paredes2; M. Veloso2; P. Barros2
1Neurology Department, ULS Gaia Espinho, Porto, Portugal; 2Stroke Unit, ULS Gaia Espinho, Porto, Portugal
Background and Aims: Females face worse functional recovery after stroke. While poorer health, older age and greater stroke severity could explain this, some population studies have shown that accessibility and timeliness of treatment also play a role. We aimed to assess sex‐related disparities in stroke treatment and functional outcomes within our population.
Methods: This retrospective, single‐center study included acute ischemic stroke patients treated with thrombolysis and/or thrombectomy from January 2015 to December 2022 at our stroke center. The primary outcome was functional status at 3‐month follow‐up, while the secondary outcome was time from symptom onset to final reperfusion therapy (TSOFT). Bivariate analysis comparing female and male patients was followed by binary logistic and linear regression to identify predictors of functional outcome and TSOFT, respectively.
Results: 1219 patients were included (54% females, mean age 74 years). Females were older, had worse baseline functional status and higher NIHSS scores at admission. Bivariate analysis showed that females were more likely to have unfavorable functional outcomes (OR 1.367; 95% CI 1.092–1.713) and significantly longer TSOFT (228 versus 200 min; p = 0.002). However, after adjusting for confounders, female sex itself did not correlate with worse functional outcomes (aOR 1.237; 95% CI 0.926–1.646), while longer TSOFT did (aOR 2.177; 95% CI 1.302–3.641). Additionally, linear regression analysis indicated a significant association between female gender and longer TSOFT, even after adjusting for confounders (B = −0.055, p = 0.003, 95% CI [−0.091, −0.019]).
Conclusion: Our findings suggest female stroke patients experience delays in treatment, and that these contribute to worse functional outcomes.
Disclosure: Nothing to disclose.
EPO‐037
Factors associated with fast infarct growth and its impact on patients treated with Mechanical Thrombectomy
D. Wróbel 1; P. Wrona2; B. Łasocha3; P. Brzegowy3; T. Popiela3; G. Kapral1; J. Staniszewska1; M. Derechowska1; A. Słowik2
1Student Scientific Group in Cerebrovascular Diseases, Jagiellonian University Medical College, Krakow Poland; 2Department of Neurology, Jagiellonian University Medical College, Krakow, Poland; 3Department of Radiology, Jagiellonian University Medical College, Krakow, Poland
Background and Aims: Infarct growth rate varies significantly between stroke patients. Fast infarct growth (FIG) is associated with more severe neurological deterioration within time lapse between stroke onset and neurological procedures; that information may be crucial for Mechanical Thrombectomy (MT) decision‐making process. We aimed to identify factors associated with FIG.
Methods: We retrospectively analyzed 641 consecutive patients with AIS in anterior circulation treated with MT in Comprehensive Stroke Center in University Hospital, Cracow (2019–2023). In all patients we obtained pre‐stroke risk factors and performed computed tomography perfusion (CTP) followed by post‐processing analysis with RAPID software. FIG was identified if ratio of CTP‐derived cerebral blood flow <30% volume/time from last known well to imaging exceeded 10ml/h. We included 151 (23.56%) patients with FIG and 490 (76.44%) without.
Results: Patients with FIG were more frequently males (58.3% vs 46.9%, p = 0.015), had significantly lower time from last known well to imaging (135 [84–213]min vs 249.5 [189–302]min, p < 0.001), higher NIHSS on admission (18 [15–21] vs 15 [10–19], p < 0.001) and higher hypoperfusion intensity ratio (HIR, defined as T10max to T6max volumes ratio) (0.57 [0.47–0.68] vs 0.3 [0.15–0.44], p < 0.001). After multivariate analysis, each increase of 0.1 in HIR increased odds for FIG 2.02 (1.76–2.33, p < 0.001). Moreover, FIG was linked with 0.57 (0.35–0.93, p = 0.024) lower odds for obtaining functional independency at day 90, after adjusting for confounders.

TABLE 1 Comparison of patients with and without FIG.
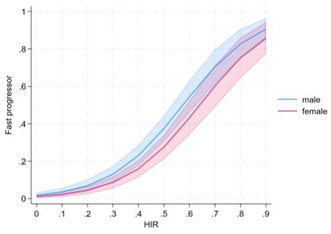
FIGURE 1 Association of hypoperfusion intensity ratio and probability of FIG (fast infarct growth) according to patient sex.
Conclusion: Higher HIR (denoting less robust leptomeningeal collaterals) and male sex are associated with FIG. Although patients with FIG may have lower time from last known well to admission, they present more severe neurological symptoms and worse long‐term prognosis.
Disclosure: ERA‐NET‐NEURON/21/2020 iBioStroke grant.
EPO‐038
Admission blood pressure: Causes and consequences in large vessel occlusion stroke
J. Donnelly 1; D. Campbell2; P. Barber3
1Department of Neurology, Auckland City Hospital, New Zealand; 2Department of Anaesthesiology, University of Auckland, New Zealand; 3Department of Medicine, University of Auckland, New Zealand
Background and Aims: The influence of sex and age on admission blood pressure and how admission blood pressure relates to clinical outcome (modified rankin score at 90 days – mRS‐90) in stroke patients treated with endovascular thrombectomy is unclear.
Methods: Retrospective analysis was performed on patients with stroke receiving clot retrieval. Systolic blood pressure was assessed as the first recorded value. Outcome was assessed by the modified Rankin scale (mRS) score with mRS of 0 to 2 denoting functional independence. A multivariable binary logistic regression was created.
Results: In a cohort of 1079 stroke patients treated with clot retrieval, systolic blood pressure was dependent on age (p < 0.0001) and there was a significant interaction of sex with females less than 50 years old presenting with lower blood pressure. Multivariable logistic regression revealed a quadratic relationship with both low and high admission systolic blood pressure associated with decreased odds of functional independence.

Relationship between age, sex and admission systolic blood pressure in stroke patients treated with endovascular thrombectomy
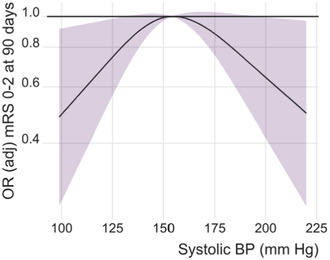
Adjusted odds ratio of admission systolic blood pressure in predicting functional independence in stroke patients treated with endovascular thrombectomy
Conclusion: Further investigation into sex differences in blood pressure control and early stroke pathophysiology is required.
Disclosure: Nothing to disclose.
EPO‐039
Renal function and Neurofilament Light chain serum concentrations in ischemic stroke
F. Ferrari 1; F. Mazzacane1; N. Loizzo2; S. Scaranzin3; C. Morandi3; M. Gastaldi3; A. Persico2; A. Cavallini2
1Department of Brain and Behavioral Sciences, University of Pavia, Pavia, Italy; 2Cerebrovascular Disease & Stroke Unit, IRCCS Neurological Institute Foundation Mondino, Pavia, Italy; 3Neuroimmunology Unit, IRCCS Neurological Institute Foundation Mondino, Pavia, Italy
Background and Aims: Neurofilament Light chain (NfL) is a leading biomarker of long‐term stroke patients' prognosis. Next step is to evaluate if NfL could be effectively employed as candidate surrogate end‐point in stroke studies. An accurate identification of potentially confounding factors is required. This longitudinal prospective observational study investigates the correlations between NfL serum concentrations and renal function in ischemic stroke patients.
Methods: We included patients with stroke at neuroimaging, 18‐80 years, onset <24h, NIHSS >1, pre‐stroke mRS < 2. Exclusion criteria: TIA/previous stroke/TBI/other neurological disease, chronic immunosuppression, pregnancy, severe chronic kidney disease (eGFR < 30mL/min). Patients were treated as standard of care; serum creatinine was measured on admission blood tests. NfL serum concentrations were determined with Ella Automated‐Immunoassay‐System on samples collected within 24h from onset (T0), after 3–5 days (T1) and 7 ± 2 days (T2).
Results: At present, 43 patients have been enrolled (12 females, median age 64y[IQR18.5]. At onset, 53.5% had NIHSS 1–4, 39.5% NIHSS 5–15, 7% NIHSS>16. NfL median values were lower at T0 (35.9pg/mL [IQR49.05]) vs T1 (66.1pg/mL [IQR97.25]; p = 0.003) and T2 (122pg/mL [IQR170.25]; p < 0.001). NfL at all time‐points correlated positively with age and mRS at 3 months, and negatively with eGFR (T0 and T1 p < 0.001, T2 p = 0.01; Figure 1). Correlation analysis showed a negative linear relationship between eGFR and NfL at all time‐points (p ≤ 0.01; Figure 2).
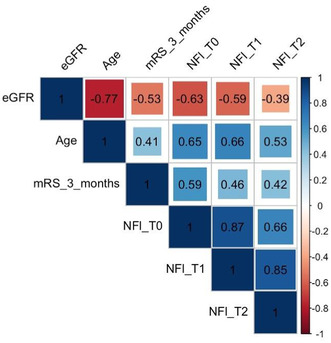
FIGURE 1 Correlation matrix between eGFR, age, mRS at 3 months, NfL.
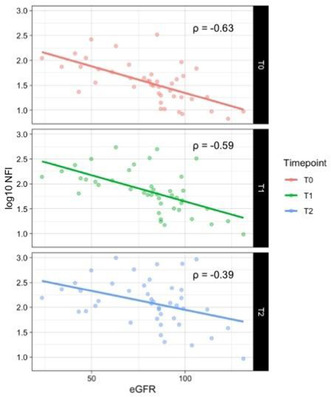
FIGURE 2 Correlations between eGFR and NfL at the three time‐points.
Conclusion: NfL serum levels are inversely correlated with renal function in ischemic stroke patients and this variable should be considered in future studies as a potential source of bias in this population.
Disclosure: This study was supported by the Italian Ministry of Health "Ricerca Corrente 2022–2024" granted to IRCCS Mondino Foundation.
EPO‐040
New metrics of hypoxic burden predict recurrent cardio‐cerebro‐vascular events following ischemic stroke
I. Filchenko 1; X. Yang1; S. Baillieul2; A. Brill3; C. Bernasconi1; M. Schmidt1; C. Bassetti1
1Department of Neurology, Inselspital, Bern University Hospital, University of Bern; 2Univ. Grenoble Alpes, Inserm, U1300, CHU Grenoble Alpes, Service Universitaire de Pneumologie Physiologie; 3Department for Pulmonary Medicine, Allergology and Clinical Immunology, Inselspital, Bern University Hospital, University of Bern
Background and Aims: Considering the limitations of conventional metrics of sleep‐disordered breathing (SDB), novel physiologically informed metrics are needed to better predict the risk of cardio‐cerebrovascular events (CCVE) associated with SDB. In this study, we suggest the use of new metrics of hypoxic burden to predict CCVE in stroke patients.
Methods: This is an exploratory analysis of the prospective observational longitudinal Sleep Deficiency & Stroke Outcome Study (ClinicalTrials.gov Identifier: NCT02559739). In acute ischemic stroke patients, hypoxic burden metrics were computed based on the oximetry signal from the respiratory polygraphy within the first week post‐stroke. Recurrent CCVE were recorded over a 3‐year follow‐up. Cox regression with adjustment for vascular risk factors was used to investigate the prognostic value of 48 cardiovascular parameters regarding CCVEs.
Results: Out of 447 recruited patients, 347 were included in this analysis (Figure 1). 15% developed a future CCVE (mean observation time is 648 days). The 99% occupied bandwidth and negative peak duration significantly predicted vascular risk, whereas no associations were significant for apnea‐hypopnea index (AHI), oxygen desaturation index (ODI), area under curve following non‐specific desaturation <90%, or hypoxic burden parameters according to Azarbarzin and Baumert (Figure 2). The 99% occupied bandwidth and negative peak duration were not significantly associated with AHI or ODI (Figure 3).
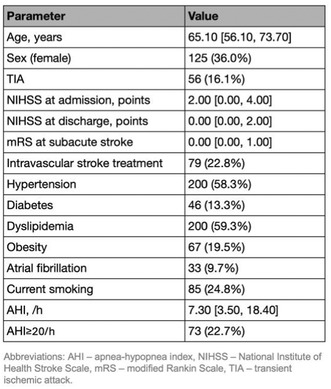
Patient characteristics.
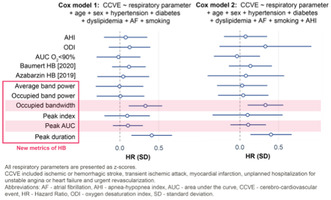
Coefficient plots of Cox regression models showing the association of respiratory parameters at acute stroke with the vascular risk.
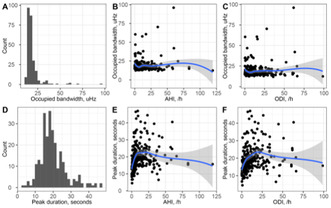
Properties of hypoxic burden metrics: histograms and associations with AHI and ODI.
Conclusion: Among investigated parameters, 99% occupied bandwidth and negative peak duration emerge as the most robust predictors of CCVE after stroke. Future studies should further validate the predictive ability of these markers.
Disclosure: Swiss National Science Foundation grant #320030_149752.
EPO‐041
Endovascular treatment in medium vessel occlusion: Experience from a stroke unit
F. Assis Jacinto 1; M. Lima2; P. Bem2; V. Tedim Cruz1; C. Duque1
1Neurology Department, Hospital Pedro Hispano, Matosinhos, Portugal; 2Neuroradiology Department, Hospital Pedro Hispano, Matosinhos, Portugal
Background and Aims: Medium vessel occlusion (MeVO) accounts for 25–40% of ischemic strokes with visible vessel occlusion. The endovascular treatment's (EVT) efficacy and safety hasn't been confirmed in MeVOs. We aim to evaluate the functional outcome of MeVOs that received EVT.
Methods: One‐year retrospective study, with descriptive and comparative analysis.
Results: From 40 patients admitted, 10 (25%) received EVT (all with M2 occlusion). The median age was 76.5 years ([Q3‐Q1]: [85.75–61.5]). The median time from symptom onset to admission was 442.5 ([Q3‐Q1]: [840–117.5]) minutes with a median NIHSS at admission of 7 ([Q3‐Q1]: [11.75–3]). Median ASPECTS was 9 ([Q3‐Q1]: [10–8]) with Tan collateral score of 3 in 10 patients. 15 patients received acute revascularization treatment: 7 EVT, 5 iv thrombolysis (rtPA) and 3 rtPA plus EVT. The median door‐in‐door‐out time was 86 ([Q3‐Q1]: [139.5–71]) minutes and the median door‐to‐needle time was 136 ([Q3‐Q1]: [193–133]) minutes. After EVT, 8 (20%) patients had a TICI 2b. At discharge, the median NIHSS was 2 ([Q3‐Q1]: [5.75–0]). The median mRS at 90 days was 3 ([Q3‐Q1]: [4–1]). EVT isn't related with mRS at 90 days (p 0.920). EVT is related with a greater variation between NIHSS at admission and at discharge (p 0.014). A favourable mRS at 90 days was significantly related with a lower NIHSS at discharge (p 0.032).
Conclusion: Despite the absence of direct correlation between EVT and favourable functional outcomes at 90 days, EVT is significantly correlated to a greater variation between NIHSS at admission and at discharge suggesting a possible efficacy of this procedure in MeVOs.
Disclosure: Nothing to disclose.
EPO‐042
Dynamic outcome prediction of alteplase‐treated acute ischemic stroke patients: A machine learning approach
I. Petrović 1; S. Njegovan2; O. Tomašević2; S. Rajić1; D. Vlahović1; Z. Božić3; I. Milosavljević1; A. Balenović1; Ž. Živanović1
1Faculty of Medicine, University of Novi Sad; 2Department of Systems, Signals and Control Engineering, Faculty of Technical Sciences, University of Novi Sad, Novi Sad, Serbia; 3Neurology Clinic, University Clinical Center of Vojvodina, Novi Sad, Serbia
Background and Aims: Numerous factors impact the functional outcomes of acute ischemic stroke (AIS) patients treated with intravenous thrombolysis (IVT). Currently, there is a lack of predictive models incorporating clinically relevant features at various time points. This study aimed to develop a machine‐learning model for dynamic prediction of functional outcomes.
Methods: Retrospective analysis involved alteplase‐treated AIS patients at the University Neurology Clinic of Vojvodina (Novi Sad, Serbia) from December 2008 to December 2022. Clinical data were categorized into four groups based on collection time: Baseline, 2‐h, 24‐h, and Discharge features. These were utilized as input for the model. The 90‐day modified Rankin scale (mRS), as an outcome measure, determined favorable (mRS ≤2) and unfavorable outcomes (mRS ≥3). The main classifier evaluation parameter was the area under the receiver operating characteristic (AUC‐ROC) curve.
Results: The study comprised 355 patients (average age 66.4 years, 64% male), with 55% achieving a favorable outcome. Models demonstrated good discrimination on the testing set (AUC = 0.80–0.96), with the highest values in the 24‐h (AUC = 0.89–0.91) and discharge models (AUC = 0.96).
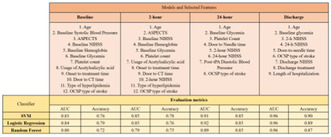
Selected features and Evaluation metrics
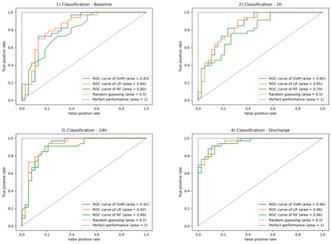
AUC‐ROC curves
Conclusion: The baseline model is applicable for predicting clinical outcomes before IVT, aiding in decision‐making for its initiation, while other models enhance predictive accuracy for post‐IVT clinical outcomes, allowing timely adaptations in treatment approaches.
Disclosure: Nothing to disclose.
EPO‐043
The outcome prediction of ischemic stroke patients with atrial fibrillation: An interpretable machine learning study
I. Petrović 1; M. Ivanišević2; A. Balenović1; I. Milosavljević1; S. Rajić1; D. Vlahović1; Z. Božić3; Ž. Živanović1
1Faculty of Medicine, University of Novi Sad, Novi Sad, Serbia; 2Faculty of Medicine, University of Belgrade, Belgrade, Serbia; 3Neurology Clinic, University Clinical Center of Vojvodina, Novi Sad, Serbia
Background and Aims: Considering that patients with atrial fibrillation (AF) can also achieve favorable outcomes, there is a noticeable literature gap in identifying contributing factors and prediction possibilities for this group. The aim was to utilize interpretable machine learning (IML) to analyze the functional outcomes of stroke patients with admission AF.
Methods: We included 381 alteplase‐treated acute ischemic stroke (AIS) patients, out of which AF was registered in 29% during admission. Based on the 90‐day modified Rankin Scale (mRS) value, two groups were made: a favorable outcome group (mRS ≤2), and an unfavorable outcome group (mRS ≥3). 63 features were used as input for the analysis and model build‐up. The decision‐making process was better understood through the interpretation packages.
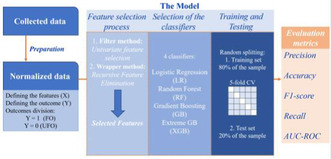
Machine Learning Model Build‐Up Process
Results: In the AF group (n = 109), a favorable outcome was achieved in 55% of patients, and 4 selected distinguishing variables were: the patient's age, the baseline and 24‐h value of NIHSS (National Institutes of Health Stroke Scale), and the type of stroke determined by OCSP (Oxfordshire Community Stroke Project). Logistic regression showed high predictive power (AUC = 0.922), and the interpretation packages revealed a 24‐h NIHSS value as the most influential factor.

SHAP analysis results – the whole group‐level interpretation
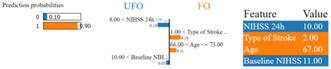
LIME analysis results – the individual‐level interpretation
Conclusion: By focusing on alteplase‐treated ischemic stroke patients with admission AF, this study identified younger age, lower baseline and 24‐h NIHSS values, and OCSP types of AIS other than TACI as important predictors of a favorable 90‐day functional outcome. IML can enhance trust and aid in understanding the decision‐making ‘black box’ of machine learning.
Disclosure: Nothing to disclose.
EPO‐044
Endovascular treatment in ischemic stroke with isolated anterior cerebral artery occlusion
J. Mayol 1; M. Rodrigo‐Gisbert1; M. Olivé‐Gadea1; F. Rizzo1; F. Diana2; M. Rubiera1; C. Molina1; A. Tomasello2; M. Ribó1; M. Requena1
1Stroke Unit, Department of Neurology, Hospital Universitari Vall d'Hebron, Barcelona, Spain; 2Department of Neuroradiology, Hospital Universitari Vall d'Hebron, Barcelona, Spain
Background and Aims: Limited data exist on endovascular treatment (EVT) for anterior cerebral artery (ACA) occlusion‐associated ischemic stroke, leading to variability in therapeutic decisions. Therefore, we aim to evaluate EVT safety and efficacy in patients with ACA occlusions compared with best medical treatment (BMT).
Methods: Retrospective cross‐sectional study involving consecutive patients presenting with isolated ACA occlusion stroke from November‐2015 to November‐2023. The study delineated baseline clinico‐radiological characteristics and treatment‐related factors. Primary safety outcomes included symptomatic intracerebral hemorrhage (sICH) and 90‐day mortality. Secondary outcome was functional independence (90‐day mRS = 0–2).
Results: Among the 68 patients, 41 (60.3%) underwent EVT. Median age was 78 (IQR 73–84) years [EVT 77, IQR 68–84 vs BMT 84, IQR 73–89; p = 0.137]. Median NIHSS score was 9 (IQR 5–16) [EVT 9, IQR 7–17 vs BMT 7, IQR 4–16; p = 0.478]. No statistically significant differences were observed between patients undergoing EVT or BMT in sICH rate (EVT 10.5% vs BMT 4.5%, OR 1.179, 95% CI 0.078–17.84; p = 0.905), 90‐day mortality (EVT 26.3% vs BMT 29.3%, OR 1.874, 95% CI 0.372–9.443; p = 0.447), or functional independence (EVT 36.4% vs BMT 25.0%, OR 0.774, 95% CI 0.078–7.634; p = 0.826). Among patients undergoing EVT, cardioembolic stroke showed higher odds of functional independence than other etiologies (OR 5.54, 95% CI 1.095–27.99; p = 0.038).
Conclusion: In our series, EVT for isolated ACA occlusion stroke was safe, although it did not significantly modify outcomes. Within EVT patients, cardioembolic stroke showed greater benefits. Ongoing randomized clinical trials will determine EVT efficacy for ACA occlusions.
Disclosure: Nothing to disclose.
EPO‐045
Obstructive sleep apnea syndrome: A cerebrovascular risk factor, linked to Alzheimer's disease
P. Guillot 1; F. Roche2; N. Barth3; N. Perek4
1Université Jean Monnet, Saint‐Etienne, France; 2CHU, Saint‐Etienne, France; 3INSERM, U1059, SAINBIOSE, Université de Lyon, Saint‐Etienne, France; 4Gérontopôle AURA, 25 boulevard Pasteur, Saint‐Etienne, France
Background and Aims: Some studies have shown a link between obstructive sleep apnea syndrome (OSA) and Alzheimer's disease (AD). Our aim is to show that OSA is associated with cognitive disorders and has biological similarities with AD.
Methods: Isolation, characterization and quantification of exosomes from blood sera of non‐AD apneic elderly subjects (n = 15); non‐AD non‐apneic elderly controls (n = 15) and AD elderly subjects (in progress, currently n = 10). Establishment of an in vitro BBB model whose permeability will be measured in contact with exosomes from each group.
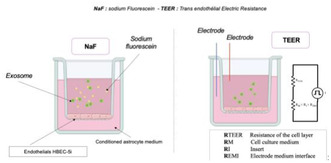
Method for permeability testing when exosomes are in contact with the BBB model
Results: After isolation by precipitation and chromatography, characterization of exosomes by Western blot (WB) and ELISA using anti‐CD81, CD63 and CD9 antibodies showed that apneic subjects had a high level of exosomes similar to AD patients. In addition, the exosomes of apneic subjects contained TAU and beta‐Amyloid proteins in almost the same quantities as those of AD patients. The in vitro BBB model (monoculture of endothelial cells in astrocyte‐conditioned medium) showed an increase in permeability of the model in contact with exosomes from apneic subjects similar to AD subjects. However, patients with very severe apnea induced a greater alteration of the BBB than AD patients.
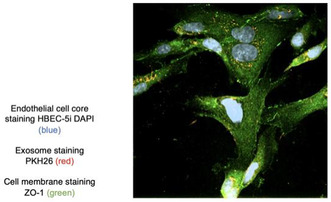
Imaging exosomes in contact with endothelial cells
Conclusion: Analysis of exosomes from the 3 groups showed similarities between the apneic and AD groups compared with controls, suggesting that OSA may be a factor in the development of AD.
Disclosure: Nothing to disclose.
Clinical neurophysiology
EPO‐046
A new way to modulate somatosensory cortex: High frequency tACS matching individual evoked HFOs frequency
A. Cruciani 1; G. Pellegrino2; A. Todisco1; F. Motolese1; M. Sferruzzi1; D. Norata1; F. Santoro1; G. Musumeci1; M. Rossi1; F. Pilato1; V. Di Lazzaro1; F. Capone1
1Department of Medicine and Surgery, Unit of Neurology, Neurophysiology, Neurobiology, and Psychiatry, Università Campus Bio‐Medico di Roma, Roma, Italy; 2Epilepsy program, Schulich School of Medicine and Dentistry, Western University, London, Ontario, Canada
Background and Aims: Transcranial Alternating Current Stimulation (tACS) modulates brain activity non‐invasively through electrical currents, with established effects on the primary motor cortex. This study explores the entrainment effects of tACS on the somatosensory system, particularly on evoked high‐frequency oscillations (HFOs), comparing individualized, standard (600 Hz), and sham settings in healthy subjects.
Methods: The study involved three blocks, each a week apart and randomized among participants: Individualized tACS at the individual's HFOs rhythm, Standard tACS at 600 Hz, and Sham stimulation. Nineteen healthy participants underwent median nerve stimulation, and somatosensory evoked potentials (SEPs) were recorded before tACS (T0), immediately after tACS (T1), and 10 minutes after tACS (T2). High‐frequency oscillations (HFOs) were identified and analyzed using a customized MATLAB pipeline. tACS was administered. Statistical analysis assessed differences across stimulations in delta values (T1‐T0, T2‐T0) using one‐way repeated measure ANOVA and post‐hoc comparisons.
Results: Comparing T0 to T1 and T0 to T2 we found that Individualized tACS significantly increased Area Early compared to Standard and Sham, but no differences were observed between Standard and Sham. Area Late, N20 amplitude, and N20 latency showed no significant effects across stimulations at both time points (T1, T2).
Schematic representation of tACS delivered over left S1. Representative HFOs from subject 7: a) HFOs before tACS (T0); b) HFOs immediately after individualized tACS (T1)
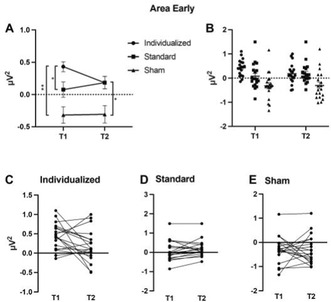
Effects of different tACS stimulations on Area Early
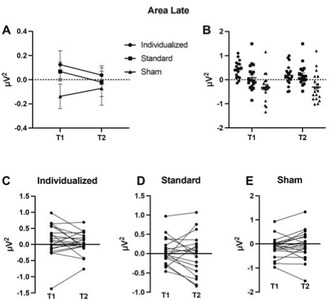
Effects of different tACS stimulations on Area Late
Conclusion: Concluding, we here provide the first evidence that tACS tuned to the individual HFOs frequency modulates the thalamocortical activity in a frequency‐ and time‐specific manner. Multiple studies have demonstrated dysregulation of HFOs in various pathological conditions. Accordingly, the evidence of individualized tACS capacity to influence somatosensory system could potentially pave the way for novel therapeutic applications.
Disclosure: Nothing to disclose.
EPO‐047
EEG and brain MRI alterations in transient global amnesia: The impact of time and gender
C. Ferrazzoli 1; A. Castelli1; V. Ferrazzoli2; A. Pagano1; G. Di Mauro1; C. Liguori1; N. Mercuri1; F. Placidi1; F. Izzi1
1Epilepsy Center, Neurology Unit, Department of Systems Medicine, University of Rome Tor Vergata, Rome; 2Diagnostic Imaging Unit, Department of Biomedicine and Prevention, University of Rome Tor Vergata, Rome
Background and Aims: The aim of the study is to evaluate the prevalence and characteristics of EEG and Brain MRI findings in patients with transient global amnesia (TGA).
Methods: This single‐center observational retrospective study examined adult inpatients admitted at Policlinico Tor Vergata (2013–2023) with transient global amnesia (TGA), diagnosed according to Hodges and Warlow criteria. Only patients who underwent both EEG and brain MRI were included.
Results: Of 69 patients meeting criteria (41 females, 28 males; mean age 62.38 ± 9.20 years), TGA symptoms lasted 5.46 ± 6.14 hours. EEG abnormalities occurred in 68.1% of patients, predominantly bilateral (38.3% left, 51% bilateral, 10% right, p = 0.002). Focal slowing was observed in 33.3%, and interictal epileptiform abnormalities in 34.8%. Epileptiform changes were more frequent in females than males (46.3% vs. 17.86%, p < 0.05). EEG latency from TGA was shorter in the epileptiform group (47 ± 22.63 vs. 61.86 ± 36.6 hours, p = 0.013). Brain MRI revealed DWI positive lesions in 23.2% (left prevalence 11/16, bilateral 4/16, right 1/16, p = 0.007). DWI‐positive patients had a shorter time interval from attack to MRI (82 ± 27.66 vs. 101.43 ± 45.54 hours, p < 0.05). No significant correlation existed between DWI positivity and EEG alterations or lateralization.
Conclusion: The study affirms timing importance, with shorter intervals correlating with increased EEG and MR‐DWI findings in TGA. Left‐sided DWI lesion dominance was noted, consistent with prior studies. No lateralization of EEG abnormalities was found, and MRI and EEG results showed no significant association. Additionally, a significant correlation between gender and paroxysmal EEG abnormalities suggests a potential gender‐specific etiology in TGA, warranting further investigation.
Disclosure: Nothing to disclose.
EPO‐048
Investigating the working mechanism of transcranial direct current stimulation
E. Lescrauwaet 1; M. Sprengers1; E. Carrette1; C. Algoet1; A. Mertens1; D. Klooster2; R. Raedt1; P. Boon1; K. Vonck1
14brain, Department of Neurology, Reference Center for Refractory Epilepsy, Ghent University Hospital, Ghent, Belgium; 2Department of Electrical Engineering, Eindhoven University of Technology, Eindhoven, The Netherlands
Background and Aims: Transcranial Direct Current Stimulation (tDCS) is used to modulate neuronal activity but its exact mechanism of action (MOA) is unclear, hampering its clinical applicability. This study investigates tDCS modulation of the corticospinal neurotransmission and its MOA. By anesthetizing the scalp before applying tDCS and by applying tDCS to the cheeks, we investigated whether stimulation of peripheral and/or cranial nerves substantially contributes to the effects of tDCS.
Methods: In a randomized cross‐over study, 4 conditions were compared in 19 healthy volunteers: (1) anodal tDCS (a‐tDCS) over the motor cortex, (2) a‐tDCS over the motor cortex with a locally applied anesthetic on the scalp, (3) a‐tDCS over the cheek region and (4) sham a‐tDCS over the motor cortex. Motor evoked potentials (MEPs) were measured before and up to 1 h after a‐tDCS. A questionnaire was used to assess the tolerability of a‐tDCS.
Results: A significant MEP amplitude increase compared to baseline was found from 30 to 60 min after motor cortex a‐tDCS. When applying a‐tDCS over the motor cortex with a local anesthetic applied, only a non‐significant small increase in MEP amplitude compared to baseline was observed. The questionnaire demonstrated that side effects are significantly lower when the local anesthetic was applied before a‐tDCS administration.
Conclusion: The significant MEP amplitude increase observed post a‐tDCS supports the modulatory effects of tDCS. The absence of significant modulation when a local anesthetic was applied suggests that effects of tDCS are not solely established through direct cortical stimulation, but stimulation of peripheral and/or cranial nerves might contribute to tDCS‐induced modulation
Disclosure: Nothing to disclose.
EPO‐049
Exploring brain network dynamics in parkinson's patients with visual hallucinations: An EEG microstate approach
E. Toplutaş 1; R. Uysal Kaba2; B. Güntekin3; L. Hanoğlu1
1Department of Neurology, Istanbul Medipol University, Istanbul, Turkey; 2Institute of Neuroscience, Istanbul Medipol University, Istanbul, Turkey; 3Department of Biophysics, Istanbul Medipol University, Istanbul, Turkey
Background and Aims: In this study, we explore the realm of Parkinson's disease (PD), focusing on the manifestation of visual hallucinations (VH), a symptom often overshadowed yet critical in understanding the disease's complexity. Our aim is to elucidate the alterations in brain networks among PD patients experiencing VH, utilizing EEG microstate analysis. This approach offers a window into the neurophysiological processes underpinning these hallucinatory experiences.
Methods: Our cohort consisted of 19 PD patients reporting VH and a matched group of 20 PD patients without such symptoms. The matching criteria included age, gender, educational level, cognitive performance, and PD motor scores. We captured the brain's electrical activity through 5‐min EEG recordings in a resting state with eyes closed. The analysis of EEG microstates was conducted using templates derived from healthy controls, segmented into seven distinct topographical maps.

The analysis of EEG microstates was conducted using templates derived from healthy controls, segmented into seven distinct topographical maps.
Results: Between the two groups, statistical analysis revealed no significant differences in demographics, cognitive assessments, or motor scores. When examining the EEG microstate parameters, including duration, occurrence, and coverage, the results were consistent across all seven microstates, showing no notable variations. However, a significant finding emerged in the transition probabilities, with the VH group exhibiting a markedly lower frequency of transitions from microstate G to microstate F (p < 0.001).
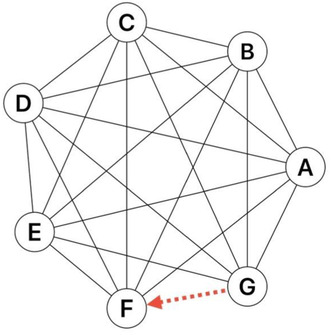
The probabilities of microstate transitions are illustrated here, with the VH group exhibiting a significantly lower frequency of transitions from microstate G to microstate F (p < 0.001).
Conclusion: This study explores at EEG microstate alterations in PD patients who have VH, providing information on the neurophysiological processes that underpin these phenomena. The findings give a more advanced understanding of the disease's neural origins than just symptomatology.
Disclosure: There are no conflicts of interest.
EPO‐050
Neurophysiological consequences of network degeneration in Alzheimer's disease
F. Freri1; E. Canu 1; G. Bertazzoli2; V. Castelnovo1; M. Marizzoni3; C. Bagattini4; C. Fracassi4; M. Bulgari4; M. Delai4; E. Ferrari4; A. Stango4; A. Geviti5; N. Bonfiglio5; M. Pievani3; D. Brignani6; V. Romei7; V. Nicolosi3; F. Agosta8; M. Filippi9; M. Bortoletto4
1Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 2Neurophysiology Lab, IRCCS Istituto Centro San Giovanni di Dio Fatebenefratelli, Brescia, Italy; and Center for Mind/Brain Sciences CIMeC, University of Trento, Rovereto, Italy; 3Laboratory Alzheimer's Neuroimaging & Epidemiology, IRCCS Istituto Centro San Giovanni di Dio Fatebenefratelli, Brescia, Italy; 4Neurophysiology Lab, IRCCS Istituto Centro San Giovanni di Dio Fatebenefratelli, Brescia, Italy; 5Unit of Statistics, IRCCS Istituto Centro San Giovanni di Dio Fatebenefratelli, Brescia, Italy; 6Department of Clinical and experimental Sciences, University of Brescia, Brescia, Italy; 7Centro Studi e Ricerche in Neuroscienze Cognitive, Dipartimento di Psicologia, Alma Mater Studiorum‐Università di Bologna, Campus di Cesena, Cesena, Italy; Facultad de Lenguas y Educacion, Universidad Antonio De Nebrija, Madrid, Spain; 8Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 9Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: Aim of this study is to demonstrate that TMS‐evoked potentials (TEPs) can track neurodegeneration within cortical networks in Alzheimer's disease (AD).
Methods: We collected TEPs, resting state functional MRI (rs‐fMRI), diffusion tensor imaging (DTI), and an extended neuropsychological evaluation in AD cases at various stages of the disease and healthy controls. TEPs were elicited by stimulating the parietal nodes of the default mode network (DMN) and the frontal nodes of the executive control network (ECN). We tested for differences in cognition, WM microstructural tract integrity and early TEP amplitudes (<50 ms) across groups.
Results: Two early TEP components generated for DMN stimulation, i.e., P20P and N20F, showed significantly higher amplitude after left stimulation than after right stimulation in mild cognitive impairment (MCI) due to AD, and not in other groups. Moreover, the N20F following a left DMN stimulation was stronger in MCI patients compared to healthy controls and to AD patients in dementia stage.
Conclusion: In the early stages of the disease, AD is associated with asymmetric alterations of neurophysiological responses in the DMN, in line with previously reported vulnerability of this network and of the left hemisphere in AD cases. The increased TEP responses only in the MCI group indicate that neurophysiological alterations within the DMN are not linearly related with the disease staging. Early TEP components from DMN stimulation have the potential to differentiate MCI due to AD from healthy individuals. Funding: Italian Ministry of Health (GR‐2016‐02364132). Foundation Research on Alzheimer Disease.
Disclosure: F Freri, G Bertazzoli, V Castelnovo, C Bagattini, C Fracassi, M Bulgari, M Delai, E Ferrari, A Stango, A Geviti, NS Bonfiglio, D Brignani, V Romei,V Nicolosi have nothing to disclose. E Canu received research supports form the Italian Ministry of Health (IMH). M. Marizzoni receives research support from IMH. M Pievani received research supports form IMH. M. Bortoletto receives research support from IMH. M. Filippi received compensation for consulting services from Alexion, Almirall, Biogen, Merck, Novartis, Roche, Sanofi, speaking activities from Bayer, Biogen, Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck‐Serono, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA, participation in Advisory Boards for Alexion, Biogen, Bristol‐Myers Squibb, Merck, Novartis, Roche, Sanofi, Sanofi‐Aventis, Sanofi‐Genzyme, Takeda, scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol‐Myers Squibb, Lilly, Novartis, Sanofi‐Genzyme, he receives research support from Biogen Idec, Merck‐Serono, Novartis, Roche, IMH, the Italian Ministry of University and Research, and FISM. F. Agosta received speaker honoraria from Biogen Idec, Italfarmaco, Roche, Zambon and Eli Lilly, and receives or has received research supports from IMH, the Italian Ministry of University and Research, AriSLA, the European Research Council, the EU Joint Programme – Neurodegenerative Disease Research, and Foundation Research on Alzheimer Disease.
EPO‐051
Repetitive transcranial magnetic stimulation of the supplementary motor complex: What is known?
K. Germanova 1; K. Panidi1; M. Nazarova2
1Institute for Cognitive Neuroscience, Centre for Cognition and Decision Making, HSE University; 2Department of Neuroscience and Biomedical Engineering, Aalto University, Finland
Background and Aims: The supplementary motor complex (SMC), consisting of the pre‐SMA and SMA‐proper, contributes to a wide variety of brain functions. Non‐invasive brain stimulation over both pre‐SMA and SMA‐proper areas effectively modulated different aspects of neurological and psychiatric disorders. In this review, we focused on studies with repetitive transcranial magnetic stimulation (rTMS) applied to these regions in both healthy individuals and clinical populations.
Methods: We collected original studies in English from the PubMed, Cochrane, and Scopus databases (PROSPERO ID – CRD42020141289) categorizing them into (1) studies on healthy volunteers and (2) studies on patients. From each study, we extracted: demographics, the function investigated, stimulation parameters including TMS coil targeting approach, and the primary outcomes.
Results: The final sample included 129 articles: 68 studies performed on healthy and 61 studies on clinical populations. Notably, the majority of studies focused on the SMA‐proper rather than the pre‐SMA. In the healthy participants, the SMA‐proper was stimulated aiming to influence both motor (65% of papers) and cognitive processes (25% of papers), 10% of the article reported only neurophysiological findings. The pre‐SMA stimulation was also applied aiming to modulate primarily motor function (79%). In the clinical population, both regions were stimulated to mitigate motor impairment symptoms. The SMA‐proper was mostly stimulated in patients with Parkinson's disease (>40% of papers), while the pre‐SMA – in patients with obsessive‐compulsive disorder.
Conclusion: We suggest that SMA‐proper/pre‐SMA is a promising target for TMS for various neuropsychiatric conditions. Nevertheless, further research is needed to understand the interhemispheric and SMA/pre‐SMA effect differences.
Disclosure: Nothing to disclose.
EPO‐052
Dopaminergic therapy and swallowing physiology in patients with Parkinson's disease: An electrophysiological study
G. Cosentino 1; M. Todisco2; M. Rossi3; G. Belluscio3; S. Malaspina3; M. Avenali1; C. Pacchetti2; R. Zangaglia2; M. Fresia2; F. Valentino2
1University of Pavia. IRCCS Mondino Foundation; 2IRCCS Mondino Foundation; 3University of Pavia
Background and Aims: Though dopaminergic therapy is the gold‐standard treatment for PD, its effects on the swallowing function are still debated. Objective of the study is to assess the swallowing function through an electrokinesigraphic approach in a group of non‐dysphagic PD patients with motor complications evaluated both in off‐ and on‐therapy.
Methods: the repeated swallowing of a liquid bolus was performed while recording the following parameters: i) surface electromyographic activity of the submental‐suprahyoid muscles (sh‐EMG), involved both in the oral and pharyngeal phases of swallowing); ii) intraswallowing apneic pause (AP); iii) pharyngo‐laryngeal mechanogram (PLM). Amplitude, duration and area of the recorded signals and time intervals were calculated using the Matlab platform. All patients were assessed both in on‐ and off‐medication state.
Results: 11 patients (64 ± 6.4, 4F/7M) were enrolled and completed the experimental assessments. A significant (p < .05) shortening of the interval between the inspiratory and expiratory peaks following the swallowing act and the end of the AP was observed in the on‐ vs. off‐medication state. Better but not statistically significant swallowing performances were also observed in patients when on‐medication, in particular we observed a shorter oro‐pharyngeal delay (p = .11) and a larger area of the PLM (p = .017)
Conclusion: dopamine therapy can improve the synergy between breathing and swallowing in accordance to previous findings that dopaminergic treatment can improve pulmonary function tests. However, based on these preliminary results in a small group of non‐dysphagic PD patients, no significant changes in the other aspects of the oral and pharyngeal phases of swallowing were observed.
Disclosure: None.
EPO‐053
Neurophysiological evidence on the intravenous methylprednisolone use in spinal surgery
J. Park; K. Kwak; J. Park; D. Kim; H. Eom; Y. Park
Department of Rehabilitation Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea
Background and Aims: Research suggests corticosteroids post‐spinal injury might increase side effects without benefits, highlighting a lack of symptom or electrophysiological controls. The hypothesis is that intravenous methylprednisolone (IVMP) could restore surgery‐induced MEP amplitude reduction in a range‐dependent manner, potentially improving postoperative motor scores.
Methods: This study reviewed spinal surgery patients with neurophysiological monitoring at a tertiary hospital, 2017–2023. Patients with over 50% MEP reduction were categorized into steroid and non‐steroid groups upon surgeon's decision. MEP monitoring occurred at set intervals post‐event, with examining MEP restoration and its correlation with motor recovery across defined MEP decline ranges. Statistical methods like T‐tests and Pearson's correlation evaluated the effect of MEP recovery on motor outcomes.
Results: The analysis included 100 patients (71, steroid; 29, non‐steroid group), with 807 muscles examined (524, steroid; 183 non‐steroid group) (Table 1). The steroid group demonstrated higher MEP amplitudes (%) compared to the non‐steroid group exclusively in the −100% to −80% MEP reduction range (Figure 1). A significant correlation was identified between the recovery of MEP amplitude and motor score improvement within the −80% to −50% reduction range (Table 2). For cases with complete MEP loss (‐100%), no recovery in MEP or motor function was observed (Figure 1 and Table 2).
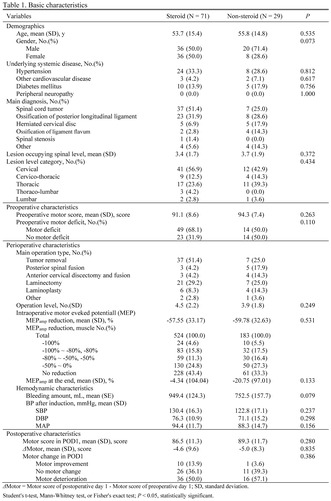
TABLE 1 Basic characteristics
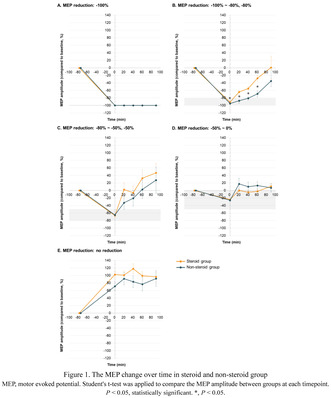
FIGURE 1 The MEP change over time in steroid and non‐steroid group

TABLE 2 Correlation between MEP change and postoperative motor outcome
Conclusion: This current study is the first to investigate the effects of IVMP on the deterioration degree of MEP waves, and it further explores the impact of IVMP on postoperative motor outcomes in relation to the degree of MEP deterioration.
Disclosure: Nothing to disclose.
EPO‐054
Detection of electrophysiological markers indicating neuropathy in children and adolescents diagnosed with type 1 DM
M. İnci 1; A. Poyraz2; G. Şirin1; E. Sarban3; M. Yıldız3; F. Baş3; E. Kocasoy Orhan1
1Istanbul University, Istanbul Faculty of Medicine, Department of Neurology; 2Istanbul University, Istanbul Faculty of Medicine, Department of Neurosurgery; 3Istanbul University, Istanbul Faculty of Medicine, Department of Pediatric Endocrinology
Background and Aims: We aimed to investigate the temporal changes and patterns of involvement in nerve conduction studies and autonomic tests in children and adolescents diagnosed with type 1 diabetes mellitus (T1DM).
Methods: We conducted nerve conduction studies and autonomic tests twice, with a one‐year interval, on 63 patients aged between 8 and 18, with a minimum disease duration of 2 years, all diagnosed with T1DM. Demographic and clinical findings were assessed, and the study design is summarized in Figure 1.
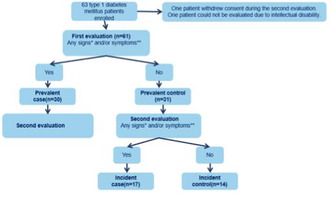
FIGURE 1 Diagram of the study design *associated with polyneuropathy, **according to Diabetic Neuropathy Symptom Score (DNS)
Results: No pathological findings consistent with the classical signs of neuropathy were observed in the parameters of nerve conduction studies. The most frequently abnormal parameters were peroneal F persistence (38.1%) and minimum F latency (30.2%), R‐R interval variability (RRIV) (21%), and tibial minimum F latency (11.1%). Sural sensory peak latency and peroneal motor distal latency were found to be longer in both prevalent and incident case groups compared to the incident control group (p < 0.05). When the prevalent case group was compared with the prevalent control group, RRIV was lower, and sympathetic skin response (SSR) latency was longer in both upper and lower extremities (p < 0.05).
Conclusion: Monitoring latencies and conduction velocities in sensory and motor nerves may be more guiding in understanding the development of polyneuropathy. In addition, it seems useful to include SSR and RRIV examinations, which are parameters not frequently evaluated, in polyneuropathy research protocols in this group.
Disclosure: None of the authors has any conflict of interest to disclose.
EPO‐055
Difference in electromyographic features of dystonic and essential tremor: A pilot study
M. Minár 1; S. Kajan2; Z. Košutzká1
1Second Department of Neurology, Faculty of Medicine, Comenius University Bratislava, Slovakia; 2Institute of Robotics and Cybernetics, Faculty of Electrical Engineering and Information Technology, Slovak University of Technology in Bratislava, Bratislava, Slovakia
Background and Aims: Many patients with dystonic tremor (DT) – especially in the form of bilateral upper limb action tremor – are misdiagnosed as having essential tremor (ET). We aimed to find specific objective electromyographic (EMG) features of DT.
Methods: We examined 25 patients with upper limb tremor referred to our laboratory with a working diagnosis of ET. Surface EMG data were recorded from the extensor and flexor carpi radialis (ECR, FCR), first dorsal interosseus muscle and accelerometer placed on the index finger of a more affected limb by the Neurosoft®Neuro‐MEP‐8 EMG.
Results: None of the patients presented with obvious clinical features of dystonia. In 13 patients, we detected antagonist co‐contraction, motor overflow, mirror dystonia, null point, and/or myoclonic jerks on EMG, thus suggesting the diagnosis of DT. From objectively measured parameters, these patients had a significantly lower ratio between maximum peak difference (measured between the highest and lowest point of discharge spike), and its maximum negative amplitude (DIFFmax/AMPmax; 0.607 ± 0.075, vs. 0.815 ± 0.102, p < 0.001, Cohen's d = 2.333). It indicates that isolated tremor bursts on EMG are less prominent in DT, perhaps due to rising from the background of sustained muscle contractions (dystonia). None of the other parameters differed significantly.
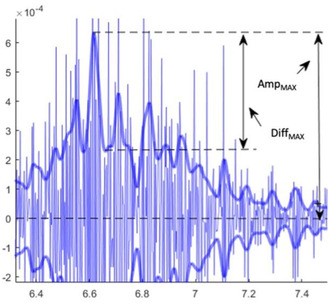
Measured parameters
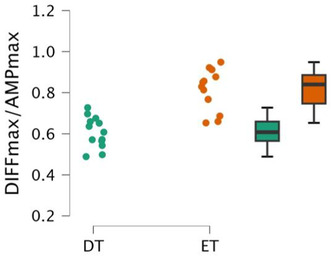
Difference between ET and DT
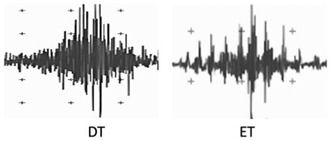
Examples of patients with DT and ET
Conclusion: Surface EMG might help to verify subclinical dystonic activity and thus distinguish clinically similar tremors. In addition, measurable parameters might be used in the objective assessment of tremor types and they can become a part of the diagnostic process using deep learning methods.
Disclosure: This study was supported by the Grant of the Ministry of Education, Science, Research and Sport of the Slovak Republic (VEGA Nr. 1/0527/22).
EPO‐056
Reference values for near fiber EMG measures in upper and lower limb muscles
O. Garnes‐Camarena 1; I. Mahillo‐Fernandez2; O. Lorenzo2; R. Mandeville3; D. Stashuk4
1Jimenez Diaz Foundation University Hospital, Madrid, Spain; 2Jimenez Diaz Foundation Research Institute, Madrid, Spain; 3Beth Israel Deaconess Medical Center, Boston (MA), USA; 4Systems Desing Engineering, University of Waterloo, Ontario, Canada
Background and Aims: Near‐fiber MUP (NF‐MUP) analysis provides novel and useful information on motor unit potential (MUP) temporal dispersion (NFM‐Dispersion) and instability (NF‐MUP segment jitter (NFM‐SJ)) from signals acquired during routine EMG protocols. NFM‐Dispersion is the spread in the times with which muscle fiber action potentials (MFAP) pass the recording electrode, whereas NFM‐SJ reflect the temporal inconsistencies in their generation.
Methods: NFM‐Dispersion and NFM‐SJ reference values were determined for six muscles (deltoid, biceps, triceps, vastus lateralis, tibialis anterior and medial gastrocnemius), based on a sample size of 20 control cases each with a minimum of 20 MUPs per muscle (age 23–79 y‐o). The EMG signals used were acquired using a standard needle EMG examination protocol. DQEMG (Decomposition‐based Quantitative EMG) software was used for the calculation of NF‐MUP parameters. Reference values were defined using a method based on the e‐norm (Jabre, 2015) and e‐ref (Nandedkar, 2018) methods.
Results: The distribution of values by quartiles indicated a small variability between subjects, with low standard errors and narrow confidence intervals. The analysis of values above the defined reference values indicated that NF‐MUP parameters are highly clustered and close to the reference values. Considering all of the MUPs for each respective group of control muscles, the percentage of unstable MUPs ranged between 4.9 and 11.2%, and the percentage of dispersed MUPs from 5.2 to 13.4%.
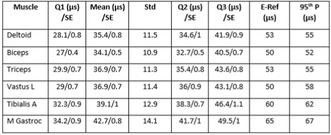
TABLE 1 NFM‐SJ reference values.
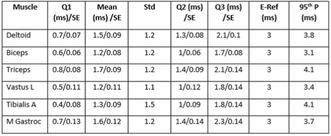
TABLE 2 NFM‐Dispersion reference values.
Conclusion: NFM‐Dispersion and NFM‐SJ stability measures, extracted from regular EMG signals, are useful and solid parameters that can augment the current understanding of neuromuscular disorders.
Disclosure: Nothing to disclose.
EPO‐057
Introduction to near fiber EMG, a novel way to measure motor unit electrophysiological properties
D. Stashuk 1; O. Garnes‐Camarena2; R. Mandeville3
1Systems Desing Engineering, University of Waterloo, Ontario, Canada; 2Jimenez Diaz Foundation University Hospital, Madrid, Spain; 3Beth Israel Deaconess Medical Center, Boston (MA), USA
Background and Aims: Motor Unit Potential (MUP) complexity and instability are key parts of EMG examinations, whose assessment can be time‐consuming or subjective. We introduce a novel and semi‐automated way of measuring MUP complexity and instability, based on Near Fiber (NF) EMG concepts. A NF‐MUP is the summation of the muscle fibre potentials of fibers near the recording electrode (NF‐MFPs). The temporal dispersion and instability of NF‐MFPs are new clinically useful MU characteristics that can be quantified using NF‐MUP parameters.
Methods: Aspects of novel signal processing algorithms used to extract MUP trains, estimate MUP and NF‐MUP templates and select isolated NF MUPs for complexity and instability analysis as well as new quantitative measures to characterize sampled MUs will be described, demonstrated, and discussed.
Results: NFEMG has been used to study and assess several neuromuscular diseases. It has been used to detect increased MUP complexity and instability in CIDP, ALS, GBS, and diabetic neuropathy. In addition, it can be used to diagnose MG with similar accuracy as provided by SFEMG.
Conclusion: NF EMG offers an exciting new, rapid, and comprehensive evaluation of MUP complexity and instability that promises to significantly advance the diagnosis and monitoring of neuromuscular diseases.
Disclosure: Nothing to disclose.
EPO‐058
Sural‐to‐medial femoral cutaneous amplitude ratio in early diagnosis of uremic neuropathy
Ş. Deveci 1; Z. Matur2; D. Mermi Dibek1; A. Öge3
1University of Health Sciences Turkey, Basaksehir Cam and Sakura City Hospital, Clinic of Neurology, Istanbul, Turkey; 2Bezmialem Vakif University Faculty of Medicine, Department of Neurology, Istanbul, Turkey; 3Istanbul University, Istanbul Faculty of Medicine, Department of Neurology, Istanbul, Turkey
Background and Aims: Chronic Renal Failure (CRF) is typically associated with length‐dependent axonal polyneuropathy and secondary demyelination. This study aimed to clinically and electrophysiologically assess CRF patients experiencing polyneuropathy‐related complaints before initiating dialysis. The sural‐to‐medial femoral cutaneous nerve action potential (NAP) amplitude ratio (SMFCAR) was evaluated for its sensitivity and specificity in early electrophysiological diagnosis.
Methods: The study included 32 CRF patients (mean age 60.0 ± 9.6 years) and 30 age and sex‐matched controls (58.9 ± 6.6 years). Assessments encompassed neurological examination, Michigan Neuropathy Screening Instrument (MNSI) A‐B, and Semmes‐Weinstein monofilament (10 g–5.07 mm) test. Radial, median, ulnar, medial femoral cutaneous, sural, and superficial peroneal sensory; median, ulnar, tibial, and peroneal motor conduction studies were performed. Sural‐to‐radial amplitude ratio (SRAR) and SFMCAR were calculated, and their diagnostic sensitivities were compared.
Results: The patients were in the CRF stages of 3 (59.4%), 4 (34.4%), and 5 (6.3%). The average CRF duration was 54.3 ± 46.1 (8–276) months. MNSI‐B indicated clinical polyneuropathy in 59% of the patients, while routine nerve conduction studies diagnosed it in 72%. Median SRAR and SMFCAR values were significantly lower in patients than controls (p < 0.001 for both). At 90% specificity, SMFCAR's cut‐off was <2.8 with a sensitivity of 59%, while SRAR's was <0.77 with a sensitivity of 35%.
Conclusion: In some CRF patients with symptoms compatible with length‐dependent polyneuropathy, peripheral nerve involvement might be in a stage that cannot be detected by routine examination and electrophysiology. SMFCAR may be a useful alternative to SRAR in the early diagnosis.
Disclosure: Nothing to disclose.
EPO‐059
Subclinical epileptic activity and cognitive decline in Parkinson's disease and atypical parkinsonisms
T. Jesus 1; R. Peralta2; A. Franco2; S. Parreira2; A. Oliveira1; A. Horváth3; C. Bentes2
1Neurology Department of Hospital de Vila Franca de Xira, Unidade Local de Saúde Estuário do Tejo, Vila Franca de Xira, Portugal; 2EEG and Sleep Laboratory‐Neurophysiology Monitoring Unit of Hospital Santa Maria, Unidade Local de Saúde de Santa Maria, Lisbon, Portugal; 3Neurocognitive Research Center, National Institute of Mental Health, Budapest, Hungary
Background and Aims: Subclinical epileptiform activity (SEA) are epileptic discharges that occur without clinical seizures. There is evidence that SEA might be associated with accelerated cognitive decline in Alzheimer's disease (AD). Its occurrence and clinical correlates in parkinsonian syndromes have not been studied yet. Our primary aim was to study the frequency of SEA in parkinsonian patients. The secondary aim was to compare clinical and demographic characteristics in patients with and without SEA and characterize SEA morphologically.
Methods: Retrospective cross‐sectional study. We examined patients with parkinsonian syndromes who underwent level 1/2 polysomnography between 1/1/2018 and 31/05/2022. Demographic information, diagnosis, and presence of mild cognitive impairment/dementia were obtained by chart review. Electroencephalogram (8 channels) was manually analysed for SEA, defined as paroxysms that fulfilled ≥4/6 epileptic discharge criteria according to the International Federation of Clinical Neurophysiology, confirmed by 3 epileptologists/neurophysiologists. Non‐parametric statistical analysis was performed.
Results: 26 polysomnographies were reviewed (15 Parkinson's disease, 6 Multiple system atrophy, 2 Dementia with Lewy bodies, 2 vascular parkinsonism and 1 progressive supranuclear palsy). 14 patients had SEA (54%). There were no statistically significant differences between patients with SEA (median age 72yrs, 64% women, 36% with cognitive decline) and without (median age 64yrs, 67% women, 25% with cognitive decline). SEA's main location was temporal and temporo‐occipital.
Conclusion: Our SEA prevalence was similar to studies with AD patients, and higher than data published from healthy controls (5–25%). Although it is a small heterogenous sample, with few EEG channels, it suggests that SEA is frequent in other neurodegenerative disorders.
Disclosure: Nothing to disclose.
EPO‐060
New national reference limits for nerve conduction studies
T. Szczepanski 1; K. Nilsen1; P. Omland2
1Department of Neurology and Clinical Neurophysiology, Oslo University Hospital, Oslo, Norway; 2Department of Neurology and Clinical Neurophysiology, St. Olavs Hospital, Trondheim, Norway
Background and Aims: Reference limits are important for correctly interpreting nerve conduction studies (NCS). Because reference limits for NCS are dependent of the examining procedure and the equipment settings used, laboratory‐specific reference limits are needed. However, creating such reference limits with traditional methods is expensive and time‐consuming. We present reference limits for NCS using a more practical approach – extrapolated norms (e‐norms) – using historical measurements from the world's largest database of NCS.
Methods: We applied the e‐norms algorithm on 2 143 280 Norwegian historical NCS measurements (conduction velocities, amplitudes, distal latencies) from 1998 to 2023 for the motor Peroneal, Tibial, Median and Ulnar nerves and the sensory Sural, Superficial Peroneal, Medial Plantar, Median, Ulnar and Radial nerves. Age was stratified into decades starting from the age of 20 up to the age of 99. Height was stratified into three brackets: 150–170 cm, 170–180 cm and 180–200 cm.
Results: The stratification gave in total 630 reference limits. In general, the reference limits decreased with age and height for conduction velocities and amplitudes, and increased for latencies. The values were close to the currently used limits derived by traditional methods. Ten references limits for nerves in the lower extremities could not be reliable calculated.
Conclusion: We have calculated new national reference limits for NCS in Norway (published at https://www.ous‐research.no/digmine). Compared to the reference limits already in use, the reference limits produced by the e‐norms algorithm are similar. In addition, the algorithm also produced reference limits for age groups where high quality reference limits are currently lacking.
Disclosure: Nothing to disclose.
Neuroimmunology 1
EPO‐061
COVID‐19 vaccination response in participants receiving efgartigimod IV or Efgartigimod PH20 SC in ADAPT+ or ADAPT‐SC+
F. Saccà 1; J. Howard Jr.2; J. Sleasman3; F. Gistelinck4; P. Duncombe4; B. Van Hoorick4; S. Steeland4; R. Mantegazza5; J. De Bleecker6; A. Azar7; K. Winthrop8
1GENESIS Department, Federico II University of Naples, Naples, Italy; 2Department of Neurology, The University of North Carolina, Chapel Hill, North Carolina, USA; 3Division of Allergy, Immunology, and Pulmonary Medicine, Duke University School of Medicine, Durham, North Carolina, USA; 4Argenx, Ghent, Belgium; 5Department of Neuroimmunology and Neuromuscular Diseases, Fondazione Istituto Neurologico Carlo Besta, Milan, Italy; 6Department of Neurology, Ghent University Hospital, Ghent, Belgium; 7Division of Allergy and Clinical Immunology, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA; 8Division of Infectious Disease, Oregon Health and Science University, Portland, Oregon, USA; Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy
Background and Aims: Patients with generalised myasthenia gravis (gMG) experience greater risk of adverse outcomes from respiratory infections, including COVID‐19. Some immunosuppressive therapies used in gMG management increase risk of infection and impair vaccine responses. We investigated the effect of treatment with efgartigimod [administered intravenously (IV) or subcutaneously (SC, coformulated with recombinant human hyaluronidase PH20), a human IgG1 antibody Fc‐fragment that reduces total and pathogenic IgG levels through neonatal Fc receptor blockade, on humoral immune responses to COVID‐19 vaccination in participants with gMG.
Methods: In ADAPT+ (completed) and ADAPT‐SC+ (ongoing open‐label extension), efgartigimod IV (10 mg/kg) or efgartigimod PH20 SC (1000 mg) were administered in cycles of 4 once‐weekly infusions/injections. Among other COVID‐19 receptor binding domain‐specific IgGs, SARS‐CoV‐2‐IgG‐RBD responses were assessed, nominally, at prevaccination, ≥4 weeks after vaccination, and subsequently at 1 week after fourth efgartigimod PH20 SC injection (when total IgG levels were maximally reduced, Figure). One sample was collected if postvaccination time points coincided with each other.
Results: Eighteen participants in ADAPT‐SC+ (Table) received a COVID‐19 vaccine during or after a cycle. For 78% (n = 14/18) of participants, this was their second or third vaccine dose. A 35.9‐fold increase in SARS‐CoV‐2‐IgG‐RBD levels occurred from prevaccination to ≥4 weeks postvaccination (Figure). Similarly, from prevaccination to 1 week after the fourth efgartigimod PH20 SC injection, a 33.8‐fold increase emerged (Figure). Similar results were observed with efgartigimod IV during ADAPT+.
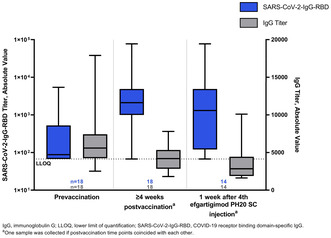
FIGURE Absolute Values of SARS‐CoV‐2‐IgG‐RBD Titer and Total IgG Titer
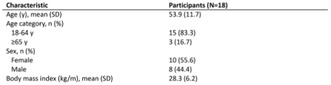
TABLE Participant Characteristics
Conclusion: Consistent with efgartigimod IV results, participants receiving efgartigimod PH20 SC were able to mount antigen‐specific IgG responses to COVID‐19 immunisation, even when total IgG levels were maximally reduced.
Disclosure: Multiple relationships financial and non‐financial nature for authors FS, JFH, JWS, FG, PD, BVH, SS, RM, JLDB, AA, and KW stated at point of presentation.
EPO‐062
Primary angiitis of the central nervous system: The experience of a tertiary center
R. Lopes 1; D. Costa1; I. Almeida1; R. Taipa2; A. Sousa3; E. Santos1; R. Samões1
1Neurology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 2Neuropathology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 3Neurophisiology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal
Background and Aims: Primary Angiitis of Central Nervous System (PACNS) is a rare inflammatory disorder affecting blood vessels in CNS without systemic involvement that exhibits a range of presentations. We aimed to characterize the population of patients with PACNS in a tertiary center.
Methods: Retrospective analysis of patients in Neuroimmunology outpatient clinic diagnosed according to Rice and Scolding (2020) criteria. Demographic, clinical, laboratory, imaging, and histological data were recorded.
Results: Twelve patients were included (male‐to‐female ratio 1:1.4) with an average age of symptom onset at 50.8 ± 16 years and diagnosis at 53.8 ± 13 years. Half were classified as definitive diagnosis, the remaining six as possible. Most frequent presenting symptoms were cognitive impairment (42%), stroke/focal neurological deficits (33%). Over the course of the disease, 66% also developed headache. MRI was abnormal in all 12 cases, with ischemic lesions (66%), microhemorrhages (33%) as the most frequent changes. Abnormalities in CSF were found in 82%, with lymphocytic pleocytosis in 54% (average 15.2 cells/μL), elevated protein levels in 45% (average 0.6 g/L), oligoclonal bands in 36%. Classical angiography was positive in 100% (5/5), and histological results in 75% (6/8) with prevalence of lymphocytic vasculitis. The treatments used were mainly corticosteroids (92%) and cyclophosphamide (75%). The patients were followed for an average of 8.4 ± 7 years, 33% with a Rankin scale ≥3. Despite treatment, gradual clinical deterioration was observed in 42% and sequelae cognitive impairment in 50%.
Conclusion: This analysis reveals a variety of clinical, radiological, and histological findings showing the complexity of the disorder. The severity of the condition despite treatment is also highlighted.
Disclosure: Nothing to disclose.
EPO‐063
CD20 T lymphocytes in multiple sclerosis: Impact on neuropsychological findings
A. Esposito 1; A. Spiezia1; F. Falco1; F. Lamagna2; M. Eliano1; M. Petracca3; C. Di Monaco1; V. Nicolella1; F. Novarella1; R. Lanzillo1; M. Moccia4; V. Brescia Morra1; A. Carotenuto1
1Department of Neurosciences, Reproductive and Odontostomatological Sciences, Federico II University, Naples, Italy; 2Department of Psychology, Università degli Studi della Campania ‘L. Vanvitelli’; 3Department of Human Neurosciences, Sapienza University, Rome, Italy; 4Department of Molecular Medicine and Medical Biotechnology, Federico II University of Naples, Italy
Background and Aims: Some T lymphocytes show molecular signature also for B lymphocytes (CD20)CD20 T lymphocytes may play a pivotal role in multiple sclerosis pathology, especially at progressive stages. This would suggest that CD20 T lymphocytes might be a marker of central nervous system (SNC) compartmentalized inflammation. We aim to investigate the correlation between CD20 T lymphocytes in peripheral blood in MS patients with neuropsychological features (i.e. cognition, depression, anxiety, fatigue and sleep quality).
Methods: We enrolled 90 MS patients. Each patient underwent cognitive assessment (BICAMS) and psychometric assessment (i.e. MFIS, BAI, BDI, PSQI). Cognitive status was defined through the cerebral functioning score (CSF). For each patient we performed blood sample collection to assess CD20 T lymphocytes and neurofilaments (NFL) levels.
Results: Forty‐four out of 90 patients were relapsing‐remitting (49%), 46 were progressive patients (51%). Seventy patients (18.9%) showed CD20 T lymphocytes in peripheral blood with a mean level of 0.38 ± 1.2. Patient with CD20 T lymphocytes were more likely to be in progressive patients (76.5% vs 23.5% of relapsing MS patients, p = 0.02), and showed a higher EDSS (3.5 vs 6, p = 0.001). Moreover, patients with CD20 T lymphocytes showed worse cognitive functioning (p = 0.004), higher global fatigue symptoms (p = 0.02) higher cognitive fatigue (p = 0.01), higher psychosocial fatigue (p = 0.005) and a trend toward worse sleep quality (p = 0.06). Conversely, NFL levels were not associated with CD20 T lymphocytes.
Conclusion: The presence of CD20 T lymphocytes in peripheral blood of MS patients, could possibly reflect an ongoing neurodegenerative process independent from inflammatory activity resulting in worse neuropsychological functioning.
Disclosure: MM has received research grants from the ECTRIMS‐MAGNIMS, the UK MS Society, and Merck; honoraria from Biogen, BMS Celgene, Ipsen, Janssen, Merck, Novartis, Roche, and Sanofi‐Genzyme. AC has received research grants from Almirall, research grants from ECTRIMS‐MAGNIMS and honoraria from Almirall, Biogen, Roche, Sanofi‐Genzyme, Merck, Ipsen and Novartis. MP has received research grants from Italian MS Foundation and Baroni Foundation, honoraria from HEALTH&LIFE S.r.l. and Biogen and sponsorship for travel/meeting expenses from Novartis, Roche and Merck. RL has received honoraria from Biogen, Merck, Novartis, Roche, and Teva. VBM has received research grants from the Italian MS Society, and Roche, and honoraria from Bayer, Biogen, Merck, Mylan, Novartis, Roche, Sanofi‐Genzyme, and Teva. AE, ALS, CDM, VN, FN, FF, FL ME have nothing to disclose.
EPO‐064
Intravenous vs subcutaneous natalizumab in the treatment of multiple sclerosis, a cohort study
S. Costa 1; D. Costa1; A. Sousa2; R. Samões1; E. Santos1
1Neurology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 2Neurophysiology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal
Background and Aims: Subcutaneous (SC) natalizumab has been recently approved for multiple sclerosis treatment. There are few studies comparing clinical effectiveness and safety of subcutaneous and intravenous Natalizumab.
Methods: Retrospective study of multiple sclerosis patients followed at a Portuguese tertiary center, currently under treatment with Natalizumab (NTZ). Analysis of efficacy and safety of intravenous (iv) and subcutaneous (sc) formulations.
Results: Data were collected from 59 patients of which 12 were treated with iv NTZ (group 1), 36 with iv and then formulation was switched to sc NTZ (group 2), and 11 with sc NTZ (group 3). At baseline, patients from group 1, 2 and 3, had respectively a median EDSS of 2.0 [IQR: 0–4.5], 1.5 [IQR: 0–6.0] and 1.0 [IQR: 0–2]. ARR (Annualized relapse rate) was 1.0 in all groups. Patients from group 1 (5/41.7%) group 2 (16/44.4%), and group 3 (6/54.5%) had disease activity on CE‐MRI. Patients from group 1, 2 and 3, had respectively a median of 4 [IQR: 1.0–14.0], 3 [IQR: 1.0–13.0], and 1.0 [IQR: 1.0–2.0] years of treatment. After treatment, median EDSS was 2.0 [IQR: 0–4.5] in group 1 and 2, and 1.5 [IQR: 1–2] in group 3, and median ARR was 0 in all groups. One patient (8.3%) of group 1 (3 years of NTZ) and 2(18.1%) patients of group 3 (1 year of NTZ) had disease activity on CE‐MRI. Both formulations were well‐tolerated. Only two patients presented minor gastrointestinal side effects and discontinued sc formulation. Three patients refused to switch to sc NTZ.
Conclusion: Both formulations of NTZ seem to be comparable in safety and in stabilizing the disease.
Disclosure: All authors declare that they have no conflicts of interest related to the manuscript.
EPO‐065
Crohn‐related CRION case report: When optic neuropathy is not synonymous with demyelinating disease
G. Mignani 1; N. Giannini1; G. Bellini1; M. Bellini2; G. Siciliano1; L. Pasquali1
1Department of Neurological Sciences, University of Pisa, Pisa, Italy; 2Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, Pisa, Italy
Background and Aims: Among the extra‐intestinal manifestations in Crohn's disease, Chronic Relapsing Inflammatory Optic Neuropathy (CRION) is an inflammatory optic neuropathy characterized by a strong responsiveness to steroids.
Methods: A 22‐year‐old woman suffering from Crohn's disease since 2014, undergoing multiple ileal resections, on Vedolizumab therapy. Since March 2023, during a flare‐up of IBD (and Vedolizumab suspension) she began to experience bilateral eyelid edema, photophobia, and pain during eye movements. She underwent endocrinological examination suspecting Graves' disease (negative autoantibodies, no hormonal profile alterations) and Ophthalmic examination (chemosis, conjunctival hyperemia, tearing). Brain MRI showed bilateral edematous impregnation of periocular soft tissues, lacrimal glands, periscleral tissues, lateral rectus muscles, and a swollen (non‐enhancing) appearance of the optic chiasm. Blood tests were normal. She went to the emergency department where a neurologist initiated high‐dose steroid therapy, with symptoms remission. A flare was observed upon tapering the dose, prompting the resumption of steroid therapy. Cervical spine MRI was negative and cerebrospinal fluid analysis showed no oligoclonal bands, negative viral and bacterial meningitis panel, polyclonal immunoglobulins, and 106 mg/dL protein. Anti‐AQP4, anti‐MOG, complement factors, myositis‐associated autoantibodies, ANA, AMA, LKM, and ENA were negative.
Results: In IBD, optic neuropathy may be ischemic (not detected during ophthalmic examination), reactive to anti‐TNF drugs (unlikely due to Vedolizumab therapy), demyelinating (ruled out by diagnostic workup), associated with rheumatological disease (excluded), or CRION. The latter seems most likely in this patient.
Conclusion: Timely diagnosis of CRION leads to rapid reversal with steroid therapy, avoiding permanent visual sequelae.
Disclosure: No disclosures.
EPO‐066
Evaluation of parameters affecting sexual dysfunction in multiple sclerosis: A preliminary study
Ö. Totuk; M. Türkkol; H. Güdek; D. Çetinkaya Tezer; İ. Güngör Doğan; Ş. Şahin; S. Demir
Neurology Clinic, Şehit Prof. Dr. İlhan Varank Sancaktepe Training and Research Hospital, İstanbul, Turkey
Background and Aims: This study aimed to analyze the factors affecting sexual dysfunction (SD) in Multiple Sclerosis (MS) which is one of the most important causes of disability in young adults.
Methods: Volunteers diagnosed with MS were included in the study. The Arizona Sexual Experiences Scale (ASEX), Beck Depression Inventory (BDI) and Short‐Form Health Survey (SF‐12) were used to screen for possible SD, assess depression and evaluate quality of life (QoL) respectively. MS types and disease‐modifying drugs (DMDs) used by patients were recorded. Disease durations were divided into four groups (1–3, 4–6, 7–9, ≥10 years).
Results: Socio‐demographic information of 418 MS patients is shown in Table 1. A positive correlation was found between ASES and BDI scores and a negative correlation with SF‐12. Multivariate variance analysis showed significant effects of BDI scores, gender and disease duration on SD. Women had higher ASES scores than men. As BDI scores increased, a significant increase in ASES was observed. SD was found in all disease duration groups, being more pronounced in the 1–3 and 4–6 year diagnosis groups. Age, MS type, DMD's used, education duration and SF‐12 levels had no significant effect on ASES scores.
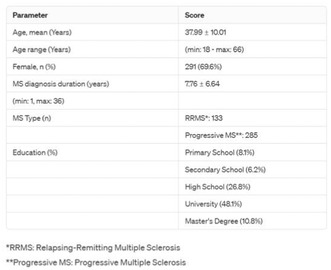
Sociodemographic Data of Patients
Conclusion: The study supports the literature in finding SD more common and associated with depression in women compared to men. SD and depression were more intense in patient groups diagnosed for up to six years, possibly due to changes in coping mechanisms over the years. Further studies are needed.
Disclosure: Nothing to disclose.
EPO‐067
The use of diffusion tensor tomography to assess the pyramidal system in patients with multiple sclerosis
A. Peshkin 1; S. Kotov2; G. Toniya3
1Multiple Sclerosis Centre, Moscow Regional Clinical and Research Institute, Moscow, Russian Federation; 2Department of Neurology, Moscow Regional Clinical and Research Institute, Moscow, Russian Federation; 3Department of Radiology, Moscow Regional Clinical and Research Institute, Moscow, Russian Federation
Background and Aims: The corticospinal tract (CSC) forms the basis of motor neurophysiology. The aim – to study CST in patients with highly active Multiple sclerosis (MS) during period of switching therapy.
Methods: 24 patients with MS were examined. Depending on severity of violations of pyramidal functional system (PFS) according to EDSS, patients were divided into 2 groups, group 1—17 patients with score of 0–2.5 points, group 2—7 patients with score of >= 3 points. Diffusion tensor images (DTI) were processed using the DTI FiberTrak software.
Results: There was a decrease in the volume of pyramidal tract in patients of group 2 (p < 0.001), an asymmetry of indicator was found, in several patients – decrease on the clinically intact side, which may indicate visually undetectable signs of damage to pyramidal tract. There was a distinct tendency towards decrease in fractional anisotropy and a decrease in length of pyramidal tract as pyramidal deficit increases (p < 0.001). Negative correlations were found between indicators of neurological deficit and volume and length of the pyramidal tract, as well as a direct correlation of duration of course of MS with apparent diffusion coefficient (ADC) and the reverse – with fractional anisotropy.
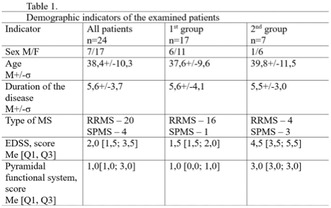
Patient data
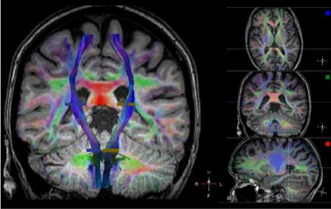
Visualization of CST using DTI
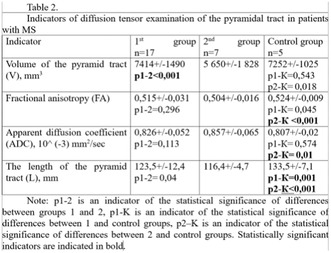
DTI results
Conclusion: The revealed decrease in volume and length of pyramidal tract, an increase in ADC, the asymmetry of these indicators, correlations with level of pyramidal insufficiency, EDSS and duration of the course of MS, obviously, can serve as additional criteria for assessing dynamics of disease and effectiveness of therapy.
Disclosure: Nothing to disclose.
EPO‐068
Characterizing double‐negative neuromyelitis optica spectrum disorder: A systematic review and meta‐analysis
A. Malvaso 1; G. Greco2; E. Ballante3; P. Businaro2; C. Morandi2; S. Scaranzin2; S. Masciocchi2; E. Marchioni4; D. Franciotta2; M. Gastaldi2
1Department of Brain and Behavioral Sciences, IRCCS “C. Mondino” National Neurological Institute, University of Pavia, Pavia, Italy; Neuroimmunology Research Unit, IRCCS “C. Mondino” National Neurological Institute, Pavia, Italy; 2Neuroimmunology Research Unit, IRCCS “C. Mondino” National Neurological Institute, Pavia, Italy; 3Political and Social Science Department, University of Pavia; BioData Science Unit, Mondino Foundation; 4Neurooncology and Neuroinflammation Unit, IRCCS “C. Mondino” National Neurological Institute, Pavia, Italy
Background and Aims: Neuromyelitis‐optica spectrum disorders (NMOSD) usually associate with aquaporin‐4 (AQP4) or myelin oligodendrocyte glycoprotein (MOG) antibodies. Seronegative‐NMOSD (SN‐NMOSD) has been described, but the clinical‐therapeutic profile is poorly defined.
Methods: We searched PubMed, Scopus and Google Scholar databases for studies reporting SN‐NMOSD patients, on which anti‐MOG‐Abs and AQP4‐Abs were tested. PRISMA guidelines and methodological quality control were assessed. Fixed or random‐effects models were used to pool results across studies.
Results: We included 36/1027 articles screened and analyzed 591 SN‐NMOSD patients (mean age: 30.3 [range 6–78]; female:male ratio; 2:1). Disease course was relapsing in 66% of cases. Brain MRI at onset showed brain abnormalities in 165/241 patients (69%) including tumefactive brain lesions in 19/241 (8%). Spinal cord MRI showed cervicothoracic lesions (99/241, 41%) and LETM (89/241, 37%). CSF analysis showed OCBs in 58/300 patients (19.3%). Mean annualized relapse ratio (ARR) was 0.77 (95% CI 0.10–1.8), and was higher in patients with late onset (>50 years, p < 0.001). Mean EDSS and late‐onset were associated with a relapsing course (p < 0.05). Relapsing SN‐NMOSD patients had a higher ARR and a worse outcome compared to AQP4‐NMOSD or MOG‐NMOSD. Among relapsing patients, 147/247 (60%) received a disease‐modifying treatment (DMT). The administration of any DMT led to a reduction of ARR (pre‐treatment: 0.83 ± 0.21 [95% CI 0.62–1.04, I 2 = 66.19%, p < 0.0001]; post‐treatment: 0.44 ± 0.17 [95% CI 0.27–0.60, I 2 = 85.81%, p < 0.0001]).
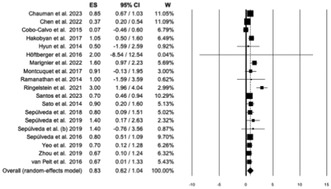
Forest plot with random‐effects models used to pool results of pre‐treatment ARR across studies, including early and late‐onset NMOSD.
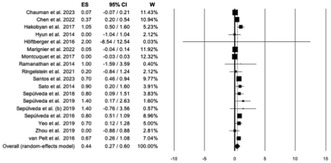
Forest plot with random‐effects models used to pool results of post‐treatment ARR across studies, including early and late‐onset NMOSD.
Conclusion: DN‐NMOSD is a severe condition with distinctive features compared to AQP4‐NMOSD. The administration of DMTs seems to be effective in this group of patients, but randomized clinical trials are needed.
Disclosure: The authors declare no conflicts of interest.
EPO‐069
Characterization of EEG patterns in a cohort of patients with autoimmune encephalitis
J. Moura 1; G. Videira1; J. Lopes1; J. Freitas2; E. Coutinho3; R. Samões1; E. Santos1
1Neurology Department, Unidade Local de Saúde Santo António, Porto, Portugal; 2Neurophysiology Department, Unidade Local de Saúde Santo António, Porto, Portugal; 3Centro de Neurociências e Biologia Celular, Universidade de Coimbra (CNC‐UC), Coimbra, Portugal
Background and Aims: Variable EEG features associated with autoimmune encephalitis (AIE) have been reported in the literature, the diagnostic/prognostic value of which remains unknown. We aim to describe the EEG features from an institutional AIE cohort.
Methods: Retrospective review of the clinical and EEG features of AIE patients (according to Graus criteria) diagnosed between 2000 and 2023.
Results: In total, 49 AIE cases were identified (57.1% male) including 30.6% anti‐NMDAr, 26.5% anti‐GAD65 and 26.5% seronegative. EEG abnormalities were present in 81.6%: 71.4% had slow activity and 46.9% had focal epileptiform activity. These mostly involved the temporal region (59.6% and 69.6%, respectively). The extreme‐delta brush pattern was present in 3 EEGs. Two patients presented with non‐convulsive status epilepticus. An abnormal EEG was present in 78.6% of patients with normal brain MRI (49.0%), corresponding to 44.8% of the cohort. The presence of any EEG abnormality was associated with seizures at presentation (p = 0.022). Even in patients without seizures, the EEG was abnormal in 65.0%. We found no significant difference in the EEG features when comparing serogroups, including seropositive vs. seronegative and intracellular vs. surface antibodies. The presence of slow activity was associated with an increased recurrence rate (p = 0.027) in AIE with intracellular antibodies, when diffuse, and with increased disability after 6.0 (3.0–8.0) years in AIE with intracellular antibodies (p = 0.042), when focal temporal.
Conclusion: EEG abnormalities are common in AIE, even in cases with normal brain MRI or without clinical seizures. The presence of slow activity may be a prognostic factor, depending on the antibody type.
Disclosure: The authors have nothing to disclose.
EPO‐070
The familiarity of romanian psychiatrists with anti‐N‐methyl‐D‐aspartate receptor encephalitis: A web‐based study
D. Pavăl 1; N. Gherghel‐Pavăl2; O. Căpățînă1; I. Micluția1
1Department of Psychiatry, “Iuliu Hațieganu” University of Medicine and Pharmacy, Cluj‐Napoca, Romania; 2Romanian Association for Autoimmune Encephalitis, Cluj‐Napoca, Romania
Background and Aims: Psychiatrists are often the first to be consulted in patients with anti‐N‐methyl‐D‐aspartate receptor (anti‐NMDAR) encephalitis. Thus, they need to be aware of clinical features, differential diagnoses, and treatment options for patients affected by this condition. In this study, we aimed to investigate the familiarity of Romanian psychiatrists with anti‐NMDAR encephalitis.
Methods: We recruited psychiatrists from Romania and conducted a cross‐sectional observational study by using a web‐based survey.
Results: 111 psychiatrists completed the survey, of whom 47 (42.34%) were specialists, while 64 (57.66%) were trainees. The median length of training for specialists was ten years (IQR 9.5), while for trainees was 2.5 years (IQR 3). In total, 31 (27.93%) psychiatrists encountered a case of anti‐NMDAR encephalitis, with no significant difference between specialists and trainees. 31 (27.93%) psychiatrists were either unaware of the disorder or only knew its name, while 77 (69.37%) had knowledge of an outline of it. Only 3 (2.7%) psychiatrists had comprehensive knowledge of the disorder. Respondents with a higher awareness level had undergone significantly longer training (p = 0.014). Unsurprisingly, having encountered a case significantly influenced awareness levels (p < 0.001). There were no significant differences between specialists and trainees regarding specific knowledge about anti‐NMDAR encephalitis. However, higher awareness levels and having encountered a case significantly influenced answer accuracy for questions regarding psychiatric presentation and epidemiological features.
Conclusion: Our study indicates that Romanian psychiatrists have suboptimal knowledge of anti‐NMDAR encephalitis, highlighting the need for improved awareness of this disorder.
Disclosure: Nothing to disclose.
EPO‐071
Neural antibodies in first‐episode psychosis patients with warning signs for autoimmune encephalitis
D. Pavăl 1; N. Gherghel‐Pavăl2; O. Căpățînă1; A. Stan3; L. Raduly4; L. Budișan4; I. Micluția1
1Department of Psychiatry, “Iuliu Hațieganu” University of Medicine and Pharmacy, Cluj‐Napoca, Romania; 2Romanian Association for Autoimmune Encephalitis, Cluj‐Napoca, Romania; 3Department of Neurology, “Iuliu Hațieganu” University of Medicine and Pharmacy, Cluj‐Napoca, Romania; 4Research Center for Functional Genomics, Biomedicine and Translational Medicine, “Iuliu Hațieganu” University of Medicine and Pharmacy, Cluj‐Napoca, Romania
Background and Aims: While autoimmune encephalitis (AE) remains an essential differential diagnosis in first‐episode psychosis (FEP), testing all FEP patients for neural antibodies is not feasible in real‐world clinical practice. Thus, some researchers suggest selective testing in patients with warning signs of AE. Moreover, criteria have been proposed for a category of so‐called autoimmune psychosis (AP). Here, we aimed to determine the prevalence of AE in a cohort of patients with FEP.
Methods: To achieve our objective, we used a phenotype‐driven algorithm. Initially, we screened patients for “yellow” and “red flags” indicating low or high pre‐test probability warning signs for AE, respectively. We also evaluated patients for previously proposed warning signs and AP criteria. Next, patients with red flags underwent cerebrospinal fluid analysis (including neural antibodies), while patients with yellow flags underwent tests for serum neural antibodies, EEG, and brain MRI.
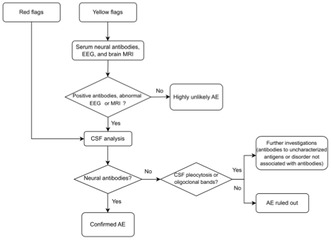
A phenotype‐driven algorithmic approach for detecting autoimmune encephalitis in patients with first‐episode psychosis. Abbreviations: AE, autoimmune encephalitis; CSF, cerebrospinal fluid.
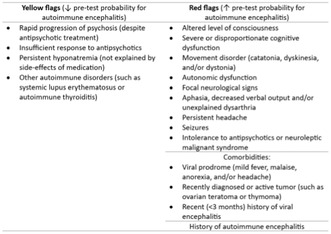
Warning signs for autoimmune encephalitis in patients with first‐episode psychosis were defined as “yellow” (low pre‐test probability) and “red flags” (high pre‐test probability).
Results: We screened 78 patients with FEP and found that eight (10.3%) had at least one warning sign for AE: four (5.13%) patients had at least one red flag, while four (5.13%) had only yellow flags. Four (5.13%) patients met the criteria for possible AP. Two patients (2.56%) had anti‐NMDAR encephalitis, while the remaining six (7.69%) received a primary psychiatric disorder diagnosis. The AP criteria failed to identify patients with definite AP due to a lack of paraclinical criteria.
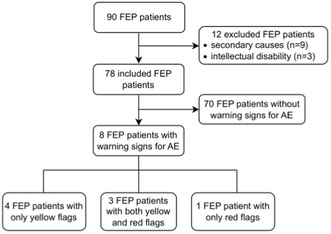
Selection and inclusion of patients with first‐episode psychosis and warning signs for autoimmune encephalitis.
Conclusion: Our study emphasizes the significance of including AE in the differential diagnosis of FEP.
Disclosure: This work was supported by the Iuliu Hațieganu University of Medicine and Pharmacy, Cluj‐Napoca, Romania (grants no. 881/41/12.01.2022 and 772/32/11.01.2023).
EPO‐072
Update of the treatment of pediatric neuromyelitis optica spectrum disorders
M. Elkhooly 1; F. Bao2; S. sriwastava3; M. Ismail4
1Department of Neurology, Southern Illinois University School of Medicine, Springfield, IL, USA; Department of Neurology, Wayne State University, Detroit, MI, USA; Department of Neurology and Psychiatry, Minia University, Minia, Egypt; 2Department of Neurology, Wayne State University, Detroit, MI, USA; 3Department of Neurology, McGovern Medical School, Houston, Texas, USA; 4Department of Neurology and Psychiatry, Minia University, Minia, Egypt
Background and Aims: Neuromyelitis Optica Spectrum Disorders (NMOSDs) is a collection of inflammatory and demyelinating disorders affecting the central nervous system. Given the severity and recurrence nature of the attacks, effective and safe treatment modalities are crucial. This study aims to provide an update on the current and emerging therapies for NMOSDs in the pediatric population.
Methods: We conducted a comprehensive analysis of the existing medications utilized in the treatment of pediatric NMO, encompassing both those currently being investigated in clinical trials for pediatric NMO on clinicaltrials.gov and the NIH website, as well as articles published on PubMed and Embase since 2008.
Results: A total of 15 studies have been conducted to examine the effects of 7 distinct drugs. A total of 231 patients were enrolled /anticipated to be enrolled, with 139 receiving Azathioprine, 21 receiving rituximab, 24 receiving mycophenolate mofetil, 12 receiving eculizumab, 15 receiving Inebilizumab, 12 receiving Ravulizumab, and 8 receiving Satralizumab. Azathioprine, mycophenolate mofetil, and rituximab are commonly utilized and generally regarded as safe. Various monoclonal antibodies, such as eculizumab, Inebilizumab, Ravulizumab, and Satralizumab, are currently undergoing testing to determine their effectiveness and safety.
Conclusion: Pediatric NMO treatment is still challenging, further clinical trials and research are warranted.
Disclosure: None.
EPO‐073
Characterization of neuropeptide cortistatin in multiple sclerosis patients
C. Adan1; R. Luque Huertas2; R. Piñar Morales1; F. Barrero Hernández1; E. González‐Rey4
1Clínico San Cecilio University Hospital, Granada, Spain; 2Maimonides Biomedical Research Institute, Cell Biology, Physiology and Immunology, Córdoba, Spain
Background and Aims: Multiple sclerosis (MS) diagnosis is based on clinical, radiological and biochemical criteria. However, it is necessary to find specific and reliable biomarkers to assess disease activity. We hypothesize that endogenous neuroimmune mediators could be a new type of molecules which address the progression of this autoimmune disorder.
Methods: To assess the potential of cortistatin (CST), an anti‐inflammatory and neuroprotective neuropeptide crucial in neuroimmune interactions, as a peripheral biomarker, blood samples were taken from patients with relapsing‐remitting MS. CST levels were analyzed in plasma and serum. We also evaluated by a microfluidic qPCR the gene expression of CST and specific receptors as well as the relationship of CST and the immune response in peripheral mononuclear blood cells isolated from MS patients.
Results: We observed that, although CST levels were unchanged in plasma they were significantly reduced in serum from MS patients compared to healthy controls. Of note, we found that CST was highly susceptible to degradation in serum. We also demonstrated that immunomodulatory therapies did not affect CST plasma levels, except for patients treated with beta interferon, they showed increased plasma CST. Interestingly, we found that the gene expression of CST and related peptides were similar between patients and controls, while expression for the GPR107 receptor, a recently discovered receptor in the somatostatin system, was significantly downregulated in MS patients.

FIGURE 1

FIGURE 2
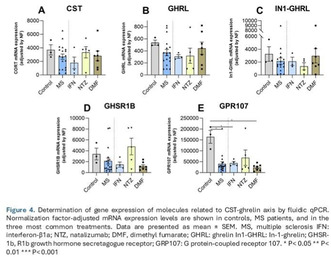
FIGURE 3
Conclusion: Our results suggest that the CST system could be altered in MS patients. However, further studies are needed to determine its role during the pathogenesis of MS and its relationship with current treatments.
Disclosure: The author declares no conflicts of interest.
EPO‐074
The role of innovative therapies in refractory myasthenia gravis: Are they interchangeable and safe? A case‐series
A. Sarnataro 1; C. Pane1; N. Cuomo1; M. Campanile1; G. Puorro1; A. Marsili1; F. Saccà2; M. Garibaldi3; L. Fiondi4
1NSRO Department, Federico II University, Naples, Italy; 2GENESIS Department, Federico II University, Naples, Italy; 3Neuromuscular and Rare Disease Centre, Sant'Andrea Hospital, Rome, Italy; 4Department of Neuroscience, Mental Health and Sensory Organs (NESMOS), Faculty of Medicine and Psychology, SAPIENZA University of Rome, Rome, Italy
Background and Aims: Myasthenia Gravis (MG) therapies have dramatically changed in the last few years with the introduction of complement inhibitors and neonatal Fc receptor blockers. There are no data available on retreatment options in non‐responder patient. We performed a case‐series including four patients treated with innovative therapies that underwent a switch from anti‐complement to FcRn blockers and viceversa.
Methods: We enrolled 4 patients with refractory MG treated with Efgartigimod (Pt. 1 and Pt. 2) and Ravulizumab (Pt. 3 and Pt. 4).They all underwent major clinical deterioration and switched to therapies with a different mechanism of action. We performed MG‐ADL at the baseline and weekly, QMG at the baseline and after induction period of Eculizumab and cycle 1 of Efgartigimod and then every 3 months.
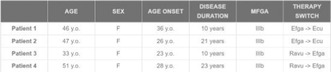
Patients’ characteristics description
Results: In the group of patients switching from Efgartigimod to Eculizumab we observed a mean MG‐ADL reduction of 9 and a QMG reduction of 8.5 points after the induction period. Patients remained in the Minimal Symptom Expression for all the maintenance period. Ravulizumab to Efgartigimod switching group observed a MG‐ADL global reduction of 5.5 points and a QMG reduction of 4 points after cycle 1. No major adverse events were observed except for Pt .4 who suffered from systemic infection. Efgartigimod was suspended and readministered after the resolution of the infection.
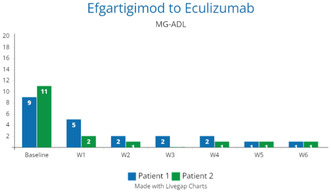
Efgartigimod to Eculizumab Group MG‐ADL
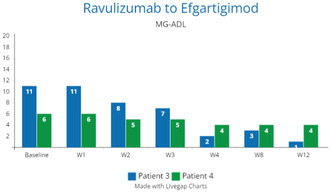
Ravulizumab to Efgartigimod Group MG‐ADL
Conclusion: Switch between innovative treatments with different mechanism of action proved to be a successful strategy in non‐responders. Both Eculizumab and Efgartigimod succeeded in improving clinical status after few weeks of treatment. Further data collection is needed to assess the long‐term efficacy of therapeutic switches.
Disclosure: Nothing to disclose.
EPO‐075
Cerebrospinal fluid interleukin‐6 as a potential biomarker in CNS neuroinflammatory diseases: A real world analysis
E. Virgilio 1; P. Garelli2; A. Dutto1; L. Giordano1; I. Pastore1; F. Franchino1; G. Micca3; G. Visconti Rossi3; M. Capobianco1
1Neurology Unit, Department of Medicine, ASO Santa Croce e Carle, Cuneo, Italy; 2MS Center and Neurologia I U, Dipartimento di Neuroscienze e Salute Mentale, A.O.U. Città della Salute e della Scienza di Torino, Torino, Italy/Dipartimento di Neuroscienze "Rita Levi Montalcini," Università di Torino, Torino, Italy; 3Clinical Biochemistry, ASO Santa Croce e Carle, Cuneo, Italy
Background and Aims: Interleukin‐6 (IL‐6) pathways have recently been described in the pathogenesis of neuromyelitis optica spectrum disorder (NMOSD). Some data suggest that CSF IL‐6 may be a short‐term prognostic biomarker in NMOSD. However, whereas various cytokines would be involved in the pathogenesis of inflammatory disease, the differences in cerebrospinal fluid (CSF) cytokines between different inflammatory diseases remain unclear. We aimed to compare CSF IL‐6 levels among various neurological inflammatory disorders and to explore the relationship between CSF IL‐6 and various intrathecal immunoglobulin (Ig) indexes.
Methods: From May 2023 we prospectively obtained IL‐6 levels in consecutive CSF samples in patients suspected of an inflammatory disease of the CNS. IL‐6 has been tested by commercially available ECLIA Kit. We also collected CSF cell count, protein levels, quantitative IgG indexes such as Link Index and Kappa‐free‐light‐chain Index using nephelometry, and oligoclonal band (OB) status using isoelectrofocusing on agarose gel.
Results: So far, 20 patients (13 female, 10MS, 4 NMOSD/MOGAD, 2 clinically isolated syndrome and 4 non‐inflammatory controls), with a mean age of 42.5 years (SD 13.4) were enrolled. Patients with NMOSD/MOGAD showed higher IL‐6 levels compared to MS (35.25 ± 33.14 vs 4.98 ± p: 0.05 pg/ml). An inverse correlation of IL‐6 levels was observed with Link Index (r: −0.56 p: 0.01), Kappa‐Index (r: −0.29 p: 0.2) and patients without OB displayed higher levels of CSF IL‐6 (17.15 ± 23.21 vs 4.93 ± 2.15 p: 0.05 pg/ml).
Conclusion: Our preliminary data support the potential of CSF IL‐6 as a diagnostic biomarker in CNS inflammatory diseases. We plan to confirm our observation on a larger sample size.
Disclosure: Nothing to disclose.
Cognitive neurology/neuropsychology 1
EPO‐076
Prevalence and pattern of cognitive impairment in patients awaiting kidney and liver transplantation
A. Golenia 1; P. Olejnik1; M. Grusiecka‐Stańczyk2; N. Żołek3; E. Wojtaszek4; P. Żebrowski4; J. Raszeja‐Wyszomirska2; J. Małyszko4
1Department of Neurology, Medical University of Warsaw, Warsaw, Poland; 2Department of Hepatology, Transplantology, and Internal Medicine, Medical University of Warsaw, Warsaw, Poland; 3Institute of Fundamental Technological Research, Polish Academy of Sciences, Warsaw, Poland; 4Department of Nephrology, Dialysis and Internal Medicine, Medical University of Warsaw, Warsaw, Poland
Background and Aims: Cognitive impairment (CI) is common in both end‐stage kidney disease (ESKD) and end‐stage liver disease (ESLD). The goal of the study was to assess the prevalence and pattern of CI in patients awaiting kidney and liver transplantation.
Methods: In this cross‐sectional, prospective study, 27 consecutive patients with ESKD and 27 consecutive patients with ESLD due to alcoholic liver disease, all currently on transplant waiting lists, were screened for cognitive decline using the Addenbrooke's Cognitive Examination. Medical history, demographics and laboratory test results were also collected.
Results: The prevalence of CI among patients with ESKD and ESLD was 27% and 88%, respectively. In both groups, the most impaired cognitive domain was memory and additionally verbal fluency in patients with ESRD and visuospatial abilities in patients with ESLD. The most statistically significant increase in the prevalence of CI was found in patients with fewer years of schooling, in both ESLD and ESKD populations, and in elderly patients, but only in the ESLD group. Additionally, better cognitive functioning in ESKD patients was associated with higher levels of total lymphocyte count and alanine transaminase (ALT), and in ESLD patients with higher levels of ALT and aspartate transaminase.
Conclusion: The prevalence of CI, especially in patients with ESLD, is high and may negatively affecting the transplantation process. Routine screening tests in this group would contribute to the implementation of effective treatments and facilitate the provision of specialized health care.
Disclosure: Nothing to disclose.
EPO‐077
A case of phonagnosia in a patient carrying C9orf72 gene mutation
E. Stanitsa; L. Apostolakopoulou; E. Angelopoulou; V. Konstadinides; R. Antonellou; G. Velonakis; G. Karadima; G. Koutsis; L. Stefanis; S. Papageorgiou
Department of Neurology, Eginition University Hospital, Athens, Greece
Background and Aims: Phonagnosia is a rare selective impairment of familiar voice recognition, with relative intact comprehension and recognition of faces. Compared to prosopagnosia, phonagnosia has been infrequently described in neurodegenerative diseases, and relative genetic evidence is scant.
Methods: We describe a case of a 56 years‐old female patient, a primary school teacher, mainly presenting with progressive difficulty in recognizing familiar voices through the telephone, with intact recognition of familiar faces. Difficulties in concentration, visuospatial abilities, low information processing speed and apathy were also reported by her husband. Family history was positive for amyotrophic lateral sclerosis.
Results: Neurological examination was normal. MMSE was 26/20, and FAB was 13/18. The extensive neuropsychological examination revealed deficits in attention, executive function, visuospatial perception and memory, as well as impaired phonological and semantic verbal fluency. Brain MRI showed mild generalized cortical and hippocampal atrophy. Routine blood tests and electroencephalogram were normal. Audiological and ophthalmological evaluation was normal. CSF examination revealed normal TAU, p‐tau and β‐amyloid levels. Genetic analysis revealed C9orf72 expansion mutation. Phonagnosia was confirmed experimentally, by examining familiar voice recognition in a small sample of cognitively normal individuals of similar age. Recently, another case of progressive phonagnosia was described in a patient with a C9orf72 expansion and frontotemporal dementia.
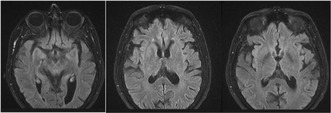
Brain MRI (FLAIR) of our patient demonstrating mild generalized cortical and hippocampal atrophy
Conclusion: To our knowledge this is the second case report of a patient with C9orf72 mutation presenting with phonagnosia. This might be partially explained by the overload οf the neural network processing voices – due to her professional activity, combined with genetic mechanisms.
Disclosure: None.
EPO‐078
Unveiling constructional apraxia in huntington's disease through neurophysiological markers
A. Giglio; A. De Rosa; G. De Michele
Department of Neurosciences and Reproductive and Odontostomatological Sciences, Federico II University, Naples, Italy
Background and Aims: This study investigates constructional apraxia (CA) in HD, a feature insufficiently explored. Our aim is to unravel CA's cognitive underpinnings within the HD population, shedding light on potential associated cognitive markers.
Methods: Seventy HD patients from the Enroll‐HD study were recruited, meeting specific inclusion criteria including a positive molecular HD test, clinically evident neurocognitive disease, ≥2 years of formal education, and the absence of other cognitive‐impairing neurological disorders. Comprehensive assessments encompassed neuropsychological, psychiatric, motor, and functional evaluations. CA presence and type were determined via a copying task.
Results: Unexpectedly, 32 HD participants exhibited constructional apraxia (CA), yet no significant differences emerged between CA and no‐CA groups in demographic, clinical, motor, or functional aspects (all p > 0.05). MANOVA revealed overall non‐significant neuropsychological differences, but AC participants scored significantly lower on Symbol digit modality test, Stroop‐color word – reading, Stroop‐color word – interference, and Phonological verbal fluency tests (all p < 0.05). Logistic regression, statistically significant (Χ2 [8] = 7.625, p = 0.006; Cox & Snell R2 = 0.057), linked AC only to Stroop‐color word – interference test (Wald: 7.166, p = 0.007, OR: 0.955, 95% CI: 0.924–0.988).
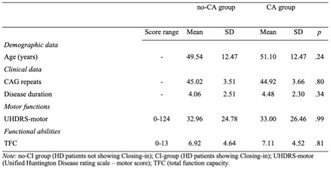
Means and SDs on demographic data, clinical data, motor functions, and functional abilities in HD patients showing or not showing CA
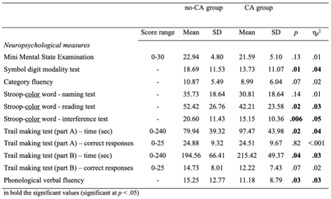
Means and SDs on neuropsychological measures in HD patients showing or not showing CA
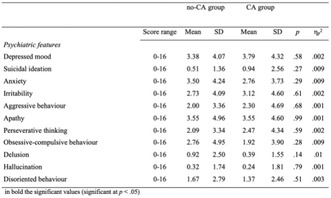
Means and SDs on psychiatric features in HD patients showing or not showing CA
Conclusion: The Stroop‐color word – interference test emerges as a predictor for constructional apraxia (CA), indicating its potential role in early detection and intervention for HD. These findings deepen our understanding of cognitive manifestations in HD, guiding future research and clinical strategies.
Disclosure: Nothing to disclose.
EPO‐079
Cognitive rehabilitation effects on grey matter volume and Go‐noGo activity in progressive MS: Results from CogEx study
M. Rocca 1; P. Valsasina2; F. Romanò2; R. Motl3; M. Amato4; G. Brichetto5; D. Boccia6; J. Chataway7; N. Chiaravalloti8; G. Cutter9; U. Dalgas10; J. DeLuca8; R. Farrell7; P. Feys11; J. Freeman12; M. Inglese6; C. Meza13; A. Salter14; B. Sandroff8; A. Feinstein13; M. Filippi15
1Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 3Department of Kinesiology and Nutrition, University of Illinois Chicago, Chicago, IL, USA; 4Department NEUROFARBA, University of Florence; and IRCCS Fondazione Don Carlo Gnocchi, Florence, Italy; 5Scientific Research Area, Italian Multiple Sclerosis Foundation (FISM), and Rehabilitation Service, Italian Multiple Sclerosis Society (AISM), Genoa, Italy; 6Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, and Center of Excellence for Biomedical Research, University of Genoa, Genoa, Italy; 7Queen Square Multiple Sclerosis Centre, Department of Neuroinflammation, UCL Queen Square Institute of Neurology, London, UK; 8Kessler Foundation, West Orange, NJ, USA, and Department of Physical Medicine & Rehabilitation, Rutgers NJ Medical School, Newark, NJ, USA; 9Department of Biostatistics, University of Alabama at Birmingham, Birmingham, AL, USA, 10Exercise Biology, Department of Public Health, Aarhus University, Aarhus, Denmark, 11REVAL, Faculty of Rehabilitation Sciences, Hasselt University, Diepenbeek, Belgium, 12Faculty of Health, School of Health Professions, University of Plymouth, Devon, UK, 13Department of Psychiatry, University of Toronto and Sunnybrook Health Sciences Centre, Toronto, ON, Canada, 14Department of Neurology, Section on Statistical Planning and Analysis, UT Southwestern Medical Center, Dallas, TX, USA, 15Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: CogEx (ClinicalTrials.gov, NCT03679468) was a randomized, sham‐controlled trial determining effectiveness of cognitive rehabilitation (CR) and aerobic exercise (EX) in progressive multiple sclerosis (PMS). We present volumetric MRI and task‐related functional MRI (fMRI) findings.
Methods: Participants were randomized (1:1:1:1) to “CR‐plus‐EX”, “CR‐plus‐sham‐EX (EX‐S)”, “EX‐plus‐sham‐CR (CR‐S)”, and “CR‐S‐plus‐EX‐S” and attended 12‐week intervention. Physical/cognitive assessments were performed at baseline, immediately after intervention (week‐12) and 6 months post‐intervention (month‐9). MRI sub‐study participants underwent volumetric MRI and fMRI (Go‐NoGo task).
Results: 104 PMS participated in the MRI sub‐study (“CR‐plus‐EX”: n = 25; “CR‐plus‐EX‐S”: n = 28; “CR‐S‐plus‐EX”: n = 25; “CR‐S‐plus‐EX‐S”: n = 26); 88 (85%) completed baseline and week‐12 volumetric MRI and 84 (81%) completed Go‐NoGo fMRI. At week‐12 and month‐9, no differences were found among interventions for symbol‐digit modalities test (SDMT) correct responses, nor for SDMT, California verbal learning test (CVLT) and brief visuospatial memory test Z‐scores (p = range 0.12–0.94). Time‐by‐treatment interactions for changes at week‐12 vs baseline of normalized grey matter (NGMV) (p = 0.10) and cortical GM (NcGMV) (p = 0.10) volumes were not significant. However, they became significant (p = 0.04; p = 0.02, respectively) when comparing all patients performing CR vs those performing CR‐S. “CR‐plus‐EX‐S” patients exhibited Go‐NoGo‐related fMRI activity increase (p < 0.05, corrected) at week‐12 vs baseline in bilateral insular regions. In all CR patients, increased NGMV (r = 0.42, p = 0.004) and NcGMV (r = 0.36, p = 0.01) at week‐12 vs baseline correlated with increased CVLT Z‐score.
Conclusion: Conclusions. CR modulated GM volumes and insular fMRI activity in PMS. Funding. Funded by the MS Society of Canada (grant #EGID3185). Ancillary funding from CMSC, Danish MS Society, and National MS Society.
Disclosure: Nothing to disclose.
EPO‐080
Altered cognition in Parkinson patients with depression compared to major depressive individuals
B. Yulug 1; S. Cankaya1; E. Ozdemir Oktem1; A. Ozsimsek1; C. Sayman1; D. Sayman1; R. Karaca1; U. Duran1; L. Hanoglu2
1Department of Neurology, Alanya Alaaddin Keykubat University, Antalya, Turkey; 2Research Institute for Health Sciences and Technologies (SABITA), Clinical Electrophysiology, Neuroimaging and Neuromodulation Laboratory, Istanbul Medipol University, Istanbul, Turkey
Background and Aims: The interaction of depression heralding PD and incidental depression after the diagnosis of PD is complex requiring a unified pathophysiological model of depression in PD. Here we explored the connectivity and cognitive differences between PD patients (with and without depression), Control and MDD patients. Our results indicate considerable cognitive and connectivity differences between PD and MDD patients suggesting a compensatory phase specific to PD, regardless of the pathophysiology of depression.
Methods: 38 Parkinson's outpatients (aged 49–86 years; 23 depressive (PDD) and 15 non depressive (PND)) and 46 healthy controls (aged 20–81 years; 22 depressive (MDD) and 24 non depressive (ND)) were recruited by their clinicians. We applied MMSE, MOCA and HDRS test to all the participants for cognitive and depression assessment.
Results: There was significant difference in terms of age (p < .001), education years (p = 0.009) and HDRS scores (p < .001). After adjusting age and education years, our findings revealed significant differences in orientation (p = 0.050) and abstraction (p = 0.005) scores which are subtests of MOCA without any difference in MOCA scores between PDD and MDD groups. We also observed that the MDD patients were clearly impaired on tests known to assess non‐verbal primary memory, as well as verbal and non‐verbal episodic memory compared to non‐demented PD, a finding that has been confirmed both in non‐depressed and depressed PD compared to MDD (p < .005).
Conclusion: Our study revealed valuable findings considering cognitive impairment in PD patients with depression compared to major depressive disorder (MDD). We believe that our results hold a clinicaş value for the literature.
Disclosure: Nothing to disclose.
EPO‐081
The affective and cognitive theory of mind and associated brain functional alterations in patients with PPA
E. Canu 1; C. Tripodi1; A. Marangon2; V. Castelnovo1; S. Basaia1; E. Spinelli3; G. Cecchetti4; F. Caso5; G. Magnani5; P. Caroppo6; S. Prioni6; C. Villa6; L. Tremolizzo7; I. Appollonio7; F. Verde8; N. Ticozzi9; V. Silani9; M. Filippi10; F. Agosta3
1Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 3Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 4Neurophysiology Service, Neurology Unit, and Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute Milan, Italy; 5Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; 6Fondazione IRCCS Istituto Neurologico Carlo Besta, Unit of Neurology 5 – Neuropathology, Milan, Italy; 7Neurology Unit, “San Gerardo” Hospital and University of Milano‐Bicocca, Monza, Italy; 8Department of Neurology and Laboratory of Neuroscience, IRCCS Istituto Auxologico Italiano, Milano, Italy; 9Department of Neurology and Laboratory of Neuroscience, IRCCS Istituto Auxologico Italiano, and “Dino Ferrari” Center, Department of Pathophysiology and Transplantation, Università degli Studi di Milano, Milan, Italy, 10Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: We aimed to investigate cognitive and affective theory of mind (ToM) abilities in semantic (svPPA) and nonfluent (nfvPPA) variants of primary progressive aphasia, compared to other frontotemporal lobar degeneration (FTLD) cases, such as behavioral (bvFTD) and right temporal variants (rtvFTD). Moreover, this study explored the neural correlates of affective and cognitive ToM alterations in these FTLD syndromes.
Methods: Sixty‐seven FTLD patients (14 nfvPPA, 17 svPPA, 23 bvFTD and 13 rtvFTD) and 98 healthy controls underwent neuropsychological evaluation, structural and resting‐state functional MRI. Based on literature, two regions of interest (medial prefrontal cortex‐lmPFC and right supramarginal gyrus‐rSMG) were created as main nodes for affective and cognitive ToM, and RS functional connectivity (RS‐FC) networks were obtained. Using graph analysis and connectomics, global and regional functional brain connectivity were assessed and compared between groups. Patients underwent the affective (SET‐EA) and cognitive (SET‐IA) ToM subtests of the Story‐Based Empathy Task (SET), and their performances were compared across groups.
Results: Affective and cognitive ToM abilities as measured by the SET appeared similarly impaired in all patients’ groups, including PPA. Significant regional RS‐FC alterations within both affective and cognitive networks were observed in each group of patients as compared with healthy controls.
Conclusion: These findings suggest a deterioration of affective and cognitive ToM skills in FTLD patients, including PPA, which seems to be related to similar functional connectivity alterations. The present study emphasizes the importance of socio‐cognitive features in the early detection of FTLD conditions. Funding. European Research Council (StG‐2016_714388_NeuroTRACK); Foundation Research on Alzheimer Disease.
Disclosure: E Canu research support from Italian Ministry of Health. C Tripodi, A Marangon, V Castelnovo, E Spinelli, F Caso, G Magnani, P Caroppo, S Prioni, C Villa, L Tremolizzo, I Appollonio, F Verde nothing to disclose. S. Basaia research support from Italian Ministry of Health (IMH). G. Cecchetti speaker honoraria from Neopharmed Gentili. N Ticozzi consulting services for Amylyx Pharmaceuticals, Zambon Biotech SA and lectures for Italfarmaco; funding from IMH and AriSLA. V Silani consulting services and/or speaking activities for AveXis, Cytokinetics, Italfarmaco; and research support from IMH, AriSLA, and E‐Rare Joint Transnational Call. M Filippi consulting or speaking activities or advisory boards for Alexion, Almirall, Biogen, Bayer, Bristol‐Myers Squibb,Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA; scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol‐Myers Squibb, Lilly, Novartis, Sanofi‐Genzyme; research support from Biogen Idec, Merck‐Serono, Novartis, Roche, IMH, Italian Ministry of University and Research, and FISM. F Agosta received speaker honoraria from Biogen Idec, Italfarmaco, Roche, Zambon and Eli Lilly, and has received research supports from IMH, Italian Ministry of University and Research, ARiSLA, ERC, EU Joint Programme – Neurodegenerative Disease Research, and Foundation Research on Alzheimer Disease.
EPO‐082
Improving cognitive functions in healthy subjects using tACS and individual theta frequency
B. Yuluğ1; C. Sayman 1; S. Cankaya1; E. Ozdemir Oktem1; A. Ozsimsek1; A. Berekelia2; U. Duran1; D. Sayman1; R. Karaca1; L. Ipek1; L. Hanoglu3
1Alanya Alaaddin Keykubat University, Department of Neurology and Neuroscience, Antalya, Turkey; 2Bahcesehir University, Department of Neurology, Istanbul, Turkey; 3Istanbul Medipol University, Department of Neurology, Istanbul, Turkey
Background and Aims: Transcranial Alternating Current Stimulation (tACS), a non‐invasive method, aims to enhance cognitive abilities in healthy individuals and those with cognitive challenges by replicating brain activity. Beyond cognitive neuroscience, it shows promise for psychiatric issues like schizophrenia. This study explores tACS effects on eight healthy individuals aged 26 to 34.
Methods: Cognitive assessments (MMSE, MoCA, STROOP test, trail making parts A and B, short‐term memory, Recall, Wechsler memory scale), EEG scans, and depression level evaluations conducted before and after tACS stimulation. Personalized tACS stimulation was administered to the dorsolateral prefrontal cortex (DLPFC) area, utilizing individual theta frequency (ITF) determined with MetLab. The 20‐minute sessions, spanning five days, employed a 2 mA sinusoidal oscillating current at minus one ITF (4–8 Hz) to enhance cognitive functions. Post‐stimulation, participants underwent the same battery of cognitive tests and EEG scans.
Results: The statistical analysis, utilizing paired samples T‐test with a significance threshold of p < 0.005, revealed no significant change in depression levels (p = 0.439). While Wechsler memory scale, MoCA, MMSE, and STROOP tests exhibited no noteworthy differences, there were significant improvements in short‐term memory (p = 0.041) and trail making part B (p = 0.008) (Table 1).
Conclusion: In conclusion, tACS, a well‐established non‐invasive brain stimulation technique, has demonstrated cognitive benefits in various conditions. This study reinforces existing literature, indicating notable enhancements in short‐term memory and executive function (trail making) after five days of tACS stimulation. Further investigations should involve larger participant groups to consolidate and expand upon these findings.
Disclosure: Nothing to disclose.
EPO‐083
Effects of episodic and chronic tension type headache on cognition and empathic neural responses: A fMRI study
B. Yulug1; S. Cankaya1; C. Sayman 1; E. Ozdemir Oktem1; A. Ozsimsek1; U. Aylak2; B. Ayyıldız3; D. Sayman1; R. Karaca1; A. Aktürk1; L. Hanoglu4; A. Velioğlu5
1Alanya Alaaddin Keykubat University, Department of Neurology and Neuroscience, Antalya, Turkey; 2Bahcesehir University, Department of Neurology, Istanbul, Turkey; 3Anatomy PhD Program, Graduate School of Health Sciences, Kocaeli University, Istanbul, Turkey; 4Istanbul Medipol University, Department of Neurology, Istanbul, Turkey; 5Center for Psychiatric Neuroscience, Feinstein Institute for Medical Research, Manhasset, New York, USA
Background and Aims: This study delves into tension‐type headache (TTH), emphasizing its prevalence and impact on health and daily life. The evolving understanding of TTH's neurological basis, particularly altered central pain perception, prompts a need for comprehensive studies on mood, cognitive function, and pain empathy. The study aims to evaluate cognitive and empathic neuroimaging correlates of TTH, addressing the lack of integrated studies in this area.
Methods: The enrollment comprised 102 participants (46 TTH patients, 41 healthy controls) from Alanya University, diagnosed following International Headache Committee criteria. Exclusion criteria covered various conditions, and ethical approval was obtained. Structural and resting‐state fMRI scans were conducted with specific parameters.
Results: Analyzing demographic and clinical data, age differences were nonsignificant (p > 0.05), while education years significantly varied (p < 0.001). MOCA scores exhibited a significant difference (p < 0.05), with tension‐type headache patients scoring lower. Subgroup analysis of episodic and chronic patients revealed no significant differences in neurocognitive tests, volume, or connectivity (p > 0.05).
Conclusion: The study proposed a potential reverse causal relationship, suggesting individuals with higher empathy levels might be more susceptible to developing TTH. The decline in cognitive scores correlated with increased headache intensity, indicating a complex interaction between acute headache episodes, pain processing, and cognition. fMRI results demonstrated changes in brain regions associated with acute pain, impacting executive functions and highlighting the cost of cognition during acute pain episodes. It provides valuable insights into the intricate relationship between TTH, cognitive function and pain empathy, contributing to the understanding of the neurological underpinnings of TTH and its broader implications.
Disclosure: Nothing to disclose.
EPO‐084
Neurocognitive correlates of awareness of everyday functioning in middle‐aged and older adults with HIV
A. Jacob1; M. Crowe1; V. Del Bene2; P. Fazeli3; D. Stavrinos4; D. Vance 3
1Department of Psychology, University of Alabama at Birmingham, Birmingham, Alabama, USA; 2Department of Neurology, University of Alabama at Birmingham, Birmingham, Alabama, USA; 3School of Nursing, University of Alabama at Birmingham; 4Institute of Social Science Research, University of Alabama, Tuscaloosa, Alabama, USA
Background and Aims: People living with HIV (PLWH) are vulnerable for cognitive decline and are at greater risk for impaired everyday functioning; however, they may lack self‐awareness of such impairments. We examined neuropsychological correlates of self‐awareness of everyday functioning in PLWH.
Methods: In this cross‐sectional study, 260 PLWH (40+ years) completed a comprehensive assessment including neuropsychological tests as well as self‐report (i.e., Lawton and Brody IADL Questionnaire) and performance‐based measures of everyday functioning (i.e., Timed Instrumental Activities of Daily Living). Self‐awareness of functional status was calculated in the domains of medication management, financial management, telephone use, and grocery shopping. An algorithm was developed to classify accurate reporters, under‐reporters, and over‐reporters using cut‐offs between actual performance vs self‐reported performance. Multinomial and binomial logistic regression equations were used.
Results: For financial management, participants with higher scores in executive function/attention were less likely to be under‐reporters, while participants with higher depression were more likely to over‐report difficulties. For medication management, word‐reading emerged as the only significant predictor of inaccurate vs accurate reporting. For telephone use, participants who scored higher on executive function/attention and word‐reading were less likely to under‐report difficulties. For grocery shopping, those of non‐white race had increased risk for inaccurate reporting.
Conclusion: Factors that impact self‐awareness of deficits may vary based on the functional domain and factors beyond cognitive function, such as mood and social factors, and should be included when examining awareness of functional difficulties. These results support the use of a domain level approach to examining awareness of functional difficulties in PLWH.
Disclosure: Nothing to disclose.
EPO‐085
From vision to language: Neuropsychological profile in a cohort of patients with Posterior Cortical Atrophy
E. Bergamin 1 ; L. Giampietri2; M. Del Chicca1; V. Nicoletti2; S. Cintoli2; G. Spadoni2; F. Baldacci1; G. Siciliano1; G. Tognoni2
1Department of Neuroscience, University of Pisa, Pisa, Italy; 2Department of Medical Specialties, Neurology Unit, AOUP, Pisa, Italy
Background and Aims: The aim of this study was to analyze the neuropsychological profile of a group of patients with Posterior Cortical Atrophy (PCA) due to Alzheimer's disease (AD). Unlike typical AD, memory, insight and judgement are relatively preserved until latter stages but patients commonly report early language difficulties. However, some inconsistencies exist among the cognitive features described.
Methods: Clinical features and neuropsychological profile of 22 subjects (13 females) aged between 49 and 73 years (61.13 ± 7.04) with PCA due to AD have been analyzed. Each patient underwent a battery of neuropsychological tests, brain MRI, brain [18F]FDG‐PET and alternatively amyloid‐PET or research for AD biomarkers on CSF. A voxel‐based analysis of [18F]FDG‐PET compared with normal control subjects has been performed for 14 patients.
Results: All patients showed impairment in visual‐perceptual, visual‐spatial abilities and visuospatial memory. Variable language impairment was detected in 68% of patients. At voxel‐based analysis of [18F]FDG‐PET the evaluation of semantic fluency positively correlated with hypometabolism in the left angular gyrus (p < 0.001) and Progressive Matrices Test positively correlated with hypometabolism in inferior and superior left parietal gyrus (p < 0.001).
Conclusion: A considerable variability in the language profile was found: specifically, in some patients an impairment of semantic verbal fluency was observed, while in others a logopenic phenotype was detected, in agreement with the literature. The positive correlations found for semantic fluency and Progressive Matrices Test are consistent with the existing literature. Further studies are needed to characterize the progressive evolution of the neuropsychological profile of PCA.
Disclosure: The authors have nothing to disclose.
EPO‐086
Sex differences in neuropsychological profile in behavioural frontotemporal dementia
F. Menegon 1; F. De Marchi1; A. Baj1; M. Sacchetti2; G. Decaroli3; P. Serra4; B. Sarasso4; C. Comi3; G. Tondo3
1Department of Translational Medicine, University of Piemonte Orientale, Neurology Unit, Azienda Ospedaliero‐Universitaria Maggiore della Carità, Novara, Italy; 2Department of Clinical Psychology, Azienda Ospedaliero‐Universitaria Maggiore della Carità, Novara, Italy; 3Department of Translational Medicine, University of Piemonte Orientale, Neurology Unit, S. Andrea Hospital, Vercelli, Italy; 4Neurology Unit, S. Andrea Hospital, Vercelli, Italy
Background and Aims: Behavioral variant (bvFTD) is the most common form of frontotemporal dementia (FTD), presenting with executive deficits and behavioural changes. Sex differences in prevalence, clinical characteristics, and biomarkers, have been described in several neurodegenerative diseases, including FTD. A previous study reported worse executive and language performances in FTD females than males, but these findings are still sparse and need further characterization.
Methods: We included 20 patients (12 females, 8 males, age‐matched) diagnosed with bvFTD at the Memory Clinics of Novara and Vercelli, Piedmont, Italy. All patients underwent a neurological and neuropsychological evaluation at baseline, to characterize the clinical presentation. Patients also underwent a brain MRI and FDG‐PET scan, and a lumbar puncture to support clinical diagnosis. In familial cases, mutations in genes frequently associated with FTD were investigated.
Results: In our cohort, sex did not influence global cognition, evaluated with the Mini Mental State Examination and the Montreal Cognitive Assessment (MOCA). When considering specific cognitive domains, we observed better performance in females compared to males in working memory (i.e., corrected Reverse Digit Span, p = 0.0198), and language (i.e., MOCA denomination subscore, p = 0.03).
Conclusion: From our preliminary data, sex might have a role in determining the type of neuropsychological impairment in bvFTD, with females performing better than males in language and working memory tests. These results confirm that sex may play a role in influencing clinical phenotype in bvFTD, supporting the hypothesis of sex as a pivotal variable for biological and clinical differences in neurodegenerative diseases.
Disclosure: Nothing to disclose.
EPO‐087
QEEG connectivity markers to predict post‐stroke cognitive impairment: A pilot study
H. Dragoș 1; L. Livint Popa1; D. Muresanu2
1Department of Neurosciences, "Iuliu Hatieganu" University of Medicine and Pharmacy, Cluj‐Napoca, Romania; 2RoNeuro Institute for Neurological Research and Diagnostic, Cluj‐Napoca, Cluj, Romania
Background and Aims: Post‐stroke cognitive impairment (PSCI) occurs in about 20% of acute ischemic stroke (AIS) patients within the first months and is associated with poor long‐term prognosis. AIS lesion seems to cause a change in the low‐frequency resting state networks, resulting in increased local connectivity, associated with a global disconnection and a disruption of subcortical‐cortical or cortico‐cortical interactions. This study aimed to develop a predictive model incorporating quantitative EEG connectivity markers to accurately predict PSCI six months after AIS.
Methods: Data were collected from 30 patients with symptomatic supratentorial AIS confirmed by brain MRI without a history of cognitive impairment or dementia. Resting‐state EEG was recorded within the first seven days after AIS onset. Relative power for delta, theta, alpha, and beta bands, delta/alpha ratio, coherence, and phase‐locking value were computed. Neuropsychological assessments consisting of the Montreal Cognitive Assessment test, Digit Symbol, Digit Backward, Stroop Color‐Word Test, and Rey Auditory Verbal Learning test were performed one and six months after AIS.
Results: Delta/alpha ratio and relative theta frequency power were independent predictors for PSCI, suggesting the association between post‐stroke alpha slowing and PSCI, which may be mediated by attentional dysfunction.
Conclusion: QEEG markers seem to be a useful tool to inform early prognostication of PSCI, particularly when cognitive function cannot be adequately assessed.
Disclosure: Nothing to disclose.
EPO‐088
Indicators of cognitive status and quality of life in patients with dystrophic myotonia (DM)
E. Malhina1; Y. Rushkevich 1; S. Likhachev1; M. Dymkovskaya1; A. Gusina2; O. Haliyeyskaya1
1Republican Scientific and Practical Center of Neurology and Neurosurgery, Minsk, Belarus; 2Republican Scientific and Practical Center "Mother and Child", Minsk, Belarus
Background and Aims: Dystrophic myotonia (DM) is a rare multisystem autosomal dominant disease. This is the most common genetic form of muscular dystrophy in adults. Clinical manifestations are varied. Intellectual impairments are observed in all forms of DM. Purpose. Study of the characteristics of cognitive status and quality of life (QoL) in patients with DM.
Methods: 21 patients with a genetically confirmed diagnosis of DM: 3 male and 18 female, ME 45.0[39.0;52.0] years (14 – type DM1, 7 – type DM2). 33 healthy controls (HC): 11 male, 31 female. ME 45.0[38.0;53.0] years.
Results: According to the MoCA, a decrease in scores was found in patients with DM (Me 27.0[25.0;29.0]) compared to the HC (Me 30.0[28.5;30.0]), (U, p = 0.007). When studying the MoCA subtests, patients with DM revealed a decrease in “attention” indicators (U, p = 0.04); “delayed reproduction” (U, p = 0.054). The SF‐36 assessment showed that in patients with DM there is a dominant decrease in the general indicator of the physical component of health (Me 34.0[29.1; 38.5]) compared to the HC (Me 30.0[45.1; 56.1]), (U, p = 0.013). A defect was identified in the subscales “physical functioning” (U, p = 0.0025), “general health” (U, p = 0.048) and “vital activity” (U, p = 0.046).
Conclusion: Patients with DM have cognitive impairment with a predominance in the “attention” and “delayed recall” subtests. A decrease in QoL indicators was revealed in terms of physical functioning”, “general health” and “life activity”. The data obtained reflect the importance of cognitive testing and the study of QoL in patients with DM for the correction of identified disorders.
Disclosure: The authors have nothing to disclose.
EPO‐089
Cognitive decline in patients with diabetes mellitus type 2: The validity of PS‐test
Y. Laykova; E. Gorobets; R. Esin; R. Gamirova
Kazan Federal University
Background and Aims: The objective of the study was to determine the validity of the tool for the early detection of cognitive impairment in patients with type 2 diabetes mellitus (DM).
Methods: The study group (SG) involved 102 patients (67 women, 35 men) with diabetes mellitus type 2, average age 67.5 ± 8.1. The comparison group (CG) included 89 respondents aged 64.3 ± 9.5 years (51 women, 38 men). Both groups were assessed by Montreal Cognitive Assessment (MoCA) test and by the specific tool for cognitive assessment in DM (PS‐test) worked out by the authors. Statistic methods: nonparametric statistical estimation methods suitable for samples that do not follow a normal distribution; the Mann‐Whitney test; Spearman test.
Results: The MoCA test results revealed statistically significant difference (SSD) between SG and CG. The average MoCA test score in SG was 21.07 ± 0.36, in CG – 28.75 ± 0.15 (p < 0.001). SSD was revealed also as a result of PS‐test performing. The average paremiological test score in SG was 14.46 ± 0.38, in CG – 19.84 ± 0.04. According to the Chaddock scale, the obtained correlation coefficient r = 0.8858 corresponds to a high degree. The level of significance of the correlation is confirmed by the p value < 0.0001. Thus, the developed test correlates well with the MoCA test chosen as an external reference criterion, which proves the validity of this tool.
Conclusion: PS‐test can be used in clinical practice for early reveal of cognitive decline in patients with DM type 2.
Disclosure: The reported study was funded by Russian Foundation for Basic Research (RFBR) according to the research project no. 20‐312‐90044.
EPO‐090
Deciphering the decline in dementia diagnoses: A 2015–2022 analysis in Sweden
B. Winblad
Division of Neurogeriatrics, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Stockholm, Sweden
Background and Aims: This study investigates age‐standardized rates of dementia diagnoses in Sweden among individuals aged 65 and older from 2015 to 2022, focusing on three primary diagnoses—F00 (Alzheimer's disease), F01 (Vascular dementia), and F03 (Unspecified dementia). The primary objective is to analyze trends, emphasizing the significant decrease post‐2019.
Methods: Data sourced from national healthcare records includes age‐standardized rates measured as dementia diagnoses per 100,000 inhabitants for individuals aged 65 and older. Gender‐specific trends for F00, F01, and F03 are analyzed using descriptive statistics and Poisson regression.
Results: For F00 dementia diagnoses, both males and females exhibit a consistent decline from 2015 to 2019, followed by a substantial reduction post‐2019. Males experience a decline from 7.4 to 6.6, while females have a notable drop from 7.3 to 3.9. Similarly, F01 vascular dementia diagnoses demonstrate a substantial decrease in both genders post‐2019. Males witness a decline from 110.6 to 78.3, while females see a drop from 91.1 to 63.9. Additionally, F03 unspecified dementia diagnoses portray a consistent decline from 2015 to 2019, with a further reduction post‐2019. Males decrease from 161.1 to 135.3, while females drop from 138.0 to 115.6.
Conclusion: Findings reveal a substantial post‐2019 decrease in dementia diagnoses, possibly impacting healthcare planning and resource allocation. Adaptability in healthcare systems is crucial for addressing the evolving needs of the aging population due to COVID‐19 infection. One conclusion could be that demented persons did not get satisfactory assessment and care during the COVID period. Further research is needed to explore contributing factors.
Disclosure: The authors declare no conflicts of interest or financial relationships that could bias the study's results or interpretation.
Neurogenetics 1
EPO‐091
Autosomal dominant SPG18: A large Italian family
N. Cuomo 1; A. Trinchillo1; V. Valente2; M. Esposito3; M. Migliaccio4; A. Iovino1; P. Michele2; C. Caccavale1; C. Nocerino1; E. Salvatore5; G. Pierantoni2; V. Menchise6; S. Paladino2; C. Criscuolo5
1Department of Neurosciences, Reproductive Sciences and Odontostomatology, University Federico II of Naples, Naples, Italy; 2Department of Molecular Medicine and Medical Biotechnology, University of Naples Federico II, Naples, Italy; 3Clinical Neurophysiology Unit, Cardarelli Hospital, Naples, Italy; 4IRCCS SDN SYNLAB, Naples, Italy; 5CDCD Neurology, “Federico II” University Hospital; 6Institute of Biostructure and Bioimaging, National Research Council (CNR) and Molecular Biotechnology Center, Turin, Italy
Background and Aims: Hereditary Spastic Paraplegias (HSP) are classified as “pure”, when spastic paraplegia is the only symptom or “complex” when other clinical features are present. SPG18 is due to ERLIN2 AD or AR gene mutations.
Methods: We describe clinical and molecular findings of a large Italian AD SPG18 family. Whole exome sequencing. Sanger sequencing was performed to verify the genetic variation in the proband and family members. Velocity gradient assay on proband's fibroblasts was performed to investigate propensity of the mutated ERLIN2 to form oligomers.
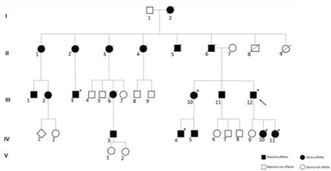
SPG18 pedigree
Results: Five affected family members showed progressive spastic paraplegia. Neuropsychological evaluation pointed out a slight mental retardation in two patients. One patient reported generalized epilepsy. The proband's father died at 58 years old with a diagnosis of amyotrophic lateral sclerosis (ALS). Some of his siblings also died around 60 years old with an anamnestic history ascribable to ALS. Genetic analysis revealed the heterozygous missense mutation, c.502G>A (p.V168M), in ERLIN2 gene, which cosegregated with the disease in the affected patients and was not present in healthy subjects. Velocity gradient assay indicated no differences in oligomerization between mutated and wild‐type protein.

velocity gradient essay
Conclusion: We report a large Italian SPG18 kindred supporting AD transmission pattern with a broad phenotypic variability. Our data strength p.V168M more frequent association to ALS while biochemical assays unravelled that V168M does not affect the ability of erlin‐2 to oligomerize, excluding a dominant negative effect.
Disclosure: Nothing to disclose.
EPO‐092
Findings from the ILLUMINATE prospective Natural History Study (NHS) in individuals with ALSP
D. Lynch 1; J. Gelfand2; C. Wade3; N. Wolf4; W. Koehler5; C. Bergner5; L. Schols6; S. Hayer6; E. Finger7; J. Orthmann‐Murphy8; B. Matys9; D. McLaren9; A. Meier9; R. Rajagovindan9; Z. Wszolek10
1Department of Molecular Neuroscience, National Hospital for Neurology & Neurosurgery, Queen Square, and UCL Institute of Neurology, London, UK; 2Department of Neurology, University of California San Francisco, San Francisco, CA, USA; 3Department of Neurosurgery, University College London, London, UK; 4Department of Child Neurology, Amsterdam Neuroscience, Amsterdam University Medical Centers, Amsterdam, The Netherlands; 5Department of Neurology, University of Leipzig Medical Center, Leipzig, Germany; 6Hertie‐Institute for Clinical Brain Research & Department of Neurology, Tübingen University Hospital, Tübingen, Germany; 7Department of Clinical Neurological Sciences, Western University, London, Ontario, Canada; 8Department of Neurology, Hospital of the University of Pennsylvania, Philadelphia, PA, USA; 9Clinical, Vigil Neuroscience, Inc., Watertown, MA, USA, 10Department of Neurology, Mayo Clinic, Jacksonville, FL, USA
Background and Aims: Adult‐onset leukoencephalopathy with axonal spheroids and pigmented glia (ALSP) is a rare, autosomal‐dominant, neurodegenerative microgliopathy caused by a CSF1R gene mutation characterised by brain white matter demyelination and atrophy, swollen axons, pigmented glial cells, and clinical symptoms of cognitive, neuropsychiatric, and motor dysfunction. ALSP symptoms typically develop around 40–50 years of age, leading to death within ≈6–8 years; no approved therapies exist.
Methods: ILLUMINATE, the first NHS in ALSP (NCT05020743), is a prospective, multicentre study of individuals with definitive (satisfying full radiological, genetic, clinical criteria) or prodromal (satisfying genetic, radiologic criteria only) ALSP. Participants (N ≈ 50) are followed for 24 months, with clinical assessments and MRI collected at screening and every 6 months and blood and cerebrospinal fluid (CSF) disease biomarkers collected at specific visits.
Results: As of Sept‐2023, 24/42 enrolled participants were symptomatic and 18/42 prodromal. Ventricular volumes were higher at baseline and expanded over time, and baseline grey matter volumes were lower and declined over time, in symptomatic vs prodromal patients (Fig‐1). Baseline soluble CSF1R in CSF was substantially lower in all participants (reflecting reduced microglial activity) than healthy individuals, whereas neurofilament light chain (NfL) in CSF and serum was elevated in symptomatic (indicating neuroaxonal injury) vs prodromal and healthy individuals (Fig‐2). Cognitive impairment was greater in symptomatic than prodromal patients and correlated with MRI volume changes (Fig‐3).
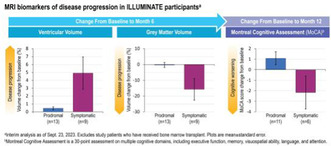
FIGURE 1
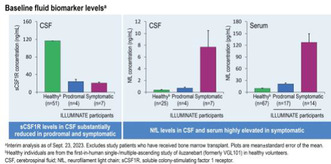
FIGURE 2
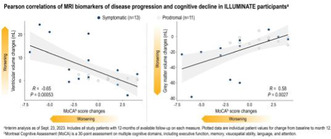
FIGURE 3
Conclusion: These findings demonstrate the sensitivity of MRI measures and NfL to ALSP pathophysiology, with potential to inform optimal clinical endpoints and interventional study design in ALSP and improve understanding of disease progression.
Disclosure: JMG receives research support to his institution for contracted research. DSL, CW, NW, WK, CB, LS, SH, EF, JO‐M, and ZKW, or their institutions, have received compensation from research and funding organisations and/or pharmaceutical companies for speaking, consulting, and contracted research. BM, DM, AM, and RR are current employees of and hold stock and/or stock options in Vigil Neuroscience, Inc. Study developed, managed, and funded by Vigil Neuroscience, Inc. Medical writing and editorial support were provided by Morgan Hill, PhD, CMPP, and Melissa Austin of Apollo Medical Communications (Guilford, CT), part of Helios Global Group, with funding from Vigil Neuroscience, Inc.
EPO‐093
A recurrent homozygous deletion in MED22 leads to a progressive neurodevelopmental disorder and neurodegeneration
E. Cali
UCL Institute of Neurology, University College London
Background and Aims: Proper neurodevelopment relies on gene expression programs influenced by signalling molecules, transcription factors (TFs), and epigenetic processes. In this study, we investigate an ultra‐rare homozygous single amino acid deletion (p.Glu133del) in MED22, a component of Mediator, a key regulator of transcription, gene expression and posttranslational epigenetic modifications. Disruption of Mediator has been implicated in various neurodevelopmental and neurodegenerative disorders.
Methods: We analysed the variant's impact into the Mediator structure and function through cellular studies and computational simulations. We investigated MED22 protein function generating knock‐out zebrafish model and knock‐in Drosophila model. We performed scRNA‐seq on zebrafish mutants.
Results: We identified eight affected individuals from six unrelated families with a severe progressive neurodevelopmental disorder, characterized by global developmental delay, microcephaly, dystonia, seizures, and microcephaly. In vivo models of Drosophila melanogaster and zebrafish demonstrate significant developmental disruption, mirroring major aspects of the human disorder. scRNA‐sequencing data obtained from zebrafish mutants implicate MED22 in dopaminergic network dysfunction.
Conclusion: We establish the first association of MED22 with a human disorder, through integration of clinical, genetic and neuroradiological data. We provide insights in the molecular dynamics of Mediator dysfunction and in the neuronal pathways that might be affected by MED22 dysfunction.
Disclosure: Nothing to disclose.
EPO‐094
MicroRNA biomarkers of large vessel occlusion strokes in cross‐sectional and longitudinal analysis
E. Sidorov 1; M. Rout2; D. Sanghera2
1Department of Neurology/The University of Oklahoa Health Sciences Center, Oklahoma City, Oklahoma; 2Department of Pediatrics/The University of Oklahoa Health Sciences Center, Oklahoma City, Oklahoma
Background and Aims: Exosomal microRNAs play an important role in developing disease biomarkers. Many microRNAs were associated with stroke in case‐control studies on heterogeneous populations, but none had solid evidence to become a biomarker. In this pilot investigation, we analyzed the microRNA of stroke patients with large vessel occlusion (LVO) using a combination of cross‐sectional and longitudinal study designs.
Methods: We performed a cross‐sectional analysis of 2,632 serum exosomal microRNAs on 55 stroke patients and 53 non‐stroke controls; and a longitudinal analysis in 10 stroke patients, collecting blood samples at <24 h, 3, 5, and 30 days after stroke. MicroRNAs were isolated using the mir VANA RNA isolation kit (Ambion, USA). We ran miRNA expression assays using TaqMan probes (Applied Biosciences, USA) on 384‐well microplates using QuantStudio 6 available in our lab. Each assay was run in duplicates using endogenous (U6) and blank controls.
Results: We identified 51 microRNAs associated with ischemic stroke, however, only microRNA 9‐3p and microRNA 233‐3p survived stringent Bonferroni correction (p < 0.01). MicroRNA 9‐3p had 9‐fold higher levels in LVO stroke patients compared to controls (p < 0.01), and a strong correlation with the infarction volume (r = 0.393; p = 2.98 × 10−3). Both microRNAs significantly increased during longitudinal analysis from presentation to days 3–5 and then slowly declined at 90 days after stroke (p < 0.01).

Significant microRNAs
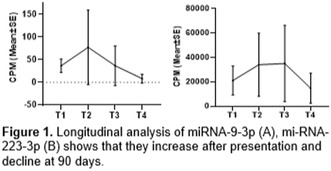
Longitudinal changes in microRNAS
Conclusion: Our study showed dysregulation of exosomal microRNAs 9‐3p and 233‐3p after ischemic stroke in cross‐sectional and longitudinal analysis. If replicated in large‐scale trials both microRNAs may be come ischemic stroke biomarkers
Disclosure: Nothing to disclose.
EPO‐095
Neurological symptoms in adults with Gaucher disease: A systematic review
G. Imbalzano; C. Ledda; A. Covolo; A. Romagnolo; L. Lopiano; C. Artusi
Department of Neuroscience "Rita Levi Montalcini", University of Turin
Background and Aims: Gaucher disease (GD) is traditionally classified into three types based on the presence or absence of neurological signs and symptoms, but their presentation can be highly variable in adulthood and they have not been adequately addressed in the literature so far. We performed a systematic literature review to analyze the entire spectrum of neurological manifestations in adult patients previously classified as GD type I, II or III, evaluating the role of variants in different neurological manifestations.
Methods: We searched databases for studies reporting clinical data of adult GD patients (age ≥18). Data extraction included GD types, GBA1 variants, age at disease onset and diagnosis, duration of GD and age at onset, and type of neurological symptoms reported.
Results: Among 4190 adult GD patients from 85 studies, 555 exhibited at least one neurological symptom. The median age at evaluation was 46.8 years (IQR 26.5), age at neurological symptoms onset was 44 years (IQR 35.1), and age at GD clinical onset was 23 years (IQR 23.4). Parkinsonism, including Parkinson's disease and Lewy Body dementia, was the most reported neurological manifestation. Other symptoms and signs encompassed oculomotor abnormalities, peripheral neuropathy, seizures, myoclonus, and cerebellar, cognitive and psychiatric symptoms. The genotype N370S/N370S mostly presented with Parkinsonism and the L444P variant with severe and earlier neurological symptoms.
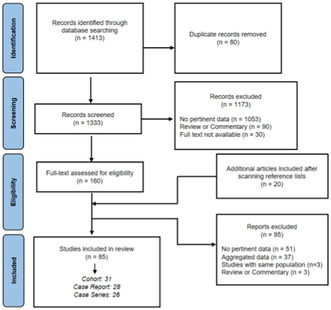
The PRISMA flow diagram of the systematic review
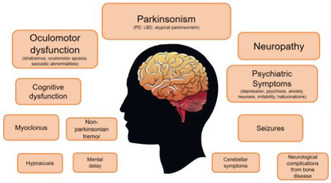
Graphic summary of the principal neurological symptoms evaluated in adult patients with Gaucher Disease. The font size decreases based on the observed prevalence.
Conclusion: The findings of this systematic review highlight: (1) the relevance of a comprehensive neurological assessment in GD patients, and (2) the importance of considering possible undiagnosed GD in adult patients with mild systemic symptoms presenting unexplained neurological symptoms.
Disclosure: Nothing to disclose.
EPO‐096
Description of a cohort of Primary Familial Calcification patients from a single centre in Italy: A systematic approach
G. Bonato 1; C. Bertolin2; F. Pistonesi3; R. Biundo3; P. Santurelli1; B. Savini1; L. Bresciani1; S. Andretta1; L. Salviati2; A. Antonini1; M. Carecchio1
1Parkinson and Movement Disorders Unit, Centre for Rare Neurological Diseases (ERN‐RND), Department of Neuroscience, University of Padova, Padova, Italy; 2Clinical Genetics Unit, Department of Women's and Children's Health, University of Padova, Padova, Italy; 3Department of General Psychology, University of Padova, Padova, Italy
Background and Aims: PFBC is a rare neurodegenerative disorder characterized by calcium deposition in the brain. Clinical manifestations include movement disorders, cognitive or psychiatric features; 50% of cases recognize a genetic cause, with an autosomal dominant (SLC20A2, XPR1, PDGFB, PDGFRB) or recessive inheritance (MYORG, JAM2, CMPK2). Almost 500 cases have been described from different centres with different clinical workup. We systematically describe a cohort from a single centre in Italy (Padova).
Methods: Clinical‐neuropsychological examination, NGS genetic panel, blood test, CT scan
Results: We examined 78 PFBC subjects, 33 males and 45 females; 46% had a positive family history; secondary causes of calcium deposition were excluded. 21% were asymptomatic; mean age at onset was 55 years (min 23, max 90). The most frequent symptoms were movement disorders (Fig. 1): parkinsonism (58%), followed by tremor (56%). Dystonia was documented in 27% (with 2 cases of paroxysmal dystonia); cerebellar signs (21%) and chorea (13%) were less frequent; pyramidal signs were also present in 45% of cases. Psychiatric features were associated in 51%, and cognitive deficits in 38% (22 MCI and 4 dementias, mainly affecting executive domains). Pathogenic mutations were found in 55% of subjects (Fig. 2), mostly in SLC20A2 (45%) and MYORG (21%). Dentate nuclei were frequently involved besides basal ganglia (Fig. 3). DAT‐Scan was positive in 21/32 (65.6%) of patients with parkinsonism.
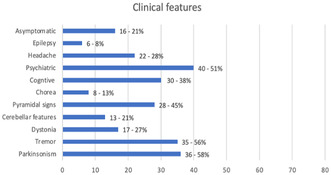
FIGURE 1 Clinical features of the cohort
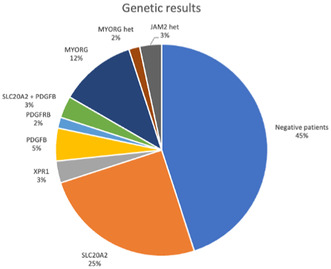
FIGURE 2 Genetic testing results in the cohort
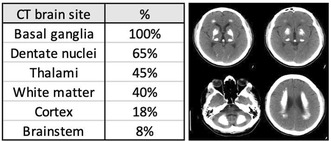
FIGURE 3 Radiologic features of the cohort and a CT example of a MYORG patient
Conclusion: Our work suggests a complete clinical, genetic and radiologic assessment to evaluate PFBC patients as a tool to obtain complete data to better understand this complex disease.
Disclosure: Nothing to disclose.
EPO‐097
Genetic study of SCA27B, CANVAS and other repeat expansion disorders in Greek patients with late‐onset cerebellar ataxia
C. Kartanou1; Z. Kontogeorgiou1; A. Mitrousias1; C. Koniari1; D. Pellerin2; M. Dicaire2; P. Iruzubieta4; M. Danzi5; K. Athanassopoulos1; M. Stamelou6; M. Rentzos7; E. Anagnostou7; S. Zuchner5; B. Brais2; H. Houlden3; M. Panas1; L. Stefanis7; G. Karadima1; G. Koutsis 1
1Neurogenetics Unit, 1st Department of Neurology, National and Kapodistrian University of Athens, Eginitio Hospital, Athens, Greece; 2Department of Neurology and Neurosurgery, Montreal Neurological Hospital and Institute, McGill University, Montreal, Québec, Canada; 3Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology London and The National Hospital for Neurology and Neurosurgery, University College London, London, UK; 4Department of Neurology, Donostia University Hospital, Biogipuzkoa Health Research Institute, Donostia‐San Sebastián, Spain; 5Dr. John T. Macdonald Foundation Department of Human Genetics and John P. Hussman Institute for Human Genomics, University of Miami Miller School of Medicine, Miami, Florida, USA; 6Parkinson's disease and Movement Disorders Department, HYGEIA Hospital, Athens, Greece, 71st Department of Neurology, National and Kapodistrian University of Athens, Eginitio Hospital, Athens, Greece
Background and Aims: Late‐onset cerebellar ataxia (LOCA) encompasses heterogeneous neurodegenerative disorders with symptom onset after 30 years of age. A genetic diagnosis is established in fewer than 30% of LOCA patients. Intronic tandem repeat expansions (TREs) in RFC1 and FGF14 have recently emerged as common causes of LOCA. This study screened Greek LOCA patients for the commonest causative TREs.
Methods: Over a 28‐year period, 206 consecutive LOCA patients were referred for genetic testing. Based on clinical data and inheritance pattern, patients were screened for FRDA, SCA1,2,3,6,7 and FXTAS, followed by testing for CANVAS and SCA27B. PCR, RP‐PCR, agarose gel electrophoresis and fragment analysis were performed, as appropriate, to detect the pathogenic TREs.
Results: A genetic diagnosis was reached in 60 of 206 cases (29.1%). Mean age was 60.1 ± 11.2 (35–87) years and mean age at onset 52.5 ± 11.4 (30–80) years. SCA27B accounted for 9.7% of LOCA cases (n = 20), CANVAS for 6.8% (n = 14) and FRDA for 4.4% (n = 9). The overall frequency of SCA1 (n = 5), SCA2 (n = 6) and SCA7 (n = 3) was estimated at 6.8%. No cases of SCA3 and SCA6 were identified. FXTAS (n = 3) contributed another 1.5% of cases.
Conclusion: Our study provides comprehensive data on the genetic basis of LOCA in the Greek population. SCA27B, followed by CANVAS, represent the commonest known genetic causes of LOCA. FRDA is also a relatively common cause of LOCA. SCA1,2,7 and FXTAS are rare, whereas SCA3 and SCA6 are virtually absent. We recommend prioritizing testing for FGF14 and RFC1 expansions in the diagnostic algorithm of LOCA.
Disclosure: Nothing to disclose.
EPO‐098
Mutational screening of greek patients with Charcot‐Marie‐Tooth disease using whole exome sequencing
Z. Kontogeorgiou1; C. Tzebetzis1; C. Kartanou1; C. Koniari1; M. Rentzos2; P. Kokotis3; E. Anagnostou3; E. Chroni4; V. Zouvelou2; M. Panas1; G. Karadima1; G. Koutsis 1
1Neurogenetics Unit, 1st Department of Neurology, Eginition Hospital, School of Medicine, National and Kapodistrian University of Athens, Athens, Greece; 21st Department of Neurology, Eginition Hospital, School of Medicine, National and Kapodistrian University of Athens, Athens, Greece; 3Clinical Neurophysiology Unit, 1st Department of Neurology, Eginition Hospital, School of Medicine, National and Kapodistrian University of Athens, Athens, Greece; 4Department of Neurology, School of Medicine, University of Patras, Patras, Greece
Background and Aims: Charcot‐Marie‐Tooth disease (CMT) is the most common cause of hereditary neuropathy, exhibiting extensive genetic heterogeneity, which can be addressed using whole exome sequencing (WES). This study screened previously undiagnosed Greek patients with CMT, using WES.
Methods: Over a 6‐year period, 441 consecutive patients were referred for CMT molecular diagnosis. Following targeted testing for CMT1A and in selected cases for CMTX, 173 index‐cases remained undiagnosed, of which 65 with a strong suspicion of hereditary neuropathy. To date, 32 of these, including 13 cases with demyelinating and 19 cases with axonal neuropathy, have been screened by WES using Ion Torrent technology and confirmed by Sanger sequencing.
Results: Causative variants were detected in 19 of 32 patients (59.4%) across 14 genes known to cause CMT, of which 3 were novel (in MPZ, SH3TC2 and KIF1A). In demyelinating forms the diagnostic yield was 76.9 % and in axonal forms 47.4%. Most causative variants were found in SH3TC2 (5 cases) and GJB1 (2 cases), all in demyelinating CMT. In patients with demyelinating CMT, single causative variants were found in EGR2, MPZ and NDGR1. In patients with axonal CMT, single causative variants were identified in HINT1, NEFH, BSCL2, NEFL, MORC2, GDAP1, KIF1A, SORD1 and MPV17.
Conclusion: The overall diagnostic yield of WES was comparable to other CMT populations. Our results contribute to the further mapping of gene variants associated with hereditary neuropathy and highlight the importance of WES in the diagnostic algorithm of disorders with high genetic heterogeneity, in the context of precision medicine.
Disclosure: Nothing to disclose.
EPO‐099
Phenotypical characterization of a cohort of SCA 27B patients
G. Falcone 1; F. Santorelli2; O. Musumeci1
1Neurology and Neuromuscular Disorders Unit, Department of Clinical and Experimental Medicine, University of Messina, Italy; 2Molecular Medicine for Neurodegenerative and Neuromuscular Diseases Unit, IRCCS Fondazione Stella Maris, Pisa, Italy
Background and Aims: FGF14 intronic heterozygous GAA expansions have recently been identified to be a frequent cause of late onset cerebellar ataxia (LOCA) (SCA27B). We evaluated the frequency and phenotype of SCA27B in a cohort of patients with unsolved hereditary cerebellar ataxia (HCA).
Methods: We recruited 25 patients affected with HCA with no age limit who had negative results on testing for repeat expansions and ataxia gene panels and screened them for the FGF14‐GAA repeat expansion.
Results: 4 of the 25 patients (16%) carried an FGF14 (GAA) ≥250 expansion. Median age at onset was 51.75 years (range 16–79). Episodic symptoms at onset were present in two patients with episodes of vertigo, sweating, gait imbalance in one case and ataxia, dysarthria, rigidity, diplopia and dysphagia in the other. On examination abnormal smooth pursuit movements, downbeat nystagmus, dysarthria and gait ataxia were present in all patients; appendicular ataxia was mildly present only in one patient. Other signs were hyporeflexia at lower limbs (¾), tremor of chin and hands (2/4), postural instability (¼). Other symptoms reported were diplopia (¼), cramps (2/4), urgency (¼), dysphagia (3/4), depression (2/4), hearing loss (2/4), chronic cough (¼). Alterations in BAEPs (¼), VEPs (2/4) and SEPs (¾) were present. Brain MRI revealed cerebellar atrophy (4/4), frontoparietal atrophy (2/4), superior cerebellar peduncle hyperintensities (¼).
Conclusion: Our results show the highly heterogeneity of SCA27B and support FGF14‐GAA repeat expansion screening in patients with LOCA and MSA look‐alikes. However, we suggest screening younger cohorts as well.
Disclosure: Nothing to disclose.
EPO‐100
Parkinsonism in primary mitochondrial disorders: Clinical characteristics and follow up
I. Arena 1; G. Falcone1; M. Porcino1; C. Terranova1; C. Rodolico1; O. Musumeci1
1Department of Clinical and Experimental Medicine, University of Messina Messina, Italy
Background and Aims: Primary mitochondrial disorders (PMDs) are a wide group of diseases characterized by a dysfunction of the mitochondrial respiratory chain, potentially involving the central and peripheral nervous system. Parkinsonism is described as a clinical feature of patients with PMDs. The objective of this study is to describe the clinical characteristics of parkinsonism in our cohort of patients affected by PMDs.
Methods: We revised the clinical records, including the extrapyramidal features, symptoms associated, the diagnostic investigations performed, genetic results, and response to therapy in all the patients presenting with parkinsonism in our PMDs cohort.
Results: 9/80 patients from our database presented characteristics of parkinsonism. Progressive external ophthalmoplegia (9/9), myopathy (9/9), ataxia (3/9), peripheral neuropathy (3/9), and optic atrophy (3/9) were the most frequent associated symptoms. Genetic analysis showed multiple mtDNA deletions with mutations in POLG1, TWNK and OPA1 nuclear genes. The most reported extrapyramidal symptom at onset was unilateral tremor. The age of onset was heterogeneous, ranging from 40 to 70 years old. Dopamine transporter imaging (DaTscan) showed a reduced or absent mostly asymmetrical striatal dopamine uptake. Overall, our cohort showed a good and sustained response to levodopa during follow up.
Conclusion: Our data confirm the role of mitochondrial nuclear genes in the pathogenesis of mitochondrial parkinsonism and the importance of screening these genes when suspecting a parkinsonism associated with “mitochondrial red flags”. Extrapyramidal features in mitochondrial parkinsonism appear to be similar to those of idiopathic parkinsonism with an overall positive response to current therapies.
Disclosure: Nothing to disclose.
EPO‐101
Mortality in tuberous sclerosis complex after the introduction of everolimus in the UK
N. Loh 1; C. Kidson2; Y. Syed3
1Paediatrics, KK Childrens Hospital, Singapore; 2Medical School, University of Bristol, UK; 3Neuroscience and Mental Health Research Institute, Hadyn Ellis Building, Cardiff, CF24 4HQ, UK
Background and Aims: Limited literature is available regarding causes of death of people with Tuberous Sclerosis Complex (TSC) since the introduction of everolimus therapy in 2016 in United Kingdom. The aim of this audit is to look for any change in the main causes of death of people with TSC
Methods: Patients who attended the Bath supra‐regional TSC specialist clinic and died between 2016 and 2022 inclusive had their medical records reviewed to identify various disease‐related factors and cause of death. Where cause of death was not available, information from the patient's general practitioner (GP) was used or their death certificate was sought from the General Registry Office. The cohort was then split into various subgroups to identify potential risk factors for earlier mortality.
Results: 369 patients attended this clinic from 2016 to 2022. Six deaths were definitely related to TSC, 5 possibly related and 8 unrelated. Primary causes of death included tumours in 7 (37%; one pancreatic neuroendocrine tumour), epilepsy in 3 (16%, including 1 probable SUDEP), aspiration pneumonia in 3 (11%), sepsis in 2 (11%), COVID in 1 (5%), hepatic AML in 1 (5%), SEGA in 1 (5%), and stroke in 1 (5%). Renal failure was a secondary cause in 2 (11%).
Conclusion: Death at the Bath TSC clinic was associated with learning disabilities and possibly larger AML size. Mortality related to SUDEP causes has become less prominent, while cancers appear to be more prevalent in this cohort. Everolimus appears to positively impact renal and LAM risk.
Disclosure: Nothing to disclose.
EPO‐102
Whole exome sequencing‐based testing of adult epilepsy in the Polish population
M. Mroczek 1; D. Szczęśniak2; K. Ziora‐Jakutowicz2; M. Kacprzak2; L. Kotuła3
1Department of Neurology, University Hospital Basel, University of Basel, Basel, Switzerland; 2Medgen Medical Centre, Warsaw, Poland, 3Institute of Psychiatry and Neurology in Warsaw, Genetics Department, Warsaw, Poland
Background and Aims: Genetic testing in pediatric populations demonstrated clinical utility and provided a diagnostic yield of 18–40%, depending on the cohort tested. However, the diagnostic yield and data on the potential classification of adult epilepsies are limited.
Methods: This study aims to investigate the diagnostic yield, analyze genetic diagnoses and apply International League Against Epilepsy (ILAE) classification for pediatric epilepsies to adult patients with epilepsies in Poland. We recruited 151 patients from 42 clinical centers across Poland. The patients had a diagnosis of epilepsy/seizures, were older than 18 years old at the time of the genetic testing and did not have a genetic diagnosis. The median age of the patient was 28 years.
Results: We reached a diagnostic yield, when considering pathogenic/likely pathogenic variants according to ClinVar of 8.6% (n = 13) and of 17% (n = 26) when applying American College of Medical Genetics (ACMG) criteria. According to the indications for genetic testing according to ILAE, most adult patients were tested for epilepsy + (n = 100, 66%), 21 patients were tested for drug‐resistant epilepsy (14%), 17 for encephalopathy (5%), and 6 patients were tested for familial epilepsy (4%).
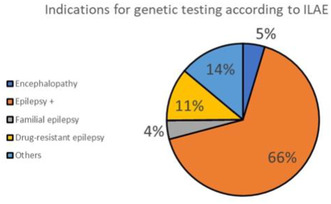
Indications for genetic testing according to ILAE

Summary of the molecular results and additional phenotypic features
Conclusion: There is a wide spectrum of diagnoses associated with epilepsy in adults. We applied the ILAE guidelines for childhood epilepsy to the adult population. Patients may have had a diagnosis related to childhood syndrome, but due to limited diagnostic possibilities it was not possible to diagnose them in childhood.
Disclosure: Nothing to disclose.
EPO‐103
Late‐onset coats plus syndrome: Broadening the differential diagnosis of intracranial calcifications in adults
C. Serrão 1; R. Rodrigues1; C. Guerreiro2; J. Oliveira3; J. Parente Freixo3; R. Barreto1
1Department of Neurosciences and Mental Health, Hospital de Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Lisbon, Portugal; 2Department of Neurological Imaging, Hospital de Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Lisbon, Portugal; 3Center for Predictive and Preventive Genetics, Instituto de Biologia Molecular e Celular, i3S, Universidade do Porto, Porto, Portugal
Background and Aims: Coats plus syndrome (CPS) is a multisystemic disorder, with intracranial calcifications, cysts and leukoencephalopathy as characteristic neurological features. CPS typically presents in infancy or childhood and is caused by bi‐allelic defects in CTC1 gene, involved in telomere maintenance and DNA replication.
Methods: A 46‐year‐old woman presented a 2‐year history of behavioral changes and cognitive decline. Her medical history was unremarkable until 33 years of age when diagnosed with infertility. At 38, she developed retinal vasculopathy and progressive restrictive lung disease under consideration for lung transplantation. Her family history was irrelevant. Clinical examination revealed greying of the hair, atrophic skin with violaceous and brownish macules and low body mass index. Neurological examination highlighted attention and executive function deficits, left homonymous hemianopsia, left central facial palsy and hyperreflexia.
Results: Head MRI revealed a frontal white matter lesion involving U fibers, with peripheral gadolinium enhancement and vasogenic oedema, as well as multifocal calcifications in the subcortical and deep white matter. MR angiography was normal. CSF analysis showed hyperproteinorrachia, mirrored oligoclonal bands and elevated neopterins, excluding infection or neoplasia. To further clarify the radiological findings, exome sequencing was ordered and identified a homozygous variant NM_025099.6:c.2954_2956del in CTC1 gene. The patient died 9 months after presentation due to pneumonia.
Conclusion: Adult‐onset CPS is very rarely reported. We presented a case associated with a homozygous in‐frame deletion (p.(Cys985del)), which presented in adulthood with a milder phenotype. Clinicians should consider CPS in the differential diagnosis of intracranial calcifications and leukoencephalopathy in adults.
Disclosure: Nothing to disclose.
EPO‐104
Optimized testing strategy for molecular diagnosis of GAA‐FGF14 (SCA27B) ataxia: French SCA27B ataxia study group
C. Bonnet1; S. Puisieux 2; V. Roth1; M. Wandzel1; D. Pellerin3; G. Clément2; B. Brais4; M. Renaud5
1Laboratory of Genetics, University Hospital of Nancy, France; 2Department of Neurology, University Hospital of Nancy, France; 3Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology and The National Hospital for Neurology and Neurosurgery, University College London, London, UK; 4Department of Neurology and Neurosurgery, Montreal Neurological Hospital and Institute, McGill University, Montreal, Canada; 5Department of Human Genetics, University Hospital of Nancy, France
Background and Aims: GAA expansions in FGF14 intron 1 are a common cause of autosomal dominant hereditary cerebellar ataxia (GAA‐FGF14 ataxia; spinocerebellar ataxia 27B, SCA27B), particularly in Late Onset Cerebellar Ataxia (LOCA). SCA27B is classically characterized by a slowly progressive cerebellar syndrome with episodic onset in more than 2/3 of cases, over 40 years of age. Until now, molecular confirmation of FGF14 GAA expansions has mainly relied on long‐read sequencing, a technology not yet routinely available in French genetics laboratories.
Methods: We developed and validated a three‐step molecular diagnostic strategy: long‐range fluorescent PCR (fLR‐PCR) to determine allele sizes, bidirectional triplet‐primed PCR (TP‐PCR) to verify the presence and nature of the expansion and LR‐PCR products gel electrophoresis and/or Sanger sequencing depending on the profile observed in TP‐PCR. We compared this strategy to nanopore long‐read sequencing on 22 Canadian SCA27B patients of French origin and then tested it on a national cohort of 560 patients with unresolved LOCA.
Results: We identified 107 patients (19.1%) carrying FGF14 expansions (GAA) ≥250 including 17/560 (3%) with expansions between 250 and 300 GAA (intermediate allele with incomplete penetrance). Further studies are needed to help in the interpretation of these intermediate alleles. We identified non‐pathogenic non‐GAA expansions and GAA‐interruptions.
Conclusion: We confirm that SCA27B is a common cause of LOCA. Detailed phenotyping of patients appears essential particularly for the interpretation of intermediate alleles. This novel strategy reliably detected and sized FGF14 GAA expansions, and compared favorably to long‐read sequencing.
Disclosure: None.
EPO‐105
Unveiling a stroke‐like onset of Creutzfeldt‐Jakob disease: A case report of V210I mutation
T. Giannelli; G. Ruta; D. Totaro; L. Parrulli; D. Paolicelli; G. Logroscino; A. Introna
Department of Translational Biomedicine and Neuroscience (DiBraiN), University of Bari “Aldo Moro”, Bari, Italy
Background and Aims: Genetic prion diseases (PrD) account for 10–15% of prion diseases and are caused by mutations in the prion protein gene (PRNP).
Methods: A 75‐year‐old man suddenly developed nominum aphasia ten days before admission. His medical history included hypertensive heart disease and atrial fibrillation. His brain computed tomography (CT) and angiography‐CT were unremarkable. At neurological evaluation the patient executed simple orders, however, comprehension and production of complex speech were compromised. A first brain magnetic resonance imaging (MRI) excluded ischemic lesions and inflammatory processes. Meanwhile, he progressively and rapidly developed ataxia, cerebellar signs, spontaneous myoclonus and mutism. Analysis of cerebrospinal fluid (CSF) revealed increased levels of total tau (>2000 pg/ml). His electroencephalogram showed pseudo‐periodic triphasic waves over the left frontotemporal regions. PrD was suspected, therefore the patient underwent a new brain MRI. Diffusion‐weighted imaging exhibited diffuse cortical ribbons in the left frontal, insular and parietal cerebral cortex. After discharge, the patient died shortly after due to ab ingestis pneumonia.
Results: CSF RT‐QuIC for prion protein returned positive. Sanger sequencing of the PRNP gene showed the heterozygous V210I genotype (c.628 G>A – p.Val210Ile) and the homozygous Met/Met genotype at codon 129. These findings were suggestive of genetic Creutzfeldt‐Jakob disease (CJD).
Conclusion: An acute onset of symptoms in CJD is rare (2% of all cases) and so far has been associated exclusively with the V203I mutation. The sudden appearance of focal symptoms without corresponding brain lesions requires a thorough investigation to rule out other rare causes including CJD, especially in rapidly progressive clinical scenarios.
Disclosure: Nothing to disclose.
Epilepsy 1
EPO‐106
Heart rate variability in patients with Epilepsy
S. Daoud1; S. Sellami 1; R. Charfi1; A. Bahloul2; N. Bouattour1; N. Farhat1; S. Sakka1; K. Moalla1; L. Abid2; K. Masmoudi3; M. Damak1; C. Mhiri1
1Neurology Department and Research Laboratory LR12SP19, Habib Bourguiba University Hospital, Sfax, Tunisia; 2Department of Cardiology, Hedi Chaker University Hospital, Sfax, Tunisia; 3Department of Physiology and Functional Exploration, Habib Bourguiba University Hospital, Sfax, Tunisia
Background and Aims: Several studies have reported alterations of heart rate variability (HRV) and decreased cardiac rhythm abnormality in patients with epilepsy. The purpose of this study is to investigate epilepsy and its impact on HRV.
Methods: We obtained HRV data from an ambulatory 24‐hour rhythm holter monitorization recordings in 73 patients with epilepsy. We calculated HRV parameters in both time and frequency domains including low frequency (LF) power, high frequency power (HF), LF/HF ratio, square root of the mean of the sum of the squares of differences between adjacent NN intervals (RMSSD), the standard deviation of all NN intervals (SDNN) and the standard deviation of the averages of NN intervals in all 5 min segments of the entire recording (SDANN). The HRV in epileptic patients was compared with 73 age‐ gender matched healthy controls.
Results: HRV analysis showed that epileptic patients presented lower values of HF than controls (p = 0.002), also a lower values of LF (764.64 vs 801.3; p = 0.63) with a significantly higher LF/HF ratio (p < 0.0001). Time domain analyses also showed lower HRV and lower vagal activity in patients with epilepsy, as shown by lower SDNN (132.40 vs 136.24; p = 0.32), lower SDANN (113.8 vs 123.11; p = 0.1) and a significant lower RMSSD (p = 0.004).
Conclusion: In conclusion, patients with epilepsy appear to have an altered autonomic control of the heart. The decrease in HRV parameters might be associated with the decrease in sympathetic tone. Further studies are warranted to explore these changes and their possible relevance for sudden death in epilepsy.
Disclosure: Nothing to disclose.
EPO‐107
Vagus Nerve Stimulation in paediatric drug‐resistant epilepsy: Two decades experience in a Portuguese Tertiary Centre
A. Costa 1; R. Lopes1; F. Sambayeta1; I. Laranjinha1; I. Carrilho2; S. Figueiroa2; T. Temudo2; C. Garrido2; M. Santos2; R. Chorão3; M. Tizziani4; R. Rangel4; J. Chaves1; R. Samões1
1Neurology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 2Neuropediatrics Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 3Neurophysiology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 4Neurosurgery Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal
Background and Aims: Vagus Nerve Stimulation (VNS) is a therapeutic option in drug‐resistant epilepsy. Real‐world data on its application in children and long‐term outcomes are crucial. We aimed to characterize an unicentric paediatric population undergoing VNS to evaluate its effectiveness/safety.
Methods: Clinical records of paediatric patients (<18 yo) implanted between 2000 and 2023 were reviewed. McHugh's classification (I‐seizure frequency reduction 80–100%; II‐50‐79%; III‐ < 50%; IV‐magnet benefit only; V‐no improvement) was applied at: a) first assessment after 1 year and stimulation > = 1.5mA (T1) b) last assessment and stimulation > = 1,5mA (T2).
Results: VNS was implanted in 56 paediatric patients; (51.8% were males. Median age and duration of epilepsy at implantation were 12 (IQR = 6.8) and 9.2 (IQR = 6.4) years. Ten patients had focal/multifocal, 20 generalized, and 26 combined focal/generalized epilepsies. Thirty were epileptic/developmental encephalopathies (16 with known mutations), 19 structural, 3 infectious, 2 immune, and 2 neurocutaneous syndromes. Median follow‐up was 1.1 years (IQR = 0.19) at T1 and 5.3 years (IQR = 4.08) at T2. A reduction in seizure frequency was observed in 70.4% (T1) and 60% (T2) of patients, with 40.7% (T1) and 29.1% (T2) achieving ≥50% response. Among patients with falls, 48.5% had less events (T2). Cognitive‐behavioural improvement was noticed in 50.9% of patients (T2). Mild complications occurred in 32.1%, most commonly dysphonia (61%) and cough (38.9%). VNS generator/battery was replaced in 15 patients, in 3 due to qualitative and/or cognitive‐behavioural improvements. In 15 patients, lack of efficacy prevented its replacement.
Conclusion: Overall, VNS proved to be safe/effective, despite a less pronounced effect at T2. Notably, a significant qualitative and cognitive‐behavioural benefit was observed.
Disclosure: Nothing to disclose.
EPO‐108
Time as a localizing sign: The challenge of identifying the origin of hyperkinetic seizures
İ. İlgezdi Kaya; G. Aliyeva; N. İşkan; A. Elmalı Yazıcı; N. Bebek
Department of Neurology, Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey
Background and Aims: Hyperkinetic seizures (HS), typically associated with the frontal lobe, are characterized by high amplitude, short duration, complex motor movements, although they may also originate from regions other than the frontal lobe. In our study, we aimed to differentiate HSs originating from the frontal and extra frontal lobes.
Methods: We retrospectively examined the data of 29 patients in whom HS was recorded with video‐EEG. We reviewed the localization characteristics of HSs, onset time, duration of hyperkinetic movements, and ictal‐postictal electrophysiological and semiological features. Two groups, early and late‐onset HS, were created based on whether the onset of hyperkinetic semiology occurred in the first 10 seconds or later during the seizure.
Results: Seizure onset originated from the frontal region in 21 patients, and from the temporal and temporo‐occipital region in 6 patients (Table 1). Clustering of hyperkinetic seizures (>3 seizures/day) was detected in 13 patients (44.8%), while > = 1 seizure within 24 hours was observed in 22 patients. HS started in the early period in 21 patients and late period in 8. HSs originating from the frontal region started earlier than those originating from the temporal region (11.7 s, 23 s; p = 0.008). Electrophysiological (12.0 s, 22.3 s; p = 0.013) and clinical (11.9 s, 22. 7 s; p = 0.011) seizure durations were shorter in frontal onset seizures (Table 2).
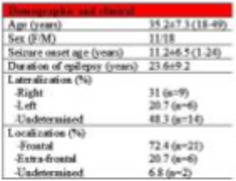
TABLE 1 Demographic and clinical data of the patients
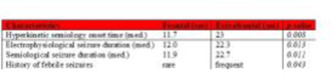
TABLE 2 Characteristics of seizures according to the region of onset
Conclusion: Our study indicates that the onset time and duration of hyperkinetic semiological findings are informative in terms of localization. Hyperkinetic semiology with earlier onset and shorter duration may suggest a frontal origin.
Disclosure: The authors declare no conflicts of interest. This study has been presented in the 39th National Clinical Neurophysiology EEG‐EMG Congress, Turkey.
EPO‐109
The preliminary results of cortical thickness measurements in elderly patients with epilepsy and Alzheimer's dementia
B. Turk 1; A. Oz2; B. Gulec3; D. Tezen1; M. Delil1; O. Kizilkilic2; M. Bozluolcay1; C. Ozkara1; S. Yeni1
1Istanbul University‐Cerrahpasa, Faculty of Medicine, Department of Neurology; 2Istanbul University‐Cerrahpasa, Faculty of Medicine, Department of Radiology; 3Bilecik Training and Research Hospital, Neurology Department
Background and Aims: Observational studies have suggested a bidirectional relationship between Alzheimer's dementia (AD) and epilepsy. However, whether a causal relationship exists and in which direction it operates is still a matter of debate. This study aims to assess the relationship between late‐onset non‐lesional epilepsy and AD by measuring cortical thickness in both patient groups.
Methods: Thirteen patients with epilepsy who experienced onset of seizures aged 50 and above, had a MOCA (Montreal Cognitive Assessment) score greater than 26, and exhibited normal findings in conventional neuroimaging, were included in the study. They were compared with 13 gender‐ and age‐matched patients diagnosed with AD and 13 healthy controls. All subjects were scanned on 3T‐MRI scanner. CAT12 software was employed to analyze T1‐weighted images from each participant. Cortical thickness maps, smoothed with a 15 Gaussian kernel, were generated from the central surface classified according to anatomical cortical brain regions.
Results: No significant difference was detected in any brain region measured between the epilepsy and control groups. A significant decrease was detected in all brain regions in the dementia group compared to both groups (Figure).
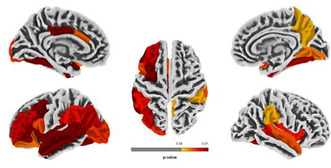
Anatomical brain regions with cortical measurements between AD and Epilepsy
Conclusion: In the study conducted with the expectation of observing cortical changes in terms of the structural relationship between epilepsy and AD, the absence of any alterations may be attributed to the limited number of participants. It is aimed to continue the study by increasing the number of patients.
Disclosure: Nothing to disclose.
EPO‐110
Implementation of urgent eeg on‐call in a tertiary hospital
A. Mas 1; M. Olivera1; A. Muñoz‐Lopetegui2; G. Maya2; P. Marrero1; A. Tercero2; M. Centeno3; C. Gaig2; E. Conde‐Blanco3
1Hospital Clínic de Barcelona; 2Hospital Clínic de Barcelona, IDIBAPS; 3Hospital Clínic de Barcelona. IDIBAPS, EPICARE
Background and Aims: Urgent video‐EEG (uvEEG) is crucial for early diagnosis and treatment of seizure and non‐convulsive status epilepticus (NCSE) but is not always available. We aimed to evaluate its yield after implementation in our center.
Methods: We retrospectively identified patients who underwent an uvEEG at a tertiary hospital from September 2021 to January 2023. We categorized uvEEG findings and evaluated antiseizure medication (ASM) escalation.
Results: A total of 498 uvEEG were collected and 245 performed on‐call (weekdays 5p‐10p and weekends 9a‐10p). Most studies were requested from the intensive care units (ICU) (47.2%) compared to neurology (21.4%) or the emergency room (ER) (17%), and other services (14.5%). UvEEG revealed non‐convulsive seizures (NCS)/NCSE in 10.2% patients, epileptiform patterns (Lateralized and generalized periodic discharges, focal and generalized epileptiform activity) in 15.9%, attenuation/burst‐suppression patterns in 8.98%, slowing/rhythmic patterns in 43.7%, normal activity in 18.8% and other patterns in 2.40%. We observed an association between hospital settings (ICU, ER or neurology) and uvEEG findings (p = 0.0003). The proportion of normal uvEEG in the ER (44.6%) and neurology (39.4%) was similar but significantly different to the ICU (4.3%) and other departments (11.7%) (p < 0.000). Most of the uvEEG were requested between 12 and 24h after clinical onset. Neurology, ICU and ER applications were significantly higher after‐hours in contrast to other departments (p < 0.000). Modifications of ASM were present in 84% (n = 95) of patients.
Conclusion: uvEEG guides initiation and modifications of ASM in complex patients with neurological focal deficits at different hospital settings. uvEEG is mandatory in patients with NCS/NCSE for appropriate care.
Disclosure: No disclosures.
EPO‐111
Perampanel as only add‐on treatment in post‐stroke epilepsy: Real‐world data from multicenter, observational study
A. Pascarella 1; S. Gasparini1; O. Marsico1; L. Manzo2; D. Abelardo1; R. Cutellè1; A. Bulgari1; V. Cianci2; E. Ferlazzo1; U. Aguglia1; PEROC Study Group3
1Department of Medical and Surgical Sciences, Magna Græcia University of Catanzaro, Italy; 2Regional Epilepsy Centre, Great Metropolitan “Bianchi‐Melacrino‐ Morelli Hospital”, Reggio Calabria, Italy; 3PEROC Study Group
Background and Aims: Post‐stroke epilepsy (PSE) is one of the most common causes of acquired epilepsy, with an estimated occurrence of 4–6% in the stroke population. Currently there is limited evidence regarding the clinical profile of antiseizure medications (ASMs) in PSE. This study aims to evaluate the 12‐months effectiveness and tolerability of adjunctive perampanel (PER) as only add‐on drug in patients with PSE in a real‐world setting
Methods: We performed a subgroup analysis of PSE patients included in a previous 12‐month retrospective, longitudinal, multicentre observational study investigating use of PER as only add‐on treatment. Effectiveness outcomes included responders’ rate (≥50% reduction of frequency), seizure‐freedom and retention rate at 3, 6 and 12 months. Safety and tolerability outcomes included incidence of adverse events (AEs) and rate of treatment discontinuation due to AEs.
Results: The sample included 56 people with PSE (median age 49 years; IQR: 18.9–67.1). The mean daily dose of PER at 12 months was 5.3 ± 2 mg. We found a one‐year retention rate of 66.7%. Responders’ rate was 83.9% at the 12‐month visit, with 51.6% of patients being seizure‐free. Poor tolerability represented the main reason for drug withdrawal (11/13, 84.6%). AEs were registered in 25 out of 54 (46.3%) patients. Only 5 serious AEs (without deaths) were noticed. Behavioural problems resulted the most frequent AE, reported by 14 subjects.
Conclusion: Adjunctive PER was efficacious and generally well tolerated in patients with PSE in a real‐world setting and could represent a suitable therapeutic option in this specific category.
Disclosure: All authors report no disclosure.
EPO‐112
Final analysis of perampanel as the only adjunctive anti‐seizure medication from the observational PERPRISE study
B. Steinhoff 1; T. Goldmann2; Y. Winter3
1Kork Epilepsy Center, Kehl‐Kork, Germany; 2Eisai GmbH, Frankfurt am Main, Germany; 3Mainz Comprehensive Epilepsy and Sleep Medicine Center, Department of Neurology, University Medical Center of the Johannes Gutenberg University, Mainz, Germany
Background and Aims: In Germany, prior to perampanel reintroduction in 2017, only limited data of its use as late‐line therapy were available. PERPRISE (PERampanel in patients with PRImary or SEcondarily generalised seizures; NCT04202159) was a 12‐month, prospective, observational, non‐interventional study in a real‐world setting in Germany evaluating the effectiveness and safety of perampanel as an only add‐on anti‐seizure medication (ASM) or a substitute for one ASM during dual therapy.
Methods: Patients (> = 18 years) with focal or idiopathic generalised epilepsy who had > = 1 focal to bilateral tonic‐clonic seizure (FBTCS) or generalised tonic‐clonic seizure (GTCS) < = 3 months prior to inclusion were eligible. The Full Analysis Set included patients who received > = 1 dose of perampanel. The primary endpoint was retention rate at 12 months; secondary endpoints were retention rate at 6 months, seizure‐freedom rate at 12 months and safety.
Results: The Full Analysis Set included 183 patients (add‐on: 86 patients; substitution: 96 patients). At 12 months, retention rates were 66.7% in the overall population and 67.4% and 66.7% in the add‐on and substitution groups, respectively (Figure 1). Seizure‐freedom rate in the overall population was 42.3% for FBTCS+GTCS at 12 months (Figure 2). Treatment‐emergent adverse events (TEAEs) occurred in 44.0% (n = 80/182 [Table 1]) of patients; 6.0% of patients reported serious TEAEs and 16.5% of patients withdrew from the study due to TEAEs.
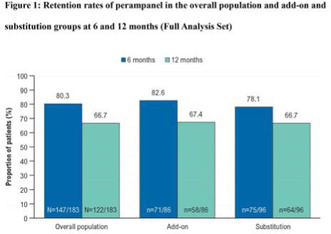
FIGURE 1
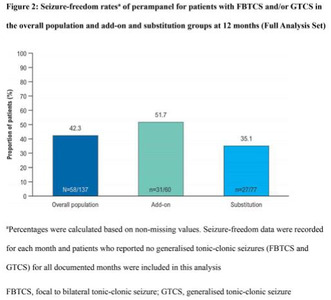
FIGURE 2

Conclusion: This study showed that perampanel, as an only adjunctive therapy, had a favourable retention rate and was well tolerated in patients with FBTCS and/or GTCS during routine clinical care in Germany.
Disclosure: This study was funded by Eisai GmbH. Bernhard J Steinhoff has received speaker honoraria from Angelini, Arvelle Therapeutics, Desitin, Eisai GmbH, GW Pharmaceuticals, Tabuk Pharmaceuticals, Teva and UCB Pharma; and has served as a paid consultant for Angelini, Arvelle Therapeutics, B. Braun Melsungen, Eisai GmbH, GW Pharmaceuticals and UCB Pharma. Tobias Goldmann is an employee of Eisai GmbH. Yaroslav Winter has received honoraria for educational presentations and consultations from Angelini Pharma, Arvelle Therapeutics, Axsome, Bayer AG, BIAL, Bioprojet, Eisai, Idorsia Pharmaceuticals, JAZZ Pharmaceuticals, LivaNova, Novartis and UCB Pharma.
EPO‐113
GATORopathies: An observational study of patients with familial focal epilepsy
C. Santos Martín; C. Amarante Cuadrado; J. Alcalá Torres; M. González Arbizu; R. Saiz Díaz; S. Bellido Cuéllar; J. González de la Aleja Tejera
Neurology, Hospital Universitario 12 de Octubre, Madrid, Spain
Background and Aims: In the last few decades, increasing interest in the genetics underlying familial focal epilepsy syndromes has emerged. Mutations in mTOR pathway regulatory genes, including the GATOR1 complex (DEPDC5, NPRL3, NPRL2), have been linked to malformations of cortical development and epilepsy.
Methods: A unicentric, retrospective observational study of adult patients with epilepsy and GATOR1 variants diagnosed between 2019 and 2023.
Results: We identified six patients (4 males) from three families. Two families had heterozygous pathogenic variants in DEPDC5 (2 patients with c.2760dupC and 2 with c.4098del) and the third family in NPRL3 (c.1374del). 4/6 patients had a known family history of epilepsy. The median age at onset of epilepsy was 10 years (3–22). One patient experienced focal impaired awareness seizures, 1/6 focal to bilateral tonic‐clonic (FBTC), and 4/6 focal and FBTC seizures, mostly nocturnal in all cases. Brain MRI did not reveal any abnormalities. Interictal focal epileptiform abnormalities were detected by electroencephalogram in 2/6. Epilepsy was drug‐resistant in three patients, 2/3 with three anti‐seizure medications, whereas the other three were seizure‐free with one drug. In family C, proband's relative III‐13 presumably died of sudden unexpected death in epilepsy (SUDEP). None of them had cognitive impairments or psychiatric comorbidities.
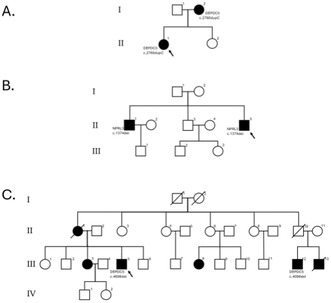
FIGURE 1 Pedigrees of the three families. Black squares/circles indicate male/female members with epilepsy in the family. Individuals with confirmed pathogenic variants in the GATOR complex are specify.
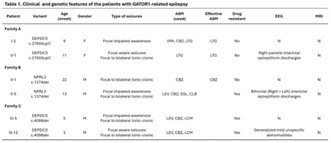
TABLE 1 Clinical and genetic characteristics of patients with GATOR1‐related epilepsy included in the study. Abbreviations: F, female; M, male; N, normal
Conclusion: Pathogenic variants in the GATOR1 complex are associated with a broad spectrum of phenotypes, even in the same family, but typically cause familiar focal epilepsy with incomplete penetrance and nocturnal seizures. Drug‐resistant epilepsy is frequent not only in our series but also in literature. Moreover, a higher risk of SUDEP has been reported.
Disclosure: Nothing to disclose.
EPO‐114
Abstract withdrawn
EPO‐115
The effect of epilepsy education on knowledge level, self‐management, and stigma in individuals with epilepsy
İ. İlgezdi Kaya1; A. Çavuşoğlu2; A. Elmalı 1; N. Bebek1
1Department of Neurology, Clinical Neurophysiology, Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey; 2Department of Neurology, Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey
Background and Aims: This study aims to examine the impact of effective education for individuals with epilepsy on their knowledge level, self‐management, and stigma.
Methods: A survey containing an 'Epilepsy Knowledge Form,' 'Epilepsy Self‐Management Scale,' and 'Stigma Scale' was sent to all patients registered at our epilepsy outpatient clinic. Afterwards, patients were invited to an online live epilepsy lesson. Participants were re‐tested after the training.
Results: Of the 265 patients who completed the pre‐education survey, 69 (26%) attended the education. University graduates and individuals who use the internet as a source of information were more motivated to attend, while singles attended less. The average age of participants was 39.1 ± 9.2 (21–68) years; 42 (60.9%) were women, 65.2% were university graduates, and 60.9% were actively working. 44.9% had focal, 21.7% had generalized, and 33.3% had both focal and generalized seizures. 69.6% of the participants had seizure frequency of less than once a month. 50.7% were on monotherapy, and 94.2% regularly took their antiseizure medication. The most common sources of information were doctors, the internet, other patients, television, and social media (100%, 65.2%, 27.5%, 20.3%, 17.4%, respectively). After the education, patients answered more knowledge questions correctly (p = 0.000, before: 37.0 ± 6, after: 40.7 ± 6.1), awareness about the risks of swimming increased, and their motivation to carry health information cards, participate in support groups, and teach epilepsy to relatives increased. No change was observed in the stigma scale.
Conclusion: Education for individuals with epilepsy positively contributes to their awareness and self‐management regarding their condition. Combating stigmatization requires broader societal involvement.
Disclosure: This study has been presented in 59th Turkish National Neurology Congress.
EPO‐116
Intraoperative recordings in bottom‐of‐the‐sulcus focal cortical dysplasia with new highly flexible cortical strip
N. Biagioli 1; S. Morandi2; E. Moriconi3; G. Giovannini4; V. Tramontano2; N. Orlandi1; M. Pugnaghi4; A. Vaudano1; S. Meletti1
1Department of Biomedical Metabolic Sciences and Neurosciences, University of Modena and Reggio Emilia; 2SSD of Clinical Neurophysiology, AOU of Modena; 3CS of Neurosurgery, Head and Neck Neuroscience Department, Modena AOU; 4CS of Neurology, Head and Neck Neuroscience Department, Modena AOU
Background and Aims: the recording of epileptiform discharges from Bottom‐Of‐Sulcus focal cortical Dysplasia (BOSD) is often difficult during intraoperative electrocorticography (iECoG) due to the deep localization. We describe how the use of new generation electrodes with high flexibility easily adapting to cortical gyri and sulci can improve electrocortical recording.

1) Example of the high flexibility of the strip 2) pre‐surgical 3D reconstruction showing major tracts (BOSD in red)
Methods: a right‐handed 20‐years‐old male with drug‐resistant focal epilepsy due to a BOSD of the inferior frontal gyrus and daily focal aware seizures was evaluated for epilepsy surgery. Based on electroclinical and neuroimaging results a focal cortectomy guided by iECoG was proposed. iECoG recordings were performed with new generation cortical strips (Wise Cortical Strip; WCS®) and with standard cortical strips. Both bipolar and referential electrode montages were reviewed to identify epileptiform activity.
Results: iECoG, performed on the convexity of the frontal cortical surface recorded only sporadic spikes with both strip's types. Then, after a microsurgical trans‐sulcal dissection, WCS was molded along the sulcal surface of the suspected BOSD based on 3D‐ imaging reconstruction, showing a continuous/subcontinuous 3–4 Hz rhythmic spikes activity from the deepest electrode. Registration after resection of the BOSD didn’t show any epileptiform activity. Pathology showed dysmorphic neuron and gliosis. No surgical complications occurred. Patient is seizure free after 12 months.

Placement of the strip on the cortical convexity with related electocorticography (WCS in blue, ICS in red), No clear epileptic activities reordered
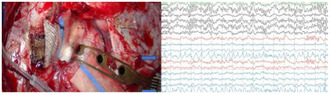
Placement of the strip at the bottom of the sulci, with electrocorticography showing continuous ictal activity from the deepest electrodes
Conclusion: This case report showed that new generation cortical electrodes with high flexibility features allowed to perform high‐quality recordings from the bottom of the sulcus, overcoming a limit of classical iECoG that typically doesn’t allow registration from the deepest of the cortical sulci.
Disclosure: Nothing to disclose.
EPO‐117
Tailored surgery guided by intraoperative electrocorticography (iEcoG) in temporal lobe encephalocele (TE)
N. BIagioli 1; S. Morandi2; E. Moriconi3; M. PPugnaghi4; N. Orlandi1; G. Giovannini4; V. Tramontano2; G. Pavesi3; A. Vaudano1; S. Meletti1
1Department of Biomedical Metabolic Sciences and Neurosciences, University of Modena and Reggio Emilia; 2SSD of Clinical Neurophysiology, AOU of Modena; 3CS of Neurosurgery, Head and Neck Neuroscience Department, Modena AOU; 4CS of Neurology, Head and Neck Neuroscience Department, Modena AOU
Background and Aims: TE can lead to medically refractory epilepsy, warranting surgical intervention. However, there is a lack of consensus on the appropriate surgical approach. This case series illustrates the potential effectiveness of iEcoG in guiding personalized lobectomy procedures for TE.
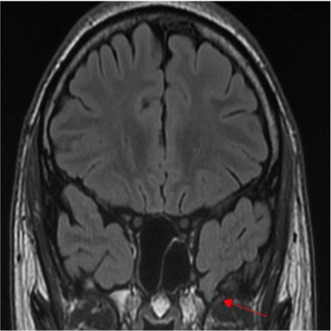
COR FLAIR brain MRI at the level of the temporal poles with finding of left temporal encephalocele (indicated by the red arrow)
Methods: patients underwent surgery following thorough anamnestic, neurophysiological, and neuroradiological assessments. iECoG were conducted on the cortical area pre‐ and post‐resection, concluding with assessments on mesial temporal structures.
Results: Patient 1: 38‐year‐old male with left temporal pole encephalocele. iECoG show sporadic spikes on the neocortical temporal surface before surgical resection, while no epileptic activity was recorded on the amygdala and hippocampus. Therefore, the mesial structures were spared. Pathology: FCD‐Ia. Patient 2: 20‐year‐old male with left mesial temporal pole encephalocele. iECoG revealed frequent irregular spiking on the neocortical temporal surface before surgical resection and persistent epileptic activity on the posterior temporal resection margin, so the surgical procedure was extended until the sylvian vein. No epileptic activity was seen on the hippocampus thus it was spared. Pathology: cortical dyslamination. Patient 3: 72‐year‐old female with extensive right temporopolar encephalocele. iECoG recorded sporadic epileptic activity in anterior section close to the borders of the encephalocele, sparing resection borders and temporomesial structures. Pathology: gliosis. All patients are in Engel class IA.
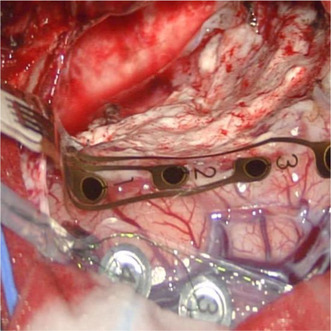
EcoG (patient 2) at the level of the encephalocele and neighboring cortex pre‐resection
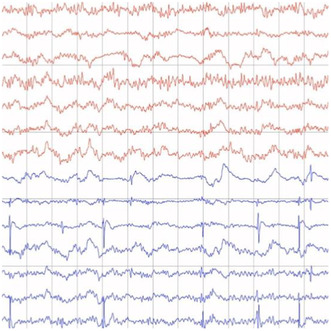
electrode strip placed on the posterior margin of the resection
Conclusion: These 3 cases show the usefulness of ECoG for a tailored surgical resection according to the irritative zone.
Disclosure: Nothing to disclose.
EPO‐118
Comparisons between traditional, brief, and ultra‐brief anxiety and depression inventories in people with epilepsy
R. João; L. Scárdua‐Silva; M. Alvim; F. Cendes; M. Nogueira; C. Yasuda
Neurology Department – University of Campinas (Unicamp), Campinas, Brazil
Background and Aims: While fast (and accurate) large scale detection of anxiety/depression symptoms is desirable for people with epilepsy (PWE), traditional inventories are time‐consuming and less practical. Here, we compared traditional questionnaires (Beck Anxiety Inventory [BAI] and Beck Depression Inventory‐II [BDI‐II]) with brief inventories (Generalized Anxiety Disorders‐7 [GAD‐7] and Neurological Disorders Depression Inventory for Epilepsy [NDDIE]) and ultra‐brief inventories (GAD‐2, GAD Single‐item [GAD‐SI], and NDDIE‐2) for symptom's detection.
Methods: We evaluated 548 consecutive PWE (60% women; median‐age 41 years) with different questionnaires for anxiety/depression. We considered as symptomatic the individuals scoring ≥14 points in both BAI/BDI‐II, ≥7 in GAD7, ≥3 in GAD‐2, ≥2 in GAD‐SI, ≥13 in NDDIE, and ≥ 4 in NDDIE‐2. We used SPSS for the Receiver Operator Characteristic (ROC) curve analysis (with area under‐curve values [AUC]) and cross‐accuracy analysis (with Kappa‐Index [KI] values).
Results: We compared the BAI's performance with GAD‐7 (AUC = 0.88; p = 0.017), GAD‐2 (AUC = 0.84; p = 0.019), and GAD‐SI (AUC = 0.80; p = 0.022 – Figure 1A). We also compared the GAD‐7's performance with GAD‐2 (AUC = 0.94; p = 0.01) and GAD‐SI (AUC = 0.85; p = 0.019 – Figure 1B). Moreover, we obtained similar values comparing BDI‐II with both NDDIE (AUC = 0.87; p < 0.001) and NDDIE‐2 (AUC = 0.84; p < 0.001 – Figure 1C) and comparing NDDIE with NDDIE‐2 (AUC = 0.93; p < 0.001 – Figure 1D). There was an overall moderate‐to‐substantial agreement in the cross‐accuracy analysis: KI = 0.57 (BAI and GAD‐7), KI = 0.49 (BAI and GAD‐2), KI = 0.5 (BAI and GAD‐SI), KI = 0.62 (BDI‐II and NDDIE), and KI = 0.43 (BDI‐II and NDDIE‐2).
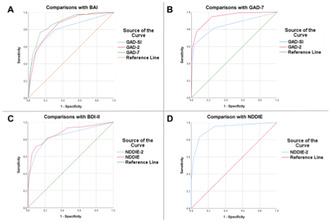
FIGURE 1 The ROC curve analysis showed high AUC in the comparisons between traditional, brief, and ultra‐brief anxiety and depression inventories in people with epilepsy.
Conclusion: The shorter anxiety/depression inventories may be a fast and reliable alternative to traditional tests for PWE.
Disclosure: Nothing to disclose.
EPO‐119
A clinical case of targeted memantine treatment in a patient with GRIN2A mutation and epileptic encephalopathy
S. Shokhimardonov; N. Tuychibaeva; S. Kuzieva
Neurology Department, Tashkent Medical Academy, Tashkent, Uzbekistan
Background and Aims: Epileptic encephalopathy with continuous spike and wave during sleep (CSWS) is a syndrome marked by progressive cognitive decline, epileptic seizures, specific EEG patterns, and a complex/polygenic inheritance. Given the elevated incidence of drug resistance, the development of more effective and targeted treatment approaches for patients is relevant.
Methods: In our study, we intentionally selected 88 patients diagnosed with epileptic encephalopathy with continuous spike and wave during sleep. All participants were tested with: neuropsychological, clinical, neurophysiological, neuroimaging, and genetic assessments, including whole exome sequencing (WES). Among these individuals, we identified one with a GRIN2A mutation showing a gain of function variant (GoF), for further targeted treatment with memantine with daily dose 0.5 mg/kg per day."
Results: At a memantine dosage of 0.5 mg/kg, with no adjustments to antiepileptic drug doses, we observed a notable 65% reduction in average seizure frequency. This decline manifested within several weeks of reaching the full memantine dose and persisted throughout the 3‐month follow‐up period. We also observed an improvement in interictal EEG recordings, with no epileptiform discharges during both wakefulness and sleep, contrasting with the EEG prior to memantine initiation. While there were slight changes in cognitive skills, overall improvement was noted.
Conclusion: This clinical case exemplifies the significant potential of targeted treatment for epilepsy. Further clinical research and continuous follow‐up are necessary to gather additional insights and information.
Disclosure: Nothing to disclose.
EPO‐120
Calponin‐3 in astrocytes accelerate astrocytic activation and adenosine metabolism affects epileptogenesis
L. Chen; Y. Han
First Department of Neurology, First Affiliated Hospital, Kunming Medical University, Kunming, Yunnan, China
Background and Aims: Calponin‐3—a member of the calponin family of actin‐binding proteins, which is highly expressed in the mammalian brain—has been found increased in temporal lobe epilepsy (TLE) patients and pilocarpine‐induced epileptic rats. However, its role in the epileptogenesis is unclear.
Methods: Serum and brain tissues of epileptic patients and Kainic acid (KA) and pentattrazene (PTZ) induced epilepsy mouse model were used to detect the expression level and cellular localization of calponin‐3. calponin‐3 in the hippocampus of C57BL/6 mice was up‐regulated, and calponin‐3 in hippocampus of KA‐induced epilepsy mice was down‐regulated. The effect of calponin‐3 expression change on the occurrence and development of epilepsy was observed in mice with specific knockout of calponin‐3 in astrocytes.
Results: In epilepsy patients and KA‐induced epilepsy models, calponin‐3 was significantly up‐regulated in serum and brain tissue. Meanwhile, the up‐regulated calponin‐3 expression was mainly in astrocytes. Behavioral and EEG findings showed that upregulation of calponin‐3 increased the susceptibility to epilepsy, while downregulation of calponin‐3 in KA‐induced mouse models had a protective effect on spontaneous seizures. Finally, it was found that the susceptibility to epilepsy was significantly reduced in transgenic GFAP‐CNN3‐KO mice. Mechanism, in vitro and in vivo confirmed that down‐regulation of calponin‐3 in astrocytes can suppress astrocyte activation and reduce adenosine metabolism.
Conclusion: Targeting calponin‐3 in astrocytes, and reducing its expression will have a protective effect on epilepsy by regulating astrocyte activation and adenosine metabolism
Disclosure: Nothing to disclose.
Headache 1
EPO‐121
Plasma calcitonin gene‐related peptide levels in idiopathic intracranial hypertension: An exploratory study
N. Krajnc; F. Frank2; S. Macher1; M. Michl3; N. Müller1; S. Maier4; S. Zaic1; C. Wöber1; B. Pemp3; G. Brössner2; G. Bsteh1
1Department of Neurology, Medical University of Vienna, Vienna, Austria; 2Department of Neurology, Headache Outpatient Clinic, Medical University of Innsbruck, Innsbruck, Austria; 3Department of Ophthalmology, Medical University of Vienna, Vienna, Austria; 4Department of Medical Statistics, Informatics and Health Economics, Medical University of Innsbruck, Innsbruck, Austria
Background and Aims: Idiopathic intracranial hypertension (IIH) is a condition characterized by increased intracranial pressure often presenting with migraine‐like headache. Calcitonin gene‐related peptide (CGRP) plays an important pathophysiological role in primary headaches, whilst its role in IIH has not been established.
Methods: This longitudinal exploratory study included patients with definite IIH, episodic migraine (EM) in a headache‐free interval and healthy controls (HC). Subjects were divided into those with: (1) log pCGRP Z scores ≤1.5 (termed as ‘non‐elevated’), and (2) log pCGRP Z scores >1.5 (termed as ‘elevated’).
Results: A total of 26 patients with IIH (mean age 33.2 years [SD 9.2], 88.5% female), 30 patients with EM (mean age 27.6 years [7.5], 66.7% female) and 57 HC (mean age 25.3 years [5.2], 56.1% female) were included. Median pCGRP levels in patients with IIH, EM and HC were 15 pg/ml (10.8–237), 30.5 pg/ml (23.2–197.4), and 56.3 pg/ml (53.4–228.2), respectively (p < 0.001). We found no differences between the prevalence of elevated pCGRP levels in patients with IIH, EM and HC (6 [23.1%], 4 [13.3%] and 8 [14.0%], respectively, p = 0.523). PwIIH with elevated pCGRP levels had more often a history of migraine (5/6 [83.3%] vs. 3/20 [15.0%], p = 0.004) and photo‐ and/or phonophobia as concomitant symptoms (6/6 [100.0%] vs. 7/20 [35.0%], p = 0.015). Elevated pCGRP levels were not associated with ophthalmological parameters.

pCGRP levels (pg/ml) in patients with IIH, EM in a headache‐free interval, and HC; linear (a) and logarithmic (b) scale. Proportion of subjects with elevated pCGRP levels (log pCGRP Z score >1.5) in pwIIH, EM and HC (c).
Conclusion: PwIIH display similar prevalence of elevated pCGRP levels as pwEM. As elevated pCGRP levels are associated with headache presence and frequency, CGRP may play a role in the pathophysiology of headache in IIH.
Disclosure: Nothing to disclose.
EPO‐122
Brain resting state networks in episodic cluster headache: Cerebral connectivity analysis with HD‐EEG
A. Antoniazzi 1; R. De Icco1; G. Vaghi1; M. Corrado1; F. Cammarota1; F. Bighiani1; E. Mazzotta1; V. Grillo1; M. Semprini2; G. Sances3; M. Allena3; C. Tassorelli1
1Department of Brain and Behavioral Sciences, University of Pavia, Pavia, Italy; 2Italian Institute of Technology, Genova, Italy; 3Headache Science & Neurorehabiitation Center, IRCCS Mondino Foundation, Pavia, Italy
Background and Aims: A convincing explanation for the switch between the active and remission phases of episodic cluster headache (eCH) is lacking. In this study, we aim to shed some light on these mechanisms by analyzing internodal connectivity patterns in the brains of eCH patients by means of high‐density electroencephalography (HD‐EEG).
Methods: Twenty‐four eCH patients underwent HD‐EEG recordings in two conditions: active phase (T0) and remission period (T1). Nineteen sex and age matched controls underwent a single HD‐EEG evaluation. Through these data we reconstructed the inter‐networks and intra‐network connectivity of six resting state networks: default mode network (DMN), dorsal attention network (DAN), ventral attention network (VAN), language attention network (LAN), somatomotor network (SMN), visual network (VN).
Results: At T1 there was a significant difference in alpha band connectivity between eCH patients and HCs in the intra‐network connectivity of the DMN (eCH = 0.089 ± 0.007; HC = 0.115 ± 0.009; mean difference 0.026 ± 0.012; p = 0.034) and of the VN (eCH = 0.085 ± 0.007; HC = 0.109 ± 0.008: mean difference 0.025 ± 0.011; p = 0.034). Moreover, eCH patients and HCs showed a significant difference at T1 in alpha band inter‐network connectivity between the DMN and the VN (eCH = 0.089 ± 0.007; HC = 0.114 ± 0.008; mean difference 0.025 ± 0.012; p = 0.038).
Conclusion: Our findings show how eCH patients have a reduced alpha band connectivity during the remission period within and between the DMN and the VN networks. These alterations may be associated to the shift between the two states of the disease and support the relevance of electrophysiological studies in providing insights into cluster headache physiopathology.
Disclosure: None.
EPO‐123
Evaluation of premonitory symptoms among patients with cluster headache
A. Gonzalez‐Martinez 1; W. Diana2; N. Karsan2; H. Gosalia2; P. Goadsby2
11NIHR King's Clinical Research Facility and Wolfson SPaRC, King's College London, UK 2Hospital Universitario de la Princesa & Instituto de Investigación Sanitaria Princesa (IIS‐Princesa), Madrid, Spain, 21NIHR King's Clinical Research Facility and Wolfson SPaRC, King's College London, UK
Background and Aims: Cluster headache (CH) is a rare primary headache known for its unilateral very severe pain accompanied by cranial autonomic symptoms, which has a strong impact in patients’ quality of life. Several studies have identified premonitory symptoms of migraine while few studies have evaluated the frequency and type of premonitory symptoms in patients with CH. This study aimed to assess the presence and type of premonitory symptoms in patients with CH.
Methods: A retrospective study was conducted to investigate the presence and type of premonitory symptoms in a cohort of patients with CH attended at a Headache Unit of a tertiary hospital specialized in CH treatment. Demographic data and premonitory symptoms in CH patients were evaluated as part of a service evaluation. The primary endpoint was the presence of premonitory symptoms in patients with CH. Secondary endpoints involved the description of the type of premonitory symptoms.
Results: A total of 164 patients, 121/165 (74%) males, 45.9 (SD: 13.8) years old, 66/164 (40%) chronic, from clinical CH cohort. Premonitory symptoms were present in 139/164 (85%) of CH patients. The most common general premonitory symptoms in CH patients were mood changes (44%), cognitive impairment (28%), neck stiffness (23%), fatigue (22%) and yawning (17%).
Conclusion: In summary, this study underscores the presence of recognisable spontaneous premonitory symptoms in CH that may have an impact in management of CH. Understanding the CH premonitory symptoms can aid in the development of more tailored treatment strategies for these patients.
Disclosure: AGM reports, over the last 36 months, speaker honoraria from TEVA and Altermedica, and reports no disclosures related with this work. PJG reports, over the last 36 months, grants from Celgene and Kallyope, and personal fees from Aeon Biopharma, Abbvie, Amgen, eNeura, CoolTech LLC, Dr Reddys, Eli‐Lilly and Company, Epalex, Linpharma, Lundbeck, Man&Science, Novartis, Pfizer, Sanofi, Satsuma, Shiratronics, and Teva Pharmaceuticals, and personal fees for advice through Gerson Lehrman Group, Guidepoint, SAI Med Partners, Vector Metric, and fees for educational materials from CME Outfitters, and publishing royalties or fees from Massachusetts Medical Society, Oxford University Press, UptoDate and Wolters Kluwer. DW, NK and HG report nothing to disclose.
EPO‐124
Neurophysiological and neuropsychological correlates of migraine with aura
A. Pjeci; M. Russo; S. Melchiorre; G. Polito; C. Ciprietti; L. Marzetti; S. Sensi
Department of Neuroscience, Imaging and Clinical Sciences, G. D’Annunzio University of Chieti‐Pescara, Chieti, Italy
Background and Aims: Migraine with aura afflicts about 5% of the population and is frequently associated with psychological disturbances like depression and anxiety. Few studies in the literature have analyzed the functional connectivity of patients with this comparing it with that of healthy subjects. This study aims to fill this gap in the literature by comparing neurophysiological correlates of functional connectivity at resting state‐EEG (rs‐EEG) of subjects with migraine with aura and controls.
Methods: Migraine with aura subjects and controls were enrolled in a 1:1 ratio. The inclusion criteria were age between 18 and 50 and absence of other neurological, psychiatric, or system disorders in both groups of subjects. A 20‐minute inter‐ictal rsEEG was performed after subjecting them to a neuropsychological assessment including BAI and BDI II. Then EEG functional connectivity was evaluated by using coherence analysis.
Results: Comparisons in the beta frequency band showed hyperconnectivity in the right central‐parietal regions in migraineurs. Furthermore, hyperconnectivity was found in the alpha band in the right occipital and parietal areas.
Conclusion: Migraineurs present a different resting state connectivity pattern in brain regions correlated with pain perception and elaboration (pain matrix), even in the inter‐ictal phase. Our results indicate that migraineurs share a neurophysiological “fingerprint” with other conditions associated with chronic or relapsing‐remitting pain (e.g., fibromyalgia).
Disclosure: Nothing to disclose.
EPO‐125
Contemporary prospective understanding of migraine real‐world evidence (CAPTURE): Baseline clinical characteristics
M. Ashina 1; M. Peres2; R. Stark3; M. Lanteri‐Minet4; E. Tucker5; Y. Liu6; J. Lam5; H. Ha5; L. Delahaye7; P. Pozo‐Rosich8
1Department of Neurology, Danish Headache Center, Copenhagen University Hospital – Rigshospitalet, and Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark; 2University of São Paulo, São Paulo, Brazil; 3Alfred Hospital and Monash University, Melbourne, VIC, Australia; 4Pain Department and FHU InovPain, CHU Nice and Côte Azur University, Nice, France and INSERM U1107 Migraine and Trigeminal Pain, Auvergne University, Clermont‐Ferrand, France; 5AbbVie, Toronto, ON, Canada; 6AbbVie, North Chicago, IL, USA; 7AbbVie, Rungis, France; 8Headache Unit, Neurology Department, Vall d’Hebron University Hospital, and Headache and Neurological Pain Research Group, Vall d’Hebron Institute of Research, Universitat Autònoma de Barcelona, Barcelona, Spain
Background and Aims: CAPTURE is a 2‐year, international, prospective, longitudinal study that aims to enhance our understanding of disease burden and treatment patterns among people living with migraine, stratified by headache frequency.
Methods: Adults with > = 1‐year migraine diagnosis aged < 50 years at onset who were taking > = 1 medication indicated for migraine and had > = 4 monthly headache days (MHDs) in the 3 months before screening were assigned to cohorts based on MHD frequency (cohort 1: 4‐ < 8; cohort 2: 8‐ < 15; cohort 3: > = 15; Figure). Descriptive data for baseline demographics and clinical characteristics (migraine duration, MHDs, monthly migraine days [MMDs], monthly acute medication use days, migraine‐related comorbidities) are presented. Changes from baseline in MHDs, MMDs, acute medication use days, and patient‐reported outcomes across the study period and durations of current and subsequent migraine treatment use will be assessed.
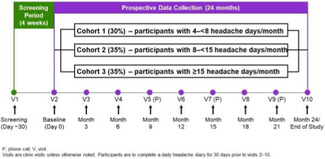
FIGURE CAPTURE Study Design
Results: As of December 2023, among the 239 participants (cohort 1: n = 68; cohort 2: n = 104; cohort 3: n = 67), mean age was 40.8–42.6 years, >95% of participants were White, >78% were female, and >77% resided in Europe (Table 1). Mean duration of migraine since onset was similar among cohorts (23.0–23.8 years) (Table 2). Past use of preventive treatments was high (cohort 1, 81.8%; cohort 2, 81.4%; cohort 3, 92.3%). The most prevalent migraine‐related comorbidity was hypertension (cohort 1: 4.4%; cohort 2: 7.7%; cohort 3: 9.0%).
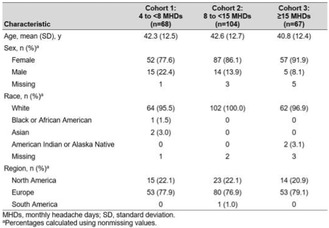
TABLE 1 Baseline Demographic Characteristics
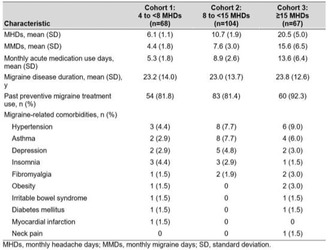
TABLE 2 Baseline Migraine Disease Characteristics
Conclusion: CAPTURE aims to provide pivotal data on the longitudinal course of migraine and associated treatment patterns, stratified by headache frequency. This study promises to provide insights for developing tailored treatment approaches for people with migraine.
Disclosure: This study was supported by AbbVie.
EPO‐126
Female sexual dysfunction and distress in migraine: Results from a tertiary referral hospital
M. Bertão1; B. Martins 2; A. Costa2
1Faculty of Medicine, University of Porto, Portugal; 2Neurology Department, Centro Hospitalar Universitário de São João, E.P.E., Porto, Portugal
Background and Aims: Female sexual dysfunction (FSD) is a persistent, underdiagnosed, and undertreated problem, associated with psychological suffering. Only a few studies have addressed the sexual distress caused by migraine. We aimed to determine if migraine is associated with sexual dysfunction/distress and what their risk factors.
Methods: Retrospective, cross‐sectional study, including 71 premenopausal female patients with migraine, followed in a tertiary hospital (05/2023–12/2023), and 34 healthy age‐matched‐controls. Female sexual function index‐6 (FSFI‐6), FS distress scale‐revised (FSDS‐R), Hospital depression and anxiety (HADS), Migraine disability assessment (MIDAS), and Satisfaction Alertness Timing Efficiency Duration of sleep (SATED) scales were applied.
Results: Of the 71 female patients [median age: 40.0 (AQR = 11.00) years; married/stable relationship: 78.9%], only 9 (12.7%) were not under migraine preventive treatment; most (33, 62.3%) reported severe disability (MIDAS‐IV). Migraine patients showed lower FSFI‐6 scores [19.0 (9.0) vs controls with 24.0 (6.0), p = 0.003), with significantly lower levels of desire (p = 0.011), lubrification (p = 0.002), and satisfaction (p = 0.013), and higher sexual distress [11.2 (25.6) vs 3.2 (9.6), p = 0.001). They had also higher anxiety [10.0 (6.0) vs 5.0 (6.0), p ≤ 0.001] and depression [7.0 (7.0) vs. 2.0 (3.0), p ≤ 0.001] levels, and lower sleep health scores [18.0 (12.0) vs 23.5 (9.0), p = 0.005] compared to healthy controls. Anxiety, depression, and dysfunctional sleep were found to be significantly related to sexual dysfunction.
Conclusion: This work showed that migraine is associated with sexual dysfunction and distress, reflecting the necessity of an evaluation of sexual health in these patients, mainly in the ones with higher levels of anxiety, depression, or poor quality of sleep.
Disclosure: Nothing to disclose.
EPO‐127
Role of venous sinus stenosis in intracranial hypertension: Pathophysiology and response to medical treatment
C. Gavancho 1; R. Lindeza2; M. Pimenta1; M. Cazola1; J. Rosa1
1Neurology Department, Hospital de São José, Unidade Local de Saúde São Jose, Lisbon, Portugal; 2Neuroradiology Department, Hospital de São José, Unidade Local de Saúde São José, Lisbon, Portugal
Background and Aims: Venous sinus stenosis (VSS) is described in intracranial hypertension (IH), but its role in its pathophysiology is not entirely established. We aimed to characterize VSS in intracranial hypertension and its possible influence in cerebrospinal fluid (CSF) opening pressure and clinical response to medical therapy.
Methods: We analyzed 21 patients admitted to the Neurology Ward of Hospital de São José in Lisbon, Portugal, between 2016 and 2023 with intracranial hypertension (19 with idiopathic IH). Using SPSS, we carried out a descriptive analysis of the variables and applied the Chi‐squared, Shapiro‐Wilk, Mann‐Whitney, and Student's t tests.
Results: We identified VSS in 19% of the patients (n = 4), half in the transverse sinus and half in the transverse‐sigmoid transition. The median CSF opening pressure was 32.67(9.5)cm H2O and it was lower in the VSS group, suggesting a negative impact of the stenosis on this measure (p = 0.017). We found a correlation between the presence of VSS and poor clinical response to medical therapy (p = 0.018). There were no statistically significant differences in the CSF opening pressure or response to medical therapy between the group with transverse sinus stenosis and the group with transverse‐sigmoid transition stenosis.
Conclusion: The presence of VSS seems to correlate with a less favorable clinical response to medical therapy in IH. We couldn’t establish a correlation between VSS and the pathophysiology of IH. The role of VSS should be further explored to clarify its pathophysiology and the therapeutic potential of venous sinus stenting.
Disclosure: Nothing to disclose.
EPO‐128
Contemporary prospective understanding of migraine real‐world evidence (CAPTURE): Baseline migraine treatment patterns
C. Tassorelli 1; M. Matharu2; J. Ailani3; M. Lanteri‐Minet4; E. Tucker5; J. Lam5; Y. Liu6; H. Ha5; L. Delahaye7; P. Pozo‐Rosich8
1University of Pavia and C. Mondino Foundation, Pavia, Italy; 2Queen Square Institute of Neurology, London, England, UK; 3MedStar, Georgetown University Hospital, Washington, DC, USA; 4Pain Department and FHU InovPain, CHU Nice and Côte Azur University, Nice, France and INSERM U1107 Migraine and Trigeminal Pain, Auvergne University, Clermont‐Ferrand, France; 5AbbVie, Toronto, ON, Canada; 6AbbVie, North Chicago, IL, USA; 7AbbVie, Rungis, France; 8Headache Unit, Neurology Department, Vall d’Hebron University Hospital and Headache and Neurological Pain Research Group, Vall d’Hebron Institute of Research, Universitat Autònoma de Barcelona, Barcelona, Spain
Background and Aims: CAPTURE is a 2‐year, international, prospective, longitudinal study that aims to elevate understanding of burden of illness, disease course, and treatment patterns among people living with migraine, stratified by headache frequency.
Methods: Adults with migraine diagnosed for > = 1 year, aged <50 years at onset, and taking > = 1 medication indicated for migraine with > = 4 monthly headache days (MHDs) in the 3 months before screening were assigned to cohorts based on MHD frequency (cohort 1: 4‐ < 8; cohort 2: 8‐ < 15; cohort 3: > = 15; Figure). Descriptive data for baseline characteristics, including current/prior migraine medications, are presented. Endpoints include change from baseline in MHDs, monthly migraine days, monthly acute medication use days, and patient‐reported outcomes across the study period. Durations of current and subsequent migraine treatment use and migraine‐related healthcare resource utilisation will also be assessed.
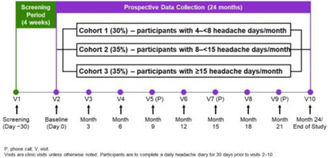
FIGURE CAPTURE Study Design
Results: This analysis set (December 2023) included 239 participants (cohort 1: n = 68; cohort 2: n = 104; cohort 3: n = 67; mean age 40.8–42.6 years); more than 78% were female (Table 1). In cohorts 1, 2, and 3, current use of acute migraine medication only was reported for 5.9%, 2.9%, and 0% of participants; preventive medication only for 19.1%, 27.9%, and 32.8%; and both acute and preventive medication for 27.9%, 20.2%, and 26.9%, respectively (Table 2). Most common current acute medications were triptans and propionic acid derivatives; most common current preventive medications were topiramate, amitriptyline and calcitonin gene–related peptide receptor monoclonal antibodies.
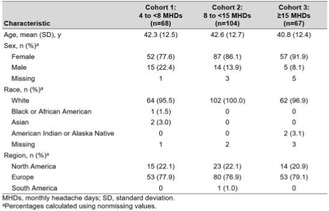
TABLE 1 Baseline Demographic Characteristics
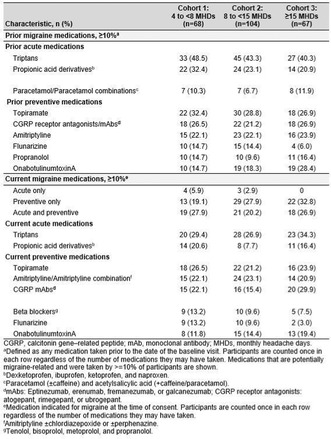
TABLE 2 Baseline Medication Use
Conclusion: The CAPTURE study will build a large, longitudinal database on migraine treatment patterns in the contemporary era and associated disease trajectories.
Disclosure: This study was supported by AbbVie.
EPO‐129
Prophylactic polytherapy for chronic migraine: Evaluating the addition of atogepant to onabotulinumtoxinA
J. Rothrock; A. Koutsandreas; L. Armstead
Inova Health/University of Virginia, Fairfax, VA, USA
Background and Aims: OnabotulinumA (BotoxA) may reduce migraine burden only partially in patients with chronic migraine (CM). We sought to determine whether adding atogepant 60 mg daily to ongoing treatment with BotoxA might be synergistic.
Methods: We prescribed atogepant 60 mg daily to a clinic population of CM patients who had been receiving BotoxA for at least one year and whose response had remained stable for the last 2 consecutive 12‐week intervals between treatments. We assessed mean monthly migraine days (MMMDs), mean monthly headache days (MMHDs), mean monthly days of functionally incapacitating headache (FIHDs), mean monthly days of symptomatic medication use (MMDSMU), migraine burden index (MBI) and MIDAS scores for the 3 months preceding initiation of treatment with atogepant and again 12 weeks following initiation of treatment with atogepant. A patient was considered to be a positive responder to polytherapy if he/she reported a 50% or greater reduction in MMMDs relative to their pre‐atogepant status (primary endpoint).
Results: Of 211 patients, 132 (63%) achieved the primary treatment endpoint of a 50% or greater reduction in MMMDs experienced over the 12 week treatment period relative to their pre‐atogepant status. MMHDs declined by 6.6 days, mean FIHDs by 2.7 days, MMDSMU by 5.4 days, MIDAS by 21.6 and MBI score by 14.6.
Conclusion: Adding atogepant 60 mg to the prophylactic regimen of CM patients receiving BotoxA resulted in apparent synergism in almost two‐thirds.
Disclosure: Dr. Rothrock has served as an consultant to/promotional speaker for AbbVie. His parent institution has received funding from AbbVie for research he has conducted.
EPO‐130
Management of migraine without aura in adolescents: The efficacy of flunarizine in a Turkish Cohort
F. İlik 1; D. Ertem2; M. İlik3
1Department of Neurology, KTO University, Medical Faculty, Konya, Turkey; 2Department of Neurology, Silivri Anadolu Hospital, Istanbul, Turkey; 3Department of Neurosurgery, Ozel Buyuksehir Hospital, Konya, Turkey
Background and Aims: Flunarizine is a specific calcium antagonist and is frequently used in adults for the prophylactic treatment of migraine. The use of flunarizine may lead to somnolence and weight gain, depression, and rarely extrapyramidal symptoms in adults. However, studies detecting the efficacy and safety of flunarizine use in adolescents are limited. In the current study, the effectiveness of flunarizine for the management of chronic migraine without aura in Turkish adolescents was evaluated.
Methods: Forty‐six patients with migraine without aura, aged 12–18 years, receiving flunarizine 5mg per day were included. In this retrospective study, the medical records of the cases were examined. Changes in the Numeric Pain Rating Scale (NPRS) and MIDAS scores were compared to assess the efficacy of the treatment in 3 months.
Results: The mean age was 14.37 ± 1.83 years. There was a significant improvement in the NPRS and MIDAS scores of the patients at the end of 3 months (p < 0.05). Side effects were detected in 23.9% of the patients, and these symptoms were sedation in 8.7% of the patients, mood swings in 4.3%, and vomiting %4.3 of them. None of the patients discontinued the treatment due to side effects.
Conclusion: Although the advancement of migraine research and treatment is inevitable, our findings support that flunarizine should still be considered in mind as an effective and tolerable treatment option in adolescent migraineurs
Disclosure: Nothing to disclose.
EPO‐131
Acute medication overuse in people with migraine from the 2022 European National Health & Wellness Survey
G. Coppola1; A. Gendolla2; M. Lewis3; A. Jenkins4; J. Cirillo5; K. Hygge Blakeman6; J. Yang7; L. Abraham4; J. Brown 3
1Department of Medico‐Surgical Sciences and Biotechnologies, Sapienza University of Rome Polo Pontino, Latina, Italy; 2Praxis Gendolla, Essen, Germany; 3Real World Evidence, Pfizer, New York, NY, USA; 4HTA, Value & Evidence, Pfizer, Tadworth, UK; 5HTA, Value & Evidence, Pfizer, New York, NY, USA; 6Global Medical Affairs, Pfizer, Stockholm, Sweden; 7Global Medical Affairs, Pfizer, New York, NY, USA
Background and Aims: Acute medication overuse (AMO) is a cycle of high‐frequency analgesic use, such as triptans and non‐steroidal anti‐inflammatory drugs (NSAIDs) that may result in medication overuse headache (MOH). There is limited understanding of the frequency of analgesic use of both prescription and over‐the‐counter analgesics among people with migraine (PwM) in Europe.
Methods: Using the 2022 5‐country European National Health and Wellness Survey (NHWS, Cerner Enviza), patients diagnosed with migraine receiving > = 1 acute medication were described. AMO criteria were: 1) > = 10 cumulative days per month with use of triptans, combination analgesics, ergotamines, or opioids; or 2) > = 15 days of nonopioid analgesic, acetaminophen, or NSAID use. AMO was assessed separately among analgesics for migraine only and those used for migraine plus other pain conditions.
Results: Among over 16.7 million PwM represented by the survey, 21.2% reported AMO of migraine‐specific medications, and 36.9% had AMO after including medications used for other conditions. Over half (51.4%) met the first AMO criterion with a cumulative mean [SD] of 21.0 [14.1] days, and 61.5% met the second criterion with 28.3 [15.9] cumulative days. PwM with AMO versus without AMO reported higher use of prescribed triptans (38.4% vs. 29.9%), NSAIDs (66.4% vs. 51.4%), and opioids (33.6% vs. 12.5%). Compared to individuals without AMO, those with AMO experienced worse quality of life, higher migraine disability scores, decreased productivity, and increased use of healthcare resources.
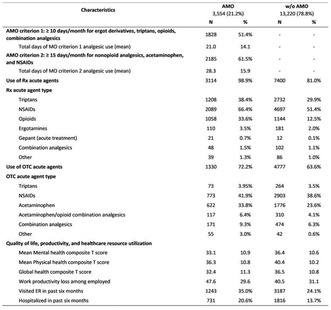
Characteristics of patients with and without AMO of migraine medications
Conclusion: AMO is common in over 20% of PwM and related to poorer quality of life. Treatments not associated with MOH are needed in this population.
Disclosure: GC has received honoraria for participation in clinical trials and contribution to advisory boards or presentations from TEVA, Biohaven, Eli Lilly, Abbvie, and Pfizer. He serves as an Associate Editor for Cephalalgia, BMC Neurology – Pain section, Frontiers in Neurology – Neurotechnology section, Frontiers in Human Neuroscience – Brain Imaging and Stimulation section, and on the Advisory Board of The Journal of Headache and Pain. AG reports financial support for ad boards, consulting and speaker honoraria from: Grünenthal, Mundipharma, Abbvie/Allergan, Lilly, Teva, Amgen, Novartis, Hormosan, Stada, Lundbeck, Pfizer, Hexal, Esanumperfood, Medscape, streamed up, Ärztekammer Nordrhein, Ärztekammer Westfalen Lippe, DGS, Regionalbeauftragte der DMKG. ML, AJ, JC, KHB, JY, LA, and JB are employees of Pfizer.
EPO‐132
Combining monoclonal antibodies and onabotulinumtoxina against highly resistant and invalidated migraine patients
A. Doretti 1; E. Colombo1; G. Demirtzidis1; S. Calzaferri1; M. Sodano1; U. Daniela1; L. Maderna1; V. Silani1; N. Ticozzi2; S. Messina1
1Department of Neurology, Istituto Auxologico Italiano IRCCS, Milan; 2Department of Pathophysiology and Transplantation, University of Milan, Milan
Background and Aims: Onabotulinumtoxin A (BonTA) and monoclonal antibodies (mAbs) are approved migraine treatment targeting CGRP cascade. However, monotherapy does not always yield satisfactory benefits, which raises the question of whether dual therapy with BonTA and mAbs hold promise in patients with treatment‐resistant chronic migraine (CM).
Methods: We retrospectively analyzed 75 subjects diagnosed with highly disabling (MIDAS >30) and resistant CM treated with BonTA that were considered responders, but had a decrease in effect or the effect was non‐sufficient after one year. Therefore, they started a dual therapy with BonTA and mAbs for 1 year. CGRP‐mAbs were stopped for 3 months continuing only BonTA, subsequently a monotherapy with CGRP‐mAbs was performed for 3 months. We evaluated the MIDAS, HIT6, VAS, PGIC and drug intake for all patients in the different timepoints.
Results: 73/75 patients completed the treatment regimen, 2 dropped out for ineffectiveness. No adverse events were reported. Analysis showed a marked decrease in the MIDAS, HIT6, VAS, PGIC scores and analgesic drug intake from visit T0 to visit T3, while on dual therapy; subsequently the scores remained stable up to T12. When patients were on BonTA alone or mAbs alone, there was a worsening of evaluated scores.
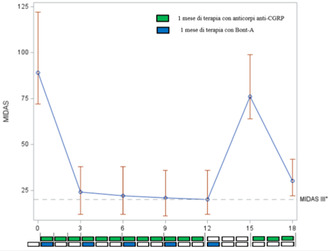
MIDAS reduction during different times of therapies. In green antiCGRP mAbs, in blue BonTA injections
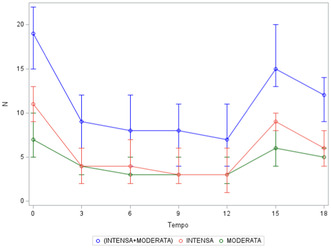
Numbers of days with headache during different times of therapies. Blue line VAS intense+ moderate, in red Intense in green moderate
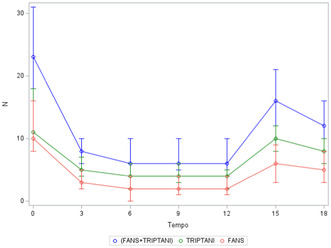
Numbers of drugs taken during different times of therapies. In blue NSAID+triptans, in green triptans, in red NSAID
Conclusion: Our work suggests a possible synergistic effect of these two different therapies in modulating CGRP cascade, determining a greater control of migraine attacks in a population of patients suffering from highly resistant CM. This result without any increase of side effects.
Disclosure: Eleonora Colombo, Daniela Ungaro, Martina Sodano, Gianluca Demirtzidis and Stefano Messina report no disclosure. Alberto Doretti received compensation for consulting services from Abbvie, Teva, Eli Lilly, Lundbeck, Novartis, Neopharmed Gentili, Zambon. Vincenzo Silani received compensation for consulting services and/or speaking activities from AveXis, Cytokinetics, Italfarmaco, LiquidWeb, Srl and Novartis Pharma AG. He receives or he has received research support from the Italian Ministry of Health, AriSla, and E‐Rare Joint Translational Call. He is on the Editorial Board of Amyotrophic Lateral Sclerosis and Frontotemproal Degeneration, European Neurology, American Journal of Neurodegenerative Disease and Frontiers in Neurology. Nicola Ticozzi received compensation for consulting services from Italfarmaco, Biogen, Amylyx Pharmaceutical and Zambon Biotech SA. He received research funding from the Italian Ministry of Health and AriSLA. He is associate editor of Frontiers in Aging Neuroscience.
EPO‐133
Slow responders instead of late responders: Assessing the time to response to anti‐CGRP/R monoclonal antibodies
L. Iannone 1; A. Burgalassi2; A. Boccalini2; F. De Cesaris2; G. Vigani1; M. Romozzi3; C. Vollono3; P. Calabresi3; P. Geppetti1; A. Chiarugi1
1Section of Clinical Pharmacology and Oncology, Department of Health Sciences, University of Florence, Florence, Italy; 2Headache Center and Clinical Pharmacology Unit, Careggi University Hospital, Florence, Italy; 3Dipartimento Universitario di Neuroscienze, University Cattolica del Sacro Cuore, Rome, Italy
Background and Aims: To evaluated whether late responders to anti‐CGRP mAbs (achieving response between 3 and 6 months) are actually slow responders, namely patients who already achieve a clinically meaningful response at 3 months and improve over time.
Methods: We performed a prospective analysis on outpatients that started treatment, with a potential 6‐month follow‐up. Based on studies on late responders, response was defined as a ≥50% reduction in MHDs at 3 and 6 months. The response rate was then evaluated using different intervals (0–9; 10–19; 20–29; 30–49; ≥50%) to assess responses at three months. The primary outcomes were the number of potential late responders and to evaluate how many patients defined as late responders have a response ≥30% at three months (slow responders).
Results: We include 332 patients and among them 283 (85.2%) continue treatment for six months. Responders were 63.6% (180/283) at six months. In particular, 40 (14.1%) patients not responders at three months achieve response status at six months, 140 (49.5%) persisted in response, 77 (27.2%) continued to be not responders and 26 (9.2%) lost the responder status. However, among the 40 patients defined as late responders, 21 (47.5%) already achieved a response ≥30% at three months with 14 (35.0%) of them with a 40–49% response.
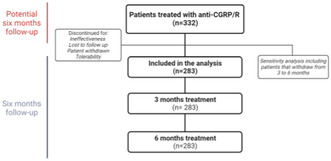
Flowchart of patients’ selection
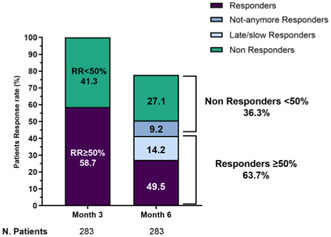
Responder rate variation from 3 to 6 months of treatment

Patients’ demographic and clinical features at baseline
Conclusion: The majority of patients designed as late responders are instead slow responders, starting a meaningful response to anti‐CGRP at three months and improving over time. Nevertheless, to maximize response, we recommend evaluating the treatment after a minimum of three to six months.
Disclosure: P.G.: received personal fees from Allergan, Eli Lilly, Novartis, Amgen, TEVA; Grants from Amgen, TEVA, Eli‐Lilly, Allergan, Chiesi; Scientific Advisory Board, Endosome Therapeutics; Founding scientist of FloNext srl, Spinoff of the University of Florence. F.D.C. received personal fees from TEVA, Eli Lilly, Novartis, Abbvie. L.F.I. received personal fees from TEVA, Eli Lilly, Pfizer, Abbvie, Lundbeck. Other authors have no conflicting interests.
EPO‐134
POTS and autoimmune conditions as predictors of vestibular migraine
M. Villar‐Martinez; S. Cheung; M. David; G. Peter J
Wolfson Sensory, Pain and Regeneration Centre, IoPPN, London, UK
Background and Aims: The vestibular migraine phenotype (VM) presents with vertigo/dizziness as a prominent non‐headache symptom. Autoimmune conditions, such as rheumatoid arthritis or psoriasis, are potentially comorbid and may have a genotypic association with migraine. Cranial autonomic symptoms in migraine has been described and could be a protective mechanism in patients with severe symptoms. Dysautonomic symptoms could correlate with chronification of headache in patients with POTS. Our aim was to search for potential comorbidities that could predict a “dizzy” phenotype.
Methods: Cross‐sectional study and clinical evaluation of migraine patients on the headache, neuro‐otology and general neurology clinics at King's College Hospital and Charing Cross Hospital in London; February 2020 to July 2023. Predictors: sex, the presence of Postural Orthostatic Tachycardia syndrome (POTS), hypermobility, inflammatory/autoimmune and cutaneous conditions such as urticaria. Dependent variable: migraine type. SPSS 28 and generalised linear model with negative binomial‐logit function were used.
Results: Age and biological sex were similar among migraine types. Of 525 cases; 185 had a diagnosis of vestibular migraine and 340 chronic migraine. Significant predictors of vestibular migraine: POTS (B = 1.08, p = 0.045) and autoimmune conditions (B = 0.53, p = 0.01). The rest of the predictors were not significant.
Conclusion: Dysautonomic conditions, such as POTS and the presence of autoimmune disorders, could predispose to a vestibular phenotype of migraine. Patients with the vestibular migraine phenotype may present a more dysfunctional autonomic nervous system with not only cranial, but also systemic symptoms.
Disclosure: Nothing to disclose.
EPO‐135
Is transcranial direct current stimulation effective as add‐on therapy to monoclonal antibodies anti‐CGRP in migraine?
F. De Santis 1; C. Rosignoli1; R. Ornello1; A. D'Atri1; F. Salfi1; D. Corigliano2; R. De Icco3; V. Grillo3; M. Corrado3; F. Bighiani3; G. Vaghi3; G. Sances3; M. Ferrara1; C. Tassorelli3; S. Sacco1
1Department of Biotechnological and Applied Clinical Sciences, University of L'Aquila, L'Aquila, Italy; 2Department of Psychology, University of Rome Sapienza, Rome, Italy; 3Department of Brain and Behavioral Sciences, University of Pavia, Pavia, Italy
Background and Aims: Transcranial direct current stimulation (tDCS) is a non‐invasive central neuromodulation technique with potential effectiveness in migraine, while monoclonal antibodies acting on the calcitonin gene‐related peptide pathway (CGRP‐MAbs) act peripherally. We aimed to assess whether tDCS, as a synergic add‐on, can enhance migraine prevention or affect cortical excitability.
Methods: TACTIC (NCT05161871) is a randomized, double‐blind, multicenter, sham‐controlled trial including patients with migraine on CGRP‐MAbs treatment, with residual monthly migraine days (MMD) ≥8. After 5‐day of tDCS bilateral occipital‐cathodal and frontal‐anodal stimulation (20‐minutes sham/active sessions) we followed‐up patients for 28 days. We recorded 64‐channel EEG at day 1 (pre‐stimulation) and day 5. We analyzed change in MMDs, clinical scales, and EEG spectral changes in the delta (2–4 Hz), theta (5–7 Hz), alpha (8–12 Hz) and beta‐bands (13–30 Hz) through two‐way mixed‐design ANOVAs with Session (baseline vs. follow‐up), as within‐subjects factor, and Treatment (Sham vs. Active) as between‐subject factor.
Results: We included 29 patients (median age = 48.0 [Interquartile‐Range 38–56], 92.0% female), 15 active session and 14 sham. We found no significant interaction between Session and Treatment. However, explorative post‐hoc t‐test showed that only in the active group tDCS led to a decrease in MMDs (mean difference = 4.00, standard error (SE) = 1.52, p = 0.014). Moreover, a noteworthy enhancement was observed in the HIT6 scale for both active (p = 0.005) and sham (p = 0.003) groups. tDCS decreased the occipital alpha‐ power and the frontal delta‐power only in the active stimulation group (both p < 0.050).
Conclusion: Centrally acting tDCS, as add‐on therapy to peripherally acting CGRP‐MAbs, has a significant preventive benefit on migraine associated with changed basal cortical activity on stimulated areas.
Disclosure: Nothing to disclose.
Movement disorders 1
EPO‐136
Plasma pTAU levels can discriminate HC, PD, PDD, DLB and AD patients
A. Lupini 1; A. Pilotto1; N. Ashton2; B. Battaglio1; E. Cottini1; C. Zatti1; C. Trasciatti1; I. Grossi3; A. Salvi3; G. De Petro3; M. Pizzi4; A. Canale5; K. Blennow6; H. Zetterberg7
1Neurology Unit, Department of Clinical and Experimental Sciences, University of Brescia, Brescia, Italy; 2Department of Psychiatry and Neurochemistry, Institute of Neuroscience and Physiology, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 3Division of Biology and Genetics, Department of Molecular and Translational Medicine, University of Brescia, Brescia, Italy; 4Division of Pharmacology, Department of Molecular and Translational Medicine, University of Brescia, Brescia, Italy; 5Department of Statistical Sciences, University of Padova, Padova, Italy; 6Clinical Neurochemistry Laboratory Sahlgrenska University Hospital, Mölndal, Sweden, 710 Department of Neurodegenerative Disease, UCL Institute of Neurology, London, UK
Background and Aims: plasma biomarkers are a promising field of research in neurodegenerative diseases, both oriented to diagnostic and therapeutic implications. Many patients with PD dementia or DLB have an AD‐pathology overlap. In this study, we seek to explore the usefulness of plasma biomarkers in distinguishing between healthy controls, PD, DLB, PDD, and AD patients.
Methods: plasma PTau181, PTau231, Aβ1‐40, Aβ1‐42, GFAP and NfL concentrations were measured by Single molecule array (Simoa) technology in healthy controls (HC) and consecutive PD and AD patients who underwent an extensive motor and non‐motor assessment. We established a cut‐off in pTau181 and pTau231 levels based on their average values in patients with AD pathology. We compared clinical and demographic variables between normal and abnormal pTAU groups.
Results: One hundred fifty‐three PD patients, thirty‐two PDD, forty‐two DLB, sixteen AD and ninety‐five age matched HC entered the analyses. The percentage of patients with abnormal pTAU levels increases from HCs to PDs but especially in patients with DLB and PDD. When considering only alpha‐synucleinopathies, the group with higher PTau231 showed lower MMSE scores at baseline.
Conclusion: The present findings confirm the potential utility of plasma AD biomarkers to differentiate healthy controls from PD patients and more importantly to separate PD cognitive unimpaired patients from patients with DLB or PDD.
Disclosure: Andrea Pilotto served in the advisory board of Z‐cube (technology division of Zambon pharmaceuticals); he received honoraria from Z‐cube s.r.l., Biomarin, Zambon, Nutricia and Chiesi pharmaceuticals. He received research support from Vitaflo Germany and Zambon Italy. Henrik Zetterberg has served at scientific advisory boards and/or as a consultant for Abbvie, Acumen, Alector, Alzinova, ALZPath, Annexon, Apellis, Artery Therapeutics, AZTherapies, CogRx, Denali, Eisai, Nervgen, Novo Nordisk, Optoceutics, Passage Bio, Pinteon Therapeutics, Prothena, Red Abbey Labs, reMYND, Roche, Samumed, Siemens Healthineers, Triplet Therapeutics, and Wave, has given lectures in symposia sponsored by Cellectricon, Fujirebio, Alzecure, Biogen, and Roche, and is a co‐founder of Brain Biomarker Solutions in Gothenburg AB (BBS), which is a part of the GU Ventures Incubator Program (outside submitted work). Alessandro Padovani is consultant and served on the scientific advisory board of GE Healthcare, Eli‐Lilly and Actelion Ltd Pharmaceuticals, received speaker honoraria from Nutricia, PIAM, Lansgstone Technology, GE Healthcare, Lilly, UCB Pharma and Chiesi Pharmaceuticals. He is founded by Grant of Ministry of University (MURST).
EPO‐137
Longitudinal impact of vascular risk factors on progression and disability in Parkinson's disease
A. Lupini 1; A. Pilotto2; M. Catania1; C. Zatti1; B. Battaglio1; F. Guarneri3; L. Bettoni3; S. Gipponi4; E. Cottini4; A. Padovani1
1Neurology Unit, Department of Clinical and Experimental Sciences, University of Brescia, Brescia, Italy; 2Laboratory of digital Neurology and biosensors, University of Brescia, Brescia, Italy; 3Hospital Central Pharmacy Unit, ASST University Hospital Spedali Civili Brescia, Brescia, Italy; 4Department of continuity of care and frailty, Neurology Unit, ASST Spedali Civili of Brescia, Brescia, Italy
Background and Aims: Vascular risk factors are common in the elder population in Western countries. Parkinson's disease incidence is increasing in the last years, along with population aging. Aim of the study was to address the impact of single and multiple vascular risk factors on cognitive and motor progression in patients with PD.
Methods: Consecutive Parkinson's disease patients underwent a comprehensive motor and non motor evaluation including baseline motor and non motor performances. A longitudinal motor and cognitive evaluation was performed with an average of 5 years of follow‐up for each patient. The impact of vascular risk factors on motor and cognitive progression was implemented by linear, COX regression and repeated measures analyses adjusting for the effect of age, motor severity and disease duration.
Results: forty‐hundred eighty six patient (62.1 % male) entered the study. 52–1% of patients had hypertension, while 21.2% had hypercholesterolemia, 17.3% had diabetes, and 27.2% had cardiac diseases. There was no correlation between vascular risk factors and neither cognitive nor motor impairment at baseline. Patients with diabetes and hypertension showed higher LEDD at follow up; patients with hypercholesterolemia had a higher incidence of falls, while patients with diabetes had a higher incidence of walking impairment at follow‐up.
Conclusion: vascular risk factors impact on disease progression and disability in PD. More studies are warranted to evaluate the causality and best management strategies to reduce the impact of vascular risk factors on PD progression and disability.
Disclosure: Nothing to disclose.
EPO‐138
The midbrain‐pons ratio as a marker for the vestibular stimulation effectiveness in the postural instability treatment
O. Alenikova; A. Chumak; G. Zobnina; S. Likhachev
Republican Research and Clinical Center of Neurology and Neurosurgery
Background and Aims: Axial symptoms associated with Parkinson's disease (PD), such as freezing of gait (FOG) and postural instability (PI) are frequently refractory to therapy. Due to the vestibular system deficiency participates in postural imbalance and gait disorders, vestibular galvanic stimulation (GVS) could become an effective neuromodulatory treatment for these symptoms. However, the effectiveness of GVS may vary depending on the neurodegeneration severity in brainstem locomotor centers, and midbrain‐pons ratio (MPR) may provide valuable information about change in these regions. Objective: To assess the GVS effectiveness on cVEMP parameters, FOG and PI severity depending on the MPR.
Methods: Participants included 34 PD and 30 age‐matched controls. Additionally to MRI‐based measurements, we assessed the cVEMP, FOG‐Q, TUG test and evaluated the PI severity before and after 12 GVS sessions.
Results: PD patients had longer of VEMP components latencies than controls, indicating slower vestibulospinal conduction. Nevertheless, there were no differences between groups in MRI measurements (table). GVS improved test scores and reduced N23 latency independent of MRI findings in PD patients. While the PI improvement depended on the MPR, and GVS was effective in PD patients with MPR >0.64 (figure).

TABLE Comparative assessment of the PD patients group and the control group
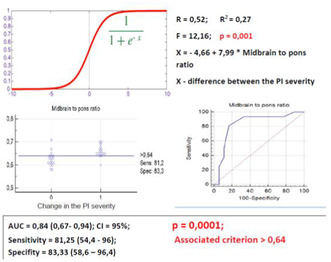
FIGURE Results of multiple regression and ROC analysis
Conclusion: GVS, acting on vestibular afferents, modifies the conflict between sensory systems and thereby reduces the severity of gait disorders. But the ability of GVS to reduce PI in PD probably depends more on morphometric features of the brainstem. Due to its high sensitivity and specificity, the MPR can be considered as a prognostic marker of the GVS effectiveness in the PI treatment.
Disclosure: Nothing to disclose.
EPO‐139
Amantadine improves executive and memory skills in patients with Parkinson's disease: A randomized controlled trial
A. Bougea 1; E. Angelopoulou1; V. Georgakopoulou2; Y. Değirmenci3; P. Zikos4
11st Department of Neurology, Medical School, National and Kapodistrian University of Athens, Eginition Hospital, Athens, Greece; 2COVID‐19 Unit, Department of Infectious Diseases, Laiko General Hospital, Athens, Greece; 3Head of Neurology Department, Istanbul Health and Technology University (ISTUN); 4Galatsi Center for Parkinson's & Memory Disorders Galatsiou Avenue 127, Galatsi, Athens, Greece
Background and Aims: Amantadine improves motor symptoms in patients with Parkinson disease (PD) as monotherapy or adjuvant therapy. However, data on cognitive functions are lacking. This Single blind randomized controlled study over 12 months investigated the effect of amantadine on PD cognition.
Methods: Mild cognitive impaired 35 PD patients (mean HY: 2), with amantadine 200 mg/day (100 mg twice a day) orally as monotherapy (Group A) and 30 PD patients without amantadine (only levodopa treatment Group B) were randomly enrolled. The data collected for each patient included: (1) verbal learning and memory (Hopkins Verbal Learning Test‐Revised immediate total recall across trials and delayed recall trial), (2) auditory working memory (Letter‐Number Sequencing subtest from the Wechsler Adult Intelligence Scale – III), (3) processing speed (Digit Symbol subtest from the Wechsler Adult Intelligence Scale‐Revised), (4) visuospatial working memory/switching (Trail Making Test, Part B), (5) semantic verbal fluency (animals), (6) phonemic verbal fluency (letters F‐A‐S or C‐F‐L), (7) visuospatial functioning (Benton Judgment of Line Orientation), 8)Depression (Geriatric Depression scale).
Results: The cognitive function improved progressively in 3‐, 6 and 12‐month treatment interval as shown by significant improvement on verbal short term (p < 0.001) and auditory working memory (p < 0.001) and visual working memory (p < 0.001) in Group A compared to Group B. Even after controlling for depression, disease duration, there are persistent differences in the above cognitive tests between the two groups over the time
Conclusion: Amantadine alone significantly improved memory and visual‐spatial skills in PD patients.
Disclosure: Nothing to disclose.
EPO‐140
Determination of clinical profile of patients with Parkinson's disease at 2‐year follow up with deep brain stimulation
A. Bougea 1; Y. Değirmenci2; E. Angelopoulou1; V. Georgakopoulou3; P. Zikos4
1Department of Neurology, Eginition Hospital, National and Kapodistrian University of Athens, Greece; 2Head of Neurology Department, Istanbul Health and Technology University (ISTUN); 3COVID‐19 Unit, Department of Infectious Diseases, Laiko General Hospital, Athens, Greece; 4Galatsi Center for Parkinson's & Memory Disorders Galatsiou Avenue 127, Galatsi, Athens, Greece
Background and Aims: Despite the beneficial effect of deep brain stimulation (DBS) on motor and non‐motor symptoms, the selection of Parkinson's disease (PD) patients is challenging. This study aims to develop a random forest (RF)‐based PD model to determine the postoperative clinical profile at 2 years follow‐up with DBS using motor and non‐ motor symptoms.
Methods: 130 PD subjects (76 male, 54 female; age at baseline: 56.24 ± 4.23) were evaluated in years 0 and 2 by the Unified Parkinson's Disease Rating Scale part III (UPDRS‐ III). Hours of “Off” and dyskinesia time (UPDRS‐IV), the Montreal Cognitive Assessment (MoCA), Geriatric Depression Scale (GDS), the Non‐Motor Symptoms Scale (NMSS), Hoehn/Yahr(HY) and PD questionnaire‐ 39(PD39). RF analysis, with 10000 trees, was used to combine both non‐motor and motor variables to determine motor outcome (UPDRS‐III year 2: 22.55 ± 12.22).
Results: The proper combination of motor and non‐motor measures significantly improved (p < 0.001) the prediction of outcome, reducing the RMSE (root‐mean‐square‐error) of predicting UPDRS‐III from 4.686567 to 4.04672 which signifies that the model was optimized quite well. Based on the "IncNodePurity", the factors of UPDRS‐III (year 2) were, in descending order of magnitude, UPDRSIII (year 0), disease duration (year 2), GDS (year 0), NMSS (year 2), Time Dyskinesia (year 0), PDQ39 (year 2) after the implementation of DBS.
Conclusion: In the new era of neuromodulation, these results are promising for accurate patient selection for DBS by artificial intelligence models.
Disclosure: Nothing to disclose.
EPO‐141
Phenotype's evolution of cervical dystonia (CD) in patients treated with Botulinum toxin
A. Trinchillo 1; N. Cuomo1; F. Habetswallner2; M. Esposito2
1Department of Neurosciences, Reproductive Sciences and Odontostomatology, “Federico II” University, Naples, Italy; 2Clinical Neurophysiology Unit, Cardarelli Hospital, Naples, Italy
Background and Aims: Cervical dystonia (CD) phenotypes may change over the years. Objective of the study is to evaluate how such phenotypes change in CD treated with botulinum toxin (BoNT). Finally, we aim to identify the time within those changes may occur, the most predisposed CD phenotypes and predisposing factors.
Methods: We divided idiopathic CD patients into two groups – switch YES/NO, collecting general clinical and demographic variables. We added to general clinical variables the duration of BoNT treatment, Tsui total scores and subscores – assessed at T0 – before BoNT start – and at T1 – switch time in the YES group or last visit in the NO group. The risk of switch was assessed by Kaplan Meyer curves and Cox regression analysis. Finally, Multivariate linear regressions were employed to assess if Tsui severity correlated with the switch.
Results: Among 100 patients (60 women) aged 47.9 years (SD 15.3) at CD onset, 37 experienced a phenotype switch, mostly in the first five years of BoNT treatment, YES and NO groups were comparable. Multivariate Cox Regression revealed the presence of laterocollis or rotatocollis at T0 as predictors of switch (respectively p = 0.01, HR = 3.5; p = 0.03, HR = 1.5). Multivariate linear regressions revealed that high Tsui subscores for the tilt and low Tsui total scores were risk factors for the switch (respectively p = 0.002, OR = 6; p = 0.03, OR = 0.8).
Conclusion: Latero and Rotatocollis are the CD phenotypes most predisposed to switch. Dystonias with a low degree of severity improve after treatment with botulinum toxin, changing to a different and even simpler phenotype.
Disclosure: Nothing to disclose.
EPO‐142
The long‐term response to botulinum toxin injections in patients with blepharospasm undergoing upper eyelid surgery
A. Trinchillo 1; N. Cuomo1; F. Habetswallner2; M. Esposito2
1Department of Neurosciences, Reproductive Sciences and Odontostomatology, “Federico II” University, Naples, Italy; 2Clinical Neurophysiology Unit, Cardarelli Hospital, Naples, Italy
Background and Aims: BACKGROUND Upper eyelid surgery (UES) is a therapeutical strategy used for those patients affected by blepharospasm (BSP) who either do not respond or experience a gradual decrease in responsiveness to botulinum toxin (BoNT) injections. Nevertheless, most of them need to restart with BoNT despite the intervention. AIM To evaluate the long‐term post‐surgical response to BoNT in patients with BSP and to identify predictive factors associated to treatment outcome.
Methods: We collected data of 60 BS patients, divided into two groups – blepharoplasty YES (8) and NO (52), collecting demographic – age, sex – and clinical data –disease duration, duration of the treatment with BoNT. Respective responses to injections – evaluated through the differences of both Jancovic Rating Scale and the Blepharospasm Disability Index pre and post BoNT (delta JRS and delta BSDI) just before their periodic three‐month injection and after 1 month from it – were compared. Finally, clinical and demographics variables were included in multivariate regression and correlation analyses to assess their impact on the long‐term response to injections.
Results: Patients who underwent UES had significantly lower delta at both scales, showing a poorer outcome after BoNT treatment. No variable was found to be associated with the response.
Conclusion: Our data seem to suggest that surgery does not improve response to BoNT injections on the long run. As such, UES could be considered as an efficacious treatment in BSP just if evaluated soon after its performing. Long‐term BSP management seems still difficult to be performed adequately and new therapeutical approaches are still needed.
Disclosure: The authors have nothing to disclose.
EPO‐143
Assessment of the deep brain stimulation efficiency for the tremor correction in Parkinson's disease: STN vs Vim
A. Buniak; S. Likhachev; U. Alexeyevets; V. Bayarchyk; T. Paulouskaya
Neurological Department, Neurosurgical Department, Republican Research and Clinical Center of Neurology and Neurosurgery, Minsk, Belarus
Background and Aims: Correcting severe tremor, one of the disabling symptoms in Parkinson's disease (PD), is the most difficult tasks for neurologists. If there is no effect from drug correction of severe tremor, neurosurgical treatment is used, including deep brain stimulation (DBS) of the ventralis intermedius thalamic nucleus (Vim) or subthalamic nucleus (STN). To evaluate the efficiency of DBS Vim vs STN for the tremor correction in PD patients.
Methods: We examined 72 (59–II stage, 13–III stage of H&Y.) PD patients during DBS. The main characteristics of patients are presented in the table (Fig. 1). In patients with DBS Vim, the primary symptom was disabling tremor. The tremor index (TI) consists of UPDRS scores 16, 20, 21. To assess the changes of drug therapy used LEDD.

FIGURE 1 Description PD patients before DBS
Results: The postoperative follow‐up period was up to 2 years. The score by III UPDRS in the off‐med decreased in patients with DBS STN ANOVA χ2 = 12.44, p < .00001 and DBS Vim ANOVA χ2 = 11.58, p = .00011(Fig 2). The TI in the off‐med period decreased in patients with DBS STN ANOVA χ2 = 14.68, p < .00001 and DBS Vim ANOVA χ2 = 4.51, p = .014 (Fig 3). The LEDD score in DBS STN was decreased ANOVA χ2 = 9.22, p < .000001, but not under DBS Vim ANOVA χ2 = 1.92, p = .15.

FIGURE 2 Changes of III part UPDRS in off‐med DBS STN vs DBS Vim up to 2 years
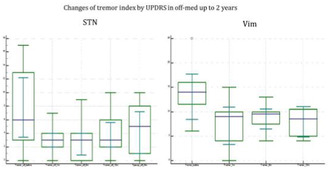
FIGURE 3 Changes of tremor index by UPDRS in off‐med DBS STN vs DBS Vim up to 2 years
Conclusion: The results indicate an improvement of tremor both by DBS STN and DBS Vim. To correct hypokinesia and rigidity during DBS Vim, patients should take levodopa at the correct dose.
Disclosure: Nothing to disclose.
EPO‐144
Pain and related factors in patients with Parkinson's disease
C. Alis 1 ; D. Selcuk Demirelli1; E. Ay2; G. Genc1
1Department of Neurology, Sisli Hamidiye Etfal Training and Research Hospital, Istanbul, Turkey; 2School of Medicine, Acibadem Mehmet Ali Aydinlar University, Istanbul, Turkey
Background and Aims: Pain is a common non‐motor symptom in Parkinson's disease (PD). We aimed to investigate pain frequency and pain‐related factors in PD.
Methods: We interviewed PD patients from our movement disorders unit to assess pain presence, categorising it into four types: musculoskeletal pain (MP), radicular or neuropathic pain (RNP), dystonia‐related pain (DRP), and central parkinsonian pain (CPP). We investigated demographic differences, General Anxiety Disorder‐7 (GAD‐7), Patient Health Questionnaire‐9 (PHQ‐9), EQ‐5D‐3L, MDS‐Unified Parkinson's Disease Rating Scale (MDS‐UPDRS) and Hoehn and Yahr scale (H&Y) scores, PD duration, PD drugs, and insomnia. Comparisons were made between patients with and without pain, and among those with different pain types.
Results: Ninety‐three patients (34 female, 59 male; median age: 66 years, IQR: 17) were included. Seventy‐five had pain (23 MP, 18 RNP, 12 DRP, 5 CPP, and 17 had a combination). No associations were found between pain and age, gender, GAD‐7, PHQ‐9, MDS‐UPDRS, H&Y scores, PD duration, PD drugs, and insomnia. However, EQ‐5D‐3L scores were higher in patients with pain (p = 0.019). Among different pain types, no relationships were identified regarding age, PHQ‐9, MDS‐UPDRS and H&Y scores, PD drugs, and insomnia. RNP correlated with longer PD duration (p = 0.01), MP with shorter PD duration (p = 0.04). MP was less common in males (p = 0.016), and anxiety was more prevalent in CPP patients (p = 0.008).
Conclusion: Pain impairs PD patients' quality of life, and longer PD duration correlates with increased RNP. Anxiety correlates with CPP, suggesting a potential link between anxiety‐control networks and CPP. Further studies are needed to support this hypothesis.
Disclosure: Nothing to disclose.
EPO‐145
Neurology survey on referral practices and perception of functional neurosurgery solutions in essential tremor in Europe
C. Ferrer 1 ; C. Tengelin1; P. Crivelli1; K. Gant2; A. Grinspan2
1Insightec Europe GmbH, Munich, Germany; 2Insightec. Inc, Miami, USA
Background and Aims: Functional neurosurgery for treatment of essential tremor (ET) has evolved in recent years. Magnetic resonance–guided focused ultrasound (MRgFUS) was introduced as an alternative neurosurgery modality. We investigated changes in referral patterns and familiarity with functional neurosurgery among European neurologists.
Methods: An anonymised web survey was conducted between 16‐01‐23 and 24‐02‐23. Relevant privacy legislation on personal data protection (GDPR 2016/679) and professional guidelines were followed. General neurologists (GN) and movement disorder neurologists (MDN) were interviewed about the ET pathway and their experience and perception of functional neurosurgery.
Results: The survey was answered by 224 neurologists (68 MDN, 156 GN). Patients came to the neurologist's attention mainly via their general practitioner (GP) and the patient's own initiative (up to 33% in Italy). Disease was mainly severe in those referred to the neurologist (approximately 55%) (Figure 1). Most were managed directly by the neurologist, without referral to another neurologist or centre (<18%); when the neurologist referred the patient to another centre, disease was generally severe (approximately 70%) (Figure 2). Most neurologists were familiar with deep brain stimulation (DBS [96.4%]), radiofrequency (RF [72.8%]), and gamma‐knife thalamotomy (GKT [79.3%]). Fewer were familiar with MRgFUS (67.5%) (Figure 3).
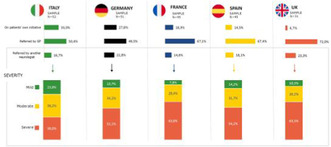
FIGURE 1 Origin and severity of essential tremor patients referred to general and movement disorder neurologists in Europe (Italy, Germany, France, Spain, and the UK). The sample number of neurologists per country is reported.

FIGURE 2 Distribution and management of essential tremor patients by and between neurologists in Europe (Italy, Germany, France, Spain, and the UK). The sample number of neurologists per country is reported.

FIGURE 3 Reported level of knowledge of non‐pharmacological therapies among both general and movement disorder neurologists. The sample number of neurologists is reported. Familiarity is defined as the overlap between the 3 highest levels of knowledge.
Conclusion: Referral of ET patients remains variable and is mainly via the GP or the patient's own initiative. The most common profile is severe disease. Despite recent inclusion in national/international guidelines, MRgFUS remains the least familiar option for neurologists, followed by RF, GKT, and DBS. Further study is necessary to explain the low referral rate (<18%).
Disclosure: The authors are all employees of Insightec. To carry out the survey, support was provided by Stethos Srl, Italy, Milan. Writing assistance was provided by Content Ed Net, Madrid, Spain. The responses were used for market research purposes.
EPO‐146
General and movement disorder neurologists survey on prescription and perception of MRgFUS in Europe
C. Ferrer 1; C. Tengelin1; P. Crivelli1; K. Gant2; A. Grinspan2
1Insightec Europe GmbH, Munich, Germany; 2Insightec. Inc, Miami, USA
Background and Aims: Magnetic resonance–guided focused ultrasound (MRgFUS) emerged in the 2010s and is now a recommended neurosurgery alternative for essential tremor (ET). The increased presence of MRgFUS means that perception and potential application in ET may have changed. We investigated changes in perception of MRgFUS among European neurologists.
Methods: An anonymised web survey was conducted between 16‐01‐23 and 24‐02‐23. Relevant data privacy legislation and guidelines were followed. Both general neurologists (GN) and movement disorder neurologists (MDN) were asked about the positioning of MRgFUS, barriers to adoption, and medical education.
Results: The survey was completed by 68 MDN and 156 GN. Approximately two‐thirds of patients had severe ET. Quality of life was poor, and many patients had not responded to previous therapy (Figure 1). Most neurologists (>70%) were satisfied with the effects of MRgFUS on patient management. The main conditions for extending referral were access to protocols and referral criteria. (Figure 2). Most felt that MRgFUS could be extended to a wider range of patients by enhancing communication with neurologists, creating access channels between MRgFUS centres and other centres, and offering staged‐bilateral treatment. The recommended educational content to extend use of MRgFUS includes clinical efficacy data, safety‐tolerability data, and side effects, as well as explanation of the technique/procedure (Figure 3).

FIGURE 1 Severity and main characteristics of essential tremor patients prescribed MRgFUS by neurologists in Europe (Italy, Germany, France, Spain, and the UK). The sample number of neurologists per country is reported.
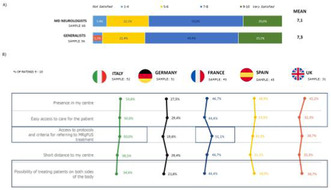
FIGURE 2 A) Level of satisfaction for post‐MRgFUS patient management among general and movement disorder neurologists. B) Conditions for extension of MRgFUS to more patients.
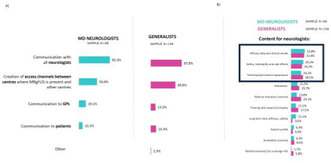
FIGURE 3 A) Channels of communication for extension of MRgFUS to more patients. B) Content to be included in communications on MRgFUS. The sample number of neurologists is reported. Outcomes are reported for general and movement disorder neurologists.
Conclusion: In Europe, MRgFUS is prescribed mainly in severe ET. Satisfaction was high. More widespread adoption depends on better access to centres, well‐defined referral criteria, and the possibility of staged‐bilateral treatment. Further education on MRgFUS is necessary.
Disclosure: The authors are all employees of Insightec. To carry out the survey, support was provided by Stethos Srl, Italy, Milan. Writing assistance was provided by Content Ed Net, Madrid, Spain. The responses were used for market research purposes.
EPO‐147
Use of the MNCD classification/staging in advanced Parkinson's disease patients treated with a device‐aided therapy
D. Santos‐García 1; L. López‐Manzanares2; I. Muro2; P. Lorenzo2; R. García‐Ramos3; C. Morata‐Martínez4; R. Baviera‐Muñoz4; I. Martínez‐Torres4; M. Álvarez‐Sauco5; J. Suárez‐Muñoz6; J. Martínez Castrillo7; A. Perona8; J. Salom9; I. Legarda10; M. Valero‐García10; E. Cubo11; N. López‐Ariztegui12; D. Alonso‐Modino13; R. Espinosa14; M. Mata15
1CHUAC (Complejo Hospitalario Universitario de A Coruña), A Coruña, Spain; 2Hospital Universitario La Princesa, Madrid, Spain; 3Hospital Clínico Universitario San Carlos, Madrid, Spain; 4Hospital Universitario la Fe, Valencia, Spain; 5Hospital General Universitario de Elche, Spain; 6Hospital Dr. Negrín, Las Palmas de Gran Canaria, Spain; 7Hospital Universitario Ramón y Cajal, Madrid, Spain; 8Complejo Hospitalario Universitario de Albacete, Spain; 9Hospital Clínico Universitario de Valencia, Spain, 10Hospital Universitario Son Espases, Palma de Mallorca, Spain, 11Hospital Universitario de Burgos, Spain, 12Hospital Universitario de Toledo, Spain, 13Hospital Universitario de la Candelaria, Santa Cruz de Tenerife, Spain, 14Hospital Universitario de Jerez, Spain, 15Hospital Infanta Sofía, Madrid, Spain
Background and Aims: Staging Parkinson´s disease (PD) with a novel simple classification called MNCD, based on 4 axes (Motor; Non‐motor; Cognition; Dependency) and 5 stages, correlated with disease severity and patients´ quality of life and caregivers´ strain and burden (1,2). Our aim was to apply the MNCD classification in patients treated with levodopa‐entacapone‐carbidopa intestinal gel (LECIG) infusion.
Methods: A multicenter observational retrospective study of the first patients to start LECIG in Spain was performed (LECIPARK). The MNCD total score (from 0 to 12) and MNCD stages (from 1 to 5) were collected by the neurologist at V0 (before starting LECIG) and V2 (follow‐up visit). Wilcoxon's signed rank and Marginal Homogeneity tests were applied to compare changes from V0 to V2.
Results: Forty‐five PD patients (55.3% males; 69.6 ± 10 years old) with a mean disease duration of 13.9 ± 6.4 years were included. The mean treatment duration (V2) was 132.2 ± 81.3 days (range, 10–302). At V0, patients were classified as in stage 2 (31.9%), 3 (44.7%) or 4 (23.4%). The frequency of patients in stage 4 decreased to 10.6% at V2 (p = 0.007) (Figure 1A). The MNCD total score decreased from 6.6 ± 1.8 at V0 to 5.4 ± 2.1 at V2 (p < 0.0001). From V0 to V2, motor and non‐motor symptoms burden decreased and autonomy for activities of daily‐living improved (Figure 1B and 2).
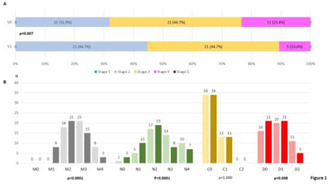
FIGURE 1 A. Frequency of different MNCD stages (from 1 to 5) at V0 (V0; pre‐LECIG) compared to at V2 (follow‐up visit; 132.2 ± 81.3 days after starting LECIG) (p = 0.007). B. Number of patients with each score of the MNCD classification (M, N, C and D) at

FIGURE 2 Change from the baseline (V0; pre‐LECIG) to the follow‐up visit (V2) in the MNCD total score (from 0 to 12), M and N scores (from 0 to 4), and C and D scores (from 0 to 2). Wilcoxon's signed rank tests was applied. The bars represent mean ± stan
Conclusion: The MNCD classification could be useful to classify advanced PD patients and to monitor the response to a device‐aided therapy.
Disclosure: The authors report no conflict of interest.
EPO‐148
Exploring the distinct effect of onset age and caudate denervation on cognitive deficits in early PD
G. Palermo 1; S. Giannoni1; L. Tommasini1; G. Bellini1; D. Frosini1; G. Aghakhanyan2; R. Morganti3; D. Volterrani2; N. Pavese4; R. Ceravolo1
1Center for Neurodegenerative Diseases – Parkinson's Disease and Movement Disorders, Unit of Neurology, Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy; 2Regional Center of Nuclear Medicine, Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy; 3Section of Statistics, University of Pisa, Pisa, Italy; 4Clinical Ageing Research Unit, Translational and Clinical Research Institute, Newcastle University, Newcastle upon Tyne, UK
Background and Aims: Older age at onset and baseline caudate dopaminergic denervation are recognized risk factors for cognitive impairment in Parkinson's disease (PD), posing challenges in identifying their relative contribution to cognitive outcomes. The objective of this study was to assess the distinct contribution of age at onset and baseline caudate dopaminergic binding to the early cognitive deficits in PD patients.
Methods: We examined the relationship between baseline dopaminergic striatal dysfunction (measured using [123I]FP‐CIT SPECT, age at disease onset and neuropsychological performance in 126 drug‐naive PD patients, utilizing putaminal and caudate binding values of 77 healthy controls (HC) for a comparative exploration of age‐dependent loss of DAT availability. Additionally, we investigated whether age at onset and caudate DAT binding could independently predict cognitive changes over a median of 7‐year follow‐up.
Results: [123I]FP‐CIT‐SPECT binding values had a significant negative correlation with age in both PD and HC, but in PD, aging was linked with a steeper slope for the caudate than the putamen. Older age at onset and lower caudate uptake were associated with worse global cognitive function and performance in specific neuropsychological tests at baseline and demonstrated to be significant independent predictors of cognitive dysfunction at follow‐up.
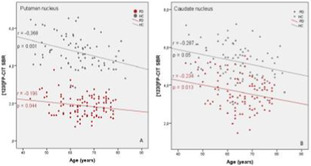
FIGURE 1 Effects of age: comparison of [123I]FP‐CIT binding values between PD and HC in the putamen (A) and caudate (B)
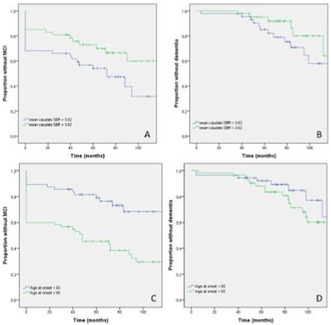
FIGURE 2 The survival curve determined using the Kaplan‐Meier for cognitive decline in our patient cohort according to baseline [123I]FP‐CIT SPECT binding values (A and B) and age at the onset of PD (C and D)
Conclusion: Our findings confirm a differential age effect on [123I]FP‐CIT binding in the striatal subregions of denovo PD patients. Notably, we found less age‐related attrition of dopaminergic binding in the putamen than in the caudate, reflecting likely the superimposition of putaminal compensatory mechanisms and an increased predisposition of old onset PD patients to develop cognitive disturbances.
Disclosure: The authors declare that there are no financial disclosures to report concerning the research related to this abstract.
EPO‐149
Vestibular and saccadic abnormalities in Parkinson's disease patients: Possible marker of neurodegenerative burdern?
G. Di Rauso 1; A. Castellucci2; F. Cavallieri3; S. Grisanti1; V. Fioravanti3; E. Monfrini4; G. Toschi3; J. Rossi1; A. Tozzi5; G. Ferrulli5; R. Sabadini3; A. Scaglioni6; A. Di Fonzo4; A. Ghidini2; F. Valzania3
1Clinical and Experimental Medicine PhD Program, University of Modena and Reggio Emilia, Modena, Italy; 2Otolaryngology Unit, Azienda USL‐IRCCS di Reggio Emilia, Reggio Emilia, Italy; 3Neurology Unit, Neuromotor & Rehabilitation Department, Azienda USL‐IRCCS di Reggio Emilia, Reggio Emilia, Italy; 4Neurology Unit, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy; 5Otorhinolaryngology‐Head and Neck Surgery Department, University Hospital of Modena, Modena, Italy; 6Centro S. Maria ai Servi, Fondazione Don Gnocchi, Parma, Italy
Background and Aims: Vestibular dysfunction has been suggested as possible non‐motor symptom in Parkinson's disease (PD), however so far data are still lacking in literature. Moreover, saccadic eye movements have been studied in PD with mixed results. The aim of our study is to assess vestibulo‐ocular reflex gain and voluntary saccade eye movements in PD patients exploring possible correlation between vestibular and saccadic variables and demographic and clinical features. Secondary aim is to compare these variables in GBA1‐PD and non‐mutated PD (NM‐PD) subgroups.
Methods: A consecutive cohort of GBA1‐PD patients has been paired for age, sex, disease duration, Hoehn & Yahr stage, and Charlson Comorbidity Index with a cohort of consecutive NM‐PD. Patients underwent clinical neurological assessment (MDS‐UPDRS total scores and subscores, the Montreal Cognitive Assessment scale (MoCA)), the video head impulse test (vHIT) and saccadic instrumental assessment.
Results: 40 PD patients were included in this study: 20 GBA1‐PD and 20 NM‐PD. Bilateral saccadic latency directly correlated with age (p < .05), disease duration (p < .001) and PIGD subscore (p < .001), while it negatively correlated with MoCA score (p < .05). The bilateral vHIT gain of the lateral semicircular canal directly correlated with disease duration (p < .05), while the gain of the posterior semicircular canal negatively correlated with rigidity subscore (p < .05). No differences were found in vestibular and saccadic variables between GBA1‐PD and NM‐PD.
Conclusion: Our results highlight that vestibular and saccadic abnormalities may be associated with specific clinical features in PD. Particularly, saccadic latency could represent a marker of neurodegenerative burden, correlating with age, disease duration and axial and cognitive impairment.
Disclosure: The authors have no conflicts of interest to declare that are relevant to the content of this abstract.
EPO‐150
Atypical presentations of Huntington disease‐like 2 in South African individuals
H. Narotam Jeena 1; M. Guttman2; L. van Hillegondsberg1; R. van Coller3; A. Krause4; J. Carr1
1Division of Neurology, Department of Medicine, University of Stellenbosch, Cape Town, South Africa; 2Centre for Movement Disorders, Markham Ontario, Division of Neurology, University of Toronto, Canada; 3Department of Neurology, University of Pretoria, South Africa; 4Division of Human Genetics, National Health Laboratory Service and School of Pathology, Faculty of Health Sciences, University of Witwatersrand, Johannesburg, South Africa
Background and Aims: Huntington's Disease Like 2 (HDL2) is a neurodegenerative disorder, described as being similar to HD with respect to phenotypic, radiologic and pathologic features. HDL2 only affects individuals of African ancestry. Affected individuals have 40–59 triplet repeats. We describe the phenotypic variability of HDL2 in a group of mixed ancestry individuals from South Africa.
Methods: Eight patients were assessed with the Unified HD Rating Scale (UHDRS), Montreal Cognitive Assessment (MoCA) tool, MR brain imaging, and analysis of repeat size.

Pedigrees of the three families studied.
Results: Cognitive domains were more severely affected than motor domains. Neuropsychiatric symptoms were common in all, evident as behavioural change, memory impairment, depression, anxiety, and/or hallucinations. MoCA scores reflected impairments across all domains, although orientation and memory were less severely affected. UHDRS motor scores were notable for bradykinesia. Tremor and dystonia were also prominent motor symptoms; only one patient had marked chorea. Repeat lengths ranged from 45 to 63 and were inversely related to age at onset (AAO). We report two unique cases of juvenile onset HDL2, noting that an AAO younger than 20 years has not been previously documented.
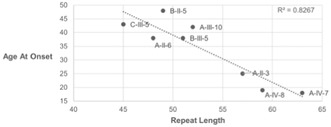
Age at onset and corresponding repeat length
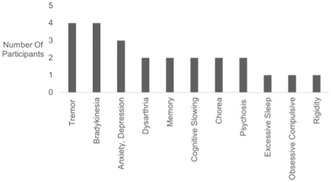
Symptoms at presentation
Conclusion: It is important for clinicians to be aware that individuals with HDL2 may present with severe and rapidly progressive cognitive and behavioural impairments, with variable degree of motor deficit and even absent chorea. The atypical HDL2 phenotype in this South African group of mixed ancestry is likely related to large repeat sizes and may represent a forme fruste of the Westphal variant seen in Huntington disease.
Disclosure: Nothing to disclose.
Movement disorders 2
EPO‐151
EEG microstate abnormalities in prodromal Lewy body diseases
D. Ondráček 1; M. Lamoš2; L. Brabenec2; K. Mitterová2; I. Rektorová3
1Brain and Mind Research Program, CEITEC, Masaryk University, Brno, Czechia + Faculty of Medicine, Masaryk University, Brno, Czechia; 2Brain and Mind Research Program, CEITEC, Masaryk University, Brno, Czechia; 3Brain and Mind Research Program, CEITEC, Masaryk University, Brno, Czechia + First Department of Neurology, Faculty of Medicine, Masaryk University and St. Anne's University Hospital, Brno, Czechia
Background and Aims: Described EEG patterns may serve as diagnostic and prognostic biomarkers for prodromal dementia with Lewy bodies (DLB). While spectral frequency analysis is used to evaluate EEG patterns, EEG microstates (MS) provide temporal and spatial characteristics. We aimed at elucidating early changes in network dynamics across spectrum of healthy controls (HC), prodromal DLB and at‐risk population using both EEG patterns and MS assessment.
Methods: 120 cognitive and dopaminergic medication‐naïve subjects with or without core and supportive clinical features of prodromal DLB +‐ presence of mild cognitive impairment underwent a 5‐minute recording of high‐density resting state scalp EEG. Participants were sorted based on their EEG patterns into groups: pattern 1 (normal EEG), pattern 2 (early DLB) and pattern 5 (advanced DLB). EEG microstates were analyzed using k‐means approach and temporal parameters were calculated.
Results: Results revealed higher mean duration (p < 0.001 and p = 0.005) and higher time coverage (TC) (p = 0.004 and p = 0.004) of the MS C, and lower TC (p = 0.003 and p < 0.001) and segment density (p < 0.001 and p < 0.001) of MS A in EEG pattern 1 compared to pattern 2 and 5, respectively. No significant differences between pattern 2 and 5.
Conclusion: MS A involves temporal cortices and represents sensory (auditory, visual) and arousal networks while MS C anterior cingulate and insular cortices representing salience network. Our results support early engagement of anterior insular cortices in prodromal DLB which reflects deficits in executive, autonomic, visual and affective/behavioral functions while abnormally enhanced involvement of the sensory/arousal network is related to cognitive fluctuations, and/or illusions/hallucinations in early DLB.
Disclosure: No disclosure.
EPO‐152
Functional Neurological Disorders (FND): Experience at a tertiary hospital in Madrid
A. Suárez Plaza; Á. Gutiérrez Viedma; C. García Campos; P. García Ruiz Espiga; J. Del Val Fernández; C. Feliz Feliz; R. Cutillas Ruiz; M. Machío Castelló; J. Serratosa Fernández; B. González Giraldez; A. Cascón Pinto; L. Salgado Calzada; M. Arias Villarán
Hospital Universitario Fundación Jiménez Díaz, Madrid, Spain
Background and Aims: Diagnosing functional neurological disorders (FND) might be daunting. Although the prevalence of overlapping structural neurological pathology in FNDs has been previously stated, the relationship between both is yet to be fully understood. Our aim was to describe all diagnoses reached at our FND‐Unit and analyze its characteristics.
Methods: Prospective observational study of all patients referred to an FND‐Unit, May‐2022 to December‐2023.
Results: 154 patients (72.7% female, median age 41 years) were included. 89.0% were diagnosed with FND, 11,0% received alternative diagnoses (non‐FND). The most prevalent reason for referral were syncopes (22.1%) and gait abnormalities (20.1%). Amongst the alternative diagnoses, the most common clinical presentation was sensory disturbances (64.7%).The most prevalent alternative diagnosis was restless legs syndrome (RLS) (44.4%), followed by peripheral neuropathy (33.3%). 3.7% of FND confirmed cases presented an overlapping RLS (FND/RLS). The resulting prevalence of RLS was 8.4%. 46.2% of RLS patients presented exclusively sensory symptoms, and most of them (87.5%) were non‐FND/RLS (p = 0.047). Within the FND/RLS group, median age was significantly lower (30.0 versus 49.5 years, p = 0.021) and median time to diagnosis after symptom onset was longer (60 versus 10 months, p = 0.08). No other differences were found.
Conclusion: The possibility of diagnostic errors at a FND‐Unit is relevant. The most frequent misdiagnosis was RLS, which also commonly overlapped with FND. Age, solely sensory symptoms, and time to diagnosis might help distinguish FND/RLS from non‐FND/RLS.
Disclosure: Nothing to disclose.
EPO‐153
Novel CACNA1A mutation associated with cerebellar ataxia and mild cognitive impairment in a Czech family; a case report
A. Afifi 1; M. Nevrlý1; Z. Mušová2; P. Hedvičáková2; K. Menšíková1; P. Kaňovský1
1Department of Neurology, University Hospital Olomouc, Czechia; 2Department of Biology and Medical Genetics, Second Faculty of Medicine, Charles University and University Hospital Motol, Prague, Czechia
Background and Aims: Spinocerebellar ataxias (SCA) are a group of heterogenous neurodegenerative hereditary disorders characterized by progressive loss of balance and coordination, as well as other distinguishing symptoms that vary with the particular type and the involved genetic defect. Pathogenic variants in CACNA1A gene have been implicated in autosomal dominant hereditary spinocerebellar ataxia 6, episodic ataxia type 2, familiar hemiplegic migraine, and infantile epileptic encephalopathy 42.
Methods: Index case, 43‐year‐old patient, presented with progressive cerebellar ataxic gait clinically manifesting at age 41, horizontal nystagmus and mild cognitive impairment. Noteworthy from his history; he suffered epileptic seizures from ages 3–16, and his biological mother developed similar gait disorder since age 44. Her examination showed cerebellar ataxic gait, horizontal nystagmus with saccadic intrusions, ataxic dysarthria, intentional tremor and mild cognitive impairment. Both patients had global cerebellar atrophy on MRI. Patients initially tested negative for most common SCAs (SCA1‐3 and SCA6‐7). Subsequently, CACNA1A gene was analysed using new generation sequencing and bioinformatic analysis.
Results: In both patients, molecular genetic examination confirmed the presence of the heterozygous variant c.1672‐1G>A in CACNA1A (NM 000068.3). In Sophia DDM, as well as Varsome and Franklin predictions, the variant is assessed as likely pathogenic (applied ACMG criteria PVS1, PM2). The mutation probably causes aberrant splicing by disrupting splicing acceptor site. To our knowledge, this variant is not yet recorded in literature and dbSNP, gnomAD and HGMD databases.
Conclusion: Based on our results, we propose that the above‐mentioned variant in CACNA1A is likely to be associated with cerebellar ataxia, nystagmus and mild cognitive impairment.
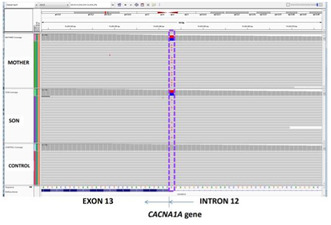
Read alignments visualized with IGV (Integrative Genomics Viewer) shows the novel heterozygous germline variant c.1672‐1G>A in the CACNA1A gene (NM 000068.3) (chr19‐13308529 C>T) in the patient and her son and a comparison with a control sample.
Disclosure: Supported by MH CZ–DRO (FNOl, 00098892).
EPO‐154
Serum biomarkers of neurodegeneration in mitochondrial membrane protein‐associated neurodegeneration (MPAN)
M. Skowrońska1; A. Cudna1; A. Antos1; M. Rydzewski1; J. Janikiewicz2; A. Dobosz2; A. Wydrych2; B. Pakuła2; P. Jakubek2; M. Lebiedzińska‐Arciszewska2; M. Cwyl3; M. Popielarz3; A. Dobrzyń2; M. Więskowski2; I. Kurkowska‐Jastrzębska 1
12nd Department of Neurology, Institute of Psychiatry and Neurology; 2Laboratory of Mitochondrial Biology and Metabolism, Nencki Institute of Experimental Biology Polish Academy of Sciences; 3Association NBIA Polska
Background and Aims: Neurodegeneration with iron accumulation (NBIA) associated with the mitochondrial protein C19orf12 – MPAN, is one of the hereditary diseases characterized by the accumulation of iron in the brain. There is currently no cure for MPAN, and the primary focus is on discovering the role of the C19orf12 protein, which may aid in the search for effective treatment. In this study, we aim to identify biomarkers that can serve as indicators of disease progression and treatment effectiveness.
Methods: Twenty‐five patients with genetically confirmed MPAN had biomarkers of inflammation and neurodamage tested, and results were compared to those of an age‐ and sex‐matched control group of healthy volunteers. Venous blood was collected in the fasting state in the morning, and serum was then frozen at −80°C for storage until testing. MMP‐9, S100B, ICAM‐1, E‐ and P‐selectins, and total α‐synuclein were measured using a sandwich‐type ELISA following the manufacturer's instructions. Serum NfL, GFAP, Tau protein, and UHC‐L1 were measured using SIMOA Quanterix methods.
Results: Our findings reveal that MPAN patients exhibited higher serum levels for all biomarkers, except BDNF. MMP‐9, E‐ and P‐selectins were increased 1.4–2 times above the control level. S100B was 10 times higher in MPAN patients, indicating potential blood‐brain barrier damage. Alpha‐synuclein was elevated 25 times, corresponding to an accumulation of this protein in the brain. NfL, GFAP, and UCH‐L1 were higher by 8, 2, and 5 times, respectively.
Conclusion: Our results suggest that S100B, alpha‐synuclein, NfL, and UHC‐L1 might be useful as biomarkers in MPAN
Disclosure: Nothing to disclose.
EPO‐155
Gait and postural responsiveness to subthalamic stimulation and levodopa: A prospective clinical‐instrumental study
I. Cani 1; I. D'Ascanio2; L. Baldelli1; G. Lopane1; P. Mantovani1; A. Conti1; P. Cortelli1; G. Calandra‐Buonaura1; L. Chiari3; G. Giannini1; L. Palmerini3
1IRCCS Istituto delle Scienze Neurologiche di Bologna, Via Altura, 3, Bologna, Italy; 2Department of Electrical, Electronic, and Information Engineering, Alma Mater Studiorum – University of Bologna, Bologna, Italy; 3Health Sciences and Technologies – Interdepartmental Center for Industrial Research (CIRI‐SDV), Alma Mater Studiorum – University of Bologna, Bologna, Italy
Background and Aims: This study delves into the dynamic interplay of balance and mobility, specifically probing their nuanced response to subthalamic stimulation.
Methods: We investigated alterations in the spatiotemporal dynamics of gait and posture in a prospective cohort of individuals with Parkinson's disease, examined both before and six months post subthalamic deep brain stimulation (STN‐DBS) surgery. The standardized motor protocol included Timed‐Up and Go, 18m walk test, quiet standing monitored by wearable inertial sensors.
Results: Twenty‐eight patients were evaluated in 2 preoperative and 4 postoperative conditions comprising OFF/ON medication and stimulation states. Standardized response mean values were computed to assess the responsiveness of sensor‐based motor parameters to treatments. Significant improvements in spatiotemporal gait parameters, including speed, cadence and stride length were observed following STN‐DBS surgery. The effect of stimulation on postural parameters was less evident.
Conclusion: Our study revealed that stimulation and levodopa had similar effects on gait parameters, with stimulation proving more effective in enhancing gait speed and stride length.
Disclosure: Nothing to disclose.
EPO‐156
Mortality analysis in a Portuguese cohort of hereditary cerebellar ataxias
L. Silva 1; S. Costa1; J. Moura1; F. Almeida2; C. Lemos3; M. Santos3; J. Oliveira3; J. Sequeiros3; J. Barros1; J. Damásio1
1Neurology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 2Neuroradiology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 3CGPP‐IBMC, i3S – Instituto de Investigação e Inovação em Saúde, Universidade do Porto, Portugal
Background and Aims: Hereditary cerebellar ataxias (HCA) are a heterogeneous group of diseases, associated with high morbidity and mortality. We aimed at analysing survival rate, causes, and place of death in a cohort of patients with HCA.
Methods: Prospective study of an HCA cohort, from the North of Portugal.
Results: Out of 252 patients with HCA, 38(15.1%) deceased, and 25(9.9%) lost to follow‐up. Among those deceased, 20(52.6%) were male; 31(81.6%) had autosomal recessive (AR) HCA [16(42.1%) CANVAS; 4(10.5%) AOA4; 3(7.9%) HSP‐MAG; 3(7.9%) FRDA; 1(2.6%) AOA1; 1(2.6%) HSP/ATX‐PGN; 1(2.6%) ATX‐PNPT1; 2(5.3%) undiagnosed]; and 7(18.4%) autosomal dominant (AD) HCA [5(13.2%) MJD/SCA3; 2(5.3%) undiagnosed]. Median age at death was 71.0 [IQR: 54.0–76.5] years. Overall survival was 35.6(±15.1) years after first symptoms, ranging from 19 (ATX‐PNPT1) to 62 years (AOA1). AR‐HCA patients lived with the disease for 39.4 (± 13.8) years and AD‐HCA patients for 20.0(±9.1) years (p < 0.05). Individuals with disease‐causing variants survived for 42.5(±14.2) years, while those with disease causing repeats lived for 33.1(±11.8) years (p < 0.05). Causes of death were identified in 21 patients: 19(90.1%) infection, 1(4.8%) neoplasia, or 1(4.8%) stroke. Death occurred at the hospital in 13(34.2%), home in 8(21.1%), or nursing‐home in 3(7.9%) [14(36.8%) unknown].
Conclusion: Life expectancy of HCA was lower than in general Portuguese population (71.0 vs. 81.5). Patients with AD‐HCA or with disease‐causing repeats had the lowest life expectancy. Survival rate, causes and places of death were similar to Huntington's disease. Knowledge on end‐stage needs is crucial for patients and relatives advance‐directive strategies and improving quality of life.
Disclosure: Nothing to disclose.
EPO‐157
The efficacy of Safinamide as an add‐on treatment in improving the quality of life and the pain in Parkinson's disease
J. Baik 1; E. Oh2; S. Cheon3; J. Cho4; Y. Sung5; J. Kim6; H. Shin7; J. Kim8; M. Park9; D. Kwan10; H. Ma11; J. Park12; S. Koh13; S. Choi14; J. Park15; P. Lee16; T. Ahn17; S. Kim18; C. Lyoo19; H. Lee20; J. Kim21
1Department of Neurology, Sanggy Paik Hospital, Inje University, Seoul, Republic of Korea; 2Department of Neurology, Chungnam National University, Daejeon, Republic of Korea; 3Department of Neurology, Dong‐A University, Busan, epublic of Korea; 4Department of Neurology, Samsung Medical Center, Sungkyunkwan University, Seoul, Republic of Korea; 5Department of Neurology, Gil Medical Center, Incheon, Republic of Korea; 6Department of Neurology, Seoul St. Mary's Hospital, The Catholic University, Seoul, Republic of Korea; 7Department of Neurology, Chung‐Ang University, Seoul, Republic of Korea; 8Department of Neurology, Bundang Hospital, Seoul National University, Seongnam, Republic of Korea; 9Department of Neurology, Yeungnam University, Daegu, Republic of Korea, 10Department of Neurology, Korea University Ansan Hospital, Ansan, Republic of Korea, 11Department of Neurology, Sacred Heart Hospital, Hallym University, Anyang, Republic of Korea, 12Department of Neurology, Bucheon Hospital, Soonchunhyang University, Bucheon, Republic of Korea, 13Department of Neurology, Korea University Guro Hospital, Seoul, Republic of Korea, 14Department of Neurology, Chonnam National University, Gwangu, Republic of Korea, 15Department of Neurology, Heaundae Paik Hospital, Inje University,Busan, Republic of Korea, 16Department of Neurology, Severance Hospital, Yonsei University, Seoul, Republic of Korea, 17Department of Neurology, Kyung Hee University, Seoul, Republic of Korea, 18Department of Neurology, Busan Paik Hospital, Inje University, Busan, Republic of Korea, 19Department of Neurology, Gangnam Severance Hospital, Yonsei University, Seoul, Republic of Korea, 20Department of Neurology, Kyungpook University, Daegu, Republic of Korea, 21Department of Medical, Eisai Korea Inc, Seoul, Republic of Korea
Background and Aims: Safinamide was found to improve on‐time without troublesome dyskinesia and reduce wearing off. Furthermore, we aimed to investigate its efficacy in enhancing patients’ quality of life and reducing pain.
Methods: This study is a prospective interventional study in Parkinson's disease patients who are receiving levodopa, and experience motor fluctuations with > = 1.5 hours of “off” time throughout the day. If there were no tolerability issues within 4 weeks, the initial dosage of 50mg/day was increased to 100 mg/day, and the patients continued with the 100 mg/day dosage for 18 weeks. The efficacy outcome was measured by the change from baseline to week 18 in the questionnaire examination of the quality of life (PDQ‐39) and the pain (KPPS).
Results: In this study, we evaluated 196 patients using PDQ‐39 and KPPS. The mean disease duration of them is 6.6 years, and the mean daily levodopa dose is 502.4 mg/day at baseline. At week 18, a significant improvement in the total PDQ‐39 score was observed compared to baseline (p < 0.001). Moreover, each domain (Mobility, Activities of daily living and Stigma) in PDQ‐39 demonstrated a significant improvement from baseline. The assessment of pain using KPPS also showed a significant decrease at week 18 compared to baseline (p = 0.013). Particularly, Safinamide significantly reduced Fluctuation–related Pain (p = 0.002).
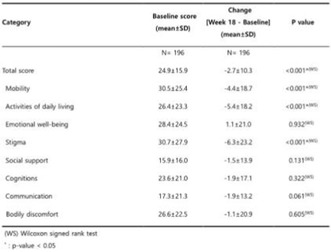
TABLE 1 PDQ‐39 change after 18 weeks compared to baseline
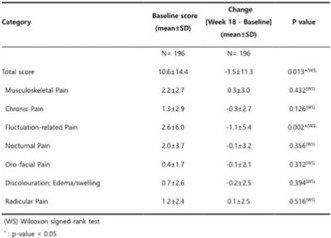
TABLE 2 KPPS change after 18 weeks compared to baseline
Conclusion: Safinamide at a dosage of 100mg/day demonstrated significant improvements in PDQ‐39 scores and significant reductions in KPPS. These findings indicate that Safinamide contributes to enhancing patients’ quality of life and reducing the pain, particularly pain associated with motor fluctuations
Disclosure: This Study sponsored by Eisai Korea Inc., Seoul, Republic of Korea.
EPO‐158
The DashPD‐Consortium: Importance of addressing bone health and anticholinergics to achieve holistic care in Parkinson's
M. Qamar 1; L. Batzu1; K. Poplawska‐Domaszewicz2; V. Metta3; I. Murasan4; D. Ziemele5; S. Khatchaturyan6; C. Falup‐Pecurariu4; K. Ray Chaudhuri1
1Parkinson's Foundation Centre of Excellence, Institute of Psychiatry, Psychology & Neuroscience, Department of Basic and Clinical Neuroscience, King's College London and King's College Hospital, London, UK; 2Department of Neurology, Poznan University of Medical Sciences, Poznan, Poland; 3Kings College Hospital London, Dubai, UAE; 4Department of Neurology, County Clinic Hospital and Transilvania University of Brasov, Brașov; 5Department of General Neurology, Riga East Clinical University Hospital, Riga, Latvia; 6Department of Neurology, Vagharshapat Polyclinic Hospital, Vagharshapat, Armenia
Background and Aims: A dashboard incorporating clinical “prompts” of the often ignored “five vitals” of Parkinson's disease (PD) (Chaudhuri et al., 2022, Qamar et al., 2023) has been published based on expert opinion and patient preferences. In an ongoing international multicentre observation survey (DashPD) we collected data on awareness and documentation of bone health and anticholinergic (ACh)‐index (risk factor for dementia and cardiovascular events) in PD in clinics.
Methods: This initial analysis refers to data from the ongoing DashPD Consortium as well as the UK‐arm of the ‘Nonmotor International Longitudinal Study’ (NILS, UKCRN.10084). A questionnaire asking “yes”, “no”, or “not applicable” format was used. Focus was on bone health, falls, and documentation of the Ach‐index.
Results: Data were collected between July 2022 to December 2022 (N = 906 PD). Results show bone health assessment in only 21%, while only 9% had bone density scans, and vitamin D and calcium levels were recorded in 25%. Despite frailty assessment performed in 61% there was no documentation of any fall prevention strategies. ACh‐index was measured in only 6% and no specific advice on dangers of ACh use was documented.

FIGURE 1 An extract of just vitals 4 and 5, from the multi‐centre international observational survey analysis for the application of the Dashboard of Vitals in Neurology outpatient clinics.
Conclusion: This initial analysis of the DashPD‐Consortium data, shows a glaring lack of awareness and documentation of bone health and Ach use related data which is likely to compromise patient health because of increased risk of fractures and negative effects of Ach use in PD.
Disclosure: Nothing to disclose.
EPO‐159
DysPKG project: Blinded clinical interrater reliability in assessing dyskinesia using the Parkinson's KinetiGraph (PKG)
M. Qamar 1; L. Batzu1; C. Santoro2; A. Rekik3; S. Landolfo2; K. Ray Chaudhuri1
1Parkinson's Foundation Centre of Excellence, Institute of Psychiatry, Psychology & Neuroscience, Department of Basic and Clinical Neuroscience, King's College London and King's College Hospital, London, UK; 2Department of Basic Medical Sciences, Neurosciences, and Sense Organs, University of Bari Aldo Moro, Bari, Italy; 3Department of Neurology, Sahloul Hospital, Sousse, Tunisia
Background and Aims: In Parkinson's disease (PD), dyskinesia is levodopa‐induced uncontrollable movements, which differ in phenomenology. We aim to visually recognise and characterise dyskinesia from reports using the validated Parkinson's KinetiGraph (PKG) and perform an interrater reliability analysis between independent clinicians to validate recognition of patterns of dyskinesia.
Methods: PKG reports with dyskinesia were identified from the UK‐PKG database and two independent clinicians rated the dyskinesias (pattern and severity). Each clinician was given ninety‐six patient PKG reports with the dyskinesia and bradykinesia graph. Raters were blinded to the patient's clinical assessment, medication, and history.
Results: PKG reports was assessed for daytime and night‐time dyskinesia, with each further analysed for severity and characteristics of dyskinesia (figure 1). Cohen's K was performed to determine interrater reliability between two clinical raters in relation to presence of dyskinesia, severity of dyskinesia, and characteristic of dyskinesia. There was significant substantial agreement between the two clinicians’ judgement for the presence, severity, and characterisation of dyskinesia at night‐time (table 1). There was a significant substantial agreement for presence of daytime dyskinesia [k = 0.669 p < 0.001] and a significant moderate agreement for the severity of daytime dyskinesia [k = 0.555 p < 0.001]. However, there was only a fair agreement regarding the characterisation of daytime dyskinesia [k = 0.336 p < 0.001].
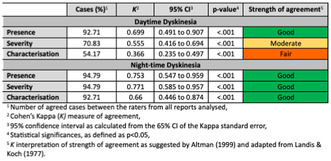
TABLE 1 Summary of Cohen Kappa (K) interrater agreement of PKG dyskinesia reports
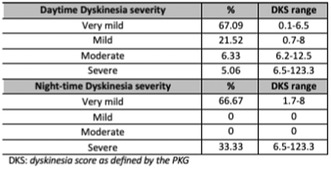
TABLE 2 Level of agreement between raters about severity of dyskinesia
Conclusion: This is the first attempt to use visual interpretation of the PKG to grade dyskinesia. The results show there to be a role for the PKG, even if interpreted visually, in identifying and characterising dyskinesia. PKG analysis could therefore aid correct recognition and personalised therapies for dyskinesias in PD.
Disclosure: Nothing to disclose.
EPO‐160
Differences in prevalence of orthostatic hypotension between Parkinson's disease subtypes
P. Oikonomou; J. Koschel; C. Altmann; W. Jost
Parkinson‐Klinik Ortneu, Wolfach, Germany
Background and Aims: Parkinson's disease (PD) is a clinically highly heterogeneous neurodegenerative disorder characterized by a wide range of motor and non‐motor manifestations. The tremor‐dominant (TD), mixed (M), and akinetic‐rigid (AR) subtypes constitute one of the most commonly used classification systems. Orthostatic hypotension (OH), a common non‐motor feature of PD, is linked to adverse outcomes and is evaluated with the modified Schellong test.
Methods: To investigate if patients with different motor subtypes also exhibit variations OH, we conducted a retrospective analysis using data of inpatients admitted to our clinic, diagnosed with PD, based on the clinical diagnostic criteria of the Movement Disorders Society. The modified Schellong test was performed according to standard protocol.
Results: Of 1,809 patients included in the study, 1,121 were classified into AR‐, 624 with M‐, and 64 with TD‐subtype. Interestingly, we found that patients with the AR‐subtype exhibited significantly worse results in the modified Schellong test compared to patients with the M‐subtype. Patients with the M‐type were younger, had significantly worse motor function measured with the Unified PD Rating Scale part III but did not differ significantly in duration of disease or Hoehn and Yahr stage.
Conclusion: Our findings indicate differences in orthostatic regulation among PD motor subtypes (AR vs. M) and support the notion that PD patients with the AR motor phenotype may have distinct pathophysiological abnormalities, i.e., a prominent affection of noradrenergic pathways and a body‐first pathogenesis. Further studies are needed to confirm these results, as they hold significant implications for personalized treatment and prognostic counseling in PD.
Disclosure: PO is an advisor for Stada. JK is an advisor and speaker for Desitin. CFA is an advisor for Zambon. WJ is an advisor and speaker for Abbvie, Bial, Desitin, Stada, UCB, and Zambon, The authors declare that they have no competing interests.
EPO‐161
Unmasking secondary parkinsonism: A case report of parkinsonism related to dural fistula
R. Ferrer Tarrés; M. Garcia Huguet; C. Vera Cáceres; C. Martínez Follana; I. Saurina Navarro; D. López Domínguez
Department of Neurology, Hospital Doctor Josep Trueta, Girona, Spain
Background and Aims: The most common cause for secondary parkinsonism is drug intake, but any disruption to the nigrostriatal dopaminergic pathway, such as a vascular insult or tumor, can prompt secondary parkinsonism. These secondary forms should always be considered in the differential diagnosis, as they often require specific therapeutic management, which may, in some cases, even lead to clinical reversal.
Methods: We present a case of a patient initially diagnosed with parkinsonism, later found to have a dural fistula, and experiencing clinical remission after undergoing fistula treatment.
Results: Presenting a 69‐year‐old woman who developed a progressive postural tremor, with a re‐emerging and resting component. This tremor notably exhibited asymmetric predominance on the left side of the upper limbs, accompanied by bradykinesia, rigid‐akinetic features, reduced arm swing, fragmented turning, and recurrent falls. The patient had no prodromal signs of synucleinopathy. DAT‐SCAN revealed minimal asymmetry in the right putamen. Magnetic Resonance Imaging (MRI) revealed a dural fistula dependent on branches of the external carotids with drainage into the superficial and deep venous system. Angiography confirmed the diagnosis, and treatment led to a clear, progressive resolution of parkinsonian symptoms. We provide a comparative video of the neurological examination pre and post dural fistula embolization.
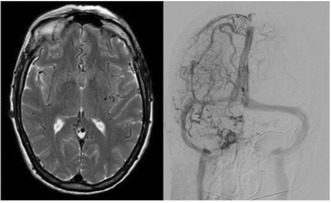
FIGURE 1 Cranial MRI with regurgitation of cerebral vessels and angiography revealing the dural fistula.
Conclusion: This case describes an uncommon cause of secondary parkinsonism‐ dural fistula, with limited instances reported in the literature. We suggest venous stasis as a potential trigger for dopaminergic pathway dysfunction, reflected in DAT‐SCAN abnormalities. Emphasizing the need to rule out reversible conditions, as timely treatment offers symptom resolution.
Disclosure: No disclosure.
EPO‐162
Adult‐onset PKAN with long disease duration: A case report and literature review
S. Othmani 1; F. Pinna1; V. Floris1; C. Bagella2; C. Frau2; P. Solla2; A. Salis3
1Department of Medical Sciences and Public Health, University of Cagliari; 2Unit of Neurology, Department of Medical, Surgical and Experimental Sciences, University of Sassari; 3Unit of Radiology, Department of Medical, Surgical and Experimental Sciences, University of Sassari
Background and Aims: Pantothenate Kinase‐Associated Neurodegeneration (PKAN), related to PANK2 gene mutation, is characterized by rapidly progressive movement disorders and cognitive impairment. While clinical presentation is typically in childhood, adult‐onset forms have been described by milder clinical manifestations and slower disease progression2, although data on the long‐term outcome are scarce.
Methods: Case report and literature review.
Results: A 30 year‐old man presented with slowly progressive speech disturbances and frequent falls. Over years, he had a gradual decline of intellectual functions, behavioral changes, orolingual dystonia with tongue protrusion, and spasticity leading to walking impairment. One brother and one sister had similar clinical manifestations with a slowly progressive course. At the age of 60, brain MRI revealed pathognomonic changes in the basal ganglia due to iron accumulation. Genetic testing showed a homozygous c.965A>G mutation in the PANK2 gene. At 68 years of age, the patient's clinical and radiological manifestations remained stable, without further deterioration compared to the time of the diagnosis. Twenty‐six additional cases of adult‐onset PKAN with long‐term follow‐up available (all due to PANK2 gene mutation) were identified in the literature, for a total of 27 cases. The median age at symptoms onset was 30 (range, 20–67) and 9 (33.3%) were female. At last available follow‐up, a median of 12 (range, 2–54) years from onset and 12 (44.4%) patients were alive.
Conclusion: The disease course in patients with adult‐onset PKAN seems characterized by early development of symptoms followed by and a subsequent phase of clinical‐MRI stability of years.
Disclosure: No disclosures.
EPO‐163
Phenotypic spectrum of GCH‐1 pathogenic variants: A case series
S. Costa 1; A. Sardoeira1; V. Oliveira1; R. Rodrigues2; E. Aires1; S. Morais3; J. Oliveira3; J. Barros1; J. Damásio1
1Neurology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 2Clinical Pathology – Laboratory of Genetic Biochemistry/Endocrinology, Hospital D. Estefânia, Centro Hospitalar Universitário de Lisboa Central, Lisbon, Portugal; 3CGPP‐Centre for Predictive and Preventive Genetics, IBMC‐Institute for Molecular and Cell Biology, i3S‐Instituto de Investigação e Inovação em Saúde, Universidade do Porto, Portugal
Background and Aims: Pathogenic variants in GCH1 are associated with dopa‐responsive dystonia, and more rarely with Parkinsonism and spastic paraparesis (SP).
Methods: Analysis of clinical and genetic profile of patients with GCH1 pathogenic variants.
Results: Six female patients, from two families, were identified. Onset occurred in childhood, at 6.8 (±1.09) years. Presenting symptoms included foot dystonia (n = 5, from the same family) and SP (n = 1). Only dystonic patients had clinical deterioration throughout the day. There was progressive worsening over the years, into generalized dystonia, and marked SP. Clinical diagnosis, when observed at our center, was achieved 31.4 (±6.98) years after onset. Five, with dystonia, were treated with 200mg sustained‐released levodopa/carbidopa and one, with SP, with 400mg immediate‐release levodopa/carbidopa. All had major clinical improvement: dystonia resolution; improvement in spasticity and disappearance of Babinski and Trommer‐Hoffman signs. With 24.0 (±16.4) years of follow‐up, all retained clinical benefit. Dystonic patients were studied through single‐gene testing of GCH1 [c.410T>A (p. (Met137Lys)], and SP with multigene panel for hereditary SP [c.541+1G>T (r.(spl))]. CSF analysis (n = 1) disclosed reduced 5‐HIAA level, increased HVA/5‐HIAA ratio, 3‐OMD, 5‐OHTrp, reduced Pterins.
Conclusion: In our case‐series the majority had a typical phenotype, of dopa‐responsive dystonia, but an atypical presentation was also observed. Clinical diagnosis and treatment were only established three decades after onset, but still a dramatic response was observed. With this work we wish to contribute into the characterization of a treatable movement disorder.
Disclosure: All authors declare that they have no conflicts of interest related to the manuscript.
EPO‐164
A tablet based on artificial intelligence system to differentiate between Essential Tremor and Parkinson's disease
S. Sellami; N. Farhat; K. Moalla; N. Bouattour; S. Daoud; S. Sakka; M. Damak; C. Mhiri
Department of Neurology and Research Laboratory LR12SP19, Habib Bourguiba University Hospital, Sfax, Tunisia
Background and Aims: Patients with Essential Tremor were initially considered to have isolated tremor, but additional motor and non‐motor features have been increasingly recognized. The term "Essential Tremor Plus" have started to be described in recent years with overlapping features that can make it difficult to differentiate between Essential Tremor (ET) and Parkinson's disease (PD). This study aims to evaluate on discriminatory features among ET and PD patients using handwriting analysis based on machine learning model.
Methods: We included a total of 90 participants: 30 ET, 30 PD and 30 age‐gender matched controls. All participants were asked to perform five different handwriting tasks on a digitizer tablet recording various signals which are x‐position, y‐position and pressure. The tasks included drawing repetitive ellipses, spiral, repetitive digits and Latin character 'l' continuously eight times. Movement time, velocity and the size of writing were analyzed to characterise handwriting patterns and to compare between ET and PD patients.
Results: The results from this study showed that PD patients perform movements significantly slower than ET (p = 0.01). Median time per repetition, median velocity and median acceleration of the 'l' task differed significantly between ET and PD (p < 0.05). PD patients also produced smaller handwriting than ET as represented by smaller average width and height of the repetitive ‘l’ task compared to ET group (p = 0.035).
Conclusion: We present a novel machine learning model that can serve as a complementary and promising support tool for the clinical diagnosis of ET and to differentiate between PD and ET.
Disclosure: Nothing to disclose.
EPO‐165
Differential diagnosis model in parkinsonian syndromes from calibrated diffusion tensor imaging
M. Grange1; L. Chougar2; J. Martini1; D. Grabli2; F. Cormier3; M. Vidailhet2; J. Corvol2; B. Degos4; V. Perlbarg 1; S. Lehéricy2
1BrainTale SAS, Strasbourg, France; 2Institut du Cerveau et de la Moelle épinière – ICM, INSERM U 1127, CNRS UMR 7225, Sorbonne Université, Team “Movement Investigations and Therapeutics” (MOV’IT), Paris, France; 3Clinique des mouvements anormaux, Département de Neurologie, Assistance Publique Hôpitaux de Paris, Hôpital Pitié‐Salpêtrière, Paris, France; 4Dynamics and Pathophysiology of Neuronal Networks Team, Center for Interdisciplinary Research in Biology, Collège de France, CNRS UMR7241/INSERM U1050, Université PSL, Paris, France
Background and Aims: Parkinson's disease (PD) poses a diagnostic challenge due to overlapping clinical features with other neurodegenerative disorders, such as multiple system atrophy (MSA) and progressive supranuclear palsy (PSP). This study aimed at evaluating the ability of diffusion tensor imaging (DTI) biomarkers provided by brainTale‐care, a CE‐marked solution, to differentiate PD from MSA and PSP and deriving reliable differential diagnosis tool.
Methods: A total of 189 subjects presenting with parkinsonian symptoms (92 patients with PD, 45 with MSA and 42 with PSP) collected from three different clinical studies were included in the study. DTI data were processed by brainTale‐care v3.0 (www.braintale.eu) to provide calibrated regional fractional anisotropy, radial, axial and mean diffusivity parameters. A classification model was implemented by using a support vector classifier and cross‐validation procedure. Classification performances were assessed through receiver operating characteristics (ROC) analysis.
Results: The classification model between PD patients and MSA and PSP patients, achieved a mean area under the ROC curve of 0.87 ± 0.05, a mean specificity of 0.74 ± 0.10, and a mean sensitivity of 0.90 ± 0.07 (Figure 1).
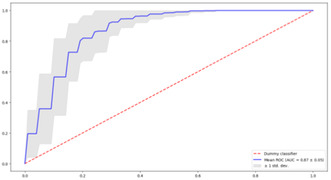
Cross‐validated receiver operating characteristic curve for the classification model PD versus MSA/PSP
Conclusion: This study shows that calibrated DTI biomarkers can be used to develop a classification model that efficiently differentiates patients with idiopathic PD and patients with MSA and PSP, two frequent parkinsonian syndromes. The easy access of diffusion tensor markers in clinical settings with brainTale‐care platform paves the way for the use of MRI‐assisted differential diagnostics in clinical settings as well as for drug development.
Disclosure: MG, VP, and JBM are BrainTale's employees. VP is co‐founders of BrainTale.
MS and related disorders 1
EPO‐166
BeeWellwithMS Podcast: A pioneering platform for brain health advocacy in multiple sclerosis
A. Straukiene; F. Moxon; S. Hughes
Torbay and South Devon NHS Foundation Trust
Background and Aims: In response to the escalating need for comprehensive brain health education among people with Multiple Sclerosis (MS), this study examines the effectiveness of the "BeeWellwithMS" podcast www.beewellwithms.com, an innovative platform for disseminating brain health knowledge. As an EAN‐certified brain health advocate, our objective was to leverage this medium to enhance understanding and self‐management of MS.

Methods: We analyzed listener engagement and feedback from the podcast, which covers diverse MS‐related topics, including brain health, emotional well‐being, and lifestyle modifications. The podcast's evolution since its inception in 2020 was studied, with a focus on its expansion post‐2024 following the integration of EAN‐endorsed brain health advocacy strategies.
Results: Since incorporating EAN‐certified brain health content, the podcast witnessed exponential growth in global listenership, with a significant increase in engagement from the MS community. Qualitative analysis of listener feedback highlighted an improved understanding of brain health issues and a more proactive approach to managing MS.

Downloads in the 25 countries, geolocation
Conclusion: The "BeeWellwithMS" podcast, underpinned by EAN's brain health initiatives, has proven to be a vital tool in educating and empowering the MS community. As an EAN brain health advocate, this platform signifies a novel approach to patient education, demonstrating significant potential in enhancing the quality of life for individuals living with MS.
Disclosure: No commercial support was received for this study. The podcast functions as an independent educational platform, with content driven by the latest research and patient needs in the MS community.
EPO‐167
Digital engagement in MS care: The impact of coordination on patient platform utilization
A. Straukiene; S. Hughes; F. Moxon
Torbay and South Devon NHS Foundation trust
Background and Aims: Innovative digital tools are reshaping MS care, aiming to enhance patient education and self‐management. This study assesses the influence of dedicated coordination on user engagement with the MS Patients Know Best (MS PKB) platform.
Methods: User engagement was analysed using the MS PKB dashboard, tracking weekly logins and registrations since its inception in 2016. In 2021, a dedicated coordinator role was introduced, providing personalized support and facilitating patient familiarity with the platform. Additionally, patient surveys and qualitative feedback assessments were conducted to measure user satisfaction and platform efficacy.
Results: Comparing 2016 to 2021, a substantial increase in engagement was observed. In 2016, user activity was minimal, with only 10 registered users. The appointment of a dedicated coordinator in July 2021 corresponded with an exponential increase in weekly logins to 130, a 225% rise from the preceding week, and total user registrations reached 100. A second peak in January 2024 demonstrated a further rise to 150 weekly logins. Qualitative feedback from patients showed high satisfaction, with the majority appreciating the platform's ease of use and the clarity of health information presented.
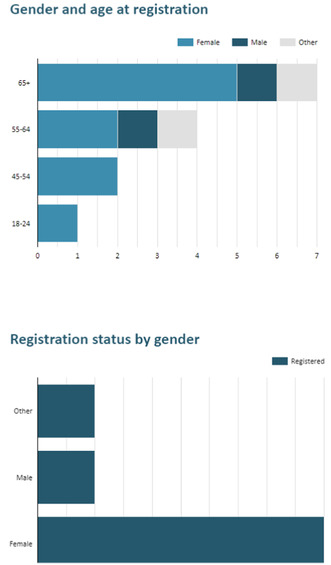
MS PKB demographics

MS PKB log in weekly

Total subscription of MS PKB
Conclusion: The implementation of a dedicated coordinator significantly boosted engagement with the MS PKB platform, as evidenced by increased logins and positive patient feedback. This suggests that personalized guidance is crucial for maximizing the benefits of digital health tools in chronic disease management.
Disclosure: There are no financial conflicts of interest to declare. Data were sourced from hospital records within NHS guidelines.
EPO‐168
Thymic hyperplasia after autologous hematopoietic stem cell transplantation in multiple sclerosis: A case series
A. Mariottini 1; R. Boncompagni2; D. Cozzi3; C. Nozzoli2; A. Repice4; V. Damato1; V. Miele3; R. Saccardi2; L. Massacesi1
1Department of Neurosciences, University of Florence, Florence, Italy; 2Cell Therapy and Transfusion Medicine Unit, Careggi University Hosptial, Florence, Italy; 3Department of Emergency Radiology, Careggi University Hospital, Florence, Italy; 4Department of Neurology 2, Careggi University Hospital, Florence, Italy
Background and Aims: Reactivation of thymopoiesis in adult patients with autoimmune disorders treated with autologous haematopoietic stem cell transplantation (AHSCT) is supported by immunological studies. Thymic hyperplasia after AHSCT was previously reported in patients with systemic sclerosis, but, to our knowledge, it has not been described in multiple sclerosis (MS).
Methods: Monocentric case series of patients previously treated with AHSCT (BEAM/ATG regimen) for aggressive MS who performed a chest CT scan for clinical purposes. Chest CT exams before and after AHSCT were reviewed by a thoracic radiologist: thymic hyperplasia was defined as a rounded mass in the thymic loggia with density around 40HU and thickness >1.3cm.
Results: Fifteen MS patients were included (Table 1). The median time interval between AHSCT and CT scan was 2 (1–15) months. Thymic hyperplasia was detected in 3/15 (20%) patients in a scan taken 1 to 3 months after AHSCT; all these patients were females, and aged 30 to 40 years. Four further patients showed a thymic rebound, with increased thickness and soft‐tissue lobulation. The time interval between AHSCT and CT was shorter in patients with thymic hyperplasia (median 1, range 1–2) vs those without (median 3; range 1–18); no differences in clinical‐demographic characteristics were observed. All the patients were free from new focal inflammatory activity over median 36 months of follow‐up (5–84).
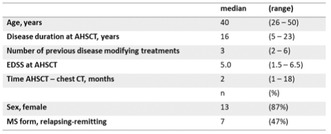
TABLE 1 Clinical‐demographic characteristics of the patients included.
Conclusion: Thymic hyperplasia was observed in 20% of MS patients recently treated with AHSCT. Our results suggest that AHSCT may promote thymic reactivation in MS patients, further supporting de‐novo thymopoiesis as a cornerstone of immunoreconstitution after AHSCT.
Disclosure: Nothing to disclose.
EPO‐169
Treatment with anti‐CD20 monoclonal antibodies after alemtuzumab in patients with relapsing‐remitting multiple sclerosis
A. Llanes Ferrer 1; D. Pérez Gil1; M. Espiño Martínez2; E. Rodríguez Martín2; A. Rodero Romero2; J. Fernández Velasco2; B. Martínez García1; P. Garay Albízuri1; R. Sainz Amo1; F. Rodríguez Jorge1; S. Sainz de la Maza1; E. Monreal Laguillo1; J. Masjuan1; M. Villar2; L. Costa Frossard1; J. Chico García1
1Neurology Department, Hospital Ramón y Cajal, Madrid, Spain; 2Immunology Department, Hospital Ramón y Cajal, Madrid, Spain
Background and Aims: The aim of this study is to describe our experience using anti‐CD20 monoclonal antibodies after alemtuzumab treatment failure in patients with relapsing‐remitting multiple sclerosis (RRMS).
Methods: Retrospective study including patients with high activity RRMS that received anti‐CD20 monoclonal antibodies after alemtuzumab. Clinical and paraclinical data were reviewed, including lipid‐specific oligoclonal IgM bands (LS‐OCMB), plasmablasts over total peripheral blood mononucleated cells (PB/PBMC) before alemtuzumab first administration, B‐lymphocytes over total lymphocytes (BL) before anti‐CD20 initiation, and light chain neurofilaments in serum (sNfL), at baseline, 6 month and 1 year follow‐up with anti‐CD20 treatment. BL threshold was stablished at 15%, PB/PBMC at 0.1%, and sNfL at 10pg/ml.
Results: Twelve patients were included [75% women, 35.78 (26.7–41.3) years‐old]. Patients received a median of 2 (2–3) cycles of alemtuzumab. An anti‐CD20 was initiated because of severe disease exacerbation (relapses and/or new lesions on MRI). Nine patients received ocrelizumab, 2 ofatumumab, and 1 rituximab. At baseline, 3/11 (27.3%) had a median of 7 (1–14) gadolinium‐enhancing lesions. All patients who underwent lumbar puncture (10/12) had LS‐OCMB, 6/7 had PB/PBMC >0.1%, and 6/12 had baseline BL>15% (data of high B‐cell activity). sNfL were elevated in 4/10 and normalized after 6 months of anti‐CD20 therapies. Eight completed 1 year follow‐up. Of them, 3 patients had new non‐enhancing lesions, one with a relapse. None experienced confirmed disability progression. Five (62.5%) achieved NEDA3. Three patients developed hypogammaglobulinemia with no serious infections.
Conclusion: In our series, anti‐CD20 monoclonal antibodies were a safe and effective alternative for RRMS patients with uncontrolled disease after alemtuzumab.
Disclosure: The authors report no relevant conflict of interest regarding the current study. JLCG has received honorary for speaking engagements or consulting services from Biogen, Bayer, Bial, Bristol‐Myers, Johnson&Johnson and Sanofi‐Genzyme. RSA has received honorary for speaking engagements from Johnson&Johnson. EM received research grants, travel support or honoraria for speaking engagements from Biogen, Merck, Novartis, Roche, Almirall, Janssen, Bristol‐Myers Squibb, and Sanofi‐Genzyme. FRJ has received honorary for speaking engagements or consulting services from Bial, Biogen, Johnson&Johnson and Sanofi‐Genzyme. SSM received payment for lecturing or travel expenses from Merck‐Serono, Biogen, Sanofi‐Genzyme, Roche, Janssen, and Novartis. LMV received research grants, travel support or honoraria for speaking engagements from Biogen, Merck, Novartis, Roche, Sanofi‐ Genzyme, Celgene and Bristol‐Myers Squib. LCF received speaker fees, travel support, and/or served on advisory boards by Biogen, Sanofi, Merck, Bayer, Novartis, Roche, Teva, Celgene, Ipsen, Biopas, Almirall. The remaining authors have no conflicts of interest to declare.
EPO‐170
Neutropenia following ocrelizumab exposure in patients with multiple sclerosis: A single‐center retrospective study
A. Favero 1; L. Rossi1; A. Sartori1; A. Dinoto2; S. Baldini1; A. Bratina1; A. Bosco1; P. Manganotti1
1Clinical Unit of Neurology, School of Neurology, Department of Medicine, Surgery and Health Sciences, University Hospital and Health Services of Trieste, ASUGI, University of Trieste, Trieste, Italy; 2Neurology Unit, Department of Neuroscience, Biomedicine and Movement Sciences, University of Verona, Verona, Italy
Background and Aims: Aim of this study is to describe the occurrence of neutropenia, defined as a reduction of the absolute neutrophil count below 1.5 × 103/uL, during treatment with ocrelizumab in patients with multiple sclerosis (pwMS), as a single‐center experience.
Methods: We retrospectively analyzed blood test including white blood cells count in particular neutrophils, lymphocytes and their subpopulation in consecutive pwMS at 1st, 3rd and 6th month after ocrelizumab infusions. Clinical and paraclinical variables were collected.
Results: Seventy‐four pwMS were enrolled. 88% was affected by a relapsing‐remitting form; 20% was treatment‐naïve and 40.5% switched from a first line therapy. Among our cohort, eight patients (10.8%) developed neutropenia. In three cases neutropenia was severe, down to 0.08 × 103/μL. In six patients, neutropenia was registered one month after the infusion, whereas in two cases after 5 and 6 months, respectively. None of them developed any infection during neutropenia. In two cases G‐CSF were administered after hematological evaluation. No MS relapses were reported during the treatment period.
Conclusion: Neutropenia after ocrelizumab treatment occurred in more than 10% of cases and it was usually observed within the first month after administration. In our cohort, all patients were asymptomatic and did not report viral or bacterial infections. Despite the quite frequent occurrence of neutropenia, our data confirm the safety of the medication under study, confirming previous data from literature.
Disclosure: L. Rossi has received funding for travel from Novartis. A. Dinoto has received funding for clinical trials from Roche and UCB, funding for travel from Horizon and research grants from Autoimmune Encephalitis Alliance and Encephalitis Internationals. S. Baldini has received funding research activity from Novartis. A. Bosco has received funding for travel and/or speaker honoraria from Sanofi, Roche, MBS, Teva and Biogen. Other authors have nothing to disclose.
EPO‐171
Early on‐treatment NfL levels are associated with MRI changes up to 4 years in dimethyl‐fumarate treated RRMS patients
T. Sejbaek1; N. Pedrosa de Barros2; A. Ribbens 2; J. B. Lewin3; J. P. Mendoza3; R. Antulov4; Z. Illes5
1Neurology, Esbjerg Hospital, University Hospital of Southern Denmark, Esbjerg, Denmark; 2icometrix, Leuven, Belgium; 3Biogen, Cambridge, MA, USA; 4Department of Regional Health Research, University of Southern Denmark, Esbjerg, Denmark; 5Neurology, Odense University Hospital, Odense, Denmark
Background and Aims: Dimethyl fumarate (DMF) is widely used in the treatment of relapsing MS and has shown a significant reduction in neurofilament light chain (NfL) levels in CSF and blood. Understanding the relationship between NfL and MRI biomarkers may help improve management of DMF‐treated patients.
Methods: The study included 42 treatment naïve newly diagnosed RRMS patients from the TREMEND phase IV trial (EudraCT 2014‐000254‐11). Plasma NfL and GFAP levels were measured using Simoa at baseline, month 6, 12 and 24. MRI data from baseline and up to year 4 since DMF initiation were included in the analysis. Annualized percent brain volume change (aPBVC) and lesion volume changes were determined with icobrain. Association between biomarkers was assessed with a generalized‐linear‐model with age as a covariate.
Results: Associations between plasma biomarkers and atrophy and lesion changes are respectively shown in Figures 1 and 2. From these, a few results seem to indicate a predictive value of plasma biomarkers in terms of brain atrophy and lesion changes. More specifically, NfL at 12 months was associated with brain atrophy measured with MRI available between year 1 and 4. Additionally, NfL at 6 months was associated with new and enlarging lesion volume at 2 and 3 years.
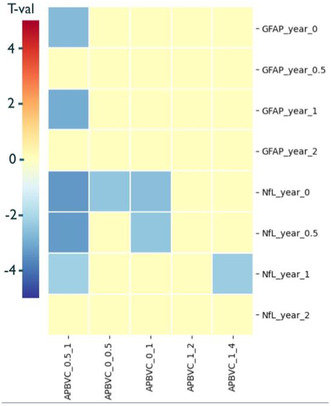
FIGURE 1 Associations between aPBVC measured in different intervals and plasma biomarkers collected at baseline, 6, 12 and 24 months. Only values with p < 0.05 shown.
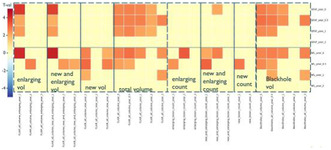
FIGURE 2 Associations between lesion volumes and plasma biomarkers collected at baseline, 6, 12 and 24 months. Only values with p < 0.05 shown.
Conclusion: In DMF‐treated patients, higher plasma‐NfL levels measured between 6 and 12 months are associated with subsequent lesion activity and brain atrophy, suggesting that NfL could be used additionally to MRI in the management of MS.
Disclosure: TS received travel grants from Biogen, Merck, Novartis and Roche, and research grants from Biogen, and served on advisory boards for Biogen, Merck and Novartis. NB and AR are employees of and hold stock/stock options in icometrix. JPM and JBL are employees of and hold stock/stock options in Biogen. ZI has received speakers’ honoraria and/or research grants from Biogen, Roche, Sanofi, Novartis, Merck, Alexion, Bristol Myers Squibb, Lundbeckfonden, and Jascha Fonden, has been member of advisory boards at Alexion, Biogen, Sanofi, Merck, Roche, Novartis, has been member of the adjudication relapse committee in phase 3 trials, and has been principal investigator in studies sponsored by Biogen, Merck, Roche and Sanofi.
EPO‐172
Lesion parenchymal fraction as empirical support for the topographical model in MS
T. Billiet1; N. de Barros1; C. Maes1; T. Phan1; W. Van Hecke1; A. Ribbens 1; T. Wang2; K. Kyle2; L. Ly2; J. Garber3; M. Barnett4; S. Krieger5
1icometrix, Leuven, Belgium; 2Brain and Mind Centre, University of Sydney, Sydney, NSW, Australia; Sydney Neuroimaging Analysis Centre. Sydney, NSW Australia; 3Brain and Mind Centre, University of Sydney, Sydney, NSW, Australia; Department of Neurology, Westmead Hospital, Sydney, NSW, Australia; 4Brain and Mind Centre, University of Sydney, Sydney, NSW, Australia; Department of Neurology, Royal Prince Alfred Hospital, Sydney, NSW, Australia; Sydney Neuroimaging Analysis Centre. Sydney, NSW Australia; 5Department of Neurology, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Background and Aims: The topographical model of MS postulates that a combination of parenchymal tissue atrophy and lesion topography contribute to a patient's disability trajectory. We previously showed that the lesion parenchymal fraction (LPF = lesion load/parenchymal volume ratio) is a useful MRI correlate of MS clinical symptoms (Fig.1). Here we validate the differential impact between cerebral, infratentorial and cervical LPF for explaining disability.

FIGURE 1 In the topographical model, the functional reserve is a water basin. Lesions (peaks) can cause clinical symptoms when crossing its surface. Lesion Parenchymal Fraction combines peaks (lesion volume) and water (parenchymal volume) in a single variable.
Methods: 78 MS patients with RRMS and SPMS were included (Table 1). Icobrain was used to measure T2‐FLAIR lesions and parenchymal volumes on brain MRI, and adapted to measure T2 lesion volumes and mean upper cervical cord area. Per patient in the sample, the measurements were transformed into percentiles with respect to the remaining sample. A linear model for decoding EDSS with compartmental LPFs as factors was compared to models including lesion and/or parenchymal tissue measurements considered separately. Pearson correlation and root‐mean‐squared error (RMSE) between estimated and true EDSS were computed.
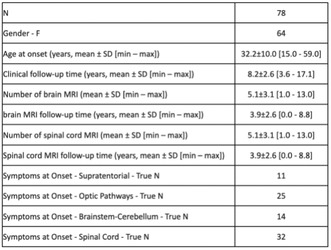
TABLE 1 Patient demographics
Results: Models with lesion or parenchymal measurements alone ranked last. In contrast, the LPF‐model had the lowest error (RMSE = 1.638) and high correlation (r = 0.275). Setting the cerebral LPF coefficient to 1 in the LPF model, the ratio of the LPF coefficients was 2.5 for infratentorial and 3.8 for cervical. An individual case is depicted using LPF in Fig.2.
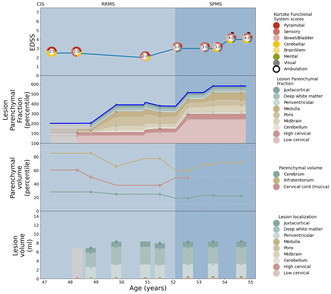
FIGURE 2 From bottom to top: Visualisation of lesion volume (bottom panel), parenchymal volume, the linear combination of local LPFs, resembling the longitudinal EDSS (top panel)
Conclusion: The results are in line with the topographical model describing proportional reserves for the spinal cord, infratentorium and cerebrum. LPF‐based modelling helps explain disability by combining lesions and their topographical location with parenchymal reserve.
Disclosure: SCK: Dr. Krieger reports consulting or advisory work with Biogen, EMD Serono, Genentech, Novartis, Octave, Genzyme/Sanofi, and TG Therapeutics; non‐promotional speaking with Biogen, EMD Serono, Novartis, and Genentech; and Grant and research support from Novartis, Biogen, BMS, and Sanofi. TB: Dr. Billiet is an employee of icometrix CM: Dr. Maes is an employee of icometrix TVP: Dr. Phan is an employee of icometrix NPdB: Dr. de Barros is an employee of icometrix WVH: Dr. Van Hecke is an employee of icometrix AR: Dr. Ribbens is an employee of icometrix TW: None KK: None LL: None JG: Dr. Garber reports research support from Biogen, and advisory work with Merck and Novartis. MHB: Dr. Barnett reports research grants from Genzyme‐Sanofi, Novartis, Biogen, Merck and BMS; and is a Research Consultant for RxMx and Research Director for the Sydney Neuroimaging Analysis Centre.
EPO‐173
Identifying neuropsychological multiple sclerosis phenotypes using latent profile analysis
A. Spiezia 1; M. Petracca2; F. Falco1; F. Lamagna3; M. Eliano1; A. Esposito1; C. Di Monaco1; F. Novarella1; V. Nicolella1; M. Moccia4; R. Lanzillo1; V. Brescia Morra1; A. Carotenuto1
1Multiple Sclerosis Clinical Care and Research Centre, Department of Neuroscience, Reproductive Science and Odontostomatology, Federico II University of Naples, Naples, Italy; 2Department of Human Neurosciences, Sapienza University, Rome, Italy; 3Department of Psychology, Università degli Studi della Campania L. Vanvitelli; 4Laboratorio di Citometria Clinica e Sperimentale CEINGE‐Biotecnologie Avanzate Franco Salvatore
Background and Aims: Multiple sclerosis (MS) patients may present with a high variability in cognitive and psychological (i.e. depression and fatigue) impairment. However, clinic‐demographic features underpinning such variability are still lacking. Hence, phenotypic classification base on clinic‐demographic features could alert clinicians for a close monitoring on these disability aspects of the disorder.
Methods: In this mono‐centric cross‐sectional study, we collected clinico‐demographic and neuropsychological data for each MS patients. Neuropsychological assessment included BICAMS battery, Beck Depression Inventory and Modified Fatigue Impact Scale. We employed a latent profile analysis (LPA) to unveil latent neuropsychological phenotype in MS patients clustering individuals in unobserved groups.
Results: We enrolled 600 MS patients. Using LPA, we unveiled five neuropsychological phenotype: 1) unaffected patients, with normal cognitive and psychological scores; 2) mild Cognition Impairment, showing mild reduction in cognitive scores; 3) mild‐to‐severe psychological impairment, showing increased psychological scores with normal cognitive scores; 4) mild neuropsychological impairment, showing mildly reduced cognitive scores, and increased psychological scores; 5) severe neuropsychological impairment, showing severely reduced cognitive scores, and increased psychological scores vs unaffected patients. Overall, cognitive and psychological impairment increases with physical disability. Older age is a determinant for psychological impairment independent from cognitive impairment. Relapsing‐remitting and paediatric‐onset patients are more likely in the unaffected and mild cognition impairment class, whilst progressive patients were mostly allocated in neuropsychological impaired class.
Conclusion: We identified five neuropsychological phenotypes in patients with MS that showed distinct clinical features. Clinicians should closely monitor neuropsychological disability level in patients with that specific characteristic.
Disclosure: All authors have nothing to disclose.
EPO‐174
Effect of siponimod on lymphocyte subsets in active secondary progressive multiple sclerosis and clinical implications
A. Spiezia 1; G. Scalia2; M. Petracca3; D. Caliendo1; M. Moccia4; A. Fiore2; V. Cerbone2; R. Lanzillo1; V. Brescia Morra1; A. Carotenuto1
1Multiple Sclerosis Clinical Care and Research Centre, Department of Neuroscience, Reproductive Science and Odontostomatology, Federico II University of Naples, Naples, Italy; 2Laboratorio di Citometria Clinica e Sperimentale CEINGE‐Biotecnologie Avanzate Franco Salvatore; 3Department of Human Neurosciences, Sapienza University, Rome, Italy; 4Department of Molecular Medicine and Medical Biotechnology, Federico II University of Naples, Italy
Background and Aims: Circulating immune cells play a pathogenic role in multiple sclerosis (MS). However, the role of specific lymphocyte subpopulations is not unveiled yet. We aimed to investigate lymphocyte changes during siponimod treatment in active secondary progressive MS (aSPMS) and their associations with clinical outcomes.
Methods: We enrolled 46 aSPMS patients with 2‐year follow‐up after the start of siponimod treatment and 14 healthy controls (HCs). Clinical and laboratory data were collected at baseline, 3rd, 6th, 12nd, and 24th month for MS patients, and at baseline for HCs.
Results: At baseline SPMS patients presented with increased naïve regulatory T lymphocytes vs HCs. Over time, SPMS patients showed decreased T CD4+ (coeff.range = −24/−17), B (coeff.range = −3.77/−2.54) and CD4/CD8 ratio (coeff.range = −4.44/−0.67) from month 3 thereafter vs baseline, and reduced CD3+CD20+ lymphocytes from month 12 thereafter (coeff.range = −0.32/−0.24). Patients not experiencing disability progression while on siponimod treatment showed B reduction from month 3 (coeff.range = −4.23/−2.32) and CD3+CD20+ lymphocyte reduction from month 12 (coeff.range = −0.32/−0.24) vs patients experiencing progression.

FIGURE 1 Flow cytometer dot plots. Plot of CD3+CD20+ cells in one male healthy control with no detectable cells (a), an aSPMS patient not progressing while on siponimod treatment at baseline with 0.9% CD3+CD20+ cells (b) and after 6 months from treatment
Conclusion: Patients treated with siponimod showed a T and B lymphocyte reduction, especially CD4+, CD3+CD20+, naïve regulatory T and memory regulatory B cells. Disability progression while on siponimod treatment was associated with a less pronounced effect on B and CD3+CD20+ lymphocytes.
Disclosure: MM has received research grants from the ECTRIMS‐MAGNIMS, the UK MS Society, and Merck; honoraria from Biogen, BMS Celgene, Ipsen, Janssen, Merck, Novartis, Roche, and Sanofi‐Genzyme. AC has received research grants from Almirall, research grants from ECTRIMS‐MAGNIMS and honoraria from Almirall, Biogen, Roche, Sanofi‐Genzyme, Merck, Ipsen and Novartis. MP has received research grants from Italian MS Foundation and Baroni Foundation, honoraria from HEALTH&LIFE S.r.l. and Biogen and sponsorship for travel/meeting expenses from Novartis, Roche and Merck. DC has received research grant from Merck. RL has received honoraria from Biogen, Merck, Novartis, Roche, and Teva. VBM has received research grants from the Italian MS Society, and Roche, and honoraria from Bayer, Biogen, Merck, Mylan, Novartis, Roche, Sanofi‐Genzyme, and Teva. ALS, GS, VC, AF have nothing to disclose.
EPO‐175
An atypical case of macular oedema in ozanimod
A. Bianco; T. Guerra; D. Intini; R. Vitobello; F. Oggiano; A. Manni
Department of Translational Biomedicines and Neurosciences, University of Bari Aldo Moro, Bari, Italy
Background and Aims: Macular edema (ME) is a well‐established side effect of fingolimod (FTY), the first oral sphingosine 1 receptor S1PR modulator approved for MS. Ozanimod is a second‐generation S1PR modulator, and it is thought to avoid some of the side effects associated with this class of drugs for its good bioavailability, high specificity and dose titration.
Methods: Our patient is a 48‐year‐old woman, diagnosed with RMS in 2009. She was treated with interferon beta 1a until 2013 when she switched to FTY for inefficacy. In 2016 FTY was discontinued for persistent and severe lymphopenia and interferon beta 1a was restarted. In August 2023, the patient began ozanimod after a new and symptomatic cervical lesion. However, in October, she reported a visual discomfort, therefore she underwent a complete ophthalmologic evaluation, including OCT, and was diagnosed as ME leading to ozanimod discontinuation.
Results: The incidence of FTY‐associated ME in the population without pre‐existing risk factors is approximately of 0.2%. ME was reported in 2882 (0.2%) participants during the ozanimod phase 3 trials, RADIACE and SUNBEAM, and in 0.4% participants during the long‐term safety trial DAYBREAK. All cases of confirmed ME had pre‐existing risk factors or confounding conditions. However, our patient did not present other risk factors and her pre‐ozanimod ophthalmologic evaluation was normal.
Conclusion: This case highlights the risk of developing ME during ozanimod exposure. Further research is needed to better understand whether a long term exposition to different S1PR, with different drug sequencing, may be associated with higher risk of ME.
Disclosure: Dr Iaffaldano received personal fees from Merk, Novartis, Biogen, Roche, Alexion and Genzyme. Dr. Manni received compensation for travel grants, participation in advisory board and/or speakink activity from Biojen, Merck Serono, Sanofi, Novartis, Bristol MS, Janssen and Roche. Dr Paolicelli received personal fees from Sanofi, Merk, Biojen and Janssenn. Dr Bianco, Dr Guerra, Dr Intini, Dr Vitobello and Dr Oggiano have nothing to disclose.
EPO‐176
Validation study of a mobile app‐based six‐minute walking test compared to smartwatch measurements introduction
S. Demir 1; E. Guven2; S. Colakoglu2; C. Benli1; Z. Polat2; M. Tutuncu3
1University of Health Science, Sehit Prof.Dr.Ilhan Varank Sancaktepe Training and Research Hospital Department of Neurology; 2Albert Heath Ltd, Clinical Development & Research; 3Istanbul University – Cerrahpasa, Department of Neurology
Background and Aims: The study focuses on validating a mobile app‐based Six‐Minute Walking Test (6MWT) by comparing its results with those obtained from a smartwatch in healthy adults. The aim is to measure the accuracy and reliability of the app‐based 6MWT for potential clinical application in monitoring patients with chronic conditions like Multiple Sclerosis (MS)
Methods: Twenty‐one healthy adults with no comorbidities participated. E 6MWT performed using a mobile app (Albert Health / MS+) and a smartwatch (Apple Watch 7 or higher) two times. The smartwatch's accuracy was validated separately on a 150‐meter course. Descriptive statistics and paired t‐tests are used to compare the standard deviation and correlation between the app and smartwatch results.
Button of Test at App
Test guideline
Results: The app‐reported walking distance decreased by 13.62 meters on average (SD = 39.99 meters), whereas the smartwatch showed a smaller average decrease of 3.81 meters (SD = 13.22 meters) between the tests. Strong positive correlations were observed between the app and smartwatch in the 6MWT (Test 1: r = 0.844; Test 2: r = 0.865). Despite a slight decrease in mean walking distances over time, no statistically significant changes were noted (app p‐value = 0.134, smartwatch p‐value = 0.202).
Result of a patient
Conclusion: The findings support that the app can be a reliable and accessible tool for assessing walking capacity, especially in clinical settings for managing chronic diseases like MS. Further research involving patients with MS is recommended to confirm the app's effectiveness in a clinical context.
Disclosure: Nothing to disclose.
EPO‐177
Calf muscles echo intensity in multiple sclerosis patients with lower limb spasticity treated with botulinum toxin
E. Bianchini 1 ; A. Massimiani1; M. Nasello1; M. Buscarinu2; M. Salvetti1; M. Giovannelli2
1Department of Neuroscience, Mental Health and Sensory Organs (NESMOS), Sapienza University of Rome, Rome, Italy; 2Neurology Unit, Sant'Andrea University Hospital, Rome, Italy
Background and Aims: Lower limb spasticity (LLS) is common in people with multiple sclerosis (PwMS). Previous studies suggested that muscle echo intensity could affect the efficacy of botulinum neurotoxin A (BoNTA) treatment and altered calf muscles echo‐intensity was reported in children with cerebral palsy and post‐stroke patients with LLS. However, this was not investigated in PwMS.
Methods: Muscle tone and echo intensity of gastrocnemius lateralis (GL), gastrocnemius medialis (GM) and soleus muscles were assessed in 19 PwMS through the modified Ashworth scale (MAS) and the modified Heckmatt scale (mHS), respectively. Patients were dichotomized into those who underwent BoNTA treatment for ≥ 3 sessions (longer group, median duration of treatment 78 months, N = 11) or < 3 sessions (shorter group, median duration of treatment 7 months, N = 8). The difference between each pair of muscles in terms of MAS and mHS in the overall population and in both subgroups was evaluated.
Results: A significantly higher mHS score in GM compared to soleus was found in the overall population and both subgroups. A significantly higher mHS score in GL than in soleus was found in the overall population and in the shorter group but not in the longer group. No difference was found between GM and GL in terms of mHS and between all pair of muscle in terms of MAS.
Conclusion: In PwMS with LLS, GL and GM showed a higher echo intensity than soleus irrespective of BoNTA treatment duration. This preliminary observation could stimulate research on muscle alterations in PwMS and its potential effect on BoNTA efficacy.
Disclosure: Nothing to disclose.
EPO‐178
Framingham risk score and patient determined disease steps in relapsing remitting multiple sclerosis
E. D'Amico; P. Di Filippo; C. Avolio; A. Zanghì
University of Foggia, Italy
Background and Aims: The associations between Multiple Sclerosis (MS) and cardiovascular diseases drawn from epidemiological studies have attracted much attention in the recent years.
Methods: The present study employed a monocentric, observational, retrospective cohort design. The primary study outcome was to describe in a cross‐sectional fashion the FRS rate in our cohort of relapsing remitting MS patients regularly followed up and then, if any, to find association with patients. Patient Determined Disease Steps (PDDS). Cardiovascular risk was classified as follow: low if the FRS is less than 10%, moderate if it is 10% to 19%, and high if it is 20% or higher.
Results: s 229 were enrolled. The sample consists of 163 women (71.2%). FRS categories were distributed as follow: 97 (42.3%) patients had low FRS, 84 (36.7%) patients had moderate FRS and 48 (21%) patients had high FRS. In the univariable ordinal regression analysis, one point increase in the PDDS scale was associated with 24% risk of high FRS (vs low) (proportional OR = 2.426, 95% CI 1.660–3.545; p < .0001). The results were confirmed also by EDSS score, with one point increase in the EDSS score was associated with 19% risk of high FRS (vs low) (proportional OR = 1.953, 95% CI 1.429–2.669–1.04; p < .0001).
Conclusion: the FRS demonstrated an association with the patients ‘perception of the disease as indicated by the PDDS. Careful attention should be given to addressing and treating cardiovascular risk factors, in addition to implementing lifestyle changes, when managing MS in the long term
Disclosure: Nothing to disclose.
EPO‐179
Silent progressive brain atrophy in clinically stable neuromyelitis optica a comparative proof‐of‐concept study
G. Medeiros Andrade Figueira; F. Faria Andrade Figueira; P. Vallegas Soares; R. Custodio Silveira; V. Tavares Carvalho Crelier; A. Seide Cardoso Vidal; M. Nunes Ferreirinha Leite de Castro
Hospital São Francisco
Background and Aims: Recently we demonstrated progressive corpus callosum atrophy occurring even in clinically stable multiple sclerosis (MS) patients, but literature data on brain atrophy in neuromyelitis optica spectrum disorder (NMOSD) patients are still scarce.
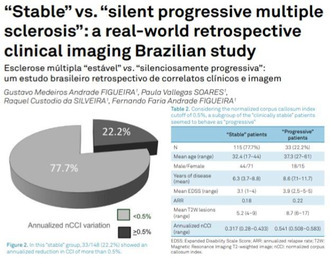
Figueira G., et al. Arq Neuropsiquiatr 2022;80(4):405–409
Methods: We compared longitudinal MRI data of 14 NMOSD (Wingerchuk, 2015), 148 relapsing remitting MS (McDonald 2001), and 23 control patients, followed regularly with clinical and imaging studies available on baseline and 5 years. All patients had at least 3 conventional MRI available studies with proper protocol leading to a reliable evaluation of activity and progression in at least 5 years. Clinical evaluation included annualized relapses rate and EDSS evolution at least annually, for at least 5 years. MRI data included gadolinium positive lesions or new/enlarging T2W lesion as well as the annualized evolution of corpus callosum index (CCI), measured as previously described.
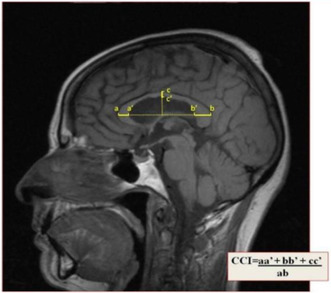
Corpus callosum index (CCI): a two‐dimensional measurement using an orthogonal semi‐automated linear model, applied to a conventional mid‐sagittal T1W MRI sequence. Figueira F., et al. Arq Neuropsiquiatr 2007;65(4‐A):931–935
Results: Patients with NMOSD were older and had EDSS scores higher than MS patients. Their mean CCI annual reduction was 0.477, ranging from 0.372 to 0.569, close to cut off and values situated between the stable and the progressive MS group.
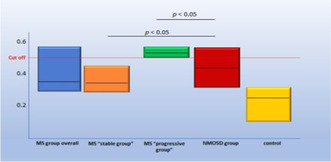
On NMOSD stable group mean CCI annualized reduction was 0.477 (range = 0.372 to 0.569), close to cut off and values were situated between the stable and the progressive MS group
Conclusion: In this small sample of 14 apparently “stable” NMOSD patients over 7 years follow up period, CCI was able to detect a reduction quite similar to that we see on relapsing remitting MS ones. More robust data are required, with a more significant sample, stratifying for clinical phenotypes and serologic status, but it seems reasonable to state that brain volumetry technique might be a useful tool for monitoring the real state of treatment response.
Disclosure: Nothing to disclose.
EPO‐180
“Stable” vs. “silent progressive multiple sclerosis”: A real world retrospective clinical imaging Brazilian study
G. Medeiros Andrade Figueira; F. Faria Andrade Figueira; P. Vallegas Soares; R. Custodio Silveira; V. Tavares Carvalho Crelier; M. Nunes Ferreirinha Leite de Castro
Hospital São Francisco
Background and Aims: Clinical and imaging are required to characterize activity and progression in MS. Parameters for activity are well defined but not progression ones. Ideal target for long term treatment includes neither clinical nor imaging signs of disease as well as no brain atrophy.
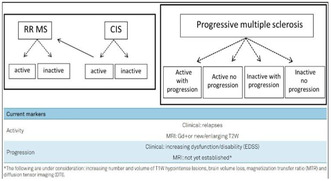
New MS phenotypes propose clinical and imaging requirements to characterize activity and progression in MS patients.
Methods: Comparative clinical‐imaging study focusing on MRI brain volumetry. 174 consecutive relapsing remitting MS patients (McDonald 2001) were studied focusing on activity and progression. Annual clinical evaluation (relapse rate and EDSS) and MRI data as well as annualized evolution of corpus callosum index (CCI) were compared.
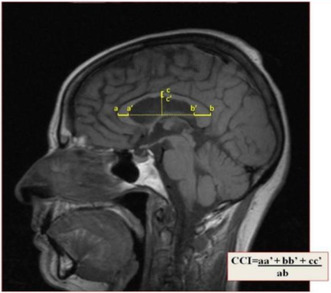
Corpus callosum index (CCI): a two‐dimensional measurement using an orthogonal semi‐automated linear model, applied to a conventional mid‐sagittal T1W MRI sequence.
Results: From 174 patients 148 were considered clinically “stable” based on EDSS. However, 33 (22.2%) out of this group showed annualized reduction of more than 0.5% on CCI, cut‐off to define significant brain atrophy.
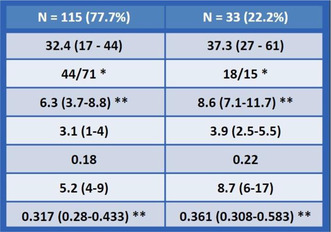
Among 148 apparently “stable” MS patients over at least 7 years follow up period, 1/5 showed significant progressive brain atrophy.
Conclusion: Among apparently “stable” relapsing‐remitting MS patients, 1/5 showed significant brain atrophy over at least 7 years follow up period. We consider reasonable to suggest that MRI volume sequences should be included in follow‐up protocols, providing information on the real treatment response status.
Disclosure: Nothing to disclose.
MS and related disorders 2
EPO‐181
Echopraxia, an underrecognized clinical sign in multiple sclerosis: A biological and neuroimaging framework
G. Álvarez Bravo 11; A. Quiroga Varela2; A. Gifreu1; C. Coll2; A. Boix Lago1; A. Miguela2; J. Huertas2
1University Hospital Dr. Josep Trueta of Girona; 2Unit of Neuroimmunology and Multiple Sclerosis of Girona
Background and Aims: The study investigates echopraxia, an unrecognized clinical sign, in the context of multiple sclerosis (MS) and explores its potential association with cognitive decline. Echopraxia, a developmental element in social learning, typically disappears with central nervous system maturity. While observed in dementias, Gilles de la Tourette syndrome, and schizophrenia, its occurrence in MS has not been previously documented. The study hypothesizes that echopraxia may serve as a predictor of cognitive impairment in MS patients.
Methods: The research involved 21 patients with relapsing‐remitting multiple sclerosis (RRMS) at the University Hospital Dr. Josep Trueta of Girona. Two cohorts, matched for age, gender, and clinical features, were established: one with 13 RRMS patients exhibiting echopraxia (RRMSwE) and another with 11 control RRMS patients. Tractography was used to identify morphological alterations in the cingulate gyrus, a region implicated in echopraxia pathogenesis. Circulating miRNAs in plasma from MS patients with and without echopraxia were also analyzed.
Results: Patients with echopraxia, particularly those with affective disorders had lower cingulate fiber numbers. Circulating miRNA analysis revealed that miR‐143‐3p and miR‐181c‐5p were twice less abundant in RRMSwE compared to RRMS patients. These miRNAs have been associated to cognitive impairment in patients with MS.
Conclusion: Atrophy of cingulum measured by tractography might be a radiological marker of echopraxia in patients with affective disorders such as depression. Some miRNAs (miR‐143‐3p and miR‐181c‐5p) involved in the cognitive impairment associated to MS could be related to echopraxia. Thus, echopraxia emerges a potential biomarker for predicting cognitive decline in patients with RRMS.
Disclosure: Nothing to disclose.
EPO‐182
Comparing adult‐onset and late‐onset multiple sclerosis: A real‐world study
K. Ahtinen1; I. Korhonen1; I. Rauma 1,2 ; H. Kuusisto1,2,3
1Faculty of Medicine and Health Technology, Tampere University, Tampere, Finland; 2Neural Medicine Responsibility Sector, Department of Sensory, Neural, and Musculoskeletal Medicine, Neurocenter Finland, Tampere Brain and Mind, Tampere University Hospital, Wellbeing Services County of Pirkanmaa, Tampere, Finland; 3Department of Health and Social Management, Faculty of Social Sciences and Business Studies, University of Eastern Finland, Kuopio, Finland
Background and Aims: The clinical presentation of multiple sclerosis (MS) may vary according to onset age. This Finnish retrospective registry study compares clinical characteristics of older adults (65+) with adult‐onset MS (AOMS, onset at 18–49 years) and late‐onset MS (LOMS, onset after 50 years).
Methods: Utilizing the Finnish MS registry, we analysed data of all older adults with MS in the catchment area of Tampere University Hospital (TUH, approximately 500,000 inhabitants) as of November 5th, 2023. Exclusions comprised patients with paediatric onset MS or unknown onset age.
Results: Altogether 248/1395 (17.8%) individuals from the catchment area of TUH were included, with 207/248 (83.5%) classified as having AOMS and 41/248 (16.5%) as having LOMS. Demographic details are presented in Table 1, age distribution in Figure 1 and MS diagnoses in Figure 2. At data acquisition, most patients had a progressive disease course (160/248, 64.5%), but primary progressive MS (PPMS) was more common in LOMS (15/41, 36.6%) compared to AOMS (26/207, 12.6%). No difference in disability outcomes emerged after 65 years. Among individuals with a current or previous relapsing‐remitting disease course, those with LOMS exhibited more relapses after 65 years (6/15, 40.0% of RRMS patients) than those with AOMS (11/130, 8.5% of RRMS patients). Disease‐modifying therapies had been used by 49/130 (37.7%) and 8/15 (53.3%) of relapsing remitting AOMS and LOMS patients, respectively.
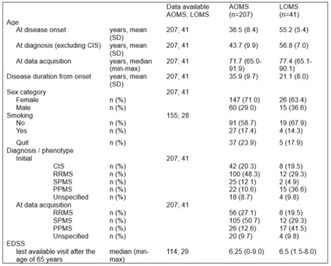
TABLE 1 Demographic details. AOMS, adult‐onset MS; LOMS, late‐onset MS; CIS, clinically isolated syndrome; RRMS, relapsing‐remitting MS; SPMS, secondary progressive MS; PPMS, primary progressive MS; EDSS, Expanded Disability Status Scale.
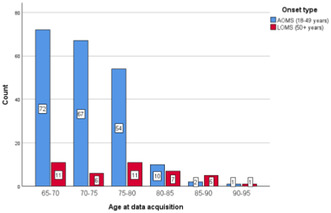
FIGURE 1 Age distribution in the study sample at data acquisition. AOMS, adult‐onset MS; LOMS, late‐onset MS.
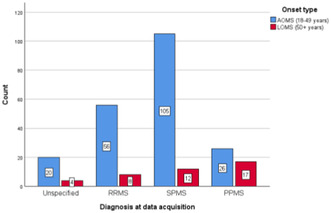
FIGURE 2 Distribution of diagnoses at data acquisition. AOMS, adult‐onset MS; LOMS, late‐onset MS; RRMS, relapsing‐remitting MS; SPMS, secondary progressive MS; PPMS, primary progressive MS.
Conclusion: Older adults with MS frequently exhibit a progressive disease course, and PPMS is particularly common in people with LOMS. However, in those with relapsing‐remitting LOMS, relapses may sometimes persist beyond 65 years.
Disclosure: KA, IK and IR have no disclosures relevant to this study. HK is the chair of the Finnish Multiple Sclerosis Current Care Guidelines working group. IR and HK contributed equally.
EPO‐183
Clinical presentation of multiple sclerosis in older adults
I. Korhonen1; K. Ahtinen1; I. Rauma 1,2 ; H. Kuusisto1,2,3
1Faculty of Medicine and Health Technology, Tampere University, Tampere, Finland; 2Neural Medicine Responsibility Sector, Department of Sensory, Neural, and Musculoskeletal Medicine, Neurocenter Finland, Tampere Brain and Mind, Tampere University Hospital, Wellbeing Services County of Pirkanmaa, Tampere, Finland; 3Department of Health and Social Management, Faculty of Social Sciences and Business Studies, University of Eastern Finland, Kuopio, Finland
Background and Aims: Older adults (65+) with multiple sclerosis (OAwMS) may carry substantial disease burden from prior activity or progression. However, limited data exists on their characteristics. We aimed to assess the clinical presentation of OAwMS in Finland.
Methods: OAwMS treated in Tampere University Hospital (TUH), Finland, were identified from the Finnish MS registry as of 5th December 2023. Clinical variables were analysed using summary statistics.
Results: At data acquisition, the Finnish MS registry included 13,037 subjects (26.8% aged 64 or older) of which 1395 were treated in TUH. Of these, 264/1395 (18.9%) were identified as OAwMS. Table 1 and Figure 1 present clinical characteristics and age distribution. Most patients exhibited a progressive disease course at data acquisition (170/264, 64.4%). Disease‐modifying therapy (DMT) had been used by 60/150 (40.8%) patients with relapsing‐remitting MS (RRMS), as well as 3/40 (7.7%) patients with secondary progressive MS who lacked a previous RRMS diagnosis and 1/46 (2.2%) patients with primary progressive MS. Only one patient with RRMS was currently on disease modifying therapy (DMT). After 65, relapses occurred in 18/150 (12.0%) patients with a current or previous RRMS. The median Expanded Disability Status Scale (EDSS) at the last available visit after the age of 65 years was 6.5 (range 0–9.0). Comorbidities were present in 205/264 (77.9%) patients.
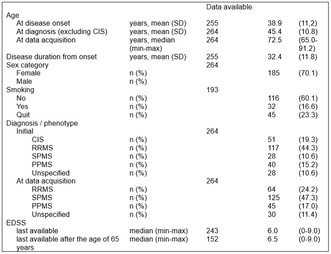
TABLE 1 Demographic details of the study sample. SD, standard deviation; CIS, clinically isolated syndrome; RRMS, relapsing‐remitting MS; SPMS, secondary progressive MS; PPMS, primary progressive MS; EDSS, Expanded Disability Status Scale.
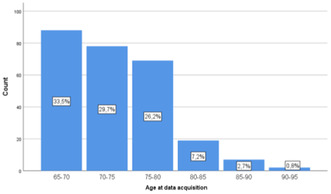
FIGURE 1 Age distribution in the study sample.
Conclusion: Most OAwMS had a progressive disease course, marked disability and comorbidities. Only one subject was on DMT. Treatment of OAwMS should adopt a multidisciplinary approach, focusing on rehabilitation, symptomatic treatment, and management of comorbidities in contrast to DMT.
Disclosure: IK, KA and IR have no disclosures relevant to this study. HK is the chair of the Finnish Multiple Sclerosis Current Care Guidelines working group. IR and HK contributed equally.
EPO‐184
Follow‐up of NMOSD course by using sensor‐based gait analysis
K. Akar 1 ; H. Youssef1; A. Vural2; A. Altıntaş2
1Movement Analysis Laboratory, Koç University Research Center for Translational Medicine (KUTTAM), Koç University, Istanbul, Turkey; 2Department of Neurology, School of Medicine, Koç University, Istanbul, Turkey
Background and Aims: Neuromyelitis Optica Spectrum Disorder (NMOSD) is a rare autoimmune astrocytopathy affecting the central nervous system. Despite advancements in targeting pathogenic factors like AQP4‐IgG, understanding the clinical course during relapse‐free periods and the impact on gait and balance remains underexplored. This pilot study employs sensor‐based gait analysis to assess NMOSD progression over one year.
Methods: Patients diagnosed with NMOSD underwent gait and balance assessments at initial, six‐month and one‐year visits using APDM OPAL sensors performing 2 MWT, T25FW, and various balance tasks. Paired Student t‐tests compared the first visit to six months and one year, while mixed‐effects analysis and Holm‐Sidak's tests assessed changes across three visits.
Results: Thirteen NMOSD patients participated, with four completing six months and three completing one‐year visits. Paired t‐test showed no change in gait and balance, but a trend emerged in mixed‐effect analysis, suggesting decreased double support (p = 0.09), increased midswing elevation (p = 0.09), increased single limb support (p = 0.07) and decreased terminal double support phase (p = 0.08). Most parameters were successfully matched except toe‐out angle, coronal ROM, and turn angle during gait analysis. Balance parameters when eyes were closed, feet apart on foam, and feet together did not change throughout a year of analysis in three visits conducted with mixed‐effect analysis.
Conclusion: This ongoing study aims to reveal sensor‐based gait analysis to monitor disability in NMOSD. Continuous tracking of the disease course is essential due to unpredictable prognosis. Highlighting parameters with matching success is crucial for effective disease follow‐up, urging an increase in participant numbers for robust outcomes.
Disclosure: Nothing to disclose.
EPO‐185
Seizures in inflammatory demyelinating disorders of the central nervous system
Ö. Ertürk Çetin; İ. Güngör Doğan; Ü. Zanapalıoğlu; F. Yadi; D. Çetinkaya Tezer; S. Demir
Department of Neurology, University of Health Sciences, Sancaktepe Şehit Prof Dr İlhan Varank Training and Research Hospital
Background and Aims: Multiple sclerosis (MS), neuromyelitis optica spectrum disorder (NMOSD), and myelin oligodendrocyte glycoprotein antibody associated disease (MOGAD), may be associated with acute symptomatic seizures and chronic epilepsy as well. The clinical features of the seizures and/or accompanying epilepsy seen in each disease group may vary. We aimed to describe the clinical features of seizures and epilepsy in our demyelinating patient population.
Methods: We retrospectively analyzed patients who were followed up in our tertiary referral center between 2019 and 2024. Those with a definite diagnosis of MS, NMO and MOGAD were identified. Patients who had at least one seizure before, simultaneously or after the diagnosis of demyelinating disease were included in the study.
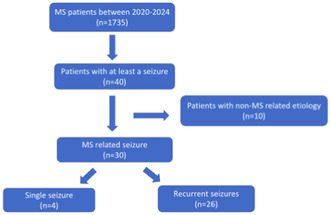
FIGURE 1
Results: Among 1735 patients with MS, 40 had experienced at least one epileptic seizure (2.3%). Thirty patients (1.7%) had seizures that could not be explained by other factor than MS. The interval between MS‐epilepsy diagnosis was longer and seizure recurrence was more in SPMS compared to RRMS. However, the prognosis of epilepsy was good in both subtypes. Out of 21 patients with NMOSD, none had a seizure during follow‐up. Out of 56 patients with MOGAD seizures were observed in three (5.4%). All of them had status epilepticus either at onset or during the course of the disease.
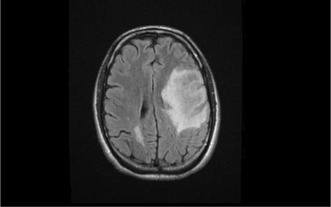
MRI of patient 1 with MOGAD
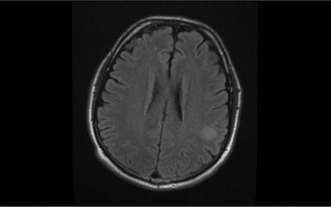
MRI of patient 3 with MOGAD
Conclusion: While the seizure seen during the relapses may be related to new cortical lesion formation and acute inflammation, it is more likely to be due to chronic atrophy, especially in SPMS. Prevalence of status epilepticus was common in MOGAD patients.
Disclosure: Nothing to disclose.
EPO‐186
Does natalizumab affect oligoclonal bands in the cerebrospinal fluid of patients with multiple sclerosis?
A. Liampas 1 ; V. Tseriotis2; G. Vavougios3; P. Zis3; G. Hadjigeorgiou3; P. Bargiotas3; C. Pourzitaki2; A. Artemiadis3
1Department of Neurology, Nicosia General Hospital, Nicosia, Cyprus; 2Laboratory of Clinical Pharmacology, Aristotle University of Thessaloniki, Thessaloniki, Greece; 3Department of Neurology, Medical School, University of Cyprus, Nicosia, Cyprus
Background and Aims: The pathological role of cerebrospinal fluid (CSF) oligoclonal bands (OCBs) in multiple sclerosis (MS) has been demonstrated. Long‐lived plasma cells are the main cells contributing to production of OCBs. Our aim was to demonstrate the quantitative effect of natalizumab (NTZ) on OCBs in the CSF of patients with MS.
Methods: A systematic search on MEDLINE, SCOPUS and Web of Science for English‐written and peer‐reviewed longitudinal studies on adults was performed. Meta‐analysis of the data was also performed.
Results: Eight eligible studies of adequate quality with a total sample of 326 relapsing‐ remitting MS patients were included. A summary rate of 14.07% [95% CI, 4.48%–36.36%] was observed for complete loss of OCBs and 42.02% [95% CI, 15.23%–74.51%] for reduction in OCB number or intensity was observed, both with considerable heterogeneity. Pooled estimates dropped (11% [95% CI, 0.04%–0.29%] and 34% [95% CI, 0.11%–0.68%] respectively) after the identification of an influential study. Multivariable meta‐regression identified IgG index as a factor contributing to heterogeneity (adj. p = 0.0279), regarding reduction of OCB number or intensity.
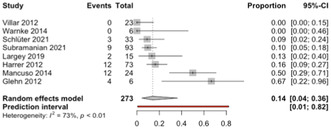
Forest plots of the meta‐analysis on the proportion of patients with complete loss of OCBs after NTZ treatment.
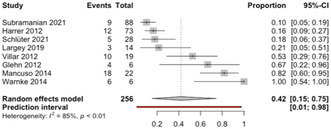
Forest plots of the meta‐analysis on the proportion of patients with reduction of OCB number or intensity after NTZ treatment.
Conclusion: In conclusion, our systematic review and meta‐analysis showed that NTZ can lead to reduction of intrathecal OCBs in MS patients, indicating a possible effect of NTZ on memory plasma cells which are the main source of OCBs in MS.
Disclosure: Nothing to disclosure.
EPO‐187
Identifying definite patterns of unmet needs in patients with multiple sclerosis using unsupervised machine learning
E. Maida 1 ; G. Abbadessa1; E. Cocco2; P. Valentino3; A. Lerede4; J. Frau2; G. Miele1; F. Bile1; M. Vercellino5; F. Patti6; G. Borriello7; P. Cavalla5; M. Sparaco1; L. Lavorgna1; S. Bonavita1
1Department of Advanced Medical and Surgical Sciences, University of Campania “Luigi Vanvitelli”, Naples, Italy; 2Department of Medical Science and Public health, Centro Sclerosi Multipla, University of Cagliari, Cagliari, Italy; 3Institute of Neurology, University Magna Graecia, Catanzaro, Viale Europa, Catanzaro, Italy; 4Department of Brain Sciences, Imperial College London, London W120BZ, UK; 5MS Center, Department of Neuroscience, City of Health and Science University Hospital of Turin, Turin, Italy; 6Department "GF Ingrassia", Section of Neurosciences, University of Catania, Catania, Italy; 7MS Center, Hospital San Pietro Fatebenefratelli, Rome, Italy
Background and Aims: People with Multiple Sclerosis (PwMS) exhibit a spectrum of needs that extend beyond solely disease‐related determinants. Investigating unmet needs from the patient perspective may address daily difficulties and optimize care. Our aim was to identify patterns of unmet needs among PwMS and their determinants.
Methods: We conducted a cross‐sectional multicentre study. Data were collected through an anonymous, self‐administered online form. To cluster PwMS according to their main unmet needs, we performed agglomerative hierarchical clustering algorithm. Principal component analysis (PCA) was applied to visualize cluster distribution. Pairwise comparisons were used to evaluate demographics and clinical distribution among clusters.
Results: Out of 1,764 mailed questionnaires, we received 690 responses. Access to primary care was the main contributor to the overall unmet need burden. Four patterns were identified: Cluster C1, "Information‐Seekers with Few Unmet Needs"; Cluster C2, "High Unmet Needs"; Cluster C3, "Socially and Assistance‐Dependent"; Cluster C4, "Self‐Sufficient with Few Unmet Needs". PCA identified two main components in determining the patterns: the “public sphere” (access to information and care) and the “private sphere” (need for assistance and social life). Older age, lower education, longer disease duration, and higher disability characterized clusters with more unmet needs in the “private sphere”. However, demographic, and clinical factors failed in explaining the four identified patterns.
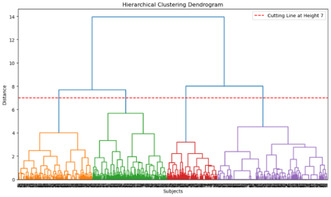
Hierarchical clustering dendrogram. The figure displays the hierarchical clustering dendrogram generated using the Ward linkage method.
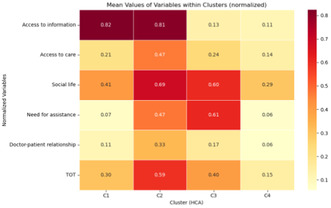
Mean values of normalized variables within clusters generated by hierarchical clustering algorithm (HCA). The heatmap presents the mean values of selected variables within distinct clusters, after the normalization process.
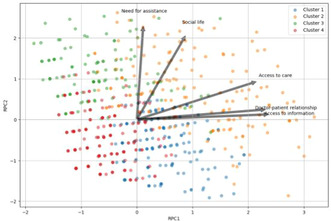
Biplots of principal component analysis (PCA) scores and component loadings with cluster assignments.
Conclusion: Our study identified four unmet need patterns among PwMS, emphasizing the importance of personalized care. While clinical and demographic factors provide some insight, additional variables warrant further investigation to fully understand unmet needs in PwMS.
Disclosure: Nothing to disclose.
EPO‐188
Systemic inflammation biomarkers in multiple sclerosis as potential indicators of underlying inflammatory process
E. Maida; G. Miele; D. Mele; G. Abbadessa; M. Sparaco; L. Lavorgna; G. Romano; E. Signoriello; G. Lus; S. Bonavita
Department of Advanced Medical and Surgical Sciences, University of Campania “Luigi Vanvitelli”, Naples, Italy
Background and Aims: The role of systemic inflammation biomarkers has been investigated in several autoimmune diseases. Our study aimed to assess whether inflammatory indices differ between healthy individuals and people with Multiple Sclerosis (PwMS), and explore whether they may correlate with demographic, clinical, and laboratory variables.
Methods: We conducted a retrospective study involving 100 PwMS admitted to our MS Center, and 83 age‐ and sex‐matched healthy controls. Demographic, MS characteristic and laboratory data, including lymphocyte subsets, were collected. Neutrophil/lymphocyte ratio (NLR), platelet/lymphocyte ratio, monocyte/lymphocyte ratio, Systemic Inflammation Index and Systemic Immune‐Inflammation Index (SIRI) were calculated.
Results: NLR and SIRI values were significantly higher in PwMS than in healthy control group (p = 0.03, p = 0.02, respectively). In the linear regression model, NLR was associated with primary‐progressive forms (PPMS) (p = 0.03), higher number of oligoclonal bands (p = 0.03) and higher frequency of relapses before the diagnosis (p = 0.03). SIRI was associated with PPMS (p = 0.03) and higher frequency of relapses before the diagnosis (p = 0.04). NLR and SIRI were associated with higher absolute CD20+ B cells count at disease onset (p = 0.02, p < 0.01, respectively).
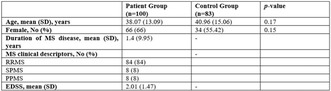
Demographic and clinical characteristics of the two groups.
Conclusion: The results may highlight the role of NLR and SIRI as potential indicators of an underlying inflammatory process. The correlation with B cells at onset can further support the evidence in favour of their critical role in MS pathogenesis. Further studies are needed to validate such findings and assess the potential impact of disease‐modifying therapies on systemic inflammation biomarkers.
Disclosure: Nothing to disclose.
EPO‐189
Natalizumab efficacy on radiological and clinical parameters in pediatric‐and adult‐onset multiple sclerosis
M. Puthenparampil 1 ; M. Gaggiola1; M. Ponzano2; G. Scialpi1; G. Zanotell1; A. Miscioscia1; A. Berardi1; M. Nosadini3; S. Sartori3; P. Perini1; F. Rinaldi1; F. Bovis2; P. Gallo1
1Department of Neurosciences, University of Padua; 2Department of Health Sciences, Section of Biostatistics, University of Genova, Genova, Italy; 3Paediatric Neurology and Neurophysiology Unit, Department of Women's and Children's Health, University Hospital of Padova, Italy
Background and Aims: Pediatric‐onset Multiple Sclerosis patients (POMS) is characterized by a more rapid accumulation of CNS inflammation than Adult‐Onset MS (AOMS). Therefore, the early use of HET has been highly recommended in POMS.
Methods: All patients who started natalizumab (NTZ) were enrolled in this retrospective single‐centre study and were clinically evaluated at baseline and then every six months with EDSS score. The cohort was then divided based on age at onset in Pediatric‐Onset (POMS) and Adult‐Onset AOMS) MS and were propensity‐matched. SDMT was assessed at baseline in all patients and in a sub‐cohort of POMS (29) and AOMS (30) at least 2 years after baseline assessment.
Results: From 38 POMS and 122 AOMS, propensity‐matching defined a cohort of 36 POMS and 72 AOMS. The effect on inflammatory MRI and clinical was evaluated by survival analysis did not differ between AOMS and POMS (p = 0.924). PIRA was documented in 9 AOMS (12.5%, p = 0.0278) during the follow‐up (LogRank p‐value 0.014). Corrected SDMT values did not differ between POMS and AOMS at baseline (49.43 ± 14.74 and 49.71 ± 10.75, p = 0.639). While z‐score improved in both AOMS and POMS (p < 0.001), annualized z‐score change was significantly higher in POMS than in AOMS (0.41 ± 0.40 vs 0.25 ± 0.34, p = 0.023).
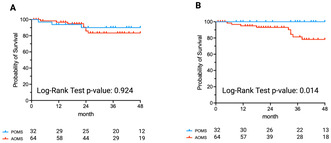
Survival analysis: NEDA and PIRA

SDMT score at baseline and during the follow up
Conclusion: Evaluation of inflammatory and clinical outcomes did not reveal any significant difference between POMS and AOMS, indicating an excellent response to NTZ in both groups. The favorable outcomes observed in clinical, radiological, and neuropsychological parameters support the use of NTZ as a viable treatment option in POMS.
Disclosure: M.P. reports grants from Almirall, Teva, Sanofi Genzyme, Merck Serono, Biogen Italy and Novartis; consultancy for Novartis, Biogen Italy and Sanofi Genzyme; board membership Sanofi Genzyme, Novartis and Biogen Italy. M.G. M.Po, G.S., G.Z., A.M., N.M., and S.S. have nothing to disclose. P.P. reports grants from Almirall, Teva, Sanofi Genzyme, Merck Serono, Biogen Italy, Novartis and Roche; consultant for Novartis, Biogen Italy, Sanofi Genzyme and Roche. F.R. report grants from Almirall, Teva, Sanofi Genzyme, Merck Serono, Biogen Italy, Novartis; consultancy for Novartis, Biogen Italy and Sanofi Genzyme. P. G. reports grant from Almirall, Teva, Sanofi Genzyme, Merck Serono, Biogen Italy, Novartis, Roche and Bristol Myers Squibb; consultancy for Novartis, Biogen Italy, Sanofi Genzyme, Roche and Bristol Myers Squibb; board membership Sanofi Genzyme, Novartis, Biogen Italy, Roche, Merck Serono and Bristol Myers Squibb.
EPO‐190
Retinal microglia changes in relapsing‐remitting multiple sclerosis under natalizumab therapy
M. Puthenparampil 1 ; E. Basili1; M. Ponzano2; V. Mauceri1; F. De Napoli1; A. Miscioscia1; E. Pilotto3; L. Rossi4; P. Perini1; F. Rinaldi1; F. Bovis2; P. Gallo1
1Department of Neurosciences, University of Padua, Padua, Italy; 2Department of Health Sciences, Section of Biostatistics, University of Genova, Genova; 3Department of Neurosciences‐Ophthalmology, University of Padua, Padua, Italy; 4Department of Medicine, Surgery and Health Sciences, University of Trieste, Italy
Background and Aims: Microglia (MG) is suggested to play an immunopathological role of in Multiple Sclerosis (MS). In vivo analysis of retinal MG proliferation/activation, evaluating Retinal Hyper‐reflective Foci (HRF) by Optic Coherence Tomography (OCT), in MS patients under disease modifying therapies may help to clarify MS immunopathology as well as drug's mechanism of intrathecal action.
Methods: The effect of NTZ in retinal MG on 36 Relapsing‐Remitting MS (RRMS) patients was investigated in a retrospective, single‐centre study. OCT was performed immediately before the first infusion and then between infusion 3 and 4, infusion 6 and 7, infusion 11 and 13. Peripapillary and macular scans were acquired, evaluating peripapillary retinal nerve fiber layer (pRNFL) thickness, macular volumes (vertical scans), and HRF count (horizontal scan) in Ganglion Cell Layer (GCL), Inner Plexiform Layer (IPL) and Inner Nuclear Layer (INL). Clinical examination was performed every six months.
Results: HRF count significantly increased under NTZ therapy (p < 0.001) in both GCL (18.85 ± 6.93 at baseline, 28.24 ± 9.55 after 12 months) and IPL (25.73 ± 7.03 at baseline, 33.21 ± 8.50 after 12 months) but remained stable in INL (33.65 ± 7.76 at baseline, 36.06 ± 6.86 after 12 months, p = 0.868), while no relevant modification of pRNFL and macular volumes were observed during the study.
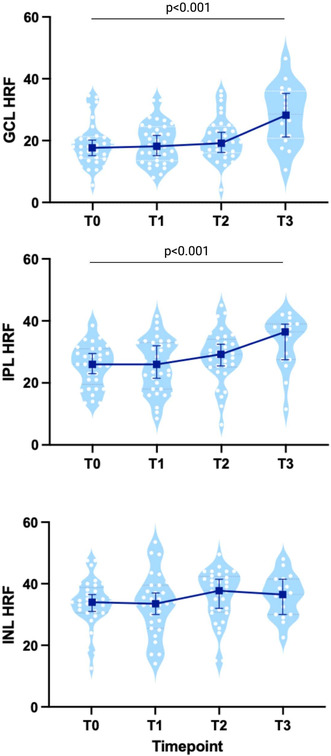
HRF count in MS patients treated with Natalizumab
Conclusion: In RRMS NTZ affects retinal MG activation (HRF count) in GCL and IPL, but not in INL, suggesting that NTZ does not impact on all the aspects of MS immunopathology.
Disclosure: M.Pu., report travel grants, consultancy, and board membership from Almirall, Teva, Sanofi Genzyme, Merck Serono, Biogen Italy, Novartis, Bristol Myers Squibb, Janssen, and Alexion. E.B., M.Po., A.M., E.P., F.B. have nothing to disclose. V.A.M reports travel grants from Sanofi Genzyme, Biogen, and Viatris. P.P. reports grants from Almirall, Teva, Sanofi Genzyme, Merck Serono, Biogen Italy, Novartis, Roche, Alexion, Janssen, Brystol Mayer Squibb; consultancy for Novartis, Biogen Italy, Sanofi Genzyme, Roche, Janssen, Brystol Mayer Squibb. RF report grants from Almirall, Teva, Sanofi Genzyme, Merck Serono, Biogen Italy, Novartis, consultancy for Novartis, Biogen Italy, Sanofi Genzyme. P.G. reports grant, consultancy, and board membership for Almirall, Teva, Sanofi Genzyme, Merck Serono, Biogen Italy, Novartis, Roche, Bristol Myers Squibb, Janssen, and Alexion.
EPO‐191
PAI mutation 4G/5G‐coagulopathy risk factor for multiple sclerosis?
M. Cholakova
Nikolay Mihnev
Background and Aims: Homozygous carrying of the PAI mutation, 4G/4G is clinical significant for thrombotic events. In multiple sclerosis (MS), malfunction of the plasminogen activation system and blood brain barrier disruption are pathological processes that might lead to an abnormal fibrin(ogen) extravasation into the parenchyma.
Methods: Healthy controls, patients with ischemic stroke, patients with MS, MRI, laboratory tests for thrombophilia, neurological examination, statistical analysis
Results: A prospective clinical trial of 54 patient with multiple sclerosis, 69 healthy controls and 101 patients with ischemic stroke. A total of number of 101 patients with ischemic stroke under 50 years were screened, 67 were examined for PAI mutation. The healthy control group consists of 44 women and 25 men. Homozygous carrier of the PAI mutation 4G/4G variant was found to increase the chance of stroke 3.00 times [OR = 3.00; CI: (0.70–12.93)]. Patients with multiple sclerosis were 54, with the majority of female – 39, and male – 15. We compared the groups of patients with stroke and multiple sclerosis to evaluate prevalence of PAI‐1 mutation in both cohorts. According to our study, PAI‐1 mutation could be a risk factor for the development of multiple sclerosis (p‐value < 0.00001) and ischemic stroke at a young age (p < 0.05), and the difference between the two groups and healthy controls is statistically significant.

TABLE 1
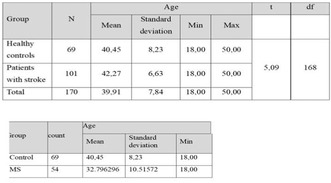
TABLE 2, 3
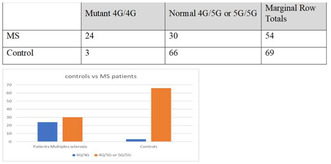
TABLE 4 Graphic 1
Conclusion: PAI mutation could play a role as a risk factor for development of demyelinating disease like MS. In the future examination of patients with MS for PAI mutation could play role for the choice of treatment and prevention of invalidation.
Disclosure: No.
EPO‐192
Efficacy and safety profile of ocrelizumab in primary progressive multiple sclerosis patients from Montenegro
M. Roganovic; S. Perunicic; J. Erakovic; L. Radulovic; D. Milikic; B. Vujovic; Z. Idrizovic; S. Vujovic; M. Debeljevic; S. Gluscevic; M. Dajevic; S. Bojovic; A. Gucci; S. Martinovic
Clinic for Neurology, Clinical Center of Montenegro, Ljubljanska bb, 81000 Podgorica, Montenegro
Background and Aims: As only registered drug for patients with primary progressive multiple sclerosis (PPMS), ocrelizumab is in use in Montenegro since March 2019. Efficacy and safety of ocrelizumab in PPMS patients was confirmed in ORATORIO trial, as well as in several real‐world studies. Our aim is to evaluate efficacy and safety of Ocrelizumab in PPMS patients in Montenegro.
Methods: We retrospectively examined data of PPMS patients treated with ocrelizumab in Montenegro from March 2019 to September 2023.
Results: During the abovementioned period, we treated 73 PPMS patients, mean aged 51.6 ± 10.6 years. In 61.6% of patients baseline Expanded Disability Status Scale (EDSS) was 5.5 or higher. During the follow‐up period, no EDSS worsening was observed in 70.3% of treated‐patients, while treatment was stopped in 16 patients: due to EDSS progression in 6 patients; due to death in 3 patients; due to adverse event (AE) in 1 patient; due to other reasons in 2 patients. Treatment discontinuation was choice of 4 patients. Regarding MRI activity during the follow‐up period, presence of T1Gd+ lesions was detected in 1 patient, while 4 patients developed new/enlarging T2 lesions. Elevation of hepatic transaminases was observed in 10.6% of patients; lymphopenia grade 2 in 1.5%; one patient developed cervical malignancy. Urinary tract infection was detected in 3% of patients.
Conclusion: Our data, similar to other real‐world studies, confirmed good efficacy as well as favorable safety profile of ocrelizumab in PPMS patients.
Disclosure: All authors have received speaker honoraria and/or travel grants.
EPO‐193
Executive dysfunction in multiple sclerosis patients
S. Sellami; N. Farhat; N. Bouattour; K. Moalla; H. Haj Kacem; S. Daoud; S. Sakka; M. Damak; C. Mhiri
Neurology Department and Research Laboratory LR12SP19, Habib Bourguiba University Hospital, Sfax, Tunisia
Background and Aims: Executive dysfunction occurs in 15%–28% of Multiple Sclerosis (MS) patients. The aim of this study is to identify characteristics of Executive Function Disorders (EFD) in a clinical cohort of Tunisian patients with MS.
Methods: A group of patients diagnosed with definite MS according to the 2017 McDonald criteria and followed up in the department of Neurology of Habib Bourguiba Hospital‐Tunisia and a group of control subjects were assessed with a battery of classical executive tests which included semantic and phonemic verbal fluency test (SVFT/PVFT), Go/no‐Go, digit‐span‐backwards and Delis Kaplan Executive Function System (D‐Kefs).
Results: 70 MS patients with an average age of 34,6 years and 50 control subjects were included. As compared to controls, 74% of MS patients had executive disorders perceived by the D‐Kefs (p = 0.03). The planning ability and the mental flexibility were disrupted as evidenced by impaired verbal fluency in all MS patients. The phonemic verbal fluency was clearly more affected (p = 0.049). There were no significant alterations regarding scores of Go/no‐Go test (p = 0.3) and digit‐span‐backwards test (p = 0.4) in MS group compared to controls. Patients with SPMS (secondary progressive multiple sclerosis) showed significant EFD than those with RRMS (relapsing‐remitting multiple sclerosis). Our study also showed a significant correlation between EFD and the EDSS (Expanded Disability Status Scale) (p = 0.002). No impact of DMT (disease modifying therapy) on EFD.
Conclusion: These results suggest that there are executive difficulties that are commonly found among patients with MS. The identification of these profiles in clinical practice could allow for more individualized rehabilitation.
Disclosure: Nothing to disclose.
EPO‐194
Assessment of visual function in multiple sclerosis patients over time
C. Oreja‐Guevara 1 ; E. Alba‐Suárez1; I. Gómez‐Estévez1; L. García‐Vasco1; E. Santos‐Bueso2; J. Rouco‐Maseda3; J. Quezada‐Sanchez1
1Neurology, Hospital Clínico San Carlos, Idissc, Madrid, Spain; 2Ophtalmology, Hospital Clínico San Carlos, Madric, Spain; 3Ciencias de la Computación, Universidad de Coruña, Spain
Background and Aims: Optic neuritis (ON) is often the first symptom at the onset of MS and can impair visual function. Objective: To longitudinally analyse the visual function in MS patients.
Methods: Stable MS patients over six months were included, with two assessments: baseline (V1) and one year later (V2). Visual acuity (VA), VA2.50% and VA1.25% were measured with ETDRS and low contrast test. Colour vision with Ishihara and Farnsworth‐Munsell D28 (FM‐D28) test. Contrast sensitivity with Pelli‐Robson test. Comparisons were drawn between eyes affected by previous optic neuritis (ON) and those not.
Results: with Pelli‐Robson test. Comparisons were drawn between eyes affected by previous optic neuritis (ON) and those not. Results Thirty‐two patients, predominantly female (22), average age 43, were studied. Twenty eyes with previous ON. VA, VA2.50%, VA1.25% and contrast sensitivity showed significant differences between both groups (ON vs. no ON) in V1 and V2 (p < 0.05). After one year a significant worsening in visual function (p < 0.05) in the non‐ON group were observed. The ON group showed significant reductions in VA1.25% (p = 0.005) and contrast sensitivity (p = 0.000). In the Ishihara test at V1 and V2, 95.5% of patients without optic neuritis had normal results. Meanwhile, 10% of the patients in the optic neuritis group displayed abnormalities. The non‐ON group showed 43.2% altered FM‐D28 values in V1 and 47.7% in V2. The ON group showed 80% of altered values in V1 and 85% in V2.
Conclusion: Visual acuity and contrast sensitivity decline as the disease progresses. The FM‐D28 test offers a more precise evaluation of color vision.
Disclosure: Nothing to disclose in relation with the abstract.
EPO‐195
Hyperreflective foci in the inner retina in multiple sclerosis: Preliminary results of an external validation study
N. Krajnc 1 ; T. Zrzavy1; F. Leutmezer1; B. Kornek1; P. Rommer1; T. Berger1; B. Pemp2; G. Bsteh1
1Department of Neurology, Medical University of Vienna, Vienna, Austria; 2Department of Ophthalmology, Medical University of Vienna, Vienna, Austria
Background and Aims: Microglia, the resident immune cells of the central nervous system, are increasingly recognized to play an important role in the pathophysiology of multiple sclerosis (MS). Retinal microglia may be visualized as hyperreflective foci (HRF) by optical coherence tomography (OCT), but their origin and clinical relevance remain controversial.
Methods: In this cross‐sectional retrospective study, we included patients with MS (pwMS) who had undergone an OCT scan. HRF counting was performed separately in the ganglion cell‐inner plexiform layer (GCIPL) and the inner nuclear layer (INL). Eyes with a clinical history of ON or asymptomatic ON (interocular asymmetry with cut‐off values of ≥5μm for pRNFL and ≥4μm for GCIPL) were excluded from the analysis.
HRF Protocol. Macular scan and HRF visualization in a patient with MS. HRF were defined as isolated, small sized (<30 μm), punctiform elements with moderate reflectivity but without any back shadowing.
Results: In total, we included 38 eyes of 36 pwMS (47.2% female, median age 31.5 years (24.9–43.8), median disease duration 1.8 years (0.1–10.2), median EDSS 1.0 (0–2.5)). Mean GCIPL and INL thicknesses were 67.3 μm (7.2) and 34.7 μm (2.2), respectively. The mean GCIPL HRF count was 10.8 (3.9), and the mean INL HRF count was 9.5 (5.5). The INL HRF count was associated with the INL thickness (β = 0.43; 95% CI 0.05, 0.30; p = 0.009), whereas the GCIPL HRF count was not associated with the GCIPL thickness (β = 0.12; 95% CI −0.42, 0.86; p = 0.490).
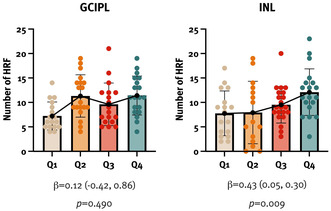
The INL HRF count was associated with the INL thickness, whereas the GCIPL HRF count was not associated with the GCIPL thickness.
Conclusion: This study demonstrated that HRF can be assessed by OCT and confirmed that the INL HRF count is associated with the INL thickness, providing indirect evidence that HRF may indeed represent activated microglia. Further studies are needed to confirm their clinical relevance.
Disclosure: Nothing to disclose.
Muscle and neuromuscular junction disorder 1
EPO‐196
Advancing clinical practice: Impact of online education on implementation of novel therapies for myasthenia gravis
A. Stan 1 ; M. Calle1; F. David1; F. Saccà2
1Medscape LLC, New York, New York, USA; 2University of Naples Federico II, Napoli, Italy
Background and Aims: We developed an online CME activity titled: “Navigating the Changing Landscape in Myasthenia Gravis: An Expert Case‐Based Discussion”. We hypothesized that participation in this education would lead to improved knowledge of implementing targeted MG treatments.
Methods: Neurologists participated in a 30‐min expert discussion educational activity (www.medscape.org/viewarticle/993422). Educational effect was assessed using a repeated‐pair design with pre‐/post‐assessment. Three multiple choice questions assessed knowledge and 1 question (Likert‐type scale) assessed confidence. A paired samples t‐test was conducted for significance testing on overall average number of correct responses and for confidence rating, and a McNemar's test was conducted at the learning objective level (5% significance level, p < .05). Cohen's d with correction for paired samples estimated the effect size of the education on number of correct responses (<.20 modest, .20–.49 small, .59–.79 moderate, ≥.80 large). Data were collected from 7/14/2023 to 10/25/2023.
Results: A total of 789 neurologists participated of which 104 completed all the pre‐ and post‐activity questions during the study period. Overall 64% neurologists improved their knowledge and competence related to implementing novel targeted therapies in the management of MG (average knowledge/competence pre: 33% vs post: 68%) p < .001, Cohen's d = 1.02) (see Table). 56% had increased confidence in appropriately integrating novel targeted therapies for MG.
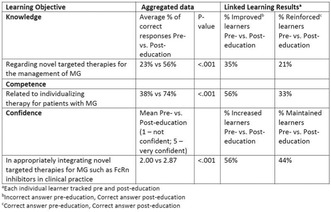
TABLE Impact of education on neurologists’ knowledge and competence
Conclusion: This online CME activity significantly improved neurologists’ knowledge and competence related to implementing novel targeted therapies in the management of MG; however, substantial gaps remain which should be addressed in future medical education.
Disclosure: Nothing to disclose.
EPO‐197
Impact of myasthenia gravis on patients' daily life: Findings from the ME&MGopen decentralised study
C. Barnett‐Tapia 1 ; S. Lehnerer2; C. Gorin3; D. Ravindra3; N. Sellami3; M. Keller4; E. Aras5; E. Touré Cuq3; J. Howard Jr6
1Department of Medicine, Division of Neurology. University of Toronto and University Health Network; 2Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt‐Universität zu Berlin,Department of Neurology with Experimental Neurology, Berlin, Germany; 3Ad Scientiam, Paris, France; 4Alexion GmbH; 5Alexion Pharmaceuticals Inc.; 6The University of North Carolina, Dept of Neurology, CB 7025
Background and Aims: Generalised myasthenia gravis (gMG) is an autoimmune disease causing fluctuating and debilitating muscle weakness, profoundly affecting patients' quality of life. Capturing its daily impacts objectively remains a challenge. The ME&MGopen study aims to address this gap. This study describes gMG impact using electronic patient‐reported outcomes (ePROs) and potential influencing factors.
Methods: 199 gMG patients were enrolled in ME&MGopen, a multicountry (USA, Canada), decentralised research study. Sociodemographic, clinical and treatment data were collected during baseline remote visit. Participants used the ME&MGopenTM digital tool for up to 8 months and completed questionnaires on a monthly basis (MG‐QOL‐15r, MG‐ADL, ISI, Chronic Pain, PHQ‐8).
Results: Of the 199 participants, 65% were female, with a mean age 57 ± 16 years. 60 self‐reported their MGFA Disease Class, with the following distribution: 55% Class III, 28% Class II, 17% Class IV. Across all participants, PHQ‐8, ISI, Chronic Pain, MG‐ADL, MG‐QOL‐15r baseline scores indicated a meaningful gMG impact on their lives [6.5 ± 5.1, 9.0 ± 6.0, 2.5 ± 2.4, 5.2 ± 3.7, 12.0 ± 8.0 respectively]. PHQ‐8, MG‐ADL, MG‐QoL‐15r scores were significantly higher when disease control was considered inadequate [9.8 ± 4.0 (p < 0.05), 10.6 ± 3.2 (p < 0.0001), 21.0 ± 6.0 (p < 0.01)] versus controlled patients. PHQ‐8 and MG‐QoL‐15r scores were significantly increased in patients unable to work [10.0 ± 5.0 (p < 0.05), 20.0 ± 5.7(p < 0.001)] versus working or unemployed patients.
Conclusion: These findings show the impact of gMG on quality of life, consistent with literature of gMG. The reliability of ME&MGopenTM to collect ePROs will be confirmed during upcoming longitudinal analyses.
Disclosure: Carolina Barnett Tapia: Research funding (paid to her institution) (Ad Scientiam, Alexion AstraZeneca (AZ) Rare Disease, Cartesian Therapeutics, US Department of Defence, Muscular Dystrophy Canada, MGNet, Grifols and Octapharma); Honoraria (consulting and/or Advisory board) fees (AcademicCME, Alexion AZ Rare Disease, argenx, Sanofi, UCB Pharma and Janssen). Sophie Lehnerer: Lecturing activity (Alexion (AZ Rare Disease), argenx, Hormosan, UCB); Consultancy work (Alexion (AZ Rare Disease), Argenx, Biogen, Roche, UCB); Research support (Alexion (AZ Rare Disease), Argenx, Hormosan, UCB (at Charité – Universitätsmedizin Berlin)) Clarissa Gorin, Dellini Ravindra, Noura Sellami, Emma Touré Cuq: employees of Ad Scientiam. Martin Keller, Emrah Aras: employees of Alexion Pharmaceuticals Inc. James Howard: Research funding (paid to his institution) (Alexion AZ Rare Disease, argenx, Cartesian Therapeutics, Centers for Disease Control and Prevention, MGFA, Muscular Dystrophy Association, NIH, PCORI, UCB Pharma); honoraria/consulting fees (AcademicCME, Alexion AZ Rare Disease, argenx, Biologix Pharma, CheckRare CME, F. Hoffmann‐LaRoche Ltd, Horizon Therapeutics plc, Medscape CME, Merck EMD Serono, NMD Pharma, Novartis Pharma, PeerView CME, Physicians' Education Resource (PER) CME, PlatformQ CME, Regeneron Pharmaceuticals, Sanofi US, UCB Pharma, Zai Labs); non‐financial support (Alexion AZ Rare Disease, argenx, Cartesian Therapeutics, Toleranzia AB, UCB Pharma and Zai Labs).
EPO‐198
The ME&MGopen study: Analysis of 8‐month adherence trends to a smartphone application in generalized Myasthenia Gravis
C. Barnett‐Tapia 1 ; S. Lehnerer2; M. Boyer3; N. Sellami3; D. Ravindra3; M. Keller4; E. Aras5; E. Touré Cuq3; J. Howard Jr6
1Department of Medicine, Division of Neurology, University of Toronto and University Health Network; 2Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt‐Universität zu Berlin, Department of Neurology with Experimental Neurology, Berlin, Germany; 3Ad Scientiam, Paris, France; 4Alexion GmbH; 5Alexion Pharmaceuticals Inc.; 6The University of North Carolina, Dept of Neurology, CB 7025
Background and Aims: Generalised Myasthenia Gravis (gMG) is a debilitating, chronic, autoimmune disease characterized by fluctuating fatigable muscle weakness. The ME&MGTM smartphone application is a research tool enabling the unsupervised data collection of gMG symptoms as well as quality of life and mental health measures. Improving users’ long term adherence will optimize data quality for research. We evaluated patient adherence to ME&MGTM digital tests and e‐questionnaires in this fully decentralized ME&MGopen study.
Methods: Patients diagnosed with anti‐AChR autoantibody positive gMG were enrolled in the USA and Canada. Five active digital tests and five e‐questionnaires were completed at baseline and on a monthly basis for one year. App adherence was assessed until Day‐240.
Results: After their remote baseline inclusion visit, 176 participants complied to the ME&MGTM tasks (adherence rate = 91%). Adherence rate dropped at Day 30 for both digital tests (78%) and e‐questionnaires (79%) and remained above 60% until Day‐240. Once a digital test or e‐questionnaires was initiated, it was generally brought to completion. The most demanding task (sit‐to‐stand test) was interrupted in less than 4% of evaluations.
Conclusion: These results show promising immediate and lasting adherence to ME&MGTM, persisting beyond 6 months, a critical turning point in digital studies. Additional subgroup analyses will inform on specific adherence profiles and offer avenues to maintain patients’ long‐term engagement.
Disclosure: Carolina Barnett Tapia: Research funding (paid to her institution) (Ad Scientiam, Alexion AstraZeneca (AZ) Rare Disease, Cartesian Therapeutics, US Department of Defence, Muscular Dystrophy Canada, MGNet, Grifols and Octapharma); Honoraria (consulting and/or Advisory board) fees (AcademicCME, Alexion AZ Rare Disease, argenx, Sanofi, UCB Pharma and Janssen). Sophie Lehnerer: Lecturing activity (Alexion (AZ Rare Disease), argenx, Hormosan, UCB); Consultancy work (Alexion (AZ Rare Disease), Argenx, Biogen, Roche, UCB); Research support (Alexion (AZ Rare Disease), Argenx, Hormosan, UCB (at Charité – Universitätsmedizin Berlin)) Clarissa Gorin, Dellini Ravindra, Noura Sellami, Emma Touré Cuq: employees of Ad Scientiam. Martin Keller, Emrah Aras: employees of Alexion Pharmaceuticals Inc. James Howard: Research funding (paid to his institution) (Alexion AZ Rare Disease, argenx, Cartesian Therapeutics, Centers for Disease Control and Prevention, MGFA, Muscular Dystrophy Association, NIH, PCORI, UCB Pharma); honoraria/consulting fees (AcademicCME, Alexion AZ Rare Disease, argenx, Biologix Pharma, CheckRare CME, F. Hoffmann‐LaRoche Ltd, Horizon Therapeutics plc, Medscape CME, Merck EMD Serono, NMD Pharma, Novartis Pharma, PeerView CME, Physicians' Education Resource (PER) CME, PlatformQ CME, Regeneron Pharmaceuticals, Sanofi US, UCB Pharma, Zai Labs); non‐financial support (Alexion AZ Rare Disease, argenx, Cartesian Therapeutics, Toleranzia AB, UCB Pharma and Zai Labs).
EPO‐199
Efficacy and safety of nusinersen and risdiplam for adult spinal muscular atrophy: A systematic review and meta‐analysis
M. Mostafa Asla 1 ; A. Abdelsalam1; A. Ahmed Nawar1; A. Saad Isa2; M. Abdelazim Rizk1; W. A. Kamel3
1Faculty of Medicine‐University of Zagazig, Egypt; 2Al‐Azhar University, Faculty of Medicine, Damietta, Egypt; 3Neurology department, Faculty of Medicine, Beni‐Suef University, Egypt
Background and Aims: Nusinersen and risdiplam were approved by the US food and drug administration (FDA) for adult SMA patients. However, clinical evidence for their efficacy in adults are still inconclusive. We conducted this meta‐analysis to establish the clinical efficacy and safety of them on the adult patients.
Methods: A literature search was conducted using the Web of Science Library, Scopus, PubMed, Wiley, and Cochrane up to August 2023. Data were pooled for analysis using OpenMeta Analyst software for Windows.
Results: 29 studies met the eligibility criteria, including 25 studies related to nusinersen and only 4 studies related to risdiplam. After 6 months of follow‐up, nusinersen showed a statistically significant improvement of the HFMSE and the 6MWT. However, its effect on the RULM was not statistically significant. Regarding risdiplam, the findings of RULM showed a significant improvement during a year of follow‐up. Frequent adverse events included headache, back pain, nausea, infections, and vomiting, which were more likely related to the disease progression or the lumbar puncture procedure as in nusinersen treatment rather than the drugs themselves. No significant serious adverse effects were reported for either.
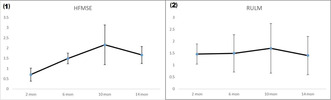
Linear graphs of the changes in the mean during the follow‐up periods of nusinersen on HFMSE and RULM.
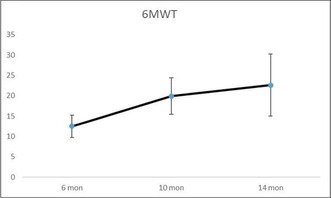
Linear graphs of the mean change during the follow‐up periods of nusinersen on 6MWT
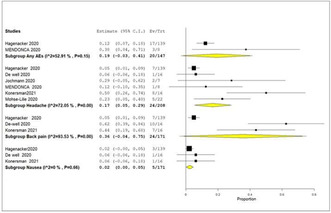
Reported Adverse effects at 6 months
Conclusion: Nusinersen can improve motor and respiratory functions in adult patients with SMA, and its effects become more pronounced with extended follow‐up periods. Risdiplam has shown promising results, but more clinical trials on adults with more sample size are needed. Both of nusinersen and risdiplam are generally tolerated and have an acceptable safety profile.
Disclosure: Nothing to disclose.
EPO‐200
Efficacy and safety of anti FcRN treatment in refractory MG: The UK experience of the Efgartigimod EAMS
J. Moniz Dionísio 1 ; N. Thambirajah2; P. Ambrose3; G. Burke4; M. Farrugia5; P. Garcia‐Reitboeck6; C. Hewamadduma7; T. Riswick7; S. Jacob8; D. Kullmann2; M. Hill9; M. Leite10; J. Miller11; A. Pinto4; J. Pritchard12; S. Sathasivam13; S. Viegas12; F. Norwood1; J. Spillane12
1Department of Neurology, Kings College Hospital London, UK; 2Department for Neuromuscular Disease, National Hospital for Neurology and Neurosurgery, Queen Square, UCLH, London, UK; 3Department of Clinical Neurology, University of Nottingham, Queen's Medical Centre, Nottingham, UK; 4Wessex Neurological Centre, Southampton General Hospital, Hampshire, UK; 5Institute of Neurological Sciences, Queen Elizabeth University Hospital, Glasgow, UK; 6St George's University Hospitals NHS Foundation Trust, London, UK; 7Department of Neuroscience, Sheffield Institute for Translational Neurosciences (SITRAN), University of Sheffield and Sheffield Teaching Hospitals Foundation NHS Trust, Sheffield, UK; 8Department of Neurology, University Hospitals Birmingham, Birmingham, UK; 9Department of Neurology, Morriston Hospital, Swansea, Wales, UK, 10Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, UK, 11Department of Neurology, Royal Victoria Infirmary, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle, UK, 12Division of Neurology, Imperial College London, UK, 13Department of Neurology, The Walton Centre, UK
Background and Aims: We report our experience of patients with generalised MG (gMG) treated with Efgartigimod an FCRN antagonist, under the early access to medicine scheme (EAMS) in the UK.
Methods: Data from all UK patients treated with Efgartigimod under the EAMS June 22‐July 23 were collected retrospectively. Efgartigimod was administered as per the ADAPT protocol (treatment cycle of 4 infusions at weekly intervals with further cycles given according to clinical need).
Results: 49 patients with AchR antibody positive gMG were treated in 12 centres. Most (76%) were female and most had a disease duration of over 10 years. The average MG‐ADL score at baseline was 11.2 (SD 3.2). Most (73%) patients had undergone thymectomy. 71.4% were taking prednisolone at baseline. All patients had utilized non‐steroidal immunosuppressant treatments, the average number tried was 4.3 (range 1–7) and 51% had received Rituximab. 57% of patients required regular IVIg/PLEX and 38% had required rescue IVIg/PLEX in the year before starting Efgartigimod. 77% of patients had a mean reduction in the MG‐ADL of ≥2 points in the first cycle and this remained stable throughout the study. The mean reduction in the MG‐ADL score in the 1st, 2nd, 3rd and 4th cycles were −4.5, −6.3, −6.9 and −7.8 respectively. Side effects were generally mild though one patient stopped treatment due to severe hypokalemia. No rescue treatments were required. At the end of the study 96% of patients remained on Efgartigimod.
Conclusion: Efgartigimod is a safe and effective treatment for patients with refractory, treatment resistant gMG.
Disclosure: J. Spillane: speaker fees and travel support from Argenx; advisory services to UCB.
EPO‐201
Navigating the triggers of fear and anxiety after diagnosis of Myasthenia Gravis
R. Govindarajan1; R. Rodriguez2; Z. Choudhry3; C. Brethenoux4; J. Pesa3; S. Ramchandren5; K. Gandhi6; K. Heerlein 7 ; N. Souayah8
1HSHS Medical Group Multispecialty Care – St. Elizabeth's, O'Fallon, IL, USA; 2Janssen Global Services, Commercial Data Science, Titusville, NJ, USA; 3Janssen Scientific Affairs, LLC, Titusville, NJ, USA; 4Human Dot Plus, TX, USA; 5Janssen R&D, LLC, Titusville, NJ, USA; 6Janssen Global, Commercial Strategy Organization, Titusville, NJ, USA; 7Janssen Global Services, Medical Affairs, Titusville, NJ, USA; 8Rutgers NJMS – Department of Neurology, Newark, NJ, USA
Background and Aims: As individuals living with Myasthenia Gravis (MG) have high rates of anxiety, we aimed to understand the experience of anxiety and its triggers among individuals discussing a recent diagnosis of MG online.
Methods: A research study was conducted using a proprietary AI‐powered methodology to examine English‐language public domain online conversations about MG from August 2022–August 2023.
Results: Of 9901 online conversations about MG, 33% (n = 3268) were immediately after diagnosis. Self‐described anxiety was expressed in 36% of posts (n = 1177) at diagnosis, which was 25% lower than at pre‐diagnosis (48%). Fear was discussed by 43% (n = 1405), an increase of ~13% from pre‐diagnosis (38%). Unknowns surrounding their future were discussed. Uncertainty (18%) was the most common anxiety trigger (n = 1177) and could be sub‐categorized into anxiety about diagnosis severity, not knowing the prognosis, and if symptoms will worsen. Symptom discomfort (13%) and fatigue (5%) were also important anxiety triggers. Fear (n = 1405) was primarily triggered by catastrophizing thoughts (21%), including fear of loss of function, limitations in lifestyle, and death. The fear about physical impact (14%) was driven by physical symptoms, discomfort, and fatigue. Other fears included financial impact (3%) and impact on relationships (5%).
Conclusion: Anxiety and fear are frequently experienced by individuals recently diagnosed with MG, primarily due to physical symptoms, uncertainty about the future, lifestyle impacts, and catastrophizing thoughts. These observations provide important insight that healthcare practitioners can consider when treating newly‐diagnosed MG, particularly the need for early symptom alleviation and mental health support.
Disclosure: Dr. Raghav Govindarajan is employed by HSHS Medical Group Multispecialty Care – St. Elizabeth's, O'Fallon, IL, USA. Rachelle Rodriguez, Jacqui Pesa, Zia Choudhry, Sindhu Ramchandren, Kavita Gandhi, and Kristin Heerlein are employees of Janssen Pharmaceuticals US, Inc., Titusville, NJ, USA. Caroline Brethenoux is employed by Human Dot Plus, TX, USA. Dr. Nizar Souayah is employed by Rutgers NJMS – Department of Neurology, Newark, NJ, USA.
EPO‐202
The impact of depression on quality of life for individuals with Myasthenia Gravis
N. Goyal1; R. Rodriguez2; Z. Choudhry3; C. Brethenoux4; J. Pesa3; S. Ramchandren5; K. Gandhi6; K. Heerlein 7 ; A. Anderson8
1Stanford Neuroscience Health Center, Palo Alto, CA, USA; 2Janssen Global Services, Commercial Data Science, Titusville, NJ, USA; 3Janssen Scientific Affairs, LLC, Titusville, NJ, USA; 4Human Dot Plus, TX, USA; 5Janssen R&D, LLC, Titusville, NJ, USA; 6Janssen Global, Commercial Strategy Organization, Titusville, NJ, USA; 7Janssen Global Services, Medical Affairs, Titusville, NJ, USA; 8Houston Methodist Hospital, Houston, TX, USA
Background and Aims: Individuals with myasthenia gravis (MG) have a higher prevalence of depression than the general population (1–4). Therefore, we aimed to evaluate the occurrence of online discussions related to MG, depression, and depression triggers.
Methods: A research study was conducted using a proprietary AI‐powered methodology to examine English‐language public domain online conversations about MG from August 2022–August 2023.
Results: Nearly 10,000 online conversations about MG were identified. One‐third of posts (33%; n = 3268) discussed experiences immediately following diagnosis. Self‐described depression was indicated in 21% (n = 686) of posts regarding recent diagnosis, representing a 50% increase from the period prior to diagnosis (14%). Out of all conversations (n = 3268), the progressive worsening of MG symptoms was the most common depression trigger (9%), and the impact of MG on quality of life (QoL) was the second most frequent depression trigger (6%). One individual shared a sentiment, "I long for my life as it used to be". A lower portion (4% of 3268) stated their depression was related to lack of control over various aspects of their life as a result of MG. Depression related to ineffective treatment experiences was also discussed (2%).
Conclusion: An increase in reported depression was observed at diagnosis compared to the pre‐diagnosis stage of MG in this social listening study. Depression was attributed to progressive worsening of symptoms and QoL, loss of control, and ineffective treatments. Healthcare practitioners can use this information to guide treatment decisions to improve symptom control and provide emotional support resources.
Disclosure: Dr. Neelam Goyal is employed by Stanford Neuroscience Health Center, Palo Alto, CA, USA, and reports advisory and consulting engagements from Alexion, Argenx, UCB/Ra Pharma, Janssen, Amgen, Lycia, as well as grant support from Argenx. Rachelle Rodriguez, Jacqui Pesa, Zia Choudhry, Sindhu Ramchandren, Kavita Gandhi, and Kristin Heerlein are employees of Janssen Pharmaceuticals US, Inc., Titusville, NJ, USA. Caroline Brethenoux is employed by Human Dot Plus, TX, USA. Dr. Ashley E.L. Anderson is employed by Houston Methodist Hospital, Houston, TX, USA. References: 1. WHO 2023. https://www.who.int/publications/i/item/depression‐global‐health‐estimates. 2. SAMHSA 2022. https://www.samhsa.gov/data/report/2021‐nsduh‐annual‐national‐report. 3. Nadali J, et al. Brain Behav. 2023;13(1):e2840. 4. Dewilde S, et al. BMJ Open. 2023;31;13(1):e066445.
EPO‐203
Interactive application for the study of neuromuscular jitter
A. Malanda 1 ; C. Valle1; D. Stashuk2; O. Garnés3; J. Rodríguez1; J. Navallas1
1Electrical, electronics and Communication Engineering Dept., Public University of Navarra. Spain; 2System Design Engineering Dept., University of Waterloo. Canada; 3Neurophysiology Service, Jiménez‐Díaz Foundation University Hospital
Background and Aims: This work presents a software application that incorporates the necessary features to perform jitter studies off‐line in a precise and efficient manner, so that comparative studies using manual jitter extraction procedures or new automatic methods can be conducted.
Methods: JitterAnalizer is a Matlab‐based application for manual jitter analysis (Fig. 1). Time alignment and jitter estimation (MCD, MSD, etc.) of motor unit potential trains (MUPTs) can be performed either by the peak method or by the flank method. Other functionalities include: selection of sampling frequency, elimination of non‐valid potentials, visualization of MUPTs in shimmer and raster modes, and results exportation.
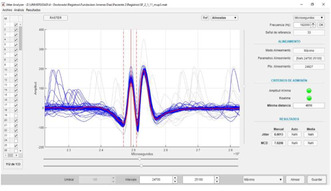
FIGURE 1 Interface of JitterAnalizer
Results: As a test example, EMG signals were recorded from 7 patients with pathologies of the neuromuscular junction or neuropathies. These signals were acquired using concentric facial needles and a Keypoint system. Jitter (MCD) measurements were then obtained from the Keypoint and from JitterAnalizer, using the peak method. Table 1 shows the statistical values of the jitter measurements obtained by each method from the 71 MUPTs that were taken as valid for the comparative study.
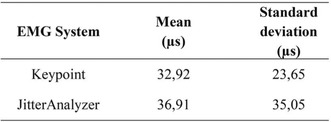
TABLE 1 Statistical results of the jitter measurements
Conclusion: JitterAnalizer has proved easy‐to‐use and fast. The statistical values of the jitter measurements obtained with the Keypoint and with JitterAnalizer are comparable. Their differences can be explained considering that the MUPTs presented to the two systems were not composed by exactly the same potentials.
Disclosure: This work has been funded by the Department of Health of the Government of Navarra (project GN2022/29) and by the Spanish Ministry of Science and Innovation (project PID2022‐136620OB‐I00).
EPO‐204
Comparison of manual methods in the measurement of neurophysiological jitter
A. Malanda 1 ; C. Valle1; D. Stashuk2; O. Garnés3; J. Navallas1; J. Rodríguez1
1Electrical, Electronics and Communication Engineering Department, Public University of Navarra, Spain; 2System Design Engineering Department, University of Waterloo, Waterloo, Canada; 3Neurophysiology Service, Jiménez‐Díaz Foundation University Hospital, Madrid, Spain
Background and Aims: The goal of this work is to compare the jitter measurements obtained by the peak method and the flank method in both small and large muscle recordings, in order to evaluate the equivalence of the two methods.
Methods: 238 EMG recordings taken from 22 patients were used for the study, following two different protocols: 1) single fiber EMG protocol, small muscles (frontalis), facial‐concentric electrodes; and 2) a similar protocol, large muscles (biceps, tibialis anterior, etc.), conventional concentric electrodes.
Results: Table 1 and Fig. 1 show statistical results of the jitter measurements obtained with both protocols, using the two methods. The Wilcoxon test was applied (0.05 significance level) and p‐values of 0.0002 and 0.0001 were obtained for protocol 1 and protocol 2, respectively, suggesting significant differences between the measurements obtained with the two methods. Linear regression models were also obtained, yielding high coefficients of determination (0.994 for protocol 1. and 0.991 for protocol 2), slope values close to 1 (0.989 and 0.992), and small intercept values (1.35 and 2.35 μs, respectively) (Fig. 2).
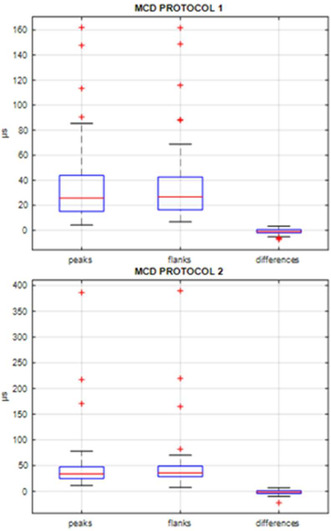
FIGURE 1 Boxplots of the jitter measurements obtained with the peak and the flank methods and the differences between them, for EMG recordings obtained from protocols 1 and 2.
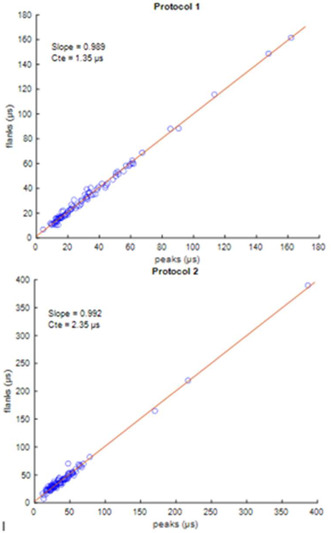
FIGURE 2 Regression models of the jitter measurements obtained with both methods in the two protocols.
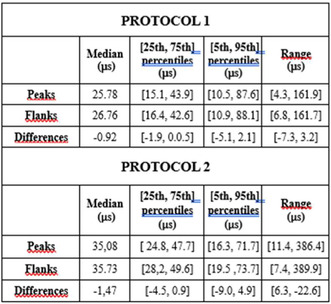
TABLE 1 Statistical parameters of jitter measurements obtained by the peak and the flank methods and their differences, for EMG recordings obtained from protocols 1 and 2.
Conclusion: Although the jitter measurements obtained with the two methods were statistically different for both protocols, this difference seems to be small and not too relevant from a clinical viewpoint. However, in some isolated cases, the difference in their measurements may be high, which could affect the diagnosis.
Disclosure: This work has been funded by the Department of Health of the Government of Navarra (project GN2022/29) and by the Spanish Ministry of Science and Innovation (project PID2022‐136620OB‐I00).
EPO‐205
Myocarditis/myositis/myasthenia gravis overlap syndrome: Description of three patients
M. Domine; M. Olivé Plana; B. Albertí Vall; N. Blanco Sanroman; M. Coronel Coronel; R. Sainz Torres; M. Borrell Pichot; T. Mederer Fernández
Neurology Department, Hospital de la Santa Creu I Sant Pau, Barcelona, Spain
Background and Aims: Immune checkpoint inhibitors (ICIs) have revolutionized the treatment of tumors with a poor prognosis. Despite their high effectiveness, these therapies are associated with a broad spectrum of adverse effects, including the overlap syndrome of myocarditis/myositis/myasthenia gravis (IM3OS Syndrome).
Methods: We report on three patients undergoing treatment with ICIs (pembrolizumab and nivolumab). The first patient presented with binocular diplopia and ptosis. The second patient complained of muscle weakness, diplopia, chest pain, and recurrent syncope. The third patient was asymptomatic but was referred due to elevated CK levels.
Results: In all three patients, serum CK levels (>1000 IU/L) and troponins (>200 ng/L) were elevated. Whole‐body muscle MRI was normal. EMG showed spontaneous activity at rest and myopathic patterns suggestive of inflammatory myopathy. The repetitive nerve stimulation test was normal. AntiRACh and anti‐MUSK (anti‐receptor tyrosine kinase) antibodies were positive only in one of the patients. Muscle biopsy revealed inflammatory myopathy. Two patients received corticosteroid therapy, intravenous immunoglobulins, and pyridostigmine. The second patient also required a pacemaker implantation due to complete atrioventricular block and ultimately succumbed to respiratory failure. The third patient only required corticosteroid treatment.
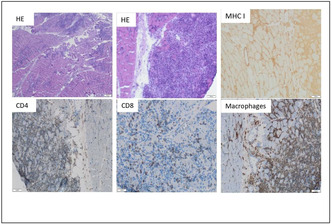
Patient 1. Biopsy of the right quadriceps
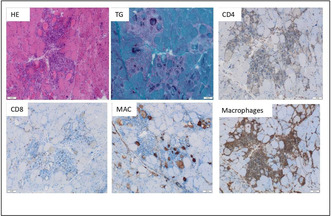
Patient 2. Biopsy of the brachial biceps muscle.
Conclusion: An increased incidence of IM3OS Syndrome has been observed in patients treated with ICIs, associated with high mortality. The presence of any of the symptoms should alert to the possibility of coexistence of others. Early diagnosis is essential for the management and prevention of potentially fatal complications.
Disclosure: Nothing to disclose.
EPO‐206
Efgartigimod consistently improved health‐related quality of life in AChR‐Ab+ participants with gMG in IV and SC trials
F. Saccà 1 ; J. L. De Bleecker2; K. Utsugisawa3; D. Korobko4; S. Steeland5; B. Van Hoorick5; R. Kerstens5; J. Podhorna5; A. Meisel6; R. Mantegazza7
1NRSO Department, Genesis Center, Federico II University of Naples, Naples, Italy; 2Department of Neurology, Ghent University Hospital, Ghent, Belgium; 3Department of Neurology, Hanamaki General Hospital, Hanamaki, Japan; 4State Budgetary Healthcare Institution of Novosibirsk Region “State Novosibirsk Regional Clinical Hospital,” Novosibirsk, Russian Federation, 5argenx, Ghent, Belgium; 6Department of Neurology and Neuroscience Clinical Research Center, Charité – Universitätsmedizin Berlin, Berlin, Germany; 7Department of Neuroimmunology and Neuromuscular Diseases, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy
Background and Aims: Myasthenia gravis (MG) causes substantial burdens on patient health‐related quality of life (HRQoL). Recent MG guidelines indicate that therapeutic goals should aim for the best possible disease control, with the best possible preservation/restoration of QoL. Here we report HRQoL outcomes from efgartigimod‐treated, AChR‐Ab+ generalised MG (gMG) participants in the completed, placebo‐controlled, Phase 3 ADAPT (IV) and ongoing, open‐label extension ADAPT‐SC+ (SC) trials.
Methods: Efgartigimod was administered via IV infusion (10mg/kg) or SC injection (coformulated with recombinant human hyaluronidase PH20; 1000mg), in cycles of 4 once‐weekly administrations. Subsequent cycles were initiated > = 5 weeks (ADAPT) or > = 4 weeks (ADAPT‐SC+) from last dose based on clinical evaluation. HRQoL was assessed by validated MG‐specific (MG‐QoL15r) and general (EQ‐5D‐5L VAS) scales.
Results: Demographics/baseline characteristics for AChR‐Ab+ participants are in Table 1. In ADAPT, efgartigimod‐treated AChR‐Ab+ participants (n = 63) showed statistically significant improvements in HRQoL versus placebo (n = 60). Mean (SE) MG‐QoL15r score decreased from baseline to week 4, cycle 1: efgartigimod, –7.3 (0.79); placebo, –2.3 (0.51). Mean (SE) EQ‐5D‐5L VAS score increased from baseline to week 4, cycle 1: efgartigimod, 15.8 (2.20); placebo, 4.1 (1.64)(Fig.1). Improvements in QoL were consistent in ADAPT‐SC+, with peak mean (SE) changes from baseline in MG‐QoL15r and EQ‐5D‐5L VAS scores of –5.1 (0.44) and 13.8 (1.54), respectively, at week 4, cycle 1 (Fig. 1). In ADAPT‐SC+, MG‐QoL15r and EQ‐5D‐5L VAS cycle baseline scores improved with subsequent cycles, indicating durable QoL improvements.
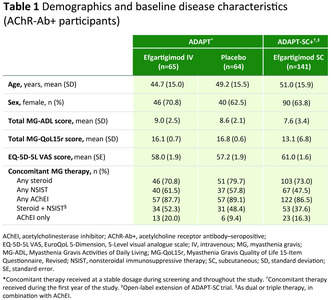
TABLE 1
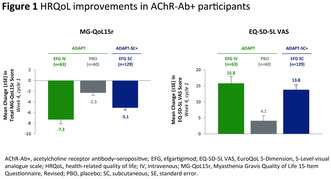
FIGURE 1
Conclusion: Efgartigimod IV/SC demonstrated consistent and meaningful improvements in QoL across clinical trials in AChR‐Ab+ gMG, achieving an important treatment goal for these participants.
Disclosure: FS: Agenzia Italiana del Farmaco, Alexion, Almirall, argenx, Dianthus, Friedrich's Ataxia Research Alliance, Genpharm, Immunovant, Leadiant Biosciences, Lexeo Therapeutics, Madison Pharma, Medpharma, Novartis, Prilenia, Reata, Sandoz, Sanofi, Zai Lab. JLDB: Alexion, Alnylam, argenx, CSL, Janssen, Sanofi Genzyme, UCB. KU: Alexion, argenx, Chugai, Horizon, Janssen, Japan Blood Products Organisation, Mitsubishi Tanabe, UCB, Viela Bio. DK: argenx, BIOCAD, Bristol Myers Squibb, Horizon, Janssen, Merck, Novartis Russia, Roche, Sanofi, UCB. SS, BVH, RK and JP: Employees of argenx. AM: Alexion, argenx, German Myasthenia Gravis Society, Grifols, Hormosan, Janssen, Merck, Octapharma, UCB, Vitaccess. RM: Alexion, argenx, Biogen, BioMarin, Catalyst, Merck, Roche, Teva, UCB.
EPO‐207
Eculizumab as rescue therapy in two gMG patients with worsening symptoms while on Efgartigimod
N. Cuomo; A. Sarnataro; A. Marsili; G. Puorro; M. Campanile; C. Pane; F. Saccà
Department of Neurosciences, Reproductive and Odontostomatological Sciences – Federico II University – Naples
Background and Aims: Eculizumab and Efgartigimod are available for refractory anti‐AChR+ gMG. We describe two cases who suffered a relapse while on Efgartigimod, rescued with Eculizumab.
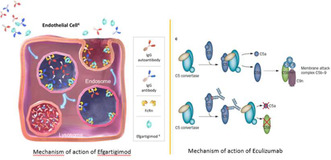
Efgartigimod and Eculizumab mechanisms of action
Methods: Case 1: A 46 yo woman treated with thymectomy, pyridostigmine, prednisone, azathioprine, IVIg. In December 2022 she started Efgartigimod IV (10 mg/kg weekly for four weeks, every two months). Her MG‐ADL and qMG were 5 and 16. Case 2: A 47 yo woman treated with thymectomy, pyridostigmine, prednisone and azathioprine. In November 2022 she started Efgartigimod. Her MG‐ADL and qMG were 8 and 17.
Results: Case 1: After the first cycle her MG‐ADL and qMG dropped to 1 and 11 and remained stable, until, during the third cycle (18th week) she worsened (MG‐ADL 9, qMG 20). We discontinued Efgartigimod and started Eculizumab (900 mg iv weekly for 4 weeks, followed by 1200 mg from the fifth week and every two weeks). Her MG‐ADL dropped to 5 and at the fifth week her MG‐ADL and qMG were 1 and 14. Case 2: After the first Efgartigimod cycle her MG‐ADL and qMG were 2 and 10. 48 weeks later her symptoms worsened (MG‐ADL 11 and qMG 16). We stopped Efgartigimod and started Eculizumab: after the first infusion her MG‐ADL was 2 and at the beginning of the maintenance phase her MG‐ADL and qMG were 0 and 5.
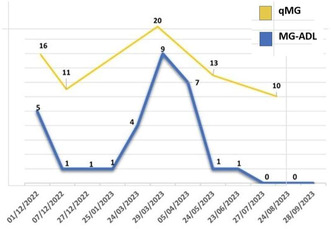
Case 1 – MG‐ADL and qMG scores
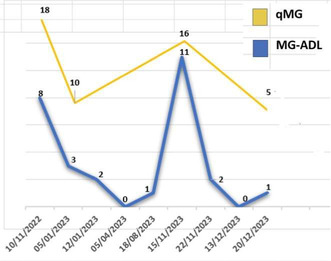
Case 2 – MG‐ADL and qMG scores
Conclusion: As far as we know, these are two of the first reports of Eculizumab as rescue therapy in patients not responding to Efgartigimod.
Disclosure: Nothing to disclose.
EPO‐208
Dysferlinopathies: Insights from two Portuguese tertiary centers
R. Lopes 1 ; A. Ferreira2; D. Barros3; E. Vieira4; A. Gonçalves5; M. Oliveira5; R. Santos6; R. Maré2; A. Sousa7; M. Pinto8; M. Cardoso7; T. Coelho7
1Neurology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 2Neurology Department, Hospital de Braga, Braga, Portugal; 3Radiology Department, Hospital de Braga, Braga, Portugal; 4Medical genetics Department, Centro de Genética Médica Jacinto Magalhães, Centro Hospitalar Universitário de Santo António (CHUdSA), Porto, Portugal; 5Unidade Multidisciplinar de Investigação Biomédica (UMIB), Instituto de Ciências Biomédicas Abel Salazar (ICBAS), University of Porto, Porto, Portugal; 6European Reference Center of Neuromuscular Diseases (EURO‐NMD), Centro Hospitalar Universitário de Santo António (CHUdSA), Porto, Portugal; 7Neurophisiology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal; 8Neuropathology Department, Centro Hospitalar Universitário de Santo António, Porto, Portugal
Background and Aims: Dysferlinopathies constitute a subgroup of rare autosomal recessive muscular dystrophies characterized by high phenotypic and genetic heterogeneity. We aimed to characterize the adult patient population with dysferlinopathy from two Portuguese centers.
Methods: Retrospective analysis of patients with a molecular diagnosis of dysferlinopathy followed in an outpatient setting. Recording of demographic, clinical, laboratory, imaging and molecular data were used.
Results: Twenty‐one patients from 19 families were identified (male‐to‐female ratio 1.65:1) with an average age of 48.3 years and symptom onset at 23 ± 9 years. Fifteen different pathogenic variants were identified in the DYSF gene (2 homozygous, 9 compound heterozygous). Most patients reported symptoms in the 20 years preceding molecular diagnosis. Eleven (52%) underwent muscle biopsy, with most showing absence of dysferlin staining. Fourteen patients presented with limb‐girdle muscular dystrophy type R2 (LGMDR2) phenotype, two with Miyoshi myopathy, two with distal anterior compartment myopathy, two with hyperCKemia, and one with proximodistal. Fifteen patients progressed to generalized weakness. At an average of 26 years of disease progression, 11 patients (52%) were unable to walk, and 14% required walking aids. Four patients reported dyspnea, 8 with abnormal respiratory function tests, and 3 with cardiomyopathy. Initial CK levels were globally elevated (average 4,953 U/L). Muscle MRI, performed in 4 patients, revealed a similar pattern of adipose infiltration.
Conclusion: Our findings are consistent with the existing literature, demonstrating a diverse spectrum of phenotypes, onset patterns, and progression rates. Given the described clinical and molecular heterogeneity, the ongoing progress in molecular genetic techniques have facilitated a more rapid and definitive diagnosis.
Disclosure: Nothing to disclose.
EPO‐209
Efficacy and safety of Efgartigimod IV and PH20 SC in gMG: analysis of AChR‐Ab− participants in ADAPT+/ADAPT‐SC+
S. Hoffmann 1 ; J. F. Howard; Jr2; T. Vu3; J. L. De Bleecker4; K. Utsugisawa5; H. Murai6; F. Saccà7; D. Korobko8; C. T’joen9; S. Steeland9; B. Van Hoorick9; J. Podhorna9; A. Meisel10; R. Mantegazza11
1Department of Neurology with Experimental Neurology, and the Neuroscience Clinical Research Center, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt Universität, Berlin, Germany; 2Department of Neurology, The University of North Carolina, Chapel Hill, North Carolina, USA; 3Department of Neurology, University of South Florida Morsani College of Medicine, Tampa, Florida, USA; 4Department of Neurology, Ghent University Hospital, Ghent, Belgium; 5Department of Neurology, Hanamaki General Hospital, Hanamaki, Japan; 6Department of Neurology, School of Medicine, International University of Health and Welfare, Tokyo, Japan; 7NRSO Department, Genesis Center, Federico II University of Naples, Naples, Italy; 8State Budgetary Healthcare Institution of Novosibirsk Region "State Novosibirsk Regional Clinical Hospital," Novosibirsk, Russian Federation, 9argenx, Ghent, Belgium, 10Department of Neurology with Experimental Neurology, Integrated Myasthenia Gravis Center, Neuroscience Clinical Research Center, Charité Universitätsmedizin Berlin, Berlin, Germany, 11Department of Neuroimmunology and Neuromuscular Diseases, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy
Background and Aims: Efgartigimod, a human IgG1 antibody Fc fragment, reduces IgG autoantibody levels by blocking the neonatal Fc receptor. AChR‐Ab− patients comprise 15–20% of the generalised myasthenia gravis (gMG) population but have limited treatment options. Efficacy (AChR‐Ab− participants) and safety (overall population) from the completed, Phase 3 ADAPT+ (IV) and ongoing, open‐label extension ADAPT‐SC+ (SC) trials are reported.
Methods: Efgartigimod was administered via IV infusion (10mg/kg [ADAPT+]) or SC injection (coformulated with recombinant human hyaluronidase PH20; 1000mg [ADAPT‐SC+]) in cycles of 4 once‐weekly administrations. Subsequent cycles were initiated based on clinical evaluation. Efficacy was assessed using MG‐ADL scores from final (ADAPT+) and interim (ADAPT‐SC+; cut‐off December 2022) analyses.
Results: Demographics/baseline characteristics were similar between AChR‐Ab− and AChR‐Ab+ populations (Table 1). Efgartigimod improved total mean (SE) MG‐ADL scores in AChR‐Ab− participants (week 3, cycle 1): ADAPT+, –5.3 (0.74); ADAPT‐SC+, –3.5 (0.51), with most achieving clinically meaningful improvements (ADAPT+: 79.4%; ADAPT‐SC+: 67.6%). MG‐ADL score improvements were consistent across multiple cycles (Fig.1). A subset of AChR‐Ab− participants achieved minimal symptom expression (MSE) at any time during cycle 1 (ADAPT+: 26.5%; ADAPT‐SC+: 13.2%). Proportions achieving MSE were consistent across multiple cycles in both trials. Efgartigimod was well tolerated, and most adverse events (AEs) were mild/moderate in severity. The most frequent AEs were headache (24.8%, 20.1%), nasopharyngitis (13.8%, 15.6%) and COVID‐19 (12.4%, 22.3%) in ADAPT+ and ADAPT‐SC+, respectively (Table 2). Reported deaths (ADAPT+: n = 5; ADAPT‐SC+: n = 4) were unrelated to treatment.
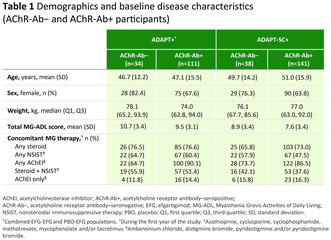
TABLE 1
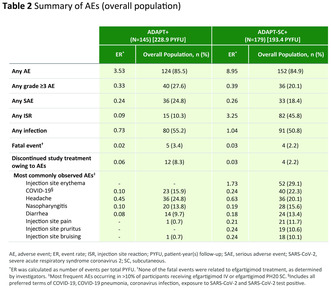
TABLE 2
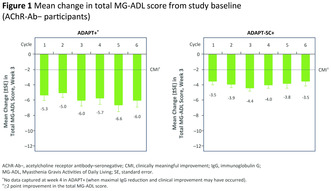
FIGURE 1
Conclusion: Efgartigimod was well tolerated and provided clinically meaningful improvements in AChR‐Ab− gMG participants across IV and SC trials.
Disclosure: SH: Alexion, argenx, UCB JFH: Academic CME, Ad Scientiam, Alexion, AstraZeneca Rare Disease, argenx, Biologix, Cartesian Therapeutics, Centers for Disease Control and Prevention, CheckRare CME, F. Hoffmann‐LaRoche Ltd, Amgen, Medscape CME, Merck EMB Serono, MGFA, Muscular Dystrophy Association, NIH, NMD Pharma, Novartis, PCORI, PeerView CME, Physicians' Education Resource (PER) CME, PlatformQ CME, Regeneron Pharmaceuticals, Sanofi US, Toleranzia AB, UCB, Zai Lab TV: AbbVie, Alexion, argenx, AstraZeneca, Cartesians Therapeutics, CSL Behring, Dianthus, Horizon, Immunovant, ImmunoAbs, Janssen, Sanofi Genzyme, UCB JLDB: Alexion, Alnylam, argenx, CSL, Janssen, Sanofi Genzyme, UCB KU: Alexion, argenx, Chugai, Horizon, Janssen, Japan Blood Products Organisation, Mitsubishi Tanabe, UCB, Viela Bio HM: Alexion, argenx, AstraZeneca, Chugai, Japan Blood Products Organisation, Ministry of Health, Labour and Welfare of Japan, Roche, UCB FS: Agenzia Italiana del Farmaco, Alexion, Almirall, argenx, Dianthus, Friedrich Ataxia Research Alliance, Genpharm, Immunovant, Lediant, Lexeo therapeutics, Madison, Medpharma, Novartis, Prilenia, Reata, Sandoz, Sanofi, Zai Lab DK: argenx, BIOCAD, Bristol Myers Squibb, Horizon, Janssen, Merck, Novartis, Roche, Sanofi, UCB CT’j, SS, BVH, JP: Employees of argenx AM: Alexion, argenx, German Myasthenia Gravis Society, Grifols, Hormosan, Janssen, Merck, Octapharma, UCB, Vitaccess RM: Alexion, argenx, Biogen, BioMarin, Catalyst, Merck, Roche, Teva, UCB.
EPO‐210
Achievement of minimal symptom expression in participants treated with Efgartigimod in ADAPT+ and ADAPT‐SC+
S. Hoffman 1 ; S. Muppidi2; J. Howard Jr.3; H. Murai4; G. Phillips5; C. Qi5; D. Gelinas5; E. Brauer5; S. Zhao5; V. Bril6; J. Vissing7; J. Verschuuren8; R. Mantegazza9; ADAPT and ADAPT‐SC Study Groups10
1Department of Neurology and NeuroCure Clinical Research Center, Charité – Universitätsmedizin Berlin, Berlin, Germany; 2Stanford Healthcare, Palo Alto, California, USA; 3Department of Neurology, The University of North Carolina, Chapel Hill, North Carolina, USA; 4Department of Neurology, School of Medicine, International University of Health and Welfare, Tokyo, Japan, 5argenx, Ghent, Belgium; 6Ellen & Martin Prosserman Centre for Neuromuscular Diseases, University Health Network, Toronto, Ontario, Canada; University of Toronto, Toronto, Ontario, Canada; 7Copenhagen Neuromuscular Center, Rigshospitalet, University of Copenhagen, Denmark; 8Department of Neuroimmunology and Neuromuscular Diseases, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy; 9Department of Neuroimmunology and Neuromuscular Diseases, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy
Background and Aims: Efgartigimod, a human IgG1 antibody Fc‐fragment, reduces IgG levels through neonatal Fc receptor blockade. Efgartigimod has been investigated in the treatment of generalised myasthenia gravis (gMG) through intravenous (IV) and subcutaneous (SC, coformulated with recombinant human hyaluronidase PH20) administration in the ADAPT/ADAPT+ and ADAPT‐SC/ADAPT‐SC+ studies, respectively. A key efficacy indicator in gMG treatment is MG‐ADL score improvement. Minimal symptom expression (MSE, MG‐ADL total score of 0 or 1) is explored as a novel proposed treatment target in gMG.
Methods: The proportion of acetylcholine receptor antibody positive (AChR‐Ab+) participants in ADAPT+ (n = 111) and ADAPT‐SC+ (n = 141) to achieve MSE was assessed.
Results: In ADAPT, MSE was achieved in 44.6% of efgartigimod‐treated participants vs 10.9% of placebo‐treated participants at any time point up to 3 cycles. In ADAPT+, the number of participants achieving MSE at any time in up to 19 cycles was 40.5%. Eighty‐one percent of efgartigimod‐treated participants who achieved MSE in ADAPT also achieved MSE during ADAPT+; 23% who had not achieved MSE in ADAPT did so in ADAPT+. In ADAPT‐SC, 45.5% and 41.3% of participants receiving efgartigimod PH20 SC or efgartigimod IV achieved MSE at any time in cycle 1, respectively. In ADAPT‐SC+, the number of participants achieving MSE at any time in up to 9 cycles was 54.6%. Clinical improvements may not have been fully captured in OLEs (ADAPT+/ADAPT‐SC+) due to the limited number of assessment timepoints.
Conclusion: Achievement of MSE was consistently seen across cycles in AChR‐Ab+ participants of both ADAPT+ and ADAPT‐SC+, similar to results demonstrated in ADAPT and ADAPT‐SC.
Disclosure: Multiple relationships financial and non‐financial nature for authors SH, SP, JFH, HM, GP, CQ, DG, EB, SZ, VB, JV, JVV, and RM stated at point of presentation.
Sunday, June 30, 2024
Ageing and dementia 2
EPO‐211
Knockdown of hippocampal calponin‐3 alleviates memory impairment and Aβ deposition in APP/PS1 mice
W. Yang; Y. Han; L. Chen; K. Wang
First Department of Neurology, First Affiliated Hospital, Kunming, Yunnan, China
Background and Aims: Alzheimer's disease (AD) is characterized by progressive cognitive decline, with senile plaques of beta‐amyloid (Aβ). Calponin‐3, encoded by CNN3, is highly expressed in the brain and regulates cytoskeletal reorganization and dynamics as well as actin interactions through efficient binding to F‐actin, thereby controlling dendritic spine morphology, density and plasticity.
Methods: Adenovirus with calponin‐3 knockdown or control virus were injected into the hippocampi of APP/PS1 mice to construct APP/PS1‐CNN3‐KD or APP/ PS1‐CNN3‐Ctrl mice. The expression of calponin‐3 in the hippocampi of experimental mice were confirmed by western blot and Immunofluorescence (IF). Cognitive function of mice were tested by novel object recognition testing(NOR)for working memory, and object location recognition testing(OLR)and morris water maze (MWM) for spatial memory.
Results: The level of hippocampal calponin‐3 of 4‐, 6‐ and 9‐month old APP/PS1 mice were significantly higher than those of wide type (WT) mice at the same age. IF revealed that calponin‐3 distributed in clusters and colocalized with Aβ in the hippocampi of APP/PS1 mice. 7‐month old APP/PS1‐CNN3‐KD mice showed significantly better the working memory and spatial memory, and reduced Aβ deposition and β secretase enzyme 1 (BACE1) levels than APP/ PS1‐CNN3‐Ctrl mice.
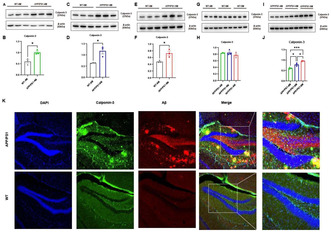
FIGURE 1

FIGURE 2
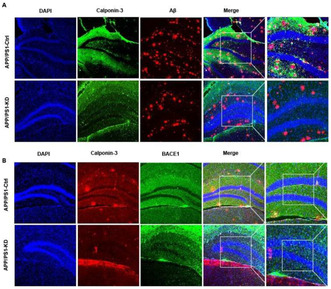
FIGURE 3
Conclusion: Knockdown of hippocampal calponin‐3 can improve working and spatial memory and alleviate deposition of Aβ in APP/PS1 mice. Abnormally up‐regulation of hippocampal calponin‐3 may involve in pathogenesis of AD.
Disclosure: Nothing to disclose.
EPO‐212
Randomized, placebo‐controlled, multiple ascending dose study of NX210c safety/tolerability and PK/PD in the elderly
D. Dumas1; J. Le Douce2; S. Marie2; P. Kremer1; F. Sips3; P. Bambury4; G. Pasculli4; R. Bursi3; Y. Godfrin2; S. Lemarchant2; A. Janus 2
1Centre for Human Drug Research, Leiden, The Netherlands; 2Axoltis Pharma, Lyon, France; 3InSilicoTrials Technologies B.V., s’ Hertogenbosch, The Netherlands; 4InSilicoTrials Technologies S.p.A, Trieste, Italy
Background and Aims: Blood‐brain barrier (BBB) dysfunction underlies various neurodegenerative diseases (NDD). NX210c is an oligopeptide that reduces blood‐brain barrier (BBB) permeability via claudin‐5, supports neuroprotection and promotes synaptic transmission in preclinical models. multiple A multiple ascending dose (MAD) study assessed safety and tolerability of intravenously (IV) administered NX210c (at 5 and 10 mg/kg) in healthy elderly volunteers (HEV) with secondary and exploratory objectives to assess blood pharmacokinetics (PK) and pharmacodynamic (PD) parameters, respectively, including blood biomarkers relevant to NDD.
Methods: We report results of a randomized, double‐blind, placebo‐controlled, MAD study of two doses of NX201c in HEVs run in a single centre with two cohorts of 15 HEVs randomized (4:1 ratio) to NX210c dose or placebo 3x/week (w) for 4w with a follow‐up visit 2w after last dosing.
Results: Of 29 HEV randomized, 20 registered 73 treatment‐emergent adverse events with all possibly related adverse events mild and no serious adverse events or evidence of NX210c accumulation. According to modelling data, NX210c treatment demonstrated a robust PK/PD relationship, characterized by inhibition of claudin‐5, NfL, and SPARCL‐1 production, as well as degradation of homocysteine.
Conclusion: NX210c demonstrated a good safety profile following multiple doses in HEV and showed a PD relationship for biomarkers relevant to the BBB, including a reduction of plasma claudin‐5. As BBB disruption is a driving feature of NDD, NX210c effect on target biomarkers may represent an important disease‐modifying treatment for several neurological disorders and warrants further study in patients with NDD.
Disclosure: DD and PK are employed by CHDR. JLD, SM, SL and AJ are employed by Axoltis Pharma. YG is a shareholder of Axoltis Pharma.
EPO‐213
Neuropathological, clinical and genetic comparison of four peculiar FTLD cases from the Abbiategrasso Brain Bank
A. Gatti 1 ; G. Negro2; C. Calatozzolo3; V. Medici4; X. Profka3; A. Costa1; E. Poloni3
1IRCCS “C. Mondino” Foundation, National Neurological Institute, Department of Behavioral Sciences, University of Pavia, Italy; 2Department of Neurology and School of Medicine and Surgery, University of Milano Bicocca, Monza; Italy Department of Neuropathology, Golgi‐Cenci Foundation, Abbiategrasso, Italy; 3Department of Neurology and Neuropathology, Golgi‐Cenci Foundation, Abbiategrasso, Milan, Italy; 4Department of Translational Medicine, University of Eastern Piedmont, Novara, Italy
Background and Aims: The spectrum of fronto‐temporal lobar degeneration (FTLD) encompasses several proteinopathies and clinico‐pathological features: (1) heterogeneous clinical presentations; (2) heterogeneous neuropathology; (3) involvement of many genes; (4) atrophy of the frontal and/or temporal cortex. The aim of the study is to present four emblematic cases in order to emphasize the clinical and pathological heterogeneity of FTLD.
Methods: We followed four subjects with major‐neurocognitive disorder (major‐NCD), belonging to the Abbiategrasso Brain Bank, and analyzed the neuropathology of their brains.
Results: Case 1 – Major‐NCD: nfv‐PPA/CBS: progressive non‐fluent aphasia (nfPPA), apraxia, disinhibition, apathy, hyperorality, severe right hemiparkinsonism and dystonia; neuroimaging: asymmetrical left frontal atrophy; neuropathology: prevalent type A TDP‐43 histopathology, limbic co‐localization of synuclein pathology and low AD pathology. Case 2 – Major‐NCD: behavioral variant FTD (bvFTD): spatial disorientation, wandering, disinhibition, delusions, apathy, hyperorality, postural instability and bilateral parkinsonism; neuroimaging: asymmetrical right temporo‐parieto‐occipital atrophy; neuropathology: pure type A TDP‐43 histopathology. Case 3 – Major‐NCD: frontal variant AD (fvAD): logopenic language impairment, progressive memory loss, social withdrawal, apathy, aggressivity, wandering, sleep disturbances, delusions, hallucinations, bilateral rigid‐hypokinetic parkinsonism in the advanced stages; neuroimaging: symmetrical fronto‐temporal atrophy; neuropathology: predominant AD pathology, limbic co‐localization of synuclein pathology and mild TDP‐43 pathology. Case 4 – Major‐NCD: semantic variant FTD (svFTD): spatial disorientation, fluent aphasia with comprehension and naming deficits, delusions, wandering, aggressivity, postural instability and rigid‐hypokinetic parkinsonism; neuroimaging: symmetrical temporal atrophy; neuropathology: predominant AD pathology.
Conclusion: The clinical‐pathological comparison of these four cases demonstrates the heterogeneity of FTLD and the essential role of neuropathology in determination of definitive diagnosis of neurodegenerative diseases.
Disclosure: Nothing to disclose.
EPO‐214
CSF biomarkers of Alzheimer's disease, neuropsychological tests and UPDRS‐III in patients with Parkinson's disease
A. Scalese; G. Giuffrè; T. Morganti; F. Musso; A. Cimmino; G. Di Lazzaro; D. Quaranta; C. Marra; P. Calabresi
Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy; Institute of Neurology, Catholic University of the Sacred Heart, Rome, Italy
Background and Aims: CSF biomarkers of amyloidopathy (Aβ42 and Aβ42/40), tauopathy (p‐tau) and neurodegeneration (t‐tau) have been widely used as a measure of Alzheimer's disease (AD) pathology in vivo and as a predictor of cognitive impairment in AD. These biomarkers have been proven to predict cognitive decline in PD as well. We aimed to assess the associations between CSF biomarkers of AD pathology and cognitive/motor impairment in a cohort of PD patients.
Methods: We recruited 45 subjects with diagnosis of PD. A lumbar puncture (LP) was performed and CSF biomarkers of AD were quantified. At the time of LP, a complete neuropsychological battery and UPDRS‐III motor scale were used to assess cognitive and motor domains respectively. A 12–24 months follow‐up UPDRS‐III was available for every patient. Correlations between CSF biomarkers, neuropsychological tests and UPDRS‐III at the time of LP and after 12–24 months were carried out.
Results: Our results revealed a significant correlation between biomarkers of amyloidopathy and poorer performances in MMSE, RAVLT delayed recall, Spatial Span, Raven matrices, MFTC, semantic verbal fluency, ROCF delayed. Aβ42/40 was found to predict the change between the UPDRS‐III score at the baseline and follow‐up.
Conclusion: Amyloidopathy is a frequent PD co‐pathology. This study highlighted the role of CSF biomarkers of amyloidopathy as a tool to predict worse performances in some common neuropsychological tests. Furthermore, Aβ42/40 showed potential in identifying PD patients at risk of accelerated motor decline, suggesting a possible synergistic role of Aβ42 with alpha‐synuclein in the clinical progression of Parkinson disease.
Disclosure: Nothing to disclose.
EPO‐215
Genetically proxied PDE5 inhibition and risk of dementia: A drug target Mendelian randomisation study
S. Brennan; A. Tinworth
The Mater Misericordiae University Hospital
Background and Aims: Phosphodiesterase‐5 (PDE5) inhibitors have gained interest as a potential treatment for dementia. However, current evidence is limited to observational and pre‐clinical studies. This drug‐target Mendelian Randomisation (MR) study aims to elucidate the on‐target effects of pharmacological PDE5 inhibition on dementia subtypes, cognitive traits, and neuro‐imaging phenotypes.
Methods: Two independent (r 2 < 0.001) blood pressure lowering variants from around the PDE5A locus were used in two‐sample MR to assess the effect of genetically proxied PDE5 inhibition on risk of dementia subtypes, cognitive performance, and neuroimaging traits (cortical thickness, surface area and volume of white matter hyperintensities) in large‐scale genomic consortia. The instrument's predictive validity was assessed against erectile dysfunction and pulmonary arterial hypertension (PAH) as positive controls.
Results: Following correction for multiple comparisons, genetically proxied PDE5 inhibition was associated with lower odds of erectile dysfunction (OR 0.85, 95% CI 0.83–0.87) and PAH (OR 0.58, 95% CI 0.55–0.61), and higher odds of Alzheimer's disease (OR 1.07, 95% CI 1.04–1.10), Lewy body dementia (OR 1.20, 95% CI 1.17–1.23) and vascular dementia (OR 1.04, CI 1.02–1.07). Furthermore, genetically proxied PDE5 inhibition was associated with reduced cortical thickness (SD change −0.003, 95% CI −0.004, −0.002) and cognitive performance (SD change −0.010, 95% CI −0.013, −0.007), but not cortical surface area or volume of white matter hyperintensities.
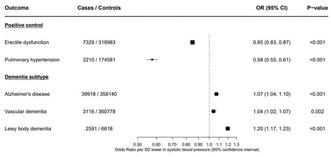
FIGURE 1 Forest plot depicting Mendelian randomisation estimates for genetically proxied PDE5 inhibition and associations with positive controls and dementia subtypes (Bonferroni correction: p < 0.0036 for statistical significance)
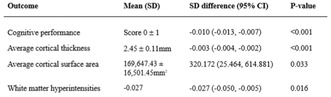
TABLE 1 Mendelian randomisation estimates for genetically proxied PDE5 inhibition and associations with cognitive traits and neuro‐imaging phenotypes (Bonferroni correction: p < 0.0036 for statistical significance)
Conclusion: In contrast to evidence from observational studies, our findings indicate that inhibition of PDE5 is associated with higher risk of dementia, and an unfavourable neurocognitive profile. This risk should be further investigated prior to clinical trials of pharmacological PDE5 inhibition in the treatment and prevention of dementia.
Disclosure: The author Alexander Tinworth may receive support from the Nuffield Department of Population Health at the University of Oxford or his scholarship benefactor, the British Heart Foundation to attend conferences but has not received financial or academic support in the conducting or writing of the study.
EPO‐216
Identification of novel dysregulated proteins in Alzheimer's disease patients with therapeutic and diagnostic potential
A. Montero‐Calle 1 ; R. Coronel2; V. de los Ríos3; A. Peláez‐García4; M. Fernández‐Aceñero5; J. Martínez‐Useros6; M. Mendes7; I. Liste2; R. Barderas1
1Chronic Disease Programme (UFIEC), Instituto de Salud Carlos III, Majadahonda, Madrid, Spain; 2Unidad de Regeneración Neural, Unidad Funcional de Investigación de Enfermedades Crónicas, Instituto de Salud Carlos III (ISCIII), Majadahonda, Madrid, Spain; 3Centro de Investigaciones Biológicas, CSIC, Madrid, Spain; 4Hospital Universitario La Paz, Madrid, Spain; 5Hospital Universitario Clínico San Carlos, Madrid, Spain; 6Translational Oncology Division, OncoHealth Institute, Fundación Jimenez Diaz University Hospital, Madrid, Spain; 7Department of Infection and Immunity, Luxembourg Institute of Health, Strassen, Luxembourg
Background and Aims: Alzheimer's disease (AD) is the most common cause of dementia worldwide. Its pathogenesis has not been well elucidated yet and effective treatments are needed. We aimed to analyze protein dysregulation in AD to identify dysregulated proteins that could be key for the study of AD by two proteomics strategies, TMT (Tandem Mass Tags) 10‐plex quantitative proteomics and LFQ (Label Free Quantification).
Methods: For TMT, brain protein extracts from AD patients (Braak IV‐VI) were analyzed by tandem mass spectrometry coupled to liquid chromatography (LC‐MS/MS) using a Q‐Exactive. Protein extracts from VD (vascular dementia) and FTD (frontotemporal dementia) patients, and healthy individuals were used as controls. For LFQ, a pull‐down with in vitro synthesized Abeta (Amyloid‐beta) fibers was performed, and interacting proteins analyzed by LC‐MS/MS. Subsequent analysis of proteomics data was performed with MaxQuant and the R program.
Results: 169 out of 3281 proteins identified by TMT were found statistically significant ≥1.5‐fold dysregulated in AD in comparison to controls, with the dysregulation of 10 of them confirmed using a different cohort of tissue and plasma samples. Two of these proteins were found associated to Abeta fibers, and two as blood‐based biomarkers of AD. Regarding the pull‐down, 332 proteins were identified as potential interactors of Abeta fibers, with 18 of them validated in vitro and ex vivo.
Conclusion: Novel proteins associated to AD pathogenesis, with a potential role in AD development and as biomarkers of the disease were described here. In addition, these proteins possess a high potential as therapeutic targets.
Disclosure: This work was supported by the PI17CIII/00045 grant from the AES‐ISCIII program to R.B. The A.M‐C. FPU predoctoral contract was supported by the Spanish Ministerio de Educación, Cultura y Deporte. The authors declare no competing interests.
EPO‐217
Structure‐based discovery of choline acetyltransferase ligands as potential theranostic agents for Alzheimer's disease
A. TK Baidya 1 ; B. Das1; T. Darreh‐Shori2; R. Kumar1
1Department of Pharmaceutical Engineering & Technology, Indian Institute of Technology (Banaras Hindu University), Varanasi, Uttar Pradesh, India; 2Division of Clinical Geriatrics, Centre for Alzheimer Research, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Stockholm, Sweden
Background and Aims: Choline acetyltransferase (ChAT), is a key cholinergic enzyme that biosynthesizes neurotransmitter acetylcholine, which plays a pivotal role in fundamental brain processes. Gradual loss of cholinergic neurons is observed in the brain with Alzheimer's disease which correlates well with the progressive decline of ChAT levels. This makes ChAT a key biomarker to estimate AD progression. The absence of specific, potent, blood‐brain‐barrier permeable small molecule ligands motivated us to discover novel ChAT ligands.
Methods: In this study, we have screened a VITAS‐M small molecule library containing ~1.4 million compounds by using a structure‐based virtual screen protocol based on VinaMPI. The top scoring compounds were manually inspected for their interaction with the active site amino acid residues and fifty compounds were selected.
Results: The fifty structurally diverse hits were identified. All showed potentially good interaction with the hotspot residues in the binding pocket of ChAT. They also showed prominent interaction with the catalytic residue His324 which is necessary for inhibitory activity of ligands. These hits will be validated in an in‐house developed fluorimetric assay to evaluate their enzyme inhibition kinetics and molecular dynamic simulation to understand their dynamic interaction in the process of ChAT inhibition.
Conclusion: The potential ChAT hits identified in this study can be further developed into ChAT PET tracers for the diagnosis of cholinergic dysfunction and to initiate timely therapeutic interventions to prevent or delay the progression of AD.
Disclosure: Nothing to disclose.
EPO‐218
Clinical correlations with diffusion‐weighted MRI in probable Creutzfeldt‐Jakob Disease
H. Rhee
Department of Neurology, Kyung Hee University Hospital at Gangdong, Seoul, Republic of Korea
Background and Aims: Diffusion‐weighted imaging (DWI) of the brain is important in diagnosing CJD. Also, elevated CSF total tau (t‐tau) is considered a useful CJD biomarker revealing neuro‐axonal damage although it is not specific for CJD. In this study, we attempted to find out the association between DWI abnormality and CSF t‐tau in CJD patients.
Methods: The patients who had been diagnosed and reported as human prion disease to the Korea Disease Control and Prevention Agency (KDCA) by medical institutions in South Korea from January 1, 2019, to December 31, 2019, were included in the clinical review. A total of 186 patients had been reported as suspected human prion disease during the one year and 53 patients who satisfied the criteria for human prion disease were included in the analysis.
Results: Hyperintense lesions on DWI were observed in 52 patients (98%). The involvement of the neocortex was observed in almost all patients (98%) and asymmetrical and bilateral hyperintensities on DWI were common. Among the neocortex, the most commonly involved region was the parietal lobe, followed by the frontal lobe, temporal lobe, and occipital lobe. DWI abnormality in the striatum and/or thalamus was observed in 65.3% of patients. There was no significant association between the extent of the lesions on DWI and CSF t‐tau.
Conclusion: In this study, most of the patients with probable CJD showed DWI abnormality mainly on the neocortex (parietal > frontal > temporal > occipital). The association between the pattern of DWI abnormality and the level of CSF t‐tau was not observed.
Disclosure: Nothing to disclose.
EPO‐219
Linking mitochondrial dysfunction with glial and neuroaxonal degeneration in Creutzfeldt‐Jakob disease
C. Manco; D. Plantone; D. Righi; S. Locci; N. De Stefano
Department of Medicine, Surgery and Neuroscience, University of Siena, Siena, Italy
Background and Aims: Creutzfeldt‐Jakob Disease (CJD) is a rare human prion disease characterized by the aberrant accumulation of a misfolded prion protein in neurons, causing spongiform changes, and neuronal loss. The exact neuropathogenic mechanisms associated with the rapid neuronal death partly remain unclear, with mitochondrial dysfunction possibly giving a contribution. This study explores the serum concentrations of biomarkers of neurodegeneration, glial activation, and mitochondrial dysfunction in CJD and their associations.
Methods: We assessed the serum material of 16 CJD patients [median age 66 years (25th‐75th percentile 59.8–77.3)] and 72 healthy controls [HC median age 64 years (25th‐75th percentile 56–72)]. Serum neurofilament light chain (sNfL) and serum glial fibrillary acidic protein (sGFAP) levels were assessed with single molecule assay (SIMOA), and serum Growth Differentiation Factor‐15 (sGDF‐15) with ELISA. Spearman correlation and analysis of covariance, considering age as covariate, were performed.
Results: Significant differences were found in sNfL [median CJD sNfL: 129 pg/ml (25th–75th percentile 102–252), median HC sNfL: 12.1 pg/ml (25th–75th percentile 7.96–16.2); p < 0.001] and sGFAP [median CJD sGFAP 586 pg/ml (25th‐75th percentile 394–1300), HC 101 pg/ml (25th‐75th percentile 50.8–169); p < 0.001] between CJD and HC. No difference was shown when sGDF‐15 was considered [median CJD sGDF‐15: 780 ng/ml (25th‐75th percentile 402–2151); median HC sGDF‐15 704 ng/ml (25th‐75th percentile 444–992)]. In CJD patients, however, we found a significant positive correlation of sNfL with sGDF‐15 levels (p = 0.001, r = 0.748).
Conclusion: Our study suggests a role of mitochondrial dysfunction in the complex process of neurodegeneration in CJD.
Disclosure: Nothing to disclose.
EPO‐220
Unilateral magnetic resonance‐guided focused ultrasound thalamotomy for essential tremor and Parkinson's disease
C. Sempere Navarro 1 ; G. Fernández Pajarín1; J. García de Soto1; J. Casillas Clot2; P. Román3; M. Blanco4; E. Ares3; B. Ares3; J. Prieto1; Á. Sesar1
1Department of Neurology, Hospital Clínico Universitario, Santiago de Compostela, Spain; 2Department of Community nursing, preventive medicine and healthcare, University of Alicante, Alicante, Spain; 3Department of Neurosurgery, Hospital Clínico Universitario, Santiago de Compostela, Spain; 4Department of Radiology, Hospital Clínico Universitario, Santiago de Compostela, Spain
Background and Aims: Magnetic Resonance‐guided focused ultrasound (MRgFUS) thalamotomy is a minimally invasive procedure with proven efficacy in the management of refractory tremor. The objective of this study is to analyse differences of effectiveness in tremor reduction between Essential Tremor (ET) and Parkinson's disease (PD).
Methods: A total of 22 patients, 11 with refractory essential tremor (ET) and 11 with PD, who underwent MRgFUS thalamotomy in our center were included. The Clinical Rating Scale for Tremor of the treated hemibody (CRST A+B) and functional disability (CRST C) were compared before and 6 months after MRgFUS thalamotomy, as well as adverse effects at 1 and 6 months.
Results: At baseline, mean (±SD) age was 71.1 1 ± 8.53 for ET patients and 70.1 ± 12.89 years for PD patients (p = 0.832). Before treatment, CRST A+B scores were 21.45 ± 5.94 and 19.64 ± 5.89 (p = 0.438) and CRST C were 17.18 ± 5.4 and 14.09 ± 6.46 (p = 0.365), respectively. After 6 months of MRgFUS thalamotomy, a significant improvement in tremor severity and disability was observed (CRST A+B: 1.82 ± 2.44 and 3.45 ± 3.53 (p = 0.003); CRST C: 1.82 ± 2.18 and 4.09 ± 4.23 (p = 0.003)), although there were not significant differences between both groups (p = 0.193 and p = 0.065, respectively). Dysarthria and unsteadiness were the most common adverse effects reported, which were mild and transient.
Conclusion: Unilateral MRgFUS thalamotomy is safe and effective for refractory tremor in ET and PD. Further studies with larger sample sizes are needed to address possible differences in efficacy.
Disclosure: Nothing to disclose.
EPO‐221
Obstructive sleep apnoea and cognitive decline: Quest for new biomarkers
C. da Silva 1 ; J. Neiva Machado2; J. Moita3; C. Loureiro3; T. Almeida3; M. Lima1; J. Durães1; M. Leitão1; P. Faustino1; C. Bernardes1; I. Baldeiras1; A. Silva‐Spínola1; I. Santana1; M. Tábuas‐Pereira1
1Neurology Department, Unidade Local de Saúde Coimbra, Coimbra, Portugal; 2Pulmonology Department, Unidade Local de Saúde Região de Leiria, Leiria, Portugal; 3Pulmonology Department, Unidade Local de Saúde Coimbra, Coimbra, Portugal
Background and Aims: Obstructive sleep apnea (OSA) is the most common type of sleep‐related breathing disorder. The underlying chronic intermittent hypoxia and sleep fragmentation are pointed out as the main mechanisms leading to cognitive decline. Apnea‐hypopnea index has been used to evaluate severity of OSA, but oxygen desaturation index (ODI) is a relevant parameter, reflecting hypoxia. We aim to explore the link between different OSA markers and CSF biomarkers related to Alzheimer's disease (AD).
Methods: Transversal and retrospective study. We selected patients with cognitive complaints followed in a neurology appointment from a tertiary health center that met criteria for OSA through polysomnography (PSG). We gathered demographic and clinical data, including PSG parameters and CSF biomarkers of dementia. Statistical analysis comprised univariate and multivariate analysis adjusted for potential confounding variables. Statistical significance was set at p < 0.05.
Results: A total of 81 patients were included (mild OSA 29.6%, moderate OSA 35.8%, severe OSA 21.0%). Forty‐six (56.8%) were women, mean age of 69.2 years, 7.3 years of education, mean MMSE of 23.6, mean AHI of 22.0 events/h and mean ODI of 20.6 events/h. The univariate analysis showed a positive correlation between ODI and pTau (r = 0.29; p = 0.033). In stepwise multivariate regression analysis, the best predictors of pTau were Tau (β = 0.161, 95% CI = [0.143, 0.178], p < 0.001), Aβ42 (β = −0.023, 95% CI = [−0.036, −0.011], p = 0.001) and ODI (β = 0.446, 95% CI = [−0.011, 0.903], p = 0.055).
Conclusion: We found an association between ODI and CSF pTau levels, suggesting that severe nocturnal hypoxemia might contribute to neurodegeneration. These findings further emphasize the possible role of OSA treatment in preventing further neuronal damage.
Disclosure: Nothing to disclosure.
EPO‐222
Repetitive transcranial magnetic stimulation and mild cognitive impairment
F. D'Ammora 1 ; M. De Stefano1; D. Buonanno1; R. Pepe1; D. Atripaldi1; M. Siciliano2; A. Iavarone3; D. Ippolito3; G. Tedeschi1; F. Trojsi1; S. Esposito1
1First Division of Neurology, University of Campania "Luigi Vanvitelli", Naples, Italy; 2Department of psychology, University of Campania Luigi Vanvitelli, Caserta, Italy; 3Neurologic Unit, CTO Hospital, AORN "Ospedale dei Colli", Naples, Italy
Background and Aims: Repetitive transcranial magnetic stimulation (rTMS) can be used to improve cognition in mild cognitive impairment (MCI) and Alzheimer's disease (AD). Possible neurobiological mechanisms underlying the rTMS therapeutic effects are maladaptive plasticity, glial activation and neuroinflammation, including metalloproteases (MMP) activation. Our aim was to evaluate the effects of bilateral rTMS over the dorsolateral prefrontal cortex (DLPFC) on plasmatic levels or MMP1, ‐2, ‐9 and ‐10, MMPs‐related tissue inhibitors TIMP1 and TIMP2, and cognitive performances in MCI patients.
Methods: MCI patients (n = 18) were randomly assigned to two groups: one group received high frequency rTMS daily four weeks and the other received sham stimulation. Cognitive and psycho‐behavioural scores were measured at baseline (T0), after five weeks (T1), and six months after rTMS stimulation (T2). To determine the concentration of MMP1, ‐2, ‐9 and ‐10 and the respective inhibitors, TIMP1 and TIMP2, we used commercially available ELISA kits.
Results: We observed reduction in plasmatic levels of MMP‐1, ‐9, and ‐10 in the MCI‐TMS group and an increased in plasmatic levels of TIMP1 and TIMP2. We also detected an improvement in visuospatial performances.
Conclusion: Our study showed a possible long‐term impact of bilateral rTMS, a non‐invasive neuromodulation technique, on plasmatic levels of selected MMPs and TIMPs in MCI patients. These biological effects, after a 4‐week course of rTMS, associated with improvement of visuospatial perceptive abilities, prompt us to hypothesize a neuroprotective effect of rTMS.
Disclosure: I have no disclosure.
EPO‐223
Internetworks functional connectivity in Alzheimer's disease and Mild Cognitive impairment patients with Anosognosia
D. Ballotta 1 ; M. Tondelli1; C. Carbone1; R. Maramotti1; A. Chiari2; G. Pagnoni1; G. Zamboni1
1Department of Biomedical, Metabolic and Neural Sciences, University of Modena and Reggio Emilia, Modena, Italy; 2Neurology Unit, Azienda Ospedaliero‐Universitaria of Modena, Modena, Italy
Background and Aims: Unawareness in the Alzheimer's disease (AD) continuum has been hypothesized to arise from an impaired communication between brain regions. Reduced functional connectivity in the default‐mode network (DMN) has been demonstrated in AD patients with anosognosia; altered interaction between DMN and Frontoparietal Network (FPN) has been reported in Mild Cognitive Impairment (MCI); stronger connectivity within the salience network (SN) has been linked to anosognosia in prodromal AD. We hypothesized that anosognosia in AD could be associated with an imbalance between the activity of the DMN, the SN and the FPN, detectable using resting state functional magnetic resonance imaging (fMRI).
Methods: Sixty patients with MCI and AD underwent fMRI and neuropsychological assessment. Patients were categorized as aware or unaware of their condition, according to the Anosognosia Questionnaire Dementia. Independent component analysis (ICA) of the fMRI data was used to identify DMN, SN and FPN. Partial correlations were performed on the individual ICA time‐courses associated with each network to assess inter‐network functional connectivity. Finally, we examined whether the strength of functional connectivity between DMN and SN was a significant predictor of the connectivity strength between DMN and FPN, separately for aware and unaware patients.
Results: Functional connectivity between DMN and SN was positively correlated with functional connectivity between DMN and FPN only in aware patients (Figure 1).
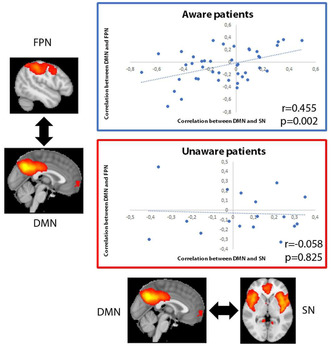
Correlation between internetwork functional connectivity in aware and unaware patients. Images represent average group maps of both aware and unaware patients obtained using independent component analysis.
Conclusion: Functional connectivity between DMN, SN and FPN is altered in MCI and AD patients with anosognosia, suggesting that a possible imbalance in these large‐scale networks might be associated to anosognosia expression in AD continuum.
Disclosure: Nothing to disclose.
EPO‐224
Mitigating Alzheimer's: Neurosteroids' effect against mitochondrial dysfunction
D. Divya 1 ; M. Faruq2; D. Vohora1
1Department of Pharmacology, School of Pharmaceutical Education & Research (SPER), Jamia Hamdard, New Delhi, India; 2Division of Genomics and Molecular Medicine, CSIR‐Institute of Genomics and Integrative Biology (IGIB), New Delhi, India
Background and Aims: Introduction: Alzheimer's disease (AD) is a neurological disorder characterized by pathological features such as synaptic and neuronal loss, the accumulation of amyloid‐beta (Aβ) deposits, and the formation of neurofibrillary tangles. The disease is closely linked to oxidative stress, stemming from increased reactive oxygen species (ROS), altered mitochondrial biogenesis, and changes in mitochondrial membrane potential (MMP), ultimately leading to disrupted mitochondrial function and cellular apoptosis. Ganaxolone and allopregnanolone have displayed neuroprotective effects; however, their impact on Aβ deposits and mitochondrial dysfunction in AD remains unclear. This study delves into the influence of Ganaxolone and allopregnanolone on Aβ toxicity‐induced mitochondrial dysfunction and explores the subsequent cellular processes.
Methods: The SH‐SY5Y neuroblastoma cell line was transfected with an amyloid precursor protein (APP) plasmid construct to establish an AD cell model. Cells underwent a 24‐hour treatment with Ganaxolone and allopregnanolone, followed by a ThT binding assay and immunoblotting to assess the effects on in vitro amyloid formation. Mitochondrial alterations were monitored using mitosox, and changes in MMP were analyzed through flow cytometry using TMRE. Additionally, apoptotic protein were investigated via Western blotting.
Results: Ganaxolone and allopregnanolone treatment significantly decreased mitochondrial ROS associated with Aβ toxicity and restored altered MMP mitigated apoptosis and amyloid‐beta toxicity. We also showed that Ganaxolone decreased the rate of apoptosis in cells by modulating important evolutionarily conserved proteins of apoptosis.
Conclusion: These findings suggest that Ganaxolone and allopregnanolone provide protection against mitochondria to APP‐transfected SH‐SY5Y cells, proposing Ganaxolone and allopregnanolone as a potential therapeutic agent for AD.
Disclosure: This work was supported by the Indian Council of Medical Research (ICMR) New Delhi, India, for SRF to DG (Ref. No. 45/05/2020‐PHA/BMS) and ICMR grant proposal no. IIRP/2023/1050 for financial support.
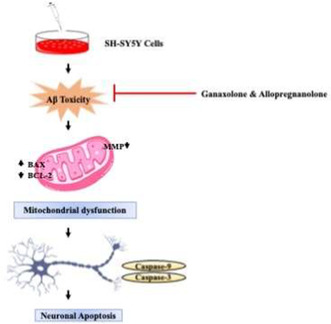
EPO‐225
Associations between PM2.5 exposure and Alzheimer's disease prevalence among elderly in eastern China
L. Yang
Zhejiang Hospital
Background and Aims: Studies showed that PM2.5 might be associated with various neurogenic diseases such as Alzheimer's disease (AD). However, this topic had been little studied in Zhejiang province of China.
Methods: We established a cohort of AD high‐risk population with 1,742 elderly aged 60 and above. The average residential exposure to PM2.5 for each participant that in a 5‐years period prior to the first survey, was estimated using a satellite‐based spatial statistical model. We determined the association between PM2.5 and AD prevalence by cox proportional hazards regression model.
Results: This study showed that an increase in the PM2.5 level was an important associated risk factor that contributed to AD. The average PM2.5 exposure levels among the study population ranged from 32.69μg/m3 to 39.67μg/m3 from 2013 to 2017, which were much higher than 5μg/m3 that specified in the WHO air quality guidelines. There was an association between PM2.5 exposure and AD, and the correlations between PM2.5 and Mini‐Mental State Examination, Montreal cognitive assessment scale scores were statistically significant. An increase in the PM2.5 level by 10μg/m3 elevated the risk of AD among residents by 2%‐5% (HR model 2‐model 4 = 1.02 to 1.05, CI model 2‐model 4 = 1.01–1.10). The subgroups of male, with old age, with low education levels, used to work as farmers or blue‐collar workers before retirement, overweight and obese were associated with a higher effect of PM2.5.
Conclusion: Reducing PM2.5 exposure might be a good way to prevent AD.
Disclosure: Nothing to disclose.
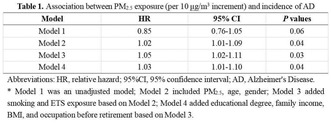
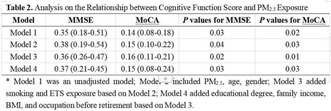
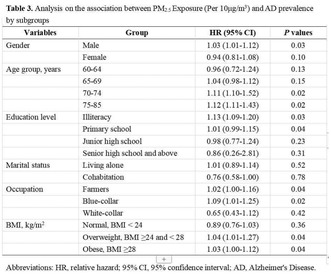
Autonomic nervous system diseases 2
EPO‐226
Heart rate variability fluctuations within 48 hours following a stroke and their association with symptom severity
E. Olbert 1 ; W. Struhal2
1Karl Landsteiner University of Health Sciences, Krems, Austria; 2Department of Neurology, University Hospital Tulln, Tulln, Austria
Background and Aims: The impact of cerebrovascular events such as stroke, transient ischemic attack (TIA), and intracranial hemorrhage (ICH) has been the subject of prior publications. However, comprehensive data pertaining to the initial stages of acute cerebral events is lacking. In this study, we conducted an examination of the fluctuation of heart rate variability, specifically analyzing standard deviation of NN intervals (SDNN), at different intervals after an acute cerebral event.
Methods: Monitoring data from 714 patients treated at the Stroke Unit of University Hospital Tulln were analyzed. For each patient, a 10‐minute ECG signal was examined hourly, and heart rate variability and baroreceptor sensitivity were calculated. Heart rate variability fluctuation was quantified as the difference between maximum and minimum values within the specified time frame for each patient.
Results: Stroke patients exhibited the lowest SDNN fluctuation (mean: 16.6, 6 h post‐onset), maintaining consistently lower levels over the initial 48 hours compared to individuals with ICH and stroke mimics (ICH: 29.8, stroke mimic: 27.3). Stroke severity influenced SDNN fluctuation, with milder strokes exhibiting increased fluctuation (mean: 26.7) at 6 hours post‐onset compared to moderate (mean: 19.8) and severe strokes (mean: 14.9). This effect diminished within 24 h post‐onset; however, distinctions between stroke, ICB, and stroke mimic persisted even after 48 h.
Conclusion: Fluctuations in autonomic parameters may suggest autonomic nervous system instability or rigidity during the acute phase following an acute cerebral event. These findings may explain discrepancies in previous analyses, dependent on variances in analyzed datasets and the specific time points considered after symptom onset.
Disclosure: Nothing to disclose.
EPO‐227
Quality indices: A pre‐requisite for using automatically monitored electrocardiograms in autonomic dysfunction research
E. Olbert 1 ; Y. Teuschl2; W. Struhal1
1Department of Neurology, University Hospital Tulln, Tulln, Austria. Karl Landsteiner University of Health Sciences, Krems, Austria; 2Department for Clinical Neurosciences and Preventive Medicine, University for Continuing Education Krems, Krems, Austria
Background and Aims: While providing indirect assessment of the autonomic nervous system, electrocardiograms (ECG) are often corrupted by noise or irregularities. Gold standard is human expert assessment, which is challenged in large databases. In this study, the performance of two automated, modulation spectrum‐based quality indicators were assessed for the detection of corrupted ECG signals in real‐life monitoring data.
Methods: Datasets included 1000 ECG‐recordings, each 600 seconds, collected at a stroke‐unit. ECG quality was evaluated by an expert, including the duration of artefacts and the number of extrasystoles. The modulation spectral based quality index (MSQI) and the Peak Distance Quality Index (PDQI) were calculated, as well as their sensitivity, specificity, accuracy and the area under the curve (AUC) for the detection of high quality ECGs compared to expert rating.
Results: The percentage of ECG signals in the recordings based on the modulation spectrum approach correlates with expert rating (r = 0.99, p < 0.001). According to expert rating, of 861 recordings, 85 (9.8%) showed more than 15% of extrasystoles and 60 (6.9%) more than 100s of artefacts and were rated as “reduced quality”. The AUC for PDQI ranges from 0.758 to 0.916 and for MSQI from 0.728 to 0.834. PDQI is superior in identifying extrasystoles, while the MSQI is better in identifying artefacts.
Conclusion: The large number of artefacts and irregularities makes automated quality indicators indispensable for the use of real‐life EGC monitoring data in science. We propose a combination of the MSQI and PDQI to select signals before analyzing data for the evaluation of the autonomic nervous system.
Disclosure: Nothing to disclose.
EPO‐228
Sex‐related differences in multiple system atrophy
F. Leys 1 ; S. Eschlböck2; N. Campese1; P. Mahlknecht1; M. Peball1; G. Goebel3; V. Sidoroff1; F. Krismer1; R. Granata1; S. Kiechl1; W. Poewe1; K. Seppi4; G. Wenning1; A. Fanciulli1
1Department of Neurology, Medical University of Innsbruck, Innsbruck, Austria; 2Department of Neurology, Hochzirl‐Natters Hospital, Zirl, Austria; 3Institute of Medical Statistics and Informatics, Medical University of Innsbruck, Innsbruck, Austria; 4Department of Neurology, Provincial Hospital of Kufstein, Kufstein, Austria
Background and Aims: Here we aimed at investigating sex‐related differences in the clinical presentation of multiple system atrophy (MSA) by means of a literature review and analysis of a retrospective Innsbruck cohort.
Methods: We searched the PubMed database for articles entailing sex‐related information in MSA. The baseline to last follow‐up clinical demographic differences between female and male individuals of the Innsbruck MSA cohort were investigated with a univariate followed by a multivariable binary regression analysis.
Results: The literature search identified 46 publications. Earlier studies showed comparable survival rates between female and male MSA individuals, while recent ones indicated that a more frequent motor‐symptomatic onset and generally less severe autonomic failure may confer female MSA individuals a survival benefit. Fifty‐six women and 60 men with a comparable median follow‐up of 27 months were included in the retrospective analysis. At baseline, female sex was associated with depression (OR = 4.7; p = 0.007), male sex with severe orthostatic hypotension (OR = 5.5; p = 0.016). At follow‐up, female sex was additionally associated with the intake of CNS‐active drugs (OR = 4.1; p = 0.029), while male sex also showed an association with the presence of supine hypertension (OR = 3.0; p = 0.020) and antihypertensive treatment (OR = 8.7; p = 0.001). We also observed an association between male sex and the initiation of antihypertensive regimes over the observational period (OR = 12.4; p = 0.004).
Conclusion: Our results indicate dynamic sex‐related differences in the clinical presentation of MSA, which need to be taken into account both for therapeutic and research purposes.
Disclosure: Academic study without external funding. Dr Leys and Dr Campese are/were supported by the US MSA Coalition and the Dr. Johannes & Hertha Tuba Foundation throughout conducting this study.
EPO‐229
DA‐9701 treatment for gastrointestinal symptoms and quality of life in postural orthostatic tachycardia syndrome
H. Jung 1 ; D. Seo1; J. Kim1; J. So1; H. Kim1; Y. Lim1; Y. Koo1; J. Lee2; E. Lee1
1Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea; 2Clinical Research Center, Asan Institute for Life Sciences, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
Background and Aims: Gastrointestinal (GI) symptoms commonly affect patients with postural tachycardia syndrome (POTS), detrimentally impacting their quality of life (QoL). DA‐9701, acting on 5‐HT1A, 5‐HT4, and D2 receptors, may improve GI symptoms and enhance the QoL in patients with POTS.
Methods: This randomized, double‐blind, placebo‐controlled, pilot trial was conducted at a single center. Patients with POTS were randomized in a 1:1 ratio following a crossover design. Participants received either oral DA‐9701 (30 mg) or a placebo thrice daily for eight weeks. This was followed by a four‐week washout period and an additional eight‐week treatment with the alternate therapy. The primary endpoint was the change from baseline in GI symptoms (total Nepean Dyspepsia Index‐Korean version (NDI‐K) symptom score) and related QoL (total NDI‐K QoL score) over the 8 week‐treatment period (cris.nih.go.kr, number KCT0006932).
Results: A total of 24 patients were randomized to initially receive either DA‐9701 (n = 12) or placebo (n = 12). DA‐9701 did not significantly improve the primary endpoints in total NDI‐K symptom (Least‐squares means, −13.9 vs. −9.5, p = 0.326) and QoL scores (4.2 vs. 2.4, p = 0.596). However, there was a tendency for improvement in specific GI symptoms, such as upper abdominal pain (−0.6 vs. 0.7, p = 0.066) and pressure (−1.4 vs. −0.1, p = 0.061). A carryover effect was observed in total NDI‐K QoL (p = 0.036), and analysis for the period 1 showed marginally significant treatment difference (‐1.3 vs. 9.2, p = 0.067).
Conclusion: Although DA‐9701 was not successful to improve GI symptom and related QoL in this crossover trial, its potential merits warrant further investigation.
Disclosure: Funded by Dong‐A Pharmaceutical.
EPO‐230
Painful small fiber neuropathy: A novel mutation in the SCN10A gene
F. Masciarelli 1 ; D. Dell'Aversana1; S. Tozza1; V. Provitera2; G. Caporaso2; F. Vitale1; R. Iodice1; L. Ruggiero1; R. Dubbioso1; F. Manganelli1; M. Nolano2
1Department of Neurosciences, Reproductive Sciences, and Odontostomatology, University of Naples Federico II, Naples, Italy; 2Neurology Department – Skin Biopsy, Lab Istituti Clinici Scientifici Maugeri, Spa SB Institute of Telese Terme – IRCCS
Background and Aims: We describe the case of a 35‐year‐old patient with severe painful small fiber neuropathy, early onset of symptoms and a long history of clinical and instrumental examinations who underwent overtime several aggressive and ineffective treatments for a putative rheumatological disease.
Methods: Symptoms started at the age of 21 with paraesthesia and burning pain in pectoral and periscapular area and at the hands. Shortly thereafter pain gradually spread to involve both feet and pelvic area. Twelve years after onset of symptoms, the patient reported generalized burning pain affecting also face and tongue. The pain was so severe he could only walk with the help of crutches. He also complained of gastroesophageal reflux, early satiety, bloating and severe constipation. Neurological examination was normal except from mechanical allodynia at both feet. He underwent functional and morphological assessment of small fibers.
Results: Spine and brain MRI, nerve conduction study, blood examination for dysmetabolic and dysimmune disorders were not relevant. Quantitative sensory testing showed abnormal thermal thresholds. Sympathetic skin response was abnormal and dynamic sweat test showed a non‐length‐dependent hypohidrosis. Cardiovascular reflexes were normal. Skin biopsy revealed a moderate non‐length dependent loss of sensory and autonomic nerves. Exome sequencing revealed a heterozygous VUS mutation (c.4852A>C; p.Met1618Leu) in the SCN10A gene. The same clinical and instrumental features were present in a sister and in the father of our patient who carried the same mutation.
Conclusion: Awareness of the genetic causes of SFN is crucial for providing correct diagnosis and treatment for patients and their family.
Disclosure: Nothing to disclose.
EPO‐231
Cardiac 123I‐MIBG Scintigraphy in the differential diagnosis of parkinsonian syndromes – monocentric cohort
J. Alves 1 ; R. Melo2; A. Moreira3; J. Lemos1; D. Reis Carneiro1
1Department of Neurology, Unidade Local de Saúde de Coimbra, Portugal; 2Faculty of Medicine, University of Coimbra, Portugal; 3Department of Nuclear Medicine, Unidade Local de Saúde de Coimbra, Portugal
Background and Aims: Cardiac [123I]metaiodobenzylguanidine scintigraphy (123I‐MIBG) reflects postganglionic cardiac sympathetic denervation (CSD). It is used for the differential diagnosis of parkinsonian syndromes, particularly between Parkinson's Disease (PD) and Multiple System Atrophy (MSA). We aimed at knowing whether there were clinical features that predict a 123I‐MIBG without CSD.
Methods: Retrospective study of a cohort of patients followed in the Neurology department of a tertiary university hospital, who performed 123I‐MIBG. Clinical data were retrieved from individual clinical registries. Patients with and without postganglionic cardiac autonomic denervation were compared to find factors associated to absence of CSD. A significant p‐value was considered below 0.05.
Results: From the thirty patients who performed 123I‐MIBG between 2018 and 2023 in our center, twenty‐seven did so for differential diagnosis between parkinsonian syndromes (22.2% presumed PD, 51.9% presumed MSA, 25.9% others). Only 44.4% of patients performed a Schellong test. The median time from the onset of the disease to the 123I‐MIBG was 3.0 (2.0–6.0) years. 44.4% exhibited cardiac denervation, while 55.6% did not. Univariate analysis revealed statistically significant differences between groups in terms of MDS‐UPDRS‐III, cardiovascular symptoms, isolated urinary symptoms (without cardiovascular symptoms), cardiovascular plus urinary symptoms, constipation, and presumed MSA diagnosis (Table 1). According to the logistic regression (Table 2), predictors of absence of CSD were isolated urinary symptoms (OR 8.1), constipation (OR 11.7), and a presumed MSA diagnosis (OR 21.2).
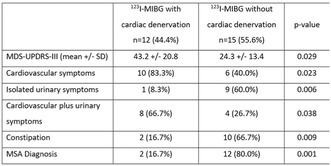
TABLE 1 Statistically Significant Differences Between Groups: Univariate Analysis Results
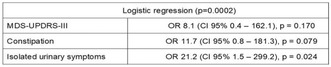
TABLE 2 Predictors of Absence of Cardiac Sympathetic Denervation: Logistic Regression Analysis
Conclusion: In our cohort, individuals presenting with isolated urinary symptoms, constipation, and a presumed MSA diagnosis are more likely to exhibit an absence of CSD.
Disclosure: Nothing to disclose.
EPO‐232
Cardiovascular autonomic disorders following COVID‐19 infection or vaccination
A. Fanciulli1; M. Verginer 1 ; F. Leys1; E. Kirchler1; L. Marino1; G. Göbel2; N. Campese1; S. Eschlböck1; S. Dürr1; G. Broessner1; A. Djamshidian1; A. Heidbreder1; B. Högl1; K. Hüfner3; S. Iglseder1; W. Löscher1; A. Stefani1; J. Wanschitz1; G. Weiss4; L. Zamarian1; J. Löffler‐Ragg4; R. Helbok5; S. Kiechl1; R. Granata1; G. Wenning1
1Department of Neurology, Medical University of Innsbruck, Innsbruck, Austria; 2Department of Medical Statistics, Informatics and Health Economics (MSIG), Medical University of Innsbruck, Innsbruck, Austria; 3Department of Psychiatry, Psychotherapy, Psychosomatics and Medical Psychology, Medical University of Innsbruck, Innsbruck, Austria; 4Department of Internal Medicine II, Medical University of Innsbruck, Innsbruck, Austria; 5Department of Neurology, Kepler Universitätsklinikum, Linz, Austria
Background and Aims: Cardiovascular autonomic disorders have been reported both after coronavirus‐disease‐2019 (COVID‐19) infection and COVID‐19 vaccination, but are not well characterized to date. Here we studied the type, frequency and clinical outcome of newly‐diagnosed cardiovascular autonomic disorders following COVID‐19 infection or vaccination in a retrospective series from the Innsbruck Dysautonomia Center.
Methods: We reviewed the medical records of all individuals referred between March 2020 and March 2023 for new‐onset of orthostatic intolerance (OI) within 6 weeks after COVID‐19 infection or vaccination.
Results: 102 individuals were studied (n = 76 with new‐onset OI after COVID‐19, n = 26 post‐vaccination). In post‐COVID‐19‐infection cases, postural orthostatic tachycardia syndrome (POTS) was the most common cardiovascular autonomic diagnosis (n = 21, 86% female, 33 ± 9 years of age). POTS was also the most frequent cardiovascular autonomic disorder in post‐COVID‐19‐vaccination cases (n = 11, 73% female, 32 ± 10 years of age). In 51 (50%) of all cases with post‐infectious or post‐vaccination OI, no cardiovascular autonomic cause was found. All newly diagnosed POTS cases were recommended non‐pharmacological measures, 33% of post‐infectious and 55% of post‐vaccination cases received additional pharmacological treatment. At follow‐up, 68% of post‐COVID‐19‐infection POTS (n = 13/19, 7 ± 4 months follow‐up) and 78% of post‐COVID‐19 vaccination cases (n = 7/9, 8 ± 6 months follow‐up) reported improvement.
Conclusion: A specialized diagnostic work‐up is pivotal to diagnose or exclude autonomic disorders in individuals with newly‐developed OI following COVID‐19 infection or vaccination. POTS is the most frequent autonomic disorder developing after both COVID‐19‐infection and COVID‐19‐vaccination, mainly affecting female individuals in their fourth decade of life. Improvement is observed under multimodal treatment at follow‐up.
Disclosure: Nothing to disclose.
EPO‐233
Indices of cardiovascular autonomic failure in multiple system atrophy
M. Kermorgant 1 ; M. Fabbri1; C. Leung1; A. Foubert‐Samier2; O. Rascol1; W. Meissner3; A. Pavy‐Le Traon1
1Centre de référence de l’AMS, Département de Neurologie, Toulouse, France; 2Univ. Bordeaux, Bordeaux Population Health Research Center, Inserm U1219, Bordeaux, France; 3CHU Bordeaux, Service de Neurologie des Maladies Neurodégénératives, IMNc, CRMRAMS, NS‐Park/FCRIN Network, Bordeaux, France
Background and Aims: Multiple system atrophy (MSA) is a rare and progressive neurodegenerative disorder. Severe cardiovascular autonomic failure (CAF) is one of the main clinical features with prognostic implications. Moreover, little is known about gender differences in CAF. In this study, we sought 1) to compare heart rate variability (HRV) and baroreflex sensitivity (BRS) as CAF indices between MSA and control patients, and 2) to determine the gender differences in these markers.
Methods: 193 MSA patients (88 men and 105 women) and 88 control patients (32 men and 56 women) were included in the study. HRV was assessed in time (pNN50, SDNN, RMSSD), frequential (LF, HF, LF/HF) and non‐linear (SD1, SD2) domains. BRS was estimated by the sequence method. Mann‐Whitney test was performed to analyze data between MSA and control patients. To compare men and women, we used two‐way ANOVA (condition × gender) with Tukey's method post‐hoc.
Results: Mean disease duration from symptom onset was 4.5 ± 2.3 years. Reduced overall variability (SDNN, LF, LF/HF, SD2), parasympathetic activity (pNN50, RMSSD, HF, SD1) and BRS were observed in MSA patients. No gender differences were observed.
Conclusion: Our results indicate a severe impairment in HRV and BRS in MSA patients. These additional markers may be considered as an index of CAF. However, there is no gender difference in the manifest of CAF. Further studies are needed to assess the prognosis value of these markers.
Disclosure: Nothing to disclose.
EPO‐234
Sudomotor function in multiple system atrophy, Parkinson's disease and four‐repeat tauopathies: A cross‐sectional report
M. Andréasson 1 ; P. Karlsson2; K. Samuelsson3; A. Terkelsen4; P. Svenningsson1
1Department of Clinical Neuroscience, Karolinska Institutet; Center for Neurology, Academic Specialist Center and Department of Neurology, Karolinska University Hospital, Stockholm, Sweden; 2Danish Pain Research Center, Department of Clinical Medicine, Aarhus University, Aarhus, Denmark; 3Department of Clinical Neuroscience, Karolinska Institutet and Department of Neurology, Karolinska University Hospital, Stockholm, Sweden; 4Department of Neurology, Aarhus University Hospital and Danish Pain Research Center, Department of Clinical Medicine, Aarhus University, Aarhus, Denmark
Background and Aims: Autonomic dysfunction is a well‐established feature of Parkinson's disease (PD) and multiple system atrophy (MSA). Sudomotor dysfunction may occur in both diseases and underlying pre‐ and postganglionic pathology have been suggested. We aimed to non‐invasively assess sudomotor function in PD and atypical parkinsonism and explore possible discriminative features.
Methods: In an ongoing longitudinal study, controls and patients with PD, MSA and four‐repeat tauopathies were prospectively included. Assessments included clinical rating scales, questionnaires, orthostatic blood pressure and quantification of electrochemical skin conductance in feet and hands using Sudoscan®. Non‐parametric testing was performed to explore group differences, and associations with measures of disease burden.
Results: An overview of the study population (n = 63) is shown in Table 1. No significant group differences were seen with regard to sex and age. Significant differences in skin conductance were evident between groups (p = 0.012 (hands); p = 0.0068 (feet)), reflecting reduced conductance in MSA (Figure 1). In a subgroup analysis, significant strong associations between skin conductance in feet and clinical rating scales were demonstrated in MSA (rho = −0.72, p = 0.0087; rho = −0.61, p = 0.034) (Table 2). No significant associations were evident in other groups (data not shown).
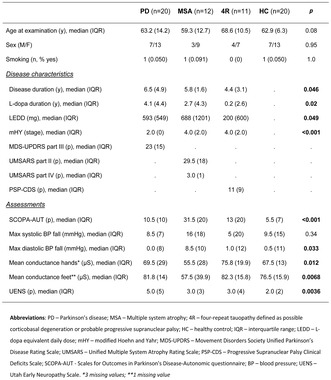
TABLE 1 Clinical and demographic characteristics of the study cohort (n = 63). Significant group differences with regard to skin conductance are shown. Group comparisons were performed with Fisher's exact test and Kruskal‐Wallis H‐test.

FIGURE 1 Mean skin conductance measured from feet (A) and hands (B). Post‐hoc comparisons with Bonferroni correction demonstrate: (A): MSA vs PD, p = 0.010; MSA vs 4R, p = 0.019; MSA vs HC, p = 0.12 (B): MSA vs PD, p = 0.054; MSA vs 4R, p = 0.018; MSA vs HC, p = 0.033
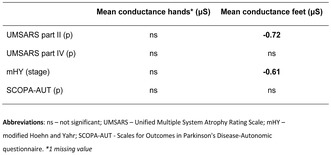
TABLE 2 Associations between skin conductance and measures of disease burden in MSA. Negative associations were demonstrated between skin conductance in feet and UMSARS part II, and mHY stage (rho = −0.72, p = 0.0087; rho = −0.61, p = 0.034 respectively).
Conclusion: Reduced electrochemical skin conductance, as measured with Sudoscan®, may be a prevalent finding in MSA relative to PD and four‐repeat tauopathies, and possible associations with clinical measures of disease burden may indicate prognostic properties. Further studies are needed to determine whether these findings are detectable in early disease or rather reflect an advanced disease stage with more widespread disease pathology.
Disclosure: MA has received funding for this study from NEURO Sweden, Svenska Läkaresällskapet (The Swedish Society of Medicine) and Hjärnfonden. PS has received funding from Region Stockholm and Wallenberg Clinical Scholarship. PK, KS, AJT report nothing to disclose.
EPO‐235
Autonomic testing in children with inflammatory bowel disease and irritable bowel syndrome: In search of dysautonomia
P. Ruška1; A. Jerković1; S. Sila1; A. Močić Pavić1; M. Krbot Skorić 2 ; M. Habek2; I. Hojsak1
1Referral Center for Pediatric Gastroenterology and Nutrition, Children's Hospital Zagreb, Zagreb, Croatia; 2Referral Center for Autonomic Nervous System, Department of Neurology, University Hospital Center Zagreb, Zagreb, Croatia
Background and Aims: The autonomic nervous system (ANS) is an important pathway connecting the brain and the gut. The aim of this study was to investigate the subjective and objective ANS abnormalities in children with irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) compared to healthy controls (HC).
Methods: A total of 58 children were enrolled: 23 in IBS group (mean age 15 years, male n = 7), 18 in IBD (mean age 14.25 years, male n = 7) and 17 HC (mean age 14.83 years, male n = 8). ANS symptoms were evaluated with the Composite Autonomic Symptom Score (COMPASS‐31). Heart rate (HR) and blood pressure (BP) responses were monitored with the Task Force Monitor (CNSystems, Austria) and quantitative sudomotor axon reflex test (QSART) were performed. The severity and distribution of ANS function was quantitated using the Composite Autonomic Severity Scale (CASS).
Results: Children with IBS scored highest on the COMPASS 31, followed by patients with IBD and HC (median scores were 10.9, 5 and 1.6, respectively; p = 0.001). Moreover, children with IBS scored the highest on questions that involved various gastrointestinal symptoms. There was no significant difference between groups in CASS (p > 0.05). However, there was a significant difference in symptomatic dysautonomia (defined as COMPASS‐31 >7.913 and CASS >0) between children with IBS (56.5%) compared to children with IBD (38.9%) and HC (11.8%), p = 0.015.
Conclusion: Symptomatic dysautonomia is most frequently observed in children with IBS, indicating important contribution of ANS abnormalities to pathophysiology of IBS.
Disclosure: Founding: Croatian science foundation (IP‐2019‐04‐3028).
EPO‐236
Parasympathetic and cerebral hemodynamic impairment in adults with sickle cell disease and cerebral microangiopathy
C. Ferreira de Matos1; P. Cougoul1; O. Zaharie2; M. Kermorgant3; A. Pavy Le Traon4; C. Gales3; J. Sénard3; M. Strumia5; F. Bonneville2; N. Nasr 3
1Internal Medicine Department—IUCT Oncopole, Toulouse, France; 2Neuroradiology Department of Toulouse University Hospital, Toulouse, France; 3UMR 1297 Team 10 Institute of Metabolic and Cardiovascular Disease (I2MC), Toulouse, France; 4Neurology Department of Toulouse University Hospital, Toulouse, Franc; 5Maintain Aging Research Team, CERPOP, INSERM, 1295, Toulouse University, Toulouse, France
Background and Aims: White matter lesions (WML) on brain imaging are common both in patients with sickle cell disease (SCD). The autonomic nervous system (ANS) is involved in the homeostasis of cerebral hemodynamics. The aim of this study was to evaluate the association between ANS parameters and cerebral microangiopathy in adult patients with SCD.
Methods: We prospectively assessed adult patients with SCD from our cohort for heart rate variability in the frequency domain, baroreflex sensitivity (BRS), cerebral autoregulation using Mx, cerebral arterial compliance (Ca) and cerebral time constant (tau) based on TCD and ABP monitoring. These patients also had cerebral MRI. Patients with history of stroke were excluded.
Results: Forty‐one patients (F/M:25/16) were included. Median age was 37.5 years (range 19–65). Twenty‐nine (70.7%) patients had SS genotype. Eleven patients had cerebral microangiopathy (26.8%). These patients were older (44.5 vs 30.6 years; p < 0.001), had a lower HF (HF 157 ms2 vs HF 467.6 ms2; p < 0.005) and impaired Ca (15.4 vs. 37.3 cm3/mmHg p < 0.014). AUC for the model with age as single predictor was of 0.876. For age and HF model, AUC was of 0.946.
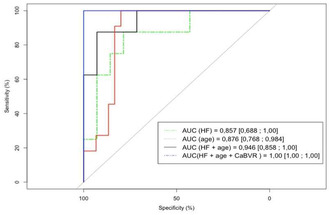
Figure AUC for the model with age as single predictor was of 0.876. For age and HF model, AUC was of 0.946. For age, HF and cerebral compliance model, AUC was of 1.
Conclusion: Lower parasympathetic activity was associated with cerebral microangiopathy in adults in SCD. Cardiovascular prevention including non‐drug treatment and physical activity could improve cerebrovascular function and parasympathetic activity. HF monitoring can help assess the cardiovascular impact of such interventions. Including novel hemodynamic parameters such as Ca could yield better understanding of integrative cardiovascular and cerebrovascular hemodynamic regulation in SCD.
Disclosure: Nothing to disclose.
EPO‐237
Pain in multiple system atrophy: A community‐based survey
N. Campese 1 ; B. Caliò1; F. Leys1; L. Kaltenbach2; G. Göbel2; J. Wanschitz1; A. Schlager3; P. Bower4; L. Kellermann4; L. Zamarian1; K. Bannister5; K. Chaudhuri6; A. Schrag7; R. Freeman8; H. Kaufmann9; R. Granata1; S. Kiechl1; W. Poewe1; K. Seppi1; G. Wenning1; A. Fanciulli1
1Department of Neurology, Medical University of Innsbruck, Innsbruck (Austria); 2Institute for Medical Statistics and Informatics, Medical University of Innsbruck, Innsbruck (Austria); 3Department of Anesthesiology and Intensive Care Medicine, Medical University of Innsbruck, Innsbruck (Austria); 4The Multiple System Atrophy Coalition, Inc., McLean, VA, USA; 5Institute of Psychiatry, Psychology and Neuroscience, King's College London, London (UK), 6Parkinson Foundation International Centre of Excellence, Kings College Hospital, London, UK; 7Department of Clinical and Movement Neurosciences, University College London, London (UK); 8Department of Neurology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts, USA; 9Department of Neurology, Dysautonomia Center, New York University Grossman School of Medicine, New York, New York, USA
Background and Aims: According to a meta‐analysis pain affects approximately 60% of individuals with multiple system atrophy (MSA), but its prevalence and characteristics remain poorly characterized. Here we assess prevalence, features, risk factors and treatment options for pain in MSA.
Methods: We performed a community‐based cross‐sectional study. Following a whole population sampling approach, MSA individuals and their informal caregivers were invited via patient advocacies, to complete a survey, available online between February and May 2023. The survey was accessed by 264 MSA individuals and 178 caregivers. After checking for data completeness and plausibility, questionnaires from 194 MSA individuals and 114 caregivers were retained for final analysis.
Results: Pain was reported by 87% of MSA individuals, more frequently by women [OR: 6.38 (95% C.I. 1.27–32.08), p = 0.025] and subjects with a self‐reported annual income below the average of the country [OR: 5.02 (95% C.I. 1.32–19.08), p = 0.018]. Pain was mostly located in the neck and shoulders (58%), back (45%) and legs (45%). Among individuals with pain, 69% received any kind of treatment, mostly non‐steroidal anti‐inflammatory drugs (30%), acetaminophen (25%) and opioids (17%) but only 52% of them was at least partially satisfied with pain management. Pain mostly affected patients’ work, household activities, and hobbies and caregivers’ social activities.
Conclusion: Pain is more common than previously reported in MSA, is mostly located in the neck, shoulders, back and legs, and especially affects women and individuals with lower income. Despite the frequent occurrence, pain remains undertreated or not satisfactorily managed, pinpointing an important unmet need in MSA.
Disclosure: Academic study supported by a grant of the MSA Coalition.
EPO‐238
Autonomic dysfunction in fibromyalgia: A skin biopsy and tilt testing study
P. Falco 1 ; E. Galosi1; C. Leone1; G. Di Pietro1; G. De Stefano1; N. Esposito1; D. Litewczuk1; G. Di Stefano1; S. Strano2; A. Truini1
1Department of Human Neuroscience, Sapienza University, Rome, Italy; 2Department of Cardiovascular, Respiratory, Nephrology, Anaesthesiology and Geriatric Science, Sapienza University, Rome, Italy
Background and Aims: Fibromyalgia patients frequently report autonomic symptoms, with previous studies suggesting sympathetic nervous system dysfunction, the pathophysiological mechanisms of which remains unknown [1]. Recent findings indicate sympathetic denervation in a subgroup of fibromyalgia patients with small fiber pathology (SFP) [2]. Our study aims to confirm the existence of cardiovascular autonomic dysfunction in fibromyalgia patients, examining its connection with peripheral autonomic denervation and the manifestation of autonomic symptoms.
References
Methods: We enrolled 35 fibromyalgia patients and assessed them using autonomic symptom scale (COMPASS‐31), skin biopsy, analyzing intraepidermal (IENFD) and dermal autonomic nerve fibers densities, and a battery of cardiovascular autonomic function tests: tilt test, Valsalva maneuver (VM), deep breathing (DB), heart rate (HR) power spectral analysis, blood pressure (BP) short‐term variability with baroreflex sensitivity (BRS) calculation. Based on distal IENFD, patients were divided into two subgroups: with and without SFP (Figure 1). Autonomic test results were compared with 35 sex and age‐ matched healthy controls and between the two patient subgroups. Correlations to skin biopsy data and autonomic symptoms were studied.
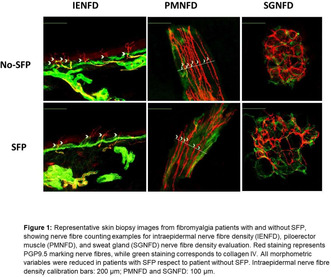
Representative skin biopsy images from fibromyalgia patients with and without SFP, showing nerve fibre counting examples for intraepidermal nerve fibre density (IENFD), piloerector muscle (PMNFD), and sweat gland (SGNFD) nerve fibre density evaluation.
Results: Fibromyalgia patients exhibit a reduced BP difference between phase IIb and IIa of VM (p < 0.001), a decreased HR difference in DB (p < 0.001) and a greater reduction of BRS during tilt (p < 0.004) compared to healthy subjects, without differences between the two patient subgroups. There isn’t correlation between functional and morphometric variables with clinical scales.
Conclusion: Fibromyalgia patients display cardiovascular autonomic dysfunction, which doesn’t correlate with peripheral autonomic denervation. This suggests that multiple mechanisms (central and peripheral) contribute to autonomic symptoms complaint by patients.
Disclosure: Nothing to disclose.
EPO‐239
The spectrum of autonomic responses to focal seizures
B. Gagaouzova1; I. van Rossum2; J. Hoey Smith – van de Wetering1; F. de Lange3; R. Thijs 1 ; J. van Dijk2
1Stichting Epilepsie Instellingen Nederland, The Netherlands; 2Leiden University Medical Centre, The Netherlands; 3Amsterdam University Medical Centre, The Netherlands
Background and Aims: The cardiovascular response to focal seizures is rarely examined in full due to lack of ictal simultaneous heart rate (HR) and blood pressure (BP) recordings. We explored the temporal patterns in three cases using the log ratio method to dissect the main hemodynamic components.
Methods: We identified three subjects who experienced a seizure during a tilt test: one had two focal with impaired awareness seizures (FIAS #1&2), one had one FIAS (#3) one had a focal to bilateral tonic‐clonic seizure (fbTCS, #4). All cases were monitored with video, HR and continuous BP (Finapres) recordings. We used the ‘log‐ratio method’ to determine the relative contributions of HR, stroke volume (SV), and total peripheral resistance (TPR) to mean arterial pressure (MAP). A 'phase' was defined as a temporary departure form baseline.
Results: During seizure 1&2 there was one phase, in which HR and TPR decreased and SV increased simultaneously. During seizure #3 we observed one negative phase for MAP and TPR, three phases for HR (positive‐negative‐positive), and only one late negative phase for SV; hence, HR changed out of phase with TPR and MAP. In seizure #4 there was no autonomic involvement during the first minute, after which MAP and HR showed an asynchronous three phasic course.
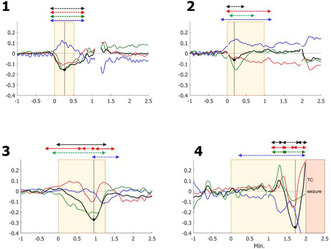
Log‐ratio results of the four focal seizures (seizure 1,2,3: focal impaired awareness seizure; seizure 4: focal to bilateral tonic‐clonic seizure).
Conclusion: This chance sample illustrates that hemodynamic variables may change during focal seizures in different directions, sometimes in phase, sometimes independently. We speculate that these complex autonomic patterns represent different ictal propagation pathways and may include ictal as well as corrective changes.
Disclosure: None.
EPO‐240
Multimodal assessment of neurogenic lower urinary tract symptoms in people with multiple sclerosis
S. Grlić1; K. Tešija1; I. Šućur1; K. Budimir1; M. Habek2; I. Adamec2; B. Barun2; I. Jurjević2; M. Krbot Skorić3; T. Gabelic 2
1School of Medicine, University of Zagreb, Zagreb, Croatia; 2University Hospital Center Zagreb, Department of Neurology, Referral Center for Autonomic Nervous System Disorders, Zagreb, Croatia; 3Faculty of Electrical Engineering, University of Zagreb, Zagreb, Croatia
Background and Aims: During the disease course symptoms of lower urinary tract (LUTS) are present in more than 80% of people with multiple sclerosis (pwMS), significantly impairing the quality of life (QoL). Objectives: to define the association between subjective LUTS symptoms, assessed by International Consultation on Incontinence Questionnaire (ICIQ) modules, with the results of neurological and neurophysiological evaluation.
Methods: 102 consecutive pwMS (90 females, age 37.7 ± 9.4 years), were included and Expanded Disability Status Scale (EDSS) with Bowel/Bladder Function System (BFS) was calculated. All participants answered the Croatian version of the ICIQ comprised of three parts (ICIQ – overactive bladder (OAB), ICIQ‐OAB QOL, and ICIQ – urinary incontinence (UI)). Somatosensory evoked potentials (SSEP) of median (latency N20, amplitude P15‐N20) and tibial (latency P40, amplitude P40‐N50) nerve were performed.
Results: Positive correlation was found between the EDSS and BFS with ICIQ‐OAB (r = 0.424 and r = 0.741), ICIQ OAB QOL (r = 0.462 and r = 0.785), and ICIQ‐UI (r = 0.484 and r = 0.705), all p values < 0.001. Latencies of the right P40 wave on the tibial SSEP positively correlated with OAB (ICIQ‐OAB: r = 0.242, p = 0.016; ICIQ‐OABqol: r = 283, p = 0.005) and latencies of both P40 waves with UI symptoms (r = 0.350, p = < .001 and r = 0.291, p = 0.004). Amplitudes of the right P40‐N50 wave on the tibial SSEP negatively correlated with OAB (ICIQ‐OAB: r = −0.214, p = 0.034; ICIQ‐OABqol: r = −0.211, p = 0.036) and amplitudes of both P40‐N50 waves with UI symptoms (r = −0.371, p = < .001 and r = −0.340, p = 0.001).
Conclusion: Subjective affection of the LUTS evaluated with ICIQ Questionnaire modules demonstrated significant association with clinical as well as neurophysiological findings.
Disclosure: Nothing to disclose.
Cerebrovascular diseases 2
EPO‐241
Can clinical risk scores predict atrial fibrillation in patient with cryptogenic stroke? A retrospective analysis
D. Galotto 1 ; M. Caccamo1; N. Marrone1; S. Grimaldi1; V. Velucci1; A. Manni1; G. Falcicchio2; G. Milella2; D. Mezzapesa2; M. Petruzzellis2; G. Defazio1
1Neurology Unit, Department of Translational Biomedicine and Neurosciences, Bari, Italy; 2Stroke Unit, Policlinic Hospital, Bari, Italy
Background and Aims: Atrial fibrillation (AF) is the most common arrhythmia and cause of acute ischemic stroke, often underdiagnosed in cryptogenic stroke (CS), mostly due to inadequate cardiac monitoring. The identification of a clinical risk score to predict AF in CS, could improve patients selection for prolonged monitoring.
Methods: We retrospectively collected data of CS patients discharged from our Stroke Unit from February 2018 to November 2023. A time‐to‐event analysis was performed to investigate variables associated to AF.
Results: We collected clinical data of 199 CS patients with median age of 70.5 years old. Median follow‐up from discharge was 16 months. 52 patients underwent loop recorder implantation of whom, 16 revealed AF after a mean time of 7 months. 14 patients without implantable device discovered AF after a mean time of 15 months. Overall 30 patients (15%) experienced AF. Univariate analysis identified left atrial (LA) dilation with diameter >40 mm (p < 0.001), supraventricular premature beats (SPB) >125 on 24‐hs electrocardiogram (p = 0.03) and multi‐territorial lesions on head TC scan (p = 0.001) as significant AF predictors. Logistic regression model integrated these three variables and showed: an area under the ROC curve of 0.80, sensitivity of 75.0 % and specificity of 85.4 %.
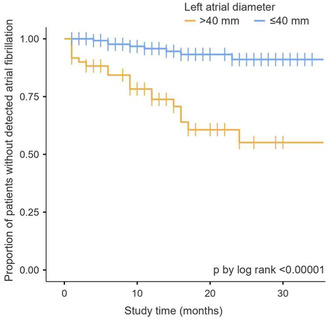
Left atrial diameter
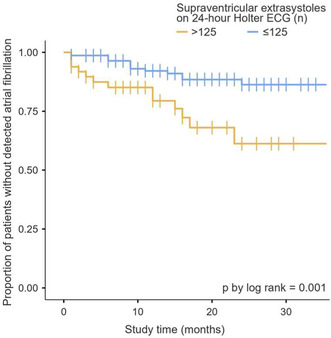
Supraventricular extrasystoles on 24h ECG

ROC curve (AUC = 0.80)
Conclusion: Our data confirmed studies reporting a significant association between AF and LA dilation, SPB and multi‐territorial lesions. For the need to select CS patients for expensive cardiac long‐term monitoring, we suggest to integrate these three variables with specificity and reasonable sensitivity in a new clinical risk score.
Disclosure: Nothing to Disclose.
EPO‐242
Does amyloid cerebral deposits influence delayed cognitive impairment after stroke?
O. Godefroy 1 ; N. Trinchard1; T. Shields2; C. Lamy1; A. Courselle‐Arnoux1; S. Canaple1; C. Leclercq1; M. Roussel1; M. Meyer2; E. Marchal2; F. Wollenweber3
1Neurology depart. Amiens University Hospital. F; 2Nuclear Med. Amiens University Hospital. F; 3Neurology Depart. Horst Schmidt Kliniken, Wiesbaden, G
Background and Aims: Amyloid deposits in has been shown to be associated with post‐stroke cognitive impairment (PSCI) at baseline. Long‐term outcomes have only been examined in a single study and remain to be documented.
Methods: We included 91 stroke patients (age: 63.3 ± 10.7; NIHSS: 5.6 ± 5.8; infarct: n = 81): 40 (44%) had subjective cognitive decline (SCD), 44 (47.2%) mild CI and 7 (8.8%) major CI) at 6 months PS. After the amyloid PET performed at baseline, they were followed up annually for 5 years using a clinical and neuropsychological battery.
Results: Amyloid PET was positive in 14 patients (15.4%). At this last visit (mean duration: 80.6 ± 27.9 months), SCT was observed in 59 patients, mild CI in 14 patients and major CI in 18 patients. Focusing on the 84 patients without major CI at baseline, Kaplan Meier survival analysis showed that amyloid PET status was associated with cognitive outcome (p = 0.03) due to a faster and higher rate of CI in PET‐positive patients (PET+: 60%; PET‐: 25.7%). The effect was significant for both mild (p = 0.03) and major CI (p = 0.003). It was independent (p = 0.5) from the stroke subtype. Cox regression analysis showed that the effect of amyloid status (p = 0.004) survived the 2 significant covariates (age at stroke: [p = 0.013] and pre‐stroke ADL impairment score [p = 0.016]).
Conclusion: In addition to the higher risk of PS CI at baseline, amyloid deposits are associated with a higher risk of developing incident CI during follow‐up, particularly dementia, with major consequences for patient outcome.
Disclosure: Scientific board of commercial entities: Biogen, Roche, Bristol‐Myers Squibb.
EPO‐243
Early cognitive trajectories after stroke: Still prevalent cognitive impairment despite neurological recovery
L. Gallucci 1 ; C. Sperber1; D. Seiffge1; U. Fischer2; A. Hakim3; M. Arnold1; R. Umarova1
1Department of Neurology, University Hospital, Inselspital, University of Bern, Bern, Switzerland; 2Department of Neurology, University Hospital and University of Basel, Basel, Switzerland; 3University Institute of Diagnostic and Interventional Neuroradiology, Bern University Hospital, Inselspital, University of Bern, Bern, Switzerland
Background and Aims: Early cognitive trajectories after stroke are barely investigated, despite their crucial significance for tailored early intervention in patients at risk for persistent post‐stroke cognitive impairment (PSCI).
Methods: We prospectively evaluated non‐aphasic patients with a first‐ever ischemic stroke without premorbid cognitive decline. Patients underwent a detailed neuropsychological testing in the acute phase and 3 months post‐stroke. PSCI was defined as performance < −1.5 SD in ≥ 2 cognitive domains. Cognitive trajectories across 3 months were evaluated using generalized linear models.
Results: Of 257 patients (66 ± 14 years old, 37% female, median NIHSS 24h = 1.00 [0.00, 4.00]) 68% had PSCI 2.8 ± 2.0 days post‐stroke. At 3 months post‐stroke, despite only minor neurological residual symptoms (NIHSS = 0.00 [0.00, 1.00]), 37% of patients had persistent PSCI and 4% newly developed PSCI. The most often affected domains were verbal episodic memory (43% of patients), constructive abilities (32%), learning (26%), and working memory (24%; Figure 1). The prevalence of PSCI at 3 months post‐stroke was comparable between young (<55 years old) and older (>55 years old) stroke adults (χ2 = 0.3, p = 0.579), meaning that this phenomenon could not be explained by covered pre‐stroke neurodegenerative processes. Higher stroke severity (NIHSS 24h, OR = 1.14, 95% CI 1.05–1.23) and lower years of education (OR = 0.81, 95% CI 0.73–0.91), but not age (OR = 1.01 95% CI 0.99–1.03), were identified as risk factors of persisting PSCI.
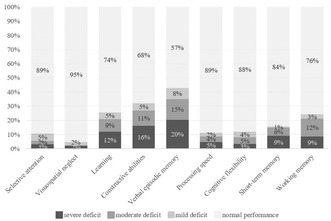
FIGURE 1 Prevalence of cognitive deficits at 3 months post‐stroke.
Conclusion: Despite favorable neurological outcome, PSCI still affects every third patient at 3 months post‐stroke, even in young adults. New early therapeutic interventions are needed to improve cognitive outcomes.
Disclosure: Nothing to disclose.
EPO‐244
Mechanical thrombectomy vs medical treatment in >85yo patients with acute ischemic stroke from large vessel occlusion
L. Vidal; C. Hervás; E. Mariño; B. Fuentes; M. Alonso de Leciñana Cases; G. Ruiz; R. Rigual; E. de Celis; L. Casado; E. Alonso; J. Rodríguez Pardo de Donlebún
Neurology, Hospital Universitario La Paz, Madrid, Spain
Background and Aims: The evidence on the benefits of mechanical thrombectomy (MT) in patients older than 85 years is scarce. Our aim was to compare the functional outcomes of patients treated with MT versus best medical treatment (BMT) exploring potentially related factors.
Methods: Retrospective observational study of consecutive stroke code patients >85 years old with large vessel occlusion attended within 24 hours of stroke onset and NIHSS>5 in a comprehensive stroke center from 1/1/2021 to 1/8/2022. We analyzed baseline characteristics, radiological findings and reperfusion treatments and their association with favorable outcomes (mRS < = 3 at 3 months) univariate analysis and binary logistic regression.
Results: We included 78 patients, 68% women, mean age 88 ± 3 years. 39 (50%) had terminal ICA occlusion‐M1, 28 (36%) M2, 3 (4%) BA, 8 (10%) ACA/PCA. Median (IQR) NIHSS was 17 (13–20) and ASPECTS 9 (6–10). Intravenous thrombolysis was administered to 30 (38.5%) patients and 52 received (66.7%) MT. We found no significant differences in the proportion of patients with favorable outcomes between the MT group and the BMT group (30% vs 42.3%; p = 0.283). Univariate analysis showed that higher NIHSS, longer onset‐to‐door time, higher glycemia and lower ASPECTS were related to worse outcomes. Logistic regression showed that only baseline NIHSS and ASPECTS were independently related to functional outcomes.
Conclusion: In patients older than 85 years with large vessel occlusion, we failed to demonstrate a benefit of MT over BMT. NIHSS and ASPECTS remain the most determinant prognostic factors.
Disclosure: Nothing to disclose.
EPO‐245
Survival and functional outcomes of patients aged ≥ 85 years treated with mechanical thrombectomy after ischemic stroke
C. Moreno López 1 ; R. López Rebolledo1; G. García Alcántara1; A. Llanes Ferrer1; A. Cruz Culebras1; A. De Felipe Mimbrera1; M. Matute Lozano1; S. García Madrona1; I. Bermúdez Coronel2; J. Méndez Cendón2; E. Fandiño Benito2; J. Masjuan Vallejo1; R. Vera Lechuga1
1Department of Neurology, Ramón y Cajal University Hospital, Madrid, Spain; 2Department of Neuroradiology, Ramón y Cajal University Hospital, Madrid, Spain
Background and Aims: Age is no longer an exclusion criterion for endovascular treatment of ischemic stroke. However, the progressive aging of the population raises questions about the efficacy and safety of mechanical thrombectomy (MT) in the older population.
Methods: Retrospective study of a prospective database of patients treated with MT at our center between 2017‐ 2023. We compared our experience using MT in patients aged ≥85 years to those aged < 85 years.
Results: Among the 647 patients treated with MT, 94 (14.5%) were ≥ 85 years old (median age, 87.4 ± 2.4). Both groups had similar stroke severity evaluated by the NIHSS scale (16.5 in ≥85 years old vs 16 in the younger group, p = 0.116) and had a similar proportion of fibrinolysis treatment (50% vs 53.7%, p = 0.526). We found no significant differences in the complete recanalization rate (87.7% vs 87.7%, p = 0.903) or symptomatic hemorrhagic transformation (4.3% vs 4.9%, p = 0.792) between both groups. However, there were significant differences in the functional outcome at 3 months with a smaller proportion of independence (38% vs 53.9%, p = 0.014) and higher mortality (21% vs 13.3%, p = 0.029) in older patients. In this group, we also found higher hospital mortality differences close to significant (17% vs 10.7%, p = 0.07).
Conclusion: In our experience, treatment with MT in the older population has a high rate of recanalization with no increment in the risk of hemorrhagic transformation but with higher mortality and worse functional outcome at 3 months comparing it with the younger population.
Disclosure: Nothing to disclosure.
EPO‐246
MicroRNAs as biomarkers of carotid atherosclerotic disease in ischaemic stroke patients
P. Jansky 1 ; T. Sramkova1; K. Benesova1; A. Olserova1; H. Magerova1; V. Matoska2; A. Tomek1
1Department of Neurology, Second Faculty of Medicine, Charles University and University Hospital Motol, Prague, Czechia; 2Department of Clinical Biochemistry, Hematology and Immunology, Na Homolce Hospital, Prague, Czechia
Background and Aims: MicroRNAs are small non‐coding RNA molecules regulating gene expression at the posttranscriptional level. The carotid atherosclerotic disease (CAD) is an important cause of ischaemic stroke. MicroRNAs play a complex role at different stages of atherosclerotic plaque development. Both upregulation and downregulation of different microRNAs were described in patients with CAD and ischaemic stroke. The study aims to describe the association of selected microRNAs and biochemical biomarkers with CAD and plaque stability in ischaemic stroke patients.
Methods: Case‐control study of consecutive ischaemic stroke patients with CAD admitted to a comprehensive stroke center. A control group consisted of ischaemic stroke patients with no presence of CAD. Plaques were described as unstable (symptomatic) and stable (asymptomatic). Serum levels of microRNAs (mir‐21, mir‐29b, mir‐133b, mir‐142‐5p, mir‐150, mir‐499, mir‐223‐3p) and biochemical biomarkers (lipid profile, glycated hemoglobin, fibrinogen, antithrombin III, creatinine, CRP) were analyzed at admission. The predictive accuracy was assessed by calculating the AUC.
Results: The data of 117 patients were analyzed (67 with CAD, 55 with no CAD, 16 with symptomatic plaque, 46% men, median age 73 years, median NIHSS 6). In the CAD group vs. no CAD group, the mean levels of glycated hemoglobin were 43.76mmol/mol vs. 39.06mmol/mol (p = 0.031), the mean levels of fibrinogen 3.07g/l vs. 2.68g/l (p = 0.015). All other biomarkers, including microRNA levels, were not associated with CAD. No tested biomarker was associated with plaque instability.
Conclusion: Elevated levels of fibrinogen and glycated hemoglobin but no microRNAs were associated with carotid atherosclerotic disease in ischaemic stroke patients. All biomarkers failed to predict plaque stability.
Disclosure: Nothing to disclose.
EPO‐247
Predictors of early seizures in patients with cerebral venous thrombosis: A single center analysis of 109 cases
V. Radisic; T. Svabic; M. Mijajlovic; P. Stanarcevic; V. Padjen; M. Ercegovac; N. Kresojevic; D. R. Jovanovic; I. Berisavac
Neurology Clinic, University Clinical Center of Serbia
Background and Aims: Early seizures (ES) are frequent manifestation of cerebral venous thrombosis (CVT) which complicates the course and impacts the outcome of the disease. The aim of our study was to identify predictors of ES in patients with CVT.
Methods: This retrospective observational study included 109 patients diagnosed with CVT over the 13‐ year period. Demographic, clinical, and radiological findings were collected and their association with seizure occurrence was studied. The impact of ESS on modified Rankin score at discharge was also explored.
Results: Among 109 patients, 30 (27.5%) had ESS. Bilateral motor seizures with or without clear focal onset were the most frequent (23 patients), whereas focal seizures were noted in 7 patients. Epileptic status was observed in 6 (20%) patients. In 30% of patients, ESS were the presenting feature, while the rest of patients developed seizures during the first two weeks following CVT. Patients who suffered ESS were younger (34 (18–63) vs. 41 (19–76), p < 0.05). Among clinical characteristics, coma at admission stood out as a predictor of ESS (5 (16.7%) vs. 3 (3.9%), p < 0.05). Parenchymal supratentorial lesion on neuroimaging and infarction with hemorrhagic transformation were associated with higher risk of seizure occurrence (p = 0.01, p < 0.05). ESS were not associated with poor outcome (mRS‐3). However, epileptic status was an important factor of morbidity.
Conclusion: Coma at admission and structural lesions on neuroimaging such as parenchymal supratentorial changes and infarction with hemorrhagic transformation stood out as predictors of ESS in patients with CVT.
Disclosure: Nothing to disclose.
EPO‐248
Effects of EGFr domain on CADASIL clinical and neuroradiological outcomes: A retrospective study of 115 cases
N. Rifino 1 ; B. Storti1; I. Canavero1; G. Boncoraglio1; S. Baratta2; F. Taroni2; A. Bersano1
1Cerebrovascular Unit, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy; 2Unit of Medical Genetics and Neurogenetics, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy
Background and Aims: Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is a rare heritable small vessel disease caused by a cysteine‐altering mutation in one of the thirty‐four epidermal growth factor‐like repeat(EGFr)‐domains of the NOTCH3 gene. CADASIL has a highly variable disease severity. It is supposed that the strongest known disease‐modifier may be the NOTCH3cys variant position. In 2023, a new clinical three‐tiered EGFr risk classification was proposed. EGFr domains were classified as either low (LR), medium (MR) or high risk (HR). However, it is still unclear how the location of the variants can play a role in CADASIL clinical and neuroradiological phenotype. Herein, we aimed to investigate the influence of mutation site on the clinical and neuroradiological presentation.
Methods: We included patients with a NOTCH3 mutation. Participants were uniformly characterized with a 3Tesla brain MRI (Figure‐1A). For each patient, demographic and clinical data were collected (Figure‐1B).
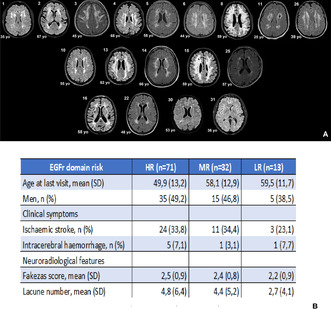
FIGURE 1A Representative brain MR FLAIR imaging of one patient for each EGFr domain clustered by high (first line), medium (second line) and low risk (third line) 1B. Demographic, clinical and neuroradiological data of HR, MR and LR patients
Results: Between 2008 and 2023, a total of 115 individuals with 43 unique NOTCH3 variant were included (Figure‐2A). Mutations clustered on the HR‐domains were associated with an increased risk of stroke compared to the LR (odds ratio [OR]:1.55; 95% CI: 5.53–0.44) and MR‐domains (OR: 1.15; 95% CI: 2.71–0.49) (Figure‐1B). On brain MRIs, patients carrying a HR‐variants had slightly higher mean Fazekas score and more lacuna than MR and LR‐patients (Figure‐2B). Furthermore, LR‐EGFr individuals had less disability, even though they were significantly older than MR and HR‐EGFr patients (Figure‐3).
FIGURE 2A Distribution and type of NOTCH3 variants across the three risk groups in our cohort 2B. Average Fazekas score and number of lacuna in the three risk groups.
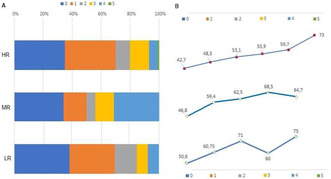
FIGURE 3A Disability for each risk group, according to modified Rankin Scale (mRS) 3B. Mean age for each patient group according to EGFr risk classification and mRS value.
Conclusion: Patients with NOTCH3 HR‐EGFr variants had not only an increased risk of stroke and earlier disability but also a more severe neuroradiological picture compared to the LR and MR‐domains.
Disclosure: Nothing to disclose.
EPO‐249
Optimal duration of dual antiplatelet therapy after carotid artery stenting: A nationwide cohort study
K. Seo 1 ; J. Yoo2; H. Lim3; D. Kim4
1Department of Neurology, National Health Insurance Service Ilsan Hospital, Goyang, Republic of Korea; 2Department of Neurology, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Republic of Korea; 3Department of Research and Analysis, National Health Insurance Service Ilsan Hospital, Goyang, Republic of Korea; 4Department of Rehabilitation Medicine, Kangdong Sacred Heart Hospital, College of Medicine, Seoul, Republic of Korea
Background and Aims: In carotid artery stenosis patients not eligible for carotid endarterectomy, carotid artery stenting (CAS) serves as an alternative. Dual antiplatelet therapy (DAPT) after CAS aims to prevent ischemic stroke, but the optimal duration remains unclear. We aimed to determine the optimal duration of DAPT by identifying differences in clinical events that occur depending on the DAPT maintenance period.
Methods: We obtained all data from the nationwide database of Health Insurance Review & Assessment Service from 2007 to 2020. The patients who received CAS, identified by procedure codes, The patients were divided into two groups according to the duration of DAPT: those who maintained DAPT for at least 90 days but less than 6 months (short‐DAPT group) and those who maintained it longer (long‐DAPT group). The primary outcome was a composite of ischemic stroke, gastrointestinal bleeding, and intracranial hemorrhage (ICH) within 12 months post‐switch to single antiplatelet therapy.
Results: Of 12,034 CAS patients, 2,529 were in the short‐DAPT group and 9,505 were in the long‐DAPT group. In the short‐DAPT group, ischemic stroke, gastrointestinal bleeding, and ICH occurred in 53 (2.1%), 24 (0.9%), and 4 (0.2%), respectively. In the long‐DAPT group, ischemic stroke, gastrointestinal bleeding, and ICH occurred in 184 (1.9%), 142 (1.5%), and 6 (0.1%), respectively. The primary outcome did not significantly differ between groups (3.0% vs. 3.4%; adjusted hazard ratio 1.104; 95% CI 0.866–1.406, p = 0.4252).
Conclusion: The short‐duration DAPT can be recommended as it shows no difference from long‐duration in terms of clinical efficacy and adverse events after CAS.
Disclosure: None.
EPO‐250
Non‐coding RNA expression profiling of the peripheral blood for patients with cervical artery dissection using RNA‐seq
P. Shlapakova; L. Dobrynina; L. Kalashnikova; M. Danilova; M. Gubanova; E. Gnedovskaya
Research Center of Neurology, Moscow, Russian Federation
Background and Aims: Cervical artery dissection (CeAD) is the main cause of young ischemic stroke. We performed bulk RNA‐seq of the peripheral blood from patients with CeAD and healthy volunteers. As we analyzed previously, the expression profile of protein‐coding genes for CeAD was associated with nucleolar stress, senescence‐associated secretory phenotype and mitochondrial malfunction. Our new research goal is to evaluate functional properties of differentially expressed non‐coding genes (ncDEGs) in peripheral blood for CeAD.
Methods: RNA was extracted from peripheral blood of 19 CeAD patients (37.6 ± 3.95 y.o.) and 18 healthy volunteers (30.1 ± 6.65 y.o.) using the Qiagen© RNeasy Mini Kit. 1000 ng of the RNA (RIN>7.0) were used to prepare each library with the Illumina© TruSeq Stranded Total RNA Library Prep Gold kit. 30–50 million paired‐end reads per sample were sequenced on the Illumina© NovaSeq 6000. 80% of the reads were aligned to the human reference genome using STAR. 60% of the aligned reads were counted in the features (genes) using Htseq‐count. Differential expression analysis with covariate adjustment (for age, sex and batch factors) was performed in EdgeR (CeAD vs Norma; adj.p‐value < 0.05). Enrichment analysis for ncDEGs was performed using RNAenrich against Reactome, KEGG and GO BP.
Results: We identified 62 upregulated and 302 downregulated ncDEGs for CeAD, which are most significantly involved in the pathways relevant to carcinogenesis and angiogenesis: epithelial cell proliferation, cellular senescence, regulation of apoptosis and response to oxygen levels, VEGFA‐VEGFR2/PI3K‐AKT/MAPK signaling.
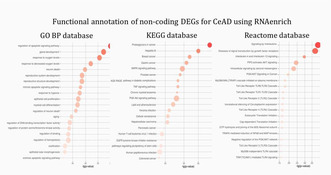
Enrichment bubble plots for the top representative pathways enriched in ncDEGs for CeAD. The pathways from GO BP, KEGG and Reactome databases are shown.
Conclusion: Functional profiling of ncDEGs for CeAD confirms our previous results about the probable intersection of CeAD with paraneoplastic mechanisms.
Disclosure: Nothing to disclose.
EPO‐251
Large artery atherosclerosis association with tissue‐level collaterals and outcomes in mechanical thrombectomy patients
P. Wrona 1 ; D. Wrobel2; J. Jozwik2; K. Jakobschy2; T. Popiela3; T. Homa4; A. Slowik1
1Department of Neurology, Jagiellonian University Medical College, Krakow, Poland; 2Student Scientific Group in Cerebrovascular Diseases, Jagiellonian University Medical College, Krakow Poland; 3Department of Radiology, Jagiellonian University Medical College, Krakow, Poland; 4Department of Neurology, University Hospital, Krakow, Poland
Background and Aims: Large artery atherosclerosis (LAA) is responsible for approximately 15% of acute ischemic strokes (AIS). Studies showed that LAA foster leptomeningeal development. We aimed to determine whether LAA is associated with better tissue‐level‐collaterals (TLC), denoted by lower computed tomography perfusion (CTP)‐derived hypoperfusion intensity ratio (HIR), as well as smaller early infarct volume (EIV) and if HIR and EIV affect functional outcomes.
Methods: We retrospectively analyzed 460 consecutive patients with AIS in anterior circulation treated with MT in Comprehensive Stroke Center in Krakow (2019–2023). We included 120 (26.09%) patients with LAA and 340 (73.91%) with cardioembolic AIS etiology. We obtained pre‐stroke risk factors and performed CTP followed by post‐processing analysis with RAPID software. HIR was defined as ratio of T10max/T6max; EIV as tissue with cerebral blood flow < 30% on admission, good functional outcome (GFO) as modified Rankin Score < 3 at day 90.
Results: LAA was associated with male sex (75% vs 41.2%, p < 0.001), smoking history (42.5% vs 14.5%, p < 0.001), younger age (66 [59–71 years]vs 76 [69–84 years], p < 0.001), lower initial National Institutes of Health Stroke Scale score (15 [10–18] vs 17 [10–20], p = 0.003) and lower HIR (0.26 [0.1–0.434] vs 0.386 [0.204–0.521], p < 0.001). Despite that, LAA was not associated with lower EIV (8 ml [0–32] vs 7 ml [0–22], p = 0.502). LAA etiology predicted GFO in univariate analysis (73.3% vs 60.6%, p = 0.012), although significance was lost after adjustment for confounders (p = 0.394).
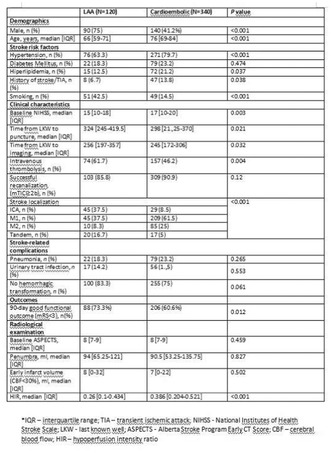
TABLE 1 Characteristics of patients with LAA vs cardioembolic ischemic stroke etiology
Conclusion: LAA is associated with male sex, smoking history, younger age, lower initial stroke severity and more robust TLC. Despite better TLC, LAA patients have neither smaller EIV nor better prognosis than cardioembolic patients.
Disclosure: ERA‐NET‐NEURON/21/2020 iBioStroke grant.
COVID‐19
EPO‐252
Long‐COVID‐19: A biomedical model of post‐viral chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME)
A. Chaudhuri; A. Goldsmith Lister
Department of Neurology, CFS/ME Unit, Queen's Hospital, Romford, UK
Background and Aims: The pathogenesis of post‐viral chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) is poorly understood. Long‐COVID‐19 is a post‐viral syndrome that shares clinical features of CFS/ME.
Methods: We reviewed the data of 487 adults (age range 16–70 years) with CFS/ME seen in our clinic al unit with the clinical features of adult post‐COVID‐19 population from literature search.
Results: Symptoms of post‐viral CFS/ME and long‐COVID‐19 were remarkably similar; fatigue, headache, cognitive deficit and chronic pain were common in both groups and tended to be more pervasive for those with longer symptom durations. Quality of life was severely impacted by physical fatigue with post‐exertional malaise, cognitive impairment that did not progress over time, and neuropsychiatric symptoms from low mood and anxiety.
Conclusion: Population with CFS/ME and post‐COVID‐19 experience persistent central fatigue, pain and non‐progressive cognitive deficits. Modification of post‐translational cell signalling by viral infection and host immune response leading to metabolic reprogramming and consequent alterations in synaptic and ion channel functions is a possible explanation and further work is required for better understanding of biomedical mechanisms of post‐viral syndromes to develop effective therapy. Long COVID‐19 is a valid biomedical model of post‐viral CFS/ME and post‐viral syndromes are not primarily a somatoform or functional neurological disorders.
Disclosure: There is no competing interest.
EPO‐253
SARS‐CoV‐2 impact on disability in Southern Italy's MS patients: Tertiary center findings
C. Di Monaco 1 ; A. Esposito1; E. Zappulo2; I. Di Filippo2; A. Spiezia1; M. Pretracca3; V. Nicolella1; F. Novarella1; R. Lanzillo1; M. Moccia1; A. Buonomo2; I. Gentile2; V. Brescia Morra1; A. Carotenuto1
1Department of Neurosciences, Reproductive and Odontostomatological Sciences, Federico II University, Naples, Italy, 2Department of Clinical Medicine and Surgery, Division of Infectious Diseases, "Federico II" University hospital, Naples, Italy, 3Department of Human Neurosciences, Sapienza University, Rome, Italy
Background and Aims: In Multiple Sclerosis (MS) patients, the occurrence of COVID‐19 has been associated with worsening clinical course. This study aimed to assess the incidence of SARS‐CoV2 infection during various pandemic waves and evaluate risk factors for clinical disability worsening in the post‐COVID‐19 era within an MS setting.
Methods: A retrospective study was conducted on patients with MS and neuromyelitis optica spectrum disorder (NMO) at the Multiple Sclerosis Center at the University of Naples "Federico II" between March 2020 and October 2023. Patients were monitored for virologically documented SARS‐CoV2 infection during follow‐up. Data on Expanded Disability Status Scale (EDSS) scores were collected at MS diagnosis, the latest follow‐up before March 2020, and the last available follow‐up
Results: Among 276 patients enrolled, 46% (127 patients) were infected with SARS‐CoV2, predominantly during the Omicron BA1/2 wave. Infected patients had a lower EDSS at MS diagnosis (3.0 [2.5–3.5] vs. 3.5 [2.5–4.5], p = 0.015) and at the last follow‐up (4.5 [3–6] vs. 5.5 [3.5–6.5], p = 0.03). No significant differences in EDSS change were observed between infected and non‐infected patients. Multivariate Cox analysis revealed that EDSS worsening was associated with age younger than 50 years (HR = 3.57, p = 0.03), while anti‐CD20 treatment was protective against disability accrual (HR = 0.09, p = 0.04).
Conclusion: 46% of MS or NMO patients experienced SARS‐CoV2 infection while under mAb treatment. Infected individuals exhibited lower motor impairment, suggesting that higher disability might be protective due to increased awareness of fragility status or limited outdoor and social activities. Importantly, COVID‐19 infection did not seem to impact the disease course
Disclosure: Lanzillo R received compensations for speaking or consultancy from Biogen, Teva, Genzyme, Merck, Bristol myer squibb, Jansenn, Novartis and Roche Carotenuto A served on advisory boards for: Merk, Novartis, Roche and Almirall Brescia Morra V received funding from Novartis, Roche, Biogen, Teva, Almirall, Sanofi‐Genzyme, Merk, Bayer, Mylan, Bristol Myers Squibb Moccia M received honoraria from Biogen, BMS Celgene, Janssen, Merck, Roche, and Sanofi‐Genzyme; and serves in the Editorial Board of the Multiple Sclerosis Journal Others authors declare not conflict of interest.
EPO‐254
SARS‐CoV‐2‐induced type I interferon signalling dysregulation in the olfactory‐amygdala pathway
G. Vavougios 1 ; T. Mavridis2; T. Doskas3; O. Papaggeli4; P. Foka4; G. Hadjigeorgiou1
1Department of Neurology, Medical School, University of Cyprus, Nicosia, Cyprus; 2Tallaght University Hospital (TUH)/The Adelaide and Meath Hospital, Dublin, incorporating the National Children's Hospital (AMNCH), Dublin, Ireland; 3Athens Naval Hospital, Athens, Greece; 4Hellenic Pasteur Institute, Athens, Greece
Background and Aims: Previous works from our group have proposed a model where peripheral induction of IFN‐I may be relayed to the CNS, even in the absence of fulminant infection. The aim of our study was to identify significantly enriched IFN‐I signatures and genes along the transolfactory route, utilizing published datasets of nasal mucosa, olfactory bulb amygdala transcriptomes of COVID‐19 patients. We furthermore sought to identify in these IFN‐I signature gene networks associated with Alzheimer's disease pathology and risk.
Methods: Gene expression data involving the nasal epithelium, olfactory bulb and amygdala of COVID‐19 patients and transcriptomic data from Alzheimer's disease patients were scrutinized for enriched Type I interferon pathways. Gene set enrichment analyses and gene – Venn approaches were used to determine genes in IFN‐I enriched signatures. The Agora web resource was used to identify genes in IFN‐I signatures associated with Alzheimer's disease risk based on its aggregated multi‐omic data.
Results: Pathways associated with type I interferon signalling were found in all samples tested. Each type I interferon signature was enriched by IFITM and OAS family genes. A 14 gene signature associated with COVID‐19 CNS and the response to Alzheimer's disease pathology, whereas 9 genes were associated with increased risk for Alzheimer's disease.
Conclusion: Our study provides further support to a type I interferon signalling dysregulation along the extended olfactory network as reconstructed herein, ranging from the nasal epithelium and extending to the amygdala. We furthermore identify the 14 genes implicated in this dysregulated pathway with Alzheimer's disease pathology, conferring increased risk for the latter.
Disclosure: None declared.
EPO‐255
Serum interleukins in children with neurological complications of SARS‐CoV‐2 infection
E. Capestru 1 ; S. Hadjiu1; C. Calcii3; O. Constantin1; I. Calistru1; I. Istratuc1; N. Revenco1; S. Groppa2
1State University of Medicine and Pharmacy “Nicolae Testemiţanu” Pediatric Neurology Clinic of the Department of Pediatrics; 2State University of Medicine and Pharmacy „Nicolae Testemiţanu” Neurology Department No. 2; 3PMI, Institute of Mother and Child
Background and Aims: Neuroinflammation is one of the key mechanisms involved in the pathogenesis of brain lesions associated with SARS‐CoV‐2 infection. The aim. To estimate the correlation between serum levels of IL‐1beta, IL‐10, and nervous system damage in children with SARS‐CoV‐2 infection.
Methods: We evaluated 100 children (age 29 days – 7 years) with neurological manifestations associated with SARS‐CoV‐2 (moderate and severe form), divided into two groups: (1) acute neurological complications (CN) and (2) post‐acute, in which we evaluated the serum values of IL‐1beta and IL‐10, by the ELISA method. Clinical manifestations were scored to perform statistical calculations. Statistical processing: t‐student test, 95 CI confidence coefficient, correlation coefficient (rxy).
Results: In the group with acute CN, 89 (89%; 95 CI 92.13 −85.87) cases were registered, and post‐acute CN – 11 (11%; 95 CI 7.87–14.13). In the group with acute CN, encephalopathy (72%; 95 CI 67.51–76.49) and seizures (9%; 95 CI 6.14–11.86) prevailed, compared to those with post‐acute CN (2%; 95 CI 0.6–3.4) in which headache predominated (90%; 95 CI 87–93). Serum levels of IL‐10 and IL‐beta were significantly increased in the acute CN group compared to those with post‐acute CN. Strong correlations were found between elevated serum levels of IL‐1beta and encephalopathy (rxy = 0.786), IL‐1beta and seizures (rxy = 0.824), and between IL‐10 and encephalopathy (rxy = 0.758), IL‐10 and seizures (rxy = 0.806).
Conclusion: Strong correlations between elevated levels of IL‐1β and IL‐10 and acute CN suggest the presence of pronounced inflammation and the risk of long‐term neurological complications in children who were infected with SARS‐CoV‐2.
Disclosure: Nothing to disclose.
EPO‐256
Cortical and spinal excitability testing in patients with long‐term post‐COVID myopathy
G. Fanella 1 ; B. Khan1; A. De Grado2; J. Agergaard3; L. Østergaard3; B. Schiøttz‐Christensen3; H. Tankisi1
1Department of Clinical Neurophysiology, Aarhus University Hospital, Aarhus, Denmark; 2Unit of Rare Neurological Diseases, Department of Clinical Neurosciences, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy; 3Department of Infectious Diseases, Aarhus University Hospital, Aarhus, Denmark
Background and Aims: The objective of this study was to investigate cortical and spinal excitability in patients diagnosed with post‐COVID myopathy, exploring the possibility of a multisystemic involvement of both muscles and central nervous system (CNS).
Methods: In this case‐control study, we compared 32 patients with post‐COVID myopathy to 15 age‐matched healthy controls. Cortical excitability was assessed using threshold‐tracking transcranial magnetic stimulation (TT‐TMS), with the following protocols: Short‐Interval Intracortical Inhibition (SICI), Short‐Interval Intracortical Facilitation (SICF), Long‐Interval Intracortical Inhibition (LICI), Intracortical Facilitation (ICF), Short‐latency afferent inhibition (SAI). Spinal cord excitability was evaluated by recording H‐reflex and long latency reflexes (LLRs). Cognitive status was assessed using Montreal Cognitive Assessment (MoCA) and Symbol Digit Modalities Test (SDMT).
Results: TT‐TMS showed a statistically significant decreased SICI across the entire averaged 1–3.5 ms interval range (t(45) = 2.411, p‐value = 0.01) in patients compared to controls (Fig 1). The most affected ISI was 2.5ms, with values of 9.2% ± 1.9 for patients vs. 21.3% ± 2.3 for controls (t(45) = 3.761, p‐value = 0.0005). No significant differences were found in SAI, SICF, ICF and LICI between the two groups. Statistically significant differences were observed in LLR II (U = 126.0, p‐value = 0.02) and LLR III (U = 53.0, p‐value = 0.03) amplitudes. MoCA median score was 27 for patients and 29 for controls, showing a statistically significant difference between the two groups (U = 96.50, p‐value = 0.002). We found no differences in H reflex and SDMT score in the two groups.
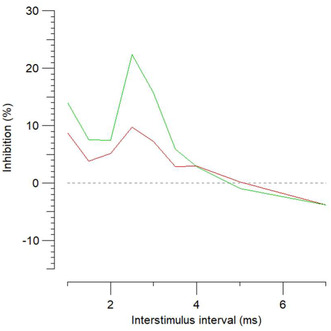
FIGURE 1 Overview of SICI protocol 1–7 ms. Red: patients, Green: healthy controls
Conclusion: This study demonstrates that patients with post‐COVID myopathy exhibit reduced cortical inhibition and increased LLR amplitudes. These findings point towards a potential concomitant involvement of CNS in individuals with post‐COVID myopathy.
Disclosure: Nothing to disclose.
EPO‐257
The different neuropsychological phenotypes of Post‐COVID subjects
Í. Karmann Aventurato; L. Scárdua‐Silva; B. Amorim da Costa; R. Batista João; M. Rabelo de Brito; J. Bechelli; L. Santos Silva; A. Ferreira dos Santos; M. Koutsodontis Machado Alvim; T. Alves Silva Souza; M. Mendes; T. Waku; M. Rocha da Silva; M. Nogueira; F. Cendes; C. Lin Yasuda
Laboratório de Neuroimagem, Departamento de Neurologia, Faculdade de Ciências Médicas, Universidade de Campinas
Background and Aims: Although cognitive dysfunction of patients after COVID‐19 infection has been described, a systematic search of neuropsychological subgroups has not been conducted. The present study aims to derive the neuropsychological profile of different subgroups using a data‐centric hierarchical clustering method.
Methods: We analyzed the data from the NeuroCovid cohort, comprising different neuropsychological tests (comprising multiple cognitive domains). After outlier removal, a factor analysis was performed to derive the latent cognitive factors in the data. Factor‐transformed data were renormalized according to the expected population mean and standard deviation and used in hierarchical analysis with Ward's method. Subjects were compared between clusters regarding demographics, illness severity, depression and anxiety scores.
Results: We applied factor analysis to neuropsychological data from 265 subjects. Data were deemed proper for factor analysis (Kayser‐Meyerz‐Olkin statistic 0.63), and the number of factors was determined to be 6 by parallel analysis. Factors regarding memory, executive functions (EF), automatic processes (AP), motor, visuospatial construction (VSP) and visuospatial construction speed were identified. One was excluded from the six clusters identified due to insufficient subjects (n = 2). The remaining clusters were (A) unimpaired (n = 86), (B) visuospatial impaired (n = 18), (C) memory impaired (n = 83), (D) AP impairment (n = 24), and (E) EF impairment (n = 36). Cluster C comprised older subjects, whereas subjects were younger in Cluster E. Depression scores (Beck's Depression Inventory‐II) were increased in both clusters C and E.
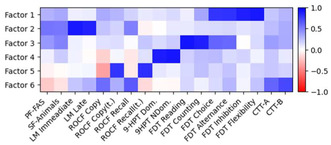
Weighting matrix of the final factor analysis after ObliMin rotation. PF: Phonetic Fluency, SF: Semantic Fluency, ROCF: Rey‐Osterieth Complex Figure test, 9‐HPT: nine‐hole peg test, FDT: Five‐Digit test, CTT: Color Trails test.
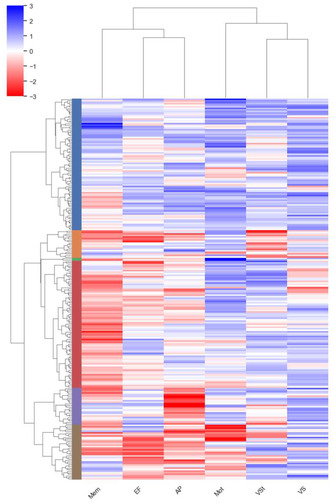
Clustergram of the Hierarchical Clustering analysis applied to factor‐transformed renormalized data. Colors under the dendogram (left) divide the data in different clusters.
Conclusion: Our data shows that the individuals with persistent symptoms after mild COVID present a heterogeneous neuropsychological profile with subgroups showing impairments in different cognitive domains.
Disclosure: Nothing to disclose.
EPO‐258
Assessing the potential neurological impact of COVID‐19 vaccines: An in‐depth examination of reported complications
J. Salimjonov; N. Rashidova; K. Khalimova
Department of Neurology and Medical Psychology, Tashkent Medical Academy, Tashkent, Uzbekistan
Background and Aims: During the COVID‐19 pandemic, several types of vaccines were developed, which successfully passed all stages of clinical trials and were used into practice. Like other types of vaccines, COVID‐19 vaccines have their own local and systemic side effects, as well as other systemic complications, including neurological ones.
Methods: The medical records of people were examined, who received a full course of vaccination between April 2021 and March 2023 in the Tashkent city. Adverse reactions and neurological complications were identified by retrospective analysis, spontaneous reporting, and stimulated reporting.
Results: A total of 1,585,014 people have been completed the full course of vaccination (minimum age 18 years, maximum 85 years) and 6,796,188 doses of vaccines have been used (Oxford/AstraZeneca 240,144 doses, ZF2001 3,411,125 doses, Sputnik V 257,593 doses, Moderna 1,132 121 doses, Pfizer/BioNTech 1,441,627 doses, Sinovac 251,146 doses, Sputnik Light 51,141 doses, Johnson&Johnson 11,291 doses). Among the neurological complications after vaccination were identified: ischemic stroke (12 cases, 0.00075%), cavernous sinus thrombosis (1 case, 0.00006%), acute disseminated encephalomyelitis (1 case, 0.00006%), meningoencephalitis (3 cases, 0.00019%), sensorineural hearing loss (4 cases, 0.00025%), Guillain‐Barré syndrome (4 cases, 0.00025%), Bell's palsy (2 cases, 0.000125%), multisystem inflammatory syndrome (1 case, 0.00006%). No deaths have been reported following vaccination. Neurological complications occurred within 28 days after vaccination.
Conclusion: Given the risk of neurological complications is extremely rare (0.001%), vaccination is the only way to protect against COVID‐19. At a time when the COVID‐19 infection has enormous complications not only in the nervous system, but also in other systems, even death.
Disclosure: Agree.
EPO‐259
Analysis of IgG antibodies against S1‐RBD of SARS‐CoV2 in patients with MS treated with DMT in North‐Eastern Poland
J. Kulikowska 1 ; K. Kapica‐Topczewska1; M. Gudowska‐Sawczuk2; A. Kulczyńska‐Przybik2; M. Bazylewicz1; A. Mirończuk1; A. Czarnowska1; B. Mroczko2; J. Kochanowicz1; A. Kułakowska1
1Department of Neurology, Medical University of Bialystok, Bialystok, Poland; 2Department of Neurodegeneration Diagnostics, Medical University of Bialystok, Bialystok, Poland
Background and Aims: The coronavirus disease 2019 (COVID‐19) course and serological statuses of patients with relapsing‐remitting multiple sclerosis (RRMS) treated with disease‐modifying therapies (DMTs) is similar to the general population. Over the pandemic course a notable increase in the number of RRMS patients who received vaccination against severe acute respiratory coronavirus 2 (SARS‐CoV‐2) and those who had COVID‐19 was reported. This virus and/or vaccination likely influenced DMT‐treated RRMS patients’ serological statuses.
Methods: This investigation assessed the presence and levels of the antibody directed against the S1 protein receptor binding domain (S1RBD) of SARS‐CoV‐2 in 38 DMT‐treated RRMS patients. The antibodies were assessed twice: between March‐June 2021 (visit 1) and March‐June 2023 (visit 2).
Results: Statistical analysis showed that percentages of IgGS1‐RBD results between vaccinated and unvaccinated patients with RRMS were not statistically significant (visit 1: p = 0.089; visit 2 p = 0.501). However, at visit 1, the number of positives was higher in the vaccinated group than in the unvaccinated group, which was significant at the trend level. Moreover, vaccination had a statistically significant effect on anti‐S1RBD antibody levels at visit 1 (p < 0.001) and visit 2 (p = 0.038).
Conclusion: Study group are immunocompetent in terms of the production of neutralizing antibodies. Our research shows that vaccinated group of patients have statistically significantly higher levels of neutralizing antibodies compared to unvaccinated. It was observed over the course of two years of the pandemic. Levels of neutralizing antibodies seem to better reflect the level of protection against the SARS‐CoV‐2 virus than their presence alone, but this requires further research.
Disclosure: No disclosure.
EPO‐260
Radiological markers of neurological manifestations of post‐acute sequelae of SARS‐CoV‐2 infection: A mini‐review
L. Al Qadi 1 ; O. Cull1; J. Stadler1; M. Martin1; A. El Helou2; J. Wagner3; D. Maillet4; L. Chamard‐Witkowski5
1Centre de formation médicale du Nouveau Brunswick, University of Sherbrooke, Moncton, NB, Canada; 2Department of Neurosurgery, The Moncton Hospital, Moncton, NB, Canada; 3Department of Diagnostic Imaging, The Moncton Hospital, Moncton, NB, Canada; 4Vitalité Health Network, Dr. Georges‐L.‐Dumont University Hospital Centre, Moncton, NB, Canada; 5Department of Neurology, Dr.‐Georges‐L.‐Dumont University Hospital Center, Moncton, NB, Canada
Background and Aims: The neurological impact of COVID‐19 infection is concerning, as patients continue to experience various cognitive and psychiatric symptoms for more than 12 weeks post‐infection—a condition known as neurological post‐acute sequelae of COVID‐19 (Neuro‐PASC). Considering significant challenges exist in evaluating its impact, this mini‐review aims to provide up‐to‐date information on the optimal usage, limitations, and benefits of neuroimaging techniques for Neuro‐PASC.
Methods: Our search on PubMed and Google Scholar databases used specific equations for each imaging, such as structural MRI (magnetic resonance imaging), functional MRI, diffusion MRI, SWI (susceptibility‐weighted imaging), SPECT (single‐photon emission computed tomography) imaging, OR PET (positron emission tomography) imaging AND COVID‐19. Articles were then selected with 2 independent reviewers.

FIGURE 1 Prisma Flowchart
Results: 18F‐FDG‐PET/CT and functional MRI demonstrated hypometabolism in cerebral regions directly linked to patient symptoms. Structural MRI studies revealed different findings, such as infarcts, white matter atrophy, and gray matter volume changes. One SPECT imaging study noted frontal lobe hypometabolism, while diffusion MRI showed increased diffusivity in limbic and olfactory cortical systems. The SWI sequence showed abnormalities in white matter near the gray‐white matter junction. A study on 18F‐amyloid PET/CT found amyloid lesions in frontal and anterior cingulate cortex areas, and a study on arterial spin labeling (ASL) found hypoperfusion in the frontal lobe.
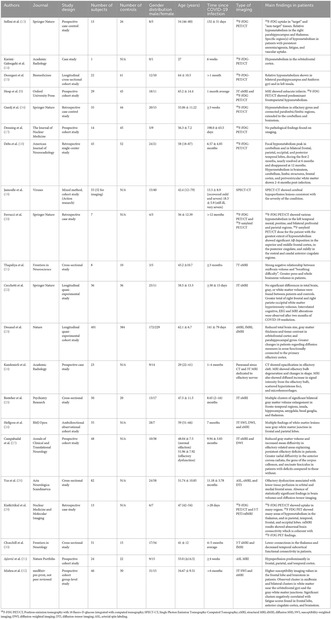
TABLE 1 Summary of the characteristics and findings of the imaging studies included in this review
Conclusion: While accessibility and cost limit the widespread use of 18F‐FDG‐PET/CT scans and functional MRI, they appeared to be the most promising techniques. SPECT, SWI sequence, and 18F‐amyloid PET/CT required further investigation. Nevertheless, imaging remains a reliable tool for diagnosing Neuro‐PASC and monitoring recovery.
Disclosure: Nothing to disclose.
EPO‐261
Functional and cognitive outcomes and trajectories three years after hospitalization for COVID‐19
M. Li 1 ; T. Wisniewski1; Z. Alvarez1; N. Bilici1; L. Caba Caceres1; N. De La Cruz1; C. Engelson1; J. Greenberg1; S. Hammam4; J. Hunter1; S. Karimi1; J. Links3; M. Rodriguez1; F. Silva1; A. Vedvyas3; A. Yakubov1; Y. Ge2; J. Frontera1
1Department of Neurology, NYU Grossmann School of Medicine, New York, NY, USA; 4Hunter College at CUNY, New York, NY, USA; 3Department of Radiology, NYU Grossmann School of Medicine, New York, NY, USA; 2Alzeimer's Disease Research Center, NYU Grossmann School of Medicine, New York, NY, USA
Background and Aims: Little is known about long‐term outcomes and trajectories of recovery after hospitalization for COVID‐19.
Methods: We conducted a prospective, longitudinal cohort study of patients hospitalized for COVID‐19 between 3/2020 and 5/2020. Healthy control patients with no history of COVID‐19 and negative SARS‐COV‐2 nucleocapsid IgG antibodies were also enrolled. Cognitive and functional outcomes as well as post‐COVID symptoms were assessed at 6 and 36 months. Outcomes and symptoms were compared between cases and controls using Mann‐Whitney U‐test and multivariable logistic regression analyses were performed to evaluate the impact of COVID‐19 on 3‐year outcomes. Non‐parametric paired samples Sign test was performed to evaluate changes in metrics over time.
Results: Of 83 subjects, N = 61 COVID‐19 cases (median age 62, 57% female), and N = 22 non‐COVID‐19 controls (median age 75, 23% female) were enrolled. At 3‐years, t‐MoCA was abnormal in 36% of COVID‐19 patients compared to 23% of controls. Multiple neuropsychiatric symptoms occurred at higher frequencies in COVID‐19 patients compared to controls (p < 0.001). eGOS scores were significantly lower in COVID patients compared to controls after adjusting for age and sex (aOR 0.05, 95% CI 0.006–0.440, p = 0.007). Among N = 24 patients that completed 6 and 36‐month follow‐up, mRS scores significantly improved over time (p = 0.003), while no changes were observed in t‐MoCA scores.
Conclusion: At 3 years post‐hospitalization for COVID‐19, neuropsychiatric symptoms were significantly more prevalent and functional outcomes (eGOS) were significantly worse than in controls, even after adjusting for age and sex, despite improvements in mRS from 6 to 36 months.
Disclosure: Thomas Wisniewski has NIH/NIA R01 grant. Yulin Ge has NIH/NIA R01 grant. Jennifer Frontera has NIH R01 grant and NIH/NINDS funding for COVID research. Melanie Li, Zariya Alvarez, Nadir Bilici, Leomaris Caba Caceres, Natasha De La Cruz, Celia Engelson, Julia Greenberg, Salma Hammam, Jessica Hunter, Sohail Karimi, Jon Links, Miguel Rodriguez, Floyd Silva, Alok Vedvyas, Amin Yakubov, have nothing to disclose.
EPO‐262
Innovative in vitro model of human blood‐brain barrier mimicry to study neurological effects of SARS‐CoV‐2
K. Papakosta‐Sampatakaki 1 ; C. Kaldirimitzian1; R. Pontes dos Santos Silva2; J. Júnior Ferraz de Magalhães3; M. Brito Ferreira4; C. Campello Bresani‐Salvi2
1Medical School, National and Kapodistrian University of Athens, Athens, Greece; 2Laboratory of Virology and Experimental Therapy, Oswaldo Cruz Foundation, Ministry of Health of Brazil, Recife, Brazil; 3Central Laboratory of Pernambuco, Secretariate of Health of Pernambuco State, Recife, Brazil, Medicine Department, University of Pernambuco, Serra Talhada, Brazil; 4Neurology Department, Restauração Hospital, Secretariat of Health of Pernambuco, Recife, Brazil
Background and Aims: SARS‐CoV‐2 is implicated in cerebral manifestations, like meningoencephalitis and stroke. Clinical findings and animal models suggest direct and indirect effects of SARS‐CoV‐2 on the cerebral microvascular bed. Few studies have applied in vitro models of human BBB to examine interactions between SARS‐CoV‐2 and the brain. This study aims to validate a novel human BBB model for experiments on molecular and cellular effects of SARS‐CoV‐2.
Methods: Designed as a triple monolayer membrane, this 2D model includes human cerebral microvascular endothelial cells (hCMEC/D3), human neurons (SH‐Sy5y) and human glial cells (U‐87MG). Each cell lineage was cultured alongside Vero cells E6 and CCL81, at 37°C and 5% CO2, in flasks with respective medium: 199 (hCMEC); MEM/F‐12 (SH‐Sy5y); MEM (U‐87MG); DMEM‐HG (Vero). Each 48–72 h, cells’ morphology was checked with an inverted light microscope. Once ≥ 80% confluency was reached, the cells were expanded by transferring to more flasks, until a maximum of 60 transfers. Eventually, a monolayer of each cell was placed into plates’ wells with a semipermeable membrane (Figure 1).
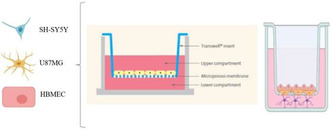
The transwell plates of 96 wells plus inserts with an 8 μm porous membrane (Corning Life Science, USA); a monolayer of endothelial cells in the top chamber (BBB luminal side), and neural and glial cells in the bottom chamber (BBB parenchymal side).
Results: We reached a cell storage (Figure 2) required to plaque 80,000 endothelial cells/mm3 and 150.000 neuronal and glial cells/mm3 per well (concentrations from pilot experiments), and perform all planned experiments: in vitro SARS‐CoV‐2 exposition, in situ cytokines and chemokines measurements, ex vivo observation of white blood cells from patients.
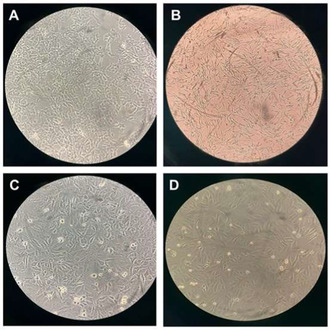
A. Human Neurons (SH‐Sy5y); B. Human Glial Cells (U‐87MG); C. Human Cerebral Microvascular Endothelial Cells (hCMEC/D3); D. Vero Cells CCL81.
Conclusion: This is the first in vitro endothelial‐neural‐glial triple layer model validated to study the interaction between SARS‐CoV‐2, the neurovascular unit and the immunocytes of patients with cerebrovascular or neuroinflammatory syndromes.
Disclosure: Nothing to disclose.
EPO‐263
Small fiber neuropathy following COVID‐19 vaccination: A case series
G. Primicerio; M. Bastholm Bille; S. Birk
Clinical Neurophysiology, Rigshospitalet, Copenhagen, Denmark
Background and Aims: In several vaccination contexts, different peripheral neuropathies have been described as possible adverse effects. Small fiber neuropathy (SFN) is no exception. Therefore, we investigated the relation between SFN and COVID‐19 vaccination.
Methods: We present a case series of 16 patients (F = 14; M = 2) with age 27–64 (50.1 ± 12.1) referred to our Department of Clinical Neurophysiology, Rigshospitalet, Copenhagen, Denmark, with the suspicion of a SFN related to COVID‐19 vaccination, with symptoms ‘debut within the first month after vaccination. Patients were vaccinated towards COVID‐19 with different vaccines and different doses.
Results: All patients underwent nerve conduction studies to exclude a large fiber polyneuropathy, and the following small fiber tests: quantitative sensory testing (QST), quantitative sudomotor axon reflex test (QSART), cutaneous biopsy for intraepidermal fiber density count (IEFND). Following actual criteria, 9 patients were diagnosed with SFN.
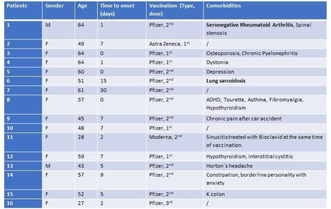
Demographics and general information of patients. In bold most relevant comorbidities.
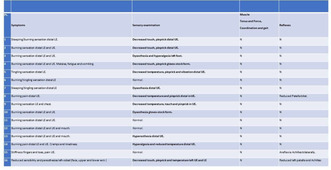
Clinical findings: neurological symptoms and signs.
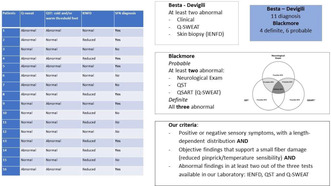
Small Fiber Tests and Small Fiber Neuropathy diagnosis with comparison of different sets of criteria. (Q‐sweat, quantitative sweat test; QST: quantitative sensory test; IENFD: intraepidermal nerve fiber density).
Conclusion: Assessing the causality between a vaccination and a supposed adverse effect is very difficult. However, a wealth of evidence supports our hypothesis. Firstly, other single cases with similar findings are described, both in association with COVID and other vaccines. Secondly, other neurological complications are described in association with vaccination, pointing to a common pathogenesis. Lastly, same neurological symptoms/affections are described with COVID‐19 infection itself. We therefore underline the importance of post‐authorization surveillance to assess adverse effects of vaccines.
Disclosure: Nothing to disclose.
EPO‐264
Patients with neurological or psychiatric complications of COVID‐19 have worse long term functional outcomes: COVID‐CNS
R. Shil 1 ; A. Seed2; B. Sargent3; G. Wood1; Y. Huang1; M. Ellul1; T. Solomon1; B. Michael1
1Clinical Infection, Microbiology & Immunology, Institute of Infection, Veterinary and Ecological Sciences, University of Liverpool, Liverpool, UK; 2Liverpool University Hospitals NHS Foundation Trust, Liverpool, UK; 3Department of Psychiatry, University of Oxford, Oxford, UK
Background and Aims: Patients hospitalised with COVID‐19 often have ongoing morbidity affecting activities of daily living (ADLs), employment, and mental health. However, functional outcomes in patients with COVID‐19 neurological or psychiatric complications are poorly understood. We aimed to assess post‐discharge functional outcomes of these patients relative to those with isolated respiratory COVID‐19.
Methods: We conducted a UK multicentre case‐control study of patients hospitalised with COVID‐19 (controls) and those with acute neurological or psychiatric complications (cases). Data were collected from clinical records and participants followed‐up at 13–16 months for assessment of ADLs, employment, anxiety, and depression.
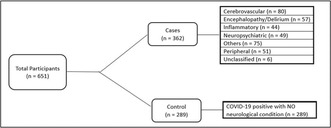
FIGURE 1 Recruitment flowchart
Results: Between March 2020‐July 2022, for 651 patients (362 [56%] cases and 289 [44%] controls), where data were available, a higher proportion of cases than controls had impairment in ADLs (199 [68.9%] vs 101 [51.8%], OR [95% CI] 2.01 [1.40–2.98]) and reported symptoms impacting employment (159 [58.2%] vs 69 [35.6%], OR 2.53 [1.72–3.71]). There was no significant difference in depression or anxiety between overall. For cases, impairment of ADLs was associated with increased risk in females, age >50 years and hypertension (OR 5.43 [1.79–16.96], 3.11 [1.17–8.26], and 3.67 [1.06–12.68]). Those receiving either statins or angiotensin converting enzyme inhibitors had a lower risk (OR 0.09 [0.03–0.37], and 0.17 [0.03–0.84]; AUROC 0.794 [0.71–0.88]).
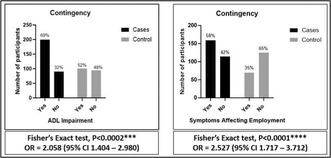
FIGURE 2 Cases vs controls, ADL and Employment. OR: Odds Ratio, CI: Confidence interval
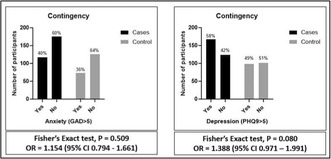
FIGURE 3 Cases vs Controls, anxiety, and depression. OR: Odds Ratio, CI: Confidence Intervals
Conclusion: Patients with neurological or psychiatric complications of COVID‐19 had worse functional outcomes than those with respiratory COVID‐19 alone in terms of ADLs and employment. Female sex, age >50 years, and hypertension were associated with worse outcomes, and statins or ACE inhibitors with better outcomes.
Disclosure: RS, GK and YH are funded by the UK National Institute for Health Research (NIHR) as NIHR academic clinical fellows and ME as NIHR academic clinical lecturers. YH, TS, ME and BM are funded by the NIHR Health Protection Research Unit (HPRU) in Emerging and Zoonotic Infections at University of Liverpool. BM is supported to conduct COVID‐19 neuroscience research by the UKRI/ MRC (MR/V03605X/1). BM is also supported for additional neurological inflammation research due to viral infection by grants from the NIHR (award CO‐CIN‐01), the Medical Research Council (MC_PC_19059) and by the NIHR Health Protection Research Unit (HPRU) in Emerging and Zoonotic Infections at University of Liverpool in partnership with Public Health England (PHE), in collaboration with Liverpool School of Tropical Medicine and the University of Oxford (award 200907), NIHR HPRU in Respiratory Infections at Imperial College London with PHE (award 200927), the MRC/UKRI (MR/ V007181/1), MRC (MR/T028750/1), and Wellcome (ISSF201902/3).
EPO‐265
Longitudinal analysis of 92 subjects reveals structural brain alterations after 1 year of COVID‐19
L. Scardua‐Silva; I. Karmann Aventurato; R. Batista João; A. Beppler Lazaro Lino; B. Amorim da Costa; M. Koutsodontis Machado Alvim; F. Cendes; C. Lin Yasuda
Neuroimaging Laboratory, Universidade Estadual de Campinas (UNICAMP), Campinas, Brasil
Background and Aims: Although Neuroimaging studies have demonstrated structural alterations (most subacute and chronic changes) in individuals after COVID‐19 infection, few studies have assessed brain changes longitudinally. Here, we present a longitudinal analysis of post‐infected individuals, comparing individuals after 3 and 12 months and controls.
Methods: we acquired two longitudinal T1‐structural 3T‐MRI images of 92 post‐infected participants (median interval for the first MRI (T1) = 102 days and second MRI (T2) = 388 days; median age = 42 years; 62 women); and an image of 142 controls (median age = 39.5 years; 99 women). We performed a Voxel‐Based Morphometry analysis with CAT12 longitudinal tools (http://www.neuro.uni‐jena.de/cat/;/SPM12/MATLAB2019b). T‐tests were performed (control group [CG], T1‐patients and T2‐patients) between the different groups (paired t‐test T2P–T1P, t‐test CG–T1P, t‐test CG–T2P). All results were FDR‐corrected for multiple comparisons, and we used total intracranial volume, sex and age as covariates (only for independent t‐tests).
Results: The CG‐T1 analysis showed a trend of atrophy in the left supramarginal atrophy (did not survive FDR correction). The paired comparison (T2P–T1P) revealed atrophy of the right caudate nucleus and hypertrophy of the cerebellum. The CG‐T2 comparison exhibited atrophy of the left supramarginal and left postcentral gyri in the post‐infected subjects.
Conclusion: Our results suggest persistent left supramarginal gyrus atrophy after one year of infection and signs of progressive right caudate atrophy and cerebellum hypertrophy. Further analysis of larger groups (stratified for severity and symptomology) with longitudinal controls is necessary to confirm persistent and dynamic brain changes over time.
Disclosure: Nothing to disclose.
Neuroimmunology 2
EPO‐266
EEG findings in autoimmune encephalitis‐associated epilepsy compared with structural temporal lobe epilepsy
M. Farazdaghi1; A. Burini 2; G. Pauletto3; A. Asadi‐Pooya4; M. Fabris5; F. Lavezzi6; L. Verriello3; M. Valente2; A. Vogrig2
1Epilepsy Research Center, Shiraz University of Medical Sciences, Shiraz, Iran; 2Clinical Neurology, Department of Medicine (DMED), University of Udine, Udine, Italy; 3Neurology Unit, Department of Head‐Neck and Neuroscience, Azienda Sanitaria Universitaria Friuli Centrale (ASU FC), Udine, Italy; 4Department of Neurology, Jefferson Comprehensive Epilepsy Center, Thomas Jefferson University, Philadelphia, PA, USA; 5Clinical Pathology, Department of Laboratory Medicine, Azienda Sanitaria Universitaria Friuli Centrale (ASU FC), Udine, Italy; 6Neurophysiopathology Unit, Department of Head‐Neck and Neuroscience, Azienda Sanitaria Universitaria Friuli Centrale (ASU FC), Udine, Italy
Background and Aims: Autoimmune encephalitis (AE) is a rare yet relevant cause of seizures that requires early treatment to reduce the risk of neurological sequelae and to improve long‐term epilepsy outcome. Clinical scores and diagnostic criteria are useful to suspect AE as the aetiology of seizures, but still fail to identify some patients. An extensive description of electroencephalogram (EEG) specificities in AE patients may facilitate an early diagnosis, using an inexpensive and non‐invasive test.
Methods: We retrospectively reviewed clinical, neuroradiological, laboratory, and EEG data from 19 patients with AE‐associated epilepsy who were treated at Udine University Hospital, Italy. We compared them with a group of 19 consecutive patients with temporal lobe epilepsy (TLE) of structural, non‐immune‐mediated aetiology. EEG findings were classified according to the American Clinical Neurophysiology Society (ACNS) guidelines.
Results: Patients with immune‐mediated seizures had a later age at epilepsy onset (p = 0.024), likely due to the inclusion of paraneoplastic cases, and had more frequent status epilepticus (p < 0.001). Rhythmic and periodic EEG patterns were significantly more frequent in patients with immune‐mediated seizures (p = 0.001; Figure 1: generalized rhythmic delta activity; Figure 2a and b: lateralized periodic discharges), while the presence of focal polymorphic delta activity was higher in the other group (p = 0.004). Seizure outcome was comparable among the two groups: 12/19 seizure‐free AE patients and 10/19 TLE patients at their last follow‐up (p = 0.847).
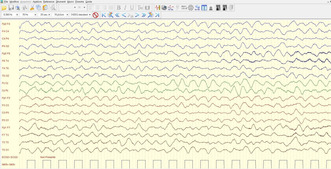
Generalized rhythmic delta activity in a patient with autoimmune encephalitis‐associated epilepsy.
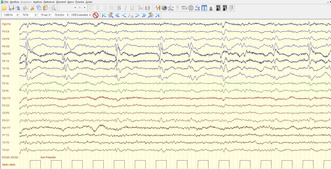
Lateralized periodic discharges in a patient with autoimmune encephalitis‐associated epilepsy.
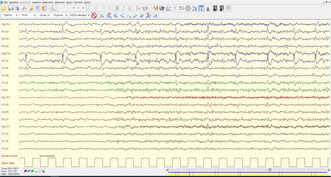
Lateralized periodic discharges in a patient with autoimmune encephalitis‐associated epilepsy.
Conclusion: We highlight some EEG features that may help the clinician to suspect AE and might be integrated into future clinical scores and diagnostic criteria to suspect an immune‐mediated aetiology for focal seizures.
Disclosure: None.
EPO‐267
Clinicoradiological spectrum of primary CNS vasculitis/primary angitis of CNS (PACNS): A case series
B. Bhattacharya; K. Biswas; S. Banerjee; B. Kanti Ray; A. Pandit; S. Dubey
Department of Neurology, Bangur Institute of Neurosciences, Kolkata, India
Background and Aims: PACNS is a rare and devastating inflammatory disorder affecting the CNS. Although headache, cognitive decline and focal neurologic deficits are the clinical hallmarks of PACNS, the disease can have a heterogeneous presentation, leading to diagnostic dilemma. While brain biopsy is confirmatory, it is invasive and patients often opt out of this procedure. In such cases, clinical profiling with imaging (MR studies and DSA) are paramount for prompt diagnosis and treatment. We present 6 atypical cases of probable PACNS, diagnosed clinicoradiologically, to highlight the clinical heterogeneity of the disease and underscore the importance of brain imaging/angiography in establishing earlier diagnosis, when biopsy is not feasible.
Methods: Number of patients: 6 Period: 2022‐2023 Symptomatology: Heterogeneous, suspicious of PACNS (illustrated in attached images) Investigations: Infectious and immune profile, Ophthalmoscopy, MRI (Brain/Cord), MR Vessel Wall, DSA, CSF Study
Results: In MRI, all patients had diffuse white matter lesions with enhancing lesions in 2, ring lesions in 1. Parenchymal and sulcal bleeds were present in 5 patients. 3 patients had evidence of myelopathy, and 2 patients patient had optic neuropathy. All patients showed concentric vessel wall enhancement in MRI with classic beading pattern in DSA. Atherosclerosis and secondary immune causes were excluded in all.
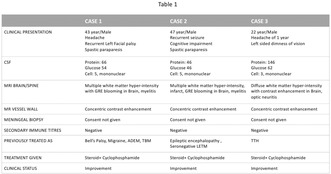
Clinicoradiological profile of patients (table 1).
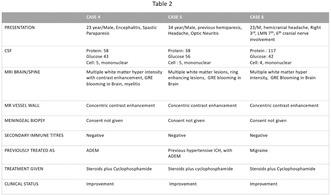
Clinicoradiological profile of patients (table 2).
Vessel wall MRI showing contrast enhancement in bilateral internal carotid arteries.
Conclusion: The cases highlight the importance of imaging findings of parenchymal/sulcal microbleeds, underscoring the role of vessel wall MRI and angiographic findings in suspected cases of PACNS as virtual biopsy, where histopathology is missing. Further, isolated myelitis and optic neuropathy can be the first or sole presentation of PACNS, as elucidated.
Disclosure: Nothing to disclose.
EPO‐268
Exploring the role of EBV in MS pathogenesis starting from EBV interactome
C. Ballerini 1; E. Portaccio1; E. De Meo1; V. Penati1; A. Caporali1; R. Amoriello2; O. Maghrebi2; M. Amato1
1Department of Neurosciences, Psychology, Drug Research and Child Health (NEUROFARBA), University of Florence, Florence, Italy; 2Department of Clinical and Experimental Medicine (DMSC), University of Florence, Florence, Italy
Background and Aims: Epstein‐Barr virus (EBV) has been described as one of the main risk factors for developing multiple sclerosis (MS). The molecular mechanisms of this association are complex and may involve different immunological routes; however, the ultimate role of EBV in the pathogenesis of MS is still missing. To identify MS associated genes overlapping with EBV interactome and their expression in immune cell subtypes.
Methods: We obtained EBV interactome from p‐HIPSTER, the MS associated genes from NHGRI‐EBI and the single cell gene expression from B and T‐cells, astrocytes, macrophages, granulocytes, monocytes, microglia, dendritic and natural killer cells from the Human Protein Atlas. We overlapped the lists thus obtained by using the geneOverlap R package.
Results: We identified a “core” group of 15 genes resulting from the overlap between EBV interactome and MS associated genes and expressed in all immune cell type selected (p < 0.001). We selected transcriptomic studies from GEO that analyze gene expression at glial cell's level.
Conclusion: The present findings suggest a broad range immune system involvement in mediating EBV effect on MS pathogenesis. We find a statistically significant up regulation compared to healthy controls for MINK1 in glial cells, MEF2C for astrocytes and MAPK3 for microglia.
Disclosure: Nothing to disclose.
EPO‐269
Real‐world evidence for ofatumumab in multiple sclerosis: A sicilian multicenter experience
C. Chisari 1; S. Bucello2; S. Cottone3; L. Grimaldi4; P. Ragonese5; S. Realmuto6; S. Toscano7; G. Salemi5; F. Patti1
1Department of Medical and Surgical Sciences and Advanced Technologies “G.F. Ingrassia”, University of Catania, Catania, Italy; 2Multiple Sclerosis Center, “E. Muscatello” Hospital – ASP8, Augusta (SR), Italy; 3A.R.N.A.S. CIVICO, Palermo, Italy; 4Neurology and Multiple Sclerosis Center, Unità Operativa Complessa (UOC), Foundation Institute “G. Giglio”, Cefalù, PA, Italy; 5Department of Biomedicine, Neurosciences and Advanced Diagnostics, University of Palermo, Palermo, Italy; 6Multiple Sclerosis Centre, Neurology Unit and Stroke Unit, AOOR “Villa Sofia‐Cervello”, Palermo, Italy; 7Department of Neurology, Ospedale Garibaldi Centro, Catania, Italy
Background and Aims: Ofatumumab (OFA), a human recombinant IgG1 CD20 next‐generation monoclonal antibody, was investigated in two phase III trials, showing significant reductions of the relapse‐rate and of confirmed disability compared to teriflunomide. However, to date, real world data about the effectiveness of OFA are still scarce. We aimed to evaluate efficacy and safety of OFA in a real‐world setting.
Methods: this prospective real‐world study consecutively screened all relapsing‐remitting Multiple Sclerosis (RRMS) patients from seven Italian MS centers, who were treated with OFA in the period between August 2022 and January 2024. Data about Expanded Disability Status Scale (EDSS), relapses, previous treatments, adverse events (AEs) and magnetic resonance imaging (MRI) were collected.
Results: A total of 223 patients (136 [61%] women, mean age of 39.8±10 years), were enrolled. Of these, 68 (30.5%) were naïve to treatment and 155 (69.5%) switched from another DMTs. After 6 months from OFA initiation, 206 (92.4%) of patients were EDSS progression free, 220 (98.7%) were relapse‐free and 188 (84.3%) were MRI activity‐free. Among 64 (28.7%) who continued treated for 12 months, 62 (96.9%) were EDSS progression free, 64 (100%) were relapse‐free and 60 (93.8%) were MRI activity‐free. No significant differences were found between naive and switch groups. No serious AEs were reported. Particularly, fever at the first administration was the most frequent AE reported in 179 (80.3%) patients.
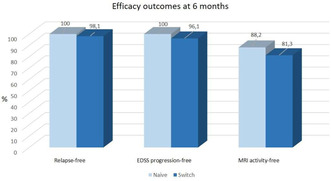
Efficacy outcomes after 6 months of treatment with Ofatumumab in naive and switch groups.
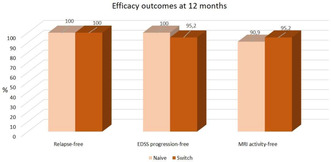
Efficacy outcomes after 12 months of treatment with Ofatumumab in naive and switch groups.
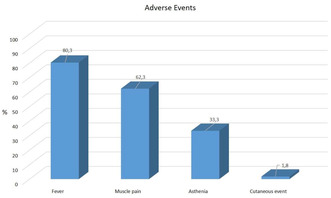
Percentage of patients reporting adverse events.
Conclusion: We confirmed that OFA is effective in reducing risk of progression and disease progression in a real‐world cohort of RRMS patients, also demonstrating a favorable safety profile.
Disclosure: Francesco Patti has received honoraria for speaking activities by Almirall, Bayer Schering, Biogen, Merck Serono, Novartis, Roche, Sanofi Genzyme, and TEVA; he also served as advisory board member the following companies: Bayer Schering, Biogen Idec, Merck Serono, Novartis, Roche, Sanofi Genzyme, and TEVA; he was also funded by Pfizer and FISM for epidemiological studies; he received grants for congress participation from Almirall, Bayer Shering, Biogen Idec, Merck Serono, Novartis, Roche, Sanofi Genzyme, and TEVA. Other authors have nothing to disclose.
EPO‐270
Rituximab as first‐line or escalation immunotherapy in aquaporin‐4‐IgG‐positive neuromyelitis optica spectrum disorder
D. Engels 1; C. Rocchi2; M. Forcadela2; J. Havla1; M. Ringelstein3; O. Aktas3; K. Giglhuber4; A. Berthele4; M. Hümmert5; C. Trebst5; S. Huda2; T. Kümpfel1
1Institute of Clinical Neuroimmunology, LMU Hospital, Ludwig‐Maximilians University Munich, Munich, Germany; 2Department of Neurology, Walton Centre NHS Foundation Trust, Liverpool, UK; 3Department of Neurology, Medical Faculty and University Hospital Düsseldorf, Heinrich Heine University Duesseldorf, Germany; 4Department of Neurology, School of Medicine, Technical University Munich, Klinikum rechts der Isar, Munich, Germany; 5Department of Neurology, Hannover Medical School, Hannover, Germany
Background and Aims: Aquaporin‐4‐IgG‐positive neuromyelitis optica spectrum disorder (AQP4‐IgG+ NMOSD) primarily manifests with attacks of optic neuritis or myelitis. Rituximab is highly efficient in reducing the likelihood of NMOSD attacks. However, not all patients receive rituximab as first‐line therapy. Here, we compared the treatment efficacy between rituximab as first‐line and escalation immunotherapy.
Methods: We analyzed retrospective clinical data from AQP4‐IgG+ NMOSD patients from neuroimmunology outpatient clinics in the United Kingdom (Liverpool) and Germany (Duesseldorf, Hannover, Munich).
Results: AQP4‐IgG+ NMOSD patients received rituximab as first‐line (n = 58) or escalation (n = 96) immunotherapy. Administered as first‐line immunotherapy, rituximab was associated with a higher probability of an attack‐free disease course (beta [95%‐CI] = ‐0.92 [‐1.52;‐0.33], p < 0.005, Cox proportional hazards regression coefficient, H0: beta = 0). Younger age at diagnosis and being male was associated with a higher probability of an attack‐free disease course. Eleven patients showed a significant annualized expanded disability status scale (EDSS) progression (AEP) during rituximab immunotherapy. Higher annualized attack rates (AAR) during rituximab immunotherapy predicted a significant AEP. In contrast, AAR before rituximab immunotherapy, age at diagnosis and whether rituximab was administered first‐line or as escalation immunotherapy showed no effect on AEP. Patients who showed significant AEP during rituximab had competing risk factors for attacks such as severe comorbidities, anti‐rituximab antibodies or deviations from their treatment protocol (e. g. due to pregnancy).
Conclusion: Early use of highly effective immunotherapies in AQP4‐IgG+ NMOSD such as rituximab can reduce further disease activity and thereby potentially prevent disability progression.
Disclosure: DE received speaker honoraria from Alexion and Horizon. CR is currently a clinical and research training fellow funded by ECTRIMS. JH reports a grant for OCT research from the Friedrich‐Baur‐Stiftung and Merck, personal fees and nonfinancial support from Merck, Alexion, Novartis, Roche, Celgene, Biogen, Bayer and Horizon and nonfinancial support of the Sumaira‐Foundation and Guthy‐Jackson Charitable Foundation, all outside the submitted work. AB receives funding from the Innovationsausschuss of the German Federal Joint Committee (G‐BA; grant 01VSF23040) and from the German Federal Ministry of Education and Research (BMBF; grant 01ZZ2102B). He has received consulting and/or speaker fees from Alexion, Argenx, Biogen, Horizon, Merck, Novartis, Roche and Sandoz/Hexal, and his institution has received compensation for clinical trials from Alexion, Biogen, Merck, Novartis, Roche, and Sanofi Genzyme; all outside the present work. MWH received research support from Myelitis e. V., speaker honoraria from selpers og, Horizon and Alexion, and reimbursement of travel expenses and compensation for serving on an advisory board from Alexion. TK has received speaker honoraria and/or personal fees for advisory boards from Novartis Pharma, Roche Pharma, Alexion/AstraZeneca and Biogen. All other authors have nothing to disclose in relation to this project.
EPO‐271
Cerebral thrombi analysis in cancer‐related stroke
B. Dell'acqua 1; M. Montano2; A. Bergamaschi2; P. Panni3; G. Saliou4; P. Michel5; L. Roveri6; G. Martino2; M. Filippi6; D. Strambo5; M. Bacigaluppi1
1Neuroimmunology Unit, Division of neuroscience, Department of Neurology, Institute of Experimental Neurology, Stroke Unit San Raffaele Hospital, Milan, Italy; 2Neuroimmunology Unit, Division of neuroscience, Institute of Experimental Neurology, San Raffaele Scientific Institute, Milan, Italy; 3Department of Neuroradiology, San Raffaele Hospital, Milan, Italy; 4Department of Diagnostic and Interventional Radiology, Lausanne University Hospital, Lausanne, Switzerland; 5Department of Clinical Neurosciences, Stroke Centre, Neurology Service, Lausanne University Hospital, Switzerland; 6Department of Neurology, Stroke Unit San Raffaele Hospital, Milan, Italy
Background and Aims: Stroke is a frequent complication in neoplastic patients. Lung, gastrointestinal, gynecologic tumors have a higher incidence of cerebral thrombosis. The mechanism undergoing the stroke presentation in active cancer patients is unclear; primary and secondary prevention therapy need further studies.
Methods: We analyzed 20 patients with a diagnosis of active cancer (AC) with large vessel occlusion stroke treated with mechanical endovascular thrombectomy (EMT). Active cancer was defined as a tumor diagnosis <6 months and/or undergoing an active treatment over the past 6 months and/or metastatic cancers. 7 patients had lung tumor, 5 gynecologic neoplasm (breast and ovary), 6 gastrointestinal (pancreatic, gastric, colorectal) and 2 urinary tract cancer. We evaluated the histological composition of AC thrombi compared to 20 matched controls (for sex, age and pre‐stroke therapy) with an history of inactive tumor.
Results: The median baseline NIHSS was higher (21) in lung tumor patients (p 0.03). D‐dimer values had a higher trend in gastrointestinal tumors, with a major risk of coagulopathy (p 0.04). AC thrombi displayed lower neutrophil (MPO+) counts (p 0.03) and higher platelets (CD61+) counts (p 0.04) compared to controls. No differences were found in term of neutrophil extracellular traps (CITH3+). A statistically significant correlation between acute blood fibrinogen value and the platelets thrombus content (p value 0.01).
Conclusion: Thrombus composition and blood biomarkers could be important tools to understand pathophysiological mechanism and possible secondary prevention therapy in cancer related stroke patients.
Disclosure: Nothing to disclose.
EPO‐272
Comparison of serum NFL values in multiple sclerosis using SIMOA and lumipulse platforms: A real‐world study in Greece
D. Tzanetakos 1; C. Stergiou2; J. Kuhle3; E. Dimitriadou1; A. Akrivaki1; G. Papagiannopoulou1; S. Giannopoulos1; G. Tsivgoulis1; S. Tzartos2; J. Tzartos1
1Second Department of Neurology, School of Medicine, Attikon University Hospital, National and Kapodistrian University of Athens, Athens, Greece; 2Tzartos NeuroDiagnostics, Athens, Greece; 3Department of Neurology, University Hospital Basel and University of Basel, Basel, Switzerland
Background and Aims: Serum neurofilament light chain (sNfL) as a biomarker of neuronal axonal loss has an emerging value in monitoring disease activity and progression in Multiple Sclerosis (MS). SIMOA™ and Lumipulse™ are two platforms for sNfL measurement. Our aim was to compare sNfL measurements by both methodologies in MS patients investigating for discrepancies in the comparative results.
To compare serum neurofilament light chain (sNFL) measurements by SIMOA and Lumipulse in Multiple Sclerosis (MS) patients.
Methods: sNfL concentrations from 44 patients (57 samples) with Relapsing Remitting (RRMS) and Progressive MS (PMS) from an MS center were measured by SIMOA and Lumipulse. Results were stratified by z‐scores in 4 groups: a) low, z‐score≤0.84, b) medium, 0.84 < z‐score≤1.5, c) high, 1.5 < z‐score≤ 2, d) very high, z‐score >2.
Results: 33 RRMS and 11 PMS (5 Secondary Progressive, 6 Primary Progressive) were included; median age 36.97 and 47.42 years respectively. In the RRMS‐group (46 samples), 31 had sNfL z‐scores in agreement between both methods (67.39% agreement): 16 with low, 5 with medium, 4 with high, 6 with very high z‐scores. In 15/46 RRMS samples there was disagreement between SIMOA and Lumipulse z‐scores; in 10 samples, differences were by one step (low‐vs‐medium, medium‐vs‐high, high‐vs‐very high), in 5 differences were by two steps. In the PMS‐group, sNfL‐z‐scores in 8/11 (72.73%) samples were in agreement between platforms, whereas in 3 samples there was disagreement by one step.
sNfL z‐scores from 33 Relapsing Remitting (RRMS) and 11 Progressive MS (PMS) patients showed a percentage of agreement between both methods 67.39% for the RRMS‐group and 72.73% for the PMS‐group.
Conclusion: SIMOA‐ and Lumipulse‐measured sNfL z‐scores were similar in the ~70% of MS patients (in both PMS and RRMS groups). Our next goal is to elaborate on the sera with different z‐scores between methods to compare their clinical value.
SIMOA‐ and Lumipulse‐measured sNfL z‐scores were similar in the ~70% of MS patients (in both PMS and RRMS groups).
Disclosure: ST has shares in the company Tzartos NeuroDiagnostics. DT, CS, JK, EMD, AA, GP, SG, GT, JT: Nothing to disclose.
EPO‐273
Autoimmune screening panel in patients with multiple sclerosis – A Vienna MS database study
F. Foettinger; N. Krajnc; K. Riedl; F. Leutmezer; P. Rommer; B. Kornek; G. Zulehner; T. Berger; G. Bsteh
Department of Neurology, Medical University of Vienna, Vienna, Austria
Background and Aims: Autoimmune screening panel (ASP) is routinely ordered as a part of diagnostic work‐up in people with suspected multiple sclerosis (MS). However, data on prevalence and significance of ASP seropositivity in MS is scarce.
Methods: We retrospectively investigated patients from the Vienna MS database (VMSD) who were diagnosed with MS between 2014 and 2023 according to current McDonald criteria and had blood samples drawn for ASP. Autoantibody titers were defined as either negative, or mildly (≤1:160), moderately (1:320‐1:640) and strongly (≥1:1280) positive.
Results: We analyzed 212 patients (median age 29 [IQR 25–36] years, 67.0% female). Ten (4.7%) patients had red flags for presence of systemic autoimmune disease (joint pain [n = 4], dermatitis [n = 3], sicca syndrome [n = 2], bronchial asthma/rheumatic fever in childhood [each n = 1]). Complement levels (C3c and C4) were below the lower reference level in 26/134 (19.4%) and 3/134 (2.2%), respectively, and C4 levels were above the upper reference level in 3/134 (2.2%). Antinuclear antibodies (ANA) were positive in 24/210 (11.4%) with 18 (8.6%), 5 (2.4%), and 1 (0.5%) having mildly, moderately, and strongly positive ANA titers, respectively. Positive autoantibodies were found as follows: anti‐Ro (5/211; 2.4%), IgM against cardiolipin (4/205; 2.0%), anti‐centromere B (2/211; 0.9%), anti‐dsDNA (1/208; 0.5%) and anti‐La (1/211; 0.5%). Further evaluation following positive results led to diagnosis of rheumatoid arthritis (n = 2) and Sjögren's syndrome (n = 1). (ASP positive predictive value 9.1%, negative predictive value 97.2%)
Conclusion: Rate of ASP seropositivity in MS is low, aligning with the general population. Performance of ASP without clinical suspicion of systemic autoimmune disease appears unwarranted.
Disclosure: Nothing to disclose.
EPO‐274
Retinal neuroaxonal loss and disease progression in multiple sclerosis
F. Burguet Villena 1; L. Hofer2; N. Cerdá Fuertes2; S. Sellathurai2; S. Schaedelin2; K. Schoenholzer1; M. D'Souza1; J. Oechtering1; L. Kappos3; C. Granziera4; P. Benkert2; J. Kuhle1; A. Papadopoulou1
1Department of Neurology, University Hospital Basel, Basel, Switzerland; 2Department of Clinical Research, University Hospital and University of Basel, Basel, Switzerland; 3Research Center for Clinical Neuroimmunology and Neuroscience Basel (RC2NB), University Hospital and University of Basel, Basel, Switzerland; 4Translational Imaging in Neurology (ThINK) Basel, Department of Biomedical Engineering, Faculty of Medicine, University Hospital and University of Basel, Basel, Switzerland
Background and Aims: Progression Independent of Relapse Activity (PIRA) is the main driver of disability in multiple sclerosis (MS). Retinal neuroaxonal loss measured by optical coherence tomography (OCT) is associated with cortical thinning and neurodegeneration. We aimed to evaluate the association between OCT markers and PIRA in patients with MS.
Methods: We included patients from the Swiss MS Cohort Study with ≥1 OCT. Peripapillary retinal nerve fiber layer (pRNFL) thickness, ganglion cell inner plexiform layer (GCIPL)‐, and inner nuclear layer (INL) volumes were assessed. Eyes with prior optic neuritis were excluded. Neurological examination was performed every 6‐12 months including the Expanded Disability Status Scale. PIRA events were defined as previously described (Table 1). Annualized PIRA rate was the number of PIRA events divided by years of follow‐up, during a period of ≥4 years before the OCT (Table 1). We examined the association of OCT markers with annualized PIRA rate in linear regression models adjusted for disease duration, age at disease onset, sex, body mass index, and treatment.
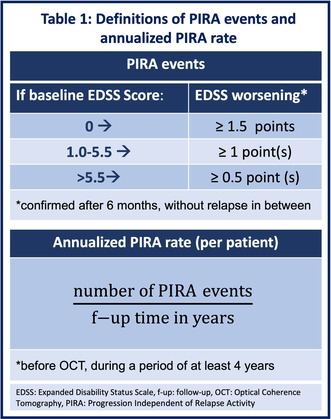
Results: Baseline characteristics at time of OCT are shown in Table 2. The adjusted models estimated that mean pRNFL thickness and GCIPL volume decrease by 28.4 μm respectively 0.53 mm3 with each additional PIRA event per year (Table 3). No association was found for INL.
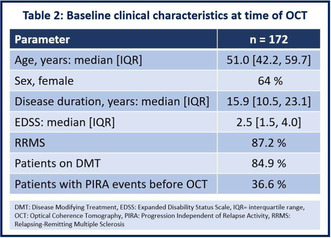
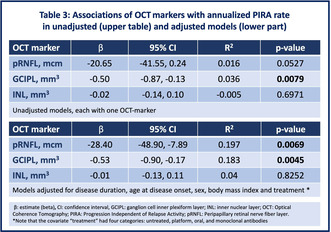
Conclusion: Our findings show an association between rate of PIRA and retinal neuroaxonal integrity. pRNFL and GCIPL may represent a sensitive measure of disease progression in MS.
Disclosure: FBV support by TEVA and research grant (“Young talents in clinical research”) MD: CEO of NeurostatusAG, support from BayerAG, Biogen, TevaPharmaceuticals and SanofiGenzyme and from the University Hospital of Basel (UHB). JO advisory boards for Roche and Merck. LK institutions (UHB and RC2NB) support by Actelion,Addex,Almirall,BayerHealthCare,Celgene,CLC,Behring,Genentech,GeNeuro,Genzyme,MerckSerono,Mitsubishi,Pharma,Novartis,Octapharma,Ono,Pfizer,Receptos,Roche,Sanofi‐Aventis,Santhera,Siemens,Teva,UCB,andXenoPort; licence fees for Neurostatus products; research grants from the Swiss MS Society (SMSS), the Swiss National Research Foundation (SNRF), the EU, and the Roche Research Foundation. Stefano Magon, SMSS, Swiss National Science Foundation (SNSF), University of Basel (UB) and Stiftung zur Förderung der gastroenterologischen und allgemeinen klinischen Forschung sowie der medizinischen Bildauswertung (SFGAKFMB).Travel support from Biogen and Genzyme. CG:UHB (USB),as the employer of C.G., received fees for research support: (i) advisory board from ActelionGenzyme‐Sanofi, Novartis, GeNeuro and Roche; (ii) speaker fees from Genzyme‐Sanofi, Novartis, GeNeuro and Roche. JK received support and/or served on advisory boards by SMSS,SNRF,UB,ProgressiveMSAlliance,Bayer,Biogen,BristolMyersSquibb,Celgene,Merck,Novartis,OctaveBioscience,Roche,Sanofi. AP speaker‐fees/fees for advisory boards from Sanofi‐Genzyme, EliLilly, AbbVie, Lundbeck, TEVA, BayerAG and Roche. All other authors have nothing to disclose.
EPO‐275
Safety of inebilizumab in participants over 50 and 65 years of age with neuromyelitis optica spectrum disorder (NMOSD)
F. Paul 1; Y. Mao‐Draayer2; D. Wingerchuk3; J. Graves4; A. Kunchok5; E. Lackey6; K. Fujihara7; D. Sato8; Z. Wang9; K. Patterson9; B. Cree10
1Experimental and Clinical Research Center, Max Delbrück Center for Molecular Medicine and Charité Universitätsmedizin Berlin, Germany; 2MS Center of Excellence, Oklahoma Medical Research Foundation, Oklahoma City, OK, USA; 3Department of Neurology, Mayo Clinic, Scottsdale, AZ, USA; 4Department of Neurology, University of San Diego Health, San Diego, CA, USA; 5Department of Neurology, Mellen Center for Multiple Sclerosis, Cleveland Clinic, Cleveland, OH, USA; 6Department of Neurology, Division of MS & Neuroimmunology, Duke University, Durham, NC, USA; 7Department of Multiple Sclerosis Therapeutics, Fukushima Medical University, Fukushima, Japan, and Multiple Sclerosis and Neuromyelitis Optica Center, Southern Tohoku Research Institute for Neuroscience, Koriyama, Japan; 8Department of Multiple Sclerosis Therapeutics, Fukushima Medical University, Fukushima, Japan, and Multiple Sclerosis and Neuromyelitis Optica Center, Southern Tohoku Research Institute for Neuroscience, Koriyama, Japan; 9Amgen Inc, Thousand Oaks, CA USA; 10UCSF Weill Institute for Neurosciences, Department of Neurology, University of California San Francisco, San Francisco, CA, USA
Background and Aims: Inebilizumab is approved for aquaporin‐4 seropositive (AQP4‐IgG+) NMOSD. Here we evaluate the safety of inebilizumab in AQP4‐IgG+ NMOSD participants ≥50 and ≥65 years of age.
Methods: N‐Momentum (NCT02200770) was a phase 2/3 trial (randomized 3:1, inebilizumab 300 mg: placebo) with an open‐label‐extension‐period (OLP) ≥2 years. Post hoc analyses were conducted to analyze outcomes in AQP4‐IgG+ participants <50, ≥50, and ≥65 years of age.
Results: Of 213 AQP4‐IgG+ NMOSD participants, 65 (30.5%) were ≥50 years, 10 (4.9%) were ≥65 years. In the RCP, among inebilizumab participants ≥50 years, 31.3% (15/48) reported ≥1 investigational product related treatment emergent AE (IP‐TEAE) versus 35.3% (6/17) in placebo. Among participants <50 years IP‐TEAEs were 22.1%(25/113) in the inebilizumab group and 20.0% (7/35) in the placebo group. For patients ≥65 years in the RCP, 66.7% (4/6) inebilizumab and 25% (1/4) placebo patients had IP‐TEAEs. Infections were reported in 66.7% (4/6) of inebilizumab and 100% (4/4) of placebo patients ≥65 years. The most frequent AE was urinary tract infection in 50% (3/6) of inebilizumab and 75% (3/4) of placebo participants ≥65 years. No IP‐related serious AEs or deaths occurred in the participants ≥50 years in either treatment group of the RCP. The NMOSD related annualized hospitalization rate (95% CI) in the OLP for participants ≥50 years, ≥65 years, and <50 years were 0.16 (0.06 – 0.42, n = 65), 0.19 (0.04‐1.01, n = 10), and 0.13 (0.08– 0.22, n = 148) respectively.
Conclusion: This data supports the safety of inebilizumab in AQP4‐IgG+ NMOSD participants ≥50 and ≥65 years of age although evaluation of larger populations is needed to confirm these results.
Disclosure: F Paul: Bayer, Biogen Idec, Merck Serono, Novartis, Sanofi Genzyme, Teva, DFG Exc 257, GCNMS, Guthy‐Jackson Charitable Foundation, Novartis. Y Mao‐Draayer: Acorda, Bayer, Biogen, Bristol Myers Squibb‐Celgene, Chugai, EMD Serono, Genentech‐Roche, Janssen, TG Therapeutics, Horizon, Novartis, Sanofi‐Genzyme, Teva Pharmaceuticals, Chugai, Genentech‐Roche, NIAID Autoimmune Center of Excellence, NIH NINDS, Novartis, PCORI, Sanofi‐Genzyme. D Wingerchuk: Genentech, Horizon, Novartis, Reistone Biopharma, Bristol Meyer Squib, Imcyse, Merck, Roche, UCB Pharma, Alexion, and UCB Pharma. J Graves: Horizon, TG Therapeutics, and Novartis. A Kunchok: Genentech, Horizon, and EMD Serono. EA Lackey: EMD Serono, Sanofi, and Doximity. K Fujihara: AbbVie, Alexion, Asahi Kasei Kuraray Medical Co., Biogen, Chugai/Roche, Eisai, Japan Tobacco, MedImmune/Viela Bio, Merck, Merck Biopharma, Mitsubishi‐Tanabe, Novartis, Teijin, Takeda, UCB, and Ministry of HWL of Japan. DK Sato: CNPq, FAPERGS, Teva, Merck, Biogen, Merck, Roche, Horizon, and Alexion. Z Wang, D Cimbora and KR Patterson: Amgen Inc. BAC Cree: Alexion, Atara, Autobahn, Avotres, Biogen, Boston Pharma, EMD Serono, Gossamer Bio, Hexal/Sandoz, Horizon, Immunic AG, Kyverna, Neuron23, Novartis, Sanofi, Siemens, TG Therapeutics and Genentech.
EPO‐276
Clinical and pathophysiological implications of intrathecal MOG‐IgG synthesis for cerebrospinal fluid MOG‐IgG detection
G. Greco 1; M. Risi2; S. Masciocchi1; P. Businaro1; E. Rigoni3; L. Diamanti3; T. Foiadelli4; M. Giannoccaro5; R. Liguori5; P. Barone6; A. Tozzo7; S. Gelibter8; F. Patti9; P. Banfi10; A. Simone11; M. Ruggieri12; G. Bruno13; S. Siliquini14; S. Bova15; M. Di Filippo16; R. Lanzillo17; A. Gallo2; E. Colombo3; D. Franciotta3; M. Gastaldi3
1Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; 2Department of Advanced Medical and Surgical Sciences, University of Campania “Luigi Vanvitelli”, Naples, Italy; 3IRCCS C. Mondino Foundation National Neurological Institute, Pavia, Italy; 4Clinica Pediatrica, Fondazione IRCCS Policlinico San Matteo, University of Pavia, Pavia, Italy; 5Department of Biomedical and Neuromotor Sciences, University of Bologna, Bologna, Italy; 6Neurology Unit, University Hospital “San Giovanni di Dio e Ruggi d’Aragona”, Salerno, Italy; 7Department of Pediatric Neuroscience, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy; 8Department of Neurosciences, Neurology and Stroke Unit, ASST Grande Ospedale Metropolitano Niguarda, Milan, Italy; 9Department of Medical and Surgical Sciences and Advanced Technologies, University of Catania ‘G.F. Ingrassia’, Catania, Italy; 10Neurology and Stroke Unit, ASST SetteLaghi, Ospedale di Circolo/Fondazione Macchi, Varese, Italy; 11Neurology Unit, Carpi Hospital, AUSL Modena, Carpi, Italy; 12Department of Clinical and Experimental Medicine, Section of Pediatrics and Child Neuropsychiatry, University of Catania, Catania, Italy; 13Pediatric Neurology Unit, Department of Neurosciences, Santobono‐Pausilipon Children's Hospital, Naples, Italy; 14Child Neurology and Psychiatry Unit, “G. Salesi” Children's Hospital, Azienda Ospedaliero Universitaria delle Marche, Ancona, Italy; 15Pediatric Neurology Unit, Buzzi Children's Hospital, Milan, Italy; 16Section of Neurology, Department of Medicine and Surgery, University of Perugia, Perugia, Italy; 17Department of Neurosciences and Reproductive and Odontostomatological Sciences, University of Naples Federico II, Naples, Italy
Background and Aims: Diagnosis of MOG antibody‐associated disease (MOGAD) relies on the detection of serum MOG‐IgG with cell‐based assays (CBA). Clinical and diagnostic relevance of CSF MOG‐IgG needs further assessment.
Methods: we retrospectively studied consecutive patients with paired serum and CSF samples screened for MOG‐IgG using a live CBA. Antigen‐specific Antibody Index (AIMOG‐IgG) was calculated to assess intrathecal MOG‐IgG synthesis (MOG‐IgG ITS). An aggregated analysis of literature data on CSF MOG‐IgG and findings from another centre were used for comparison with our results.
Results: MOG‐IgG were found in 55/960 patients. Serum/CSF MOG‐IgG titres showed a significant correlation in patients without ITS (rho = 0.47, p < 0.001), but not in those with ITS (rho = 0.14, p = 0.65). There were no clinical‐paraclinical differences between MOG‐IgG CSF+ vs CSF‐ patients. Conversely, patients with MOG‐IgG ITS showed more frequent pyramidal symptoms (73% vs 32%, p = 0.03), spinal cord involvement (82% vs 39%, p = 0.02), and severe outcome at follow up (36% vs 5%, p = 0.02) than those without MOG‐IgG ITS. MOG‐IgG ITS was the only predictor of a poor outcome in the multivariate logistic regression model (OR: 9.87 [CI: 1.22–86.88], p = 0.039). In cohorts with consecutive patients (n = 3148), positive predictive value (PPV) was higher for MOG‐IgG seropositivity (99.43% [CI: 97.76%–99.86%]), than for CSF‐restricted MOG‐IgG positivity (83.9% [CI: 72.07% ‐ 91.36%]).
Conclusion: Consistently with physiopathology, our data suggest that the implementation of ITS calculation could enhance clinical, prognostic, and therapeutic purposes of CSF MOG‐IgG testing, making a case for its introduction in clinical practice.
Disclosure: Nothing to disclose.
EPO‐277
Evaluating the role of MOG antibodies in pseudotumor cerebri presentations: A clinical perspective
G. Çetin Erci; H. Güdek; D. Çetinkaya Tezer; İ. Güngör Doğan; S. Demir
Sancaktepe Research and Training Hospital, İstanbul, Turkey
Background and Aims: Pseudotumor cerebri (PTC), characterized by symptoms and signs of increased intracranial pressure without an occupying lesion, can overlap clinically with Optic Neuritis (ON) and may co‐occur in patients. This study examines the relationship between Myelin Oligodendrocyte Glycoprotein (MOG) antibodies, which can be observed in ON, and PTC in patients presenting with symptoms indicative of increased intracranial pressure.
Methods: The study included 42 patients who were evaluated with a preliminary diagnosis of PTC. Anti‐MOG antibodies were assessed using flow cytometry and live cell‐based assays.
Results: Findings revealed MOG IgG positivity in 9 female patients, with significantly high titers in two patients. Notably, one patient was initially diagnosed with PTC, but was later identified as having ON and was diagnosed with MOGAD. A significant portion of MOG+ patients met the Dandy criteria for 'Definite PTC', whereas MOG positivity was more prevalent in patients classified as 'Probable' or 'Possible PTC' according to the Friedman criteria but did not meet the Dandy criteria. Common symptoms in both MOG positive and negative groups included transient visual loss and headache, with the former significantly associated with positivity.
Conclusion: This study emphasizes including MOG‐AD in PTC differential diagnosis, noting the need for thorough evaluation and exploring MOG antibodies' role in Pseudotumor Cerebri etiology.
Disclosure: Nothing to disclosure.
EPO‐278
Real‐world experience of efgartigimod treatment for autoimmune encephalitis
C. Han; B. Zhihong; W. Haotian; Q. Wei; L. Zhengqi; Z. Bingjun
The Department of Neurology, The Third Affiliated Hospital of Sun Yat‐sen University, Guangzhou, China
Background and Aims: Efgartigimod, approved in China for AChR Ab+gMG in September 2023, mechanism of action involves binding to FcRn and competitively blocking endogenous IgG binding to FcRn, leading to IgG degradation at lysosomes and subsequent acceleration of IgG clearance in vivo. However, limited evidence in other IgG‐mediated disorders like autoimmune encephalitis (AE). This study aims to describe the treatment outcomes of autoimmune encephalitis patients treated with efgartigimod.
Methods: 12 AE patients treated in Neurological Care Unit (NICU) in 2023 were included and categorized into traditional treatment group and add‐on efgartigimod treatment group. The latter received efgartigimod at 20mg/kg at weekly intervals. The evaluation relied on electronic medical records, focusing on Modified Rankin Scale (mRS) scores and post‐immunotherapy hospitalization duration.
Results: Among the 12 AE patients (median age 23.19 years; 11 with anti‐NMDA receptor, 1 with GFAP antibody), baseline treatment averaged 2.16 immunomodulatory therapies (including steroids, IVIG, and plasma exchange). The efgartigimod group demonstrated IgG reduction (average decrease 13.69±5.71 mg/ml) and more mRS score improvement from baseline (mean reduction 21.67% vs 13.33%) compared to the traditional treatment group. Additionally, the efgartigimod group experienced shorter hospital stays (20.83±12.3 days vs. 31.67±8.48 days).
Conclusion: The study is the first to suggest that the addition of efgartigimod to immunosuppression therapy in patients with autoimmune encephalitis may result in a shorter hospital stay and accelerate recovery (evidenced by lower mRS scores). Despite the small sample size, these findings warrant further investigation.
Disclosure: Nothing to disclose.
EPO‐279
Use of rituximab in primary angiitis of the central nervous system: Observational study in a tertiary center
I. Elosua‐Bayes 1; A. Vilaseca1; H. Ariño1; A. Zabalza1; M. Olivé‐Gadea2; F. Martinez‐Valle3; E. Martinez‐Saez4; J. Rio1; L. Bollo1; J. Castillo1; A. Pappolla1; A. Cobo‐Calvo1; M. Comabella1; L. Midaglia1; C. Nos1; B. Rodriguez‐Acevedo1; C. Tur1; A. Vidal‐Jordana1; G. Arrambide1; À. Rovira5; J. Sastre‐Garriga1; M. Tintoré1; X. Montalban1
1Centre d’Esclerosis Múltiple de Catalunya and Neurology Department, University Hospital Vall d’Hebron, Barcelona; 2Stroke Unit, University Hospital Vall d’Hebron, Barcelona; 3Internal Medicine Department, University Hospital Vall d’Hebron, Barcelona; 4Pathological Anatomy Department, University Hospital Vall d’Hebron, Barcelona; 5Neuroradiology Department, University Hospital Vall d’Hebron, Barcelona
Background and Aims: There is paucity of data on treatment for primary angiitis of the central nervous system (PACNS), especially regarding rituximab. We aim to characterize the cohort of patients diagnosed with PACNS in our center, evaluating radiological and clinical response, comparing rituximab to other treatments.
Methods: Observational retrospective study of patients diagnosed with PACNS (Birnbaum criteria) in a tertiary hospital. Clinical information was obtained from electronic health records. Patients were grouped according to use of rituximab at any time‐point. A favorable outcome was defined as a modified Rankin scale (mRS) score ≤2 at last follow‐up. Clinical and radiological response was defined as absence of relapse during treatment.
Results: 23 patients were included (women 65.2%). All patients received several lines of immunotherapy (21 included cyclophosphamide). Median age at onset was 38 years (IQR: 29.9–60.1), 28.0 in the group treated with rituximab (n = 9, IQR: 21.7‐36.8) and 52.8 in the non‐rituximab group (n = 14, IQR: 37.1‐65.9, p = 0.019). mRS at peak was 4 (IQR: 1‐5) in rituximab patients and 3 (IQR: 2‐4) in non‐rituximab (p = 0.369). At last follow‐up, median mRS for rituximab was 1 (IQR: 1‐4) and 2 for non‐rituximab (1‐4) (p = 0.439). Throughout the duration of treatment, rituximab patients presented a similar clinical and radiological response to the 21 patients receiving cyclophosphamide (77.7% and 45.5% vs. 71.4% and 57.1% respectively).
Conclusion: In our cohort, rituximab and cyclophosphamide presented similar rates of clinical and radiological response. Recognizing age difference between groups, this study suggests rituximab could be a non‐inferior alternative to treat PACNS, especially more severe cases.
Disclosure: Nothing to disclose.
Cognitive neurology/neuropsychology 2
EPO‐280
Spontaneous speech alterations and evolution in primary progressive aphasia variants
V. Castelnovo1; E. Canu 1; L. Lumaca1; S. Basaia1; S. Santicioli1; E. Gatti1; A. Lamanuzzi1; E. Spinelli2; G. Cecchetti3; F. Caso4; G. Magnani4; P. Caroppo5; S. Prioni5; C. Villa5; S. Cappa6; M. Filippi7; F. Agosta2
1Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 3Neurophysiology Service, Neurology Unit, and Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute Milan, Italy; 4Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; 5Fondazione IRCCS Istituto Neurologico Carlo Besta, Unit of Neurology 5 – Neuropathology, Milan, Italy; 6Department of Humanities and Life Sciences, University Institute for Advanced Studies IUSS Pavia, and Dementia Research Center, IRCCS Mondino Foundation, Pavia, Italy; 7Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: To identify: which features of speech, standard language and gray matter (GM) parameters most effectively distinguish primary progressive aphasia (PPA) variants from each other; how speech evolves over time, and the best combination of features predicting speech evolution.
Methods: 95 PPA patients underwent the “Picnic Scene” test and structural MRI. 34 patients underwent a follow‐up. Stepwise‐regression‐models were used to identify speech, standard‐language tests and GM parameters that best distinguished groups. In each PPA group, linear‐mixed‐effect models were performed for defining speech changes over time, and the prediction analysis was conducted using variables from the best stepwise‐models.
Results: The best models to differentiate PPA variants included: left temporal and frontal volumes, and syntax production features when comparing nfvPPA vs svPPA (R2 = 0.89); lexical contents, syntax complexity, left temporal and insular volumes in nfvPPA vs lvPPA (R2 = 0.81); left temporal volumes and speech production rates in svPPA vs lvPPA (R2 = 0.86). Over time, nfvPPA patients showed more phonological errors, which were predicted by syntax production features at baseline. SvPPA and lvPPA showed reduced naming and reduced number of words in sentences, respectively, which were predicted by left temporal volumes.
Conclusion: The speech, standard‐language and GM variables that we identified as the most affected at baseline and over time by each PPA variant, may be used in the clinical practice for increasing knowledge on disease progression, patients’ prognosis and for planning speech language therapy interventions. Funding. ERC (StG‐2016_714388_NeuroTRACK); Foundation Research on Alzheimer Disease. Next Generation EU/National Recovery and Resilience Plan, Investment PE8‐Project Age‐It.
Disclosure: V Castelnovo, L Lumaca, S Santicioli, E Gatti, A Lamanuzzi, E Spinelli, F Caso, G Magnani, P Caroppo, S Prioni, C Villa, SF Cappa have nothing to disclose. E Canu receives research support from Italian Ministry of Health (IHM). S Basaia receives research support from IHM. G Cecchetti received speaker honoraria from Neopharmed Gentili. M Filippi consulting or speaking activities or advisory boards for Alexion, Almirall, Biogen, Bayer, Bristol‐Myers Squibb, Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA; scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol‐Myers Squibb, Lilly, Novartis, Sanofi‐Genzyme; research support from Biogen Idec, Merck‐Serono, Novartis, Roche, IMH, Italian Ministry of University and Research, and FISM. F Agosta received speaker honoraria from Biogen Idec, Italfarmaco, Roche, Zambon and Eli Lilly, and has received research supports from IMH, Italian Ministry of University and Research, ARiSLA, ERC, EU Joint Programme – Neurodegenerative Disease Research, and Foundation Research on Alzheimer Disease.
EPO‐281
Cognitive deficits in asymptomatic carotid stenosis: A FMRI study
E. Ozdemir Oktem 1; B. Yulug1; D. Sayman1; S. Cankaya1; A. Ozsimsek1; C. Sayman1; U. Duran1; R. Karaca1; L. Hanoglu2
1Department o Neurology, Alanya Alaaddin Keykubat University, Antalya, Turkey; 2Research Institute for Health Sciences and Technologies (SABITA), Clinical Electrophysiology, Neuroimaging and Neuromodulation Laboratory, Istanbul Medipol University, Istanbul, Turkey
Background and Aims: Asymptomatic carotid stenosis may cause cognitive loss in patients. In our study, cognitive status and functional connectivity changes and cognitive functions in patients with asymptomatic carotid stenosis (CS group) were evaluated compared to healthy controls.
Methods: Thirty‐five individuals (21 male/ 14 female) were enrolled in the study. Nineteen of the participants had carotid stenosis and 16 were healthy controls. CS group and control groups’ carotid stenosis evaluations were done and confirmed by radiologists. Participants’ brain morphology alterations were evaluated with non‐contrast brain MRI, using Schelten's score. Montreal Cognitive Assessment test (MOCA) and Mini Mental State Examination (MMSE) test were used to evaluate cognitive state. Structural and resting‐state fMRI scans were conducted with specific parameters.
Results: The two groups had similar demographic characteristics in terms of age (p = 0.051), education level (p = 0.786) and gender (p = 0.557). In addition, there was no difference between the Schelten scores of the carotid stenosis group and the control group (p = 0.362). Finally, our analysis revealed that there was a significantly lower MOCA scores in carotid stenosis group compared to control group (p = 0.030). Our whole‐group partial correlation analysis showed a significant correlation between rostral prefrontal cortex prominence. Our findings showed that the CS group exhibited significantly lower MOCA scores and showed a significant correlation with salience networks compared to the control group, suggesting that carotid stenosis leads to consequential cognitive decline.
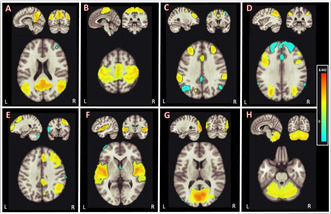
FIGURE 1 Resting‐state networks identified via independent component analysis (ICA) A) DMN, B) Sensorimotor, C) Salience, D) Dorsal attention, E) Frontal‐parietal, F) Language, G) Visual, H) Cerebellar.
Conclusion: Our study revealed that individuals with asymptomatic carotid artery stenosis had significantly worse cognitive functions which correlated with frontoparietal, and sensorimotor networks.
Disclosure: Nothing to disclose.
EPO‐282
Investigation of functional brain dynamics in Alzheimer's disease with short‐term TMS stimulation on the DLPFC and EEG
F. Aydin 1; S. Yilmaz2; H. Velioğlu3; B. Güntekin4; L. Hanoğlu5
1Istanbul Medipol University, Institute of Health Sciences, Department of Neuroscience PhD Program, Istanbul, Turkey; 2İstanbul Medipol Mega University Hospital, Department of Neurology, Istanbul, Turkey; 3Center for Psychiatric Neuroscience, Feinstein Institute for Medical Research, Manhasset, New York, USA; 4Istanbul Medipol University, School of Medicine, Department of Biophysics, Istanbul, Turkey; 5Department of Neurology, Istanbul Medipol University, Istanbul, Turkey
Background and Aims: Transcranial magnetic stimulation (TMS) and electroencephalography (EEG) are combined and used to investigate the brain network dynamics of neuropsychiatric diseases. Objectives: Our study aims to investigate the changes caused by short‐term repetitive TMS stimulation applied to the left DLPFC region in Alzheimer's Disease (AD) on the brain's resting‐state electrophysiological activity (Resting‐State EEG).
Methods: 26 early/mid‐stage AD patients, including active (n = 13) and sham (n = 13), were included in the study. 150 pulses of 20 Hz rTMS (two stimulations consisting of 75 pulses; pulse duration = 3.5 sec; time between pulses = 45 sec) were applied to the left DLPFC. Resting‐state EEG was recorded at baseline and immediately after TMS to assess the effects of TMS on the functional brain network.
Results: There was no statistically significant difference between the active and sham groups in demographic, clinical, and cognitive characteristics. In the active group, a significant increase in beta activity was observed in the occipital regions after TMS application (p < 0.05).
Conclusion: Increased beta activity may indicate the neuroplastic effects of TMS stimulation of DLPFC in AD. Monitoring the changes caused by short‐term stimulation in resting EEG may play an important role in understanding the nature of brain network dynamics resulting from TMS stimulation in AD and in planning individualized treatments in the future.
Disclosure: This study was supported by TÜBİTAK.
EPO‐283
Vocabulary knowledge as a reliable proxy of cognitive reserve in multiple sclerosis: A validation study
G. Maggi 1; M. Altieri1; M. Risi1; V. Rippa1; R. Borgo1; R. Sacco2; D. Buonanno1; A. D'Ambrosio1; A. Bisecco1; G. Santangelo3; A. Gallo1
1Department of Advanced Medical and Surgical Sciences, University of Campania “Luigi Vanvitelli”, Naples, Italy; 2Department of Neurology, Neurocenter of Southern Switzerland (NSI), Regional Hospital of Lugano, Ente Ospedaliero Cantonale, Lugano, Switzerland; 3Department of Psychology, University of Campania “Luigi Vanvitelli”, Caserta, Italy
Background and Aims: Cognitive reserve (CR) operationalization is often limited to the educational/occupational attainment, but the lifetime intellectual enrichment represents a crucial source of CR, estimated by objective measures such as Vocabulary knowledge (VOC) test [2]. Thus, this study aimed to explore the suitability of the VOC as an accurate and reliable proxy of CR by evaluating its psychometric properties and discrimination accuracy compared to other CR measures in Multiple Sclerosis (MS).
Methods: Sixty‐eight consecutive people with MS (pwMS) completed a clinical evaluation and a neuropsychological assessment including: VOC, Brief Repeatable Battery of Neuropsychological Tests, Cognitive Reserve Index questionnaire (CRIq), and questionnaires on neuropsychiatric aspects. Reliability, convergent and divergent validity, and discrimination accuracy of the VOC using educational level as reference standard were assessed. The possible effect of sociodemographic and clinical factors on the VOC and its role in predicting the global cognitive status were also explored.
Results: The VOC demonstrated good internal consistency (Cronbach's alpha = 0.894) and an adequate construct validity. It showed a level of discrimination of pwMS with high and low CR comparable to the CRIq score (Figure 1). VOC scores were independent of MS features and predicted, together with MS‐related disability, the global cognitive status.
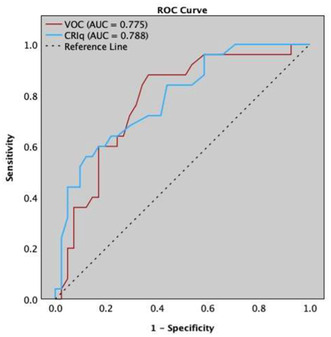
FIGURE 1 ROC of the Vocabulary Knowledge (VOC) and Cognitive Reserve Index questionnaire (CRIq) when discriminating people with Multiple Sclerosis (pwMS) with high and low cognitive reserve measured using educational level as reference standard.
Conclusion: CR should be measured by fixed objective measures independent of brain pathology and clinical features such as the VOC found to be a reliable and valid instrument for CR estimation in pwMS. Early CR estimation may help clinicians in identifying pwMS at higher risk of cognitive decline to plan a strict neuropsychological monitoring and cognitive interventions.
Disclosure: Nothing to disclose.
EPO‐284
Psychophysiological markers of creative thinking: Preliminary findings from an experimental study
J. Giannì; V. Borsa; A. Brugnera; G. Fusi; M. Crepaldi; F. Colombi; A. Compare; M. Rusconi
Department of Human and Social Sciences, University of Bergamo, Bergamo, Italy
Background and Aims: According to the Neurovisceral Integration Model, brain regions involved in self‐regulation are implicated in cardiac autonomic activity through the vagus nerve. Previous literature showed that greater parasympathetic activity at rest predicts better cognitive performances, but its association with creative thinking processes is still under‐investigated. Moreover, both cognitive control mechanisms and creative thinking appear to be modulated by specific psychological traits. Thus, the aim of this study is to explore the relationship between Heart Rate Variability (HRV) at rest, specific psychological traits, and creative thinking.
Methods: A preliminary sample of 44 participants (age: 25.24 ± 3.74; education: 16.02 ± 2.04) filled out an online survey investigating psychological dimensions; then underwent an experimental procedure that included a baseline, two creative thinking tasks (figural and verbal) and a recovery condition. An electrocardiogram (ECG) was recorded during the procedure and two HRV indices of parasympathetic activity (i.e., Mean HR and RMSSD) were computed. We performed non‐parametric correlations between HRV indices at rest, creative thinking scores and psychological traits.
Results: We found a significant, positive correlation between parasympathetic activity and a verbal creative index (i.e. flexibility) associated with executive functioning. Conversely, we found a significant negative correlation between perfectionistic traits and parasympathetic activity.
Conclusion: Results showed a relation between HRV and cognitive performance during a creative thinking task; the more executive component of verbal creative thinking was associated with vagal activity. Additionally, perfectionistic tendencies were associated with a vagal withdrawal at rest, suggesting a possible greater effort expenditure in cognitive control mechanisms in those individuals.
Disclosure: The present work has not been financed, in whole or in part, by any company with economic interests in the products, equipment or similar mentioned in it.
EPO‐285
Vertigoheel promotes rodent cognitive performance in multiple memory tests
K. Ott1; T. Heikkinen2; K. Lehtimäki2; K. Paldanius2; J. Puoliväli2; R. Pussinen2; E. Andriambeloson3; B. Huyard3; S. Wagner3; C. Schnack4; A. Wahler4; B. von Einem4; C. von Arnim5; Y. Burmeister1; K. Weyer 1; B. Seilheimer1
1Heel GmbH, Baden‐Baden, Germany; 2Charles River Discovery Services, Kuopio, Finland; 3Neurofit SAS, Illkirch, France; 4Department of Neurology, Ulm University, Ulm, Germany; 5Department of Neurology, Ulm University, Ulm, Germany and Department of Geriatrics, University Medical Center Göttingen, Göttingen, Germany
Background and Aims: Cognitive deficits associated with old age or various pathological conditions influence up to 3% of the general population. Repurposing drugs that had been safely used for other indications may be a promising approach to reverse or slow down cognitive impairment. Vertigoheel (VH‐04) is a multicomponent medication made of Ambra grisea, Anamirta cocculus L., Conium maculatum and Petroleum rectificatum that has been successfully and safely used for several decades in the treatment of vertigo. Here, we explored its potential as a cognitive enhancer.
Methods: We have examined the effects of single and repeated administrations of VH‐04 on the performance of mice and rats in several standard behavioral tests assessing different types of memory.
Results: We found that VH‐04 positively influenced visual recognition memory in the novel object recognition test and alleviated impairments in spatial working memory and olfactory memory caused by the muscarinic antagonist scopolamine in the spontaneous alternation and social transmission of food preference tests. In addition, VH‐04 improved retention of the spatial orientation memory of old rats in the Morris water maze. In contrast, VH‐04 did not significantly modify scopolamine‐induced impairments in tests of fear‐aggravated memory or rewarded alternation. Experiments in vitro showed that incubation with VH‐04 stimulated neurite growth of mouse primary hippocampal neurons and possibly reversed the decrease in synaptophysin mRNA expression in the hippocampus of aged rats, which implies that VH‐04 may preserve synaptic integrity in the aging brain.
Conclusion: Our findings allow a cautious conclusion that VH‐04 may improve cognitive performance in individuals with memory deficits.
Disclosure: This study received funding from Heel GmbH, an international pharmaceutical company that specializes in developing and manufacturing medicines made from natural ingredients. Charles River Discovery Services Finland Oy and Neurofit are contract research organizations. At the time of the study, KW, KO, YB, and BS were employed by Heel GmbH. TH, KL, KP, JP, and RP were employed by Charles River Discovery Services Finland Oy. EA, BH, and SW were employed by Neurofit. CS, AW, BE, and CA were employed by the Ulm University.
EPO‐286
Vocabulary knowledge as predictor of cognitive decline in multiple sclerosis: A long‐term follow‐up study
M. Altieri 1; G. Maggi1; M. Risi1; V. Rippa1; R. Borgo1; R. Sacco2; R. Docimo1; A. d'Ambrosio1; A. Bisecco1; G. Santangelo3; A. Gallo1
1Department of Advanced Medical and Surgical Sciences, University of Campania “Luigi Vanvitelli”, Naples, Italy; 2Department of Neurology, Neurocenter of Southern Switzerland (NSI), Regional Hospital of Lugano, Ente Ospedaliero Cantonale, Lugano, Switzerland; 3Department of Psychology, University of Campania “Luigi Vanvitelli”, Caserta, Italy
Background and Aims: Few studies longitudinally evaluated the effect of Cognitive Reserve (CR) on cognition in people with Multiple Sclerosis (pwMS) [1,2] reporting mixed results. This study assessed changes in CR ‐ evaluated with an objective measure of lifetime enrichment, the Vocabulary subtest (VOC) of WAIS ‐ and cognition after more than 6 years.
Methods: Eighty pwMS (35% males) were evaluated at baseline and after a follow‐up of 6.39 (1.84) years. A global cognition score (COG) was computed by meaning all scores of BRB‐N and Stroop test. Repeated measures and mixed‐design ANOVAs, regression and receiver operating characteristics (ROC) analyses evaluated: 1) changes in VOC over time, 2) demographic/clinical predictors of changes of VOC and COG over time, 3) accuracy of VOC compared to baseline COG in predicting cognitive decline.
Results: We found that higher VOC scores at follow‐up evaluation and this change was independent of demographic/clinical aspects. VOC was the only predictor of COG changes. pwMS with high CR reported higher COG scores at both baseline and follow‐up; moreover, COG scores improved at follow‐up only in pwMS with high CR. ROC analysis (with presence of cognitive decline as gold standard) indicated that VOC predicted future cognitive decline, better than educational level and slightly lower than baseline COG.
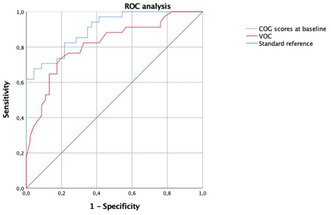
FIGURE 1 ROC analysis of Vocabulary Knowledge and overall cognition score at baseline evaluation as predictors of cognitive decline at follow up evaluation.
Conclusion: The results revealed that CR can be increased over time independently from the effect of disease, and that the measurement of CR can be useful after MS diagnosis to identify people at risk of future cognitive decline.
Disclosure: Antonio Gallo reports a relationship with Biogen, Merck Serono, Mylan, Novartis, Roche, Teva, Sanofi Genzyme that includes: consulting or advisory, speaking and lecture fees, and travel reimbursement. Alvino Bisecco reports a relationship with Biogen, Merck&Co Inc, Celgene Corp, Sanofi Genzy that includes: consulting or advisory and speaking and lecture fees. Rosaria Sacco received compensation for consulting fees and speaking activities from Biogen Idec, Merck, Novartis, Sanofi, and Roche.
EPO‐287
Advancing neurological assessment: The importance of social cognition screening
M. Eicher; R. Johannessen; A. Hansen; M. Regli; L. Ramseier; T. Hibbert; M. Ruepp; L. Imbach; H. Jokeit
Swiss Epilepsy Centre, Zurich, Switzerland
Background and Aims: Social cognition, the capacity to recognize, understand, and predict emotional and mental states in oneself and others, has gained prominence in the last decade. Acknowledging its impact, the DSM‐V includes social cognition as a core neurocognitive domain. However, there is a shortage of screening tools for assessing social cognition in neurological disorders. To bridge this gap, we created the Cognition of Social Interaction in Movies (COSIMO) screening tool – a brief, video‐based, ecologically valid, freely accessible, browser‐based test providing immediate results (https://cosimo‐project.com).
Example of a COSIMO item.
Methods: 1) To explore potential applications in neurology, we conducted a systematic second‐order literature review to identify and characterise the nature and extent of social cognitive dysfunction in different neurological conditions. 2) Preliminary data analyses examined COSIMO test scores in healthy controls (N = 900) and in neurological populations with epilepsy (N = 50) and multiple sclerosis (N = 100).
Results: Our systematic second‐order review reveals the presence of significant social cognitive deficits in several neurological disorders. Analyses of COSIMO showed satisfactory psychometric properties, with particularly high sensitivity in detecting deficits in patients with temporal lobe epilepsy (N = 25, g = 1.02, p = 0.006).
Conclusion: Neurological disorders can be associated with social cognitive dysfunction, highlighting the urgent need for concise and reliable screening tools for clinical use. COSIMO shows promising potential for the efficient identification of such deficits. We are actively collecting normative data and validating COSIMO across a range of neurological and psychiatric conditions.
Disclosure: Nothing to disclose.
EPO‐288
Longitudinal assessment of cognitive function in non‐relapsing MOG‐IgG associated disease: A case series
M. Risi 1; M. Altieri2; R. Borgo1; A. d'Ambrosio1; R. Docimo1; C. Marotta1; R. Capuano1; V. Rippa2; M. Cirillo3; G. Tedeschi1; A. Bisecco1; A. Gallo1
1Division of Neurology, Department of Advanced Medical and Surgical Sciences (DAMSS), University of Campania “Luigi Vanvitelli”, Naples, Italy; 2Department of Psychology, University of Campania “Luigi Vanvitelli”, Napoli, Italy; 3MRI Research Center SUN‐FISM, University of Campania “Luigi Vanvitelli”, Naples, Italy
Background and Aims: MOGAD is an inflammatory antibody‐mediated disease, affecting both white and grey matter of CNS. It is more frequent in children and young adults. The clinical course can be either monophasic or relapsing, often with complete recovery. To date, only few studies explored cognitive function in patients with MOGAD. Patients with relapsing MOGAD have been reported to have impaired reasoning skills and overall response time, compared to healthy controls. To assess longitudinal change in cognitive function in a cohort of six patients with non‐relapsing MOGAD.
Methods: we assessed cognitive function with the Rao's Brief Repeatable Battery and the Stroop test after ≥12 months from recovery and after 1‐year. Patients who failed ≥2 subtests (Z‐scores < ‐1.5 SD) were defined cognitively impaired (CI). Results were adjusted for age, sex, and education.
Results: as disease onset, 3 had ADEM, 1 had cortical encephalitis, and 2 had optic neuritis. Complete clinical recovery occurred for all patients. Only one received Rituximab due to severity of initial attack. Basal cognitive evaluation revealed a mild multidomain impairment only in the two pediatric‐onset patients of the cohort, without worsening over 1‐year. Annualized brain atrophy rate was normal for all patients.
Conclusion: differently from patients with relapsing MOGAD, we found no CI subjects within our cohort of non‐relapsing adult patients, while the two with pediatric‐onset showed a mild cognitive impairment. Interestingly, no patients had worsening in cognitive function and brain atrophy rate over 1‐year follow‐up. These data suggest that the relapsing course and pediatric onset could be risk factors for cognitive impairment in MOGAD.
Disclosure: The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this work.
EPO‐289
Spontaneous intracranial hypotension presenting as frontotemporal dementia: Two case reports and literature review
M. Del Chicca 1; D. Viola1; E. Bergamin1; L. Tommasini1; L. Giampietri1; E. Del Prete2; V. Nicoletti2; G. Tognoni2; R. Ceravolo1; G. Siciliano1; F. Baldacci1
1Neurology Unit, Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy; 2Neurology Unit, Department of Medical Specialties, Azienda Ospedaliero‐Universitaria Pisana, Pisa, Italy
Background and Aims: Spontaneous intracranial hypotension (SIH) can present with cognitive and behavioral changes resembling behavioral variant‐frontotemporal dementia (bvFTD). This study reports two cases of SIH manifesting with behavioral alterations and reviews the existing literature on other reported cases.
Methods: Two male patients experienced subacute orthostatic headache, behavioral changes (disinhibition, apathy) and impaired executive and attentional functions on neuropsychological tests. Brain Magnetic Resonance Imaging (MRI) revealed brain sagging and dural contrast enhancement, leading to an SIH diagnosis. Despite unsuccessful blood patching in one case, subsequent exploration identified a cerebrospinal fluid (CSF)‐venous fistula and embolization resolved SIH, improving cognition. In addition the study compares clinical and radiological features, as well as treatment options, of these cases, with existing literature to consolidate our understanding of clinical features, diagnosis and management of this condition.
Results: Radiological and clinical data, in our cases, support a diagnosis of Brain Sagging Dementia (BSD). Literature review identified well‐documented cases of BSD, highlighting its rarity and potential reversibility with identified SIH causes and proper treatment.
Conclusion: SIH presenting as bvFTD may result from frontotemporal cortex stretching and/or from venous stagnation at the confluence of the straight sinus and Galenic vein. Given its treatable nature, when symptoms typical of bvFTD coexist with brain sagging without clear cerebral atrophy on MRI, it is crucial to consider BSD. Further investigations are recommended to identify CSF hypotension causes and implement appropriate treatments. Considering the potential reversibility of BSD, such interventions frequently result in the improvement of cognitive disorders.
Disclosure: Nothing to disclose.
EPO‐290
Exploring cognitive function in subarachnoid hemorrhage patients: A mini‐mental state examination analysis
O. Cibuku 1; V. Leka1; E. Enesi2; A. Rroji2; F. Bilaj2; K. Caci2; M. Loka3; S. Nokshiqi3
1Neurologist, American Hospital Tirana, Albania; 2Neuroradiologist, American Hospital Tirana, Albania; 3Medical doctor, American Hospital Tirana, Albania
Background and Aims: This study examines the cognitive status of individuals recovering from subarachnoid hemorrhage (SAH) using the Mini‐Mental State Examination (MMSE). The findings elucidate the extent of cognitive impairment post‐SAH and highlight specific areas of vulnerability
Methods: A prospective study utilizing Mini‐Mental State Examination (MMSE) to assess cognitive function in 97 patients diagnosed with subarachnoid hemorrhage (SAH) patients from June 2022‐December 2023 in American Hospital in Tirana, Albania. Standardized MMSE protocols applied at discharge and 6 months follow up, with data analyzed for correlations with SAH severity and outcome.
Results: 97 patients diagnosed with SAH from a ruptured brain aneurism, mean age 39.27 (SD17.21), with a female predominance (60.82% female vs 39.18% male). 59 (60.82%) aneurism ACoA, 7 (7.22) aneurism MCA, 27 (27.85) aneurism ACoP, 4 (4.12%) aneurism BA. In patients admitted with Hunt‐Hess scores of 0‐2, MMSE yielded 3‐4 points higher compared to those with Hunt‐Hess scores of 3‐5.(p < 0.05). Statistical analysis revealed no significant changes in MMSE scores upon reevaluation after 6 months (p > 0.01).
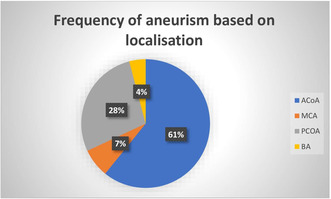
Frequency of aneurism based on localisation.
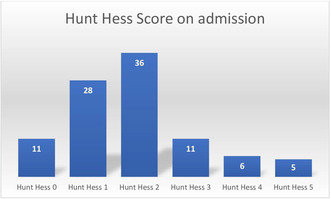
Hunt Hess score on admission.
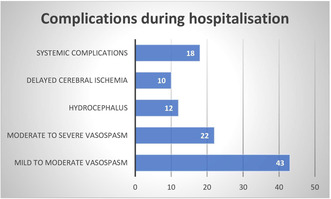
Complications during hospitalisation.
Conclusion: MMSE in SAH patients provides valuable insights into cognitive function. While initial scores may correlate with Hunt‐Hess severity, long‐term stability suggests the need for continuous monitoring and tailored interventions for optimal cognitive outcomes. Study limitations: MMSE may not fully capture subtle cognitive changes, emphasizing the importance of supplementary assessments for a comprehensive understanding of cognitive function in this population
Disclosure: Nothing to disclose.
EPO‐291
Executive functioning training to reduce cognitive intra‐individual variability in HIV adults: A case comparison study
O. Odii1; S. Brooks1; N. Wright1; A. Azuero1; P. Fazeli 1; C. Chapman Lambert1; D. James2; E. Kay1; J. Lee3; D. Vance1
1School of Nursing, University of Alabama at Birmingham; 2Edson College of Nursing and Health Innovation, Arizona State University; 3Department of Psychiatry and Behavioral Neurobiology, University of Alabama at Birmingham, Birmingham, Alabama, USA
Background and Aims: As people with HIV (PWH) age, they experience increased risk of developing cognitive impairments. To mitigate these challenges, healthcare professionals must create intervention strategies. An emerging concept in the realm of cognitive vulnerabilities is cognitive intra‐individual variability (IIV). Cognitive IIV pertains to the variations observed in cognitive performance, offering predictive insights beyond conventional mean‐based cognitive assessments. In the context of HIV, cognitive IIV has shown associations with the prediction of cognitive decline, cortical atrophy, and mortality. Based on the Executive Dysfunction Hypothesis, improvement in executive functioning could reduce cognitive IIV.
Methods: In our feasibility study, a two‐group pre/posttest randomized controlled trial involving 120 PWH, participants are randomized into either the executive functioning training group or a no‐contact control group. The training group undergoes 20 hours of computerized exercises aimed at enhancing executive function. To characterize this study, an interim case comparison was performed, focusing on the initial two participants who completed the training and two demographically matched control participants.
Results: Utilizing the Connor's Continuous Performance Test 3rd Edition, a computerized assessment of reaction time and cognitive IIV, the findings indicated significant enhancements in reaction time (i.e., Hit RT) and cognitive variability (i.e., HRT SD, Variability) within the training group when compared to the no‐contact control group.
Conclusion: While preliminary, these initial promising findings imply that delving deeper into cognitive IIV could offer insights into enhancing cognition in aging PWH. This provides a new avenue for cognitive interventions, specifically targeting the reduction of cognitive IIV.
Disclosure: Nothing to disclose.
EPO‐292
Accelerated TMS for Alzheimer's disease; bilateral DLPFC stimulation twice daily for 5 days: Randomized controlled trial
S. Yilmaz 1; F. Aydin2; C. Parlatan2; E. Uluçam3; U. Benli3; H. Velioğlu4; L. Hanoğlu5
1Department of Neurology, İstanbul Medipol Mega University Hospital, Istanbul, Turkey; 2Department of Neuroscience PhD Program, Institute of Health Sciences, Istanbul Medipol University, Istanbul, Turkey; 3School of Medicine, Istanbul Medipol University, Istanbul, Turkey; 4Center for Psychiatric Neuroscience, Feinstein Institute for Medical Research, Manhasset, New York, USA; 5Department of Neurology, Istanbul Medipol University, Istanbul, Turkey
Background and Aims: Different protocols have been developed to affect mood, anxiety, cognition, memory, executive functions, and behavioral and motor symptoms in Alzheimer's patients. Our aim with this study is to investigate the changes of short‐term intensified rTMS on cognitive, behavioral and daily living activities in AD patients.
Methods: 31 early and mid‐term AHD were included in the rTMS Group (n = 19) and the control group (n = 12). Before and after rTMS; Mini Mental State Test and Alzheimer's Disease Assessment Scale, Geriatric Depression Scale, Activities of Daily Living Scale and neuropsychometric inventory were used. In the rTMS group, 20 Hz rTMS was applied to bilateral DLPFC.
Results: The average age of the rTMS group is 72.36 ± 3.81; the control group is 68.50 ± 7.72. The average education year of the rTMS group is 8.36 ± 5.15. The average education year of the control group is 10.25 ± 4.88. Intra‐group and intergroup analyzes of rTMS and control groups are shown in Tables 1&2 and 2 and Table 3.
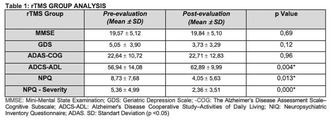
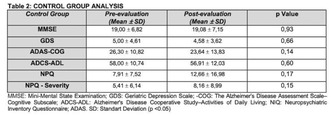
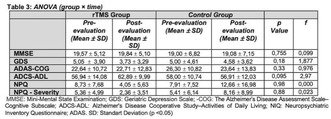
Conclusion: After the rTMS, there were positive changes in the behavioral and daily living activities of individuals with AD. The main goal is to slow or stop the progression of the disease as a result of TMS stimulation. Although magnetic stimulation does not compensate for the loss of cell number resulting from atrophy, it is thought that TMS increases the synaptic connectivity between neurons and thus plays a role in slowing down the progression.
Disclosure: This study was supported by TÜBİTAK.
EPO‐293
Late‐onset vs adult‐onset multiple sclerosis: Comparison of clinical and cognitive features and sex‐related differences
N. Tedone1; P. Preziosa2; D. Mistri1; M. Azzimonti2; M. Filippi3; M. Rocca 2
1Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 3Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: The proportion of patients with multiple sclerosis (MS) experiencing disease onset after 45 years (late‐onset [LO] MS) is increasing. Although previous studies suggested different clinical features between LOMS and adult‐onset (AO) MS patients, a comprehensive evaluation including cognitive profiles and sex influence has not been investigated yet. This study compares clinical and cognitive characteristics between LOMS and AOMS patients and explores sex‐related differences.
Methods: Sixty‐one LOMS patients (females = 31) and 122 sex‐matched AOMS patients (females = 62) underwent neurological and neuropsychological assessments. Differences in clinical (onset type, disability status, 9‐hole Peg Test, Timed 25‐Foot Walk [T25FWT]) and neuropsychological features (performance and frequency of impairment of global cognitive function and specific domains, presence and severity of fatigue and depression) were evaluated, also considering sex differences.
Results: Compared to AOMS, LOMS patients exhibited higher motor onset prevalence, worse T25FWT and visual memory performance (p ≤ 0.036). LOMS males had more frequent motor onset, worse T25FWT, higher prevalence of depression and cognitive impairment compared to AOMS males (p ≤ 0.030). LOMS females performed worse in visual memory (p ≤ 0.006) and had lower fatigue compared to AOMS females (p ≤ 0.005). Compared to AOMS females, males showed worse performance in global cognitive function, attention, and verbal memory with higher prevalence of impairment in the latter (p ≤ 0.011). Compared to LOMS females, males showed higher prevalence of depression and impairment in attention (p ≤ 0.035).
Conclusion: LOMS patients exhibited worse clinical and cognitive features compared to AOMS patients, regardless from sex. Male patients showed more severe clinical and cognitive impairment in both AOMS and LOMS.
Disclosure: N Tedone, D Mistri, M Azzimonti have nothing to disclose. P. Preziosa received speaker honoraria from Roche, Biogen, Novartis, Merck, Bristol Myers Squibb, Genzyme, Horizon and Sanofi. He has received research support from Italian Ministry of Health and Fondazione Italiana Sclerosi Multipla (FISM). M. Filippi received compensation for consulting or speaking activities services from Alexion, Almirall, Biogen, Bayer, Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA; participation in Advisory Boards for Alexion, Biogen, Bristol‐Myers Squibb, Merck, Novartis, Roche, Sanofi, Sanofi‐Aventis, Sanofi‐Genzyme, Takeda; scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol‐Myers Squibb, Lilly, Novartis, Sanofi‐Genzyme; he receives research support from Biogen Idec, Merck‐Serono, Novartis, Roche, Italian Ministry of Health, Italian Ministry of University and Research, and FISM. MA Rocca received consulting fees from Biogen, Bristol Myers Squibb, Eli Lilly, Janssen, Roche; speaker honoraria from AstraZaneca, Biogen, Bristol Myers Squibb, Bromatech, Celgene, Genzyme, Horizon Therapeutics Italy, Merck Serono SpA, Novartis, Roche, Sanofi and Teva; research support from MS Society of Canada, Italian Ministry of Health, Italian Ministry of University and Research, and FISM.
EPO‐294
The development of a multimodal AI‐assisted Thai mini‐mental state examination (MMSE‐T) framework for Thai population
C. Sirilertmekasakul1; W. Rattanawong 1; A. Gongvatana1; T. Tongloy2; A. Srikiatkhachorn1
1Faculty of Medicine, King Mongkut's Institute of Technology Ladkrabang, Bangkok, Thailand; 2College of Advanced Manufacturing Innovation, King Mongkut's Institute of Technology Ladkrabang, Bangkok, Thailand
Background and aims: With approximately 50 million people affected globally, dementia prevalence is expected to triple by 2050. Early detection, traditionally reliant on manual, paper‐based cognitive screening, is shifting towards digitized, artificial intelligence (AI)‐assisted methods. This study aims to develop a multimodal AI‐assisted neurocognitive assessment framework, using the MMSE‐T 2002 as a model, and compare its effectiveness with the traditional version.
Methods: MMSE‐T was completed by 233 individuals who visited the medical center of King Mongkut Institute of Technology, Ladkrabang (KMITL). Data were captured via videos and images. AI models for 11 MMSE‐T test batteries were developed using 150 dataset. Speech‐based and handwritten answers were converted to digital text using Microsoft Azure's speech‐to‐text (STT) and Google Cloud AI's optical character recognition (OCR), respectively, and scored by the ChatGPT. The deep learning (DL) algorithms‐based object detection were trained to detect drawing and action‐based answers. The primary outcome of the correlation between the scoring of MMSE‐T by traditional paper‐based and digital AI‐assisted versions was analyzed using the intraclass correlation coefficient (ICC).
Results: Of 83 records analyzed, a high correlation between traditional and digital AI‐assisted versions was observed (r = 0.85; p < 0.001). Among 11 test batteries, the eye‐action test battery has the highest correlation of r = 1 (p < 0.001). The AI‐assisted version demonstrated sensitivity, specificity, positive (PPV) and negative predictive values (NPV) of 68.7%, 89.6%, 61.1%, and 92.3%, respectively, compared to human grading.
Conclusion: The study indicates a high correlation between traditional paper‐based and digital AI‐assisted MMSE‐T, suggesting the effectiveness of AI integration in cognitive screening for dementia.
Disclosure: Nothing to disclose.
Neurogenetics 2
EPO‐295
REKLAIM, a novel Phase Ib clinical trial of intravenous FBX‐101 (AAVrh10.GALC) after UCBT for infantile Krabbe disease
M. Escolar 1; M. Poe1; J. Ruiz1; M. Vander Lugt2; R. Wang3; P. Sabolcs4
1FORGE BIOLOGICS, Grove City, OH, USA; 2University of Michigan Medical Center, Ann Arbor, MI, USA; 3Children's Hospital of Orange County, Orange County, CA, USA; 4Paul Szabolcs, University of Pittsburgh, Pittsburgh, PA, USA
Background and Aims: REKLAIM is a novel intravenous AAVrh10.GALC gene therapy administered after umbilical cord blood transplantation (UCBT) for Krabbe disease. We report on the first 5 subjects treated. Infantile Krabbe is a neurodegenerative disorder due to galactocerebrosidase (GALC) deficiency that results in psychosine toxicity to myelinating cells and death by 2 years. UCBT in pre‐symptomatic neonates halts brain disease, but motor function declines due to progressive peripheral neuropathy. We hypothesized that FBX‐101 administered during myeloablation for UCBT will override the antibody response to the vector's capsid and transgene and increase GALC.
Methods: REKLAIM is a Phase 1b dose‐escalating intravenous gene therapy of FBX‐101 given >21 days after UCBT during myeloablation or immune suppression approved by an independent committee. It includes a protocol using Rituximab, Serolimus and Prednisolone adjusted to subject needs.
Results: Five subjects with IKD treated with FBX‐101 low dose (1.6 x1013 gc/kg). FBX‐101 was well tolerated, with no treatment‐related serious adverse events or development of antibodies to the transgene after follow up of 4 to 24 months. In the 2 subjects treated during myeloablation, there were no AAV antibodies, plasma and CSF GALC significantly increased, psychosine dropped below detection and subjects achieved normal gross motor skills. The three subjects treated during immune suppression developed total antibodies to AAV with no humoral or cellular toxicity and improved gross motor skills.
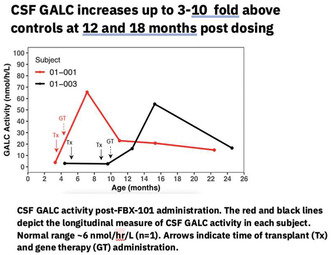
CSF GALC
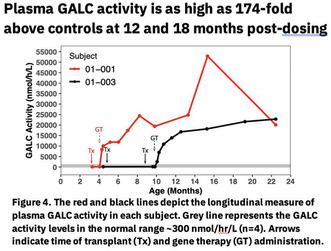
Plasma GALC activity
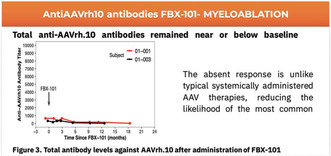
Anti AAVrh antibodies
Conclusion: FBX‐101 leverages the myeloablation and immune suppression after UCBT, resulting in efficient AAV transduction and increased GALC enzyme supporting brain myelination and gross motor development
Disclosure: M. Escolar is an inventor on the patent application describing FBX‐101 (WO2018/136710), licensed by Forge Biologics from the University of Pittsburgh. Dr. Escolar receives salary from Forge Biologics. Adjunct Professor of Pediatrics, University of Pittsburgh.
EPO‐296
Case report: DYNC1H1 mutation as a rare mimic of spinal muscular atrophy (SMA) type 3
M. Baldauf; A. Felbecker; T. Hundsberger
Department of Neurology, Cantonal Hospital, St. Gallen, Switzerland
Background and Aims: Our patient developed weakness of the legs at the age of 6y, being slowly progressive over decades. Since childhood, he was diagnosed of suffering from spinal muscular atrophy (SMA) type 3 (never genetically confirmed). At the age of 48y, he was admitted to us. He reported, that his mother, sister and niece have similar symptoms (onset ~5‐7 years).
Methods: Neurological examination, ENMG, genetics
Results: Clinically he presented with proximally pronounced pareses of both legs with areflexia. Interestingly, atrophy was distally pronounced. There were no sensory or cognitive deficits. Nerve conduction studies were normal, but EMG detected severe chronic denervation with partial reinnervation. Genetically, there was no deletion of the SMN1 gene. Finally, we found a heterozygous mutation in the DYNC1H1 gene, classified as probably pathogenic (ACMG guidelines). It's a c.1793G>T missense mutation leading to an amino acid exchange p.(Arg598Leu). The same mutation was also found in his niece. This mutation was described first in 2015 (Scoto et al.), who found it in 4 patients (2 families) with symptom onset at birth or in childhood. Since then, there are no further reports about that mutation in the literature, to our knowledge.
Conclusion: The clinical picture of SMA3 is similar to that of DYNC1H1 mutation associated lower extremity predominant SMA. The autosomal‐dominant inheritance (versus autosomal‐recessive in SMA3) is an important clinical hint. Describing the clinical follow up of patients with such rare mutations is essential, to gather information about their prognosis, avoid false diagnosis/treatment and to collect patients for future therapeutic studies.
Disclosure: Nothing to disclose.
EPO‐297
Frequency of LRRK2 p.L1795F variant in Parkinson's disease patients from Central Europe within the CEGEMOD consortium
M. Ostrozovicova 1; G. Tamas2; K. Soos2; P. Dusek3; M. Grofik4; V. Han5; P. Holly3; R. Jech3; P. Klivenyi6; N. Kovacs7; K. Kulcsarova5; E. Kurca4; A. Lackova5; J. Necpal8; D. Pinter7; E. Ruzicka3; T. Serranova3; K. Smilowska9; I. Straka10; T. Svorenova5; P. Valkovic11; K. Zarubova12; H. Houlden13; M. Rizig13; M. Skorvanek5
1Department of Neurology, P.J. Safarik University and University Hospital of L. Pasteur, Kosice, Slovak Republic; Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, UK; 2Department of Neurology, Semmelweis University, Budapest, Hungary; 3Department of Neurology and Centre of Clinical Neuroscience, First Faculty of Medicine, Charles University and General University Hospital in Prague, Prague, Czechia; 4Department of Neurology, Jessenius Medical Faculty, Comenius University and University Hospital Martin, Martin, Slovak Republic; 5Department of Neurology, P.J. Safarik University and University Hospital of L. Pasteur, Kosice, Slovak Republic; 6Department of Neurology, University of Szeged, Szeged, Hungary; 7University of Pecs, Medical School, Department of Neurology and HUN‐REN–PTE Clinical Neuroscience MR Research Group; 8Department of Neurology, Zvolen Hospital, Zvolen, Slovak Republic; 9Department of Neurology Silesian Centre of Neurology, Katowice, Poland; 10Second Department of Neurology, Comenius University in Bratislava Faculty of Medicine, University Hospital Bratislava, Bratislava, Slovak Republic; 11Second Department of Neurology, Comenius University in Bratislava Faculty of Medicine, University Hospital Bratislava; Institute of Normal and Pathological Physiology, Centre of Experimental Medicine, Slovak Academy of Science, Bratislava, Slovak Republic; 12Department of Neurology, Second Faculty of Medicine, Charles University and Motol University Hospital, Prague, Prague, Czechia; 13Department of Neuromuscular Diseases, UCL Queen Square Institute of Neurology, London, UK
Background and Aims: Pathogenic variants in LRRK2 are one of the most common high‐risk genetic factors for Parkinson's disease (PD). Recently, the lesser‐known LRRK2 p.L1795F variant was proposed as a strong genetic risk factor for PD [1], with a functional effect via stimulating the LRRK2 kinase activity [2]. However, further families are currently lacking in the literature.
Methods: A multicentre early‐onset and familial PD cohort from 9 movement disorder centres across Central Europe within the CEGEMOD consortium [3] was screened for rare LRRK2 variants using whole exome sequencing data (n = 219).
Results: We identified 3 PD cases with heterozygous LRRK2 p.L1795F variant and 1 PD case was additionally identified through standard genetic testing. All 4 patients were from a region close to Slovak‐Hungarian borders. The age of onset was 25, 45, 55 and 69 respectively and 3 cases had positive family history with several family members affected. All 4 cases were characterized by early onset of severe motor fluctuations, with 2 of them receiving LCIG therapy and 2 implanted with STN DBS; 3/4 of these cases showed unsatisfactory effect on motor fluctuations.
Conclusion: Our data suggest that the p.L1795F may represent the most common currently known pathogenic LRRK2 variant in Central Europe (AF = 0.0091) compared to more studied p.G2019S (AF = 0.00164), which is lower than in North‐West Europe as reported previously [4]. Together with the ongoing clinical trials for LRRK2 inhibitors, this finding emphasizes the urgent need for more ethnic diversity in PD genetic research.
Disclosure: This study was funded by the Slovak Grant and Development Agency under contracts APVV‐22‐0279 and by the Slovak Scientific Grant Agency under contract VEGA 1/0712/22.
EPO‐298
First description of c.3478 A>G DYNC1H1, a potentially pathogenic variant in a SMALED sibship
M. Boix Codony 1; Y. Lin Miao2; A. Massot‐Tarrus2; C. Lombardia Gonzalez3; L. Ejarque Vila3; J. Roige Buixade3
1Department of Neurology, Hospital Universitari Sagrat Cor, Barcelona, Spain; 2Department of Neurology, Hospital Universitari Mutua de Terrassa; 3Department of Genetics, CATLAB clinical Laboratories, Terrassa, Spain
Background and Aims: Pathogenic variants of the DYNC1H1 gene were first identified in 2012 as the cause of a group of autosomal dominant spinal atrophy affecting the lower limbs (SMALED). We describe a previously unreported variant of unknown significance (VUS) with features to suggest a pathogenic loss of function.
Methods: 3 members of the same sibship were assessed in our centre: a female (p1) with a prior diagnosis of SMA type 4 displaying a full SMALED phenotype, another female (p2) with a milder SMALED phenotype and no previous diagnosis and a male (p3) with CNS features of DYNC1H1 dysfunction since childhood (Intellectual disability, seizures, behavioural disturbance). EMG showed features of dHMN in p1 and p2 while MRI of the lower limbs demonstrated a pattern of muscular atrophy typical for SMALED. Brain MRI for p3 showed focal cortical thickening on the left precentral gyrus; however, those were not diagnostic for a neuronal migration disorder.
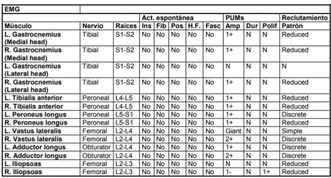
EMG findings for p1, demonstrating chronic longstanding denervation. NCS and H reflex were normal.
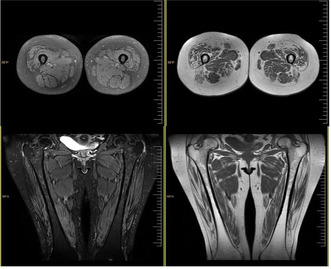
Thigh MRI images from p2: widespread asymmetrical atrophy and fatty infiltration, sparing the Gracilis and Semitendinosus muscles.

Proband p1 has prominent Genu valgo and pes planovalgus, with significant calf atrophy.
Results: Genetic testing identified a c.3478 A>G DYNC1H1 VUS in all probands, a single nucleotide polymorphism (SNP) leading to a Thr1163Ala substitution, not currently present in any of the available databases. Protein function modelling using the PolyPhen‐2 tool predicted a potentially damaging effect with high confidence.
Conclusion: Although the lack of an animal model and limited in‐silico modelling does not allow to establish definite pathogenicity according to current ACGM/ACGS scoring, the familiar aggregation, clinical presentation and paraclinical findings would endorse its inclusion on databases at least as a high risk VUS.
Disclosure: Dr Boix Codony has received honoraria (<500€) for contributing to the MAVEN‐4 study (MS700568_073), promoted by Merck Serono. The other Authors declare no relevant disclosures.
EPO‐299
Autosomal dominant optic neuropathy without polyneuropathy due to novel c.1988G>A MFN2 mutation
O. Marsico 1; V. Cianci2; A. Pascarella1; S. Gasparini1; A. Mammì1; V. Bova1; M. Pasquale1; R. Caridi1; C. Paleologa2; G. Tripodi2; D. Abelardo1; B. Falcomatà3; E. Ferlazzo1; U. Aguglia1
1Department of Medical and Surgical Sciences, Magna Græcia University, Catanzaro, Italy; 2Regional Epilepsy Centre, Great Metropolitan Hospital, Reggio Calabria, Italy; 3Department of Ophthalmology, Great Metropolitan Hospital, Reggio Calabria, Italy
Background and Aims: The mitofusin‐2 (MFN2) gene (1p36.22) encodes GTPase proteins involved in the fusion of mitochondrial membranes. Numerous MFN‐2 mutations have been associated with the axonal form of Charcot–Marie‐Tooth (CMT) disease type 2A and hereditary optic atrophies [1, 2]. Here we describe a Southern Italian family with a novel missense c.1988G>A MFN2 variant presenting with painless progressive visual impairment without peripheral motor or sensitive manifestations.
Methods: Twenty‐three subjects across three generations underwent serum DNA analysis screening tests with next‐generation sequencing (NGS). All MFN2‐mutated carriers performed an ophthalmological evaluation with optical coherence tomography (OCT), instrumental evaluation with visual evoked potentials (VEP) and electroneurography (ENG).
Results: Serum DNA analysis revealed the MFN2 c.1988G>A variant in 8 out of 23 (5F, median age: 41.5 years, IQR: 20.5‐65) patients (see pedigree chart, figure 1). In silico analysis by PolyPhen‐2, Mutation Taster and Align‐GVGD predicted this variant as pathogenic. Neurological evaluation revealed decreased visual acuity in 5 subjects (2M, 3F mean age: 49 ± 24.1 years), while no abnormalities resulted in three asymptomatic younger carriers (2M, 1F mean age 32 ± 15.1 years). VEP was bilaterally delayed in all five symptomatic patients. One also showed a bilaterally reduced radial nerve fibre layer thickness on OCT. Motor and sensory nerve conductions on ENG were normal in all mutated subjects.

Pedigree of family with MFN‐2 c.1988G>A variant, demonstrating an autosomal dominant inheritance.
Conclusion: Our study illustrated a distinctive clinical presentation marked by adult‐onset isolated optic neuropathy without peripheral neuropathy, associated with a newly identified c.1988G>A MFN‐2 variant exhibiting autosomal dominant inheritance.
Disclosure: Nothing to disclose.
EPO‐300
Clustering analysis of a cohort of primary mitochondrial diseases patients: Novel associations from the GENOMIT registry
P. Lopriore 1; S. Mazzucato2; G. Cecchi1; C. Lamperti3; V. Carelli4; C. La Morgia4; M. Valentino4; S. Micera2; S. Moccia2; M. Mancuso1; A. Bandini2
1Neurological Institute, Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy; 2The BioRobotics Institute and the Department of Excellence in Robotics and Artificial Intelligence, Scuola Superiore Sant'Anna, Pontedera (Pisa), Italy; 3Unit of Medical Genetics and Neurogenetics, Fondazione IRCCS (Istituto di Ricovero e Cura a Carattere Scientifico) Istituto Neurologico Carlo Besta, Milan, Italy; 4Department of Biomedical and Neuromotor Sciences, University of Bologna and IRCCS Istituto delle Scienze Neurologiche di Bologna, Bologna, Italy
Background and Aims: Primary mitochondrial diseases (PMDs), characterized by a complex genotype‐phenotype interplay, demand innovative approaches for comprehension. This study leverages artificial intelligence (AI), specifically clustering techniques, on a polycentric dataset to reveal genotype‐phenotype subgroupings, offering valuable insights to enhance clinical decision‐making in the intricate landscape of PMDs.
Methods: The dataset includes 770 PMD patients (female: 54%; age of onset: ≤16 yo 21%, >16yo 79%) from 3 Italian centres, extracted from the GENOMIT international clinical registry (https://genomit.eu/). Pre‐processing reduced variables to 71 from 802 using clinical knowledge's discriminative capabilities. Principal Component Analysis (PCA) further condensed them to 44 components. Subsequently, K‐means clustering was performed, determining optimal clusters via silhouette score, which ensured homogeneity within clusters while maximizing inter‐cluster separation.
Results: The optimal cluster count was three. Distinctive genotype patterns include a prevalence of nuclear DNA (44.4%) and mitochondrial DNA single large‐scale deletions (24.1%) in cluster 3, which showed the youngest age of onset (53.4% <16 yo), and SURF1 gene mutations prevalence. Regarding phenotypes, apparently similar clinical diagnosis distribution was found, with multisystem involvement more prevalent in cluster 1 and 3 and more diverse systems involved in cluster 2.
Conclusion: This study used clustering analysis for exploring genotype and phenotype distributions in PMDs. Employing unsupervised clustering on a comprehensive dataset identified distinct PMDs patient subgroups but still heterogenous distribution which needs further interpretation. These preliminary findings hold promise for personalized medicine, marking a significant step in unravelling the complexities of these rare diseases through innovative AI‐driven approaches.
Disclosure: The authors have no conflicts of interest to declare.
EPO‐301
Ataxia‐neuropathy due to a novel mtDNA mutation affecting processing of MT‐ATP6 and MT‐CO3, subunits of complex 4 and 5
J. Schaefer; A. Saak; S. Jackson
Department of Neurology, Uniklinikum C.G.Carus, Dresden, Germany
Background and Aims: The ataxia‐neuropathy spectrum covers a large variety of diseases and also includes hereditary mitochondrial disorders. In mitochondrial disease, the ataxia typically occurs in combination with other central nervous system features, including epilepsy and cognitive decline, or optic atrophy. The nuclear‐encoded mutations in mitochondrial polymerase‐gamma (POLG) have been recognized as the commonest cause of mitochondrial disease leading to ataxia‐neuropathy, but a considerable proportion of patients harbor mtDNA mutations.
Methods: A 41‐year old patient developed progressive gait ataxia, sensory neuropathy, bilateral deafness and mild visual impairment. There was a strong family history of an ataxia‐neuropathy‐deafness syndrome in 1st degree relatives. After exclusion of POLG‐mutations, workup of the clinical presentation and sequencing of the entire mitochondrial DNA were performed in the patient and her affected relatives.
Results: The patient, her mother and all affected sibs were found to carry a novel, homoplasmic mutation in MT‐ATP6 (m.9198delC). One sib also fulfilled the Barkhof MRI‐criteria for Multiple Sclerosis.
Conclusion: We identified a family with a late‐onset ataxia‐neuropathy‐deafness syndrome caused by a unique mtDNA mutation. The mutation leads to the loss of the Stop Codon in MT‐ATP6, and thus can also affect the processing of the polycistronic mRNA transcript, consisting of the MT‐ATP6 and the MT‐CO3 mRNAs. This scenario is expected to reduce the synthesis of both MT‐ATP6 and MT‐CO3, a subunit of mitochondrial complex 4.
Disclosure: Nothing to disclose.
EPO‐302
Novel homozygous KCNJ10 mutation in sisters with clinical picture of complex hereditary spastic paraparesis
J. Paulasová Schwabová Jaroslava 1; J. Paulasová Schwabová2; A. Uhrová Mészárosová3; M. Kuzmiak1; L. Novotná2; D. Šafka Brožková3; M. Vyhnálek1
1Department of Neurology, Center of Hereditary Ataxias, Second Faculty of Medicine and Motol University Hospital, Charles University, Prague, Czechia; 2Department of Pediatric Neurology, Center of Hereditary Ataxias, Charles University, Second Faculty of Medicine and Motol University Hospital, Prague, Czechia; 3Neurogenetic Laboratory, Department of Pediatric Neurology, Second Faculty of Medicine and Motol University Hospital, Charles University, Prague, Czechia
Background and Aims: Mutations in KCNJ10 gene encoding the inwardly rectifying potassium channel Kir4.1 cause a complex syndrome characterized by seizures, sensorineural deafness, ataxia, intellectual disability, and electrolyte imbalance known as SeSAME/EAST syndrome. One patient with non‐syndromic early‐onset cerebellar ataxia was described. Until now, hereditary spastic paraparesis has not been considered as part of the clinical spectrum of this channelopathy.
Methods: Genetic and clinical investigations were performed in two sisters (S1 and S2) with early‐onset progressive spastic paraparesis (combined with focal dystonia in S2) and their asymptomatic father, referred to the Center of Hereditary Ataxia, Motol University Hospital. Clinical data, medical history, neurological examination, laboratory tests, MRI of the brain, and results of other electrophysiological methods and clinical examinations, were collected.
Results: Targeted next‐generation sequencing identified previously described homozygous c. 179T>C, p.(Ile60Thr) variant in the KCNJ10 gene (NM_002241.5) in both sisters (S1,S2), with the same heterozygous mutation in the father. In both patients, the clinical picture was dominated by spastic paraparesis, ataxia and suspected cognitive deficit. Sister S1 suffered from the epilepsy from the age of 6 months with gait disturbances appearing in the first decade. Sister S2 observed first difficulties with running at the age of 11. Audiometry and neuropsychological examination confirmed perceptual hearing loss and cognitive deficit in both siblings. Electrolyte imbalance/tubulopathy was absent.
Conclusion: Our findings broaden the clinical and mutational spectrum of KCNJ10‐related disorders and suggest that screening for this gene should be performed in patients suspected of having complex hereditary spastic paraparesis.
Disclosure: No disclosure.
EPO‐303
Spatial perspective taking is impaired in spinocerebellar ataxias
S. Karamazovova 1; M. Laczo2; J. Laczo2; J. Paulasova‐Schwabova1; L. Stovickova1; M. Kuzmiak1; M. Vyhnalek1
1Department of Neurology, Second Faculty of Medicine, Centre of Hereditary Ataxias, Charles University and Motol University Hospital, Prague, Czechia; 2Department of Neurology, Second Faculty of Medicine, Memory Clinic, Charles University and Motol University Hospital, Prague, Czechia
Background and Aims: Perspective taking, the ability to imagine the environment from a different viewpoint, is an essential component of spatial navigation. Animal and functional neuroimaging studies have shown that the cerebellum is important for spatial navigation, but studies in patients with cerebellar disorders, including those with hereditary ataxias, are lacking. The current study aimed to investigate perspective taking in patients with spinocerebellar ataxias (SCA) and Friedreich's ataxia (FRDA).
Methods: We recruited 23 SCA patients 19 FRDA patients from the Centre of Hereditary Ataxias, and 34 age‐matched healthy controls (HC). All participants underwent the Perspective Taking/Spatial Orientation Test (PTSOT), an established paper‐and‐pencil test of perspective taking. Participants were asked to imagine standing at one object and facing another. Their task was to indicate the direction to a third object in a circular diagram.
Results: The SCA group performed significantly worse than the HC group. Specifically, the mean angular error was 63.02° compared to 26.01° (p < 0.001), and the mean percentage of responses lying in the correct quadrant of the circular diagram was 46.1% compared to 82.8% (p < 0.001), respectively. The FRDA group did not differ significantly from the HC group.
Conclusion: Perspective taking is impaired in SCA but not in FRDA patients. This may be due to more pronounced cerebellar grey matter atrophy in patients with SCA. More research is needed on spatial navigation in patients with cerebellar diseases, as navigation impairment may have a negative impact on patients' mobility and independence.
Disclosure: Supported by Charles University Grant Agency (GAUK) projects No. 224522, 309121, and 226423, and project National Institute for Neurological Research (Programme EXCELES, ID Project No. LX22NPO5107). The authors are members of the European Reference Network for Rare Neurological Diseases (ERN‐RND).
EPO‐304
The role of serotonergic gene polymorphisms in functional motor disorder: A case‐control association study
T. Serranová 1; D. Záhoráková2; L. Nováková1; O. Fiala3; Z. Forejtova1; M. Slovák1; E. Růžička1; D. Kemlink1
1Department of Neurology and Center of Clinical Neuroscience Charles University, 1st Faculty of Medicine and General University Hospital in Prague, Czechia; 2Department of Pediatrics and Inherited Metabolic Disorders, Charles University, 1st Faculty of Medicine, Czechia; 3Institut Neuropsychiatrické péče, Praha, Czechia
Background and Aims: Understanding the genetic factors contributing to functional motor disorders (FMD) remains limited. A previous study in a small FMD group (n = 69) found a link between the T allele variant of the tryptophan hydroxylase 2 gene (TPH2) polymorphism c.‐703G>T and an earlier onset of FMD symptoms.1 In our case‐control study, we aimed to investigate the association between single‐nucleotide polymorphisms (SNPs) within the TPH2 and 5‐hydroxytryptamine receptor 2A (HTR2A) genes, both involved in serotonin regulation, and FMD, as well as their impact on the age of symptom onset.
Methods: We genotyped 357 FMD patients and 243 healthy controls for 5 SNPs including rs4570625, rs10784941 for TPH2 gene, and rs6311, rs6313, rs6314 for HTRA2 gene using TaqMan Assays. We performed standard association tests, including allelic, genotypic, dominant, and recessive models, as well as the Cochran–Armitage test for trend using the PLINK statistical package v1.9.2 Linear regression and quantitative association tests assessed the influence of selected SNPs on the age of FMD onset.
Results: We found significant associations between rs4570625 (recessive model, p = 0.007; nominal) and rs6311 (dominant model, p = 0.0030; nominal) SNPs with FMD. There was no observed link between these genetic variants and an earlier onset of FMD.
Conclusion: These preliminary findings suggest possible involvement of the serotonergic pathway in FMD, but its link to earlier symptom onset was not confirmed. Results emphasize the need for further research in a broader cohort, considering potential confounding factors such as psychiatric comorbidities.
Disclosure: Supported by NU20‐04‐00332, NW24‐04‐00456 and Cooperation by Charles University.
EPO‐305
The first clinical and genetic characterization of patients with cerebrotendinous xanthomatosis in Hungary
N. Varga 1; P. Balicza1; D. Zadori2; I. Kapas3; A. Salamon2; Z. Grosz1; L. Szpisjak2; M. Harangi4; Z. Arányi5; P. Klivényi2; M. Molnár1
1Institute of Genomic Medicine and Rare Disorders, Semmelweis University; 2Department of Neurology, University of Szeged; 3Departmen of Neurology and Stroke, St. Janos Hospital; 4Division of Metabolic Diseases, Department of Internal Medicine, Faculty of Medicine, University of Debrecen; 5Department of Neurology, Semmelweis University
Background and Aims: Cerebrotendinous xanthomatosis (CTX) is a rare lipid storage disorder caused by mutations in CYP27A1 gene which leads to reduced production of chenodeoxycholic acid (CDCA) and excess of cholestanol, causing a wide spectrum of neurological and non‐neurological symptoms.
Methods: We aimed to characterize the patients diagnosed with CTX in Hungary and follow the efficacy of the treatment with CDCA.
Results: We present 9 patients from 6 families (two females and seven males (mean age = 44.7±8, range = 29‐52). Mean age at onset was 24.7±12 years. In 3‐3 cases the c.1184+1G>A. and c.819delT rare variants of the CYP27A1 caused the disease. The most common clinical manifestations were cerebellar ataxia, polyneuropathy, cognitive impairment and juvenile cataract. Xanthomas were present only in 22.2%. Of the cases, diverse non‐neurological findings (diarrhea, severe atherosclerosis) were observed in five patients. Brain MRI detected T2, FLAIR hyperintensity in the dentate nuclei in all patients. ENG and nerve ultrasound revealed neuropathy in all cases, and suspected intraneural cholesterol accumulation in two. Elevated cholesterol and oxysterols were detected in all cases, but the levels didn’t correlate with the severity of the disorder. Six patients are on CDCA supplementation for an average of 38±25 months which resulted in the normalization of the cholesterol level and the stagnation of the ataxia score and polyneuropathy.
Conclusion: CDCA supplementation may reverse the pathophysiological process in patients with CTX, especially if treatment is initiated early in the disease process. Therefore, early diagnosis and treatment are crucial in preventing clinical deterioration.
Disclosure: Nothing to disclose.
EPO‐306
Abstract withdrawn
EPO‐307
SCA27B – New ataxia with late onset and response to 4‐aminopyridine – First 14 cases diagnosed in the Czechia
M. Vyhnalek 1; J. Paulasova‐Schwabova1; M. Kuzmiak1; Z. Blichova1; E. Vyhnalkova2; S. Karamazovova1; J. Jerabek1; L. Stovickova3; A. Zumrova3; Z. Musova2
1Department of Neurology, Center of Hereditary Ataxias, Second Faculty of Medicine and Motol University Hospital, Charles University, Prague, Czechia; 2Department of Biology and Medical Genetics, Center of Hereditary Ataxias, Second Faculty of Medicine and Motol University Hospital, Charles University, Prague, Czechia; 3Department of Paediatric Neurology, Center of Hereditary Ataxias, Second Faculty of Medicine and Motol University Hospital, Charles University, Prague, Czechia
Background and Aims: SCA27B is a newly described autosomal dominantly inherited late‐onset ataxia caused by the expansion of GAA repeats in the first intron of the FGF14 (Fibroblast growth factor 14) gene. Recently, an excellent response to 4‐aminopyridine has been published.
Methods: 28 patients followed at the Center of Hereditary Ataxia, Motol University Hospital with chronic degenerative ataxia of unknown origin with adult‐onset were molecular‐genetically examined for the presence of the FGF14 GAA repeat expansion.
Results: The expansion in the FGF14 gene within the pathological range (GAA≥300) was found in 11 (39%) patients, and 3 patients (11%) had a borderline repeat length (GAA250‐299) with presumed incomplete penetrance. Eight patients had a positive family history of ataxia in a parent or sibling, and 6 cases were sporadic. The mean age of onset was 52 years. All patients had progressive cerebellar syndrome. Four patients (37%) presented with a parkinsonian syndrome. Significant fluctuations of symptoms during the day were present in 9 patients. Treatment with 4‐aminopyridine was initiated in 5 patients, with an excellent effect in 4 of them.
Conclusion: SCA27B is a newly described common cause of hereditary late‐onset ataxia in the Czechia. Based on the estimated frequency in the Czech population, we have included targeted molecular genetic testing for SCA27B as a standard investigation in patients with adult‐onset chronic ataxia. This step is important not only for accurate diagnosis but also because of the significant therapeutic benefit observed with 4‐aminopyridine treatment in SCA27B cases.
Disclosure: Supported by project No. LX22NPO5107 (Ministry of Education and Science).
EPO‐308
Abstract withdrawn
Epilepsy 2
EPO‐309
Therapeutic drug monitoring of antiseizure medications through quantitative dried blood spot
C. Cancellerini 1; A. Caravelli2; E. Esposito2; M. Soldà2; L. Vignatelli2; F. Bisulli1; L. Licchetta2; J. Fiori3
1Department of Biomedical and Neuromotor Sciences, University of Bologna, Bologna, Italy; 2IRCCS, Istituto delle Scienze Neurologiche di Bologna, Full Member of the European Reference Network for Rare and Complex Epilepsies (EpiCARE), Bologna; 3Department of Chemistry “G. Ciamician”, University of Bologna, Italy
Background and Aims: Therapeutic drug monitoring (TDM) of antiseizure medications (ASMs) is an essential tool for persons with epilepsy (PWE). Traditional venipuncture for TDM requires high‐volume blood and physically mandates patients at hospital1,2. Microsampling requires lower‐blood volume through less painful and invasive fingerprick offering a sampling methodology potentially performed at‐home. This study aimed to validate the extraction method of ASMs from a quantitative Dried‐Blood‐Spot microsampling (qDBS)2.
Methods: Carbamazepine (CBZ), lacosamide (LCS), levetiracetam (LEV) lamotrigine (LTG) and valproic acid (VPA) were considered. The quantification of ASMs from 10μl qDBS‐device by UHPLC‐Mass spectrometry (UHPLC‐MS/MS) was performed through an extraction technical validation, according to EMA guidelines3. Bland‐Altman analysis and Passing‐Bablok regression were performed to compare ASMS concentrations in qDBS collected with leftover venous blood and plasma samples.
Results: The method was proven accurate and precise using the chosen extraction procedure. Indeed, intra and inter‐assay reproducibility analyses showed accuracy and precision ≤15% across the calibration range (0.4‐15μg/ml CBZ; 0.5‐10μg/ml LCS; 0.5‐20μg/ml LTG; 1‐80μg/ml LEV; 10‐120 μg/ml VPA). Recovery was found >85 % and matrix effect <10% for most of the ASMs considered. Stability was tested at 7, 15, 30 days of storage, showing mutual robustness at 7‐days room‐temperature. Preliminary statistics via Bland‐Altman analysis and Passing‐Bablok regression indicated a linear correlation for most of the ASMs.
Conclusion: A UHPLC‐MS/MS assay was developed and validated according to EMA guidelines for quantifying ASMs‐qDBS3. Advantage of this validation allows the potential for utilizing the new microsampling qDBS devices, providing a patient‐friendly approach to blood sampling even at‐home in PWE.
Disclosure: Nothing to disclose.
EPO‐310
Repetitive transcranial magnetic stimulation in refractory and super‐refractory status epilepticus: A systematic review
C. Algoet; P. Boon; S. Carrette; R. Raedt; A. Mertens; K. Vonck
4BRAIN, Department of Neurology, Ghent University Hospital, Ghent, Belgium
Background and Aims: Currently, there are no guidelines available on the treatment of refractory status epilepticus (RSE) and super‐refractory status epilepticus (SRSE). Therefore, off‐label treatments are often used. We performed a systematic review regarding the efficacy of repetitive transcranial magnetic stimulation (rTMS) as a treatment in RSE/SRSE.
Methods: We systematically searched EMBASE, PubMed, Opengre.eu, CENTRAL and conference abstracts from AES and EAN meetings (2005‐2023) to identify trials investigating the use of rTMS in RSE and/or SRSE. The following parameters were collected: RSE/SRSE etiology, RSE/SRSE classification, RSE/SRSE abortion, latency to abortion, duration of RSE/SRSE before rTMS.
Results: We identified 32 patients, whereof 15 with epilepsia partialis continua (EPC). 19/32 were classified as focal motor SE, 7/32 as non‐convulsive SE and 3/32 as convulsive SE. Cortical malformations were the most frequent cause (10/32), followed by stroke (5/32) and genetic mutations (5/32). NORSE accounted for eight cases. For three and four patients respectively, data were lacking regarding classification and etiology. In 81.25% (26/32) of patients rTMS resulted in cessation of RSE/SRSE. After rTMS, two deaths (6.25%) were reported but considered unrelated to rTMS and attributed to the underlying disease. Median duration of acute/subacute RSE/SRSE and RSE/SRSE in EPC patients before rTMS was 44 days (range: 0‐140 days) and 128 days (range: 28‐7300 days) respectively. After rTMS, the latency to abortion ranged from 0‐4 days.
Conclusion: rTMS interrupts RSE and SRSE in 81.25% of patients. Data originates from studies graded as level IV with a high risk of reporting bias, warranting further studies.
Disclosure: Nothing to disclose.
EPO‐311
Deep learning‐based automated detection of focal interictal epileptiform discharges on electroencephalogram
C. Bour 1; S. Groppa2
1Neurology Department No. 2, “Nicolae Testemitanu” University, Chisinau, Republic of Moldova; 2Institute of Emergency Medicine, Chisinau, Republic of Moldova
Background and Aims: The lack of specialists in the field, combined with technical and scientific progress, is stimulating interest in developing new methods for diagnosing, classifying, and treating focal epilepsy. In this study, we focus on the use of deep learning neural networks (DLNN) for epileptic discharges detection on electroencephalography during the interictal phase.
Methods: The dataset used in this research comprises interictal electroencephalographic (EEG) recordings from thirteen patients with a diagnosis of focal epilepsy, provided by the Institute of Emergency Medicine, Republic of Moldova. Data preprocessing techniques were applied to EEG signals stored in European Data Format files. This study employed convolutional neural networks (CNNs) and long short‐term memory (LSTM) networks, which are most commonly used in the field of EEG processing. The focal discharges on EEG were split randomly into training, validation, and test sets. The accuracy, precision, and F1‐score were evaluated on the training, validation, and test sets.
Results: The study had an average accuracy of 95.7%, precision of 0.997 and an average F1 score of 0.94 on the training, validation and test sets.
Conclusion: This study substantiates the potential of DLNN in accurately identifying epileptic seizures through EEG analysis. Nonetheless, it underscores the necessity for the compilation of an extensive learning database for the algorithm, potentially introducing an additional layer of complexity to the deployment process.
Disclosure: Nothing to disclose.
EPO‐312
Stereoencephalography‐guided thermocoagulation: Experience in our center
A. Celdrán de Castro 1; H. Kevin Gil1; M. Garcés‐Sánchez1; A. Gutiérrez2; R. Conde2; V. Vicente1
1Refractory Epilepsy Unit, Neurology Service, Member of ERN EpiCARE, University Hospital La Fe, Valencia, Spain; 2Refractory Epilepsy Unit, Neurosurgery Service, Member of ERN EpiCARE, University Hospital La Fe, Valencia, Spain
Background and Aims: Stereoelectroencephalography‐guided thermocoagulation (SEEG‐guided TC) stands as an advanced therapeutic modality in the management of refractory focal epilepsy, boasting a 25% estimated seizure freedom rate, and a >50% seizure reduction rate in 58% at one year of follow‐up in some series. We conducted a retrospective analysis of outcomes in our centre.
Methods: We retrospectively analyzed patients undergoing SEEG‐guided TC at Hospital Universitario y Politécnico La Fe, Valencia, Spain´s Refractory Epilepsy Unit, spanning from January 2019 to January 2023. Patients with at least one year of follow‐up were only included. Clinical data were systematically extracted using a standardized collection form from an electronic database.
Results: The study included 41 patients (20 males, 48.8%) with a median age of 34 (9‐63). The mean follow‐up duration was 16.42 months (12‐36). At the last follow‐up, 19 patients (46.64%) remained seizure‐free, and the responder rates at 75% and 90% were 65.85% and 60.9%, respectively. In 10 out of 13 patients (76.9%) with follow‐ups exceeding two years, a seizure reduction rate of >90% was maintained. Medication was modified for only one patient, with adjustments made in two others, while the remainder maintained their existing therapeutic schedules. Postoperative permanent complications were observed in 1 patient as hemianopsia (2.4%).
Conclusion: In appropriately selected patients, SEEG‐guided TC emerges as a promising intervention, demonstrating the potential for sustained outcomes, especially when combined with pharmacological therapy.
Disclosure: Nothing to disclose.
EPO‐313
First experience with cenobamate in the treatment of paediatric patients with epilepsy: A single‐centre study
P. Danhofer; O. Horák; M. Ryzí; K. Česká; K. Španělová; H. Ošlejšková
Department of Paediatric Neurology, Faculty of Medicine, Masaryk Center for Epilepsy Brno, University and University Hospital Brno, Czechia
Background and Aims: Cenobamate is a new anti‐seizure drug currently indicated for the adjunctive treatment of focal seizures with or without secondary generalization in adult patients with epilepsy without adequate control despite prior treatment with at least 2 antiepileptic drugs.
Methods: Retrospective evaluation of paediatric patients treated at the Department of Paediatric Neurology, Faculty of Medicine, Masaryk University and University Hospital Brno, Czechia starting CNB between 4/2023 and 12/2023. We evaluated dosing and efficacy on seizures in relation to the type of epilepsy.
Results: A total of 16 patients with a mean age of 13.7 years (min 7 years; max 17 years), 8 boys and 8 girls, were included in the study. 6 patients were diagnosed with focal epilepsy, 4 patients with multifocal epilepsy, and 6 patients with LGS. Before CNB deployment, patients tried an average of 2.5 ASMs (min 1, max 4). Patients older than 12 years were dosed at 150‐200mg/day, younger patients were titrated to 100mg/day. Seizure reduction of more than 75% was achieved in 5 of 16 patients (31.2%), and seizure reduction of more than 50% was achieved in 8 of 16 patients (50.0%). Interestingly, 4 of the 6 LGS patients were included in the responder group, one of whom experienced a transient 3‐month seizure‐free period.
Conclusion: The results of our cohort are promising and show that even pharmacoresistant patients with DEE can benefit from CNB medication. Further data regarding pediatric patients and longer follow‐up will definitely be beneficial.
Disclosure: Nothing to disclose.
EPO‐314
Epilepsy and co‐morbid depression in Northern Rwanda
D. Teuwen 1; J. Kayirangwa2; I. Garrez1; J. Umwiringirwa3; T. Leers4; F. Sebera5; P. Boon1; P. Dedeken6
1Department of Neurology, University Hospital, Ghent, Belgium; 2Department of Mental Health, Ruhengeri Hospital, Musanze, Rwanda; 3Division of Education, Training and Research, King Faisal Hospital Rwanda, Kigali, Rwanda; 4Dataroots, Leuven, Belgium; 5Department of Neurology, Ndera Neuropsychiatric Teaching Hospital, Kigali, Rwanda; 6Department of Neurology, Heilig Hart Ziekenhuis, Lier, Belgium
Background and Aims: In persons living with epilepsy (PwE), depression is the most frequent co‐morbidity. The prevalence of epilepsy in Rwanda ranges between 2.9‐7.6%. In a tertiary hospital, depression is observed in more than 22% of PwE. This prospective interventional study determined the prevalence and incidence of depression in PwE in three rural villages in Northern Rwanda.
Methods: PwE enrolled between June 2018 and December 2018. At each study visit, PwE were screened for depression with Patient Health Questionnaire‐9 (PHQ‐9). If positive, the Hamilton Depression Rating Scale (HDRS) was administered to confirm diagnosis of depression. PwE with moderate to severe depression (MSD), were followed for one year and started on anti‐depressant treatment. We report depression prevalence and incidence, baseline characteristics of PwE, and clinical outcomes of PwE with and without depression.
Results: Of 304 PwE enrolled, 25 (8.2%) were diagnosed with MSD during the study. At baseline visit, prevalence of any depression and MSD was 27% and 4.3% respectively. Incidence of any depression or MSD was 245 and 48/1000 patient‐years. Improvement in seizure frequency was observed in both PwE with and without depression. There was a significant reduction in HDRS score for PwE with depression from 22.8 at baseline to 7.9 after 12 months, resulting in 94.7% of PwE having no or mild depression.
Conclusion: The Kinyarwanda versions of PHQ‐9 and HDRS were successful in screening and diagnosing depression in PwE. Treatment of epilepsy and co‐morbid depression resulted in improved outcomes, implementation of depression screening in daily neurology practice in Rwanda is warranted.
Disclosure: Peter Dedeken received consultancy fees from UCB Pharma, Merck, Pfizer, and Novartis. Dirk E Teuwen received consultancy fees from UCB Pharma. Paul AMJ Boon received speaker and consultancy fees from UCB Pharma, LivaNova, and Medtronic, as well as research grants through his institution. Ieme Garrez and Fidèle Sebera received research grants through his institution.
EPO‐315
Effects on memory of chronic hippocampal stimulation in patients with refractory mesial temporal epilepsy
E. Ray Chaudhuri 1; I. Stavropoulos2; D. Wang3; M. Cloherty4; E. Demosthenous1; R. Selway3; A. Valentín2
1Faculty of Life Sciences and Medicine, King's College London, London, England; 2Department of Clinical Neurophysiology, King's College Hospital, London, England; 3Department of Neurosurgery, King's College Hospital, London, England; 4Department of Clinical Neuropsychology, King's College Hospital, London, England
Background and Aims: Chronic, continuous, bilateral, hippocampal stimulation (CHS) is a novel treatment for refractory epilepsy in patients with bilateral independent hippocampal seizure onset unsuitable for resective surgery. This report will present a review of the current use of hippocampal stimulation (Hip‐DBS) in clinical practice and the effects of CHS on the memory of two patients with an average of 10 focal impaired awareness seizures per month (pre‐CHS).
Methods: Two patients (K1 and K2) were implanted with depth electrodes in both hippocampi for CHS in 2016 and 2017 at King's College Hospital (KCH). Both had continuous bilateral hippocampal stimulation (amplitude 1‐1.5mA, pulse duration 300‐360 microseconds, frequency 130 Hz) for more than seven years. Neuropsychological assessment was performed pre‐CHS: patient K1 had a full‐scale IQ (FSIQ) of 96 and patient K2 of 98. We also conducted a review of the use of Hip‐DBS and noted outcomes on seizure frequency and memory.
Results: At the follow up at 67 and 84 months, both patients had a marked (>90%) decrease in seizure frequency post CHS. Neuropsychometry found mildly less efficient memory in the context of low mood for patient K1 (FSIQ = 99) and potential improvement in verbal memory for patient K2 with other parameters stable (FSIQ = 103). This is in general agreement with other studies.
Conclusion: Chronic, continuous, bilateral, hippocampal stimulation has not shown clear adverse effects on memory in the literature and in the two patients implanted at KCH. The reduction of seizures and interictal activity by CHS may instead lead to an improvement in memory.
Disclosure: Nothing to disclose.
EPO‐316
Translation and validation of an epilepsy screening instrument for use in resource‐poor settings
E. Darkwa 1; S. Asiamah1; E. Awini2; C. Sottie2; A. Godi1; A. Akpalu1; J. Williams3; J. Cross4; J. Sander5; C. Newton6; A. Sen6; A. Danso‐Appiah1; P. Adjei1
1University of Ghana; 2Ghana Health Service; 3Dodowa Health Research Centre; 4UCL Ormond Street Institute of Child Health; 5UCL Queen Square Institute of Neurology; 6Oxford Epilepsy Research Group, Nuffield Department of Clinical Neurosciences, John Radcliffe Hospital, Oxford, UK
Background and Aims: The prevalence of epilepsy in sub‐Saharan Africa varies considerably and there is little data from peri‐urban areas. More community‐based studies are required to understand the true burden of epilepsy in these areas and access to Healthcare.
Methods: We developed a 17‐item epilepsy screening instrument by modifying validated English language questionnaires. We included questions on convulsive and non‐convulsive seizures. Language experts translated and back‐translated the survey instrument to two languages spoken in this region: Asante Twi and Dangme. Cases were persons with epilepsy attending healthcare facilities where these languages are spoken. Controls were unaffected relatives of cases or people attending the healthcare centers for other medical conditions.
Results: A total of 100 (50 cases and 50 controls) for Twi and 140 (70 cases and 70 controls) for Ga‐Dangme were recruited. The sensitivity and specificity of the questionnaire were: Stage 1; (Twi 98 % and 92%, Ga‐Adangme 100% and 80% respectively) and stage 2 (Twi 96% and 94%, Ga‐Adangme 98.6% and 85.7% respectively). The two versions reliably indicated epilepsy with positive predictive values of 92.5% and 83.3% for Twi and 83.8% and 87.3% for Ga‐Dangme at stages 1 and 2 respectively.
Conclusion: The current data shows that our questionnaire has good validity for the two test languages and can be used for community‐based epilepsy surveys in Ghana. The questionnaire can be adapted for other resource‐poor settings, although there will need to be iterative in‐country testing to ensure validity is maintained.
Disclosure: Nothing to disclose.
EPO‐317
The association of excessive daytime sleepiness with quality of life and mood in adults with epilepsy
E. Balian1; L. Atabekyan1; N. Nadryan1; H. Hovakimyan2; Y. Tunyan1; S. Khachatryan 1
1Department of Neurology and Neurosurgery, National Institute of Health, Yerevan, Armenia; 2Somnus Neurology Clinic, Yerevan, Armenia
Background and Aims: Excessive daytime sleepiness (EDS) is considered common in adults with epilepsy (AWE). EDS in AWE is multifactorial, including antiseizure medication (ASM) effects, seizures, poor sleep quality and accompanying affective states. We aimed to study the interconnection of EDS with health‐related quality of life (HRQOL) and mood among AWE.
Methods: AWE were examined for EDS using the Epworth Sleepiness Scale (ESS) and divided into two groups: Non‐EDS ‐ ESS score <9, EDS ‐ ESS score ≥9. HRQOL was evaluated by SF‐36 questionnaire, consisting of 8 domains (Table 1). Sleep quality was assessed using Pittsburgh Sleep Quality Index (PSQI). Validated Armenian versions were used. Hamilton scales for anxiety (HAMA) and depression (HAMD) were also used. Mann‐Whitney U test was used for statistical analysis.
Results: We included 169 AWE (mean age‐35.3 (18‐71) years, males‐52.1%), 30 (21.6%) of whom had EDS by ESS. No significant difference according to ASM status was found for EDS (ESS 5.5/4.7, p > 0.05). For the groups NonEDS/EDS ‐ BMI = 23.7/25.3kg/m2 (p > 0.05), means for SF‐36 domains for the groups are presented in Table 1. AWE with EDS had significantly lower levels of HRQOL. AWE with higher scores of the ESS had higher scores of anxiety and depression: HAMA‐13.45/20.3 (p < 0.05), HAMD‐11.5/18 (p < 0.05), and poorer sleep quality: PSQI‐7.5/9.9 (p < 0.05).
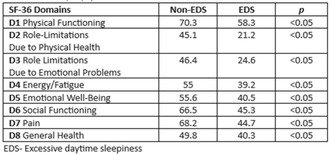
Health‐related quality of life measured by SF‐36 questionnaire in adults with epilepsy with and without EDS.
Conclusion: We found EDS in one‐fifth of AWE and it seemed not associated with ASM. AWE with EDS, had more depression and anxiety, their HRQOL was significantly lower. Our study underscores the importance of considering multiple factors behind EDS’ significant impact on quality of life in AWE.
Disclosure: Nothing to disclose.
EPO‐318
Status epilepticus as a complication of COVID‐19 vaccination: A literature review
G. Evangelista; F. Dono; M. Dasara; C. Corniello; S. Sensi
Department of Neuroscience, Imaging and Clinical Science, “G. D'Annunzio” University of Chieti‐Pescara, Chieti, Italy
Background and Aims: Status Epilepticus (SE) stands as a prominent neurological emergency, showing a mortality rate of approximately 20%. Since February 2021, a worldwide vaccination campaign has been settled to fight against the Coronavirus 19 disease (COVID‐19) pandemic. Several possible vaccine‐related adverse events have been identified including neurological manifestations. SE is beginning to surface in literature as an emergent condition in COVID‐19‐vaccinated individuals, though defined reasons accounting for this correlation are still missing.
Methods: We performed a systematic search of the literature to identify the consistency of the association between the SARS‐CoV‐2 vaccine and the SE onset. The following databases: are PubMed, Google Scholar, and EMBASE. Patient data, encompassing demographics, comorbidities, history of epilepsy, type, and dosage of SARS‐CoV‐2 vaccine, SE semiology, treatment, and prognosis were extracted.
Results: Six studies with a total of seven patients were included. Four patients showed non‐convulsive SE, 3 a convulsive one. Four patients received the mRNA‐1273 (Moderna) vaccine, 2 patients the BNT162b2 (Pfizer/Biotech), and 1 patient the ChAdOx1‐s (AstraZeneca) vaccine. The first vaccine dose (5/7, 71.4%) emerged as the most frequently associated with SE onset which manifested at an average of 4.5 days (± 3.4) post‐vaccination. Five patients presented a refractory SE and needed continuous intravenous anesthetic drug administration. Resolution of SE was achieved in all cases.
Conclusion: Status Epilepticus appears to be a rare complication associated with both SARS‐CoV‐2 vaccines. Additional studies are needed to ascertain the potential association between the Sars‐CoV‐2 vaccine and status epilepticus.
Disclosure: None.
EPO‐319
Patient outcomes in KCNQ2 developmental and epileptic encephalopathy (KCNQ2‐DEE): Systematic literature review
G. Maclaine 1; M. Potashman2; D. Pawar3; S. Sharma3; K. Rudell3; J. Lerner2; V. Coric2; A. Berg4; J. Millichap5; G. L'Italien2
1Biohaven Bioscience Ireland Ltd, Dublin, Ireland; 2Biohaven Pharmaceuticals, Inc, New Haven, CT, USA; 3Parexel International Limited, London, UK; 4Department of Neurology, Northwestern University Feinberg School of Medicine, Chicago, IL, USA and DEE‐P Connections, Washington, DC, USA; 5Department of Neurology, Northwestern University Feinberg School of Medicine, Chicago, IL, USA and Precision Epilepsy, PLLC, Chicago, IL, USA
Background and Aims: We conducted a systematic literature review to describe seizure and non‐seizure outcomes in KCNQ2‐DEE.
Methods: A systematic literature search was conducted, applying Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines, to identify and describe seizure and non‐seizure outcomes in KCNQ2‐DEE patients ≤18 years of age. Case reports/series, observational studies, non‐randomised and single arm trials, and surveys were eligible for inclusion. No geographical or publication time restrictions were applied.
Results: Of 92 publications identified, 74 reported individual patient data, of which 41 (55.4%) were case reports or series, from 363 patients. Most patients, where age data available, (42/137, 30.7%) were aged 2‐5 years. Seizures had initial onset in the first week of life for 328 (90.4%) patients. Seizure frequency, where data were available, was “multiple daily” for most patients. Seizure freedom was reported for 202 patients with cumulative proportions seizure free of 57% and 66.7% by ages 1 and 2 years respectively. Seizures recurred in 33 of 176 (18.8%) individuals. In 19 individuals for whom data were available, time to recurrence ranged from <1 month to 5 years. Non‐seizure outcomes, predominantly developmental and often other neurological and medical, were reported in 348 individuals, among whom communication issues were specified for 63 (18.1%). Other reported non‐seizure issues included vision, breathing and bulbar function (typically feeding/eating difficulties), orthopaedic and sleep.
Conclusion: Although seizure control is often achieved in KCNQ‐DEE in early childhood or infancy, most patients experience various ongoing challenges related to development, including communication.
Disclosure: This study was sponsored by Biohaven Pharmaceuticals, Inc. ATB has received consulting fees from Biogen, Biohaven Pharmaceuticals Inc, and Encoded Therapeutics; Speakers bureau for Biomarin Pharmaceuticals. JM has received royalties or licenses from UpToDate; received consultancy fees from Biohaven, Eisai, Neurocrine, and Xenon; received speaker honoraria from Biomarin and Greenwich; has participated in a Data Safety Monitoring Board for Praxis; and serves on the board of directors for Child Neurology Foundation (unpaid). GM, MHP, JL, VC and GL have received personal compensation for serving as an employee of Biohaven Pharmaceuticals. DP, SS and KR are employees of Parexel International who conducted the study on behalf of Biohaven Pharmaceuticals, Inc.
EPO‐320
Disability and depression in children and adolescents with epilepsy at a tertiary hospital in Rwanda
I. Garrez 1; D. Kajeneza2; K. Touré3; F. Sebera4; J. Umwiringirwa5; G. Umuhoza5; P. Dedeken6; P. Boon1; D. Teuwen1
1Department of Neurology, Ghent University Hospital, Ghent, Belgium; 2Department of Internal Medicine, University Hospital Center, Kigali, Rwanda; 3Centre Hospitalier Universitaire de FANN, Faculty of Medicine, Pharmacy and Odontology, Université Cheik Anta Diop, Dakar, Sénégal; 4Department of Neurology, Ndera Neuropsychiatric Teaching Hospital, Kigali, Rwanda; 5Division of Education, Training, and Research, King Faisal Hospital Rwanda, Kigali, Rwanda; 6Department of Neurology, Heilig Hart Ziekenhuis, Lier, Belgium
Background and Aims: Epilepsy is one of the most common neurological diseases in children and adolescents. The disorder affects a child's development and increases mental health diseases. We assessed the impact of epilepsy on disability and depression in children and adolescents living with epilepsy (CwE) in Rwanda.
Methods: In 2018, 74 CwE aged ≤20 years were enrolled in an observational study during their monthly neurology consultation at the tertiary Ndera Neuropsychiatric Teaching Hospital. During follow‐up in 2022, CwE or their caregivers were contacted to assess disability and to screen for depression using the Kinyarwanda Washington Group‐Short Scale (WG‐SS) and Patient Health Questionnaire‐9.
Results: In 2022, only 29 CwE (39.2%) had continued routine hospital visits. Thirty CwE or caregivers (40.5%) were identified at home and 15 (20.3%) cases remained unascertained. Among 59 CwE, five had died yielding a mortality rate of 24.2/1000 person‐years. Mean age of the remaining 54 (46.3% female) was 12.6 ± 5.6 years. Mean age at seizure‐onset was 5.7 ± 4.8 years. Generalized‐onset seizures occurred in 59.3%, with 97% motor‐onset. Focal‐onset seizures occurred in 37.0%, with 42.9% exhibiting focal‐to‐bilateral tonic‐clonic seizures. WG‐SS revealed a handicap in three (54%) and four domains (23%) and the cognitive domain was mostly affected (71%). Mild and moderate‐to‐severe depression was present in 38.1% and 14.3%, respectively.
Conclusion: This study documents prominent disability and mental health challenges in Rwandan children and adolescents with epilepsy. Improved healthcare accessibility and holistic care are required to manage disability and prevent mortality.
Disclosure: Ieme Garrez is supported by the Fund for Scientific Research Flanders (FWO). Delphine Kajeneza was supported by a grant of Fracarita Belgium. Peter Dedeken received consultancy fees from Merck, UCB Pharma and Novartis. Paul Boon received consultancy fees from UCB Pharma and grants through his institution. Dirk Teuwen received consultancy fees from UCB.
EPO‐321
Spanish validation of the Epilepsy Self‐Stigma Scale
I. Manzanares; M. Olivera; M. Centeno; M. Khawaja; A. Donaire; M. Carreño; E. Conde‐Blanco
Hospital Clínic de Barcelona, IDIBAPS, EPICARE
Background and Aims: The Epilepsy Self‐Stigma Scale (ESSS) has been developed in Japan for patients with epilepsy (PWE). We aimed to validate the scale into Spanish and examine its reliability.
Methods: We validated the ESSS to the Spanish version (ESSS‐S). Recruitment took place in September 2023. PWE also completed the Rosenberg Self‐Esteem Scale (RSES), the Hospital Anxiety and Depression Scale (HADS), and the 10‐item questionnaire (QOLIE‐10).
Results: 260 study questionnaires were completed. A two‐factor analysis explained 61.3% of the total variance: factor 1 “perceived discrimination” Cronbach's α = 0.80 and factor 2 “social isolation” 0.75. External validity was tested with both anxiety (Cronbach's α = 0.86) and depression (Cronbach's α = 0.86) sets of the HADS; stigma using the RSES (Cronbach's α = 0.92), and quality of life with QOLIE‐10 (Cronbach's α = 0.90). Perceived discrimination scores were associated with higher anxiety/depression scores (r = 0.53/0.54; p < 0.001), lower self‐esteem (‐0.53; p ≤ 0.001) and lower quality of life (r = ‐0.66; p < 0.001). Social isolation scores were also associated with higher anxiety/depression scores (r = 0.41/0.33; p < 0.001), lower self‐esteem (‐0.34; p ≤ 0.001), and lower quality of life (r = ‐0.35; p < 0.001). Perceived discrimination scores were inversely correlated with age (r = ‐0.12, p = 0.045) and directly with epilepsy duration (r = 0.20, p = 0.001), while social isolation scores were directly associated with epilepsy duration (r = 0.15, p = 0.013). The retest was stable (r = 0.77) with strong internal validity (ICC = 0.87).
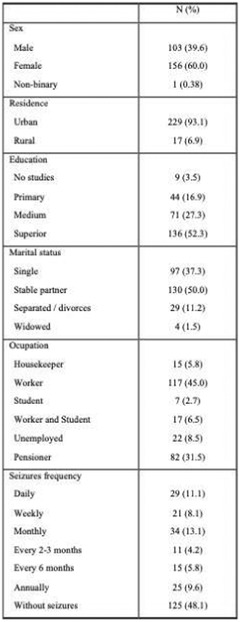
TABLE 1 Sample descriptive (N = 260).
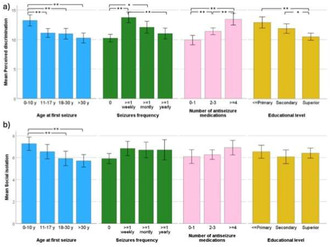
FIGURE 1 Group comparison of Perceived discrimination scores (a), and Social isolation scores (b).
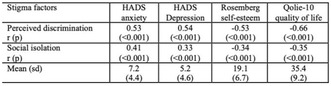
TABLE 2 Correlation of stigma factors with anxiety, depression, self‐esteem and quality of life, and descriptive. HADS: Hospital anxiety and depression scale.
Conclusion: The E‐ESSS is a valid and reliable tool for the assessment of self‐stigma in PWE among Spanish speakers.
Disclosure: No disclosures.
EPO‐322
Family history of epilepsy and seizure disorders and age of epilepsy onset in focal cortical dysplasia
I. Mihailović 1; M. Kovačević1; M. Kovačević2; D. Sokić1; D. Sokić2; A. Ristić1; A. Ristić2; I. Berisavac1; I. Berisavac2; M. Ercegovac1; M. Ercegovac2; T. Švabić‐Međevdović1; T. Švabić‐Međevdović2; N. Vojvodić1; N. Vojvodić2
1Neurology Clinic, University Clinical Center of Serbia; 2Faculty of Medicine, University of Belgrade
Background and Aims: Previous studies have established the familial occurrence and early age of epilepsy onset as predictors of genetic epilepsy but have not evaluated the rate of their occurrence based on structural epilepsy etiology. Our study determines the rate of familial occurrence and age of epilepsy onset (AEO) in patients with FCD compared to patients with known acquired causes of focal epilepsy (FE).
Methods: We retrospectively analyzed 965 patients with FE evaluated in Neurology Clinic, University Clinical Center of Serbia and identified 88 patients with radiologically defined focal cortical dysplasia (FCD). 272 patients with acquired FE (AFE) constituted the control group. Data were obtained from patient records, including sociodemographic data, AEO, family history (FH) and FE lobar diagnosis. Statistical analysis was performed in SPSS version 23.
Results: FCD patients constituted 29.7% of evaluated patients. Mean age at the disease onset was 15.06±13.22 and 20.21±14.80 years in FCD and AFE group, respectively. Positive FH was present in 10 (11.4%) FCD patients and 27 (10.7%) AFE patients, without statistically significant difference (p = 0.85) and without difference in number or degree of relatives with epilepsy (RWE) (12 RWE in FCD vs. 30 in AFE, p = 0.38). Disease onset was significantly earlier in patients with FCD and positive FH (p < 0.001), especially in those with two or more relatives with epilepsy (p = 0.01) and with insular or posterior quadrant epilepsy (p < 0.001).
Conclusion: Positive family history of epilepsy and presence of FCD are associated with earlier disease onset due to presumably higher genetic burden, which should be further evaluated by detailed genetic analysis.
Disclosure: The authors have nothing to disclose.
EPO‐323
Antiseizure medication adherence during the COVID‐19 Pandemic in South Korea: National Health Insurance data analysis
Y. Kim1; Y. Jang1; H. Lee 1; G. Park2; Y. Yoon2; S. Bong2; S. Hwang3; H. Son4; S. Lee1; K. Lee2; K. Park5
1Department of Neurology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Republic of Korea; 2Department of Statistics, Seoul National University, Seoul, Republic of Korea; 3Departments of Neurology, Ewha Womans University Mokdong Hospital, Seoul, Republic of Korea; 4Department of Neurology, Eunpyeong St. Mary's Hospital, The Catholic University of Korea, Seoul, Republic of Korea; 5Department of Neurology, Seoul National University Hospital Healthcare system Gangnam Center, Seoul National University College of Medicine, Seoul, Republic of Korea
Background and Aims: Considering the decline in prescription rates for chronic conditions throughout the COVID‐19 pandemic, this study was conducted to assess anti‐seizure medication (ASM) adherence among epilepsy patients during the pandemic.
Methods: Prevalent groups were defined by epilepsy patients of 2018, 2019, and 2020. Chronic groups of year 2018, 2019, and 2020 were defined by prevalent patients of each year who were prescribed with ASM annually from 2002 to 2010. Acute groups of year 2018, 2019, and 2020 were defined by prevalent patients of each year who were first diagnosed with epilepsy two years ago. For each group, the proportion of days covered (PDC) was analyzed to assess ASM compliance. Patients with ASM adherence more than 0.95 of PDC was categorized as the good compliance group, and others as the poor compliance group. Multifactor analyses were conducted in the prevalent groups.
Results: In 2020, 210.314, 72.051, and 30.097 patients were included in the prevalent, chronic, and acute group respectively. When compared to the previous year, ASM adherence of the prevalent and chronic group has increased in 2019 and 2020. However, for the acute group, ASM adherence has increased in 2019 but decreased in 2020 compared to the previous year.

FIGURE 1 ASM adherence of epilepsy patients by year and study design.
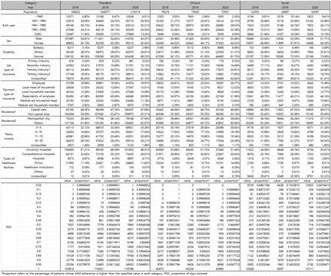
TABLE 1 Demographic profile of prevalent, chronic, and acute groups.
Conclusion: During the COVID‐19 pandemic prevailed in 2020, ASM adherence of the epilepsy patients has decreased. Further analysis of relevant subcategory will inform policy design during large‐scale pandemics and evaluate factors influencing adherence in the context of remote healthcare environments.
Disclosure: This study was supported by the SNUH Research Fund (Global Excellence center), Korea Health Industry Development Institute, Republic of Korea (RS‐2023‐00265638) and Samjin Pharm (06‐2023‐2320).
Headache 2
EPO‐324
Relationship between migraine, eating attitudes, and psychiatric symptoms: A multi‐center study in Turkey
R. Ocal1; B. Karakurum Goksel 2; M. Van1; C. Ozlem3; T. Turkish Headache Study Group4
1Department of Neurology,Antalya Training and Research Hospital, Health Sciences University; 2Faculty of Medicine, Baskent University; 3Faculty of Medicine, Gazi University; 4Turkish Headache Study Group
Background and Aims: Migraine and eating disorders may involve similar biochemical mechanisms. Previous research has indicated a higher prevalence of eating disorders in individuals with migraines compared to the general population. This study, conducted by the Turkey Headache Study Group, aimed to investigate the relationship between migraine severity, depression, anxiety, and irregular eating attitudes.
Methods: This multi‐center, prospective, case‐control study involved 20 centers across Turkey. Participants underwent assessments using the Eating Attitude Test‐26 (short form), was recorded centrally. From a pool of 1200 individuals diagnosed with headaches, a sample of 531 migraine patients meeting diagnostic criteria was selected using propensity score matching. Patient data were compared with those of 531 healthy controls. The Eating Attitude Test‐26, Beck Depression, and Beck Anxiety scales were administered to all migraine patients, and the results were compared with the healthy control group.
Results: Migraine patients exhibited significantly higher Eating Attitude Test‐26 scores and symptoms requiring referral to a psychiatrist due to eating disorders compared to the control group (p = 0.034, p = 0.0001). I. No statistically significant relationship was found between pain severity, attack frequency, and eating attitudes (r: 0.09, p = 0.055).
Conclusion: This study demonstrated statistically significant higher scores on the Eating Attitude Test‐26 in migraine patients compared to a healthy control group. These findings emphasize the need to inquire about eating disorders in individuals with migraines and highlight the importance of addressing eating attitudes in migraine management.
Disclosure: Nothing to disclose.
EPO‐325
H‐MR spectroscopy in vestibular and episodic migraine patients
H. Cubuk1; C. Cubuk 2; S. Bicakci2; Y. Bicakci1
1Department of Radiology, Faculty of Medicine, Cukurova University, Adana, Turkey; 2Department of Neurology, Faculty of Medicine, Cukurova University, Adana, Turkey
Background and Aims: The study aimed to evaluate the metabolite changes in thalamus in patients with vestibular and episodic migraine.
Methods: Fifteen patients with vestibular migraine and 15 patients with episodic migraine who had been diagnosed at Çukurova University Neurology Department were included in this prospective study. Magnetic resonance spectroscopy (MRS) was obtained at 3 Tesla MR 32‐channel head coil. SPSS v20 was used for the statistical analysis.
Results: In cases of vestibular migraine, loss of choline in the left thalamus posterior was detected. The left thalamus posterior N‐acetyl aspartate (NAA)/Choline ratio was found to increase in patients with vestibular migraine with no migraine history (p < 0.05).
Conclusion: Metabolite changes in thalamus in vestibular and episodic migraine patients could provide information about the pathophysiology of the disease and may help explain the different mechanisms of episodic migraine and vestibular migraine occurrence.
Disclosure: Nothing to disclose.
EPO‐326
Effectiveness and tolerability of eptinezumab: A retrospective analysis at 3 and 6 months in migraine patients
C. Nieves Castellanos; M. Olivier; S. Díaz Insa
Headache Unit, Hospital Universitari i Politécnic la Fe, Valencia, Spain
Background and Aims: Since April 2023, Eptinezumab has been used at our hospital to treat migraine patients, including both anti‐CGRP‐naïve individuals and those who failed other anti‐CGRP therapies. Our objective was to evaluate the response to Eptinezumab after 3 and 6 months of treatment.
Methods: Retrospective study analyzing patients treated with Eptinezumab from April to December 2023. Our analysis includes individuals with chronic and high‐frequency episodic migraine. Examining demographic features, prior treatments, migraine frequency, pain intensity (Visual Analogue Scale (VAS)), and patients' global impression of change (PGIC). Additionally, we documented any treatment‐related side effects.
Results: We analyzed 121 patients with Eptinezumab, mean age 48 years, 84.3% of women. They have failed 7.5 previous preventive treatments and in 57%, botulinum toxin was used concomitantly. 99 patients reached 3 months of treatment. Among them, 50 had tried 3 anti‐CGRP mAbs, 22 with 2, 20 with 1, and 7 had never tried anti‐CGRP. Migraine days decreased from 23.6 to 18.6, with a PGIC of 2.75. 65% experienced improvement, and 69% continued treatment after 3 months. 29 patients reached 6 months of treatment and they showed a reduction of an average of 8.6 days of migraine with an average PGIC of 2. Mild side effects occurred in 6% of patients, including two cases of mild hypersensitivity reactions.
Conclusion: Even though many patients suffer from chronic migraine and are highly refractory, a significant percentage showed benefit with eptinezumab. Therefore, we recommend prescribing eptinezumab even in cases where patients have experienced failures with other anti‐CGRP agents.
Disclosure: There are no conflicts of interest in this study.
EPO‐327
Comparison of efficacy and safety of anti‐CGRP monoclonal antibodies across age groups: A multicenter, real‐life study
I. Cetta 1; R. Messina1; L. Zanandrea1; F. Genovese1; S. Guerrieri2; B. Colombo2; M. Filippi1; I. Study Group3
1Neuroimaging Research Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; Vita‐Salute San Raffaele University, Milan, Italy; 2Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; 3IGRAINE Study Group
Background and Aims: Limited data on anti‐calcitonin gene‐related peptide (CGRP) monoclonal antibodies (mAbs)'s safety and efficacy across age groups exists. This study investigates efficacy and safety variations among age‐related groups treated with mAbs and aims to identify response predictors.
Methods: This Italian, multicentric, prospective, observational study, part of the I‐GRAINE registry, categorized patients into age quartiles (1: 18 – 40 years; 2: 40 – 50; 3: 50 – 57; 4: ≥57). Data were collected at baseline (T0) and at 3 (M3), 6 (M6), and 12 (M12) months, including monthly headache (MHD) and migraine (MMD) days, acute treatment intake in terms of days (AMD) and pills (AMP) and adverse events (AEs). At T0, psychiatric comorbidities, medication‐overuse headache (MOH) and migraine type (episodic or chronic) were also assessed.
Results: One thousand eight hundred ninety migraine patients participated, predominantly females (80%), median age 49 years (IQR: 18 – 80), 62% were chronic, 58% had MOH and 32% psychiatric comorbidities. All age groups showed significant clinical improvements at M3, M6, and M12 (p < 0.001). No significant age‐related differences in AEs (p > 0.05) were found. Females had favorable treatment responses (OR 1.3 to 3). Psychiatric comorbidity predicted positive response (OR 1.5 to 2.5) from month 6 onward. Chronic migraine (OR 2.1 to 5.8) and MOH (OR 1.8 to 4.7) indicated good response over 12 months.
Conclusion: Our findings confirm mAbs' consistent efficacy across all ages, indicating their suitability for patients with contraindications to oral preventives. Additionally, our study emphasizes considering clinical factors to predict patients’ treatment response.
Disclosure: Nothing to disclose.
EPO‐328
The presence of positive signs for functional neurological disorders is associated with migraine frequency
E. Morel1; A. Klein1; A. Scutelnic1; J. Bühler2; S. Aybek3; C. Schankin 1
1Department of Neurology, Inselspital, Bern, University Hospital, University of Bern, Bern, Switzerland; 2Psychosomatic Medicine, Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland; 3Faculty of Medicine, University of Fribourg, Fribourg, Switzerland
Background and Aims: Positive signs (PS) are the hallmark of functional neurological disorders (FND). However, in clinical practice, migraine patients without known FND may also present PS. Our aim was to evaluate the role of PS among migraine patients.
Methods: This study recruited migraine patients without a diagnosis of FND and treated at a tertiary outpatient clinic. We performed a clinical assessment for the following validated PS: give‐away, co‐contraction, sternocleidomastoid sign, trapezius elevation test, head flexion test, drift without pronation, Hoover I & II, spinal injury test, arm drop test, lip pulling sign, midline splitting, splitting of vibration sign and expressive behavior sign.
Results: Among the 72 recruited patients (mean age: 37.6 ± 15.1yo; 75% female), 31 (43.1%) had PS, of which 20 had only one PS. Splitting of vibration was the most common PS (28% of the whole cohort). Compared with patients without PS, patients with PS were older, had more comorbidities, more headache days per month and more headache intensity at the consultation. Even after adjusting for age and comorbidities, the association between the presence of PS and the number of headache days per month remained significant (OR: 1.058; 95% CI (1.000; 1.119); p = 0.049) as well as between the presence of PS and the subjective headache intensity at consultation (OR 1.277; 95% CI (1.030; 1.582); p = 0.026).
Conclusion: PS are frequent among migraine patients, mostly as isolated signs. They are associated with headache frequency and intensity. Our findings highlight the complexity of the clinical spectrum of migraine.
Disclosure: None.
EPO‐329
The effectiveness of erenumab and galcanezumab is associated with a decrease in plasma CGRP levels
D. García‐Estévez 1; A. Juanatey‐Garcia1; N. Sabbagh‐Casado1; L. Blanco‐Garcia1; J. Rodriguez‐Garrido2
1Neurology Service, University Hospital of Ourense, Ourense, Spain; 2Laboratory Service, University Hospital of Ourense, Ourense, Spain
Background and Aims: It is well established that calcitonin gene‐related peptide (CGRP) is involved in the pathophysiology of migraine. Monoclonal antibodies may work by blocking the CGRP receptor (erenumab) or binding to circulating CGRP (galcanezumab). However, how plasma levels of CGRP would be modified with the aforementioned monoclonal antibodies has not been formally studied. Our research group developed a study to determine the influence of treatment with erenumab or galcanezumab on plasma levels of CGRP.
Methods: Seventeen patients (2M/15F) with clinical criteria for high‐frequency episodic migraine or chronic migraine (CM) were studied. Previous preventive treatments with neuromodulators (topiramate or zonisamide) and the administration of onabotulinumtoxinA were allowed. Patients were treated with erenumab (n = 9) or galcanezumab (n = 8) at the discretion of the neurologist responsible for each patient's care. Plasma levels of CGRP were quantified at baseline and 6 months after follow‐up. Statistical analysis was performed using Student's T test for paired samples.
Results: The mean age of the patients was 47.4±7.9 years. Thirteen patients (76%) had the diagnosis of CM. All patients with CM maintained preventive treatment with onabotulinumtoxinA. A statistically significant reduction in the level of CGRP was found at 6 months post‐treatment (21.15±13.55 vs 15.04±8.05; p = 0.014). No significant differences were found between patients treated with erenumab or galcanezumab. Patients experienced a significant reduction in the HIT‐6 migraine disability scale (68.9±6.2 vs 63.9±6.9; p = 0.005).
Conclusion: Our study suggests that the effectiveness of erenumab and galcanezumab in improving the impact of migraine on quality of life is associated with a significant decrease in plasma CGRP levels.
Disclosure: Nothing to disclose.
EPO‐330
Hyperexcitability and precipitation/resolution of migraines. A study by sound induced flash illusions in migraine cycle
F. Brighina 1; L. Vassallo1; A. Torrente1; P. Alonge1; N. Rini1; U. Quartetti1; V. Di Stefano1; N. Bolognini2
1Department of Biomedicine, Neuroscience and advanced Diagnostic (BIND), University of Palermo, Palermo, Italy; 2Department of Psychology & Milan Centre for Neuroscience (NeuroMI), University of Milan‐Bicocca, Milan, Italy
Background and Aims: Sound‐induced flash illusions (SIFI) that critically depend on excitability of occipital cortex are reduced in migraine according to a condition of visual cortical hyperexcitability. Here we explored SIFI across the different phases of migraine cycle (ictal, pre‐ and post‐ictal) to assess how changes in cortical excitability can be related to precipitation and resolution of migraine attacks.
Methods: SIFI were evaluated in 78 migraine without‐aura patients: 18 interictal, 20 ictal, 20 pre‐ and 20 post‐ictal) and in 25 healthy controls with no different age and sex distribution across groups. Visual stimuli (flashes) and sounds (beeps) were given in different combinations: single flash/multiple beeps to induce "fission" illusion (perception of multiple flashes), multiple flashes/single beep to reduce the perceived flashes ("fusion" illusion).
Results: Fissions were significantly reduced in all migraineurs vs healthy controls (p: < .001).The highest level of reduction was observed in the ictal‐migraineurs that was significantly lower with respect to all migraine‐group (p: < .001 vs interictal, .01 vs pre‐ and post‐ictal); pre‐ and post‐ictal migraineurs perceived significantly less illusions with respect to the interictal group (p < .01).
Conclusion: Visual cortex of migraine patients was found to be hyperexcitable interictally. Excitability increases in preparatory phase (preictal), reaches its acme during the attack and then lowers toward attack‐end. This suggest a role of cortical excitability in mechanisms of migraine precipitation and ending. Moreover, they shed also light on previous paradoxical RTMS evidence by our study in migraine cycle, supporting the interpretation that the inhibitory responses are likely due homeostatic inhibitory mechanisms.
Disclosure: Nothing to disclose.
EPO‐331
Impact of erenumab treatment duration on cutaneous allodynia in patient with episodic and chronic migraine
F. Genovese 1; R. Messina1; I. Cetta1; L. Zanandrea1; S. Guerrieri2; G. Vaghi3; R. De Icco3; G. Sances4; B. Colombo2; M. Filippi1
1Neurology Unit and Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute; Vita‐Salute San Raffaele University, Milan, Italy; 2Neurology Unit; Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 3Department of Brain and Behavioral Sciences, University of Pavia; Headache Science & Neurorehabilitation Center, IRCCS Mondino Foundation, Pavia, Italy; 4Headache Science & Neurorehabilitation Center, IRCCS Mondino Foundation, Pavia, Italy
Background and Aims: This study aims to evaluate the efficacy of erenumab, a monoclonal antibody targeting the CGRP receptor, over a one‐year period in comparison to treatment lasting beyond one year, among patients with episodic and chronic migraine
Methods: In the episodic patient cohort, 25 received treatment over a one‐year period (GroupA), while 16 were treated beyond one year, up to a maximum of 21 months (GroupB). Among chronic patients, 71 and 68 were allocated to GroupA and GroupB, respectively. Clinical data were collected at baseline (T0), end of treatment (T1), after an average of 3.5 months of treatment suspension (T2), and 3‐month after resuming therapy (T3). Variables encompassed monthly headache and migraine days, acute medication usage, patients’ disability, migraine impact, pain intensity (NRS scores) and intra‐ictal allodynia (ASC‐12 scores). Intra‐group variations were assessed using Wilcoxon tests whereas between‐group differences of clinical variables modification among timepoints were explored through linear and cumulative effect statistical models.
Results: Both chronic and episodic migraine patients exhibited significant reductions in most clinical variables between T0 and T1, with no differences between the two treatment groups. Notably, in chronic patients, GroupB demonstrated a reduction in ASC12 scores during treatment, maintaining the effect post‐discontinuation. Conversely, GroupA showed no reduction during treatment, but a delayed effect during suspension. After resuming therapy all patients showed significant improvement with no differences between groups.
Conclusion: These findings suggest that erenumab could modulate nociceptive networks, contributing to allodynia symptom. However, to achieve and maintain this effect an extended treatment duration is required
Disclosure: Authors have nothing to disclose in relation to this work.
EPO‐332
White matter lesions (WML) in migraine with aura
G. Querzola 1; A. Galli1; A. Sala2; F. Frediani1
1Headache Center, Neurology and Stroke Unit Division, San Carlo Borromeo Hospital (ASST Santi Paolo e Carlo), Milan, Italy; 2Headache Center, Neurology and Stroke Unit Division, San Carlo Borromeo Hospital (ASST Santi Paolo e Carlo), Milan, Italy; Università degli Studi di Milano, Italy
Background and Aims: Several studies report the presence of WML, also potential vanishing, on brain‐MRI in patients with migraine, especially with aura (MA). There is no univocal interpretation: vascular hypothesis seems to be more probable, considering MA as a risk factor for WML and ischemic stroke, but these studies are biased, and there are controversies in literature about the prevalence of WML in MA, compared with general population.
Methods: To reduce vascular co‐morbidities, old age, misdiagnosis, and drugs biases, we enrolled 177, highly‐selected, young, subsequent patients, afferent to our Headache Center. In 146 patients we performed Brain‐MRI studies at enrollment (T0), and 12 months (T1). We compared T0‐MRI with MRI of 120 matched “healthy”, non‐migraineurs subjects, and we evaluated clinical features, co‐morbidities, cardiovascular risk factors, and thrombophilia.
Results: We found WML in 29% of the MA patients, and in 27% of the controls. There was not statistically significant difference regarding the incidence of WML, and regarding MRI‐WML between T0 and T1. We found neither association between MA features and side or number of lesions.
Conclusion: Available scientific literature about increased WML in MA patients is biased, limited, and controversial. Our study, both control‐compared and longitudinal, of highly selected and relatively young patients, shows that MA patients have not more WML than healthy subjects, rejecting the proposed correlation between MA, as an independent cerebro‐cardio‐vascular risk factor, and ischemic stroke. We are currently performing a further analysis to demonstrate whether the presence of WML is related to other co‐morbidities and risk factors.
Disclosure: Nothing to disclose.
EPO‐333
A novel ATP1A2 gene variant associated with atypical phenotype of SHM identified in a 6‐year‐old Italian female
G. Fazio 1; A. Cervellino2; M. Tagliente3; S. Manieri3; M. Di Giacomo4; N. Paciello2; E. Ferrante5; M. Trimboli6; E. Chiarella1
1Institute of Neurology, Magna Graecia University, Catanzaro, Italy; 2Department of Neurology, AOR San Carlo, Potenza, Italy; 3Department of Pediatrics, AOR San Carlo, Potenza, Italy; 4Department of Genetics, AOR San Carlo, Potenza, Italy; 5Department of Neurology, IRCCS Ospedale San Camillo, Lido Venezia, Italy; 6Department of Neurology, AOU Renato Dulbecco, Catanzaro, Italy
Background and Aims: Sporadic hemiplegic migraine (SHM) can be caused by a novel mutation in a gene that causes the familial form (CACNA1A,ATP1A2,SCN1A) or by inheritance of a gene mutation from a parent with “non hemiplegic” typical aura (2). Here, we describe a case of SHM, who carries a novel mutation in the ATP1A2gene.
Methods: A 6‐year‐old female, without family history of migraine, was admitted because she presented pulsating left‐sided fronto‐temporal headache, associated with photophobia, phonophobia, nausea/vomiting, right‐sided weakness and paresthesia, dysarthria, ataxia, acute confusion. Two similar episodes of motor weakness without loss of consciousness and dysarthria, have occurred 3 and 6 months before that admission, with complete/spontaneous resolution after 3 days.
Results: Neurological examination showed confusion, moderate right hemiparesis and hypoesthesia. CT scan was normal; brain MRI showed a slightly prominent draining sulcal veins on the left hemisphere (Fig.1). The EEG showed alteration in the background activity with prominent involvement of the left hemisphere with continuous abnormal frontal and centro‐temporal slow waves (Fig.2). SHM diagnosis was made. Sequence analysis detected a novel mutation, c.2456T>C p.(Leus819Ser), into the ATP1A2gene. Right‐sided hemiparesis and hypoesthesia disappeared 6 days after the symptoms’ onset, dysarthria lasted for 30 days before disappearing. Nimodipine and sodium valproate were introduced after the third attack and no further SHM episodes were recorded at 2‐years follow‐up.
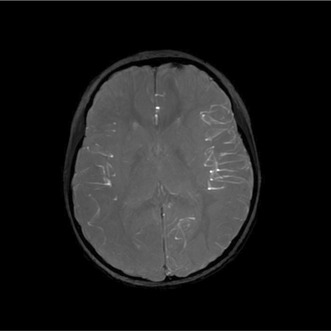
Brain MRI swan axial sequence shows a slightly prominent draining sulcal veins on the left hemisphere.
Conclusion: Early‐onset HM should be considered among the causes of focal neurological deficits. We found a novel ATP1A2 mutation, which could be responsible for the atypical phenotype, since different mutations in FHM genes partly account for clinical variability
Disclosure: Nothing to disclose.
EPO‐334
Headache in acromegaly: Not only a secondary disorder
G. Giuliani 1; D. Costa2; C. Pellicano3; M. Altieri1; P. Gargiulo2; V. Di Piero1
1Department of Human Neuroscience, Sapienza University of Rome, Rome, Italy; 2Department of Experimental Medicine, Endocrinology‐Pituitary Disease, Sapienza University of Rome, Rome, Italy; 3Department of Translational and Precision Medicine, Sapienza University of Rome, Rome, Italy
Background and Aims: Headache is frequently associated with pituitary disease, in which it can persist despite effective therapy. To better understand its actual secondary nature, we analyzed the headache characteristics in an acromegalic population.
Methods: 39 acromegalic patients, regularly followed for a long period, were examined to evaluate headache. Headache features were collected retrospectively through a structured interview. We carefully studied its time course and relationship with acromegaly, exploring the influence of adenoma and its treatment.
Results: Out of 39 patients, 27 (69.2%) reported headache. Twenty‐one patients (53.8%) met the criteria for a primary headache: 14 had episodic migraine, 4 had chronic migraine while 3 patients presented tension‐type headache. No trigeminal autonomic cephalalgia was observed. Six patients (15.4 %) fulfilled secondary headache criteria, with complete headache resolution after acromegaly treatment. Overall, a family history of headache was present in 20 cases (51.3%). Tumor size (p = 0.4) and treatment of acromegaly (p = 0.67) did not significantly influence the course of the disease.
Conclusion: In our population, only a small percentage (15.4%) of patients presented a picture consistent with a secondary headache that disappeared after acromegaly treatment. Interestingly, we observed a high prevalence of family history of headache and a high prevalence of migraine in acromegalic patients. A genetic predisposition to primary headache may be present: in this light, acromegaly, by favoring a pro‐inflammatory state (1), might act as a trigger for migraine development. Due to the limited effect of acromegaly therapy on migraine course, headache may become disabling comorbidity, requiring careful evaluation and personalized management.
Disclosure: Nothing to disclose.
EPO‐335
6‐months‐follow up of migraine patients treated with eptinezumab: Efficiency and tolerance
G. Baille 1; S. Chabalier2; A. Le Floch3
1Neurology Department, Hôpital Delafontaine, St Denis, France; 2Biostatistics, Nimes University, Nimes, France; 3Neurology Department, Nimes University Hospital, Nîmes, France
Background and Aims: Since January 2023, eptinezumab, an intravenous anti‐CGRP antibody, is authorized and reimbursed in France to treat severe episodic and chronic migraine patients. Our aim was to assess its efficiency and its tolerance "in real life" at 6 months, in an observational cohort in 2 hospitals (St Denis and Nimes university).
Methods: Patients with severe and chronic migraine, with failure of at least 2 preventive treatments and without cardiovascular comorbidities, were included if they had received 2 intravenous infusions of eptinezumab (every 3 months). The primary endpoint was change from baseline in monthly migraine days (MMDs) over weeks 1‐24. Patients completed the following patient‐reported outcomes: headache diary, intake of acute treatment for headache, 6‐item Headache Impact Test (HIT‐6) and the Hospital Anxiety and Depression scale (HAD). Other concomitant preventive treatments was also reported.
Results: 24 patients were included (M/F: 4/20), mean age (43.25 years old (SD 18.73), among them 16 had chronic migraine. The reduction of MMDs was 4.71 (SD 6.52). The >75% and >50% migraine responder rates were respectively 1% and 45.8%. No severe side effects were notified. The medication overuse rate decreased from 72.2% to 43.3%.
Conclusion: In this observational "real life" cohort, we highlighted that eptinezumab is efficient to prevent headaches in severe episodic and chronic migraine patients, with a reduction of medication overuse.
Disclosure: GB: advisory/Lecture for Lundbeck.
EPO‐336
Clinical presentation of occipital neuralgia in a headache unit
I. Ros González; Y. González Osorio; Á. Sierra Mencía; A. Recio García; S. García García; E. Varas Martín; D. García Azorín; Á. Guerrero Peral
Neurology Department, Hospital Clínico de Valladolid, Spain
Background and Aims: Occipital neuralgia is defined as a pain in one or more distributions of the occipital nerves. Case series of this entity are scarce. We aim to describe a large series of patients with occipital neuralgia.
Methods: Prospective registry of patients attended in a headache unit of a tertiary hospital. In those diagnosed with occipital neuralgia we collected demographic and clinical data.
Results: Between January‐2008 and January‐2024, we included 102 patients (78, 76.5% female) with occipital neuralgia out of 9388 (1.08%) attended in our unit. Age at inclusion was 58.2±16.4 years (range: 17‐85) and latency from onset to diagnosis 23.7±47.5 months (1‐360). In 39 cases (38.2%) pain affected right side, in 54 (52.9%) the left, and in 9 (8.8%) it was bilateral. 90 patients (88.2%) described a background pain, mostly oppressive (70 patients), and rated as 5.5±1.6 (2‐10) on a verbal analogical scale (VAS). In 59 cases (57.8%) we registered exacerbations, mostly stabbing (36 patients) and rated as 8.1±1.5 (3‐10) on a VAS. In 11 patients (10.8%) we recorded an event on the onset of pain (trauma in 10 cases). In 92 patients (90.2%) there was dysesthesia upon palpation of the scalp. Neuralgia affected in 18 cases (17.6%) the lesser occipital nerve. Before arriving at our unit 24 patients (23.5%) received an oral preventative with little or no effect.
Conclusion: Occipital neuralgia is a rare entity even in a headache unit. It is necessary to increase knowledge of this neuralgia to avoid diagnostic delays with the use of ineffective treatments.
Disclosure: No disclosure related to this work.
EPO‐337
Patterns of long‐term response to anti‐CGRP monoclonal antibodies in a 2‐year prospective cohort of migraine patients
L. Gómez‐Dabó 1; E. Caronna2; R. Mas‐de‐les‐Valls3; V. Gallardo3; E. Gine‐Cipres2; A. Alpuente2; M. Torres‐Ferrus2; P. Pozo‐Rosich2
1Headache Clinic, Neurology Department, Vall d’Hebron Hospital, Barcelona, Spain; 2Headache Clinic, Neurology Department, Vall d’Hebron Hospital; Headache and Neurological Pain Research Group, VHIR, Department of Medicine, Universitat Autònoma de Barcelona, Barcelona, Spain; 3Headache and Neurological Pain Research Group, VHIR, Department of Medicine, Universitat Autònoma de Barcelona, Barcelona, Spain
Background and Aims: Real‐world evidence on long‐term response to monoclonal antibodies targeting calcitonin gene‐related peptide (anti‐CGRP mAbs) in migraine remains limited. Objective: To describe the long‐term effectiveness and patterns of response at 2 years of anti‐CGRP mAbs in a cohort of migraine patients.
Methods: Prospective unicentric observational study including high frequency episodic and chronic migraine patients treated with anti‐CGRP mAbs. Demographics and efficacy variables (monthly headache days‐MHD; monthly migraine days ‐MMD) were collected for 24 months. We defined 4 time points (6‐12‐18‐24 months), matching to the follow‐up visits. We defined sustained response (SR) as ≥50% reduction in MHD at all time points; quasi‐sustained response (QSR) as a ≥50% reduction in MHD at 3 out of 4 time points; unsustained response (UR) as ≥50% reduction in MHD at 1‐2 out of 4 time points; and never response (NR) as <50% at all time points.
Results: 148 patients were included (mean age 47 years [40.8‐54], 82.4% (122/218) females). Median basal frequencies were 18 [14, 25.5] MHD, 13 [8, 18] MMD. After 24 months of follow‐up, 31% (46/148) had SR; 26% (38/148) had QSR; 23% (34/148) had UR; and 20% (30/148) had NR. Long‐term responders (SR+QSR) presented less allodynia (41.7%vs59.4%; p < 0.04) and higher baseline MHD and MMD (median HDM 21 vs 15.5, p < 0.014; MDM 15 vs 12.5; p < 0.016) compared to non‐long‐term responders (UR+NR).
Conclusion: Over 50% of migraine patients treated with anti‐CGRP mAbs exhibit a long‐term response that is sustained over time. Understanding patterns of long‐term response could help treatment decisions in the future.
Disclosure: LGD, RMDLV and VJG report no disclosures. EC has received honoraria from Novartis, Chiesi, Lundbeck, MedScape and his salary partially funded by Río Hortega grant Acción Estratégica en Salud 2017–2020, Instituto de Salud Carlos III (CM20/00217). He is a junior editor for Cephalalgia. AA has received honoraria from Allergan‐AbbVie, Novartis, Chiesi. MTF has received honoraria from Allergan‐AbbVie, Novartis, Chiesi and Teva. PPR has received, in the last three years, honoraria as a consultant and speaker for: AbbVie, Biohaven, Chiesi, Eli Lilly, Lundbeck, Medscape, Novartis, Pfizer and Teva. Her research group has received research grants from AbbVie, Novartis and Teva; also, Instituto Salud Carlos III, EraNet Neuron, European Regional Development Fund (001‐P‐001682) under the framework of the FEDER Operative Programme for Catalunya 2014‐2020 ‐ RIS3CAT; has received funding for RCT from AbbVie, Amgen, Biohaven, Eli Lilly, Novartis, Teva. She has been Honorary Secretary of the International Headache Society. She is in the editorial board of Revista de Neurologia. She is an associate editor for Cephalalgia, Headache, Neurologia, The Journal of Headache and Pain and Frontiers of Neurology. She is a member of the Clinical Trials Guidelines Committee of the IHS. She has edited the Guidelines for the Diagnosis and Treatment of Headache of the Spanish Neurological Society. PPR does not own stocks from any pharmaceutical company.
EPO‐338
Assessing the relative utility of a two headache “rescue rooms” and their respective treatment protocols
L. Armistead; A. Koutsandreas; J. Rothrock
Inova Health/University of Virginia, Fairfax, VA, USA
Background and Aims: We compared the relative utility of two treatment algorithms in two separate outpatient clinic headache “rescue rooms" (RRs).
Methods: In two separate university‐based RRs we compared clinical outcome, healthcare resource utilization (HRU), RR cost, patient satisfaction and mean RR time/visit using two different treatment algorithms. "A" involved primarily intramuscular (IM) administration of droperidol, and (B) involved an evidence‐based sequence of therapies beginning with subcutaneously administered sumatriptan and proceeding as needed to intravenous ketorolac, metoclopramide, DHE/prochlorperazine, metoclopramide, magnesium, divalproex sodium and dexamethasone.
Results: 100 consecutive patients were treated according to algorithm A and 100 according to algorithm B. Clinical outcomes, RR costs, decline in ER utilization and patient satisfaction were similar in the two groups. Mean time required for an RR visit was less in group A than in the group B (47 minutes versus 127 minutes). None of the 100 group A patients treated with IM droperidol exhibited QTc prolongation.
Conclusion: An outpatient headache “rescue room" conveys a high level of clinical efficacy, decreased ER utilization, and a high degree of patient satisfaction. Droperidol IM appears to be a particularly safe, effective and efficient treatment for use in this setting.
Disclosure: Nothing to disclose.
Movement disorders 3
EPO‐339
Transcranial sonography evaluation in patients with cerebellar neurodegenerative ataxias
A. Milovanović 1; O. Tamaš1; M. Mijajlović1; T. Švabić1; M. Kostić2; G. Marić3; M. Jeremić1; N. Dragašević Mišković1
1Neurology Clinic, University Clinical Centre of Serbia; 2Faculty of Medicine, Institute of Mental Health, University of Belgrade, Belgrade, Serbia; 3Institute of Epidemiology, Faculty of Medicine, University of Belgrade, Belgrade, Serbia
Background and Aims: Cerebellar neurodegenerative ataxias are disorders affecting the cerebellum and its pathways. Transcranial sonography (TCS) is widely used for the evaluation of brain parenchymal structures in various diseases especially in neuropsychiatric and neurodegenerative diseases. The objective of this study was to investigate TCS characteristics of patients with neurodegenerative cerebellar ataxias.
Methods: We included a total of 74 patients with cerebellar degenerative ataxia, 36.5% had autosomal dominant, 20.2% with autosomal recessive pattern of inheritance, and 43.3% had sporadic onset. Standardized ultrasonographic planes were used for the identification of brain structures of interest. All patients were clinically evaluated using SARA, INAS, neuropsychological, and psychiatric scales.
Results: The brainstem raphe was discontinued in 33.8% of patients. The substantia nigra (SN) hyperechogenicity was identified in 79.7%. Third and fourth ventricle enlargement had 79.7% and 45.9% of patients, respectively. A positive and statistically significant correlation was found between SN hyperechogenicity with dystonia (p < 0.01), rigidity, and dyskinesia (p < 0.05). Higher SARA total score statistically significantly correlated with the larger diameter of III (r = 0.373; p = 0.001) and IV ventricle (r = 0.324; p = 0.005).
Conclusion: Hyperechogenicity of substantia nigra has been linked to extrapyramidal signs, while raphe discontinuity to depression. Furthermore, severity of ataxia has positively correlated with III and IV ventricle diameter indicating brain atrophy.
Disclosure: None.
EPO‐340
The genetic landscape of Parkinson's disease in an Italian cohort and the need for a standardized approach
A. Cimmino 1; P. Sanginario1; F. Musso1; L. Rigon1; D. Genovese2; A. De Biase2; M. Petracca2; F. Bove2; C. Piano2; F. Tiziano3; A. Bentivoglio2; P. Calabresi2; G. Di Lazzaro2
1Università Cattolica del Sacro Cuore, Department of Neurosciences, Rome, Italy; 2Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Neurology Unit, Rome, Italy; 3Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Institute of Genomic Medicine, Rome, Italy
Background and Aims: Advances in genetics have expanded the known spectrum of Parkinson's disease (PD)‐related genes, and broadened access to genetic analysis, allowing for rapid sequencing of many disease‐associated genes and unraveling a high genetic variability. Our study aimed to determine the genetic characteristics in an Italian cohort of PD patients.
Methods: PD patients with family history, early‐onset (≤55 years), and/or atypical phenotype underwent genetic analysis through an NGS panel containing 45 known‐PD‐causative genes, coupled with MLPA when needed. Variants were interpreted according to ACMG criteria, and reports were categorized as positive (≥1 variant, with definite genetic diagnosis), inconclusive (≥1 variant, insufficient for genetic diagnosis), or negative. Heterozygous pathogenic/likely‐pathogenic variants in dominant genes and biallelic pathogenic/likely‐pathogenic variants in recessive genes were considered positive. GBA1 variants were considered pathogenic and classified based on PD‐development risk. Inconclusive reports underwent reassessment: heterozygous pathogenic variants in recessive genes and VUS with genotype‐phenotype mismatch were considered negative; VUS not otherwise interpretable were clarified through family segregation studies.
Results: We recruited 197 patients. 74 (37.6%) reports revealed ≥1 variant. Of the inconclusive reports, after reinterpretation, 1 was considered positive, while 22 negative. Eventually, positive reports were 36 (18.3%), and inconclusive 16 (8.1%). The most common diagnoses were GBA1 (23, 11.7%), LRRK2 (5, 2.5%), PRKN (4, 2.0%), PINK1 (1, 0.5%) FBXO7 (1, 0.5%). The gene with the most reported variants was GBA1.
Conclusion: Our results contribute to a more in‐depth understanding of PD genetic spectrum in Italian patients and underscore the importance of a standardized approach for the interpretation of genetic findings.
Disclosure: Nothing to disclose.
EPO‐341
Stigma among Tunisian patients with Parkinson's disease: The hidden side of the burden
A. Rekik; A. Mili; K. Jemai; E. Jarrar; S. Naija; A. Hassine; S. Ben Amor
Department of Neurology of Sahloul Hospital Sousse, Faculty of medicine of Sousse, Tunisia
Background and Aims: Stigma among patients with Parkinson's disease (PD) is multilayered and a determinant of the quality of life. The social and cultural components can modulate efficiently this aspect. Thus, we aim to investigate stigma among PD patients in Tunisia in order to boost their quality of life.
Methods: We have conducted a cross‐sectional study including patients with PD who presented to our clinic for regular follow‐up from October to December 2023 and consent to participate. We identified general and motor characteristics using UPDRS‐III score. We used MMSE for cognitive function and SCOPA‐Aut questionnaire to identify dysautonomic features. Stigma was assessed based on the 8‐item Stigma Scale for Chronic Illness (SSCI‐8) and we used the raw summed score ranging from 8 to 40.
Results: We included 62 patients (sex‐ratio = 1.4; mean disease duration of 11; 62%; illiterate). Mean UPDRS‐III score was 23.6±5 with tremor‐dominant PD being the most frequent (56.5%), followed by postural instability gait disorder (PIGD) phenotype (24%). Mean MMSE score was 21.4±6. Dysautonomia was noted in 66% of cases with gastrointestinal dysfunction being the most prominent (60%). Mean SSCI‐8 score was 66.3 [40; 77]. SSCI score correlated positively with illiteracy (p = 0.023), higher UPDRS‐III score (p = 0.001), PIGD‐phenotype (p = 0.048), tremor‐dominant phenotype (p = 0.026), cognitive dysfunction (p = 0.036) and gastrointestinal dysfunction (p = 0.042).
Conclusion: Stigma is frequent and severe among Tunisian patients and exceeds the rates reported from Europa and North America. It is conditioned by educational level, motor and non‐motor features. Our findings highlight the necessity of a holistic approach beyond the motor aspect. Raising awareness is mandatory to pave the way for a more tolerable environment.
Disclosure: None.
EPO‐342
Suvecaltamide metabolites are CaV3 modulators and contribute to pharmacological effect
E. Brigham; W. Zeng; N. Shanks; M. Lee
Jazz Pharmaceuticals, Palo Alto, CA, USA
Background and Aims: T‐type calcium (CaV3) channels regulate neuronal excitability and are thought to play a key role in mediating pathological tremor‐producing oscillations in conditions like essential tremor (ET). Suvecaltamide (JZP385), a potent, selective CaV3 modulator, improved function in adults with moderate‐to‐severe ET in a phase 2 study (T‐CALM/NCT03101241). We present potency‐concentration relationships and combined pharmacological effects for suvecaltamide and its 2 active metabolites (JZZ05000034 = M01, JZZ05000035 = M02; total active moiety [TAM]).
Methods: Automated patch‐clamp recordings in HEK293 cells stably overexpressing human CaV3 subtypes were used to generate steady‐state inactivation curves with/without analyte treatments; concentration‐response curves used protocols enriching for resting or inactivated channel states. Off‐target effects were tested in enzyme and receptor binding panels.
Results: All analytes inhibited all CaV3 channels in a concentration‐ and state‐dependent manner (Table) and slowed recovery from inactivation. Selectivity (<50% [10 μM]) was demonstrated for all targets/analytes, except suvecaltamide at CB2 receptor (IC50 = 5.3 μM) and M01 at human PPAR‐gamma (54% at 10 μM) and guinea‐pig adenosine transporter (IC50 = 2.9 μM), which are likely not relevant at projected therapeutic doses.
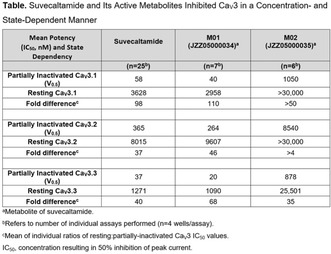
Suvecaltamide and Its Active Metabolites Inhibited CaV3 in a Concentration‐ and State‐Dependent Manner.
Conclusion: Suvecaltamide and its active metabolites demonstrate selective, state‐dependent modulation of all CaV3 subtypes with markedly higher affinity for partially inactivated channels. Modelling TAM shows that, at clinically relevant concentrations, suvecaltamide and its metabolites may selectively inhibit channels enriched under hyperexcitable conditions (eg, pathological neuronal firing) while sparing channels involved in normal signalling, which may contribute to a more optimal clinical profile. Two ongoing phase 2 studies are evaluating suvecaltamide in adults with moderate‐to‐severe ET (NCT05122650) or residual Parkinson's disease tremor (NCT05642442).
Disclosure: Supported by Jazz Pharmaceuticals. All authors are full‐time employees of Jazz Pharmaceuticals who, during this employment, have received stock options exercisable for, and other stock awards of, ordinary shares of Jazz Pharmaceuticals, plc.
EPO‐343
Reprogramming options after IPG replacement in STN DBS for Parkinson's disease: Is the upgrade worth the cost?
A. Boogers 1; M. Justich1; M. Montiel1; I. Alhashyan1; S. Naghdlou1; S. Kalia2; A. Lozano2; R. Munhoz1; A. Fasano1
1Department of Neurology, Toronto Western Hospital, Toronto, Canada; 2Department of Neurosurgery, Toronto Western Hospital, Toronto, Canada
Background and Aims: People with Parkinson's disease (PD) having motor fluctuations can be treated with deep brain stimulation targeting the subthalamic nucleus (STN DBS)1. The lifetime of non‐rechargeable implantable pulse generators (IPG) requires battery replacements every 3‐5 years2. Recently, IPGs with more programming features have become readily available.
Methods: This double‐blind cross‐over randomized study recruited consecutive PD patients undergoing IPG replacement surgery in whom the Activa PC was replaced with a Percept PC (Medtronic, Minneapolis, MN, USA). Reprogramming was done to reduce stimulation‐induced side effect and/or to lower battery consumption (i.e. avoiding bipolar or interleaving settings). Change of active contact could only be done based on the Brainsense Survey (contact with highest beta peak). Bipolar and interleaving settings were replaced by monopolar, double, triple or quadruple monopolar settings (Shapelock). Pulse width could be shortened beyond 60 mcsec. Change in frequency was only allowed when switching to independent frequencies per hemisphere.

During the baseline visit, patients underwent reprogramming in medication‐off condition using novel stimulation features. They were randomized between the established and the novel stimulation paradigm for a month. Thereafter, they were crossed over.
Results: 19 patients (38 STNs) were included (four females). In 19 STNs (50%), the stimulation settings were changed from bipolar or interleaving to a (multiple) monopolar configuration using the Shapelock feature. Pulse width was shortened in 15 STNs (39.5%). A change in contact was done in 4 STNs (10.5%) after an average of 6.5 years on another contact. Eleven patients (57.9%) preferred the novel stimulation paradigm, while 6 patients (31.6%) preferred their established program. Two patients were undecided.
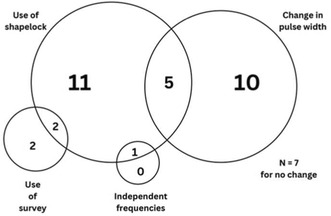
Features used when reprogramming after battery replacement surgery.
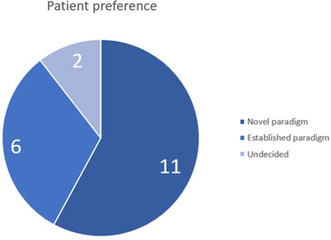
Pie chart of patient preference between the novel stimulation paradigm (n = 11) and the established stimulation paradigm (n = 6). Two patients did not have a preference between the two programs.
Conclusion: DBS reprogramming using novel additional features after IPG replacement can lead to improved outcomes and/or reduced battery consumption in a sizable proportion of patients.
Disclosure: AL received honoraria and research support from Medtronic. SK received honoraria and research support from Medtronic. AF received honoraria and research support from Medtronic.
EPO‐344
Incidence and risk factors of glaucoma in Parkinson's disease: A population‐based study
B. Yoon 1; S. Jung2; Y. Shim3; H. Kim4
1Department of Neurology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea; 2Department of Neurology, Hallym University Medical Center Kangnam Sacred Heart Hospital, Seoul, Republic of Korea; 3Department of Neurology, The Catholic University of Korea Eunpyeong St. Mary's Hospital, Seoul, Republic of Korea; 4Department of Clinical Epidemiology and Biostatistics, Asan Medical Center, Ulsan University College of Medicine, Seoul, Republic of Korea
Background and Aims: The potential association between Parkinson's disease (PD) and glaucoma remains unclear. We aimed to investigate glaucoma incidence in PD patients, explore the differences by age and sex, and identify potential risk factors for glaucoma in Korean PD patients.
Methods: We conducted a comprehensive study using data from the Korean National Health Insurance System database, encompassing 97% of the Korean population from 2002 to 2019. We calculated the incidence of newly developed glaucoma among PD patients and estimated the adjusted hazard ratio (aHR) with 95% confidence intervals (CI) using Cox proportional‐hazards models to elucidate glaucoma risk factors.
Results: Among 176,673 patients with PD, 9,718 patients developed glaucoma during the follow‐up period (3,670 men and 6,048 women), yielding an overall incidence of 8.02 per 1,000 person‐years. Stratified by age group and sex, we observed an increasing incidence with age until 80, with minimal sex differences. In particular, older age (aHR = 1.78, 95%CI: 1.55‐2.05 in the 60s), diabetes mellitus (DM) (aHR = 1.19, 95%CI: 1.14‐1.25), and hyperlipidemia (aHR = 1.06, 95%CI: 1.01‐1.10) emerged as significant risk factors for glaucoma in PD patients.
Conclusion: Our study suggests that PD patients face an elevated risk of glaucoma compared to the general population, with no substantial sex differences. Older age, the presence of DM, or hyperlipidemia were identified as risk factors for glaucoma in PD patients. These findings emphasize the significance of considering regular ophthalmologic evaluation as part of their management in PD patients, particularly among those with a history of DM or hyperlipidemia, regardless of age or the presence of visual symptoms.
Disclosure: Nothing to disclose.
EPO‐345
Neuroleptic malignant syndrome in Huntington's disease
B. Ravera 1; A. Funcis1; P. Zinzi2; M. Solito2; M. Petracca1; P. Calabresi1; A. Bentivoglio1
1Institute of Neurology, Catholic University of the Sacred Heart, Rome; 2Institute of Neurology, Policlinic A. Gemelli Foundation, Rome
Background and Aims: Huntington's disease (HD) is often treated with tetrabenazine (TBZ) and dopamine receptor blocking agents (DRBAs). Few data are available regarding the likelihood of neuroleptic malignant syndrome (NMS) development in HD patients. In this article we investigate the main risk factors that lead to the development of NMS in HD patients, and discuss the measures to avoid this potentially life‐threatening condition.
Methods: We gathered data from the 5th data set of the Enroll‐HD study (PDS5), a literature review, and described a case report. We selected HD patients treated with TBZ and/or DRBAs, who presented at least one of the core symptoms of NMS, therefore including atypical forms.
Results: We identified 12 cases of NMS in HD patients in total, three of which showed atypical forms of NMS. Only one out of 5108 patients, treated with DBRA and/or TBZ, was identified in the Enroll‐HD dataset. All patients developed NMS in conjunction with drug‐therapy changes, with average onset within a month, except one patient during ongoing treatment with TBZ. Five out of the twelve patients developed NMS while undergoing TBZ. Overall, the patients showed a long clinical history of HD.
Conclusion: NMS is likely underestimated in HD patients partly due to missed diagnosis of cases with atypical presentation. Therefore, careful monitoring of symptoms may allow early detection of this potentially fatal condition. Abrupt changes in therapy, are the main risk factors for NMS development, hence the importance of periodic revision of treatment and cautious drug management, especially in advanced stages of HD.
Disclosure: Nothing to disclose.
EPO‐346
Deep brain stimulation as an effective therapy in atypical two stage evolution adult‐onset KMT2B‐related dystonia
C. Desjardins; S. Sangla; C. Hubsch
Department of Neurology, Movement Disorders Unit, Fondation Adolphe de Rothschild, Paris, France
Background and Aims: In KMT2B‐related dystonia (DYT‐KMT2B), onset occurs typically, in the first decade of life with focal involvement progressing to generalized dystonia, prominently affecting the cranial, cervical and bulbar regions. Later onset has been reported, with upper body parts and oromandibular involvement. We report an adult‐onset case of severe DYT‐KMT2B with improvement after bi‐pallidal deep brain stimulation (GPi‐DBS).
Methods: We report the phenomenology and genetic data of an adult with DYT‐KMT2B.
Results: Cervical dystonia initiated at 33y, evolving through two phases: an initial calm period and a subsequent exacerbation phase. While botulinum toxin injections provided relief from 33 to 47 years, the dystonia significantly worsened from 47 to 49 years, manifesting a cranio‐caudal progression with blepharospasm, oromandibular dystonia, upper limb and trunk dystonia, and a myoclonus component (Video). Chewing difficulties necessitated a gastrostomy. The Burke‐Fahn‐Marsden Movement and Disability Subscales (BFMMS and BFMDS) scores were 30 and 21, respectively, with ineffective conventional therapies and botulinum toxin injections. Genetic analysis unveiled a heterozygous variant in KMT2B: NM_014727.2:c.631T>G/p.(Cys211Gly). GPi‐DBS led to a postoperative dystonic crisis, requiring a one‐week stay in intensive care. Rapid clinical improvement ensued within a month, with BFMMS and BFMDS scores reduced to 5 and 1, respectively (monopolar stimulation,3.2 mA, 210 μs pulse width, 130 Hertz). Although oral feeding resumed, blepharospasm persisted, prompting medication discontinuation.
Conclusion: Only a few studies demonstrate the benefit of GPi‐DBS in adult‐onset DYT‐KMT2B. Our case highlights that GPi DBS appears to be as effective in adult‐onset as in childhood‐onset DYT‐KTM2B and emphasized the importance of postoperative monitoring.
Disclosure: The authors declare that there are no conflicts of interest relevant to this work.
EPO‐347
Striatal dopamine correlates to spatial gait parameters in dual task conditions
C. Zatti 1; A. Pilotto1; A. Rizzardi1; A. Galli1; C. Hansen2; M. Catania1; R. Romijnders2; W. Maetzler2; A. Padovani1
1Department of Clinical and Experimental Sciences, Neurology Unit, University of Brescia, Italy; 2Department of Neurology, Christian‐Albrechts‐University of Kiel, Kiel, Germany
Background and Aims: Parkinson's disease (PD) is clinically defined by motor symptoms and the underlying mechanism is determined by loss of dopaminergic neurons in the substantia nigra, leading to dopamine depletion in the basal ganglia circuit. Despite this, the MDS‐UPDRS‐III, the standard motor assessment, does not correlate with the dopaminergic deficit. The aim of this study was to investigate the relationship between dopamine uptake and motor changes using inertial sensors.
Methods: Forty de novo PD patients were enrolled. They underwent a comprehensive motor assessment including MDS‐UPDRS‐III and digital assessment of gait parameters in normal, fast and dual‐task conditions using mobile health technologies (MHT) in a supervised setting. All patients underwent 123I‐FP‐CIT‐SPECT imaging to quantify dopaminergic uptake. The relationship between motor parameters and dopamine binding was assessed using partial correlations corrected for age, sex and height.
Results: No correlation was observed between MDS‐UPDRS‐III and dopamine uptake in the striatal circuit. Step length in single and dual task conditions correlates directly with MDS‐UPDRS‐III (p: 0.001 R: 0.376), while reduced step length in dual task conditions is associated with reduced DAT availability in both putamen and pallidum (p: 0.022 and 0.013 with R: 0.417 and R: 0.428).
Conclusion: Dopamine depletion is known to be the pathological mechanism underlying motor changes in PD. Our study suggests that the use of more sensitive parameters, specifically spatial parameters in dual task conditions, can identify this relationship.
Disclosure: Nothing to disclose.
EPO‐348
Efficacy of safinamide in Parkinson's disease: Focus on gender differences
C. Cattaneo 1; I. Marjanovic2
1Medical Department Zambon SpA, Bresso, Italy; 2Medical Department Zambon SpA, Bresso, Italy
Background and Aims: There is an increasing evidence of gender differences in the epidemiology and clinical manifestation of both motor and non‐motor symptoms of Parkinson's disease (PD). Nevertheless, few data are available on gender differences in the response to antiparkinsonian drugs. Safinamide has a unique dopaminergic and non‐dopaminergic mechanism of action that might improve patients’ care in both sexes.
Methods: The gender differences in safinamide efficacy were investigated using the data from two clinical trials, studies SYNAPSES (Europe) and XINDI (China).
Results: 616 (38%) out of 1610 patients enrolled in the SYNAPSES study were women and 994 (62%) men, while in the XINDI study 128 (42%) out of 305 patients enrolled were women and 177 (58%) men. Safinamide significantly improved motor symptoms (p < 0001), motor fluctuations (p = 0.0007) and quality of life (p = 0.0014) in both genders, with a good safety profile and without requiring any change in the concomitant dopaminergic therapy. Moreover, safinamide improved three out of four PD cardinal symptoms and reduced tremor in females and rigidity in males, the two peculiar gender features of PD.
Conclusion: Safinamide, administered as add‐on therapy in fluctuating PD patients, improved motor symptoms and motor complications without increasing troublesome dyskinesia in both male and female subjects. Further prospective studies specifically addressing potential gender differences in response to PD therapies are needed to develop tailored management strategies.
Disclosure: Carlo Cattaneo is an employee of Zambon SpA; Ivan Marjanovic is a consultant of Zambon SpA.
EPO‐349
Navigating the maze: Unmasking the influence of cerebral small vessel disease on non‐motor symptoms burden in PD
C. Santoro 1; D. Urso2; V. Gnoni2; L. Batzu3; S. Landolfo1; A. Giugno2; S. Rota3; D. Vilella2; R. De Blasi4; K. Chaudhuri3; G. Logroscino2
1Department of Basic Medical Sciences, Neuroscience and Organ Sense, University "Aldo Moro", Bari, Italy; 2Center for Neurodegenerative Diseases and the Aging, Department of Clinical Research in Neurology, University of Bari “Aldo Moro”, “Pia Fondazione Cardinale G. Panico”, Tricase, Lecce, Italy; 3Institute of Psychiatry, Psychology and Neuroscience, Department of Basic and Clinical Neuroscience, Division of Neuroscience, King's College London, London, UK; 4Department of Diagnostic Imaging, Pia Fondazione di Culto e Religione “Card. G. Panico”, Tricase, Lecce, Italy
Background and Aims: Managing Parkinson's disease (PD) poses a significant challenge, primarily due to the prevalence of non‐motor symptoms (NMS). While the impact of Lewy‐Body and Amyloid pathology on PD‐related cognitive impairment is known, the role of vascular co‐pathology remains uncertain. This study explores potential links between white matter hyperintensities (WMH) and specific NMS‐clusters.
Methods: A cohort of 66 PD patients underwent comprehensive assessments, including clinical evaluations of both motor and NMS, neuropsychological tests covering five major cognitive domains and brain 3.0T magnetic resonance imaging. The severity and distribution of WMH were visually rated using Fazekas and Scheltens scales. Statistical analyses, including Mann‐Whitney tests and Spearman correlations, were employed to assess associations between WMH burden, cognitive functions, and NMS.
Results: Prominent connections with NMS, particularly urinary dysfunction, were observed in the frontal and parietal lobes. Significant correlations were found between WMH burden and cognitive functions. MMSE scores negatively correlated with Fazekas WMH total and frontal deep white matter loads. Executive dysfunction was linked to greater Fazekas and Scheltens lobar WMH loads, while language impairment was associated with frontal and parietal WMH burdens.
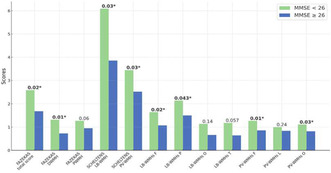
Examining two groups (MMSE < 26, n = 22; MMSE > 26, n = 44), this chart reveals significant associations between lower MMSE scores and increased Fazekas and Scheltens total burden and sub‐scores especially in the deep lobar areas.
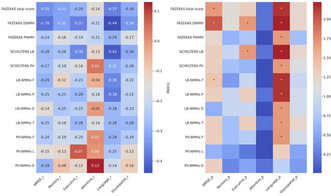
The left heatmap shows Spearman correlation coefficients exploring the interplay between cognitive domains (including MMSE) and white matter lesion severity and distribution; the right one instead highlights p‐values post‐Benjamini correction.
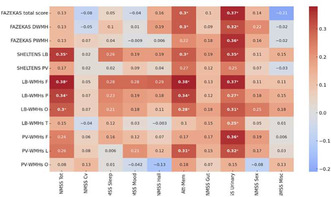
This heatmap illustrates Spearman correlation coefficients (r) examining the relationship between the vascular burden of WMH (measured by Fazekas and Scheltens scales) and various domains of NMS assessed by NMS scale.
Conclusion: Our findings suggest significant associations between radiological WMH sites and distinct NMS that might be unintentionally overlooked in clinical contexts. We propose a cortical‐subcortical "disconnection syndrome," indicating disruptions in communication between different cortical and subcortical regions. This syndrome may play a crucial role in the development or progression of distinct non‐motor and cognitive patterns in PD. Recognizing regional‐specific white matter damage enriches cognitive and NMS assessments, offering refined options for personalized medicine.
Disclosure: Nothing to disclose.
EPO‐350
Beta power circadian modulation in patients with Parkinson's disease and conventional or adaptive deep brain stimulation
C. Baiata 1; S. Manfroni1; L. Caffi2; M. Locatelli3; A. Ampollini3; S. Bonvegna1; C. Palmisano4; I. Isaias5
1Parkinson Institute Milan, ASST G.Pini‐CTO, Milano, Italy; 2Parkinson Institute Milan, ASST G.Pini‐CTO, Milano, Italy; University Hospital Würzburg and Julius Maximilian University of Würzburg, Würzburg, Germany; The BioRobotics Institute, Scuola Superiore Sant’Anna, Pisa, Italy; 3Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milano, Italy; 4University Hospital Würzburg and Julius Maximilian University of Würzburg, Würzburg, Germany; 5Parkinson Institute Milan, ASST G.Pini‐CTO, Milano, Italy; University Hospital Würzburg and Julius Maximilian University of Würzburg, Würzburg, Germany
Background and Aims: Increased beta power oscillations in the subthalamic nucleus (STN) are a key feature of Parkinson's disease (PD). However, their physiological contribution to motor and non‐motor tasks, such as the sleep‐awake cycle, is still poorly understood, and may influence the effect of deep brain stimulation (DBS), both in conventional (cDBS) and adaptive (aDBS) modes. The aim of the study is to investigate the impact of cDBS and aDBS on sleep‐wake subthalamic beta power fluctuations in PD
Methods: We acquired subthalamic local field potentials (LFP) in four patients with idiopathic PD and implanted with the AlphaDBS device (Newronika SpA). This device can operate in either cDBS, with constant stimulation parameters, or aDBS, adjusting linearly the current amplitude with respect to subthalamic beta power. Patients were recorded consecutively for 10 days in both stimulation modes and with unchanged drugs doses. We calculated the amplitude of the STN‐LFP in a patient‐specific frequency range centered around the most prominent beta peak with 1 min resolution and analyzed the distribution of the beta amplitude separately for the sleeping and waking time
Results: One patient showed a median reduction in subthalamic beta power during sleep compared to waking hours of 15%, under both stimulation modes. All other patients had sleep‐awake beta power modulation <5% in both stimulation modes. The stimulation modes did not affect the sleep‐awake modulation of subthalamic beta power.
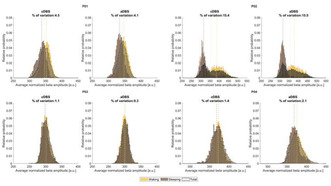
Sleep‐awake beta power distribution.
Conclusion: Our preliminary data show a variable modulation of subthalamic beta power during sleep‐wake cycle in parkinsonian patients with comparable impact of cDBS and aDBS
Disclosure: Nothing to disclose.
EPO‐351
Effects of loading, tapping performance, and ballistic movements on tremor features in patients with essential tremor
D. Birreci; D. Costa; L. Angelini; A. Cannavacciuolo; M. Passaretti; A. Martini; S. Grandolfo; M. De Riggi; G. Paparella; M. Bologna
Department of Human Neurosciences, Sapienza, University of Rome, Rome, Italy
Background and Aims: In recent years, a comprehensive set of neurophysiological tests, including the loading test, tapping performance analysis, and the evaluation of response to ballistic movements, has been proposed to formulate laboratory‐supported criteria for diagnosing functional tremor. Our aim is to comprehensively evaluate the effects of these manoeuvres on tremor features in patients with essential tremor (ET).
Methods: ET patients were evaluated using a standardized clinical scale, the Fahn‐Tolosa‐Marin Tremor Rating Scale (FTM‐TRS). A comprehensive tremor evaluation at baseline and during loading, finger tapping (at 1, 3, and 5 Hz), and ballistic movements was conducted using an optoelectronic system. Data were analyzed through non‐parametric Friedman Analysis of Variance (ANOVA).
Results: Thirteen ET patients were included (6 females, 64.9±17.6 years), with a mean disease duration of 15.6±10.9 years and a FTM‐TRS score of 20.6±10.1. At baseline, postural tremor had a mean frequency of 5.98±1.42 Hz and a mean amplitude of 0.053±0.036 GRMS^2. ANOVA unveiled a difference in amplitude (p = 0.03), with lower values during 1 Hz finger‐tapping movements, compared to the other conditions. Moreover, we found an inverse correlation between baseline tremor amplitude and the reduction in tremor amplitude during 1 Hz tapping (p = 0.021). No variation in tremor frequency was revealed across different manoeuvres (p = 0.62).
Conclusion: Gaining insights into the impact of loading, tapping performance, and ballistic movements on tremor features in patients with ET holds relevance for clinical applications, especially within the diagnostic process. Expanding the analysis to larger patient samples could contribute to a deeper understanding of how clinical factors influence the observed effects.
Disclosure: Nothing to disclose.
EPO‐352
Altered motor cortex excitability in Parkinson's disease patients
P. Ortelli1; V. Versace1; S. Dezi1; A. Precup1; S. Buechner2; C. Raccagni2; L. Saltuari1; A. Oliviero3; R. Maestri4; N. Giladi5; D. Ferrazzoli 1; L. Sebastianelli1
1Department of Neurorehabilitation, Hospital of Vipiteno (SABES‐ASDAA), Vipiteno‐Sterzing, Italy; Teaching Hospital of the Paracelsus Medical Private University (PMU), Salzburg, Austria; 2Department of Neurology, Hospital of Bolzano (SABES‐ASDAA) – Teaching Hospital of the Paracelsus Medical Private University (PMU), Bolzano, Italy; 3FENNSI Group, Hospital Nacional de Parapléjicos, Servicio de Salud de Castilla La Mancha, Toledo, Spain; 4Istituti Clinici Scientifici Maugeri, IRCCS, Department of Biomedical Engineering of Montescano Institute, Pavia, Italy; 5Brain Institute, Tel Aviv Soursky Medical Center, Tel Aviv, Israel
Background and Aims: In Parkinson's disease (PD), pathological activity of basal ganglia‐thalamocortical circuits affect neural networks subtending motor and non‐motor symptoms. This disruption could be unveiled by exploring primary motor cortex (M1) with transcranial magnetic stimulation (TMS). We extensively assessed a combined neurophysiological‐neuropsychological evaluation in a cognitively spared population of PD patients (PDp).
Methods: 15 PDp and 11 healthy controls (HC) were enrolled. Fatigue was evaluated with Parkinson Fatigue Scale (PFS‐16), attention was measured with computerized Sustained Attention Task (SAT) and Stroop Task (ST). Global cognition in PDp was evaluated with Montreal Cognitive Assessment (MoCA). Following TMS of dominant M1, we assessed Resting Motor Threshold (RMT), Motor Evoked Potential (MEP) amplitude and Silent Period (SP) duration. Intracortical activity was explored with Short‐Interval Intracortical Inhibition (SICI), Intracortical Facilitation (ICF) and Long‐Interval Intracortical Inhibition (LICI).
Results: Mean MoCA score was 24.2 (SD ± 3.3). PFS score was higher in PDp (p = 0.03). Reaction times were longer in PDp in SAT (p = 0.002), ST‐incongruent condition and ST‐interference (p = 0.005 and p = 0.036, respectively). In PDp, RMT was higher (p = 0.43), MEP amplitude was lower (p = 0.26), SP duration was shorter (p = 0.001) and LICI at 100 ms interstimulus interval (ISI) was reduced (p = 0.013). SICI at 2 and 3 ms ISI was disrupted (MEPs were facilitated) in both groups. No difference was observed in ICF.
Conclusion: Neurophysiological findings suggest that M1 hypoexcitability and altered GABAB activity possibly affect motor control and attention in PD. Aging‐related GABAA circuits disruption we found in both groups may contribute to fatigue perception in PD.
Disclosure: Nothing to disclose.
EPO‐353
The influence of deep brain stimulation on saccades in Parkinson's disease: A transversal and longitudinal study
D. Damas 1; I. Carvalho1; S. Matos1; A. Jorge1; A. Martins1; F. Cidade2; J. Castelhano3; R. Pereira4; F. Moreira1; J. Lemos1
1Neurology Department, Coimbra University Hospital; 2Faculty of Sciences and Technology of the University of Coimbra; 3Faculty of Medicine of the University of Coimbra; 4Neurosurgery Department, Coimbra University Hospital
Background and Aims: Saccades are disrupted in Parkinson's disease (PD), both involuntary (i.e., saccadic intrusions [SI]), reflexive (i.e., prosaccades [PS]) and more voluntary (i.e., antisaccades [AS]) saccades, eventually deteriorating vision. Deep Brain Stimulation (DBS) seems to improve saccadic parameters in PD patients. There is need to evaluate if such effect is sustained over time and if saccades’ planes are individually influenced by DBS.
Methods: We recruited 23 PD patients (14 males, mean age 65±8.2 years) with bilateral subthalamic nucleus‐DBS that underwent eye‐tracking assessment at baseline and one year follow‐up, both with DBS on‐ and off‐state. Number of SI, velocity, latency and gain of PS and AS, and AS errors/corrected errors were analysed.
Results: At baseline, when compared to off‐state, DBS significantly decreased SI number, increased the gain/velocity of correct horizontal/vertical AS and the gain of corrected horizontal/vertical errors, while decreasing the latency of incorrect vertical AS. At one year follow‐up, DBS increased the gain of horizontal PS, the gain/velocity of correct horizontal/vertical AS and the gain of corrected horizontal/vertical errors, while decreasing the latency of correct/incorrect vertical AS. Saccadic parameters remained unchanged in off‐state after one year and there was no interaction between DBS status and time of assessment.
Conclusion: DBS significantly improves fixation instability, speeds up and widens predominantly voluntary eye movements in PD patients, in addition to accelerate their start strictly along the vertical plane. Remarkably, these effects are sustained over time. This data highlights the overlooked benefit of DBS on vision of PD patients.
Disclosure: Nothing to disclose.
Movement disorders 4
EPO‐354
HeBA‐online Parkinson disease risk factors survey diffusion: Digital versus traditional approaches
D. Pilco‐Janeta 1; A. Garrido2; M. De la Cruz‐Puebla1; F. Farfán Alé1; A. Granolles3; S. Hajiantilaki1; Y. Rodríguez1; E. Tolosa2; M. Martí2
1Institut d’Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Barcelona, Catalonia; 2Parkinson Disease and Movement Disorders Unit, Neurology Service, Institut Clínic de Neurociències, Hospital Clínic de Barcelona, Barcelona, Catalonia; 3Altoclick Digital Marketing Agency, Barcelona, Catalonia, Spain
Background and Aims: The Healthy Brain Ageing (HeBA) is a European multicenter project using innovative approaches for early detection and intervention in Parkinson's disease. In the first phase, the project aims to gather comprehensive data through online surveys. This study specifically focuses on evaluating and comparing the effectiveness of various dissemination strategies, particularly digital platforms like META's platforms and Google Ads against traditional media in collecting data from Catalonia's population.
Methods: We gathered data from META campaigns (Facebook, Instagram), Google Ads, and traditional media (radio, press, online press, and television). Analyzed metrics included clicks for HeBA online survey in META and Google, along with audience size for traditional media. Quantitative analysis assessed campaign clicks, and audience engagement trends.
Results: In the context of HeBA diffusion strategies, digital dissemination methods, such as META campaigns, achieved a total of 102,248 clicks (Figure 1A). For Google Ads campaigns, there were a total of 2,089 clicks to the HeBA survey (Figure 1B). Notably, our traditional media campaigns reached an impressive overall audience of approximately 97,432,694. Newspapers emerged as the medium with the highest reach (Figure 1C). Additionally, in the HeBa survey response distribution, we obtained 6,943 complete responses and 6,749 partial responses out of a total of 13,692 responses collected between June 13, 2022, and January 15, 2024 (Figure 1D).
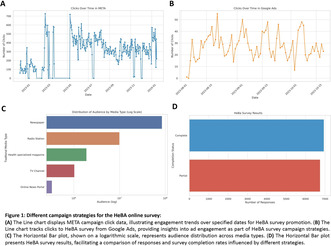
FIGURE 1 Different campaign strategies for the HeBA online survey.
Conclusion: The HeBA Project's media strategy effectively merges the broad audience reach of traditional media with the targeted engagement of digital platforms, providing a valuable blueprint for future health communication campaigns.
Disclosure: Nothing to disclose.
EPO‐355
Clinical features and outcomes of neuroacanthocytosis: A single center experience
Z. Huseynli; B. Samanci; E. Sahin; S. Yusifli; B. Bilgic; H. Hanagası
Neurology, Istanbul Unıversity, Topkapı, Istanbul, Turkey
Background and Aims: Neuroacanthocytosis (NA) is a rare disorder with multisystem involvement, and characterized by progressive basal ganglia degeneration. We aimed to report clinical characteristics and outcomes of NA patients in a Turkish cohort.
Methods: Eleven patients with NA diagnosis of our database were included. Clinical characteristics, laboratory and MRI examinations were recorded.
Results: The mean age of the patients (5 male, 6 female) was 39.5±3.65 years, with symptom onset at 29±4.86 years. Mean follow‐up duration was 3.9±2.1 years. Psychiatric symptoms (n = 4), tics (n = 3), dystonia (n = 2), chorea (n = 1), seizure (n = 1) were noted as first symptoms. Self‐mutilation were observed in 5 patients. In the follow up, vocal (n = 5) and motor tics (n = 3), choreiform movements (n = 11), dystonia (n = 6), dysarthria (n = 11), dysphagia (n = 11), weight loss (n = 11), psychiatric issues (n = 7) were observed. Seizures occurred in 10, with 4 focal and 6 generalized. Acanthocytes ratio were seen in 10‐50% of blood smears. MRI revealed caudate in all, and parietal atrophy in 2 patients. Three patients had sensory neuropathy, 1 had motor neuropathy, and 2 showed myogenic changes in EMG. VPS13A mutation was detected in 4 patients for whom molecular analysis was available. Six started on olanzapine, five on haloperidol, and two underwent deep brain stimulation for severe dystonia. Significant worsening of involuntary movements and dysphagia was observed in all patients during follow‐up, and three patients died after 11±2.82 years follow‐up.
Conclusion: It is crucial to assess patients showing multisystem involvement such as early psychiatric issues, self‐mutilation, movement disorders, acanthocytosis, and caudate atrophy for an accurate NA diagnosis.
Disclosure: The authors affirm that there are no conflicts of interest pertinent to this study.
EPO‐356
Experience with safinamide in Parkinson's disease patients after STN‐DBS
K. Del Giudice; J. Bejarano; F. Valldeoriola; A. Sanchez
Institute of Neuroscience, Neurology Service, Parkinson's Disease and Movement disorders Unit, Hospital Clinic of Barcelona
Background and Aims: Subthalamic nucleus ‐Deep Brains Stimulation (STN‐DBS) has been stablished as a well‐defined therapy for treating Parkinson's disease (PD) motor symptoms; however, some non‐motor symptoms may not respond as expected, which significantly impact on quality of life of the patients (QoL). Antiparkinsonian drugs with dopaminergic and non‐dopaminergic properties like “safinamide” have been suggested to have a positive effect on non‐motor symptoms. The aim of this study was to investigate the efficacy of safinamide to improve apathy, fatigue and QoL in PD patients after STN‐DBS.
Methods: We studied prospectively 13 PD patients that presented bothersome nonmotor symptoms after intensive setting of electrical parameters, stimulation contacts and optimal drug therapy. Patients were evaluated 32 week after 100mg of safinamide was started. Clinical assessment included Apathy Scale Starktein (AS), Parkinson Fatigue scale‐16 (PFS‐16) and Parkinson´s Disease Quality of life questionnaire ‐8 (PDQ‐8).
Results: Thirteen PD patients were analyzed. The median age was 59 years old, with a median disease duration of 10 years at surgery. All patients were H&Y 2 in the ON state, and median of 400 levodopa equivalent daily dose. An improvement of 58.3% on the AS, 38% on the PFS‐16 and 41.6% on the PDQ‐8 was observed.
Conclusion: In this pilot study, safinamide proved to be an effective add‐on treatment in PD patients treated with bilateral STN‐DBS, leading to an improvement of non‐motor complications, such as apathy, fatigue and QoL. Further studies with a higher number of patients are necessary to establish the value of this drug in the clinical practice.
Disclosure: Nothing to disclose.
EPO‐357
Clinicians' information provision during diagnostic consultations regarding Parkinson's disease
E. Kurpershoek 1; M. Hillen2; R. de Bie1; J. Dijk1
1Department of Neurology, Amsterdam UMC, Amsterdam, The Netherlands; 2Department of Medical Psychology, Amsterdam UMC, Amsterdam, The Netherlands
Background and Aims: People with Parkinson's disease (PD) have reported feeling insufficiently informed by clinicians during diagnostic consultations, which might hinder patients’ ability to manage their day‐to‐day lives. We aimed to (1) assess the amount and content of provided information during diagnostic consultations; and to test if the provided information is associated with (2) patients’ evaluation thereof and (3) clinician and patient characteristics.
Methods: This observational longitudinal study video recorded diagnostic consultations of PD patients at seven neurology outpatient clinics in The Netherlands. We systematically coded the recordings for time spent on pre‐defined information topics. Clinician and patient characteristics, a priori information needs, and retrospective perception and evaluation of received information were assessed using questionnaires. Analyses included descriptive statistics and regressions.
Results: Patients’ information need was high overall (M = 4.5 ± 0.8, potential range 1–5). Clinicians’ information provision varied across patients (n = 50) and clinicians (n = 37). All patients were provided with information regarding their diagnosis, treatment options, and the follow‐up plan. About half were not informed about PD being incurable (44%) and the long‐term effects of dopaminergic medication (58%). Patients reported to have perceived quite some information (M = 2.8 ± 0.9, PR 1‐5), and were quite satisfied (M = 3.4 ± 0.9, PR 1‐5). 30% reported a wish for more information, particularly regarding the prognosis. Regression analyses will be completed at the time of the conference.
Conclusion: Most clinicians mainly focus on treatment during PD diagnostic consultations, and may not sufficiently meet patients’ prognostic information needs. We recommend clinicians to actively inquire about patients’ information preferences during diagnostic consultations, and tailor their information provision accordingly.
Disclosure: Nothing to disclose.
EPO‐358
Diagnostic accuracy of Parkinson's disease by neurologists in an outpatient setting: The Parklink Bologna cohort
E. Umbertini 1; L. Vignatelli2; F. Baccari2; L. Belotti2; C. Zenesini2; R. D'Alessandro2; F. Nonino2; G. Giannini2; G. Calandra Buonaura2; G. Calandra Buonaura1
1DIBINEM Dipartimento di Scienze Biomediche e Neuromotorie; 2IRCCS Istituto delle Scienze Neurologiche di Bologna
Background and Aims: The diagnosis of Parkinson's disease (PD) is still mainly clinical and with variable accuracy in different settings. The Parklink Bologna project is an ongoing record linkage system started in 2015 in the Local Health Trust of Bologna (LHTB), devised for epidemiological and research purposes, including prevalent and incident cases of PD or atypical parkinsonism. The objective of this study is to evaluate the accuracy of the diagnosis of PD recorded by neurologists participating in the Parklink project. Interobserver agreement between two movement disorder experienced neurologists was assessed.
Methods: Diagnostic accuracy cross‐sectional study on a random sample of 220 patients representative of the ParkLink cohort. Sensitivity, specificity, positive/negative predictive value (PPV/NPV) were calculated by assuming as reference standard the blinded diagnosis of two movement disorder experienced neurologists, applying Postuma international diagnostic criteria for PD, and as index‐test the diagnosis recorded by outpatients neurologists within the ParkLink project. Interobserver agreement was assessed using Cohen's Kappa.
Results: In 193 patients (mean age 72.8 years) clinical documentation for a diagnosis was available. A sensitivity of 94.1% (95% CI: 88.7‐97.4) and specificity of 63.2% (49.3‐75.6), PPV of 85.9% (79.3‐91.1) and NPV of 75% (59.7‐86.8) were found for the first assessor. Interobserver agreement was “substantial” (Kappa 0.77, 95% CI: 0.67‐0.87) between the two experts.
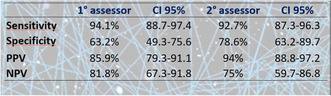
Accuracy parameters
Conclusion: Diagnosis of PD according to the 2015 Postuma criteria showed good PPV and NPV in an outpatient real‐world setting. It is possible to build reliable cohorts of people with PD for epidemiological research, based on both community neurologists and neurologists from movement disorder centres.
Disclosure: Nothing to disclose.
EPO‐359
TremAn3: A new tool for the analysis of tremor and other oscillatory movements in video recordings
E. Růžička 1; J. Tesař2; T. Serranová1; T. Hubená2; P. Hollý1; Y. Yilmaz3; A. Hollmannová1; J. Jankovic3; R. Krupička2
1Department of Neurology, Charles University and General University Hospital, Prague, Czechia; 2Department of Biomedical Informatics, Faculty of Biomedical Engineering, Czech Technical University, Prague, Czechia; 3Parkinson's Disease Center and Movement Disorders Clinic, Baylor College of Medicine, Houston, Texas
Background and Aims: Neurophysiological techniques used to quantify tremor are not readily available in clinical practice, whereas video recording is a part of routine evaluation. We describe TremAn3, a novel application that enables kinematic analysis of tremor or other rhythmic movements from standard video recordings of patients.
Methods: We analyzed video recordings of 17 patients with essential tremor (ET) and 19 patients with functional tremor (FT) diagnosed at the General University Hospital in Prague, Czechia and of 9 subjects with leg stereotypy syndrome (LSS) recruited at the Baylor College of Medicine in Houston, Texas. In the video recordings, oscillating part(s) of the body are delineated in TremAn3 as the region(s) of interest. The algorithm then calculates the center of motion (CoM) derived from the normalized frame differences and defines the motion trajectory, followed by a fast Fourier transform (FFT) generating an amplitude spectrum of oscillations.
Results: In patients with ET, analysis demonstrated stable frequency spectra with intraindividual variation below 1 Hz. In FT patients, increased intraindividual variability of tremor frequency exceeding 1 Hz was found, with marked distractibility and entrainment by contralateral rhythmic movements. Of the 9 individuals with LSS, regular rhythmic oscillations of the lower limbs were present in 7 cases, ranging between 4.5 and 6.5 Hz, with a variance below 0.5 Hz in individual cases (Yilmaz et al., manuscript in preparation).
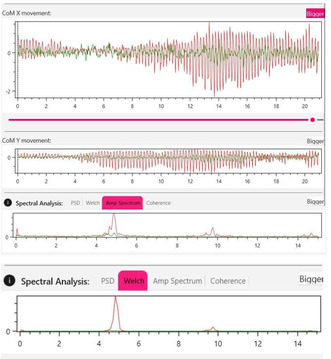
Sample output from TremAn3: video analysis of a patient with ET.
Conclusion: TremAn3 appears as a tool suitable for supporting the differential diagnosis of tremor in daily practice and to analyze video recordings obtained in large participant cohorts.
Disclosure: Nothing to disclose.
EPO‐360
Prospective study of gait and multimodal MRI biomarkers Multiple System Atrophy (MSA)
F. Marchand 1; R. Viard2; D. Devos3; L. Defebvre1; T. Ollivier1; D. Guehl4; G. Kuchcinski5; C. Moreau1
1Neurology, Movement Disorders Department and Memory Center, CHU Lille, Licend, Lille, France; Univ. Lille, INSERM, CHU Lille, U1172 – LilNCog – Lille Neurosciences & Cognition, F‐59000 Lille, France; 2Univ. Lille, INSERM, CHU Lille, U1172 – LilNCog – Lille Neurosciences & Cognition, F‐59000 Lille, France; Univ. Lille, CNRS, Inserm, CHU Lille, Institut Pasteur de Lille, US 41 – UAR 2014 – PLBS, F‐59000 Lille, France; 3Univ. Lille, INSERM, CHU Lille, U1172 – LilNCog – Lille Neurosciences & Cognition, F‐59000 Lille, France; Department of Medical pharmacology CHU Lille; 4Department of Clinical Neurophysiology, Bordeaux University Hospital, Bordeaux, France; Institute of Neurodegenerative Disorders, Bordeaux University, Bordeaux, France; 5Univ. Lille, INSERM, CHU Lille, U1172 – LilNCog – Lille Neurosciences & Cognition, F‐59000 Lille, France; Department of Neuroradiology CHU Lille
Background and Aims: MSA is a rare neurodegenerative condition characterized by a rapid gait deterioration with severe prognosis. Currently, no treatment is available to slow down disease progression. We aimed to develop new multimodal biomarkers allowing objective monitoring of early MSA progression to improve outcome definition for future neuroprotective trials.
Methods: This analysis focuses on 19 MSA patients, enrolled in the Gait’N’Park multicentric cohort (NCT04653688). Longitudinal data, including clinical scales (UMSARS), unsupervised gait analysis (at home using smart insoles), and multimodal MRI data (volumetric, R2*, QSM for iron load, and DTI for microstructural alterations), were collected at baseline (W0) and 24 weeks (W24).
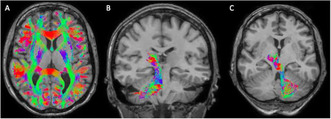
Tractography: (A) Whole brain; (B) Substantia Nigra‐Dentate Nucleus; (C) Dentate Nucleus‐Thalamus.
Results: At W24, there was a significant increase of mean diffusivity in cerebellar white matter (pFDR = 0.029) and in fiber bundles between: Substantia Nigra and Dentate Nuclei (pFDR = 0.0013); and Dentate Nuclei and Thalamus (pFDR = 0.0013). No significant worsening was observed at W24 for other parameters, such as UMSARS, gait speed (95th centile) or stride length (mean), putamen, cerebellum or pons volume, or putamen R2* and QSM values.
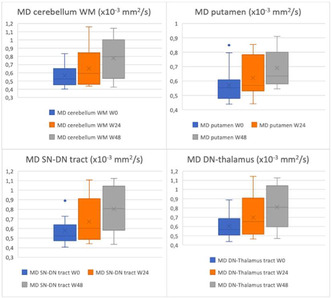
Mean diffusivity evolution along time (MD = Mean Diffusivity; WM = White Matter; SN = Substantia Nigra; DN = Dentate Nucleus).
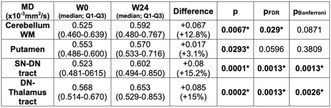
Mean diffusivity analysis at W24 vs W0 (MD = Mean Diffusivity; WM = White Matter; SN = Substantia Nigra; DN = Dentate Nucleus).
Conclusion: Our data confirm the low sensitivity to early change of UMSARS, currently use as the gold standard to monitor disease progression. Whereas diffusion imaging of white matter appears to be sensitive to change as early as 6 months of follow‐up, with high statistical significance, supporting early involvement of oligodendrocytes. This kind of biomarker should be considered to enhance outcome definition for future neuroprotection trials.
Disclosure: This study was sponsored and funded by H. Lundbeck A/S, FeetMe, France Parkinson, Vaincre Parkinson. Félix Marchand has nothing to disclose.
EPO‐361
Improvement of troublesome dyskinesia in people with Parkinson's disease treated with foslevodopa/foscarbidopa
M. Blaabjerg1; T. Liang2; E. Peckham3; S. Zauber4; L. Bergmann5; R. Gupta5; L. Harmer5; M. Shah5; F. Bergquist 6
1Department of Neurology, Odense University Hospital, Odense, Denmark; 2Department of Neurology, Thomas Jefferson University, Philadelphia, Pennsylvania, USA; 3Central Texas Neurology Consultants, Round Rock, Texas, USA; 4Department of Neurology, Indiana University School of Medicine, Indianapolis, Indiana, USA; 5AbbVie Inc., North Chicago, Illinois, USA; 6Department of Pharmacology, University of Gothenburg, Gothenburg, Sweden; Sahlgrenska University Hospital, Gothenburg, Sweden
Background and Aims: Troublesome dyskinesia, a complication from Parkinson's disease (PD) progression and pulsatile dopaminergic stimulation, impairs daily living. Foslevodopa/foscarbidopa (LDp/CDp), a formulation of levodopa/carbidopa prodrugs delivered as a continuous (24‐hour/day) subcutaneous infusion, increased “On” time without troublesome dyskinesia in 2 phase 3 clinical trials. This post hoc analysis evaluated LDp/CDp efficacy by baseline duration of troublesome dyskinesia.
Methods: Patients with levodopa‐responsive idiopathic PD aged ≥30 years who were inadequately controlled by current therapy and had ≥2.5 “Off” hours/day received LDp/CDp in a 52‐week, phase 3, open‐label trial (NCT03781167). The change from baseline (CFB) to final visit was assessed for “On” time with troublesome dyskinesia (PD diary; normalized to 16‐hour waking day), time spent with dyskinesias (Movement Disorder Society‐Unified PD Rating Scale [MDS UPDRS] Part 4.1), functional impact of dyskinesias (MDS‐UPDRS Part 4.2), and 39‐item PD Questionnaire (PDQ‐39) in patient subgroups with >0.5 and >1.0 hours of troublesome dyskinesia at baseline.
Results: Baseline characteristics were similar across subgroups with >0.5 (n = 83) and >1.0 hours (n = 66) of troublesome dyskinesia at baseline; mean (SD) duration of troublesome dyskinesia was 2.7 (2.0) and 3.1 (2.0) hours, respectively (Table). In both subgroups, LDp/CDp led to numerical or significant improvements from baseline in troublesome dyskinesia (mean [SD] CFB −1.4 [3.4] and −2.5 [2.2] hours, respectively; p < 0.05; Figure1), time spent with dyskinesias (p ≤ 0.001), functional impact of dyskinesias (p ≤ 0.001), and PDQ‐39 (p < 0.05 for >0.5 hour subgroup; Figure 2).
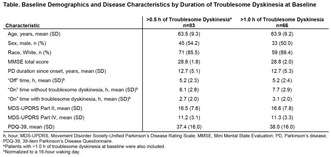
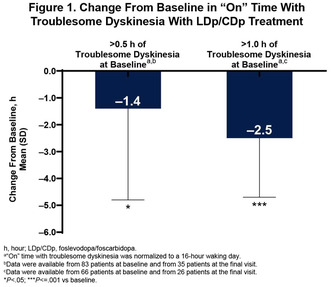
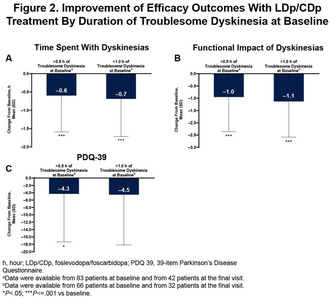
Conclusion: Continuous delivery of LDp/CDp was associated with significant improvements in dyskinesia and quality of life in patients with relevant/significant troublesome dyskinesia at baseline.
Disclosure: MB has received research funding from Aptinyx Inc. T‐WL has served as a site principal investigator for the AbbVie M15‐736 study and for the Abbott PROGRESS trial. ELP has received research and grant support from Sunovion Pharmaceuticals and has conducted prior and/or ongoing clinical trials with AbbVie, Acadia Pharmaceuticals, Cala Health, Cerevance, Cerevel, Covance, Evidera, Lilly, Lundbeck, Osmotica Pharmaceutical, Revance Therapeutics, Roche, Sunovion Pharmaceuticals, and Sun Pharma. SEZ has received research support for clinical trials from AbbVie, Abbott, and Boston Scientific. LB, RG, LH, and MS are full‐time employees of AbbVie, and may hold AbbVie stock or stock options. FB has received financial compensation for lectures and advisory services as well as in‐kind donations of PKG reports for clinical studies from GKC, and honorarium for an advisory board from AbbVie. He owns stock options in Dizlin Pharmaceuticals AB. AbbVie funded this study and participated in the study design, research, analysis, data collection, interpretation of data, reviewing, and approval of the abstract. All authors had access to relevant data and participated in the drafting, review, and approval of this abstract. No honoraria or payments were made for authorship. AbbVie and authors thank all the trial investigators and the patients who participated in this clinical trial. Medical writing support was provided by Jay Parekh, PharmD, ISMPP CMPP™, of JB Ashtin, and funded by AbbVie.
EPO‐362
Opicapone as first‐line strategy for the treatment of wearing‐off in Korean patients with Parkinson's disease
J. Lee1; J. Ferreira2; H. Ma3; J. Rocha 4; B. Jeon5
1Department of Neurology, SMG‐SNU Boramae Medical Center, Seoul, Republic of Korea; 2CNS Campus Neurológico, Torres Vedras, Portugal and IMM – Instituto de Medicina Molecular João Lobo Antunes, Faculdade de Medicina, Universidade Lisboa, Lisbon, Portugal; 3Department of Neurology, Hallym University Sacred Heart Hospital, Anyang, Republic of Korea; 4BIAL–Portela & Ca S.A, Coronado, Portugal; 5Department of Neurology, Seoul National University Hospital, Seoul, Republic of Korea
Background and Aims: Opicapone (OPC) proved effective for end‐of‐dose motor fluctuations in patients with Parkinson's disease (PD) treated with levodopa (L‐dopa)/dopa decarboxylase inhibitor (DDCi). This study aimed to explore the efficacy of OPC 50 mg versus an extra 100 mg L‐dopa dose to treat early wearing‐off in Korean patients with PD.
Methods: This was a prospective, multicentre, randomised, active‐controlled study in which 169 levodopa‐treated patients with PD and wearing‐off were randomly assigned (1:1) to OPC 50 mg once‐daily (n = 88) or an additional 100 mg L‐dopa dose (n = 81). A 1‐week screening period was followed by a 4‐week maintenance phase. Main endpoint was change from baseline in absolute OFF‐time. Secondary endpoints included tolerability, Movement Disorder Society‐Unified‐PD‐Rating‐Scale (MDS‐UPDRS), 8‐item PD Questionnaire (PDQ‐8), Clinical Global Impression of Improvement (CGI‐I), and Patient Global Impression of Change (PGI‐C).
Results: At week 4, mean (standard error [SE]) change from baseline in absolute OFF‐time was ‐62.1 min (9.8) for the OPC 50 mg group and ‐16.7 min (10.0) for the L‐dopa 100 mg group, resulting in a significant difference of ‐45.4 min (p = 0.0015). No significant differences were observed in MDS‐UPDRS and PDQ‐8 scores between the two groups. The OPC group tended to show greater improvements on CGI‐I/PGI‐C than the L‐dopa group. OPC was well tolerated, but adverse events (AEs) were more frequent in the OPC than the L‐dopa group (37.9% vs 18.5%), with dyskinesia (6.9%) being the most common drug‐related AE.
Conclusion: OPC can be considered a potential first‐line therapy to treat early wearing‐off versus the standard L‐dopa dose increase approach.
Disclosure: Supported by BIAL.
EPO‐363
Early‐onset Parkinson's disease in women: A comparison of hormonal exposure with late‐onset PD and unaffected controls
G. Patanè 1; A. Mullan2; C. Piat1; P. Turcano1; R. Savica1
1Mayo Clinic Department of Neurology, Rochester, Minnesota, USA; 2Mayo Clinic Department of Health Sciences Research, Rochester, Minnesota, USA
Background and Aims: PD is almost twice as common in men than in women. There is a paucity of studies evaluating the role of hormonal exposure in EOPD women. The objective was to compare the demographic characteristics and exposure to endogenous, exogenous estrogens and progestins between patients with EOPD, LOPD, and EOPD‐matched unaffected controls.
Methods: We identified all female patients with EOPD in an incident cohort study from 1991 to 2010. EOPD patients were defined as having motor symptoms onset before age 50, after age 50 as LOPD. Each EOPD patient was matched to an unaffected control. Their medical records were reviewed to determine demographic characteristics, medical, reproductive, and menopausal history.
Results: 318 women with EOPD and 170 women with LOPD were identified. Of these, 87 EOPD patients, 91 controls, and 84 LOPD patients had sufficient hormonal exposure data in their records to be included. There were no significant differences in demographic characteristics between the three groups. EOPD patients were significantly more likely to have used hormonal contraception compared to controls and LOPD patients (p < 0.001). The number of pelvic surgeries and the use of perimenopausal hormonal therapy preceding the onset of motor symptoms (both p < 0.001) was significantly higher in LOPD compared to EOPD.
Conclusion: Our study reports that there are no significant differences in hormonal exposure between controls and EOPD patients, except for exposure to hormonal contraception. The differences in the history of hormonal contraception, oophorectomy and perimenopausal treatment between EOPD and LOPD are probably linked to the age gap between the two cohorts.
Disclosure: Nothing to disclose.
EPO‐364
Dopaminergic medication and STN‐DBS increase motor, but not reflection and cognitive impulsivity in PD
M. Hendriks1; S. Vinke2; R. Berlot1; M. Benedičič3; M. Jahanshahi4; M. Trošt1; D. Georgiev 1
1Department of Neurology, University Medical Centre Ljubljana, Ljubljana, Slovenia; 2Department of Neurosurgery, Donders Institute for Brain, Cognition and Behaviour, Radboud University Medical Centre, Nijmegen, The Netherlands; 3Department of Neurosurgery, University Medical Centre Ljubljana, Ljubljana, Slovenia; 4Department Clinical and Motor Neurosciences, Institute of Neurology, University College London, London, UK
Background and Aims: Parkinson's disease is associated with increased impulsivity, which can be divided into several domains: motor (consisting of proactive and reactive subdomains), reflection and cognitive impulsivity. Evidence suggests that both dopaminergic medication and subthalamic nucleus deep brain stimulation can affect impulsivity. Therefore, we set out to investigate the effect of dopaminergic medication and subthalamic nucleus deep brain stimulation on motor, reflection and cognitive impulsivity in PD patients.
Methods: Twenty consecutive Parkinson's disease patients operated with subthalamic nucleus deep brain stimulation were tested ON and OFF dopaminergic medication and ON and OFF subthalamic nucleus deep brain stimulation. They performed three different impulsivity tasks: AX Continuing Performance Task to test for motor impulsivity, Beads Task for reflection impulsivity and Delay Discounting Task for cognitive impulsivity.
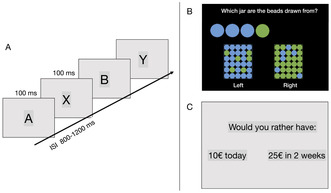
A ‐ AX continuous performance task, B ‐ Beads task, C ‐ Delay discounting task. ISI = Interstimulus interval.
Results: The combination of subthalamic nucleus deep brain stimulation and dopaminergic medication led to an increase in motor impulsivity (p = 0.036), both proactive (p = 0.045) and reactive (p = 0.006). There was no effect of either dopaminergic medication or subthalamic nucleus deep brain stimulation on reflection and cognitive impulsivity.
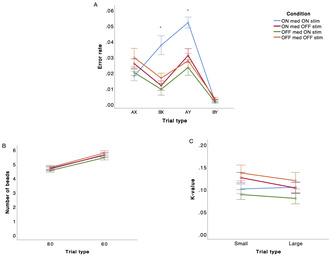
FIGURE 2 The performance on different tasks (A ‐ AX‐CPT, B‐ Beads task, C ‐ Delay Discounting Task) in STN‐DBS PD patients in four different conditions are presented.
Conclusion: The combination of dopaminergic medication and subthalamic nucleus deep brain stimulation leads to increased motor, but not cognitive or reflection impulsivity in patients with Parkinson's disease. Both, proactive and reactive motor impulsivity were impaired by the combination of dopaminergic medication and subthalamic nucleus deep brain stimulation.
Disclosure: Nothing to disclose.
EPO‐365
Gender differences in patients with Parkinson's disease treated with STN or GPi DBS: Results from a single center
G. Belluscio 1; S. Malaspina1; M. Avenali1; G. Cosentino2; C. Pacchetti3; R. Zangaglia3; F. Valentino3
1Parkinson's Disease and Movement Disorders Unit, IRCCS Mondino Foundation, Pavia, Italy; Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; 2Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; Translational Neurophysiology Research Unit, IRCCS Mondino Foundation, Pavia, Italy; 3Parkinson's Disease and Movement Disorders Unit, IRCCS Mondino Foundation, Pavia, Italy
Background and Aims: We investigated gender‐differences in response to DBS of the STN or GPi in a group of patients with advanced PD
Methods: 123 patients with PD (30% F, 70% M) and DBS targeting the STN (93 patients, 32.2 % females) or GPi (30 patients, 23.3% females) were enrolled. At baseline, MDS‐UPDRS part III was collected in both OFF and ON state; at 1 year follow up, it was assessed in the ON state with the stimulator turned on. Dopaminergic therapy was converted in Levodopa Equivalent Daily Dose (LEDD)
Results: At baseline, there were no gender differences as regards disease duration, LEDD and MDS‐UPDRS part III score. At 1‐year follow‐up, we found reduced MDS‐UPDRS III scores for both GPi‐ and STN‐DBS and a significant LEDD reduction compared to baseline only after STN‐DBS (p = 0.0001), with no gender‐specific differences. The percentage of patients with dyskinesias decreased from 86% to 20% in females and from 91% to 50% in males after GPi‐DBS. After STN‐DBS the decrease was from 93.3% to 66% in females, and from 73% to 34% in males. The percentage of patients with clinical fluctuations decreased from 86% to 14% in females and from 39% to 13% in males after GPi‐DBS, while after STN‐DBS the decrease was from 56.6% to 27% in females, and from 44% to 28% in males. Overall, the effect of sex was not statistically significant
Conclusion: Bilateral STN‐ and GPi‐DBS are equally effective in males and females as a treatment for motor complications of PD
Disclosure: Nothing to disclose.
EPO‐366
Mapping cortical nodes for targeted neuromodulation in focal dystonia: A TMS‐EEG study
G. Leodori1; M. Mancuso 1; M. Costanzo2; F. Marchet2; S. Pellegrini2; C. Santellani2; G. Ferrazzano2; D. Belvisi1; A. Berardelli1; G. Fabbrini1; A. Conte1
1Department of Human Neurosciences, Sapienza University of Rome, Rome, Italy; IRCCS Neuromed, Pozzilli, Italy; 2Department of Human Neurosciences, Sapienza University of Rome, Rome, Italy
Background and Aims: Focal dystonia (FD) manifests as involuntary movements and abnormal postures in specific body regions, often with non‐motor symptoms, due to brain network dysfunctions. Our objective is the therapeutic modulation of these networks using non‐invasive brain stimulation. We present preliminary Transcranial Magnetic Stimulation‐Electroencephalography (TMS‐EEG) findings that identify dysfunctional cortical nodes in motor and non‐motor networks of cervical dystonia (CD) patients. Pinpointing these nodes is vital for developing targeted neuromodulatory strategies.
Methods: Eighteen CD patients and 15 healthy subjects (HS) were evaluated using TMS‐EEG to record TMS‐evoked potentials (TEPs) from the primary motor cortex (M1), supplementary motor area (SMA), and dorsolateral prefrontal cortex (DLPFC), key nodes involved in the pathophysiology of motor and non‐motor symptoms in CD. The Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS) was employed for clinical assessment.
Results: Preliminary findings revealed a significantly larger early local M1 TEP amplitude in CD patients versus HS. Conversely, DLPFC showed a non‐significant trend toward reduced early local TEP amplitude in CD patients. SMA TEPs did not differ significantly between groups. No significant correlations were found between TEP amplitudes and TWSTRS scores.
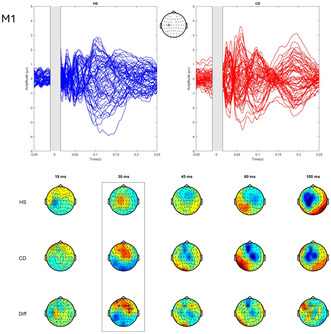
Butterfly plots (top) and topoplots (bottom) of TEPs from M1 stimulation in cervical dystonia (CD) compared to healthy subjects (HS). Top: Stimulation site marked by an asterisk. Bottom: Asterisks highlight significant electrodes in CD vs HS.
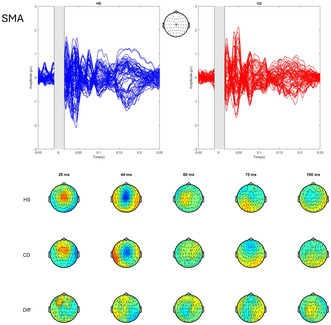
Butterfly plots (top) and topoplots (bottom) of TEPs from SMA stimulation in cervical dystonia (CD) compared to healthy subjects (HS). Top: Stimulation site marked by an asterisk.
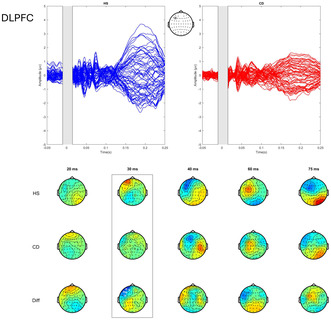
Butterfly plots (top) and topoplots (bottom) of TEPs from DLPFC stimulation in cervical dystonia (CD) compared to healthy subjects (HS). Top: Stimulation site marked by an asterisk. Bottom: Asterisks mark electrodes with a trend towards significant comparison.
Conclusion: Identifying dysfunctions in specific cortical nodes within CD patients' motor and frontoparietal networks lays the groundwork for developing neuromodulation strategies aimed at symptom relief. This study is ongoing, and it includes data collection from other pathophysiologically relevant areas in various forms of FD, and correlations with an extensive array of clinical parameters.
Disclosure: Nothing to disclose.
EPO‐367
Abstract withdrawn
EPO‐368
Olfactory and gustatory function is associated with global cognition in early‐stage Parkinson's disease
H. Ma 1; Y. Kim1; J. Baik2
1Neurology, Sacred Heart Hospital Hallym University; 2Neurology, Sanggye Baik hospital, Seoul, Republic of Korea
Background and Aims: Hyposmia and hypogeusia is a prevalent non‐motor symptom of Parkinson's disease (PD). Although there have been reports linking hyposmia to the development of dementia in PD, the association between cognitive and olfactory and gustatory function remains largely unexplored. This study evaluate the olfactory, gustatory function in early‐stage of PD patients without dementia.
Methods: This study included drug‐naive early PD patients with normal cognition (PD‐NC) or mild cognitive impairment (PD‐MCI). Olfactory function was evaluated using the YSK olfactory function test, which consisted of threshold, discrimination, and identification. The gustatory function was assessed using the YSK function test, which measures thresholds for the sweet, bitter, salty, sour, and umami tastes.
Results: Among the 84 individuals with PD, the average value of the olfactory function test fell within the hyposmia range, while taste function remained within the normal range. The study encompassed 39 patients with PD‐NC and 45 with PD‐MCI. Notably, no significant disparities were identified in olfactory and gustatory function tests between the two groups, with this trend persisting across the subdomains of each respective test. The result indicated a direct correlation between diminished global cognition (Montreal Cognitive Assessment scores) and decreased performance in both odor discrimination and gustatory function in all patients with early PD.
Conclusion: This study demonstrates that olfactory and gustatory function was associated with global cognition in the early stages of PD without dementia. Further study is warranted to ascertain whether early olfactory or gustatory dysfunction in PD could serve as an indicator for future dementia development.
Disclosure: None.
MS and related disorders 3
EPO‐369
Intrathecal synthesis biomarkers in late‐onset multiple sclerosis: Any difference from adult‐onset cases?
V. Ciampana 1; E. Virgilio2; L. Paciolla1; A. Bianchi1; P. Naldi1; M. Capobianco2; D. Vecchio1; R. Cantello1; C. Comi3
1Department of Neurology, University of Piemonte Orientale, Maggiore della Carità University‐Hospital, Novara, Italy; 2Department of Neurology, Santa Croce e Carle Hospital, Cuneo, Italy; 3Department of Neurology, Sant'Andrea Hospital, University of Piemonte Orientale, Vercelli, Italy
Background and Aims: The clinical and radiological features of Late‐Onset Multiple Sclerosis (LOMS), characterized by onset after the age of 50, have been recently described, while limited data are available about fluid biomarkers. This multicenter retrospective study aims to compare intrathecal synthesis index markers between LOMS and Adult‐Onset MS (AOMS).
Methods: A total of 152 patients (LOMS n = 39, AOMS n = 113) undergoing lumbar puncture for MS‐diagnosis were included. We confirmed homogeneity between the groups, except for age, using Pearson's chi‐square analysis. We collected Cerebrospinal Fluid (CSF) biomarkers, including kappa‐free light chains to calculate K‐index, immunoglobulin‐G for Link‐index, and Oligoclonal Bands (OB). Median (IQR) differences were analyzed using Mann‐Whitney analysis (normality excluded with Shapiro‐Wilk test).
Results: Among clinical variables (gender, EDSS, brain and spinal lesion load, type of onset, autoimmune comorbidities), only mean age at onset differed between the groups (LOMS: 55.9±5.4; AOMS: 31.3±8.0). The OB‐positivity was similar in LOMS and AOMS (82% vs. 93%), whereas we observed significantly lower values of intrathecal synthesis indexes in LOMS, with median K‐index at 18.95 (32.35) and median Link‐index at 0.5 (0.28), compared to AOMS, with 32.60 (67.44; p = 0.008) and 0.6 (0.3; p = 0.001). No other significant differences were found in CSF proteins.
Conclusion: LOMS exhibits lower values of the intrathecal synthesis markers, both K‐index and Link‐index, whereas they do not differ in OB status. These results may reflect a less pronounced inflammatory component in LOMS. Quantitative markers of intrathecal synthesis may help in understanding pathological differences for LOMS, with future potential therapeutic implications. Larger cohort confirmation is needed.
Disclosure: Nothing to disclose.
EPO‐370
Ten years of Kappa Index: Revision of intrathecal synthesis biomarkers in multiple sclerosis on a cohort of 1,000 cases
D. Vecchio1; C. Puricelli 2; E. Virgilio1; G. Bellomo2; I. Crespi2; P. Naldi1; R. Cantello1; C. Comi1; U. Dianzani2
1Neurology Unit, Department of Translational Medicine, Maggiore della Carità University Hospital, Novara, Italy; 2Clinical Biochemistry Laboratory, Department of Health Sciences, Maggiore della Carità University Hospital, Novara, Italy
Background and Aims: Cerebrospinal fluid (CSF) kappa free light chains (KFLC) are becoming a diagnostic biomarker for multiple sclerosis (MS). We aimed to compare the diagnostic performances of intrathecal synthesis biomarkers to that of oligoclonal bands (OB) in diagnosing MS, radiological and clinical isolated syndromes (RIS‐CIS) on a large cohort of patients collected over 10 years.
Methods: We collected 1057 patients (59% females) in 10 years, who underwent CSF analysis for intrathecal synthesis in the diagnostic work‐up, and they were classified according to their diagnosis as: 395 MS, 260 with other neurological inflammatory (including 76 RIS‐CIS), and 402 non‐inflammatory diseases (excluding lymphoproliferative and infective diagnosis).
Results: MS patients significantly differ from all other groups (including if considering the RIS‐CIS cohort) for: CSF KFLC, KFLC intrathecal fraction, Kappa index, and OB. Evaluating diagnostic performance, the Kappa index cut‐off was 5.6 for the diagnosis of MS, and 5.7 in predicting OB (that showed the best diagnostic accuracy).
Conclusion: The KFLC index confirmed the accuracy in MS diagnosis in this large Italian cohort, adding information also in the RIS‐CIS population.
Disclosure: None.
EPO‐371
Reassessing Balo's concentric sclerosis: Diverse clinical presentations and therapeutic implications
A. Kalfat; R. Zouari; A. Rachdi; D. Ben Mohamed; Z. Saied; F. Nabli; S. Ben Sassi
Neurology Department, National Institute Mongi Ben Hamida of Neurology, Tunis, Tunisia
Background and Aims: Balo's concentric sclerosis (BCS) represents a rare variant of multiple sclerosis (MS), characterized by concentric lamellae of alternating demyelinated and partially myelinated tissues. Historically considered to have a severe and often fatal course, recent imaging studies have identified cases with a more benign evolution.
Methods: This descriptive retrospective study involved seven BCS patients from the neurology department at the National Institute Mongi Ben Hamida of Neurology. Demographic, clinical and paraclinical data were analyzed.
Results: At diagnosis, the average age was 31.71 years [18; 47], with a sex ratio of 2:5. Inaugural relapses included motor (n = 4), visual (n = 1), multifocal (n = 1) presentations, and focal seizures (n = 1). The initial Expanded Disability Status Scale (EDSS) averaged 2 [1; 4], reaching a maximum of 5.5 during relapse. Imaging revealed a single concentric Balo lesion in most of the cases and multiple Balo lesions in one case, the majority exhibiting contrast enhancement (n = 6). All cases presented associated lesions in typical MS areas. Treatment outcomes showed that most patients responded well to corticosteroid therapy (n = 6). One patient with corticosteroid‐resistant optic neuritis underwent plasmapheresis with a poor outcome. First‐line treatment was initiated for two patients, with an indication for escalation after four years in one case.
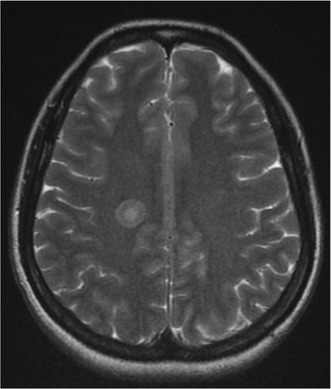
Right periventricular hyperintense signal on T2‐weighted sequence showing concentric layering.
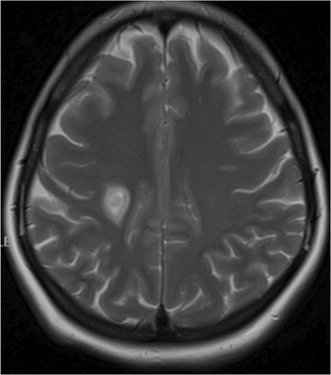
Hyperintense signal on T2‐weighted sequence in the right annular semi‐oval center showing typical ‘onion‐like’ appearance.
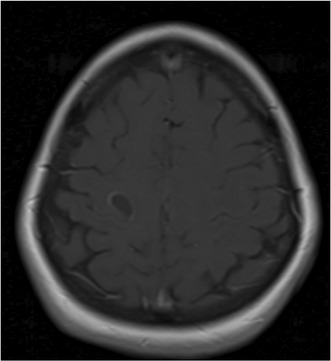
Peripheral incomplete ring enhancement on T1 post contrast (gadolinium).
Conclusion: This study challenges the historical perspective on BCS, emphasizing the need for ongoing research to refine its clinical course and treatment. For cases meeting MS diagnostic criteria, first‐line therapy is recommended, while immunosuppressive treatment may be considered for more severe progression.
Disclosure: Nothing to disclose.
EPO‐372
Analysing B‐cell depletion kinetics and clinical outcomes of ocrelizumab and rituximab in multiple sclerosis
A. Roldão Alferes 1; I. Correia1; C. Cecília Nunes1; C. Macário1; A. Paiva2; S. Batista1
1Neurology Department, Coimbra Hospital and University Centre (CHUC), Coimbra, Portugal; 2Operational Management Unit of Cytometry, Clinical Pathology Department, Coimbra Hospital and University Centre (CHUC), Coimbra, Portugal
Background and Aims: Rituximab and ocrelizumab deplete B‐lymphocytes from the pre‐B stage to the mature B stage and are used for multiple sclerosis (MS) treatment. This study aims to compare their effects on overall lymphocyte levels and subpopulations over 12 months in MS patients and explore possible clinical correlates.
Methods: We included 107 patients with MS, treated with rituximab (n = 84) or ocrelizumab (n = 23). We used flow cytometry in the peripheral blood to count total lymphocytes and B‐lymphocytes subpopulations, before treatment and after 6 and 12 months.
Results: After 6 and 12 months, patients treated with Rituximab and Ocrelizumab were similar in total B‐cell count and in B‐cell subpopulations except for Naïve B‐cells at 6 months (p < 0.001) and at 12 months (p = 0.001) and Memory B‐cells at 12 months (p = 0.002). Regarding EDSS progression, relapse occurrence and treatment discontinuation rate, no significant differences between the two treatment groups were found. In the whole sample, total B‐cell count after 12 months of treatment was significantly lower in patients with treatment discontinuation due to infectious complications (p = 0.024) and with EDSS progression (p = 0.014). Naïve and Immature B‐cells counts after 12 months were also significantly lower in patients with EDSS progression (p = 0.014 and p = 0.006 respectively).
Conclusion: Both anti‐CD20 treatments equally decreased total B‐cell counts in the peripheral blood. No between‐treatment difference in clinical outcomes was found. B‐cell subpopulation counts may be used as predictors of disability progression and infectious adverse events.
Disclosure: Nothing to disclose.
EPO‐373
Multiple Sclerosis Implementation Network: A patient‐engaged practiced based research network to improve patient care
A. Montague 1; L. Freeman2; J. Freeman3; M. Fernandez4
1Multiple Sclerosis Association of America, Cherry Hill, NJ, USA; 2Dell Medical School, The University of Texas at Austin, Austin, TX, USA; 3Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA; 4UTHealth Houston Institute for Implementation Science, University of Texas Health Science Center at Houston, Houston, TX, USA
Background and Aims: The Multiple Sclerosis Implementation Network (MSIN) is a patient‐centric collaboration between MS providers, patient advocacy organizations, academia, and industry, aimed at improving MS care and patient outcomes through the development of a practice‐based research network.
Methods: The goals for MSIN Phase I are to: 1) establish an MSIN governance structure; 2) develop a practice‐based research network composed of a diverse group of clinicians and practice settings providing care for people living with MS, and 3) establish a patient registry providing multilevel data enabling the assessment of both implementation and patient care outcomes across diverse clinical settings. The MSIN leadership designed and administered a survey assessing preliminary interest and capacity for joining the network. In Phase II MSIN will establish an implementation research program focused on the design and evaluation of implementation strategies to accelerate the adoption, implementation and sustainment of evidence‐based interventions to improve MS care.
Results: Led by the Multiple Sclerosis Association of America (MSAA), the MSIN governance structure includes people living with MS, the University of Texas Health Science Center at Houston, Dell Medical School at The University of Texas at Austin, and Novartis Pharmaceuticals Corporation. The initial recruitment effort includes 12 providers, with an anticipated 24 providers expected to join the network in 2024. Through coordinated data collection MSIN will enable rapid cycle implementation research a collaborative learning community.
Conclusion: MSIN will accelerate the translation of best MS practices into routine clinical care, improving the outcomes for people living with MS equitably.
Disclosure: AM: Nothing to disclose MF: Nothing to disclose LF: Has received fees for consultancy and/or advisory board participation from Bristol Myers Squibb, EMD Serono, Genetech, Horizon Therapeutics, Novartis, Sanofi, and TG Therapeutics; has received speaker fees from EMD Serono, MSAA, and Sanofi; has received honorarium for participation in educational programs from Medscape, Inc and MSAA; has received program sponsorship from EMD Serono; and grant support from EMD Serono, Genentech, NIH/NINDS, and PCORI through her institution. JF: Is an employee of Novartis Pharmaceuticals Corporation.
EPO‐374
Longitudinal changes in hippocampal subfield volumes of relapsing remitting multiple sclerosis patients
A. Caporali 1; E. Portaccio1; V. Penati1; M. Betti1; C. Ballerini1; C. Fabbiani2; E. Fainardi2; R. Bonacchi3; E. De Meo1; M. Amato1
1Department of Neurofarba, University of Florence, Florence, Italy; 2Department of Neuroradiology, Careggi, Florence, Italy; 3Department of Neuroradiology, Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: Due to the coexistence of neurogenesis and neurodegeneration, the hippocampus represents an interesting structure to analyze the interplay between these two processes in MS patients. We aimed to identify longitudinal trajectories of hippocampal subfield volume loss and its contribution to clinical disability and cognitive impairment.
Methods: We analyzed 3DT1‐weighted images from 108 early relapsing remitting MS patients at baseline and yearly for a maximum of 8 years, together with clinical and cognitive evaluation. We segmented hippocampal subfields by using Freesurfer version 7.2.0.
Results: All the hippocampal subfields showed progressive volume loss over disease course, but with different trajectories. On the right hippocampus dentate gyrus and cornus ammonis 1 (CA1) – related to neurogenesis – showed a bimodal pattern: early volume stability, then rapid volume decrease, and finally again stability. We identified an index of relative progression "gamma", considering the shared variance among hippocampal subfields. Significant associations were observed between gamma and performance at visuo‐spatial memory and attention.
Conclusion: The different pattern of progression of hippocampal subfield volume loss suggests an initial resilience of hippocampal regions related to neurogenesis, which then experience volume exhaustion after few years of disease. Gamma might become a relevant index for monitoring specific cognitive abilities.
Disclosure: Nothing to disclose.
EPO‐375
Predictors of longitudinal cognitive decline assessed using processing speed test in patients with multiple sclerosis
P. Garay Albízuri; F. Rodríguez Jorge; A. Llanes Ferrer; R. Sainz Amo; B. Martínez García; S. Sainz De La Maza; D. Pérez Gil; J. Chico García; G. García Alcántara; C. Moreno López; L. Costa‐Frossard; J. Masjuan; E. Monreal
Department of Neurology, Hospital Ramón y Cajal, Madrid, Spain
Background and Aims: Cognitive impairment is highly prevalent in multiple sclerosis (MS) with a profound impact on quality of life and socio‐economic levels. Our objective was to longitudinally evaluate predictors of deterioration in the Processing Speed Test (PST) using the CogEval® application.
Methods: A prospective single‐center study of MS patients with PST evaluations every 3‐6 months from October 2019 to May 2023. Significant deterioration in PST was defined as declines of ≥10% from the baseline value each year. Multivariate logistic regressions were performed for each year of follow‐up.
Results: Eight hundred eighty‐one patients with ≥1 year of follow‐up were included: 604 (68.6%) women, with a mean age of 45.3 (SD±11.41) years in the first test. The majority (79.8%) had relapsing‐remitting MS. Follow‐up was at least at two and three years was achieved in 455 and 65 patients, respectively. Confirmed worsening on the Expanded Disability Status Scale (EDSS), whether due to relapse or independent of it, was significantly associated with PST deterioration in all models, increasing each year: OR 1.85, 95% CI 1.03‐3.32, p = 0.04 in the first year; OR 2.01, 95% CI 1.1‐3.69, p = 0.02 in the second year; and OR 4.25, 95% CI 1.02‐17.6, p = 0.046 in the third year. Other factors were not consistently associated with cognitive deterioration in all models.
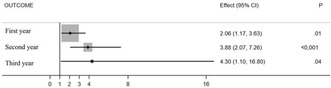
Forest plot graph to estimate the risk of annual decline in PST.
Conclusion: Cognitive impairment measured by PST in MS patients is common and is associated with worsening EDSS, regardless of clinical phenotype, disability acquisition pathways, and treatments received.
Disclosure: None.
EPO‐376
The MS‐LOTUS initiative, a digital cohort collecting real‐world evidence on multiple sclerosis relying on MSCopilot®
P. Vermersch 1; G. Comi2; L. Leocani3; L. Carment4; A. Vives4; S. Bieuvelet4; S. Zinaï4; T. Ziemssen5
1Univ. Lille, UMR Inserm U1172, CHU Lille, FHU Precise, F‐59000, Lille, France; 2Department of Neurorehabilitative Sciences, MS Centre, Casa di Cura Igea, Milan; 3Department of Neurorehabilitative Sciences, MS Centre, San Raffaele Vita‐Salute University, Department of Neurorehabilitation Sciences, Casa di Cura Igea, Milan, Italy; 4Ad Scientiam, Paris, France; 5Center of Clinical Neuroscience, Dep. Of Neurology, University Clinic Carl Gustav Carus, TU Dresden, Dresden, Germany
Background and Aims: Several pharmaceutical companies are actively developing novel treatments for multiple sclerosis (MS). However, there is still a need for a more comprehensive characterization of MS‐related disability to achieve a holistic understanding of the disease. Additionally, there are no coordinated patient registries across Europe and North America. The MS‐LOTUS cohort will gather valuable insights that will enhance patient care by harnessing the power of digital biomarkers.
Methods: MS‐LOTUS is an international, decentralised research initiative facilitating the direct enrolment of patients by their respective hospitals or private neurologists in France, Germany, Italy, Spain, Canada, amongst others. Circa 8000 participants will be recruited around the world. 300 digital biomarkers will be derived from assessments such as mobility, cognition, vision, and hand dexterity through MSCopilot®, a smartphone‐based medical device evaluating MS‐related disability. Quality of life and treatment‐related variables will be assessed using in‐app validated scales.
Results: The MS‐LOTUS study, with its innovative design, will collect data directly from the patients at home in unsupervised conditions, to complement national registries data. MS‐LOTUS will provide new information on the progression of MS and the dynamics of treatments. Healthcare providers will be able to access the data generated by the patients through a web dashboard. Agnostic MS‐LOTUS data will be published regularly, to better inform the whole MS community (learned societies, neurologists and rehabilitation specialists, pharmaceutical companies and patient associations).
Conclusion: The interest for MS‐LOTUS is strong in the community and presents a promising approach to advance our collective understanding of MS and improve patients' care pathways.
Disclosure: P. Vermersch received honorarium for contributions to meeting from Biogen, Sanofi‐Genzyme, Novartis, Teva, Merck, Roche, Imcyse, AB Science, Janssen, Ad Scientiam and BMS‐Celgene and research supports from Novartis, Sanofi‐Genzyme and Merck. G. Comi received consulting and speaking fees from Novartis, Sanofi Genzyme, Merck, Bristol‐Myers Squibb, Janssen, Rewind L. Leocani received research support from Novartis, Almirall, Biogen, Merck and consultancy or speaker fees from Novartis, Almirall, Biogen, Merck, Janssen‐Cilag, Bristol‐Myers Squibb, Roche. T. Ziemssen reports consulting or serving on speaker bureaus for Almiral, Biogen, BMS, Roche, Novartis, Sandoz, Viatris, TEVA, Merck, and Sanofi as well as research support from Biogen, Novartis, Roche, TEVA and Sanofi. L. Carment, A.Vivès, S. Bieuvelet, and S. Zinaï are employees of Ad Scientiam.
EPO‐377
Late‐onset myelin oligodendrocyte glycoprotein antibody‐associated disease: An unusual case
P. Dodu; A. Barros Ruiz; N. Ciano Petersen; I. Lopez‐Ventura Jimeno
Department of Neurology, Málaga's Regional and University Hospital, Málaga, Spain
Background and Aims: Myelin oligodendrocyte glycoprotein antibody‐associated disease (MOGAD) is an inflammatory disease of the nervous system characterized by a wide range of symptoms that vary according to age. It's usually more common in pediatric‐aged patients and young adults, although it can also debut in older patients.
Methods: We present the case of a 72‐year‐old female patient diagnosed with MOGAD, with uncommon symptoms for late‐onset patients.
Results: We have a 72‐year‐old woman who starts with acute paraparesis and is admitted for complementary tests. Brain resonance showed multiple hyperintense lesions in T2/FLAIR in periventricular white matter, subcortical, both internal capsules and bilateral temporobasal level. At the medullary level there was extensive myelitis, from T2 to L1, with areas of contrast uptake. In the cerebrospinal fluid there was proteinorrachia (48.2 mg/dL), leukocytosis (20 leu/ μL) and positivity of anti‐MOG antibodies analyzed with indirect immunofluorescence. In blood tests there was also positivity for anti‐MOG antibodies at 1/40 titer. After treatment with corticosteroids and plasmapheresis she improved, but after 2 weeks she was readmitted due to a new outbreak.
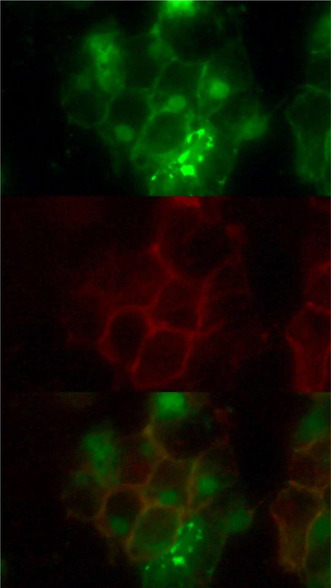
Indirect immunofluorescence in cerebrospinal fluid. Green = anti‐MOG antibodies in native form. Red = patient's antibodies. Yellow = Colocalization of the prior confirming positive to anti‐MOG antibodies.
Conclusion: According to the literature, late‐onset MOGAD is a rare condition, with a usually more subacute, monophasic clinical picture, with more cerebral symptoms, without many cases of extensive myelitis at the onset and with less inflammatory burden. The patient that we present differs greatly from what has been described so far on late‐onset MOGAD. Therefore, we consider that this diagnosis should be kept in mind in elderly patients, although it is not the most common clinical presentation.
Disclosure: Nothing to disclose.
EPO‐378
Longitudinally extensive myelitis in MS: A single centre experience
S. Othmani 1; P. Zara1; V. Floris1; S. Leoni2; P. Solla2; E. Sechi2
1Department of Medical Sciences and Public Health, University of Cagliari; 2Department of Medical Surgery and Experimental Sciences, University of Sassari, Sassari, Italy
Background and Aims: The reported frequency of longitudinally extensive myelitis lesions ‐ LEMs in MS varies, ranging from 0% to 32%. Most prior studies, however, predate the discovery of AQP4‐IgG and MOG‐IgG, potentially resulting in overestimation of LEMs. We sought to determine the frequency of LEMs at first myelitis attack in a single‐centre cohort of patients with CNS demyelinating disorders.
Methods: We retrospectively identified patients with CNS demyelinating disorders seen at the University‐Hospital of Sassari from January 1, 2017 to December 31, 2022. We included the following inclusion criteria: 1) First myelitis attack; and 2) available spinal cord MRI during the myelitis attack. The frequency of LEMs was determined and classified according to the diagnosis at last follow‐up.
Results: Among 336 patients with CNS demyelinating disorders consecutively seen over 6 years, 158 were included in the study. The frequency of LEMs in MS was 0.7% (1/138). The only MS patient with LEMs was a 55‐year‐old man who developed subacute weakness of right limbs, accompanied by numbness and gait instability. Spinal cord MRI showed a longitudinally extensive T2‐hyperintense enhancing lesion extending from C2‐D11. Brain MRI showed typical MS lesions. CSF analysis revealed moderate pleocytosis and absence of oligoclonal bands; AQP4‐IgG and MOG‐IgG were absent in both serum and CSF by live cell‐based assay.
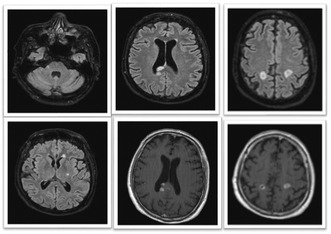
Axial T2 FLAIR brain MRI showing brainstem, periventricular and cortico‐juxtacortical white matter lesions (A‐E), some of which presents gadolinium enhancement (D,F) consistent with multiple sclerosis.

Sagittal T2‐weighted spinal cord MRI showing one short cervical lesion (A) and one longitudinally extensive lesion in the thoracic cord extending over >3 contiguous vertebral body segments (C), showing intense gadolinium enhancement in a nodular and ring.
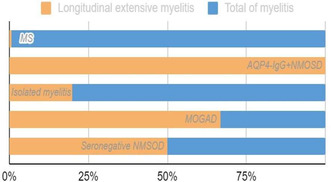
Distribution of LEM in patients with CNS demyelinating diseases with at least one episode of myelitis attack.
Conclusion: LEMs is rare among adult MS patients at first myelitis attack. Although our MS patient with LEMs met the 2017 diagnostic criteria for MS, he showed several atypical features that raise the possibility of an alternative aetiology of the myelitis.
Disclosure: No disclosures.
EPO‐379
Modified Charlson Comorbidity Index as new tool to predict prognosis in multiple sclerosis
S. Iacono; G. Schirò; P. Aridon; M. Andolina; G. Sorbello; A. Calì; M. D'Amelio; G. Salemi; P. Ragonese
Department of Biomedicine, Neuroscience and Advanced Diagnostics (BiND), University of Palermo, Italy
Background and Aims: Comorbidities have recently attracted increasing interest because of their impact in MS outcomes. The aims of this study are to predict the risk of reaching two disability milestones evaluated trough the Expanded Disability Status Scale (EDSS) and the risk of conversion from relapsing‐remitting MS to Secondary Progressive MS (SPMS) by using a modified version of the Charlson Comorbidity Index (mCCI).
Methods: comorbidity data of people included in our local MS database were extracted. The mCCI was obtained by incorporating the grade of pyramidal functional system scores into the original CCI version. The capability of mCCI at first visit to predict the reaching of EDSS 4, EDSS 6 and SPMS conversion was estimated by carrying out multivariable Cox regression models.
Results: a total of n = 622 pwMS were included (72.7% women; median age 30.8 years [24‐40]). The mCCI at first visit comprised between 1 and 2 was associated with higher risk of reaching EDSS 4 (HR = 1.53 [1.1‐2.1], p = 0.011), EDSS 6 (HR = 2.17 [1.48‐2.96], p < 0.0001) and SPMS conversion (HR = 1.57 [1.16‐2.1], p = 0.003). The mCCI at first visit >3 was associated with higher risk of reaching EDSS 6 (HR = 2.34 [1.44‐3.8], p = 0.001) and SPMS conversion (HR = 2.38 [1.29‐4.01], p = 0.004).
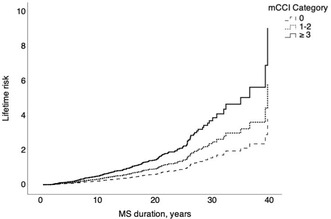
Lifetime risk of reaching the milestone EDSS 4 by mCCI categories according to MS duration on the x axis and the risk on the y axis.
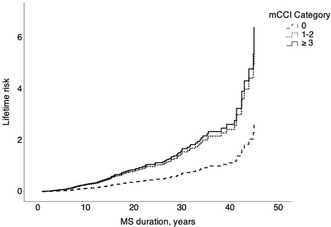
Lifetime risk of reaching the milestone EDSS 6 by mCCI categories according to MS duration on the x axis and the risk on the y axis.
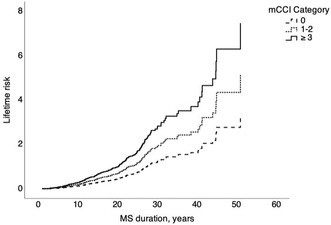
Lifetime risk of reaching the SPMS conversion according to mCCI categories according to MS duration on the x axis and the risk on the y axis.
Conclusion: comorbidity significantly affects MS prognosis as well as patient's age and motor impairment. In this study, the mCCI calculated at first visit appeared a simple and faster tool to predict MS prognosis by estimating the risk of disability worsening and SPMS conversion.
Disclosure: Nothing to disclose.
EPO‐380
The first study of real‐world efficacy and safety of Natalizumab (Tysabri) in Iran
M. Shahrbaf1; M. Samimi1; S. Karimi1; Salari2; M. Ghaffari3; S. Yazdanbakhsh4; M. Vosough1; S. Nabavi 1; A. Najafian4
1Department of Regenerative Medicine, Cell Science Research Center, Royan Institute for Stem Cell Biology and Technology; 2Neurofunctional Research Center, School of Medicine, Shahid Beheshti University of Medical Sciences; 3Neurology Department, Shahid Beheshti University of Medical Sciences; 4Department of Neurology, Tehran University
Background and Aims: This study was aimed to evaluate the real‐world effectiveness of Natalizumab in a referral center in Tehran, Iran. This study is the first real world analysis of efficacy and safety of Natalizumab in our country.
Methods: In this retrospective study, patients with RRMS were investigated in a high‐volume center in Tehran from 2019 to 2021. MS patients under treatment with Natalizumab who have received at least 3 infusions of the drug and had completed follow‐up data, have been evaluated for safety and efficacy of Natalizumab.
Results: 100 patients were included in the final analysis. The mean follow‐up time was 20 months (6‐33 months). The median EDSS score [1] of patients reached to 2 from 2.5 after the treatment course (p < 0.0001). The annualized relapse rate (ARR) decreased from 0.81 (95% CI: 0.73‐0.87) to 0.023 (95% CI 0.009 – 0.061). The median JCV index [2] remained unchanged before treatment 0.85 (IQR: 0.21‐2.41) compare to after the treatment 0.85 (IQR: 0.21‐2.31). The number of patients with active brain and cervical MRI lesions decreased significantly (p = 0.001). NEDA‐3 (No evidence of disease activity) was improved from 9% to 87% after the treatment with Natalizumab. No serious adverse events except than one progressive multifocal encephalopathy (PML) case have been found.
Conclusion: Natalizumab is a safe and effective choice in RRMS patients for reducing relapse rate, disability score, active MRI lesion, and improving the NEDA.
Disclosure: Nothing to disclose.
EPO‐381
Treatment failure rates in patients with neuromyelitis optica spectrum disorder included in an Argentinean registry
V. Tkachuk 1; E. Carnero Contentti2; P. López2; L. Patrucco3; J. Miguez4; S. Liwacki5; C. Vrech6; N. Deri7; J. Correale8; M. Ysrraelit8; F. Leguizamon9; G. Luetic10; M. Menichini11; D. Tavolini12; C. Mainella13; G. Zanga14; M. Burgos15; J. Hryb16; A. Barboza17; R. Alonso18; B. Silva18; N. Fernández Liguori19; A. Carrá20; O. Garcea18; J. Rojas21
1Neuroimmunology Hospital de Clínicas “José de San Martín”; 2Neuroimmunology Hospital Alemán; 3CEMBA Centro de Esclerosis Múltiple de Buenos Aires; 4Enfermedades desmielinizantes Hospital Italiano Buenos Aires; 5Clínica Reina Fabiola de Córdoba; 6Servicio de Neurología – Hospital Córdoba; 7Centro de Investigaciones Diabaid, CABA; 8Departamento de Neurología – FLENI, Buenos Aires; 9Hospital de Agudos, Dr. Teodoro Álvarez, Buenos Aires; 10Instituto de Neurociencias de Rosario, Santa Fe; 11Sanatorio Británico, Rosario, Santa Fe; 12INECO Neurociencias Oroño; 13Hospital Español de Rosario, Santa Fé; 14Unidad Asistencial César Milstein Buenos Aires; 15Servicio de Neurología ‐ Hospital San Bernardo, Salta; 16Servicio de Neurología ‐ Hospital Carlos G. Durand, Buenos Aires; 17Hospital Central de Mendoza; 18CUEM Ramos Mejía de Buenos Aires; 19Sanatorio Guemes de Buenos Aires; 20Hospital Británico de Buenos Aires; 21CEMIC, Buenos Aires
Background and Aims: Immunosuppressive therapies such as azathioprine (AZA), mycophenolate mofetil (MMF) and rituximab (RTX) are commonly used to prevent relapses in NMOSD. However, the response rate to these traditional therapies are unknown in Argentina. We aimed to describe and compare treatment failure rates in NMOSD (seropositive and seronegative for aquaporin‐4 antibody) patients included in the Argentinean MS and NMOSD registry (RelevarEM, NCT 03375177)
Methods: Retrospective cohort study conducted in NMOSD patients. Only who received AZA or MMF for at least 6 months or RTX for at least 1 month were included. Patients who had initially received AZA, MMF, or RTX and then switched to another 1 of these 3 therapies were included if they met the specified criteria. Data on patient demographics, clinical and neuroradiological findings, and treatments administered were collected. Treatment failure was defined as any new attack/relapse that occurred despite immunosuppressive treatment
Results: We included 139 NMOSD patients: AZA (n = 105), MMF (n = 5) or RTX (n = 29) with a mean follow‐up time of 41.3 ±11.4 months and a median EDSS at treatment initiation of 3. We observed a reduction in the annualized relapse rate from pretreatment to post treatment of 56%, 48%, and 79% respectively, with a Hazard Risk relative to RTX (95% CI) of 1.67 (1.34‐3.54, p = 0.01) for AZA and 2.01 (1.86‐4.43, p = 0.008) for MMF. AZA, MMF and RTX failure was observed in 45 (42.8%), 2 (40%) and 3 (10.3%) patients, respectively.
Conclusion: Treatment failure rates were higher for AZA and MMF than RTX in Argentinean NMOSD patients in a real‐word setting
Disclosure: Nothing to disclose.
EPO‐382
Treatment strategies for neuromyelitis optica spectrum disorder relapses: A study from a nationwide registry in Argentina
V. Tkachuk 1; E. Carnero Contentti2; P. López2; J. Miguez3; L. Patrucco4; S. Liwacki5; C. Vrech6; N. Deri7; J. Correale8; M. Ysrraelit8; F. Leguizamón9; G. Luetic10; M. Menichini11; D. Tavolini12; C. Mainella13; G. Zanga14; M. Burgos15; J. Hryb16; A. Barboza17; R. Alonso18; N. Fernandez Liguori18; D. Nadur19; J. Rojas20
1Neuroimmunology Hospital de Clínicas “José de San Martín”, Buenos Aires; 2Neuroimmunology Unit, Department of Neurosciences, Hospital Alemán, Buenos Aires; 3Enfermedades Desmielinizantes, Hospital Italiano, Buenos Aires; 4CEMBA Centro de esclerosis múltiple de Buenos Aires,; 5Clínica Universitaria Reina Fabiola, Córdoba; 6Departamento de Enfermedades desmielinizantes – Sanatorio Allende, Córdoba; 7Centro de Investigaciones Diabaid, Buenos Aires; 8Departamento de Neurología – FLENI, Buenos Aires; 9Hospital de Agudos, Dr. Teodoro Álvarez, Buenos Aires; 10Instituto de Neurociencias de Rosario, Santa Fe; 11Sanatorio Británico, Rosario, Santa Fe; 12INECO Neurociencias Oroño, Rosario, Santa Fe; 13Hospital Español de Rosario, Santa Fe; 14Unidad asistencial César Milstein, Buenos Aires; 15Servicio de Neurología – Hospital San Bernardo, Salta; 16Servicio de Neurología – Hospital Carlos G. Durand, Buenos Aires; 17Hospital Central de Mendoza; 18Sanatorio Güemes, Buenos Aires; 19Hospital Naval, Buenos Aires; 20Servicio de Neurología, Hospital Universitario de CEMIC, Buenos Aires
Background and Aims: We aimed to assess treatment strategies selected in patients with neuromyelitis optica spectrum disorder (NMOSD) experiencing relapses: frequency, types, and response after 6 months based on the Expanded Disability Status Scale (EDSS) score.
Methods: We conducted a retrospective study from the Argentinean MS and NMOSD registry (RelevarEM, NCT 03375177). We collected data: patient demographics, clinical and radiological findings, and treatments. Treatment response at 6 months was categorized as “good” if the EDSS score decreased by ≥1 point after a nadir EDSS score ≤3, or by ≥2 points after a nadir EDSS score >3, “poor” if the EDSS score decrease was slighter, and as “absent” if the EDSS score remained unchanged or worsened. We used ordinal logistic regression to identify statistical associations with the outcome
Results: We included 131 patients (120 NMOSD [seropositive N = 75 and seronegative N = 45] and 11 myelin oligodendrocyte glycoprotein‐antibody‐positive [MOGAD]), who experienced 262 NMOSD‐related relapses and received 270 treatments. Most common treatment: intravenous methylprednisolone (81.4%), followed by plasmapheresis (15.5%). At 6 months, complete recovery was achieved in 74/102 (74.5%) of the NMOSD patients. In NMOSD we did not observe differences in treatment response based on serostatus. Predictors of “good” response were: younger age at disease onset (OR: 3.54, CI95% 2.45‐5.01, p < 0.0001) and a short delay from onset of relapse to treatment initiation (OR: 1.56, CI95% 1.22‐2.13, p = 0.004)
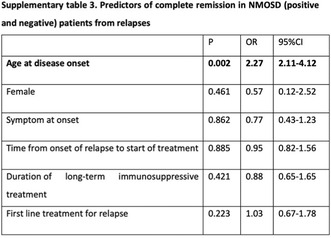
Predictors of complete remission in NMOSD (positive and negative) patients from relapses.
Conclusion: In Argentina, plasmapheresis is not commonly used to treat NMOSD relapses. Approximately two‐thirds of patients experienced complete recovery, and younger age and a short delay to start treatment were independent predictors of a “good” response.
Disclosure: Nothing to disclose.
EPO‐383
Tocilizumab treatment in naïve adult MOGAD patients: A single center experience
E. Virgilio 1; A. Dutto1; L. Giordano1; I. Pastore1; F. Franchino1; C. Fruttero2; L. Infante2; N. Fasano3; F. Venturi3; M. Capobianco1
1Neurology Unit, Department of Medicine, ASO Santa Croce e Carle, Cuneo, Italy; 2Pharmacy Unit, ASO S. Croce e Carle, Cuneo, Italy; 3Neuroradiology Unit, ASO S. Croce e Carle, Cuneo, Italy
Background and Aims: Myelin oligodendrocyte glycoprotein antibody‐associated disease (MOGAD) is a rare autoimmune oligodendrocytopathy. Differential diagnosis from multiple sclerosis (MS) and neuromyelitis optica spectrum disorder (NMOSD) is challenging, and diagnostic criteria have been recently proposed. Moreover, treatment guidelines are still lacking, and traditional MS treatments are ineffective. Several case reports have documented the efficacy and safety of tocilizumab (TCZ), a humanized antibody targeting the IL‐6 receptor, as a rescue therapy from other immunotherapies. Experience for naïve patients is otherwise lacking in adult patients.
Methods: In this single‐center case series, we report three female (mean age at diagnosis 28±10 years) adult MOGAD naïve patients treated with TCZ. MOG antibodies tested positive on serum using fixed or live cell‐based assay. Two patients presented with myelitis and one with bilateral optic neuritis (ON) (median EDSS at diagnosis 4, range 4‐9). All patients fulfilled the 2023 diagnostic criteria.
Results: All patients were initially treated with steroids. Myelitis needed plasma exchanges and immunoglobulin for short‐term worsening or relapses (one patient with extending myelitis and the other developing bilateral ON). After a mean time of 2.5 (SD1.5) months from diagnosis, TCZ 8 mg/kg every 4 weeks was started. Clinical and radiological stability was obtained for all patients (median EDSS 3.5, range 2‐9). No adverse events were recorded.
Conclusion: MOGAD is rare but highly disabling and must be treated effectively early. TCZ is reported as a useful second‐line immunotherapy in MOGAD patients. However, our observations highlight its efficacy and safety as a first‐line disease‐modifying treatment.
Disclosure: Nothing to disclose.
MS and related disorders 4
EPO‐384
Neuromyelitis Optica Spectrum Disorder (NMOSD) and effects of AQP4 status: A multicenter Turkish cohort
İ. Çalışkan1; A. Dursun2; B. Tay 2; A. Saysal3; C. Boz4; M. Terzi5; E. Toğrol6; N. Bülbül6; M. Yetkin7; N. Kale8; S. Hoca8; C. Emir9; İ. Aydın Cantürk10; A. Altıntaş11
1Department of Pathology and Laboratory Medicine, UCSF, San Francisco, United States; 2School of Medicine, Koç University, Istanbul, Turkey; 3Department of Neurology, İstanbul Bakırköy Prof. Dr. Mazhar Osman Ruh Sağlığı ve Sinir Hastalıkları Sağlık Uygulama ve Araştırma Merkezi, Istanbul, Turkey; 4Department of Neurology, Karadeniz Technical University, Trabzon, Turkey; 5Department of Neurology, Ondokuz Mayıs University, Samsun, Turkey; 6Department of Neurology, Haydarpaşa Sultan Abdülhamid Han Training and Research Hospital, Istanbul, Turkey; 7Department of Neurology, Erciyes University School of Medicine, Kayseri, Turkey; 8Department of Neurology, Istanbul Bağcılar Training and Research Hospital, Istanbul, Turkey; 9Department of Neurology, Sağlık Bilimleri University Istanbul Okmeydanı Health Application and Research Center, Istanbul, Turkey; 10Department of Neurology, Istanbul Prof. Dr. Süleyman Yalçın Göztepe City Hospital, Istanbul, Turkey; 11Department of Neurology, Koç University, Istanbul, Turkey
Background and Aims: The detection of serum immunoglobulin G (IgG) autoantibodies to aquaporin‐4 (AQP‐4) is an important diagnostic tool for Neuromyelitis Optica Spectrum Disorder (NMOSD).While the precise mechanisms remain elusive, the pathogenic role of AQP‐4 antibodies is well‐established. However, the influence of variables such as gestation and menopause on NMOSD remains largely unknown. Exploring these factors within AQP‐4 serostatus may reveal a linkage between AQP‐4 IgG and hormonal dynamics, namely in the case of pregnancy where hormonal changes are fairly pronounced.
Methods: This retrospective analysis leverages medical records from nine centers in Turkiye, comprising 120 NMOSD patients (94 Females: F, 26 Males: M) diagnosed per the 2015 IPDN diagnostic criteria. A spreadsheet, filled out by the primary neurologists and was analysed using IBM SPSS Statistics Version 28.
Results: In the AQP‐4 seropositive group, a significant association was revealed between presenting symptoms and treatment response (p = 0.043) (Figure 1, Table 1). In 41 women, 87 pregnancies before the disease onset were evaluated. Pregnancy exhibited a remarkable relationship with the onset age, in which multiple gestations postponed disease manifestation (p < 0.001) (Figure 2).
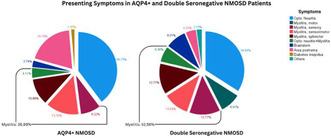
FIGURE 1 Presenting symptom of the first attack of the patients according to serostatus.
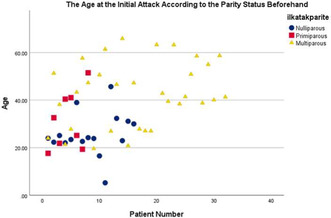
FIGURE 2 The age at the first attack of the patients categorised according to the parity status before the onset of the disease.
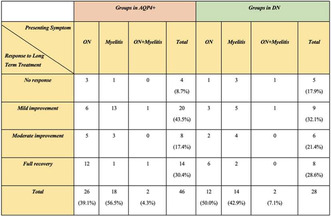
TABLE 1 Long term treatment responses of the AQP4+NMOSD patients according to their presenting symptoms.
Conclusion: This study provides valuable insights into the interplay of clinical, reproductive, and immunological factors in NMOSD, focusing on serostatus and diverse patient profiles. The AQP4+ serostatus emerges as a potential prognosis predictor, prompting physicians to initiate targeted diagnostic assessments earlier which could guide therapeutic strategies and mitigate disability. Compared to double seronegative (25 F, 13 M), AQP4‐NMOSD (66 F, 13 M) predominantly affects females and manifests later in life. Pregnancy initially delays disease onset, potentially influencing prognosis and disability in ways yet to be fully discovered.
Disclosure: Nothing to disclosure.
EPO‐385
Replacing PASAT with SDMT in the MSFC score improves the prediction of thalamic volume in multiple sclerosis
C. Marotta; A. Bisecco; R. Capuano; A. d'Ambrosio; M. Altieri; M. Cirillo; A. Gallo
Department of Advanced Medical and Surgical Sciences, University of Campania Luigi Vanvitelli, Napoli, Italy
Background and Aims: Multiple Sclerosis Functional Composite (MSFC) is a disability measure in Multiple Sclerosis that includes the “Timed 25‐Foot Walk” (T25FW) to evaluate leg function, the “9‐Hole Peg Test” (9HPT) to evaluate arm function and the “Paced Auditory Serial Addition test 3 seconds” (PASAT) to assess cognitive function. An alternative MSFC version replace the PASAT (MSFCp) with the Symbol Digit Modalities Test (SDMT) (MSFCs), that is less influenced by patient's psychological status. Among other MRI structural measures, thalamic volume is strictly associated to physical/cognitive disability in MS. The objective is to evaluate which is the best predictor of thalamic volume between MSFCs and MSFCp.
Methods: One hundred and fifteen relapsing remitting MS (RRMS) patients and 46 sex, age and education‐matched healthy controls (HC) underwent clinical evaluation (EDSS, MSFCp and MSFCs), and a 3T–MRI protocol including high resolution 3D–T1 imaging. Brain and Thalamic volumes were calculated using SIENAX and FIRST tool of the FMRIB Software Library. To compare the different relationship between the thalamic volumes and disability measures we applied linear regression models, introducing the thalamic volumes as dependent variable and EDSS, MSFCp and MSFCs as independent variables.
Results: Compared to HC, MS patients showed a significant thalamic atrophy (p < 0.001). Thalamic volume was independently predicted only by MSFCs (β = 0.67, t 4.16, p < 0.001), while not by EDSS and MSFCp.
Conclusion: MSFCs score performs better than MSFCp in prediction of thalamic volume in MS. Therefore MSFCs might be a better outcome measure in clinical trials in MS.
Disclosure: Nothing to disclose.
EPO‐386
Association of CSF levels of osteopontin with cortical atrophy and disability in early multiple sclerosis
D. Marastoni 1; E. Turano1; A. Tamanti1; E. Colato1; A. Pisani1; A. Scartezzini1; S. Carotenutoi1; V. Mazziotti1; V. Camera1; D. Anni1; S. Ziccardi1; M. Guandalini1; F. Pizzini2; F. Virla1; R. Mariotti3; R. Magliozzi1; B. Bonetti4; L. Steinman5; M. Calabrese1
1Neurology B, Department of Neurosciences, Biomedicine and Movement Sciences, University of Verona, Verona, Italy; 2Neuroradiology & Radiology Units, Department of Engineering for Innovation Medicine, University of Verona, Verona Italy; 3Anatomy and Histology section, Department of Neurosciences, Biomedicine and Movement Sciences, University of Verona, Verona, Italy; 4Neurology A, Azienda Ospedaliera Universitaria Integrata di Verona, Verona, Italy; 5Department of Neurology and Neurological Sciences Stanford University, Stanford CA, USA
Background and Aims: We aimed to evaluate cerebrospinal fluid (CSF) inflammatory markers of accumulation of cortical damage as well as disease activity in patients with early relapsing remitting MS (RRMS).
Methods: CSF levels of Osteopontin (OPN) and 66 inflammatory markers were assessed using an immune‐assay multiplex technique in 107 patients with RRMS (82F/25M, mean age 35.7±11.8 years). All patients underwent regular clinical assessment and yearly 3T MRI scans for 2 years, while 39 patients had a 4‐year follow‐up. White matter lesion number and volume, cortical lesion (CLs) and volume and global cortical thickness (CTh) were evaluated together with the ‘no evidence of disease activity’ (NEDA‐3) status.
Results: The random forest algorithm selected OPN and CXCL13 as most related to CTh changes after 2 and 4 years. In a regression model, OPN (p < 0.001), CXCL13 (p = 0.001), and sTNFR1 (p = 0.024) were increased in those patients with accumulating atrophy (adjusted R‐squared 0.615). The markers were added in a model that included all clinical, demographic and MRI variables: OPN (p = 0.002) and IL19 (p = 0.022) levels were confirmed to be significantly increased in patients developing more CTh change over the follow‐up (adjusted R‐squared 0.619). CXCL13 and OPN also revealed the best association with NEDA‐3 after two years, with OPN significantly linked to disability accumulation (OR 2.468 [1.46‐5.034], p = 0.004).
Conclusion: The data emphasize a crucial role of OPN in predicting changes in cortical pathology and disease activity in early MS.
Disclosure: Nothing to disclose.
EPO‐387
Neuro‐physiological evidences of cerebellar impairment unrelated to structural damage in early multiple sclerosis
V. Boccia 1; A. Botta2; S. Terranova1; E. Cipriano1; G. Grasselli3; E. Capello2; L. Avanzino4; M. Inglese1
1Department of Neurology, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (DINOGMI), University of Genoa, Genoa, Italy; 2IRCCS Ospedale Policlinico San Martino, Genoa, Italy; 3Department of Pharmacy (DIFAR), University of Genoa, Genoa, Italy; 4Department of Experimental Medicine (DIMES), Section of Human Physiology, University of Genoa, Genoa, Italy
Background and Aims: Despite early radiological involvement, clinically‐evident cerebellar impairment (CI) is uncommon in early multiple sclerosis (MS). We used transcranial magnetic stimulation (TMS) to assess cerebellar function and explore its relationship with structural damage in this population.
Methods: Early, right‐handed MS patients without clinically‐evident CI underwent 3T‐MRI and TMS assessment. FLAIR and Double‐Inversion Recovery (DIR) sequences were analyzed to detect both white‐matter and grey‐matter cerebellar lesions (CLs). Cortico‐spinal tract (CST) and middle cerebellar peduncle (MCP) masks from Johns Hopkins University atlas were registered to Diffusion‐Tensor Imaging (DTI)‐maps to obtain mean fractional‐anisotropy (FA). CST excitability was studied through TMS recruitment curve (RC). Cerebellar‐brain inhibition (CBI) was computed as the ratio between test stimulus and motor evoked potential amplitudes recorded after a paired‐pulse protocol stimulating the cerebellum and the primary motor cortex with an interstimulus interval of 5ms.
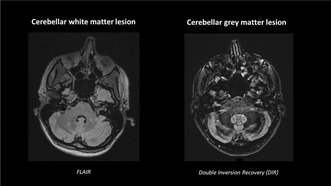
FIGURE 1 FLAIR and Double‐Inversion Recovery (DIR) sequences allow for the detection of both white‐matter and grey‐matter cerebellar lesions.
Results: Seventeen MS patients (F: 12; mean (SD) age: 35.2 (11.3)) with disease‐duration 6.7 (2.6) months and ten healthy‐controls (HCs) (F: 5; age: 32.7 (11.2)) were included. ANCOVA analysis showed CBI reduction (MS: 0.18 (0.11) mV; HCs: 0.28 (0.12) mV; p = 0.05) and RCs slope reduction (MS: 0.56 (0.26) μV/%; HCs: 1.01 (0.36) μV/%; p = 0.01) in MS. No differences in CBI were shown comparing MS patients with and without CLs (p = 0.92). MCP‐FA and CST‐FA showed no effect on CBI (p = 0.86) and RC slope (p = 0.28) reduction respectively.
Conclusion: CBI and RC slope reduction may indicate CI and decreased cortico‐spinal excitability in early‐MS. TMS‐detected functional deficits appeared unrelated to lesion‐related and microstructural damage. TMS may unveil distinct intracortical damage mechanism inaccessible to traditional MRI.
Disclosure: This research was funded by the Italian Ministry of Research through the 5x1000 project 'Cortical Excitability and MS.
EPO‐388
Post‐pandemic pneumonia cases excess in multiple sclerosis patients treated with intravenous anti‐CD 20 drugs
D. Quartana; M. Lo Re; M. Malentacchi; R. Bottero; F. Sperli; A. Oggero; S. Malucchi; A. Di Sapio
CRESM – Hospital Neurology Unit, San Luigi Hospital, Orbassano (Turin), Italy
Background and Aims: Pneumonia is rare in multiple sclerosis (MS) disease‐modifying therapies (DMT) trials. In particular pneumonia in ocrelizumab (OCR) was 0.12% in OPERA I and II, 0.41% in ORATORIO trials. In rituximab (RTX) OLYMPUS trial was 1.4%.
Methods: From January 2023 we collected radiologically confirmed pneumonia cases among MS patients. Our cohort included 1543 subjects, distributed among the different DMTs as shown in the graph.
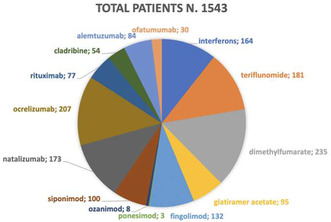
Results: We found 17 pneumonia cases, 11/207 treated with OCR and 6/77 with RTX (5.3% and 7.8% of total patients respectively). No cases occurred in other DMTs. Three cases were COVID related; 7 patients were hospitalized (one with hypogammaglobulinemia in ICU). All patients recovered. Demographic and clinical data are reported in table 1.
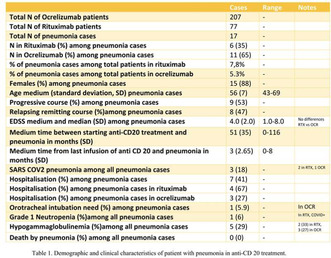
TABLE 1
Conclusion: We observed a higher incidence of pneumonia among patients in intravenous anti‐CD20 therapies compared with clinical trials data. We suppose that risk of pneumonia increases according to treatment duration. A shorter treatment may account for absence of pneumonia cases in ofatumumab treated patients. Considering the age of pneumonia cases, immunosenescence could have an addictive role in increasing infective risk, while hypogammaglobulinemia does not seem as much. Cases mainly occurred in winter, in accordance with epidemic flu peaks; in long lasting immunosuppressed older patients, the post‐ pandemia abandoning of the use of masks and social distancing could account for the recent increase of incidence of pneumonia. Further and larger case‐control study are needed, focused on others environmental factors like smoking and air pollution. Selection bias could account for imbalance between DMTs.
Disclosure: ‐D. Quartana received speaking fee in events sponsored by Merck and Novartis. Merck, Roche and Novartis sustained his travel and accommodation expenses during scientific events. ‐M. Lo Re received speaking fee in events sponsored by Merck and writing fee from Novartis. Biogen sustained her travel and accommodation expenses during scientific events. ‐M. Malentacchi received a grant from Alexion and Novartis. ‐R. Bottero received writing fee from Novartis and speaking fee in events sponsored by Sanofi and Novartis. Bristol Myers and Janssen sustained her travel and accommodation expenses during scientific events. ‐F. Sperli received speaking fee in events sponsored by Novartis. Bristol Mayers sustained her travel and accommodation expenses during scientific events. ‐A. Oggero declared nothing to disclose ‐S. Malucchi received speaking fee in events sponsored by Biogen, Merck, Novartis and Roche. ‐A. Di Sapio received honoraria for speaking and consulting by Biogen, Novartis, Roche, Sanofi, Merck, Alexion and Sandoz and has been reimbursed by Merck, Biogen, Sanofi, Novartis and Roche for attending several conferences.
EPO‐389
Secondary autoimmune diseases in multiple sclerosis after autologous hematopoietic stem cell transplantation
E. Sbragia 1; G. Boffa2; R. Varaldo3; A. Raiola3; A. Ghiso3; M. Gambella3; E. Angelucci3; G. Mancardi2; M. Inglese4
1Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics and Maternal‐Child Health (DiNOGMI), University of Genova, Genova, Liguria, Italy and Department of Neurology, Galliera Hospital, Genova, Liguria, Italy; 2Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics and Maternal‐Child Health (DiNOGMI), University of Genova, Genova, Liguria, Italy; 3Division of Hematology and Bone Marrow Transplantation, IRCCS Ospedale Policlinico San Martino, Genova, Liguria, Italy; 4Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics and Maternal‐Child Health (DiNOGMI), University of Genova, Genova, Liguria, Italy and Neurology Unit, IRCCS Ospedale Policlinico San Martino, Genova, Liguria, Italy
Background and Aims: Autologous hematopoietic stem cell transplantation (aHSCT) has been described as an effective treatment strategy for aggressive multiple sclerosis (MS). Between the possible side effects, secondary autoimmune diseases (SAD) are reported, depending mostly on conditioning regimen (CR) intensity. We aimed to describe the occurrence of both clinical and subclinical SADs in a cohort of MS patients (pwMS) treated with intense immunosuppression followed by aHSCT.
Methods: All pwMS treated at our center with aHSCT with minimum one‐year follow‐up were included and we analysed clinical‐radiological data, blood samples for SADs and lymphocitary‐immunophenotype at baseline and every year.
Results: We evaluated 21 pwMS treated from 2015 to 2022. Medium FU was 3.5 years (range 1‐7). All patients underwent the same CR (carmustine‐cytarabine‐etoposide‐melphalan plus anti‐thymocyte‐globulin), besides one that received high‐dosage cyclophosphamide (Cy). No clinical SADs were noted. Eight out of 21 (38.1%) patients already presented clinical/laboratorical (lab)‐autoimmunity (AI) before aHSCT; of these, in 4 (50.0%) cases lab‐AI disappeared or reduced, in 2 (25.0%) lab‐thyroid‐AI temporarily compared and 2 (25.0%) presented mild anti‐cyclic‐citrullinated‐peptide (CCP) positivity. Of the remaining 13 negative at basal screening, 4 (30.8%) presented transient lab‐AI, 4 (30.8%) mild but persistent lab‐AI (mostly anti‐nuclear antibody, CCP or gastric‐parietal‐cells; one of these patient received high‐dosage Cy as CR) and 5 (38.4%) none. Lab‐AI occurred even after long time from procedure (4 years).
Conclusion: Isolated subclinical positivity with no clinical significance can occur in pwMS after aHSCT with myeloablative CR even after a long FU. Interestingly, previous laboratoristic autoantibodies might disappear.
Disclosure: Nothing to disclose.
EPO‐390
Ketogenic diet as a promising intervention for fatigue management in multiple sclerosis: Results of the CHE‐FATICA study
M. Valente1; S. Dal Bello2; E. Lamon2; F. Filippi2; I. Del Negro2; A. Bernardini2; S. Lorenzut3; E. Saccomano 2; S. Naliato2; C. Prezza2; M. Fabris4; B. Tomasino5; G. Gigli1; R. Garbo6
1University of Udine, Udine, Italy; 2Clinical Neurology Unit, Santa Maria della Misericordia University Hospital, Udine, Italy; 3Neurology Unit, Santa Maria della Misericordia University Hospital, Udine, Italy; 4Clinical Pathology, Department of Laboratory Medicine, Azienda Ospedaliero Universitaria Friuli Centrale, Udine, Italy; 5Scientific Institute IRCCS “Eugenio Medea”, Polo FVG, Pasian di Prato (UD), Italy; 6Neurology Unit, Hospital of Gorizia, Gorizia, Italy
Background and Aims: Fatigue is a frequent, disabling and difficult to treat symptom of multiple sclerosis. Low grade inflammation and energetic dysfunction are proposed mechanisms in the pathogenesis of this symptom. Due to its anti‐inflammatory and metabolic properties, there is a rational for ketogenic diet application in this setting.
Methods: We conducted a single arm open label interventional study on a strictly selected group of 16 non obese patients with multiple sclerosis who were prescribed a KD for three months.
Results: With respect to baseline, at 3 months we observed a significant reduction of fatigue severity scale (5.18±1.02 v.s. 4.16±0.98; p = 0.042), Epworth Sleepiness Scale (5.64±2.46 v.s 8.46±3.05; p < 0.001), Pittsburgh Sleep Quality Index (5.64±3.53 v.s. 7.62±2.59; p = 0.009), Depression Anxiety Stress Scales‐21 depression (3.18±2.93 v.s. 6.15±3.81; p = 0.036) and anxiety (5.15±4.10 v.s. 1.55±1.92; p = 0.019) sub‐scales, and an improvement in energy sub‐scale of Multiple Sclerosis Quality of Life‐54 (52.49±12.83 v.s. 37.43±14.26; p = 0.042).
Conclusion: These findings suggest that ketogenic diet may be useful in the treatment of fatigue and other symptoms frequently encountered in multiple sclerosis.
Disclosure: Nothing to disclose.
EPO‐391
A case of multiple sclerosis combined with polyradiculoneuropathy associated with antiCASPR‐1 antibodies
F. Oggiano; A. Manni; R. Vitobello; A. Bianco; P. Iaffaldano; D. Paolicelli
Department of Translational Biomedicine and Neuroscience (DiBraiN), Policlinico of Bari, Bari, Italy
Background and Aims: Multiple Sclerosis (MS) is an inflammatory demyelinating and neurodegenerative disease of the Central Nervous System (CNS) with almost complete sparing of the Peripheral Nervous System (PNS). Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP) is the most common acquired inflammatory polyneuropathy worldwide. It can be associated with Antibodies to molecules of the paranodal complex, such as Contactin‐associated protein‐1 (CASPR‐1). Cases of CIDP in MS have been reported.
Methods: We report the case of a 50‐year‐old woman with a ten‐years history of CIDP related to Anti‐CASPR‐1 Antibodies who developed MS.
Results: During the diagnostic work‐up for CIDP, to exclude alternative diagnosis, she underwent Magnetic Resonance Imaging (MRI) of the brain in 2010 that was unremarkable. In May 2014 she had diplopia related to right abducens nerve palsy. In November 2014 she had optic neuritis. Therefore she was admitted to our Neurology Department. The neurological examination showed mild right upper limb weakness, facial nerve palsy and absent lower limbs reflexes. Expanded Disability Status Scale was 2.0. She repeated brain and spinal cord MRI that revealed multiple T2 hyperintense lesions involving juxtacortical and periventricular white matter and dorsal segment of the spinal cord. All paraclinical and laboratory tests were normal; the cerebrospinal fluid analysis showed Oligoclonal Bands. A diagnosis of MS was made according to 2017 McDonald criteria.
Conclusion: The co‐existence of MS and CIDP has been reported. It can be due to a shared immune pathogenesis with common antigen between CNS and PNS. It may cause an additional disability burden in patients.
Disclosure: Nothing to disclose.
EPO‐392
A multicentric Italian project: Family functioning and multiple sclerosis
F. Bile 1; L. Lavorgna1; G. Miele1; M. Ponzano2; S. Bonavita1; G. Abbadessa1; G. Marfia3; D. Landi3; F. Proietti3; M. Inglese4; A. Laroni4; I. Poire4; E. Signoriello1; G. Lus1; G. Romano1; R. Lanzillo5; F. Lauro5; L. Rosa5; S. De Mercanti6; V. Perutelli6; M. Di Tella7; L. Streito6; L. Castelli6; M. Clerico5
1Department of Advanced Medical and Surgical Sciences, University of Campania Luigi Vanvitelli, Naples, Italy; 2Department of Health Sciences – Section of Biostatistics University of Genoa, Italy; 3Multiple Sclerosis Clinical and Research Unit, Department of Systems Medicine, Tor Vergata, University, Rome, Italy; 4Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (DINOGMI), University of Genoa, Genoa, Italy; 5Multiple Sclerosis Clinical Care and Research Centre, Department of Neuroscience, Reproductive Sciences and Odontostomatology, Federico II University of Naples, Naples, Italy; 6Department of Psychology, University of Turin, Turin, Italy; 7Department of Clinical and Biological Sciences, School of Medicine, University of Turin, Azienda Ospedaliera Universitaria San Luigi Gonzaga, Turin, Italy
Background and Aims: The impact of Multiple Sclerosis (MS) on family dynamics includes effects on both marital relationships and parental bonding1. In this study we aim to evaluate family functioning and related factors in patients with MS and their families.
Methods: To fill‐out the questionnaires for MS patients and their families, a dedicated platform was employed2. Families without members reporting chronic diseases were selected as healthy controls (HC), and data on socio‐demographics and clinical information were gathered. The administered questionnaires included: The short form of the Family Assessment Measure Third Edition (FAM3), The Hospital Anxiety and Depression Scale (HADS), The Multidimensional Scale of Perceived Social Support (MSPSS), 20‐item Toronto Alexithymia Scale (TAS‐20), Dyadic Adjustment Scale (DAS) and Inventory of Parent and Peer Attachment (IPPA).
Results: Out 164 MS patients enrolled, we selected those individuals for whom a family member had completed the questionnaires. Two patients were excluded due to language limitations, resulting in a final cohort of 50 individuals. Sociodemographic characteristics are displayed in table 1. Compared with HC, MS patients (>20 years) relatives tend to perceive greater support from “others” (p = 0.044), while MS patients partners exhibit a higher dyadic agreement (on finances, leisure time, home organization) (p = 0.005)(Table 2). Moreover, young individuals (13 – 20 years), who have at least one family member with MS, have higher overall IPPA scores (table 3).

Characteristics of the included participants.
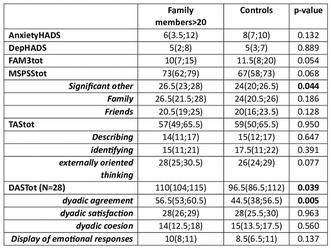
Family members >20 matched with controls based on sex and age.
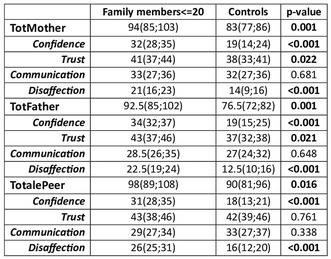
Family members ≤20 matched with controls based on sex and age.
Conclusion: MS influences dynamics of interpersonal relationships within families, Specifically, it molds relationships with partners, showing an higher level of dyadic consensus and leading to a positive impact on MS younger family members.
Disclosure: Nothing to disclose.
EPO‐393
White matter integrity and the brief repeatable battery: A combined neuropsychological and MRI study
F. Certo 1; T. Difonzo1; L. Sacchi1; M. Mancini2; C. Scarpazza3; G. Verrini4; A. Peitroboni1; L. Ghezzi4; M. De Riz1; F. Triulzi1; D. Galimberti5; C. Saetti4; T. Carandini1
1Fondazione IRCCS Cà Granda, Ospedale Maggiore Policlinico, Milan, Italy; 2Cardiff University Brain Research Imaging Center (CUBRIC), Cardiff University, Cardiff, UK; 3Department of General Psychology, University of Padova, Padova, Italy; 4University of Milan, Milan, Italy; 5Department of Biomedical, Surgical and Dental Sciences, Dino Ferrari Center, University of Milan, Milan, Italy
Background and Aims: Cognitive impairment is frequent in people with multiple sclerosis (pwMS) and the brief repeatable battery (BRB) is a sensitive measure for its early detection. Our aim was to test BRB in recently‐diagnosed (<2 years from diagnosis) relapsing‐MS in association with white matter (WM) integrity as measured by diffusion tensor imaging tractography to find possible correlations between cognitive performances and microstructural WM damage
Methods: BRB and 3T‐MRI were acquired in 26 pwMS (16 F, 10 M). WM fibers density and cross‐section (FDC) were measured by fixel‐based analysis within 72 WM tracts of interest using TractSeg. Correlations between WM‐tracts FDC and BRB‐scores were assessed by Pearson correlations (setting p < 0.05) and regression analyses for potential confounders were carried out. Sex differences in Paced Auditory Serial Addition Test (PASAT) scoring were tested by t‐test.
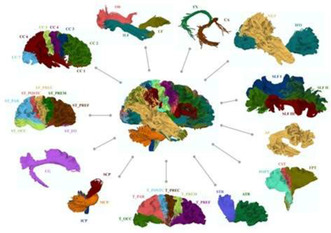
Overview of the 72 WM tracts. WM fiber density and cross‐section (FDC) measures were extracted from 72 WM tracts, by using fixel‐based analysis (MRtrix and TractSeg) (picture from Wasserthal J et al. 2018).
Results: BRB scores were not significantly correlated with clinical and radiological activity, EDSS, depression or fatigue. We found a significant correlation between PASAT 3, 2 and word list generation (WLG) scores and FDC within certain WM tracts, as shown in figure 2. Linear regression found that sex significantly affects PASAT scoring, with males showing higher performances (Fig.3).
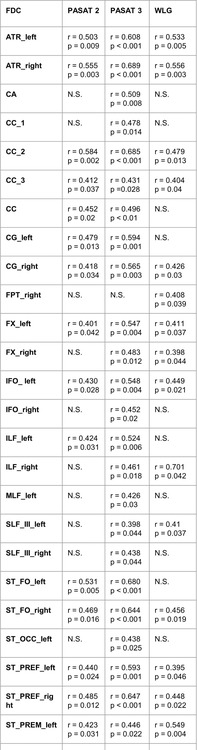
Significant correlation between scoring of PASAT 2, PASAT 3 and WLG with FDC within different WM tract. Pearson correlations were used (p < 0.05). *Persistance of statistical significance when inserting sex as a covariant during regression analyses.
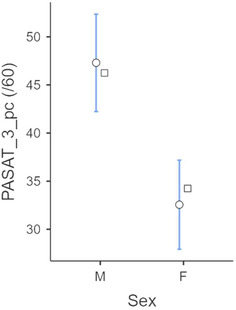
T‐test shows higher PASAT 3 scores in the male group. The same was confirmed for PASAT 2.
Conclusion: In people with recently‐diagnosed‐MS, PASAT and WLG scoring are affected by regional WM axonal damage within specific WM tracts as measured by FDC reduction. From our preliminary results sex seems to affect PASAT performance in MS patients. Larger sample is needed to confirm preliminary result.
Disclosure: Nothing to disclose.
EPO‐394
Treatment switch or retreatment with cladribine tablets during CLARIFY‐MS & CLARIFY‐MS extension studies: Patient profile
F. Piehl 1; K. Selmaj2; E. Havrdova3; A. Smyk4; B. Keller4; X. Montalban5; F. Patti6; J. Lechner‐Scott7
1Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden; 2Center for Neurology, Lodz, Poland; Department of Neurology, University of Warmia and Mazury, Olsztyn, Poland; 3Charles University, First Medical Faculty, Department of Neurology and Center for Clinical Neuroscience, Prague, Czechia; 4Merck Healthcare KGaA, Darmstadt, Germany; 5Department of Neurology Neuroimmunology Centre of Multiple Sclerosis of Catalonia (Cemcat), University Hospital Vall d’Hebron, Barcelona, Spain; 6Department of Medical and Surgical Sciences and Advanced Technologies, GF Ingrassia, University of Catania, and Azienda Ospedaliero Universitaria Policlinico “G Rodolico” – San Marco, University of Catania, Italy; 7University of Newcastle, Newcastle, NSW, Australia; Division of Neurology, John Hunter Hospital, Newcastle, NSW, Australia
Background and Aims: The objective of CLARIFY‐MS Extension (NCT04776213), a follow up study to CLARIFY‐MS, was to assess long‐term effects on cognition and health‐related quality of life in patients with relapsing multiple sclerosis treated with cladribine tablets (CladT). We also evaluated the individual characteristics of patients who switched to other disease modifying therapies (DMTs) or were retreated with CladT during CLARIFY‐MS and CLARIFY‐MS Extension.
Methods: We evaluated potential reasons for switching to other DMTs or CladT retreatment during the total 4‐year observation period of the CLARIFY‐MS Extension study (N = 280), during which no CladT treatment was planned, as per protocol. Decisions to switch to other DMTs or re‐treat with CladT were based on the investigators´ discretion.
Results: Overall, 37/280 patients (13.2%) switched to another DMT, among whom 33 (89%) showed evidence of disease activity (EDA, i.e., 6‐month confirmed disability progression, qualifying relapse, or magnetic resonance imaging [MRI] activity) before switch; MRI activity was the most frequently observed EDA event (28/37; 75.7%). None of the patients switched to another DMT during Year 1 of CladT treatment; 4, 17 and 16 patients switched during Years 2, 3, and 4, respectively. One patient in Year 3 and 7 patients in Year 4 (2.9% in total) were retreated with CladT; all had an EDA event before CladT retreatment. Individual patient profiles and reasons for switching or CladT retreatment will be presented.
Conclusion: A low proportion of patients switched to other DMTs or required CladT retreatment during the CLARIFY‐MS and CLARIFY‐MS Extension studies, suggesting durable CladT efficacy.
Disclosure: This study was sponsored by Merck (CrossRef Funder ID: 10.13039/100009945). Detailed author disclosures will be included in the presentation.
EPO‐395
Ocrelizumab versus siponimod: A real life comparison study
G. Miele 1; G. Abbadessa1; G. Maniscalco2; E. Prestipino2; E. D'Amico3; A. Zanghi3; E. Cocco4; G. Coghe4; L. Lavorgna1; G. Romano1; M. Sparaco1; L. Pasquali5; T. Guerra6; P. Iaffaldano6; E. Signoriello1; G. Lus1; S. Bonavita1
1Department of Advanced Medical and Surgical Sciences, University of Campania Luigi Vanvitelli, Naples, Italy; 2Neurological Clinic and Stroke Unit and Multiple Sclerosis Center “A. Cardarelli” Hospital, Naples, Italy; 3Department of Medical and Surgical Sciences, University of Foggia, Foggia, Italy; 4Multiple Sclerosis Center, ATS Sardinia, Cagliari, Italy; 5Department of Clinical and Experimental Medicine, Neurology Unit, University of Pisa, Pisa, Italy; 6Department of Basic Medical Sciences, Neurosciences and Sense Organs, University of Bari “Aldo Moro”, Bari, Italy
Background and Aims: Ocrelizumab (OCR) and Siponimod (SIP) are licensed to treat patients with Progressive Multiple Sclerosis with disease activity (paMS). This study aims to compare the effectiveness and side effects of OCR and SIP in paMS patients.
Methods: This is a multicenter, retrospective, real‐world study conducted in Italy on paMS patients treated with SIP or OCR. Clinical data, including demographics and laboratory information, were collected at baseline, 6, 12 and 18 months during routine clinical visits. A propensity score matching approach (PSMA) was used to compare the effectiveness and safety of the two treatments.
Results: We enrolled 116 paMS patients treated with OCR and 76 with SIP. These groups showed significant differences in age and annualized relapse rate (ARR) one and two years before treatment. After PSMA, both groups consist of 76 paMS patients, with a mean age of 50.8 (SD 6.95) for the OCR and 51.8 (SD 8.10) for the SIP group (Table 1). No differences in relapses and EDSS scores at 6, 12, and 18 months follow‐up, and Gd+ lesions at MRI at 6 and 18 months follow‐up. The SIP compared to the OCR group showed lower white blood cells and lymphocytes count at 6, 12, and 18 months (p < 0.001); no significant differences were found in the two groups for the number of infections at 6, 12, and 18 months follow‐up.
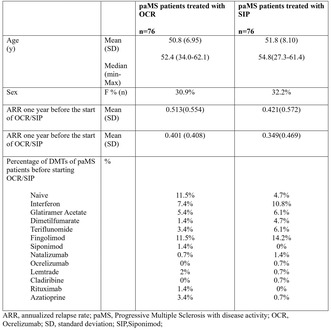
TABLE 1 Demographic and clinic characteristics of paMS patients.
Conclusion: Despite a short 18‐month follow‐up, similar treatment outcomes in elderly paMS patients in SIP or OCR therapy suggest that both treatments are similarly effective and safe in elderly patients.
Disclosure: Nothing to disclose.
EPO‐396
Comparing lymphocyte count among different S1P modulators in multiple sclerosis: A multicenter real‐world study
G. Maniscalco 1; M. Di Gregorio2; G. Cafasso3; E. Signoriello4; S. Bonavita4; F. Romano5; R. Iodice6; R. Fantozzi7; P. Bellantonio7; A. Zanghi8; L. Sinisi9; A. D'Ambrosio10; V. Busillo11; V. Scarano3; L. Lavorgna4; S. Simona1; M. Di Battista1; D. Daniele1; G. Lus4; E. Cassano6; P. Di Filippo8; G. Sibilia9; G. Abbadessa4; V. Andreone1
1Neurological Clinic and Stroke Unit and Multiple Sclerosis Center “A. Cardarelli” Hospital, Naples, Italy; 2Neurology Unit, University Hospital “San Giovanni di Dio E Ruggi d'Aragona”, Salerno, Italy; 3Department of Neurology, AORN San G. Moscati, Avellino, Italy; 4Second Division of Neurology, Department of Advanced Medical and Surgical Sciences, University of Campania Luigi Vanvitelli, Naples, Italy; 5Multiple Sclerosis Center and Neurological and Stroke Unit, CTO Hospital, AORN Ospedale dei Colli, Naples, Italy; 6Department of Neurosciences, Reproductive Sciences and Odontostomatology, University Federico II Naples, Italy; 7IRCCS Neuromed, Pozzilli, Isernia, Italy; 8Department of Medical and Surgical Sciences, University of Foggia, Foggia, Italy; 9Department of Neurology and MS Center, San Paolo Hospital, Naples, Italy; 10Department of Advanced Medical and Surgical Sciences, and 3T MRI‐Center, University of Campania “Luigi Vanvitelli”, Naples, Italy; 11MS Centre, Maria SS. Addolorata Hospital, ASL Salerno, Eboli, SA, Italy
Background and aims: Sphingosine‐1‐phosphate (S1P) modulators are a class of molecules targeting S1P receptors (S1PR) with different S1PR‐subtype selectivity. They cause a reduction in circulating lymphocytes by inhibiting lymphocytes egress from lymph nodes. Our study aims to compare the absolute lymphocytes counts (ALCs) of MS patients treated with Fingolimod (FTY), Siponimod (SIP), Ozanimod (OZA), and Ponesimod (PON).
Methods: We enrolled 219 pwMS from eleven Italian Centers. Out of 219 pwMS, 69 (31.5%) were treated with SIP, 62 (28.3%) with OZA, 46 (21%) with FTY and 42 (19.2%) with PON. We excluded patients who had already received previous treatment with S1P modulators.
Results: OZA showed a significantly higher ALCs compared either to SIP in all time points (p < 0.001 at T1 and T3; p = 0.003 at T6), or FTY at T1 (p < 0.001) and T3 (p = 0.02). PON showed significantly higher ALCs compared to SIP at T1 and T3 (p = 0.003; p = 0.03 respectively). Furthermore, we analyzed the percentage of severe lymphopenia (including grade 3 and grade 4) among the different S1P modulators. PON and OZA showed a significantly lower percentage of patients with severe lymphopenia (23.8 % p = 0.006, 25.8% p = 0.005 respectively) compared to FTY (52.2%) and SIP (60.9%).
Conclusion: Despite a short follow‐up, our study demonstrated a different degree of induced‐lymphopenia among S1P modulators, as OZA and PON showed higher ALCs and a lower percentage of severe lymphopenia in pwMS.
Disclosure: Nothing to disclose.
EPO‐397
Identifying multiple sclerosis patients within a control population using online cognitive and motor assessments
H. Karoui 1; A. Moura1; A. Lerede1; R. Middleton2; A. Hampshire1; R. Nicholas1
1Brain Sciences, Imperial College London, London, UK; 2Population Data Science, FHMLS, Swansea University, Swansea, UK
Background and Aims: Multiple Sclerosis (MS) is characterised by a complex interplay of motor, cognitive and neuropsychiatric features which vary between individuals and across time. Whilst MS diagnosis has improved over time, there remains a need for more rapid and reliable diagnostic tools. We use classification algorithms to investigate the feasibility of online cognitive and motor assessments in identifying MS patients from controls.
Methods: We trained a random forest classifier on cognitive metrics from a randomly sampled population of 1777 patients with MS (pwMS), 1189 patients with depression and anxiety (pwDA) and 1777 healthy controls (HC) from Cognitron. The model uses performance metrics (response time and accuracy) from 7 online cognitive tasks specific to MS, as features to predict the participant's group label. We also trained a support vector machine (SVM) classifier on motor performance metrics from pwMS and HC. This model uses the MS Impact Scale (MSIS‐29v2) from the UKMS Register to determine the participant's group label.
Results: The random forest classifier discriminates between HC and pwMS (ROC AUC = 0.81), and between pwDA and pwMS (ROC AUC = 0.85) using online cognitive testing metrics. Our SVM classifier robustly distinguished pwMS from HC (ROC AUC = 0.96) using the MSIS‐29v2. A sub‐analysis of pwMS (five years from onset) also showed high classification accuracy (ROC AUC = 0.94).
Conclusion: Online cognitive testing and motor MSIS‐29v2 can accurately distinguish pwMS from controls. Our findings provide a novel data‐driven approach to MS identification, offering an opportunity for earlier intervention and tailored treatment approaches in the clinical setting.
Disclosure: RN: Advisory boards for Roche/Novartis.
EPO‐398
Longer‐term safety and efficacy of ofatumumab in people with relapsing multiple sclerosis for up to 6 years
H. Wiendl 1; S. Hauser2; J. Nicholas3; J. de Sèze4; S. Meuth5; P. Giacomini6; D. Robertson7; S. Wray8; A. Bhatt9; X. Hu10; H. Fu10; V. Jehl11; R. Sullivan10; I. Boer11; J. Cohen12; L. Kappos13
1University of Muenster, Muenster, Germany; 2UCSF Weill Institute for Neurosciences, University of California, San Francisco, CA, USA; 3OhioHealth Multiple Sclerosis Center, Columbus, OH, USA; 4University Hospital of Strasbourg, Strasbourg, France; 5Department of Neurology, Medical Faculty, Heinrich‐Heine‐University, Düsseldorf, Germany; 6Department of Neurology and Neurosurgery, Montreal Neurological Institute, McGill University, Montreal, Quebec, Canada; 7Multiple Sclerosis Division, Department of Neurology, University of South Florida, Tampa, FL, USA; 8Hope Neurology MS Center, Knoxville, TN, USA; 9Novartis Healthcare Pvt. Ltd., Hyderabad, India; 10Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA; 11Novartis Pharma A.G. Basel, Switzerland; 12Department of Neurology, Mellen MS Center, Neurological Institute, Cleveland Clinic, Cleveland, OH, USA; 13Research Center for Clinical Neuroimmunology and Neuroscience Basel (RC2NB) and MS Center, Departments of Headorgans, Spine and Neuromedicine, Clinical Research, Biomedicine and Biomedical Engineering, University Hospital, University of Basel, Switzerland
Background and Aims: Ofatumumab demonstrated superior efficacy and favourable safety versus teriflunomide in the Phase 3 ASCLEPIOS I/II trials in people with relapsing multiple sclerosis (pwRMS). Previously reported data showed sustained efficacy and a favourable safety profile of ofatumumab in pwRMS up to 5 years. Here, we aim to present the safety and efficacy of ofatumumab treatment for up to 6 years.
Methods: Efficacy analyses will include all participants randomised in ASCLEPIOS I/II and their data from first dose in ASCLEPIOS I/II, whereas safety analyses will include all participants who received at least one dose of ofatumumab in either ASCLEPIOS I/II, APOLITOS, APLIOS or ALITHIOS (cut‐off date: 25‐Sep‐2023). Efficacy will be analysed by randomised treatment in the core study, with those randomised to ofatumumab referred to as continuous group and to teriflunomide as switch group.
Results: Previously reported 5‐year data (cut‐off: 25‐Sep‐2022) showed a sustained low annualised relapse rate (ARR) and almost complete suppression of MRI lesion activity in the continuous group. In the switch group, ARR was markedly reduced from Year 2–3 (0.16–0.06) and remained low through Years 3–5 (0.05), and MRI lesion activity was almost completely suppressed through Years 3–5. At Year 5, 90% of patients reached NEDA‐3 in both groups. The safety profile of ofatumumab remained consistent with no new safety signals over 5 years. Updated 6‐year efficacy and safety results will be presented at the congress.
Conclusion: These analyses will help inform physicians on the longer‐term safety and efficacy profile of ofatumumab in pwRMS.
Disclosure: The study was supported by Novartis Pharma AG, Switzerland. The detailed author disclosures will be presented in the subsequent presentation.
Muscle and neuromuscular junction disorder 2
EPO‐399
Association of the initiation timing of oral steroids with clinical prognosis in adult generalized myasthenia gravis
D. He; C. Yan; H. Zhong; Y. Zhou; Y. Zhang; X. Huan; J. Xi; C. Zhao
Department of Neurology, Huashan Hospital, Fudan University
Background and Aims: To explore the association of the initiation timing of oral corticosteroids with the prognosis of adult generalized myasthenia gravis (GMG) patients.
Methods: We retrospectively screened adult GMG patients and divided them into early treatment group (initiation of oral steroids within one year from disease onset) and late treatment group. The clinical information at baseline and one‐year follow‐up were collected. The propensity score matching (PSM) analysis was used to select the candidates of two cohorts. The prognosis after one year therapy between the two groups was compared after matching.
Results: 50 patients were enrolled in both groups after PSM. Both quantitative MG (QMG) and MG‐activities of daily living (MG‐ADL) points were significantly lower in the early‐treatment group than in the late‐treatment group. In particular, the QMG and MG‐ADL points of appendicular muscles were significantly lower in the early‐treatment group than in the late‐treatment group. The proportion of minimal symptom expression (MSE) is significantly higher in early treatment group compared to late treatment group (74% vs 44%, p = 0.0223), while the proportion of refractory MG is lower (8% vs 26%, p = 0.0166).
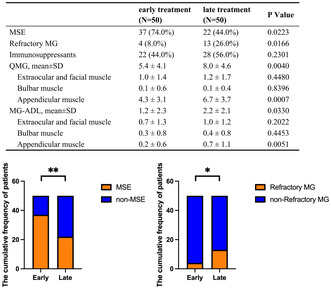
Clinical prognosis of the patients between early treatment and late treatment groups after propensity score matching. Values are presented as the mean±SD or n (%). MSE, minimal symptom expression; MG, Myasthenia Gravis; QMG, Quantitative Myasthenia Gravis.
Conclusion: Adult GMG patients who received corticosteroid therapy within one year of the onset date show a higher rate of MSE and a lower rate of refractory status than the late‐treatment GMG patients, indicating that treatment of corticosteroids starting within 12 months gave rise to a more favorable prognosis in GMG patients.
Disclosure: China's National Natural Science Foundation Youth Project (No. 8210052671).
EPO‐400
Safety profile of intravenous efgartigimod from clinical trials in immunoglobulin G–mediated autoimmune diseases
A. Meisel 1; K. Gwathmey2; C. Broome3; M. Goebeler4; H. Murai5; Z. Bata‐Csörgo6; A. Newland7; P. Ulrichts8; R. Kerstens8; J. Guptill9; S. Agha8; M. Jiang8; J. Howard Jr10; K. Claeys11
1Department of Neurology with Experimental Neurology, Integrated Myasthenia Gravis Center, Neuroscience Clinical Research Center, Charité Universitätsmedizin Berlin, Berlin, Germany; 2Department of Neurology, Virginia Commonwealth University, Richmond, Virginia, USA; 3Department of Medicine, Georgetown University, Washington, DC, USA; 4Department of Dermatology, Venereology and Allergology, University Hospital Wϋrzburg, Wϋrzburg, Germany; 5Department of Neurology, School of Medicine, International University of Health and Welfare, Narita, Japan; 6Department of Dermatology and Allergology, University of Szeged, Szeged, Hungary; 7Centre for Haematology, Barts and the London School of Medicine & Dentistry, Queen Mary University of London, London, UK; 8Argenx, Ghent, Belgium; 9Argenx, Ghent, Belgium; School of Medicine, Duke University, Durham, North Carolina, USA; 10Department of Neurology, The University of North Carolina at Chapel Hill, Chapel Hill, North Carolina, USA; 11Department of Neurology, University Hospitals Leuven, Leuven, Belgium; Laboratory for Muscle Diseases and Neuropathies, Department of Neurosciences, KU Leuven, and Leuven Brain Institute (LBI), Leuven, Belgium
Background and Aims: Efgartigimod (EFG), a human immunoglobulin G (IgG)1 Fc fragment, blocks the neonatal Fc receptor, selectively decreasing IgG levels. The safety profile of intravenous (IV) EFG was assessed across different IgG‐mediated diseases.
Methods: EFG IV was assessed in different dosing regimens (10–25 mg/kg IV, including cyclical and continuous weekly dosing) in generalised myasthenia gravis (gMG; Phase 2 trial and Phase 3 placebo‐controlled ADAPT and open‐label extension ADAPT+ trials), in primary immune thrombocytopenia (ITP; Phase 3 placebo‐controlled ADVANCE IV and ongoing open‐label extension ADVANCE IV+ [data cut‐off: 24 November 2023] trials) and in pemphigus vulgaris and foliaceus (Phase 2 trial). Pooled data represent participants receiving EFG 10 mg/kg IV in the Phase 2, ADAPT and ADAPT+ trials for gMG and in the ADVANCE IV and ADVANCE IV+ trials for ITP.
Results: EFG IV was well‐tolerated and demonstrated a consistent safety profile across all indications and doses studied, with comparable rates of treatment‐emergent adverse events (TEAEs) to placebo and across indications (Table 1; TEAEs ranged from 77.4–95.6% across studies and pooled analyses). Most TEAEs across studies were mild to moderate in severity. Discontinuation rates due to TEAEs were consistently low across studies and pooled analyses (ranged from 0–9.1%). There was no increase in TEAE or infection event rates with repeated treatment (Table 1). EFG treatment did not reduce albumin levels or increase cholesterol levels.

Conclusion: EFG IV was well‐tolerated across indications and doses studied. Most TEAEs were mild to moderate in severity and event rates did not increase with repeated treatment.
Disclosure: AM: Alexion, argenx, Axunio, Grifols, Hormosan, Janssen, Merck, Octapharma, UCB, Vitaccess. KG: Alexion, argenx, UCB, Xeris Pharmaceuticals. CMB: Alexion, Apellis, argenx, Sanofi. MG: Almirall, argenx, Biotest, GSK, Janssen, Leo Pharma, Lilly, Novartis, UCB. HM: Alexion, argenx, Chugai, Japan Blood Products Organization, Roche, UCB. ZBC: NKFI Hungary, Orvostovábbképzo Szemle, Sanofi Genzyme Hungary. AN: Amgen, Angle, argenx, Dova, Novartis, Ono, Rigel, Shionogi. PU, RK, JTG, SA, and MJ: Employees of argenx. JFH: AcademicCME, Ad Scientiam, Alexion, AstraZeneca Rare Disease, argenx, Biologix Pharma, Cartesian Therapeutics, Centers for Disease Control and Prevention, CheckRare CME, F. Hoffmann‐LaRoche Ltd, Amgen, Medscape CME, Merck EMB Serono, MGFA, Muscular Dystrophy Association, NIH, NMD Pharma, Novartis, PCORI, PeerView CME, Physicians' Education Resource (PER) CME, PlatformQ CME, Regeneron Pharmaceuticals, Sanofi US, Toleranzia AB, UCB, Zai Lab. KGC: Alexion, Alnylam, Amicus, argenx, Biogen, CSL Behring, Ipsen, Janssen, Roche, UCB.
EPO‐401
Adverse pregnancy outcomes in myasthenia gravis: A retrospective cohort study in a US health insurance claims database
M. Jacobson1; R. Makadia1; C. Gary 2; N. Hall1; J. Hardin1; S. Huang3; R. Sun4; R. Zaha4; A. Krumme1
1Johnson & Johnson, Innovative Medicine, Global Epidemiology; 2Johnson & Johnson, Innovative Medicine, Medical Affairs, Immunology; 3Johnson & Johnson, Innovative Medicine, Immunology; 4Johnson & Johnson, Innovative Medicine, R&D Data Science
Background and Aims: Pregnancy is common among individuals with autoantibody conditions and adverse perinatal outcomes have been documented. However, previous studies in myasthenia gravis (MG) have produced mixed results.
Methods: We conducted a retrospective cohort study in the United States (US) Marketscan Commercial Claims and Encounters database between 2000‐2022. Pregnancies in females aged 18‐49 were identified and among live births, maternal and infant records were linked. MG was defined by ≥1 inpatient or ≥2 outpatient diagnoses within a 365‐day period, with ≥1 diagnosis required before pregnancy end. The prevalence of six perinatal outcomes was calculated in the MG and total populations: live birth, spontaneous abortion, Cesarean section, preeclampsia, preterm birth, and small for gestational age (SGA). Outcome prevalence in the total population was standardized to the MG population age distribution.
Results: A total of 694 individuals with MG had 900 pregnancies and 3,928,256 individuals in the total population had 5,185,726 pregnancies. The prevalence of live birth (75.0% vs. 73.9%) and spontaneous abortion (20.4% vs. 20.8%) was similar in the MG and age‐adjusted total population, respectively. Preeclampsia and Cesarean section were more frequent among MG than the total population (10.7% vs. 7.1%; 42.9% and 35.0%, respectively). The largest differences were noted for preterm birth and SGA, which were more prevalent among MG than the total population (18.0% vs. 9.7%; 4.3% vs. 1.7%, respectively).
Conclusion: MG was associated with a greater burden of certain adverse perinatal outcomes, occurring in both mother and infant. Further research is needed to understand drivers of pregnancy outcomes in MG.
Disclosure: This study was conducted by Johnson & Johnson. All authors are employed by, and hold stock in, Johnson & Johnson.
EPO‐402
Rituximab alone is as effective as associated with steroids on naive patients with generalized myasthenia gravis
C. Héraud 1; S. Bresch2; C. Landes‐Château2; C. Lebrun‐Frenay2
1Neurology Department, CHU de Nice, Nice, France; 2Unité de Recherche Clinique Côte d'Azur
Background and Aims: Rituximab (RTX) has been proven effective in managing refractory generalized myasthenia gravis (MG), and its use is increasing worldwide. MG stabilization may initially require oral corticosteroid (CS) therapy, but its long‐term side effects require the shortest duration of treatment. We studied the clinical effectiveness and usefulness of corticosteroids associated with RTX compared to RTX alone on MG remission.
Methods: In a monocentric retrospective cohort in the Nice University Hospital, we compared naïve MG patients treated with RTX as first‐line therapy alone (G1) or associated with CS (G2). After the RTX induction, we evaluated efficacy with the Osserman score (OS) and the requirement for any rescue therapy (IgIV or plasmapheresis).
Results: Sixty‐eight patients were treated with RTX, of which 19 (27.94%) benefited from an association with at least 0.5 mg/kg of corticosteroids. RTX‐CS patients were more severe than RTX alone (OS: G1: 74.1 and G2: 64.94, p = 0.044). However, OS at three (83.44 and 83.12, p = 0.993), six (88.69 and 86.36, p = 0.545), nine (82.91 and 85.73, p = 0.563), and twelve months (86.6 and 88.69, p = 0.761) from the treatment induction were similar. Rescue therapy following RTX induction was significantly higher for the RTX‐CS (20.41% and 47.37%, p = 0.037). Regarding safety, adverse event rates were similar in the two groups (0% and 14.29%, p = 0.178).
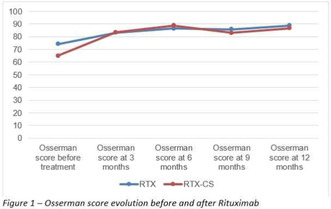
Conclusion: We suggest that RTX alone is as effective as RTX‐CS in MG patients, indicating that avoiding steroids could reduce side effects, decrease rescue therapies, and not affect MG outcomes.
Disclosure: The authors have no conflict of interest to declare.
EPO‐403
Intensive care due to exacerbation of myasthenia gravis: Risk factors and prognosis
C. Myllynen 1; A. Tuulasvaara2; S. Atula2; S. Laakso2
1Department of Neurosciences, University of Helsinki, Helsinki, Finland; 2Department of Neurology, Brain Center, Helsinki University Hospital, Helsinki, Finland
Background and Aims: Exacerbation of myasthenia gravis (MG) with imminent respiratory failure requires intensive care. We studied the risk factors for intensive care and patients’ prognosis thereafter.
Methods: This retrospective registry study covered Helsinki and Uusimaa hospital district from 2008 to 2021. Patients were identified using the ICD‐10 code (G70.0) through a data repository search, followed by a chart review of patient medical records. The risk factors for intensive care (intensive care unit or intensive monitoring ward) were evaluated as compared with the patients never in need of in‐hospital care for MG (outpatient group) and with those treated at a neurological ward for MG exacerbation. We compared the outcome between MG exacerbation and all reasons of intensive care.
Results: A total of 35 (9%) out of 386 MG patients required intensive care for MG exacerbation, within a median of 5.3 months from diagnosis. The intensive care group had a higher mean age at MG diagnosis and more comorbidities than the outpatient group. Thymoma (OR 4.8; p = 0.028) and female sex (OR 2.1; p = 0.045) were independent risk factors for intensive care due to MG exacerbation. High modified Rankin scale pre‐hospitalization and late‐onset MG (LOMG) were associated with prolonged intensive care stay and 6‐month mortality (14.3%) was higher in patients with prolonged intensive care stay and older age.
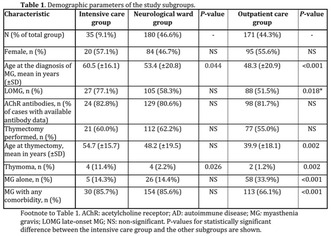

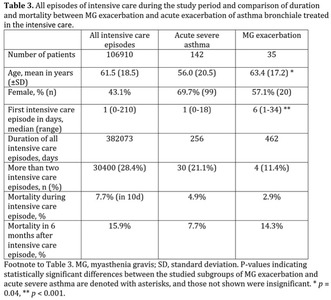
Conclusion: Our study shows an increased risk of intensive care for patients with LOMG or thymoma, occurring usually within six months from diagnosis. Special attention to early treatment choices should thus be given.
Disclosure: CM: received a grant from Maire Taponen Foundation; AT: travel expenses UCB Pharma, received research funding of the state of Finland governed through Helsinki University Hospital (project code Y223230047); SA: Nothing to disclose; SML: travel expenses UCB Pharma, lecture fee Argenx, advisory fee UCB Pharma, Argenx, received research funding of the state of Finland governed through Helsinki University Hospital (project code TYH2023316).
EPO‐404
Clinical and genetic features of a cohort of patients with myoadenilate deaminase deficiency: A new mutation
C. Alberti 1; S. Lucchiari1; M. Rimoldi2; F. Fortunato2; D. Velardo1; L. Napoli3; M. Moggio1; N. Bresolin1; G. Comi1; S. Corti1; E. Abati1; M. Moggio3; N. Bresolin2; G. Comi2; S. Corti3; E. Abati2
1Department of Pathophysiology and Transplantation (DEPT), Dino Ferrari Centre, Neuroscience Section, University of Milan, Milan, Italy; 2Neurology Unit, Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milan, Italy; 3Neuromuscular and Rare Diseases Unit, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy
Background and Aims: Myoadenylate deaminase deficiency is the predominant metabolic disorder affecting skeletal muscles in the Caucasian population, involving approximately 2% of individuals. While the majority of those with the deficiency remain asymptomatic, some experience symptoms induced by exercise, suggesting a link between reduced enzyme activity and muscle function.
Methods: We conducted a cross‐sectional analysis on 8 patients harboring mutations in AMPD1 and exhibiting a biochemical deficiency of myoadenylate deaminase (MAD) at histopathological analyses.
Results: Evaluated patients demonstrated a variable age of onset and a broad phenotypic spectrum, with most presenting exercise‐induced myalgia and proximal weakness. Routine blood tests showed no significant abnormalities, except for persistent elevation in serum creatine kinase (CK). DNA analysis revealed the nonsense mutation c.34C>T (p.Q45*) in all patients, except for one with a novel compound heterozygous mutations p.Arg494Ser and p.Met511Val. These mutations located at a highly conserved position were predicted to be pathogenic by in silico tools. In comparison to other patients, the carrier of the novel mutation exhibited an earlier onset within the first months of life with primary dropped head syndrome and a more pronounced elevation of serum creatine kinase (CK) levels, which then progressed to proximal, limb‐girdle type myopathy.
Conclusion: In conclusion, our work expands the genetic spectrum of MAD deficiency, disclosing a novel mutation and its related clinical effect, and provides a detailed description of the clinical features of a cohort of patients with AMPD1 mutations.
Disclosure: Nothing to disclose.
EPO‐405
Short‐term and long‐term prognoses in sub‐very‐late‐onset and super‐late‐onset myasthenia gravis patients
N. Xie1; Q. Liu2; S. Zhang1; Q. Wen1; Y. Wang1; Y. Li3; H. Liu1; Y. Jiang1; Y. Lu1; L. Di1; M. Wang1; M. Xu1; H. Chen1; . Zhu1; X. Wen1; X. Shen4; Y. Da 1
1Department of Neurology, Xuanwu Hospital, Capital Medical University, Beijing, China; 2Department of Neurology, Beijing Fengtai You'anmen Hospital, Beijing, China; 3Department of Neurology, Electric Power Teaching Hospital, Capital Medical University, Beijing, China; 4Department of Neurology and Neuromuscular Research Laboratory, Mayo Clinic, Rochester, Minnesota, USA
Background and Aims: To find the clinical factors that affect the short‐ and long‐term prognosis of myasthenia gravis (MG) patients with onset age ≥65 years.
Methods: This was a retrospective, observational case‐control study. Patients were classified into two age subgroups: sub‐very‐late‐onset MG (S‐VLOMG, onset age ≥65 and ≤69 years), and super‐late‐onset MG (SLOMG, onset age ≥70 years). The main outcome was the time to achieve minimal manifestations status (MMS) or better. We used the Cox proportional hazards model to identify factors influencing short‐ and long‐term prognosis in all patients.
Results: A total of 59 patients were included, 28 of S‐VLOMG and 31 of SLOMG. All patients reached MMS within 2 years, with a median time to MMS of 168.0 days. In S‐VLOMG group, compared to SLOMG group, had lower MG‐activities of daily living (MG‐ADL) scores at 3rd and 6th months (p = 0.002, p = 0.001), and shorter time from treatment to MMS (p = 0.02). In the COX proportional hazards model, we found that age at onset (≥65 to ≤69, HR = 2.339, p = 0.022), baseline MGFA classification (OMG, HR = 2.534, p = 0.020), baseline MG‐ADL≤ 2 (HR = 10.463, p < 0.0001) and no limb weakness at baseline (HR = 3.356, p = 0.004) were associated with the 6th month prognosis (short‐term). The factors affecting the prognosis of patients at 24th months (long‐term) were like those at 6th months with the addition of changes of ΔMG‐ADL at 6th months (HR = 1.155, 95%CI = 1.042‐1.280, p = 0.006).
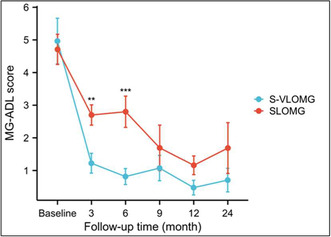
Change in MG‐ADL score in two groups over follow‐up time. ** = p≤0.01; *** = p≤0.001.
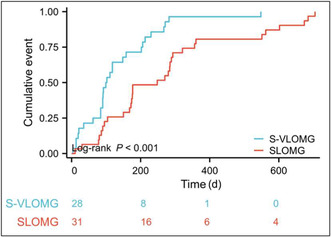
Kaplan‐Meier curve of the time from treatment to MMS between two groups.
Conclusion: The patients with S‐VLOMG had a better short‐term prognosis compared to SLOMG patients, while their long‐term prognosis remains similar.
Disclosure: Nothing to disclose.
EPO‐406
Positive predictive value of acetylcholine receptor autoantibody testing by radioimmunoprecipitation assay
P. Zara; P. Chessa; G. Deiana; A. Morette; M. Puci; G. Sotgiu; P. Solla; E. Sechi
Department of Medical, Surgical, and Experimental Science, University of Sassari
Background and Aims: Antibodies against the acetylcholine receptor (AChR‐IgG) confirm a diagnosis of autoimmune myasthenia gravis (MG). Radioimmunoprecipitation assay (RIPA) is the gold standard for AChR‐IgG detection with a reported specificity of ≈99%. However, its accuracy in large, unselected populations has not been fully elucidated. We determined the positive predictive value (PPV) and risk of false AChR‐IgG positivity in a real‐life setting.
Methods: The retrospective analysis included 4795 patients consecutively tested between 2003 and 2022. Medical records of patients with AChR‐IgG positivity (antibody titer of ≥0.5 nmol/L) were reviewed to determine true vs false antibody positivity. AChR‐IgG‐positive patients with insufficient clinical information were excluded (n = 84).
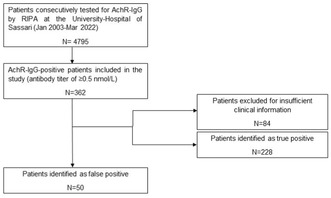
The flow chart summarizes the steps towards identification of patient with false Ach‐R IgG positivity.
Results: Of 362 AChR‐IgG‐positive patients included in the study, 50 (13.8%) were designated as false positives. Specificity and PPV were 98.9% and 86.2%, respectively. Alternative diagnoses in patients with false AChR‐IgG positivity included ocular diseases (n = 8), rheumatic diseases (n = 7), and others (n = 35). Main reasons for antibody testing included isolated diplopia (n = 18), nonspecific asthenia (n = 16), or others. Compared to patients with true AChR‐IgG positivity, false positive patients were younger, more frequently female and had a lower antibody titer. After stratification by AChR‐IgG titers of ≥1 nmol/L, specificity and PPV increased to 99.8% and 96.6%, respectively.
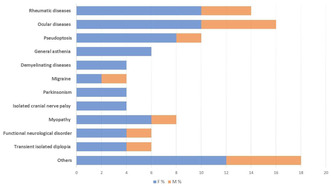
The bar graph shows the percentage of alternative diagnoses.
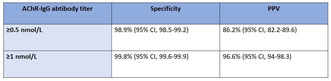
Variation of specificity and PPV after stratification.
Conclusion: Despite the high specificity of AChR‐IgG testing by RIPA, the risk of false antibody positivity is not negligible in clinical practice (14% in this study). Caution is needed when low titer AChR‐IgG positivity (0.5‐0.9 nmol/L) is detected in patients with symptoms that are nonspecific for MG.
Disclosure: Nothing to disclose.
EPO‐407
The safety and efficacy profile of eculizumab in myasthenic crisis: A prospective case series
J. Song 1; X. Huan1; Y. Chen1; Y. Luo2; H. Zhong1; Y. Wang3; L. Yang4; C. Xi4; Y. Yang5; J. Xi1; J. Zheng6; S. Luo1; C. Zhao1
1Huashan Rare Disease Center and Department of Neurology, Huashan Hospital, Shanghai Medical College, National Center for Neurological Disorders, Fudan University, Shanghai, China; 2Department of Neurology, Ganzhou People's Hospital, Nanchang University, Jiangxi province, China; 3Department of Blood Transfusion, Huashan Hospital, Fudan University, Shanghai, China; 4Department of Laboratory Medicine, Huashan Hospital, Fudan University, Shanghai, China; 5Department of Thoracic Surgery, Shanghai Chest Hospital, Shanghai Jiaotong University, Shanghai, China; 6Department of Infectious Diseases, Huashan Hospital, National Medical Center for Infectious Diseases, Fudan University, Shanghai, China
Background and Aims: Myasthenic crisis (MC) represents a severe exacerbation of myasthenia gravis. While eculizumab has shown promise in case reports, there is a lack of prospective data on its safety and efficacy. This study aims to investigate eculizumab as an adjunct therapy in refractory MC patients.
Methods: We conducted a prospective case series study over 12 weeks, targeting patients with acetylcholine receptor (AChR) subtype refractory MC. Participants were administered eculizumab as an add‐on to standard therapy. Outcomes were measured using the MGFA‐quantitative MG test (MGFA‐QMG) and the MG‐Activities of Daily Living (MG‐ADL) scale, with additional monitoring of muscle strength across various domains. Additionally, serum anti‐AChR antibody titers, CH50, C1q, C5a, and soluble C5b‐9 (SC5b‐9) levels were measured at the baseline and 12 weeks after eculizumab treatment.
Results: Patients exhibited significant improvements in both MGFA‐QMG (baseline: 22.25±4.92, 12 weeks: 7.5±5.74) and MG‐ADL (baseline: 18.25±2.5, 12 weeks: 2.75±4.86) scores from the 4‐week mark onward. Muscle strength consistently increased across ocular, bulbar, respiratory, and limb/gross domains. One patient succumbed to cardiac failure at 16 weeks, but three cases remained in remission at 24 weeks. There were sustained declines in serum CH50 and soluble C5b‐9 levels, with no significant changes in anti‐AChR antibody titers, C1q and C5a. No significant side effects were reported.
Conclusion: Eculizumab was well‐tolerated and effective in enhancing recovery and reducing disease activity in patients with MC. These findings support further large‐scale prospective studies with extended follow‐up to establish the safety and efficacy profile of eculizumab in a real‐world setting.
Disclosure: Nothing to disclose.
EPO‐408
Real‐world reduction in oral corticosteroid utilization following efgartigimod initiation
T. Ruck 1; N. Goyal2; C. Qi3; J. Stone4; D. Gelinas3; M. Jefferson3; T. Suthagar5; R. R Menon5; M. Sato6; G. Phillips3
1Department of Neurology, Heinrich Heine University Düsseldorf, Düsseldorf, Germany; 2Department of Neurology & Neurological Sciences, Stanford Medicine, Palo Alto, CA, USA; 3Argenx US Inc., Boston, MA, USA; 4Department of Clinical Rheumatology, Massachusetts General Hospital, Boston, MA, USA; 5ZS Associates, Bengaluru, Karnataka, India; 6ZS Associates, New York, NY, USA
Background and Aims: Reducing or tapering oral corticosteroids (OCS, prednisone equivalent), a common treatment used in generalised myasthenia gravis (gMG), can alleviate risk related to long‐term OCS usage. The objective of this study was to evaluate OCS usage following efgartigimod initiation.
Methods: In this retrospective study, patients with gMG using OCS who initiated efgartigimod were identified from a United States medical and pharmacy claims database (based on information licenced from IQVIA: Longitudinal Access and Adjudication Data [LAAD] for the period April 2016−April 2023, reflecting estimates of real‐world activity [all rights reserved]). Mean (SD) average daily dose (ADD) of OCS was evaluated during the 3‐months prior to, and at 3‐ and 6‐months post‐efgartigimod initiation. Any patients enrolled in the “My VYVGART Path” patient support program that had baseline and follow‐up myasthenia gravis activities of daily living (MG‐ADL) scores available were identified to assess score change.
Results: Among 576 patients who initiated efgartigimod by September 30, 2022, and continued efgartigimod for ≥6 months, 231 (40%) were using OCS at baseline. Mean (SD) OCS ADD was significantly reduced at 3‐ (15.6 [14.8] mg/day, p = 0.0007) and 6‐months (14.5 [15.5] mg/day, p = 3.99x10‐6) post‐efgartigimod initiation compared with baseline (19.0 [15.1] mg/day). A subset of 75 patients (32%) had MG‐ADL scores available both before and during the 6‐months following efgartigimod initiation. Among them, significant reduction was observed in best‐follow up mean (SD) MG‐ADL (from 8.7 [3.7] to 4.5 [3.3], p = 1.2x10‐14).
Conclusion: Early insights indicate that OCS usage was significantly reduced over 6 months post‐efgartigimod initiation, while retaining MG‐ADL response.
Disclosure: This research was funded by argenx US, Inc. (Boston, MA, USA). TR received honoraria and/or research support from Alexion, argenx, Biogen, Merck, Novartis and Roche. NG has received consulting fees from argenx, UCB, Janssen and Alexion, and grant support from argenx. CQ, DG, MJ, and GP are employees of argenx. JS has consulted for argenx on glucocorticoid toxicity. TBS, RRM and MS are employees of ZS Associates (Evanston, IL, USA) and serve as paid consultants for argenx.
EPO‐409
Steroid toxicity in adults with myasthenia gravis in the United States based on electronic health records
T. Ruck 1; N. Goyal2; M. Hehir3; G. Phillips4; J. Stone5; C. Qi6; M. Stone7; D. Gelinas6; A. Chamberas7; D. Amirthaganesan8; R. Kulkarni9; A. Whangbo10
1Department of Neurology, Medical Faculty and University Hospital Düsseldorf, Heinrich Heine University Düsseldorf, Düsseldorf, Germany; 2Department of Neurology & Neurological Sciences, Stanford Medicine, Palo Alto, CA, USA; 3Department of Neurology, University of Vermont Medical Center, Burlington, VT, USA; 4Argenx BVBA, Ghent, Belgium; 5Harvard Medical School, Massachusetts General Hospital, Boston, MA, USA; 6Argenx US, Inc., Boston, MA, USA; 7Steritas, Concord, MA, USA; 8ZS Associates, Bengaluru, Karnataka, India; 9ZS Associates, Bethesda, MD, USA; 10ZS Associates, Durham, NC, USA
Background and Aims: While benefits/risks of steroids in myasthenia gravis (MG) have been studied, quantifying steroid toxicity is challenging using real‐world data.
Methods: Adults with MG (≥2 MG diagnoses 30‐730 days apart between Jan 2014‐Sep 2021) were identified in United States (US)‐based Optum® de‐identified Electronic Health Record data set (Optum® EHR) (Jan 2013‐Dec 2022). Index dates were defined as first steroid prescription (for steroid initiators [MG‐SI]) or assigned after age/gender match (for steroid‐naïve [MG‐SN]). Patients with available lab measures for main criteria of the Glucocorticoid Toxicity Index‐Metabolic Domains (GTI‐MD) were included. GTI‐MD scores (Aggregate Improvement Score [AIS] and Cumulative Worsening Score [CWS], higher scores represent higher toxicity) were compared between MG‐SI vs. MG‐SN cohorts. Multivariate regression assessed the relationship of steroid usage, strength, and timing of follow‐up assessment to GTI‐MD.
Results: Among 27,157 patients with MG, 377 and 305 were included in the MG‐SI and MG‐SN cohorts, respectively. 30% of the MG‐SI cohort had multiple steroid prescriptions and ≥20mg prescription at index. GTI‐MD (SD) scores were higher in MG‐SI compared with MG‐SN (AIS: 4.9 [34.5] vs. 1.9 [34.3], p = 0.27; CWS: 22.6 [22.8] vs. 18.7 [21.2], p = 0.023). Regression results showed MG‐SI patients with ≥2 records and ≥20mg at index had an average AIS 10.2 higher than MG‐SN (p = 0.01). Each additional month of follow‐up since index was associated with a decrease of 1.5 AIS (p < 0.001).
Conclusion: Our results demonstrated steroid toxicity is significantly higher in patients with higher strength and repeated steroid usage. Patients experienced consistent elevation in steroid toxicity over time.
Disclosure: This study was funded by argenx US, Inc. (Boston, MA, USA). TR received honoraria and/or research support from Alexion, Argenx, Biogen, Merck, Novartis and Roche. NG has served as a paid consultant for argenx, UCB, Janssen and Alexion, and has grant support from argenx. MH consults for argenx, Alexion, Janssen, UCB and Immunovant; received compensation as Guest Editor for Continuum Lifelong Learning in Neurology 2023; and is supported by UVM Medical Center grant for unrelated work. GP, CQ, and DG are employees of argenx. JHS has consulted for argenx on glucocorticoid toxicity; JHS's employer, the Massachusetts General Hospital, owns the intellectual property of the Glucocorticoid Toxicity Index (GTI). The intellectual property of the GTI‐MD (Metabolic Domains) is co‐owned by the Massachusetts General Hospital and Steritas, LLC. JHS co‐founded Steritas and is the chair of the Scientific Advisory Board but has no fiduciary responsibility at the company. MS is an employee of Steritas. AC is a consultant to Steritas. DA, RK and AW are employees of ZS Associates (Evanston, IL, USA) and serve as paid consultants for argenx.
EPO‐410
Duchenne muscular dystrophy (DMD) patient vignettes development methodology
V. Merla 1; P. Nathaniel1; O. Borecka2; S. Vincent2
1Pfizer Inc., New York, USA; 2Vitaccess, Oxford, UK
Background and Aims: Duchenne muscular dystrophy (DMD) is a severe, rare neuromuscular disease with wide‐ranging impacts, therefore, accurately describing the quality of life (QoL) of people with DMD can be challenging. This study describes the methodology in the development and validation of DMD patient vignettes prepared for rating by neurologists using the 5‐level EQ‐5D (EQ‐5D‐5L) proxy version 1, to derive health‐state utility values.
Methods: Eight vignettes representing DMD health states (based on Project HERCULES) were developed. The draft vignettes were developed through an extensive literature search. Following the development of the draft vignettes, two DMD PAG representatives with caregiver experience were interviewed to validate the vignettes. After incorporating PAG feedback, four specialist neurologists were recruited to review and score the vignettes using the EQ‐5D‐5L.
Results: The feedback obtained from PAG representatives on the draft vignettes was positive and confirmed their overall accuracy. The comments allowed for minor changes to some domains including requirements of 24‐hour care in later non‐ambulatory stages, a need for specialist equipment to assist with self‐care and adjustments to mental health impacts, such as, additional wording around the patient feeling isolated and escalation of the severity descriptor of depression in the last health state.
Conclusion: Development of patient vignettes in rare conditions can be challenging; hence, PAG and specialist clinician feedback can play an important role in more accurately describing the QoL of people with DMD and other severe, rare diseases. The mental health impacts and the intensity of the care and assistance required by people with DMD should not be underestimated.
Disclosure: Val Merla and Nate Posner are employees of Pfizer Inc., and this study was funded by Pfizer Inc. Octavia Borecka and Sally Vincent are employees of Vitaccess Ltd.
EPO‐411
Early real‐life experience of Zilucoplan in refractory generalized myasthenia gravis
V. Di Stefano; P. Luppino; P. Alonge; N. Rini; A. Lupica; F. Brighina
Department of Biomedicine, Neuroscience, and advanced Diagnostic (BIND), University of Palermo, Palermo, Italy
Background and Aims: Myasthenia gravis is a rare chronic autoimmune disease affecting the post‐synaptic membrane of the muscle junction characterized by debilitating, and potentially fatal, muscle weakness. (1, 2). Treatment options available for generalized myasthenia gravis (gMG) have grown in recent years with the introduction of new drugs, such as the complement factor C5 inhibitors (2, 3). The objective of the Compassionate Use Program (GM0025IT) is to provide early access to Zilucoplan for gMG patients with a high unmet medical need and severe disease burden.
Methods: Zilucoplan was administered by daily subcutaneous self‐injection as for protocol (2). Efficacy was assessed by using the MG‐ADL scale and QMG. The patients' baseline therapy remained unchanged during the entire course of treatment.
Results: Three female patients (mean age 32 y) affected by AChR‐seropositive gMG received Zilucoplan. A reduction in MG‐ADL scores was observed in the first week from the first injection compared to baseline with a mean change of – 2.33 points (ranging from ‐4 to ‐1). The main change at one month was – 4.0 points. Regarding QMG, a reduction of ‐2 points was achieved in two patients at one month. All three patients reported a significant improvement in the quality of daily life. No safety issues were identified.
Conclusion: The decline in scores obtained testifies to the efficacy of treatment with Zilucoplan and the rapidity of its action onset. Also, Zilucoplan appears to be very easy to administer and has a favorable safety profile (2). Further data and longer observations are needed to confirm our data.
Disclosure: Vincenzo Di Stefano received compensation for speaking from Alexion, and Alnylam; he is SI in clinical trials for Alexion, Alnylam, Argenx, Dianthus, and Sanofi.
EPO‐412
A predictive nomogram for short‐term outcomes of myasthenia gravis patients treated with low‐dose rituximab
Y. Zhou 1; R. Guo2; X. Xia1; S. Jing3; J. Lu1; Z. Ruan2; S. Luo1; X. Huan1; C. Zhao1; T. Chang2; J. Xi1
1Department of Neurology, Huashan Hospital, Fudan University, Shanghai, China; 2Department of Neurology, Tangdu Hospital, The Fourth Military Medical University, Xi’an, China; 3Department of Neurology, Banan Hospital, Chongqing Medical University, Chongqing, China
Background and Aims: This study aims to establish and validate a predictive nomogram for the short‐term clinical outcomes of myasthenia gravis (MG) patients treated with low‐dose rituximab.
Methods: We retrospectively reviewed 108 patients who received rituximab of 600 mg every six months in Huashan Hospital and Tangdu Hospital. Of them, 76 patients from Huashan Hospital were included in the derivation cohort to develop the predictive nomogram, which was externally validated using 32 patients from Tangdu Hospital. The clinical response is defined as a ≥3 points decrease in QMG score within 6 months. Both clinical and genetic characteristics were included to screen predictors via multivariate logistic regression. Discrimination and calibration were measured by the area under the receiver operating characteristic curve (AUC‐ROC) and Hosmer‐Lemeshow test, respectively.
Results: Disease duration (OR = 0.987, p = 0.032), positive anti‐muscle specific tyrosine kinase antibodies (OR = 19.8, p = 0.007), and genotypes in FCGR2A rs1801274 (AG: OR = 0.131, p = 0.024; GG: OR = 0.037, p = 0.010) were independently associated with clinical response of post‐rituximab patients. The nomogram identified MG patients with clinical response with an AUC‐ROC (95%CI) of 0.875 (0.798‐0.952) in the derivation cohort and 0.741 (0.501‐0.982) in the validation cohort. Hosmer‐Lemeshow test showed a good calibration (derivation: chi‐square = 3.181, p = 0.923; validation: chi‐square = 8.098, p = 0.424).
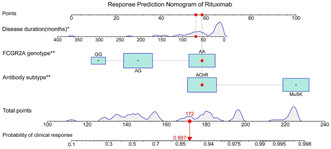
Nomogram to estimate the probability of clinical response in MG patients after low‐dose rituximab treatment.
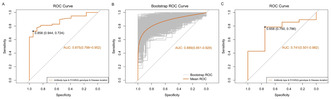
ROC‐AUC of nomogram A. Derivation cohort: ROC‐AUC = 0.875, 95%CI: 0.798‐0.952. B. Resampling: mean ROC‐AUC = 0.889, 95%CI: 0.851‐0.929. C. Validation cohort: ROC‐AUC = 0.741, 95%CI: 0.501‐0.982.
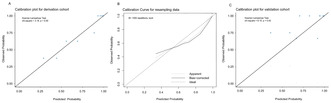
Model calibration of derivation cohort (A), resampling data using bootstrap (B), and validation cohort (C) The x‐ and y‐axes in the graph represent the predicted and actual response probabilities from the nomogram, respectively.
Conclusion: The nomogram achieved an optimal prediction of short‐term outcomes in patients treated with low‐dose rituximab.
Disclosure: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
EPO‐413
Response to single rituximab can predict a better outcome of multi‐cycle treatment in refractory myasthenia gravis
Y. Zhou 1; S. Jing2; J. Lu1; S. Luo1; X. Huan1; J. Song1; C. Yan1; C. Zhao1; J. Xi1
1Department of Neurology, Huashan Hospital, Fudan University, Shanghai, China; 2Department of Neurology, Banan Hospital, Chongqing Medical University, Chongqing, China
Background and Aims: This study aims to access the long‐term clinical outcomes of myasthenia gravis (MG) patients treated with multi‐cycle low‐dose rituximab.
Methods: This retrospective cohort study with prospectively collected data involved 47 refractory patients who received 500/600 mg rituximab every six months in Huashan Hospital. We divided them into a response group (n = 30) and a non‐response group (n = 17) based on a decrease of ≥3 scores in Quantitative Myasthenia Gravis (QMG) score 6 months after first rituximab treatment. We compared the change of QMG and Activities of Daily Living (ADL) scores and the time to minimal symptom expression (MSE, i.e., ADL 0‐1 score) between the two groups.
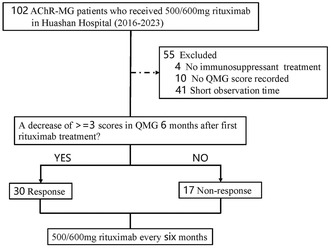
Recruitment of patients with refractory generalized myasthenia gravis.
Results: There were significant group×visit interactions for QMG score and ADL score. Six months after the fourth rituximab treatment, QMG score was lower for the response group (‐6.07; p = 0.005; 95%CI, ‐10.26 to ‐1.88) compared with the non‐response group; the equivalent mean changes from baseline were ‐9.95 (95%CI, ‐11.78 to ‐8.12) and ‐0.45 (95%CI, ‐3.38 to 2.49), respectively. ADL score was lower for the response group (‐2.84; p = 0.006; 95%CI, ‐4.83 to ‐0.852) compared with the non‐response group; the equivalent mean changes from baseline were ‐5.40 (95%CI, ‐6.74 to ‐4.05) and ‐1.99 (95%CI, ‐4.18 to 0.21), respectively. The median time to MSE was shorter in the response group (6.5 months versus not available; HR: 15.83; 95%CI,3.53‐70.91; p<0.001).
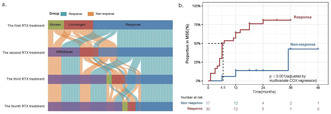
Post‐treatment status (a) and time to MSE (b) after multi‐cycle rituximab treatment in refractory generalized AChR‐MG.
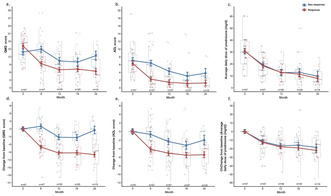
Clinical efficacy
Conclusion: The response to single low‐dose rituximab can predict a better outcome of multi‐cycle treatment in refractory MG.
Disclosure: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Monday, July 01 2024
Ageing and dementia 3
EPO‐414
Exploring the interplay among neuroinflammation, neurodegeneration and mitochondrial damage in Alzheimer's disease
D. Plantone 1; M. Pardini2; C. Manco1; D. Righi1; P. Alì2; D. Arnaldi2; V. Pelagotti2; F. Massa2; N. De Stefano1
1Department of Medicine, Surgery and Neuroscience, University of Siena, Siena, Italy; 2Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, University of Genoa, Genova, Italy
Background and Aims: This study aims to conduct a comprehensive assessment of various biomarkers related to different aspects of AD pathology. These aspects encompass neurodegeneration, glial activation, mitochondrial dysfunction, and immune response. The objective is to correlate these results among them and with the "classic" diagnostic AD biomarkers.
Methods: Neurofilament light chain (NfL), glial fibrillary acidic protein (GFAP) and transactive response DNA binding protein (TDP‐43) concentrations were assessed through the use of Simoa technology. Growth Differentiation Factor 15 (GDF‐15) was assessed using ELISA. Concentrations of 11 selected cytokines were determined using a multiplex bead‐based flow cytometry assay. Non‐parametric statistical analyses were performed.
Results: CSF samples of the 52 AD patients were collected. Twenty‐four patients were recruited in Genova and 28 patients in Siena. The median age was 74.3 years (25th–75th percentiles, 71.3–77.3) and 35% were male. MMSE score showed a positive correlation with the CSF Aβ1‐42 concentrations (r = 0.485; p < 0.001), as well as with CSF interleukin (IL)‐17A concentrations (r = 0.34; p = 0.015), and a negative correlation with CSF GDF‐15 concentrations (r = −0.418; p = 0.002). CSF IL‐17A concentrations also showed a positive correlation with CSF Aβ1‐42 concentrations (r = 0.302; p = 0.031). CSF IL‐6 concentrations showed a positive correlation with CSF NfL concentrations (r = 0.312; p = 0.026) and a negative correlation with CSF TDP‐43 concentrations (r = −0.322; p = 0.021). CSF t‐Tau concentrations were negatively correlated with CSF IL‐10 (r = −0.301; p = 0.032;), IFN‐gamma (r = −0.315; p = 0.024), and IL‐8 concentrations (r = −0.305; p 0.029), CSF p‐Tau concentrations were negatively correlated with CSF IFN‐gamma concentrations (r = −0.312; p 0.026).
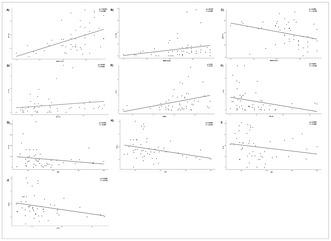
Partial correlation between A) MMSE and Aβ1‐42; B) MMSE and IL‐17A; C) MMSE and GDF‐15; D) IL‐17A and Aβ1‐42; E) IL‐6 and NfL; F) IL‐17A and TDP‐43; G) t‐Tau and IL‐10; H) t‐Tau and IFN‐g; I) t‐Tau and IL‐8; J) p‐Tau and IFN‐g; with age as control variable.
Conclusion: This ongoing study starts to cast light on the intricate interplay that exists among neuroinflammation, neurodegeneration, mitochondrial damage, and clinical disability in AD.
Disclosure: Nothing to disclose.
EPO‐415
Cholinesterase inhibitors and risk of epilepsy in Alzheimer's disease – Study on 32 121 patients from SveDem
D. Religa; L. Liv Törner Monsenego; M. Eriksdotter; H. Xu
Department of Neurobiology, Care Sciences and Society (NVS) Karolinska Institutet, Stockholm, Sweden
Background and Aims: Alzheimer's disease (AD) is the most common type of dementia and Cholinesterase inhibitors (ChEIs) are the first line symptomatic treatment. Given the increased incidence of epilepsy (EP) in AD, the question arises about whether ChEIs influences the risk of developing EP.
Methods: This cohort study was based on 32,121 patients with AD in the Swedish Dementia Registry SveDem with a study period of ten years. Incidence rates and Cox proportional hazard modeling were applied to the study outcomes epilepsy and mortality, for a total and PS‐matched cohort, with ChEI use as the exposure. The primary aim was to explore a possible association between ChEI use and EP in AD. The secondary aim was to examine if ChEI use influences mortality.
Results: No association was found between ChEI use and EP, apart from in patients with a MMSE score above 25 who experienced a decreased EP risk of 30.5% when treated (HR 0.69; 95% CI: 0.49–0.99). A significant association was found between ChEI use and decreased mortality (HR 0.88; 95% CI: 0.85–0.92).
Conclusion: In line with existing research, this study has not identified a link between ChEI and increased EP risk. The association between ChEI use and decreased mortality is coherent with other studies. The decreased EP risk found in patients with early‐stage dementia is understandable given disease characteristics and emerging research on an anti‐epileptogenic ChEI element, such as the recently outlined cholinergic anti‐inflammatory pathway. Such an element could also constitute an explanation behind the decreased mortality.
Disclosure: None.
EPO‐416
Abstract withdrawn
EPO‐417
Development and use of cognition bolt‐ons for the EQ‐5D‐3L and EQ‐5D‐5L: A systematic review
F. Rencz 1; S. Pangestu2; B. Mulhern3; A. P. Finch4; M. F. Janssen5
1Department of Health Policy, Corvinus University of Budapest, Hungary; 2Department of Health Policy & Doctoral School of Business and Management, Corvinus University of Budapest, Budapest, Hungary; Faculty of Economics and Business, Atma Jaya Catholic University of Indonesia, Jakarta, Indonesia; 3Centre for Health Economics, Research and Evaluation (CHERE), University of Technology Sydney, Sydney, Australia; 4EuroQol Research Foundation, Rotterdam, The Netherlands; 5Section Medical Psychology and Psychotherapy, Department of Psychiatry, Erasmus MC, Rotterdam, The Netherlands
Background and Aims: The widely used EQ‐5D measures health‐related quality of life across five dimensions. Cognition has been one of the earliest and most extensively applied additional dimensions (‘bolt‐on’). Our aim was to systematically review the literature on cognition bolt‐ons for the EQ‐5D, categorising existing items and their wordings across various populations.
Methods: We conducted a systematic literature search using PubMed, Web of Science and Google Scholar to identify publications that used cognition bolt‐ons for the two adult versions of the EQ‐5D (3L and 5L), following the PRISMA guidelines (PROSPERO CRD42023445567).
Results: The included 181 publications (1997‐2023) from 137 studies revealed an increasing trend in using cognition bolt‐ons. Cognition bolt‐ons have been applied in 28 languages across 23 countries, with the Netherlands leading (64%). Overall, 71 different patient populations were included in these studies, with the most common being head or brain injury (n = 13), dementia (n = 12), depression (n = 5), stroke, HIV and burn (n = 4 each). We identified 52 different wordings (3L: n = 23 and 5L: n = 29). The most frequent descriptors, cognition (29%) and thinking ability (19%), included examples such as concentration (60%), memory (39%) and remembering (31%). Most bolt‐on items lacked any qualitative input and they commonly deviated from the EQ‐5D‐format (e.g. extended dimension title, inappropriate examples or not severity‐type response scale).
Conclusion: The growing and extensive use of cognition bolt‐ons for the EQ‐5D signals a demand from users for this bolt‐on. The parallel existence of various wordings and the absence of proper development highlight the necessity for future bolt‐on development and harmonisation efforts.
Disclosure: Funded by the EuroQol Research Foundation (ERF; EQ Project 1700‐RA). FR, BM, APF and MFJ are members of the EuroQol Group. APF is employed by the ERF. Views expressed in the abstract are those of the authors and are not necessarily those of the ERF.
EPO‐418
Serum GFAP levels discriminate between AD and bvFTD but are influenced by renal function
F. Verde 1; I. Milone1; F. Solca1; A. Maranzano1; S. Torre1; A. Dubini2; E. Torresani2; B. Poletti1; A. Ratti1; V. Silani1; N. Ticozzi1
1Neurology Unit and Laboratory of Neurosciences, Department of Neurosciences, IRCCS Istituto Auxologico Italiano, Milan, Italy; 2Laboratory of Clinical Chemistry and Microbiology, Department of Laboratory Medicine, IRCCS Istituto Auxologico Italiano, Milan, Italy
Background and Aims: Blood levels of GFAP are increased in Alzheimer's disease (AD).
Methods: We measured serum GFAP (sGFAP) in 38 patients with AD, 25 patients with the behavioural variant of FTD (bvFTD), and 25 neurologically healthy controls (NHCs).
Results: sGFAP was increased in AD compared to NHCs and to bvFTD, and in bvFTD compared to NHCs (all p < 0.05). The ROC curves for the discrimination between AD and NHCs and between AD and bvFTD had AUCs of 0.9095 (p < 0.0001) and 0.75 (p = 0.0008), respectively. In (AD + bvFTD) (N = 51), sGFAP correlated negatively with CSF Aβ42/40 ratio (r = ‐0.2931) and positively with P‐tau181 (r = 0.3973) and T‐tau (r = 0.3355) (all p < 0.05). Accordingly, sGFAP was higher in neurochemically defined A+ vs. A‐, T+ vs. T‐, and N+ vs. N‐ patients (all p < 0.05). In the whole cohort, sGFAP positively correlated with age (r = 0.5111; p < 0.0001). In (AD + bvFTD + CTRL), sGFAP negatively correlated with estimated glomerular filtration rate (eGFR) (r = ‐0.4142; p = 0.0003; N = 72). Interestingly, in (AD + bvFTD), sGFAP also negatively correlated with the CSF/serum albumin ratio (Q‐Alb) (r = ‐0.3557; p = 0.0066; N = 57).

Serum GFAP levels in patients with AD, patients with bvFTD, and neurologically healthy controls.
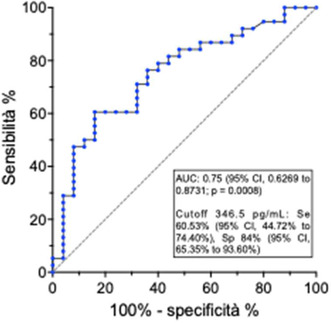
ROC curve of serum GFAP for the discrimination between AD and bvFTD.
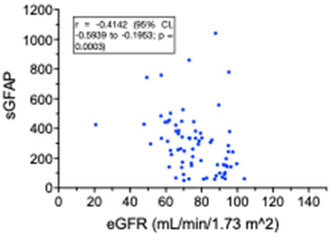
Negative correlation between serum GFAP and estimated glomerular filtration rate.
Conclusion: sGFAP is a promising biomarker for the discrimination between AD and bvFTD and is associated with neurochemical evidence of both Aβ and tau pathology. The negative correlation between sGFAP and eGFR may be practically important. The negative correlation with Q‐Alb deserves further investigation.
Disclosure: Nothing to disclose.
EPO‐419
CSF synaptic proteins and monoaminergic systems in prodromal Alzheimer's disease: Insights from [18F]FDG PET correlations
F. Massa 1; B. Orso2; V. Pelagotti2; M. Losa2; L. Argenti2; L. Lombardo2; P. Mattioli1; A. Brugnolo1; N. Girtler1; D. Arnaldi1; A. Chincarini3; S. Morbelli4; G. Sambuceti5; M. Pardini1
1Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (DINOGMI), University of Genoa, and IRCCS Ospedale Policlinico San Martino, Genoa, Italy; 2Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (DINOGMI), University of Genoa; 3Istituto Nazionale di Fisica Nucleare (INFN), Genoa section, Italy; 4Department of Medical Sciences, University of Turin, and Nuclear Medicine Unit, AOU Città Della Salute e Della Scienza di Torino, Turin, Italy; 5Department of Health Sciences (DISSAL), University of Genoa, and IRCCS Ospedale Policlinico San Martino, Genoa, Italy
Background and Aims: Understanding the interaction between molecular aberrations in prodromal Alzheimer's disease (AD) and diffuse projection systems may foster pharmacological intervention. With this aim, we assessed baseline [18F]FDG‐PET metabolism colocalization with PET maps of monoaminergic systems and correlated with cerebrospinal fluid (CSF) biomarkers of AD pathology and synaptopathy in prodromal AD patients.
Methods: We retrospectively analyzed 49 MCI‐AD patients with positive CSF AD biomarkers (Aβ42/40, pTau, t‐Tau), then grouped by time until dementia (Early MCI,EMCI, n = 34 progressing within two years; late MCI,LMCI, n = 15 stable/progressing later). Using the JuSpace toolbox, [18F]FDG‐PET images were compared voxel‐wise against 40 matched healthy controls (HC) to generate hypometabolism maps. Spearman's correlation coefficients evaluated the colocalization strength between hypometabolism and neurotransmitter maps, with negative values signifying heightened disease involvement in cortical regions normally abundant in receptors/transmitters. Coefficients were correlated with CSF standard AD and synaptopathy biomarkers (NPTX2, Neurogranin) in MCI‐AD and EMCI/LMCI subgroups.
Results: Voxel‐wise analyses showed hypometabolism patterns in MCI‐AD, primarily in the temporoparietal and precuneus/posterior cingulate cortices. CSF pTau negatively correlated with hypometabolism‐5HT1B receptor colocalization in the MCI‐AD group and EMCI (r = −.306, p = 0.035 and r = −.394, p = 0.028). In the LMCI subgroup, CSF NPTX2 and Neurogranin positively correlated with colocalization strength of hypometabolism with 5HT4‐ (r = .719, p = .011; r = .603, p = 0.008) and D1‐receptor maps (r = .707, p = 0.010; r = .603, p = 0.038).
Conclusion: Reduced CSF synaptic biomarker levels in late MCI parallel hypometabolism in regions rich in dopaminergic and serotonergic terminals, consistent with their role in disease staging and suggesting an interplay between synaptopathy and diffuse projection system alterations.
Disclosure: Nothing to disclose.
EPO‐420
Creative thinking as a resource in pathology: A cognitive stimulation training for mild cognitive impairment patients
F. Colombi 1; G. Fusi1; M. Crepaldi1; J. Giannì1; M. Zanetti2; I. Di Fazio2; E. Facchi2; L. Colautti3; A. Antonietti3; L. Rozzini4; M. Rusconi1
1Department of Human and Social Sciences, University of Bergamo, Italy; 2Geriatric Evaluation and Rehabilitation Unit Richiedei Foundation, Palazzolo sull’Oglio, Brescia, Italy; 3Psychology Department, Catholic University of the Sacred Heart, Milan, Italy; 4Department of Clinical and Experimental Sciences, University of Brescia, Italy
Background and Aims: Considering the increase in life expectancy and the incidence rate of age‐related chronic neurodegenerative diseases, non‐pharmacological treatments are relevant to prevent and slow cognitive decline in prodromal stages of disease such as dementia. Creative thinking training has shown promising potential. The aim of the present research is to show the efficacy of a creativity‐based training on cognitive and psychological variables in patients affected by Mild Cognitive Impairment (MCI).
Methods: An individual 10‐sessions training (CREC, CReativity in Everyday life Challenges), based on exercises that stimulate divergent thinking, was administered to a sample of 30 patients with MCI (9 men; age: 77.57 ± 3.51; education: 7.07 ± 2.70). Other 16 MCI patients (3 men; age: 79.38 ± 8.03; education: 5.75 ± 1.34) were assigned to an active control group. Specific cognitive functions, divergent thinking abilities and psychological well‐being were assessed before and after the training sessions.
Results: Although the study is still ongoing, the first results highlight a significant improvement in the experimental group compared to the control group in semantic fluency abilities. Moreover, both groups show improvement in praxic‐constructive skills and in the perception of overall well‐being, along with a reduction in anxious symptomatology.
Conclusion: CREC appears to be effective in promoting improvement in cognitive skills such as semantic abilities. These results suggest that creative thinking could be a useful resource against cognitive decline in patients with MCI, playing an important role in reducing or delaying progression of symptoms.
Disclosure: This research was funded by Fondazione Cariplo, grant no. 2018‐0792. The authors declare no conflict of interest.
EPO‐421
Usability of tele‐medicine and tele‐rehabilitation applications in subjects with mild cognitive impairment
G. Arabia 1; R. Di Lorenzo2; F. Abate3; L. Arcudi4; R. Bruno BOSSIO5; N. Caravona6; R. Colao2; G. Frontera7; F. Galati8; P. Insarda'9; M. Lupo10; A. Gambardella1; M. Bernardi11; N. Vanacore12
1Institute of Neurology, Department of Medical and Surgical Sciences, “Magna Graecia” University of Catanzaro, Italy; 2CDCD Lamezia Terme, Italy; 3CDCD Crotone, Italy; 4CDCD Reggio Calabria, Italy; 5CDCD Serraspiga‐CS, Italy; 6CDCD Corigliano‐Rossano‐CS, Italy; 7CDCD Catanzaro, Italy; 8CDCD Vibo Valentia, Italy; 9CDCD Cinquefrondi‐RC, Italy; 10CDCD Cosenza, Italy; 11Department of Health Protection, Social and Socio‐Health Services, Calabria Region, Italy; 12National Center for Disease Prevention and Health Promotion, National Institute of Health, Rome, Italy
Background and Aims: Tele‐medicine and tele‐rehabilitation systems are increasingly proposed approaches to improve or stabilize cognitive functions of patients with mild to moderate cognitive decline. The aim of the present project was to investigate the usability of tele‐medicine and tele‐rehabilitation systems designed for remote assistance and treatment of patients with mild cognitive impairment (MCI) and in their caregivers.
Methods: The project included two lines of intervention for which usability was analyzed: 1) a program of tele‐rehabilitation for the MCI patients, using at home a dedicated software installed on a tablet (Neurotablet), for 4 consecutive weeks; 2) a program of visits in Tele‐Medicine for educational and psychological support, for patients and caregivers, for 4 consecutive weeks. Ten Cognitive Disorders and Dementia Centers (CDCD), distributed throughout the Calabria region, in Italy, participated to the project. Usability was evaluated through the System Usability Scale (SUS) and measuring the patients performances using Neurotablet.
Results: All CDCDs consecutively recruited 134 patients with amnestic MCI (46.3% M/53.7% F; mean age 69.5 ± 6.8 years; mean education: 9.6 ± 3.7 years) and 131 caregivers (28.7% M/71.3% F; age strata (18‐45 y): 36.2%, (45‐65 y): 35%, (>65 y): 28.8%). As preliminary results on the usability of the system, SUS was good for patients (mean SUS score: 74.01) and excellent for caregivers (mean SUS score: 83.27). Other usability measurements analyses are currently ongoing.
Conclusion: The results of this project allow to highlight the strengths and the limitations of the use of tele‐medicine and tele‐rehabilitation in patients with MCI and in their caregivers.
Disclosure: This project was founded by the Alzheimer's and Dementia Fund 2021‐2023 of the Italian Ministry of Health (Project Line #4) and coordinated by the Italian National Institute of Health.
EPO‐422
Correlation between alterations in rs‐functional alterations of brain and CSF markers in patients with AD
H. Zhao; C. Gong
Department of Neurology, Nanjing Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School
Background and Aims: The aim of this study was to explore the correlation between brain functional alterations and CSF pathological biomarkers in AD patients.
Methods: 23 AD patients and 16 control subjects were recruited. All subjects underwent CSF measurement and multimodal MRI scans. Independent component analysis was used to investigate the variations of FC by utilizing RS‐fMRI data. Differences in ALFF and ReHo between the two groups were also calculated. Then correlation analyses were used to estimate the possible association between functional alterations and CSF biomarkers.
Results: In the AD group, ALFF decreased in the right Superior Frontal Gyrus, Middle Frontal Gyrus, left superior temporal gyrus, and increased in the right cerebellum anterior lobe, and caudate nucleus as compared to Non‐AD CI group (p < 0.001). In addition, ReHo decreased in the right insula and left middle temporal gyrus (p < 0.001). Dynamic fluctuations of CSF Tau were observed to be associated with changes in FC between VN and PCC, FC of SMN, as well as the altered ReHo in the right insula and left middle temporal gyrus. Compared the AD group with the non‐AD CI group, the aforementioned altered functional brain connectivity, with the exception of FC in the PCC and VN, was significantly associated with a decrease in CSF Aβ1‐42.
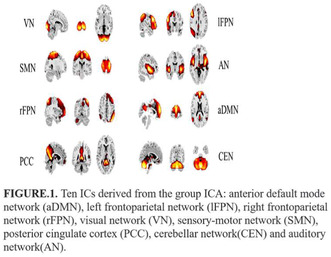
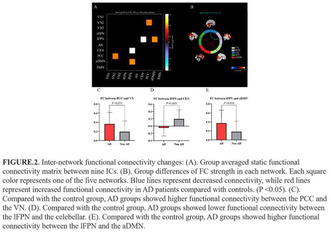
Conclusion: These functional changes in AD patients are linked to the variations of Tau protein and Aβ1‐42 in CSF, with Aβ1‐42 having a particularly large impact on brain network function.
Disclosure: Nothing to disclose.
EPO‐423
Neuroinflammation biomarkers and clinical progression in amnestic mild cognitive impairment due to Alzheimer's disease
G. Giuffrè 1; S. Citro2; D. Quaranta2; M. Vita2; N. Martellacci1; P. Calabresi2; C. Marra1
1Memory Clinic, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy; 2Institute of Neurology, Catholic University of the Sacred Heart, Rome, Italy
Background and Aims: Ongoing Alzheimer's disease (AD) research has unveiled a promising range of fluid biomarkers with diagnostic and prognostic potential. In addition to established biomarkers of amyloidopathy (A), tauopathy (T), and neurodegeneration (N), novel biomarkers of inflammation (I) such as soluble Triggering receptor expressed on myeloid cells 2 (sTREM2), chitinase‐3‐like‐1 protein (YKL‐40), and glial fibrillary acidic protein (GFAP) are gaining attention. This study aims to investigate the role of “A”, “T”, “N” and “I” biomarkers in predicting clinical progression in mild cognitive impairment (MCI) due to AD.
Methods: Sixty subjects diagnosed with MCI due to AD underwent a comprehensive clinical evaluation, an extensive neuropsychological assessment, and CSF biomarkers analysis. CSF Aβ42/40 ratio, p‐tau181, total‐tau NfL, sTREM2, YKL‐40 and GFAP were quantified using automated immunoassay systems. After a two‐year follow‐up, forty‐nine subjects were re‐evaluated and classified as “progressors” or “stable” based on clinical progression to dementia.
Results: Twenty‐one subjects were classified as “progressors” and twenty‐eight as “stable”. The two groups exhibited no significant differences in terms of age, literacy and MMSE score at baseline. When comparing CSF biomarker levels between the cohorts, concentrations of p‐tau181, t‐tau, NfL and YKL‐40 were significantly higher in the “progressors” group.
Conclusion: These results confirmed the importance of “T” and “N” biomarkers in predicting AD progression and identified YKL‐40 as a novel potential predictor of cognitive decline since the early stages of AD. Future research should aim on validating these findings in larger cohorts, further exploring the potential role of inflammation biomarkers in refining diagnostics, prognostics, and treatment strategies.
Disclosure: Nothing to disclosure.
EPO‐424
A digitally supported lifestyle program to promote brain health among elderly (LETHE trial): Study design and progress
A. Rosenberg1; H. Untersteiner 2; A. Guazzarini3; M. Bödenler4; J. Bruinsma5; B. Buchgraber‐Schnalzer4; M. Colombo6; R. Crutzen5; A. Diaz7; D. Fotiadis8; H. Hilberger4; S. Huber4; N. Kaartinen9; T. Kassiotis8; M. Kivipelto10; J. Lehtisalo1; V. Loukas8; J. Lötjönen11; M. Pirani6; C. Thunborg10; S. Hanke4; F. Mangialasche10; P. Mecocci3; E. Stögmann2; T. Ngandu1
1Population Health Unit, Finnish Institute for Health and Welfare, Helsinki, Finland; 2Department of Neurology, Medical University of Vienna, Vienna, Austria; 3Department of Medicine and Surgery, Section of Gerontology and Geriatrics, University of Perugia, Perugia, Italy; 4eHealth Institute, FH JOANNEUM University of Applied Sciences, Graz, Austria; 5Department of Health Promotion, Care and Public Health Research Institute, Maastricht University, Maastricht, The Netherlands; 6Innovation2Grow (i2G), Milan, Italy; 7Alzheimer Europe, Luxembourg, Luxembourg; 8Biomedical Research Institute, Foundation for Research and Technology – Hellas, FORTH‐BRI, Ioannina, Greece; 9Kaasa Solution GmbH, Düsseldorf, Germany; 10Division of Clinical Geriatrics, Center for Alzheimer Research, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Solna, Sweden; 11Combinostics Ltd, Tampere, Finland
Background and Aims: The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) multimodal lifestyle intervention yielded cognitive benefits in elderly at risk of dementia. The two‐year multinational randomized controlled LETHE trial evaluates the feasibility of a digitally supported, adapted FINGER intervention among at‐risk older adults.
Methods: The trial includes older adults (60–77 years) with digital readiness and increased dementia risk without substantial cognitive impairment. Participants are enrolled at four sites (Austria, Finland, Italy, Sweden). They were randomized in a 1:1 ratio to: 1) the intervention group (structured multimodal lifestyle program where in‐person activities are supported with the LETHE App); or 2) the control group (self‐guided program with simplified App and no personalized content). All participants wear smartwatches to gather passive data. Primary outcomes are retention/adherence and change in dementia risk scores. Secondary and exploratory outcomes include changes in lifestyle, cognition, stress, sleep, and dementia‐related biomarkers. A sub‐study explores the feasibility of novel interactive technology (audio glasses, social robot).
Results: Recruitment took place between September 2022 and June 2023. In total, 156 individuals were randomized (mean age 69 years, 65% women). Vascular/lifestyle risk factors were common (e.g., 65% with hypertension, 39% physically inactive). The trial will be completed by summer 2025. Retention until the first post‐baseline visit (after 6 months) is high (n = 2 discontinued).
Conclusion: LETHE provides crucial information about the feasibility of technology and a digitally supported FINGER program. Digital tools specifically designed for older adults could offer potential for large‐scale, cost‐effective prevention programs. The trial is registered at ClinicalTrials.gov (NCT05565170).
Disclosure: AR, HU, AG, MB, JB, BBS, RC, AD, DF, HH, SiH, TK, MK, JeL, VL, CT, StH, FM, PM, ES, and TN declare that they have no disclosures. MC and MP are employed by Innovation Grow. NK is employed by Kaasa Solution GmbH. JyL is employed by Combinostics Ltd. The LETHE project has received funding from the European Union's Horizon 2020 research and innovation programme under grant agreement no 101017405.
EPO‐425
Comparing oral anticoagulants for dementia risk in atrial fibrillation: A network meta‐analysis
J. Hsu 1; Y. Li2; C. Loh1; Y. Tu3
1Center for Aging and Health, Hualein Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan; 2Department of Pharmacy, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan; 3Institute of Epidemiology and Preventive Medicine, College of Public Health, National Taiwan University, Taipei, Taiwan
Background and Aims: Atrial fibrillation (AF) is a potentially modifiable risk factor for dementia. Research has shown that oral anticoagulant (OAC) use may lower dementia risk in patients with AF. However, few studies have discussed dementia risk in patients with AF who receive different OACs.
Methods: This systematic review and network meta‐analysis included randomized controlled trials (RCTs) and observational studies investigating the dementia risk in patients with AF, who were and were not administered OACs. We included studies in which patients received non‐vitamin K antagonist oral anticoagulants (NOACs), warfarin, and non‐OAC users. p‐Scores were used to determine the ranking of the association between OAC use and dementia risk.
Results: We analyzed data from 1,096,125 patients (10 RCTs and nine cohort studies). The dementia risk was lower in patients administered NOACs (edoxaban, rivaroxaban, apixaban, dabigatran) and warfarin than in non‐OAC users. When compared to warfarin, all NOACs (edoxaban 0.68, 95% CI: 0.54‐0.87; rivaroxaban 0.77, 95% CI: 0.65‐0.91; apixaban 0.80, 95% CI: 0.66‐0.96; dabigatran 0.83, 95% CI: 0.71‐0.98) exhibited a reduced dementia risk. NOACs did not show statistically significant intergroup differences. Edoxaban (p‐score = 0.927) ranked highest in the association of reducing dementia risk in AF patients, followed by rivaroxaban, apixaban, and dabigatran.
Conclusion: The dementia risk was lower in NOAC and warfarin users than non‐OAC users, and all NOACs outperformed warfarin. There were no statistically significant differences observed between different NOACs. These findings might highlight that NOAC (particularly edoxaban) administration may be preferred to minimize dementia risk in patients with AF.
Disclosure: Nothing to disclose.
EPO‐426
Effect of long‐term exercise and lifestyle multidomain interventions on cognition in older adults: A meta‐analysis
I. Reparaz‐Escudero 1; M. Izquierdo1; H. Bischoff‐Ferrari2; M. Lopez Saez de Asteasu1
1Navarrabiomed, Hospital Universitario de Navarra (HUN)‐Universidad Pública de Navarra (UPNA), IdiSNA, Pamplona, Spain; 2Center on Ageing and Mobility, University Hospital and University of Zurich, Zurich, Switzerland
Background and Aims: Emerging evidence suggests that multidomain lifestyle strategies including physical exercise may be effective the prevention of dementia. Observational data supports a protective role of physical activity in preserving cognition, yet randomized controlled trials (RCTs) examining physical exercise interventions provide unclear results, potentially due to short‐term designs. We investigated the effect of long‐term physical exercise and multidomain interventions on the global cognition of older adults.
Methods: Databases of Pubmed, WoS, CINAHL and PsychInfo were systematically searched from inception to May 1, 2023. RCTs enrolling non‐demented, community‐dwelling older adults (≥55 years) that assessed the effect of long‐term (≥12 months) exercise or multidomain interventions on any validated global cognition measure were included. Random‐effects inverse‐variance meta‐analysis with the Hartung‐Knapp‐Sidik‐Jonkman adjustment was performed. Standardized mean differences (SMD) and 95% confidence intervals were calculated. Risk of bias and publication bias were assessed by the Cochrane Risk‐of‐Bias‐2 tool, and Luis Furuya‐Kanamori Index (LFKi), respectively. The certainty of the evidence was assessed with GRADE.

Flow chart of the literature adapted from PRISMA guidelines.
Results: We included 12 trials with 9,165 participants (mean age 73.3 [±4.3] years; 64.8% women). The overall risk of bias was low and minor presence of publication bias was observed for exercise (LFKi: 1.9) and multidomain interventions (LFKi: 2.0). Exercise interventions yielded a non‐significant effect on global cognition, SMD = 0.05 (95% CI: ‐0.02 to 0.12, p = 0.15), while multidomain strategies had a small beneficial effect, SMD = 0.09 (95% CI: 0.01 to 0.17, p = 0.04).
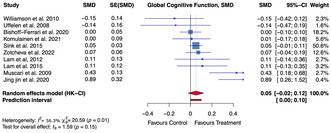
Forest plot showing the effect of long‐term physical exercise interventions on global cognitive function. SMD, Standardized Mean Difference. SE, Standard Error. HK‐CI, Hartung‐Knapp confidence intervals.
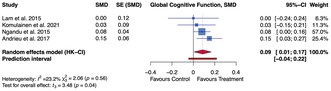
Forest plot showing the effect of long‐term multidomain interventions on global cognitive function. SMD, Standardized Mean Difference. SE, Standard Error. HK‐CI, Hartung‐Knapp confidence intervals.
Conclusion: Moderate certainty evidence supports a small impact of multidomain approaches inclusive of physical exercise for the prevention of cognitive decline in the older population.
Disclosure: Nothing to disclose.
EPO‐427
Association between neuropsychiatric symptoms and biomarkers of Alzheimer's disease
I. Carvalho1; F. Gomes1; D. Valente2; C. Fernandes1; F. Millet Barros1; C. Bernardes 1; P. Faustino1; J. Durães1; M. Lima1; I. Baldeiras1; M. Tábuas‐Pereira1; I. Santana1
1Neurology Department, ULS Coimbra, Coimbra, Portugal; 2Neurology Department, Centro Hospitalar do Algarve, Faro, Portugal
Background and Aims: Neuropsychiatric symptoms (NPS) are frequent in patients with Alzheimer's disease (AD). The association between AD pathophysiology and NPS remains unclear. Understanding the biological mechanisms of NPS in AD can expand our understanding and improve treatment. Aim: Evaluate the association between NPS and the levels of AD biomarkers [CSF amyloid‐β protein (Aβ42), total tau (t‐tau) and phosphorylated‐tau (p‐tau)] and serum Neurofilament light chain (NfL) in patients with AD.
Methods: We performed a cross‐sectional study, including patients with the diagnosis of AD, supported by CSF biomarkers. The presence of NPS was assessed with Neuropsychiatric Inventory (NPI) and Frontal Behavioral Inventory (FBI) through a structured interview with the patient and the caregiver. Global cognition was evaluated with Mini‐Mental State Examination (MMSE).
Results: We included 60 patients (72.0% female). Average age of onset was of 64.3 (±6.8). Median education was 4.0 (IQR = 5.0). Aβ42 was correlated with NPI apathy (r = −0.56, p = 0.001), FBI loss of spontaneity (r = −0.54, p = 0.003), personal neglect (r = −0.44, p = 0.019), loss of insight (r = −0.48, p = 0.010) and incontinence (r = −0.51, p = 0.005). Aβ42/Aβ40 was correlated with indifference (r = 0.41, p = 0.033), personal neglect (r = 0.38, p = 0.045), disorganization (r = 0.38, p = 0.045), perseveration (r = 0.38, p = 0.42) and agitation (r = 0.39, p = 0.039). P‐tau was correlated with NPI nocturnal behavior (r = 0.259; p = 0.047).
Conclusion: Lower levels of CSF Aβ42 were associated with the presence of apathy, loss of spontaneity, personal neglect and loss of insight. Differential relationships between Aβ42 and Aβ40 and some NPS may reflect the different rates of parenchymal vs vascular deposition, and comorbid cerebral amyloid angiopathy, meriting further studies.
Disclosure: Nothing to disclose.
EPO‐428
Plasma biomarkers profiles in Alzheimer's disease and Parkinson's disease
B. Fernandes Gomes1; K. Johansen 2; F. Gonzalez‐Ortiz1; B. Kirsebom3; H. Zetterberg1; T. Fladby4; K. Blennow1
1Department of Psychiatry and Neurochemistry, Institute of Neuroscience and Physiology, the Sahlgrenska Academy at the University of Gothenburg, Mölndal, Sweden; 2Department of Neurology, Akershus University Hospital, Lørenskog Norway; 3Department of Neurology, University Hospital of North Norway, Tromsø, Norway; 4Oslo University, Institute for Clinical Medicine, Campus Ahus, Norway
Background and Aims: Plasma biomarkers are accessible tools that are lacking in neurodegenerative diseases, especially in Parkinson's disease (PD). Biomarkers like phospho‐tau217 (p‐tau217) and brain‐derived tau (BD‐tau) have proven to be accurate and robust for Alzheimer's disease (AD) diagnosis. Similarly, glial fibrillary acidic protein (GFAP) and neurofilament light chain (NfL) have been proposed as biomarkers, predicting conversion to dementia and neuronal damage, respectively. To better characterize these biomarkers profiles and their relationship, our goal was to evaluate the levels of plasma p‐tau217, BD‐tau, NfL, and GFAP in PD and AD.
Methods: Plasma p‐tau217, BD‐tau, NfL, and GFAP were measured using SIMOA in patients with PD (n = 108) and AD (n = 220), as well as cognitively normal (NC) controls (n = 157).
Results: We found increased levels of p‐tau217 and BD‐tau in AD, and decreased levels in PD, compared to CN (p < 0.001). GFAP was increased in AD, compared to NC, but not in PD (p < 0.001). NfL was markedly increased in PD (p < 0.001), however with a large variability within the group, while being unchanged in AD, compared to NC. Correlations were found between p‐tau217 and NfL, and the Trailmaking test part B (TMT‐B) (r = 0.22, p = 0.001, r = 0.24, p < 0.001, respectively) in the AD, and NfL and Unified Parkinson's Disease Rating Scale (UPDRS) (r = 0.3, p = 0.01) in PD. Markers were also highly correlated between each other in both AD and PD.
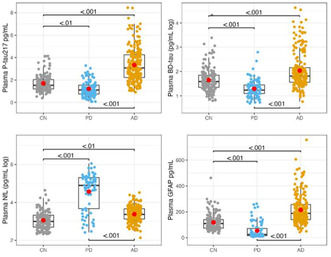
Plasma p‐tau217, BD‐tau, NfL, and GFAP levels in CN, AD, and PD individuals.
Conclusion: We found that p‐tau217, BD‐tau and GFAP are increased in AD, while increased NfL levels were associated with PD, with associations with motor and cognitive impairment.
Disclosure: Nothing to disclose.
Motor neurone diseases
EPO‐429
Takotsubo syndrome in a Sardinian amyotrophic lateral sclerosis cohort
A. Maccabeo; M. Pateri; F. Pili; M. Puligheddu; G. Borghero
Department of Medical Sciences and Public Health, Institute of Neurology, University Hospital D. Casula Monserrato, Cagliari, Italy
Background and Aims: Amyotrophic lateral sclerosis (ALS) is known to be associated with varying degrees of autonomic and cardiovascular dysfunction. Recent case reports showed that ALS may be linked to Takotsubo syndrome (TTS), an acute heart failure syndrome characterized by left ventricular dysfunction with a peculiar pattern, resulting in apical ballooning. Here we reported and described five ALS patients who developed TTS.
Methods: We retrospectively examined a ten‐year incident ALS cohort (2010‐2019), identified patients who developed TTS and described their clinical characteristics.
Results: Our Sardinian cohort included 344 ALS patients and five of them (1.45%) developed TTS. All were female and their median onset age was 71.5 years (IQR 62.75‐77). No relevant genetic mutation was detected. Three patients had spinal and two bulbar onset, though all had bulbar involvement and were at an advanced stage of disease (ALSFRS ≤ 25, King's ≥3) at TTS diagnosis. We identified a potential physical and emotional TTS trigger in four patients (hospitalization for pneumonia, tracheostomy, PEG placement). Survival time was variable (up to 25 months after TTS).
Conclusion: TTS is not an infrequent condition in ALS and may influence these patients’ prognosis. Female sex, bulbar involvement and later age of onset may be important risk factors for developing this cardiac condition and a physical or psychological trigger is often observed. Despite autonomic dysfunction in ALS has been demonstrated, the precise physiopathological mechanism underlying TTS needs to be furtherly clarified.
Disclosure: Nothing to disclose.
EPO‐430
Vitamin D levels and disease severity in ALS patients
A. Alungulese 1; I. Catalina Alvarez1; E. Trasobares Iglesias2; A. Lozano Ros1; J. Muñoz Blanco1
1Department of Neurology, Gregorio Marañón General University Hospital, Madrid, Spain; 2Gregorio Marañón Health Research Institute, Madrid, Spain
Background and Aims: The hypothesis that vitamin D may play a role in ALS disease mechanisms stems from pre‐clinical studies and epidemiological findings in other neurological diseases. The objective of this study was to determine the levels of vitamin D in ALS patients compared with those in control subjects and correlate the levels of vitamin D with disease severity.
Methods: Vitamin D levels were measured in 45 ALS subjects and 45 controls. We estimated associations with ALSFRS‐R scores by multivariate linear regression using data from baseline visit. As potential confounders were considered: age, gender, ethnicity, body mass index, smoking, history of performing physical exercise, vitamin D supplements, site of symptom onset, diagnostic delay, familial ALS cases.
Results: The majority of ALS subjects (73.3%) had levels below the recommended level of 30 ng/ml. Vitamin D levels in ALS patients were slightly lower than those in control subjects by a mean difference of −9.5 ng/ml; 95% CI (−15.0; −4.0). Demographics, body mass index, smoking, history of performing physical exercise, site of symptom onset, diagnostic delay did not differ across strata of baseline vitamin D level. The association between vitamin D and ALSFRS‐R total scores did not appreciably change after adjusting for multiple baseline clinical characteristics.
Conclusion: We found that people with ALS had vitamin D levels below the recommended level in line with other reports in neurodegenerative disease. Worse severity score at baseline due to vitamin D deficiency, however, is unlikely based on our study.
Disclosure: Nothing to disclose.
EPO‐431
Ulnar CMAP and MUNE in adult SMA patients treated with nusinersen
A. Frączek 1; E. Sobieszczuk1; A. Potulska‐Chromik1; A. Łusakowska1; K. Aragon‐Gawińska1; M. Burlewicz2; Z. Gierlak‐Wójcicka2; A. Kostera‐Pruszczyk1
1Department of Neurology, Medical University of Warsaw, Warsaw, Poland; 2Department of Neurology, University Hospital, Warsaw, Poland
Background and Aims: Spinal muscular atrophy (SMA) is a progressive disease leading to motor neuron loss. Nusinersen treatment in adult patients can halt disease progression. Improvement of compound muscle action potential (CMAP) and estimation of the number of motor units (MUNE) in nusinersen‐treated pediatric SMA patients were demonstrated by some authors.
Methods: 17 adult patients with SMA type 2 (N = 1) or 3 (N = 16)(35.3%F) treated with nusinersen were included in the study, 70.6% of patients were walkers. Sex‐ and age‐matched healthy volunteers served as the control group (HC). All the patients were assessed at baseline, 6th, 14th months of treatment and consecutive infusions with functional scales (Hammersmith Functional Motor Scale Expanded‐HFMSE or CHOP‐INTEND and Revised Upper Limb Module‐RULM) and CMAP, multipoint incremental MUNE, single motor unit potential (SMUP) of the abductor digiti minimi (ADM). The duration of observation was 30‐50 months.
Results: CMAP and MUNE were significantly lower in SMA patients than in HC (p < 0.001); SMUP was significantly higher in SMA patients than in HC (p < 0.001). We have observed decrease in mean CMAP and MUNE in SMA patients at 6 months in the first year of treatment, since 14th month of treatment there was an increase and followed by stabilization of those parameters but there was no significant difference between baseline evaluation of CMAP and MUNE and evaluation at next infusions. Only SMUP value was significantly higher after six months in comparison with baseline value (p = 0.039).
Conclusion: Nusinersen treatment stabilizes CMAP, MUNE and SMUP after 6 months of treatment in SMA adults with SMA2‐3 observed for up to 50 months.
Disclosure: Anna Kostera‐Pruszczyk ‐ honoraria for advisory boards, speaking at educational events for Biogen, Novartis/AveXis, PTC and Roche, support for congress participation: Biogen, Roche, Novartis; institutional grant support from Biogen Anna Potulska‐Chromik ‐ honoraria for speaking at educational events for Biogen, Abbvie, PTC and Roche, support for congress participation: Biogen, Novartis Anna Łusakowska ‐ honoraria for speaking at educational events for Biogen, Roche, support for congress participation: Biogen, Roche Anna Frączek ‐ honoraria for speaking at educational events for Biogen, Roche, support for congress participation: Biogen, Roche Karolina Aragon‐Gawińska ‐ ‐ honoraria for speaking at educational events for Biogen, Roche, PTC, support for congress participation: Biogen, Roche, PTC Małgorzata Burlewicz, Zuzanna Gierlak‐Wójcicka – speaker at the conferences and meetings organized by Biogen, Roche, support for congress participation: Biogen, Roche Ewa Sobieszczuk – nothing to disclose.
EPO‐432
Iron metabolism‐genetic interplay in an ALS cohort: A single‐center study
B. Risi 1; B. Labella2; F. Caria1; S. Damioli1; E. Bertella1; L. Poli3; L. Ferullo2; E. Olivieri2; I. Bianchi4; A. Padovani2; I. Zanella5; M. Filosto6
1NeMO‐Brescia Clinical Center for Neuromuscular Diseases, Brescia, Italy; 2Department of Clinical and Experimental Sciences, University of Brescia; Unit of Neurology, ASST “Spedali Civili” of Brescia, Italy; 3Unit of Neurology, ASST “Spedali Civili” of Brescia, Italy; 4Medical Genetics Laboratory, ASST "Spedali Civili" of Brescia, Italy; 5Department of Molecular and Translational Medicine, University of Brescia; Medical Genetics Laboratory, ASST "Spedali Civili" of Brescia, Italy; 6Department of Clinical and Experimental Sciences, University of Brescia; NeMO‐Brescia Clinical Center for Neuromuscular Diseases, Brescia, Italy
Background and Aims: Impaired iron metabolism has been observed in ALS, but it is not known whether it is a cause or a consequence of the disease. The aim of our study is to investigate the interplay between iron homeostasis and ALS by analysing a panel of iron‐related genes.
Methods: 20 ALS patients (male, n = 12) were tested for common variants in iron‐related genes, among which the p.Asp358Ala variant in the IL6R (interleukin 6‐receptor) gene, known to increase soluble IL6‐R levels. Patients were dichotomized into carriers (both heterozygous and homozygous) and non‐carriers; all underwent blood sampling for measurement of iron‐related molecules. Adjusted ANCOVA and correlation analysis and linear regression (with site of onset, sex, age and disease duration as independent variables) were performed.
Results: Median ferritin levels were 424.2 ng/ml in men (UNL: 400) and 192.4 ng/ml in women (UNL: 150), with 55% of patients having higher than normal levels. Higher ferritin levels were associated with the group of bulbar*fast progressor patients (p = 0.012) and correlated with the disease progression rate [DPR] (r = 0.518, p = 0.028). The IL6R358Ala variant carriers had lower ferritin levels than non‐carriers (p = 0.023). In the multivariate analysis, this variant was found to be the only predictor of ferritin levels (p = 0.013).
Conclusion: Our preliminary results may suggest a role of the IL6R358Ala variant in reducing ferritinemia. This could be explained by a kind of “buffering” system mediated by higher s‐IL6‐R levels, dampening the pro‐inflammatory IL‐6 signalling. These findings may help to better define the relationship between iron metabolism abnormalities and clinical features in ALS.
Disclosure: The authors have no potential conflict of interest to disclose.
EPO‐433
Evaluation of clinical effectiveness of edaravone in the treatment of amyotrophic lateral sclerosis in Uzbekistan
C. Rustamova; M. Yakubova
Neurology department, Doctor M clinic, Tashkent, Uzbekistan, Kichik khalqa yuli street, Takhtapul
Background and Aims: Amyotrophic lateral sclerosis (ALS) is a progressive, neurodegenerative disease of the central nervous system. Despite the positive outcome of clinical trial of edaravone for treatment of ALS, there are limitations which makes it difficult for clinicians to prescribe the drug with an expectation of efficacy. Our study aims to investigate the clinical efficacy of edaravone in the treatment of ALS in Uzbek patients.
Methods: We examined 36 patients with ALS, aged from 24 to 78 years, who were hospitalized between 2019 and 2023. Patients were divided into 2 groups: 1) main group: 25 (70%) patients who received Edaravone; 2) control group: 11 (30%) patients who received standard ALS treatment. All patients underwent a standard examinations: clinical and neurological examination; Electroneuromyography; ALS‐FRS‐Revised functional rating scale before and after treatment.
Results: The incidence of clinical symptoms in ALS before treatment with edaravone was reduced by 27% after the treatment of edaravone. The incidence of clinical symptoms in ALS before treatment with standard therapy was reduced by 15% after the treatment of standard therapy (p < 0.005). According to ALS‐FRS‐R scale, scale index in the patients treated with edaravone significantly increased by 21% (40 +0.93) and the scale index in the patients treated with standard therapy increased by 11% (37+ 0.74), (p < 0.001). According to ENMG parameters, the maximum amplitude of the M‐response increased for all nerves in the edaravone group compared to the control group (p < 0.005).
Conclusion: Our research showed that 60% of patients with ALS show positive dynamics in the initial stage of focal motor disorders in the treatment with edaravone. The use of edaravone in the therapy of ALS was highly effective, especially in the early stages of the disease, in cervico‐thoracic and bulbar forms of ALS.
Disclosure: Nothing to disclose.
EPO‐434
Retrospective study of a cohort of patients with amyotrophic lateral sclerosis from the University of Pisa
C. Meoni; C. Carlesi; F. Bianchi; L. Becattini; L. Fontanelli; G. Vadi; B. Giovannini; G. Siciliano
Department of Clinical and Experimental Medicine, Neurological Clinic, University of Pisa, Pisa, Italy
Background and Aims: Amyotrophic Lateral Sclerosis (ALS) is a neurodegenerative disorder that involves upper and lower motor neurons. Different phenotypes are possible, with sometimes differences in survival. According to the epidemiological data, bulbar subtypes show a more rapid progression and shorter survival, compared to the spinal subtypes. The objective of our study was to analyze the survival of a cohort of patients with ALS across the different disease phenotypes.
Methods: All patients diagnosed, according to the Gold Coast Criteria, with ALS from January 2021 to January 2024 at our Center for Motor Neuron Disease were retrospectively evaluated. None had been excluded from the study, but 13 patients had been lost during follow‐up, thus were excluded from the Kaplan‐Meier analysis.
Results: A total of 99 patients were enrolled (median age: 65.1 ± 11.5; 46.5% female). Among them, 73.8% had a spinal onset (57.4% male), 25.3% had a bulbar onset (64% female). The time hiatus between the disease onset and diagnosis was 18.6 ± 18.7 months on average (14.2 ± 12 months for bulbar onset, and 21.1 ± 21.2 months for spinal onset). The number of dead patients was 25 (36% of bulbar onset; 22% of spinal onset). The disease duration was on average 34 ± 23 months (28 ± 15 months for the bulbar form, 37 ± 25 months for the spinal form).
Conclusion: Our data are in line with those reported in literature. Patients stratification can help in identify prognostic factors and epidemiological data that may improve clinical, diagnostic, and therapeutic management of this complex disease.
Disclosure: Nothing to disclose.
EPO‐435
Lower Gas6 levels are associated with bulbar phenotype and faster disease progression in ALS patients
F. De Marchi 1; D. Apostolo2; L. Ferreira2; D. D'Onghia2; F. Vincenzi2; L. Mazzini1; M. Bellan2
1ALS Center, Neurology Unit, Department of Translational Medicine, University of Piemonte Orientale, Novara, Italy; 2Department of Translational Medicine, Università del Piemonte Orientale, Novara, Italy
Background and Aims: Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disorder that primarily affects the motor neurons in the brain and spinal cord. While the exact cause of ALS is not fully understood, a combination of genetic and environmental factors is believed to contribute to its development. Research into the etiology and pathogenesis of ALS is ongoing, and we investigated the role of Growth Arrest‐Specific 6 (Gas6) as a possible contributor. This vitamin K‐dependent protein has been recognized to enhance survival of oligodendrocytes and neurons and, it has been associated with different kinds of (neuro) inflammatory conditions.
Methods: We conducted a prospective observational study including 65 ALS patients aimed to assess whether circulating serum levels of Gas6 and its soluble receptors (sAxl, sMer, sTyro‐3) along with neurofilaments (NfLs) could represent a disease marker in ALS patients.
Results: In our ALS cohort, lower serum levels of Gas6, and concomitantly higher levels of NfL, were associated with a more aggressive disease, expressed with bulbar phenotype (p‐value for Gas6: 0.03) and faster progression (p‐value for Gas6: 0.03). Also, serum Gas6 can well distinguish (area under the curve, cut‐off 13.70 ng/mL, sensitivity 69.57%, specificity 72.72%) between fast and slow progressors.
Conclusion: Due to neuroprotective properties, our data suggest that Gas6, could be an intriguing biomarker in ALS patients.
Disclosure: No disclosure.
EPO‐436
Validation of the Czech and Slovak versions of questionnaires used to monitor the clinical status of patients with ALS
L. Joppekova 1; A. Betik1; D. Baumgartner2; R. Mazanec2; M. Turcanova‐Koprusakova3; I. Martinka4; E. Vlckova1
1Department of Neurology, ERN‐EURO NMD Centre, University Hospital Brno, Czechia; 2Department of Neurology, 2nd Faculty of Medicine, Charles University in Prague and Motol University Hospital, Czechia; 3Department of Neurology, Jessenius Medical Faculty of Comenius University and University Hospital Martin, Slovakia; 4Ružinov Hospital, University Hospital Bratislava, Slovakia
Background and Aims: This multicentre study aimed to validate Czech and Slovak versions of several questionnaires used to monitor patients with amyotrophic lateral sclerosis (ALS). The following scales and questionnaires were used: the ALS Functional Rating Scale – Revised (ALSFRS‐R) and its extended version (ALSFRS‐R‐EX), the ALS Assessment Questionnaire ‐ 40 items (ALSAQ‐40), the Borg scale for breathlessness intensity, and the Dysphagia in ALS (DYALS) scale for dysphagia symptoms. Both the clinician‐administered version of the ALSFRS‐R and the self‐administered version were compared.
Methods: All questionnaires and scales were translated using the forward‐backward method. The first administration was made during clinical follow‐up in four major Czech or Slovak neuromuscular centres (Brno, Prague, Bratislava, Martin), with a repeat administration by telephone after seven days. In both cases, the self‐administered version of the ALSFRS‐R was used. One week later, the ALSFRS‐R+ EX questionnaires were administered again by telephone in a non‐self‐administered version.
Results: The study involved 62 ALS patients (34 men) and showed excellent questionnaire comprehension in both languages. Statistical analysis revealed no significant differences in scores between administrations, confirming excellent reproducibility and high internal consistency (Cronbach's alpha around 0.98). The intraclass correlation coefficient ranged from 0.905 to 0.994, indicating high agreement between different versions and/or administrations of the questionnaires.
Conclusion: The Czech and Slovak versions of all tested ALS‐related questionnaires show high patient comprehensibility, internal consistency and reproducibility between repeated administrations, and excellent agreement between self‐administered and clinician‐administered versions of the ALSFRS‐R questionnaire.
Disclosure: The authors declare no conflict of interest regarding this study.
EPO‐437
Analysis of C9orf72 repeat expansions in Georgian patients with amyotrophic lateral sclerosis
M. Kekenadze 1; C. Rocca1; V. Turchetti1; N. Kvirkvelia2; S. Vashadze3; E. Kvaratskhelia4; M. Beridze4; R. Kaiyrzhanov1; H. Houlden1
1University College London, Queen Square Institute of Neurology, London, UK; 2Tbilisi State University; 3Batumi Shota Rustaveli State University; 4Tbilisi State Medical University
Background and Aims: Amyotrophic lateral sclerosis (ALS) is a fatal progressive neurodegenerative disorder that affects the upper and lower motor neurons. Several genetic risk factors have been identified in the past decade with a hexanucleotide repeat expansion in the C9orf72 gene being the most significant. However, the presence of C9orf72 repeat expansion has not been examined in the Transcaucasian region, therefore we aimed to analyze its frequency in Georgian patients with ALS.
Methods: We included 74 self‐reported Georgian patients with ALS from different parts of the country, fulfilling the Gold Coast criteria. To investigate the presence of an expanded GGGGCC hexanucleotide repeat in the non‐coding region of the C9orf72 gene, we performed Repeat‐Primed PCR (RP‐PCR).
Results: In total, 74 sporadic and two familial ALS cases were identified. Patients were aged 26 to 84 years with a mean age of 58.3 years at disease onset. Bulbar onset was observed in 21.88%, upper limb onset in 34.38%, and lower limb onset in 43.75% of the patients. Frontotemporal dementia (FTD) fulfilling the Strong criteria was diagnosed in seven patients (10.94%). C9orf72 repeat expansion was detected in only one case using RP‐PCR; the patient had a family history of dementia.
Conclusion: Our results indicate that C9orf72 hexanucleotide expansion does not belong to the major genetic risk factor of ALS in Georgian patients. Further genetic studies in a bigger study population are needed to reveal the genetic causes of ALS in the Transcaucasian population.
Disclosure: Nothing to disclose.
EPO‐438
Basal metabolism, myokine levels and disease severity in amyotrophic lateral sclerosis
M. Goglia 1; E. Frezza1; G. Greco1; F. Gruosso1; G. Vietri1; I. Petitta1; G. Nardino1; L. Boffa1; A. De Lorenzo2; R. Massa1
1Neuromuscular Diseases Unit, Department of Systems Medicine, Tor Vergata University of Rome, Rome, Italy; 2Section of Clinical Nutrition and Nutrigenomic, Department of Biomedicine and Prevention, University of Tor Vergata, Rome, Italy
Background and Aims: Amyotrophic lateral sclerosis (ALS) can be considered as a multisystemic disease affecting metabolism and body composition. Abnormal resting energy expenditure (REE) has been reported in ALS patients and could be linked to variations in circulating myokine levels. The aim of this study is to investigate metabolic impairment and plasma myokine levels and their possible connection with disease progression.
Methods: ALS patients underwent ALS‐functional rating scale‐revised (ALS‐FRS‐R), MRC sum score and blood detection of myokines (irisin, IL‐6) and 181pTau. Indirect calorimetry and dual‐X‐ray absorptiometry (DEXA) were performed on the same day to assess REE and body composition, respectively.
Results: We enrolled 10 patients and 10 healthy controls. At indirect calorimetry 8 patients were hypometabolic. REE, normalized with fat free mass, directly correlated with irisin levels. We found no correlations between either REE or irisin and functional scales of disease severity, whereas pTau levels were increased in patients (p < 0.05) and inversely correlated with MRC sum score (p < 0.05). IL‐6 directly correlated with disease duration (p < 0.05) and inversely correlated with MRC sum score (p < 0.05).
Conclusion: Basal metabolism alterations are present in ALS and irisin can be linked to them, independently on disease severity. Conversely, pTau and IL‐6 could be indicators of disease progression and severity. Further investigations are required to clarify whether metabolic abnormalities could have a role in ALS pathogenesis and disease progression or represent a consequence of secondary muscle wasting. Moreover, myokines such as irisin could be useful to investigate alterations of resting metabolic state.
Disclosure: Nothing to disclose.
EPO‐439
Study of anthropometric parameters in patients with amyotrophic lateral sclerosis (ALS)
E. Malhina; V. Haliyeyskaya; Y. Rushkevich; I. Pashkouskaya; S. Likhachev
Republican Scientific and Practical Center of Neurology and Neurosurgery, Minsk, Belarus
Background and Aims: Subclinical loss of muscle mass and subcutaneous fat in ALS patients is one of the reasons for the delayed diagnosis of latent protein‐energy malnutrition (PEM).
Methods: The study included 49 ALS patients (13 (26%) men, 36 (74%) women), 62.0 [51.0; 67.0] years, BMI 25.2 [23.0; 28.0]. Me duration of the disease 13.2 [9.3; 19.7] months. Me of ALSFRS 46.0 [42.0; 47.0]. The control group 30 patients (10 (33%) men, 20 (67%) women) without neuromuscular pathology, 56.0 [47.0; 61.0] years, BMI 29.7 [25.5; 31.9]. There was no statistical difference in age, gender and BMI.
Results: Significant decreases in circumferences were found in ALS patients (Table 1). Almost all measured parameters among ALS patients were significantly lower (U, p < 0.05) compared with the control group. No significant reduction in circumference above the ankle was revealed, that is probably due to the hidden edema in ALs patients, which is one of the clinical signs of PEM. The waist circumference in patients with ALS showed good quality of the diagnostic model, AUC = 0.732±0.08 (95%CI0.575‐0.856), p = 0.006. The threshold value of waist circumference is ≤98 cm, sensitivity 80%, specificity 67% (Figure 1).
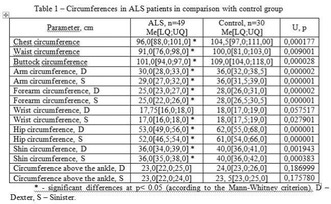
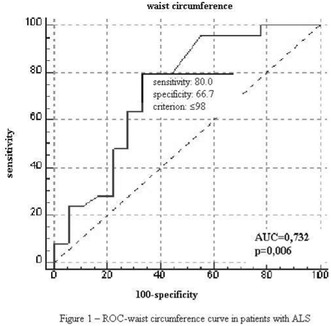
Conclusion: Despite the early stages of the disease, the preservation of functional capabilities significant decrease in circumferences were found, that indicates a progressive loss of muscle mass and subcutaneous fat in ALS patients. According to the ROC‐analysis in ALS patients with an AUC value greater than 0.7, the threshold level of waist circumference sensitivity is over 80% and can be considered objective sign of PEM.
Disclosure: The authors have nothing to disclose.
EPO‐440
Early diagnosis of ALS using near‐fiber EMG
O. Garnes‐Camarena 1; I. Mahillo‐Fernandez2; O. Lorenzo2; P. Martinez‐Ulloa1; R. Mandeville3; D. Stashuk4
1Jimenez Diaz Foundation University Hospital, Madrid, Spain; 2Jimenez Diaz Foundation Research Institute, Madrid, Spain; 3Beth Israel Deaconess Medical Center, Boston, MA, USA; 4Systems Desing Engineering, University of Waterloo, Ontario, Canada
Background and Aims: Amyotrophic lateral sclerosis is characterized by rapid and progressive motor neuron lesions. The continuous process of denervation and reinnervation is manifested in EMG signals as changes in motor unit potential (MUP) size, temporal dispersion (complexity) and instability. Current methods to assess temporal dispersion and instability are either indirect (MUP turns, jiggle) or time‐consuming (single fiber jitter). Near‐Fiber EMG (NF‐EMG) is a novel way to assess the size, temporal dispersion, and instability of routinely recorded MUPs directly and quantitatively in a semi‐automated manner.
Methods: 1441 MUs in 60 muscles of 10 patients at the time of ALS diagnosis (Gold Coast criteria) were sampled using NF‐EMG. MUP area and duration and NF‐MUP dispersion and segment jitter were studied.
Results: On average, 49.1% of MUs showed increased NF‐MUP dispersion and 53.7% exhibited increased NF‐MUP segment jitter, whereas 31% of MUs had both increased NF‐MUP dispersion and instability. Interestingly, 27% and 30% of MUs with normal sized MUPs had increased NF‐MUP dispersion and segment jitter, respectively (3 and 2 times higher than in control subjects), indicating the capability of NF‐EMG to detect electrophysiological abnormalities at early stages of the disease.
TABLE 1 Percentage of MUs with increased temporal dispersion (NFM_Disp) and instability (NFM_SJ). Compared with control subjects, a significant percentage of MUs with normal sized MUPs showed increased NFM_Disp and/or increased NFM_SJ.
Conclusion: Near Fiber EMG can effectively characterize the functional status of a motor unit, by providing novel and useful information about the degree, stability, and course of denervation and/or reinnervation.
Disclosure: Nothing to disclose.
EPO‐441
Elevated serum MCP‐2 and TARC are associated with increased risk of death in Guamanian ALS patients
R. Chowdhury1; L. Shteynman2; E. Culver3; S. Azam4; M. Azam 5; R. Garruto6; K. Wander6
1College of Behavioral and Community Sciences, University of South Florida, Tampa, FL, USA; 2Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, USA; 3Colorado Center for Personalized Medicine, University of Colorado‐Anschutz Medical Campus, Aurora, CO, USA; 4University at Buffalo School of Medicine and Biomedical Sciences, Buffalo, NY, USA; 5SUNY Upstate Norton College of Medicine, Syracuse, NY, USA; 6Department of Anthropology, Binghamton University (SUNY), Binghamton, NY, USA
Background and Aims: This study explores the relationship between inflammation and longevity in post‐WWII Guam amyotrophic lateral sclerosis (ALS). Characteristics of this focus include sudden high incidence and long lifespan in some cases. Understanding longevity in Guamanian ALS may help elucidate causal pathways and novel therapeutic targets. This research evaluates inflammation in bio‐banked Guamanian ALS patient serum to understand the relationship between immunoregulator levels and survival time.
Methods: Sera from 69 Guam ALS cases collected within early years of onset by NIH researchers from 1958‐1990 were evaluated for 11 regulators of inflammation, using custom multiplex cytokine and single‐plex CRP ELISA. Survival analysis with Cox proportional hazards models was used to determine factors associated with time to death.
FIGURE 1 C‐reactive Reactive Protein ELISA of Guamanian ALS sera.
Results: Factor 2 (MCP‐2 and TARC) was associated with a 38% increase in risk of death (HR: 1·38, 95% CI [1·19, 1·65], p: 0·00). Individually, MCP‐1 (HR: 1·03, 95% CI [1·004, 1·06], p: 0·02), MCP‐2 (HR: 1·24, 95% CI [1·08, 1·44], p: 0·00), IFN‐γ (HR: 2·34 95% CI [1·25, 4·36], p: 0·01), IP‐10 (HR: 1·18, 95% CI [1·065, 1·312], p: 0·00), IL‐6 (HR: 1·05, 95% CI [0·998, 1·108], p: 0·06), and TARC (HR: 1·03 95% CI [1·013, 1·044], p: 0·00), were also associated with increased risk of death.
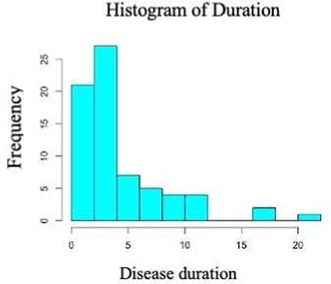
FIGURE 2 Distribution of disease duration: Cases represent a broad range of survival times (1‐22 years, n = 69).
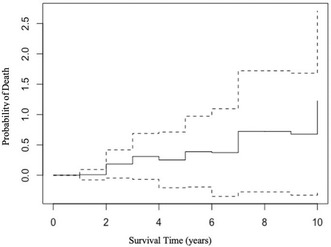
FIGURE 3 Increased probability of death with increase of Factor 2 (MCP‐2 & TARC): Horizontal lines in Kaplan‐Meier curve depict duration of survival; vertical lines depict change in probability of death; intermittent lines represent 95% confidence intervals.
Conclusion: Results suggest increased inflammation in Guamanian ALS is associated with shortened lifespan. Assessing serum levels of MCP‐2 and TARC in early stages of disease may predict severity and duration in sporadic ALS. Research on the relationship between pathways associated with TARC, MCP‐2 in ALS warrants further investigation.
Disclosure: Nothing to disclose with regard to conflicts of interest. Institutional Board Review (IRB) and Ethics disclosure: As all participant are deceased Binghamton University IRB has classified this as non‐human subjects research, which does not require IRB approval. However, at time of collection, all specimens were obtained with informed written consent from patients following ethical standards set forth by the 1947 Nuremburg Code, the 1965 Declaration of Helsinki, and the 1974 Belmont Report. This research is consistent with the original use for which the samples were collected. All samples included in study were collected prior to 1985 when ALS was still highly prevalent on Guam.
EPO‐442
Exploring glymphatic system function in the ALS‐FTD spectrum
T. Russo 1; E. Spinelli2; T. Domi1; P. Schito3; Y. Falzone3; F. Agosta4; A. Quattrini1; M. Filippi5
1Experimental Neuropathology Unit, Institute of Experimental Neurology (INSPE), Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 3Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; 4Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; Vita‐Salute San Raffaele University; 5Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute; Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute; Vita‐Salute San Raffaele University
Background and Aims: Growing evidence suggests that glymphatic function is impaired in patients with several neurodegenerative diseases and neuroinflammation is thought to be entangled with glymphatic function. However, there are few available in vivo data about glymphatic function in patients with amyotrophic lateral sclerosis and/or frontotemporal dementia (ALS‐FTD).
Methods: We measured serum levels of osteopontin, a neuroinflammatory biomarker which is thought to be produced by perivascular cells, in a cohort of patients with ALS and FTD, as well as in age‐matched healthy controls, and correlated it to clinical features.
Results: Osteopontin serum levels correlated with age and were higher in ALS patients compared to healthy controls. Patients with higher osteopontin serum levels had a trend for a shorter survival.
Conclusion: We confirmed that osteopontin levels are higher in ALS patients compared to controls and correlate with a worse prognosis. Correlation with MRI data will provide information about 1) glymphatic function in patients with ALS‐FTD and 2) osteopontin association with glymphatic function.
Disclosure: Nothing to disclose.
EPO‐443
Progression of cognitive impairment in ALS: Preliminary findings from a longitudinal monocentric study in Italy
V. Bettoni 1; G. Fiamingo2; S. Schillaci1; M. Collesi3; S. Cappa4; E. Ballante3; L. Diamanti5
1Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; 2UOC Neurologia ASST Bergamo Est, Seriate, Italy; 3IRCCS Mondino Foundation, Pavia, Italy; 4University School for Advance Studies IUSS, Pavia, Italy; 5Neuro‐oncology unit, IRCCS Mondino Foundation, Pavia, Italy
Background and Aims: The presence of cognitive and behavioral impairment in patients affected by Amyotrophic Lateral Sclerosis (ALS) is now well‐established. However, there is no agreement about the worsening of cognitive deficits during disease progression, and the few longitudinal studies on the topic provided inconclusive results. This monocentric, longitudinal study aims at evaluating the cognition at the time of ALS diagnosis and after 12 months.
Methods: 62 Italian subjects (F:M = 0.44; age 63.51 ± 12.46y) with a diagnosis of ALS were subjected to a standardized neuropsychological evaluation at diagnosis through the Edinburgh Cognitive and Behavioral ALS Screen (ECAS) test, the Story‐based Empathy Task (SET) test, and the Ekman 60‐faces test. The evaluation was repeated after 12 months.
Results: In the overall study population, cognitive decline, as defined by ECAS abnormalities, was observed in 13 subjects (20.97%). Some alterations in emotions recognition emerged from Ekman test (mean 45.49, sd 6.88). Only 27 subjects could be assessed at the second time‐point (F:M = 0.22; age 63.81, sd 12.99y). In this follow‐up population, cognitive decline at ECAS was observed in 5 subjects at T0 (18.51%) and in 7 subjects at 12‐months assessment (25.92%). Changes of ECAS, SET or Ekman test scores after 12 months were not statistically significant.
Conclusion: These preliminary results do not show progression of cognitive impairment. This could be influenced by the small sample size and by the attrition bias in the longitudinal study population (i.e. subjects with a better disease course being over‐represented amongst the ones reaching the follow‐up visit). More detailed data analysis is still ongoing.
Disclosure: Nothing to disclose.
Coma and chronic disorders of consciousness
EPO‐444
The functional communication measures for assessing communicative abilities in prolonged disorders of consciousness
A. Magliacano 1; M. Spinola2; C. Fasano2; B. Campana2; A. Estraneo1
1IRCCS Fondazione Don Carlo Gnocchi ONLUS, Florence, Italy; 2Polo Specialistico Riabilitativo Fondazione Don Carlo Gnocchi ONLUS, Sant'Angelo dei Lombardi (AV), Italy
Background and Aims: The present cross‐sectional study aimed to investigate the ability of the validated Italian version of the shortened Functional Communication Measures (sFCM) in assessing communication in individuals with severe Acquired Brain Injury (sABI) with and without prolonged Disorders of Consciousness (pDoC).
Methods: Participants: 17 sABI patients consecutively admitted to our sABI Rehabilitation Unit (males = 11; mean age = 60.4±15.3 years; pDoC = 7). Variables collected: i. demographic and anamnestic information at study entry; ii. Levels of Cognitive Functioning (LCF), Disability Rating Scale (DRS), Functional Oral Intake Scale (FOIS) scores, and Coma Recovery Scale‐Revised (CRS‐R) scores only in patients with pDoC; iii) sFCM scores administered independently by two blinded examiners.
Results: The sFCM inter‐rater agreement ranged from perfect to substantial. The sFCM correlated significantly with LCF, DRS and FOIS scores (all p < 0.05). In the subgroup of patients with pDoC, the oral comprehension on sFCM correlated significantly with the CRS‐R motor subscore (ρ = .794; p = 0.017). Specifically, patients with higher CRS‐R motor subscore were classified by the sFCM as being able to execute simple commands or answer with a “yes/no” code to contextual questions with consistent and maximal facilitation, although they did not meet the CRS‐R criteria for consistent command following.
Conclusion: We confirmed that sFCM are a solid and easy‐to‐administer tool for assessing communication abilities in fully conscious sABI patients. For the first time, we found that the sFCM are able to stratify patients with pDoC based on their language abilities more accurately than the CRS‐R.
Disclosure: Nothing to disclose.
EPO‐445
Clinical improvements following transcutaneous auricular vagal nerve stimulation in acute disorders of consciousness
V. Marie1; E. Remacle1; P. Cardone1; A. Regnier1; O. Gosseries1; N. Lejeune1; J. Annen1; D. Martin3; D. Ledoux2; A. Thibaut 1
1Coma Science Group, University of Liège, Belgium; 2Intensive Care Unit, University Hospital of Liège, Belgium; 3Department of Neurosurgery, University Hospital of Liège, Belgium
Background and Aims: Patients with disorders of consciousness (DoC) are a challenging population lacking effective treatment options. Among neuromodulation techniques, trans‐auricular vagal nerve stimulation (taVNS) may act through a bottom‐up manner to modulate thalamo‐cortical connectivity and promote the recovery of consciousness.
Methods: We are conducting the first randomized placebo‐controlled double‐blind clinical trial employing taVNS in 44 acute DoC. Patients randomly receive either 5 days of active bilateral vagal stimulation (45 min; 3mA; 200‐300μs current width, 25Hz) or sham stimulation. Behavioural (Coma Recovery Scale‐Revised, CRS‐R) measures are collected at baseline and at the end of the treatment.
Results: Preliminary results on 30 patients show a significant difference in the behavioral score evolution (post vs pre) between the active and sham groups following the 5‐day treatment period (W = 150; p = 0.014). Patients in the active taVNS group showed significantly increased CRS‐R total scores post‐treatment compared to baseline (median pre‐treatment = 8 [5]; median post‐treatment = 11 [12]; V = 4.5; p = 0.021), while patients from the sham group did not display such difference (median pre‐treatment = 6.5 [6.25]; median post‐treatment = 6.5 [3]; V = 16; p = 0.83). Moreover, in the active group (n = 14), 7 patients displayed a new sign of consciousness and 4 improved their diagnosis, among which 3 even emerged from DoC. In the placebo condition (n = 16), 2 patients improved and only one changed diagnosis.
Conclusion: Our results show that repeated taVNS might promote consciousness recovery in the early phase following severe brain injury. This study will contribute to define the role of taVNS for the treatment of these challenging conditions and identify patients’ clusters for responses to treatment.
Disclosure: None.
EPO‐446
Rehabilitation of language and swallowing abilities in patients with severe brain injury: An online international survey
A. Regnier1; O. Gosseries1; E. Mélotte1; S. Gillet2; P. Cassar3; B. Hakiki4; A. Estraneo4; A. Magliacano4; R. Formisano5; C. Schnakers6; S. Majerus7; E. Noé8; R. Llorens8; L. Navarro Pérez8; K. Fufaeva9; Z. Bottaeva9; P. Maurer‐Karattup10; C. Aubinet 1
1Coma Science Group, GIGA Consciousness, University of Liège, Belgium; 2Department of Speech‐Language Pathology, Faculty of Psychology and Educational Sciences, University of Liège, Belgium; 3Hospital Mater Dei, Day Centres, Elderly Homes, Msida, Malta; 4IRCCS Fondazione Don Carlo Gnocchi ONLUS, Florence, Italy; 5Post‐Coma Unit, IRCCS and Neuroreabilitation, Fondazione Santa Lucia, Rome, Italy; 6Research Institute, Casa Colina Hospital and Centers for Healthcare, Pomona, CA, USA; 7Department of Psychology, Psychology and Cognitive Neuroscience Research Unit, University of Liège, Belgium; 8IRENEA‐Instituto de Rehabilitación Neurológica, Fundación Hospitales Vithas, Valencia, Spain; 9Clinical and Research Institute of Urgent Pediatric Surgery and Traumatology, Moscow, Russian Federation; 10SRH Fachkrankenhaus Neresheim, Neresheim, Germany
Background and Aims: Patients with severe brain injury and disorders of consciousness (DoC) are unable to communicate and frequently experience severe dysphagia. The DoC Special Interest Group of the International Brain Injury Association (IBIA) created a survey to identify the tools that are used by (speech‐language) therapists, detect their needs and possibly identify new practices to improve language and swallowing rehabilitation in post‐comatose patients.
Methods: The survey was developed based on the following structure: (1) Study presentation, (2) Socio‐demographic information, (3) General questions regarding speech and language therapies (4) Swallowing assessment and management, (5) Language/communication assessment and management, and (6) Conclusion. The English questionnaire was then translated into 6 other languages, transferred to the Alchemer platform, and massively diffused.
Results: Preliminary data highlight the profile of therapists involved in the rehabilitation of language and swallowing abilities after coma, their degree of concern regarding the assessment and management of such abilities in this specific population, their recommendations as well as the tools they preferentially use in their practice.
Conclusion: This survey highlights the lack of guidelines for speech‐therapy practice in patients with severe brain injury and DoC. Early and long‐term assessment and management of both language and swallowing abilities should be improved, notably by providing (and/or adapting) new clinical tools.
Disclosure: Nothing to disclose.
EPO‐447
Hyperintense basal ganglia on T1‐MRI in two patients with elevated serum manganese due to cirrhosis
A. Tüfekçi 1; S. Şahin2
1Department of Neurology, Faculty of Medicine, Recep Tayyip Erdogan University, Rize, Turkey; 2Department of Neurology, Faculty of Medicine, Recep Tayyip Erdogan University, Rize, Turkey
Background and Aims: Hepatic encephalopathy is a neuropsychiatric complication of acute or chronic liver disease with symptoms ranging from mild confusion to coma. The pathophysiology of hepatic encephalopathy is multifactorial, ammonia, manganese deposition and inflammation are thought to lead to astrocyte swelling and brain edema. Studies have shown that in patients with end‐stage liver disease, increased serum manganese level causes manganese to accumulate in the basal ganglia.
Methods: Patient 1. A 68 ‐year ‐old female patient had a diagnosis of liver cirrhosis secondary to non‐ alcoholic steatohepatity and twice history of hepatic encephalopathy attacks. Neurological examination was unremarkable. The serum manganese level was high and the magnetic resonance images had T1 basal ganglion hyperintensity. Patient 2. A 65 ‐year ‐old male patient was detected amnesia, disorientation of time and space and psychomotor retardation. His serum manganese level was high and the magnetic resonance images had T1 basal ganglion hyperintensity. Liver cirrhosis was diagnosed after the investigations.
Results: Studies have shown a significant correlation between serum manganese levels and T1 basal ganglia hyperintensity seen on MRI, but no correlation between serum manganese and liver function or neurological findings has been demonstrated. Also, there is no correlation between T1 basal ganglia hyperintensity and neurological findings.
Conclusion: It would be useful to evaluate brain MRI and serum manganese levels in the hepatic encephalopathy clinic in patients with cirrhosis.
Disclosure: Nothing to disclose.
EPO‐448
Epileptic seizures in prolonged disorders of consciousness: Preliminary data of an Italian multicentre study
B. Hakiki 1; A. Grippo1; S. Pancani1; A. Romoli1; F. Draghi1; D. Maccanti1; A. De Nisco1; T. Toci1; R. Burali1; M. Scarpino1; A. Magliacano2; A. Estraneo2; A. Comanducci3; J. Navarro3; C. Tramonti4; P. Baldi4; C. Macchi1; F. Cecchi1
1IRCCS Fondazione Don Carlo Gnocchi ONLUS, Firenze; 2Polo Specialistico Riabilitativo, Fondazione Don Carlo Gnocchi, Sant'Angelo Dei Lombardi; 3IRCCS “S. Maria Nascente” – Fondazione Don Carlo Gnocchi, Milano; 4Polo Riabilitativo del Levante Ligure, Fondazione Don Carlo Gnocchi, La Spezia
Background and Aims: The occurrence of late‐onset epileptic seizures (LES) and epileptiform abnormalities (EA) in prolonged Disorders of Consciousness (pDoC) was poorly and inconsistently reported across studies1. Our aim is to explore the LES/AE prevalence and their influence on consciousness recovery 3 months after admission to rehabilitation units (RUs) in pDoC.
Methods: This analysis was performed in the Italian multicentre PRABI study framework2 including only patients with a pDoC. At admission, the repeated Coma Recovery Scale‐Revised‐CRS‐R and a standard electroencephalogram were performed3. The occurrence of LES was monitored during the RUs stay. The Disability Rating Scale‐DRS, the Glasgow Outcome Scale Extended‐ GOSE and the CRS‐R was performed at 3 months.
Results: One hundred eighty‐six patients were enrolled (Table 1). At admission, patients presenting LES and/or EA were those with a higher Cumulative Illness Rating Severity Scale at admission (p = 0.040) and a higher Acute ES probability (p = 0.008). At 3 months, these patients reached lower scores of CRS‐R (p = 0.004), DRS (p < 0.001), and less frequently a GOSE > 5 (p = 0.03)). The univariate and multivariate analyses showed the Minimally Conscious State instead of Unresponsive wakefulness syndrome, a lower time post onset, and the absence of LES during the RUs stay were associated with a higher probability to recover consciousness at 3 months (Table 3).
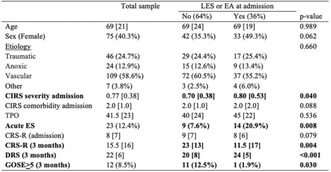
Legend: CIRS: Cumulative Illness Rating Scale; TPO: Time post‐onset; ES: Epileptic Seizures; CRS‐R: Coma Recovery Scale‐Revised; DRS: Disability rating Scale; GOSE: Glasgow Outcome Scale Extended.

Legend: CRS‐R: Coma Recovery Scale‐Revised; MCS: Minimally Conscious State; UWS: Unresponsive wakefulness syndrome; TPO: Time post‐onset; ES: Epileptic Seizures; LES: Late‐onset Epileptic seizures; EA: Epileptic Abnormalities; CIRS: Cumulative Illness Rat.
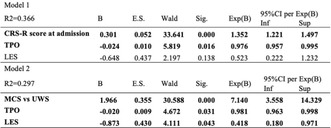
Legend: CRS‐R: Coma Recovery Scale‐Revised; TPO: Time post‐onset; LES: Late‐onset Epileptic seizures; MCS: Minimally Conscious State; UWS: Unresponsive wakefulness syndrome.
Conclusion: The presence of late‐onset epileptic seizures seems to negatively impact the short‐term recovery of consciousness. References: 1 Lejeune, N et al. doi:10.1080/02699052.2021.1973104, 2 Hakiki, B. et al., 10.3389/358fneur.2022.711312, 3 Hirsh L. J. et al.,10.1097/WNP.0000000000000806
Disclosure: The authors report no disclosure.
EPO‐449
Prognostication after cardiac arrest: Which is more accurate EEG or ERPs?
I. Holečková; J. Valeš; D. Štěpánek; V. Přibáň
Department of Neurosurgery, University Hospital and Faculty of Medicine UK, Plzeň, Czechia
Background and Aims: Neurophysiological investigations (ERPs and EEG) occupy major place among the tools available for prognostication the patients resuscitated from CA (cardiac arrest). We tested the relationships between neurological outcome after CA (measured by GOS) and ERPs and EEG results measured in coma patient's state.
Methods: All 27 patients (17 men, 10 women, mean age 64 ± 15 years) were enrolled prospectively during the ICU admission after CA. Bedside EEG (standard 19/25 EEG channel system according to the 10‐20 system) and ERPs – P3 (with patients own name as deviant stimulus) was recorded in the same day within 4‐8 days of CA in unsedated patients who were still comatose during the examination. The resulting state was assessed between 30 ‐ 64 days after arrest by GOS. The PPV, NPV, sensitivity and specificity of EEG (4 patterns) and ERPs – P3 own name (absence, presence) in relation to GOS were calculated.
Results: The presence of ERPs ‐ P3 own name had a high specificity (81%) and sensitivity (67%) for GOS 4‐5. Absence of P3 own name also had high specificity (67%) and sensitivity (81%) for GOS 1‐2. EEG pattern burst suppression and low voltage pattern had high specificity (90%) but low sensitivity (43%) for GOS 1‐2. The delta/theta EEG pattern had low sensitivity (33%) and specificity (33%) for GOS 1‐2.
Conclusion: Therefore, ERPs – P3 own name appear to be more advantageous than EEG for prognostication of patients after CA.
Disclosure: Nothing to disclose.
EPO‐450
Quantum 123 pattern: A new quantum graph‐based encephalopathy detection using EEG signals
I. Tasci 1; T. Tuncer2; B. Tasci3; S. Dogan2; G. Akca Tasci4; C. Demir1
1Firat University/Medical School, Department of Neurology, Elazig, Turkey; 2Firat University/Department of Digital Forensics Engineering, College of Technology, Elazig, Turkey; 3Firat University/Vocational School of Technical Sciences, Elazig, Turkey; 4Fethi Sekin State Hospital/Department of Psychiatry, Elazig, Turkey
Background and Aims: The primary aim of our study is to explore the capability of machine learning in detecting encephalopathy through the analysis of electroencephalography (EEG) signals. To achieve this, we have introduced a novel quantum‐inspired feature extractor and a self‐organized feature engineering model.
Methods: In this investigation, we retrospectively gathered a substantial EEG signal dataset from Firat University Hospital. The dataset consists of two classes: (i) encephalopathy and (ii) no‐findings/control. EEG signals were acquired from 54 participants using a multichannel EEG device and segmented into 15‐second intervals. For automated encephalopathy detection, our proposed self‐organized feature engineering model comprises four main phases: (1) Quantum 123 Pattern (Q123Pat) feature extraction, utilizing a graph resembling quantum circuits to select the most suitable feature extraction method based on the EEG signal structure; (2) feature selection with the neighborhood component analysis feature selector to identify the most informative features; (3) classification using k‐nearest neighbors and support vector machine classifiers; and (4) information fusion employing iterative majority voting and selecting the best outcome with a greedy algorithm. The Q123Pat‐based self‐organized model was applied to each EEG channel, and the results were used to generate a semantic cortex map.
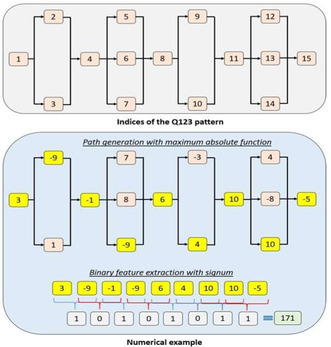
FIGURE 1 The proposed Q123 pattern. In this graph, there are 36 ( = 1×2×3×1×2×3) patterns, and the most suitable pattern has been selected using the maximum absolute function.
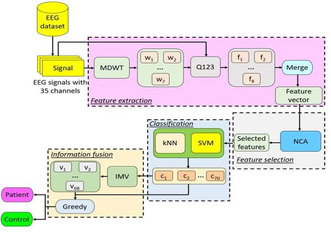
FIGURE 2 Graphical explanation of the proposed Q123‐based model. Herein, MDWT: multilevel discrete wavelet transform, w: wavelet band, f: individual feature vector, NCA: neighborhood component analysis, kNN: k‐nearest neighbors, SVM: support vector machine.
Results: The proposed Q123Pat‐based self‐organized model achieved an impressive 97.96% classification accuracy, facilitating the identification of the most informative channels.
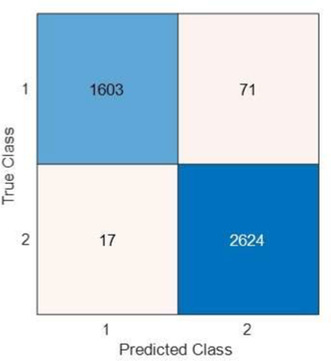
FIGURE 3 Confusion matrix of the final result. Herein, 1: Encephalopathy, 2: No‐finding. Per this confusion matrix, the calculated classification performance metrics have been given follows. Accuracy: 97.96%, sensitivity: 95.76%, specificity: 99.36%, precision.
Conclusion: The computed classification performances unequivocally demonstrate the ability of machine learning models to detect encephalopathy using EEG signals. Furthermore, our model provides interpretable results about the cortex by generating a cortex map based on the classification performances of each channel.
Disclosure: Nothing to disclose.
EPO‐451
Exploring the neurophysiological effects of combined electrical and auditory stimulation in healthy subjects
M. Louras 1; R. Panda1; A. Soria‐Frisch2; R. Salvador2; G. Ruffini2; M. Nitsche3; S. Laureys1; M. Carrière1; G. Martens1; N. Lejeune1; A. Thibaut1
1Coma Science Group, GIGA‐Consciousness, University of Liège, Liège, Belgium; 2Starlab Barcelona SL, Barcelona, Spain; 3Department Psychology and Neurosciences, Leibniz Research Centre for Working Environment and Human Factors, Dortmund, Germany
Background and Aims: Today, effective treatments for patients suffering from disorders of consciousness are lacking. Transcranial direct current stimulation (tDCS) and music have both shown promise in enhancing signs of consciousness. Given the potential for tDCS effects to be enhanced by complementary stimuli, this study aims to investigate its combination with music in a cohort of healthy participants at the cognitive and neurophysiological levels.
Methods: This randomized controlled double‐blind crossover study involved four stimulation conditions: tDCS combined with music (tDCS/music) or white noise (tDCS/noise), and sham‐tDCS with music (sham‐tDCS/music) or white noise (sham‐tDCS/noise), which were applied to 24 healthy human adults ( < 35 years old). Participants’ performance (i.e., accuracy and time response) on Stroop and 3‐back cognitive tests was measured before and after each condition. A 20‐channel electroencephalogram explored the neurophysiological effects of the interventions.
Results: Cognitive performance (behavioral measures) and power spectral analyses revealed no significant differences between the interventions. A significant increase in global connectivity in the alpha band was found in post‐ compared to pre‐intervention in music (p = 0.0026) and tDCS/music (p = 0.0028) conditions. The other conditions did not show any significant changes.
Conclusion: Overall, these findings suggest that a single tDCS session combined with music does not enhance cognitive functions in healthy subjects. However, music alone or combined with tDCS exhibited promise in increasing brain activity associated with cognitive performance. Further research, particularly involving multiple sessions of tDCS with or without music, is necessary to better understand the potential of these interventions, especially in patients with disorders of consciousness.
Disclosure: Nothing to disclose.
EPO‐452
A closed‐loop EEG‐tDCS approach to improve responsiveness of patients in minimally conscious state
M. Khosravi 1; A. Barra1; G. Martens1; D. Ibáñez‐Soria2; K. Chugani2; A. Soria‐Frisch2; A. Piarulli3; O. Gosseries1; N. Lejeune1; R. Salvador4; E. Kroupi2; M. Nitsche5; S. Laureys1; G. Ruffini4; A. Thibaut1
1Coma Science Group, GIGA Consciousness, University of Liège, Liège, Belgium; 2Starlab Barcelona SL, Barcelona, Spain; 3Department of Surgical, Medical, Molecular and Critical Area Pathology, University of Pisa, Italy; 4Neuroelectrics, Barcelona, Spain; 5Department of Psychology and Neurosciences, Leibniz Research Centre for Working Environment and Human Factors, Dortmund, Germany
Background and Aims: Previous studies have reported mixed effects of transcranial direct current stimulation (tDCS) in patients in a minimally conscious state (MCS). Considering the potential impact of vigilance level on the effectiveness of stimulation, we aimed to compare the efficacy of closed‐loop tDCS applied during high, low, and random levels of vigilance (based on online entropy measurements) in MCS patients.
Methods: In this double‐blind randomized clinical trial, we aim to include 16 MCS patients. Each patient received three stimulation sessions (2mA for 20 minutes) over the left dorsolateral prefrontal cortex (DLPFC) at high, low, and random levels of vigilance, five days apart. Real‐time analysis of spectral entropy was performed using a Starstim 20 EEG‐tDCS closed‐loop system which determined the triggering time of stimulation based on vigilance level. Patients were evaluated using the Coma Recovery Scale‐Revised (CRS‐R) before and after each session, together with a 15‐minute EEG. Pre‐ and post‐tDCS CRS‐R scores were compared using Wilcoxon test.
Results: We included 13 MCS patients (mean age 48±18 years, 5 females). Median CRS‐R score for high vigilance stimulation was 11 (8‐15) before, and 12 (10‐15.25) after stimulation (p = 0.037). The median pre‐ and post‐stimulation CRS‐R scores were not significantly different for the low vigilance (11 [8‐15] vs. 11 [8‐16], p = 0.88) and random vigilance groups (10 [8‐15] vs. 11 [8‐17], p = 0.33).
Conclusion: These preliminary results suggest that stronger effects of tDCS over the left DLPFC in patients with MCS might be achieved if applied at high vigilance levels. This needs to be confirmed with the entire sample (n = 16), where EEG data will also be analyzed.
Disclosure: MAN serves in the scientific advisory boards of Neuroelectrics and Precisis.
EPO‐453
Ketamine to treat disorders of consciousness: A feasibility study
P. Cardone1; A. Bonhomme1; V. Bonhomme2; N. Lejeune1; C. Staquet2; A. Defresne2; N. Alnagger1; P. Ezan3; M. Lee4; A. Piarulli5; S. Van Goethem6; J. Montupil2; A. Thibaut1; C. Martial1; O. Gosseries 1
1Coma Science Group, GIGA‐Consciousness, University of Liège, Belgium; 2Anesthesia and Perioperative Neuroscience, GIGA‐Consciousness, University of Liège, Belgium; 3Psychedelic Society Belgium; 4Department of Biomedical Software Engineering, The Catholic University of Korea, Bucheon, Korea; 5Department of Surgical, Medical, Molecular, Pathology and Critical Care Medicine, University of Pisa, Pisa, Italy; 6William Lennox Rehabilitation Center, Ottignies, Belgium
Background and Aims: Patients with post‐comatose disorders of consciousness (DoC) have few treatment options, making the investigation for new ones fundamental. We present the results of a feasibility study using sub‐anaesthetic doses of ketamine in DoC patients. Ketamine increases brain complexity, and this, according to several theories, should ameliorate DoC consciousness level.
Methods: We ran a double‐blind, placebo‐controlled, cross‐over study (Figure 1) on 3 male patients with DoC (UWS, 32yo, TBI; MCS‐, 50yo, subarachnoid haemorrhage; MCS+, 62yo, CO intoxication). We administered increasing concentration of ketamine or placebo intravenously (maximal concentration: 0.75 μg mL‐1; steps of 0.15 μg mL‐1) in two sessions within a week. Consciousness was assessed behaviourally using the Simplified Evaluation of CONsciousness Disorders (SECONDs). We tested spastic paresis with the Ashworth‐Modified Scale (MAS) for two patients. Simultaneously, we recorded EEG (BrainVision, 128Ch) to measure whole‐brain complexity with broadband Lempel‐Ziv complexity (LZC).
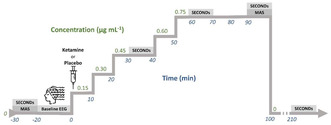
FIGURE 1 Protocol: Visual representation of one session. We assessed behavior via the SECONDs, and spastic paresis with the MAS. During the whole experiment, we recorded the brain activity using high‐density EEG. The second session would take place with.
Results: The UWS patient showed a response to a verbal command once during ketamine, which was not observed during placebo nor at baseline. All patients spent more time with eyes open. Spasticity decreased in all three patients after ketamine (Figure 2). No carry‐over effects or adverse effects were observed. LZC increases during ketamine (Figure 3).

FIGURE 2 Behavioral results. A: SECONDs scores following infusion of ketamine and placebo. UWS scoring are represented as triangles, MCS‐ as squares, MCS+ as diamonds. For representational purposes, ketamine scores were increased by 0.1, and placebo ones.
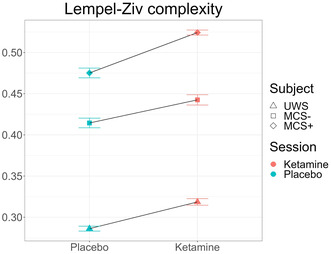
FIGURE 3 Brain Complexity: Distribution of brain complexity measured via whole‐brain LZC shown for placebo and ketamine for each patient. Standard errors are calculated over electrodes.
Conclusion: We demonstrated that ketamine can be safely administered to people with DoC, that it increases arousal and decreases spasticity. Other changes in behaviour should be investigated in a large‐scale randomized controlled trial. Ketamine increases LZC in DoC, like what observed in healthy participants.
Disclosure: VB has had financial relationships with Orion Pharma, Metronic, Elsevier, Edwards Medical, and Grunenthal. The other authors declare no conflict of interest.
EPO‐454
Reflex eye‐opening response in brain death
O. Brengaret Mata 1; G. Mayà1; A. Muñoz‐Lopetegi1; À. Iranzo1; C. Gaig1; J. Osorio Trujillo2; J. Santamaria1
1Neurology Department, Hospital Clinic de Barcelona and Universitat de Barcelona, Barcelona, Spain; 2Pneumology Department, Hospital Clinic de Barcelona and Universitat de Barcelona, Barcelona, Spain
Background and Aims: The diagnostic criteria of brain death include unreactive coma with absent brainstem reflexes. Pain stimulation should not produce responses attributed to the cranial nerves.
Methods: We report the case of a brain‐dead patient with bilateral, slow, partial eyelid opening driven by the autonomic sympathetic response to painful stimulation.

Image 1 and 2: Slow bilateral, partial eyelid elevation response to bilateral painful nipple stimulation.
Results: A 41‐year‐old man was admitted to the ICU after a prolonged cardiorespiratory arrest due to a pulmonary thromboembolism. The neurological examination without sedation after 36 hours revealed a deep unreactive coma and absent brainstem reflexes. However, with bilateral painful nipple stimulation, the patient showed a slow bilateral, partial eyelid elevation, without pupillary size changes and a lack of any motor response. Brain‐CT scan revealed extensive hypoxic‐ischemic lesions, median nerve somatosensitive evoked potentials showed bilateral absence of thalamocortical responses and the EEG was isoelectric. The patient was diagnosed with brain death.
Conclusion: Eye‐opening is determined by the combined action of voluntary and involuntary muscles, the eyelid elevator and the Muller's muscle respectively. The eyelid elevator is innervated by the third cranial nerve originating in the mesencephalon and so, its irrigation depends on the intracranial circulation. In contrast, Muller's muscle is innervated by the sympathetic autonomic nervous system through the petrosal and viridian nerves originating in the superior cervical ganglion, which are irrigated by external carotid artery branches that do not depend on intracranial circulation. Therefore, slow eyelid elevation driven by Muller's muscle may occur in brain‐dead patients due to a pain‐induced activation of the sympathetic nervous system.
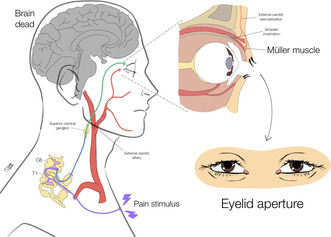
Anatomy of the sympathetic pathway of Müller's muscle.
Disclosure: The authors have nothing to disclose.
EPO‐455
Dynamic network analysis reveals lower temporal variability of functional connectivity at unconsciousness
B. Hakiki1; D. Bartolini1; P. Liuzzi 1; A. Romoli1; F. Draghi1; D. Maccanti1; R. Burali1; T. Toci1; M. Scarpino1; A. De Nisco1; A. di Palma1; A. Grippo1; C. Macchi2; F. Cecchi1; A. Frosini3; A. Mannini1
1IRCCS Fondazione Don Carlo Gnocchi ONLUS; 2Dipartimento di Medicina Sperimentale e Clinica, Università di Firenze; 3Dipartimento di Matematica, Università di Firenze
Background and Aims: Severe Acquired Brain Injuries (sABI) may disrupt networks sustaining arousal and awareness, the two essential components of consciousness leading to atypical connectivity in such cortical/subcortical networks [1]. This study aims to use low‐density EEG and its high temporal resolution to estimate the temporal variability of functional connectivity in prolonged Disorders of Consciousness (pDoC).
Methods: This analysis has been made in the framework of the PRABI study [2] including sABI patients in intensive rehabilitation unit. Consciousness was diagnosed with repetitive Coma Recovery Scale Revised assessments grouping patients between pDoC and emerged sABI patients. EEG was pre‐processed following the PREP pipeline [3]. Debiased weighted Phase Lag Index was computed in the α, θ, and δ bands, at different connection (60%,70%,80%) and electrodes (6, 9, 15, and 19) densities. Burstiness, estimated via the coefficient of variation of the inter‐contact times vector (i.e., temporal difference between two consecutive edges in a binarized adjacency matrix) was compared between groups (Mann‐Whitney tests), Fig.1.
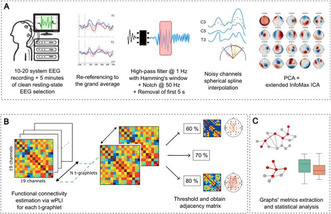
FIGURE 1 Work pipeline: (A) data collection and EEG preprocessing, (B) time‐varying graphs (TVG) development and computation of adjacency matrixes (thresholding), (C) TVG metrics extraction and statistical comparison between pDoC and No‐DoC.
Results: Two‐hundred seventeen sABI patients (median age of 62 years old [IQR = 17.6]; 79 (36.4%) females; 121 (46.4%) eMCS) were included (Tab.1). No significant differences were found for what concerns age, sex, and etiology between the two groups (p > 0.05). Burstiness was always found to be negative, leading to non‐bursty TVGs. However, emerged patients showed larger periodic temporal connectivity pattern variability than pDoC (Fig.2), independently from the frequency band.
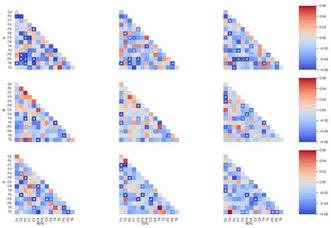
FIGURE 2 Difference in burstiness between the pDoC and the No‐DoC patients for the 15‐electrodes configuration. Each line refers to a bandwidth (α, θ, and δ) with significant differences (p < 0.05) marked with asterisks.
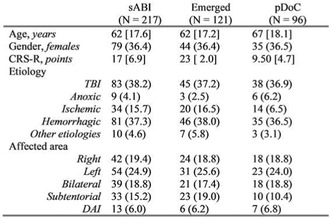
TABLE 1 Population details. Data are presented as follows: numerical variables with median [interquartile range, in brackets], while categorical variables are reported as counts (percentages, in parenthesis).
Conclusion: eMCS patients are confirmed to preserve at all frequencies a higher spatial connectivity patterns’ irregularity than pDoC. Such capability calls for further investigations as a consciousness marker.
Disclosure: Nothing to disclose.
EPO‐456
CSF hydrodynamics in prolonged disorders of consciousness
E. Schmidt 1; J. Pickard2; S. Silva3
1Department of Neurosurgery, University of Toulouse, France; 2Department of Neurosurgery, University Hospital Cambridge, UK; 3Department of Intensive Care, University Hospital of Toulouse, France
Background and Aims: Prolonged (i.e. >1 month) disorders of consciousness (PDOC) after brain injury is a major public health problem. Advances in intensive care allow patients to survive after brain injury, however, one third of patients do not regain consciousness. To date, no specific treatment has been shown to be effective in restoring consciousness. Brain imaging in PDOC patients often shows cerebral atrophy and ventriculomegaly, suggesting hydrocephalus due to impaired intracranial fluid circulation. Controversies remain about how to diagnose hydrocephalus in PDOC patients and whether to propose CSF diversion. We hypothesise that CSF hydrodynamics is relevant to better identify hydrocephalus in PDOC patients.
Methods: We retrospectively analysed 41 patients (26M/15W) with i) acute brain injury, ii) PDOC and iii) ventriculomegaly (i.e. Evan's ratio >0.3). These hydrocephalus‐suspected PDOC patients were studied with a lumbar infusion test to measure CSF hydrodynamics using ICM+.
Results: Acute brain injury was related to: head trauma (17), subarachnoid haemorrhage (16), intracerebral haematoma (6), cardiopulmonary arrest (1), metabolic (1). The mean CSF outflow resistance (Rcsf) was increased (i.e. ≥12 mmHg/ml/min, see Table 1). 20 patients (49%) had increased Rcsf (i.e. ≥12 mmHg/ml/min above the dashed line) several months (up to 40 months) after brain injury (see Figure 1).
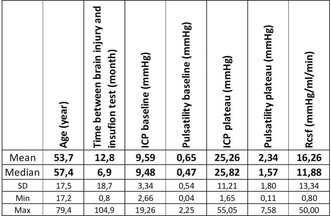
TABLE 1
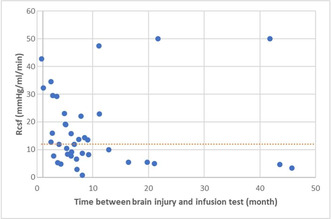
FIGURE 1
Conclusion: Half of the patients with PDOC and ventriculomegaly exhibit altered CSF hydrodynamics. Rcsf seems to be a useful metric that should be implemented in the management algorithm of PDOC patient to better advocate for CSF diversion when hydrocephalus is suspected, even months or years after brain injury.
Disclosure: None.
Infectious diseases
EPO‐457
Meningitis infection: Epidemiological analysis of the disease outcome among Brazilian regions
A. Grande 1; G. Garute Zenatti2; A. Wosniacki Filho2; I. Darella Lorenzin Fernandes Neto2; R. Endler Iachinski2
1Assis Gurgacz University Center – FAG, Cascavel, Paraná, Brazil; 2São Lucas Hospital Center, Cascavel, Paraná, Brazil
Background and Aims: A large number of pathogens cause Meningitis infection (MI), which accounts for more than 200,000 deaths and 2.5 million cases globally in 2019. After introducing the Meningococcal C vaccine into the national vaccination program (1975), Brazil's incidence and mortality rate has decreased over the years.
Methods: Data were available on the National Notifiable Diseases Information System (SINAN). The different outcomes and male/female rate (M/F) among Brazilian regions were searched from 2012‐2023.
Results: MI total cases from 2012‐2023 was 158,111, 58.83% male (M/F rate = 1.42). The Southeast region leads with 53.72% (n = 84,953), followed by the South, Northeast, North, and Central‐West (% = 4.85). The M/F rate medium value was 1.45, highest in the Northeast (M/F = 1.5) and lowest in the Southeast (M/F = 1.93). The discharge rate was 0.85 (n = 134,633). Death by MI rate was 0.10 (n = 16,116), with an increase observed in the North (% = 15.64) and Central‐West regions (% = 13.02), followed by the Northeast, Southeast, and South. Death with MI but by other causes rate was 0.04 (n = 7,362), of which 75.4% was distributed in the Southeast (% = 44.41) and South (% = 30.99).
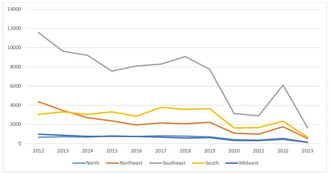
FIGURE 1 Total cases per year between regions.
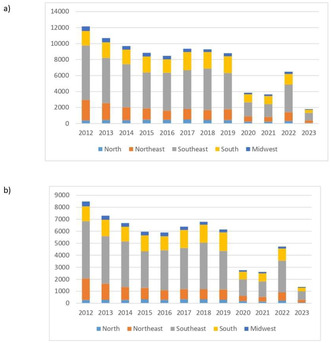
FIGURE 2 (a) Male cases between regions; (b) Female cases between regions.
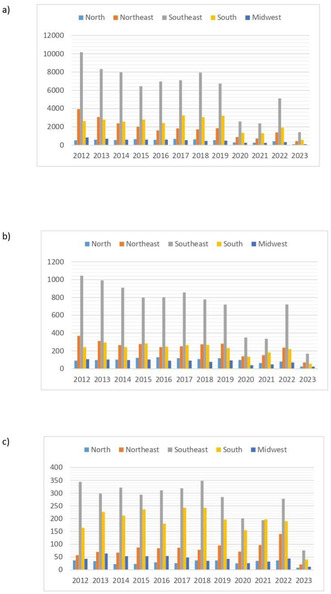
FIGURE 3 (a) Discharge cases between regions; (b) Death by MI between regions; (c) Death by other causes between regions.
Conclusion: A decrease in cases was observed in all regions. Whereas its largest population, the highest prevalence of cases and discharge rate was in the Southeast but it was not the same in the mortality rate, led by the neediest one, North.
Disclosure: Nothing to disclose.
EPO‐458
Dengue‐induced acute cerebellitis
A. Grande 1; A. De Barros Coelho Brandalise1; A. Wunsch Dias1; G. Garute Zenatti2; A. Wosniacki Filho2; I. Darella Lorenzin Fernandes Neto2; R. Endler Iachinski2
1Assis Gurgacz University Center – FAG, Cascavel, Paraná, Brazil; 2São Lucas Hospital Center, Cascavel, Paraná, Brazil
Background and Aims: The incidence of dengue has grown exponentially in recent years and has been associated with several neurological complications, with cerebellar involvement being one of the rarest of them, with few cases found in the literature.
Methods: We present an atypical case, occurring in the south of Brazil, of dengue fever, associated with cerebellar syndrome in a 10‐year‐old child.
Results: A 10‐year‐old child admitted due to a change in gait 3 days ago. Medical history of herpetic encephalitis associated with gait alteration, fever, and emesis 1 month ago, treated with IV Acyclovir for 15 days and with total clinical improvement. No comorbidities, medication, or allergies and no family history of neurological diseases. 15 days later, presented with fever and emesis, and after 2 days, gait alterations. Clinically stable on first assessment, complaining of mild headache and gait ataxia. No acute alterations on neuroaxis MRI and CSF. NS1 (Dengue) laboratory test was positive. After a neuropediatrician consult was suggested a post‐infectious cerebellitis induced by the Dengue virus. After 5 days of Dexamethasone, analgesics, and antiemetics treatment, the patient had progressive improvement in both clinical and motor conditions and was discharged for follow‐up care at an outpatient clinic.
FIGURE 1 Magnetic resonance showing brain parenchyma with usual morphology and signal intensity for the age group.
Conclusion: Cerebellar syndrome in children after or during dengue fever is a rare case, being one of the first cases to be reported in the literature until this report was produced. Therefore, it is important to recognize atypical clinical conditions so that the best measures can be taken early without leaving consequences.
Disclosure: Nothing to disclose.
EPO‐459
Unveiling the Mimic: Progressive multifocal leukoencephalopathy presenting as acute ischemic stroke – A dual case report
A. Ali 1; M. Khan1; S. Munshi1; M. Nawaz2; S. Saleem2; S. Sewilam3
1Nottingham University Hospitals; 2Sandwell and West Birmingham Hospitals; 3Torbay and South Devon NHS Foundation Trust
Background and Aims: Progressive multifocal leukoencephalopathy, a demyelinating infectious disorder of the CNS, is seen in immunocompromised individuals with a history of AIDS, hematologic malignancies, or immunosuppressive drug therapy. We present two cases where patients initially diagnosed with acute ischemic stroke were later identified to have PML, as their symptoms mimicked stroke manifestations.
Methods: 1‐ A 56‐year‐old woman experienced left‐sided numbness escalating to severe weakness in three days. Admission revealed an NIHSS score of 8 and imaging displayed enhancement along the right parietal gyrus. Whole‐body CT raised suspicion of haematological malignancy. Inconclusive tumour marker assessment prompted a PML investigation, confirmed by JC Virus. Unexpectedly, HAART initiation led to IRIS, complicating the clinical course. Despite interventions, rapid deterioration ensued with IRIS‐related complications. 2‐A 79 a patient who present a stroke unit with symptoms that were consistent initially with a posterior circulation stroke. Prior chemotherapy with Rituximab, for a lymphoma, had predisposed the patient to infection with the JC virus.
Results: PML's subacute presentation can mimic a stroke, emphasizing the importance of understanding its background and potential complications, particularly in patients with HIV/AIDS or other immunocompromised conditions. Delayed diagnosis due to the absence of known immunocompromised status underscores the need for heightened awareness and early initiation of antiretroviral therapy.
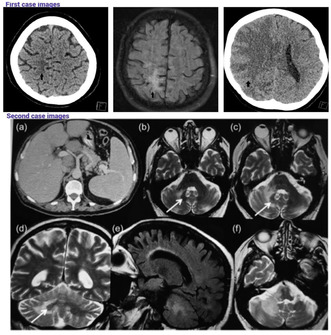
CT scans and MRI findings
CT scans and MRI findings
Conclusion: In the complex realm of diagnoses, PML often masquerades as a stroke look‐alike, demanding nuanced consideration in individuals with HIV/AIDS. Clinicians need a keen eye to distinguish between the two. Those undergoing Rituximab treatment should be made aware of the risk of opportunistic infections, including PML.
Disclosure: Nothing to disclose.
EPO‐460
Acute motor sensory axonal neuropathy as a presentation of Lyme disease
J. Alves; R. Guerreiro; R. Matos; C. Rosado; G. Bonifácio
Department of Neurology, Unidade Local Saude Arrabida EPE, Setubal, Portugal
Background and Aims: Neuroborreliosis affects up to 15% of patients with Lyme disease and usually presents as lymphocytic meningitis, facial nerve palsy or radiculoneuritis. Alternative neurological manifestations are possible, so this diagnosis may easily be overlooked.
Methods: A 36‐year‐old male, previously healthy, presented to the emergency room with abdominal pain radiating to the back, followed by speech changes, incoordination, diplopia, dysphagia, lower limb weakness, loss of sphincter control and respiratory failure needing invasive ventilatory support. Initial neurological assessment additionally revealed left peripheral facial palsy, flaccid areflexic quadriparesis (lower limbs MRC score 2, upper limbs score 4) and decreased pinprick on both feet. CSF analysis revealed 160 cells/μL (95% lymphocytes) and protein level of 268 mg/dL. Atypical Guillain‐Barré Syndrome was assumed, and the patient was started on IV immunoglobulin therapy. Upon reassessment, on day 4 of IVIg, he was clinically worsened, quadriplegic and with ophthalmoparesis. Ceftriaxone was started empirically and then plasmapheresis, without clinical improvement.
Results: Laboratory workup revealed positive Borrelia burgdorferi antibodies in serum and CSF (IgG and IgM); EMG showed severe sensorimotor axonal polyneuropathy and spinal MRI presented with cauda equina roots and dorsal radicular emergences thickening and T1 enhancement following gadolinium administration. Neuroborreliosis was assumed and the patient completed a 4‐week course of IV Ceftriaxone, with slow clinical improvement since.
Conclusion: Neuroborreliosis presents as a highly heterogenous, easily overlooked clinical entity, especially upon atypical manifestations. Awareness regarding this condition's many possible presentations is needed to prevent misdiagnoses and start prompt effective treatment, thus minimizing negative outcomes.
Disclosure: Nothing to disclose.
EPO‐461
Double doughnut over and above dengue dystonia
A. Kumar; D. Joshi; V. Singh; A. Pathak; R. Chaurasia; V. Mishra
Department of Neurology, IMS, BHU, Varanasi, India
Background and Aims: The clinical manifestations of dengue range from mild febrile illness to severe dengue shock syndrome and dengue hemorrhagic fever. Recently, its various neurological manifestations have been reported. Dystonia as early presentation in dengue is very rare.
Methods: None.
Results: Results: A 60‐year‐old male presented with high‐grade fever for 5 days associated with arthralgias and myalgias. For the past 3 days, the patient developed gradual deterioration in the sensorium such that he could not communicate although he could comprehend and was lethargic on presentation. On day 4 of admission, he was observed to have developed generalized dystonia. His fever profile was positive for NS1 the (Non‐structural protein 1) antigen of Dengue virus. He had raised levels of aspartate aminotransferase alanine aminotransferase and thrombocytopenia. His magnetic resonance imaging showed bilateral thalamic involvement with a “double doughnut sign”. His CSF analysis showed 5 cells with protein 92 mg/dl and sugar 60 mg/dl and opening pressure of 8 cm of water. It was negative for gram stain, CBNAAT for mycobacterium tuberculosis, cryptococcal antigen, and other neurotropic viruses. He was managed with benzodiazepines, tetrabenazine, and pulse steroid therapy. Gradually his dystonia subsided and he could articulate and was discharged in stable condition.
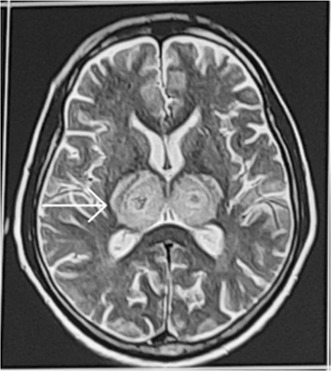
MRI Brain: shows T2 weighted MRI image with double doughnut sign with bilateral thalamic involvement.
Conclusion: A high index of suspicion especially in highly endemic countries required to suspect dengue dystonia. Double doughnut sign in MRI brain will help in identification. Morbidity in dengue dystonia can be reduced by early and prompt treatment.
Disclosure: Nothing to disclose.
EPO‐462
Challenging diagnosis of Creutzfeldt‐Jakob disease with atypical early symptoms: A case series
C. Algar Ramírez; H. Antolí Martinez; D. Rodriguez Martínez; P. Dodu
Department of Neurology, Hospital Regional Universitario de Málaga, Málaga, Spain
Background and Aims: Creutzfeldt‐Jakob disease (CJD) is a rapidly progressing neurodegenerative disorder whose classical presentation is characterized by the association of dementia, myoclonus and motor impairment in variable degree. However, atypical and non‐specific presentations have been described, making the early clinical diagnosis difficult and challenging.
Methods: We present three cases admitted to a tertiary hospital after seeking emergency care for rapidly developing neurological abnormalities.
Results: The first patient experienced a decline in bilateral visual sharpness (Heidenhain variant). The second case showcased alien limb phenomenon, rigidity, cortical sensory loss and apraxia in the left upper limb, resembling a corticobasal syndrome. The third patient, upon examination, displayed restricted coordinated gaze, particularly in the vertical direction, accompanied by short steps and disrupted turns in walking, indicating a progressive supranuclear palsy. Diagnostic tests revealed: EEG findings consistent with paroxysmal focal activity, MRI with diffusion restriction in cortical áreas and fluid analysis showed positive 14‐3‐3 protein. These findings support the diagnosis of CJD.
Conclusion: The early manifestations of CJD with unusual symptoms are not extensively covered in scientific literature. Consequently, reviewing and underscoring the significance of promptly identifying these cases is essential for appropriate patient care. Results from additional tests may offer guidance in considering this prionic pathology.
Disclosure: Nothing to disclose.
EPO‐463
An atypical presentation of progressive multifocal leukoencephalopathy in a “well controlled” HIV patient
C. Ortega Hiraldo; A. Gómez González; A. Aguilar Monge; M. Vicente Domínguez; J. Sempere Fernández
Servicio de Neurología y Neurofisiología, Hospital Universitario Virgen de la Victoria, Málaga, España
Background and Aims: Progressive Multifocal Leukoencephalopathy (PML) is a demyelinating disease of the central nervous system caused by JC virus, typically seen in inmunocompromised patients. It affects white matter, giving magnetic resonance (MRI) images predominantly involving supratentorial matter. We report a case of PML in an HIV‐patient under combination antiretroviral therapy (cART) with an atypical clinical and radiologic presentation, with predominance involvement of the brainstem and cerebellum.
Methods: Case report.
Results: A 46‐years old male, HIV well controlled with cART for years, consulted for dizziness, nausea, gait and speech disturbance, that were developed progressively in the last 5 months. Neurological exploration revealed nystagmus, mild paresis of the left hand, right hypoesthesia, exalted reflexes predominantly on the left with Babinski's sign, as well as bilateral dysmetria and gait ataxia. Brain MRI showed T2‐hyperintense and T1‐hypointense lesions in cerebellar peduncles and pons, with no restricted‐diffusion; and a small similar lesion in frontal lobes. Blood tests were normal, CD4 count was preserved, but an inverted CD4/CD8 ratio was observed; and CSF‐fluid showed hyperproteinorrachia, with Flow‐cytometry, cultures and typical virus PCRs negative. The patient experienced a rapidly progressive course, dying two months later. In the necropsy was diagnosed as PML, with lesions involving brainstem, cerebellum, spinal cord, and supratentorial regions.

T2 hyperintense lesions involving pons and both cerebellar penduncles.

The described lesions extends to the medulla.
Conclusion: Although PML is usually seen in severe immunocompromised patients affecting the supratentorial regions, the clinical and radiological presentation can be unusual sometimes. Furthermore, the presence of an inverted CD4/CD8 ratio is noteworthy as a possible marker of immune dysfunction in an apparently well‐controlled HIV patient.
Disclosure: The authors do not have any disclosure of interests.
EPO‐464
Headaches and fever: Disseminated cryptococcosis in an immunocompetent patient: A case report
M. Alfonso
Internal Medicine, Amang Rodriguez Memorial Medical Center, Marikina City, Philippines
Background and Aims: Cryptococcosis is an opportunistic infection caused by encapsulated yeast Cryptococcus. The two species commonly infecting humans are C. neoformans and C. gatii and it commonly affects immunocompromised patients. Disseminated infection in immunocompetent is rare. In this study, we present a case of disseminated cryptococcus with lung and cerebral involvement in an immunocompetent patient.
Methods: The case is about a 28‐year‐old female from Marikina City who presented with fever, headaches and cough. Patient was initially treated as a case of Pulmonary Tuberculosis, but no improvement was noted during hospital stay. Further workup was done including chest and cranial CT scans which guided for definitive diagnosis. Cultures of CSF and lung mass biopsy were also done which revealed positive for cryptococcus infection. Patient was also tested for other immunodeficiency tests including HIV where she tested negative. Since the patient was confirmed with cryptococcus infection, patient was treated with systemic anti‐fungal medications. Patient improved symptomatically and significantly hence was then discharged and advised follow up at OPD.
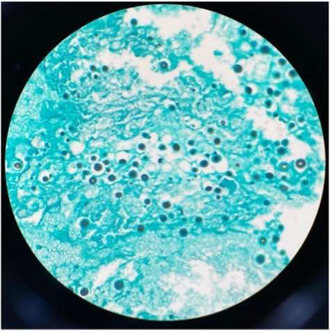
Grams stain of CSF for analysis.
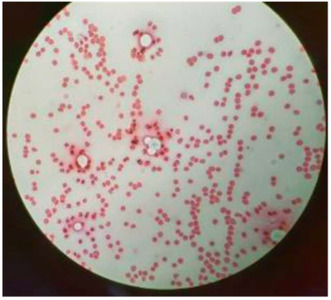
H&E stain of CSF for analysis.
Results: Not applicable.
Conclusion: In this study, we present a rare case of disseminated cryptococcosis with lung and cerebral involvement in an apparent immunocompetent patient. Early recognition of the disease and treatment leads to better outcomes.
Disclosure: Nothing to disclose.
EPO‐465
Non‐compressive myelopathy complicating acute community‐acquired bacterial meningitis
E. Drost; N. Chekrouni; M. Brouwer; D. van de Beek
Department of Neurology, Amsterdam UMC, Amsterdam, The Netherlands
Background and Aims: Bacterial meningitis is a severe disease with high rates of complications and unfavourable outcome. Complications involving the spinal cord, such as myelitis or infarction, are infrequently reported.
Methods: Cases of non‐compressive myelopathy were identified when included in a nationwide cohort study of adults with community‐acquired bacterial meningitis in the Netherlands. Outcome was scored at discharge using the Glasgow Outcome Scale and a score of 1‐4 was considered an unfavourable outcome. Subsequently, we reviewed the literature on non‐compressive myelopathy as a complication of bacterial meningitis.
Results: Non‐compressive myelopathy was reported in 5 of 3047 episodes of community‐acquired bacterial meningitis (0.16%). The median age of these patients was 56 years (range 17‐72). Causative pathogens were Streptococcus pneumoniae in 2, and Neisseria meningitidis, Haemophilus influenzae and Streptococcus agalactiae each in 1. Paresis of legs (n = 4) or arms and legs (n = 1) were the presenting symptoms during admission, occurring after a median duration of 13 days after admission (range 2‐28). Spinal MRI showed T2‐weighted abnormalities of the spinal cord in all patients. Outcome was unfavourable in all patients despite additional corticosteroid treatment in two. The literature review yielded 14 cases of non‐compressive myelopathy in bacterial meningitis patients. The most reported causative pathogen was Neisseria meningitidis in 8 patients. Outcome was unfavourable in 12 of 14 of reported patients in literature (86%).
Conclusion: Non‐compressive myelopathy is an uncommon but severe complication of bacterial meningitis. It is not constrained to one specific pathogen and is associated with high rates of unfavourable outcome.
Disclosure: Nothing to disclose.
EPO‐466
Even the smallest of organisms could change the course of life
I. Llera López 1; L. Santos Sánchez de las Matas1; M. Montalvo Moraleda1; A. Saldaña Díaz1; I. Navas Clemente2; Á. Bonelli Franco1; J. Cebrián Escudero1; J. Martínez Ramos1; D. Landaeta Chinchilla1; Z. Ghazizadeh‐Monfared Croigny3; R. Berigüete Alcántara3; M. Domínguez Sepulveda2; P. Bermejo Acevedo2; N. Barbero Bordallo1
1Department of Neurology, Hospital Universitario Rey Juan Carlos, Móstoles, Spain; 2Department of Internal Medicine, Infectious Disease, Hospital Universitario Rey Juan Carlos, Móstoles, Spain; 3Department of Clinical Neurophysiology, Hospital Universitario Rey Juan Carlos, Móstoles, Spain
Background and Aims: Lumbosacral adhesive arachnoiditis is a serious and rare condition with multiple aetiologies, as it may be related to postoperative changes, inflammatory conditions, or secondary to previous infectious disease. In general, it presents as a polyradiculopathy, being uncommon its presentation as cauda equina syndrome, an entity that is associated with significant disability.
Methods: Case report.
Results: Female, 35 years old. History of fully recovered cytomegalovirus (CMV)‐related polyradiculopathy secondary to stage 3 HIV the previous year. Progressive worsening of motor function started 2 months before hospital admission. Neurological examination: paresis of the left lower limb (2/5) and bilateral areflexia in lower extremities, without other alterations. Laboratory tests: CD4+ 226 cells/mm^3, undetectable HIV viral load. CSF: proteinorraquia, mild leukocytorrhea and oligoclonal bands with identical distribution in CSF and serum. Negative infectious and autoimmune panels. MRI of the lumbar spine showed thinning of the L1‐2 nerve roots, hyperintensity and thickening of the L2 cauda equina and downward, narrow and adherent nerve roots that resembled an image of an empty L3‐S1 thecal sac. The neurophysiological study evidenced active motor denervation, eminently of the distal left lower limb. The study was completed with a biopsy that confirmed focal fibrosis and chronic inflammation of the ligamentum flavum and the lumbar thecal sac.
Conclusion: The final diagnosis was postinfectious adhesive arachnoiditis. To our knowledge, this is the first case described following CMV‐related polyradiculopathy. Diagnosis is based on clinical presentation, neuroimaging and biopsy. Pharmacological (e.g. immunoglobulins) and surgical treatments have been described, without clear benefit. Intensive physical rehabilitation is recommended.
Disclosure: Nothing to disclose.
EPO‐467
Neurovascular complications in patients with central nervous system infections
I. Stavila 1; C. Gutu1; E. Manole2; O. Grosu1; O. Odainic1; M. Gavriliuc2
1“Diomid Gherman” Institute of Neurology and Neurosurgery, Chisinau, Republic of Moldova; 2“Nicolae Testemițanu” State Universities of Medicine and Pharmacy, Chisinau, Republic of Moldova
Background and Aims: Neurovascular complications are common with nervous system infections, such as cerebral vascular insult, venous thrombosis, vasculitis and aneurysm formation. The aim of our study was to analyze clinical features of a group of patients with central nervous system (CNS) infection who developed neurovascular complication.
Methods: Prospective observational study collecting all the patients with CNS infections from a tertiary neurology center between 2007 and 2023 was made. Study sample consists of 265 patients with CNS infections and 42 (15.8%) with cerebrovascular complications.
Results: The mean age was 47.21 years, 57.1% men. The most common infections were meningitis (28.6%) and meningoencephalitis (42.9%). Neurovascular complications presented as: ischemic stroke (78.8%), multiple lesions (48%), cerebral vasculitis (30.9%), and cerebral venous thrombosis (31%). The most frequent predisposing factors were bronchopneumonia (52.4%), parameningeal infection (19.0%), and septicemia (16.7%). The pathogens were identified in 35.7% case, mostly cocci species. When compared to patients without neurovascular complications those with stroke presented higher blood sedimentation rate (41.00 vs 32.65mm/h, p = 0.017), CSF protein (4.17 g/l vs 1.62, p < 0.05), motor deficit (50% vs. 36.3%), seizures (9.5% vs 5.8%), and in‐hospital mortality (28.6% vs 22.4%) but fever was less common (66.7% vs 76.7%). Logistic regression model shows that the presence of bronchopneumonia, smoking and pregnancy can predict the occurrence of the neurovascular complication with good probability (B = 1.67o, df = 1, p = 0.00, Exp B = 5.310).
Conclusion: Neurovascular complications in CNS infections affect mostly young patients and are more likely to manifest focal neurologic deficit and higher mortality rates.
Disclosure: Nothing to disclose.
EPO‐468
Exploring the neurological outcomes of Nipah virus: A narrative review of state from 1998 to 2023
A. Kayode; A. Moradeyo
Department of Medicine and Surgery, Ladoke Akintola University of Technology, Ogbomoso, Nigeria
Background and Aims: Nipah virus (NiV) is an emerging zoonotic RNA virus causing severe respiratory and acute febrile encephalitic illness in humans. Pteropus fruit bats serve as reservoirs for the virus which led to human spread via consumption of food contaminated with bat secretion, contact with infected animals and human‐to‐human spread. This study aims to access the early, late‐onset and long‐term neurological outcomes of Nipah virus infection among affected individuals.
Methods: Articles from existing literature in PubMed, Medline and Google Scholar databases investigating Nipah virus‐associated neurological outcomes were examined. 79 relevant articles were screened for this study using predefined inclusion and exclusion criteria.
Results: NiV infection in humans produces an encephalitic syndrome ranging from headache and pyrexia to brain stem abnormalities; and reduced level of consciousness (55% in Malaysia, 90% in Bangladesh) including tonic‐clonic convulsions and segmental myoclonus. Fever with altered sensorium was the most common presentation in Siliguri, India (97%) and Bangladesh (90%), with a case fatality ratio (CFR) of about 40‐100% in recent outbreaks. Residual neurological deficits were seen in 10‐15% of survivors an average of 8 months after primary encephalitis. Brain MRI showed small discrete hyperintense lesions, widespread in the cortex, subcortical and deep white matter from microinfarctions due to underlying vasculitis of the cerebral blood vessels, seen in acute infections and patchy confluent hyperintense cortical lesions seen in relapsing NiV infections.
Conclusion: Proper education on good hygiene is important to prevent reemergence of the infection in affected areas. Effective neurorehabilitation is also necessary to reduce long‐term neurological complications in NiV survivors.
Disclosure: Nothing to disclose.
EPO‐469
Diagnostic deadlock: A case of disseminated tuberculosis with neuroleptospirosis
V. Singh 1; S. Chouksey2; P. Batra2; R. Chaurasia3
1Department of Neurology Institute of Medical Science, Banaras Hindu University, Varanasi, India; 2Department of Neurology, Institute of Medical Science, Banaras Hindu University, Varanasi, India; 3Department of Neurology Institute of Medical Science, Banaras Hindu University, Varanasi, India
Background and Aims: Neuroleptospirosis may present with features like altered sensorium, GTCS, headache, and focal neurological deficit which are shared with other common neuro‐infection like tuberculous meningitis. Coexistence of these two illnesses has not been yet reported.
Methods: A 19‐years old male presented with high‐grade fever, headache and vomiting for 4 days and right focal to bilateral tonic clonic seizures and altered sensorium for 3 days. On examination, he was febrile (101°F) and GCS score was E2V1M5. There was no papilledema and focal motor deficit. Signs of meningeal irritation were present.
Results: Serum IgM leptospira titre was high [26.4 Units (<9 units)] and creatine kinase [493 U/L (24‐195 U/L)] was elevated. Patient received doxycycline with antiepileptic drugs (levetiracetam and lacosamide) for two weeks. There was improvement in sensorium and subsidence of seizure; however, high‐grade fever persisted. CECT thorax, abdomen and pelvis revealed disseminated tuberculosis (Figure 1). MRI brain and spine with contrast revealed diffuse leptomeningeal enhancement and basal exudates with hydrocephalus and lytic lesion at L4 vertebrae suggestive of tuberculous meningitis and Pott's spine (Figure 2). Four drugs antitubercular therapy was started. Ventriculoperitoneal (VP) shunting was done. GCS improved to E3V3M5. However, he developed refractory status epilepticus, followed by ventilator associated pneumonia, septic shock and succumbed to the illness.
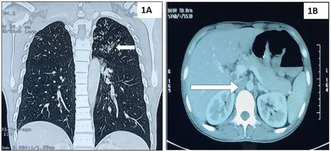
Contrast enhanced computed tomography of chest and abdomen revealing multiple centrilobular nodules in upper lobe of left lung parenchyma (1A) and multiple enlarged mediastinal, bilateral hilar and intraabdominal (arrow) lymph nodes (1B) suggestive of dis.
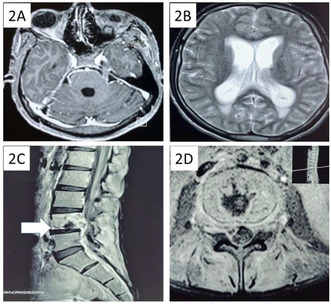
Contrast magnetic resonance imaging of brain showing leptomeningeal enhancement and basal exudates on T1W (2A) and hydrocephalus on T2W with periventricular ooze (2B) suggestive of tuberculous meningitis. Contrast magnetic resonance imaging of lumbosacral.
Conclusion: This is the first case report of coexistent neuroleptospirosis and disseminated tuberculosis creating diagnostic dilemma. One should revise his/her own diagnosis and work up plan once the anticipated therapeutic response is inadequate.
Disclosure: Nothing to disclose.
EPO‐470
Linking the unseen: Marchiafava‐Bignami disease and tuberculous meningo‐myelitis
M. Creta 1; E. Ballabio2; G. Nuzzaco2; K. Khouri Chalouhi3; S. Tonietti2; F. Frediani2
1Department of Health Sciences, University of Milan, Milan, Italy; 2Neurological and Stroke Unit Department, San Carlo Bartolomeo Hospital, ASST Santi Paolo e Carlo, Milan, Italy; 3Neuroradiology Department, San Carlo Bartolomeo Hospital, ASST Santi Paolo e Carlo, Milan, Italy
Background and Aims: This work reports the first‐ever described case of tuberculous meningo‐myelitis (TBMM) associated with Marchiafava‐Bignami disease (MBD), complicated by communicating hydrocephalus, multiple acute ischemic strokes, and diabetes insipidus.
Methods: We present the case of a 33‐year‐old homeless Afghan male with a significant history of alcohol abuse, who presented to the Emergency Room with a recent‐onset fever and a sudden and rapidly progressive impaired level of consciousness. Clinical manifestations included focal neurological deficits such as left motor facial and brachial sparing, flaccid paraplegia, sphincter release, and jerking movements.
Results: CT‐scan and MRI revealed severe generalized cerebral atrophy with symmetrical hypodensity of the hemispheric white matter and splenium of the corpus callosum. EEG showed widespread slowing without epileptiform abnormalities. Laboratory results indicated electrolyte imbalances and diluted urine. Supportive therapy and vitaminic supplementation were initiated. A second CT‐scan revealed communicating hydrocephalus with initial decompensation, necessitating immediate external ventricular drain insertion. CSF analysis showed lymphocytosis, elevated protein levels, decreased glucose levels, and positive cultures for Mycobacterium tuberculosis. A second MRI with gadolinium unveiled multiple acute ischemic strokes and diffuse meningeal enhancement and a cervical‐dorsal lesion consistent with TBMM. Despite antituberculous chemotherapy, the patient's condition deteriorated, culminating in coma and death.
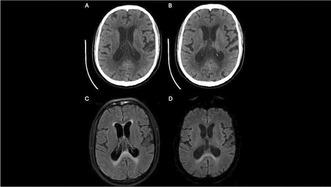
CT scan: Splenium hypodensity in corpus callosum, suggestive of Marchiafava‐Bignami; mild age‐related ventricular and cerebral sulci enlargement (A,B). MRI FLAIR: Signal hyperintensity in splenium, supporting suspected Marchiafava‐Bignami diagnosis (C,D).
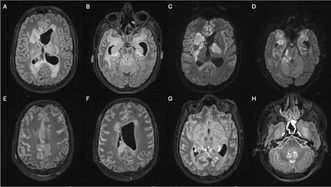
MRI FLAIR: Hydrocephalus, periventricular hyperintensity (A). Mesencephalic and interpeduncular cistern hyperintensity suggests leptomeningitis (B). DWI: acute ischemia (C,D). Contrast‐enhanced FLAIR: diffuse leptomeningeal enhancement (E,F,G,H).
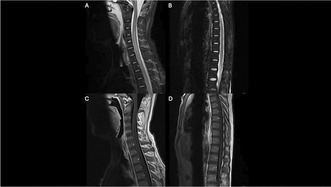
MRI sagittal STIR: Hyperintensity in the spinal cord from C4 to C7 (A) and into the upper thoracic tract (B). Post‐contrast T1‐weighted sequences: Subtle enhancement along spinal cord margins (C,D). Findings suggest suspected myelitis.
Conclusion: Establishing a clear link between TBMM and MBD remains challenging. Speculation suggests a potential nutritional imbalance induced by TBMM's high metabolic demand in a multi‐system disease, resembling a toxic‐like state that can precipitate MBD. Both conditions require a high level of suspicion and prompt empiric treatment initiation in patients with behavioral and socioeconomic risk factors.
Disclosure: Nothing to disclose.
EPO‐471
Horner syndrome besides the obvious – Pantoea spp. as a rare cause of cervical spinal epidural abscess
J. Neiva Correia; M. Saianda Duarte; V. Fonseca; A. Arraiolos; J. Morgado; J. Vale
Neurology Department, Hospital Beatriz Ângelo, Loures, Portugal
Background and Aims: Cervical spinal epidural abscess (CSEA) is an uncommon disease, associated with significant morbidity. Diagnosis can be elusive, especially if the classic triad of back pain, fever, and neurological deficit is not present. Horner syndrome (HS) is a rare but possible presentation. MRI with gadolinium is crucial for swift diagnosis and timely initiation of antimicrobial therapy. We present a case linked to the rare Pantoea spp, a group of plant pathogens that can cause human disease.
Methods: Case report.
Results: 53‐year‐old male, without relevant past medical history, was admitted to the ER after the acute onset of right eye ptosis and gait unsteadiness after osteopathic manipulation for neck and shoulder pain. Physical examination showed marked cervical neck tenderness. Neurological examination revealed a right HS and mild ataxia of the right leg. Brain CT angiography and cervical spine CT scans were normal. Markedly increased inflammatory markers in the workup prompted a lumbar puncture. CSF analysis revealed pleocytosis and hyperproteinorrachia. Empirical ceftriaxone IV 2g q12h was initiated. Spine MRI revealed septic arthritis at C7‐D1 with an associated CSEA. Subsequent blood culture identified Pantoea spp, sensitive to ceftriaxone. After six weeks of treatment, there was clinical and radiological improvement.
Conclusion: We report an uncommon presentation of a rare entity caused by a very rare pathogen. This case is also unique because there was no direct inoculation or haematogenous spread, and the few cases of infection reported in the literature were on pediatric or immunocompromised adults. A prompt diagnosis and treatment is needed to achieve a good outcome.
Disclosure: Nothing to disclose.
Neuroimmunology 3
EPO‐472
Plasma proteomics and autoantibody screening: A tool for patient stratification and monitoring CIDP treatment responses
A. Casano1; M. Castillo‐Dreyfuss2; L. Shen2; J. Vowinckel3; B. Gangadharan1; I. Bilic 1
1Baxalta Innovations GmbH, a Takeda Company, Vienna, Austria; 2Takeda Development Center Americas, Inc., Cambridge, MA, USA; 3Biognosys AG, Schlieren, Zürich, Switzerland
Background and Aims: Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) is an inflammatory neuropathy with heterogeneous presentation. Precise diagnosis and patient‐tailored treatment decisions are hindered by lack of unbiased, quantifiable molecular markers. Although aberrant immune cell‐mediated responses and circulating autoantibodies may accompany CIDP, underlying pathomechanisms remain elusive. We investigated correlation of clinically defined disease states with changes in plasma homeostasis in patients receiving immunoglobulin/placebo during remission versus relapse.
Methods: Plasma samples from patients with CIDP receiving hyaluronidase‐facilitated subcutaneous immunoglobulin 10% (fSCIG 10%) or placebo during ADVANCE‐CIDP 1 (NCT02549170) were analysed. Proteomic analysis (data‐independent acquisition liquid chromatography‐mass spectrometry and Olink®) compared longitudinal samples from patients experiencing remission/relapse. A novel multiplex in‐solution method to simultaneously detect autoantibodies against 32 CIDP‐relevant antigens was also developed, potentially alleviating current technical hurdles associated with autoantibody detection in CIDP.
Results: For >1500 plasma proteins, concentration profiles differed significantly in patients with CIDP versus healthy controls. Identified CIDP profiles emphasized natural killer‐ and B‐cell‐mediated immune pathway involvement. When comparing remitting and relapsing patients, differences in profiles involved in extracellular matrix homeostasis, microtubule organization, tight junction assembly, and cytokine production were observed. fSCIG 10% progressively lowered proinflammatory cytokine levels versus placebo. Autoantibody profiling uncovered a CIDP signature for evaluation in larger cohorts.
Conclusion: Versus healthy controls, pronounced plasma protein dynamics were identified in patients with CIDP, providing a broad base for biomarker discovery. Combining plasma proteomics and autoantibody screening may identify unbiased, quantifiable biomarkers for patient stratification and/or monitoring pharmacodynamics following high‐dose immunoglobulin administration. Study/writing support funders: Takeda Development Center Americas, Inc./Takeda Pharmaceuticals International AG.
Disclosure: AMC, IB, BG*: employees of Baxalta Innovations GmbH, a Takeda Company; IB: Takeda shareholder; MJC‐D, LS: employees of Takeda Development Center Americas, Inc., and Takeda shareholders; JV: employee of Biognosys AG. *At the time of the study.
EPO‐473
The wide spectrum of Anti‐Hu Paraneoplastic Neurological Syndromes (PNS): Case‐series and review of the literature
K. Rizonaki*; P. Stamatelos*; A. Antoniou; E. Kinnis; E. Petrou; A. Gamvroula; V. Gourbali; G. Kolovos; M. Lentza; E. Alexiou
Neurology Department, Evaggelismos General Hospital, Athens, Greece
Background and Aims: PNS are autoimmune disorders arising from immune response to tumor antigens and they may precede cancer diagnosis for years. Anti‐Hu neuronal autoantibodies are related to a wide and heterogeneous range of both Central and Peripheral Nervous System presentations.
Methods: We present four cases of Anti‐Hu PNS, along with a systematic review of the literature. We searched MEDLINE for Anti‐Hu case‐series or case‐reports, initially identifying 588 articles. Finally, 181 articles were included.
Results: Our case‐series consists of 4 patients (1 Female, Mean Age 69 years). Two patients presented with Subacute Sensory Neuronopathy (SSN) and pronounced autonomic involvement, one patient with Limbic Encephalitis (LE) and one with Encephalomyelitis. Three patients had a concomitant small‐cell lung cancer (SCLC), diagnosed after the PNS in two of them. Two patients died after 1 and 11 months, respectively. In our review, we found 1424 anti‐Hu cases (Mean age: 63 years, 42% Women). The most common presentations were SSN (49%), LE (16%) and Encephalomyelitis (15%). In 1193 (84%) patients, a neoplasm (most commonly SCLC‐84%) was identified and in 79% of them, PNS preceded cancer diagnosis. Immunosuppression along with neoplasm treatment were the preferable approaches in 52% and 51% of patients, respectively. 660 (55%) patients died during follow‐up (Mean time to death: 13 months).
Conclusion: Anti‐Hu PNS are rare but potentially treatable. They should always be included in the differential diagnosis of patients with compatible neurological syndromes, even without history of cancer. Thorough investigation to identify and treat an underlying neoplasm along with immunosuppressive agents may improve prognosis of these patients.
Disclosure: Nothing to disclose.
EPO‐474
Neurofilament light chain: The importance of plasma biomarkers in therapeutic decision‐making in multiple sclerosis
L. Araujo Duarte 1; A. Salvio Lemos2; R. Amphilophio Fernandes2; M. Ataíde Teixeira2; H. França Alcarraz Ferreira1; E. Gutman Gouvea2; V. Coutinho Costa1; J. Dib Farinhas2; V. Coelho Santa Rita Pereira1; S. Vieira Alves‐Leon1
1Universidade Federal do Rio de Janeiro; 2Universidade Federal do Estado do Rio de Janeiro
Background and Aims: Relapsing remitting Multiple Sclerosis (RRMS) is a subtype of MS, an autoimmune chronic inflammatory neurodegenerative disease. During the last decades MS has been remarkably impacted by the advances in knowledge on the pathophysiology, new therapeutic targets, early diagnosis criteria and monitoring of treatment response. Disease follow‐up biomarkers as Neurofilament Light Chain (NfL) are not yet available in most locations, but since non‐invasive techniques as SiMoA technique have been used to monitor progression and therapeutic response in RRMS, therapeutic decision making has been reviewed.
Methods: In this prospective study, SiMoA technique was used to assess NfL levels in RRMS classified as EDA, NEDA, naïve and patients that switched from first line therapy to moderate‐high efficacy DMD.
Results: Sixty‐six RRMS patients and 24 age‐matched health controls were included. In EDA group, NfL mean level was 30.25 pg/mL, and 6.65 pg/mL for NEDA patients. Among patients without DMD and under first line therapy, NfL mean level were 13.98 pg/mL and 12.94 pg/mL, respectively. After therapy switch, or under moderate‐high DMD, NfL levels significantly decreased (6.96 pg/mL; p < 0.05), similar to NEDA patients and healthy control (6.7 pg/mL).
Conclusion: The significant difference in NfL levels before and after moderate‐high efficacy DMD showed the impact of new drugs in both efficacy and control of NFL levels. The role of NFL can contribute on treatment management, especially in the monitoring of the therapeutic failure beyond the usual outcomes as clinical relapsing and new lesions in MRI, aiming to early impact on the course of MS disability.
Disclosure: Nothing to disclose.
EPO‐475
Immune checkpoint inhibitor‐related cerebellar toxicity and comparison with paraneoplastic cerebellar ataxia
M. Dentoni 1; I. Florean1; A. Farina2; B. Joubert2; J. Honnorat2; V. Damato3; M. Fabris4; G. Gigli1; M. Valente1; A. Vogrig1
1Clinical Neurology, Department of Medicine (DMED), University of Udine, Udine, Italy; 2French Reference Centre for Paraneoplastic Neurological Syndromes and Autoimmune Encephalitis, Hospices Civils de Lyon, Lyon, France; 3Department of Neurosciences, Drugs and Child Health, University of Florence, Firenze, Italy; 4Laboratory of Immunopathology, Institute of Clinical Pathology, Department of Laboratory Medicine, University Hospital of Udine, Udine, Italy
Background and Aims: Immune checkpoint inhibitors (ICIs) have revolutionized cancer therapy, and the association with immune‐related adverse events (irAEs) is well‐established. Our aim was (i) to characterize ICI‐related cerebellar toxicity; (ii) to compare ICI‐related cerebellar toxicity to paraneoplastic cerebellar ataxia (PCA).
Methods: Systematic review of the literature following PRISMA guidelines, with the addition of 8 original cases. We included adult patients developing new‐onset, isolated or predominant cerebellar dysfunction within 12 months from the last ICI infusion. Such cases were compared with a consecutive cohort of patients with PCA.
Results: Thirty‐five patients were included (males: 25/35 (71%), median age: 65 [range: 20‐82]). The most frequent tumour was non‐small cell lung cancer (12/35, 34%). Anti‐PD1 were adopted in most cases (19/35, 54%). Symptoms developed a median of 11 weeks (range: 0.1‐82) after ICI initiation; “isolated cerebellar ataxia” (gait and/or limb and/or trunk ataxia) prevailed at disease peak (13/35, 37%). Antibody positivity was detected in 15/31 patients tested (48%). Cerebrospinal fluid was inflammatory in 26/30 (87%). Magnetic resonance imaging showed cerebellar hyperintensities in 8/35 (23%). Immune‐modulating therapy was applied in 33/35 cases (94%), and most patients showed neurological improvement with residual disability (17/35, 49%). When compared with PCA (n = 15), the ICI group was significantly associated with NSCLC, isolated ataxia, and a better neurological outcome.
Conclusion: We provided a characterization of ICI‐related cerebellar toxicity. Compared to PCA, differences exist in terms of tumour association, clinical features, and outcome. Clinical presentation‐antibody‐tumor triad in the ICI group poorly reflects the typical associations of paraneoplastic disorders.
Disclosure: Nothing to disclose.
EPO‐476
Abstract withdrawn
EPO‐477
Novel approaches for immune‐mediated chronic intestinal pseudo‐obstruction: A case series
A. Vilaseca1; P. Arranz 1; A. Zabalza1; M. Sanz‐Martínez2; L. Viñas2; L. Alcala‐González3; H. Ariño1; X. Montalban1; X. Montalban4; X. Montalban5; C. Malagelada3; C. Malagelada4
1Department of Neurology and MS Centre of Catalonia (Cemcat), Vall d’Hebron University Hospital, Barcelona, Spain; 2Immunology Department, Vall d’Hebron University Hospital, Barcelona, Spain; 3Gastroenterology Department, Vall d’Hebron University Hospital, Barcelona, Spain; 4Universitat Autònoma de Barcelona (UAB), Barcelona, Spain; 5Universitat de Vic‐Central de Catalunya (UVic‐UCC)
Background and Aims: Neurologic autoimmune gastrointestinal dysmotility (nAGID) represents a significant contributor to gastrointestinal motility disorders, often leading to chronic intestinal pseudo‐obstruction (CIPO). The response to immunotherapy varies based on the specific autoimmune disorder. Our goal is to describe the treatment responses of various drugs in 3 patients with CIPO.
Methods: Three consecutive cases diagnosed at a referral center for CIPO during 2023 are described. We collected baseline characteristics, clinical symptoms, radiologic tests, and histopathologic examination. The clinical and radiological response to treatment was used to measure outcome.
Results: All 3 patients had severe CIPO, refractory to previous treatments. Two patients underwent a full‐thickness intestinal biopsy that detected lymphocytic myenteric ganglionitis. The first patient was a 35‐year‐old‐male with myasthenia gravis associated to thymoma, who developed a nAGID without any serological marker of autoimmunity. He received vedolizumab with improvement of his digestive symptoms and nutritional status. The second patient was an 18 year old woman who had a non‐paraneoplastic anti‐Hu associated nAGID. She achieved clinical remission after rituximab. The third patient was a 60‐year‐old woman, with small cell lung cancer, who developed a paraneoplastic anti‐Hu associated nAGID. She received cyclophosphamide, but did not improve and eventually died.
Conclusion: Our findings underscore the potential efficacy of rituximab and vedolizumab in the management of neurologic autoimmune gastrointestinal dysmotility with chronic intestinal pseudo‐obstruction, particularly in refractory cases. Although a larger sample is needed, these interventions should be considered valuable options in the therapeutic landscape for such patients.
Disclosure: Nothing to disclose.
EPO‐478
Single fiber EMG in the diagnostic workup of diplopia and ptosis
S. Cornacchini 1; M. Verza1; A. Farina1; M. Bastianelli2; A. Cassardo2; C. Mei2; A. Barilaro3; L. Massacesi1; A. Grippo2; V. Damato1
1Department of Neurosciences Drugs and Child Health, University of Florence, Florence, Italy; 3Department of Neurology 2, Careggi University Hospital, Florence, Italy; 2Department of Neurophysiology, Careggi University Hospital, Florence, Italy
Background and Aims: Diplopia and ptosis are common neuro‐ophthalmologic signs. Yet identifying the specific aetiology can be challenging due to the different possible causes. In this prospective study, we evaluated the reliability of the stimulated single fiber electromyography (SFEMG) in supporting the diagnosis of myasthenia gravis (MG) presenting with diplopia and ptosis.
Methods: We included 80 patients who presented with diplopia (n = 34), ptosis (n = 16), or both (n = 30), and underwent SFEMG. Patients received a comprehensive diagnostic workup involving detailed history investigation, physical examination, orbital and brain imaging, thyroid function, antibody screening, orthoptic evaluation, ice pack test (when applicable) and repetitive nerve stimulation test (RNS).
Results: SFEMG yielded positive results in 29 of 80 (36.3%) patients of the cohort. Among the patients diagnosed with MG (n = 35), SFEMG showed a sensitivity of 71.4% (95% CI: 0.55 – 0.84) and specificity of 91.1% (95% CI: 0.79 – 0.96) with a positive predictive value of 86.2% (95% CI: 0.69 – 0.95) and a negative predictive value of 80.3% (95% CI: 0.68 – 0.89). Notably, SFEMG was positive in 6 seronegative MG cases and in 14 cases with negative RNS. In the non‐MG group (45/80 patients), SFEMG was negative in the majority (41 patients, 91.1%) of cases, further supporting its value in ruling out MG. A relevant proportion (21/45) of these cases remained undiagnosed.
Conclusion: Our findings suggest that SFEMG is a valuable tool in the diagnostic workup of diplopia and ptosis and in the differential diagnosis of MG, especially in seronegative MG cases and in those with negative RNS results.
Disclosure: Nothing to disclose.
EPO‐479
Difference between high‐dose and moderate‐dose vitamin D supplement in an animal model of progressive multiple sclerosis
M. Haindl1; M. Ücal2; M. Nowakowska2; W. Wonisch3; C. Enzinger1; S. Hochmeister 1
1Department of Neurology, Medical University of Graz, Graz, Austria; 2Department of Neurosurgery, Medical University of Graz, Graz, Austria; 3Department of Physiological Medicine, Medical University of Graz, Graz, Austria
Background and Aims: Although many studies have found correlations between low vitamin D (VD) serum levels and the onset/progression of Multiple Sclerosis (MS), negative effects of VD supplementation are also reported. Uncritical intake of excessively high VD doses can lead to hypercalcemia and kidney damage. However, little is known about high dose effects on the central nervous system in neuroimmunological diseases. We developed an animal model that represents the cellular characteristics of progressive MS very well. In previous experiments we detected positive effects of moderate doses of VD in terms of alleviating brain pathology.
Methods: This work investigates whether high‐dose VD (400IU/day; VD++) leads to histopathological differences compared to moderate doses (400IU/week; VD+) in our animal model. For this purpose, female rats (n = 20) received VD (Fresenius‐Kabi, Graz, Austria) accordingly from age 3 weeks on and underwent the standard procedure of our animal model (Ücal et al., 2017). Tissue was harvested on peak disease, and immunohistochemical evaluation was performed.
Results: Overall, there was no significant difference detectable between VD+ and VD++ with respect to preservation of myelin structures. However, microglial activation was significantly increased in the VD++ group on day 15 (p = 0.003) and 30 (p = 0.002). Furthermore, our preliminary data showed a lower number of apoptotic cells in the VD++ group, but at the same time increased neuronal cell loss.
Conclusion: We found no significant difference between VD+ and VD++ doses in preventing myelin damage but an increased microglial activation and neuronal loss in the VD++ group. Our data highlight the need for medically controlled VD supplementation.
Disclosure: This study was partially funded by Fresenius‐Kabi (to Hochmeister S).
EPO‐480
Clinical impact of high dose corticosteroids on hospitalisations and complications in patients with Myasthenia Gravis
N. Numajiri1; M. Takahashi2; M. Waratani3; T. Kobayashi4; T. Yamamoto 1; T. Yajima1
1Medical Affairs Division, Alexion Pharma GK, Tokyo, Japan; 2Department of Clinical Laboratory and Biomedical Sciences, Osaka University Graduate School of Medicine, Osaka, Japan; 3Medical and Payer Evidence Strategy, AstraZeneca UK, Ltd, Cambridge, UK; 4Evidence Observational Research, Data Science, AstraZeneca KK, Osaka, Japan
Background and Aims: Oral corticosteroids (OCS) are medications for controlling symptoms in patients with Myasthenia Gravis (MG). While long‐term use of high dose OCS is associated with serious side effects, the real‐world clinical impact of high‐dose OCS in patients with MG is not well understood.
Methods: A retrospective cohort study was performed using JMDC, a Japanese claims database. Patients with newly diagnosed MG were identified by standard disease codes and the first diagnosis date of MG was defined as the index date. Patients were stratified into two groups by OCS dose level (high OCS ≥7.5 mg/day; low OCS < 7.5mg/day). Patient characteristics, treatment patterns, long‐term hospitalization (≥10 days), and clinical complications were compared between the two groups.
Results: We identified total 2,107 patients with a diagnosis of MG, 576 of whom were on OCS (high OCS, n = 210; low OCS, n = 366) during the follow‐up period. There were no obvious differences in baseline comorbidities between high and low OCS groups. Intravenous immunoglobulin therapy was more frequent in the high OCS group versus the low OCS group (1.72 vs 1.30 courses/year). A significant increase in long‐term hospitalization was observed in the high OCS group versus the low OCS group (odds ratio; 1.832, p = 0.007). The incidence of new complications such as diabetes, fracture or osteoporosis, neuropsychiatric disease, and sepsis was significantly higher with high OCS versus low OCS (p = 0.0015, 0.0000, 0.0001 and 0.0022, respectively).
Conclusion: Use of high‐dose OCS in patients with MG was associated with adverse outcomes including increased rates of long‐term hospitalizations and clinical complications.
Disclosure: This study was funded by Alexion Pharma GK of which NN, TY and TY are employees. MW and TK are employees of AstraZeneca.
EPO‐481
Bio‐markers profile in different types of encephalitis: Evidences from cerebrospinal fluid analyses
V. Cristillo 1; A. Pilotto1; D. Arici1; I. Volonghi1; E. Magni2; M. Turla3; S. Mariotto4; S. Ferrari4; A. Ciccone5; M. Sessa6; U. Balducci7; V. De Giuli8; F. Castelli9; N. J Ashton10; K. Blennov10; H. Zetterberg10; A. Padovani1
1Neurology Unit, Department odf Clinical and Experimental Sciences, University of Brescia, Italy; 2Neurology Unit, Poliambulanza Hospital, Brescia, Italy; 3Neurology Unit, ASST Valcamonica, Esine, Brescia, Italy; 4Neurology Unit, Department of Neurosciences, Biomedicine and Movement Sciences, University of Verona, Verona, Italy; 5Department of Neurology and Stroke Unit, Carlo Poma Hospital, ASST Mantova, Mantova, Italy; 6Department of Neurology, Papa Giovanni XXIII Hospital, ASST Papa Giovanni XXII, Bergamo, Italy; 7Neurology Unit, ASST Chiari, Chiari, Italy; 8Neurology Unit, Istituti Ospedalieri, ASST Cremona, Cremona, Italy; 9University Division of Infectious and Tropical Diseases, University of Brescia and ASST Spedali Civili Hospital, Brescia, Italy; 10Department of Psychiatry and Neurochemistry, Institute of Neuroscience & Physiology, The Sahlgrenska Academy at the University of Gothenburg, Mölndal, Sweden
Background and Aims: Encephalitis is defined by the presence of brain inflammation. This study was conducted to determine whether neuroinflammation, neuronal and neuroaxonal injury biomarkers could help to differentiate encephalitis and to improve diagnostic approach.
Methods: In this observational multicenter study, adult inpatients, with diagnosis of encephalitis were recruited. Clinical and laboratory features, inclusive of CSF inflammatory (IL‐1β, IL‐6, Il‐8, TNF‐ α, CXCL‐13), neuronal (NfL, p‐Tau, aβ40, aβ42) and glial (GFAP, sTREM‐2, YKL‐40) damage biomarkers, were compared among the 4 groups through ANOVA and k2 test, were appropriate. Post‐hoc analyses were performed using Bonferroni correction at p = 0.05.
Results: One‐hundred‐fifty‐eight encephalitis patients, namely 45 immune‐mediated, 38 infectious, 69 not otherwise specified encephalitis (ENOS) and 63 HC entered the study. CSF cell count and protein levels were higher in the infectious group, compared to IE and ENOS. Infectious encephalitis showed higher inflammation parameters (IL‐6, IL‐8, TNF‐α,) compared to HC and ENOS patients; whereas the chemokine CXCL13 was significant higher in both infectious (p = 0.012) and immune‐mediated (p = 0.013) groups. Glial damage biomarkers were higher in the three different types of encephalitis compared to HC, excepted for sTREM‐2, which showed higher values in both infectious (p < 0.001) and immune‐mediated (p = 0.004) groups, compared to ENOS and HC.
Conclusion: This study indicates a different signature of encephalitis based on different etiologies. Inflammatory alteration was prominent in infectious encephalitis, whereas the B‐cell–attracting CXCL13 was overexpressed in both infectious and immune‐mediated patients, as for axonal damage biomarkers. Further studies are warranted to confirm and improve the diagnostic value of these biomarkers.
Disclosure: Nothing to disclose.
EPO‐482
Evaluating the effect of efgartigimod in myasthenia gravis crisis
W. Haiyan; S. Fangyi; C. Jiaxin; H. Xin; F. Huiyu
Department of Neurology, The First Affiliated Hospital of Sun Yat‐sen University, Guangzhou, China
Background and Aims: In myasthenia gravis (MG) crisis, plasma exchange and immunoglobulin infusion are confirmed effective treatment options, but plasma exchange may not always be available in time, and the response rate to immunoglobulin is not always satisfactory. This study aims to investigate whether the addition of efgartigimod gain benefits for patients with MG crisis.
Methods: We enrolled MG crisis patients who were followed for one year in the NICU and were categorized into two groups: the traditional immunotherapy group and the additional efgartigimod treatment group. The efgartigimod treatment group received a regimen of 20mg/kg, administered on the first and fifth day. The primary endpoints were the duration of mechanical ventilation and the time of discharge.
Results: 19 patients were recruited. The median age at MG onset was 40.89 years. Plasma exchange was performed in 9/19 (47.3%) cases and intravenous immunoglobulin was performed in 15/19 (78.9%) cases. Six patients in the efgartigimod group had shorter hospital stays (16.8 ± 8.7 days vs. 27.41 ± 21.33 days, p = 0.03) and mechanical ventilation durations (17.0 ± 12.71 days vs. 18.25 ± 15.17 days) compared to 13 patients in the conventional treatment group. Additionally, in the efgartigimod group, 66.7% of patients showed a 50% reduction in ADL score from baseline, compared to 38.46% in the conventional treatment group.
Conclusion: The efgartigimod group shows shorter hospital stays and mechanical ventilation durations and the potential to improve muscle weakness in the short term. The trend suggests that efgartigimod could potentially offer advantages in managing the MG crisis.
Disclosure: Nothing to disclose.
EPO‐483
Efgartigimod therapies in N‐methyl‐D‐aspartate receptor encephalitis
D. Wu; B. Luo
Department of Neurology, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, China
Background and Aims: N‐methyl‐D‐aspartate receptor (NMDAR) encephalitis is the most common subtype of autoimmune encephalitis. Patients with NMDAR encephalitis develop an intrathecal immune response against NMDARs with antibodies. The therapeutic response to immunotherapy is often delayed and some patients develop complex neurologic and/or neuropsychiatric syndromes with prolonged course.
Methods: Efgartigimod, a human IgG1 antibody Fc fragment engineered to reduce pathogenic IgG autoantibody levels, was used in 5 patients with NMDAR encephalitis. The mean length of stay in these patients was more than 6 months before the use of efgartigimod.
Results: The patients had all used high‐dose methylprednisolone, immunoglobulin, and rituximab, but they had not improved. Four of 5 patients showed a significant improvement in symptoms within a week after the use of efgartigimod. At the 3‐month follow‐up, they continued to improve without the addition of other medication.
Conclusion: Efgartigimod showed improvement in patient with NMDAR encephalitis with prolonged course.
Disclosure: Our study suggests that efgartigimod may have some potential in the treatment of long‐standing autoimmune encephalitis.
EPO‐484
The therapeutic effect of efgartigimod in autoimmune encephalitis
Q. Zhou 1; H. Meng1; Q. Lin2; S. Chen1
1Department of Neurology, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China; 2Department of Neurology, Fuzhou Second Hospital, Fuzhou, China
Background and Aims: In some cases of autoimmune encephalitis, patients may not respond to first‐line treatments or may experience intolerable side effects of high‐dose steroids or certain immunosuppressive agents, thereby limiting available treatment options. This study explores the therapeutic potential of efgartigimod, a fully humanized FcRn antagonist approved for generalized myasthenia gravis, for the treatment of anti‐LGI1 encephalitis.
Methods: Two patients diagnosed with anti‐LGI1 encephalitis were enrolled, who presenting seizures, cognitive impairment, and psychiatric disorders. Initial treatments with high‐dose steroids and intravenous immunoglobulin showed no significant improvement. Efgartigimod was administered at 10mg/kg once a week for four doses.
Results: In the first 1‐2 weeks of efgartigimod treatment, both patients exhibited notable alleviation of clinical symptoms. Antibody titers decreased, and no severe adverse reactions were observed. A 30‐day follow‐up indicated stable symptoms.
Conclusion: This study is the first to document the application of efgartigimod in treating autoimmune encephalitis. Efgartigimod shows promise as a safe and effective treatment for autoimmune encephalitis. This pioneering report highlights its potential as an innovative therapeutic option for this condition.
Disclosure: Nothing to disclose.
Sleep‐wake disorders 1
EPO‐485
Sleep disorders in children with myotonic dystrophy type 1
E. Erokhina 1; K. Shamtieva2; E. Melnik3; D. Vlodavets1
1Pirogov Russian National Research Medical University, Russian Federation; 2Lomonosov Medical Scientific and Educational Center of Moscow State University, Moscow, Russian Federation; 3Russian Federation Research Centre for Medical Genetics, Moscow, Russian Federation
Background and Aims: Sleep disturbances are common in myotonic dystrophy type 1 (DM1), but most studies have focused on the prevalence of this symptomatology among adults. The purpose of the study was to evaluate the presence and nature of sleep disorders in children with DM1.
Methods: 9 children were examined: 5 girls, 4 boys, average age 11.7+2.7 years. Three patients (33%) had congenital DM1, six (67%) had childhood DM1. Patients underwent polysomnography (PSG) using a portable Somnolab2 PSG device (Loewenstein Medical (Weinmann), Germany).
Results: Changes in sleep architecture among children were similar to those previously described in adults: increased duration of stage 1 sleep, decreased stage 2 sleep, decreased sleep efficiency index. In 7 children (78%), according to PSG results, mild OSA was registered, in 3 (33%) ‐ in combination with REM‐dependent apnea, in 2 (22%) ‐ with central apnea. No sleep disturbances were detected in 2 children (22%). In 87.5% of children, obstructive sleep apnea syndrome was observed in the absence of muscle weakness (8 children (89%) had 2 points on the MIRS scale, which corresponds to the presence of minimal muscle symptoms, 1 patient (11%) had 4 points).
Conclusion: The high incidence of obstructive sleep apnea syndrome in children with DM1 has been confirmed, which occurs even in the absence of significant muscle weakness. So it is advisable to conduct PSG in all patients for earlier diagnosis and treatment of breathing disorders during sleep.
Disclosure: Nothing to disclose.
EPO‐486
Dream experiences during intensive care unit stay: Prevalence, content, vividness, and associated factors
A. van der Hoeven 1; R. Fronczek1; D. Bijlenga1; S. Hadra1; C. Ridder1; M. Henneman2; J. Maas2; S. Goedemans‐de Graaf2; G. Lammers1; D. van Westerloo2; M. Schinkelshoek1
1Neurology Department, Leiden University Medical Center, Leiden, The Netherlands; 2Intensive Care department, Leiden University Medical Center, Leiden, The Netherlands
Background and Aims: Vivid dream experiences in the Intensive Care Unit (ICU) are common, but poorly understood. We investigated the prevalence, vividness, content, emotional impact, and associated factors of dream experiences in the ICU.
Methods: Retrospective qualitative study with subjects ≥18 years, previously admitted to the ICU for ≥4 days and/or due to COVID‐19, who were not sedated for ≥24 hours during their stay (n = 80). Participants were interviewed by telephone. Clinical data were collected from patient files.
Results: Interviews were conducted a median of 9 months post‐discharge. At the time of the interview, dream experiences were reported by 79%. Of patients with dream experiences, 73% reported “life‐like” dreams, and 49% associated their dreams with negative emotions. Some participants (28.6%) continued to have similar dreams at home. The dream content was often related to the ICU admission. Younger age and longer length of stay were related to vivid dream experiences. Of participants with dream experiences 62.5% had experienced delirium during their ICU stay. Perceptual disturbances were also frequently reported by patients (50%) and only 45% could clearly distinguish them from dream experiences. There was an overlap between participants reporting perceptual disturbances and confirmed delirium (70%).
Conclusion: Life‐like dream experiences are common in patients in the ICU and often have a negative emotional impact. To mitigate this impact, some participants suggest receiving information during their hospital stay about the potential for vivid dream experiences could be beneficial. Future studies should explore effective ways to distinguish dreams, delirium, and perceptual disturbances and how to reduce their impact.
Disclosure: Nothing to disclose.
EPO‐487
The burden of gender and depression on sleep inertia in central hypersomnias
A. Pagano; F. Placidi; A. Castelli; G. Di Mauro; C. Ferrazzoli; C. Liguori; N. Mercuri; F. Izzi
Sleep Medicine Center, Department of Systems Medicine, Policlinico Tor Vergata – University of Rome “Tor Vergata”, Rome, Italy
Background and Aims: Sleep inertia (SI) can be defined as difficulty becoming fully awake after sleep. We aimed to evaluate SI in patients affected by hypersomnias of central origin, including narcolepsy type 1 (NT1), narcolepsy type 2 (NT2) and idiopathic hypersomnia (IH) and to study possible association with sex, age, depression, daytime somnolence and polysomnographic (PSG) parameters.
Methods: Patients with NT1, NT2 and IH underwent to nocturnal PSG recording, 5 naps Multi‐sleep latency test (MSLT), Epworth Sleepiness Scale (ESS), Sleep Inertia Questionnaire (SIQ) and Beck Depression Inventory (BDI‐II). SIQ total score and four SIQ subdomains (physiological, SIQ‐P cognitive, SIQ‐C, emotional, SIQ‐E and responses to SI, SIQ‐R) were assessed.
Results: 45 patients (27 females, 18 males, mean age 39.4±15 years) with diagnosis of NT1 (n = 11), NT2 (n = 15), IH (n = 19). Mean SIQ total score didn’t show differences among the three groups (NT1 53±21 vs NT2 56.9±21.4 vs IH 53.6±21.6, p > 0.05), whereas was significantly higher in female (62.7±19.6 vs 42.3±16.9, p < 0.005). Age, BDI, BMI, ESS were comparable in males and females. Strong positive correlation was observed between SIQ (total score and all SIQ subdomains) and BDI‐II (p < 0.01). SIQ‐R negatively correlated with N3 (p < 0.01), whereas was positively associated with Sleep Period Time and Total Sleep Time (p < 0.05). Finally, SIQ does not correlate with age and ESS.
Conclusion: SI assessed by SIQ does not help in the differential diagnosis among hypersomnias of central origin, but appears to be strongly associated with female sex, depression and some polysomnographic parameters.
Disclosure: Nothing to disclose.
EPO‐488
Obstructive Sleep Apnea before and after CPAP titration: Can real‐life data detect gender differences?
A. Pascazio; F. Buracchi Torresi; M. Maestri Tassoni; M. Fabbrini; D. Hoxhaj; M. Barsotti; A. Morana; A. Colitta; G. Siciliano; E. Bonanni
Neurology Unit, Department of Neuroscience, Azienda Ospedaliero Universitaria Pisana, University of Pisa, Pisa, Italy
Background and Aims: Since Obstructive Sleep Apnea (OSA) can have atypical features in women, our aim was to assess gender differences in OSA patients with an indication to use Continuous Positive Airway Pressure (CPAP) before and after treatment.
Methods: In this monocentric retrospective study, we recruited 199 OSA patients with an indication to use CPAP. We assessed gender differences in demographic, polygraphic and clinical features, and CPAP adherence.
Results: Median age was 59.5 (51.0‐69.2) years, with 47 (23.6%) female patients. Median BMI was 31.0 (27.1‐35.6) and apnea hypopnea index (AHI) 45.9 (31.9‐66.0), indicating severe OSA. Twenty‐seven patients (13.6%) suffered from insomnia. Thirty‐eight patients (12.0%) refused CPAP treatment. After 6 (4‐10) months, 85 patients underwent a follow‐up visit showing a residual AHI of 3.3 (1.3‐8.1) and 5.3 (4.4‐6.3) hours of CPAP use. These variables did not show any gender differences. While snoring was the most reported symptom in both women and men (95.8%), women reported more nonrestorative sleep (72.0% vs 55.9%, 0.046), less witnessed apneas (64.0% vs 73.1%, p 0.047) more insomnia (25.5% vs 9.9%, p 0.006) and hypothyroidism (15.0% vs 3.3.% p 0.005). Women with insomnia were older than those without (71 (64‐72) vs 59 (51‐67), p 0.012) and tended to use CPAP for less hours (5.4 (4.4‐5.5) vs 6 (5.5‐6.1), p = 0.072).
Conclusion: In our sample women shared most of clinical features with men, probably due to the severity of OSA. However, women had more nonrestorative sleep and/or insomnia, possibly affecting CPAP adherence, showing it is crucial to take gender into account in clinical practice.
Disclosure: The authors declare no conflict of interest with regards to this paper.
EPO‐489
Heart rate response in spontaneous microarousals uncovers an autonomous nervous dysfunction in narcolepsy type 1
C. Bernardes 1; P. Correia2; M. Ferreira2; J. Moita2; I. Luzeiro1; A. Brás1
1Neurology Department, Coimbra University Hospital Centre, Coimbra, Portugal; 2Sleep Medicine Centre, Coimbra University Hospital Centre, Coimbra, Portugal
Background and Aims: Narcolepsy type 1 (NT1) is characterized by the loss of hypothalamic orexin neurons important in the regulation of sleep‐wake transitions. These cells have also been implicated in autonomous nervous system regulation and its disturbance has been recently suggested in NT1, although still unclear. This study aimed to assess heart rate (HR) response associated with spontaneous microarousals across sleep stages in NT1 compared to healthy controls.
Methods: Ten NT1 patients and 10 age‐matched controls polysomnograpies were examined. Three to seven spontaneous microarousals in each sleep stage preceded by at least 30 seconds of stable sleep were randomly selected and analysed. The HR response was calculated based on the difference between the maximal and average HR during microarousal and average basal HR 10 seconds before the microarousal, and compared between groups.
Results: A total of 428 spontaneous microarousals were analysed (214 NT1 and 214 controls). The duration of spontaneous microarousals was significantly higher in NT1 for N1 (7.6 ± 3.2vs5.8 ± 1.6), N2 (7.0 ± 2.2vs5.8 ± 1.9) and N3 (7.1 ± 2.6vs5.4 ± 1.6). The difference between the average HR during and before microarousals was significantly higher in NT1 across all stages (N1 3.8 ± 5vs0.5 ± 4.3, N2 4 ± 4.5vs0.5 ± 3.9, N3 5.3 ± 6.4vs2.3 ± 4.3 and REM 3.9 ± 6.1vs1 ± 3.3). Considering the difference between maximal HR during and average basal HR before microarousals, a significantly higher variation was verified in N2 (11.5 ± 6.9vs8.9 ± 5.4) and REM (13.4 ± 8.4vs9.2 ± 6.7) for NT1.
Conclusion: The higher HR response in spontaneous microarousals during sleep points toward an enhanced sympathetic activity in the context of possible autonomic dysfunction. This reinforces the importance of looking for dysautonomia in NT1, given the associated morbimortality.
Disclosure: Nothing to disclose.
EPO‐490
REM without atonia index is inversely correlated with asymmetric nigrostriatal denervation in Dementia with Lewy Body
A. Castelli 1; C. Bonomi2; C. Motta2; F. Placidi1; F. Izzi1; N. Mercuri3; A. Martorana2
1Sleep Center, University of Rome Tor Vergata; 2Memory Clinic, University of Rome Tor Vergata; 3Neurology Unit, University of Rome Tor Vergata
Background and Aims: The clinical heterogeneity of alpha‐synucleinopathies is supported by different pathways of Lewy body accumulation. REM sleep behavioural disorder (RBD) is held as clinical marker of “body‐first” phenotype, while nigrostriatal denervation is thought to reflect a “brain‐first” involvement in the context of Parkinson's disease. We investigated the associations between polysomnographic features and DAT‐SPECT findings in a cohort of patients with Dementia with Lewy Bodies (DLB).
Methods: We enrolled 13 patients with DLB (69.71±8.39 years old) diagnosed according to McKeith 2017 criteria, who underwent clinical examination, polysomnography (PSG) ‐ with evaluation of REM without atonia (RWA) index (%) (AASM criteria) ‐ and DAT‐SPECT. Quantitative analyses were performed with the DaT‐QUANT software. We evaluated sleep features in DLB patients and used Pearson's analysis to correlate PSG findings with DaT‐QUANT measures.
Results: In our cohort, 11/13 patients showed PSG‐RWA, 11/13 had altered DAT‐SPECT. We observed a positive correlation between sleep efficiency and Striatal Asymmetry (r = 0.866, p = 0.001) and a negative correlation between sleep latency and Putamen Asymmetry (r = ‐0.608. p = 0.036). Moreover, Caudate Asymmetry correlated inversely with RWA index (r = ‐0.690, p = 0.019) and positively with extrapyramidal motor symptoms measured with UPDRS (r = ‐0.697, p = 0.025).
Conclusion: Asymmetry in nigrostriatal denervation points to brain‐first involvement, due to prevalent ipsilateral connections in the connectome. Our results suggests that in DLB a higher RWA index is linked with more symmetric nigrostriatal impairment (body‐first phenotype), while lower RWA is found in patients with more prominent motor symptoms and asymmetric DAT‐SPECT alterations (brain‐first), supporting the existence of two distinct phenotypes in the disease.
Disclosure: Nothing to disclose.
EPO‐491
Bright light therapy in myalgic encephalomyelitis/chronic fatigue syndrome patients
B. Ludwig; D. Moser; L. Hauer; K. Trimmel; S. Seidel
Department of Neurology, Medical University of Vienna, Vienna, Austria
Background and Aims: Chronic Fatigue Syndrome (CFS), also referred to as Myalgic Encephalomyelitis (ME), is a chronic, debilitating condition of unknown etiology and limited treatment options. Bright light therapy (BLT) has shown controversial results in studies with neurological patients experiencing fatigue symptoms. The aim of the current study was to test the effectiveness of BLT treatment on fatigue and cognitive function in patients with ME/CFS.
Methods: A randomized‐controlled cross‐over study design was chosen in order to provide all patients access to BLT treatment. 33 outpatients who met the diagnostic criteria according to the Institute of Medicine (2015) were randomly assigned to either start out with BLT or waitlist for the course of 2 weeks. After a 2‐week wash‐out phase, the assignment was reversed. Primary outcomes of the study were the Chalder Fatigue Score (CFQ) and the Test of Attentional Performance (TAP). A repeated measures ANOVA was performed to compare the effect of BLT on fatigue and cognitive function at baseline and the end of study.
Results: A statistically significant effect of BLT on subjective fatigue levels (F(1,27) = 6.12, p = 0.02) was found, irrespective of sequence of treatment/waitlist (F(1,27) = 0.587, p = 0.45). There was also a statistically significant effect of BLT on the domains Attention, (F(1,26) = 11.96, p = 0.002), irrespective of sequence of treatment/waitlist (F(1,26) = 0.447, p = 0.51). There was no statistically significant effect of BLT on the domains Divided Attention (F(1,26) = 1.487, p = 0.23) and Go‐No Go (F(1,27) = 1.93, p = 0.18).
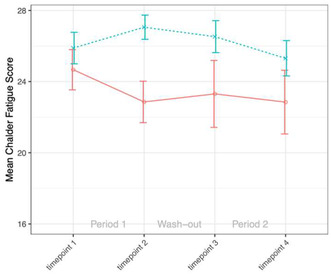
Rating of subjective fatigue with the Chalder Fatigue Score. Red line: group started with bright light therapy. Blue line: group started with waitlist.
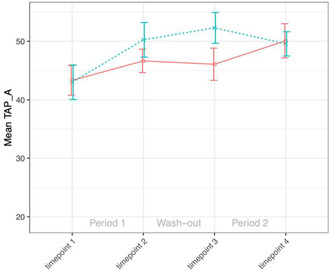
Performance in the subdomain Attention of the standardized Test of Attentional Performance. Red line: group started with bright light therapy. Blue line: group started with waitlist.
Conclusion: These preliminary results suggest moderate effects of BLT on fatigue and cognition. Additional analyses accounting for possible placebo effects need to be considered.
Disclosure: Nothing to disclose.
EPO‐492
Periodic SREDA (subclinical rhythmic electrographic discharges of adults): A case report
C. Brenlla; G. Mayà; A. Muñoz‐Lopetegi; O. Brengaret; C. Gaig; A. Iranzo; J. Santamaría
Neurology Department, Hospital Clínic Barcelona, Barcelona
Background and Aims: SREDA (subclinical rhythmic electrographic discharges of adults) is a benign electroencephalographic (EEG) pattern, consisting of episodes during wakefulness of rhythmic theta activity in the frontoparietotemporal regions, without associated clinical findings. Atypical presentations with focal predominance, delta activity, or appearance during sleep have rarely been reported. It is important to recognize atypical SREDA patterns because they can mimic electrographic seizures.
Methods: We report a patient with atypical SREDA with a high number of episodes occurring periodically during sleep and wakefulness.
Results: A 70‐year‐old woman without past clinical history consulted because of chronic insomnia and nightmares. A nocturnal polysomnogram revealed a moderately reduced sleep efficiency with normal sleep architecture and 67 episodes of SREDA characterized by trains of moderate‐high amplitude, diffuse theta‐delta activity of anterior predominance, at 3‐7 Hz, lasting 1‐2 minutes, recurring every 8‐9 minutes (range 2‐15) throughout all phases of sleep and easily visible in the spectrogram (Figure 2A). A video‐EEG during wakefulness revealed 7 episodes of SREDA (2 of them induced by hyperventilation which also increased their duration, figure 2B). The patient was able to talk, calculate, and perform simple and complex commands correctly.
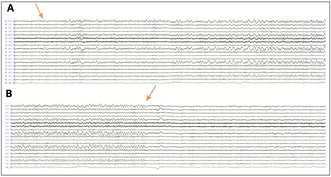
An episode of SREDA starts in A (arrow) consisting of trains of theta‐delta activity at 3‐7 Hz, lasting 1‐2 minutes, with an abrupt ending (arrow in B) and an immediate normalization of the record.
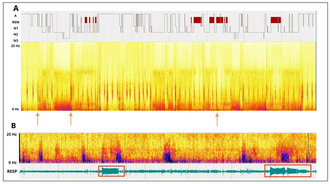
A) Hypnogram of 8 hr sleep recording and B) Daytime wake EEG showing more than 60 episodes of SREDA, indicated by the vertical red lines, appear periodically throughout all stages.
Conclusion: To our knowledge, this is the first report of a SREDA occurring periodically with a high frequency during wakefulness and all stages of sleep. Failure to recognize SREDA can lead to misdiagnoses and unnecessary and potentially harmful use of medication.
Disclosure: Nothing to disclose.
EPO‐493
The role of astrocytes in sleep and memory consolidation
C. Nome; A. Witoelar; P. Qanbari; L. Roth; L. Bojarskaite; L. Bordoni; R. Enger
GliaLab and The Letten Centre, Division of Anatomy, Department of Molecular Medicine, Institute of Basic Medical Sciences, University of Oslo, Oslo, Norway
Background and Aims: Astrocytes are known to participate in homeostatic functions, such as the regulation of extracellular ions, stabilization of the environment surrounding synapses, and regulation of blood flow. Some studies have also indicated that astrocytes might play a role in the regulation of sleep and transitions between sleep states. In this study, our aim is to investigate the role of astrocytes in sleep and memory consolidation in the hippocampus.
Methods: We conducted experiments on 5 BL6 mice, in which we expressed genetically encoded calcium indicators (GCaMP6f) to monitor intracellular calcium levels in astrocytes. Additionally, we surgically inserted a window to the hippocampal CA1 region, as well as LFP and ECoG electrodes. Two‐photon microscopy and electrophysiology recordings were utilized to examine astrocytic calcium signals throughout the sleep‐wake cycle.
Results: Our findings revealed a reduction in astrocytic calcium signaling during sleep, with an increase shortly before awakening. Currently, we are analyzing the relationship between astrocytic calcium signals and various electrophysiological oscillations linked to memory consolidation. We hope to present these results at the conference this year.
Conclusion: Our findings support the hypothesis that astrocytes might be involved in regulation of the different sleep states, and potentially can facilitate EEG oscillations involved in memory consolidation.
Disclosure: None.
EPO‐494
Assessing Obstructive Sleep Apnoea Syndrome risk in Behçet Syndrome patients: An actigraphic approach
A. Colitta 1; S. Bruno2; F. Cruz‐Sanabria2; A. Bazzani3; F. Starace2; E. Bonanni1; G. Siciliano1; M. Mosca4; R. Talarico4; U. Faraguna2
1Department of Clinical and Experimental Medicine, Neurology Unit, University of Pisa, Pisa, Italy; 2Department of Translational Research and of New Surgical and Medical Technologies, University of Pisa, Pisa, Italy; 3Institute of Management, Scuola Superiore Sant'Anna, Pisa, Italy; 4Department of Clinical and Experimental Medicine, Rheumatology Unit, University of Pisa, Pisa, Italy
Background and Aims: Previous studies found a higher risk of Obstructive Sleep Apnoea Syndrome (OSAS) in Behçet Syndrome (BS) patients compared to healthy controls (HCs). However, limited research with proper matching criteria assessed differences in OSAS risk between these populations. Furthermore, actigraphy has recently emerged as a valuable screening tool to estimate OSAS risk, with no studies used actigraphy to characterize BS patients’ sleep. This cross‐sectional study aimed at testing possible differences in both sleep parameters and actigraphic OSAS risk among BS patients and age‐, BMI‐, sex‐, smoking habits‐matched HCs.
Methods: Sleep parameters were evaluated through the Pittsburgh Sleep Quality Index and a 7‐day actigraphic continuous monitoring. Actigraphic OSAS risk was estimated through a validated machine‐learning algorithm, dividing participants into two classes of OSAS risk, i.e., high and non‐high OSAS risk. Possible differences in sleep parameters and actigraphic OSAS risk were tested through nonparametric tests. A binomial logistic regression model with Firth bias reduction method was estimated to test possible predictors of high OSAS risk among participants, i.e., HCs group, age, sex, BMI, being a smoker and smoking intensity.
Results: 45 BS patients (Table 1) and 60 HCs were included in the study. Compared to HCs, BS patients showed significantly lower perceived sleep quality (p < 0.001), actigraphic sleep efficiency (p < 0.044), and OSAS risk (p < 0.010)(Table 2). In the regression model, high OSAS risk was significantly predicted only by the HCs group (beta = 3.16; p < 0.025).
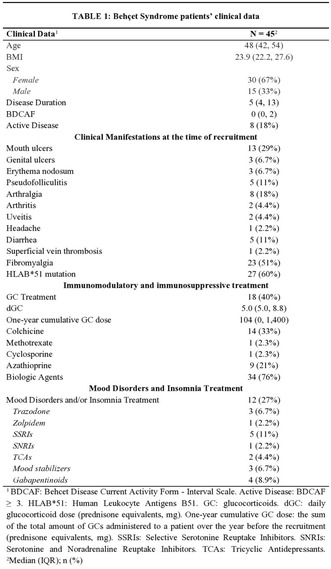

Conclusion: Compared to HCs, BS patients show lower perceived sleep quality, actigraphic sleep efficiency, and OSAS risk, irrespective of age, BMI, sex, and smoking habits.
Disclosure: Ugo Faraguna is President and co‐founder of Sleepacta s.r.l., a University of Pisa spin‐off private company, focused on sleep diagnostics.
EPO‐495
Utilizing transcranial direct current stimulation (tDCS) for insomnia
P. Yi1; Y. Su2; F. Chang 2
1Department of Sport Management/Aletheia University; 2Graduate Institute of Veterinary Medicine/National Taiwan University
Background and Aims: Transcranial direct current stimulation (tDCS) is acknowledged for its non‐invasive modulation of neuronal activity in psychiatric disorders, with varied outcomes observed in insomnia research based on different tDCS types and patient conditions. Our primary goal is to elucidate the effectiveness of tDCS and reveal the underlying mechanisms in treating insomnia. We hypothesize that anodal prefrontal cortex stimulation activates glutamatergic projections from the infralimbic cortex (IL) to the ventrolateral preoptic area (VLPO), promoting sleep.
Methods: Electroencephalogram (EEG) electrodes were surgically implanted for sleep‐wake data capture. The tDCS electrode was positioned over the infralimbic cortex on the skull, with the reference electrode using the EEG reference electrode. Designer receptors exclusively activated by designer drugs (DREADDs) selectively inhibited the IL‐VLPO pathway, aiming to unveil its contribution to tDCS effects.
Results: Administering 0.06 mA of electrical currents for 8 minutes led to a significant increase in non‐rapid eye movement (NREM) sleep in naive mice during the initial 3 hours post‐stimulation, persisting up to 16‐24 hours. In the insomnia group, tDCS enhanced NREM sleep bouts during acute stress response and improved both NREM and REM sleep duration in subsequent acute insomnia. NREM delta powers, assessing sleep quality, remained unchanged. Intervention in the IL‐VLPO pathway using DREADDs with the cre‐DIO system partially inhibited tDCS efficacy in improving sleep in stress‐induced insomnia.
Conclusion: This research clarified that the activation of the IL‐VLPO pathway mediates tDCS's impact on stress‐induced insomnia, providing valuable insights for future investigations and clinical applications in sleep therapy.
Disclosure: Nothing to disclose.
EPO‐496
Screening restless leg syndrome in neuromyelitis optica and myelin oligodendrocyte glycoprotein‐IgG associated disorder
I. Albajar; P. Iruzubieta; J. Equiza; D. Campo‐Caballero; G. Nuñez; N. Andres; M. Arruti; T. Castillo; A. Muñoz‐Lopetegi
Neurology, Donostia University Hospital, Spain
Background and Aims: Restless legs syndrome (RLS) is a sleep disorder which is diagnosed clinically, affecting 5.6% of Spanish population. Neuromyelitis optica spectrum disorder (NMOSD) and Myelin oligodendrocyte glycoprotein‐IgG associated disorder (MOGAD) are immune‐mediated inflammatory conditions of the central nervous system. To our knowledge, RLS in NMOSD or MOGAD had not been studied.
Methods: We designed an observational retrospective study. We reviewed data from 151 patients coded as “NMO”, “MOGAD”, “optic neuritis”, “mielitis” or “isolated clinical syndrome”. 12 met 2015 criteria for NMOSD and 11 met 2023 criteria for MOGAD. 1 met exclusion criteria and we were unable to contact 2. We administered the Cambridge–Hopkins RLS questionnaire by phone, with follow up open ended questions.
Results: In the NMOSD group, median age was 56 (39‐80 y.o.), all female, median EDSS of 4 (0‐8), 9/10 suffered spinal cord lesions. In the MOGAD group, median age was 46 (19‐61 y.o.), 5 female, 5 male, median EDSS of 0 (0‐2), 5/10 suffered spinal cord lesions. 7/10 NMOSD and 3/10 MOGAD had paresthesia, 4/10 NMOSD and 2/10 MOGAD had chronic neuropathic pain and 5/10 NMOSD and 2/10 MOGAD had leg cramps. 4/10 NMOSD and 1/10 MOGAD questionnaires were compatible with definite RLS. However, when asked open‐ended questions 4 patients presented RLS‐mimicks. Only 1 NMOSD patient was diagnosed with mild RLS.
Conclusion: Our work highlights the importance of validating RLS questionnaires in NMOSD and MOGAD patients, as RLS mimics are common. We did not find a higher‐than‐expected prevalence of RLS in these patients.
Disclosure: No disclosures.
EPO‐497
Prevalence of sleep disorders in the elderly: A questionnaire‐based study
S. Maio 1; M. Fernandes2; M. Antonucci2; F. Capecci2; N. Mercuri2; D. Della Morte2; C. Liguori1
1Sleep Medicine Center, Neurology Unit, University Hospital of Rome “Tor Vergata”, Rome, Italy; 2Department of Systems Medicine, University of Rome “Tor Vergata”, Rome, Italy
Background and Aims: Several studies highlighted a high prevalence of sleep disorders in the elderly population: this could depend on different factors including neuropsychiatric comorbidities, medication use or circadian sleep‐wake cycle alterations. The aim of the present study is to assess the prevalence of sleep disorders in geriatrics patients, according to sex and age, through validated screening questionnaires for sleep disorders, global cognition and depression.
Methods: This study included 58 subjects (58.6% women) with a mean age of 77.36 (SD = 6.07) admitted to the geriatrics clinic of the University Hospital of Rome “Tor Vergata”. All participants were clinically evaluated and answered different questionnaires assessing sleep quality (Pittsburgh Sleep Quality Index‐PSQI), insomnia (Insomnia Severity Index‐ISI), sleep apnea risk (Berlin Questionnaire), excessive daytime sleepiness (Epworth sleepiness scale‐ESS), restless legs syndrome (International RLS Study Group Scale‐IRLSS), chronotype (Morningness‐Eveningness Questionnaire‐MEQ), depression (Geriatric Depression Scale‐GDS) and global cognition (Mini‐Mental Examination State‐MMSE).
Results: We observed that the most frequent sleep‐related complaint was worse quality of sleep measured through the PSQI (36.2%; n = 21), followed by sleep apnea risk (34.5%, n = 20), insomnia symptoms (25.9%, n = 15), EDS (15.5%, n = 9) and RLS (12.1%, n = 7). Insomnia symptoms, depression and worse sleep quality were more common in women than in men, while older patients (≥ 75 years) had more comorbidities and higher sleep apnea risk than the younger ones (<75 years).
Conclusion: Sleep disorders are frequent in the elderly and the screening through suitable questionnaires may facilitate their recognition and timely treatment.
Disclosure: Nothing to disclose.
EPO‐498
Nocturnal hypokinesia and sleep in Parkinson's disease
S. Diaconu 1; I. Murasan2; D. Rusu1; B. Opritoiu1; L. Ungureanu1; C. Kakucs3; C. Falup‐Pecurariu1
1Department of Neurology, County Clinic Hospital, Brasov, Romania; Faculty of Medicine, Transilvania University, Brasov, Romania; 2Department of Neurology, County Clinic Hospital, Brasov, Romania; 3Faculty of Medicine, Transilvania University, Brasov, Romania
Background and Aims: Bradykinesia is one of the main pillars in establishing the diagnosis of Parkinson's disease (PD). In addition to affecting diurnal movement, hypokinesia can also occur during the night, affecting the quality of patients' sleep. Objective: Establishing the degree to which nocturnal hypokinesia impacts the sleep of PD patients.
Methods: The sleep of 131 PD patients was analysed using the Parkinson's Disease Sleep Scale (PDSS‐2), Pittsburgh Sleep Quality Index (PSQI), Insomnia Severity Index (ISI) and Athens Insomnia Scale (AIS).
Results: Based on the response to item 9 of the PDSS‐2 ("Did you feel uncomfortable at night because you were unable to turn around in bed or move due to immobility?"), PD patients were grouped into two categories: with nocturnal hypokinesia (PD + hypokinesia), which included 97 (74.04%) participants and no nocturnal hypokinesia (PD – hypokinesia), which included 34 (25.95%) participants. PD + hypokinesia patients showed statistically significantly higher scores than PD ‐ hypokinesia patients for the PSQI scales (10.42 ± 4.84 vs. 6.50 ± 4.22, p < 0.001), PDSS‐2 (27.14 ± 9.61 vs. 13.76 ± 8.44, p < 0.001), ISI (12.23 ± 5.58 vs. 6.21 ± 4.73, p < 0.001) and AIS (9.64 ± 4.59 vs. 4.68 ± 4.48, p < 0.001).
Conclusion: The prevalence of nocturnal hypokinesia among PD patients is high, and the sleep quality of these patients is significantly lower, compared to those with normal mobility during the night. A higher degree of insomnia was also identified among this category.
Disclosure: Nothing to disclose.
EPO‐499
Self‐reported sleep difficulties and potentially inappropriate z‐hypnotic use among older adults in primary care
T. Siddiqui 1; T. Simonsen1; M. Bjelkarøy2; C. Lundqvist2
1Health Services Research Unit, Akershus University Hospital, Lørenskog, Norway; 2Health Services Research, Akershus University Hospital and Inst.Clin.Med, University of Oslo, Norway
Background and Aims: This study aims to assess prevalence and severity of sleep difficulties and potentially inappropriate z‐hypnotic use in a General Practitioner (GP) population, and further to examine the association between potentially inappropriate z‐hypnotics and self‐reported sleep difficulties.
Methods: A cross‐sectional study, including 687 older adults recruited through 31 GPs in south‐east Norway. We defined z‐hypnotics inappropriate use as use over four weeks, three times or more per week. Sleep difficulties were reported as yes/no/sometimes, type, and reasons. Descriptive statistics and logistic regression mixed effect models were conducted.
Results: Out of 687 patients included, 10% had potentially inappropriate z‐hypnotic use. Among all the participants, 22% reported difficulty sleeping. The participants reported trouble falling asleep (12%), trouble staying asleep (24%), and 29% experienced both. They reported various reasons for sleep difficulties, including pain (9%), overthinking at bedtime (27%), and 20 % experienced both, including bereavement in close relations. Patients experiencing difficulty sleeping, problems with falling asleep and staying asleep, and experiencing pain and overthinking at bedtime, had higher odds of being users of potentially inappropriate z‐hypnotics, than patients without these experiences.
Conclusion: Older adults in primary care have a high prevalence of self‐reported sleeping problems and a high proportion of potentially inappropriate z‐hypnotics use. GPs need to be aware of patients sleeping problems and their appropriate treatments.
Disclosure: C.L had support for clinical studies (Lundbeck pharma) and received lecture honoraria. All other authors have nothing to disclose.
Neuroimaging 1
EPO‐500
Evidence for hypometabolism in epileptic focus and GABA alterations in drug‐resistant MRI‐negative TLE
S. Wu 1; G. Yan2; R. Wu1
1Department of Radiology, Second Affiliated Hospital of Shantou University Medical College, Shantou, China; 2Department of Radiology, Second Affiliated Hospital of Xiamen Medical College, Xiamen, China
Background and Aims: Increasing evidence suggests that the hypometabolism of the epileptogenic focus affects the treatment prognosis of temporal lobe epilepsy (TLE). Epileptic seizures involve neurotransmitter synthesis and consumption, accompanied by central nervous system energy substance depletion. Therefore, we attempted to investigate the metabolic levels of the epileptogenic focus through single‐voxel MRS to provide more evidence for the correlation between hypometabolism of the epileptogenic focus and drug‐resistant epilepsy in MRI‐negative TLE.
Methods: 47 patients of MRI‐negative TLE were divided into a drug‐resistant group (n = 9) and a drug‐responsive group (n = 38) based on their response to medication. Brain metabolite concentrations were quantitatively analyzed by using LCModel. MRS data were compared with those of 20 age‐ and gender‐matched healthy controls, analyzing differences in epileptic focus indicated by video‐EEG metabolite changes among different groups.
Results: GABA (gamma‐aminobutyric acid) (p = 0.048), Glu (p = 0.039), NAA (p = 0.002), NAAG (p < 0.001), Cho (p = 0.004), Cr (p = 0.046) concentrations on the epileptic side were significantly lower than contralateral in patients. Interestingly, the difference was most evident in patients with drug‐resistant epilepsy. GABA was significantly different between the drug‐resistant, drug‐responsive, and healthy controls group (p = 0.019).
Conclusion: GABA and Glu levels are significantly reduced on the epileptic side. These metabolite levels were even lower in drug‐resistant epilepsy. Cho and Cr are important substances for brain energy regulation and supply, the reduction of them also affects neurotransmitter synthesis, thereby influencing neuronal excitability. This study supports the correlation between hypometabolism of the epileptic focus and poor prognosis in drug‐resistant MRI‐negative TLE.
Disclosure: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
EPO‐501
Before and after: Favorable radiological evolution in a pseudotumoral form of multiple sclerosis treated with rituximab
B. Rodríguez García 1; M. Ravelo León1; A. González García1; D. Gómez de la Torre Morales1; J. Rodríguez Carrillo1; J. Aguilera Aguilera1; J. Morán Sánchez1; G. Carvalho Monteiro1; J. Velázquez Pérez1; J. Paniagua Escudero2; A. Hernández Lain3; Y. el Berdei Montero1
1Neurology Department, Hospital Universitario de Salamanca, Salamanca, Spain; 2Radiology Department, Hospital Universitario de Salamanca, Salamanca, Spain; 3Pathological Anatomy Department, Hospital Universitario 12 de Octubre, Madrid, Spain
Background and Aims: Pseudotumoral lesions are an unusual demyelinating disease that could be related to multiple sclerosis and may simulate brain tumors, being necessary an appropriate differential diagnosis, even including brain biopsy. We report a case of a relapsing and progressive pseudotumoral form of multiple sclerosis (PFMS) in a patient controlled due to Rituximab.
Methods: Medical history review of a previously healthy 31‐year‐old man who developed ten days of progressive left hemiparesis.
Results: A brain magnetic resonance imaging (MRI) verified a T1 hypointense, T2/FLAIR hyperintense right centrum semiovale lesion with restricted diffusion and incomplete ring enhancement, and another similar left parietooccipital lesion (Fig.1). Cerebrospinal fluid (CSF) analysis showed hyperproteinorrachia, absence of IgG oligoclonal bands, negative anti‐AQP4 and anti‐MOG antibodies and positive HHV‐6 PCR. He was treated with dexamethasone and ganciclovir with full recovery. Nine months later he presented a sudden right homonymous hemianopsia. A brain MRI revealed a new occipitotemporal lesion with the same radiological behaviour (Fig.1). CFS analysis without changes except negativization of HHV‐6. He received five days of intravenous methylprednisolone with full recovery in the visual field. A new control brain MRI few months later manifested an asymptomatic left frontal injury and consequently a brain biopsy was performed. Pathological findings confirmed demyelination and the diagnosis of PFMS (Fig.2). He started biannual rituximab with good tolerability, remaining clinically stable and next brain MRIs didn’t manifest progression (Fig.3).
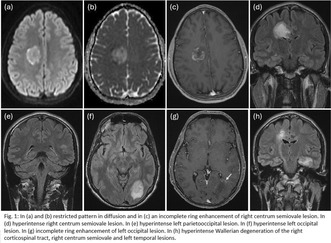
FIGURE 1 Brain MRI: (a) DWI in axial plane. (b) ADC in axial plane. (c) post‐gadolinium T1 in axial plane. (d) and (e) FLAIR in coronal plane. 9 months later: (f) FLAIR in axial plane. (g) post‐gadolinium T1 in axial plane. (h) FLAIR in coronal plane.
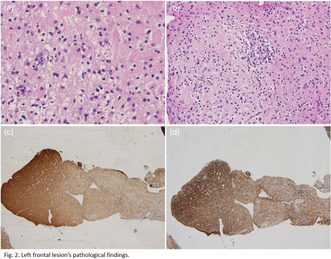
FIGURE 2 (a) Astrogliosis and infiltration by macrophages. Hematoxylin‐eosin (HE). (b) Perivascular inflammatory infiltrates. HE. (c) demyelinating areas. Luxol and staining for myelin. (d) Neurofilaments.
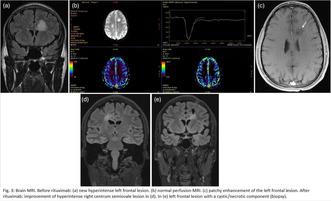
Conclusion: Sometimes the PFMS's diagnosis and treatment are delayed. Further studies and guidelines are required in this field to establish optimal treatment strategies.
Disclosure: Nothing to disclose.
EPO‐502
Unveiling the hippocampal subfield changes across the Alzheimer's disease continuum: a systematic review
B. Pancaldi 1; A. Zilioli1; G. Busi1; F. Misirocchi1; I. Florindo1; D. Berron2; E. Westman3; M. Spallazzi1
1Department of Medicine and Surgery, Unit of Neurology, University‐Hospital of Parma, Parma, Italy; 2German Center for Neurodegenerative Diseases (DZNE), Magdeburg, Germany; 3Division of Clinical Geriatrics; Center for Alzheimer Research; Department of Neurobiology, Care Sciences and Society, Karolinska Institute, Huddinge, Stockholm, Sweden
Background and aims: Studies exploring the hippocampal subregional changes in Alzheimer's disease (AD) have shown contradictory results. This review aims to disentangle such heterogeneity by systematically investigating the dynamic changes of hippocampal subfields across the AD continuum, from the asymptomatic to the dementia stage.
Methods: We systematically searched the PubMed and EMBASE databases for case‐control studies. Selected studies included investigations of biomarker‐based amyloid status and reported data on hippocampal subfield atrophy using advanced neuroimaging techniques. We assessed the quality of the studies using the Joanna Briggs Institute (JBI) Collaboration's ten‐item checklist for case‐control studies.
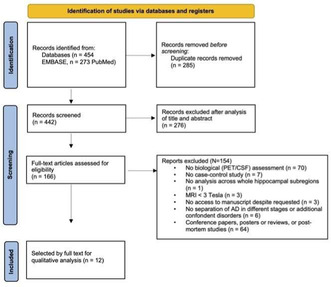
TABLE 1 Modified version of the PRISMA flow chart (Page et al., 2021).
Results: We systematically searched the PubMed and EMBASE databases for case‐control studies. Selected studies included investigations of biomarker‐based amyloid status and reported data on hippocampal subfield atrophy using advanced neuroimaging techniques. We assessed the quality of the studies using the Joanna Briggs Institute (JBI) Collaboration's ten‐item checklist for case‐control studies.
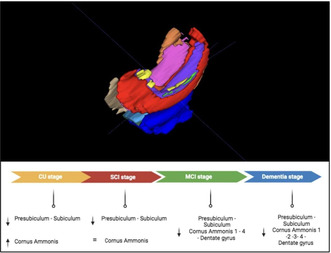
FIGURE 1 An example of hippocampal subfield segmentation with 3D reconstruction obtained using the Automated Segmentation of Hippocampal Subfields software on a high‐resolution T2 coronal sequence, along with an exploration of the dynamic changes in hippoca.
Conclusion: A distinguishable pattern of involvement of hippocampal subfields can be recognized from the cognitively unimpaired phase to the dementia stage, shedding light on hippocampal changes with disease progression, as well as the functional role of hippocampal subregions.
Disclosure: Nothing to disclose.
EPO‐503
Right temporal variant frontotemporal dementia: A multimodal MRI analysis of a new emerging syndrome
D. Salvatori 1; C. Gallingani1; C. Carbone1; M. Tondelli1; R. Bedin2; G. Vinceti2; A. Chiari2; G. Zamboni1
1Department of Biomedical, Metabolic and Neural Sciences, University of Modena and Reggio Emilia, Italy; 2Neurology Clinic, Azienda Ospedaliero Universitaria of Modena, Italy
Background and Aims: Right‐temporal‐variant frontotemporal dementia (rtvFTD) is characterized by right anterior temporal lobe (rATL) atrophy and peculiar clinical presentation. Clinical diagnosis is challenging since rtvFTD shares features with both behavioral‐variant FTD (bvFTD) and semantic‐variant primary progressive aphasia (svPPA). Few studies investigated patterns of gray matter (GM) atrophy. Even less is known about white matter (WM) involvement. We conducted a preliminary‐MRI‐study on the rtvFTD neuroimaging features.
Methods: We compared GM volume and WM microstructural integrity in rtvFTD and svPPA patients and healthy controls, using voxel‐based morphometry (VBM) and tract‐based spatial statistics (TBSS), considering age and disease duration as covariates of no interest.
Results: SvPPA patients showed GM atrophy in the left temporal structures relative to HC. rtvFTD patients compared to HC showed GM atrophy in the right fronto‐temporal structures, but also in insula bilaterally and in left temporal and orbitofrontal cortices. RtvFTD were more atrophic than svPPA patients in fronto‐temporal regions bilaterally. Moreover, rtvFTD patients had less WM integrity than controls in corpus callosum, right inferior fronto‐occipital, inferior longitudinal and uncinate fasciculi. SvPPA patients had decreased WM integrity in corpus callosum and left inferior fronto‐occipital fasciculus.
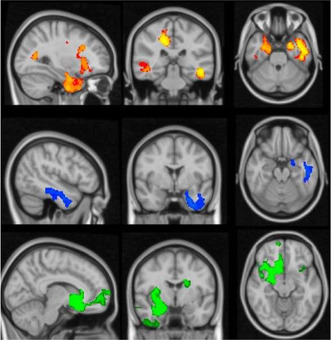
Results of VBM analysis. In red‐yellow, regions of rtvFTD patients’ GM atrophy compared to controls. In blue svPPA patients’ GM atrophy compared to controls. In green regions of rtvFTD patients’ GM volume greater reduction in comparison to svPPA patients.
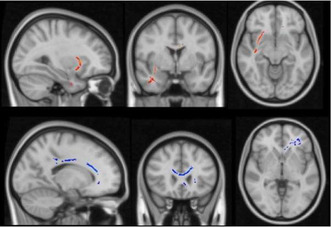
Results of TBSS analysis. In red‐yellow, regions of rtvFTD patients’ decreased WM integrity compared to controls. In blue‐light blue regions of svPPA patients’ decreased WM integrity compared to controls.
Conclusion: RtvFTD patients show greater atrophy compared to svPPA patients in both hemisphere, independently of disease duration, suggesting that rtvFTD and svPPA do not mirror each other in GM loss and that a neurodegenerative process starting in the right hemisphere must be more widespread to become clinically evident. Moreover rtvFTD patients show WM disruption in fasciculi which have been implicated in face recognition, emotion processing and language functions.
Disclosure: Nothing to disclose.
EPO‐504
In‐vivo PET study of mitochondrial complex 1, sigma‐1, & synaptic vesicle 2A in amyotrophic lateral sclerosis patients
E. de Natale 1 ; J. Verghese1; A. Terry1; H. Wilson1; P. Khosropanah1; H. Wright1; L. Passamonti2; K. Evans2; R. Comley3; H. Tsukada4; J. Passchie5; G. Searle5; E. Pererva5; R. Gunn5; E. Rabiner5; M. Politis1; MIND‐MAPS Consortium
1Neurodegeneration Imaging Group, University of Exeter Medical School, London, UK; 2Biogen, Cambridge, MA, USA; 3AbbVie, North Chicago, IL, USA; 4Hamamatsu Photonics, Hamakita, Hamamatsu, Shizuoka, Japan; 5Invicro Centre for Imaging Sciences, Hammersmith Hospital, London UK
Background and Aims: This study investigates the potential link between mitochondrial energy dysfunction and synaptic impairment that may contribute to neurodegeneration in Amyotrophic Lateral Sclerosis (ALS). We present preliminary findings from an ongoing longitudinal in‐vivo imaging study of mitochondrial complex‐1 (MC1), synaptic vesicle protein‐2A (SV2A), and sigma‐1 receptor (S1R), in ALS patients.
Methods: Nine patients with sporadic ALS (mean age: 59.1±9.7 years, King's staging: 2.42±1.08), and nine matched healthy controls (HC, mean age: 54.2±13.7 years), underwent clinical evaluation, a 3T MRI, and PET/CT scans using [18F]BCPP‐EF for MC1, [11C]UCB‐J for SV2A, and [11C]SA‐4503 for S1R. Analysis deployed the Clinical Imaging Centre atlas for cortical and subcortical Region of Interest (ROI). Volume of distribution (VT) was the primary outcome measure for each tracer. Additional measures included VT corrected for plasma free fraction (VT/fp), and Distribution Volume Ratio minus 1 (DVR‐1), using the Centrum Semiovale as reference. Due to notable volumetric differences between ALS and HC in cortical and subcortical ROIs, partial volume correction was applied.
Results: The ALS cohort had a mean ALSFRS of 41.44±4.5. Trends of lower [18F]BCPP‐EF VT was observed in ALS patients, with significant difference in the amygdala (‐16.4%, p = 0.026). Conversely, [11C]UCB‐J VT was significantly greater in the posterior cingulate (+11.2%, p = 0.036) in ALS. No significant differences were detected in [11C]SA‐4503 binding.
Conclusion: These preliminary, cross‐sectional findings, provide initial evidence of altered MC1 and SV2A expression in ALS patients, compared with healthy controls. Collection of clinical and imaging data for up to 16 ALS patients, at baseline and at follow‐up, is ongoing.
Disclosure: This research was conducted with support from Invicro, a Konica Minolta Company and the MIND‐MAPS Consortium, incorporating AbbVie, Inc., Biogen, Inc., Celgene, Inc., Pfizer, Inc., and Takeda, Inc. EAR is an employee of Invicro, KCE was an employee and stock‐holder of Biogen at the time the study was conducted. RAC is an employee and shareholder of AbbVie Inc.
EPO‐505
Synaptic density loss in patients with multiple system atrophy: An in‐vivo [11C]UCB‐J PET molecular imaging study
H. Wilson1; E. de Natale1; A. Terry 1; J. Verghese1; G. Pagano1; P. Khosropanah1; L. Passamonti2; R. Hutchison2; K. Evans2; H. Wright1; M. Howard1; L. Cashmore1; Y. Lewis3; E. Rabiner3; M. Politis1
1Neurodegeneration Imaging Group, University of Exeter Medical School, UK; 2Biogen, Cambridge, MA, USA; 3Invicro Centre for Imaging Sciences, Hammersmith Hospital, London UK
Background and Aims: This study represents an initial in‐vivo investigation of pre‐synaptic terminal density in patients with Multiple System Atrophy (MSA), using the synaptic vesicle glycoprotein 2A (SV2A) selective PET radioligand [11C]UCB‐J.
Methods: Ten MSA patients classified according to the 2022 Movement Disorders Society diagnostic criteria (n = 5 MSA‐P; n = 5 MSA‐C, age: 61.6±5.7), underwent a [11C]UCB‐J PET scan with arterial blood collection. For comparison, [11C]UCB‐J PET previously acquired from 11 Parkinson's disease (PD, age: 59.0±9.0) and 16 healthy controls (HCs, age: 61.4±12.5). We employed a one tissue‐compartment model to calculate total volumes of distribution (VT) for each a priori defined region‐of‐interest, and subsequently calculated a regional distribution volume ratio parameter (VTROI/ VTCSO = DVR‐1) using the centrum semiovale (CSO) as a pseudo‐reference region.
Results: [11C]UCB‐J DVR‐1 was significantly decreased in MSA compared to HCs in the putamen (‐17%; p = 0.001), brainstem (‐39%; p = 0.022) and cerebellum (‐22%; p = 0.003). MSA‐P exhibited a reduction in [11C]UCB‐J DVR‐1 in the putamen compared with HCs (‐27%; p < 0.001) and PD (‐20%; p = 0.05), and additionally in the brainstem (‐42%; p = 0.03) and cerebellum (‐26%; p < 0.001) compared to HCs. MSA‐C showed decreased [11C]UCB‐J DVR‐1 in the cerebellum (‐18%; p = 0.053) compared to HCs. [11C]UCB‐J DVR‐1 in the putamen was lower in MSA‐P compared to MSA‐C (‐28%; p = 0.014). Alternative outcome parameters (VT and VT/plasma free fraction) showed similar patterns of reduction.
Conclusion: Our initial findings show evidence of reduced SV2A density in brain regions known to be affected by MSA pathology. Baseline and longitudinal follow‐up data collection is ongoing to assess if [11C]UCB‐J PET can effectively track disease progression.
Disclosure: This research was conducted with support from Invicro, a Konica Minolta Company and the MIND‐MAPS Consortium, incorporating AbbVie, Inc., Biogen, Inc., Celgene, Inc., Pfizer, Inc., and Takeda, Inc. EAR is an employee of Invicro, KCE was an employee and stock‐holder of Biogen at the time the study was conducted.
EPO‐506
Abstract withdrawn
EPO‐507
Functional connectivity and microstructural integrity changes in Amyotrophic Lateral Sclerosis
P. Khosropanah1; H. Wilson 1; E. Rosario de Natale1; J. Verghese1; A. Terry1; L. Passamonti2; K. Evans2; C. Bishop3; J. O’Callaghan3; E. Rabiner3; M. Politis1
1Neurodegeneration Imaging Group, University of Exeter Medical School, UK; 2Biogen, Cambridge, MA, USA; 3Invicro Centre for Imaging Sciences, Hammersmith Hospital, London UK
Background and aims: This study aims to provide a comprehensive analysis, integrating structural, microstructural, and functional aspects, to understand brain changes and functional reorganization in Amyotrophic Lateral Sclerosis (ALS) through Magnetic Resonance Imaging (MRI). This differs from prior research focusing on individual MRI aspects.
Methods: We conducted 3‐Tesla MRI scan on twelve ALS patients (age = 56±12.3) and sixteen healthy (age = 56±15.8) individuals. The sequences included diffusion tensor imaging, resting‐state functional MRI, and structural‐MRI. We analysed fractional anisotropy (FA), local functional connectivity, and cortical thickness using Tract‐Based Spatial Statistics, Regional Homogeneity (ReHo), and surface‐based methodologies, respectively.
Results: ALS patients exhibited significant atrophy in the bilateral precentral gyrus, left temporal pole, right‐caudal‐middle frontal gyrus, and pars‐opercularis (p < 0.01). Left precentral atrophy correlated with King's scale‐staging (r = ‐0.67, p = 0.022). Compared to controls, ALS showed altered local signal coherence (ReHo) in multiple regions (pAlphaSim < 0.05, cluster‐size >45 voxels), including frontal lobes, occipital, hippocampal areas, fusiform gyrus, and cingulum. ReHo was decreased in regions displaying significant atrophy (p < 0.05), except for increased coherence in the right precentral. Reduced ReHo in the right middle frontal gyrus correlated with worse executive function on ECAS (r = 0.73, p = 0.009). FA was reduced in ALS in the bilateral posterior thalamic radiation, superior longitudinal fasciculus, posterior and anterior limb of internal capsule, corona radiata, cerebral peduncle, corpus callosum (body and splenium), motor fibers, fornix, and sagittal stratum (p < 0.05).
Conclusion: Our multiparametric MRI study highlights complex compensatory mechanisms in ALS brain. Cortical atrophic areas, especially precentral, showed increased local functional connectivity. This underscores the intricate interplay between structural and functional changes in ALS.
Disclosure: This research was conducted with support from Invicro, a Konica Minolta Company and the MIND‐MAPS Consortium, incorporating AbbVie, Inc., Biogen, Inc., Celgene, Inc., Pfizer, Inc., and Takeda, Inc. EAR is an employee of Invicro, KCE was an employee and stock‐holder of Biogen at the time the study was conducted.
EPO‐508
Lipopolysaccharide induced microglial activation in Parkinson's disease patients: An in vivo PET study
E. de Natale1; J. Verghese1; A. Terry1; H. Wilson 1; S. Antoniadis1; P. Khosropanah1; M. Howard1; H. Wright1; L. Cashmore1; A. Thomann2; V. Machado2; B. Zinnhardt2; G. Pagano2; M. Politis1
1Neurodegeneration Imaging Group, University of Exeter Medical School, UK; 2Roche Pharma Research and Early Development, Neuroscience and Rare Diseases Discovery and Translational Area, Roche Innovation Center Basel, Switzerland
Background and Aims: Neuroinflammation plays a critical role in Parkinson's disease (PD) pathophysiology, but the exact underlying mechanisms are still unclear. We present preliminary data of an in vivo Positron Emission Tomography (PET) study with [11C]PBR28 and a pharmacological challenge with Lipopolysaccharide (LPS), aiming to visualise acute translocator protein (TSPO) changes reflecting microglial activation in PD.
Methods: Four people with Parkinson's (PwP), three with early disease (mean age 63.3±15 years) and one with MCI (age 61 years), and three healthy controls (mean age 61.33±10.41 years), underwent a PET/MR scan with [11C]PBR28 before, and four hours after intravenous injection of LPS (dose: 1ng/Kg). Percentage change of volume distribution (VT) in cortical and subcortical regions of interest was calculated with the formula %ΔVT = [(VTpostLPS/VTpreLPS) −1] x 100.
Results: PwP with early disease showed higher post‐LPS TSPO levels compared to controls, more marked in frontal cortex (42.6% vs 32.1%), temporal cortex (45.4% vs 34.0%), hippocampus (34.3% vs 21.8%), amygdala (48.1% vs 13.6%), thalamus (48.8% vs 32.9%) and midbrain (38.8% vs 18.7%). The PwP with MCI showed smaller change of TSPO levels after LPS challenge in frontal cortex (15.2%), temporal cortex (13.4%), hippocampus (13.5%), amygdala (8.6%), thalamus (15.1%), and midbrain (15.0%).
Conclusion: These preliminary data show a trend for the differential widespread expression of microglial activation of PwP and healthy controls following a challenge with LPS which may provide valuable insights in the understanding of innate immune response. The process of gathering more data from additional PwP and healthy control subjects is currently in progress.
Disclosure: G.P., A.E.T., B.Z., and V.M. are full‐time employees and shareholders of F.Hoffmann‐La Roche Ltd.
EPO‐509
MRI–based radiomics features to predict post‐stroke cognitive impairment: A pilot study
H. Dragoș 1; A. Stan1; D. Muresanu2
1Department of Neurosciences, “Iuliu Hatieganu” University of Medicine and Pharmacy, Cluj‐Napoca, Romania; 2RoNeuro Institute for Neurological Research and Diagnostic, Cluj‐Napoca, Cluj, Romania
Background and Aims: Post‐stroke cognitive impairment (PSCI) occurs in about 20% of acute ischemic stroke (AIS) patients within the first months and is associated with poor long‐term prognosis. MRI radiomics surpasses standard MRI in assessing the heterogeneity of AIS lesions and the subtle regional changes. This study aimed to develop a predictive model incorporating MRI radiomics features and clinical factors to accurately predict PSCI six months after AIS.
Methods: Data were collected from 40 patients with first‐ever symptomatic supratentorial AIS confirmed by brain MRI without a history of cognitive impairment or dementia. AIS lesions were segmented using ADC and FLAIR images. First‐ and second‐order statistics radiomics features were extracted using PyRadiomics software. Neuropsychological assessments consisting of the Montreal Cognitive Assessment test, Digit Symbol, Digit Backward, Stroop Color‐Word Test, and Rey Auditory Verbal Learning test were performed one and six months after AIS.
Results: Baseline modified Rankin scale, National Institutes of Health Stroke Scale (NIHSS) score and radiomics score were independent predictors of PSCI. The area under the ROC curve of the clinical‐radiomics model was 0.84 in the training cohort and 0.87 in the validation cohort.
Conclusion: The clinical‐radiomics models outperformed individual clinical or radiomics models and seem to be a useful tool in predicting PSCI.
Disclosure: Nothing to disclose.
EPO‐510
New Year, new headache: A case report of spontaneous intracranial hypotension following a fall on New Year's Eve
I. Pueschel 1; J. Gerber2; J. Schaefer1
1Department of Neurology, University Hospital Carl Gustav Carus, Technische Universität Dresden; 2Department of Diagnostic and Interventional Neuroradiology, University Hospital Carl Gustav Carus, Technische Universität Dresden
Background and Aims: Spontaneous intracranial hypotension (SIH) is characterised by postural headache and is usually associated with cerebrospinal fluid (CSF) leaks. The main reasons for CSF leaks include dural tears and meningeal diverticula [1]. Tarlov cysts, CSF filled perineural cysts, constitute a very cause of SIH.
Methods: A 26‐year‐old female presented to the emergency department with postural headaches following a fall on New Year's Eve. Spinal magnetic resonance imaging (MRI) revealed a large sacral Tarlov cyst, as well as fluid accumulation along the S1 nerve root and free fluid in the presacral area. Cerebral MRI disclosed bilateral subdural hygromas. Digital subtraction myelography (DSM) and postmyelographic CT revealed a communication between the Tarlov cyst, the epidural and intrathecal spaces as well as a pathologic contrast distribution pattern beyond the cyst. Conservative management, encompassing bed rest, analgesics, caffeine, and intravenous fluids, was initiated.
Results: After ten days of conservative treatment, the patient achieved sufficient symptom control, even after discontinuation of all analgesics. Gradual mobilization was successful, leading to discharge after a total of 14 days.
Conclusion: Clinical and imaging findings indicated spontaneous intracranial hypotension, triggered by a traumatic rupture of an unusually large Tarlov cyst. The success of conservative management in this case suggests that, even with traumatic dural tears, a watchful waiting strategy may be considered before opting for more invasive interventions such as autologous blood patch or surgical treatment.
Disclosure: Nothing to disclose.
EPO‐511
Nerve ultrasound versus MR‐Neurography monitoring disease course in chronic inflammatory demyelinating polyneuropathy
B. Lüling1; F. Preisner2; J. Motte1; A. Fisse1; T. Grüter3; T. Godel2; D. Schwarz2; S. Heiland2; M. Yoon4; R. Gold1; M. Bendszus2; M. Kronlage2; K. Pitarokoili 1
1Department of Neurology, St. Josef Hospital, Ruhr University of Bochum, Bochum, Germany; 2Department of Neuroradiology, Neurological Clinic, Heidelberg University Hospital, Heidelberg, Germany; 3Department of Neurology, Evangelical Hospital Lippstadt, Lippstadt, Germany; 4Department of Neurology, Evangelical Hospital, Hattingen, Germany
Background and Aims: We evaluated nerve ultrasound (NUS) and magnetic resonance neurography (MRN) for the longitudinal assessment of patients with chronic inflammatory demyelinating polyradiculoneuropathy (CIDP).
Methods: Twelve CIDP patients, who had received an initial MRN and NUS examination in 2016, were re‐examined six years later in 2022. The cross‐sectional area (CSA) of all peripheral nerves were evaluated with NUS bilaterally. The lumbosacral plexus, and sciatic, tibial and fibular nerves were evaluated using MRN (T2 weighted imaging and diffusion tensor imaging (DTI)). Imaging parameters were compared between time‐points in correlation to clinical assessment.
Results: Over six years, nerve CSA of CIDP patients decreased at the lumbosacral plexus in MRN (p = 0.015) and remained stable in NUS. Comparison of the MRN values of the tibial nerve and fibular nerve at the popliteal fossa with a Bland‐Altman analysis showed of bias of 2.195 and – 1.903 respectively. Longitudinally, changes in CSA of the lumbosacral plexus (MRN) and tibial nerve (MRN and NUS) correlated with changes in the inflammatory neuropathy cause and treatment validated overall disability sum score (INCAT/ODSS) (p = 0.006). Nerve CSA in the initial scan in MRN and nerve ultrasound were inversely correlated with changes in the INCAT/ODSS over six years (p < 0.05).
Conclusion: This study confirms the relevance of imaging studies for treatment monitoring in CIDP showing that nerve ultrasound and magnetic resonance neurography can provide reliably CSA values of proximal nerve segments and that changes in nerve CSA for proximal nerve segments reflects the clinical course of CIDP patients.
Disclosure: Nothing to disclose.
EPO‐512
Drop attacks as a presenting form of superficial central nervous system siderosis
D. Cerdán Santacruz1; C. Gómez López de San Román1; M. Capra 1; M. Vargas Cobos1; L. Caballero Sánchez1; I. Bermejo Casado1; M. Álvarez de Eulate2; A. Castrillo Sanz1; P. Guerrero Becerra1; A. Mendoza Rodríguez1
1General Hospital of Segovia, Neurology; 2General Hospital of Segovia, Radiology
Background and Aims: Superficial siderosis of the CNS is a chronic condition with a broad differential diagnosis consisting of hemosiderin deposition in the subpial layers of the brain and spinal cord due to chronic bleeding into the subarachnoid space.
Methods: A 41‐year‐old female patient attended at neurology clinic for 4 months history of episodes consisting in sudden falls without warning. The patient's gaze remained fixed, with no speech, no sphincter relaxation or other abnormal movements with recovery in a few minutes but with a feeling of "slowness". The neurological examination is normal. In view of the suspicion of possible complex focal seizures, an EEG study was requested, as well as cranial and spinal MRI.
Results: EEG showed only isolated theta wave bursts of sharp morphology in the right temporal region. Axial T2‐weighted brain MR images show hemosiderin deposition along the cerebellar folia, vermis and around the midbrain, pons and Sylvian fissures. Lumbar cord MRI T2‐weighted image showed a fluid‐filled epidural collection anterior to the spinal cord.
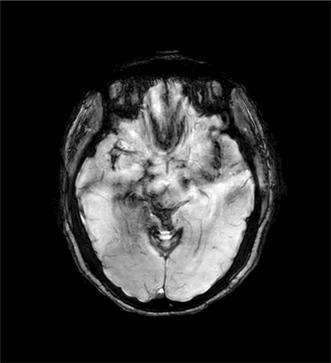
Axial T2_Sylvian fissures
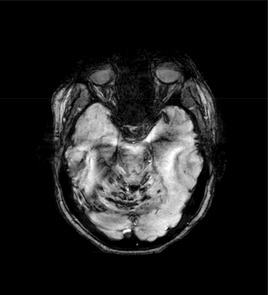
Axial T2_cerebellar folia, midbrain, pons
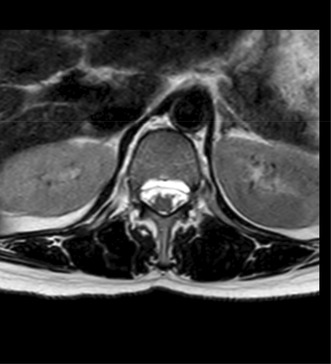
Lumbar cord
Conclusion: Superficial central nervous system siderosis has a myriad of underlying aetiologies, which vary according to the age of presentation. The clinical picture is varied, depending on where the haemosiderin deposits are located, ranging from asymptomatic cases to frequent symptoms such as gait ataxia, hearing loss or myelopathy. Seizures may occur in less than 5% of patients.
Disclosure: Nothing to disclose.
EPO‐513
Neuroimaging of the brain in children with myotonic dystrophy type 1
E. Erokhina 1; K. Shamtieva2; E. Melnik3; D. Kazakov1; D. Vlodavets1
1Pirogov Russian National Research Medical University, Moscow, Russian Federation; 2Lomonosov Medical Scientific and Educational Center of Moscow State University, Moscow, Russian Federation; 3Research Centre for Medical Genetics, Moscow, Russian Federation
Background and Aims: Myotonic dystrophy type 1 (DM1) is characterized by multisystem symptoms, in particular damage of the central nervous system. The purpose of the study was to evaluate changes in brain in children with different forms of DM1.
Methods: 13 children underwent magnetic resonance imaging (MRI) on a Magnetom Avanto Siemens Healthineers (Germany) with a magnetic induction value of 1.5 Tesla using a head coil. The MRI protocol included T1, T2 and T2 FLAIR weighted sequences (WI).
Results: All children with congenital DM1 had changes in the brain based on MRI. Lesions in the white matter were identified in 66.7%, including periventricular localization (50%), frontal and temporal (33.3%), parietal and occipital (16.7%). A third of patients with congenital DM1 have ventriculomegaly. Only two patients (28.6%) with the childhood form had hyperintense foci in the periventricular region and frontal regions of the brain on MRI. The pattern of lesions in the white matter of the temporal regions characteristic of DM1 was not detected in any patient, either with congenital or childhood forms. Signs of atrophy of the gray matter of the brain when assessed on the GCA scale were detected in 66.7% of patients with the congenital form. Patients with the childhood form were not characterized by gray matter damage.
Conclusion: The congenital form of DM1 is characterized by more pronounced damage white and gray matter of the brain compared to the childhood form. Children are not characterized by a specific pattern of hyperintensity of the temporal poles, which apparently appears at a later age.
Disclosure: Nothing to disclose.
Epilepsy 3
EPO‐514
Abstract withdrawn
EPO‐515
Epileptic seizures and cardiac disturbances: Expanding the brain‐heart connection
L. Fernández Llarena 1; A. Marinas Alejo2; P. De Ceballos Cerrajería2; I. Garamendi Ruiz2; A. Moreno Estébanez1; S. Ontiveros Navarro3; M. Sánchez Horvath3; C. Santos Sánchez3; C. Valido Reyes1; A. Rebollo Pérez1; V. Fernández Rodríguez1; A. Lagüela Alonso1; V. Anciones Martín1; Á. López Prado1; M. Martínez Seijas1; A. Rodríguez‐Antigüedad Zarrantz1
1Neurology Department, Cruces University Hospital, Osakidetza Basque Health Service, Barakaldo, Spain; 2Epilepsy Monitoring Unit, Neurology Department, Cruces University Hospital, Osakidetza Basque Health Service, Barakaldo, Spain; Epilepsy Group, Biocruces Bizkaia Health Research Institute, Osakidetza Basque Health Service, Barakaldo, Spain; 3Epilepsy Monitoring Unit, Neurophysiology Department, Cruces University Hospital, Osakidetza Basque Health Service, Barakaldo, Spain; Epilepsy Group, Biocruces Bizkaia Health Research Institute, Osakidetza Basque Health Service, Barakaldo, Spain
Background and Aims: The objective of this work is to analyse cardiac rhythm disorders induced by epileptic seizures registered in a long‐term video‐electroencephalography (v‐EEG) monitoring unit.
Methods: Single‐centre retrospective study of cases of ictal bradycardia, atrioventricular block (AVB), asystole and atrial fibrillation (AF) in patients admitted to the long‐term v‐EEG monitoring unit of our hospital, between 2012 and 2023. We excluded cases with ictal tachycardia due to its high frequency and those with cardiac arrhythmia.
Results: Cardiac rhythm disorders produced by a concomitant ictal discharge were documented in 30 patients (3’3%) out of 908 monitoring conducted over the 12 years of the study. Ictal bradycardia was detected in 19 patients (2.1%), 7 of them occurring in the postictal phase; 9 patients (1%) presented ictal asystole, with the lengthiest episode lasting 31 seconds; 1 patient (0.1%) had ictal AVB, and 1 patient (0.1%) experienced ictal AF. Long‐term v‐EEG monitoring revealed a temporal onset in 21 patients and an extratemporal onset in 9 patients, which usually were frontal or fronto‐central. Among the recorded cases of ictal asystole, 2 patients required pacemaker placement. No patient experienced Sudden Unexpected Death in Epilepsy (SUDEP).
Conclusion: Ictal cardiac rhythm disturbances are an uncommon, poorly known, and underdiagnosed entity that have prognostic implications due to their association with increased morbidity and mortality. In our series, they were mostly related to epilepsies with temporal onset or involvement. The role of combined long‐term v‐EEG and electrocardiographic (ECG) monitoring is essential for their diagnosis, particularly in patients who exhibit sudden generalized hypotonia during epileptic seizures.
Disclosure: No disclosure to declare.
EPO‐516
Status epilepticus and acute cauda equina syndrome following intrathecal lidocaine administration: A case series
L. Pellegrino; G. Bruschi; D. Seppi; S. Favaretto; F. Dainese
Department of Neuroscience, Neurophysiopathology Unit, Neurology Clinic, Azienda Ospedale Università Padova, Padua (PD)
Background and Aims: Lidocaine (LA) is a widely used local anesthetic and analgesic, and a potential therapeutic option for status epilepticus; however, due to its neurotoxicity, it carries an associated risk of inducing life‐threatening seizures and other neurological condition. The semiology and the treatment of these induced seizures remain poorly understood.
Methods: To describe the seizure‐related behavior, clinical presentation, electroencephalographic patterns, and management strategies associated with incidental intrathecal LA administration.
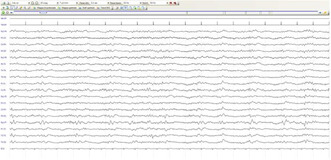
EEG_second_patient
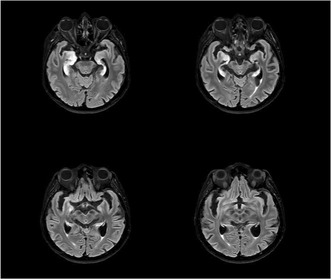
RM_assial_FLAIR
Results: We present the three cases of two female of 80‐ and 42‐year‐old and a 39‐year‐old man who developed sudden cauda equina syndrome, bilateral mydriasis, altered state of consciousness, trismus, and clonic movements in the limbs after incidental paravertebral LA injection for chronic lumbar back pain. All patients were admitted to Intensive Care Unit. Blood and CFS tests were unremarkable. In two cases EEG showed generalized and lateralized periodic pattern. In one case, brain MRI showed bilateral hippocampal cytotoxic edema. Outcomes were various, one patient died and another developed mild cognitive impairment.
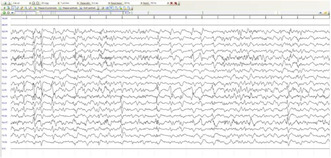
EEG_first_patient
Conclusion: To this day, toxicity of intrathecal lidocaine administration is not clearly defined. This work can help healthcare personnel to provide accurate management of this rare iatrogenic condition.
Disclosure: Nothing to disclose.
EPO‐517
Digital biomarkers and cognitive proxies for personalized care in epilepsy
L. Imbach; H. Jokeit
Swiss Epilepsy Center, Zurich, Switzerland
Background and Aims: Patients with epilepsy often suffer from cognitive impairments, including psychomotor speed, memory, attention, and executive function. The severity of these cognitive impairments may vary over time depending on seizure burden, interictal epileptic activity, medication and neuromodulation. In particular, intermittent deep brain stimulation may affect an individual's typical cognitive processing at short and intermediate time intervals. However, the severity and time course of these putative cognitive changes at the individual level cannot be adequately assessed by traditional neuropsychological tests.
Methods: Here we present pilot data from serial neuropsychological assessments in a cohort of pharmaco‐resistant epilepsy patients in a controlled ANT‐DBS ON/OFF/ON paradigm over several days (n = 10).
Results: We observed recognizable but partly inconsistent DBS effects on cognitive test performance, mainly in verbal and non‐verbal memory domains, associated with active ANT‐DBS. These results suggest that immediate (<24 h) and intermediate (>24h) patterns of DBS‐induced cognitive effects may act independently. However, the time course of these dynamic changes is currently difficult to monitor using repeated point measures of neuropsychological test performance.
Conclusion: These partly inconsistent results favor a novel diagnostic approach: The widespread accessibility of smart devices offers new opportunities to use passively accessible biomarkers (heart rate, movement, written communication) as proxies for cognitive function in a continuous manner. We propose to use ecological "digital cognitive proxies" from smart devices that infer mental capacity from the speed, results and errors in cognitive tasks such as navigation, memory (codes, names, shortcuts), reading speed and writing errors to guide optimal personalized treatment while monitoring cognitive side effects.
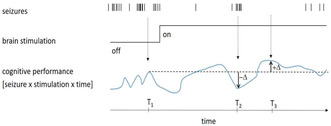
Cognitive performance in a particular domain (e.g. memory) fluctuates over time and is influenced by the interaction of seizure burden, pharmacotherapy, or neuromodulation. Point measurements over long periods of time (T1‐T3) do not reveal the true fluctu.
Disclosure: None.
EPO‐518
First seizure clinic: Experience at a tertiary hospital in Madrid
M. Arias Villaran; A. Suárez Plaza; M. Machío Castelló; E. González Villar; B. González Giraldez; J. Serratosa Fernández; L. Olivié García
Neurology, Fundación Jiménez Díaz Hospital, Madrid, Spain
Background and Aims: The diagnosis of epilepsy after a first seizure can be a challenge in clinical practice. The aim of this study was to analyze the diagnostic yield of a First Seizure Clinic (FSC) and describe the determining factors to establish a diagnosis of epilepsy.
Methods: Retrospective chart review for all patients referred to our FSC between June 2019 and December 2023. Our protocol includes a clinical evaluation within 1‐6 days by an epilepsy specialist, a 1‐hour sleep video‐EEG and a brain‐MRI.
Results: Ninety‐five patients were included, 49/95 (51.6%) were diagnosed at the first visit: 28/95 (29.5%) were diagnosed of epilepsy and 21/95 (22.1%) with non‐epileptic events. The diagnosis of epilepsy was based on the presence of previous unrecognized seizures in 11/28 patients (39.3%), on an abnormal EEG in 10/28 patients (35.7%), and on an abnormal MRI in 1/28 (3.6%). Eight patients lost follow‐up after the first visit. During follow up, another 8 patients were diagnosed with epilepsy: 5/8 based on overnight video‐EEG abnormalities and 1/8 on an abnormal MRI. Only in 2 patients the diagnosis remained unclear after follow‐up. In the non‐epileptic events group the diagnoses were convulsive syncope, anxiety, acute symptomatic seizures and TIAs.
Conclusion: In the setting of the FSC in our center, the diagnosis of epilepsy was mainly reached after a comprehensive clinical history and a 1 hour video‐EEG. When the diagnosis of epilepsy remains unclear after a first seizure, an overnight video‐EEG should be prioritized over brain MRI.
Disclosure: Nothing to disclosure.
EPO‐519
The impact of drug‐resistant epilepsy in an outpatient clinic of a tertiary hospital
M. Grávalos 1; J. Mayol1; E. Fonseca2; M. Quintana2; S. López‐Maza2; D. Campos‐Fernández2; L. Abraira2; E. Santamarina2; M. Toledo2
1Epilepsy Unit, Neurology Department, Medicine Department, Universitat Autònoma de Barcelona, Vall d’Hebron University Hospital, Barcelona, Spain; 2Research group on Status Epilepticus and Acute Seizures, Vall d’Hebron Research Institute (VHIR), Vall d’Hebron University Hospital, Vall d’Hebron Hospital Campus, Barcelona, Spain
Background and Aims: We aimed to describe the differences in medical management and complications between refractory and non‐refractory epilepsy patients.
Methods: Longitudinal prospective study including adult patients with epilepsy (PWE) evaluated at least once in an outpatient clinic of a tertiary hospital during 2023. Demographic and clinical data were collected, and emergency department consultations (ED) and antiseizure medications (ASM) were documented at each visit. Patients were categorized into non‐resistant or drug‐resistant epilepsy (DRE) according to the ILAE criteria.
Results: 2835 PWE (4935 visits; 51.1% men) were included, of which 785 (27.7%) had DRE. Drug‐resistance was more common in focal epilepsy (29.7% vs. 19.6% in generalized epilepsy; p < 0.001), in younger patients (44.1±17.8 vs. 51.1±20.7 years; p < 0.001), and in patients with an earlier onset (24.3±22.4 vs. 42.4±26 years; p < 0.001). DRE rate was significantly higher (p < 0.001) in mesial temporal sclerosis (69.9%), malformations of cortical development (54.4%), genetic (46.1%) and perinatal hypoxia (44.4%). Patients with DRE accounted for a higher rate of outpatient consultations [median per patient/year: 2 (1‐3) vs. 1 (1‐2), p < 0.001], ED consultations (25.5% vs. 16.9%; p < 0.001) and traumatic injury resulting from seizures (2.1% vs. 0.8%; p = 0.014). ASM changes were also higher in DRE patients (43.7% vs. 20.2%, p < 0.001), especially in patients with mesial temporal sclerosis (49.5% vs 28%; p < 0.001).
Conclusion: In our cohort, DRE patients exhibit a younger age, an earlier onset, and a higher prevalence of focal‐related etiologies. They generate more outpatient and ED consultations and more changes in ASM regimen. These results reflect the challenge of managing these cases in clinical practice.
Disclosure: Nothing to disclose.
EPO‐520
Towards therapeutic innovation in temporal lobe epilepsy: Focal adenosinergic modulation of hippocampal excitability
M. Vergaelen 1; J. Spanoghe1; J. Missinne2; S. Van Calenbergh3; K. Vonck1; P. Boon1; R. Raedt1
14BRAIN, Department of Head and Skin, Ghent University, Belgium; 2Center for Microsystems Technology, Imec and Ghent University, Ghent, Belgium; 3Laboratory of Medicinal Chemistry, Department of Pharmaceutics, Ghent University, Ghent, Belgium
Background and Aims: The adenosine A1 receptor (A1R) is a promising therapeutic target in epilepsy by mediating neuronal inhibition. In this study, we investigated whether A1R signaling is still functional in the intrahippocampal kainic acid (IHKA) mouse model for temporal lobe epilepsy (TLE). The feasibility of spatial selective inhibition was evaluated by illumination of specific hippocampal subregions for optical uncaging of CPA from coumarin‐caged CPA (cCPA).
Methods: In the CA1 and DG of acute hippocampal slices, the effect of adding 40 nM of the A1R agonist N6cyclopentyladenosine (CPA) on population spike (PS) amplitude to field postsynaptic potential (fPSP) slope, an index of excitability, was evaluated in epileptic IHKA versus healthy mice. Subregion selective inhibition of fPSPs was evaluated through application of 405nm light pulses (10 pulses of 100ms at 0.1Hz) spatially restricted to CA1 or DG of healthy slices incubated with 3μM cCPA.
Results: Administration of CPA resulted in a similar decrease in PS amplitude to fPSP slope ratio in epileptic versus healthy mice for the CA1 and DG (n = 19, Figure1). In a slice incubated with cCPA, the excitability decreased selectively in the illuminated hippocampal subregion (n = 1, Figure 2).
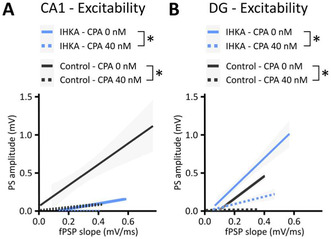
FIGURE 1 Similar decrease in CA1 and DG excitability (PS amplitude in function of fPSP slope) in epileptic IHKA versus healthy mice after administration of 40nM CPA. Data are shown as mean ± SEM. *p < 0.01.
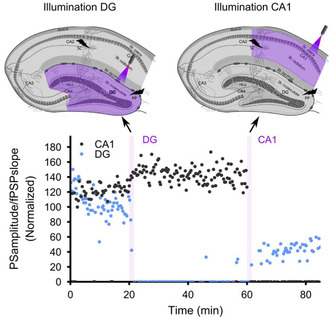
FIGURE 2 cCPA and focal illumination of DG or CA1 results in a decreased excitability (PS amplitude to fPSP slope) selectively in the illuminated region (n = 1).
Conclusion: The decrease in excitability is comparable in hippocampal slices of IHKA versus healthy mice upon exposure to CPA, indicating preserved A1R signaling in IHKA mice. The use of cCPA allows modulation of hippocampal subregions through localized illumination. These results indicate that photopharmacology has the potential to become a targeted therapy for TLE.
Disclosure: This research is funded by the Ghent University Special Research fund.
EPO‐521
Is the salivary concentration of lamotrigine and levetiracetam associated with clinical outcome and side effects?
P. Vassallo 1,2; E. Choong3; I. Aícua‐Rapún1; C. Stampfli3; P. André2; A. Rossetti1; T. Buclin3; L. Decosterd3; J. Novy1
1Department of Clinical Neurosciences, Neurology Service, University Hospital (CHUV) and Faculty of Biology and Medicine of Lausanne, Switzerland; 2Department of Clinical and Experimental Epilepsy, UCL Queen Square Institute of Neurology, London, UK; 3Service and Laboratory of Clinical Pharmacology, University Hospital (CHUV) and Faculty of Biology and Medicine, Lausanne, Switzerland
Background and Aims: The correlation between plasma and saliva concentration of anti‐seizure medication (ASM) is well established. However, clinical acceptance of saliva therapeutic drug monitoring (TDM) is constrained by significant variability and limited sensitivity. We analysed the correlation between salivary levetiracetam and lamotrigine levels, and clinical efficacy and tolerance.
Methods: We collected blood and saliva samples over two years. Seizure freedom, defined as three times the longest pre‐treatment inter‐seizure interval or one year seizure‐free without treatment changes, and adverse effects were assessed during programmed visits. Predictors of treatment response and adverse events were adjusted in a binary logistic regression model. Lamotrigine and levetiracetam median salivary and plasmatic concentrations were compared between groups categorised by treatment response and adverse effects.
Results: Among 296 adults with epilepsy, 84 (28%) achieving seizure freedom, were older, predominantly on monotherapy, and underwent fewer past ASM trials. 27 (9%), reporting adverse effects, had an older age at epilepsy onset. Seizure‐free individuals on lamotrigine had a lower medication dosage (median 2.03 vs 3.26 mg/kg, p = 0.07) and salivary concentrations (median 1.39 vs 2.4 mg/L, p = 0.11). For levetiracetam, seizure‐free individuals displayed lower plasma levels and medication dosage (median dosage 10.87 vs 19.23 mg/kg, p < 0.000), while those reporting side effects showed higher salivary concentrations (median 20 vs 14.40 mg/L, p = 0.04).
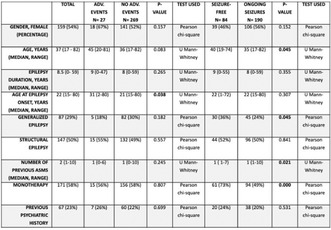
TABLE General characteristics of participants.
Conclusion: This study provides insights about clinical relevance of saliva TDM, linking salivary levels to clinical response for lamotrigine, and adverse events for levetiracetam. Further validation on a larger scale and with other ASM is essential for strengthening these findings.
Disclosure: This study (NCT0273928clinical trials.gov) was independently monitored and funded by the Swiss National Scientific Foundation (grant 320030_163430 to JN). PV received personal funding for research from Ancrage Foundation and Novartis Stiftung für medizinisch‐biologische Forschung unrelated to the current project. This external support played no role in the design, execution, or analysis of the present study.
EPO‐522
Abstract withdrawn
EPO‐523
Neuroimaging as a SUDEP predictor: what is known and what still needs to be uncovered? A systematic review
P. Quintieri; F. Dono; G. Evangelista; S. Consoli; S. De Angelis; C. Corniello; D. Liviello; S. Cipollone; F. Anzellotti; S. Sensi
Department of Neuroscience, Imaging and Clinical Science, “G. D’Annunzio” University of Chieti‐Pescara, Chieti, Italy
Background and Aims: Sudden Unexpected Death in Epilepsy (SUDEP) is the most common cause of death in patients with poorly controlled epilepsy. To date, a higher risk of developing SUDEP is mainly identified by clinical factors, among which generalized tonic‐clonic seizures and their frequency stand out. This review investigates the role of neuroimaging‐based approaches as a tool to help predicting SUDEP.
Methods: We reviewed twelve articles investigating 62 SUDEP cases assessed with a variety of neuroimaging techniques. We set to compare these 62 cases with 469 epileptic patients and 132 non‐epileptic controls (overall mean age 31.5 ± 7.7). MRI, fMRI, PET and SPECT were carried out in all these groups.
Results: SUDEP and non‐SUDEP cases differ anatomically and functionally. MRI data indicate differences in gray matter volumes in the hippocampal and cerebellar cortex. In addition, functional imaging revealed discrepancies in terms of network modulation within the brainstem, whose metabolism and perfusion deviate from physiological values assessed by PET and SPECT scans.
Conclusion: Correlations between the occurrence of SUDEP and neuroimaging alterations are emerging, but their predictive significance must be the object of further intensive investigation.
Disclosure: Nothing to disclose.
EPO‐524
Identification of risk factors for drug resistant epilepsy
R. Coa 1; R. Lecca2; F. Arippa3; D. Fonti4; L. Polizzi1; A. Muroni1; M. Melis1; M. Figorilli1; M. Puligheddu5
1Epilepsy Centre, AOU Cagliari, Cagliari; 2S.C Neurorehabilitation Po SS Trinità ASL Cagliari, Cagliari; 3Department of Mechanical, Chemical engineering, University of Cagliari; 4U.O. Neurology, P.O. Sirai, ASL Sulcis, Carbonia; 5Department of Medical Sciences and Public Health, University of Cagliari
Background and Aims: Drug‐resistant epilepsy (DRE) represents a significant challenge for epileptologists, affecting approximately 30% of their patients. Early identification of people at risk for DRE is crucial for optimizing both pharmacological and non‐pharmacological management strategies. Our study aims to pinpoint the risk factors associated with DRE within the patient population at the Epilepsy Centre of the University of Cagliari.
Methods: Data were retrieved from the medical records of people treated at our Epilepsy Centre. To identify predictive risk factors for DRE, we employed a combination of univariate analysis and logistic regression to assess the collective impact of various factors. We investigated different conditions linked to DRE, including gender, age of onset, etiology (structural, genetic), history of status epilepticus, type of seizures (focal, generalized, combined), learning disabilities, comorbidities, illness duration, and family history of epilepsy.
Results: Out of a total of 804 subjects, 201 were identified as having DRE (26%). Univariate analysis revealed a significant association between DRE and age of onset, structural etiology, presence of status epilepticus, type of seizure, presence of psychiatric and neurological comorbidities, learning disability, and family history of epilepsy. Subsequent multiple regression analysis identified several factors significantly associated with DRE, including age of onset, structural etiology, psychiatric and neurological comorbidities, and learning disability.
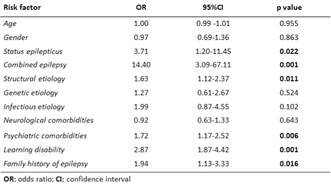
Statistical analysis of risk factors.
Conclusion: The presence of a structural etiology, psychiatric and neurological comorbidities, learning disability, and early age of onset were identified as significant risk factors for DRE. Early identification of these factors holds promise for improving the management of affected people and refining clinical strategies.
Disclosure: Nothing to disclose.
EPO‐525
Late seizure relapse after anterior temporal lobectomy: The prevalence and its prognostic factors
S. Lee 1; T. Kim1; B. Kim1; J. Kang1; Y. Koo1; J. Lee2; S. Hong2
1Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea; 2Department of Neurosurgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
Background and Aims: We investigated the proportion of late seizure relapse (LSR) and its prognostic factors after epilepsy surgery in patients with drug‐resistant temporal lobe epilepsy (TLE).
Methods: This retrospective study recruited 178 adults who underwent anterior temporal lobectomy (ATL). We excluded if they had seizure recurrence in the first two years after surgery and if they had less than 3 years of follow‐up. Finally, 99 patients were included. Seizure freedom was defined as ILAE outcome class 1 and 2. LSR was defined as seizure relapse after initial 2‐year seizure freedom. The Cox regression analysis was performed. Age, sex, and the potential variables exhibiting a p‐value of < 0.2 in the univariate analysis were entered in the initial model.
Results: The follow‐up period after surgery ranged 36 to 191 months. Hippocampal sclerosis was the most common pathology (71.7%). The rate of LSR was 29.3% and its timing was mean 44.0±16.2 months after surgery. Univariate analyses showed that the presence of seizure risk factor, extratemporal interictal epileptiform discharges (IEDs) during video‐EEG monitoring, ATL without hippocampectomy, weekly seizure recurrence before surgery, and vascular etiology had a p‐value of < 0.2 in association with LSR. The Cox regression showed that LSR was independently predicted by the presence of extratemporal IEDs (odds ratio 4.597, p = 0.002) and ATL without hippocampectomy (odds ratio 2.679, p = 0.027).
Conclusion: About one third of TLE patients with initial 2‐year seizure freedom after ATL may have LSR. TLE patients with extratemporal IEDs or ATL without hippocampectomy may be at high risk for LSR.
Disclosure: Nothing.
EPO‐526
Cognitive symptoms in autoimmune limbic encephalitis: Long term follow up
S. Corsi; G. Tognoni; F. Iannaccone; F. Baldacci; L. Tommasini; L. Giampietri; S. Gabriele; C. Pizzanelli
Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
Background and Aims: Cognitive impairment is one of the cardinal symptoms of autoimmune limbic encephalitis. This study aims to describe long‐term cognitive profile in a group of 9 patients diagnosed with autoimmune limbic encephalitis.
Methods: Clinical data and detailed neuropsychological assessment were collected from 9 patients one year after the acute phase of encephalitis. The average age of the patients was 62 years. Seven patients were males. Neuropsychological battery explored verbal and visuo‐spatial memory, language, attentive and executive functions. Cerebrospinal fluid analysis (CSF), brain magnetic resonance imaging, brain 18‐fluorodeoxyglucose positron emission tomographic imaging were performed. In 89% of CSF analysis autoantibodies were found (LG1 50%; CASPR2 38%; Glu3 peptide A e B 12%).
Results: All the patients showed severe cognitive deficits in the acute phase. In the long‐term follow up only 2 patients showed a full neuropsychological recovery. 56% of the 9 subjects had verbal memory deficits, while visual memory impairment was observed in 33% of patients. Attention was affected in 44% of patients, while executive functions were impacted in 22% of cases, respectively. No language domain impairment was observed in any patients. Only 33% of patients have resumed their previous work activity
Conclusion: Verbal memory emerged as the most frequently impaired cognitive domain in long‐term follow up of autoimmune limbic encephalitis. However, other cognitive domains were also affected. Despite being considered a form of encephalitis with a benign prognosis, in our case series, patients exhibited long‐term cognitive deficits with an impact on social and occupational functioning.
Disclosure: Nothing to disclose.
EPO‐527
Effectiveness and tolerability of cenobamate as add‐on therapy: A historical monocentric comparative study
T. Intravooth; D. Georgiou; A. Barbu; A. Staack; B. Steinhoff
Kork Epilepsy Center, Kehl‐Kork, Germany
Background and Aims: Cenobamate is a novel antiseizure medication approved in Europe for adjunctive therapy in adults with drug‐resistant focal seizures. However, there are limited data from clinical practice. In this study, our new data on cenobamate were compared with our historical data on lacosamide, perampanel, and brivaracetam.
Methods: Data were collected from our three studies conducted between 2016 and 2023. The retention rate, 50% response rate, and seizure freedom rate at 6 months, as well as the frequency of adverse events, were evaluated. Cenobamate was compared with the three antiseizure medications. Using Bonferroni correction, a result was considered statistically significant at a p‐value < 0.017.
Results: A total of 391 patients were included. In terms of retention rate, cenobamate was superior to other antiseizure medications (p < 0.001). There was no significant difference in the 50% response rates and seizure freedom rates between patients treated with cenobamate, lacosamide, brivaracetam, and perampanel. The frequency of adverse events was higher with perampanel than with cenobamate (p < 0.001).
Conclusion: The results of this study show that cenobamate was a superior option for adjunctive therapy in refractory epilepsies in terms of retention rate in our patients. Significantly more adverse events occurred with perampanel. The higher retention rate under cenobamate therapy compared to other antiseizure medications can most likely be explained by the high efficacy of cenobamate with a more favorable side effect profile. Due to a possible bias of the results, further prospective randomized controlled trials are needed to confirm these results.
Disclosure: Bernhard J Steinhoff has served as a paid consultant for Angelini Pharma, B. Braun Melsungen, Eisai, GW Pharmaceuticals, and UCB. Other authors have nothing to disclose.
EPO‐528
Attributional bias – Misinterpretation of social behaviour in people with epilepsy
V. Ogurcakova 1; J. Zalud2; P. Marusic1; J. Amlerova1
1Department of Neurology, Second Faculty of Medicine, ERN EpiCARE, Charles University and Motol University Hospital, Prague, Czechia; 2Department of Clinical Psychology, University Motol Hospital, Prague, Czechia
Background and Aims: Attributional bias is characterised by an impaired ability to predict behaviour of our environment based on social cues. As a consequence, we judge intentions of others as hostile and harmful rather than the result of chance or external factors. People with epilepsy (PWE) find it challenging to engage in social activities or maintain stable employment. Misinterpreting social situations can contribute to their social maladaptation and lower quality of life.
Methods: We examined 53 PWE, 26 with idiopathic generalised epilepsy (IGE), 27 with temporal lobe epilepsy (TLE) from Motol Epilepsy Centre in Prague, and 43 healthy controls (HC). We used the Ambiguous Intentions Hostility Questionnaire (AIHQ) to assess attributional bias (social misinterpretation). It yields 3 scores ‐ aggression bias (AB), hostility bias (HB) and blame score (BS) in different types of situations in terms of intentionality ‐ accidental, ambiguous and intentional. The higher the score in AIHQ, the more impaired the social judgement. We measured depression by Neurological Disorders Depression Inventory in Epilepsy (NDDI‐E).
Results: PWE scored higher than HC in AB in ambiguous situations. Both IGE and TLE groups demonstrated HB in ambiguous situations, but TLE group also in accidental situations and IGE group in intentional situations. Duration of the disease or antiseizure medication did not correlate with scores in AIHQ. NDDI‐E scores correlated with HB in TLE group.
Conclusion: Attributional bias is an unexplored area of social cognition in PWE. This study suggests an impairment of social judgement which may contribute to social dysfunction and affect quality of life in PWE.
Disclosure: Supported by Ministry of Health, Czechia ‐ conceptual development of research organization, Motol University Hospital, Prague, Czechia 00064203.
Headache 3
EPO‐529
Efficacy of mindfulness added to treatment as usual in patients with chronic migraine and medication overuse headache
L. Grazzi 1; D. Montisano1; E. Guastafierro2; D. D'Amico1; B. Del Corso3; A. Raggi2
1Headache Center, Neuroalgology Dapartment – Neurological Institute Carlo Besta IRCCS Foundation, Milan, Italy; 2Neurology, Public Health and Disability Unit – Neurological Institute Carlo Besta IRCCS Foundation, Milan, Italy; 3Neuroscience Institute – National Research Council, Padova, Italy;
Background and Aims: To assess the efficacy of a six‐session mindfulness‐based treatment added to treatment as usual (TaU) on headache frequency and medication intake.
Methods: This is a phase‐III single blind RCT single‐center study. Patients were enrolled between November 2018 and December 2021, and followed‐up for 12 months. 177 patients with Chronic Migraine and Medication Overuse Headache (CM and MOH) were randomized 1:1 to either TaU or mindfulness added to TaU (TaU+MIND). Exclusion criteria were: psychiatric comorbidities; pregnancy; secondary headaches; withdrawal from MOH at least twice in the previous two years; previous experience with mindfulness. TaU consisted of withdrawal from overused drugs, patients’ education, and prescription of prophylaxis. Patients attending mindfulness sessions were taught on tackling the pain‐pill automatism, and were encouraged to engage in a 7‐10 minute/day self‐practice. The primary endpoint was the achievement, at 12 months of ≥50% headache frequency reduction compared to baseline. Secondary endpoints included medication intake.
Results: Out or the 177 participants (median age 47.9 years [Q1‐Q3: 40.1‐54.2]; 19 [11.3%] males; median CM duration 14.6 years [Q1‐Q3: 4.9‐22.2]) 89 were randomized to TaU and 88 to TaU+MIND. Patients in the TaU+MIND group outperformed those in TaU for the primary endpoint, achievement of ≥50% headache frequency reduction (78.4% vs 48.3%; p < 0.0001). They also showed superiority in some secondary endpoints, namely headache frequency and medication intake.
Conclusion: : These findings show that a six‐week mindfulness‐based treatment as add on to TaU is superior to TaU for the treatment of patient with CM and MOH
Disclosure: Nothing to disclose.
EPO‐530
Cerebral compliance in pseudotumor cerebri and transversus sinus stenosis undergoing venoplasty or CSF puncture
L. Souza Viana 1; F. Moulin de Moraes2; S. De Andrade Matas2; G. Sampaio Silva2
1Department of Neurology, Hospital Israelita Albert Einstein, Sao Paulo, Brazil; 2Department of Neurology, Hospital Sao Paulo/Federal University of Sao Paulo, Sao Paulo, Brazil
Background and Aims: Pseudotumor cerebri (PTC) has a high prevalence among women, and 30% to 93% of patients have transverse sinus stenosis (TSS). In addition, venoplasty improves symptoms in up to 87% of patients. Intracranial complacency (IC) can be a surrogate marker for intracranial hypertension. The FDA approved a non‐invasive Brazilian method for monitoring intracranial pressure waves, Brain4care (B4C), in 2021. We aimed to compare the IC in patients with PTC and TSS only with lumbar punctures (LP) versus venoplasty.
Methods: This is an observational and single‐centered study from 2020 to 2022. Inclusion criteria: ≥18 years with PTC; with presence of TSS. Data were reported as mean (± SD) or median (± IQR). Categorical variables were reported as percentage and compared using the Χ2 test or Fisher's test. p‐Values were considered significant when <0.05, using SPSS.
Results: We enrolled 158 patients, among whom nine were excluded due to age: 12 without PTC, 13 without stenosis, 22 with CVT and 35 with missing data. We analyzed 67 patients: In the LP group (50), we found 100% female, mean age 37.6 (SD: 11.6), B4C mean TTP 0.24 (SD: 0.07) in lay‐position and 0.23 (SD: 0.06) in sit‐position. In the venoplasty group (17), we noticed 88.2% females, with a mean age of 45.6. (SD: 12.6), B4C mean TTP 0.24 (SD: 0.07), and 0.23 (SD: 0.06) in positions. There were no differences in IC between the two groups.
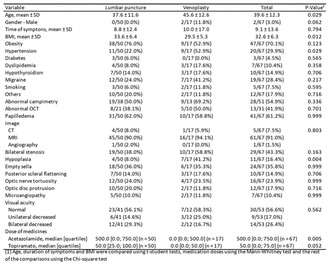
Baseline characteristics
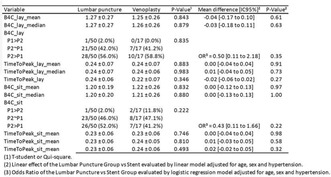
Primary outcomes
Conclusion: We demonstrated no significant difference in IC between patients with PTC associated with TSS submitted only to LP vs venoplasty.
Disclosure: Nothing to disclose.
EPO‐531
Underdiagnosis and impact of menstrual migraine in real‐world clinical practice
G. Terwindt1; J. Ailani2; B. Galabova3; J. Cirillo4; A. Jenkins3; L. Abraham3; J. Brown4; K. Hygge Blakeman 4; J. Jackson5; W. Whitton5; L. Hancock5
1Department of Neurology, Leiden University Medical Center, Leiden, The Netherlands; 2MedStar Georgetown University Hospital, Washington DC USA; 3Pfizer, Ltd., Tadworth, Surrey; 4Pfizer, Inc., New York, NY USA; 5Adelphi Real World, Bollington, UK
Background and Aims: Patients with menstrual migraine (MM) experience more severe, disabling and prolonged attacks than non‐MM patients. Research indicates that approximately 2/3 of female migraine sufferers may experience MM and diagnoses are often unreliable without a validated monitoring tool. This cross‐sectional study aimed to assess how often MM is reported in clinical practice.
Methods: Data were drawn from the 2022/23 Adelphi Migraine Disease Specific Programme™, a real‐world cross‐sectional survey across France, Germany, Italy, Spain, the UK, and the USA. The cross‐sectional study involved retrospective data collection from physicians and their female patients providing data on migraine diagnosis, including MM, and attack severity. Analyses were descriptive.
Results: There were 264 primary care practitioners (PCPs) and 340 neurologists who provided data on 3,049 female patients aged ≤55 years, with 32% (n = 986) diagnosed with MM. Physicians estimated that 38% of their patients had diagnosis of MM, with an additional 20% of patients without a physician‐confirmed MM diagnosis who reported menstruation as a trigger for their migraines. Patients with MM experienced more severe migraine attacks than those without MM. Physicians tended to underestimate the severity, particularly for MM patients compared to those without MM. The reporting disparity in attack severity was more pronounced in MM patients when managed by a PCP. (Table 1). Treatment prescribed to both patient groups were similar, but MM patients reported less satisfaction with their preventive treatment, than those without MM.
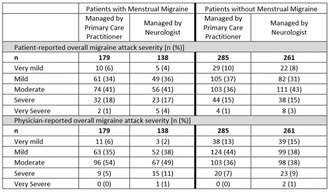
TABLE 1 Patient and physician reported overall migraine attack severity. Note‐ data reported on patient/physician pairs, where patients had fully completed the patient‐reported questionnaire and full physician‐reported data were concurrently available.
Conclusion: Optimal treatment for MM requires heightened physician awareness, recognition, and understanding of its implications, aiming to alleviate additional burdens for affected females.
Disclosure: G.M.T reports consultancy or industry support from Abbvie, Lilly, Lundbeck, Novartis, Pfizer, Teva, and Interactive Studios BV, and independent support from the European Community, Dutch Heart and Brain Foundations, Dutch Research Council, Dioraphte, and the Clayco Foundation. JA reports consulting honoraria from Abbvie, Amgen, Aeon (2022), Axsome, Biohaven, BioDeliveryScientificInternational (2022), Eli‐Lilly, GlaxoSmithKline, Lundbeck, Linpharma, Impel, Ipsen, Merz, Miravio, Pfizer, Neurolief, Neso, Gore, Satsuma, Theranica, and Teva; clinical trials support (grant to institution) from Abbvie, Satsuma (2022), Zosano (2021), Parema, and Ipsen; Editorial Boards/Steering Committee for Medscape, SELF magazine (medical editor) JC, AJ, LA, JB and KHB are employed by and hold stock/options in Pfizer BG is employed by Pfizer. JJ, WW, LH‐ Nothing to disclose.
EPO‐532
A machine‐learning‐based algorithm to predict response to anti‐CGRP monoclonal antibodies in patients with migraine
M. Romozzi 1; A. Lokhandwala2; C. Vollono1; G. Vigani3; A. Burgalassi3; D. García‐Azorín4; P. Calabresi1; P. Geppetti3; L. Iannone3
1Dipartimento Universitario di Neuroscienze, Università Cattolica del Sacro Cuore, Rome, Italy; 2YPrime, Philadelphia, PA, USA; 3Section of Clinical Pharmacology and Oncology, Department of Health Sciences, University of Florence, Florence, Italy; 4Hospital Clinico Universitario de Valladolid, Headache Unit, Department of Neurology, Valladolid, Spain
Background and Aims: The study aimed to determine whether machine‐learning (ML)‐based models can predict responses to monoclonal antibodies (mAbs) against the calcitonin gene‐related peptide (CGRP) in patients with migraine using early predictors and to create a prediction tool.
Methods: We collected data from patients receiving anti‐CGRP mAbs for 12 months. Demographic and monthly clinical variables were collected, including monthly headache days (MHD), monthly days with acute medication use (AMD), number of analgesics, Headache Impact Test‐6 (HIT‐6). Response rates were categorized as <25%, 25‐50%, 50‐75%, and >75% reduction in MHD. ML models were trained using random forest algorithm. ML models were optimized to maximize the F1 score, and their performance was evaluated using standard evaluation metrics, including accuracy, precision, and area under the receiver operating characteristic curve (AUC‐ROC). Sequential backward feature selection was employed to identify the most relevant predictors. Each model was given 11 baseline data inputs (type of mAb, age, gender, migraine diagnosis, disease duration, aura, MHD, AMD, HIT‐6, number of analgesics) and month‐based predictors for months 1, 3, 6.
Results: We included 336 patients treated with anti‐CGRP mAbs. We developed 6 models to predict 3‐,6‐,and 12‐month responses using early predictors. ML‐based models yielded predictions with F1 score of 0.42‐0.71 and AUC‐ROC score of 0.44‐0.72. Shapley Additive explanations summary plots were generated to interpret the contribution of each feature for each model. Based on these findings, a response prediction tool was developed.
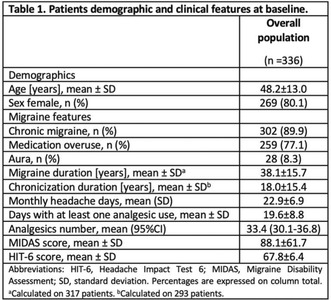
Patients’ demographic and clinical features at baseline.
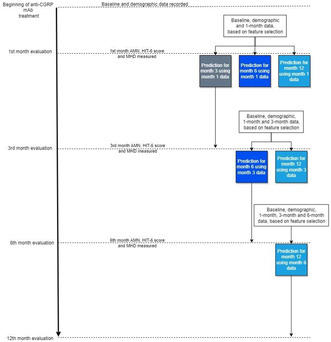
Flow chart of the anti‐calcitonin gene‐related peptide (CGRP) monoclonal antibodies calculator tool at 3, 6 and 12 months. AMNs, absolute number of analgesics; Headache Impact Test‐6 (HIT‐6); MHDs, monthly headache days.
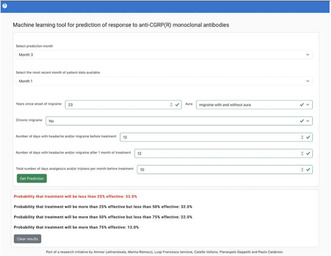
Demo of the Machine‐learning (ML)‐based tool to predict anti‐calcitonin gene‐related peptide (CGRP) monoclonal antibodies response at 3, 6 and 12 months.
Conclusion: The ML‐based response prediction tool holds promise in predicting treatment outcomes for patients with migraine undergoing anti‐CGRP mAbs treatment, potentially aiding in clinical decision‐making and cost‐optimization.
Disclosure: Nothing to disclose.
EPO‐533
Functional neurological symptoms in headache disorders: A case‐series retrospective study
M. Gonçalves; I. Pinto; G. Cabral
Neurology Department, Hospital de Egas Moniz, ULS Lisboa Ocidental, Lisbon, Portugal
Background and Aims: To evaluate functional neurological symptoms (FNS) within a population diagnosed with headache disorders and to investigate the influence of preventive headache treatments on FNS.
Methods: We conducted a retrospective study involving patients diagnosed with headache disorders according to the ICHD‐3, presenting with FNS at an outpatient clinic from 2020 to 2022.
Results: We identified 23 patients (82.6% female, mean age 40 years) diagnosed with headache disorders, with episodic or chronic migraine being the most prevalent (n = 17, 73.9%), all without aura who presented with FNS. Most patients (60.9%) presented with multiple FNS (sensorimotor, visual, or related to speech); these were followed by sensory symptoms (30.4%), impaired gait, and non‐epileptic seizures (4.3% each). FNS were mostly paroxysmal (65.2%) and occurred between and during headache crises, with a notable exacerbation of FNS during heightened headache episodes (65.2%). Neurological examinations revealed at least one positive sign of functionality in 69.6% of cases. Preventive treatment for headaches was started in 20 patients, predominantly antidepressant drugs (47.8%). Eight patients (34.8%) failed at least one preventive. During the follow‐up period, 50% reported an improvement in headache frequency (≥50%) and 75% patients had an improvement of their FNS. Patients with better control of headache frequency had higher rates of improvement of FNS (70% versus 30%).
Conclusion: In our study, the predominant presentation of FNS was characterized by its multiplicity, often displaying a paroxysmal nature and exacerbations during concurrent headache crises. The effectiveness of preventive treatment, aimed at reducing headaches, translated into improvement in FNS.
Disclosure: None.
EPO‐534
Efficacy of anti‐CGRP mAbs in migraine: A comparative analysis between overweight and normal‐weight populations
G. Cretella; R. De Simone; S. Braca; A. Miele; A. Stornaiuolo; C. Giannini; C. Russo
Neurology Department, University of Naples Federico II, Naples, Italy
Background and Aims: Migraine and excess weight share a relationship not yet fully understood. Moreover, the Body Mass Index (BMI) has been positively correlated with the frequency of migraine attacks. Anti‐CGRP monoclonal antibodies (mABs) hold a pivotal role in targeting peripheral mediators in migraine treatments. Consequently, this study endeavors to assess the efficacy of mABs in a population characterized by excess weight compared to a normal weight control group
Methods: We enrolled 120 chronic migraine patients treated with anti‐CGRP mAbs divided into two groups according to BMI (BMI > 25 and <25). Over a time period of 12 months, we recorded mean monthly headache, BMI, midas, headache intensity and acute medication intake every three months
Results: A monthly migraine frequency of 22+‐7 days was found in the control group and 20+‐7 days in the group of overweight patients before starting treatment. At month 12, an average of 9.5+‐8.6 and 8.8+‐7.0 days were found, respectively. Preliminary analysis of the data reveals a decrease in the monthly frequency of migraine in both the overweight patient group and the control group (p < 0.001). When comparing the difference in the decrease, it does not appear statistically significant (p = 0.6). Further analyses are still in progress
Conclusion: The current analysis reveals that antibody treatment retains efficacy in the overweight population in the same way as in the normal‐weight group. There are limited data in literature on the use of CGRP inhibitor monoclonal antibodies in individuals who are overweight/obese and further studies are needed to better understand efficacy in this patient population
Disclosure: Nothing to disclose.
EPO‐535
The stigma of cluster headache and its comparison with migraine
J. Membrilla 1; S. Quintas2; E. Caronna3; A. Alpuente3; A. Muñoz‐Vendrell4; S. Campoy4; C. Morales5; L. Sevillano Orte6; M. Castro Sánchez7; A. Layos8; A. Andrés López8; A. Sánchez Soblechero9; A. Lozano Ros9; J. Garcia Ull10; S. Pérez Pereda11; A. González Martínez2; M. Cordova Infantes12; M. Fernández Recio12; C. Nieves Castellanos13; M. Álvarez Álvarez14; C. Moreno Rodrígez3; A. López Bravo6
1Neurology, Hospital Universitari Francesc de Borja, Gandia, Spain; 2Neurology, Hospital Universitario La Princesa, Madrid, Spain; 3Neurology, Hospital Universitari Vall d'Hebron, Barcelona, Spain; 4Neurology, Hospital Universitari de Bellvitge‐Viladecans, L'Hospitalet de Llobgregat, Spain; 5Neurology, Hospital Universitario de Canarias, La Laguna, Spain; 6Neurology, Hospital Reina Sofía, Tudela; 7Neurology, Hospital Regional Universitario, Málaga, Spain; 8Neurology, Hospital General Universitario, Albacete, Spain; 9Neurology, Hospital General Universitario Gregorio Marañón, Madrid, Spain; 10Neurology, Hospital Clínico Universitario, València; 11Neurology, Hospital Universitario Marqués de Valdecilla, Santander, Spain; 12Neurology, Hospital Universitario Virgen de Valme, Sevilla, Spain; 13Neurology, Hospital Universitario y Politécnico La Fe, València, Spain; 14Hospital Universitario de Cabueñes, Gijón, Spain
Background and Aims: Stigma refers to the situation in which an individual is disqualified from full social acceptance, manifesting itself in the form of stereotypes, prejudice and discrimination. There are validated measures to measure the stigma associated with neurological diseases, but cluster headache (CH) has not been investigated so far. Our aim is to study the stigma of CH and compare it with that of migraine.
Methods: This is a multicenter cross‐sectional study conducted by junior members of the Spanish Headache Study Group. Migraine and CH patients were recruited. Stigma was assessed with the SSCI (Stigma Scale for Chronic Illness). Other psychosocial aspects (cognitive reserve, self‐esteem, anxiety, depression, stress and catastrophizing) were evaluated by specific scores. Migraine cases were classified into refractory/refractory migraine (RRM) or non‐refractory/refractory migraine (non‐RRM) according to the EHF criteria. CR patients were classified into episodic (ECH) or chronic (CCH).
Results: Ninety‐six patients were enrolled: 37 ECH, 19 CCH, 17 non‐RRM and 23 RRM. SSCI score was higher in CCH and RRM, 56.0 (34.0‐77.0) and 59.0 (39.0‐71.0) respectively; in ECH it was scored 42.0 (30.5‐64.0) and in non‐RRM, 37.0 (30.0‐52.5). The difference between non‐RRM and CCH (p = 0.038), between non‐RRM and RRM (p = 0.006) and between ECH and RRM (p = 0.019) was statistically significant. CCH and RRM also showed higher scores in the depression assessment with respect to non‐RRM. No statistically significant differences were found in the rest of the assessments.
Conclusion: Chronic cluster headache patients, like resistant or refractory migraine patients, show a higher degree of stigma relative to non‐resistant and non‐refractory migraine.
Disclosure: Nothing to disclose.
EPO‐536
Impact of migraine preventive treatment on interictal burden
M. Lorenzo Diéguez; A. Sánchez Huertas; M. Aledo Serrano; J. Díaz de Terán
Department of Neurology, La Paz University Hospital
Background and Aims: To analyze the impact of migraine preventive treatment on interictal burden (IB) and interictal predictors of response to preventive treatment.
Methods: Prospective cohort study in a headache unit. Patients with migraine who started treatment between January‐February 2023 and followed up for 3 months were included. Epidemiological and clinical variables such as monthly migraine days (MMD), monthly consumption of NSAIDs and triptans, and IB (determined by the Migraine Interictal Burden Scale‐4 and an ad‐hoc questionnaire, including interictal symptoms) were collected at the beginning of treatment and at 3 months.
Results: 100 patients; 90 women (90%) (age mean 48.5 ± 10.9 years) 11% low‐frequency episodic migraine; 20% high‐frequency; 69% chronic. Of these last two groups, 54% started treatment with monoclonal anti‐CGRP (Mab), 31% with botulinum toxin type A (OnabotA) and 8% with oral preventives. At similar reduction of MMD (61% vs. 58%), a greater decrease of IB (57% vs. 41%), consumption of NSAIDs (68% vs. 50%) and triptans (64% vs. 41%) with higher improvement index in response to symptomatic treatment (68.5% vs 46%) was observed in those patients treated with anti‐CGRP compared to OnabotA.
Conclusion: In addition to reducing MMD, preventive treatment significantly reduces IB, being this reduction greater in patients treated with MaB. We also identified IA as a possible predictive factor of non‐response to preventive treatment.
Disclosure: Nothing to disclose.
EPO‐537
Role of dexamethasone as a possible protective factor against long‐COVID headache
O. Duraníková 1; S. Horváthová1; P. Sabaka2; M. Minár1; I. Straka1; P. Valkovič1
12nd Department of Neurology, Comenius University, Faculty of Medicine and University Hospital in Bratislava, Slovakia; 2Department of Infectology and Geographical Medicine, Comenius University, Faculty of Medicine and University Hospital in Bratislava, Slovakia
Background and Aims: Although respiratory symptoms prevail in COVID‐19 infection, headache is one of the most common symptoms that may persist for months in the form of long‐COVID headache. The aim of our study was to evaluate long‐COVID headache characteristics and search for possible biomarkers.
Methods: We conducted retrospective analysis of 295 (126 women) hospitalized patients with COVID‐19 infection in Slovakia after 12‐15 months. Retrospectively we contacted patients via video call with self‐administered questionnaire. In headache patients we searched for participants with persisting headache up to 15 months. Subsequently we evaluated persisting headache's phenotype and its possible biomarkers.
Results: 34.6% (n = 102) of patients had COVID‐19 associated headache, with 41.2% (n = 42) reporting persisting headache. It was unilateral in 40%, pulsating in 38% and accompanied by nausea and phonophobia in 60% and 74% respectively. While no specific laboratory marker was associated with persisting headache, we found a significant association between persisting headache and treatment with dexamethasone. Patients treated with dexamethasone during hospitalization had lower chance of developing persisting headache (52% vs. 73% p = 0.029).
Conclusion: We confirmed persisting headache for 12‐15 months in almost half of our patients with predominance of migraine‐like characteristics. Patients with administered dexamethasone had a statistically lower probability of developing long‐COVID headache. This has relevant implications into clinical practice, as long‐COVID headache remains a therapeutic challenge worldwide with specific recommendations and a tailored approach needed.
Disclosure: Nothing to disclose.
EPO‐538
Anti‐CGRP monoclonal antibodies effectiveness among men and women: Are there differences?
P. Gallego Fuentes; L. Rodríguez Jiménez; M. Castro Sánchez; L. García Trujillo
Neurology, Hospital Regional Universitario, Málaga, Spain
Background and Aims: Migraine affects more women and there is evidence that supports the influence of female sex hormones on its pathophysiology. CGRP is the main neuropeptide that causes pain during migraine attacks and its blood levels can be modified by those hormones.
Methods: We reviewed 225 patients that started anti‐CGRP monoclonal antibodies (mAbs) between 2019 and 2022, in order to ensure a long follow‐up. 14 were excluded for lost to follow‐up. Our objective is to assess if there are differences in the response to this treatment in males versus women.
Results: There were 189 women and 31 men with an average age of 45 years old. 77% of men and 79% of women had chronic migraine with an average of 5 preventive medications failed. The average reduction of monthly migraine days was 4 for women and 6 for men, while the average reduction of monthly headache days was 7 for women and 11 for men. 58% of men and 66 % of women achieved a reduction of 50% of monthly headache or migraine days. Constipation was the main adverse effect for women (17%), but no men had it. There were not statistically significant differences between groups except from the response to an antibody switch that was higher in men (50% vs 22%)
Conclusion: In our series, response to anti‐CGRP mAbs was similar in women and men, what suggests a significant role of CGRP in migraine pathophysiology in both sexes. Gastrointestinal adverse effects were not reported by men, so this should be assessed in future studies.
Disclosure: Nothing to disclose.
EPO‐539
Sleep quality assessment in resistant migraine
R. Cagigal; S. Casanova; A. Rocha; M. Branco
Neurology Department, Unidade de Saúde Local Gaia/Espinho
Background and Aims: Resistant migraine is defined by having failed at least 3 classes of migraine preventatives and suffer from at least 8 debilitating headache days per month for at least 3 consecutive months without improvement. Sleep disorders are known contributors for resistant migraine. Pittsburgh Sleep Quality Index (PSQI) is a validated self‐report questionnaire that assesses sleep quality. If higher than 5, it is considered pathological. We report a series of patients with resistant migraine in whom sleep quality was assessed.
Methods: We included patients suffering from migraine followed in Neurology appointments that fulfilled the European Headache Federation criteria for resistant migraine and were waiting to start anti‐CGRP (calcitonin gene‐related peptide) monoclonal antibody treatment and. PSQI was assessed.
Results: We included 34 patients, 91.2% female, mean age of 44.7 years. 61.8% had chronic migraine, 85.3% without aura. Only 29.4% were formally diagnosed with sleep pathology (26.5% insomnia, 2.9% obstructive sleep apnea) and 26.5% were medicated (17.6% trazodone, 11.8% benzodiazepine). Patients were medicated with a mean of 1.15 migraine preventatives, haven previously tried a mean of 3.32 preventatives. The mean number of monthly debilitating headache days was 12.03. 82.4% of patients had a pathological PSQI, with a mean score of 10.56. The most impaired component score was subjective sleep quality.
Conclusion: Our series’ results suggest that sleep disorders could be underassessed in Neurology appointments and, therefore undertreated. Strengthening PSQI assessment in migraine patients could be of value in preventing resistant migraine, allowing therapeutic optimization.
Disclosure: Nothing to disclosure.
EPO‐540
Effectiveness and tolerability of lasmiditan as acute migraine treatment (DART): A real‐world multicentric Italian study
R. De Icco 1; G. Vaghi1; L. Iannone2; M. Corrado1; A. Burgalassi2; E. De Matteis3; F. De Santis3; C. Fasano2; E. Piella4; M. Romozzi5; G. Sebastianelli6; G. Avino7; S. Cevoli8; G. Coppola6; G. Dalla Volta9; A. Granato10; F. Boscain11; R. Ornello3; F. Pistoia3; I. Rainero12; M. Trimboli13; A. Russo14; M. Valente15; C. Vollono16; C. Tassorelli1
1Department of Brain and Behavioral Sciences, University of Pavia, Pavia, Italy; Headache Science & Neurorehabilitation Center, IRCCS Mondino Foundation, Pavia, Italy; 2Headache Centre and Clinical Pharmacology Unit, Careggi University Hospital Florence, Florence, Italy; 3Department of Biotechnological and Applied Clinical Sciences, University of L'Aquila, Italy; 4Department of Neurosciences “Rita Levi Montalcini”, University of Torino, Torino, Italy; 5UOC Neurologia, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy; 6Sapienza University of Rome Polo Pontino ICOT, Department of Medico‐Surgical Sciences and Biotechnologies, Latina, Italy; 7Ospedale di Prato Santo Stefano, Prato, Italy; 8IRCCS Istituto delle Scienze Neurologiche Bologna, Bologna, Italy; 9Headache Centre of Istituto clinico città di Brescia (gruppo SAN DONATO), Brescia, Italy; 10Azienda Ospedaliero‐Universitaria di Trieste, Trieste, Italy; 11Headache Centre, Neurology – Euganea Health Unit, Padua, Italy; 12Headache Center, Department of Neuroscience, University of Torino, Torino, Italy; 13Centro Interaziendale Cefalee, Azienda Ospedaliero‐Universitaria Renato Dulbecco, Catanzaro, Italy; 14Department of Advanced Medical and Surgical Sciences, University of Campania “Luigi Vanvitelli”, Naples, Italy; 15Azienda Sanitaria Universitaria Friuli Centrale, Presidio Ospedaliero Santa Maria della Misericordia, Udine, Italy; 16Department of Neurosciences, Università Cattolica del Sacro Cuore, Rome, Italy
Background and Aims: Lasmiditan, a serotonin 5‐HT1F receptor agonist, has been recently approved in Italy for the acute migraine treatment. We designed a prospective multicentric study to evaluate lasmiditan effectiveness and tolerability in the real‐world setting (NCT05903040).
Methods: We enrolled 55 patients (87.3% females, 45.4 + 14.4 years, 21.8% – n = 12 with chronic migraine‐CM, baseline monthly migraine days 9.1 + 7.2) from 13 Italian headache centers. Patients were instructed to treat up to four migraine attacks with lasmiditan 50 mg (20.4%) or 100 mg (79.6%). Using an ad hoc diary, we prospectively collected migraine‐attack features every 30 minutes after lasmiditan administration, up to 2 hours (2 h).
Results: Preliminary analyses were conducted on 28 first‐treated attacks (1/28 in a CM patient) and 49 total attacks. At lasmiditan intake, 42.9% patients rated migraine intensity as severe (0–3 rating scale). Pain freedom 2 h post‐dose was reported in 35.7% (10/28) of first‐treated attacks, and in 36.7% (18/49) of total attacks. The rate of pain freedom was not influenced by timing of lasmiditan intake (p = 0.145), baseline pain severity (p = 0.262) and presence of chronic vs episodic migraine (p = 0.683). Freedom from the most bothersome symptom 2 h post‐dose was reported in 47.7% of attacks. Adverse events were reported in 26 of total attacks treated (53.1%), predominantly as dizziness (n = 11), fatigue (n = 8) and paraesthesia (n = 6). Tolerability was rated as good‐to‐excellent in 50% of cases.
Conclusion: Our real‐world data support lasmiditan effectiveness in the acute treatment of migraine. Adverse events were reported in 53.1% of attacks.
Disclosure: CT has participated in advisory boards for AbbVie, Dompé, Eli Lilly, Lundbeck, Novartis, Pfizer, and Teva; lectured at symposia and is a principal investigator or collaborator in clinical trials sponsored by AbbVie, Eli Lilly, Lundbeck, Novartis, and Teva; received research grants from the European Commission, the Italian Ministry of Health, the Italian Multiple Sclerosis Foundation, and the Migraine Research Foundation; and serves as an associate editor for Cephalalgia and The Journal of Headache and Pain. R.D.I received speaker honoraria for scientific presentations from Eli‐Lilly, and Teva, and has participated as advisory board for Pfizer. GV reports consultant fees from Lundbeck.
EPO‐541
The relationship of medication overuse to vertigo, sleep, anxiety, depression and comorbidities in migraine patients
R. Wilcha; P. Amarasena; L. Villar Martinez; J. Hoffmann; P. Goadsby
NIHR King's Clinical Research Facility, SLaM Biomedical Research Centre, and Wolfson Sensory, Pain and Regeneration Centre, King's College London, UK
Background and Aims: The global prevalence of medication overuse headache (MOH) is 1–2%. Migraine is the predominant risk factor, impacting 78% of individuals with MOH. Despite well‐established evidence that MO can contribute to the deterioration and chronification of a pre‐existing headache syndrome, little is known about its role in relation to existing comorbidities and other disabling symptoms of migraine. We sought to examine the relationship between medication overuse and the total number of comorbidities and the symptoms of vertigo, sleep disturbance, anxiety and depression.
Methods: Data were collected (n = 192) through the use of patient self‐completed health questionnaires utilising a variety of standardised tools including the Dizziness Handicap Inventory (DHI), Subjective Vertigo Questionnaire (SVQ), Epworth Sleepiness Scale (ESS), Pittsburgh Sleep Quality Index (PSQI), Generalized Anxiety Disorder 7 (GAD‐7), and Patient Health Questionnaire 8 (PHQ‐8). Binomial logistic regression was applied to examine the predictive role of medication overuse in relation to symptoms of vertigo, poor sleep, anxiety, and depression and the total number of comorbidities.
Results: The model demonstrated that medication overuse was associated with an increased total number of comorbidities (χ2(4) = 6.978, p = 0.008). There was no statistically significant difference observed in scores related to the symptoms of vertigo, sleep disturbance, anxiety and depression.
Conclusion: This data shows medication overuse is associated with an increased total number of comorbidities in migraine patients. Moving forward, physicians must recognise the impact of other comorbidities, not only headache that may contribute to medication overuse.
Disclosure: Nothing to disclose.
EPO‐542
An interdisciplinary integrated one‐stop‐shop special outpatient clinic for idiopathic intracranial hypertension
G. Bsteh1; S. Macher 1; N. Krajnc2; W. Marik3; M. Michl4; N. Müller1; S. Zaic1; J. Harreiter5; K. Novak6; C. Wöber1; B. Pemp4
1Department of Neurology, Medical University of Vienna, Vienna, Austria; 2Comprehensive Center for Clinical Neurosciences & Mental Health, Medical University of Vienna, Vienna, Austria; 3Department of Neuroradiology, Medical University of Vienna, Vienna, Austria; 4Department of Ophthalmology, Medical University of Vienna, Vienna, Austria; 5Department of Neurosurgery, Medical University of Vienna, Vienna, Austria; 6Division of Endocrinology, Department of Internal Medicine, Medical University of Vienna, Vienna, Austria
Background and Aims: Management of idiopathic intracranial hypertension (IIH) is complex requiring contributions from multiple specialized disciplines. In practice, this creates considerable organizational and communicational challenges for health care professionals and patients. To meet those challenges, we established an interdisciplinary integrated outpatient clinic for IIH (comprising neurology, neuroophthalmology, neuroradiology, neurosurgery and endocrinology) with a central coordination and a one‐stop‐shop concept. Here, we aimed to evaluate effects of this one‐stop‐shop concept on objective clinical outcome of patients with IIH.
Methods: Using the Vienna‐IIH database, we compared the one‐stop‐shop era (1‐JUL‐2021 to 31‐DEC‐2022) to a reference group receiving standard care (1‐JUL‐2018 to 31‐DEC‐2019) regarding clinical outcome parameters (visual impairment/worsening, headache improvement/freedom) assessed 6 months after diagnosis. Multivariate binary logistic regression models were used to adjust for confounders (age, body mass index [BMI], CSF opening pressure, visual impairment and chronic headache at diagnosis).
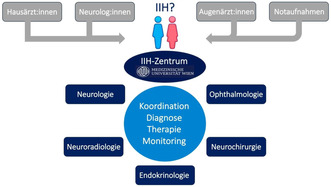
FIGURE 1 IIH one‐stop‐shop concept.
Results: Baseline characteristics of the one‐stop‐shop group (n = 85) and standard care group (n = 81) were comparable (female: 90.6% vs. 90.1%; mean age: 33.6 vs. 32.8 years, median BMI: 31.8 vs. 33.0, median CSF opening pressure: 320 vs. 341 mmH2O, visual impairment at diagnosis: 71.8% vs. 69.1%, chronic headache at diagnosis: 55.3% vs. 56.8%). Compared to standard care, the one‐stop‐shop concept was associated with a significantly higher likelihood of achieving both headache improvement (odds ratio [OR] 2.24, p < 0.001) and headache freedom (OR 1.75, p = 0.031), whereas the risk for visual impairment (OR 0.87, p = 0.231) and visual worsening (OR 0.67, p = 0.354) was not significantly reduced.
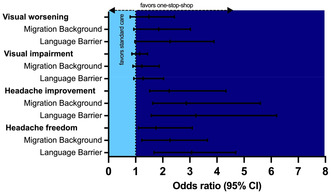
FIGURE 2 Outcome in the one‐stop‐shop concept compared to standard management.
Conclusion: Interdisciplinary integrated management of IIH significantly improves headache outcome and potentially also visual outcome.
Disclosure: GB: has participated in meetings sponsored by, received speaker honoraria or travel funding from Biogen, Celgene/BMS, Lilly, Merck, Novartis, Roche, Sanofi‐Genzyme and Teva, and received honoraria for consulting Biogen, Celgene/BMS, Merck, Novartis, Roche, Sanofi‐Genzyme and Teva. He has received unrestricted research grants from Celgene/BMS and Novartis.
Movement disorders 5
EPO‐543
The influence of thyroid disorders on the course of idiopathic adult‐onset dystonia
S. Idrissi 1; V. Velucci1; M. Esposito2; A. Trinchillo3; D. Belvisi4; V. Rizzo5; L. Avanzino6; F. Di Biasio7; F. Bono8; C. Lettieri9; S. Rinaldo10; A. Castagna11; M. Altavista12; P. Barone13; P. Barbero14; R. Ceravolo15; M. Mascia16; M. Zibetti17; C. Scaglione18; A. Bentivoglio19; L. Magistrelli20; M. Cotelli21; R. Pellicciari1; A. Berardelli4; G. Defazio1
1Department of Translational Biomedicine and Neuroscience (DiBraiN), “Aldo Moro” University of Bari, Bari, Italy; 2Clinical Neurophysiology Unit, Cardarelli Hospital, Naples, Italy; 3Department of Neurosciences, Reproductive Sciences and Odontostomatology, “Federico II” University, Naples, Italy; 4Department of Human Neurosciences, Sapienza University of Rome, Rome, Italy; 5Department of Clinical and Experimental Medicine, University of Messina, Messina, Italy; 6Department of Experimental Medicine (DIMES), University of Genoa, Genoa, Italy; 7IRCCS, Ospedale Policlinico San Martino, Genoa, Italy; 8Centre for Botulinum Toxin Therapy, Neurologic Unit, A.O.U. Mater Domini, Catanzaro, Italy; 9Clinical Neurology Unit, “S. Maria della Misericordia” University‐Hospital, Udine, Italy; 10Parkinson and Movement Disorders Unit, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy; 11IRCCS, Don Carlo Gnocchi Foundation Onlus, Milan, Italy; 12Neurology Unit San Filippo Neri Hospital ASL Rome, Rome, Italy; 13Department of Medicine, Surgery and Dentistry “Scuola Medica Salernitana”, University of Salerno, Salerno, Italy; 14Neurology Unit, Mauriziano Umberto I Hospital, Turin, Italy; 15Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy; 16Neurology Unit, University Hospital of Cagliari, Cagliari, Italy; 17Department of Neuroscience “Rita Levi Montalcini”, University of Turin, Turin, Italy; 18IRCCS Institute of Neurological Sciences, Bologna, Italy; 19Institute of Neurology, Università Cattolica del Sacro Cuore, Rome, Italy; 20Department of Translational Medicine, Movement Disorders Centre, Neurology Unit, University of Eastern Piedmont, Novara, Italy; 21Neurology Unit, ASST Valcamonica, Esine (Brescia), Italy
Background and Aims: A few earlier observations and recent controlled studies pointed to the possible contribution of thyroid diseases in idiopathic adult‐onset dystonia (IAOD).
Methods: To investigate the association between thyroid status and clinical characteristics of IAOD, focusing on dystonia localization, spread, and associated features such as tremors and sensory tricks. Patients were identified from the Italian Dystonia Registry, a multicentre dataset of patients with adult‐onset dystonia. The study population included 1518 IAOD patients. Patients with hypothyroidism and hyperthyroidism were compared with those without any thyroid disease.
Results: In the 1518 IAOD patients, 167 patients (11%; 95% CI, 9.5%–12.6%) were diagnosed with hypothyroidism and 42 (2.8 %; 95% CI, 1.99–3.74) with hyperthyroidism. The three groups were comparable in age at dystonia onset, but there were more women than men in groups with thyroid disease. We found more patients with blepharospasm in the hyperthyroidism group, but the difference lacked significance after the Bonferroni correction. The remaining dystonia‐affected body sites were similarly distributed in the three groups, as did dystonia‐associated features and spread.
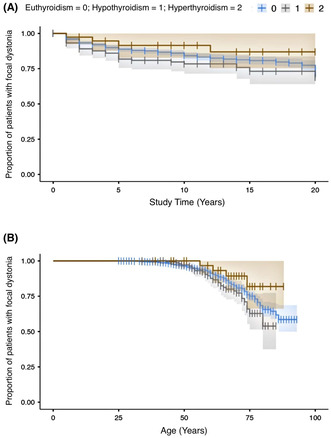
Kaplan–Meier's survival analysis of the spread of dystonia in patients with focal onset. (A) Study time was represented by the time elapsed between dystonia onset and spread. (B) Study time was represented by age at spread.
Conclusion: Even if the frequency of patients with thyroid disease is higher than the general European population, we cannot discuss the results in terms of risk factors due to the different ascertainment methodology. However, our findings provided novel information indicating that the high rate of thyroid diseases is not specific for any distinct dystonia subpopulation and does not appear to influence the natural history of IAOD.
Disclosure: Nothing to disclose.
EPO‐544
Neuropathological characteristics of the patients with old‐onset Parkinson's disease
K. Inoue 1; H. Fujimura1; T. Saito1; K. Toyooka1; M. Yamadera1; C. Mori1; M. Sudo1; Y. Izumi2
1Department of Neurology, NHO Osaka Toneyama Medical Center, Toyonaka, Japan; 2Department of Neurology, Tokushima University Faculty of Medicine
Background and Aims: The clinical features of the patients with old‐onset Parkinson's disease (PD) are characterized by postural areflexia, frozen gait, hallucinations, cognitive impairment, and autonomic failure.
Methods: From a consecutive autopsy series of 187 patients, 25 patients, pathologically confirmed Parkinson's disease and aged 50 years or older at onset, were selected. Their median age at onset was 72 years, median age at death: 83 years and 18 males (72%). We compared the age of onset, sex, duration of disease, presence or absence of dementia, Lewy body (LB) score, and lesions of Alzheimer's disease (AD) in the group with onset under 75 (normal) and after 75 years of age (elderly).
Results: In PD cases that developed after the age of 75 years, the duration of the disease was significantly shorter, and many cases were clinically diagnosed with dementia. In the elderly group, LB scores tended to be smaller in the brainstem and larger in the limbic system and neocortex than in the normal group, but there was no significant difference. Many of the cases in both groups were accompanied by mild to moderate AD lesions, but only a small number were diagnosed with pathological AD.
Conclusion: In elderly PD, LB lesions to the limbic ~ neocortex may expand prematurely.
Disclosure: Nothing to disclose.
EPO‐545
MRI volumetric assessment of neuropsychiatric symptoms in multiple system atrophy
I. Ruiz Barrio; A. Horta Barba; A. Puig Davi; S. Martinez Horta; J. Kulisevsky; J. Pagonabarraga
Movement Disorders Unit, Neurology Department, Hospital de Sant Pau, Barcelona, Spain
Background and Aims: Multiple system atrophy (MSA) presents diverse motor and non‐motor symptoms, with growing recognition of cognitive and neuropsychiatric manifestations. This study aims to address this gap by investigating neuropsychiatric symptoms and their neuroanatomical correlations in MSA.
Methods: Ten consecutive patients diagnosed with MSA based on current clinical criteria were included. Frontal Behavioral Inventory (FBI) and Neuropsychiatric Inventory (NPI) were administered to all patients. T1‐weighted scans were obtained using a 3 Tesla Philips Achieva station, and structural image processing was conducted with FreeSurfer (v.7.4.1). Volumetric analysis, involving the correlation of volumetric data with neuropsychiatric scales, was performed using R statistical software (v.4.3.0). Multiple comparisons were corrected using False Discovery Rate.
Results: High prevalence of neuropsychiatric symptoms was observed in MSA (44.4% with ≥3 points in FBI, mean NPI score 6.8 ± 3.9). Demographics are summarised in table 1. There were no significant differences among clinical subtypes in analyzed variables. Linear modeling revealed significant amygdala atrophy across higher scores of FBI and NPI (p = 0.025 and 0.014, respectively), independent of clinical subtype (Figures 1 and 2).
Conclusion: Neuropsychiatric symptoms, prevalent in both parkinsonian and cerebellar subtypes of MSA, may be associated with amygdala atrophy. Further studies exploring the pathophysiology of neuropsychiatric alterations in MSA are essential, considering the significant impact on daily activities.
Disclosure: Nothing to disclose.
EPO‐546
MRI volumetric assessment of neuropsychiatric symptoms in multiple system atrophy
I. Ruiz Barrio; A. Horta Barba; A. Puig Davi; S. Martinez Horta; J. Kulisevsky; J. Pagonabarraga
Movement Disorders Unit, Neurology Department, Hospital de Sant Pau, Barcelona, Spain
Background and Aims: Multiple system atrophy (MSA) presents diverse motor and non‐motor symptoms, with growing recognition of cognitive and neuropsychiatric manifestations. This study aims to address this gap by investigating neuropsychiatric symptoms and their neuroanatomical correlations in MSA.
Methods: Ten consecutive patients diagnosed with MSA based on current clinical criteria were included. Frontal Behavioral Inventory (FBI) and Neuropsychiatric Inventory (NPI) were administered to all patients. T1‐weighted scans were obtained using a 3 Tesla Philips Achieva station, and structural image processing was conducted with FreeSurfer (v.7.4.1). Volumetric analysis, involving the correlation of volumetric data with neuropsychiatric scales, was performed using R statistical software (v.4.3.0). Multiple comparisons were corrected using False Discovery Rate.
Results: High prevalence of neuropsychiatric symptoms was observed in MSA (44.4% with ≥3 points in FBI, mean NPI score 6.8 ± 3.9). Demographics are summarised in table 1. There were no significant differences among clinical subtypes in analyzed variables (table 2). Linear modeling revealed significant amygdala atrophy across higher scores of FBI and NPI (p = 0.025 and 0.014, respectively), independent of clinical subtype (Figures 1 and 2).
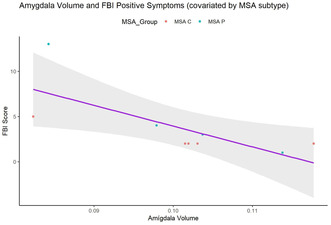
FIGURE 1 Correlation between amygdala volume and FBI positive symptoms.
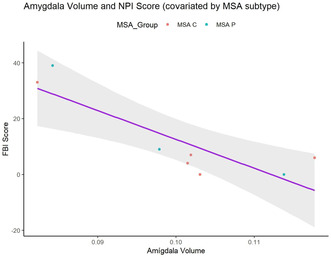
FIGURE 2 Correlation between amygdala volume and NPI score.
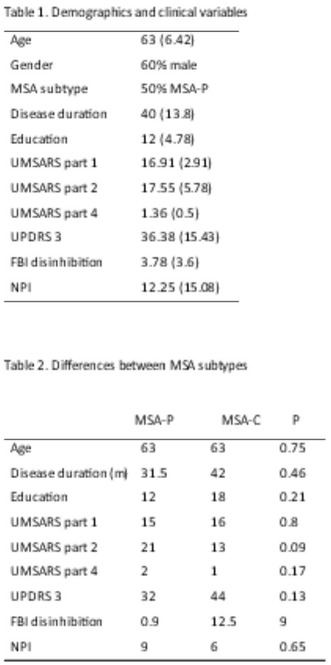
TABLE 1 and 2 Demographics and differences between MSA subtypes.
Conclusion: Neuropsychiatric symptoms, prevalent in both parkinsonian and cerebellar subtypes of MSA, may be associated with amygdala atrophy. Further studies exploring the pathophysiology of neuropsychiatric alterations in MSA are essential, considering the significant impact on daily activities.
Disclosure: Nothing to disclose.
EPO‐547
A randomized, double‐blinded, placebo‐controlled QTc study to evaluate BIA 286156 effect on cardiac repolarization
I. Peixoto 1; D. Hilt2; H. Gama1; J. Holenz1
1Research & Development Division, BIAL‐Portela & Cª, S.A., S. Mamede do Coronado, Portugal; 2BIAL BioTech Investments, Inc.
Background and Aims: Betaglucocerebrosidase (GCase) is encoded by the GBA1 gene. Its mutations are the most common genetic risk factor for Parkinson's disease (PD). BIA 28‐6156 is an allosteric activator of GCase developed to treat the causative processes in GBA‐PD. This study primarily aimed to evaluate the effect of BIA 286156 on QT interval corrected (QTc) for heart rate (HR) based on the Fridericia correction (QTcF) in healthy subjects.
Methods: Phase 1, randomized, double‐blinded, placebo‐controlled, 4‐period crossover study. Subjects received 1 of 12 treatment sequences. A single dose of 60 mg or 150 mg BIA 28‐6156, 400 mg moxifloxacin or placebo was administered in fed state (Table 1). Relationship between BIA 28‐6156 plasma concentrations and change‐from‐baseline QTcF (ΔQTcF) was analyzed to exclude an effect of ΔΔQTcF >10 msec at clinically relevant plasma levels. HR, PR, and QRS intervals, and electrocardiogram (ECG) waveform morphology were evaluated. Incidence and severity of treatment emergent adverse events (TEAEs) were analyzed.

Results: A total of 37 subjects were enrolled, with 33 completing the study. Based on the concentration‐QTc analysis, an effect on ΔΔQTcF exceeding 10 msec can be excluded within the full observed range of plasma concentrations of BIA 28‐6156 up to ~7150 ng/mL. No clinically relevant effects on studied ECG parameters were found. No deaths or other serious AEs were reported. 2 subjects withdrew due to AEs.
Conclusion: BIA‐28‐6156 doses were well tolerated, with a favorable safety profile. These results showed no clinically relevant effects on ECG parameters, constituting a negative thorough QT/QTc study.
Disclosure: Supported by Bial‐Portela & Cª, S.A.
EPO‐548
Baseline variables associated with apomorphine sublingual film retention
J. Kassubek 1,2; J. Schwarz3; L. López Manzanares4; M. Fonseca5; C. Denecke Muhr5
1Department of Neurology, University Hospital Ulm, Ulm, Germany; 2German Centre for Neurodegenerative Diseases, Ulm, Germany; 3Department of Geriatrics, Kreisklinik Ebersberg, Ebersberg, Germany; 4La Princesa University Hospital, Madrid, Spain; 5Bial – Portela & Ca, S.A., Coronado, Portugal
Background and Aims: The Phase 3 Study CTH‐301 evaluated the long‐term safety/tolerability and efficacy of apomorphine sublingual film (SL‐APO) for treating OFF‐episodes in Parkinson's disease patients with motor fluctuations. Data from this study were used to build a model to identify baseline variables that differ between patients who completed the study and those who discontinued during the dose optimisation or long‐term maintenance phase due to either lack of efficacy or adverse events (AEs), therefore influencing retention.
Methods: Baseline variables were ranked based on their correlation (Chi‐square) with the discrete target variable (completers vs non‐completers due to lack of efficacy or AEs). A logistic regression classification algorithm with LASSO regularisation was used to select the final variables.
Results: Of 496 patients, 120 completed the study, 26 discontinued due to lack of efficacy, 167 due to AEs, and 183 due to other reasons. Median time on SL‐APO was 204 days. Compared to completers, non‐completers due to lack of efficacy demonstrated a higher levodopa total daily dose (p < 0.001), lower rate of morning akinesia (p = 0.036), higher rate of de novo enrolment (no previous SL‐APO exposure; p = 0.048) and higher number of levodopa intakes (p = 0.027) (Figure 1). Compared to completers, non‐completers due to AEs had a lower rate of concomitant dopamine agonists use (p < 0.001) and higher rate of de novo enrolment (p = 0.019) (Figure 2).
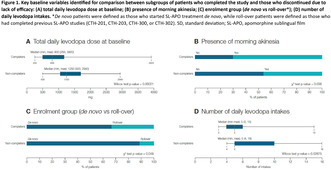
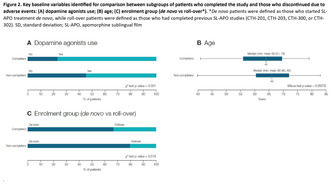
Conclusion: Levodopa dose and intakes, morning akinesia, previous SL‐APO exposure and concomitant dopamine agonist use might influence retention. These results may help identify patients more likely to remain on SL‐APO over the long term.
Disclosure: Supported by Bial.
EPO‐549
Efficacy and safety of levodopa in dystonia in Wilson disease (LIDWID): A randomized placebo‐controlled trial
P. Kalita; D. Ahmed; D. Mahajan
Sanjay Gandhi Post Graduate Institute of Medical Sciences
Background and Aims: Dystonia is the commonest movement disorder in neurologic Wilson disease (NWD). Levodopa is used in primary dystonia, but has not been systematically evaluated in NWD. We report the efficacy and safety of levodopa compared to placebo in NWD patients with dystonia.
Methods: NWD patients having a Fahn‐Marsden Dystonia Rating (FMDR) score of >20 were included in whom other possible causes were ruled out. Patients were randomized to levodopa‐carbidopa (LCD) or placebo using 1:1 randomization. LCD (100 mg + 10 mg) was started in a dose of half tab thrice daily, and increased every week to 2 tablets thrice daily. Placebo group received saccharine tablet. Outcome was defined at 3 months. The primary outcome was improvement in FMDR score by >50%, and secondary outcomes were Neurological Severity score (NSS), Dysphagia Outcome and Severity Scale (DOSS) score and side effects.
Results: 13 patients each were randomized to LCD and placebo. Their baseline characteristics were comparable. Only one patient in each group achieved primary outcome. At 3 months, both LCD and placebo groups had significant improvement in FMRD score, NSS and DOSS score. The improvement in FMRD (55.00 ± 35.35 vs 45.92 ± 41.40; p = 0.55), NSS (7.61 ± 4.61 vs 5.77 ± 3.37; p = 0.25) and DOSS score (4.92 ± 1.70 vs 4.77 ± 2.16; p = 0.84) however were not significantly different between LCD and placebo groups. Four patients had minor side effects (3 LCD and 1 placebo).
Conclusion: LCD is safe in NWD and well tolerated. Patients in both LCD and placebo group improved at 3 months, but LCD did not have advantage over placebo in reducing dystonia.
Disclosure: Nothing to disclose.
EPO‐550
Foslevodopa/foscarbidopa in advanced Parkinson's disease: Demonstration of savings from a societal perspective in the UK
K. Chaudhuri1; L. Bergmann2; J. Belsey 3; T. Boodhna4; E. Leoncini4; J. Zamudio5
1Institute of Psychiatry, Psychology & Neuroscience, King's College London, UK; 2AbbVie, Ludwigshafen, Germany; 3JB Medical Ltd, London, UK; 4AbbVie, Marlow, UK; 5AbbVie, North Chicago IL, USA
Background and Aims: In patients with advanced Parkinson's disease (aPD), adequate control of OFF time may not be achievable using oral/transdermal therapies. Clinical trials of Foslevodopa/foscarbidopa (LDp/CDP) have shown meaningful reductions in OFF‐time and sleep disturbance – both strong predictors of healthcare resource use. Previous analyses have only considered direct medical costs: this analysis considers a broader societal perspective.
Methods: Clinical trial and real‐world evidence were used to drive a cost‐utility model comparing LDp/CDp with best medical treatment (BMT), which was accepted by the UK National Institute of Health and Care Excellence. Using outputs from this analysis, a societal impact model was developed. Quintiles of normalised OFF‐time across a 16‐hour waking day in each treatment group were applied to literature‐based estimates for direct medical, non‐medical and indirect costs. The resulting state‐specific cost estimates were applied to the modelled aPD patient population.
Results: The mean overall cost of care per patient on BMT was estimated as £115,667 in year 1, rising to £123,943 in year 5 (2022 GBP). For LDp/CDp, the corresponding costs were £111,491 and £118,495 respectively. Savings were approximately evenly split across the three cost categories. If applied to all 17,500 aPD patients in the UK, this would amount to a net saving in LDp/CDp‐treated patients of £73.1 million in year 1, rising to £95.4 million in year 5.
Conclusion: The use of LDp/CDp in aPD patients inadequately controlled on oral therapy, is associated with net annual savings of over £73 million compared to BMT, when considered from a societal perspective.
Disclosure: KRC: K. Ray Chaudhuri is a study investigator and has served as an advisory board member for AbbVie, UCB, GKC, Bial, Cynapsus, Lobsor, Stada, Medtronic, Zambon, Profile, Sunovion, Roche, Therevance, Scion, Britannia, Acadia, and 4D. He received honoraria for lectures from AbbVie, Britannia, UCB, Zambon, Novartis, Boehringer Ingelheim, Bial, Kyowa Kirin, and SK Pharma. He has received grants (investigator initiated) from Britannia Pharmaceuticals, AbbVie, UCB, GKC, and Bial, and academic grants from EU, IMI EU, Horizon 2020, Parkinson's UK, NIHR, PDNMG, EU (Horizon 2020), Kirby Laing Foundation, NPF, MRC, and Wellcome Trust. He receives royalties from Oxford University Press and holds intellectual property rights for the King's Parkinson's Pain Scale and Parkinson's Disease Sleep Scale. LB: Lars Bergmann is a full‐time employee of AbbVie, and may hold AbbVie stock or stock options. JB: Jonathan Belsey has carried out commercial analytical consultancy work for a wide range of pharmaceutical and medical device companies. In the past 5 years, he has undertaken projects in the field of neuroscience for AbbVie, Bioprojet and Global Kinetics TB: Trishal Boodhna is a full‐time employee of AbbVie, and may hold AbbVie stock or stock options. EL: Emanuele Leoncini is a full‐time employee of AbbVie, and may hold AbbVie stock or stock options. JZ: Jorge Zamudio is a full‐time employee of AbbVie, and may hold AbbVie stock or stock options.
EPO‐551
Fractures and emergency department contacts among patients with Parkinson's disease in denmark
T. Henriksen1; U. Lønberg2; J. Samuelsson 3; P. Schwarz4
1Movement Disorder Unit, University Hospital of Bispebjerg, Copenhagen, Denmark; 2Formerly AbbVie Denmark, København, Denmark; 3AbbVie Sweden, Solna, Stockholm, Sweden; 4Department of Endocrinology, Bone‐metabolic Research Unit, Rigshospitalet, København Ø, Denmark
Background and Aims: Parkinson's Disease (PD) patients often experience symptoms like freezing of gait, axial rigidity, and postural instability, increasing their risk of falls. Osteoporosis in PD is common, which increases the risk of fractures if falling. Falls resulting in fractures could require surgical intervention, significantly contributing to morbidity and mortality. However, there is currently no data on fracture rates within the Danish PD population. This study aimed to analyze fracture rates and other fall‐related injuries among Danish PD patients.
Methods: This study is a retrospective, nationwide analysis that used data from the National Patient Registry, Danish National Prescription Registry, and Statistic Denmark. We evaluated the standardized incidence ratio (SIR) of hip fractures, major osteoporotic fractures (MOF, including hip, vertebral, humerus, and forearm fractures), and traumatic emergency department (ED) visits in PD patients compared to the general population.
Results: The analysis incorporated 7,242 patients with PD and 2,851,000 matched controls. Hip fracture rates in patients with PD were four times higher compared to the general population, when standardised by sex and age. Additionally, the incidence rates of major osteoporotic fractures (MOF) and traumatic emergency department visits were three times and two times higher, respectively. When considering multiple fractures, the incidence rate of traumatic emergency department visits is 2.6 times higher in Parkinson's patients.
Conclusion: Our study shows a significantly increased risk of fractures for PD patients compared to the general population, indicating a need for optimal medical treatment, fall‐prevention, and potential use of anti‐resorptive medication in PD patient care.
Disclosure: Tove Henriksen (TH) has received honorary for talks from AbbVie, Britannia, Nordic Infucare, NeuroDerm, Convatec. TH has been a principal investigator for a study sponsored by AbbVie. TH has served as DMC board member at a study sponsored by Lundbeck. Ulla Sofie Lønberg is a former AbbVie employee Jenny Samuelsson is an AbbVie employee and shareholder of AbbVie stocks Peter Schwartz has nothing to disclose. This study was funded by AbbVie. AbbVie participated in the study design, interpretation of data and in reviewing, and approving the final version of the abstract.
EPO‐552
Cognitive phenotyping of GBA‐Parkinson's disease: A study on deep brain stimulation outcomes
J. Fernández‐Vidal; I. Aracil‐Bolaños; C. García; J. Kulisevsky; B. Pascual‐Sedano
Movement Disorders Unit, Department of Neurology, Hospital de la Santa Creu i Sant Pau
Background and Aims: Glucocerebrosidase (GBA) gene in Parkinson's disease (PD) associates earlier onset and worse cognitive decline. Deep Brain Stimulation (DBS) in GBA‐PD effectively treats motor symptoms but long‐term cognitive effects are unclear. Our study investigated 5‐year outcomes in GBA‐PD‐DBS.
Methods: Retrospective cohort at H.Sant Pau (Barcelona, Spain) of DBS‐PD with pre/postDBS assessments: cognitive (MDRS), frontal behavior (FrSBe), verbal fluencies, motor (MDS‐UPDRS), L‐dopa (LEDD), life quality (PDQ‐39), and depression (BDI). Non‐GBA‐PD cluster analysis was conducted based on first‐year cognitive impairment (CI).
Results: Out of 96 PD patients, 13 (13.5%) were GBA‐PD. Cluster analysis identified progressors//non‐progressors. Progressors’ trajectory showed similarities to GBA‐PD in cognition, FrSBe and PDQ‐39, whereas non‐progressors remained stable. In 56 PD‐patients with 5‐year cognitive follow‐up, 8 were gene‐carriers. GBA‐PD showed faster CI to dementia (p = 0.05), especially in attention (p = 0.015), conceptualization (p = 0.004) memory (p = 0.05), with no age or education baseline differences. Regarding FrSBe, GBA‐PD exhibited worse baseline disinhibition (p = 0.03) with progressive improvement, while apathy and executive dysfunction deteriorated like non‐GBA‐PD. Depression scales showed higher values during the first two years in GBA‐PD (p = 0.04). Motor outcomes, LEDD, and phonetic fluency showed no differences, while GBA‐PD‐semantic‐fluency worsened over time (p = 0.02). No long‐term differences were found in GBA‐PD‐PDQ‐39.
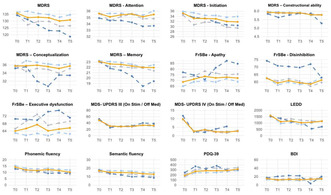
Evolution of studied variables. Groups: GBA‐PD (dark blue), non‐GBA‐PD (orange), non‐GBA‐progressors (grey), non‐GBA‐non‐progressors (light blue).
Conclusion: GBA‐PD‐CI was centered on attention, conceptualization, and memory; similar profile as progressors. Semantic fluency correlates with cognitive worsening in GBA‐PD. From onset, GBA‐PD‐FrSBe was poorer and fluctuating but stable; also as progressors. Motor outcomes and quality of life were similar between GBA‐PD, non‐GBA‐PD, and clusters, unaffected by CI. Previous surgery, FrSBe and fluencies, rather than MDRS/subscales, predict CI in non‐GBA‐PD‐clusters.
Disclosure: Nothing to disclose.
EPO‐553
Neurophysiological architecture of visual categorization in Parkinson's disease with minor visual hallucinations
L. Perez‐Carasol; S. Martinez‐Horta; A. Horta‐Barba; A. Puig‐Davi; J. Kulisevsk; J. Pagonabarraga
Movement Disorders Unit, Department of Neurology, Hospital de la Santa Creu i Sant Pau, Barcelona, Spain
Background and Aims: Although minor hallucinations are common in Parkinson's disease (PD, its precise neural mechanisms remain partially understood. Here, we addressed behavioral and neurophysiological anomalies accompanying visual categorization in patients with minor hallucinations.
Methods: We performed task‐related EEG on 23 patients with (HAL‐PD) and 23 without (nHAL‐PD) minor hallucinations during a visual‐categorization task based on objects, faces and facial‐pareidolias. We identified the main neurophysiological components along the time course of processing and we studied its spectral characteristics to build functional connectivity models based on the signal sources.
Results: No differences were found in any of the clinical/sociodemographic parameters. HAL‐PD showed difficulties identifying the most ambiguous stimuli. The neurophysiological components along visual processing showed abnormalities in HAL‐PD in: (1) early visual categorization processes (N170) for stimuli requiring less specialized analysis (objects [t(23) = 1.9; p < 0.05]; pareidolias [t(23) = 2.23; p < 0.05]) and (2), in the late processes of semantic attribution (P600) [t = (23) = 2.2; p < 0.05]. Time‐frequency analysis showed a main slow‐wave component (3 Hz–8 Hz) decreased in HAL‐PD along the time interval of interest. The HAL‐PD group showed an overall decreased connectivity between different areas of the brain (green), accompanied by an increased connectivity between left‐sided inferior/anterior nodes of the semantic system and posterior nodes of the default‐mode network.

Task‐related components and connectivity analysis.
Conclusion: Minor hallucinations are associated with a combined impairment of early visual recognition (N170) and later semantic attribution (P600). This is accompanied by several differences in the neural architecture subserving these processes. Our results emphasize the use of inadequate semantic information to confer meaning to the deficiently processed stimulus as the central mechanism for minor hallucinations.
Disclosure: Nothing to disclose.
EPO‐554
Mixed brain pathology in neurodegenerative parkinsonism and dementia
K. Mensikova 1; L. Tuckova2; D. Hrabos2; J. Bouchal2; J. Ehrmann2; P. Kanovsky1
1Department of Neurology and Clinical Neuroscience Center, Faculty of Medicine and Dentistry, Palacky University and University Hospital Olomouc, Olomouc, Czechia; 2Department of Clinical and Molecular Pathology, Faculty of Medicine and Dentistry, Palacky University, Olomouc, Czechia
Background and Aims: The aim of the study was to assess the presence and proportion of mixed neurodegenerative pathology in a prospective cohort of patients treated for any phenotype of neurodegenerative parkinsonism and its impact on the accuracy of clinical diagnosis.
Methods: A total of 49 brains of patients who were diagnosed with neurodegenerative parkinsonism or dementia and who consented to join the donor programme were autopsied; neuropathological examinations were performed according to the standard protocol.
Results: There were 25 patients, in whom the pathological examination confirmed the presence of single pathology: 13 patients suffered from alfa‐synucleinopathy (syn), 5 patients suffered from tauopathy (tau), 1 patient suffered from TDP‐34‐pathology (TDP‐43) and 6 suffered from AD‐related proteinopathy (AD). In 21 patient examinations revealed the presence of double pathology (4 syn/tau, 7 syn/AD, 6 tau/AD, 4 AD/TDP‐43), and in 3 patients examination revealed the presence of triple pathology (syn/tau/AD). The correct clinical diagnosis was confirmed in 26 cases, the incorrect clinical diagnosis was done in 23 cases; 13 of them suffered from the mixed brain pathology.
Conclusion: The mixed brain pathology is relatively common finding at brain autopsy in patients who suffered from neurodegenerative parkinsonism, even when the recent and validated clinical diagnostic criteria were used during the diagnostic process. This fact should serve as a basis for the further discussion about their usefulness. These findings also point to the need of intensive research aimed at identifying biomarkers capable of predicting the corresponding types of pathological processes.
Disclosure: Supported by: MH CZ‐DRO (FNOl, 00098892) and IGA LF 2023‐015.
EPO‐555
Impact of ADORA2A gene polymorphism on Dyskinesia in Parkinson's disease
S. Kuzieva; S. Shokhimardonov
Neurology Department, Tashkent Medical Academy, Tashkent, Uzbekistan
Background and Aims: Parkinson's progression leads to motor complications and dyskinesias with levodopa use. This study investigates the link between ADORA2A gene polymorphisms (rs2298383, rs35060421, and rs5751876) and dyskinesia in Parkinson's patients, inspired by the positive effects of ADORA2A receptor antagonism on motor symptoms and dyskinesias.
Methods: A cohort of 200 Parkinson's disease (PD) patients, aged 25 and above, with a minimum of one year of levodopa treatment, participated in the study. Among them, 70 patients exhibiting dyskinesia were designated as cases, while 130 patients without dyskinesia comprised the control group. Genetic evaluations were conducted on both groups, utilizing DNA extracted from peripheral venous blood. The genetic analysis involved high‐resolution melting analyses to assess and compare genetic profiles.
Results: While no significant association was observed between the investigated polymorphisms of rs5751876 and rs2298383 alleles and dyskinesia, the rs35060421 allele showed a notably higher frequency in the patient group (odds ratio: 1.39). In regression analysis, considering factors such as gender, age of disease onset, duration of levodopa treatment, and total drug dosage, the odds ratio for rs35060421 increased to 1.608. This suggests that the presence of this allele, in conjunction with other factors, elevates the risk of developing dyskinesia.
Conclusion: Patients with Parkinson's disease (PD) experiencing dyskinesia exhibited longer disease duration, more severe symptoms, and a higher dosage of levodopa. Although no statistically significant difference was identified between dyskinesia and the studied polymorphisms, there is a potential association suggesting that individuals with the rs35060421 polymorphism may face an increased risk of developing dyskinesia.
Disclosure: Nothing to disclose.
EPO‐556
Oropharyngeal adverse events in Parkinson's patients with motor fluctuations treated with apomorphine sublingual film
L. Wojtecki 1,2; F. Moreira3; E. Cubo4; M. Fonseca5; G. Harrison‐Jones5; C. Denecke Muhr5
1Department of Neurology & Institute of Clinical Neuroscience and Medical Psychology, University Clinic Duesseldorf, Duesseldorf, Germany; 2Department of Neurology and Neurorehabilitation, Hospital Zum Heiligen Geist, Duesseldorf, Kempen, Germany; 3Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal; 4Department of Geriatrics, Hospital Universitario de Burgos, Burgos, Spain; 5Bial – Portela & Ca, S.A., Coronado, Portugal
Background and Aims: Study CTH‐301 demonstrated that apomorphine sublingual film (SL‐APO) was well‐tolerated and efficacious for treating OFF‐episodes in Parkinson's disease patients with motor fluctuations. This post‐hoc analysis explored the occurrence of oropharyngeal treatment‐emergent adverse events (TEAEs) in patients included in this study.
Methods: Study CTH‐301 was a Phase 3, multicentre, open‐label trial composed of a dose‐optimisation (DO) and long‐term safety (LTS) phase. Incidence, severity and time to onset of oropharyngeal TEAEs and discontinuations due to oropharyngeal TEAEs were evaluated. Baseline characteristics that differed between patients who developed oropharyngeal TEAEs and those who did not and between patients who discontinued due to oropharyngeal TEAEs and those who did not were also identified.
Results: Of 496 patients, 206 (41.5%) experienced oropharyngeal TEAEs and 81 (16.3%) discontinued due to oropharyngeal TEAEs (both DO + LTS) (Table 1). The majority of oropharyngeal TEAEs overall and those leading to discontinuation were mild or moderate (Table 1), with more severe TEAEs being associated with higher discontinuation rates. Median time to onset for oropharyngeal TEAEs and oropharyngeal TEAEs leading to discontinuation was 89.5 and 114.5 days from study initiation, respectively (Figure 1). Baseline characteristics significantly associated with the occurrence of oropharyngeal TEAEs were dopamine agonists use (p < 0.001), older age (p < 0.01) and other dopaminergic medications use (p < 0.01). Baseline characteristics significantly associated with occurrence of oropharyngeal TEAEs leading to discontinuation were older age (p < 0.01) and dopamine agonists use (p = 0.042).

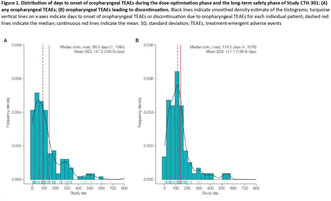
Conclusion: Oropharyngeal TEAEs, including those leading to discontinuation, were mostly mild or moderate and predominantly occurred within the first few months of SL‐APO initiation.
Disclosure: Supported by Bial.
EPO‐557
Remote monitoring of symptoms helps to maintain the quality of life in Parkinson's disease
L. Mäkitie 1; J. Niskala1; K. Redecop2; W. van Deen2; C. Godoy junior2; H. Mueller3; B. Tas3; E. Fiorenzato4; L. Weis4; A. Antonini4; M. Koivu1
1Department of Neurology, Brain Center, Helsinki University Hospital and Department of Clinical Neurosciences, University of Helsinki, Helsinki, Finland; 2Erasmus School of Health Policy and Management, Section Health Technology Assessment, Erasmus University, Rotterdam, The Netherlands; 3NeuroPath SRL/BV, Engheim, Belgium; 4Parkinson's Disease & Movement Disorders Unit, Department of Neuroscience (DNS), University of Padua, Italy
Background and Aims: Remote monitoring of patients provides objective information for the healthcare to adjust the treatment. Simultaneously the patient has a better insight into the disease giving opportunity for improvements in self‐care and lifestyle. In AICCELERATE‐project, we develop remote monitoring of persons with Parkinson's disease (pwp).
Methods: 26 pwps were randomized either to an intervention group (N = 14) provided with a wrist‐worn wellness wearable (Polar Ignite 2), a videomonitoring solution (NeuroPath), and a mobile symptom diary (Health Village, HUS) or to a control group (N = 12). Patients were asked to use the devices monthly. All patients were clinically evaluated twice in 6 months by validated scores (MDS‐UPDRS, NMSS and PDQ39). Adherence was evaluated by the number of measurements taken. Quality of life, Parkinson‐symptoms and levodopa equivalent daily doses were compared between groups with statistical tests (Wilcoxon for pre‐post comparisons and Mann‐Whitney U for between group comparisons).
Results: During 6 months, patients had performed median of 4.8 video‐monitoring sessions (12 motor tasks/session), reported symptoms 2.4 times with the diary, and used the wellness wearable for median of 103 days. Three patients wished to discontinue in the study during the follow‐up. Quality of life (PDQ39) had improved after remote monitoring period compared to control group (the changes in PDQ‐4.5 and 3.5, respectively, p = 0.017). There was no statistical difference between baseline demographics or the progression of symptoms between groups.
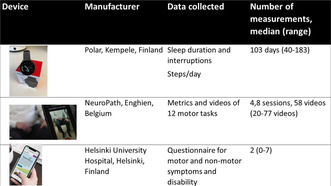
TABLE 1 Median number of remote measurements taken in 6 months at home by intervention group.
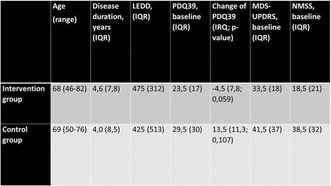
TABLE 2 Demographics at baseline and validated scores as median values in intervention and control groups. Interquartile range (IQR), range and p‐values in parentheses. LEDD, levodopa equivalent daily dose.
Conclusion: Patients are motivated to use technology for months to acquire detailed information on their disease. The quality of life is not affected by monitoring, rather promotes better well‐being.
Disclosure: The project has been funded by EU's Horizon2020.
Movement disorders 6
EPO‐558
Home‐based non‐invasive brain stimulation in combination with speech therapy in Parkinson's disease – Preliminary data
L. Brabenec 1; D. Kovac2; J. Mekyska2; P. Klobusiakova1; L. Rehulkova3; V. Kabrtova3; I. Rektorova1
1Central European Institute of Technology – CEITEC, Masaryk University, Applied Neuroscience Research Group, Brno, Czechia; 2Brno University of Technology, Department of Telecommunications, Brno, Czechia; 3Faculty of Medicine and St. Anne's University Hospital, First Department of Neurology, Brno, Czechia
Background and Aims: Hypokinetic dysarthria (HD) affects up to 90 % of Parkinson's disease (PD) patients, manifesting as reduced loudness, imprecise articulation, and impaired speech prosody. This ongoing study aims to investigate the effects of home‐based transcranial direct‐current stimulation (tDCS) as an add‐on to the remote Lee‐Silverman Voice Treatment (LSVT), compared to LSVT alone (coupled with sham stimulation), in PD patients.
Methods: Using a double‐blinded, randomized design, PD patients are divided into two groups, receiving either real or sham anodal tDCS (2 mA, 20 min) of the right superior temporal gyrus (rSTG – auditory‐feedback area) over 20 sessions in four weeks. Concurrently, both groups undergo remote LSVT. All participants undergo MRI scanning (fMRI‐reading task and resting state) and evaluation by speech therapists, at baseline and after the treatment.
Results: Analysis of the first 12 subjects (6 sham, 6 real stimulation) revealed significant improvements for all participants in the Dysarthric profile scale Total score (median relative change = 5.87, p = 0.005) and Phonetics score (median relative change = 4.0, p = 0.038). Changes in Phonetics score correlated with changes in left supplementary motor area (lSMA) activations (R = 0.678, p = 0.045). Interestingly, changes in resting state connectivity between rSTG and lSMA were higher after real stimulation (median = 63.8) than after sham (median = −100.4), though not statistically significant (p = 0.114).
Conclusion: Preliminary data suggest that the remote LSVT is beneficial for PD patients and combination with home‐based stimulation is feasible. We also observed neural correlates of induced speech improvements.
Disclosure: Nothing to disclose.
EPO‐559
Levodopa‐induced dyskinesias impact on quality of life in Parkinson's disease: A 5‐year follow‐up study
L. Samaniego 1; D. Santos‐García1; T. de Deus2; S. Jesús3; M. Cosgaya4; J. García‐Caldentey5; N. Caballol6; I. Legarda7; J. Hernández‐Vara8; I. Cabo9; L. López‐Manzanares10; I. González‐Aramburu11; M. Ávila‐Rivera12; V. Gómez Mayordomo13; V. Nogueira14; J. Dotor García‐Soto15,16; C. Borrué17; B. Álvarez Sauco18; M. Mir19; P. Coppadis3; S. Coppadis20
1CHUAC, Complejo Hospitalario Universitario de A Coruña, A Coruña, Spain; 2CHUF, Complejo Hospitalario Universitario de Ferrol, A Coruña, Spain; 3Unidad de Trastornos del Movimiento, Servicio de Neurología y Neurofisiología Clínica, Instituto de Biomedicina de Sevilla, Hospital Universitario Virgen del Rocío/CSIC/Universidad de Sevilla, Seville, Spain; 4Hospital Clínic de Barcelona, Barcelona, Spain; 5Centro Neurológico Oms 42, Palma de Mallorca, Spain; 6Consorci Sanitari Integral, Hospital Moisés Broggi, Sant Joan Despí, Barcelona, Spain; 7Hospital Universitario Son Espases, Palma de Mallorca, Spain; 8Hospital Universitario Vall d´Hebron, Barcelona, Spain; 9Complejo Hospitalario Universitario de Pontevedra (CHOP), Pontevedra, Spain; 10Hospital Universitario La Princesa, Madrid, Spain; 11Hospital Universitario Marqués de Valdecilla – IDIVAL, Santander, Spain; 12Consorci Sanitari Integral, Hospital General de L´Hospitalet, L´Hospitalet de Llobregat, Barcelona, Spain; 13Neurology Department, Institute of Neuroscience, Vithas Madrid La Milagrosa University Hospital, Vithas Hospital Group, Spain; 14Hospital Universitario Lucus Augusti, Lugo, Spain; 15Hospital Universitario Virgen Macarena, Sevilla, Spain; 16Hospital Infanta Sofía, Madrid, Spain; 17Hospital Infanta Sofía, Madrid, Spain; 18Institut d'Assistència Sanitària (IAS) – Institut Català de la Salut, Girona, Spain; 19Hospital General Universitario de Elche, Elche, Spain; 20Fundación Degen, A Coruña, Spain
Background and Aims: Levodopa‐induced dyskinesias (LID) are frequent in Parkinson´s disease (PD). Our aim was to analyze the change in the frequency of LID over time and identify LID related factors and know how LID impact on patients´ quality of life (QoL).
Methods: PD patients from the COPPADIS cohort were included. LID was defined as a non‐zero score in the item “Time spent with dyskinesia” of the UPDRS‐IV. It was applied at baseline (V0) and annually for 5 years. The 39‐item Parkinson's disease Questionnaire Summary Index (PQ‐39SI) was used to asses health‐related QoL.
Results: The frequency of LID at V0 in 672 PD patients (62.4 ± 8.9 years old; 60.1% males) with a mean disease duration of 5.5 ± 4.3 years was 18.9% (127/672) and increased progressively to 42.6% (185/434) at 5‐year follow‐up (V5y) (Figure 1A). LID was associated with disease duration and time under levodopa therapy (Figure 1A‐1D). Significant Independent factors associated with LID (p < 0.005) were a longer time under levodopa treatment and disease duration, a higher dose of levodopa, a lower dose of dopamine agonist and weight, and the presence of motor fluctuations and pain (Table 1). Patients with LID had a higher score on the PDQ‐39SI in all visits (p < 0.005) and at V0 LID was independently associated with a greater score on the PDQ‐39SI (β = 0.073; 95% CI, 0.274–4.534, p = 0.027; R 2 = 0.62) (Table 2).

TABLE 1 Factors associated with the presence of LID at baseline (V0) in the COPPADIS cohort (N = 672).
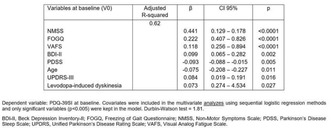
TABLE 2 Effect of LID (levodopa‐induced dyskinesia) on quality of life after adjustment to other covariates at baseline (V0) in the COPPADIS cohort (N = 672).
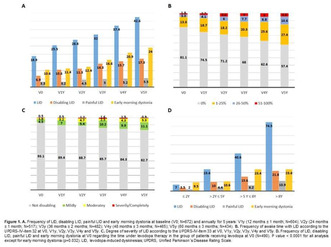
Conclusion: LID are frequent in PD patients. A higher dose of levodopa and lower weight were factors associated to LID. LID impact on QoL.
Disclosure: The authors report no conflict of interest.
EPO‐560
Effects of sensory modulation on balance control, a preliminary study with healthy individuals and chronic stroke
R. Chang; L. Chou
National Yang Ming Chiao Tung University
Background and Aims: Individuals with sensory deficits rely on feedforward control for better motor performance. Additional sensory afferent input can induce feedforward control. EEG event‐related synchronization/desynchronization (ERD/ERS) and theta‐gamma coupling are thought to be related to feedforward control. This study aims to determine if sensory afferent input induced by local vibration (sensory modulation) induces feedforward control.
Methods: Participants underwent a sensory modulation experiment and placebo experiment in random order. Participants first received 30 s of high‐frequency vibration stimulation on the dominant foot's tibialis anterior muscle, then received balance assessment and training (five rounds total). The placebo condition used sham vibration. The Balance Index (Biodex balance system) and EEG (TMSi‐64 channel system) were collected before and after sensory modulation. The EEG data were processed with time‐frequency analysis and the frequency‐profile of theta and gamma bands and ERD/ERS peak values were calculated. Pearson's correlations determined theta‐gamma coupling and two‐way repeated measures ANOVA was used to compare the ERD/ERS between the two conditions. The statistical significant level was set to <0.05.
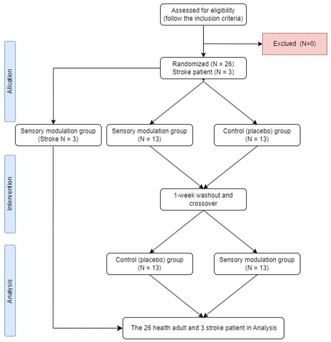
The study flowchart.
Results: Our study with 26 healthy adults found that sensory modulation significantly improved the dynamic balance index (p = 0.004) and induced greater theta gamma phase‐amplitude coupling in the motor cortex (r = 0.9; p < 0.001). Our results also found that the gamma ERD in the sensory modulation condition was significantly lower, but earlier than the placebo condition (p = 0.013).
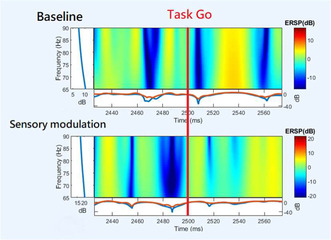
With the intervention of sensory modulation, the sensory modulation group showed greater and earlier event‐relative desynchronization peaks in the time‐frequency analysis of EEG measurements.
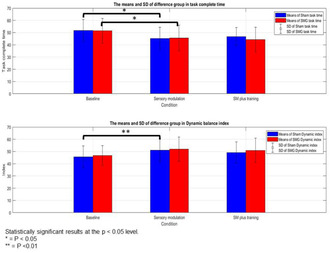
The sensory modulation group and the Sham group showed a significant reduction in task completion time at baseline and after sensory modulation. The sensory modulation group showed a significant increase in balance dynamic index at baseline and after sensitivity.
Conclusion: Our study found that sensory modulation with local vibration can induce feedforward control, and a similar trend was also observed in stroke patients.
Disclosure: Nothing to disclose.
EPO‐561
The use of opicapone for motor fluctuations in Parkinson: Real‐life experience of two Italian Movement Disorders Centers
M. Liccari 1; R. Bacchin2; M. Catalan1; M. Malaguti2; L. Antonutti1; B. Giometto2; P. Manganotti1
1Clinical Unit of Neurology, Department of Medicine, Surgery and Health Sciences, University Hospital of Trieste ASUGI, University of Trieste, Trieste, Italy; 2Clinical Unit of Neurology, Department of Emergency, Santa Chiara Hospital, Azienda Provinciale per i Servizi Sanitari (APSS), Trento, Italy
Background and Aims: Opicapone (OPC) is used as add‐on to L‐Dopa (LD) therapy for management of motor fluctuations (MFs) in Parkinson's disease (PD). Its benefit on PD population has been established by different clinical trials, and a recent post‐hoc analysis has demonstrated its better tolerability when used early in iPD. Data are missing about the use of OPC on Italian population of PD patients, so the aim of this paper is to report the real‐life experience of the two Centers of Trieste and Trento.
Methods: Retrospective data have been gathered of Italian PD patients followed for at least two years after OPC introduction for MFs.
Results: 152 patients have been enrolled, 35% reported adverse events (AEs) on the two‐year follow‐up. 27% discontinued OPC because of a severe AE, which in 76% of cases was a dopamine‐related AE. Univariate analysis recognized as clinical predictors of treatment discontinuation because of any AE were age, disease duration, MFs duration, Hoehn‐Yahr stage, past history of hallucinations or addictive behaviour, mild cognitive complaint, falls, and for treatment discontinuation due to dopamine‐related AE were age, MFs duration, Hoehn‐Yahr, previous addictive behaviour, MCI, and falls. Predictors of OPC withdrawn accordingly to multivariate were MFs duration and Hoehn‐Yahr.
Conclusion: Real‐life data on Italian PD population confirm good tolerability and safety of OPC for the treatment of MFs, moreover when introduced early according to disease course and LD treatment pathway. MFs duration and Hoehn‐Yahr stage have been shown to be important predictors of OPC therapy maintenance over a follow‐up of at least 2 years.
Disclosure: Nothing to disclose.
EPO‐562
Clinical correlates of iron deposition within subcortical nuclei in early drug‐naïve Parkinson's disease patients
M. D'Anna 1; R. De Micco1; N. Piramide1; F. Di Nardo1; M. Pirozzi1; M. Siciliano2; G. Tedeschi1; F. Esposito1; A. Tessitore1
1Department of Advanced Medical and Surgical Sciences, University of Campania “Luigi Vanvitelli”, Napoli, Italy; 2Neuropsychology Laboratory, Department of Psychology, University of Campania “Luigi Vanvitelli”, Caserta, Italy
Background and Aims: Iron deposition using Quantitative Susceptibility Mapping (QSM) has been reported in patients with Parkinson's disease (PD)1. We explored the association between 3TMRI‐derived iron deposition content within 12 bilateral subcortical nuclei and several motor, nonmotor and neuropsychological features in a cohort of 58 early drug‐naïve PD patients.
Methods: Disease severity was assessed by UPDRS‐III, nonmotor symptoms by Nonmotor symptoms scale (NMSS), autonomic dysfunction by Scale for Outcomes in Parkinson's disease for Autonomic symptoms (SCOPA‐AUT), behavioral symptoms by Beck Depression Inventory (BDI‐II), Parkinson Anxiety Scale (PAS) and Apathy Evaluation scale (AES). An extensive neuropsychological assessment was acquired and a z‐score for each cognitive domain was calculated. QSM values were extracted from 12 bilateral subcortical nuclei by applying the HybraPD atlas2. A partial correlation analysis was run between MRI and clinical data.
Results: We found significant correlations between the iron content within bilateral dentate nuclei and UPDRS‐III scores; left externus globus pallidus/right red nucleus and AES scores; left subthalamic nucleus/externus globus pallidus and z‐score executive; bilateral putamina/right externus globus pallidus and z‐score attention; left substantia nigra (pars reticulate) and PAS scores; right substantia nigra (pars compacta) and BDI‐II scores; right red nucleus and several thalamic subregions and SCOPA‐AUT scores.
Conclusion: The presence of specific clinical features is associated with increased iron deposition within different subcortical nuclei in PD patients in the early stages. These findings may be associated with a more severe clinical picture at baseline and may potentially lead to more rapid worsening over time.
Disclosure: The Authors have no disclosures.
EPO‐563
Subacute cerebellar ataxia: Always look for malignancy: A case report
C. Martin de la Morena1; M. Gómez Dunlop1; E. Gamo González1; R. Martín García1; S. Novo Ponte1; P. Sánchez Alonso1; P. Rábano Suárez 2
1Hospital Puerta de Hierro de Majadahonda, Madrid, Spain; 2Hospital Doce de Octubre, Madrid, Spain
Background and Aims: Intracellular anti‐SOX1 antibodies are associated with several neurological síndromes. Lambert‐Eaton syndrome and subacute cerebellar degeneration (CD) are the most frequent. Almost all cases are paraneoplastic, and small cell lung carcinoma (SCLC) is the most frequently detected malignancy.
Methods: Case description.
Results: We present the case of a 62‐year‐old male patient, ex‐smoker, with mild active alcohol intake, who seeked neurology consultation for a 9‐month progressive gait and speech disorder. On neurological examination, he had moderate dysarthria, hypermetric saccades on horizontal plane, mild bilateral dysmetria, and severe gait ataxia, requiring constant bilateral support. There was no cognitive impairment. On further questioning, he had lost 10 kg during that period. He was diagnosed with subacute cerebellar degeneration. Brain magnetic resonance showed mild cerebellar atrophy, possibly related to chronic alcohol intake. Focusing on treatable causes, lumbar puncture revealed normal CSF cell count, glucose and proteins, but positive anti‐SOX1 antibodies were found in serum and CSF (confirmed with indirect immunofluorescence and Western Blot). Electromiography showed no evidence of Lambert‐Eaton. Seeking for occult malignancy, a carinal adenopathy was found on PET‐CT scan and a biopsy revealed a SCLC stage III. Three months after chemotherapy and 2 cycles of immunoglobulins, his neurological condition has mildly improved, now being able to walk with one support.
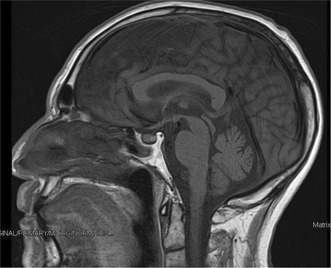
IMAGE 1 Mild cerebellar atrophy in MRI.
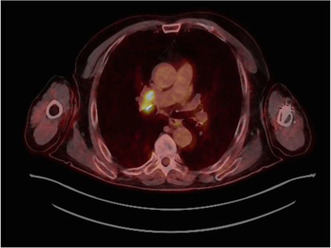
IMAGE 2 A pathological carinal adenopathy is found in PET‐CT scan.
Conclusion: Subacute cerebellar degeneration has some treatable causes. When anti‐SOX1 antibodies are found, search for malignancy is a must. Knowledge of paraneoplastic neurological syndromes can improve cancer detection and treatment.
Disclosure: None.
EPO‐564
Effectiveness of a multidisciplinary approach to prevent falls and gait impairment in patients with Parkinson's disease
E. Cubo 1; A. Garcia‐Bustillo2; J. Ramirez‐Sanz2; J. Garrido‐Labrador2; A. Olivares‐Gil2; F. valiñas‐Sieiro1; M. Allende‐Rio1; J. Trejo1; s. calvo1; J. Diez‐Pastor2; D. Garcia‐Garcia2; A. Arnaiz Gonzalez2
1Neurology Department, Hospital Universitario Burgos, Spain; 2University of Burgos
Background and Aims: Managing Parkinson's disease (PD) requires a multidisciplinary approach to address the diverse needs of patients. We aimed to study the short and long‐term effectiveness of a multidisciplinary telemedicine program in addition to in‐office usual care in non‐demented patients with PD at risk for falling.
Methods: Longitudinal, randomized, case‐control study. All participants in the office were evaluated at baseline, four, and eight months (V0, V1, and V2). Patients included in the telemedicine program received additional multidisciplinary care with nurse, neurologist, and occupational therapist interventions from V0 to V1. The severity of motor, non‐motor symptoms, and quality of life were compared at each visit.
Results: Fifty patients were included, 25 patients [telemedicine program, 48% males, mean age of 71.1 ± 9.0 years, median number of falls (last month) of 1.0 (IQR: 0.0; 1.5)] and 25 patients [control group, 52% males, mean age of 69.2 ± 9.4 years, median number of falls (last month) of 1.0 (IQR: 0.0; 2.0)]. When both groups were compared, in the telemedicine group, apathy, and depression symptomatology, freezing of gait and balance were improved at V1 compared to V0 (all p values < 0.0001), and freezing of gait and balance at V2. In post‐hoc analyses, quality of life improvement was correlated with improvement in depression in the telemedicine group.
Conclusion: By leveraging multidisciplinary telemedicine interventions in addition to in‐office visits, healthcare providers can deliver patient‐centric care, improving non‐motor symptoms and gait impairment in PD. These hybrid interventions could solve current barriers to health systems with limited capacity.
Disclosure: This work was supported by the project PI19/00670 of the Ministerio de Ciencia, Innovación y Universidades, Instituto de Salud Carlos III, Spain.
EPO‐565
Reduced glucocerebrosidase activity in patients with sporadic Parkinson's disease
A. Mili; S. Naija; A. Rekik; E. Jarrar; K. Jemai; A. Hassine; S. Ben Amor
Department of Neurology, Sahloul Hospital, Sousse, Tunisia
Background and Aims: The pathogenesis of sporadic Parkinson's disease (PD) is thought to be resulting from a complex interplay between genetic and environmental factors. While GBA1 mutation is a confirmed risk factor of PD, little is known about glucocerebrosidase (Gcase) activity in sporadic PD. Our work aims to measure the Gcase activity in sporadic PD patients and matched healthy controls and identify any clinical or biological correlation with disease severity.
Methods: Flow cytometry was used to measure lysosomal Gcase activity in lymphocytes from 50 sporadic PD patients and 50 age/gender‐matched healthy controls. All participants underwent a neurological examination, including a motor severity assessment by MDS‐UPDRS score and modified Hoehn and Yahr scale (H&Y), along with a measure of blood glucose and lipids.
Results: Gcase activity was significantly reduced in PD group (6.84 nmol/h/mg ± 4.16 vs 16.06 ± 5.9; p = 0.013; OR = 2.13). Within PD group, lower Gcase activity was correlated with age >65 (p = 0.049; OR = 1.27) and PD onset before 50 (p = 0.046; OR = 1.49). Enzymatic activity was not correlated to the other studied variables: Sex, BMI, PD duration, MDS‐UPDRS score, H&Y stage, glucose and lipids levels (p > 0.05).
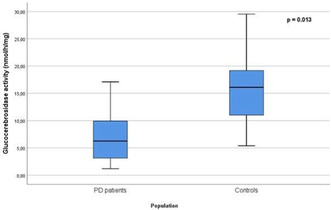
Glucocerebrosidase activity in PD patients and controls.
Conclusion: Our study revealed a reduced glucocerebrosidase activity in patients with sporadic PD but did not find a correlation with its severity. Larger sample studies are needed to corroborate these findings. If confirmed, it could be a step towards the first biomarker for PD.
Disclosure: Nothing to disclose.
EPO‐566
Effect of fecal microbiota transplantation on clinical symptoms of Parkinson disease – A pilot study
M. Figura 1; Ł. Milanowski1; J. Nowak2; A. Antoniak2; M. Kopczyński2; K. Sadowski2; W. Zając2; D. Koziorowski1
1Department of Neurology, Faculty of Health Science, Medical University of Warsaw, Warsaw, Poland; 2Student Scientific Group “Nekon” by the Department of Neurology, Faculty of Health Science, Medical University of Warsaw, Warsaw, Poland
Background and Aims: The gastroenteric tract is involved in the pathogenesis of Parkinson's disease (PD) from its early, premotor stage. Gut bacteria may play a role in the pathogenesis and progression of PD. The aim of the study is to assess the impact of Fecal Microbiota Transplantation (FMT) on clinical symptoms of PD.
Methods: 25 patients with a diagnosis of PD were included in the analysis. Patients were randomly assigned to two groups: FMT from healthy donor or identically looking placebo produced from the patients’ stool. Patients and clinicians were blinded to group allocation. FMT/placebo were administered into the distal part of the small intestine via colonoscopy. Patients underwent clinical assessments before and 1, 3, 6 and 12 months after the procedure (v0, v1, v3, v6 and v12 respectively). UPDRS I‐IV, EQ5D, Constipation Assessment Scale (CAS), PDQ‐39, NMSS, Gastrointestinal Dysfunction Scale for PD (GIDS‐PD) were performed. Levodopa equivalent daily dose (LEDD) was calculated for each visit. Statistical analysis was performed with R version 4.1.2.
Results: Significant differences in LEDD between visits v1‐3 after the procedure (p = 0.003) and difference in EQ5D between v1‐3, v1‐12 and v0‐12 (p < 0.05) were observed. CAS and GIDS‐constipation subscale varied significantly between v0‐12 (p < 0.05). Significant differences were observed between V1 and 3 in several subscales of NMSS, particularly assessing psychiatric symptoms. No significant change in UPDRS III in the “off” state was observed.
Conclusion: FMT may influence clinical picture of PD, especially regarding its non‐motor symptoms. Results suggest that the impact of the procedure diminishes with time, so repeated interventions could be considered.
Disclosure: Nothing to disclose.
EPO‐567
Long‐term monitoring of copper metabolism parameters during treatment in patients with Wilson's disease
M. Misztal 1; A. Członkowska1; A. Wiśniewska2
1Second Department of Neurology, Institute of Psychiatry and Neurology, Warsaw, Poland; 2Department of Genetics, Institute of Psychiatry and Neurology, Warsaw, Poland
Background and Aims: In Wilson's disease (WD), therapy aims to achieve homeostasis of copper metabolism and prevent excessive copper accumulation and deficiency. WD patients require lifelong treatment and regular monitoring of copper metabolism parameters.
Methods: This retrospective study is based on medical records collected from patients diagnosed with WD from the 1970s to 2022. The study groups included compliant patients, 237 treated with D‐penicillamine (DPA) (89 hepatic, 120 neurological, 28 asymptomatic) and 228 with zinc sulfate (ZS) (94 hepatic, 70 neurological and 64 asymptomatic). The daily urinary copper excretion (UCE), serum copper and ceruloplasmin concentrations were analysed before and during long‐term treatment.
Results: A significant decrease in serum copper and ceruloplasmin is observed during the first year of therapy, regardless of medication type. These parameters stabilise in the following years, but a slight increase occurs after ten years. A greater decline is obtained in the neurological form than in the hepatic and asymptomatic. The pattern of UCE differs in the DPA group, with a significant increase within half a year of starting treatment. In the ZS group, the trend is similar to the other copper metabolism parameters.
Conclusion: The copper metabolism parameters reach optimal values in the first year of treatment and then stabilise. The decrease in serum copper leads to decreased ceruloplasmin, which can increase during long‐term therapy improving liver functions. Patients with a neurological form are more prone to excessive decopperization. The obtained ranges of copper metabolism results may contribute to developing optimal long‐term monitoring of WD patients.
Disclosure: Nothing to disclose.
EPO‐568
Correlations between CSF biomarkers of AD, neuropsychological tests and UPDRS‐III in a cohort of PD patients
F. Musso 1; A. Cimmino1; A. Scalese1; G. Giuffrè2; M. Petracca2; A. Bentivoglio2; P. Calabresi2; G. Di Lazzaro2
1Sezione di Neurologia, Dipartimento di Neuroscienze, Facoltà di Medicina e Chirurgia, Università Cattolica del Sacro Cuore, Roma, Italy; 2Neurologia, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Roma, Italy
Background and Aims: Cerebrospinal fluid (CSF) biomarkers for biological diagnosis of Parkinson's Disease (PD) are lacking a wide clinical application. CSF biomarkers of amyloidopathy, tauopathy and neurodegeneration have been used in the last decades to measure Alzheimer's disease (AD) pathology in vivo and as a predictor of cognitive impairment in AD and have been proven to predict cognitive decline in PD as well. The objective is to assess the correlations between CSF biomarkers of AD pathology and cognitive/motor impairment in a cohort of PD patients.
Methods: We recruited 89 subjects with a diagnosis of PD. A lumbar puncture was performed and AD CSF biomarkers were quantified. When lumbar puncture was done, neuropsychological battery and UPDRS‐III were performed. Correlations between CSF biomarkers, neuropsychological tests and UPDRS‐III at the time of lumbar puncture and at last follow‐up were carried out.
Results: Our results revealed a statistically significant correlation between biomarkers of amyloidopathy (Aβ42 and Aβ42/40) and poorer performances in MMSE, RAVLT delayed recall, Spatial Span, Raven matrices, MFTC, semantic verbal fluency, ROCF delayed recall. Interestingly, t‐tau and p‐tau levels were found to predict the % change between the UPDRS‐III score at the baseline and follow‐up, also when corrected with follow‐up duration, LEDD and baseline UPDRS score.
Conclusion: This study highlighted how biomarkers of amyloidopathy can predict worse performances in some common neuropsychological tests. Furthermore, tau species showed potential in identifying PD patients at risk of accelerated motor decline, suggesting a possible synergistic role of tau with alpha‐synuclein in the clinical progression of Parkinson's disease.
Disclosure: Nothing to disclose.
EPO‐569
Contribution to efficacy by active metabolites of suvecaltamide in a preclinical rat model of essential tremor
N. Shanks 1; S. Markova1; R. Mukkavilli2; L. Tan1; M. Lee1; E. Brigham1
1Jazz Pharmaceuticals, Palo Alto, CA, USA; 2Jazz Pharmaceuticals, Philadelphia, PA, USA
Background and Aims: Suvecaltamide (JZP385), a potent, selective T‐type calcium channel modulator, reduced the functional impact of essential tremor (ET) in a phase 2 trial (NCT03101241). We present the pharmacokinetic/pharmacodynamic (PK/PD) relationship and contribution to anti‐tremor efficacy in a harmaline‐induced rat ET model for suvecaltamide and its active metabolites (JZZ05000034 = M01, JZZ05000035 = M02).
Methods: Tremor was quantified using piezoelectric signals in rats receiving harmaline (15 mg/kg, intraperitoneal) 1 hour before single oral doses of suvecaltamide or its metabolites (analytes). Plasma and brain analyte concentrations were measured in satellite experiments following harmaline and analyte administration.
Results: Suvecaltamide dose‐dependently suppressed existing tremor when administered post‐harmaline, with significant effects at ≥1 mg/kg. Tremor reduction was rapid and sustained during 4‐hour recordings. All analytes were measurable in plasma and brain. While suvecaltamide concentrations peaked early and then decreased, active metabolite concentrations were more sustained over the experimental period. When dosed directly, both metabolites reduced tremor at plasma concentrations consistent with those achieved after suvecaltamide administration. Plasma suvecaltamide, M01, and M02 concentrations at 1 mg/kg were consistent with those achieved at steady state in humans at projected therapeutic doses. We characterized the PK/PD relationship of the suvecaltamide total active moiety in rats and utilized CaV3 potency and unbound plasma concentrations to translate to humans.
Conclusion: These results illustrate contributions to efficacy by active suvecaltamide metabolites in rats, which must be considered clinically given they are predicted to translate to human efficacy. These data support continued clinical development of suvecaltamide for adults with moderate‐to‐severe ET (NCT05122650) or residual Parkinson's disease tremor (NCT05642442).
Disclosure: Supported by Jazz Pharmaceuticals. All authors are full‐time employees of Jazz Pharmaceuticals who, during this employment, have received stock options exercisable for, and other stock awards of, ordinary shares of Jazz Pharmaceuticals, plc.
EPO‐570
Cerebellar ataxia in mitochondrial pathology: Review based on a case series
N. Blanco Sanromán 1; G. Olmedo Saura2; M. Domine1; M. Coronel Coronel1; L. Querol Gutierrez3; I. Ruiz Barrio2; S. Bernal Nogueral4; J. Kulisevsky2; M. Olivé3; J. Pérez Pérez2
1Neurology Department, Hospital de la Santa Creu i Sant Pau, Barcelona; 2Movement Disorders Unit, Neurology Department, Hospital de la Santa Creu i Sant Pau, Barcelona; 3Neuromuscular Diseases Unit, Neurology Department, Hospital de la Santa Creu i Sant Pau; 4Genetics Department, Hospital de la Santa Creu i Sant Pau
Background and Aims: Cerebellar involvement in mitochondrial pathology is under‐recognized, especially when it manifests as the initial symptom without a family history of such conditions. This study aimed to characterize the casuistry and clinical features of patients presenting with cerebellar ataxia due to mitochondrial pathology.
Methods: A descriptive, retrospective, single‐center study was conducted on patients assessed in the ataxia unit of a tertiary hospital over five years. Patients diagnosed with mitochondrial cerebellar ataxia (CAM) were included, and demographic, clinical, and neuroimaging data were examined.
Results: Out of 221 patients, six were diagnosed with CAM (prevalence 2.7%). The average onset age was 48.3 years, with a diagnostic delay of 11.7 years. None had a family history of mitochondrial pathology, although two had history of deafness and diabetes. All patients presented with ataxia, scanning dysarthria and oculomotor impairment: ophthalmoparesis (cases 1, 2, 3, 5), gaze‐evoked nystagmus (4). Other common clinical features included reduced visual acuity due to optic atrophy (4, 5, 6), sensory‐motor polyneuropathy (2, 3, 4, 5, 6), myopathy (1, 2, 3) and spasticity (4), alongside other neurological manifestations such as stroke‐like episodes (1), generalized epilepsy (1, 3, 5), chorea (3) and pes cavus (5, 6). Systemic symptoms included diabetes, early‐onset hearing loss, and dilated cardiomyopathy. MRI findings reflected predominantly cerebellar atrophy or vermian volume loss. Genetic mutations were identified in genes including MT‐TL1 (cases 1, 2), POLG (3) OPA1 (4), and TSFM (5, 6).
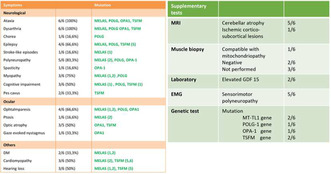
Clinical characteristics and supplementary studies results.
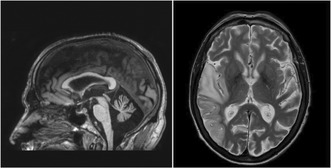
MRI‐ (A) T1‐sagittal (B) T2‐ axial.
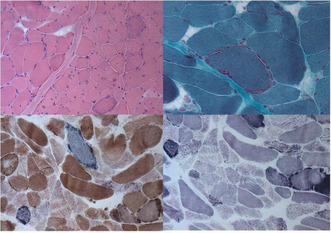
Muscle biopsy‐ (A) Hematoxylin‐eosin (B) Gomori trichrome stain (C) COX (D) SDH.
Conclusion: Mitochondrial etiology should be considered in the differential diagnosis of late‐onset cerebellar ataxias, even in the absence of family history. Recognizing associated symptoms could aid the diagnosis, with implications for prognosis, therapy, and genetic counseling.
Disclosure: Nothing to disclose.
EPO‐571
Wearable sensor detects early morning bradykinesia (EMB): From Parkinson's watch to bedside
P. Gómez López 1; L. Neumaier2; M. Qamar3; L. Batzu3; K. Ray Chaudhuri3
1Neurology Department, Hospital Universitario Virgen del Rocio, Sevilla, Spain; 2Parkinson‐Klinik Ortenau, Wolfach, Germany; 3Institute of Psychiatry, Psychology & Neuroscience at King's College and Parkinson Foundation International Centre of Excellence at King's College Hospital, London, UK
Background and Aims: Early Morning Bradykinesia (EMB) is clinically noted as early morning off (EMO) period which presents with motor and a range of non‐motor symptoms (Rizos et al 2014) often undetected in clinical practice with a negative effect on quality of life in Parkinson's disease (PD). Continuous objective monitoring using the PD validated Personal KinetiGraph (PKG) can detect EMB in clinically unrecognized cases.
Methods: We report interrater reliability of detecting EMB using PKG criteria from two blinded who visually identify EMB from PKG reports and commented on severity (moderate or severe).
Results: A total of 100 PKG reports of PwP were analyzed (63% female and 37% male, median Hoehn and Yahr (HY) score 2–3), mean disease duration 9.4 years (±7.1), mean levodopa equivalent daily dose 633.98 mg (±558.24). EMB was observed in 73% PD and was reported as moderate in 64.3%, severe in 35.6%. Cohen‘s Kappa Interrater reliability score was 0.71 (substantial) for EMB diagnosis and 0.51 (moderate) for severity. No statistical significant correlations were found between EMB and motor scales.
Conclusion: PKG is an objective measurement device with a good interrater reliability for the identification of EMB and its severity. Our findings provide important evidence of the use of PKG for nocturnal monitoring in PD.
Disclosure: All authors report no conflict of interest.
EPO‐572
Elevation of alpha‐fetoprotein in patients with dystonia
P. Havrankova 1; L. Kunc1; J. Roth1; J. Rajmonová1; M. Zech2; R. Jech1
1Department of Neurology and Centre of Clinical Neuroscience, First Faculty of Medicine and General University Hospital in Prague, Charles University in Prague, Prague, Czechia; 2Institute of Neurogenomics, Helmholtz Zentrum München, Munich, Germany Institute of Human Genetics, Technical University of Munich, Munich, Germany Institute for Advanced Study, Technical University of Munich, Garching, Germany
Background and Aims: Alpha‐fetoprotein (AFP) is a glycoprotein produced by the liver, and it is a tumor marker. Elevated levels are nevertheless associated with ataxia telangiectasia (AT), caused by a mutation in the ATM gene. The variant form of AT usually manifests in adolescence or adulthood, dystonia may be the only symptom. Telangiectasia and other symptoms of classic AT may be absent. Therefore, AFP seems to be an important biomarker in patients with dystonia. A screening study was conducted to determine the incidence of alpha‐fetoprotein elevation in patients with dystonia.
Methods: Patients with dystonia occurred before the age of 50 years, were included. Alpha‐fetoprotein levels were examined on an Atellica IM analyzer, with normal levels in the range of 0–8 ng/ml. Whole exome sequencing (WES) was performed in patients with elevated AFP levels.
Results: A total of 167 patients (48 men) were included, mean age of 56.5 years (±10 years). Elevated AFP levels (8.1–96.7 ng/ml) were detected in 14 (8.3%) patients (2 men), mean age 61.8 years (±12 years). In patients with elevated AFP levels, neither ATM nor any other mutation was detected in WES. The incidence of elevated AFP levels for the Atellica IM analyzer is 1.6% in the healthy population.
Conclusion: Elevated AFP levels with negative results in WES were present in a higher number of patients than it corresponds to the healthy population. This is a result that should be confirmed/refuted by further studies. AFP should be considered as a new biomarker in dystonia patients.
Disclosure: Nothing to disclose.
MS and related disorders 5
EPO‐573
Benefits of early highly effective vs escalation treatment in relapsing MS estimated using a treatment‐sequence model
I. Smets 1; M. Versteegh2; S. Huygens2; B. Wokke1; J. Smolders1
1MS Centre ErasMS, Department of Neurology, Erasmus Medical Center, Rotterdam, The Netherlands; 2Huygens & Versteegh, Zwijndrecht, The Netherlands
Background and Aims: Uncertainty about disproportionate impact on healthcare budgets limits implementation of early highly effective treatment (EHT) in multiple sclerosis (MS). Therefore, it is necessary to estimate cost‐effectiveness of escalation vs. EHT disease‐modifying treatment (DMT) sequences.
Methods: Using a health‐economic approach, we analyzed health benefits (relapse rate reduction, disability prevention), direct/indirect DMT and societal costs of escalation vs. EHT DMT sequences. In scenario analyses, we allowed (1) earlier use of alemtuzumab and (2) a single retreatment with cladribine.
Results: In our model, we showed that the ratio between costs and quality‐adjusted life years for the most cost‐effective EHT and escalation sequence results into a similar net health benefit with higher costs but also higher QALYs associated with an EHT vs escalation strategy. Earlier use of alemtuzumab is more cost‐effective than in later lines, even when aggravating the impact of its side effects tenfold. Retreatment with cladribine was more cost‐effective in both escalation and EHT sequences.
Conclusion: Certain EHT sequences are equally cost‐effective to escalation sequences and are likely to result in more health at uncertain additional costs. The favourable cost‐benefit ratio of cladribine and alemtuzumab suggests that a wider application of affordable highly‐effective therapies could promote the cost‐effectiveness both EHT and escalation approaches.
Disclosure: I.S. has received honoraria from Merck, Biogen Idec and Sanofi. B.H.A.W. declares no conflict of interest. S.A.H. and M.M.V. are shareholders of Huygens & Versteegh which conducts research for government organizations and pharmaceutical companies, including research in MS. J.S. received lecture and/or consultancy fee from Biogen, Merck, Novartis, and Sanofi Genzyme.
EPO‐574
Choroid plexus volume as proxy of higher cerebrospinal fluid inflammatory activity in multiple sclerosis
I. Addazio 1; E. Portaccio1; C. Ballerini1; V. Penati1; A. Caporali1; C. Fabbiani2; E. Fainardi2; E. De Meo1; M. Amato1
1Department Neurofarba, Section of Neurosciences, University of Florence, Florence, Italy; 2Department of Experimental and Clinical Biomedical Sciences, Neuroradiology Unit, University of Firenze, AOU Careggi, Firenze, Italy
Background and Aims: In our study, we investigate the hypothesis that Choroid Plexus volume (CPv) enlargement serves as a surrogate marker for heightened inflammatory cerebrospinal fluid (CSF) activity. This last, in turn, contribute to damage gradients observed in the normal‐appearing white matter (NAWM) near the ventricles of patients with relapsing Multiple Sclerosis (MS) at disease onset.
Methods: Our cross‐sectional evaluation involved 108 subjects. Using the nephelometric method and the Reiber formula, we quantified IgM intrathecal synthesis (ITMS) as an inflammatory activity biomarker in CSF. We performed advanced post‐processing MRI analysis, encompassing brain, lesion and choroid plexus (CP) volume assessment. Additionally, we used T1/T2 mapping to evaluate the NAWM damage gradient.
Results: Comparing MRI features between the groups and exploring the link between NAWM damage gradient and CPv, we employed multiple linear regression models. Among the 108 patients subjected to MRI analysis, 32 tested positive for ITMS (ITMS+), while 76 were ITMS‐negative (ITMS‐). Importantly, ITMS+ and ITMS‐ patients exhibited comparable baseline clinical and demographic characteristics. While no significant differences were found in brain and lesion volumes between the two groups, CPv was notably enlarged in the ITMS+ group (beta 0.57, 95% c.i. 0.35–0.79, p < 0.001). Additionally, a significant relationship emerged between the T1/T2 ratio gradient and CPv (beta = 0.46, <0.001).
Conclusion: Our findings suggested a potential role for the CP in influencing NAWM changes. Further research is essential to validate this hypothesis and identify specific CSF biomarkers associated with CPv and NAWM damage.
Disclosure: E.P. received funding from Biogen, Merck, Sanofi, Novartis. M.P.A received funding from Biogen Idec, Merck Serono, Bayer Schering and Sanofi. E.D.M., I.A., C.B., V.P., A.C., C.F., E.F., report no disclosures.
EPO‐575
Demographic, clinical and serum parameters for the prediction of apheresis outcome in the steroid‐refractory MS relapse
I. Vardakas; J. Dorst; A. Huss; T. Fangerau; D. Taranu; H. Tumani; M. Senel
Department of Neurology, University of Ulm, Ulm, Germany
Background and Aims: The optimal treatment strategy for steroid‐refractory MS relapses remains unclear. We investigated the predictive power of multiple serum parameters, demographic and clinical data on apheresis outcome.
Methods: We examined sera of 38 participants of the IAPEMS‐trial (randomized‐controlled trial to evaluate the safety and efficacy of immunoadsorption versus therapeutic plasma exchange in steroid refractory MS relapses, NCT02671682) and conducted statistical analysis using serum parameters, demographic and clinical trial data. We classified apheresis outcome assessing the improvement of the affected functional system score four weeks after the procedure.
Results: In binary logistic regression analysis younger age (OR 0.948, 95% CI 0.903–0.995, p = 0.03) and lower sGFAP concentrations (RR 0.948, 95% CI 0.903 –0.995, p = 0.03) were associated with a favorable relapse outcome. In addition, we observed a strong trend towards a positive apheresis outcome with higher sNfL (RR 1.413, 95% CI 0.965–2.069, p = 0.08). Further analysis of our data showed no predictive power for further serum parameters (immunoglobulins, immunoglobulin free light chains, CXCL13, CXCL12, BCMA, BAFF), Symbol Digit Modalities Test (SDMT) and optical coherence tomography (OCT) measures in our study.
Conclusion: In line with published data, our study confirmed that patients with younger age and lower serum GFAP levels are more likely to benefit from apheresis. The potential predictive value of sNfL needs to be investigated in further prospective studies.
Disclosure: None of the authors have any disclosure related to this study.
EPO‐576
Real‐life efficacy and safety of ofatumumab for highly active multiple sclerosis: The San Raffaele Hospital experience
I. Gattuso 1; S. Guerrieri1; A. Genchi1; A. Nozzolillo1; C. Zanetta1; T. Zaccone1; M. Martire1; L. Ferrè1; F. Esposito1; M. Rocca2; M. Filippi3; L. Moiola1
1Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; Vita‐Salute San Raffaele University, Milan, Italy; 3Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; Vita‐Salute San Raffaele University, Milan, Italy; Neurophysiology Service
Background and Aims: Ofatumumab is a highly effective treatment for multiple sclerosis (MS), approved in Europe in April 2021. Post‐marketing information is still limited. We report our real‐life experience (San Raffaele Hospital MS cohort, Milan, Italy).
Methods: Data from MS patients receiving ofatumumab for at least 1 year were obtained: clinical information, neuroradiological examinations and lymphocyte subsets values were collected.
Results: Among 100 MS patients receiving ofatumumab, 37 were treated for at least 1 year (33 relapsing‐remitting‐RRMS; 4 relapsing‐RMS; mean age 38.42 ± 10.6 years; 27 females, 10 males; mean disease duration 8.77 years – range 0.5–31.9; median EDSS 2.0 – range 0–8.0; 15/37 treatment‐naïve; mean follow up 1.16 years – range 1.00–1.78). During the year before treatment start 35/37 patients showed MRI activity (2/37 shifted from Natalizumab for safety reasons), while 27/37 also experienced relapses. While treated with ofatumumab, no patients showed further relapses, while only 3/37 had persistent MRI activity (3/3 at rebaseline examination 6 months after treatment start, none with Gd‐enhancing lesions). CD19+ lymphocyte count was available at 3 months in 24/37 participants: all patients showed B cells depletion (i.e. <0.5% – mean 0.09% – range 0.0–0.33%), with persistence at 1 year. Treatment was well tolerated, with no serious adverse event: 31/37 patients reported fever after first injection, while only 3/37 after titration; 5/37 patients presented mild‐to‐moderate upper respiratory tract infections. No pregnancy occurred.
Conclusion: Our short‐term data suggest ofatumumab is effective, safe and well tolerated in MS. Long‐term follow‐up and larger cohorts are needed to confirm our observations.
Disclosure: LM received compensations for speaking activities and/or for participating to advisory board from Merck, Celgene, Biogen, Sanofi, Novartis, Roche, Alexion. FM received compensation for consulting services from Alexion, Almirall, Biogen, Merck, Novartis, Roche, Sanofi; speaking activities from Bayer, Biogen, Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck‐Serono, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA. MAR received consulting fees from Biogen, Bristol Myers Squibb, Eli Lilly, Janssen, Roche; and speaker honoraria from AstraZaneca, Biogen, Bristol Myers Squibb, Bromatech, Celgene, Genzyme, Horizon Therapeutics Italy, Merck Serono SpA, Novartis, Roche, Sanofi and Teva. FE received compensation from Merck and Biogen. AG received consulting fee from Novartis. CZ received compensation for speaking activities and/or consulting activities from Biogen, Bristol Myers Squibb, Janssen, Roche, Astrazeneca, Sanofi, Merck, Alexion, Novartis. LF received compensation for speaking activities and/or travel from Novartis, Merck, Jannsen. IG, SG, SMM, TZ, have nothing to disclose.
EPO‐577
Patient‐reported fatigue in patients with relapsing multiple sclerosis receiving ocrelizumab: MoOzaRt interim analysis
I. Penner 1; J. Leemhuis2; T. Maier2; E. Weber2; H. Schreiber3
1Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Switzerland; COGITO Center for Applied Neurocognition and Neuropsychological Research, Düsseldorf, Germany; 2Roche Pharma AG, Grenzach‐Wyhlen, Germany; 3Neurological Practice Center, Ulm, Germany
Background and Aims: Fatigue is considered the most common and one of the most debilitating symptoms in multiple sclerosis (MS). MoOzaRt aims to assess the impact of ocrelizumab on patient‐reported long term (trait) and transient (state) fatigue in patients with relapsing forms of MS (RMS) under therapy with ocrelizumab.
Methods: The ongoing non‐interventional study MoOzaRt (ISRCTN55332718) aims to recruit ~740 RMS patients initiating therapy with ocrelizumab from Germany and Switzerland. The primary endpoint is the change in the Fatigue Scale for Motor and Cognitive Functions (FSMC) total score from baseline to month 24, evaluating trait fatigue. Secondary endpoints include changes in state fatigue (Visual Analogue Scale, VAS), in Expanded Disability Status Scale (EDSS) and in safety.
Results: The first interim analysis (data cut off Dec 14, 2023) included 80 patients (72.5% female, mean age 37.5 (SD 9.9) years) with a mean EDSS score of 2.31 (SD 1.39) (table 1). Overall, FSMC total scores remained stable over 12 months (N = 71), while the proportion of patients with severe fatigue decreased markedly from in this period (table 2). VAS scores and detailed patient reported outcomes will be presented at the EAN.
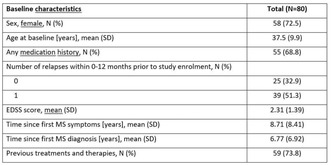
TABLE 1 Baseline characteristics.
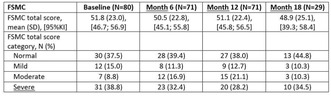
TABLE 2 FSMC scores at baseline and month 6, 12 and 18.
Conclusion: The first interim analysis of the MoOzaRt study revealed stable FSMC total scores with a trend towards a decline in the proportion of patients with severe trait fatigue already during the early treatment phase. Further results will deepen our insights into the specific impact of ocrelizumab on trait and state fatigue and factors that may influence fatigue in RMS patients.
Disclosure: IKP: Almirall, Biogen, BMS, Celgene, Genzyme, Janssen, Merck, Novartis, Roche, Teva // speakers bureau or advisory board, consulting fees; The German MS Society, Celgene, Novartis, Roche, Teva // research grants. JL: Roche // employee TM: Roche // employee EW: Roche // employee HS: Almirall, Biogen, BMS, Genzyme, Janssen, Merck, Novartis, Roche, Teva // speakers bureau or advisory board, consulting fees, travel reimbursement; Biogen, Novartis, Teva // research grants; Biogen, Novartis, Roche // data monitoring or steering committees.
EPO‐578
Updated real world immunogenicity data on Tysabri S.C. and Tysabri I.V.
J. Lizrova Preiningerova 1; E. Kubala Havrdova1; O. Vencourova1; K. White2; Z. Benova3; A. Drenth4
1General University Hospital and First School of Medicine, Charles University, Prague, Czechia; 2Biogen, Cambridge, MA, USA; 3Biogen, Prague, Czechia; 4Biogen, Baar, Switzerland
Background and Aims: Natalizumab (Biogen), approved for relapsing forms of multiple sclerosis, is available in both subcutaneous (SC) and intravenous (IV) formulations, with administration intervals of every four weeks (Q4W) or every six weeks (Q6W) in off‐label use. This study offers a real‐world observational analysis of the immunogenicity, tolerability, and effectiveness of Tysabri administered through both SC and IV methods over a 24‐month period at a single academic center.
Methods: Anti‐natalizumab antibody in serum (NTZ‐Ab, Unilabs, Copenhagen, Denmark) are tested at baseline and at every 3rd administration. All subjects are followed with EDSS, relapse rate, JCV index and yearly brain MRI.
Results: There are 242 patients with mean length of follow up: 20.4 months (0.7–26.7) divided into 4 cohorts based on their treatment pattern: (1) Switch from IV‐Q6W to SC‐Q6W (SC‐Q6W), n = 156; (2) Ongoing IV‐Q6W (IV‐Q6W), n = 38; (3) Treatment‐naïve to IV‐Q4W (IV‐N), n = 13; and (4) Treatment‐naïve to SC‐Q4W (SC‐N), n = 35. We observed three cases of NTZ‐Ab positivity (1.2%). One patient on long term treatment Q6W had NTZ‐Ab+ at the time of switch from IV to SC and thereafter (listed in SC‐Q6W cohort); the treatment was discontinued. Two patients in the SC‐N cohort showed persistent NTZ‐Ab from 3 months on treatment. One of them remains on treatment with no clinical or radiological disease activity despite of persistent NTZ‐Ab+ and one was switched to a different treatment due to radiological activity. There was no new occurrence of NTZ‐Ab later during treatment.
Conclusion: The immunogenic potential of Tysabri is low and NTZ‐Ab occur early.
Disclosure: This study is supported by Biogen. EKH received honoraria/research support from Biogen, Merck Serono, Novartis, Roche, and Teva; has been a member of advisory boards for Actelion, Biogen, Celgene, Merck Serono, Novartis, and Sanofi Genzyme. JLP has received research funding from Biogen and honoraria from Merck Serono, Novartis and Roche. OV has nothing to disclose. KW, ZB, AG, and AD are employees of and may hold stock and/or stock options in Biogen.
EPO‐579
Evaluating association of chronic active lesions with disability in multiple sclerosis: A systematic literature review
F. Bagnato1; M. Mordin2; N. Greene3; S. Mahida2; K. Higuchi4; J. Wingerden 5
1Neuroimaging Unit, Neuroimmunology Division, Department of Neurology, Vanderbilt University Medical Center, Nashville, TN, USA; 2RTI Health Solutions, Research Triangle Park, NC, USA; 3Sanofi, Cambridge, MA, USA; 4Sanofi, Bridgewater, NJ, USA; 5Sanofi, Amsterdam, The Netherlands
Background and Aims: Chronic active lesions (CAL) are important component of multiple sclerosis (MS) disease pathology and indicate the presence of a smoldering neuroinflammatory processes. Yet, only recent advances in magnetic resonance imaging (MRI) and positron emission tomography have made it possible to identify CAL in vivo in people with MS (pwMS). Several studies assessed the association between CAL and disability accumulation in pwMS.
Methods: A systematic literature search was conducted following PRISMA guidelines 2020 using PubMed, Embase, and Cochrane Library on April 21, 2023. The review included studies assessing associations between CAL and clinical/radiological outcome of disability accumulation in people with any MS phenotype.
Results: A total of 149 unique studies were identified and 31 met the inclusion criteria. Of these, 21 evaluated paramagnetic rim lesions (PRL) using susceptibility‐based MRI, 9 evaluated slow expanding lesions (SEL) on T1‐weighted (T1‐w)/T2‐w MRI, and 1 studied both. The presence of PRL was associated with disability accumulation in 19 studies, with 9 of those studies reporting an association between the number or volume of PRL and disability accumulation. SEL were associated with disability accumulation in 10 studies, with 5 of those studies reporting association between the number or volume of SEL and disability accumulation.
Conclusion: This literature review found significant associations between CAL and disability accumulation that may lead to transitioning to progressive disease in pwMS. This illustrates role of CAL and smoldering disease in MS in driving disability accumulation. CAL remains an important unmet therapeutic target and development of treatments promoting their resolution is crucial.
Disclosure: Nothing to disclose.
EPO‐580
EMbrace the diversity in MS with a Value Based Healthcare (VBHC) implementation model in Portugal
J. Cerqueira 2; S. Aguiar3; A. Fontainhas4; A. Pimenta5; A. Morganho3; C. Domingues5; E. Bettencourt5; H. Cardoso4; J. Soares6; L. Leitão7; M. Reis5; M. Santos7; M. Garcia8; R. Silva9; R. Cunha4; R. Araujo5; R. Rolim9; S. Faria9; T. Aguiar3; B. Candeias5; F. Costa1
1NOVA School of Business and Economics, Lisbon, Portugal; 2School of Health Sciences, University of Minho and Unidade Local de Saúde de Braga, Braga, Portugal; 3Neurology Department, Health Service of the Autonomous Region of Madeira – SESARAM, EPERAM; 4Day Hospital Unit, Hospital Prof. Doutor Fernando Fonseca, ULS Amadora/Sintra EPE; 5Roche Farmacêutica Química, Lda, Portugal; 6Pharmaceutical Services, Hospital Prof. Doutor Fernando Fonseca, ULS Amadora/Sintra EPE; 7Neurology Department, Hospital Prof. Doutor Fernando Fonseca, ULS Amadora/Sintra EPE; 8Pharmaceutical Services, Health Service of the Autonomous Region of Madeira – SESARAM, EPERAM; 9Unidade Local de Saúde de Braga, Braga, Portugal
Background and Aims: Managing multiple sclerosis (MS) is challenging, due to its chronic degenerative nature, young patient population, and unpredictability and diversity of its symptoms. In such a setting, adoption of a Value‐based Healthcare (VBHC) approach can increase efficiency and improve care by incorporating patient values and quality of life considerations. This paper outlines the implementation of a VBHC framework in three Portuguese multiple sclerosis centers, with different multidisciplinary teams, as part of the European consensus “S.O.S. MS Project”.
Methods: The Portuguese project (EMbrace), started in March 2021, includes a basic education on VBHC concepts, an analysis and refinement of the patient journey in each center and a prospective longitudinal collection of a standard dataset comprising patient‐reported outcomes. Periodic meetings allow the sharing of experiences and practices. Central to this initiative is the application of a process reengineering methodology to healthcare environments, focusing on five pillars: patient‐centered value, work rhythm, waste‐minimization, definition of value streams, and continuous improvement.
Results: EMBrace resulted in an alignment of clinical pathways, validation of Key Performance Indicators, and benchmarking against international models. Its implementation faced challenges in timing and data collection, highlighting the need for more streamlined processes and the integration of technology. Nevertheless, it demonstrated the feasibility of a VBHC approach in MS care and its potential for more efficient, patient‐centric healthcare models.
Conclusion: The EMbrace Project, still in development, has the potential to significantly influence MS care by providing evidence to guide implementation of VHBC projects.
Disclosure: This project has been supported by ROCHE that facilitated the contact between all the centers, coordinated the meetings and provided know‐how and technical assistance. The authors have no other disclosures relevant to this work.
EPO‐581
8‐Point change in symbol digit modalities test scores: Findings from the phase 3 SUNBEAM and DAYBREAK ozanimod trials
J. DeLuca1; J. Cohen2; B. Cree3; G. Comi4; L. Kappos5; C. Cheng6; J. Sheffield6; J. Riolo6; A. Thorpe 6; R. Benedict7
1Kessler Foundation, West Orange, NJ, USA and Departments of Physical Medicine and Rehabilitation, and Neurology, Rutgers – New Jersey Medical School, Newark, NJ, USA; 2Mellen Center for MS Treatment and Research, Cleveland Clinic, Cleveland, OH, USA; 3Weill Institute for Neurosciences, Department of Neurology, University of California San Francisco, San Francisco, CA, USA; 4Vita‐Salute San Raffaele University and Casa di Cura Igea, Milan, Italy; 5Research Center for Clinical Neuroimmunology and Neuroscience Basel (RC2NB), Departments of Head, Spine and Neuromedicine, Clinical Research, Biomedicine, and Biomedical Engineering, University Hospital and University of Basel, Basel, Switzerland; 6Bristol Myers Squibb, Princeton, NJ, USA; 7Jacobs MS Center, Department of Neurology, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, State University of New York, Buffalo, NY, USA
Background and Aims: In a post hoc analysis of the phase 3 SUNBEAM trial, more ozanimod‐treated participants had clinically meaningful (≥4‐point) improvement on the Symbol Digit Modalities Test (SDMT) than those treated with interferon beta‐1a (IFN). In this analysis, the long‐term effects of ozanimod on cognitive processing speed (CPS) in participants with relapsing multiple sclerosis (RMS) were evaluated using 8‐point SDMT change, which may better represent individual‐level CPS changes than a 4‐point threshold.
Methods: In SUNBEAM (NCT02294058), adults with RMS were randomly assigned oral ozanimod 0.46 or 0.92 mg/d or intramuscular IFN 30 μg/wk for ≥12 months (mean treatment duration 13.5 months); completers were eligible for an ozanimod 0.92 mg open‐label extension (OLE) trial (DAYBREAK, NCT02576717; database lock: 7 April 2023). The percentage of participants with 8‐point SDMT change relative to SUNBEAM baseline is reported.
Results: SUNBEAM participants entering the OLE were included (ozanimod 0.92 mg, n = 397; IFN, n = 395). Mean (SE) baseline SDMT scores were 48.0 (0.69) and 47.4 (0.68), respectively. Compared with participants receiving IFN, those in the ozanimod group were more likely to achieve 8‐point SDMT improvement at SUNBEAM month 12 (nominal p = 0.0048; Figure). After IFN‐randomised participants switched to ozanimod, statistical group differences were no longer apparent (Figure). After 6–8 years of ozanimod (end of OLE), the proportion of participants with 8‐point improvement was numerically, but not nominally significantly, higher in the continuously ozanimod‐treated group compared with those initially randomised to IFN (Figure).
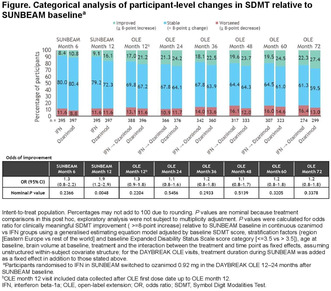
Conclusion: Long‐term ozanimod treatment protects from cognitive deterioration. These data support the early use of ozanimod in patients with RMS.
Disclosure: JD: personal compensation for consulting from Biogen Idec, Bristol Myers Squibb, Janssen Pharmaceuticals, and Novartis; speaker for Consortium of MS Centers; and grant funding from Biogen Idec, Canadian MS Society, Consortium of MS Centers, EMD Serono, and National MS Society. All authors’ disclosures will be included in the presentation. This study was sponsored by Bristol Myers Squibb. Writing and editorial assistance was provided by Noud van Helmond, MD, PhD, of Peloton Advantage, LLC, an OPEN Health company, and was funded by Bristol Myers Squibb.
EPO‐582
Real‐world data on effectiveness and tolerability of Ofatumumab at short‐term follow‐up
J. Arzalluz‐Luque; A. Torres‐Moral; J. Dotor; R. López‐Ruiz; M. Ben‐Yelun; S. Eichau
Department of Neurology, Hospital Universitario Virgen Macarena (Sevilla)
Background and Aims: Ofatumumab is a highly effective disease‐modifying therapy (DMT) for relapsing multiple sclerosis (MS). Real‐world outcome data are needed for clinical practice. Our aim was to describe effectiveness and tolerability at 6 and 12‐month follow‐up.
Methods: Patients diagnosed with MS starting Ofatumumab between December 2022‐December 2023 were included. Baseline demographics, disease characteristics and clinical/radiologic features were collected. Effectiveness/tolerability outcomes were assessed after 6 and 12 months.
Results: We included 43 relapsing MS patients; 29 (67.4%) were women. Mean age was 37.2 ± 10.2 years and disease duration was 10.1 ± 7.9 years. Median baseline EDSS was 3 (range: 0–6). The median number of relapses in the two previous years was 1 (range: 0–4). Last MRI before Ofatumumab showed 5–10 lesions in 11 (25.6%) patients, 10–30 in 20 (46.5%) and >30 in 11 (25.6%); 32 (74.4%) had spinal‐cord lesions. Prior DMT exposure was reported in 31 (72.1%) vs 12 (27.9%) naive patients. Switch to Ofatumumab was mostly due to ineffectiveness (27/31 [87.1%]) vs lack of tolerability/safety (4/31 [12.9%]). There were no discontinuations during a mean follow‐up of 8.6 ± 2.9 months. Only 3 (7%) patients had a relapse, which happened in the first 6 months. At 6‐month and 12‐month follow‐up median EDSS was 2.8 (range: 0–6) and 1.5 (range: 0–6), respectively. Overall, 3/21 (14.3%) had EDSS worsening in the first year and 2/21 (9.5%) had new lesions on rebaseline 6‐month MRI. Adverse events occurred in 30/41 (73.2%) patients, mainly at the first injection (21/30 [70%]); the most common was flu‐like syndrome in 25/30 (83.3%).
Conclusion: Ofatumumab was effective and well‐tolerated in our population. Most patients were stable; few had disease activity early after starting Ofatumumab and were therefore not considered treatment failures. Minor self‐limited tolerability issues were reported.
Disclosure: Nothing to disclose.
EPO‐583
Epstein‐Barr virus DNA in the cerebrospinal fluid of multiple sclerosis patients and controls
J. Lehikoinen 1; K. Nurmi1; M. Ainola1; J. Clancy2; J. Nieminen3; L. Jansson1; H. Vauhkonen4; A. Vaheri4; T. Smura4; S. Laakso3; K. Eklund5; P. Tienari3
1Translational Immunology Research Program, University of Helsinki, Helsinki, Finland; 2Research and Development, Finnish Red Cross Blood Service, Helsinki, Finland; 3Department of Neurology, Neurocenter, Helsinki University Hospital, Helsinki, Finland; 4Department of Virology, Medicum, University of Helsinki, Helsinki, Finland; 5Rheumatology, Helsinki University Hospital, Helsinki, Finland
Background and Aims: Epstein‐Barr virus (EBV) infection is a major risk factor for multiple sclerosis (MS). We examined the presence of EBV DNA in the cerebrospinal fluid (CSF) and blood of MS patients and controls and estimated the proportions of EBV‐positive B cells in CSF and blood.
Methods: CSF was collected at diagnostic lumbar punctures from 45 MS patients and 45 HLA‐DR15 matched controls; all subjects were EBV seropositive. Cellular DNA was amplified and representative samples were obtained in 28 cases and 28 controls. In a subset of participants, non‐amplified DNA from CSF cells and blood B cells were analysed. Multiple droplet digital PCR (ddPCR) runs were performed to assess the cumulative EBV positivity rate.
Results: One of the 45 MS patients and none of the 45 controls was positive for EBV DNA in CSF supernatants. CSF cellular DNA was analysed in eight independent ddPCRs: EBV DNA was detected at least once in 18 (64%) of the 28 MS patients and in 15 (54%) of the 28 controls (p = 0.59, Fisher's test). The cumulative EBV positivity increased up to 59%, suggesting that all subjects would have tested EBV positive, had more DNA been analysed. The estimated proportion of EBV positive B cells was >1/10,000 in both CSF and blood.
Conclusion: EBV‐DNA is equally detectable in the CSF cells of both MS patients and controls with ddPCR, and the probabilistic approach indicates that the true positivity rate approaches 100% in EBV‐positive individuals. The proportion of EBV positive B cells appears higher than previously estimated.
Disclosure: JL: Congress expenses; Merck. SML: Lecture fees Merck, Biogen, Novartis, Janssen, Teva; congress expenses Roche, Merck, Novartis; advisory fees Roche, Novartis, UCB Pharma, Argenx. PJT: Lecture and consulting fees Roche, Merck, Biogen, Novartis, Janssen, Sanofi, Alexion; congress expenses Biogen, Merck. KKE: Lecture fees: Novartis, Celltrion, Sobi. JKN: Congress expenses; Biogen, Novartis, Merck.
EPO‐584
Final analysis of long‐term hepatic safety of ozanimod in an open‐label extension trial of relapsing multiple sclerosis
K. Selmaj1; L. Steinman2; G. Comi3; A. Bar‐Or4; H. Hartung5; X. Montalbán6; E. Havrdová7; J. Sheffield8; A. Thorpe 8; J. Riolo8; A. Krakovich8; C. Cheng8; L. Kappos9; J. Cohen10; B. Cree11
1Center for Neurology, Łódź, Poland, and Collegium Medicum, Department of Neurology, University of Warmia and Mazury, Olsztyn, Poland; 2Department of Neurology and Neurological Sciences, Beckman Center for Molecular Medicine, Stanford University Medical Center, Stanford, CA, USA; 3Vita‐Salute San Raffaele University and Casa di Cura Igea, Milan, Italy; 4Center for Neuroinflammation and Experimental Therapeutics, and Department of Neurology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA; 5Medical Faculty, Heinrich‐Heine University, Düsseldorf, Germany; Brain and Mind Centre, University of Sydney, NSW, Australia; Medical University of Vienna, Vienna, Austria; and Palacký University Olomouc, Olomouc, Czechia; 6Department of Neurology‐Neuroimmunology, Centre d'Esclerosi Múltiple de Catalunya (Cemcat), Hospital Universitari Vall d'Hebron, Barcelona, Spain; 7Department of Neurology and Center for Clinical Neuroscience, First Medical Faculty, Charles University, Prague, Czechia; 8Bristol Myers Squibb, Princeton, NJ, USA; 9Research Center for Clinical Neuroimmunology and Neuroscience Basel (RC2NB), Departments of Head, Spine and Neuromedicine, Clinical Research, Biomedicine, and Biomedical Engineering, University Hospital and University of Basel, Basel, Switzerland; 10Mellen Center for MS Treatment and Research, Cleveland Clinic, Cleveland, OH, USA; 11Weill Institute for Neurosciences, Department of Neurology, University of California San Francisco, San Francisco, CA, USA
Background and Aims: We report long‐term hepatic safety during an open‐label extension study (DAYBREAK) of ozanimod.
Methods: Patients with relapsing multiple sclerosis who completed a phase 1–3 ozanimod trial were eligible for DAYBREAK (NCT02576717), where they received ozanimod 0.92 mg/d. Liver enzymes were measured every 3 months for 3 years, then every 6 months. Database lock: 7 April 2023.
Results: The 2494 patients had a mean (SD) 60.9 (17.9) (range 0.03–81.5) months of ozanimod exposure during DAYBREAK. Alanine aminotransferase (ALT) or aspartate aminotransferase (AST) levels ≥3× upper limit of normal (ULN) or bilirubin >2× ULN were infrequent (<4% each; Table 1); there were no cases of severe drug‐induced liver injury (DILI). Mean (SD) time to onset was 27.3 (17.7) and 30.2 (18.9) months for ALT and AST ≥3× ULN, respectively, and 16.4 (15.8) months for bilirubin >2× ULN. First ALT >1×ULN during DAYBREAK primarily occurred during year 1. Consecutive ALT elevations ≥3× ULN were uncommon (Table 1). Hepatobiliary treatment‐emergent adverse events (TEAEs) occurred in 104 (4.2%) participants (Table 2) and led to treatment discontinuation in 2 (0.08%); 10 (0.4%) discontinued due to hepatic enzyme elevation–related TEAEs. Fifteen (0.6%) patients had serious hepatobiliary TEAEs (Table 3).

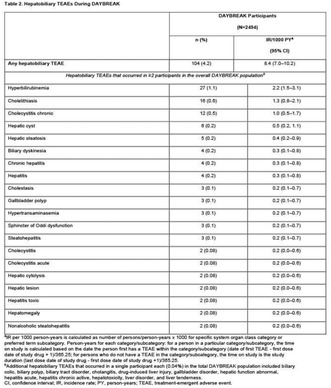
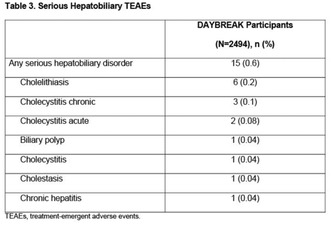
Conclusion: After up to nearly 7 years of ozanimod in DAYBREAK (mean 60.9 months), ALT and AST elevations ≥3× ULN remained infrequent. Severe DILI did not occur in this dataset. Consecutive ALT elevations ≥3× ULN were uncommon. Rates of serious hepatic TEAEs and hepatic TEAEs leading to discontinuation were low. Postmarketing hepatic safety findings are gathered and reported separately.
Disclosure: KWS: Consulting for Biogen, Celgene, Genzyme, Merck, Novartis, Ono Pharma, Roche, Synthon, and Teva. All authors’ disclosures will be included in the presentation. This study was sponsored by Bristol Myers Squibb. Writing and editorial assistance was provided by Noud van Helmond, MD, PhD, of Peloton Advantage, LLC, an OPEN Health company, and was funded by Bristol Myers Squibb.
EPO‐585
Reliability of a digital cohort in multiple sclerosis: The MSCopilot® French patients
L. Carment 1; P. Drouin1; L. Ahamada1; L. Pillet1; A. Plaud1; A. Vives1; S. Zinai1; A. Tourbah2
1Ad Scientiam, Paris, France; 2Université Versailles Saint Quentin en Yvelines, Université Paris Saclay, Service Neurologie, Hôpital Raymond‐Poincaré AP‐HP, Garches
Background and Aims: We describe the feasibility of collecting sociodemographic and functional parameters using MSCopilot®, a clinically validated software as a medical device, and the representativeness of this French digital cohort of patients with multiple sclerosis (PwMS).
Methods: Real world data from the MSCopilot® database were collected between October‐2017 to September‐2023. Adult PwMS who had provided informed consent were included. MSCopilot® was used at home without supervision to collect sociodemographic and treatment self‐reported data and perform the digital active tests that evaluate four functional parameters (walking capacity, low contrast visual acuity, cognitive processing and dexterity).
Results: A total of 1755 PwMS were included with a 2:1 female/male ratio (1204/551), consistent with the French MS population albeit slightly younger (41.1 ± 12 years). The majority of patients self‐reported an EDSS score < 4 (71.4%, average score = 2.3 ± 2). Among the four digital assessments, three revealed significant group differences between patients with EDSS <4 and ≥4, the latter group showing a decreased performance in walking capacity, cognitive function and hand dexterity (p < 0.01).
Conclusion: MSCopilot® enables the characterization of key functional parameters in a real‐life digital cohort mirroring the French MS population sociodemographic parameters. This demonstrates the significance of digital cohorts in providing additional insights for a better understanding of the disease through real world evidence.
Disclosure: L. Carment, P. Drouin, L. Ahamada, A. Plaud, LE. Pillet, A. Vives, S. Zinai are employees of Ad Scientiam, A. Tourbah is a member of its scientific committee and received honoraria for lectures, travel grants and research support from Biocara, Hikma, Novartis, Roche.
EPO‐586
Central vein sign analysis in confluent multiple sclerosis lesions separated with an automated algorithm
L. Marchi 1; M. Pasca1; B. Lambert2; P. Rubini2; S. Doyle2; H. Dehaenne2; A. Tucholka2; P. Roca2; E. Fainardi3; L. Massacesi4
1Department of Neurosciences, Drug and Child Health, University of Florence, Florence, Italy; 2Pixyl Medical, Grenoble, France; 3Neuroradiology Unit, Careggi University Hospital, Florence, Italy; 4Department of Neurology 2 and Tuscan Region Multiple Sclerosis Referral Centre, Careggi University Hospital, Florence, Italy
Background and Aims: The Central Vein Sign (CVS) is an MRI marker that, among demyelinating syndromes, is pathognomonic of multiple sclerosis (MS). However according to the NAIMS guidelines, confluent white matter lesions (WMLs) must be excluded as in these cases veins cannot be unequivocally assigned to each lesion component. This criterion, limiting number of evaluable WMLs, sometimes prevents reliable evaluation of the CVS. In this study performance of an automated algorithm for confluent WMLs segmentation into each component was explored.
Methods: RRMS patients (n = 11; disease duration 17 years; EDSS 4) who had performed standardized 3T MRI scans, including FLAIR* sequences were recruited. Confluent WMLs, usually not eligible for CVS evaluation according to NAIMS criteria, were not excluded and their individual components were identified by LesDiv algorithm developed by Pixyl Medical.
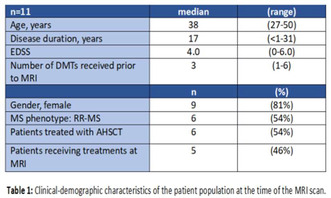
Results: The patients showed 748 lesions. Among the 589 non‐confluent lesions, 272 fulfilled the NAIMS criteria for CVS analysis and out of them 206 were perivenular (PVL) (76%). Among the 159 confluent lesions the LesDiv algorithm identified 427 sub‐components. Out of them 81 (19%) were eligible for the CVS analysis and of these 78 were PVL, increasing to 353 (30%) the number of WMLs eligible for the CVS analysis and to 80% (284/353) the total PVL proportion observed in these patients. The mean proportion of PVL/ patient increased from 67% to 70%.
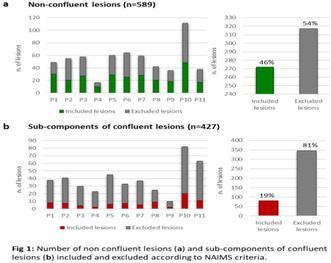
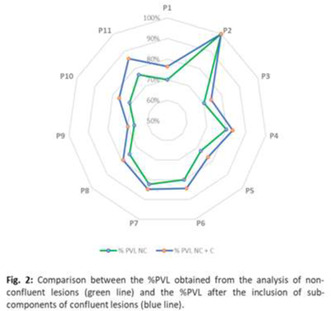
Conclusion: Segmentation of confluent WMLs in their individual components increases WMLs number fulfilling the NAIMS criteria for inclusion in CVS analysis and eventually also PVL proportion.
Disclosure: Nothing to disclose.
EPO‐587
Long‐term outcomes with ozanimod in the DAYBREAK extension trial by number of MS relapses during the phase 3 trials
L. Freeman1; A. Okai2; L. Kappos3; J. Cohen4; C. Cheng5; J. Riolo5; P. Vermersch 6
1Dell Medical School, The University of Texas at Austin, Austin, TX, USA; 2North Texas Institute of Neurology & Headache, Plano, TX, USA; 3Research Center for Clinical Neuroimmunology and Neuroscience Basel (RC2NB), Departments of Head, Spine and Neuromedicine, Clinical Research, Biomedicine, and Biomedical Engineering, University Hospital and University of Basel, Basel, Switzerland; 4Mellen Center for MS Treatment and Research, Cleveland Clinic, Cleveland, OH, USA; 5Bristol Myers Squibb, Princeton, NJ, USA; 6Univ. Lille, Inserm UMR 1172 CHU Lille, FHU Precise, Lille, France
Background and Aims: Early intervention with ozanimod results in control of multiple sclerosis (MS) disease activity that is maintained with long‐term use. Whether long‐term efficacy differs among patients with varying degrees of disease activity is unknown. Here we examine long‐term outcomes (6–7 years) among patients who had 0, 1, or ≥2 relapses during the first 1–2 years of continuous ozanimod 0.92 mg/d or intramuscular interferon (IFN) beta‐1a 30 μg/wk followed by ozanimod 0.92 mg/d.
Methods: In phase 3 “parent” trials, adults with relapsing MS were randomised to oral ozanimod 0.46 or 0.92 mg/d or intramuscular IFN 30 μg/wk for ≥12 (SUNBEAM–NCT02294058) or 24 months (RADIANCE–NCT02047734), after which they were eligible for open‐label ozanimod 0.92 mg/d in an open‐label extension trial (DAYBREAK–NCT02576717). Clinical and radiologic outcomes from parent‐trial baseline through DAYBREAK month 60 (database lock: 7 April 2023) were compared among patients who experienced 0, 1, or ≥2 relapses during SUNBEAM/RADIANCE.
Results: Patients with 1 or ≥2 relapses during SUNBEAM/RADIANCE had numerical decreases in mean annualised relapse rate during DAYBREAK (Figure 1). Patients in all relapse groups who switched from IFN to ozanimod in DAYBREAK had numerical decreases in mean gadolinium‐enhancing and new/enlarging T2 lesion counts that were maintained through month 60 (Figures 2–3). Lesion counts in patients treated with continuous ozanimod remained low through OLE month 60 in all relapse groups.
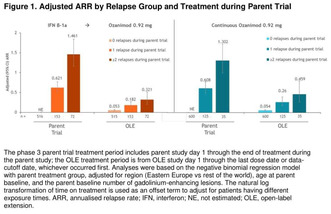
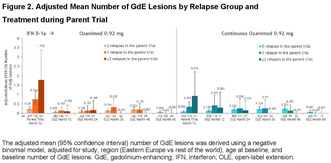
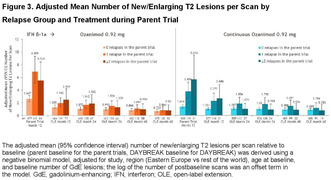
Conclusion: Regardless of prior relapse trends in phase 3 trials, long‐term treatment with ozanimod for up to 60 months in DAYBREAK was associated with clinical and radiologic improvement.
Disclosure: LF: Has received fees for consultancy and/or advisory board participation from Bristol Myers Squibb, EMD Serono, Genentech, Horizon Therapeutics, Novartis, Sanofi, and TG Therapeutics; has received speaker fees from EMD Serono, the MS Association of America, and Sanofi; has received honorarium for participation in educational programs from Medscape, Inc and the MS Association of America; has received program sponsorship from EMD Serono; and grant support from EMD Serono, Genentech, NIH/NINDS, and PCORI through her institution. All authors’ disclosures will be included in the presentation. This study was sponsored by Bristol Myers Squibb. Writing and editorial assistance was provided by Noud van Helmond, MD, PhD, of Peloton Advantage, LLC, an OPEN Health company, and was funded by Bristol Myers Squibb.
MS and related disorders 6
EPO‐588
Real‐world safety and effectiveness of ocrelizumab in different treatment lines in RMS – CONFIDENCE interim analysis
M. Buttmann 1; M. Weber2; S. Meuth3; P. Dirks4; S. Blümich5; S. Hieke‐Schulz5; J. Leemhuis5; T. Ziemssen6
1Caritas Hospital, Bad Mergentheim, Germany; 2Institute of Neuropathology, Department of Neurology, University Medicine Göttingen, Germany; 3Department of Neurology, University Clinic Düsseldorf, Heinrich‐Heine‐University Düsseldorf, Germany; 4F. Hoffmann‐La Roche Ltd., Basel, Switzerland; 5Roche Pharma AG, Grenzach‐Wyhlen, Germany; 6Center of Clinical Neuroscience, Neurological Clinic, Carl Gustav Carus University Clinic, University of Technology, Dresden, Germany
Background and Aims: CONFIDENCE (ML39632, EUPAS22951) is a German non‐interventional, post‐authorization safety study including multiple sclerosis (MS) patients newly treated with ocrelizumab (OCR) and other disease‐modifying therapies. This analysis included real‐world patients with RMS treated with OCR up to 5.5 years.
Methods: Data cut‐off was 11/10/2023. Safety and effectiveness were described for OCR in treatment‐naïve patients (TN‐patients) and patients with ≥1 prior MS‐specific therapies (pwPMST). Safety analysis included OCR patients with ≥1 dose; effectiveness analyses for patients with ≥1 follow‐up visit(s) evaluated annual relapse rate (ARR), Kaplan‐Meier estimate for 24‐week confirmed disability progression (CDP) and 24‐week confirmed disability improvement (CDI), as well as Treatment Satisfaction Questionnaire for Medications© (TSQM).
Results: Mean (SD) observation time for safety was 3.21 (1.32) years with 2267 patients equaling 7743.41 patient years (of which 404 TN‐patients, 780 pwPMST ≥3). Adverse events (AEs) occurred in 56.7/100 patient years (PY) in TN‐patients (88.7/100PY in pwPMST ≥3); 22.9/100PY were classified as System Organ Class (SOC) “Infections and infestations” (32.3/100PY in pwPMST ≥3). Mean (SD) observation time for effectiveness was 3.21 (1.31) years with 2261 patients; overall ARR was 0.11 (SD 0.31). Over 48 months, 78.7% and 75.8% of TN‐patients (n = 326) and pwPMST ≥3 (n = 667), respectively, did not experience CDP; 18.7% of TN‐patients vs. 13.7% of pwPMST ≥3 reached CDI; overall population TSQM global satisfaction was 70.57 (20.15) at baseline and 79.39 (19.34) after 48 months.
Conclusion: Here we present real‐world safety and effectiveness of OCR in different treatment lines in RMS. No new safety signals with increasing exposure time to OCR were observed.
Disclosure: MB: honoraria for lecturing, consulting and/or travel expenses for attending meetings from Biogen, Bristol‐Myers Squibb, Das Fortbildungskolleg, Florian Schmitz Kommunikation, Janssen, Merck, Novartis, RG Ärztefortbildung, Roche, Sandoz, Sanofi, Teva, Viatris MW: research support from the DFG (WE 3547/5‐1, WE3547/7‐1; in association with SFB TRR 274), from Novartis, TEVA, Biogen‐Idec, Roche, Merck and the ProFutura Program of the Universitätsmedizin Göttingen; travel funding and/or speaker honoraria from Biogen‐Idec, Merck Serono, Novartis, Roche, TEVA, Bayer and Genzyme; editor for PLoS One SGM: honoraria for lecturing, travel expenses from Almirall, Amicus Therapeutics Germany, Bayer Health Care, Biogen, Celgene, Diamed, Genzyme, MedDay Pharmaceuticals, Merck Serono, Novartis, Novo Nordisk, ONO Pharma, Roche, Sanofi‐Aventis, Chugai Pharma, QuintilesIMS and Teva; his research is funded by BMBF, BfR, DFG, Else Kröner Fresenius Foundation, G‐BA, DAAD, Hertie Foundation, IZKF Muenster, DGN, Alexion, Almirall, Amicus Therapeutics Germany, Biogen, Diamed, Fresenius Medical Care, Genzyme, HERZ Burgdorf, Merck Serono, Novartis, ONO Pharma, Roche, Teva PD: employee of F. Hoffmann‐La Roche AG SB, JL, SHS: employees of Roche Pharma AG PD, SB, JL: shareholders of F. Hoffmann‐La Roche AG TZ: grants and personal fees from Biogen, Roche, Merck, TEVA, Almirall; grants, personal fees and non‐financial support from Genzyme, Novartis; personal fees from Bayer, BAT, Celgene, Gilead.
EPO‐589
Alemtuzumab in relapsing‐remitting multiple sclerosis: Navigating efficacy and autoimmune challenges
M. Cazola 1; C. Guerreiro1; M. Soares2; P. Faustino2; I. Gomes2; F. Ladeira2; C. Capela2; J. Sequeira2
1Neurology Department, Saint Joseph's Local Health Unit, Lisbon, Portugal; 2Multiple Sclerosis’ Centre of Integrated Responsibility, Saint Joseph's Local Health Unit, Lisbon, Portugal
Background and Aims: Alemtuzumab effectively addresses highly active relapsing‐remitting multiple sclerosis (RRMS). However, it poses potential autoimmune complications, notably thyroid eye disease (16% of cases).
Methods: We describe a case with alemtuzumab‐Induced thyroid eye disease.
Results: A 58‐year‐old non‐smoking woman, with no family history, was diagnosed with RRMS in 1996 following symptom onset in 1994. Her clinical course involved recurrent relapses, leading to hospitalizations. Treatment initially comprised interferon beta‐1b and intravenous immunoglobulin. Due to inadequate disease control, she transitioned to natalizumab and later fingolimod due to the risk of progressive multifocal leukoencephalopathy. In 2017, with an EDSS of 4 and ongoing activity, alemtuzumab was considered. Meeting prerequisites, she underwent the first alemtuzumab cycle. Six months later, elevated anti‐thyroid‐stimulating hormone receptor antibodies, painful exophthalmos, decreased visual acuity, along with horizontal ophthalmoparesis emerged, leading to a diagnosis of Graves' disease‐related orbitopathy. It was promptly managed with bilateral orbital decompression. Despite treatment (antithyroid medication, mycophenolate mofetil, tocilizumab, and methylprednisolone), progressive visual acuity decline ensued, culminating in thyroidectomy. In the latest evaluation, thyroid function normalized, with a persisting temporal scotoma and limitations in left eye abduction and elevation. Post‐thyroidectomy, she underwent a second alemtuzumab cycle without complications. Imaging studies revealed no new lesions, with no reported relapses in the past year, ARR 0.
Conclusion: Despite lacking specific risk factors for alemtuzumab‐associated thyroid eye disease, except gender, the patient proved unresponsive to immunosuppression, necessitating thyroidectomy. This case highlights alemtuzumab's efficacy in RRMS while underscoring the need for monitoring due to potential autoimmune complications, with a favorable clinical outcome despite challenges.
Disclosure: Nothing to disclose.
EPO‐590
OzEAN interim analysis: Treatment satisfaction, QoL, and fatigue in RRMS patients after 1‐year ozanimod use in Germany
M. Buttmann
Department of Neurology, Caritas Hospital Bad Mergentheim, Bad Mergentheim, Germany
Background and Aims: Ozanimod (OZA) was approved in 2020 for the treatment of adults with relapsing‐remitting MS (RRMS) in the EU. Patient‐reported outcomes from routine clinical care represent an important data gap.
Methods: OzEAN (NCT05335031) is a prospective, noninterventional study currently enrolling adult RRMS patients across 80 sites in Germany. This interim analysis reports first real‐world data on quality of life (QoL), fatigue (FSMC) and treatment satisfaction after 1 year of OZA.
Results: This analysis included 317 patients treated with OZA for an average of 17.7 months. At 6 months, most patients showed either improved or stable physical QoL (PCS) (40.1% each, n = 39/96), whereas 18.8% (n = 18) showed worsened PCS. At 12 months, most patients showed either stable or improved (39.3% each, n = 22/56) PCS, 21.4% (n = 12) showed worsened PCS. At 6 months, 46.7% (n = 49/105) of patients showed improved, 32.4% stable (n = 34) and 21.0% (n = 22) worsened mental QoL (MCS). At 12 months, 50.0% (n = 29/58), 29.3% (n = 17) and 20.7% (n = 12) of patients showed improved, stable, and worsened MCS, respectively. 60.9% (n = 112/184) of patients suffered from fatigue at baseline. At 12 months, the percentage of patients without fatigue increased from 39.1% to 44.3%; mean baseline and 12‐month FSMC was 51.6 (±20.7; n = 184) and 49.4 (±20.5; n = 79), respectively. Treatment satisfaction was high, especially regarding side effects (91.8 ± 18.9; n = 82) and convenience (92.6 ± 11.9; n = 82), with 67 of 82 patients reporting no side effects after 12 months OZA.
Conclusion: This interim analysis indicates a positive effect of ozanimod on patient QoL and fatigue, along with high treatment satisfaction.
Disclosure: Funding: This study was supported by Bristol Myers Squibb. MB: honoraria for lecturing, consulting, and/or travel expenses for attending meetings from Bayer, Biogen, Boehringer, Bristol Myers Squibb, Coloplast, Daiichi‐Sankyo, Das Fortbildungskolleg, Merck, Novartis, Roche, Sanofi, and Teva TG: advisory board honoraria from Bristol‐Myers Squibb VB: advisory board honoraria, speaker's honoraria, and scientific honoraria from Merck, Novartis, Roche, Sanofi‐Genzyme, and Teva MK: advisory boards and speaker fees / travel grants from Merck, Sanofi‐Genzyme, Novartis, Biogen, Janssen, Alexion, Celgene / Bristol‐Myers Squibb and Roche; research grants from Merck, Roche, Novartis, Sanofi‐Genzyme and Celgene / Bristol‐Myers Squibb JF: research support and/or travel expenses for attending meetings from Roche, Novartis, BMS, Hexal, Almirall, Merck, Bayer, Teva, and Zambon WKB: advisory board honoraria and scientific honoraria from Bristol Myers Squibb, Novartis, Merck, Hexal, Roche and Vertanical SB, MM, and MD: employees and/shareholder of Bristol‐Myers Squibb GmbH & Co TZ: advisory board fees from Biogen, Bristol Myers Squibb, Merck, Novartis, Roche, Sanofi, and Teva; speaker fees from Almirall, Alexion, Biogen, Bristol Myers Squibb, Hexal, Novartis, Roche, Sanofi, Teva, and Viatris; and research support from Biogen, Bristol Myers Squibb, Novartis, Roche, Sanofi, and Teva.
EPO‐591
Cardiovascular disease in patients with multiple sclerosis and their association with course, disability and progression
M. Andolina; S. Iacono; G. Schirò; G. Sorbello; A. Calì; G. Salemi; P. Ragonese
Department of Biomedicine, Neuroscience and Advanced Diagnostics, University of Palermo, Italy
Background and Aims: Comorbidities are thought to be a negative prognostic factor in people with multiple sclerosis (pwMS) although the association between cardiovascular diseases (CVDs) and MS disability severity is conflicting. The aim of this study is to explore the association between CVDs and the risk of disability worsening and secondary MS progression (SPMS).
Methods: frequency and incidence of CVDs were calculated. The independent risk of reaching EDSS 4, EDSS 6 and SPMS conversion was computed for CVDs by using multivariable Cox‐regression models.
Results: A total of 622 pwMS were included (72.8% female; age: 51.4 years [42–60]; follow‐up: 12.3 years (7–21). CVDs reached a frequency of 40.7% with an incidence of 3 cases every 100 pwMS per year of follow‐up and the commonest were hypertension (23.5%) followed by hyperlipidemia (11.7%) and type 2 diabetes mellitus (6.3%). CVDs were common in progressive MS course and the number of incident cases increased with increasing patient's age (rs = 0.37; p < 0.0001) and MS duration (rs = 0.32; p < 0.0001). T2DM at diagnosis or at any point before the index condition singled out as independent risk factor of reaching EDSS 4 (HR = 1.99 [95% CI 1.02–3.90], p = 0.04), EDSS 6 (HR = 1.61 [95% CI 0.9–2.8], p = 0.09) and SPMS conversion (HR = 1.74 [95% CI 0.99–3.1], p = 0.055).
Conclusion: CVDs are common in pwMS wherein are mainly associated with disease duration, progressive course and older age. T2DM was the only CVDs associated with higher risk of disability worsening and MS progression despite hypertension classically was also associated with bad MS prognosis.
Disclosure: Nothing to disclose.
EPO‐592
Post SARS‐CoV‐2 vaccination immune response in patients with MS treated with varying doses of parenteral cladribine
A. Zasybska; A. Pietruczuk; K. Rejdak
Department of Neurology, Medical University of Lublin, Lublin, Poland
Background and Aims: A vaccination against SARS‐CoV‐2 is recommended in the multiple sclerosis (MS) group of patients. However, the effects of DMTs on the humoral and cell‐mediated response after SARS‐CoV‐2 vaccination in MS patients remain unclear. The aim of this analysis is to compare the immune response to SARS‐CoV‐2 vaccination in MS patients treated with cladribine and those receiving DMTs.
Methods: The study group consisted of 18 patients diagnosed with progressive multiple sclerosis (PMS) who received different doses of cladribine in parenteral formulation. The antibody titers specific to N protein and S1 spike protein were measured in all patients, on average 12 months after the last dose of the vaccine. Then 11 patients were treated with cladribine only, 3 patients treated cladribine with at least one disease modifying drug in the past, 4 patients with at least one disease modifying drug). Patients who qualified for the study had received at least one dose of the vaccine against SARS‐CoV‐2.
Results: Conducted analysis shows that 91% of patients treated with cladribine showed the presence of vaccination antibodies against the SARS COV‐2 virus. One patient, with lymphopenia 0.65 × 109 and an incomplete dose of cladribine, did not obtain a positive antibody titer indicating the acquisition of immunity. No adverse effects on the post‐vaccine immune response have been shown in patients treated with at least 2 disease modifying drugs.
Conclusion: Parenteral cladribine treatment with different dosing schemes had no negative significant effect on the generation of the immune response to the SARS‐CoV‐2 virus post vaccination.
Disclosure: Nothing to disclose.
EPO‐593
Performance of the NMOSDCopilotTM digital tool for unsupervised self‐assessment of NMOSD: The OPTIS study design
M. Levy1; E. Sotirchos2; L. Carment 3; E. Touré Cuq3; S. Fam4; D. Case4; A. Kielhorn4; E. Aras4; A. Vivès3; J. De Seze5
1Department of Neurology, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA; 2Department of Neurology, Johns Hopkins University School of Medicine, Baltimore, MD, USA; 3Ad Scientiam, Paris, France; 4Alexion Pharmaceuticals Inc., Boston, MA, USA; 5Department of Neurology, Hôpital Civil, Strasbourg University, Strasbourg, France
Background and Aims: Neuromyelitis Optica Spectrum Disorder (NMOSD) is characterised by unpredictable relapses leading to the accrual of neurological disability. Regular patient assessments help understand disease burden before, during, and after relapses, which supports clinical decision making. NMOSDCopilotTM, a Software as a Medical Device, supports self‐assessment by NMOSD patients. It features a smartphone application collecting active digital biomarkers of walking, dexterity, cognitive and vision functions, and e‐questionnaires (pain, fatigue, bladder and bowel control and quality of life). A web portal allows clinicians to access patients’ data.
Methods: OPTIS is a prospective, open‐label, multicenter, single group study enrolling adults with AQP4‐IgG+ NMOSD in the United States, France, and Germany. It is designed to validate the clinical performance and the safety of NMOSDCopilotTM and demonstrate its usability. Patients will use NMOSDCopilotTM to complete tests and questionnaires during clinical visits at baseline, 6‐ and 12‐months, as well as standard clinical evaluations (Timed 25‐Foot Walk, 9‐Hole Peg Test, Symbol Digit Modalities Test, Sloan Low‐Contrast Letter Acuity Test). Remote self‐assessments will be completed every month for 12 months.
Results: OPTIS will evaluate the correlation between NMOSDCopilotTM digital active tests and standard in‐clinic testing in 103 patients with AQP4+ NMOSD. Other objectives include evaluating reliability and reproducibility of tests in NMOSDCopilotTM, as well as the safety, usability, adherence, and satisfaction with the tool.
Conclusion: The OPTIS study will generate evidence on the clinical performance of NMOSDCopilotTM. NMOSDCopilotTM has the potential to enable frequent patient self‐assessments of neurological function, characterise burden of disease, and facilitate clinician disease management decisions.
Disclosure: This work was funded by Ad Scientiam (Paris, France) and was supported by a collaborative research agreement from Alexion Pharmaceuticals Inc. (Boston, USA). Michael Levy is an employee of the Massachusetts General Hospital (Boston), one of the OPTIS study sites. Elias Sotirchos is an employee of the Johns Hopkins University School of Medicine (Baltimore), one of the OPTIS study sites. Jerôme De Sèze is an employee of the Hôpital Civil (Strasbourg), one of the OPTIS study sites. Sami Fam, Dan Case, Adrian Kielhorn, Emrah Aras are employees of Alexion Pharmaceuticals Inc. Loïc Carment, Emma Touré Cuq, and Alizé Vives are employees of Ad Scientiam.
EPO‐594
Aquaporin‐4 positive NMOSD: An atypical pathology with nerve root enlargements and peripheral nervous system damage
E. Ogawa 1; M. Otomo2; K. Tsukita1; G. Watanabe1; A. Yasaka1; A. Tamagake1; Y. Suzuki1
1Department of Neurology, National Hospital Organization Sendai Medical Center; 2Department of Neurology, Osaki Citizen Hospital
Background and Aims: Neuromyelitis optica spectrum disorder (NMOSD) is an inflammatory disease of the central nervous system (CNS). Recent studies have reported damage to the peripheral nervous system (PNS) in NMOSD. However, most studies have focused on NMOSD lesions localized in the transitional zone between the CNS and PNS at the root level. The aim of this report is to describe a patient with autoantibodies against aquaporin‐4 (AQP4) positive NMOSD, presenting with demonstrated nerve root enlargements and PNS damage in demyelination.
Methods: Conducted a descriptive analysis encompassing clinical, imaging, blood and cerebrospinal fluid (CSF) examination, and electrophysiological assessments.
Results: A 72‐year‐old woman was admitted to our hospital in March 2023 due to limb weakness. Neurological examination revealed a positive relative afferent pupillary defect, muscle weakness in her limbs, hyporeflexia of the lower extremities and sensory disturbance below Th1 level. An MRI demonstrated a left internal capsule lesion, longitudinal extensive transverse myelitis at the level of C4‐Th10, nerve root enlargements, and high‐intensity signals in the bilateral cervical/lumbar cord. Positive anti‐AQP4 antibodies in both serum and CSF led to the diagnosis of NMOSD. Testing for anti‐myelin oligodendrocyte glycoprotein, ‐neurofascin‐155, ‐Contactin‐1, and ‐ganglioside antibodies returned negative results. Her symptoms significantly improved following six sessions of plasma exchange.
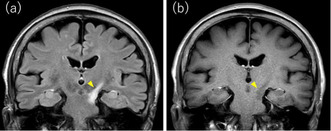
FIGURE 1 Brain MRI: FLAIR image reveals a high signal in the left internal capsule (a), while T1W1 image exhibits a low signal intensity in the same area (b). MRI, magnetic resonance imaging; FLAIR, fluid‐attenuated inversion recovery.
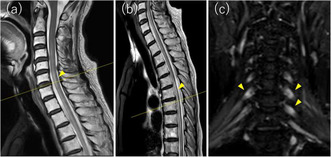
FIGURE 2 Spine MRI: Spinal MRI illustrates longitudinal extensive transverse myelitis at the level of C4‐Th10 (a), (b) and associated nerve root enlargements (c).
Conclusion: This report represents one of the few cases of anti‐AQP4 antibody‐positive NMOSD with demonstrated nerve root enlargements, contributing to an expanded understanding of NMOSD pathology. We discussed the pathomechanisms of the nerve root enlargements in this case.
Disclosure: Nothing to disclose.
EPO‐595
Assessing the clinical value of the central vein sign by MRI for the differential diagnosis of multiple sclerosis
C. Oreja‐Guevara 1; E. Alba Suárez1; L. García‐Vasco1; I. Gómez‐Estévez1; P. Salgado‐Cámara1; J. Quezada Sanchez1; J. Alvaréz‐Linera2
1Neurology, Hospital Clínico San Carlos, Idissc, Madrid, Spain; 2Radiology, Ruber Internacional Hospital, Madrid, Spain
Background and Aims: Patients with diffuse symptoms often present a few non‐specific hyperintense lesions on cranial MRI, raising diagnostic doubts. The central vein sign (CVS), indicative of a vein within a white matter lesion visible on MRI, is considered suggestive of multiple sclerosis. Objective: To study the utility of the central vein sign in differentiating diagnoses in patients with T2 hyperintense lesions, employing the SWI sequence in brain MRI.
Methods: Prospective study. Standard and SWI sequence brain MRIs were performed on Multiple Sclerosis patients and those with uncertain diagnosis who presented hyperintense lesions in T2. Clinical, CSF and OCT data were collected in cases with uncertain diagnoses.
Results: Ten patients were analyzed: 5 with uncertain diagnosis and 5 with MRI‐confirmed MS. MS patients showed between 80–100% of T2 hyperintense lesions with CVS on SWI sequence. All five patients with uncertain diagnosis tested negative for CSF IgG OCBs. Among them, two had no CVS lesions: one was later diagnosed with migraine and small vessel disease, and the other tested positive for MOG antibodies. Two others showed up to 20% of lesions with CVS: one has recently diagnosed with double negative NMOSD and the other with MOGAD. One patient, presenting with headache, had 80% of lesions with CVS; however, two performed lumbar punctures were negative for IgG OCBs, and the MRI findings did not meet the MAGNIMS criteria.
Conclusion: The central vein sign could be useful to rule out the diagnosis of MS in patients with uncertain diagnosis.
Disclosure: Nothing to disclose in relation with the abstract.
EPO‐596
BDNF and NTRK2 gene polymorphisms associations with fatigue in a cohort of multiple sclerosis patients
M. Pantuliano; V. Pozzilli; F. Motolese; M. Rossi; A. Cruciani; L. Celani; F. Santoro; V. Di Lazzaro; F. Capone
Neurology, Neurophysiology and Neurobiology Unit, Department of Medicine, Campus Bio‐Medico University of Rome, Rome, Italy
Background and Aims: Numerous studies have focused on the role of brain‐derived neurotrophic factor (BDNF) and tropomyosin‐related kinase B (TrkB) signalling in psychiatric and neurological disorders, including multiple sclerosis. There are conflicting data regarding the effects of BDNF and neurotrophic receptor tyrosine kinase 2 (NTRK2) genetic polymorphisms on brain atrophy, cortical thickness, neuroinflammation, neuroplasticity, as well as cognitive decline in patients with multiple sclerosis (pwMS). This study aimed to explore a possible correlation of BDNF and NTRK2 polymorphisms with cognitive impairment and fatigue in pwMS.
Methods: We enrolled 40 pwMS, who underwent venous sampling to analyse BDNF polymorphism rs6265 and NTRK2 polymorphisms rs1387923, rs1565445, and rs2769605. Subsequently, patients were administered various clinical tests or questionnaires, including Fatigue Severity Scale (FSS). Demographic data were collected retrospectively. We then performed a MANCOVA test and a categorical regression analysis.
Results: We found a statistically significant difference in the means of the groups of NTRK2 rs1387923 regarding FSS scores (p = 0.022). Successively, we performed a follow‐up categorical regression analysis, which showed a significant correlation between the A/G genotype and higher FSS scores compared to either the A/A genotype or G/G genotype (p = 0.019 and p < 0.001, respectively) only in patients with BDNF Val/Val or Val/Met genotype.
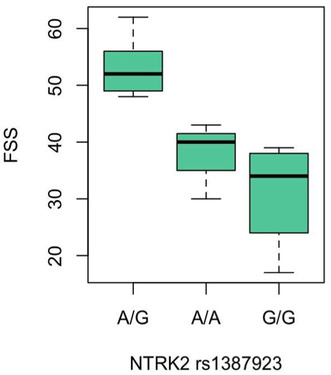
FIGURE 1 Boxplot representing averaged values of Fatigue Severity Scale (FSS) scores corresponding to A/G, A/A, and G/G genotypes of NTRK2 rs1387923 polymorphism in the subgroup of patients with BDNF Val/Val or Val/Met genotype.
Conclusion: BDNF has been linked to fatigue in cancer and chronic fatigue syndrome. To our knowledge, this is the first study to suggest that BDNF and NTRK2 polymorphisms may be associated with an increased susceptibility to fatigue in pwMS. Further studies on a larger number of patients are needed to corroborate this hypothesis.
Disclosure: Nothing to disclose.
EPO‐597
User perspectives on digital health applications for people with multiple sclerosis: A focus group investigation
B. Fasching1; R. Stark1; N. Krajnc1; F. Leutmezer1; G. Bsteh1; T. Berger1; B. Seebacher2; P. Altmann 1
1Department of Neurology, Medical University of Vienna, Austria; 2Clinic for Rehabilitation Muenster, Department of Rehabilitation Research, Muenster, Austria
Background and Aims: Digital health applications (DHA) are software tools designed to assist in healthcare management. They are particularly relevant for people with chronic diseases such as multiple sclerosis (MS). Despite advances in clinical use, further strategies are needed to facilitate DHA implementation and maintain adherence of its users. This study aimed to analyse patient perspectives on the feasibility of DHA and identify key criteria for potential clinical implementation.
Methods: People with MS (pwMS) with prior DHA interaction were recruited through the Department of Neurology, Medical University of Vienna. Semi‐structured interviews, guided by WHO digital health principles, were transcribed from two focus groups and subsequently analysed using reflexive thematic analysis.
Results: Thirteen pwMS (9 female) were interviewed in two focus groups. Participants’ median age was 43 years (range 25–60), median disability on the Expanded Disability Status Scale was 1.5 points (1–6). Key findings include the need for a user‐centred design of DHA ensuring interfaces are intuitive and tailored to the specific needs of pwMS. The integration of DHA into existing clinical workflows was seen as an opportunity to improve communication on an equal footing between pwMS and neurologists. Robust data protection measures, transparent data policies and autonomous data management were considered essential for a sustained use of DHA.
Conclusion: This study elaborates on attributes of DHA that may enhance their feasibility as an addition to standard care for pwMS. Recognizing individual patient needs and incorporating an intuitive design emerged as critical factors in DHA adherence.
Disclosure: This study was funded by Roche Austria by a research grant awarded to the corresponding author (PA). The form says I have to enter less than 1500 characters but disclosures for all authors make up 2200 characters.
EPO‐598
Autoimmune diseases associated with neuromyelitis optica spectrum disorder: Population‐based registry data
T. Pekmezovic 1; V. Jovicevic2; M. Andabaka2; N. Momcilovic2; N. Veselinovic2; O. Tamas2; M. Budimkic2; S. Todorovic3; M. Jeremic2; E. Dincic4; S. Vojinovic3; S. Mesaros2; J. Drulovic2
1Faculty of Medicine, University of Belgrade, Belgrade, Serbia; 2Clinic of Neurology, University Clinical Center of Serbia, Belgrade, Serbia; 3Clinic of Neurology, University Clinical Center Nis, Nis, Serbia; 4Clinic of Neurology, Military Medical Academy, Belgrade, Serbia
Background and Aims: The aim of our study was to estimate the frequency of autoimmune comorbidities in NMOSD patients from the national Serbian NMOSD Registry. Additionally, analysis of the frequency of related pathogenic organ‐specific and not organ‐specific autoantibodies was analyzed.
Methods: Our study comprises 136 patients with NMOSD, diagnosed according to the NMOSD criteria 2015. At the time of the study, in the Registry were collected demographic and clinical data, including those related to the coexisting comorbidities and pathogenic autoantibodies.
Results: Among 136 NMOSD patients, 50 (36.8%) had at least one associated autoimmune disorder. The most frequently reported diseases were autoimmune thyroid disease (15.4%), Sjogren's syndrome (11.0%), systemic lupus erythematosus (5.1%), myasthenia gravis (4.4%), and primary antiphospholipid antibody syndrome (2.9%). Aquaporin (AQP) 4‐IgG was present in the sera from 106 patients (77.9%) and in this subgroup, autoimmune comorbidities were statistically significantly more frequent than in the AQP4‐IgG negative subjects (p = 0.002). In the total cohort of our NMOSD patients, out of 106 tested patients, at least one pathogenic autoantibody was detected in 76 subjects (71.7%). Antinuclear antibodies (ANAs) were the most frequently detected antibodies (54.3%). ANAs and anti‐extractable nuclear antigen antibodies were statistically significantly more frequent in AQP4‐IgG positive vs. AQP4‐IgG negative patients (p = 0.006, and p = 0.033, respectively).
Conclusion: NMOSD patients, especially AQP4‐IgG seropositive ones, are rather frequently associated with wide spectrum of autoimmune diseases, including both organ‐specific and systemic autoimmune disorders, and related pathogenic autoantibodies, in our defined cohort with European ethnical background.
Disclosure: Nothing for disclose.
EPO‐599
Comparison of ocrelizumab and ofatumumab: Examining clinical characteristics within the first year of market availability
M. Peters 1; D. Ellenberger2; F. Fneish2; N. Frahm2; T. Friede3; P. Flachenecker4; K. Hellwig5; C. Kleinschnitz6; A. Stahmann2
1German MS‐Registry, Gesellschaft für Versorgungsforschung mbH (Society for Health Care Research [GfV]), Hannover, Germany; 2German MS‐Registry, MS Forschungs‐ und Projektentwicklungs‐ gGmbH (MS Research and Project Development gGmbH [MSFP]), Hannover, Germany; 3Department of Medical Statistics, University Medical Center Göttingen, Göttingen, Germany; 4Neurological Rehabilitation Center Quellenhof, Bad Wildbad, Germany; 5Department of Neurology, St. Joseph and St. Elisabeth Hospital, Ruhr University, Bochum, Germany; 6Department of Neurology and Center of Translational and Behavioral Neurosciences (C‐TNBS), University Hospital Essen, Essen, Germany
Background and Aims: The number of treatment options for relapsing multiple sclerosis (RMS) has considerably increased in recent years. Onlabel anti‐CD20 monoclonal antibodies (anti‐CD20) ocrelizumab (OCR; introduced: 2018) and ofatumumab (OFA; introduced: 2021) are highly effective disease‐modifying therapies (HE‐DMTs). This study aims comparing the clinical characteristics of people with MS (pwMS) initiating treatment with OCR/OFA within the first year of German market availability.
Methods: We analysed data from the German MS Registry as of 1‐Nov‐2023, focusing on OCR/OFA‐treated RMS patients. pwMS with DMT initiation within one year of German market availability (observation time: OCR 1‐Feb‐2018 to 1‐Feb‐2019; OFA 1‐Sep‐2021 to 1‐Sep‐2022) were characterized regarding clinical variables and DMT prescription before OCR/OFA.
Results: 452 pwMS received OCR and 175 OFA (Table 1). Age, disease duration and disability level (expanded disability status scale; EDSS) at OCR/OFA initiation were significantly lower in OFA patients than in OCR patients. Lower EDSS scores were identified to favor OFA initiation (Figure 1). OFA users were more often treatment‐naïve than OCR users (29.7% vs. 25.7%; chi‐square test p = 0.334; Figure 2). S1P receptor modulators, natalizumab, and daclizumab were the most used pre‐OCR treatments, whereas glatiramer acetate, anti‐CD20, and cladribine were more frequently prescribed before OFA.
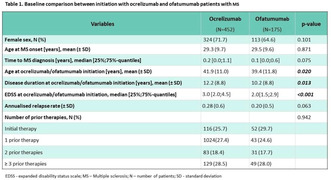
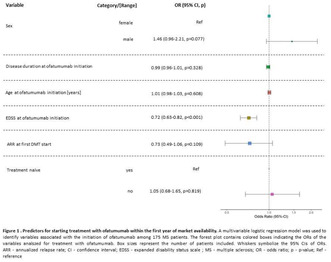
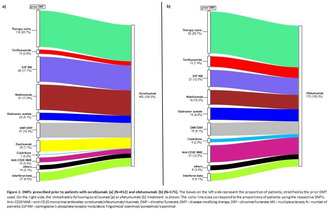
Conclusion: Differences in clinical patient characteristics and pre‐therapy may be explained by the market availability of additional HE‐DMTs. PwMS were more often initiated with OCR as the first in‐class medication compared to the subsequent OFA. The administration route of OCR (infusion) and OFA (injection) could also impact patient preferences and physician decisions in the future.
Disclosure: The authors have received speaking fees, travel support, honoraria from advisory boards, and/or financial support for research activities from pharmaceutical companies. None resulted in a conflict of interest.
EPO‐600
A phase 2 trial of tolebrutinib, a Bruton's tyrosine kinase inhibitor, for chronic active lesions in multiple sclerosis
D. Reich 1; S. Raza1; C. Donnay1; A. Blazier2; S. Sawney1; J. Akinsanya1; J. Ohayon1; A. Fletcher1; J. Dwyer1; Y. Akahata1; G. Wirak2; I. Cortese1; S. Jacobson1; D. Ofengeim2; M. Absinta3; T. Turner2; M. Gaitán1
1National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, MD, USA; 2Sanofi, Cambridge, MA, USA; 3Translational Neuropathology Unit, San Raffaele Scientific Institute, Milan, Italy
Background and Aims: In paramagnetic rim lesions (PRL), iron accumulates in activated microglia at the edge of chronic active multiple sclerosis (MS) lesions. PRL are associated with smoldering tissue degeneration and aggressive disease and are not resolved by approved disease‐modifying therapies. Tolebrutinib, a brain‐penetrant Bruton's tyrosine kinase (BTK) inhibitor, modulates B cells and microglia.
Methods: BRaKe‐MS (NCT04742400), a single‐site, open‐label, rater‐blinded, Phase 2a trial, assessed whether 48 weeks of tolebrutinib 60 mg resolved PRL on 7‐tesla MRI in adults with no new white matter lesions or clinical relapses for ≥6 months, who were on anti‐CD20 therapy at baseline. Radiological, clinical, and biological outcomes were measured at 24 and 48 weeks (primary outcome). Secondary outcomes included safety, tolerability, and other radiological outcomes.
Results: We enrolled a preplanned total of 7 participants. At baseline, the median number of PRL per participant was 9 (range: 6–46). The primary outcome (disappearance of ≥1 PRL in at least 2 participants) will be reported, together with changes in the CSF and blood proteome (Olink) and single‐cell transcriptome (10×). No participant had a clinical or radiological relapse. The most common adverse events were COVID‐19 (4), headache (3), and nausea (3). No safety‐related discontinuations or treatment‐related deaths occurred.
Conclusion: BRaKe‐MS tested whether 48 weeks of BTK inhibition with tolebrutinib reduced radiological and biological markers of inflammation associated with chronic active white matter lesions in MS.
Disclosure: This study was supported and sponsored by the Intramural Research Program of NINDS (NIH), in part via a Cooperative Research and Development Agreement with Sanofi.
Muscle and neuromuscular junction disorder 3
EPO‐601
Comparison between IVIG and plasma exchange in the management of myasthenia crisis
N. Gutti; J. Kalita; F. Ahamed
Department of Neurology, Sanjay Gandhi Postgraduate Institute of Medical Sciences
Background and Aims: Myasthenic crisis (MC) is characterized by type II respiratory failure needing mechanical ventilation (MV). Intravenous immunoglobulin (IVIg) or plasma exchange (PLEX) are used as a rescue treatment although there is paucity of information. We compare the efficacy of IVIg and membrane based PLEX in MC in an open labelled trial.
Methods: Patients with MC were included, and their clinical findings, precipitating causes and laboratory parameters were noted. Patients were either treated with IVIg (400 mg/kg/day for 5 days) or membrane based PLEX (40 ml/kg/alternate day for 5 sessions). Primary outcome was duration of MV, and secondary outcomes were duration of hospital stay, time to reach pre‐worsening status, pyridostigmine dose at discharge, and adverse events.
Results: 44 episodes of MC occurred in 17 patients. IVIg was prescribed in 15 (34.1%) and PLEX in 8 (18.18%) episodes. Mean age was higher in IVIg group than the PLEX (49.53 ± 9.93 vs 40.25 ± 7.92; p = 0.02). Other baseline characteristics are comparable. Infection was the most frequent cause (61.4%) of MC. IVIg group required longer duration of MV compared to PLEX (17.47 ± 11.32 vs 7.38 ± 7.40 days; p = 0.018). However, there was no difference in the duration of hospital stay (30.33 ± 21.39 vs 24.12 ± 7.88 days; p = 0.33) and time to reach pre‐worsening status (53.33 ± 22.25 vs 48.13 ± 31.27 days; p = 0.68). Allergic reaction (6.7%) and raise in creatinine (13.3%) were seen in IVIg group needing withdrawal in one. In PLEX group, 50% episodes were associated with transient fall in blood pressure, not required withdrawal.
Conclusion: Membrane based plasmapheresis reduced the duration of mechanical ventilation in MC compared to IVIg. Blood pressure monitoring is important during plasmapheresis.
Disclosure: Nothing to disclosure.
EPO‐602
Subcutaneous efgartigimod PH20 demonstrates improvements in gMG patients regardless of prior administration route
E. Cortés Vicente 1; J. Verschuuren2; H. Wiendl3; L. Liu4; F. Gistelinck4; S. Steeland4; B. Van Hoorick4; J. Podhorna4; K. Utsugisawa5; J. De Bleecker6; R. Mantegazza7
1Neuromuscular Diseases Unit, Department of Neurology, Hospital de la Santa Creu i Sant Pau, Universitat Autònoma de Barcelona, Barcelona, Spain; Center for Networked Biomedical Research into Rare Diseases (CIBERER), Madrid, Spain; 2Department of Neurology, Leiden University Medical Center, Leiden, Netherlands; 3Department of Neurology, University of Münster, Münster, Germany; 4argenx, Ghent, Belgium; 5Department of Neurology, Hanamaki General Hospital, Hanamaki, Japan; 6Department of Neurology, Ghent University Hospital, Ghent, Belgium; 7Department of Neuroimmunology and Neuromuscular Diseases, Fondazione Istituto Neurologico Carlo Besta, Milan, Italy
Background and Aims: ADAPT‐SC+ is an ongoing, open‐label extension trial evaluating long‐term efficacy/safety of subcutaneous (SC) efgartigimod PH20 (coformulated with recombinant human hyaluronidase PH20) in generalised myasthenia gravis (gMG). Interim analyses (December 2022) demonstrated efficacy/safety of efgartigimod PH20 SC in gMG participants rolled over from ADAPT+/ADAPT‐SC (Fig.1). Here we evaluate efgartigimod PH20 SC in gMG participants who received IV or SC formulations in antecedent studies.
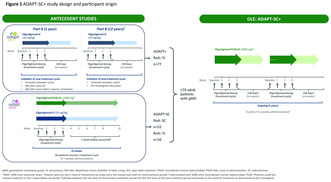
Methods: Efgartigimod PH20 SC 1000 mg was administered in cycles of 4 once‐weekly injections. Subsequent cycles were initiated ≥28 days from last dose based on clinical evaluation.
Results: As of December 2022, 179/184 participants received ≥1 efgartigimod PH20 SC dose; participants previously received efgartigimod IV (IV‐SC: 127/179 [70.9%]) or efgartigimod PH20 SC (SC‐SC: 52/179 [29.1%]). Mean (SD) study duration was 413.9 (107.9) days (136.9 patient‐years follow‐up) and 410.4 (96.7) days (56.5 patient‐years follow‐up) in the IV‐SC and SC‐SC subgroups, respectively. In AChR‐Ab+ participants (IV‐SC: n = 98; SC‐SC: n = 43), mean [SE] total MG‐ADL score improved from baseline to week 4, cycle 1 (IV‐SC: −4.3 [0.33]; SC‐SC: −3.6 [0.49]) and was consistent over subsequent cycles in both subgroups (Fig.2). Mean MG‐QoL15r/EQ‐5D‐5L scores improved from baseline over multiple cycles in both subgroups, indicating improved QoL over time. Adverse events were predominantly mild/moderate and consistent between subgroups; most frequent were injection site erythema (IV‐SC: 30.7%; SC‐SC: 25.0%), COVID‐19 (IV‐SC: 23.6%; SC‐SC: 19.2%), and headache (IV‐SC: 17.3%; SC‐SC: 26.9%). Four deaths were reported (IV‐SC), with none efgartigimod‐related, as per investigator.
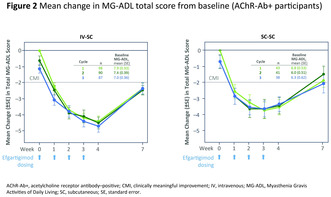
Conclusion: Efgartigimod PH20 SC demonstrated comparable efficacy/safety in gMG participants previously treated with IV or SC formulations.
Disclosure: ECV: Alexion, argenx, Janssen, UCB. JV: Alexion, argenx, Health Holland, NMD Pharma, MuSK MG patent applications, MuSK antibody assays, member of the European Reference Network for Rare Neuromuscular Diseases (ERN EURO‐NMD), Princes Beatrix Fonds. HW: Abbvie, Actelion, Alexion, Amicus, argenx, Biogen, Bristol Myers Squibb, CSL, Deutsche Forschungsgesellschaft (DFG), Deutsche Myasthenie Gesellschaft e.V., EMD Serono, Fondazione Cariplo, Genzyme, German Ministry for Education and Research (BMBF), Gossamer Bio, Idorsia, Immunic, Immunovant, Janssen, Lundbeck, Merck, Neurodiem AG, NexGen, Novartis, PSI CRO, Roche, Sanofi, Swiss Multiple Sclerosis Society, TEVA, UCB, WebMD Global and Worldwide Clinical Trials. LL, FG, SS, BVH, and JP: employees of argenx. KU: Alexion, argenx, Chugai, Horizon, Janssen, Japan Blood Products Organisation, Mitsubishi Tanabe, UCB, Viela Bio. JLDB: Alexion, Alnylam, argenx, CSL, Janssen, Sanofi Genzyme, UCB. RM: Alexion, argenx, Biogen, BioMarin, Catalyst, Merck, Roche, Teva, UCB.
EPO‐603
Cardiac organoids as in vitro model for myotonic dystrophy type 1
L. Fontanelli 1; A. Kostina2; G. Bellini1; L. Becattini1; G. Vadi1; A. Aguirre2; G. Siciliano1
1Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy; 2Institute for Quantitative Health and Engineering, Michigan State University, East Lansing, MI, USA
Background and Aims: Current animal models fail to faithful replicate the complexity of Myotonic Dystrophy. Organoids are self‐organizing in vitro culture systems that acquire in vivo‐like organ complexity, enabling them to recapitulate the architecture and functions of organs. Our aim is to generate cardiac organoids as in vitro model of DM1 to explore pathophysiology of the disease and as a preclinical model for testing candidate drugs.
Methods: Three iPSCs lines from distinct caucasian affected with myotonic dystrophy harbouring different expansion triplet numbers have been used. Cardiac organoids were generated using a published protocol by Lewis‐Israeli (2021) and cultured until day 50 (Fig. 1).
Results: Patient‐derived organoids (PdOs) showed similar contractile structures to controls (Fig. 1) and manifested different gene expression profiles. PdOs showed increased expression of COL1A1 (p < 0.01) and calcium channel (p = 0.03) and a decrease in insulin receptor (p < 0.01) and IGF receptor (p = 0.03). Of note, an increase of CACNA1C expression have been found also in vivo (Poulin, 2021), while the reduction in INSR and IGFR expression may, in part, explain the insulin resistance, We observed marked differences in PdOs and control organoids regarding the amplitude of calcium transients and conduction velocities, both reduced in DM1 organoids (Fig. 1).
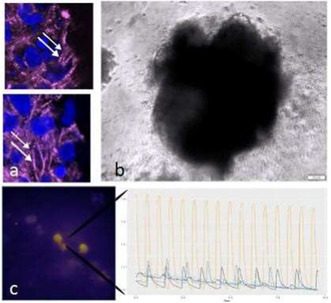
1A: Both patient‐derived and controls organoids shows characteristic contractile structures. 1B: Organoids at 50 days of culture. 1C: calcium analysis.
Conclusion: We generated PdOs that replicate certain features observed in vivo. Given their flexibility, organoids can serve as personalized disease models and may improve our understanding of pathophysiological mechanisms in DM1, as a tool to evaluate DMPK expansion effects in distinct aspects of cell physiology, as well as a test platform for candidate drugs.
Disclosure: Nothing to disclose.
EPO‐604
Safety and efficacy of amifampridine in Lambert‐Eaton myasthenic syndrome patients – Real world data
P. Szczudlik1; E. Sobieszczuk 1; M. Walczak2; A. Kostera‐Pruszczyk1
1Department of Neurology, Medical University of Warsaw, Poland, ERN EURO NMD; 2Department of Pediatrics, Endocrinology, Diabetology, Metabolic Disease and Cardiology of the Development Age, Pomeranian Medical University, Poland
Background and Aims: Lambert‐Eaton myasthenic syndrome (LEMS) is an ultrarare neurological disease with triad of symptoms: muscle paresis, dysautonomy and areflexia. Symptomatic treatment with amifampridine is available. Aim: To assess the effectiveness and safety of treatment in real‐world.
Methods: 14 patients with non‐neoplastic LEMS treated with amifampridine were enrolled in the study (F 42.9%, mean age 48.8 ± 11.4 years). The patients were assessed using Quantitative Myasthenia Gravis (QMG) scale, QMG limb domain (LD) score, spirometry, Hand Grip Strength (GRIP) test and repetitive nerve stimulation study (RNS) at baseline and end of follow‐up. Diagnostic delay was 7–260 months. The patients were treated for 21.1 ± 12.0 weeks (13–48 weeks).
Results: All patients improved in QMG score. Mean improvement was 5.1 ± 2.0 (1–8) points (p < 0.001). Clinically meaningful improvement ≥3 points achieved 85.7% of patients (N = 12) Improvement in QMG LD was seen in 78.6% of the patients (mean 2.2 ± 1.6 points, p < 0.001). Also, FVC improved on treatment (p = 0.031). Mean improvement in GRIP test was 7.0 ± 7.1 kg in right and 5.2 ± 7.5 kg in left hand (p < 0.001). In RNS before treatment, facilitation (>100%) was observed in 78.6% (N = 11) of patients and was higher before treatment (p < 0.001). Mean increase of CMAP amplitude was 2.1 ± 1.6 times. CMAP amplitude increased on treatment (p < 0.001). In 64.3% (N = 9) of patients lowering of corticosteroid dose was achieved.
Conclusion: Amifampridine is an effective treatment in non‐neoplastic LEMS patients. Treatment is well‐tolerated and allows to lower dose of corticosteroids in the majority of patients.
Disclosure: Nothing to disclose.
EPO‐605
From phenotype to genotype: Diagnosis pitfalls in atypical FSHD cases
F. Torri 1; C. Strafella2; L. Vercelli3; G. Gadaleta3; B. Risi4; L. Colantoni2; E. Giardina2; M. Filosto4; T. Mongini3; G. Siciliano1; G. Ricci1
1Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy; 2Genomic Medicine Laboratory‐UILDM, Santa Lucia Foundation IRCCS, Rome, Italy; 3Neuromuscular Unit, Department of Neurosciences; Rita Levi Montalcini, University of Turin, Turin, Italy; 4Neuromuscular Omnicenter, NeMO, Fondazione Serena Onlus, Milan, Italy
Background and Aims: Facioscapulohumeral muscular dystrophy (FSHD) is the third most common dystrophy, in which different phenotypes can be observed, showing different disease progression and/or implying distinct genetic mechanisms. To date, the diagnostic criteria are based on the detection of the genetic signature (reduced D4Z4 allele, permissive haplotype, hypomethylation, mutations in modifiers genes as SMCHD1, LRF1 or DNMT3B). Still, the interpretation of the genetic test cannot ignore a careful correlation with the phenotype.
Methods: We present data of a cohort of 43 patients from 24 families selected by phenotypic features, characterized by incomplete penetrance/atypical phenotypes according to the Comprehensive Clinical Evaluation Form (CCEF), in which a short D4Z4 allele segregated. The molecular characterization included the assessment of 4q subtype, DNA methylation levels, Whole Exome Sequencing (WES) and segregation analysis.
Results: In our cohort, methylation levels displayed high variability in relation to the disease phenotype. In more than half of the atypical phenotypes, despite the detection of the FSHD genetic signature, WES analysis identified VUS or likely pathogenic/pathogenic variants in other genes associated with neuromuscular disorders, compatible with the observed phenotype, or known FSHD‐modifying genes. A definitive alternative diagnosis was obtained in 5 families.
Conclusion: Our results further support the need to perform a detailed phenotypic characterization of patients with a suspect of FSHD, and, in cases of atypical phenotypes, to combine the D4Z4 sizing with other procedures such as WES. In this regard, methylation analysis represents a valuable tool to provide preliminary evidence for FSHD to be confirmed by further testing.
Disclosure: The authors have no conflicts of interest to disclose.
EPO‐606
The METMYD Study: Early results on efficacy and safety of metformin in myotonic dystrophy type 1 (DM1)
E. Frezza 1; S. Rossi2; A. Perna3; E. Bucci4; G. Greco1; M. Goglia1; V. Visconti5; A. Botta5; M. Nuccetelli6; G. Antonini4; A. Petrucci3; G. Silvestri2; R. Massa1
1Department of Systems Medicine, University of Rome “Tor Vergata”, Rome, Italy; 2Institute of Neurology, Department of Neuroscience, Catholic University of Sacred Heart, Rome, Italy; 3Center for Neuromuscular and Neurological Rare Diseases, San Camillo Forlanini Hospital, Rome, Italy; 4Unit of Neuromuscular Diseases, Department of Neurology Mental Health and Sensory Organs (NESMOS), Faculty of Medicine and Psychology, ‘Sapienza’ University of Rome, Sant'Andrea Hospital, Rome, Italy; 5Department of Biomedicine and Prevention, Genetics Unit, University of Rome “Tor Vergata”, Rome, Italy; 6Department of Laboratory Medicine, Tor Vergata University Hospital, Rome, Italy
Background and Aims: DM1 is still orphan of a cure or disease‐modifying treatment. While gene therapy and antisense‐oligonucleotide treatments are under investigation, recent studies showed that metformin can modify the aberrant alternative splicing causative of DM1. The aim of this study is to evaluate the superiority of a 24 month‐treatment with the biguanide drug metformin over placebo, on mobility and strength parameters in adult DM1 patients.
Methods: METMYD is a multi‐center, randomized, triple‐blind, two‐arm, placebo‐controlled, phase III clinical trial. The primary endpoint is a better performance at the 6MWT at the end of study as compared to baseline. Secondary clinical endpoints explore muscle quantitative testing of upper and lower limbs, dexterity, fatigue. In addition, quantitation of circulating alternative splicing products deficient in DM1 and of markers of oxidative stress is performed before and after treatment.
Results: Enrolment started in January 2020 and the study ended in December 2023. One‐hundred and forty‐nine patients were enrolled and 146 were randomized either to metformin or placebo. The two arms at baseline did not differ for sex, age, BMI, HOMA index and 6MWT. Fifty‐four (37%) patients (29 on metformin, 25 on placebo) dropped out for various reasons, mainly non‐compliance, consent withdrawal and diarrhea and 92 patients completed the protocol.
Conclusion: The METMYD study shows that a long‐term pharmacological intervention is feasible in DM1 patients, even during the COVID‐19 pandemics. Metformin showed to be safe when administered in non‐diabetic DM1 patients, the only common AE being diarrhea, as in general population. The analysis of clinical and laboratory efficacy measures is underway.
Disclosure: Nothing to disclose.
EPO‐607
Anti‐HMGCR necrotizing myopathy: Characterization and therapy management in 17 patients over a 10 years follow‐up
G. Brodini 1; G. Gadaleta1; G. Urbano1; L. Chiadò‐Piat1; T. Manetta2; G. Mengozzi2; T. Mongini1; L. Vercelli1
1S.S. Neuromuscular Unit, Department of Neurosciences “Rita Levi Montalcini”, AOU Città della Salute e della Scienza, Molinette Hospital, Turin, Italy; 2S.C. Biochimica Clinica, AOU Città della Salute e della Scienza, Molinette Hospital, Turin, Italy
Background and Aims: Antibodies against 3‐hydroxy‐3‐methylglutaryl‐coenzyme A reductase (HMGCR) myopathy represents an immune‐mediated necrotising myopathy (IMNM) typically associated with statin use, with a variable onset. In this retrospective study we examined 17 patients diagnosed with anti‐HMGCR IMNM according to 2017 EULAR criteria, followed at our Center in the years 2013–2014.
Methods: Medical records, encompassing clinical, histological, instrumental, and laboratory data (table 1–2), were systematically reviewed.
Results: Clinical onset manifested as a progressive proximal muscle weakness in 70.5% of patients. 29.5% of cases were only mildly symptomatic but 80% of them developed remarkable weakness within two years, before starting IVIg treatment, with only one remaining slightly symptomatic. 88% of patients had prior statin exposure; elevated serum creatine kinase (CK) levels (600–27000 UI/L) and positive anti‐HMGCR antibodies were observed in all cases. In 16/17 patients, immunomodulant/suppressive therapy was administered with steroids and/or intravenous immunoglobulin (IVIg); five patients also received azathioprine or methotrexate. IVIg yielded optimal responses in 88% of patients. Immunotherapy was gradually tapered for all patients throughout the years. Of nine patients ceasing IVIg after achieving clinical‐biochemical remission, six of them had to resume treatment, leading to rapid improvement.
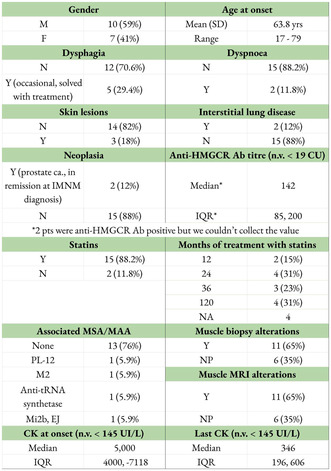
TABLE 1 Ab anti‐HMGCR‐IMNM. Clinical, serological, instrumental and histological information.
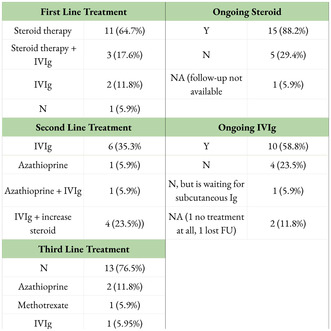
TABLE 2 Ab anti‐HMGCR‐IMNM. Treatment management.
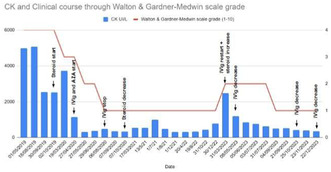
GRAPHIC 1 Ab anti‐HMGCR‐IMNM. Clinical course (calculated with Walton and Gardner‐Medwin scale grade, y axis on the right), serological course (based on CK levels, y axis on the left) and treatment modifications thorough the years of one patient.
Conclusion: Anti‐HMGCR IMNM seems to produce a persistent dysimmune process; chronic immunomodulant treatment appears to be the most suitable to maintain clinical and biochemical remission. In our cohort, 67% of patients relapsed after IVIg treatment suspension, although still well responded to IVIg reintroduction. This highlights the need for recurring treatment cycles and vigilant clinical and serological monitoring.
Disclosure: Nothing to disclose.
EPO‐608
Facioscapulohumeral muscular dystrophy (FSHD) type 1 mimics: Review of 60 cases with normal size D4Z4 alleles
G. Gadaleta 1; L. Vercelli1; G. Urbano1; G. Brodini1; E. Rolle1; R. Tupler2; T. Mongini1
1Department of Neuroscience “Rita Levi Montalcini”, Neuromuscular Unit, University of Turin, Turin, Italy; 2Department of Biomedical, Metabolic and Neural Sciences, University of Modena and Reggio Emilia, Modena, Italy
Background and Aims: Analysis of D4Z4 alleles is indicated in patients with facial‐shoulder girdle weakness and in FSHD1 patients’ relatives. Our research focused on carriers of D4Z4 alleles with ≥11 repeats, reviewing their phenotypes according to the Comprehensive Clinical Evaluation Form (CCEF) Clinical Categories, and identifying alternative genetic diagnoses.
Methods: We examined 510 patients referred for 4q35‐D4Z4 analysis to the Miogen Laboratory (Modena) in the last 15 years.
Results: Excluding 356 cases (69.8%) showing a D4Z4‐reduced allele, 154 (30.2%) carried D4Z4 alleles with ≥11 repeats: 94 (61%) were unaffected relatives (Category C), and 60 (39%) represented sporadic symptomatic patients. Among the latter group, 9 (15%) presented a full phenotype (Category A), 3 (5%) an incomplete one (Category B), and 48 (80%) an atypical involvement (Category D). Subsequent genetic analyses identified damaging variants in the following genes and Clinical Categories: 3 SMCHD1 (FSHD2) and 1 COL6A (Category A); 1 EMD (Category B1); in Category D, 4 CAPN3 (2 recessive and 2 dominant), 2 COL6A, 1 MYH7, 1 DMPK, 1 RYR1, 1 GAA, 1 DMD (Becker phenotype), 1 FKRP, and 1 SGCG. In 1 atypical case, a variant on PMP22 already described in Charcot‐Marie‐Tooth (CMT)‐like distal weakness was found. In the remaining 41 patients further genetic analyses are ongoing.
Conclusion: The study of 4q35 region is justified in FSHD‐like phenotypes and in FSHD1 patients’ relatives for segregation. In our cohort, alternative diagnoses were found in 32% of FSHD1‐mimicking phenotypes, making it a varied group needing thorough phenotyping and extensive genetic investigations.
Disclosure: Nothing to disclose.
EPO‐609
Safety and efficacy of tofacitinib in patients with refractory myasthenia gravis: A pilot study
R. Zhao; C. Yan; S. Luo; C. Zhao
Department of Neurology, Huashan Hospital Affiliated to Fudan University, National Medical Center for Neurological Diseases, Shanghai, China
Background and Aims: Myasthenia gravis is one of the most common autoimmune neuromuscular disorders. About 10 percent MG patients still are refractory and there still is an unmet need for effective, well tolerated, and convenience treatment options for these patients. We aimed to assess the safety and efficacy of tofacitinib, an inhibitor of JAK kinases with oral administration.
Methods: This registered open‐label, single‐arm pilot study was conducted from June 2020 through December 2023 (NCT04431895). Refractory gMG patients received tofacitinib (5mg, twice a day) as the only IS in combination with corticosteroids. Clinical scales, including QMG score, MG‐ADL, MG‐QoL15, and MGC were assessed prospectively from the baseline to 24 weeks after Tofacitinib initiation. The phosphorylation level of STAT3 in peripheral blood CD4+T cells for MG patients were detected by multi‐color flow cytometry.
Results: We enrolled 19 anti‐AChR antibody‐positive gMG cases. By week 24 after tofacitinib administration, a significant reduction was observed in MG‐ADL (6.0 vs 1.5 at baseline; p = 0.0004) and QMG (14 vs 11 at baseline; p = 0.0391), respectively. Corticosteroids dose were significantly reduced from 20 mg to 15 mg (p = 0.0074). Tofacitinib induced the elevation of triglycerides in some patients. Phosphorylation flow cytometry revealed that tofacitinib inhibits the phosphorylation levels of STAT3 protein in Th17.1 cells in MG who received tofacitinib.
Conclusion: The study provided preliminary evidence of the safety and efficacy profile of tofacitinib in treating patients with refractory gMG. The therapeutic effect of Tofacitinib was probably associated with the inhibition of pro‐inflammatory Th17.1 cells.
Disclosure: Nothing to disclose.
EPO‐610
Germinal centers are associated with the prognosis of thymoma‐associated myasthenia gravis
H. Chung 1; H. Shin2; S. Kim2
1Department of Neurology, Yongin Severance Hospital, Yonsei University Health System, Yongin, Korea; 2Department of Neurology, Yonsei University College of Medicine, Seoul, Korea
Background and Aims: Some studies have observed that the presence of germinal centers (GCs) in the non‐neoplastic thymic tissues play a part in the pathogenesis of thymoma‐associated myasthenia gravis (TAMG). The aim of this study is to analyze whether the presence of GCs in the thymus of patients with TAMG are associated with clinical outcome of myasthenia gravis after removal of thymoma.
Methods: We conducted a retrospective analysis of TAMG patients who underwent surgical removal of the thymoma. Clinical characteristics were collected and thymic tissue slides were rereviewed by a pathologist. Patients were classified into GC‐positive and GC‐negative groups based on the presence of GC.
Results: Preoperative use of prednisolone is known to reduce the number of GCs, and the proportion of patients who were on preoperative prednisolone treatment was lower in the GC‐positive group (Table 1) After excluding the patients with preoperative prednisolone use, a total of 83 patients with 37 (44.6%) in the GC‐positive group and 46 (55.4%) in the GC‐negative group were analyzed. The clinical differences between the two groups are presented in Table 2. Multivariate analysis using cox regression revealed a negatively significant between minimal manifestation and the presence of GCs (Table 3).
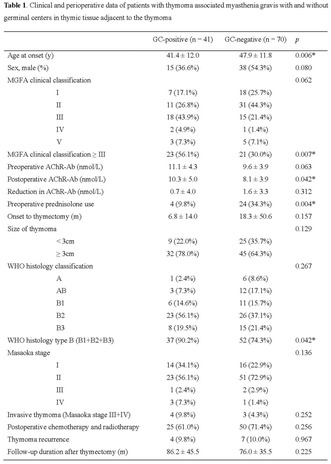

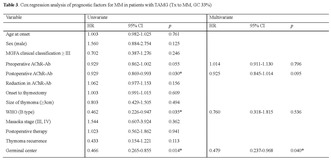
Conclusion: Presence of GCs in the nonthymomatous tissue of TAMG patients was associated with greater disease severity and worse clinical outcome after thymectomy. The presence of thymic GCs could be used as a predictor of clinical outcome in patients with TAMG.
Disclosure: Nothing to disclose.
EPO‐611
Real world experience of Efgartigimod in a single UK centre – A 17 month follow up study
J. Spillane; N. Thambirajah; G. Logou; S. Sumaria; R. Howard; D. Kullmann
National Hospital for Neurology and Neurosurgery, Queen Square, UCLH NHS Foundation Trust, London, UK
Background and Aims: We present our experience of treating patients with generalised Myasthenia Gravis (gMG) with the neonatal Fc receptor (FcRN) antagonist Efgartigimod under the UK Early Access to Medicine Scheme (EAMs) in single centre over a 16 month period.
Methods: Data regarding all patients receiving Efgartigimod in the National Hospital for Neurology and Neurosurgery were collected prospectively. Efgartigimod was given as per the ADAPT protocol. Response to Efgartigimod was measured with MG‐ADL scores, change in prednisolone dose and need for rescue therapies.
Results: 18 patients with gMG were treated with Efgartigimod over the 17 month period, 12 were female and the average disease duration was 14.6 years (range 1–40). 66% had required IVIG/PLEX regularly and 22% had required intermittent rescue treatment prior to starting Efgartigimod. All patients had previously received prednisolone and non‐steroidal immunosuppressant therapies (NSITs). The average NSITs tried was 2.4. 50% had received Rituximab. The mean MG‐ADL at baseline was 11.3. Following the first treatment cycle 89% were defined as MG‐ADL responders with an average reduction of 7 points. Two patients stopped taking Efgartigimod due to lack of efficacy. 89% remained on it with a mean inter‐cycle interval of 6.5 weeks. 83% of patients reduced their steroid doses. Rescue IVIG and PLEX were required in the two patients that stopped treatment but otherwise no rescue treatments were required Efgartigimod was well tolerated with only minor side effects reported.
Conclusion: Efgartigimod is an effective and well tolerated treatment in patients with refractory gMG.
Disclosure: JS received speakers fees, and travel support from UCB and argenx and has served on UCB advisory boards.
EPO‐612
Cyclic and continuous dosing of intravenous Efgartigimod for generalised myasthenia gravis: Part A of ADAPT NXT
K. Claeys1,2; V. Bril2; Y. Hussain3; K. Gwathmey4; G. Sahagian5; A. Habib6; E. Cortés‐Vicente 7; E. Brauer8; D. Gelinas8; A. Sumbul8; R. Jimenez8; D. Hristova8; R. Mantegazza9; A. Meisel10; S. Attarian11; ADAPT NXT Study Group12
1Department of Neurology, University Hospitals Leuven, Leuven, Belgium; Laboratory for Muscle Diseases and Neuropathies, KU Leuven, Leuven, Belgium; 2Ellen & Martin Prosserman Centre for Neuromuscular Diseases, University Health Network, Toronto, Ontario, Canada; University of Toronto, Toronto, Ontario, Canada; 3Austin Neuromuscular Center, Austin, Texas, USA; 4Department of Neurology, Virginia Commonwealth University, Richmond, Virginia, USA; 5The Neurology Center of Southern California, Carlsbad, California, USA; 6Department of Neurology, University of California, Irvine, Irvine, California, USA; 7Neuromuscular Diseases Unit, Department of Neurology, Hospital de la Santa Creu i Sant Pau, Barcelona, Spain; Biomedical Research Institute Sant Pau, Barcelona, Spain; argenx, Ghent, Belgium; 8argenx, Ghent, Belgium; 9Department of Neuroimmunology and Neuromuscular Diseases, Fondazione Istituto Neurologico Carlo Besta, Milan, Italy; 10Department of Neurology and NeuroScience Clinical Research Center, Charité – Universitätsmedizin Berlin, Berlin, Germany; 11Reference Center for Neuromuscular Disorders and ALS Timone Hospital University, Marseille, France
Background and Aims: Individualised cyclic administration of efgartigimod, a human immunoglobulin G1 Fc‐fragment that blocks the neonatal Fc receptor, was well tolerated and efficacious in the ADAPT/ADAPT+ phase 3 trials in generalised myasthenia gravis (gMG). In an effort to evaluate additional dosing regimens, the phase 3b ADAPT NXT study (NCT04980495) is investigating the efficacy, safety, and tolerability of 10 mg/kg intravenous efgartigimod administered in a cyclic (4 once‐weekly infusions, 4‐week intertreatment period) or continuous dosing regimen [every 2 weeks (Q2W)].
Methods: Adult participants with acetylcholine receptor antibody positive gMG who had MG‐ADL total score ≥5 (with >50% of the score due to nonocular symptoms), and on a stable dose of ≥1 concomitant gMG treatment were recruited. Sixty‐nine participants were randomised 3:1 on Day 1 to either continuous or cyclic dosing regimens for the initial 21‐week comparison period (Part A; Figure). In Part B, participants in the cyclic arm received a final cycle before being rolled over to continuous Q2W dosing, while participants in the continuous dosing arm maintained Q2W dosing. Participants were followed for an additional 105‐week extension period, and participants who maintained clinical improvement had the option to reduce dosing frequency to every 3 weeks.
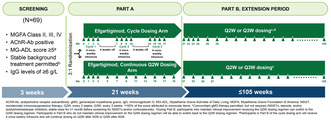
FIGURE ADAPT NXT study design.
Results: The primary endpoint is mean (SD) of the average change in MG‐ADL total score from study baseline to Week 21 for each regimen. Safety, tolerability, and pharmacokinetic/pharmacodynamic effects are also being assessed; results will be presented at the congress.
Conclusion: ADAPT NXT will provide important efficacy and safety data on different treatment regimens in patients with gMG.
Disclosure: Multiple relationships financial and non‐financial nature for authors KGC, VB, YH, KG, GS, AAH, ECV, EB, DG, AS, RHJ, DH, RM, AM, and SA stated at point of presentation.
EPO‐613
Danon disease in Japan: A phenotype‐genotype correlation
K. Sugie 1; A. Uruha2; M. Yamaoka1; A. Yamanaka1; H. Shimizu1; Y. Nishimori1; T. Shiota1; H. Nanaura1; N. Eura1; I. Nonaka3; I. Nishino3
1Department of Neurology, Nara Medical University; 2Department of Neurology, Tokyo Metropolitan Neurological Hospital; 3Department of Neuromuscular Research, National Institute of Neurology, National Center of Neurology and Psychiatry
Background and Aims: Danon disease, an X‐linked dominant vacuolar cardiomyopathy and skeletal myopathy, is caused by primary deficiency of lysosome‐associated membrane protein‐2 (LAMP‐2). However, the clinical and genetic characteristics of Danon disease have not been well established.
Methods: We conducted a nationwide, questionnaire‐based survey on Danon disease to 2,617 hospitals in Japan. We reviewed clinical histories, muscle specimens, and genetic analyses of the LAMP‐2 gene in patients. We added patients newly found and reported since the national survey in Japan.
Results: As a result, we identified 47 Danon disease patients (23 men and 24 women) from 26 families. Hypertrophic cardiomyopathy and ECG abnormalities were documented in most patients with Danon disease. Among the 20 patients who had died, 19 (95%) died of cardiac failure or sudden cardiac arrest. Heart transplantation, the most effective therapy, was performed in only one woman and is just now required by 5 patients. Pathologically, all patients showed autophagic vacuoles with sarcolemmal features in muscles. In this study, 22 different LAMP‐2 mutations were identified in 26 families with Danon disease. Half of the probands showed de novo mutations. The distribution of mutations widely ranged from exon 1 to 9. Four families with mutations in exon 9B (c.1097_1098 delAA) that encodes LAMP‐2B showed markedly mild or no cardiomyopathy.
Conclusion: Cardiomyopathy is the most important prognostic factor and the main cause of death among Danon disease patients. However, clinical phenotypes of only mutations in exon 9B were markedly mild, suggesting that this particular mutation causes an exceptionally mild phenotype.
Disclosure: Nothing to disclose.
EPO‐614
Ventilatory function and sleep‐disordered breathing in patients with facioscapulohumeral muscular dystrophy type 1
M. Lima; R. Rocha; S. Moreira
Serviço de Neurologia, Unidade Local de Saúde de Matosinhos, Matosinhos
Background and Aims: Facioscapulohumeral muscular dystrophy type 1 (FSHD1) is rarely associated with ventilatory dysfunction. The prevalence of sleep‐disordered breathing (SDB) is thought to be high but remains poorly characterized and likely underestimated.
Methods: Observational study on demographic and clinical characteristics of adult FSHD1 patients.
Results: Twenty‐nine patients were included, 52% males, with a mean current age of 49.6 ± 15.7 years. The mean duration of disease was 26.8 ± 16.4 years, with 5 (17%) patients showing childhood onset. The median Clinical Severity Score (CSS) was 3 (IQR = 2.25–3). Twenty‐four patients (83%) were able to walk unaided, 2 with unilateral support, 1 with bilateral support, and 2 were wheelchair‐bounded. Respiratory function tests were conducted in 28 patients. Spirometric curves were normal in 20 (69%) patients, with a restrictive pattern in 4 (14%), and obstructive in another 4 (2 with a history of asthma). Patients with mild to moderate symptoms (CSS ≤3) showed higher mean forced vital capacity (FVC) than those with severe disease (CSS ≥3.5) (p = 0.01). No correlation was found between respiratory function parameters (FEV1, FVC) and disease duration. Nine patients underwent maximal respiratory pressure studies, with altered results in 4, showing a tendency for greater compromise in expiratory pressures. Sleep studies were conducted in 27 patients, with 13 (48%) presenting sleep apnea syndrome, 6 of which requiring nocturnal non‐invasive ventilation.
Conclusion: Our results support previous studies suggesting a high prevalence of SDB in FSHD1 patients. We would also like to emphasize the importance of an active search for ventilatory dysfunction in these patients, especially in more severe motor presentations.
Disclosure: Nothing to disclose.
EPO‐615
Clinical outcome measures in a prospective cohort of myasthenia gravis patients
M. Verza 1; G. Spagni2; S. Falso1; S. Cornacchini1; E. Cencini1; L. Palazzo1; A. Farina1; A. Mariottini1; A. Barilaro1; L. Massacesi1; A. Evoli3; V. Damato1
1Department of Neurosciences, Psychology, Drug Research and Child Health, University of Florence, Florence, Italy; 2German Center for Neurodegenerative Diseases (DZNE) Berlin; Berlin, Germany; 3Department of Neuroscienze, Università Cattolica del Sacro Cuore, Rome, Italy
Background and Aims: Clinical assessment of myasthenia gravis (MG) relies on validated patient‐reported outcome (PRO) and physician reported outcome (PhyRO) measures, coupled with post‐intervention status (PIS) or the recently proposed “PASS question”. The aim of this study is to validate the PASS question and assess PIS and PASS cut‐off values for PRO and PhyRO scales in a prospective cohort.
Methods: The clinical status of AChR‐MG patients was assessed with MG‐ADL, MG‐QOL15r and QMG scores over a 1 year‐period. Favourable outcomes were defined by a positive response to the PASS question and a PIS of minimal manifestation (MM)‐or‐better. ROC curve analysis was used to determine cut‐off values of the QMG, MG‐ADL and MG‐QOL15r in relation to PASS and PIS.
Results: 107 AChR‐MG patients were included, of whom 42% females, with a median age at onset of 46 years. Patients with a favourable PASS and in MM‐or‐better status had a lower median QMG, MG‐ADL, MG‐QOL15 scores than symptomatic patients (p < 0.0001). A QMG ≤9, MG‐ADL ≤2 and MG‐QOL15r ≤6 identified patients with a favourable PASS status. Same cut‐offs for the QMG and MG‐ADL scores were found to identify patients in MM‐or‐better, while the cut‐off for the MG‐QOL15r was much lower (≤4). In the multivariable logistic regression both MG‐ADL (p = 0.025) and MG‐QOL15r (p = 0.043) were independently associated with “PASS = yes”, while QMG score was not.
Conclusion: PASS and PIS provide complementary information on the MG clinical status. The PASS cut‐off values found for the most common MG scales support the use of the PASS question in clinical practice and clinical trials.
Disclosure: Work supported by: (1) #NEXTGENERATIONEU (NGEU) and funded by the Ministry of University and Research (MUR), National Recovery and Resilience Plan (NRRP), project MNESYS (PE0000006) – A Multiscale integrated approach to the study of the nervous system in health and disease (DN. 1553 11.10.2022); (2) Myasthenia Gravis Rare Disease Network–MGNet, a member of the Rare Disease Clinical Research Network Consortium (RDCRN) NIH U54 NS115054. All RDCRN consortia are supported by the network's Data Management and Coordinating Center (DMCC) (U2CTR002818). Funding support for the DMCC is provided by the National Center for Advancing Translational Sciences (NCATS) and the National Institute of Neurological Disorders and Stroke (NINDS).
Tuesday, July 02, 2024
Ageing and dementia 4
EPO‐616
Alzheimer disease prognostic from early clinical assessment: A two‐year follow‐up study
L. Álvarez‐Sánchez 1; Á. Balaguer2; M. Peretó‐Pamblanco1; C. Peña‐Bautista1; L. Ferré‐González1; M. Baquero‐Toledo3; C. Cháfer‐Pericás1
1Alzheimer Disease Research Group, Instituto de Investigación Sanitaria La Fe; Valencia; Spain; 2Math Faculty, Universitat de València, Valencia, Spain; 3Division of Neurology; University and Polytechnic Hospital La Fe, Valencia, Spain
Background and Aims: Alzheimer Disease (AD) evolution is characterized by high heterogenicity. Some patients show fast evolution, and further research is required. The aim of this study is to develop a prognostic model using clinical variables to detect patients at high risk of fast AD progression.
Methods: This observational study has been carried out in the Cognitive Disorders Unit in the Neurology Service of the Hospital Universitari i Politècnic La Fe (HULAFE). Participants were patients diagnosed with mild cognitive impairment (MCI) due to Alzheimer's disease (AD) at time‐1 (T1). For this, CSF biomarkers, and neuropsychological evaluation (CDR sum of boxes, MMSE, and RBANS) were obtained atT1. Two years after diagnosis (T2) the neuropsychological evaluation was repeated. From these data, a prognosis model for the probability of fast AD progression was developed using neuropsychological and CSF variables at T1 as predictor variables; and neuropsychological score (sum of the 3 tests) difference (T2‐T1), as response variable.
Results: The developed model predicted the probability of fast progression, with an AUC of 0.79 (sensitivity 63.6% (95% CI 35.4–84.8); specificity 85.4% (95% CI 71.6–93.1); positive predictive value 53.8% (29.1–76.8); negative predictive value 89.7% (95% CI 76.4–95.9). Among the predictor variables, sex, CSF NfL and RBANS (language, immediate memory and visuospatial/constructional) could be relevant.
Conclusion: Some variables obtained from the MCI‐AD diagnosis time (neuropsychology, CSF) could be helpful for detecting patients with a high risk of fast AD progression.
Disclosure: Nothing to disclose.
EPO‐617
Role of pro‐inflammatory S100A9 protein in amyloid‐neuroinflammatory cascade in neurodegenerative diseases
L. Morozova‐Roche
Department of Medical Biochemistry and Biophysics, Umeå University
Background and Aims: The amyloid cascade and neuroinflammation are central to onset of Alzheimer's and other neurodegenerative diseases. S100A9 may serve as a critical link in the amyloid‐neuroinflammatory cascade in these diseases, as this protein possesses both amyloidogenic properties and acts as alarmin, triggering inflammatory responses.
Methods: The kinetic analysis of amyloid aggregation by thioflavin‐T fluorescence, microfluidic analyses, charge‐detection mass‐spectroscopy, AFM, molecular dynamic simulation and gamma‐oscillation were used in synergy. The level of S100A9 in CSF was measured by ELISA and dot‐blots.
Results: We found that S1009 is intrinsically amyloidogenic and forms amyloids in vitro, in cells and in the brain tissues during Alzheimer's, Parkinson's and traumatic brain injury. We showed that S100A9 co‐assembles with Aβ42 fibrils, forming new type of hetero‐amyloid complexes. In these complexes the autocatalytic surfaces of Aβ42 fibrils template S100A9 amyloids. The formation of Aβ42‐S100A9 complexes may sequestrate smaller toxic species, which is consistent with finding that their co‐aggregation mitigates amyloid cytotoxicity. Small molecules, regulating S100A9 amyloid aggregation, including cell penetrating NCAM1 peptides, oleuropein aglycone, Nb10 and TiNb9 polyoxometalates, cyclin and DOPA derivatives, are viewed in the light of their prospective therapeutic applications in blocking amyloid formation. We have shown also that the levels of S100A9 follow those of Aβ in CSF during the development of Alzheimer's and S100A9 together with Aβ can serve as a biomarker for early stages of Alzheimer's disease.
Conclusion: The finding of S100A9 involvement in neurodegenerative diseases may open a new avenue for therapeutic interventions targeting S100A9 primarily and via this pathway affecting the whole amyloid‐neuroinflammatory cascade.
Disclosure: There is no conflict of interest in presented data.
EPO‐618
Effects of frailty on hospital outcomes among patients with neurological disorders: A cohort study
M. Toccaceli Blasi 1; F. Raffaele1; D. Belvisi1,2; G. Bruno1; M. Canevelli1,3; G. Fabbrini1,2
1Department of Human Neuroscience, “Sapienza” University, Rome, Italy; 2IRCCS Neuromed, Pozzilli IS, Italy; 3National Center for Disease Prevention and Health Promotion, Italian National Institute of Health, Rome, Italy; Aging Research Center, Karolinska Institutet and Stockholm University
Background and Aims: Patients acutely presenting with neurological disorders exhibit highly heterogeneous clinical courses. We explored whether baseline frailty predicts adverse hospital outcomes among patients admitted to neurological wards.
Methods: All patients consecutively admitted to the neurology wards of the Policlinico Umberto I University Hospital of Rome (Italy) were considered. A 40‐item Frailty Index (FI) was calculated from the emergency department assessment. Hospitalization outcomes were prospectively collected. Linear and logistic regression models were conducted to test the association between FI and adverse hospital outcomes.
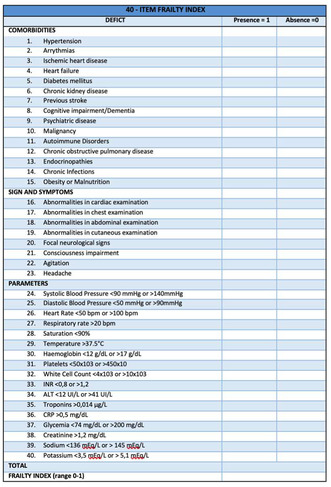
40‐item Frailty Index.
Results: Overall, 185 participants (women 50.3%; mean age 68.6, SD 18.6 years) were enrolled. FI scores ranged between 0 and 0.43, with a median value of 0.15 (IQR 0.10–0.20), and were positively correlated with age (Spearman's rho 0.55, p < 0.001). In multivariate regression models adjusted by age, sex, and neurological diagnosis, the FI was significantly associated with the number of days spent in the neurological ward (B 2.19, 95% CI 0.36–4.02, per 0.1 increase; p = 0.02), with a lower likelihood of being discharged at home (OR 0.38, 95% CI 0.23–0.64, per 0.1 increase; p < 0.001), with higher odds of nosocomial infections (OR 1.55, 95% CI 1.00–2.42 per 0.1 increase; p = 0.05), prescription of antibiotics (OR 1.74, 95% CI 1.12–2.72, per 0.1 increase; p = 0.01) and sedatives (OR 1.84, 95% CI 1.04–3.29 per 0.1 increase; p = 0.04).
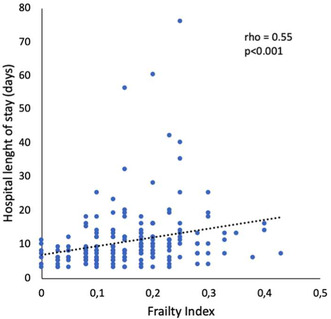
Correlation between Frailty Index and hospital length of stay (days).
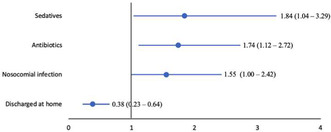
Bivariate logistic regression model adjusted by age, sex, and neurological diagnosis exploring the factors associated with the 40‐item Frailty Index (dichotomized dependent variable of interest). Data are shown as odds ratios (95% confidence intervals).
Conclusion: Assessing the frailty status of patients with acute neurological conditions can improve prognostication. This can have relevant implications for care planning and allocation of healthcare resources.
Disclosure: Nothing to disclose.
EPO‐619
Cross‐sectional and longitudinal associations between sTREM2 and synapses‐related biomarkers in healthy individuals
M. Munoz Garcia 1; Y. Deming2; S. Johnson2; S. Asthana2; C. Carlsson2; O. Okonkwo2; D. Perez‐Martinez3; A. Villarejo3; K. Blennow4; H. Zetterberg4; B. Bendlin2; E. Morenas‐Rodriguez5
1Group of Neurovascular Investigation, Research institute Hospital 12 de Octubre (imas12), Madrid, Spain; 2Wisconsin Alzheimer's Disease Research Center, University of Wisconsin School of Medicine and Public Health, Madison, WI, USA; 3Memory Unit, Department of Neurology, Hospital Universitario 12 de Octubre, Madrid, Spain; 4Department of Psychiatry and Neurochemistry, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 5Group of Neurogenerative Diseases, Hospital Universitario 12 de Octubre Research Institute (imas12), Madrid, Spain
Background and Aims: We aimed to study the association between TREM2‐dependent microglial activation and synaptic dysfunction, and whether this relationship is influenced by AD core biomarkers in asymptomatic volunteers.
Methods: We studied cross‐sectional (n = 239) and longitudinal (n = 117) associations between cleaved sTREM2 (cTREM2) and synapse‐related biomarkers (neurogranin, alpha‐synuclein and s100b) in cerebrospinal fluid (CSF) from asymptomatic volunteers. cTREM2 was measured by an in‐house MSD‐based immunoassay, while synapse‐related and AD core markers were quantified by the Elecsys® platform (Neurotoolkit). We defined subgroups according to the AT classification, and medians of p‐tau and Aβ42/Aβ40 ratio. We used R program (v‐4.3.1) for statistical analysis.
Results: Cross‐sectional associations are shown in table 1. Higher s100b levels were associated with higher cTREM2 levels independently of AD core biomarkers in participants with Aβ42/Aβ40 ratio < median, and in participants with p‐tau levels >median. Higher cTREM2 levels were also independently associated with higher alpha‐synuclein levels in the T+ group, with a trend for an association in A+ participants. Higher baseline s100b levels independently predicted a larger longitudinal increase of cTREM2 (beta = 0.28, p‐value = 0.03). Baseline cTREM2 levels were not associated with any synaptic biomarker longitudinally.
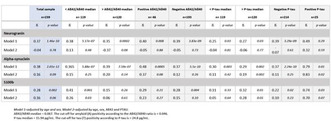
TABLE 1 Beta‐coefficients and p‐values for cross‐sectional associations between synaptic biomarkers and cleaved TREM2 (cTREM2) in linear regression models.
Conclusion: cTREM2 is associated with s100b and alpha‐synuclein in asymptomatic participants with a biomarker profile suggestive of first stages of Aβ‐aggregation and tau pathology. Higher baseline levels of s100b predicts a larger longitudinal increase of cTREM2 in asymptomatic volunteers. Our findings suggest an early influence of synaptic dysfunction on the TREM2‐dependent microglial response in neurodegenerative processes.
Disclosure: Nothing to disclose.
EPO‐620
Association of Helicobacter pylori infection and Alzheimer's disease risk – A meta‐analysis of case‐control studies
A. Menegaz de Almeida1; M. Reis 2; E. Assis3; F. Machado4; J. Limongi5
1Department of Medicine, Federal University of Mato Grosso, Mato Grosso, Brazil; 2Department of Medicine, National University of Rosario, Rosario, Argentina; 3Department of Medicine, Baltic Federal University, Kaliningrad, Russian Federation; 4Department of Medicine, State University of Southwest Bahia, Bahia, Brazil; 5Department of Neurology, University of São Paulo, São Paulo, Brazil
Background and Aims: Alzheimer's disease (AD) remains a challenge in public health due to the aging of the global population. The potential link between bacterial infections, specifically by Helicobacter pylori (HP), and the pathogenesis of AD is still unclear. Hence, we sought to explore the association between HP infection and AD.
Methods: MEDLINE, Embase, and Cochrane databases were systematically searched. Data were examined using the Mantel‐Haenszel method, with Odds Ratio (OR) as the primary measure of association and 95% confidence intervals (CI). Heterogeneity was assessed using I 2 statistics. Statistical analysis were performed using Review Manager software, version 5.4.1.
Results: A total of 1,651,849 patients from 5 population‐based case‐control studies were included in this analysis. Within these patients, 41.054 composed the case group of patients previously diagnosed with AD. In the AD group, 869 individuals were found to be positive for HP infection, meanwhile, in the non‐AD group, this number was 17,649 individuals. Comparing the incidence of HP infection between both groups, statistically significant correlation was observed between AD and HP infection (2.11% vs 1.09%, OR. 1.19, 95% CI 1.10–1.30, p < 0.01, I 2 = 74%).
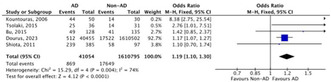
Odds Ratio – Forest Plot.
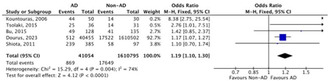
Odds Ratio – Forest Plot.
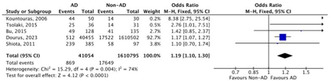
Odds Ratio – Forest Plot.
Conclusion: In this meta‐analysis, consistent results suggest that HP infection is associated with an increased odds for AD.
Disclosure: All authors declare no conflicts of interest and assume responsibility for data reliability and freedom from bias in presentation and interpretation.
EPO‐621
Combining a semantic cued recall paradigm with blood‐based biomarkers in the detection of Alzheimer's disease pathology
M. Lima 1; A. Silva‐Spínola2; D. Damas1; D. Duro1; M. Leitão2; M. Tábuas‐Pereira1; J. Durães1; I. Santana3; I. Baldeiras3
1Neurology Department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal; 2Center for Innovative Biomedicine and Biotechnology, University of Coimbra, Coimbra, Portugal; 3Faculty of Medicine, University of Coimbra, Coimbra, Portugal
Background and Aims: Episodic memory impairment defined by the Free and Cued Selective Reminding test (FCSRT) is a reliable marker of the early involvement of medial temporal structures in AD. Blood‐based biomarkers (BBM) (p‐tau181, NfL and GFAP) were developed for the diagnosis and prognosis of AD. We aim to study the association between FCSRT and BBM in detecting prodromal AD.
Methods: We included 70 non‐demented individuals (66 years of median age, 67% female) with memory complaints and available cerebrospinal fluid (CSF)‐AD biomarkers. Baseline and longitudinal neuropsychological evaluation were performed. Median follow‐up duration was 8 months. BBM were determined using Single Molecule Array (SiMoA). Amyloid pathology was determined by amyloid status (A) using CSF Abeta42/40 ratio.
Results: In the comparison between A+ (n = 28) and A‐ individuals (n = 42), we observed significant differences in all the FCSRT‐selected measures (p < 0.05), except for FCSRT cued‐delayed recall. Longitudinally, significant differences in the change of normative z‐scores for MoCA and MPCR were shown (p < 0.001). A+ individuals had significantly higher levels of serum GFAP and plasma p‐Tau181. Additionally, multinomial logistic regression model, adjusted for age, identified blood p‐Tau181 (B = 1.8, p = 0.002), GFAP (B = 0.02, p = 0.008) and NfL (B = −0.2, p = 0.01) as independent significant predictors of amyloid status, particularly in relation to FCSRT free‐delayed recall (B = −0.4, p = 0.006).
Conclusion: This study shows the utility of a semantic and cued recall paradigm (FCSRT) for detecting AD at its prodromal stage, supporting its use as a valid clinic marker together with BBM. These results can now be used to develop individual predictive models of disease progression.
Disclosure: Nothing to disclose.
EPO‐622
Association between frailty and neurophysiological measures of peripheral nerve conduction
M. Salzillo; M. Canevelli; G. Di Stefano; G. Bruno; A. Truini
Department of Human Neuroscience, La Sapienza University of Rome
Background and Aims: Frailty is a marker of biological age and has been associated with a higher risk of adverse neurological outcomes. The present study aimed at investigating the association between frailty and neurophysiological measures of nerve conduction.
Methods: Patients with no peripheral nervous system disorders were subjected to a nerve conduction study at the Department of Human Neuroscience, Sapienza University of Rome. Frailty was assessed through a Frailty Index (FI), designed on the model of deficit accumulation and constituted by 36 items including symptoms, signs, disabilities, and laboratory findings. Spearman's correlations were used to conduct the statistical analysis.
Results: Overall, 25 participants (mean age 59.9, standard deviation [SD] 16.1; 64.7 % women) were recruited. SNAP amplitudes were significantly, inversely correlated with age (ulnar: rho = −0.48, p = 0.03; sural: rho = −0.73, p < 0.001). A negative correlation was also observed between SNAP amplitudes and FI scores (ulnar: rho = −0.09, p = 0.03; sural: rho = −0.73, p = 0.06). In partial correlations adjusted by FI, age was no longer correlated with the SNAP amplitude of the ulnar nerve (rho = −0.35, p = 0.18); the correlation coefficient between age and the SNAP amplitude of the sural nerve decreased to −0.54, p = 0.03.
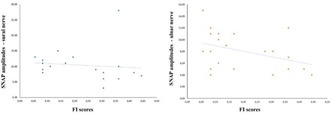
Correlation between SNAP amplitude and sural and ulnar nerve.
Conclusion: The negative correlation between increasing age and measures of SNAP amplitudes seems to be partly moderated by frailty. The FI may be useful to explore the impact of the ageing process on peripheral nerve conduction, beyond chronological age.

Bibliography
Disclosure: Nothing to disclose.
EPO‐623
Quantitative T1‐mapping changes in the gray matter of patients with Alzheimer's disease
M. Losa 1; L. Gualco1; E. Peira2; B. Orso1; L. Argenti1; L. Lombardo1; D. Arnaldi1; N. Montobbio3; M. Sormani3; F. Massa1; A. Chincarini2; M. Costagli1; L. Roccatagliata3; M. Pardini1
1Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (DiNOGMI), University of Genoa, Genoa, Italy; 2Istituto Nazionale di Fisica Nucleare (INFN), Genoa, Italy; 3Department of Health Sciences (DISSAL), University of Genoa, Genoa, Italy
Background and Aims: Structural MRI plays an important role in the diagnosis of Alzheimer's disease (AD) so that it is included in the A/T/N classification. However, structural changes occur late in the course of the disease and lack of a specific correlation with the underlying pathogenetic process. The purpose of our study is to analyze the role of brain quantitative T1‐mapping as a possible index of AD pathology.
Methods: 27 AD patients and 22 healthy controls underwent an MR scan on a clinical 3T MR scanner with a protocol including an MP2RAGE sequence whose output include a set of 3D structural T1‐weighted images and a coupled quantitative T1 map. 3D T1 images were then segmented using FreeSurfer obtaining segmentation masks of the brain that were used to extract regional quantitative T1 (qT1) values of the subjects' gray matter.
Results: Statistical analysis performed with a volume‐corrected model (so corrected for regional atrophy) demonstrated a significant increase in qT1 values in regions known to be involved in AD. For example, hippocampi demonstrated significantly increased qT1 values (p = 0.0055). Moreover, we found a significant difference in overall cortical values (p = 0.028) primarily driven by parietal lobe (p = 0.0197).
Conclusion: Our results demonstrate the presence of alterations in qT1 values in AD that do not seem to be justified by atrophy alone, suggesting in this way that other changes in the microscopic composition of the brain of these subjects can influence this MR‐derived metric.
Disclosure: Nothing to disclose.
EPO‐624
Cerebral amyloid angiopathy in the basal ganglia and brainstem in routine autopsies
Okamoto 1; M. Amari1; M. Ikeda1; T. Fukuda2; K. Suzuki2; M. Takatama3
1Department of Neurology, Geriatrics Research Institute and Hospital, Maebashi, Japan; 2Department of Pathology, Geriatrics Research Institute and Hospital, Maebashi, Japan; 3Department of Internal Medicine, Geriatrics Research Institute and Hospital, Maebashi, Japan
Background and Aims: Previously, we confirmed that cerebellar CAA was observed in 29 cases (48.3%), and the severity of cerebellar CAA was relatively mild compared with 60 cases with CAA‐positive occipital lobe. On the other hand, CAA are said a few in the basal ganglia and brainstem, but the frequency and severity of CAA in the basal ganglia and brainstem are obscure.
Methods: We selected 54 cases with CAA observed in the occipital lobe. Analyses were performed on the occipital lobe, cerebellum, basal ganglia, and brainstem. Brain sections were mainly immunostained with monoclonal amyloid β (Aβ) peptides 17–24 (4G8) and monoclonal anti‐phosphorylated tau (AT8) antibodies.
Results: Of the 54 cases, CAA was observed in the basal ganglia and brainstem in 13 cases (24.1%). In the basal ganglia, CAA was rarely or slightly observed in the claustrum, putamen, and thalamus in 10 cases, with no evidence of CAA in the pallidum. In the putamen and thalamus, Aβ deposits were mainly located in the abdominal portions of the tunica media and adventitia of the vessels. In the brainstem, two cases showed rare CAA in the midbrain. In five cases, CAA was only rarely observed in the meningeal vessels of the brainstem.
Conclusion: These findings suggest that CAA initially develops in the leptomeningeal and cortical vessels of the neocortex, followed by the vessels of cerebellum, and then vessels of the putamen, thalamus, and brainstem.
Disclosure: Nothing to disclose.
EPO‐625
Performance and concordance of plasma versus CSF biomarkers of Alzheimer's disease: A single center Memory Clinic cohort
M. Poli 1; C. Bonomi1; M. Nuccetelli2; S. Bernardini2; C. Motta1; A. Martorana1
1UOSD Centro Demenze, Department of Systems Medicine, University of Rome “Tor Vergata”, Rome, Italy; 2Department of Experimental Medicine, University of Rome “Tor Vergata”, Rome, Italy
Background and Aims: Cerebrospinal fluid (CSF) for Alzheimer's disease (AD) comes with several limitations, namely relative invasiveness, restricted access and high costs, hence the recent focus on plasma biomarkers. Previous studies identified a good accuracy of plasma phosphorylated‐tau181 (plasma/p‐tau181) and plasma amyloid ratio (plasma/amyR, Aβ42/Aβ40) to identify patients with biologically‐defined AD. We addressed their use in clinical practice, verifying their performance accounting for possible confounders, such as renal function (serum creatinine) and blood‐brain barrier permeability (Albumin Quotient), and concordance with CSF biomarkers.
Methods: We enrolled 99 patients with CSF and plasma AD biomarkers, measured using fully‐automized CLEIA (Fujirebio LUMIPULSE® G1200). Patients were stratified into CSF/A+T+ (n = 45, CSF Aβ42/Aβ40 < 0.06, CSF/p‐tau181 > 55 pg/ml) or CSF/non‐A+T+ (n = 54). We evaluated accuracy, sensitivity and specificity of pathological plasma/p‐tau181 (>2.01 pg/ml), plasma/amyR (<0.083) and these combined (plasma/A+T+) in differentiating CSF/A+T+ vs CSF/non‐A+T+, as well as inter‐test reliability (Cohen's K).
Results: Plasma/p‐tau181 showed good sensitivity (82.22%), specificity (87.041%) and agreement with CSF/A+T+ status (K = 0.694); plasma/amyR had lower sensitivity (57.78%), good specificity (81.48%) and modest agreement (K = 0.399); plasma/A+T+ had the overall best sensitivity (94.44%), but low specificity (51.11%) and moderate agreement (K = 0.472). The multivariate logistic regression highlighted that both pathological plasma/p‐tau181 and plasma/amyR are strongly associated with CSF/A+T+ (respectively OR = 31 and OR = 6; p < 0.001), additionally when adjusting plasma/p‐tau181 for creatinine levels (OR = 32) and amyR for Albumin Quotient (OR = 7.7).
Conclusion: Our findings confirm plasma/p‐tau181 as the most reliable stand‐alone predictor of AD. Moreover, renal function and measures of blood‐brain barrier permeability should be considered in order to improve the consistency of plasma biomarkers in clinical practice.
Disclosure: Nothing to disclose.
EPO‐626
Synthesis and evaluation of ketoamide derivatives in modulating amyloid beta aggregation for Alzheimer's disease therapy
R. Kumar 1; B. Das2; A. Baidya2; L. Wang1; B. Winblad1,3
1Department of Pharmaceutical Engineering & Technology, Indian Institute of Technology (BHU), Varanasi, India and Department of Neurobiology, Care Sciences and Society, Division of Neurogeriatrics, Karolinska Institutet, Solna, Sweden; 2Department of Pharmaceutical Engineering & Technology, Indian Institute of Technology (BHU), Varanasi, India; 4Theme Inflammation and Aging, Karolinska University Hospital, Huddinge, Sweden
Background and Aims: The prevalence of Alzheimer's disease (AD), a multifactorial disorder, is on the rise, and the absence of effective therapies necessitates the discovery of novel treatment options. Previous attempts at target‐based therapeutics for AD have faced challenges, but recent successes in amyloid beta‐targeted immunotherapies have inspired new approaches. Motivated by recent advancements, in this study, we aimed to design and develop amyloid beta aggregation inhibitors with an α‐ketoamide scaffold. Specifically, we synthesized a series of piperazine and piperidine‐substituted ketoamide derivatives and further evaluated them for their potential in modulating amyloid beta aggregation.
Methods: The piperazine and piperidine‐substituted ketoamide derivatives were synthesised in high purity and high yield using an appropriate chemical methodology and structurally characterized using NMR spectroscopy and mass spectrometry. Further, the synthesized compounds were subjected to in vitro evaluation for their potential to modulate the aggregation of amyloid beta 42 (Aβ42) using ThT‐based aggregation kinetic assays.
Results: The percentage purity for all the compounds was >95. Among all the synthesized compounds, three compounds demonstrated a significant delay in amyloid beta aggregation, as evidenced by the aggregation kinetics assay.
Conclusion: Our findings highlight the potential of the α‐ketoamide derivatives as promising hit compounds for further development into lead candidate for modulating the Aβ42 aggregation activity which is relevant to Alzheimer's disease treatment.
Disclosure: The authors declare no conflict of interest.
EPO‐627
Survival analysis in patients with early‐onset fronto‐temporal lobar degeneration
M. Šarčević 1; T. Stojković2; G. Mandić Stojemnović2; A. Živković1; P. Aleksić1; V. Kostić2; E. Stefanova2
1Neurology Clinic University Clinical Center of Serbia; 2Neurology Clinic University Clinical Center of Serbia, Medical Faculty University of Belgrade
Background and Aims: The survival rate of patients with early onset FTLD is still undefined. The aim of this study is to determine the survival rates of FTLD behavioral variant (FTLDbv) and primary progressive aphasia (FTLDppa), and to identify clinical and demographic factors that influence it.
Methods: We included 82 patients, 61 with FTLDbv and 21 FTLDppa, observed from 2012 to 2019. Kaplan‐Meier curve and Cox proportional hazard models were used for survival analysis with time from diagnosis to outcome (death or 2019y.) as independent variable.
Results: The mean age at diagnosis in the FTLDbv group was 55.36 ± 7.34 y, with 55.7% males, and 58.3 ± 5.8 y in FTLDppa group, with 47.6% men. In total 53 patients died (32 FTLDbv, 21 FTLDppa). The median survival in the FTLDbv group was 7 y. Age, age at onset, time from symptoms to diagnosis, MMSE and FAB scores were estimated, none of which influenced survival in these patients. Only the presence of motor symptoms (oculomotor disorders, dysphagia) shortened the lifespan of these patients (p = 0.002, median survival 3.75 y in group with, and 8 y without motor symptoms). Median survival in the FTLDppa group is 4.5 y, and older age (p = 0.03, median survival 5.5 y for younger, and 4 y for older patients) as well as older age at onset (p = 0.03, median survival 5.5 y in group below 60, and 3.75 y in group beyond 60) influenced survival in these patients.
Conclusion: Presence of motor symptoms is a clear indicator of faster progression of FTLDbv patients, while older age at onset shortens lifespan of FTLDppa early onset patients.
Disclosure: Nothing to disclose.
EPO‐628
MRI‐guided brain stimulation with TPS ameliorates cognitive deficits and depressive symptoms in Alzheimer's disease (AD)
U. Sprick 1; A. Günes1; M. Köhne2
1Department of Neurostimulation Alexius/Josef Clinic, Neuss, Germany; 2Alexius/Josef Clinic, Neuss, Germany
Background and Aims: No effective long‐term treatment has been found for the treatment of AD so far. MRI‐guided TPS (Transcranial Pulse Stimulation) offers new perspectives to ameliorate AD‐deficits. Pilot studies show beneficial effects on learning and memory of TPS.
Methods: 21 out‐patients with AD (with light to moderate symptoms) received MRI‐guided 6.000 pulses of TPS (0.2 mJ/mm2 per single pulse, with a frequency of 4 Hz) per session bilaterally into the frontal, parietal and temporal cortex with Neurolith by Storz Medical. TPS‐pulses were administered. Pulses were applicated over a period of 2 weeks (3 sessions per week). Cognitive capabilities (especially executive functions) of the patients were tested using the Stroop‐Test (colour‐word‐interference‐test) and the CERAD. Patients were tested using a pre – post design (t0 pre stimulation: t1 after 6 sessions, two weeks later).
Results: TPS‐stimulation over a period of two weeks (6 sessions) showed ameliorating effects on performance in the Stroop‐Test (pre vs. post; p < 0.05 – paired T‐test). Single patients showed extraordinary improvements by shortening completer times in the Stroop‐Test by half. Depressive symptoms of the patients were also ameliorated. The BDI measured before and after the treatment diminished form 18.1 to 12.4 in the mean. No significant side‐effects occurred during all the sessions in none of the patients.
Conclusion: The results of this pilot‐trial show that cognitive impairments of executive functions and depressive symptoms in Alzheimer's disease may be ameliorated using TPS as a noninvasive brain stimulation method. No severe side‐effects were observed.
Disclosure: The authors have no conflicts of interests to disclose.
EPO‐629
Disentangling empathy impairment along Alzheimer's disease continuum
V. Moschini 1; G. Giacomucci2; D. Piazzesi1; S. Padiglioni3; S. Mazzeo2; G. Galdo2; C. Polito4; F. Emiliani2; D. Frigerio2; C. Morinelli1; S. Bagnoli2; A. Ingannato2; B. Nacmias2; S. Sorbi4; V. Berti5
1SOD Neurologia I, Dipartimento Neuromuscolo‐Scheletrico e degli Organi di Senso, AOU Careggi, Florence, Italy; 2Department of Neuroscience, Psychology, Drug Research and Child Health, University of Florence, Florence, Italy; 3Regional Referral Centre for Relational Criticalities – Tuscany Region, Italy; 4IRCCS Fondazione Don Carlo Gnocchi, Florence, Italy; 5Nuclear Medicine Unit, Azienda Ospedaliero‐Universitaria Careggi, Florence, Italy
Background and Aims: Little is known about empathy changes from the early stages of Alzheimer's Disease (AD). The aim of this study is to investigate empathy from Subjective Cognitive Decline (SCD) to Mild Cognitive Impairment (MCI) and AD dementia (AD‐d).
Methods: Forty‐five SCD, 83 MCI and 80 AD‐d patients were included. Empathy was assessed by Interpersonal Reactivity Index (IRI) rated by caregivers before (T0) and after (T1) cognitive symptoms' onset. IRI was also self‐administered to SCD patients. Facial emotion recognition was assessed by Ekman‐60 Faces Test. Patients underwent CSF biomarkers analysis and cerebral FDG‐PET SPM analysis.
Results: PD scores significantly increased from T0 to T1 in SCD, MCI and AD‐d (p < 0.001), while PT scores decreased in MCI and in AD‐d (p < 0.001). SCD AP+ showed a greater increase in PD scores over time (∆PD T0‐T1) than SCD AP‐ (p < 0.001). SCD self‐reported PT scores were lower than those of general Italian population (14.94 ± 3.94, 95% C.I. [13.68–16.20] vs 17.70 ± 4.36, 95% C.I. [17.30–18.10]). In AD continuum (SCD AP+, MCI AP+, AD‐d), a positive correlation was detected between PT‐T1 and brain metabolism in left posterior cingulate gyrus, precuneus and right frontal gyri; a negative correlation was found between ∆PT and brain metabolism in bilateral posterior cingulate gyri.
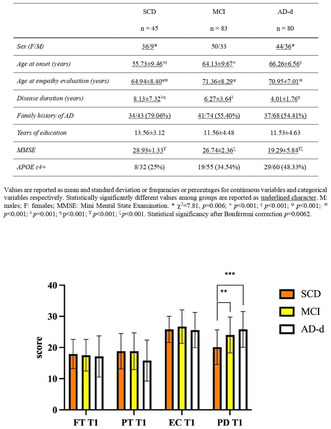
Table about descriptives and graphs.
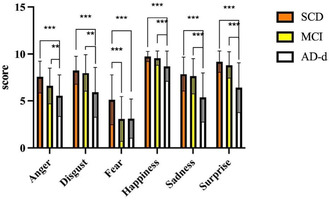
Table about descriptives and graphs.
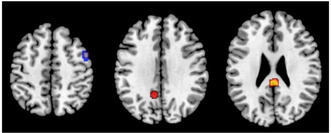
SPM analysis.
Conclusion: PT may be subtly involved since the preclinical phase of AD. Changes over time of PD are influenced by the underlying Alzheimer's pathology and could potentially serve as an early AD neuropsychological marker.
Disclosure: Nothing to disclose.
EPO‐630
Brexpiprazole for agitation in Alzheimer's disease: A systematic review and meta‐analysis of randomized controlled trials
Z. Bakir 1; R. Sudo2; M. Gobbo3
1Department of Medicine, Sapienza University of Rome, Italy; 2Department of Medicine, Federal University of Grande Dourados, Brazil; 3Department of Medicine, Pontifical Catholic University of Rio Grande do Sul, Brazil
Background and Aims: Agitation in Alzheimer's disease (AD) requires effective and well‐tolerated interventions. Recently, Brexpiprazole has emerged as a promising therapeutic avenue.
Methods: We systematically searched ClinicalTrials.gov, PubMed, Embase, and Cochrane Library for randomized controlled trials (RCT) comparing Brexpiprazole to placebo in patients with AD presenting with agitation. A random‐effects model was employed to compute mean differences and risk ratios using R software 4.3.1. The results were reported following the PRISMA guideline.
Results: A total of 3 double‐blind RCTs were included, comprising 1,028 patients with an average age of 74 years. Throughout a 12‐week mean follow‐up period, Brexpiprazole was associated with no changes in Clinical Global Impression‐Severity of illness (MD −0.19; 95% CI −0.38 to 0.00; p = 0.05) and Neuropsychiatric Inventory‐Nursing Home scores (MD −1.51; 95% CI −3.63 to 0.62; p = 0.16). However, there was a notable improvement in Cohen‐Mansfield Agitation Inventory score (MD −3.04; 95% CI −5.04 to −1.04; p < 0.01). Additionally, no difference was observed for the incidence of at least 1 treatment‐emergent adverse events (TEAE) (RR 1.10; 95% CI 0.94 to 1.28; p = 0.52), discontinuation due to TEAE (RR 1.50; 95% CI 0.81 to 2.78; p = 0.20), dizziness (RR 1.04; 95% CI 0.52 to 2.11; p = 0.86), extrapyramidal disorders (RR 2.60; 95% CI 0.44 to 15.40; p = 0.99), and all‐cause death (RR 1.51; 95% CI 0.25 to 8.94; p = 0.48)

Change in the Agitation Scores.

Adverse Events.
Conclusion: In this systematic review and meta‐analysis of 3 RCTs and 1,028 patients, Brexpiprazole was associated with a modestly favorable modulation in agitation score, concurrent with a positive safety profile.
Disclosure: Nothing to disclose.
Child neurology/developmental neurology
EPO‐631
Neuroplasticity in children post‐war trauma: A critical review of prefrontal, amygdaloid, and hippocampal alterations
R. Grace1; M. Polestino 2; B. Carr3
1College of Medicine, University of Florida, Gainesville, FL, USA; 2College of Liberal Arts and Science, University of Florida, Gainesville, FL, USA; 3Department of Psychiatry, University of Florida College of Medicine, Gainesville, FL, USA
Background and Aims: This literature review endeavors to amalgamate current understanding of the impact of war trauma on neuroplasticity in children, with a specific focus on the prefrontal cortex, amygdala, and hippocampus. It examines the intricate interplay between these brain regions and their role in the cognitive, emotional, and behavioral development of traumatized children, elucidating how trauma‐induced alterations in these areas contribute to various psychological disorders.
Methods: A comprehensive analysis of peer‐reviewed journals was conducted, emphasizing neuroimaging studies (MRI and fMRI) that reveal changes in brain volume, activity levels, and functional connectivity in the prefrontal cortex, amygdala, and hippocampus. Attention was given to studies showcasing the effects of trauma on the developmental trajectory of these brain regions, including both adaptive and maladaptive neuroplasticity.
Results: The review delineates significant neuroplastic changes in the prefrontal cortex, amygdala, and hippocampus of children exposed to war trauma. It highlights a reduction in prefrontal cortex volume, associated with impaired decision‐making and emotion regulation; amygdala hyperactivation, linked to increased anxiety and stress responses; and hippocampal volume reduction, correlated with memory impairments and altered stress regulation. Additionally, it discusses variations in neuroplastic responses based on the age at which trauma was experienced.
Conclusion: This review integrates diverse findings to provide a nuanced understanding of the neuroplastic changes in children following war trauma, underscoring the critical need for specialized therapeutic interventions. These insights are pivotal for developing strategies to mitigate the long‐term psychological and neurobiological impacts of such trauma, with a view towards fostering resilience and recovery in affected children.
Disclosure: Nothing to disclose.
EPO‐632
Clinical, humanistic, and economic burden of Rett syndrome: A systematic review
D. May 1; M. Gill2; M. Arregui3; S. Cadarette2
1Acadia Pharmaceuticals, San Diego, CA, USA; 2Xcenda L.L.C, part of Cencora, Conshohocken, PA, USA; 3Xcenda GmbH, part of Cencora, Hannover, Germany
Background and Aims: Rett syndrome is a rare neurodevelopmental disorder characterized by severe functional impairment. A systematic literature review was conducted to examine the clinical, humanistic, and economic burden associated with Rett syndrome and its treatment.
Methods: Literature from relevant databases (through June 2023), recent congress proceedings, and clinical trial registries was reviewed. References were independently screened by two authors. Predefined outcomes from highly relevant publications were extracted and validated.
Results: Data were extracted from publications reporting on clinical (n = 40), humanistic (n = 32), and cost/healthcare resource use (n = 11) outcomes (Figure 1). Only 7 trials designed to assess treatment effect on clinical severity or other key components of Rett syndrome specified a primary endpoint (Table 1). Trofinetide led to significant improvement of the co‐primary endpoints. Dextromethorphan polistirex led to a significant improvement in some clinical outcomes though the primary endpoint was not met. Mixed findings, including life‐threatening safety concerns, were reported with glatiramer acetate. Mecasermin was associated with symptom worsening. Across humanistic outcomes, physical functioning and physical component quality of life scores were generally low while caregiver burden was high. Direct costs and healthcare resource utilization were high in the few studies reporting these outcomes.
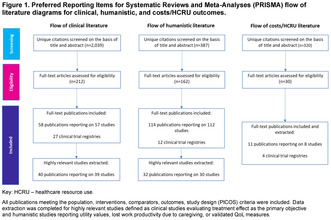
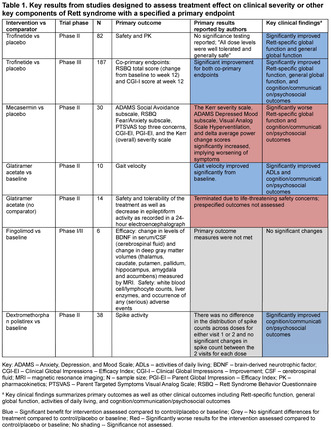
Conclusion: Rett syndrome is associated with significant challenges including limited functional abilities for those affected, substantial cost, and caregiver burden. Several potential treatments have been studied but only trofinetide has been evaluated in a phase 3 trial and been approved in the US. Future research should consider the impact of this approval on the burden associated with Rett syndrome.
Disclosure: DM is employed by Acadia Pharmaceuticals Inc. MG, MA, and SC are employed by Cencora which received funds from Acadia Pharmaceuticals to support this research.
EPO‐633
Parsonage‐Turner disease due to SEPTIN9 mutation: First report of an Italian family
F. Germano 1; L. Bosisio2; M. Cataldi3; M. Grandis4; B. Tappino5; M. Traverso6; C. Solaro1; L. Nobili2; C. Fiorillo2
1Neurology Unit, E.O. Ospedali Galliera, Genoa, Italy; 2Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health Department of Neuroscience (DINOGMI), University of Genoa, Italy; 3Child Neuropsychiatry Unit, IRCCS G. Gaslini Institute, Genoa, Italy; 4Neurology Clinic, IRCCS, Ospedale Policlinico San Martino, Genova, Italy; 5Central Laboratory of Analysis, IRCCS G. Gaslini Institute, Genoa, Italy; 6UOC Medical Genetic, IRCCS G. Gaslini Institute, Genoa, Italy
Background and Aims: Parsonage Turner disease is a neuralgic amyotrophy (NA) of the brachial plexus including idiopathic and rare hereditary forms (HNA). SEPTIN9‐associated mutations have been involved. We report a HNA Italian family carrying a missense variant and reviewed related literature.
Methods: We provide clinical, electrophysiologic and genetic data of an 8‐year‐old girl with an HNA heterozygous pathogenic variant of SEPTIN9‐gene and her affected father. A PubMed search was performed for cases of neurological diseases associated with SEPTIN9‐mutations.
Results: A 6 years Italian girl with normal development came to our institute for pain in both shoulders with scapular girdle asymmetric hypotrophy, hyposthenia and hypotonia and dysmorphic features (hypotelorism, neck skin folds). No abnormalities were detected on NCS (nerve‐conduction‐study). After two years no more episodes of limbs pain were reported. NCS/EMG were repeated showing only chronic denervation signs. A closer look at the family history revealed that the child's father suffered from two episodes of transient upper‐limbs pain/weakness in the past. Genetic test showed a heterozygous SEPTIN9‐gene variant (c.262C>T;p.Arg88Trp) inherited from her father. We reviewed 107 subjects (49M, 58F) with SEPTIN9‐mutations (Three missense mutations and several SEPTIN9‐gene duplications); symptoms onset 13 years, time onset‐diagnosis 22 years. Typical NA features were founded.
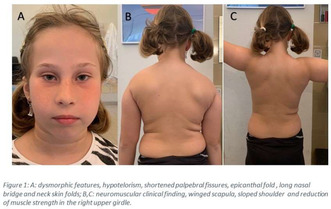
Dysmorphic features.
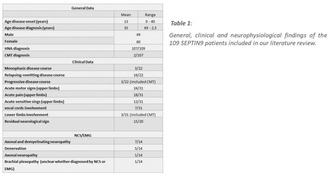
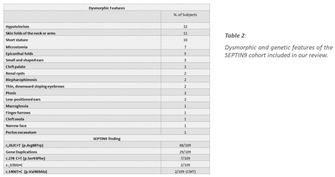
Conclusion: To the best of our knowledge, this is the first case of SEPTIN9‐gene mutation associated with an HNA phenotype in an Italian family. The reported subjects’ phenotypes don’t appear related to the mutation type. Clinicians should consider HNA diagnosis in children with family history of upper‐limbs neuralgia and dysmorphic features in order to improve long‐term clinical outcome.
Disclosure: No disclosure.
EPO‐634
Sex‐specific gut microbiome changes in a novel mouse model of autism
G. O'Byrne 1; C. Fernando2; M. Quartey1; R. Heistad1; J. Hill2; D. Mousseau1
1Cell Signalling Laboratory, Department of Psychiatry, University of Saskatchewan, Saskatoon, Canada; 2Western College of Veterinary Medicine, University of Saskatchewan, Saskatoon, Canada
Background and Aims: A bidirectional relationship has been demonstrated between the gut microbiome and the central nervous system. Though this field of study is still nascent, the so‐called ‘Gut‐Brain Axis’ (GBA) has been implicated as a major factor in neurological and psychiatric disease. TgsAPPα mice, which carry the transgene for human soluble amyloid precursor protein alpha, exhibit behavioral, neurochemical, and immunological phenotypes analogous to Autism Spectrum Disorder (ASD).
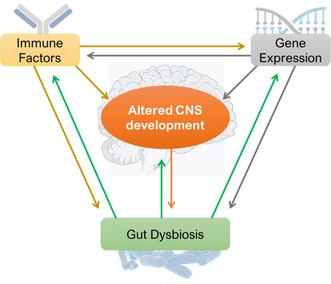
Role of the Gut‐Brain‐Axis in Autism Spectrum Disorder.
Methods: To further investigate the relationship between ASD and the GBA, we profiled the gut microbiomes of 3‐month old heterozygous TgsAPPα mice and age‐ and sex‐matched wildtype littermates, using cpn60 barcode sequencing.
Results: Pooled male and female data revealed differences in the proportional abundances of Bacteroides coprophilus, Pseudoflavonifractor capillosus, Bacteroides caecimuris, and Akkermansia muciniphila between TgsAPPα and wildtype groups. Stratifying the data for sex revealed a decrease in the proportional abundance of Prevotella dentalis, Lachnoanaerobaculum umeaense, and Clostridium amygdalinum in TgsAPPα males (cf. wildtype males) and an increase in the abundance of Flavonifractor sp. in TgsAPPα females (cf. wildtype females). The proportional decrease of Akkermansia muciniphila observed was maintained in TgsAPPα mice, regardless of sex.
Conclusion: Our observations reinforce established links between Akkermansia muciniphila and ASD, and support the future use of TgsAPPα mice as a translational model for the development of microbiota‐bases therapies for ASD.
Disclosure: Nothing to disclose.
EPO‐635
Rotational vertebral artery syndrome in a pediatric patient
I. Albajar Gomez 1; J. Equiza1; P. Iruzubieta1; G. Nuñez1; J. Larrea2; M. Imaz3; B. Laña3; O. Martinez‐mugica3; I. de Goñi4; I. Martí3
1Neurology, Donostia University Hospital; 2Radiology, Donostia University Hospital; 3Pediatrics, Donostia University Hospital; 4Neurosurgery, Donostia University Hospital
Background and Aims: Rotational vertebral artery syndrome is an uncommon cause of vertebrobasilar stroke. Literature concerning pediatric patients is scarce.
Methods: We report a rare pediatric case of bow hunter's syndrome with illustrative neuroimaging findings.
Results: A 10‐year‐old patient, without relevant medical or family history, presented with cerebellar ataxia and nystagmus due to his third stroke since age 6. In previous episodes, etiologic studies were negative. Brain‐MRI (image 1) showed multi‐territory acute and chronic ischemic strokes. Brain‐MRI showed an acute ischemic stroke in the cerebellum on Diffusion‐WI (A), as well as contralateral lacunar chronic ischemic lesions on T2‐WI (B). The previous episode presented as an acute right thalamic lesion with an intense restriction on Diffusion‐WI (C) which initially misguided us towards metabolic and mitochondrial diseases. Cardiologic and hematologic tests were normal. His brain‐CTA, brain‐MRA, metabolic tests, vasculitis panel and exome for mitochondrial pathology were reported as normal. He underwent an angiography and CTA reconstruction (image 2). Angiography (A) revealed a basilar artery embolism, suggesting a proximal active embolic source, and a pseudo‐aneurysmatic dilation of the vertebral artery. CTA reconstruction showed the left vertebral artery compressed by a protrusion of the inferior facet of the atlas (B), known as rotational vertebral artery syndrome or bow hunter's syndrome. Following excision, the patient has remained asymptomatic.
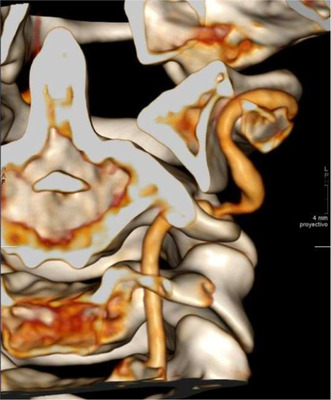
CTA reconstruction shows the left vertebral artery compressed by a protrusion of the inferior facet of the atlas.
Conclusion: Rotational vertebral artery syndrome must be ruled out in pediatric patients with vertebrobasilar strokes.
Disclosure: Nothing to disclose.
EPO‐636
Epidemiology of autism spectrum disorder in children in Kazakhstan: Data from UNEHS 2014–2021
K. Mussina; D. Syssoyev; A. Gaipov; D. Poddighe; D. Galiyeva
Department of Medicine, School of Medicine Nazarbayev University, Astana, Kazakhstan
Background and Aims: We aimed to describe incidence and prevalence of Autism Spectrum Disorder (ASD) and examine factors associated with all‐cause hospitalizations in children registered in the Unified National Electronic Healthcare System (UNEHS) in 2014–2021 in Kazakhstan.
Methods: Cohort comprised of patients less than 18 years old with ASD defined according to the International Classification of Diseases, 10th revision (ICD‐10) as codes: F84.0‐F84.1, registered in the UNEHS from 2014 to 2021. Socio‐demographic factors were analyzed using descriptive, bivariate and multivariable statistical analyses. ASD incidence and prevalence were calculated per 100,000 population. Cox proportional hazard regression analysis was performed to examine factors associated with all‐cause hospitalizations.
Results: Cohort consisted of 8,660 children with ASD, 6,834 (78.9%) were males and 6,384 (73.7%) were urban residents. The mean age at diagnosis was 6.0 ± 2.2 years. The majority of hospitalizations were due to psychiatric/neuropsychiatric cause (73%). Number of hospitalized children with ASD increased from 305 to 1053 patients from 2014 to 2021. Median follow‐up was 2.8 (1.2–4.9) years. Pediatric ASD incidence rate increased from 9.0 to 25.8 per 100 000 from 2014 to 2021. Period prevalence rate significantly raised from 6.7 to 130.2 per 100 000 from 2014 to 2021. Age specific ASD incidence was highest for 6–10 years age group. Younger age, having GI disorders, anemia, epilepsy, hydrocephalus and cerebral palsy are significantly associated with all‐cause hospitalizations.

TABLE 1 Socio‐demographic characteristics of pediatric patients (0–17 years old) by hospitalizations registered in UNEHS with ASD between 2014–2021 in Kazakhstan.
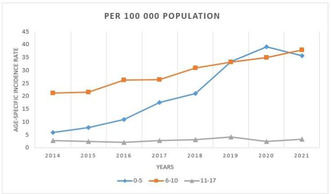
FIGURE 1 Age‐specific incidence rate of pediatric ASD cohort in Kazakhstan for the period 2014–2021.

TABLE 2 Cox PH regression analysis on predicting association between socio‐demographic factors and all‐cause hospitalization among pediatric ASD patients from 2014–2021.
Conclusion: The incidence and prevalence rates increased significantly during the study period. Younger age and comorbidities such as GI disorders, anemia, epilepsy, hydrocephalus and cerebral palsy are significantly associated with all‐cause hospitalizations.
Disclosure: Nothing to disclose.
EPO‐637
Early but not delayed cannabinoid treatment augments hypothermic neuroprotection after neonatal asphyxia
M. Chillida 1; J. Alart1; G. Beldarrain1; A. Álvarez1; A. Bouzier‐Sore2; D. Alonso‐Alconada1
1Department of Cell Biology and Histology, School of Medicine and Nursing, University of the Basque Country (UPV/EHU), Leioa, Spain; 2Centre de Résonance Magnétique des Systèmes Biologiques, CNRS, University of Bordeaux, Bordeaux, France
Background and Aims: Neonatal hypoxic‐ischemic encephalopathy is one of the main causes of adverse neurological disabilities in newborns. Therapeutic hypothermia (TH) is the standard treatment used in clinics; unfortunately, it is not efficient in all cases. Promising new treatments are being investigated and cannabinoids have gained importance due to their neuroprotective properties. In a preclinical model of hypoxia‐ischemia (HI), we aimed to establish the treatment window of the cannabinoid URB447 combined with TH.
Methods: On postnatal day 7, 101 Sprague Dawley rats were subjected to ischemia (left common carotid artery ligation) followed by hypoxia (120 min, 8%oxygen/92%nitrogen). The experiment included sham‐operated controls (n = 10). After HI, rats were cooled at 32.5–33°C for 3 h (TH‐only; n = 32). URB447 administration (i.p. 1 mg/kg) was before (URB447 + TH, n = 13) or after (TH + URB447 n = 33) the TH. The neuroprotective effect of the combined therapy was analyzed by histopathology.
Results: Animals that received URB447 before TH showed augmented hemispheric neuroprotection (95.08%) compared to TH‐only (72.93%) and TH + URB447 (50.93%). This was further confirmed in the hippocampus, with percentage values of 98.54%, 45.49% and 40.29%, respectively. The tissue loss was also reduced when administering the compound before TH: URB447 + TH animals showed 9.51% of tissue loss, significantly lower (p < 0.05) than those for TH‐only (27.56%) and TH + URB447 (29.70%).
Conclusion: These results suggest that the administration of the cannabinoid URB447 before TH, but not after cooling, exerts adjuvant neuroprotective effects in a rat model of neonatal hypoxia‐ischemia.
Disclosure: Acknowledgments: Grant MINECOR20/P66 funded by MCIN/AEI/10.13039/501100011033 and by “ERDF A way of making Europe”, UPV/EHU predoctoral grant (PIFBUR22/03).
EPO‐638
URB447 reduces white matter demyelination and cerebral asymmetry and improves motor function after hypoxia‐ischemia
M. Chillida 1; J. Alart1; G. Beldarrain1; A. Álvarez1; A. Bouzier‐Sore2; D. Alonso‐Alconada1
1Department of Cell Biology and Histology, School of Medicine and Nursing, University of the Basque Country (UPV/EHU), Bizkaia, Spain; 2Centre de Résonance Magnétique des Systèmes Biologiques, CNRS, University of Bordeaux, Bordeaux, France
Background and Aims: Perinatal hypoxia‐ischemia may cause white matter injury, leading to newborn morbidities. Although therapeutic hypothermia (TH) is efficient, a substantial number of babies suffer from behavioral impairments. Here, we wanted to assess white matter demyelination and long‐term outcomes after the administration of the CB1‐antagonist/CB2‐agonist drug URB447 combined with TH in a model of neonatal asphyxia.
Methods: 117 Sprague Dawley rats were subjected to hypoxia‐ischemia (HI) by left common carotid artery electrocoagulation + 2 h at 8%oxygen/92%nitrogen on postnatal day 7 (P7). TH‐treated rats were maintained at 32.5–33°C for 3 h. URB447 was administered immediately after HI. Resulting groups were: Sham (n = 18), HI (n = 34), HI+TH (n = 44) and HI+URB447+TH (n = 21). White matter was assessed at P14 by immunohistochemistry for myelin basic protein (MBP) and motor impairments evaluated at P40‐P42 and P90.
Results: HI+URB447+TH obtained the best results on protecting white matter, with higher MBP ratios (1.01; p < 0.05) than HI (0.34) and HI+TH‐only (0.69), and similar to Sham (1.00). The cylinder test revealed no signs of hemiparesis or cerebral asymmetry in the combined therapy group (−5.57%; p < 0.05), unlike HI (43.37%) or HI+TH‐only (43.17%). Motor coordination was also better in the combined therapy group: Sham (190.5), HI (120.3), HI+TH‐only (111.8) and URB447+TH (171.3).
Conclusion: CB1‐antagonist/CB2‐agonist drug URB447 enhanced hypothermia by ameliorating both white matter injury and long‐term motor function in a preclinical model of neonatal encephalopathy.
Disclosure: Acknowledgments: Grant MINECOR20/P66 funded by MCIN/AEI/10.13039/501100011033 and by “ERDF A way of making Europe”, UPV/EHU predoctoral grant (PIFBUR22/03).
EPO‐639
Motor ability and neural correlates in children with aromatic L‐amino acid decarboxylase deficit
Y. Lee 1; H. Lee2; W. Hwu2; L. Chou1
1Department of Physical Therapy and Assistive Technology, National Yang Ming Chiao Tung University, Taipei, Taiwan; 2Department of Medical Genetics, National Taiwan University Children's Hospital, Taipei, Taiwan
Background and Aims: Aromatic L‐amino acid decarboxylase deficit (AADCD) is a rare, autosomal recessive neurometabolic disorder resulting in impaired or delayed motor development. Traditional motor assessment tools were unsuitable for AADCD children due to variable motor ability among individuals. Cortical neural activity and connectivity are associated with the maturation of the motor system in typically developed children. This study aims to use EEG to explore the relationship between motor ability and cortical neural activity in children with AADCD.
Methods: Children with definitive diagnosis of AADC deficiency and were older than 24 months were recruited. Cortical activity (32‐channel EEG system, ANT Neuro, Netherlands) was collected during the resting and the execution of arm reaches. The arm reach performance was graded by the Grasping and Reaching Assessment of Brisbane (GRAB). The EEG data were divided into motor preparation and execution segments. Power spectral densities of the C3, Cz, and C4 channels were calculated in the alpha and beta frequency range. The Spearman correlation test measured the correlation between reaching abilities and power spectral density. The significant level is established at p < 0.05.
Results: Eight individuals who underwent gene therapy were enrolled; one participant demonstrated a GRAB score of 1, while the remaining participants all scored GRAB 3. Our preliminary results showed that AADC individuals with lower GRAB scores exhibited lower alpha power spectrum density in the resting phase.
Conclusion: Our findings provide a preliminary observation of the relationship between cortical neural activities and motor ability in AADCD children.
Disclosure: Nothing to disclose.
EPO‐640
Understanding lived experiences with KCNQ2‐development and epileptic encephalopathy (KCNQ2‐DEE) – Parent interviews
M. Potashman 1; K. Rudell2; L. Abetz‐Webb3; N. Suminski2; R. Doma2; A. Gold2; K. Jarodia2; C. Buckley2; M. Ridley2; J. Lerner1; J. Mather1; V. Coric1; J. Millichap4; A. Berg5
1Biohaven Pharmaceuticals, Inc; 2Parexel International, US, UK and India; 3Patient‐Centered Outcomes Assessments, Ltd. Bollington, Macclesfield, UK; 4Department of Neurology, Northwestern University Feinberg School of Medicine, Chicago, IL, USA and Precision Epilepsy, PLLC, Chicago, IL, USA; 5Department of Neurology, Northwestern University Feinberg School of Medicine, Chicago, IL, USA and DEE‐P Connections, Washington, DC, USA
Background and Aims: While quantitative descriptions of KCNQ2‐DEE have been provided from in‐depth survey data, limited qualitative interview‐based data exists describing the patient‐caregiver experiences with KCNQ2‐DEE and the burden of disease. We performed this study to develop KCNQ2‐DEE conceptual models to illustrate the disease‐ and quality of life (QoL)‐related experiences and identify its most burdensome aspects.
Methods: One‐on‐one interviews were conducted with US‐based parental caregivers of children (1–18 years‐old, September through November 2023) with mild, severe, and profound KCNQ2‐DEE phenotypes. Parents were recruited via a patient advocacy group (KCNQ2 Cures Alliance). Semi‐structured interviews were audio recorded, transcribed, coded and analysed by ATLS.TI, following established qualitative research methods. Concept saturation was assessed, and 4 models were derived – one for each phenotype severity level and one overall model. The most burdensome disease aspects were discussed (rated on a 0–10 scale).
Results: Based on interviews with 53 parents, the most common concepts reported were communication difficulties, gross and fine motor problems, and chewing/eating difficulties; each worsening with increasing phenotype severity and with age. Communication challenges was the most burdensome symptom (mean = 8.6/10, n = 47, 87% participants). Epileptic seizures were a key concern in infancy, but once adequately controlled were rated as one of the least burdensome symptoms post‐infancy (mean = 5.0/10, n = 23, 43% participants).
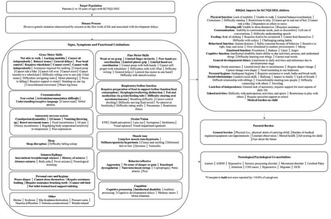
FIGURE 1 Parent‐informed conceptual model (inclusive of all phenotypes and ages).
Conclusion: KCNQ2‐DEE is a multifactorial condition that manifests through numerous symptoms, resulting in significant impacts on the child and parent. These findings identify the outcome domains important to families and patients that could inform measurement tools and endpoint selection in future therapeutic trials.
Disclosure: This study was sponsored by Biohaven Pharmaceuticals, Inc. ATB has received consulting fees from Biogen, Biohaven Pharmaceuticals Inc, and Encoded Therapeutics; Speakers bureau for Biomarin Pharmaceuticals. JL, GL, and MHP have received personal compensation for serving as an employee of Biohaven Pharmaceuticals. JM has received royalties or licenses from UpToDate; received consultancy fees from Biohaven, Eisai, Neurocrine, and Xenon; received speaker honoraria from Biomarin and Greenwich; has participated in a Data Safety Monitoring Board for Praxis; and serves on the board of directors for Child Neurology Foundation (unpaid). Parexel International has conducted the study on behalf of Biohaven Pharmaceuticals, Inc. LAW received compensation from Parexel International for serving as a pediatric clinical outcomes assessments expert on the project.
EPO‐641
Identification of neonates through prospective newborn screening for metachromatic leukodystrophy
L. Laugwitz1; T. Mechtler2; N. Janzen3; P. Oliva2; C. Teunissen4; F. Bürger5; J. Janda5; M. Döring6; P. Martin7; M. Weitz6; P. Lang6; S. Beck‐Woedl8; C. Chanson9; M. Essing 9; H. Rosewich1; B. Streubel10; D. Kasper2; S. Gröschel1
1Neuropediatrics, General Pediatrics, Diabetology, Endocrinology and Social Pediatrics, University of Tuebingen, University Hospital Tübingen, Tübingen, Germany; 2ARCHIMEDlife Medical Laboratories, Vienna, Austria; 3Screening‐Laboratory Hannover, Hannover, Germany; 4Neurochemistry Laboratory, Department of Laboratory Medicine, Amsterdam Neuroscience, Neurodegeneration, Amsterdam UMC, Vrije Universiteit Amsterdam, The Netherlands; 5Metabolic Laboratory, Center for Pediatric Metabolic Medicine, University Children's Hospital Heidelberg, Heidelberg, Germany; 6Department of General Pediatrics and Hematology/Oncology, University Children's Hospital, University Hospital Tübingen, Tübingen, Germany; 7Department of Neurology and Epileptology, Hertie Institute for Clinical Brain Research, University Hospitals Tubingen, Tubingen, Germany; 8Institute of Medical Genetics and Applied Genomics, University of Tuebingen, Germany; 9Orchard Therapeutics (Europe) Ltd., London, UK; 10Department of Pathology, Medical University of Vienna, Vienna, Austria
Background and Aims: Metachromatic leukodystrophy (MLD) is a lysosomal storage disorder caused by arylsulfatase A (ARSA) deficiency, leading to toxic sulfatide accumulation. Symptom onset varies, causing neurological deterioration. Pre‐symptomatic interventions like autologous hematopoietic stem cell gene therapy (arsa‐cel) for early‐onset and hematopoietic stem cell transplantation (HSCT) for late‐onset show success. This study details the first prospective newborn screening (NBS) for MLD, focusing on management and treatment experiences.
Methods: First‐tier dried blood spot (DBS) samples from 109,259 newborns in the German NBS program were analyzed using electrospray ionization tandem mass spectrometry for sulfatide levels. Next‐generation sequencing of the ARSA gene in samples with elevated sulfatides was conducted in the second tier. Confirmation involved assessing ARSA enzyme activity in blood, urinary sulfatides, and genetic sequencing. Identified neonates followed a standardized care pathway for management and treatment.
Results: Elevated sulfatide levels were found in 386 neonates, and genetic sequencing revealed ARSA gene variants in three samples. Conventional diagnostic testing confirmed MLD in all three cases. Two predicted with early‐onset MLD underwent successful pre‐symptomatic arsa‐cel treatment at 9 months, while the third, predicted with late‐onset MLD, was scheduled for allogeneic HSCT between 2 and 5 years.
Conclusion: This study highlights NBS for MLD's technical feasibility and high efficiency, emphasizing specificity and sensitivity. Disease onset prediction in three neonates allows timely treatment or monitoring following a standardized care pathway.
Disclosure: Lucia Laugwitz, Nils Janzen, E. Teunissen6, Friedericke Buerger, Joachim Janda, Michaela Döring, Marcus Weitz, Pascal Martin, Stefanie Beck‐Woedl, Samuel Gröschel, hendrik Rosewich: Nothing to discolose Thomas P. Mechtler, Petra Oliva, Berthold Streubel, David Kasper are Archimedlife employees. Charlotte 0, Charlotte Chanson, Mirko M. Essing are Orchard employees.
EPO‐642
Neuroimmunological indicators of children with autism spectrum disorders
N. Khusenova; Y. Madjidova
Tashkent Pediatric Medical Institute
Background and Aims: Various neurochemical systems (glutamatergic, GABAergic, etc.) play an important role in the activity and maturation of the central nervous system. This makes it necessary to clarify and revise the existing hypotheses of the pathogenesis of neuropsychiatric diseases in children with ASD.
Methods: 45 children with ASD (main group; MG) were examined. Determination of neurotropic autoantibodies (NAAB) was performed using standard procedures of solid‐phase immunoassay ELI‐N‐Test and test kits "Immunculus". The control group consisted of 20 practically healthy children of similar age (control group, CG).
Results: when assessing the average content of S100B protein in serum of the children of the MG children, a significant increase was observed in comparison with that of the CG children (p = 0.005). In 14 (31%) children with ASD, S100B values were slightly higher or at the upper limit of the norm in contrast to CG children. In children with ASD, there was a 12.4‐fold increase in NSE relative to normal values (5.46 ± 0.84 vs. 0.44 ± 0.03; p < 0.001). The appearance of decreased indices of antibodies to OBP in serum testifies to the disruption of the blood‐brain barrier, most significant in patients with ASD (0.69 ± 0.02 vs. 0.35 ± 0.03; p < 0.05). There was a 12.3‐fold increase in GFAP values relative to normal values (0.37 ± 0.008 versus 0.03 ± 0.002; p < 0.001).
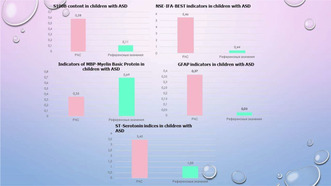
The content of neuroproteins in children with ASD was analyzed.
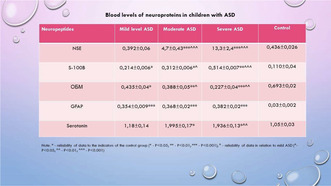
Blood levels of neuroproteins in children with ASD.
Conclusion: Thus, in children with ASD, there is an imbalance in neuroimmunological status, so there is an increase in the level of S100B, NSE, GFAP, and a decrease in OBP.
Disclosure: To investigate the role of neuroproteins in the blood of children with autism spectrum disorders.
EPO‐643
Deriving reference limits for visual evoked potentials from historical data
P. Omland 1; R. Li2; T. Szczepanski3; M. Engstrøm1; M. Uglem1; T. Sand1; K. Nilsen3
1Department of Neurology and Clinical Neurophysiology, St. Olavs Hospital, Trondheim, Norway; Department of Neuromedicine and Movement Science, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology, Trondheim, Norway; 2Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology, Trondheim, Norway; 3Department of Neurology and Clinical Neurophysiology, Oslo University Hospital, Oslo, Norway
Background and Aims: Neurophysiological methods, including visual evoked potentials (VEP), rely on valid and accurate reference limits. VEP variables vary between laboratories, and may change over time because of changes in equipment and procedures. Therefore, there is a need for laboratory specific and updated reference limits. The traditional method for development of reference limits from healthy subjects has several ethical, practical, and economical challenges. We attempt to bypass these challenges by generating reference limits for VEP from historical data using the extrapolated norms (e‐norms) method.
Methods: In the Norwegian DIGMINE project we have collected data from 1500 adult patients examined with pattern‐reversal VEP at the section of Clinical Neurophysiology at St. Olavs University Hospital in Trondheim. VEP for 1138 and 362 patients were recorded on a Keypoint‐Classic system (2006–2018) and a TruTrace‐system (2018–2023) respectively. VEPs were recorded with a standardized procedure. Using e‐norms we calculated reference limits for VEP variables, including P100 latency and N70‐P100 amplitude.
Results: The resulting reference limits (+3SD) for P100 latency were 111 ms for both systems combined, 110 ms for the TruTrace‐system and 112 ms for the Keypoint‐system. The resulting reference limits (−3SD) for N70‐P100 amplitude were 2.5, 2.7 and 2.3 μV respectively.
Conclusion: Historical data can efficiently be used to calculate reference limits for VEP. The resulting reference limits were similar but slightly stricter than those currently used in clinical practice at our laboratory. Our results indicate that historical data can be useful for developing and maintaining reference limits, and for monitoring data quality and effects of changes in equipment and procedures.
Disclosure: Nothing to disclose.
EPO‐644
Quality care for people with CDKL5 deficiency disorder: An expert panel opinion on the European patient journey
S. Amin 1; R. Møller2; A. Aledo‐Serrano3; A. Arzimanoglou4; P. Bager5; S. Jóźwiak6; G. Kluger7; S. López‐Cabeza8; R. Nabbout9; C. Partridge10; S. Schubert‐Bast11; N. Specchio12; R. Kälviäinen13
1University Hospitals Bristol, Bristol, UK; 2Danish Epilepsy Centre, Dianalund, Denmark; Faculty of Health Sciences, University of Southern Denmark, Odense, Denmark; Member of the European Reference Network for Rare and Complex Epilepsies (ERN EpiCARE); 3Vithas Madrid La Milagrosa University Hospital, Vithas Hospital Group, Madrid, Spain; 4University Hospitals of Lyon, Lyon, France; San Juan de Dios Children's Hospital, Barcelona, Spain; Member of the European Reference Network for Rare and Complex Epilepsies (ERN EpiCARE); 5CDKL5 Deutschland e.V., Mainz, Germany; 6The Children's Memorial Health Institute, Warsaw, Poland; Member of the European Reference Network for Rare and Complex Epilepsies (ERN EpiCARE); 7Epilepsy Center for Children and Adolescents, Vogtareuth, Germany; Paracelsus Medical University, Salzburg, Austria; 8Asociación de Afectados CDKL5, Madrid, Spain; 9Necker‐Enfants Malades Hospital, Université Paris Cité, Imagine Institute, Paris, France; Member of the European Reference Network for Rare and Complex Epilepsies (ERN EpiCARE); 10CDKL5 UK, Somerset, UK; 11Epilepsy Center Frankfurt Rhine‐Main, Goethe‐University and University Hospital Frankfurt; LOEWE CePTER, Goethe‐University; University Children's Hospital, Goethe‐University and University Hospital Frankfurt, Frankfurt am Main, Germany; 12Bambino Gesu' Children's Hospital, IRCCS, Rome, Italy; Member of the European Reference Network for Rare and Complex Epilepsies (ERN EpiCARE); 13University of Eastern Finland and Epilepsy Center, Kuopio University Hospital, Kuopio, Finland; Member of the European Reference Network for Rare and Complex Epilepsies (ERN EpiCARE)
Background and Aims: Introduction: CDKL5 deficiency disorder (CDD) is a rare genetic disorder characterised by seizures and neurodevelopmental delays from infancy. To address the lack of evidence‐based guidelines for standardised care of CDD in Europe, clinical experts and patient advocacy group (PAG) representatives from Europe convened to map the patient journey and provide consensus on how to ensure quality care in routine clinical practice within the European setting.
Methods: Methods: Semi‐structured one‐to‐one interviews were conducted by a third‐party agency. Insights were collated into a visual representation of the Europe‐specific clinical journey in CDD. Workshops followed to reach consensus, and validate the journey, and to identify challenges and provide expert opinion on potential solutions.
Results: Results: The CDD patient journey has three elements: clinical presentation/diagnosis, seizure management and multidisciplinary care. Clinical criteria for CDD diagnosis include seizure semiology and age at epilepsy onset. Genetic testing is crucial for diagnosis, allowing for appropriate seizure management, multidisciplinary care and outcomes. When planning pharmacotherapy, the refractory and variable seizure semiology, comorbidities, effects of polypharmacy and safety profiles of concomitant medications should be considered. Multidisciplinary collaboration and specialist access are essential for long‐term care, support and improved quality of life, each adapting with the changing needs of the patients. The expert group highlighted disparity in management approaches and available resources; therefore, cross‐country knowledge‐sharing is key.
Conclusion: Conclusion: To achieve quality care of people with CDD, European practice recommendations are required that align on realistic treatment goals, diagnostic criteria and management approaches, and are adaptable.
Disclosure: Editorial support was provided by AXON Communications, supported by Orion Corporation.
Education & history of neurology
EPO‐645
Abstract withdrawn
EPO‐646
Abstract withdrawn
EPO‐647
Optimising continuing medical education: Exploring learning trends and preferences among European and US neurologists
P. Chen; J. White; C. Forde; C. Walsh
PeerVoice, Luxembourg, Luxembourg
Background and Aims: To optimise continuing medical education (CME) tailored for neurologists, this study investigates neurologists’ CME participation patterns and preferences.
Methods: In 2023, a 20‐minute electronic survey was administered to practicing neurologists in Europe and the United States. Recruitment employed the LiMA network of validated healthcare professionals. Question sequences were randomised to mitigate response bias. Each clinician was remunerated in their local currency for participating.
Results: Data were collected from 50 neurologists. Peer‐reviewed journal articles (92%) and CME websites (70%) are the top two channels that neurologists used frequently to acquire medical information. Measured using a 5‐point scale, content credibility (4.18) and clinical applicability (4.16) were rated as being notably more important than interactivity (2.96) and format novelty (2.84) in driving neurologists’ CME participation. Most neurologists reported spending ≤20 minutes per online CME engagement (72%), and identified “having to complete assessment questions to access the education” as a barrier to their CME participation (80%). Linear regression analysis demonstrated a positive correlation (b = 0.16, p < 0.05) between neurologists' CME participation and increased frequencies of self‐reported clinical practice change implementation. Primary changes implemented occurred in treatment plan management (59%), screening and/or diagnosis (51%), and patient monitoring (41%).
Conclusion: CME design needs to prioritize content over format. The identified barriers, notably the time constraints and compulsory assessment questions, highlight the importance of eliminating roadblocks to CME participation. The alignment between clinical practice change and CME participation amongst neurologists validates the effectiveness of CME in driving critical clinical behaviour to improve patient care.
Disclosure: Nothing to disclose.
EPO‐648
PhD and clinician‐scientist pathway among neurology residents and junior neurologists in Europe – A survey from the RRFS
V. Carvalho 1; T. Kobulashvili2; L. Cuffaro3; N. Vashchenko4; G. Sferruzza5; A. Gonzalez‐Martinez6; A. Accoroni7
1Department of Neurosciences and Mental Health (Neurology), Hospital Santa Maria‐CHLN; 2Department of Neurology, Neurocritical Care, and Neurorehabilitation, Christian‐Doppler University Hospital, Paracelsus Medical University, Centre for Cognitive Neuroscience, Member of EpiCARE, Salzburg, Austria; 3School of Medicine and Surgery, University of Milano‐Bicocca, Milan, Italy; 4Department of Neurology, Danish Headache Center, Copenhagen University Hospital – Rigshospitalet, Glostrup, Copenhagen, Denmark; 5Vita‐Salute San Raffaele University, Milan, Italy; 6Department of Neurology and Immunology, Hospital Universitario de la Princesa & Instituto de Investigación Sanitaria Princesa (IIS‐Princesa), Madrid, Spain; 7Department of Clinical Neurosciences, Neurology Unit, Geneva University Hospital, Geneva, Switzerland
Background and Aims: The decreasing number of clinician‐scientists in neurology underscores the urgency of understanding the challenges encountered by early‐career professionals to safeguard the future of academia in neurology. Our aim is to explore the characteristics of Ph.D. programs across Europe and the main challenges faced when embarking on an academic career.
Methods: From September to December 2023, an online survey was sent through email to EAN‐RRFS members.
Results: We obtained 297 valid responders. 49% were residents, 43% had completed training, and 85% aspired to become a clinician‐scientist. Of the 82% who were doing research, 39% were enrolled in a Ph.D. programme and 15% already completed one. Ph.D. access and graduation criteria varied significantly and 74% of the respondents believed that better harmonization of PhD programs could be beneficial. Less than half of the Ph.D. were fully funded, with universities (31%) and governmental bodies (20%) being the most frequent funding sources. The most commonly perceived challenges included combining clinical activities with research (59%) and finding funding (52%). Among Ph.D. students, over 60% experienced stress, struggled with time management and maintaining a work/life balance, with around one‐third expressing concerns about lack of supervision/communication from their supervisor.
Conclusion: We provide insight into the structure, content, perceived benefits, and challenges of doing a Ph.D. in Europe, as well as the difficulties perceived by early career neurologists entering research. Future measures could address these challenges to reduce the barriers for trainees to access a career in Academia.
Disclosure: Nothing to disclose.
EPO‐649
Assessing the digital care pathways unmet needs for rare brain diseases: The case of phenylketonuria
S. Cannizzo1; V. Quoidbach 2; E. Treacy3; A. Hermida4; A. McDonald5; M. Scarpa6; F. Van Spronsen7; E. Lange8; B. Sheehan‐Gilroy9; T. Hagedorn10; A. Bak11; G. Turchetti1
1Institute of Management, Scuola Superiore Sant’Anna, Pisa, Italy; 2European brain Council, Brussels, Belgium; 3National Centre for Inherited Metabolic Disorders, Mater Misericordiae University Hospital, Dublin, Ireland; 4Universidad de Santiago de Compostela, Santiago de Compostela, Spain; 5Dietetic Department, Birmingham Children's Hospital, Birmingham, UK; 6Center for Rare Diseases, Udine University Hospital, Udine, Italy; European Reference Network For Hereditary Metabolic Diseases (MetabERN); 7Beatrix Children's Hospital, University Medical Centre of Groningen (UMCG), The Netherlands, European Reference Network For Hereditary Metabolic Diseases (MetabERN); 8The European Society for Phenylketonuria and allied disorders; 9Munster Technological University Kerry Campus, Tralee, Ireland, PKU Association of Ireland; 10German PKU and Allied Disorders Patients Association DIG PKU, European Society for Phenylketonuria & Allied Disorders; 11Universidad Nacional de Educación a Distancia. Federación Española de Enfermedades Metabólicas Hereditarias. European Society for Phenylketonuria and Allied Disorders
Background and Aims: Digital Care Pathways for Rare Brain Diseases research project (2023–2024) is coordinated by the European Brain Council. The study is looking at unmet needs while using digital care pathways and aims to assess benefits of digital tools from patient's perspective after COVID‐19 pandemic, presenting the phenylketonuria (PKU) case‐study.
Methods: A survey was co‐designed with PKU patients’ representatives, translated into German and Spanish, and anonymously launched in EU Survey platform. The survey contained demographic questions, 13 questions about patient unmet needs on information, communication and education, 8 questions regarding patients' experience on access to care pathways during the COVID‐19, and 13 questions on the role of digital tools in supporting PKU management.
Results: 75 respondents (59% patients, 41% parents) participated to the survey. Information about PKU and communication between patient and healthcare professionals are extremely important (44% and 60%), and education on digital platforms for the management of PKU is very important (47%). Digital tools are needed for sharing information and for communicating before the clinic visit (75%) and enhance understanding the information provided for treatment or monitoring (90%). On day‐to‐day PKU management, Apps, wearables, e‐mail, telephone call could help in understanding information received from center and for communication (90%).
Conclusion: Treatment management and care delivered to PKU patients demonstrated benefits and interest for more use of digital tools in management and follow‐up. Preliminary results provided valuable insight into understanding needs of PKU patients and defining best channels to engage and communicate with them. While looking at patient perspective, clinician perspective is equally important.
Disclosure: The study received financial support from Pfizer.
EPO‐650
Persistent postural perceptual dizziness (PPPD) in the neurology clinic
K. Radhakrishna; M. Gaughan; C. Russel
Neurology, St. Vincent's University Hospital, Dublin, Ireland
Background and Aims: Persistent postural perceptual dizziness (PPPD) is a recently introduced diagnosis which may be underrecognized. The Bárány Society has defined the condition as persistent dizziness/unsteadiness for ≥3 months causing significant functional impairment. Diagnosis is made clinically and vestibular diagnostic tests and neuroimaging are typically negative. The objectives of the study were to determine the proportion of referrals to a General Neurology New Patient Clinic which met the diagnostic criteria of PPPD and to determine response to treatment.
Methods: In this retrospective review, referral letters of 1315 patients to a General Neurology New Patient Clinic from 2021–2023 were screened for terms ‘dizziness’, ‘vertigo’, ‘unsteadiness’ and ‘vestibular’. A chart review was performed to establish the group that met the diagnostic criteria for PPPD. Follow‐up correspondences was reviewed to establish response to treatment.
Results: 202 (15.4%) patients were referred with ‘Dizziness’, ‘Vertigo’ or ‘Unsteadiness’. 22 (1.7%) patients fulfilled the diagnostic criteria of PPPD. 10 (45.5%) were treated with Venlafaxine, conferred ≥50% subjective improvement of symptoms for 8 (80%) patients. Vestibular physiotherapy improved symptoms by ≥25% in 7 (100%) patients. CBT and effective communication of the diagnosis alone alleviated symptoms by 50% in 3 (14%) patients respectively.
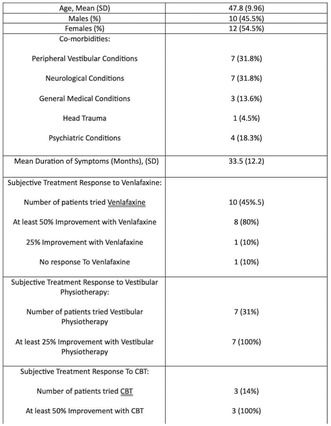
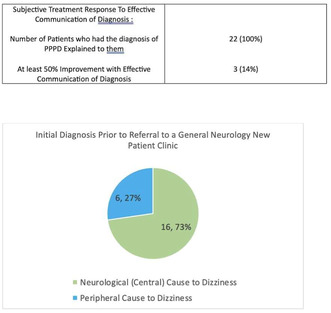
Conclusion: PPPD is a relatively common neurological condition, should be considered in patients with chronic vestibular symptoms which result in significant functional morbidity. In this cohort, treatment with Venlafaxine and vestibular physiotherapy resulted in significant improvement in symptoms.
Disclosure: Nothing to disclose.
EPO‐651
Online education improves specialists' knowledge and competence on management of depression in people with epilepsy
L. Thevathasan 1; K. Carpenter1; C. Scot‐Smith1; M. Mula2; L. Sander3
1Medscape LLC, London, UK; 2St George's University of London, London, UK; 3UCL Queen Square Institute of Neurology, London, UK
Background and Aims: To evaluate whether an online educational programme directed at European‐based specialists, could improve knowledge on identification of depression in people with epilepsy and competence relating to management of depression in people with epilepsy.
Methods: The educational activity was a 15‐minute online video with 2 European experts in Epilepsy. Educational effect was assessed using a 3‐question repeated pairs, pre/post assessment survey. A paired‐samples t‐test was conducted to assess overall number correct and confidence change. p values < 0.05 (McNemar's test) are statistically significant. Cohen's d test was used for magnitude of effect of education on the overall outcomes (knowledge). The activity launched on 29 September 2023 and data analysed as of 11 December 2023.
Results: 461 neurologists and 196 psychiatrists participated in the programme, of which 54 neurologists and 39 psychiatrists completed pre‐ and post‐assessment tests. Significant improvements were seen for both groups, with an average correct response rate of 33% and 27% pre‐assessment, which increased to 69% and 64% post‐assessment, for neurologists (p < 0.001; Cohen's d = 1.12) and psychiatrists (p < 0.001; Cohen's d = 1.11) respectively. Table 1 provides further results for each learning objective. Based on a self‐reporting question, neurologists expressed a 61%, and psychiatrists expressed a 59%, increase in confidence following the education in managing depression in people with epilepsy.
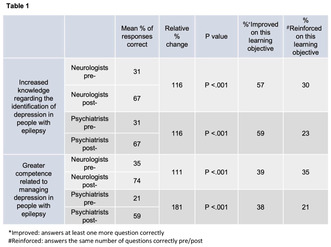
Table expressing knowledge and competence changes for neurologists and psychiatrists before and after education.
Conclusion: This study demonstrates the positive effect of online medical education on specialists’ knowledge, competence and confidence in managing comorbid depression in people with epilepsy in Europe.
Disclosure: Lionel Thevathasan, Katherine Carpenter and Camille Scott‐Smith are employed by Medscape LLC. An unrestricted educational grant for this programme was provided by Angelini Pharma. Marco Mula and Ley Sander have nothing to disclose.
EPO‐652
Online medical education improves specialists’ knowledge on selecting antiseizure medications in people with epilepsy
L. Thevathasan 1; K. Carpenter1; C. Scot‐Smith1; R. Thomas2
1Medscape LLC, London, UK; 2Newcastle University Newcastle upon Tyne, UK
Background and Aims: Post‐pandemic education is variable, so we evaluated whether an online educational programme directed at European‐based specialists, could improve knowledge on appropriate selection of antiseizure medications (ASMs) for people with focal epilepsy, particularly relating to mechanisms of action and latest clinical trial data.
Methods: The educational activity was a 29‐minute online video with 1 European expert in Epilepsy. Educational effect was assessed using a 3‐question repeated pairs, pre/post assessment survey. A paired‐samples t‐test was conducted to assess overall number correct and confidence change. p values < 0.05 (McNemar's test) are statistically significant. Cohen's d test was used for magnitude of effect of education on the overall outcomes (knowledge). The activity launched on 15 June 2023 and data analysed as of 20 October 2023.
Results: 2,214 neurologists and 769 psychiatrists participated in the programme, of which 218 neurologists and 38 psychiatrists completed pre‐ and post‐assessment tests. Significant improvements were seen for both groups, with an average correct response rate of 49% and 31% pre‐assessment, which increased to 72% and 47% post‐assessment, for neurologists (p < 0.001; Cohen's d = 0.80) and psychiatrists (p < 0.001; Cohen's d = 0.63) respectively. Table 1 provides further results for each learning objective. Based on a self‐reporting question, neurologists expressed a 43%, and psychiatrists expressed a 34%, increase in confidence following the education in knowledge on antiseizure medication selection.
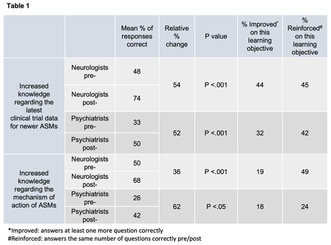
Table of results expressing changes in knowledge on mode of action and clinical trial data before and after education.
Conclusion: This study demonstrates the positive effect of online medical education on specialists’ knowledge and confidence in selection of antiseizure medications for people with focal epilepsy in Europe.
Disclosure: Lionel Thevathasan, Katherine Carpenter and Camille Scot‐Smith are employed by Medscape LLC. Rhys Thomas has nothing to disclose. This educational programme was supported by an unrestricted educational grant by Angelini Pharma.
EPO‐653
Online medical education improves specialists’ knowledge and confidence on sudden unexpected death in epilepsy
L. Thevathasan 1; K. Carpenter1; C. Scot‐Smith1; R. Shankar2; P. Ryvlin3; T. Tomson4
1Medscape LLC, London, UK; 2University of Plymouth Peninsula School of Medicine Plymouth, UK; 3Department of Clinical Neurosciences Lausanne University Hospital (CHUV) Lausanne, Switzerland; 4Department of Clinical Neuroscience Karolinska Institute, Stockholm, Sweden
Background and Aims: To evaluate whether an online educational programme directed at European‐based specialists, could improve knowledge and confidence relating to SUDEP, specifically the risks of SUDEP and desire among patients and caregivers to receive this information.
Methods: The educational activity was a 36‐minute online video with 3 European experts in Epilepsy. Educational effect was assessed using a 3‐question repeated pairs, pre/post assessment survey. A paired‐samples t‐test was conducted to assess overall number correct and confidence change. p values < 0.05 (McNemar's test) are statistically significant. Cohen's d test was used for magnitude of effect of education on the overall outcomes (knowledge). The activity launched on 3 August 2023 and data analysed as of 9 October 2023.
Results: 598 neurologists and 326 psychiatrists participated in the programme, of which 76 neurologists and 39 psychiatrists completed pre‐ and post‐assessment tests. Significant improvements were seen for both groups, with an average correct response rate of 32% and 22% pre‐assessment, which increased to 76% and 58% post‐assessment, for neurologists (p < 0.001; Cohen's d = 1.22) and psychiatrists (p < 0.001; Cohen's d = 1.04) respectively. Table 1 provides further results for each learning objective. Based on a self‐reporting question, neurologists expressed a 54%, and psychiatrists expressed a 51%, increase in confidence following the education in discussing SUDEP with patients/caregivers.
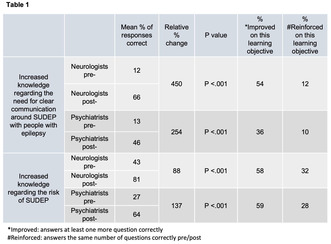
Table of results expressing changes in knowledge relating to need for communication and risk associated with SUDEP before and after education.
Conclusion: This study demonstrates the positive effect of online medical education on specialists’ knowledge and confidence in risks associated with and communication on SUDEP in Europe.
Disclosure: Lionel Thevathasan, Katherine Carpenter and Camille Scot‐Smith are employed by Medscape LLC. Rohit Shankar, Philippe Ryvlin and Torbjörn Tomson have no disclosures. This educational programme was supported by an unrestricted educational grant by Angelini Pharma.
EPO‐654
Abstract withdrawn
EPO‐655
Antiseizure prophylaxis in routine neurosurgery practice: Urgent need for training
L. Manzo 1; A. Pascarella2; S. Gasparini2; O. Marsico2; D. Tedeschi2; G. Idone2; R. Di Iorio2; D. Abelardo2; V. Cianci1; E. Ferlazzo2; U. Aguglia2
1Regional Epilepsy Centre, Great Metropolitan “Bianchi‐Melacrino‐Morelli Hospital”, Reggio Calabria, Italy; 2Department of Medical and Surgical Sciences, Magna Græcia University of Catanzaro, Italy
Background and Aims: Prophylactic antiseizure medications (ASMs) to prevent early and late seizures after craniotomy is not currently recommended, yet it is a common practice among neurosurgeons. This study investigates decision‐making strategies regarding post‐craniotomy ASM prescription in Italian Neurosurgery Units.
Methods: An online cross‐sectional survey was conducted (November 2022‐March 2023). The survey link was distributed via email to neurosurgeons of 110 Italian Pediatric and Adult Neurosurgery Units. The survey comprised 11 multiple‐choice questions addressing ASM prescription for individuals without seizures or those experiencing early post‐surgical seizures. Questions explored type and timing of prescribed ASMs, factors influencing decision, and drug withdrawal management.
Results: Eighty‐two neurosurgeons from 64/110 Neurosurgery Units answered the survey. Forty‐two out 82 (52.1%) neurosurgeons prescribed post‐craniotomy ASMs for individuals without seizures: 9 routinely prescribed ASMs, 33 only under specific conditions (e.g., febrile seizures history, familiarity for epilepsy) or based on the surgical site. Levetiracetam was the most prescribed ASM (41/42; 97.6%). Thirty‐one (73.8%) surgeons initiated ASMs before surgery. Thirty‐two (39%) surgeons planned withdrawal within 6 months while 10 (10.2%) chose later suspension. Seventy‐nine (96.3%) neurosurgeons prescribed ASM (mostly levetiracetam: 77/79; 97.5%) after an early post‐surgical seizure. Only 4 (5.1%) surgeons routinely discontinued ASMs within 1 month, while 43 (54.4%) suspended them within 6 months and 32 (40.5%) continued beyond 6 months. Notably, 42 neurosurgeons managed ASM treatment independently, while 40 sought neurologist assistance.
Conclusion: This survey revealed widespread adoption of ASM prophylaxis after craniotomy in neurosurgery practice, despite lack of evidence about its usefulness, emphasizing the urgent need for training in this area.
Disclosure: Nothing to disclose.
EPO‐656
Gender disparities among neurology residents classifications in Portugal
F. Ladeira1; P. Faustino2; M. Soares 2; V. Carvalho3
1Multiple Sclerosis Centre of Integrated Responsibility, Saint Joseph's Local Health Unit, Lisbon, Portugal; 2Neurology Department, Saint Joseph's Local Health Unit, Lisbon, Portugal; 3Neurology Department, Saint Mary's Local Health Unit, Lisbon, Portugal
Background and Aims: Gender disparities in medical professions have long been a subject of concern, with research consistently pointing to the role of implicit bias in shaping differential career outcomes for men and women. This study endeavors to investigate whether gender‐based differentials exist in the evaluation of Neurology residents in Portugal.
Methods: We collected publicly available data encompassing gender (as a social construct), grades and rankings from two pivotal assessments administered at the beginning and ending of Neurology Residency: the National Board Exam (NBE) and Neurology Exam (NE), respectively. The NBE is a multiple‐choice gender‐blinded evaluation, whereas the NE involves an oral gender‐unblinded evaluation.
Results: Our analysis revealed that 36.5% of women and 21.6% of male residents achieved the superior quartile of the NBE ranking, which reflects a similar representation among top classifications when accessed through a gender‐blinded exam. On the contrary, the proportion of male residents on the top classification of NE, a gender‐unblinded evaluation, was more than twice higher than women (37.8% vs. 18.3%, p < 0.05), indicating a statistically significant disparity in performance between genders in the oral examination setting (Table 1).
Conclusion: The findings of the present study may imply that there are nuanced disparities in women's career as a neurologist resident in Portugal. Although the recruitment seems relatively balanced between genders, the gender‐unblinded assessments unveil significant discrepancies favoring men.
Disclosure: Nothing to disclose.
EPO‐657
Burnout, depression and anxiety among neurology residents in Türkiye: A preliminary report
İ. Arslan1; B. Kılboz2; D. Arslan 3; C. Ayvacıoğlu Çağan4; T. Saltoğlu5; M. Topçuoğlu6
1Gazi University Medical Faculty Neurology Departmant; 2İstanbul Prof. Dr. Cemil Taşcıoğlu City Hospital; 3Sincan State Hospital; 4Bozkır State Hospital; 5Ankara Bilkent City Hospital; 6Hacettepe University Medical Faculty Neurology Departmant
Background and Aims: Neurology residency is a long and difficult journey in which the physical and mental well‐being of trainees are essential for their clinical and academic success. This ongoing study aims to determine the mental status and factors that affect mental health of neurology residents in Türkiye and therefore improve the quality of neurology training.
Methods: Neurology residents throughout Türkiye were invited to take part in an online survey by the support of Turkish Neurological Association. Additionally to demographic and institutional data of all participants; Minnesota Job Satisfaction Questionnaire, Maslach Burnout Inventory, Beck Anxiety Inventory and Beck Depression Inventory were assessed.
Results: Anxiety was found in 62%, depression in 63.3% and burnout in 44% of the participants (n: 79). In correlation analyses, an increase in the duration of neurology training was associated with lower levels of depression (r: −0.21, p: 0.05) and anxiety (r: −0.34, p: 0.002). Working long hours was associated with a decrease in job satisfaction (r: −0.22, p: 0.04) and an increase in depression (r: 0.24, p: 0.02). Job satisfaction scores increased with more time devoted to education (r: 0.28, p: 0.01) and research (r: 0.22, p: 0.04). The presence of depression was less in residents who were able to rest after night shift (p: 0.01).
Conclusion: Preliminary data from our ongoing study demonstrates a high prevalence of burnout, depression, and anxiety among neurology residents in Türkiye. To reduce these factors, it may be beneficial to decrease the daily working hours, increase the time allotted for education and research, and provide rest after night shifts.
Disclosure: The current results are preliminary and the study continues.
EPO‐658
Ethical and neurological dimensions of Dr. Robert G. Heath's deep brain stimulation experiments
B. De1; M. Polestino 2; B. Carr3
1School of Medicine, University of California San Francisco, San Francisco, CA, USA; 2College of Liberal Arts and Science, University of Florida, Gainesville, FL, USA; 3Department of Psychiatry, University of Florida College of Medicine, Gainesville, FL, USA
Background and Aims: This historical analysis revisits the pioneering yet ethically contentious deep brain stimulation (DBS) experiments of Dr. Robert Galbraith Heath. Heath's work in the mid‐20th century focused on targeting limbic system components, such as the open‐brain targeting of septal area, amygdala, and thalamus, aiming to unravel neurological foundations of psychiatric disorders. This retrospective study scrutinizes the specific neural circuits and neurotransmitter systems engaged in Heath's DBS trials, alongside their profound ethical implications.
Methods: A detailed examination of Heath's seminal publications and experiment records, particularly those documenting the septal stimulation for modulating depressive symptoms, the B‐11 implant for psychiatric disorders, and interventions in schizophrenia and homosexuality, was conducted. The analysis involves a comprehensive review of limbic system circuitry, specifically the role of septal nuclei, amygdaloid complex, and thalamic connections, in conjunction with the dopaminergic and serotonergic pathways implicated in Heath's studies.
Results: Heath's DBS experiments revealed notable alterations in limbic circuitry functioning, particularly highlighting the role of septal and amygdaloid stimulation in modulating emotional and behavioral responses. The B‐11 implant trials underscored the intricate interplay between deep brain regions in psychiatric symptomatology. Additionally, Heath's work raised pivotal ethical concerns regarding patient consent and the invasive nature of DBS, catalyzing a reevaluation of research protocols in neuropsychiatry.
Conclusion: Heath's forays into DBS epitomize a seminal yet polarizing epoch in neurology, spotlighting the nascent interplay between limbic neuromodulation and psychiatric therapeutics. This retrospection not only venerates his pioneering ethos but also subtly adumbrates the era's nascent ethical paradigms, affirming Heath's indelible imprint on the neurological vanguard.
Disclosure: An artifact supplementing this study is a book on psychosurgery, containing Heath's personal annotations and signature, providing a unique historical perspective.
EPO‐659
The history of Danish neuroscience
O. Paulson 1; A. Schousboe2; H. Hultborn3
1Neurobiology Research Unit, Department of Neurology, Rigshospitalet and University of Copenhagen, Faculty of Health and Medical Science, Copenhagen, Denmark; 2Department of Drug Design and Pharmacology, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark; 3Department of Neuroscience, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark
Background and Aims: The history of Danish neuroscience dates back at the 17th century, and was from the start linked to clinical disciplines. This continued in the 19th and 20th century with new initiatives linking basic neuroscience to clinical neurology and psychiatry. From the middle of the 20th century, basic neuroscience was developing rapidly within the preclinical university sectors. Clinical neuroscience continued and was even reinforced during this period with important translational research.
Methods: Literature review.
Results: Some highlights: Steno (1638–1686) was active in many scientific fields. Among his main contributions to neuroscience was the investigation of the anatomy of the pineal gland. René Descartes had proposed how the pineal gland was the seat of the soul, acting by rotation to distribute animal spirits. Steno demonstrated that the pineal gland was merely grey matter with black spots. In the 19th century Carl Lange (1834–1900) had main contributions in neurology and psychiatry. He rode a book in Danish, “On emotions – Psycho‐Physiological Study” in 1885, translated to German, French and English. Fritz Buchthal (1907–2003) had a main role in the Danish and international development of clinical neurophysiology and especially electromyography. Niels A. Lassen (1926–1997) main research field was the cerebral circulation. He, his group and collaborators were the first to demonstrate that activation led to blood flow increase – functional activation. Finally, Jens Christian Skou (1918–2018) received the Nobel Prize in 1997 for the discovery of the sodium‐potassium pump.
Conclusion: Danish Neuroscience has a strong history.
Disclosure: Nothing to disclose.
Neuro‐oncology
EPO‐660
Hemifacial spasm of central origin due to structural cause
A. Lorenzo Montilla; S. López Anguita; B. Gutiérrez Ruano; A. Muñoz González; C. Alarcón Morcillo; M. Olmedilla
Department of Neurology, Hospital Central de la Defensa Gómez Ulla
Background and Aims: Hemifacial spasm is a peripheral movement disorder consisting of irregular clonic/tonic involuntary movements of muscles innervated by the facial nerve. Its principal cause is an hyperexcitability of its nucleus or an abnormal transmission of the proximal nerve segment, usually of compressive origin due to a vascular structure; some atypical cases are caused by brain tumors, mainly infratentorial location. We present a case with central origin due to supratentorial lesion.
Methods: A 60‐year‐old male under neurology follow‐up for epilepsy (motor focal aware seizures) of structural cause (right frontal SOL: non mutated IDH diffuse glioblastoma, TERT mutation, WHO CNS4), went to the emergency room because of arrhythmic spasmodic movements in bilateral frontal region (predominantly left), left orbicularis oculi and left hemiface. Thinking of continuous partial epilepsy, anti‐seizure medication was increased, without any improvement. Asking again, these movements could be in relation to a distony: they improve during sleep and with sensory tricks and exacerbates with light, nervousness and speech, so infiltrations with botulinum toxin were performed, with marked improvement.
Results: Brain MRI: right fronto‐parietal cortical thickening with obliteration of the sulci, hypertense on T2 / FLAIR and hypointense on T1, affecting opercular area and pre/post‐central gyri; small subcortical pseudonodular area (12 × 5 mm) with subtle hypersignal in diffusion and a faint ring enhancement; stable compared to the previous one.
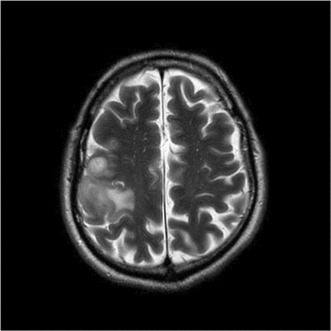
Brain MRI, axial T2.
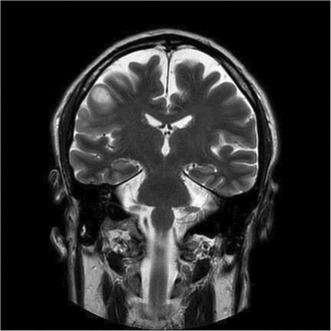
Brain MRI, coronal T2.
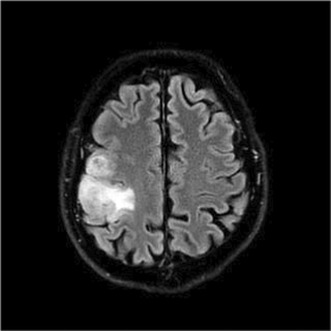
Brain MRI, axial FLAIR.
Conclusion: Hemifacial spasm due to supratentorial tumors may be explained by affectation of the contralateral motor cerebral cortex (irritation of the lower motor unit of the facial nerve) based on anatomical investigation in veterinary medicine.
Disclosure: Nothing to disclose.
EPO‐661
A biopsy‐verified case of CNS involvement of mycosis fungoides with positive RT‐QuIC assay
A. Alexandratou 1; E. Petrou1; A. Gamvroula1; A. Antoniou1; P. Vlahou2; G. Kolovos1; E. Alexiou1
1Neurology Department, Evangelismos Hospital, Athens, Greece; 2Pathology Department, Evangelismos Hospital, Athens, Greece
Background and Aims: We report a rare case of positive RT‐QuIC assay in CNS involvement of mycosis fungoides.
Methods: A 73‐year‐old man presented with decreased consciousness and generalized convulsions. He had been formerly diagnosed with mycosis fungoides, which was in full remission. Clinical examination revealed profound cognitive deficits with fluctuating level of alertness during admission. A brain MRI showed multiple contrast‐enhancing lesions in both hemispheres, while a first lumbar puncture indicated lymphocytic pleocytosis with elevated CSF protein.
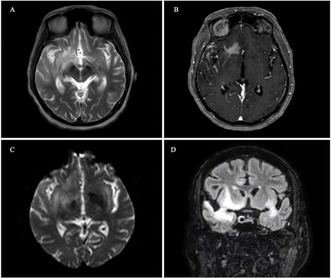
Initial MRI scans of the brain. A. Axial T2 showing high signal in the right temporal lobe, B. Axial post‐contrast scan, demonstrating an area of contrast enhancement in the right temporal lobe, C. Axial DWI, depicting a similar area of high signal in the right temporal lobe, D. Coronal FLAIR with high signal in both temporal lobes and extending to basal ganglia bilaterally.
Results: The rapidly progressive cognitive decline prompted investigations for Creutzfeldt‐Jakob disease (CJD) with 14‐3‐3 and RT‐QuIC assay, both of which came back positive. Meanwhile, flow cytometry analysis reported increased T‐cell population, suggestive of CNS lymphoma. The RT‐QuIC assay remained positive in the second, acellular, lumbar puncture. The CJD diagnosis was not further supported by imaging or EEG findings. A brain biopsy was performed, reporting brain infiltration by a highly malignant T‐cell lymphoma, believed to represent large cell transformation of mycosis fungoides with CD30 expression. Treatment with pulsed steroids had some effect on the level of consciousness, although a degree of memory impairment remained.
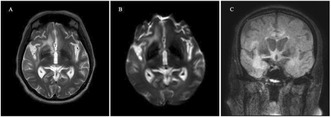
Serial MRI scans of the brain after steroid treatment. A. Axial T2 and B. Axial DWI showing slight improvement of the high signal in the right frontotemporal area. C. Coronal FLAIR demonstrating bilateral temporal high signal to a lesser extent compared to the initial MRI; some areas of high signal are evident in the medial frontal lobes bilaterally. Image degraded my motion artefact.
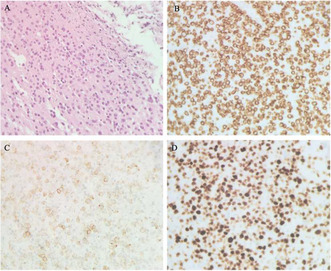
Histological images from the patient's brain biopsy. A. Infiltration of brain parenchyma by medium‐sized lymphocytes with dark chromatin and irregular nuclear membrane (Haematoxylin and eosin × 400 magnification), B. CD3 expression in medium‐sized lymphocytes.
Conclusion: RT‐QuIC assay is able to accurately detect the pathogenic agent (PrPSc), identified to be responsible for CJD occurrence. Positive RT‐QuIC assay has been strongly linked to CJD, with specificity reaching 99%, although it has been suggested that high CSF white cell count and protein can affect the results. The brain biopsy has confirmed CNS involvement of the cutaneous lymphoma; however, a possibility of subclinical coexistence of CJD remains.
Disclosure: Nothing to disclose.
EPO‐662
Primary leptomeningeal sarcomatosis: An exceptional cause of chronic, aseptic meningitis
S. Alejandro 1; U. Patricia1; D. Renata1; V. Ana2; A. Carlos1; G. Guillermina1
1Departamento de Neurología, Hospital Regional Universitario de Málaga; 2Departamento de Anatomía Patológica, Hospital Regional Universitario de Málaga
Background and Aims: Primary leptomeningeal sarcomatosis (PLS) represents less than 1% of primary intracranial tumors and is an even less frequent cause of non‐infectious, chronic meningitis. Therefore, it should be taken into consideration when other causes of chronic meningitis have been dismissed.
Methods: We present the case of a 58‐year‐old man who presented a very suggestive granulomatous, subacute meningitis based on clinical findings. Nevertheless, every microbiological determination tested was negative and there were no specific findings in image tests.
Results: Our patient presented a wide range of symptoms: behavioral disorder, cognitive impairment, right hand drift, facial supranuclear partial palsy but no neck rigidity. Also, during hospitalization the patient developed seizures that required antiseizure medication. CT and MRI found digitiform edema in left parietotemporal lobes, meningeal thickening at that level and communicating hydrocephalus. Lumbar puncture resulted negative for every test underwent, as well as every other diagnostic procedure. Tuberculous meningitis was suspected at first, and antituberculous treatment was initiated. Due to poor evolution, brain biopsy was subsequently performed.
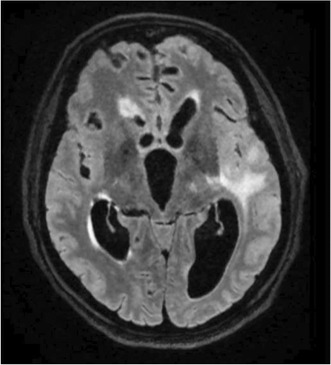
FLAIR‐powered MRI showing digitiform left parietotemporal edema and meningeal thickening at that level.
Conclusion: PLS is an exceptional cause of chronic, aseptic meningitis which must be suspected when other more frequent etiologies are not present. Despite its fatal prognosis, holocranial radiotherapy showed little survival increasing, reaching up to 3 years in certain patients. Therefore, this diagnosis must be considered in certain scenarios.
Disclosure: Nothing to disclosure.
EPO‐663
The Last Bastion – 7 Cases of tectal gliomas with long follow up
D. Antão; J. Costa; J. Marques; I. Costa; D. Salgado
Neurology Department, Instituto Português de Oncologia de Lisboa Francisco Gentil, Lisbon, Portugal
Background and Aims: Brainstem gliomas are an heterogenous group of gliomas that appear predominately during childhood. Mesencephalic gliomas are usually invasive; however, tectal gliomas are a subtype with a slow growth rate. These are low grade gliomas with a relatively benign course, that turn symptomatic when patients develop obstructive hydrocephalus. Permanent neurological deficits are rare.
Methods: This work will explore demographic, clinical and radiological features of 7 patients with tectal gliomas with active follow up at an oncological hospital in Lisbon.
Results: The median age of these patients was 14 years and 57.1% were female. In 4 of 7 cases, the clinical manifestation was supratentorial hydrocephalus demanding neurosurgical treatment – 3 had ventriculoperitoneal shunt placement and 1 had ventriculostomy. The diagnostic was incidental in the remaining. 28.6% of the tumors had a cystic‐like appearance on brain magnetic resonance. The majority (85.7%) had no enhancement after gadolinium injection. Only 1 patient was submitted to neurosurgical biopsy and the histology showed grade II astrocytoma. More than half of the subjects (57.1%) have no neurological deficits. The remaining had pupillary or oculomotor abnormalities. All patients are under surveillance, without treatment, with radiologic stability for many years.
Conclusion: Tectal gliomas are indolent brain tumors whose main symptoms relate to obstructive hydrocephalus. Similarly to the literature, this cohort shows slow growth tumors, with few associated symptoms and sustained imagiologic stability. This entity is a rare case in Neuro‐Oncology as brain biopsy may be dispensed due to the risk of worsening symptoms while not changing patient management.
Disclosure: Nothing to disclose.
EPO‐664
Prognostic impact of surgical resection versus biopsy in patients with primary central nervous system lymphoma (PCNSL)
F. Bruno 1; A. Pellerino1; E. Pronello2; R. Palmiero1; F. Cavallo3; L. Orsucci4; L. Bertero5; F. Rizzo6; F. Cofano6; D. Garbossa6; R. Rudà1
1Division of Neuro‐Oncology, Department of Neurosciences, University and City of Health and Science Hospital, Turin, Italy; 2Neurology Unit, Department of Translational Medicine, University of Eastern Piedmont, Novara, Italy; 3Department of Molecular Biotechnologies and Health Sciences, Division of Haematology, University of Turin, Turin, Italy; 4Division of Hematology, University and City of Health and Science Hospital, Turin, Italy; 5Pathology Unit, Department of Medical Sciences, University of Turin and City of Health and Science University Hospital, Turin, Italy; 6Division of Neurosurgery, Department of Neurosciences, University and City of Health and Science Hospital, Turin, Italy
Background and Aims: Whether surgical resection, as compared to biopsy, may positively affect the outcome of Primary Central Nervous System Lymphoma (PCNSL) patients is controversial. In this study, we compared the clinical characteristics and outcome of PCNSL patients receiving either surgical resection or biopsy in our Institution.
Methods: We retrospectively collected clinical data of PCNSL patients, who underwent biopsy or surgical resection and were subsequently treated in our Institution from 2004 to 2023. Progression‐free survival (PFS) and overall survival (OS) were defined as time from diagnosis and recurrence or death/censoring).
Results: We included 55 patients, with a median age of 66.0 years. 36 (65.5%) showed multifocal lesions at presentation. 32 (58.2%) underwent biopsy, whereas 23 (41.8%) surgical resection. 48 (87.3%) underwent adjuvant methotrexate‐based chemotherapy. Unifocal vs multifocal lesions prevailed among patients undergoing surgical resection (20/23, 87.0%) vs biopsy (15/32, 46.9%), p = 0.002. Median PFS and OS of the whole cohort were 8.0 and 26.0 months. Surgical resection vs biopsy correlated with longer median PFS and OS both in a univariate (mPFS: 64.0 vs 7.0 months, p = 0.031; mOS: 68.0 vs 10.0 months, p = 0.007), and a multivariable analysis (HR 0.390, 0.168–0.907, p = 0.029). Conversely, unifocal vs multifocal presentation was the only variable with a favourable impact on the OS.
Conclusion: In our study, surgical resection, as compared to biopsy, was associated with longer PFS, but not OS, in PCNSL patients. Further studies on larger cohorts are needed to clarify whether surgical resection may be a feasible and safe option to improve survival in selected PCNSL patients.
Disclosure: Nothing to disclose.
EPO‐665
Progressive supra and infratentorial hypermetabolic white matter lesions non‐typical of multiple sclerosis
G. Mena Gomez; M. Carcelen Gadea; E. Sanchez Villanueva; A. Acsente Acsente; H. Coquillat Mora; J. Escudero Torrella; F. Domingo Monge
Department of Neurology, Consorcio Hospital General Universitario de Valencia, Valencia, Spain
Background and Aims: A case report of a patient presenting progressive brainstem symptoms along with progressive supra and infratentorial white matter lesions (WML), hypermetabolic on Positron Emission Tomography‐Computerized Tomography (PET‐CT), mistakenly characterized as demyelinating.
Methods: Descriptive retrospective study of a case.
Results: a 43‐year‐old female presenting with progressive gait instability, paresthesia, left hemiparesis and left inferior facial palsy. Brain Magnetic Resonance Imaging (MRI) showed multiple supra and infratentorial WML, which were characterized radiologically as demyelinating. A total PET‐CT showed hypermetabolic brainstem lesions, with no thoracoabdominal findings. Bloodwork, including tumor markers, autoimmunity serologies (antiMOG and AQ4 antibodies), as well as ophthalmologic slit‐lamp examination and two cerebrospinal fluid (CSF) samples were all unremarkable. A course of intravenous corticosteroids resulted in slight clinical and radiological improvement. Further on, she presented signs of clinical worsening with multidirectional nystagmus, dysphagia, complete left facial and hypoglossal palsy with left hemianesthesia, and growth of the previous lesions in subsequent MRIs. A biopsy of the caudate lesion along with an intraventricular CSF sample were taken, showing findings suggestive of diffuse large B‐cell lymphoma. MATRIX chemotherapy protocol was started, followed by autologous stem cell transplantation, with subsequent clinical and radiological improvement.
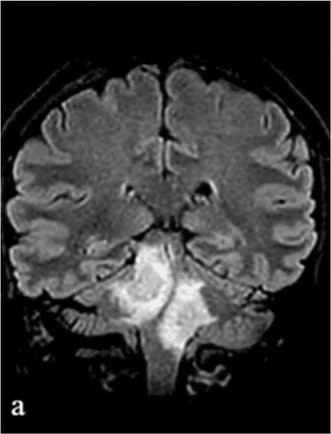
(a) T2‐FLAIR weighted image showing hyperintense bilateral brainstem lesions.
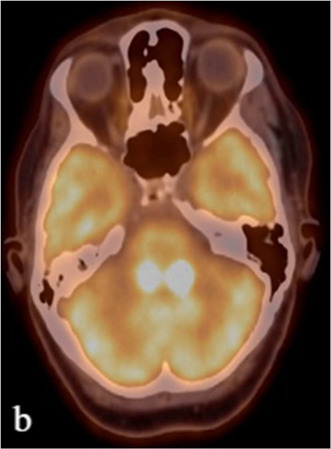
(b) Brain PET‐TC showing hypermetabolic activity in these lesions (calculated as SUV max 21, 8 [right] and 23.8 [left]).
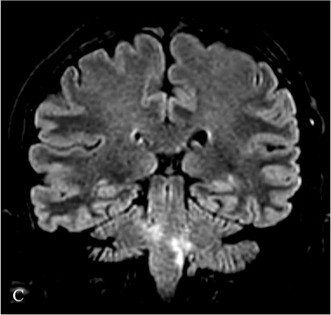
(c) T2‐FLAIR weighted image after 3rd chemotherapy cycle (MATRIX scheme) showing noticeable decrease in the size of the infratentorial lesions.
Conclusion: Primary central nervous system lymphoma is a rare cause of WML, with less than 10% showing infratentorial lesions. Previously associated with AIDS patients, neurologists should have a clinical suspicion in patients showing WML non‐typical of known demyelinating diseases. A transient clinical and radiological improvement after corticosteroids is typical.
Disclosure: The author has no conflict of interest.
EPO‐666
MPNST as a very late complication of radiotherapy: Red flags, diagnostic considerations and role of nerve biopsy
G. Salvucci 1; R. Colombo1; M. Vizziello1; B. Pollo2; M. Grisoli3; G. Marucci2; E. Dalla Bella1; S. Usai1; G. Giaccone2; G. Lauria Pinter1; N. Riva1
1Unit of Neuroalgology, IRCCS Foundation “Carlo Besta” Neurological Institute, Milan, Italy; 2Unit of Neuropathology and Neurology, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy; 3Neuroradiology Unit, Foundation IRCCS Neurological Institute Carlo Besta, Milan, Italy
Background and Aims: MPNST is a rare, aggressive sarcoma that may arise up to many years following radiotherapy. We report a case of a fatal MPNST mimicking at onset an inflammatory brachial plexopathy and we propose diagnostic recommendations based on evidence from a systematic review.
Methods: case report of MPNST and systematic literature review.
Results: A 60‐year‐old female presented with progressive left upper limb proximal weakness. She was known for neck radiotherapy 36 years prior for Hodgkin lymphoma. Cervical MRI, CSF and FDG‐PET were normal. Remarkably, brachial plexus MRI showed nerve roots modest thickening. IvIg and steroids treatment were not effective. Progression of symptoms occurred in the following year, when a new MRI revealed multiple cerebral and cervical T2‐hyperintensities. An intradural biopsy allowed histological diagnosis of MPNST. The patients died 18 months after onset. Our literature review highlighted as major risk factors for post‐radiation MPNST head and neck irradiation (77% of cases), occurred before the age of 35 years (62%). Mean time from radiation was 13.7 years. Importantly, 21/22 (95.5%) of cases presented with focal tumor‐like enlargement, one case had brachial plexopathy without enlargement with hypermetabolism at PET‐FDG. Mean survival from diagnosis in patients that underwent surgery is 14.3 months with 29.4% still alive at the moment of publication.
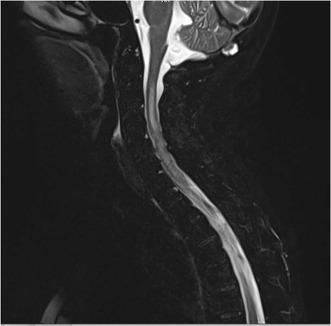
Cervical spine MPNST infiltration at MRI: diffuse C2‐C7 intramedullary hyperintensity on T2‐weighted sequences.
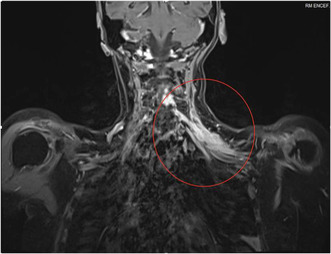
Brachial plexus MRI: T2 hyperintensity, thickening and enhancement of brachial plexus, especially first and second trunk.
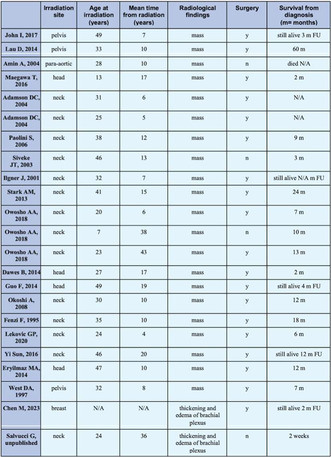
Clinical and radiological characteristics of all malignant peripheral nerve sheath tumors reported in the literature.
Conclusion: post‐radiation MPNST can occur up to 40 years after radiotherapy and it can present as an isolate brachial plexopathy without focal hypermetabolism. Since surgery may be beneficial, close radiological monitoring and early diagnostic biopsy in high‐risk patients with brachial plexopathy is strongly recommended.
Disclosure: Nothing to disclose.
EPO‐667
Extending the spectrum of paraneoplastic syndromes mediated by anti‐Yo antibody
J. Bandeira Costa 1; D. Antão1; A. Opinião2; J. Nunes1; J. Marques1
1Neurology Department, Instituto Português de Oncologia de Lisboa, Lisbon, Portugal; 2Medical Oncology Department, Instituto Português de Oncologia de Lisboa, Lisbon, Portugal
Background and Aims: Stiff‐person syndrome (SPS) is characterized by fluctuating hypertonia and painful muscular spasms increasing with external stimuli being frequently mediated by anti‐GAD antibodies, or amphiphysin antibodies in paraneoplastic variants. We report a case of SPS, preceded by cerebellar ataxia, with positive titles of anti‐Yo antibody.
Methods:
Results: A female patient, 69 years old – with previous history of peritoneal carcinomatosis secondary to Fallopian tube carcinoma, which underwent chemotherapy with carboplatin and paclitaxel and cytoreductive surgery – developed subacute dizziness, axial and appendicular ataxia and memory disturbances during the chemotherapy cycles. While brain‐CT and MRI were normal, EMG documented an axonal sensory‐motor polyneuropathy. Anti‐Yo antibody was positive both in serum and LCR. Assuming a cerebellar degeneration associated with anti‐Yo syndrome, intravenous immunoglobulin and high dose methylprednisolone were started. Due to absence of benefit regarding the ataxia and falls with osteoporotic fractures, treatment was suspended. During the following two months, she developed painful inferior limbs spasms, aggravated by external stimuli, with an ascending pattern of truncal and cervical involuntary muscular contractions, with hypertonia and gait impairment. While maintaining exclusively anti‐Yo antibody positivity, a second EMG registered abundant continuous motor unit potentials detected on the inferior limb muscles, independent of voluntary muscular activity. Neuraxis‐MRI, anti‐GAD and amphiphysin were negative. Gradual recovery of autonomous gait occurred with 9 cycles of monthly IVIG.
Conclusion: We underline the diversity of clinical presentations of SPS while highlighting a possible association with Anti‐Yo antibody, not yet described, and emphasizing the positive therapeutical response.
Disclosure: Nothing to disclose.
EPO‐668
Extranodal NK/T cell lymphoma with primary CNS manifestation – A case report
L. Müller‐Miny; L. Lohmann; O. Grauer
Department of Neurology with Institute of Translational Neurology, University Hospital Münster, Münster, Germany
Background and Aims: Rare extranodal NK/T cell lymphoma (ENKTCL) occurs predominantly in Asian and Latin American countries and preferentially arises in the nasopharynx. Although EBV is normally restricted to B lymphocytes, it has been associated with tumor cells of NK/T cell origin in malignant NK and T cell tumors. EBV increases gene instability, incidence of ENKTCL and enhances escape mechanisms from T cell‐mediated immune responses. We report here a rare case of EBV associated ENKTCL with a primary CNS manifestation and haemophagocytic lymphohistiocytosis (HLH).
Methods: This retrospective case report fulfills the CARE criteria.
Results: The patient initially presented herself for nuclear facial palsy. MRI of the brain showed brain stem lesions and elevated EBV copies were detected in the cerebrospinal fluid. An initial CT scan of the lungs and a sonography of the abdomen revealed no lesions. Over the course of two months, the patient developed progressive clinical symptoms and multilocular CNS lesions. Due to the high EBV copies, a rituximab infusion was performed to deplete the B cells, but did not improve clinical symptoms. The patient successively developed a secondary HLH. A liver biopsy was performed due to the HLH‐associated hepatomegaly, revealed an ENKTCL. An additional brain biopsy detected lymphocytic infiltration consistent with ENKTCL, mainly of NK cells and localized EBV type 1 in the tumor cells.
Conclusion: ENKTCL may initially manifest in the CNS. Unclear CNS lesions with massively increased intrathecal EBV copies may indicate a lymphoma in which malignant cells derived from NK/T cells can be infected with EBV.
Disclosure: Nothing to disclose.
EPO‐669
Successful identification and management of a SMART syndrome occurring 36 years after cranial radiotherapy
L. Lebrun 1; D. Di Perri2; J. Raymackers1; C. Van Ruyssevelt3; V. Marneffe4
1Department of Neurology, Clinique Saint‐Pierre Ottignies, Ottignies‐Louvain‐la‐Neuve, Belgium; 2Department of Radiation Oncology, Cliniques Universitaires Saint‐Luc, Brussels, Belgium; 3Department of Radiology, Clinique Saint‐Pierre Ottignies, Ottignies‐Louvain‐la‐Neuve, Belgium; 4Department of Neurosurgery, Clinique Saint‐Pierre Ottignies, Ottignies‐Louvain‐la‐Neuve, Belgium
Background and Aims: Radiation therapy (RT) is a cornerstone in the management of brain tumors, either alone or combined with surgery and/or systemic therapy. SMART syndrome (stroke‐like migraine attacks after RT) is a rare neurological disease believed to be a late‐onset side effect of cranial RT and consists in stroke‐like symptoms, epilepsy and migraine (Dossin et al., 2023; Shuper et al., 1995). This syndrome has been observed within a timeframe of 1 to 37 years after RT. Pathophysiology is believed to be multifactorial, involving white matter necrosis, vascular endothelial damage, demyelination and gliosis (Ota et al., 2023; Turnquist et al., 2020). We report a case of SMART syndrome presented with severe left hemiparesis and left facial palsy which was successfully managed with steroid pulse therapy (1000 mg/day, 5 days) (Jia et al., 2018; Ota et al., 2023).
Methods: We reviewed literature.
Results: On 4th day of treatment, he was able to walk again with a return to his basis state. Six weeks later, the patient condition was stable without any relapse. Strength on the left side was back to its initial level (i.e., slight paresis without any facial asymmetry).
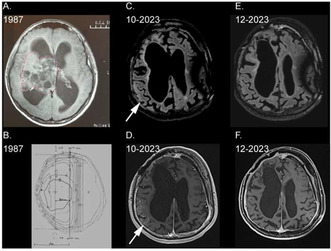
A. T1 MRI sequence showing the tumour at the time of diagnosis (1987). B. Radiation dose distribution for the 24‐Gy sequential boost (1987). C. T2 FLAIR MRI sequence showing hyperintensity of right parieto‐occipital cortex (10‐2023). D. T1 post‐gadoliniu.
Conclusion: In conclusion, we report here a case of successful treatment of SMART syndrome occurring 36 years after RT, which is one of the latest occurrences of this syndrome ever described (Ota et al., 2023). We believe that recognizing SMART syndrome in patients with a history of cranial RT, even after a prolonged period, is crucial to avoid misdiagnosis and subsequent improper treatment.
Disclosure: Nothing to disclose.
EPO‐670
Autoimmune encephalitis in the era of immune‐checkpoint inhibitors: Descriptive study in a tertiary hospital
M. Alanís Bernal 1; A. Zabalza1; A. Vilaseca1; M. Sanz‐Martínez2; L. Viñas Giménez2; X. Montalban1; H. Ariño1
1Department of Neurology and Centre d’Esclerosi Múltiple de Catalunya (Cemcat); Vall d’Hebron University Hospital, Barcelona, Spain; 2Immunology Department, Vall d’Hebron University Hospital, Barcelona, Spain
Background and Aims: This study aims to characterize patients with autoimmune encephalitis (AE) in a tertiary hospital and explore its association with cancer and immune checkpoint‐inhibitors (ICI) treatment, providing valuable insights for effective treatment strategies.
Methods: Retrospective single‐centre study from 2017 to 2023 including patients with antineuronal antibody (ANA) (2 techniques) or with definite immune‐related encephalitis secondary to ICI. We analyzed clinical differences between subgroups with or without cancer and with or without ICI exposure.
Results: Thirty‐one patients were included [64.5% female, median age 59.7 (range 37.9–69.1)] with a median follow‐up of 34.6 months (range 10.5–69.6). Patients had various ANA including GAD65 (n = 6), Hu (n = 4), NMDAR (n = 3), Yo (n = 3), other ANA (n = 13) and two seronegative treated with ICIs. Median PNS‐Care score was 7 (range 4–9.5). 19/31 (61.3%) were cancer‐associated, 8 had neurological symptoms before cancer diagnosis, 7 after ICI and 4 after cancer diagnosis without ICI. Among patients with cancer, 14 were advanced (lymph nodes or distant metastasis) at neurological onset. 5/31 (16.1%) patients deceased, 4 due to tumor progression. Patients with concomitant cancer were older (median 62.0 years [range 49.8–71.0] vs 38.8 [range 21.2–61.6] p < 0.05) and had a shorter time to treatment from disease onset (median 1.2 months [range 0.5–5.0] vs 20.4 [range 3.4–33.3] p < 0.05), without differences in prognosis or ICI treatment in alive patients.
Conclusion: Our study suggests that patients diagnosed with AE in recent years are frequently associated with advanced cancer which is already under treatment. Future studies are needed to optimize the management of this prevalent subpopulation.
Disclosure: Nothing to disclose.
EPO‐671
Outcomes of patients with neoplastic meningitis undergoing ventriculoperitoneal shunting and intrathecal chemotherapy
M. Loghin
Department of Neuro‐oncology, MD Anderson Cancer Center, Houston, TX, USA
Background and Aims: To present the outcomes of a retrospective cohort of patients with leptomeningeal disease (LMD) who received placement of ventriculoperitoneal shunt (VPS) and Ommaya reservoir for intrathecal chemotherapy.
Methods: We performed an in‐depth chart review using electronic medical records of patients with LMD who had undergone placement of VPS and Ommaya in a single institution over a three‐year period.
Results: Eighteen patients with LMD underwent VPS placement and Ommaya reservoir for intrathecal chemotherapy. Eleven patients had breast cancer, four had lung cancer, and the remaining three patients had thyroid, esophageal and uterine cancer respectively. Seventeen patients are deceased, and one patient was lost to follow up, and not included in our analysis. Sixteen (94%) patients had brain metastases. Eleven patients (61.1%) received radiotherapy prior to VPS placement. Karnofsky scores ranged from 60 to 90. Seven (41%) patients did not receive intrathecal chemotherapy due to rapid LMD progression. Ten (59%) patients received intrathecal Topotecan, and one received Cytarabine at the time of disease progression. The overall survival of these patients from time of VPS placement was 15.15 weeks (range 4.1–203.2), of which seven (41%) survived less than eight weeks. Six (60%) patients died from LMD progression, three (30%) from systemic disease progression, and one (10%) died of medical complications.
Conclusion: Our retrospective analysis suggests urgency for early diagnosis of LMD with increased intracranial pressure, along with spinal fluid diversion procedures for intrathecal chemotherapy administration. These interventions may allow for prolongation and improvement in quality of life.
Disclosure: Amulya Gottiparthy, Lauren Orda, Emily Morrow, and Monica LoghinDr. Gottiparthy has nothing to disclose. Mrs. Orda‐Nguyen has nothing to disclose. Mrs. Morrow has nothing to disclose. Dr. Loghin has nothing to disclose.
EPO‐672
Prevalence of systemic neoplasms in a cohort of adult neurofibromatosis 1 patients: A single‐center retrospective study
N. Setola 1; G. Miele1; C. Santoro2; E. Vanore1; F. Napolitano1; M. Melone1
1Center for Neurofibromatosis & Rare Diseases and InterUniversity Center for Research in Neurosciences, Department of Advanced Medical and Surgical Sciences, 2nd Division of Neurology, University of Campania Luigi Vanvitelli, Napoli, Italy; 2Department of Precision Medicine, University of Campania “Luigi Vanvitelli”, Napoli, Italy
Background and Aims: Neurofibromatosis type 1 (NF1), the most frequent hereditary cancer predisposition syndrome, is characterised by occurrence of tumours in both central and peripheral nervous systems (CNS and SNP), with a 5–15% higher risk of developing a neoplasm outside CNS and SNP, compared to general population. Our study aims to assess systemic cancer prevalence in a patient's cohort.
Methods: Demographic and clinical data of NF1 patients, diagnosed according to established international criteria, were analysed.
Results: In a cohort of 127 individuals [54.2% women, median age 44.6 years (SD 17.5)], participating in NF1 surveillance programme for median duration of about 10 years, 13.38% (17/127) had systemic cancer. Patients' mean age at cancer diagnosis was 43.4 years (range 6.84–76.6). Breast cancer (23.8%) was the most frequently encountered malignancy, followed by prostate cancer (17.6%), gastrointestinal (11.8%), gynaecological (11.8%), bone (11.8%), pheochromocytoma (5.9%), melanoma (5.9%) and haematological cancers (5.9%). Except for sex‐unrelated tumours, no difference was found between sexes. However, 2 out of 3 patients with a previous diagnosis of malignant peripheral nerve sheath tumour (MPSNT) developed bladder cancer and pheochromocytoma at a median follow‐up of 3 years, with a significant correlation (p = 0.041).
Conclusion: NF1 patients develop systemic neoplasms more frequently than the general population. Co‐presence of a MPSNT tumour seems to be correlated with an increased risk of developing systemic tumours later in life. Adequate cancer screening in NF1 patients therefore requires a lifelong care model to prevent aggressive cancer development and to improve patients' life expectancy and quality of life.
Disclosure: Nothing to disclose.
EPO‐673
Atypical debut of systemic lymphoma with CNS involvement
P. Garrido Jiménez; S. López Anguita; A. Lorenzo Montilla; J. Rodríguez Quinchanegua; A. Rodríguez Herrera; B. Gutiérrez Ruano; A. Muñoz González; F. Valenzuela Rojas; M. Olmedilla González
Hospital Central de la Defensa “Gómez Ulla”
Background and Aims: CNS involvement in patients with systemic lymphoma is an uncommon complication affecting ≤5% of patients, being even more atypical to debut with neurological manifestations. We present a case debuting with CNS symptoms with final diagnosis of lymphoma.
Methods: A 68‐year‐old male with 5 days of dysarthria, gait disturbance, bradypsychia and incoherent speech after tooth extraction 15 days before with uncertain infection, without fever or other systemic data.
Results: Brain CT was normal, laboratory tests showed hypercalcemia, EEG displayed moderate diffuse encephalopathy and LP showed 10 mononuclear leukocytes/mm3 and hyperproteinorrachia 85 mg/dl without glucose consumption, suspecting possible encephalopathy due to hypercalcemia. The patient's level of consciousness worsened and he was admitted to the ICU requiring OIT. Suspicion of infectious encephalitis led to initiate antibiotic, which was suspended after negative microbiology. LP was repeated with 12 leukocytes/mm3 and hyperproteinuria 53 mg/dl. Given the persistence of non‐infectious inflammatory LP, a complete blood test performed showed pancytopenia, elevated beta2‐microglobulin and LDH, a brain MRI without findings and another EEG with moderate‐severe encephalopathy, so high‐dose corticotherapy was started with excellent response and complete resolution of the symptoms. BM biopsy was normal. In the complementary etiological study, a PET‐CT scan showed a hypermetabolic lesion in the left adrenal gland which was biopsied and demonstrated an intravascular lymphoma. Intrathecal+R‐CHOP systemic chemotherapy was started with poor response.
Conclusion: Intravascular lymphoma is a rare subtype of diffuse large cell B‐cell lymphoma that presents CNS involvement in 30–40% of cases and can be associated with adrenal gland involvement in up to 50–75%. This entity represents an important diagnostic challenge that requires a high clinical suspicion given the wide variability in its presentation and its low incidence.
Disclosure: Nothing to disclose.
EPO‐674
Peri‐ictal Pseudoprogression: A rare entity to bear in mind in patients with brain tumors treated with radiotherapy
T. Mederer‐Fernandez 1; R. Sainz‐Torres1; M. Borrell‐Pichot1; M. Delgado‐Romeu1; E. Granell‐Moreno2; V. Ros‐Castelló1; A. Sierra‐Marcos1
1Neurology Department, Hospital de la Santa Creu i Sant Pau; 2Neuroradiology Department, Hospital de la Santa Creu i Sant Pau
Background and Aims: The differential diagnosis in patients with brain tumors treated with radiotherapy who present with epileptic seizures might be challenging. Apart from tumoral progression, one entity to consider is peri‐ictal pseudoprogression (PIPG). Clinical features include recurrent epileptic seizures or status epilepticus and progressive focal deficits.
Methods: We present the case of a 63‐year‐old woman who presented in the emergency room due to progressive weakness in the left upper limb and recurrent focal motor seizures involving the left face with impaired awareness. She had a history of a grade II oligodendroglioma treated with surgery and adjuvant chemoradiotherapy seven years before. She was on remission accordingly to the brain MRI performed one month earlier.
Results: The electroencephalogram (EEG) showed electrographical seizures involving the right centrotemporal region (Figure A, B). Levetiracetam 1.5 g/12 h was initiated. Due to the persistence of clinical and electrographical seizures in the follow‐up EEGs, lacosamide 150 mg/12 h was added with clinical improvement. However, the brachial paresis persisted. Brain MRI showed a cortical hyperintensity with meningeal enhancement in the right frontotemporal‐parietal region, suggestive of PIPG. Patient was discharged. In the outpatient clinic, there was evidence of motor improvement and a gradual reduction of antiseizure drugs was performed without seizure recurrence.
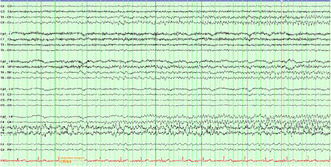
FIGURE A EEG part 1.
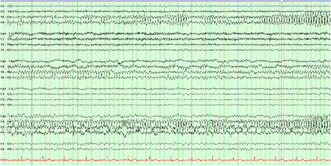
FIGURE B EEG part 2.
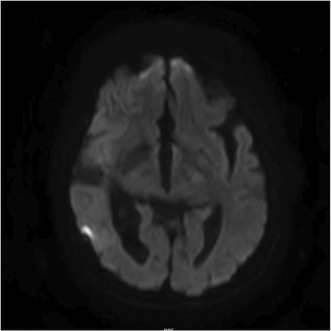
FIGURE C MRI.
Conclusion: PIPG is a rare entity that should be considered in patients treated with radiotherapy who present with typical clinical and neuroimaging features. In the coming years, the incidence is likely to increase due to the recent indication of radiotherapy in low‐grade gliomas, a treatment that was previously reserved for high‐grade gliomas.
Disclosure: Nothing to disclose.
Neurological manifestation of systemic diseases
EPO‐675
Acute intermittent porphyria as a rare cause of pontine and extrapontine myelinolysis: A case report
A. Afanasieva1; M. Palchukovska 2; M. Kholodova1; Y. Korets1; T. Slobodin2
1Department of Neurology and Neurosurgery, LLC “Dobrobut‐Clinic”, Kyiv, Ukraine; 2Department of Neurology, Shupyk National Healthcare University of Ukraine, Kyiv, Ukraine
Background and Aims: Developing of severe hyponatremia attributed to inappropriate antidiuretic hormone secretion during a crisis of acute porphyria can be complicated by central pontine (CPM) and extrapontine myelinolysis (EPM). Usually acute intermittent porphyria (AIP) attacks manifest as a combination of abdominal pain, neuropsychiatric symptoms, and autonomic dysfunction.
Methods: A single case presentation.
Results: A 24‐year‐old female was admitted with a clinical and MRI signs of EPM and CPM. During 3 weeks before admission she was staying at the local clinic with intense abdominal pain, nausea with episodes of repeated vomiting, episodes of hyperthermia, hallucinations, confusion and electrolyte imbalance: Na – 117, K – 2.7, CI – 78 mmol/L. Despite of electrolyte normalization, neurological examination revealed cognitive and behavioral changes, bulbar disorders, paresis of the right arm, head and hand tremors, cerebellar ataxia, and unable to walk independently. MRI showed symmetrical lesions of the basal nuclei, thalamus, central parts of the Varolii pons and cortex of both frontal lobes. After transferring to our clinic patient was successfully treated with intravenous immunoglobulin with resolving neurological symptoms of EPM and CPM. After accidental raspberry color of urine detection the assumption of possible intermittent porphyria was made. Urine analyses revealed increased concentration of porphyrin precursors porphobilinogen, delta‐aminolevulinic acid, uroporphyrin, coproporphyrin.
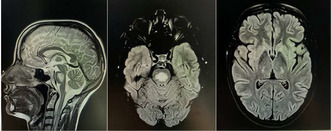
Brain MRI shows hyperintensive pontine lesion (14 × 18 × 24 mm) and bilateral thalamic lesions (6 × 9 mm).
Conclusion: We report this case to emphasize the clinical manifestations of AIP, including combination of gastrointestinal syndrome and electrolyte imbalance, especially hyponatremia due to possible antidiuretic hormone deficiency that may threaten of CPM/EPM development.
Disclosure: Nothing to disclose.
EPO‐676
Cerebellopontine abscess due to Listeria monocytogenes
D. Landaeta Chinchilla
Integrated Neurology Department of Rey Juan Carlos University Hospital, Infanta Elena University Hospital and Villalba University Hospital/Mostoles‐Madrid, Spain
Background and Aims: Listeria monocytogenes is a gram‐positive anaerobic bacillus with special tropism for the central nervous system. The main form of neurological involvement in adults is meningitis, with rhombencephalitis and brain abscess being rarer, but with a worse prognosis.
Methods: Clinical case.
Results: A 62‐year‐old man with type 2 diabetes came to the emergency department with fever, headache and hypoesthesia in the left hemibody of three days of evolution. Baseline CT, CT angiography and complete blood tests were performed in the emergency room without alterations. Brain MRI showed a heterogeneous lesion in the cerebellopontine angle and raised the possibility of infectious vs. tumor pathology. CSF study was performed with normal cell count and biochemical composition and negative multiparametric PCR. Given the persistence of fever and clinical progression with the appearance of dysphagia and dysmetria in the left extremities, neurosurgery was contacted to propose a stereotactic biopsy of the lesion. Multiplex PCR was performed on the extracted material and was positive for Lysteria Monocytogenes. In view of these findings, ampicillin was started at high doses.
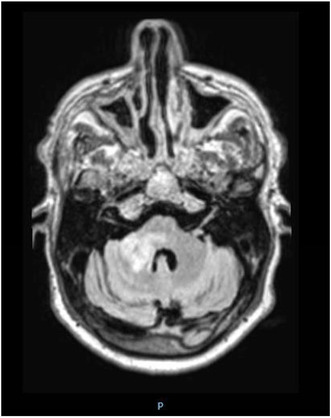
Conclusion: We present the case of a patient with cerebellopontine abscess due to Listeria monocytogenes, an atypical presentation with high morbidity and mortality rates. In our patient, support with diagnostic tools such as stereotactic biopsy was key to lead to the etiologic diagnosis and guide targeted antibiotic treatment.
Disclosure: Nothing to disclose.
EPO‐677
Papilledema in hypocalcaemia: A condition not to overlook
A. Cordeiro; M. Grunho
Department of Neurology, Hospital Garcia de Orta, Almada, Portugal
Background and Aims: Papilledema associated with hypocalcaemia is rare, and its precise pathophysiology remains unclear. The proposed causal mechanisms include vasoconstriction and disturbances in cerebrospinal fluid (CSF) dynamics. The prognosis depends on the underlying cause of hypocalcaemia, as well as the promptness of the diagnosis and treatment.
Methods: Review of the patient’s clinical records and of the relevant available literature on the topic.
Results: A 48‐year‐old female patient experienced a two‐week progression of bilateral decreased visual acuity, more pronounced on the left eye. She also reported occasional generalized cramps and hand paresthesias over the prior year. Her past medical history included iatrogenic hypothyroidism (9 years before, due to multinodular goitre), gastric bypass surgery (3 years before), and obesity. Neurological examination revealed bilateral papilledema and reduced visual acuity (left: 0.3; right: 0.8). Optical coherence tomography confirmed asymmetric bilateral papilledema. Brain and orbital MRI were unremarkable. Blood work revealed severe hypocalcaemia (5.2 mg/dL [8.7–10.4 mg/dL]) and low parathormone. Extensive autoimmune and infectious serological testing was all negative. Calcium replacement was initiated. Lumbar puncture, performed already under treatment, showed normal opening pressure. The remaining CSF tests were normal/negative. Hypocalcaemia was attributed to the surgical hypoparathyroidism and the bariatric surgery. Three months later visual acuity had improved (0.8 bilaterally) and the papilledema had resolved.
Conclusion: Hypocalcaemia‐associated papilledema is a rare, yet manageable condition. When faced with cases of papilledema, assessing calcium metabolism may prove essential, especially in people with a past history of thyroid/parathyroid surgery or other risk factors for hypocalcaemia. Awareness and prompt treatment, as in our case, is crucial for improving the prognosis in this clinical setting.
Disclosure: Nothing to disclose.
EPO‐678
CSF and blood signatures aid in distinguishing subtypes of limbic encephalitis
A. Dik 1; A. Schulte‐Mecklenbeck1; C. Strippel1; L. Bierhansl1; N. Meyer1; L. Korn1; M. Pawlowski1; S. Räuber2; S. Meuth2; N. Melzer2; J. Alferink3; C. Elger4; G. Meyer zu Hörste1; H. Prüß5; H. Wiendl1; C. Gross1; S. Kovac1
1Department of Neurology with Institute of Translational Neurology, University of Münster, Münster, Germany; 2Department of Neurology, Medical Faculty, Heinrich‐Heine University of Düsseldorf, Düsseldorf, Germany; 3Department of Psychiatry and Psychotherapy, University of Münster, Münster, Germany; 4Department of Epileptology, University of Bonn, Bonn, Germany; 5Department of Neurology and Experimental Neurology, Charité – Universitätsmedizin Berlin, Berlin, Germany
Background and Aims: Limbic encephalitis (LE) represents a heterogeneous disease with antibodies targeting extracellular (LEextra) epitopes, intracellular (LEintra) epitopes, and anti‐glutamic acid decarboxylase 65 LE (LE‐GAD65). Moreover, LE can be diagnosed without evidence of antibodies (LEabneg). We aimed to determine immune profiles of these distinct forms of LE.
Methods: We apply computational biology to flow cytometry data of CSF/blood of LE patients comparing them to non‐inflammatory controls (Ctrl) or patients suffering from relapsing remitting MS (RRMS).
Results: We identified discrete immune signatures in LE with antibody producing plasma cells and B cells as a specific feature of LEextra. In contrast, LE‐GAD65 lacked inflammatory changes in CSF/blood immune profiles with LEintra falling in‐between the two (LE‐GAD65 and LEextra). Interestingly, similar to LE_GAD65 LEabneg showed no prominent inflammatory immune‐signature.
Conclusion: Profiles identified may explain different treatment response to immunotherapy in subtypes of LE.
Disclosure: The authors have no relevant financial or non‐financial interests to disclose.
EPO‐679
Risk factors, treatment and clinical outcomes of decompression sickness with neurological symptoms: A case‐series study
B. Gómez Gozálvez; J. Sánchez Villalobos; J. Fajardo Sanchís; J. Bermejillo Barrera; M. Ruiz Perelló; F. Salazar Hernández; E. Carreón Guarnizo; D. Vidal Mena; E. Conesa García; M. Martínez Zarco; I. Díaz Jiménez; M. Ortega Ortega; M. López López; J. García Carmona
Neurology, University hospital Santa Lucía, Cartagena, Spain
Background and Aims: The decompression sickness (DCS) is related to diving practice and could affect multiple organs, including the central nervous system. The incidence of DCS with neurological symptoms is estimated in 2.7/10,000 dives and may cause both brain and spinal cord symptoms. Given the little knowledge about the DCS, the potential severity of its neurological symptoms and the difficult acute diagnosis and treatment, here we report a case‐series.
Methods: This is a retrospective single centre case‐series study evaluating the risk factors and treatment of consecutive patients diagnosed with DCS at the Santa Lucía University Hospital, Cartagena; Spain, between 2003–2023. All patients received hyperbaric oxygen therapy.
Results: 15 patients were included in this study. All were Caucasian male, the median age was 47.3 (range: 22–66). The time of symptoms onset was 37.8 minutes after diving. 6 (40%) patients were diagnosed with brain hemispheric syndromes, 1 (6%) with posterior reversible encephalopathy syndrome (PRES), 3 (20%) with brainstem syndromes and 5 (33%) with spinal cord syndromes. MRI scans demonstrated multiple territory stroke lesions and spinal cord lesions in 12 (80%) and 5 (33%) patients, respectively. The main risk factor for DCS was an inadequate diving profile while patent foramen ovale was demonstrated in 4 patients (27%). The mean of the Modified Rankin Scale (mRS) after 3 months was 1.9.
Conclusion: An unsecure diving profile is the main risk factor. Both, a correct diagnosis and emergent treatment are the cornerstones in the management of the DCS by neurologists.
Disclosure: The authors declare no conflict of interest.
EPO‐680
Post‐cytomegalovirus Guillain‐Barre syndrome with anti‐GM2 antibodies and acute transverse myelitis overlap syndrome
H. Ling
Department of Neurology, National Neuroscience Institute (SGH campus), Singapore
Background and Aims: A 55‐year‐old male presented with a three‐week history of progressive lower limb weakness, distal limb paresthesia, resulting in gait instability and multiple falls. With a medical history of Angioimmunoblastic T Lymphoma and autologous stem cell transplant, he was immunosuppressed with tacrolimus. A recent hospitalization for CMV viremia infection, resolved with antiviral therapy, was noted. Clinical examination revealed flaccid lower limb weakness, impaired distal proprioception sense, and diminished deep tendon reflexes.
Methods: Nerve conduction studies demonstrated demyelinating sensorimotor polyradiculoneuropathy predominantly lower limbs. MRI of the lumbosacral spine exhibited mild enhancement along the cauda equina nerve roots. Cerebrospinal fluid (CSF) analysis revealed characteristic albuminocytologic dissociation. Anti‐GM2 IgG was strongly positive. The patient was initiated on intravenous immunoglobulin (IVIG) infusion.
Results: He subsequently developed worsening of weakness with new sensory deficit up to T10 and urinary retention. MRI of the cervical and thoracic spine revealed longitudinally extensive transverse myelitis. Infective workup, autoimmune screen, paraneoplastic panel, anti‐NMO Antibody, and anti‐MOG Antibody, yielded unremarkable results. Treatment involved intravenous methylprednisolone with concurrent plasmapheresis, resulting in neurology recovery.

T2 sequence of the MRI cervical and thoracic spine.
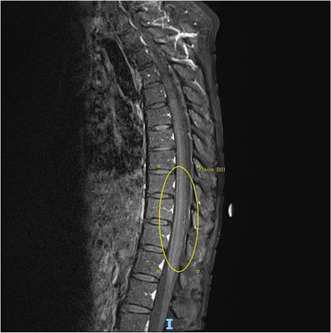
T1 sequence with contrast of the MRI cervical and thoracic spine.
Conclusion: Previous cases of GBS and ATM overlap syndrome were associated with various infections, including campylobacter jejuni, Zika virus, Mycoplasma pneumonia, Legionella pneumophila, Bartonella henselae, influenza virus, paramyxovirus, mumps virus, and varicella infection. Our patient represents the first reported case of GBS and TM overlap syndrome associated with CMV infection. First‐line therapy for GBS and ATM overlap are not well defined. Our case responded well to treatment with intravenous methylprednisolone and plasmapheresis, resulting in a favorable neurological recovery.
Disclosure: Nothing to disclose.
EPO‐681
Clinical manifestation and treatment efficacy of visual pathway involved neurosarcoidosis: A multicentre cohort
X. Zhang 1; B. Balasubramaniam2; A. Patil2; S. Sharma1; T. Arun3
1Oxford University Hospitals NHS Trust; 2University Hospitals Birmingham NHS Trust; 3University Hospitals Coventry and Warwickshire
Background and Aims: Sarcoidosis affecting the anterior visual pathway (AVP) presents distinctly compared to other optic neuropathies, with delayed diagnosis leading to impaired visual outcomes. The objective of this study is to evaluate visual outcomes in neurosarcoidosis patients with AVP involvement, focusing on the impact of different manifestations and treatment initiation times.
Methods: Retrospective multi‐centre cohort study.
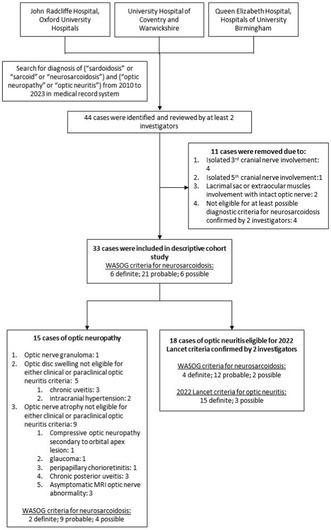
FIGURE 1 Retrospective Screening Flowchart.
Results: Forty‐six neurosarcoidosis patients with AVP involvement from four UK tertiary centers were analyzed over a median follow‐up of 1.90 years. Patients were categorized into optic neuritis (ON, n = 25) and non‐optic neuritis (NON, n = 21) groups, and further into early treatment (ET, n = 13) and delayed treatment (DT, n = 10) groups. The ON group exhibited a more significant visual decline compared to the NON group (p = 0.015), with similar baseline vision (p = 0.828) and a slightly worse nadir vision (median 0.96LogMAR vs 0.3LogMar, p = 0.078). Additional findings in the ON group included sudden visual loss (p = 0.072), disc swelling (p = 0.086), RAPD (p = 0.017), T2 hyperintensity in AVP (p = 0.033), and uninvolved chiasma (p = 0.064). Visual acuity improvement, stability, and deterioration rates did not significantly differ between ON and NON groups (p = 0.765). 22.2% of patients had final visual acuity worse than LogMAR 1.0 (29.1% in ON, 14.3% in NON). No significant difference was observed in overall visual improvement between ET and DT groups (61.5% vs 50%, p = 0.685), with 30.8% in ET and 20% in DT having final visual acuity worse than LogMAR 1.0.
Conclusion: AVP involvement in neurosarcoidosis shows varied clinical presentations. Delayed treatment yields a 50% non‐responsiveness rate, not significantly differing from early treatment outcomes.
Disclosure: Nothing to disclose.
EPO‐682
Sensory involvement in patients with Sjogren's disease electrophysiological investigation
F. Erbaş; H. Erdem Tilki
Department of Neurology, Ondokuz Mayıs University, Samsun, Turkey
Background and Aims: Sjogren's syndrome (SS) is a chronic, progressive, systemic inflammatory disease characterized by lymphocytic infiltration of exocrine glands. The main objectives of the study were to determine phenotypical patterns of peripheral nervous system involvement and the frequency of peripheral and central sensory involvement. We have also aimed to show the topography and extent of peripheral and central involvement by electrophysiological methods, and to examine the correlation of clinical and electrophysiological findings in patients with primary Sjogren's syndrome.
Methods: Thirty patients with Sjogren's disease were examined clinically with sensory symptoms, neurologic examination, modified Toronto Clinical Neuropathy Score and electrophysiologically with nerve conduction studies and somatosensory evoked potentials (SEP). The control group consisted of 30 healthy volunteers matched with the study group in terms of age and gender.
Results: A statistically significant difference was found in the mean median motor latency, mean tibial motor latency and mean tibial minimum F latency in the nerve conduction study parameters compared between the patient and control groups. Polyneuropathy was detected in three patients and all of them had pure sensory neuropathy. There was a significant correlation between the modified Toronto Clinical Neuropathy Score and the presence of polyneuropathy. In SEP examination no difference was detected in P37 latency, P37‐N45 amplitude and P37‐TP latency between the two groups.
Conclusion: In conclusion, this finding may indicate; 1. Sensory involvement was found to be present in Sjogren's syndrome. The sensory involvement was localized to peripheral nerves. 2. The sensory fibers in the dorsal column of the spinal cord were preserved.
Disclosure: there is nothing to explain.
EPO‐683
Combined subacute degeneration of spinal cord due to b12 deficiency: Pernicious anemia with hemolysis
G. Rodrigo Stevens; S. Escalante Arroyo
Neurology Department, Hospital Verge de la Cinta, Tortosa, Spain
Background and Aims: Combined subacute degeneration is a neurological complication of B12 deficiency. Most common cause in adults is anemia perniciosa, due to autoimmune destruction of gastric parietal cells. It is associated to megaloblastic anemia with macrocytosis. Hemolysis is very rare and seen in only 10% of cases. It produces intramedullary ineffective erythropoiesis. B12 deficiency related hemolysis, presents as a pseudo‐thrombotic microangiopathy (pseudo‐TMA). Key features are low reticulocyte count and normal or mildly decreased platelets.
Methods: A 62 year‐old male, with distal paresthesia, gait disturbance, fatigue and macrocytic anemia. His lab results showed low Hb 10 g/dl, elevated VCM 123 fL, elevated LDH 440 U/L, low haptoglobin 7.75 mg/dl, and schistocytes, with low absolute reticulocyte count (44.2 × 9, 1.72%). B12 levels were normal, but near to the normal low range 255 pg/ml. Hematology evaluation, ruled out autoimmune causes and TTP.
Results: He was admitted with suspicion of myelopathy. Initially, since B12 levels were normal and he had hemolytic anemia, cobalamin deficiency was not suspected. However, homocysteine levels were elevated 115 μmol/L. B12 deficiency was then suspected and intramuscular cobalamin was initiated. MRI showed typical signs of combined subacute degeneration. Pernicious anemia with elevated titers of anti‐intrinsic factor antibodies (253.3 U/ml) was confirmed.
MRI. T2 axial. Inverted V sign: hyperintensity of dorsal horns, associated with combined subacute degeneration.
Conclusion: B12 deficiency can induce pseudo‐microangiopathic hemolytic anemia in 10% of cases. Often, once hemolysis is seen, cobalamin deficiency is not investigated, leading to unnecessary tests. A normal lab result, must not rule out B12 deficiency when there is high clinical suspicion.
Disclosure: Nothing to disclose.
EPO‐684
A unique presentation of IgG4 disease with ocular, neurologic, and mastoid involvement
H. Narotam Jeena 1; A. Afrogheh2; J. West3; F. van der Colff4; N. Brey1
1Division of Neurology, Tygerberg Hospital and Stellenbosch University, Cape Town, South Africa; 2NHLS, Tygerberg Hospital and Stellenbosch University, Cape Town, South Africa; 3Division of Otorhinolaryngology, Tygerberg Hospital and Stellenbosch University, Cape Town, South Africa; 4Division of Ophthalmology, Tygerberg Hospital and Stellenbosch University, Cape Town, South Africa
Background and Aims: Immunoglobulin G4 (IgG4) disease typically presents as pancreatitis, retroperitoneal fibrosis, sclerosing cholangitis or interstitial lung disease. Central nervous system (CNS) manifestations are rare. This is the first description of IgG4 disease presenting as panuveitis with associated mastoiditis and raised intracranial pressure. Case presentation: 27 year old male with sudden onset unilateral headache. After a few days, acute bilateral loss of vision, associated with tinnitus. He was found to have a non‐granulomatous panuveitis and papilloedema.
Methods: CT brain demonstrated thickened optic nerves bilaterally and hyperostosis of the right mastoid. Right mastoid effusion in keeping with chronic mastoiditis was found on MRI. Lumbar puncture (LP) showed initial opening pressure exceeding 50 cm water, with normal chemistry and cell count. Serum ACE was raised, but CT chest and skin biopsy did not reveal any features of sarcoidosis. Mycobacterium tuberculosis, syphilis, mycoplasma pneumonia, HIV, and lymphoma test results were all negative. Sjogren, rheumatoid arthritis, and ANCA‐vasculitis tests were also negative. There was no evidence of localised CNS infiltration and sinus thrombosis on imaging. Whole body FDG‐PET confirmed mastoiditis.
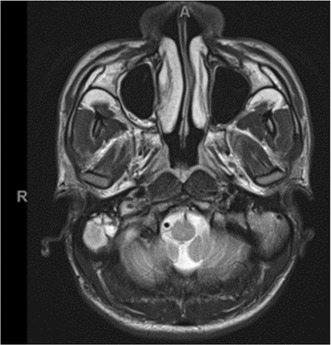
T2 sequence MRI brain showing the hyperintense signal in the right mastoid.
Results: Mastoid biopsy demonstrated a dense lymphoplasmacytic infiltrate with increased plasma cells and a storiform pattern of fibrosis.
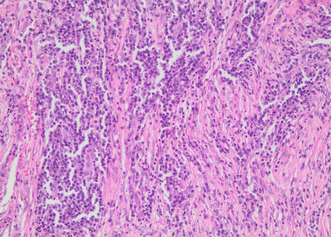
200× microscopic examination revealing storiform fibrosis with an abundance of plasma cells.
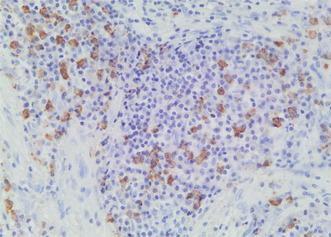
400× immunohistochemistry showing more than 10 IgG4 positive cells per high power field.
Conclusion: The constellation of panuveitis, papilloedema (in the absence of inflammatory pseudotumour or secondary obstructive hydrocephalus following pachymeningitis), has not been previously described. There are only a limited number of reports of IgG4 chronic mastoiditis. The combination of FDG‐PET/CT, along with biopsy may be prudent in atypical presentations. The patient was treated with high dose steroids, followed by long‐term immunosuppressive therapy.
Disclosure: Nothing to disclose.
EPO‐685
The multisystem involvement of MERRF syndrome
J. Barbosa; A. Aldomiro; C. Semedo; C. Rosado Coelho
Neurology Department, Setúbal Hospital Center, Lisbon, Portugal
Background and Aims: Myoclonic epilepsy with ragged‐red fibers syndrome (MERRF) is a mitochondrial multisystem disorder whose canonical clinical features are myoclonus, generalized seizures, ataxia, and ragged‐red fiber myopathy. Approximately 80% of MERRF cases have the m.8344A>G mutation in the MTTK gene. Other clinical features include peripheral neuropathy, hearing loss, dementia, and multiple lipomas. The diagnosis is made in the presence of suggestive clinical findings and a genetic pathogenic variant.
Methods: A 63 year old man reports progressive proximal tetraparesia, exercise intolerance and involuntary movements of the right hand and foot. Additionally he has hearing loss and cervical lipomas. His mother also had cervical lipomas and died during his childhood. He has no siblings or children. Neurological examination showed proximal tetraparesis with muscular atrophy, right hand and foot dystonia with occasional focal myoclonia, ataxia, binasal hemianopsia, and hipoacusia.
Results: Cranial and cervical MRI were normal. EMG described axonal sensorimotor polyneuropathy. Blood analysis was unremarkable except for elevated CK. Ophthalmology evaluation revealed bitemporal optic atrophy. Cardiac evaluation revealed frequent supra ventricular extrasystole. The patient refused muscular biopsy. A mitochondrial disease genetic panel revealed m.8344A>G mutation in the MTTK gene.
Conclusion: This case shows a defying diagnosis of a rare disease. Despite not all MERRF canonical features are present and the late age of onset, the patient has multiple suggestive clinical findings. The typical pathological genetic mutation found supports a MERRF diagnosis. The clinical and genetic heterogeneity of this disease renders this diagnosis a challenge, highlighting the need for future investigation.
Disclosure: Nothing to disclose.
EPO‐686
CAR T‐cell‐associated neurotoxicity: Single‐center experience in a tertiary center
P. Martinez Agredano; I. Lorite Fuentes; A. Rodriguez Martin; M. Alvarez Soria; F. Acebron Sanchez‐Herrera
Department of Neurology, University Hospital Reina Sofia, Cordoba, Spain
Background and Aims: Chimeric antigen receptor T cells therapy (CAR‐T) have revolutionized the treatment of patients with relapsed and refractory B‐ cell malignancies. CART therapy is associated with significant toxicities including cytokine release syndrome (CRS) and immune cell associated neurological syndrome (ICANS). The objective of this study is to describe the outcomes and treatments of CRS and ICANS in our hospital.
Methods: Retrospective descriptive study following five patients diagnosed of refractory diffuse large B cell lymphoma (DLBCL) treated with CAR‐T therapy by the Department of Hematology. We registered age, sex, type of CAR‐T used, MRI, EEG, acute phase reactant, CRS grade, ICANS, and treatment either with Tocilizumab or steroid.
Results: All five patients treated in our center developed CRS. About 60% developed CRS grade 1 and 40% CRS grade 3. Acute phase reactant (Interleukin‐6, C‐reactive protein and ferritin) increased in all CRS presenting patients. ICANS incidence was 80% from whom 75% were treated with steroids. Neurological related symptoms improved in all patients after steroid therapy.
Conclusion: Early recognition and treatment of ICANS associated with CAR‐T is determinant for successful outcomes in patient receiving this therapy. A multidisciplinary approach is crucial to improve patient outcomes.
Disclosure: The authors have nothing to disclose.
EPO‐687
Myositis, axonal polyneuropathy and stroke in acute toxoplasmosis infection
R. Ferrer Tarrés 1; M. Garcia Huguet1; C. Vera Cáceres1; C. Martínez Follana1; I. Saurina Navarro1; C. Marco Cazcarra2; D. López Domínguez1
1Department of Neurology, Hospital Doctor Josep Trueta, Girona, Spain; 2Neuromuscular Unit, University Hospital of Bellvitge, Barcelona, Spain
Background and Aims: Toxoplasma gondii is the most common cause of protozoan infection in humans. Toxoplasmosis has been associated with myositis and, in rare instances, with other neurological illnesses like polyneuropathies.
Methods: Description of a clinical case of a patient with systemic toxoplasmosis presenting several neurological affections such as myositis and sensory‐motor axonal polyneuropathy.
Results: We present the case of a 56‐year‐old man from Gambia with heterozygous sickle cell disease. Following a recent trip to his native country, he was admitted to the hospital with a 20‐day history of persistent fever, muscle pain, proximal debility, with an increase in CK levels. Serological tests showed positive IgM for T. gondii with a positive polymerase chain reaction. Antiprotozoal treatment and corticosteroids improved weakness and CK levels. Two weeks after admission, the patient experienced a progressive worsening of gait, autonomic dysfunction, and neuropathic pain. Examination revealed tetraparesis, bilateral facial paralysis, sensory ataxia, and generalized areflexia. Lumbar puncture indicated albumin‐cytological dissociation, with no evidence of Toxoplasma in the cerebrospinal fluid. Electromyogram showed decreased sensory‐motor amplitudes, with myopathic muscle recruitment. Plasma exchange was initiated suspecting Guillain‐Barré syndrome, resulting in slight improvement. Brain MRI showed subacute thalamic ischemic lesion. Other autoimmune and infectious studies were rule out. Muscle biopsy indicated lymphocyte‐predominant inflammation, MHC I overexpression and toxoplasma cysts, and peripheral nerve biopsy revealed mild axonal neuropathy.
Conclusion: In conclusion, we present a case of a patient with multiple systemic complications following toxoplasmosis infection. While neuromuscular complications have been documented, simultaneous involvement with polyneuropathy and myopathy has not been previously reported.
Disclosure: No disclosure.
EPO‐688
Acute neurological complications in liver transplanted patients: A retrospective single centre study
V. Lo Re 1; F. Avorio1; G. Russelli2; G. Panarello3; R. Alduino2; A. Arcadipane3; S. Gruttadauria4
1Neurology Service, IRCCS – ISMETT (Mediterranean Institute for Transplantation and Advanced Specialized Therapies), Palermo, Italy; 2Research Department, IRCCS – ISMETT (Mediterranean Institute for Transplantation and Advanced Specialized Therapies), Palermo, Italy; 3Department of Anaesthesia and Critical Care, IRCCS – ISMETT (Mediterranean Institute for Transplantation and Advanced Specialized Therapies), Palermo, Italy; 4Department for the Treatment and Study of Abdominal Diseases and Abdominal Transplantation, IRCCS ISMETT (Mediterranean Institute for Transplantation and Advanced Specialized Therapies), Palermo, Italy
Background and Aims: Neurological complications (NCs) occur in about 30 % of patients after orthotopic liver transplant (OLT). This study aimed to investigate early post‐operative (PO) NCs after OLT in our cohort of adult cirrhotic patients and to identify risk factors associated with the neurological outcomes.
Methods: We performed a retrospective single centre study; all patients who underwent deceased‐ and living‐donor liver transplant between June 2014 and October 2021 were included. A PO acute NC was confirmed when symptoms and/or signs of central or peripheral central nervous system (NS) impairment occurred from the transplant but within the hospital stay.
Results: 275 men (73.14%) and 101 women (26.86%) were included; median age was 58 (range 22–70) years. NC occurred in 25% of patients. Encephalopathy was the most common NC (15.2%), followed by neurotoxicity (5.9%), seizures (3.7%) and central pontine myelinolysis (CPM) (3.2%). Patients with NCs had history of pre‐transplant hepatic encephalopathy (p < 0.0001), pre‐surgical critical condition (p = 0.015), higher Mayo End stage Liver Disease score (p = 0.0002), history of pre‐transplant renal insufficiency (p = 0.0124) and a higher PO sodium shift (p = 0.01).
Conclusion: Pre‐operative neurological comorbidities, psychoactive drugs and age were not risk factors for PO NCs. NCs were correlated with PO adverse outcomes as infections, graft rejection, Intensive Care Unit (ICU) re‐admission, in‐hospital death, need of rehabilitation, in‐hospital and ICU length of stay, post‐surgical acute renal insufficiency. Our data confirm that the occurrence of NCs mostly depends on the severity of the pre‐operative hepatic disease and/or systemic factors and do not depend on pre‐operative neurological diseases other than HE.
Disclosure: The authors have nothing to disclose.
Sleep‐wake disorders 2
EPO‐689
Clinical practice and actigraphic findings of daridorexant in chronic insomnia
D. Hoxhaj 1; A. Colitta1; L. Troilo1; A. Pascazio1; F. Buracchi Torresi1; M. Fabbrini1; M. Maestri Tassoni1; F. Turco1; U. Faraguna2; G. Siciliano1; E. Bonanni1
1Department of Clinical and Experimental Medicine, Neurological Clinic, University of Pisa; 2Department of Translational Research and of New Surgical and Medical Technologies, University of Pisa, Pisa, Italy
Background and Aims: Chronic insomnia, a prevalent sleep disorder, adversely affects daytime function and quality of life. This real‐world study assesses the efficacy of daridorexant, a novel dual orexin receptor antagonist, in treating chronic insomnia using actigraphy over 1 and ongoing 3‐month follow‐ups.
Methods: Twenty‐three adults (M 43.5%, F 56.5%, mean age: 56.5 ± 11.0 years) with chronic insomnia, according to the ICSD‐3 criteria, were included in the study. Baseline and subsequent assessments at one month (23 patients) and three months (6 patients) involved the collection of subjective sleep parameters, including total sleep time (TST), wake after sleep onset (WASO), and latency to persistent sleep (LPS). Additionally, participants completed the Insomnia Severity Index (ISI) and the Insomnia Daytime Symptoms and Impacts Questionnaire (IDSIQ). Ten patients underwent actigraphy at both baseline and one month.
Results: After one month of treatment, there was a statistically significant reduction in subjective LPS by 28 minutes (p 0.050) and WASO by 57 minutes (p 0.007), accompanied by a 32‐minutes increase in TST (p 0.046). Questionnaire scores indicated a clinically meaningful reduction: ISI by 6 points (p < 0.001), IDSIQ‐total score by 22 (cut‐off >17, p 0.012), and IDSIQ‐cognitive domain by 10 (cut‐off >4, p 0.004). Actigraphic data revealed a noteworthy 52‐minutes increase in TST (p 0.042).
Conclusion: Our data confirmed Daridorexant efficacy after 1 month of treatment. Not only all sleep subjective parameters improved, but actigraphy showed an objective TST increase of almost one hour. It positively impacted quality of life, enhancing daytime cognitive functions, and significantly reducing insomnia severity.
Disclosure: Nothing to disclose.
EPO‐690
Compulsive gambling associated with modafinil: A case report
D. Račić
Department of neurology, University Clinical Center Republic of Srpska, Banja Luka, Bosnia and Herzegovina
Background and Aims: We describe a case of new‐onset compulsive gambling associated with the use of modafinil in a patient with type 1 narcolepsy (NT1).
Methods: Case report:
Results: A 21‐year‐old white woman presented to our clinic in 2023. She had history of excessive daytime sleepiness (EDS), cataplexy and sleep paralysis dating back for one year. She underwent diagnostic polysomnography (PSG) showed 7 REM sleep‐onset periods, multiple sleep latency test (MSLT) with five naps showed an average sleep latency of 8 minutes and 2 sleep‐onset REM periods, brain magnetic resonance (MR) imaging was normal. She was diagnosed with NT1 and commenced modafinil therapy started at a dose of 100 mg daily together with clomipramine 25 mg daily. She had no longer episodes of cataplexy but EDS symptoms only moderate controlled. One month later modafinil was increased at a dose of 200 mg daily. The patient′s symptoms remained stable for the 8 months when she began gambling activities together with excessive alcohol abuse. On a follow‐up visit she was refereed to psychotherapy together with lowering modafinil dose to 100 mg daily. Three months later, she reported improvement in the compulsive gambling and stopped drinking alcohol.
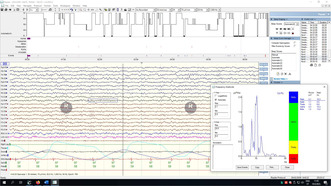
Polysomnography.
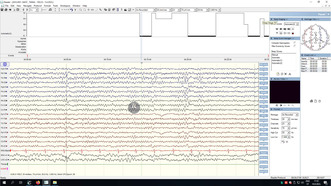
Multiple sleep latency test.
Conclusion: We described new‐onset impairment of impulse control after taking modafinil which has been more commonly described in patients receiving dopamine agonist therapy.
Disclosure: Nothing to disclose.
EPO‐691
Pain in isolated REM sleep behavior disorder (iRBD): Study of association
G. Malomo 1; E. Capriglia1; M. Solbiati1; L. Spelta2; A. Rubino2; C. Totaro2; D. Arnaldi3; P. Mattioli3; M. Pardini4; B. Orso5; F. Casoni6; L. Ferini Strambi7; A. Castelnuovo7; S. Natoli8; A. Pisani9; M. Terzaghi1
1Department of Brain and Behavioral Sciences, University of Pavia, Unit of Sleep Medicine and Epilepsy, IRCCS Mondino Foundation, Pavia, Italy; 2IRCCS Mondino Foundation Pavia, Unit of Sleep Medicine and Epilepsy; 3Neurophysiopathology, IRCCS Ospedale Policlinico San Martino, DINOGMI, University of Genoa; 4DINOGMI, University of Genoa, Clinical Neurology, IRCCS Ospedale Policlinico San Martino; 5DINOGMI, University of Genoa; 6Department of Clinical Neurosciences, Neurology – Sleep Disorders Center, IRCCS San Raffaele Scientific Institute, Milan, Italy; 7Department of Clinical Neurosciences, Neurology – Sleep Disorders Center, IRCCS San Raffaele Scientific Institute, Milan, Italy; “Vita‐Salute” San Raffaele University, Milan, Italy; 8Department of Clinical‐Surgical, Diagnostic, and Pediatric Sciences, University of Pavia, Pavia, Italy; 9Department of Brain and Behavioral Sciences, University of Pavia, IRCCS Mondino Foundation Pavia
Background and Aims: Non‐motor symptoms in Parkinson's disease (PD) include chronic pain, which may occur in 20–80% of PD patients during the course of the disease. iRBD represents a prodromal phase for alpha‐synucleinopathies including PD. Therefore, we aimed to identify the occurrence of pain and its characterization in an iRBD cohort.
Methods: 88 iRBD patients and 75 age‐ and sex‐matched healthy controls were included; iRBD diagnosis was made according to ICSD‐3rd criteria. Clinical evaluation included pain typology (PainDetect questionnaire) and pain perception (Brief Pain Inventory) together with motor evaluation (MDS‐UPDRS), sleepiness (Epworth Sleepiness Scale), insomnia symptoms (Sleep Condition Indicator) and quality of sleep (Pittsburgh Sleep Quality Index), anxiety and depression (HADS‐A, HADS‐D) global cognition (MOCA), RBD scale (RBD questionnaire HK) and dopaminergic transmission (DAT‐scan), measurements derived from PSG.
Results: Analysis of pain occurrence, typology and perception showed no statistically significant differences between patients and controls. In the iRBD group, statistically significant associations were detected between pain typology and perception and insomnia symptoms (p = 0.01 and p = 0.15 respectively) and sleep quality (p < 0.001 and p = 0.03 respectively). No association was found with other variables.
Conclusion: Chronic pain was not significantly increased in patients with iRBD. Mechanisms behind pain perception in iRBD may differ from those of PD‐related neurodegeneration. We found a bidirectional correlation between pain and poor sleep quality in iRBD. Longitudinal data should be considered to evaluate a possible role as a marker of neurodegeneration.
Disclosure: Nothing to disclose.
EPO‐692
The levels of anxiety and depression in epilepsy based on insomnia phenotypes
H. Karkourian 1; L. Atabekyan1; E. Balian1; A. Bichakhchyan2; H. Hovakimyan2; S. Khachatryan1
1Department of Neurology and Neurosurgery, National Institute of Health, Yerevan, Armenia; 2Center for Sleep and Movement Disorders, Somnus Neurology Clinic, Yerevan, Armenia
Background and Aims: Insomnia is the commonest sleep disorder and is one of the most frequent of all mental health challenges. Insomnia phenotypes, namely sleep‐onset (SOI), sleep‐maintenance (SMI) and mixed insomnia (MI) are frequently encountered in adults with epilepsy (AWE). Our aim was to discover links between particular insomnia phenotypes with levels of depression and anxiety in AWE.
Methods: AWE were diagnosed according to international diagnostic criteria and enrolled from a specialized sleep and epilepsy clinic. According to insomnia clinical presentation we distinguished patients with no insomnia, SOI, SMI, and MI phenotypes based on interviews. Anxiety and depression were assessed using Hamilton Anxiety and Depression Rating Scales (HAMA and HAMD respectively). The ANOVA test was utilized for statistical analysis.
Results: A total of 170 AWE were interviewed for this study, with mean age 34.9 ± 13.4 (18–71), females – 46.5%. Seventy‐eight patients had insomnia (54.1%), divided into 29 (17.06%) with SOI, 11 (6.47%) with SMI, and 52 (30.59%) had MI. The mean values for HAMA and HAMD scales were 9.17 and 7.96 for no insomnia, 12.86 and 11.07 for SOI, 21.91 and 16.18 for SMI, 22.12 and 19.38 for MI, respectively (p < 0.01 for both scales). Box plots are presented in Figure 1 for HAMA and Figure 2 for HAMD.

FIGURE 1 Box plot for Hamilton Anxiety Rating Scale (HAMA) according to insomnia phenotypes (SOI – sleep‐onset insomnia, SMI – sleep‐maintenance insomnia).

FIGURE 2 Box plot for Hamilton Depression Rating Scale (HAMD) according to insomnia phenotypes (SOI – sleep‐onset insomnia, SMI – sleep‐maintenance insomnia).
Conclusion: Our study highlighted a statistically significant difference in prevalence of anxiety and depression among AWE with different insomnia phenotypes. Specifically, AWE with no insomnia had the best profile, with gradually increasing severity in SOI, SMI, and MI respectively. Further research is needed to corroborate our findings.
Disclosure: Nothing to disclose.
EPO‐693
Case series of Prader‐Willi syndrome and narcolepsy
I. Čelpačenko 1; D. Burkojus2; G. Liakaitė‐Obolevičienė3; E. Pajėdienė1
1Neurology Department, Lithuanian University of Health Sciences, Kaunas, Lithuania; 2Department of Pediatric Neurology, Lithuanian University of Health Sciences, Kaunas, Lithuania; 3Department of Pediatric Pulmonology, Lithuanian University of Health Sciences, Kaunas, Lithuania
Background and Aims: Prader‐Willi syndrome (PWS) is a rare genetic neuroendocrine disorder, which frequently presents with excessive daytime sleepiness (EDS) that may contribute to many clinical features of PWS. Sleep apnoea is a widely recognized cause of EDS in PWS, whereas other sleep disorders (SD), such as narcolepsy and cataplexy are only gaining recognition. PWS patients routinely undergo a polysomnography (PSG), however, more detailed differential diagnostics should be considered in patients exhibiting disproportionate EDS, as an effective treatment for narcolepsy is readily available and could substantially enhance patients’ health, cognition, and behavioral problems.
Methods: Summarized patient's information included case history, Ullanlinna narcolepsy and Epworth Sleepiness scale scores, hypocretin‐1 levels in cerebrospinal fluid (CSF), polysomnography (PSG) and Multiple Sleep Latency test (MSLT) results.
Results: Case series presents 1 male and 3 female patients with PWS, whose age ranged from 1 to 16 y/o. Based on clinical presentation, sleep studies and hypocretin‐1 levels, all patients have been diagnosed with concomitant narcolepsy 1 type and sleep apnoea (Table 1)
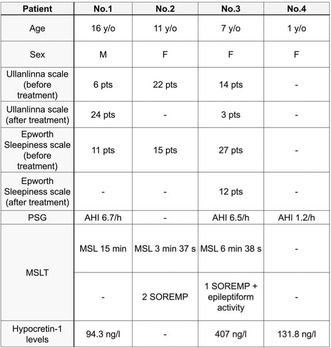
TABLE 1 Summary of patients’ characteristics.
FIGURE 2 Hypnogram (patient No. 4).
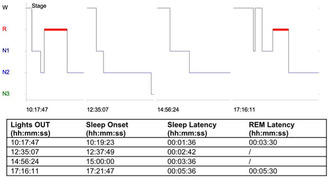
FIGURE 1 Multiple Sleep Latency test (patient No. 2).
Conclusion: This case series demonstrates that excessive daytime sleepiness in PWS may be attributable not only to sleep apnoea, but also to coexisting narcolepsy. Similarities in clinical presentation pose a challenge for the clinicians, therefore narcolepsy tends to be underdiagnosed. Multidisciplinary care is crucial for timely narcolepsy diagnosis and treatment.
Disclosure: Evelina Pajėdienė is a Co‐chair of the EAN Scientific Panel for Sleep‐wake disorders.
EPO‐694
iSPHYNCS: A multi‐omics approach towards novel biomarkers for narcolepsy and its borderland
J. D. Warncke 1; K. Zub1; E. Wenz1; L. G. Fregolente1; J. van der Meer1; O. Gnarra1; R. Morrand1; A. Helmy1; Z. Zhang2; R. Khatami2; S. von Manitius3; S. Miano4; J. Acker5; M. Tafti6; A. Datta7; R. Rezaei8; U. Kallweit8; D. Bijlenga9; J. de Boer9; G. Lammers9; B. Yilmaz10; S. Mougiakakou11; A. Tzovara12; M. H. Schmidt1; C. L. A. Bassetti1
1Sleep‐Wake Epilepsy Center, NeuroTec, Department of Neurology, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland; 2Clinic Barmelweid, Center for Sleep Medicine and Sleep Research, Barmelweid, Switzerland; 3Department of Neurology, Kantonsspital St. Gallen St, Gallen, Switzerland; 4Sleep and Epilepsy Center, Neurocenter of Southern Switzerland, Regional Hospital (EOC) of Lugano, Lugano, Switzerland; 5ZurzachCare, Clinic for Sleep Medicine, Bad Zurzach, Switzerland; 6Department of Biomedical Science, Faculty of Biology and Medicine, University of Lausanne, Lausanne, Switzerland; 7Neuropaediatrics, University Children's Hospital Basel, Basel, Switzerland; 8Center for Narcolepsy and Hypersomnias, Professorship for Narcolepsy and Hypersomnolence Research, Department of Medicine, University Witten/Herdecke, Witten, Germany; 9Sleep Wake Centre SEIN, Heemstede, The Netherlands; 10Department for Biomedical Research, Department of Visceral Surgery and Medicine, Bern University Hospital, University of Bern, Bern, Switzerland; 11ARTORG Center for Biomedical Engineering Research, University of Bern, Bern, Switzerland; 12Institute of Computer Science, University of Bern, Bern, Switzerland
Background and Aims: The international Swiss Primary Hypersomnolence and Narcolepsy Cohort Study (iSPHYNCS) aims at providing new data to improve the management of primary central disorders of hypersomnolence (CDH). The main aims of iSPHYNCS are: (1) discovery of new biomarkers, and assessment of (2) treatment adherence, and (3) outcomes related to patients. This abstract presents initial data related to the first objective.
Methods: The study is ongoing at 11 study sites in Switzerland, Germany and The Netherlands and plans to prospectively include 500 CDH patients and 60 healthy controls by the end of 2026. Initial evaluations comprise questionnaires, video‐polysomnography, the Multiple Sleep Latency Test (MSLT), the Sustained Attention Response Task (SART), and actigraphy. Further analyses include a wearable Fitbit device, the microbiome, peptidomics/proteomics, and genetics. This comprehensive approach includes the collection of bio‐samples: plasma, serum, DNA, stool samples, and cerebrospinal fluid. AI‐driven analyses, including unsupervised clustering, will be used for data‐driven patient phenotyping, followed by a multimodal approach that combines various data types after domain‐specific analyses.
Results: 194 participants have been recruited, including 7 children. This group comprises 37 individuals with narcolepsy with cataplexy (NT1), 134 with other primary CDH, such as narcolepsy borderland (NBL), and 23 HC. Initial analyses reveal notable differences among NT1, NBL, and HC groups across various domains, including questionnaire responses, neuropsychiatric profiles, microbiome, and Fitbit data.
Conclusion: Following an initial three‐year phase in Switzerland, the internationalization of iSPHYNCS in 2023 was successful. Preliminary results suggest novel and promising clinical, biological and digital markers of CDH.
Disclosure: The authors declare no conflict of interest and the study is supported by the Swiss National Science Foundation (320030_185362 and 32003B_215721).
EPO‐695
Comparative characteristics of patients with obstructive sleep apnea and COMISA syndrome and their adherence to therapy
K. Magomedova; Z. Umachanova; L. Geybatova
Department of Neurology, Dagestan State Medical University
Background and Aims: Insomnia and obstructive sleep apnea (OSA) are the two most common sleep disorders that are often comorbid to each other (comorbid insomnia and sleep apnea, COMISA).
Methods: Pittsburgh Questionnaire to determine sleep quality, the Epworth Sleepiness Scale. The study included 33 patients divided into 2 groups: 22 people with moderate and severe OSA and 11 people with moderate and severe COMISA syndrome. The diagnosis of OSA was verified according to respiratory sleep monitoring data. Average age of patients in group 1 was 53.5 years, the second group was 54.5 years. CPAP therapy was initiated for everyone, an automatic mode for 21 days. Follow‐up visits were conducted after 1 and 2 weeks to monitor the effectiveness, technical characteristics and compliance of the treatment.
Results: Interpretation of the therapy data showed that in 11 patients of the first group, IAG averaged 6.9/h during the period of use, 5 patients were unable to use the device and refused therapy, in 7 patients of the 2nd group IAG was 14.9 /h, 6 patients were unable to use therapy and refused the study.
Conclusion: The data obtained indicate better adherence and better results of constant positive pressure therapy in patients with OSA without concomitant insomnia. It is advisable to offer treatment for both sleep disorders to patients with COMISA.
Disclosure: Nothing to disclose.
EPO‐696
Sex differences in isolated REM sleep behavior disorder: Insights from the FARPRESTO cohort
M. Maestri Tassoni 1; E. Casaglia2; M. Figorilli2; F. Meloni3; F. Ingravallo4; P. Mattioli5; E. Capriglia6; S. Marelli7; L. Baldelli8; C. Liguori9; E. Antelmi10; G. Plazzi11; V. Brunetti12; R. Ferri13; B. Guarnieri14; G. Rossato15; G. Pellitteri16; M. Puligheddu2
1Section of Neurology, Department of Clinical and Experimental Medicine, University of Pisa, Italy; 2Interdepartmental Sleep Research Centre, Department of Medical Sciences and Public Health, University of Cagliari, Italy; 3Unit of Occupational Medicine, Department of Medical Sciences and Public Health, University of Cagliari, Italy; 4Department of Medical and Surgical Sciences (DIMEC), Alma Mater Studiorum, University of Bologna, Bologna, Italy; 5DINOGMI and IRCCS Ospedale Policlinico San Martino, Genoa, Italy; 6Department of Brain and Behavioral Sciences, University of Pavia, Pavia, Italy; Unit of Sleep Medicine and Epilepsy, IRCCS Mondino Foundation, Pavia, Italy; 7Sleep Disorders Center, Division of Neuroscience, Università Vita‐Salute San Raffaele, Milan, Italy; 8Department of Biomedical and NeuroMotor Sciences, University of Bologna, and IRCCS, Istituto delle Scienze Neurologiche di Bologna, Bologna, Italy; 9Sleep Medicine Centre, Neurology Unit, University of Rome Tor Vergata, Rome and Department of Systems Medicine, University of Rome Tor Vergata, Rome, Italy; 10Department of Neurosciences, Biomedicine and Movement Sciences, University of Verona, Verona, Italy; 11IRCCS, Istituto delle Scienze Neurologiche di Bologna, Bologna, and Department of Biomedical, Metabolic, and Neural Sciences, University of Modena and Reggio Emilia, Modena, Italy; 12UOC di Neurologia, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Roma and Department of Neuroscience, Università Cattolica del Sacro Cuore, Roma, Italy; 13Sleep Research Centre, Oasi Research Institute – IRCCS, Troina, Italy; 14Center of Sleep Medicine, Villa Serena Hospital, Città S. Angelo, Pescara and Villaserena Foundation for the Research, Città S. Angelo, Pescara, Italy; 15Sleep Center, Dept. of Neurology, IRCCS Sacro Cuore Don Calabria, Verona, Italy; 16Clinica Neurologica, DMED, Università di Udine, Italy
Background and Aims: Inconsistent literature data hinders a comprehensive understanding of sex predominance and other sex‐related distinctions in RBD. This investigation within the FARPRESTO multicentric, Italian, longitudinal cohort, aims to investigate variances between sexes in terms of the age of onset, diagnosis, and phenoconversion and to explore differences in cognitive and non‐motor variables.
Methods: 558 iRBD patients were enrolled in the FARPRESTO study from 13 Italian centers, Age at RBD diagnosis, diagnostic delay, motor and non‐motor symptoms, cognitive deficits, conversion rate to neurodegenerative disorders, and RBD‐related injuries were analyzed according to sex. Statistical analysis utilized Mann‐Whitney U and Pearson's chi‐squared tests with significance set at p < 0.05.
Results: Mean age at the diagnosis was higher in females (males 62.0, females 65.0), whereas no significant sex differences in cognitive test scores were detected. Orthostatic hypotension and depression were more prevalent in females (38.1 % vs 20.4 and 27.4 % vs 43.3 %, respectively). No difference in conversion rate has been reported. In addition, in women, injuries affecting patients at the first visit were significantly more frequent (71.0% vs 53.5%) than injuries affecting the partner or both.
Conclusion: Studies investigating sex differences in this field are still limited. However, as diagnostic and therapeutic possibilities advance, a nuanced understanding of sex‐specific characteristics becomes increasingly essential for tailored clinical approach.
Disclosure: Nothing to disclose.
EPO‐697
The burden of insomnia and excessive daytime sleepiness: Switzerland's pilot study preliminary results
M. Tüzün 1; U. Kallweit2,3; S. Seidel4; O. Endrich5; S. Trelle6; M. Leone7; O. Bruni8; R. Dodel9; A. Fiorillo10,11; I. Holmerova12,13; J. Jaarsma14; M. Lolich15; M. Konti15; D. Ramankulov15; D. Pervernagie16; E. Pupillo7; W. Randerath17,18; L. Vignatelli19; C. Meyer‐Massetti20; M. Schmidt1; C. Bassetti1,21,22
1Interdisciplinary Sleep‐Wake‐Epilepsy‐Center, Bern University Hospital (Inselspital) and University of Bern, Bern, Switzerland, 2University Witten/Herdecke, Faculty of Medicine, Professorship for Narcolepsy and Hypersomnolence Research, Witten, Germany, 3Center for Biomedical Education and Research (ZBAF), Witten, Germany, 4Rehabilitation Clinic Pirawarth, Bad Pirawarth, Austria, 5University Institute of Clinical Chemistry, Inselspital, Bern University Hospital, University of Bern, Switzerland, 6Medical Directorate, Inselspital, Bern University Hospital, Switzerland, 7Department of Neurosciences, Istituto di Ricerche Farmacologiche “Mario Negri” IRCCS, Milano, Italy, 8Department of Developmental and Social Psychology, Sapienza University, Rome, Italy, 9Department of Geriatric Medicine, University Duisburg‐Essen, Essen, Germany, 10Department of Psychiatry, University of Campania “L. Vanvitelli”, Naples, Italy, 11European Psychiatric Association, 12Centre of Expertise in Longevity and Long‐term Care, Charles University, Prague, Czechia, 13Alzheimer Europe, 14European Alliance for Restless Legs Syndrome, Brussels, Belgium, 15European Academy of Neurology, Vienna, Austria, 16Department of Internal Medicine and Paediatrics, Faculty of Medicine and Health Sciences, Ghent University, Ghent, Belgium, 17Department of Respiratory Diseases and Sleep Disorders Centre, AZ Delta, Roeselare, Belgium, 18Institute of Pneumology, University of Cologne, Cologne, Germany, 19Clinic for Pneumology and Allergolony center of sleep medicine and respiratory care, Hospital Bethanien Solingen, Solingen, Germany, 20IRCCS Istituto delle Scienze Neurologiche di Bologna, Bologna, Italy, 21Clinical Pharmacology & Toxicology, Department of General Internal Medicine, Inselspital ‐ University Hospital Bern, Switzerland; 22Department of Neurology, Bern University Hospital (Inselspital) and University of Bern, Bern, Switzerland
Background and Aims: At present, the specific needs of individuals affected by excessive daytime sleepiness (EDS) and/or insomnia (IN) complaints, in conjunction with its overall socio‐economic burden remains unexplored. To address this gap, a pilot trial for a multi‐stage, European‐wide, multi‐center research study is being conducted in Switzerland since mid‐2023.
Methods: prospective, national, cohort observational study for the systematic evaluation of the burden of EDS and IN and its evolution 12 months after the first assessment. Patient recruitment is facilitated through nine primary care providers, concluding in June 2024. Primary outcomes include the feasibility of the study, while secondary outcomes focus on the prevalence of EDS/IN in primary care settings and the association between EDS/IN and health‐related quality of life (QOL), assessed using validated instruments. Patients are screened for EDS/IN, and those with positive indications are invited to participate in the online portion of the study comprised standardized and socio‐economic/health status questionnaires.
Results: To date, 632 subjects have been screened, with 238 (44%) presenting EDS and/or IN. Of these, 111 expressed interest in participation, with 43 enrolled in an online segment. Among those with symptoms, 58% of individuals expressed concern for their symptomatology. A significant positive correlation was found between the presence of concern and medication usage (p < 0.01).
Conclusion: This research will provide long‐due information and report on important aspects of the QOL most associated with EDS/IN. First data indicate a high frequency of these disorders as well as significant links between patients ‘concerns and pharmacotherapy use.
Disclosure: Nothing to disclose.
EPO‐698
“Wet, wobbly, wacky and woke?”
M. McDowell‐Hook
Taranaki Base Hospital, New Zealand
Background and Aims: Normal pressure hydrocephalus (NPH) is defined by a clinical triad of urinary incontinence, gait apraxia and cognitive impairment. Recent research has identified a high prevalence of sleep disordered breathing (SDB) in these patients. This audit investigates the diagnosis and management of patients with NPH and the prevalence of SDB in clinical practice.
Methods: Retrospective audit of clinical records from January 2014 to January 2024 (n = 26). Audit standards for diagnosis, investigation and management were defined from regional NPH guidelines. Prevalence of SDB in clinical practice was defined by Epworth Sleepiness Scale of 10–15 or diagnostic polysomnography.
Results: 26 (100%) patients had supportive neuroimaging and 23 (88.5%) patients had the full symptom triad. 22 patients (84.6%) had documented high volume CSF lumbar punctures and underwent gait assessment pre‐ and post‐procedure. 13 patients (50%) progressed to ventriculoperitoneal shunt insertion, with all demonstrating symptomatic improvement. Only 2 patients (7.7%) were diagnosed with SDB, managed with non‐invasive ventilation.
Conclusion: Documentation of diagnostic symptom triad, investigation, and management was completed to a high standard. However, the documented prevalence of SDB was significantly lower than in previous studies. These results suggest that SDB in NPH patients may be underdiagnosed, prompting inclusion of SDB to local protocols. Future studies could investigate whether diagnosis and treatment of SDB improves outcomes for these patients.
Disclosure: Nothing to disclose.
EPO‐699
Importance of sleep quality and the effects of deprivation on doctors amidst conflict in Sudan
M. Jaber Amin 1; L. Mohamed Ali Elomeir2
1Faculty of Medicine Alzaiem Alazhari University, Khartoum, Sudan; 2Faculty of Medicine, University of Khartoum, Khartoum, Sudan
Background and Aims: Healthcare professionals working in demanding environments and leading busy lives are more prone to burnout, disruptions in their sleep schedules, and sleep deprivation. These factors can affect their productivity and performance, potentially compromising patient care and medical outcomes. The main objective of this study was to evaluate the effects of sleep quality and deprivation on healthcare professionals in Sudan.
Methods: To achieve this objective, we conducted a cross‐sectional study using a structured questionnaire after thoroughly reviewing the existing literature on Sudanese healthcare professionals. The study aimed to assess sleep quality, stress, anxiety, and depression and evaluate their impact on performance. Additionally, we explored the associations between personal backgrounds, susceptibility to burnout, and sleep disturbance.
Results: Our results revealed that the majority of participants experienced poor sleep quality and daytime sleepiness. We also found a significant prevalence of stress, anxiety, and depression among Sudanese healthcare professionals. Furthermore, we identified associations between demographic factors such as sex, marital status, profession, and sleep quality.
Conclusion: This study underscores a critical issue for physicians' health programs in Sudan, highlighting the importance for hospitals to implement measures that enable healthcare professionals to take more days off, obtain adequate sleep, and reduce on‐call service days. It is imperative for healthcare professionals themselves to acknowledge the significance of these factors in preserving their own health and delivering sustainable healthcare services.
Disclosure: Nothing to disclose.
EPO‐700
Insomnia and excessive daytime sleepiness in patients with breast cancer
S. Slemenšek Avšič 1; M. Ravnik2; M. Rakuša3
1Faculty of Medicine, University of Maribor, Slovenia; 2Department of Oncology, University Medical Centre Maribor, Maribor, Slovenia; 3Division of Neurology, University Medical Centre Maribor, Maribor, Slovenia
Background and Aims: Sleep disturbances in women with breast cancer are poorly detected and managed in routine clinical practice. Our study aim was to evaluate sleep patterns and excessive daytime sleepiness (EDS) in patients during breast cancer treatment.
Methods: Fifty‐nine women were recruited. Demographic data, sleep, neuropathic pain, anxiety, and depression were evaluated with the Epworth scale (ES), Insomnia Severity Index (ISI), PainDetect, DN4, Beck Anxiety Inventory (BAI), and Hamilton Depression Rating Scale (HDRS). We calculated descriptive statistics. Mean values for demographic data and scale scores were calculated using an unpaired T‐test or Chi‐square test between patients with EDS (ES >10) and clinically moderate to severe insomnia (ISI >15). At the end, we calculated Spearman´s correlations.
Results: Mean age was 60.6 ± 14.4 years, mean disease duration was 15.4 ± 20.9 months, mean ES was 7.6 ± 5.6 and mean ISI was 10.4 ± 7.7. Twenty‐two percent of patients had EDS, and 27% had clinically moderate to severe insomnia. There were no statistically significant differences between groups in age, disease duration, BMI, metastases, hormone receptor status, therapy, presence of neuropathic pain, polyneuropathy symptoms, and severity of depression and anxiety. We found a positive correlation between ES and ISI (rho = 0.397; p < 0.01). Clinically moderate to severe insomnia and EDS correlated with depression (rho = 0.572; p < 0.01 and rho = 0.355; p < 0.01, respectively), anxiety (rho = 0.613; p < 0.01 and rho = 0.290; p < 0.05, respectively), and neuropathic pain (rho = 0.272, p < 0.05, both conditions). Additionally, EDS correlated with BMI (rho = 0.271; p < 0.05).
Conclusion: Our results indicate that insomnia is more prevalent than EDS in patients with breast cancer. We should be vigilant for patients with neuropathic pain and neuropsychiatric symptoms.
Disclosure: I disclose no conflict of interest.
EPO‐701
Sleep‐wake cycle disturbance as the first symptom in an anti‐CV2/CRMP‐5 encephalitis
B. Alberti Vall1; A. Martinez Viguera1; T. Mederer Fernandez 1; S. Berton Ocampos2; S. Gimenez Badia2; L. Martin Aguilar1
1Neurology Department, Hospital de la Santa Creu i Sant Pau, Barcelona, Spain; 2Multidisciplinary Sleep Unit, Hospital de la Santa Creu i Sant Pau, Barcelona, Spain
Background and Aims: We present the case of a patient with an anti‐CV2/CRMP5 autoimmune encephalitis, whose initial and predominant symptoms were sleep disturbances. To our knowledge, no reported cases have highlighted sleep disturbances as the predominant clinical symptom, which tend to be overshadowed.
Methods: A 67‐year‐old male with a history of smoking, hypertension, and diabetes presented with a four‐month course of symptoms that abruptly began with a severe alteration of the circadian sleep‐wake pattern with night‐time insomnia and excessive daytime sleepiness, and involuntary movements during sleep. Three months later he developed generalized weakness, gait disturbances, a toxic syndrome, dysarthria, and dysphagia. Neurological examination showed bradypsychia, dysarthria, dysphagia, apraxia, bradykinesia, appendicular rigidity, and truncal ataxia.
Results: Video‐polysomnography recorded undifferentiated periods of sleep and wakefulness, non‐specific NREM sleep, with increased limb movements, and vocalizations during sleep. Positive anti‐CRMP5/CV2 antibodies were detected in serum. Brain MRI revealed hyperintensities in the brainstem, both medial temporal lobes, and basal ganglia, consistent with striatal and limbic encephalitis. PET‐CT scanning detected a thoracic hypermetabolic later confirmed as metastatic small cell lung carcinoma. Corticosteroid treatment as well as chemotherapy were started, with neurological improvement observed in a few days, and resolution of the sleep‐wake cycle disturbance.
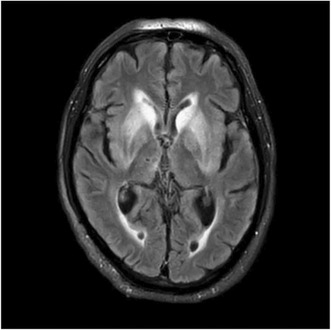
Brain MRI. Symmetrical hyperintensities in bilateral striatal regions as well as bilateral mesial temporal regions, compatible with a striatal and limbic encephalitis.
V‐Polisomnography. Undifferentiated sleep and wakefulness periods, with undifferentiated N‐REM (no graphoelements) and no registered periods of REM. OSA with significant desaturation.
Conclusion: This case underscores the importance of considering autoimmune encephalitis in the differential diagnosis of patients presenting with sleep disturbances and nonspecific neurological symptoms. These symptoms tend to be elusive and nonspecific and can lead to diagnostic delays. A multidisciplinary approach engaging both neurologists and sleep specialists can facilitate in an accurate and earlier diagnosis.
Disclosure: Nothing to disclose.
EPO‐702
Sleep architecture of patients with idiopathic hypersomnia and identification of neurophysiological markers for subtypes
B. Harmes1; F. Tepel1; K. Šonka2; U. Kallweit 1
1Center for Narcolepsy and Hypersomnias, Professorship for Narcolepsy and Hypersomnolence Research, Department of Medicine, University Witten/Herdecke, Germany; 2Department of Neurology and Clinical Neuroscience Centre, Centre for Sleep and Waking Disorders, 1. Faculty of Medicine, Charles University, Prague, Czechia
Background and Aims: Idiopathic hypersomnia (IH) is a rare neurologic disease characterised by excessive need of sleep including prolonged nocturnal sleep and excessive daytime sleepiness. Clinical observations have indicated at least two subtypes of IH, one associated with long sleep cycles. The aim of the study is to systematically examine differences in sleep architecture of patients with IH in order to identify particular neurophysiological parameters for subtypes.
Methods: In this retrospective pilot study polysomnography of 35 consecutive IH patients between 2017 and 2023 from two major sleep centres are analysed. Only patients without any psychopharmacological medication and without moderate or severe depression were included.
Results: 35 patients were included (27 female, 8 male). Mean age was 24.4 years. Mean total sleep duration was 605 ± 122 mins. Mean number of sleep cycles (MNSC) was 6.5 ± 1.9. Mean sleep efficiency was 93.8 %. Mean sleep cycle duration (MSCD) was 105 ± 20 mins. The MSCD of 22 patients was 92 ± 8 mins, their MNSC was 7.5 ± 1.5. The MSCD of the other 13 patients was 128 ± 13 mins, with a MNSC of 4.8 ± 0.8. With p < 0.001 for these two groups the difference in sleep cycle length is statistically highly significant.
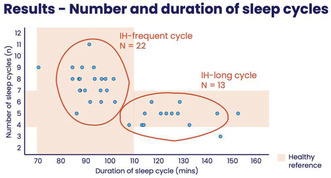
Number (n) and duration of sleep cycles (mins).
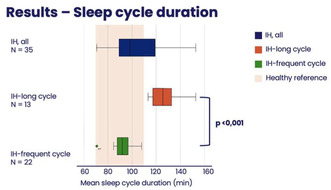
Mean sleep cycle duration (mins).
Conclusion: Data indicates two subtypes of IH: IH‐long cycle is associated with long sleep cycles and a normal number of sleep cycles. IH‐frequent cycle shows an increased number of sleep cycles and normal length of sleep cycles. Subtyping will contribute to the understanding of the etiopathogenesis and possibly to individualized therapy.
Disclosure: Nothing to disclose.
Neuroimaging 2
EPO‐703
MERS (Mild encephalitis with a reversible splenial lesion); a case report
A. Morillas; P. Gil; L. Carazo; V. González
Department of Neurology, Complejo Hospitalario of Jaén, Jaén, Spain
Background and Aims: Case of MERS (Mild encephalitis with a reversible splenial lesion) due to psychotropic drugs VS metabolic disorder.
Methods: In our hospital, we report the case of a 69‐year‐old man with a previous Bipolar Disorder, who develops abruptly a behavioral alteration and disorientation. Due to this, he is transferred to Neurology where he is diagnosed of MERS in possible relation to psychiatric medication and acute diarrhea.
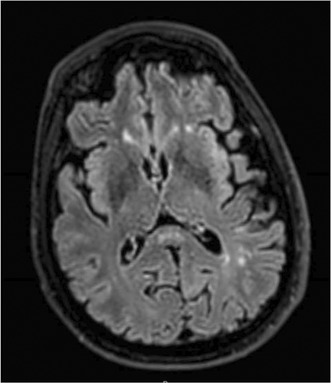
Initial cranial MRI of the patient shows an hyperintense lesion in the middle of SCC in FLAIR.
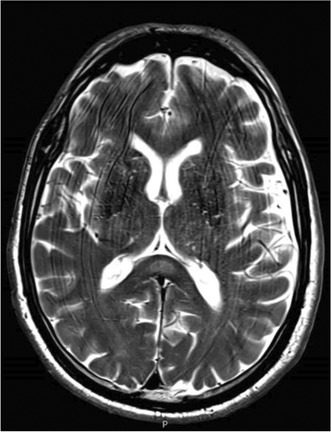
Initial cranial MRI of the patient shows an hyperintense lesion in the middle of SCC in T2.
Results: After the adjustment of the psychotropic drugs and the resolution of the diarrhea, the patient improved from the symptomatology and the hyperintense lesions disappeared in the Magnetic Resonance.
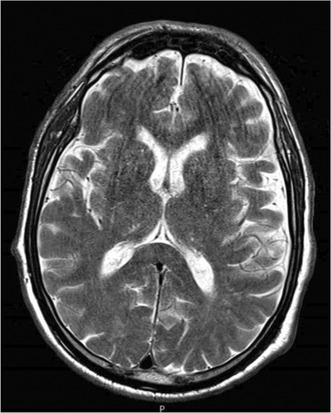
Last cranial MRI shows a resolution of the lesion.
Conclusion: MERS is a reversible encephalopathy that affects the corpus callosum and can produce both neurological and psychiatric symptoms in relation to different etiologies, finding a hyperintense lesion in T2 and FLAIR sequences that are located in the splenium of the corpus callosum.
Disclosure: Nothing to disclose.
EPO‐704
Large scale white matter disruption and longitudinal degeneration in stroke
M. Aarabi1; L. Pini 2; M. Corbetta2
1Padova Neuroscience Center (PNC), University of Padova, Padova, Italy; 2Department of Neuroscience, University of Padova, Padova, Italy
Background and Aims: Stroke result in both local and distal brain connectivity alterations. While functional connectivity changes have been widely established, alterations in the structural connectivity patterns are still unclear. Here we assessed longitudinal changes of white matter organization in stroke and the relationship with behavior.
Methods: We prospectively enrolled first‐time stroke patients, assessed at two‐week and three‐month intervals. Patients underwent behavioral and diffusion weighted‐imaging (DWI) assessments. A latent factorial analysis was applied to behavioral data. Structural gradients were assessed for both intra‐ and inter‐hemispheric tractography and averaged across networks. Statistical analyses included analysis of variance and longitudinal assessments through linear mixed model. Finally, we explored the relationships between structural gradients and behavior.
Results: Fifty patients (age 59 ± 11) and 29 controls (age 57 ± 11) were enrolled. Factorial analysis identified five cognitive factors, explaining 50% of variances. We reported three gradients for both intra‐ and inter‐hemispheric connections (50% of variance). Network‐wise analysis unveiled widespread acute stage alterations, impacting multiple networks for both intra‐ and inter‐connectivity. Longitudinal assessment suggested significant degradation of this gradient structural organization. There was also an association between structural connectivity patterns and visuospatial‐memory performance more strongly at the acute stage.
Conclusion: Stroke‐induced structural connectivity damage extends beyond the lesion and worsens over time. The weak relationship between longitudinal changes in the structural organization and behavioral performance might implying that white matter modifications are independent with the recovery or disability status of stroke patients.
Disclosure: Nothing to disclose.
EPO‐705
High resolution intracranial vessel wall imaging in small vessel vasculitis of the central nervous system
A. Lotti1; A. Mariottini2; A. Barilaro3; G. Costantini1; E. Fainardi4; L. Massacesi 2
1Department of Neurosciences, Drug and Child Health, University of Florence, Florence, Italy; 2Department of Neurology 2, Careggi University Hospital; Department of Neurosciences, Drug and Child Health, University of Florence, Florence, Italy; 3Department of Neurology 2, Careggi University Hospital, Florence, Italy; 4Neuroradiology Unit, Department of Experimental and Clinical Biomedical Sciences, University of Florence, Florence, Italy
Background and Aims: Diagnosis of small vessels primary angiitis of CNS (SV‐PACNS) is based on meninge/brain biopsy, but criteria for exposing to this invasive procedure high‐risk cases only are lacking. In this study, accuracy of high resolution vessel wall MR imaging HR‐VWI, a non‐invasive method for visualizing SVs inflammation, for detecting patients at high risk of SV‐PACNS was explored.
Methods: Patients with relapsing or chronic neurological symptoms/syndromes suggesting SV‐PACNS (n = 11) or with secondary SV vasculitis of the CNS (SV‐SACNS; n = 4) and patients with non‐vasculitic brain hyperintensities (NVBH; n = 34; – multiple sclerosis, n = 18; – small vessel disease, n = 12; – migraine, n = 4) were enrolled. The patients received one MRI scan including HR‐VWI sequences (3D PD weighted black blood with gadolinium) on a 3T scanner. SVs inflammation was considered present if linear HR‐VWI enhancements corresponding to SVs and/or >3 punctiform enhancements noticeable in HR‐VWI but not in other sequences were observed. HR‐VWI enhancements corresponding to leptomeningeal enhancement, restricted diffusion areas or to microbleeds were excluded.
Results: HR‐VWI positive SVs were observed in 7/15 SV‐PACNS/SACNS (47%) and in 0/34 NVBH (0%), corresponding to 47% sensitivity and 100% specificity. Stratifying the SV‐ PACNS/SACNS according to disease duration, 7/8 of the <1 year duration cases (87%) showed SV inflammation, thus in this setting increasing HR‐VWI sensitivity to 87%.
Conclusion: In patients with short disease duration HR‐VWI could represent an accurate tool for selecting patients at high risk of SV‐PANCS eligible for cerebral/meninge biopsy. This probably because over time therapies mask the disease‐related pathogenic inflammation.
Disclosure: Nothing to disclose.
EPO‐706
DAI changes of head injury patients in CT imaging: The HEAD Helsinki study
O. Raassina 1; R. Autio2; J. Kinnunen3; M. Patronen4; I. Marinkovic3; H. Isokuortti5; J. Satopää6; J. Putaala3; M. Niemelä6
1Department of Radiology, University of Helsinki, Helsinki University Hospital, Helsinki, Finland; 2Department of Radiology, Vaasa Central Hospital, Vaasa, Finland; 3Department of Neurology, University of Helsinki, Helsinki University Hospital, Helsinki, Finland; 4Statistics Finland, Helsinki, Finland; 5Department of Intensive Care, University of Helsinki, Helsinki University Hospital, Helsinki, Finland; 6Department of Neurosurgery, University of Helsinki, Helsinki University Hospital, Helsinki, Finland
Background and Aims: Diagnostic value of computed tomography (CT) imaging for diffuse axonal injury (DAI) changes is considered limited. We determined how many patients with magnetic resonance imaging (MRI) positive DAI changes had them visible in head CT after diagnosed traumatic brain injury (TBI).
Methods: Our retrospective register‐based study cohort of patients with head injury treated at emergency hospitals in Helsinki between 01 January and 31 December in years 2010 and 2018. Confirmed DAI patients’ initial and follow up head CTs were analyzed. Based on MRI findings, definitive corresponding CT findings were accepted according to Gentry's classification: Hemorrhagic and/or edematous strands at grey‐white matter junctions in grade 1 and edematous and/or petechial contusions in grade 2 and 3. Small single petechial contusions located in the subcortical or white matter regions were excluded in grade 1.
Results: Of the 1963 screened patients, 64 had MRI positive DAI changes. A total of 24/64 (37.5%) MRI‐DAI patients had visible DAI changes in CT, of which 9/24 (37.5%) were grade I, 6/24 (25.0%) grade II and 9/24 (37.5%) grade III. However, 7/24 (29.0%) did not show any visible changes during the primary CT obtained within 24 hours after the accident, and they only became evident in follow‐up CTs taken 1–4 days after the initial scan.
Conclusion: Detection of DAI‐changes in CT compared with MRI was low despite of increased sensitivity in follow‐up CT scans. MRI‐imaging combined with clinical history remain the primary source of tool for assessing DAI‐changes in TBI‐patients.
Disclosure: Nothing to disclose.
EPO‐707
Stroke echo scan from a neurologist perspective
P. Lochner; J. Stögbauer; F. Merzou; S. Krakau; S. Kottackal
Neurology, Saarland University Center
Background and Aims: More than 20% of ischaemic strokes occur due to a cardioembolic cause The point of care echocardiography (PoCUS) protocol comprises eleven aspects with binary responses focussing on specific target structures: functions of left ventricle, left atrium, right ventricle, valvular abnormalities, large intracardiac thrombi, aortic plaque thrombi, aortic plaque, pericardium and signs of hypovolaemia.
Methods: We applied this screening to identify stroke patients associated with an increased cardioembolic risk in order to find treatable cardioembolic causes and to find an interrater reliability between neurologist and cardiologist, whose diagnosis was chosen as the gold standard.
Results: According to the defined protocol, 50 patients (female, n = 24; mean age = 62 a, SD 17 a) underwent the PoCUS echocardiography test. It displayed a global sensitivity of 77.8% and global specificity of 94.1% (k = 0.73). This high sensitivity and specificity were achieved particularly with regard to the assessment of pumping function and enlargement of the cardiac cavities, but less for other items such as heart valve abnormalities (SEN 30%; SPE 97.4%), large intracardiac thrombi (SEN not available, SPE 100%).
Conclusion: A good interobsever reliability was found between neurologist and cardiologist. Future prospective studies are warranted to improve the interrater reliability.
Disclosure: Nothing to disclosure.
EPO‐708
Supra and infratentorial atrophy in cerebellar ataxias: Unveiling distinctions across different etiologies
S. Pisano1; S. Basaia 2; O. Stojiljković3; S. Mesaros3; N. Dragasevic3; V. Kostic3; F. Agosta4; M. Filippi5
1Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; and Neurology Department, Istituto Clinico S. Anna Hospital, Brescia, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 3Clinic of Neurology, Faculty of Medicine, University of Belgrade, Belgrade, Serbia; 4Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 5Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: This study investigates structural changes in patients with cerebellar ataxias (CA) due to different causes.
Methods: 28 Autosomal dominant (AD) CA patients, 17 autosomal recessive (AR) CA patients, 29 sporadic cases of CA, 8 multiple system atrophy patients (MSAc) and 20 controls were included. MRI was performed; whole‐brain Voxel‐Based Morphometry (VBM) and cerebellar‐optimized VBM (SUIT toolbox) were used to assess gray matter (GM) atrophy. Brainstem and superior cerebellar peduncles (SCP) volumes were estimated and compared.
Results: Compared to controls, all CA groups showed widespread GM cerebellar atrophy; additionally, AD and AR groups showed distinct clusters of supratentorial atrophy, mainly involving temporal and parietal regions. No supratentorial GM differences were found among CA groups. SUIT‐VBM revealed more severe atrophy in the medial Crus‐I and II in MSAc compared to AD, and in AR compared to AD. AD, AR, and MSAc groups exhibited reduced whole‐brainstem, midbrain, and pons volumes compared to controls; AD and MSAc groups also exhibited reduced whole‐brainstem and pons volumes compared to sporadic cases. AD and AR showed reduced medulla volumes compared to controls and sporadic cases. SCP volume reduction was evident in all CA groups compared to controls, with AD showing also decreased SCP volume compared to sporadic cases.
Conclusion: AD and AR groups showed supratentorial patterns of atrophy. Conversely, the sporadic group showed less involvement of brainstem structures. The evidence of distinct patterns of structural alterations in different CA etiologies might contribute to an improved differential diagnosis.
Disclosure: S Pisano, O Stojiljković, S Mesaros, and N Dragasevic have nothing to disclose. S Basaia received research supports from the Italian Ministry of Health. VS Kostic has received speaker honoraria from Actavis and Solveo. F Agosta received speaker honoraria from Biogen Idec, Italfarmaco, Roche, Zambon and Eli Lilly, and has received research supports from IMH, Italian Ministry of University and Research, ARiSLA, ERC, EU Joint Programme – Neurodegenerative Disease Research, and Foundation Research on Alzheimer Disease. M Filippi consulting or speaking activities or advisory boards for Alexion, Almirall, Biogen, Bayer, Bristol‐Myers Squibb, Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA; scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol‐Myers Squibb, Lilly, Novartis, Sanofi‐Genzyme; research support from Biogen Idec, Merck‐Serono, Novartis, Roche, IMH, Italian Ministry of University and Research, and FISM.
EPO‐709
Chronic active lesions contribute to depression in multiple sclerosis
M. Rubin1; P. Preziosa 1; A. Meani2; M. Margoni3; N. Tedone2; M. Filippi4; M. Rocca1
1Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 3Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, and Neurorehabilitation Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy; 4Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: Chronic neuroinflammatory processes may contribute to depression in multiple sclerosis (MS). Paramagnetic rim lesions (PRLs) and choroid plexus (CP) enlargement represent novel magnetic resonance imaging (MRI) markers of chronic inflammation in MS that are associated with more severe clinical disability. Currently, their interplay with the presence of depression remains unexplored. Here, we examined whether the number and volume of PRLs and CP enlargement may contribute to depression in MS patients.
Methods: Brain 3T MRI and clinical evaluation with the assessment of depression using Montgomery–Asberg Depression Rating Scale (MADRS) were obtained from 126 MS patients and 72 age‐ and sex‐matched healthy controls (HC). Patients with MADRS score >9 were classified as depressed. PRLs were identified on phase images of susceptibility‐weighted imaging, whereas CP volume was quantified using a fully‐automatic method on 3D T1‐weighted and FLAIR MRI sequences. Predictors of depression were identified using LASSO logistic regression.
Results: Forty‐six out of 126 (36.5%) MS patients were depressed. Fifty‐nine (46.8%) MS patients had ≥1 PRLs (median = 0, interquartile range = 0; 2). Compared to HC, MS patients showed significantly higher T2‐hyperintense white matter lesion (WM) and normalized CP volume volumes, as well as lower normalized brain, thalamic, hippocampal and WM volumes (p from <0.001 to 0.023). PRL number (standardized‐β = 0.078) and volume (standardized‐β = 0.029) were independent predictors of depression (area under the curve = 0.60).
Conclusion: Higher number and volume of PRLs may contribute to the pathophysiology of depression in MS patients, emphasizing the role of chronic neuroinflammatory processes in determining depression independently from disease severity.
Disclosure: M Rubin, A Meani, N Tedone have nothing to disclose. P Preziosa received speaker honoraria from Roche, Biogen, Novartis, Merck, Bristol Myers Squibb, Genzyme, Horizon and Sanofi. He has received research support from Italian Ministry of Health and Fondazione Italiana Sclerosi Multipla (FISM). M Margoni reports grants and personal fees from Sanofi Genzyme, Merck Serono, Novartis and Almiral. M Filippi received compensation for consulting or speaking activities from Alexion, Almirall, Biogen, Bayer, Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA; participation in Advisory Boards for Alexion, Biogen, Bristol‐Myers Squibb, Merck, Novartis, Roche, Sanofi, Sanofi‐Aventis, Sanofi‐Genzyme, Takeda; scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol‐Myers Squibb, Lilly, Novartis, Sanofi‐Genzyme; he receives research support from Biogen Idec, Merck‐Serono, Novartis, Roche, Italian Ministry of Health, Italian Ministry of University and Research, and FISM. MA Rocca received consulting fees from Biogen, Bristol Myers Squibb, Eli Lilly, Janssen, Roche; speaker honoraria from AstraZaneca, Biogen, Bristol Myers Squibb, Bromatech, Celgene, Genzyme, Horizon Therapeutics Italy, Merck Serono SpA, Novartis, Roche, Sanofi and Teva; research support from MS Society of Canada, Italian Ministry of Health, Italian Ministry of University and Research, and FISM.
EPO‐710
Loss of serotonergic function in carriers of Parkin mutations: A [11C]DASB PET study
E. de Natale1; H. Wilson1; J. Verghese1; S. Antoniadis 1; A. Terry1; P. Khosropanah1; M. Howard1; L. Cashmore1; K. Bhatia2; E. Mulroy2; V. Marshall3; E. Sammler4; F. Valzania5; F. Cavallieri5; N. Tambasco6; P. Nigro6; M. Pellecchia7; G. Xiromerisiou8; E. Rabiner9; M. Politis1
1Neurodegeneration Imaging Group, University of Exeter Medical School, London, UK; 2Department of Clinical and Movement Neurosciences, UCL Queen Square Institute of Neurology, University College London, London, UK; 3Institute of Neurology, Queen Elizabeth University Hospital, Institute of Neurological Sciences, Glasgow, UK; 4Molecular and Clinical Medicine, Ninewells Hospital and Medical School, University of Dundee, Dundee UK; 5Neurology Unit, Neuromotor & Rehabilitation Department, Azienda USL‐IRCCS di Reggio Emilia, Reggio Emilia, Italy; 6Movement Disorders Center, Neurology Department, Perugia General Hospital and University of Perugia, Perugia, Italy; 7Neuroscience Section, Department of Medicine, Surgery and Dentistry “Scuola Medica Salernitana”, University of Salerno, Salerno, Italy; 8School of Medicine, University of Thessaly, Larissa, Greece; 9Invicro Centre for Imaging Sciences, Hammersmith Hospital, London, UK
Background and Aims: Idiopathic Parkinson's disease (iPD) features loss of presynaptic serotonergic function. Serotonergic loss has also been detected in autosomal dominant forms of monogenic Parkinsonism. In this study we present preliminary in vivo data of serotonergic terminal integrity in the striatum of symptomatic PRKN mutation carriers (PRKN‐PD), an autosomal recessive form of monogenic Parkinsonism.
Methods: Eight individuals with PRKN‐PD (mean age 49.32 ± 8.74, disease duration 9.51 ± 5.59 years, Hoehn & Yahr 1.81 ± 0.53), eight iPD patients (mean age 65.38 ± 7.58, disease duration 4.82 ± 4.17 years, Hoehn & Yahr 1.88 ± 0.99) and eight healthy controls (HC, mean age 46.25 ± 6.02) underwent clinical assessments, Magnetic Resonance Imaging (MRI) scans, and single [11C]DASB PET scan. Regions of Interest (ROIs) were delineated on each subject's T1 space MRI, using Multi‐Atlas Propagation with Enhanced Registration (MAPER), with grey matter masking. The Logan reference model, with the posterior cerebellar grey matter excluding the vermis as the reference region, was utilised to generate parametric [11C]DASB distribution volume ratio (DVR) images with DVR‐1 equal to non displaceable binding potential (BPND).
Results: PRKN‐PD patients exhibited significant reduction in [11C]DASB BPND compared to HC in Putamen (−33.8%, p < 0.001), and Caudate (−37.2%, p = 0.005). iPD patients showed significant decrease of [11C]DASB BPND in putamen (−36.1%; p < 0.001) and caudate (−43.9%; p < 0.001) compared to HC. No significant difference in [11C]DASB BPND was observed between iPD and PRKN‐PD patients in these regions.
Conclusion: These findings offer preliminary evidence of a noteworthy striatal loss in presynaptic serotonergic integrity among symptomatic PRKN mutation carriers. Ongoing data collection for additional PRKN carriers will further illuminate these findings.
Disclosure: Nothing to disclose.
EPO‐711
BOLD fMRI functional connectivity informed by IEDs in high‐risk and low‐risk SUDEP epilepsy patients
S. Scolastico; F. Talami; A. Ballerini; S. Meletti; A. Vaudano
Department of Biomedical, Metabolic and Neural Sciences, University of Modena and Reggio Emilia, Modena
Background and Aims: According to recent literature, interictal epileptiform discharges (IEDs) might provide a facilitating environment for Sudden Unexpected Death in Epilepsy (SUDEP) to happen. Here, we explore the effects of IEDs on the functional connectivity between regions of interest (ROIs) known to be involved in the SUDEP pathogenesis and the rest of the brain in a population of high‐risk (HR) and low‐risk (LR) SUDEP epilepsy patients.
Methods: A cohort of 39 adult epilepsy patients was investigated with EEG‐coregistered to fMRI and then stratified in HR and LR according to SUDEP‐3 and SUDEP‐7 inventories. Additional stratification was performed based on the occurrence of tonic‐clonic seizures (GTC criteria). Seven ROIs were considered: Anterior Cingulate Cortex, Insula, Brainstem, Thalamus, Amygdala, Putamen. The IED‐related functional connectivity between the ROIs and the rest of the brain was investigated through a Psychophysiological Interaction (PPI) analysis.
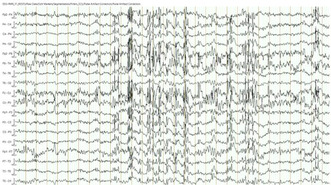
“Probable SUDEP” case interictal EEG trace acquired during fMRI.
Results: In the SUDEP‐7 and GTC stratified groups, PPI analyses show in HR versus LR an increased IEA‐informed functional connectivity between amygdala, thalamus and putamen seeds and supramarginal gyrus and a decreased functional connectivity between the same ROIs and motor and premotor cortex. These patterns are consistent with the PPI results obtained with the same approach in a single "Probable SUDEP" case.
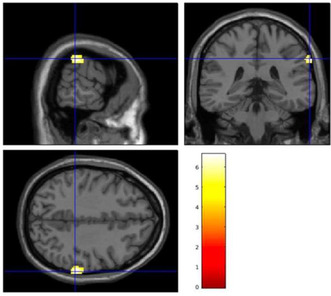
Increased spike‐related FC in the GTC HR group compared with LR patients between bilateral putamen and left supramaginal Gyrus.
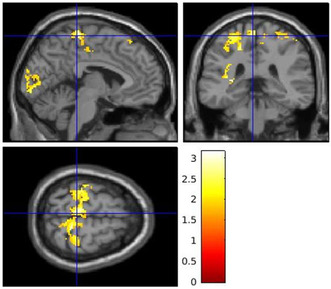
Reduced spike‐related FC in the SUDEP‐7 HR groups compared with LR patients between bilateral thalamus and premotor cortex.
Conclusion: Our findings suggest that in SUDEP and HR patients compared to LR, IEA modulate the functional connectivity between specific subcortical ROIs and brain networks involved in response to stimuli and surroundings (SMG) and in the regulation of the cardiovascular system (premotor cortex) thus providing new insights in the pathogenesis of SUDEP.
Disclosure: Nothing to disclose.
EPO‐712
Availability and integration of neuroimaging research database in Nigeria
U. Ibrahim 1; A. Moradeyo2; A. Idris1; I. Junaid1; Y. Olamilekan3
1Medicine and Surgery Department, Aminu Kano Teaching Hospital, Kano, Nigeria; 2Medicine and Surgery Department, Lautech Teaching Hospital, Ogbomosho, Ibadan, Nigeria; 3Physiology Department, University of Ilorin/University of Ilorin Teaching Hospital (U.I.T.H), Illorin, Nigeria
Background and Aims: Brain injuries and brain diseases in Nigeria are particularly prevalent, with an annual incidence of 2170 per 100,000 individuals. Approximately 78% of Nigeria's neuroimaging institutes use low‐field‐strength systems that are inefficient for generating conventional neuroimaging database.
Methods: DATA COLLECTION. The central repository data would be established in accordance with the highest ethical standards approved by the ethical committee of the diagnostic centers or its equivalent. Data would be collected from consented individuals presenting to the diagnostic centers for neuroimaging services. DATA PROCESSING. This neuroimaging data would be de‐identified, with personal information removed for research accessibility by the help of African Brain Data Network.
Results: The prospective result of integrating neuroimaging research data would increase the availability of neuroimaging data, which would allow for more robust research. It would contribute to the advancement of neuroimaging and healthcare research in Nigeria.
Conclusion: Our research underscores the pressing need for an integrated neuroimaging data platform in Nigeria, a nation grappling with limitations in neuroimaging capabilities.
Disclosure: Nothing to disclose.
EPO‐713
Clinical use of tau PET in Aβ PET positive individuals: A case series – The HEAD study
V. Machado 1; G. Povala1; G. Negrini1; P. Ferreira1; L. Amaral1; B. Bellaver1; L. Firoza1; D. Tudorascu1; W. Klunk1; W. Jagust2; V. Lowe3; D. Soleimani‐Meigooni4; H. Oh5; B. Pascual6; B. Gordon7; P. Rosa‐Neto8; S. Baker2; V. Machado9; T. Pascoal1
1University of Pittsburgh, Department of Psychiatry, PA, USA; 2Lawrence Berkeley National Laboratory, Berkeley, CA, USA; 3Mayo Clinic, Department of Radiology, Rochester, MN, USA; 4University of California San Francisco, Memory and Aging Center, San Francisco, CA, USA; 5Brown University, Department of Psychiatry and Human Behavior, Providence, RI, USA; 6Houston Methodist Research Institute, Department of Neurology, Houston, TX, USA; 7Washington University in St. Louis, Department of Radiology, St. Louis, MO, USA; 8Translational Neuroimaging Laboratory, McGill University Research Centre for Studies in Aging, Douglas Research Institute, Montréal, QC, Canada; 9UNIVATES, School of Medicine, Lajeado, Brazil
Background and Aims: Clinical phenotypes combined with structure imaging biomarkers, as levels of tau PET pathology, allow a sensitive and specific diagnosis of Alzheimer's disease (AD). We present here the cases of four patients who visited the memory clinic at the University of Pittsburgh Medical Center between June and December 2023 and underwent both Aβ and tau‐PET scans.
Methods: These individuals had standard clinical and cognitive outcomes, typical blood tests ordered in patients with memory impairment, MRI, PET PIB Aβ and two tau PET tracers (MK6240 and Flortaucipir).
Results: All patients had their blood tests normal. Patients 2–4 exhibited mild ischemic changes (Table 1). All patients tested positive for amyloid PET, with varied tau PET results. Patients 1 (MOCA = 6) and 3 (MOCA = 19), who were demented with impaired Instrumental Activities of Daily Living (IADL), had Braak stages V‐VI using both tau PET tracers. Conversely, the mild cognitive impairment (MCI) Patients 2 (MOCA = 19) and 4 (MOCA = 9, neuropsych evaluation indicating MCI) tested positive for MK6240 but negative for FTP.
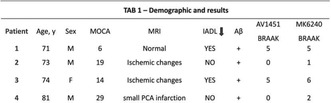
Conclusion: The symptoms of typical amnestic AD presentation were confirmed with similar pattern of Aβ PET. Tau PET demonstrated greater variability, with lower levels observed in less cognitively impaired patients (Figure 1). This small series did not exclude that a low MOCA score combined with Aβ PET could be useful in identifying individuals in the earliest stages candidates to Aβ‐ lowering therapies. Larger samples are necessary in regarding these discrepancies between tau PET uptake and cognitive tests, reinforcing the need for tau PET markers as complementary tests.
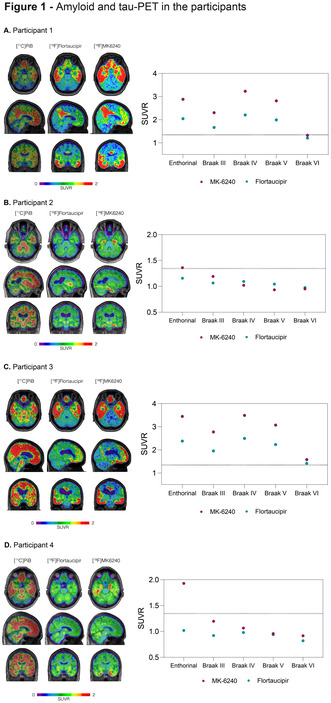
Tau PET‐scans and the difference between the tracers.
Disclosure: Nothing to disclose.
EPO‐714
Exploring atypical forms of Alzheimer's disease through connectomics in early and late‐phase amyloid PET and FDG PET
W. Kreshpa 1; A. Cirone2; S. Garbarino2; F. Massa1; S. Raffa2; A. Chincarini3; L. Roccatagliata2; A. Uccelli2; S. Morbelli4; M. Pardini1
1Università degli studi di Genova, Genoa, Italy; 2IRCCS Ospedale Policlinico San Martino, Genoa, Italy; 3Genoa Division, National Institute for Nuclear Physics, Genoa, Italy; 4Università degli studi di Torino, Turin, Italy
Background and Aims: Alzheimer's disease (AD) is the most common form of dementia, characterized by prominent amnestic impairment of insidious onset. However, atypical presentations such as logopenic variant of primary progressive aphasia, posterior cortical atrophy, corticobasal syndrome and frontal AD, pose diagnostic challenges. This study presents retrospective analysis investigating brain functional differences between typical and atypical AD. Specifically, a structural connectome, a comprehensive map of anatomical white matter connections, was employed alongside late‐phase amyloid‐PET, which resembles regional amyloid uptake. Additionally, this research aims to examine whether early‐phase amyloid‐PET can serve as a surrogate for synaptic dysfunction, similar to [18F]FDG‐PET.
Methods: Thirty patients were selected: 13 with atypical AD and 17 with typical amnestic phenotype. Neuropsychological tests, MRI, [18F]FDG‐PET, and [18F]FBB‐PET were performed for each subject. Structural and functional images underwent spatial registration, segmentation, and intensity normalization, using a custom Python pipeline based on FreeSurfer and ANTs tools. Structural connectomes derived from probabilistic tractography on DWI images of 30 healthy subjects were employed.
Results: Results revealed a significant preservation of the hippocampus in atypical AD (p < 0.05). The connectome analysis demonstrated variations in interconnections among late‐phase amyloid‐PET uptake regions between atypical and typical AD. Furthermore, our findings support the hypothesis that early‐phase amyloid‐PET serves as a reliable marker for synaptic dysfunction.
Conclusion: These findings suggest that structural connectomes in PET imaging can reveil unique neurodegenerative pathways in atypical AD. Moreover, this study supports that early amyloid‐PET phases provides similar information to [18F]FDG‐PET on neurodegeneration among atypical AD patients.
Disclosure: Nothing to disclose.
EPO‐715
Integrated diagnosis and treatment of acute ischemic stroke by nanoparticles based on MRI/NIR dual‐modality imaging
L. Yang
Department of Radiology, The Second Affiliated Hospital, Medical College of Shantou University, Shantou, China
Background and Aims: Rapamycin (RAPA) is an effective autophagy modulator that can promote neuronal survival under ischemic conditions through rational autophagy regulation and is receiving increasing attention. However, its low solubility and poor stability seriously hinder its further application.
Methods: In this study, RAPA, indocyanine green (ICG), epigallocatechin gallate (EGCG), and Gd3+ serving as neuroprotective drugs, near‐infrared fluorescence (NIRF) imaging agents, biomimetic coatings, and magnetic resonance imaging agents, respectively, were co‐assembled into carrier‐free, highly biocompatible ICG‐RAPA‐EGCG‐Gd nanoparticles (IREGd NPs) for synergistic diagnosis and treatment of acute ischemic stroke.
Results: The results showed that the IREGd NPs had good stability and could load RAPA efficiently. IREGd NPs were efficiently uptaken by PC‐12 cells and had a superior neuroprotective effect on oxygen‐glucose deprivation and reoxygenation (OGD/R)‐treated PC‐12 cells than RAPA or EGCG. In addition, IREGd NPs showed good signal characteristics for MRI and NIRF imaging. Finally, in vivo, experiments confirmed that IREGd NPs preferentially aggregated in the ischemic hemisphere and were neuroprotective in transient middle cerebral artery occlusion (tMCAO) rats.

TEM (A) and DLS (B) display the characteristics of IREGd NPs. (C) Cell viability of PC12 cells after incubation with different concentrations of IREGd NPs for 24 h and (D) after incubation with EGCG+RAPA, EGCG, and RAPA for 24 h. (E) CLSM images of cell.
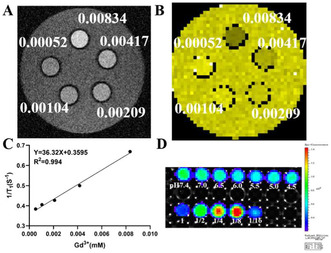
MR and NIF imaging properties of IREGd NPs. (A, B) T1‐WI and T1‐mapping images of different Gd3+ concentrations (mM) at pH = 7.4; (C) functions made with the Gd3+ concentration as the horizontal coordinate and 1/T1 (T1 represents the longitudinal relaxation.
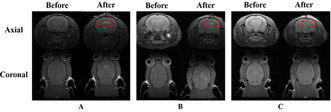
T1‐WI images of in vivo lateral ventricles (A) and brain parenchyma (B) injected with IREGd NPs or PBS (C). Signal altered (A, B)/unaltered (C) areas are within the red ovals.
Conclusion: Overall, carrier‐free IREGd NPs provided a simple alternative approach to achieve bimodal imaging and therapeutic integration in acute ischemic stroke.
Disclosure: Nothing to disclose.
EPO‐716
Contribution of spinal cord magnetic résonance imaging (MRI) as a prognostic biomarker in multiple sclerosis
Y. Koubci; N. Lakri; H. Bouzenada
Central Hospital of Army, Algiers, Algeria
Background and Aims: Multiple sclerosis (MS) is the leading cause of acquired motor disability in young adults. The aim of this study was to determine the prognostic value of spinal cord lesions on the occurrence of relapses and the progression of short‐term disability in MS patients.
Methods: A descriptive, monocentric, prognostic study of a cohort of 100 remittent MS patients, followed for 3 years, all with baseline MRI and follow‐up MRI at 12 months and 30 months. Clinical evaluation was based on the Expanded Disability status scale (EDSS).
Results: Mean age at onset was 28.06 years, mean duration of the disease was 41 months. 68% of patients had spinal cord lesions at the initial stage; initial spinal cord involvement was predictive of relapse onset and worsening of disability over the course of the disease (p < 0.001), and an impact on ambulation in 19% of cases. Multiple spinal cord lesions were significantly associated with a high initial and final EDSS score (≥3) (p = 0.001; p < 0.001). Cervical and cervico‐dorsal sites were predictive of disability aggravation in more than half the cases. In axial terms, >60% of lateral lesions were associated with disability. Posterior lesions were associated with a final EDSS score <3 (p < 0.001). The absence of spinal cord lesions (32%) was associated with an initial and final EDSS score <3 (p = 0.04; p < 0.001)
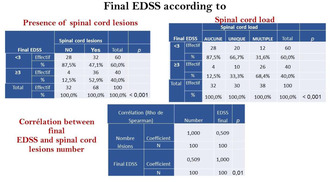
Final EDSS according to spinal cord load lesions.
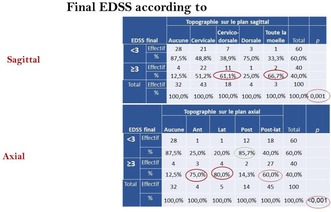
Final EDSS according to sagittal and axial topography of spinal cord lesions.
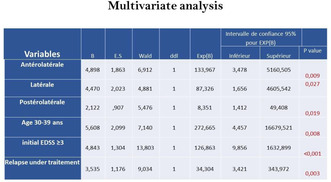
Multivariate analysis; risk factors to reach EDSS 3.
Conclusion: The presence of spinal cord lesions at the start of the disease has a major prognostic role in the development of ambulatory disability, but must be taken into account with other known prognostic factors.
Disclosure: Nothing to disclose.
Peripheral nerve disorders
EPO‐717
Guillain Barre syndrome; clinical features and outcome in three referral hospitals in Cameroon
D. Gams Massi 1; A. Shehou2; V. Sini3; M. Magnerou4; N. Mapoure2
1Douala General Hospital/Faculty of Health Sciences, University of Buea; 2Douala General Hospital/Faculty of Medicine and Pharmaceutical Sciences, the University of Douala; 3Yaoundé General Hospital/Institut Supérieur de Technologie Médicale Yaoundé; 4Douala Laquintinie hospital/Faculty of Medicine and Pharmaceutical Sciences, the University of Douala
Background and Aims: Guillain Barré Syndrome (GBS) is an inflammatory pathology of the peripheral nervous which is characterized by bilateral and progressive sensory‐motor impairment of the peripheral limbs, sometimes extending to the respiratory muscles and cranial nerves. We aimed to determine the clinical features and outcome of Guillain Barré Syndrome cases in Cameroon.
Methods: We reviewed all cases of GBS admitted from January 2017 to March 2023, in General and Laquintinie hospitals of Douala and in Yaoundé General hospital. We excluded patient aged under 16 and incomplete files based on the Brighton diagnostic criteria. Data on sociodemographic characteristic, clinical features, workup, treatments and outcome data were collected and analyzed using SPSS 23.0.
Results: A total of 21 cases of GBS were included, and patients aged < 40 years represented 52.4% of cases. Men represented 61.9% of patients. The average admission rate was 3.5 cases/year. Mean age was 40.8 ± 17.6 years. Most frequent triggering factors were respiratory tract infection (38.1%), and immunization (14.3%). The most common signs were tetraparésis (85.7%), deep tendon areflexia (71.42%) and hyperesthesia (52.38%). Albumino‐cytology dissociation was observed in 6 cases out of 11 CSF sampled. ENMG was performed in 11 patients and classified axonal type (n = 7) and the demyelinating type (n = 4). IV immunoglobulins were administered in 28.6% of patients. Pressure sores (57.9%) and autonomic disorders (14.3%) were the most frequent intra‐hospital complications. We recorded 2 cases of in‐hospital death.
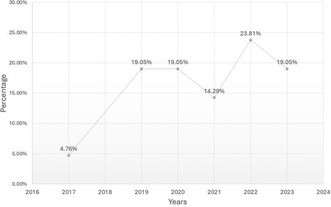
Trend of admission of patients with GBS in Douala General and Laquintinie hospitals and Yaoundé General hospital.
Conclusion: Guillain Barré syndrome is an uncommon condition with sometimes dramatic complication which need more attention.
Disclosure: Nothing to disclose.
EPO‐718
Charcot‐Marie‐tooth type 2CC misdiagnosed as chronic inflammatory demyelinating polyneuropathy
I. Di Sarno 1; S. Tozza1; F. Santorelli2; R. Iodice1; R. Dubbioso1; L. Ruggiero1; M. Nolano1
1Department of Neurosciences, Reproductive and Odonstomatological Sciences, University of Naples “Federico II”, Naples, Italy; 2Molecular Medicine, IRCCS Fondazione Stella Maris, Pisa, Italy
Background and Aims: Charcot‐Marie‐Tooth (CMT) is a group of genetic neuropathies typically characterized by distal muscle wasting and sensory loss, pes cavus and areflexia. Herein we describe a case of Charcot‐Marie‐Tooth with equivocal features misdiagnosed as chronic inflammatory demyelinating polyneuropathy.
Methods: A 30‐year‐old woman was referred to our neuromuscular unit at 28 years old with proximal muscle weakness. Neurological examination showed weakness in lower limb (LL) muscles, marked proximally and mild distally, and absence of ankle deep tendon reflexes. Familial history was negative for neuromuscular diseases. Electromyography showed chronic neurogenic changes in proximal and distal muscles of LL. Nerve conduction study (NCS) showed both normal NCV and slowing with conduction blocks, so a diagnosis of CIDP was advanced and she was treated with intravenous immunoglobulins that were ineffective. At electrophysiological revaluation (after two months) CB in peroneal nerve was not more detectable as also distal CMAP had decreased.
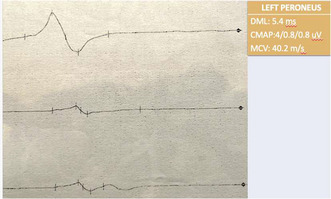
Conduction block in the proband peroneal nerve.
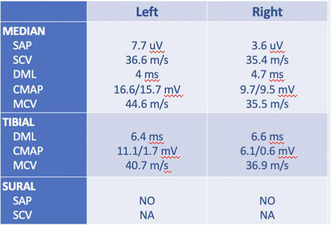
Proband electrophysiological findings.
Results: The hypothesis of genetic neuropathy was considered, and her 8‐year‐old son was evaluated. Neurological examination revealed mild weakness of distal and proximal muscles at lower limbs and mild pes cavus. Neurophysiological investigation showed an intermediate‐axonal pattern. A targeted‐NGS showed heterozygous frameshift mutation (c.3057dupG; p.K1020fs*43) in the NEFH gene, coding for the neurofilament heavy chain and causing CMT2CC, a rare form of axonal CMT with proximal weakness.
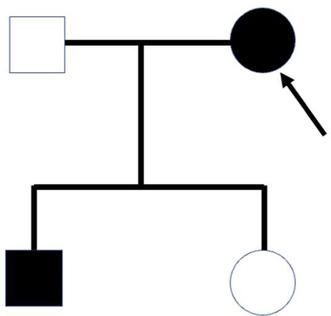
Proband family tree.
Conclusion: Diagnosis of a genetic neuropathy may be challenging when clinical features are atypical or electrophysiological findings suggest acquired demyelination.
Disclosure: Nothing to disclose.
EPO‐719
Abstract withdrawn
EPO‐720
Redundant nerve roots on MRI can predict ongoing denervations in lumbar spinal stenosis patients
K. Kim 1; S. Park1; S. Hong2
1Department of Rehabilitation Medicine, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea; 2Department of Radiology, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea
Background and Aims: Redundant nerve roots (RNRs), which are abnormally elongated and tortuous nerve roots, can be developed secondary to degenerative spinal stenosis. It has been reported that RNRs are associated with worse clinical outcome after decompressive surgery. However, there are limited studies about clinical significance of RNR. This study aims to investigate association of RNRs and denervation potentials observed in electromyographic study (EMG).
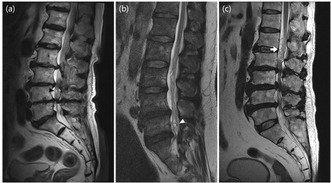
Grading of RNR. (a) mild: the angulation at the most tortuous portion of the roots (black arrowhead) is less than 120 degrees but equal to or greater than 90 degrees, (b) moderate: the angulation at the most tortuous portion of the roots (white arrowhead).
Methods: Among 2003 patients who underwent electrodiagnostic study of lower extremities from January 2020 to March 2023, 193 patients were included demonstrating lumbar spinal stenosis on their spinal MRI. Their clinical information and image findings including presence and of RNRs were investigated. In the EMG study, presence of abnormal spontaneous activity (ASA) was collected. Statistical analysis was performed to compare the difference between patients with and without RNRs. Multivariate logistic regression analysis was conducted to find out factors associated with development of ASA.
Results: RNRs were associated with advanced age (p < 0.001), longer symptom duration (p = 0.009), narrower CSA (p < 0.001) and higher frequency of ASA (p < 0.001). Higher probability of ASA was correlated to the increasing redundancy of nerve (p < 0.001). Multiple logistic regression analysis showed that occurrence of ASA was associated with narrower CSA, multiple stenotic sites, severe RNR.
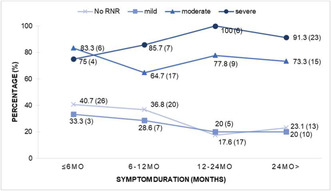
Percentage of patients with ASA at extremities as symptom durations.
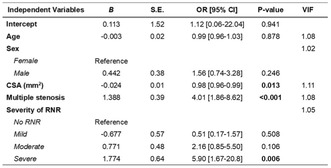
Multivariate logistic regression model for factors potentially associated with presence of abnormal spontaneous activity at extremity muscles.
Conclusion: Presence of RNR, especially severe RNR, is a significant risk factor for development of denervation potentials in electromyographic study. It may help physicians to predict the prognosis of spinal stenosis patients.
Disclosure: None to disclose.
EPO‐721
Neurofilament light chain correlate with small nerve fibre damage parameters in hereditary transthyretin amyloidosis
L. Leonardi
AOU Sant'Andrea, Neurology Department
Background and Aims: Both serum neurofilament light chain (sNfL) levels and small fibre related variables, as skin biopsy and quantitative sensory testing (QST), are valuable disease biomarkers of hereditary transthyretin amyloidosis with polyneuropathy (ATTRv‐PN). Our study aimed to explore the relations between sNfL and small fibre related skin biopsy and QST data in a cohort of ATTRv‐PN patients and asymptomatic carriers.
Methods: We conducted a retrospective analysis of data from 34 individuals (13 ATTRv symptomatic patients and 21 pre‐symptomatic carriers) who underwent sNfL dosage, skin biopsy, and QST, and analyzed correlations between sNFL, IENFD, and thermal cold (CDT) and warm detection thresholds (WDT).
Results: We found that both sNfL and small fibre related skin biopsy and QST parameters significantly differed between carriers and patients (sNfL: p < 0.0001; IENFD: p = 0.0008; CDT, WDT: <0.0001). sNFL levels were normal in all carriers and altered in 85% of patients; IENFD was abnormal in 41% of carriers and 77% of patients, CDT and/or WDT were impaired in 19% of carriers and 54% of patients. sNfL negatively correlated with distal IENFD (r = −0.47, p = 0.005) and significantly correlated with small fibre related QST parameters impairment (CDT: r = −0.68, p < 0.0001; WDT: r = 0.57).
Conclusion: Our study showed that sNfL reliably discriminates symptomatic ATTRv‐PN patients from pre‐symptomatic carriers, and found significant relations between sNfL, skin biopsy, and QST small fibre related parameters, suggesting that sNfL might be a supportive criterion for symptomatic disease transition.
Disclosure: Nothing to disclose.
EPO‐722
Short‐term treatment of CIDP with Efgartigimod: A single center experience in China
J. Lin; C. Sun; C. Zhao
Department of Neurology, Huashan Hospital, Fudan University, Shanghai, China
Background and Aims: Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) is a type of autoimmune neuropathy that presents treatment challenges due to the limitations of standard‐of‐care therapies. Efgartigimod, a neonatal Fc receptor antagonist, has shown potential in treating antibody‐mediated disorders, but its effectiveness for CIDP treatment has not been established.
Methods: This single‐center study in China evaluated the short‐term efficacy and safety of Efgartigimod in five CIDP patients. Clinical effectiveness was assessed using the Inflammatory Neuropathy Cause and Treatment (INCAT) disability scale, Inflammatory Rasch‐built Overall Disability Scale (IRODS), Medical Research Council (MRC) sum score, grip strength, Neuropathy Impairment Score (NIS), and Time Up and Go Test (TUG). Safety was evaluated by monitoring adverse events and measuring white blood cell count, serum albumin concentration, and plasma IgG concentration.
Results: All five (100%) patients responded to Efgartigimod treatment, with four (80%) meeting predefined effectiveness criteria within 8 weeks. Significant improvements were observed across clinical scales, with varied responses among patients. The average reduction rate in total IgG was 43%. Adverse events were minimal, with one patient experiencing transient diarrhea, and no aggravation of pre‐existing conditions was noted.
Conclusion: Efgartigimod demonstrates promising efficacy and safety for short‐term treatment of CIDP, offering a potential alternative therapy. This study provides valuable evidence from real‐world application of Efgartigimod in CIDP, and the results indicate further research is warranted.
Disclosure: Nothing to disclose.
EPO‐723
Effectiveness and safety of ofatumumab in autoimmune nodopathy: A single‐center cohort study
J. Lin; J. Hu; C. Zhao
Department of Neurology, Huashan Hospital, Fudan University, Shanghai, China
Background and Aims: Autoimmune nodopathy is a peripheral neuropathy characterized by acquired motor and sensory deficit with autoantibodies against the node of Ranvier or paranodal region in the peripheral nervous system. Ofatumumab is the first fully human anti‐CD20 monoclonal antibody, and may bring benefits to patients with autoimmune nodopathy.
Methods: This prospective observational study included 7 patients with autoimmune nodopathy, receiving subcutaneous ofatumumab 20 mg every 4 weeks (q4w) (from Week 4, after initial doses on Days 1, 7, and 14). The INCAT disability score, I‐RODS, grip strength, and TUG were collected at entry and every 4 weeks. Antibodies against NF155 and CNTN1 were tested every 4 weeks, using a cell‐based assay at a titer of 1:100.
Results: Six patients with anti‐NF155 antibodies and one patient with anti‐CNTN1 antibodies were included in the studies. At the last visit, six of the seven patients showed clinical improvement on either the INCAT, centile I‐RODS or grip strength. Three of the six patients did not respond well to rituximab. The median time of reaching minimal clinically important difference was 16 weeks. Six of the seven patients improved in the 3m‐TUG, and the median time of the first improvement was 4 weeks. The paranodal antibodies in these patients remain positive during the follow up visit.
Conclusion: Ofatumumab 20 mg q4w subcutaneously was effective and safe in a part of patients with autoimmune nodopathy. The association between clinical improvement and anti‐paranodal antibodies needs further investigation.
Disclosure: Nothing to disclose.
EPO‐724
Fatigue in chronic inflammatory demyelinating polyradiculoneuropathy
N. Başcı; A. Gündüz; M. Tütüncü; N. Uzun Adatepe
Department of Neurology, Cerrahpasa Medical Faculty, IUC, Istanbul, Turkey
Background and Aims: Fatigue is a common symptom in chronic inflammatory demyelinating polyradiculoneuropathy (CIDP), significantly affecting the patients’ quality of life. In this study, we aimed to evaluate the severity of fatigue in CIDP patients and its correlation to other clinical and electrophysiological parameters.
Methods: This is a prospective study. We invited all patients with CIDP diagnosis according to latest criteria and performed Fatigue Severity Scale (FSS), INCAT (Inflammatory Neuropathy Cause and Treatment Disability Scale), I‐RODS (Inflammatory Rasch‐built Overall Disability Scale), Hamilton Depression Rating Scale (HAM‐D), Pittsburgh Sleep Quality Index (PSQI) and Visual Analogue Scale (VAS) for pain, nerve conduction studies. The final score on FSS represents the average of nine items; a score above 4.0 indicates the presence of fatigue. We compared the clinical and electrophysiological findings between patients with and without fatigue.
Results: There were 27 patients with CIDP in study period (mean age: 54 ± 12.6 years; age range 19 and 73 years; %29.6 women). Among patients included, 26% had fatigue. All patients with fatigue had axonal involvement in the follow‐up examination. The number of nerves with conduction block or reduced conduction velocity did not differ between groups. INCAT and I‐RODS scales did not differ significantly between groups while PSQI, HAM‐D and VAS scores were slightly higher in the fatigue group.
Conclusion: Fatigue can be related to various factors independent of disease progression; such as sleep, depression and pain.
Disclosure: Funding: TUSEB 2023‐B‐01 Group B Project.
EPO‐725
CASPR2 antibodies in CSF in Isaac's syndrome: Altering the central neuropathic pain perception?
R. Theologou 1; Achilleos1; Liampas1; P. Neophytou1; R. Louka1; A. Artemiadis2; Tzartos3; G. Hadjigeorgiou2; P. Zis2
1Neurology Clinic, Nicosia General Hospital, Nicosia, Cyprus; 2Medical School, University of Cyprus, Nicosia, Cyprus; 3Neurology Clinic, Attikon Hospital, National and Kapodistrian University of Athens, Athens, Greece
Background and Aims: Isaacs syndrome (IS) or acquired neuromyotonia is a rare immune‐mediated neuromuscular disorder, resulting in increased excitability of the peripheral nerves. Clinically it is characterized by fasciculations, cramps, excessive sweating and often presence of CASPR2 autoantibodies. IS can occur as a paraneoplastic condition, or it can remain idiopathic.
Methods: Case report and review of the literature.
Results: A 65‐year‐old man with a past medical history of prostate cancer, treated with radiotherapy 4 years ago, was referred to our Department because of a 3‐year history of neuropathic pain and painful cramps in the lower limbs. Neurophysiological examination revealed spontaneous duplet, triplet and multiplet potentials in all muscles examined. IS was suspected and confirmed with the presence of positive VGKC, CASPR2 and LGI1 auto‐antibodies in the serum and the cerebrospinal fluid, despite the fact there was no CNS involvement clinically. Our literature review identified six more IS cases in which CASPR2 antibodies were checked in the CSF. Out of these, two showed positive CASPR2 antibodies. In one IS remained idiopathic while in the other was associated with recurrence of malignant thymoma. Including ours, all 3 cases reported neuropathic pain.
Conclusion: To our knowledge, this is the first reported case of IS in a patient with a past medical history of prostate cancer and one of a few where CASPR2 antibodies were present in the CSF despite the lack of clinical features of CNS involvement. Presence of CASPR2 antibodies in the CSF in IS patients may be associated with an increased perception of neuropathic pain.
Disclosure: Nothing to disclose.
EPO‐726
Peripheral neural correlates of isolated genital numbness with selective serotonin reuptake inhibitor exposure
S. Wright 1; P. Malladi1; S. Simeoni1; J. Panicker2
1Uro‐Neurology, National Hospital for Neurology and Neurosurgery, UCLH NHS Foundation Trust, London, UK; 2UCL Queen Square Institute of Neurology, Faculty of Brain Sciences, University College London, London, UK
Background and Aims: Isolated genital numbness is an uncommon neurological presentation and very little guidance exists on its assessment and aetiology. Selective serotonin reuptake inhibitors are an effective treatment for depression and anxiety disorders however in recent years, it has become apparent there are sexual side effects and genital sensory changes have been described. We aim to describe the clinico‐neurophysiologic profile in non‐neurological individuals with isolated genital numbness and exposure to selective serotonin reuptake inhibitor (SSRI).
Methods: Consecutive referrals with impairment of genital sensation to a tertiary referral centre from 2018 to 2023. Urogenital clinical symptoms, contributing factors and past medical history were recorded. Pelvic sensory examination (pinprick and von frey hair) was performed at the time of sacral sensory neurophysiology testing.
Results: 12 Individuals were identified with genital numbness and current or previous exposure to SSRI (female, 33.3%). The median age was 37 years. Nine individuals reported an abnormal clinical pelvic sensory examination and had normal pelvic neurophysiology. Two individuals with SSRI exposure had abnormal pelvic neurophysiology. SSRI exposure was not a significant predictor for genital numbness. Seven reported sexual dysfunction.
Conclusion: Recent diagnostic criteria for post‐SSRI sexual dysfunction is defined as somatic or erogenous genital sensation after treatment stops. We found 83% of individuals with genital numbness and exposure to SSRI had a normal pelvic neurophysiology examination. The concept of erogenous sensation is relevant and we postulate that the aetiology of SSRI associated genital numbness with normal neurophysiology is due to central sensory and emotional processing dysfunction.
Disclosure: SLW reports a relationship with Roche that includes honoraria and support to attend conferences; with Merck for speaking honoraria and support to attend conferences. Jalesh Panicker reports a relationship with: Wellspect HealthCare UK that includes: speaking and lecture fees; with Idorsia Pharmaceuticals Ltd that includes: consulting or advisory; with Coloplast Ltd that includes: consulting or advisory and speaking and lecture fees; with Corporate Allergan Inc that includes: speaking and lecture fees; with Novartis that includes: speaking and lecture fees; Cambridge University Press: royalties; Continence Reports Editorial Board.
EPO‐727
Unmet need in patients with chronic inflammatory demyelinating polyneuropathy: Results from a Real‐World Survey
S. Rinaldi 1; A. Borsi2; C. Gary2; W. Noel2; W. Karmous2; J. DeCourcy3; J. Wright3; Y. Taylor3; H. Iqbal3; L. Querol4
1Nuffield Department of Clinical Neurosciences, University of Oxford; 2Johnson & Johnson Innovative Medicine EMEA; 3Adelphi Real World, Bollington, UK; 4Hospital de la Santa Creu i Sant Pau, Barcelona, Spain
Background and Aims: Chronic inflammatory demyelinating polyneuropathy (CIDP) is a disabling neurological condition characterised by progressive muscle weakness and impaired sensory function. The aim of this study was to identify unmet needs among patients with CIDP.
Methods: Data were drawn from the Adelphi CIDP Disease Specific Programme™, a cross‐sectional survey of neurologists in France, Germany, Italy, Spain, UK (September 2022 – April 2023), treating at least two CIDP patients per typical month. Patients completed patient‐reported outcome assessments, including the Inflammatory Rasch‐Built Overall Disability Scale (I‐RODS) and Work Productivity and Activity Impairment questionnaire (WPAI:SHP). This real‐world data is limited by participating physicians’ confirmation of the included patient's CIDP diagnosis.
Results: 83 physicians provided data for 542 patients with CIDP, of whom 463 were receiving maintenance treatment (1st line: 293; 2nd: 140; 3rd: 26; 4th/5th: 4 [excluded from analyses]). Physicians reported dissatisfaction, or partial satisfaction with treatment for 57.9% of patients (1st: 57.7%; 2nd: 52.1%; 3rd: 92.3%). Across all lines, the most frequent reason for lack of satisfaction was “efficacy declining over time”. Patients reported a mean (SD) I‐RODS centile score of 59.8 (18.5) (1st: 61.8 [19.4]; 2nd: 56.6 [16.4]; 3rd: 57.4 [21.4]), and a mean WPAI percentage activity impairment of 43.0 (25.2) (1st: 40.1 [24.4]; 2nd: 47.3 [25.5]; 3rd: 50.0 [32.2]).
Conclusion: Patients with CIDP reported substantial disability and impairment in daily activities, and in many cases their physicians were not fully satisfied with treatment. Identifying factors associated with poor initial treatment response and loss‐of‐efficacy, and new therapeutic developments, may lead to improved outcomes for these patients.
Disclosure: Data collection was undertaken by Adelphi Real World as part of an independent survey, entitled the Adelphi Real World CIDP Disease Specific Programme. Janssen were one of multiple subscribers to the dataset. The study described here was funded by Janssen.
EPO‐728
Nodal‐/paranodal autoantibody‐associated autoimmune nodopathies in Estonian population
T. Unt; K. Kannel; S. Ütt; U. Thomson; A. Reitsnik; M. Maiorova; K. Gross‐Paju
West‐Tallinn Central Hospital, Neurology and Psychiatry Clinic
Background and Aims: Autoantibodies to peripheral nerve molecules seem to play role in the pathogenesis and also provide diagnostic, prognostic, and therapeutic value for autoimmune peripheral neuropathies, such as CIDP. Corticosteroids, intravenous immunoglobulin (IVIg) and plasma exchange are mainstays of treatment, yet some patients respond poorly to standard treatments. Disease‐specific antibodies targeting proteins at the node and paranode of Ranvier, such as neurofascin‐155 (NF155), contactin‐1 (CNTN1), contactin‐associated protein 1 (Caspr1), neurofascin‐140/186 (NF140/186), have been described in small subsets of CIDP patients with similar clinical features, treatment response, namely poor response to IVig and more favourable to rituximab, and hence differing from typical CIDP.
Methods: This study presents an overview of autoimmune nodopathies in Estonian population based on cohort of polyneuropathy patients in West‐Tallinn Central Hospital's Neurology department tested over a period form October 2022 to October 2023.
Results: 11 out of 112 patients tested positive for nodal‐/paranodal autoantibodies: 7 for contactin1, 3 for NF155 IgG, 1 for NF155 IgM, 3 for NF155 IgG and IgM, 1 for contactin1 and NF155 IgG antibodies. Most frequent clinical picture among nodopathy patients was severe flaccid tetra‐ or paraparesis with sensory disturbances. Other clinical pictures included cerebellar findings, gait problems, but also central symptoms not reported in scientific literature as part of nodopathy syndrome.
Conclusion: Testing for nodal/paranodal antibodies can help improve diagnostic accuracy and guide treatment for polyneuropathy patients, especially those suspected of having inflammatory demyelinating polyneuropathy. Considering the varied clinical picture in our cohort, there also remains the question whether all positive results are of clinical significance.
Disclosure: Nothing to disclose.
EPO‐729
Characteristics and outcome of CIDP patients according to their electrodiagnostic certainty (2021 EAN/PNS criteria)
V. Loser; A. Vicino; K. Staedler; T. Kuntzer; M. Theaudin
Nerve‐Muscle Unit, Neurology Service, Department of Clinical Neurosciences, Lausanne University Hospital and University of Lausanne, Lausanne, Switzerland
Background and Aims: Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) has heterogeneous presentation and clinical course. The aims of this study are to describe the clinical and electrophysiological characteristics of patients with CIDP or possible CIDP, according to the latest 2021 EAN/PNS criteria, and to compare the long‐term outcome in both groups.
Methods: We retrospectively included 29 adult “CIDP” and 21 “possible CIDP” patients. We reviewed their clinical data, which included the neuropathy impairment scale (NIS) and modified Rankin Scale (mRS), response to treatment, cerebrospinal fluid examination, and nerve conduction studies parameters. Data were collected at first evaluation of the patient (T0), and at one (T1), two (T2) and three years (T3).
Results: At baseline, CIDP patients had a higher NIS score (median NIS score of 38 versus 20.5, p = 0.03), and more frequently a “typical CIDP” phenotype (p = 0.02) than possible CIDP patients. Other variables did not differ significantly. CIDP patients tended to have a better objective response to immunotherapy (66% responders) than possible CIDP patients (43% responders, p = 0.15). Between baseline and T3, there was a median (IQR) Δ NIS of −12.8 (−32, 0) and Δ mRS of −1 (−2, 0) for CIDP patients and 2.5 (−7.8, 8.5) and 0 (−0.8, 0) for possible CIDP patients (p = 0.01 and <0.01 respectively).
Conclusion: “CIDP” patients had a more severe neuropathy, estimated with the NIS score, and “possible CIDP” patients had a more atypical phenotype at baseline. Our data suggest that patient outcome is better in CIDP than possible CIDP.
Disclosure: Nothing to disclose.
Neurorehabilitation
EPO‐730
TDCS effects on motor and cognitive function in paediatric brain injury: Systematic review and meta‐analysis
A. Cerezo‐Zarzuelo 1; M. Rios‐Lago2; F. Sanchez‐Cuesta3; B. Gavilan‐Agusti4; A. Hurtado‐Martinez3; J. Romero‐Muñoz3
1Psychology PhD Program, Universidad Nacional de Educación a Distancia (UNED), Madrid, Spain; 2Department of Basic Psychology II, School of Psychology, Universidad Nacional de Educación a Distancia (UNED), Madrid, Spain; 3Brain injury and Movement Disorders Neurorehabilitation Group (GINDAT), Institute of Life Sciences, Francisco de Vitoria University, Pozuelo de Alarcón, Spain; 4Brain Damage Unit, Beata Maria Ana Hospital, Madrid, Spain
Background and Aims: Paediatric non‐progressive brain injuries result in diverse impairments, including motor and cognitive issues. Transcranial direct current stimulation (tDCS), emerges as a technique to influence neuroplasticity processes as an adjunct therapy in rehabilitation. This review aims to assess tDCS effects on motor and cognitive variables in non‐progressive paediatric brain injuries, correlation with intervention parameters and associations between functions.
Methods: A systematic review and meta‐analysis were conducted, assessing randomized controlled trials in patients with paediatric brain damage and cognitive or motor variables with tDCS interventions. 5 databases were searched. PEDro scale, ROB‐2 and GRADE assessed methodological and evidence quality.
Results: Data from 19 studies (447 participants) (fig.1) revealed positive effects on gait, balance, functional performance, and cognition. Upper limb function evidence remains inconsistent due to limited publications. Cognitive intervention influenced motor outcomes, and motor‐centered interventions impacted functionality related to cognition. Meta‐analysis showed statistically significant improvements in gait (SMDs: 0.83–0.90, p < 0.0001), balance (Centre of pressure oscillations SMDs: −0.51 to −1.13, p < 0.02; PBS SMDs: 0.48 to 0.56, p < 0.0001) and self‐care (SMD: 0.40, p < 0.01) (Table 1). Mean PEDro scale score was 7.46. According to ROB‐2, two studies presented low risk of bias, 12 studies had some concerns and 5 presented high risk. Quality of evidence is small for gait and self‐care, and medium for balance.
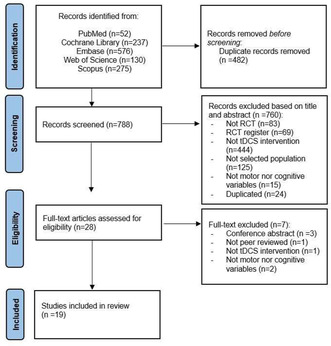
PRISMA flow diagram.
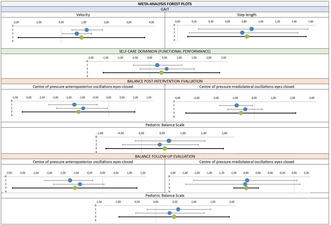
Meta‐analysis forest plots.
Conclusion: TDCS seems beneficial for cognitive and motor variables in paediatric brain damage. Both variables seem to be interconnected, so further research with homogeneous samples, standardized and combined protocols is needed.
Disclosure: Authors had no conflicts of interest. Funding by GMP foundation.
EPO‐731
Aerobic capacity moderates the association between cervical cord atrophy and disability in MS patients
M. Albergoni1; C. Dallari1; P. Preziosa 2; A. Meani1; P. Valsasina1; M. Filippi3; M. Rocca2
1Neuroimaging Research Unit, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy; 2Neuroimaging Research Unit, Division of Neuroscience, and Neurology Unit, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy; 3Neuroimaging Research Unit, Division of Neuroscience, Neurology Unit, Neurorehabilitation Unit, and Neurophysiology Service, IRCCS San Raffaele Scientific Institute, and Vita‐Salute San Raffaele University, Milan, Italy
Background and Aims: Cervical cord atrophy has been associated with disability in multiple sclerosis (MS). Higher aerobic capacity (AC) has shown positive effects on several symptoms related to MS, which may also influence disability level. This study aimed to understand whether AC moderates the association between cervical cord atrophy and disability in MS.
Methods: In this cross‐sectional analysis, expanded disability status scale (EDSS), peak of maximal oxygen consumption (VO2max) and mean upper cervical cord area (MUCCA) calculated from 3D T1‐weighted brain MRI images were obtained for 60 MS patients and 36 healthy controls (HC). The HC group was used to define VO2max z‐scores and −1 standard deviation was considered as cut‐off to identify patients with low or high AC. In MS patients, an age‐ and sex‐corrected analysis was conducted to understand if AC can moderate the association between MUCCA and EDSS.
Results: Compared to HC, MS patients showed lower MUCCA and VO2max values (p < 0.001). The interaction between MUCCA and AC was significant (β = −0.142, p = 0.002), indicating that the relationship between MUCCA and EDSS was moderated by AC. Lower MUCCA was associated with higher EDSS score only in patients with low AC (β = −0.115, p < 0.001), no association was found in patients with high AC (β = 0.027, p = 0.486).
Conclusion: This study shows that AC is a moderator of the relationship between MUCCA and EDSS, suggesting that high level of AC may represent a functional reserve able to prevent or limit clinical disability in MS patients. Funding. Partially supported by Italian Ministry of Health (GR‐2019‐12369599).
Disclosure: M Albergoni, C Dallari, A Meani, and P Valsasina have nothing to disclose; P Preziosa received speaker honoraria from Roche, Biogen, Novartis, Merck Serono, Bristol Myers Squibb, Genzyme, Horizon and Sanofi, and research support from Italian Ministry of Health and Fondazione Italiana Sclerosi Multipla (FISM). M. Filippi received compensation for consulting or speaking activities services from Alexion, Almirall, Biogen, Bayer, Celgene, Chiesi Italia SpA, Eli Lilly, Genzyme, Janssen, Merck, Neopharmed Gentili, Novartis, Novo Nordisk, Roche, Sanofi, Takeda, and TEVA; participation in Advisory Boards for Alexion, Biogen, Bristol‐Myers Squibb, Merck, Novartis, Roche, Sanofi, Sanofi‐Aventis, Sanofi‐Genzyme, Takeda; scientific direction of educational events for Biogen, Merck, Roche, Celgene, Bristol‐Myers Squibb, Lilly, Novartis, Sanofi‐Genzyme; he receives research support from Biogen Idec, Merck‐Serono, Novartis, Roche, Italian Ministry of Health, Italian Ministry of University and Research, and FISM. MA Rocca received consulting fees from Biogen, Bristol Myers Squibb, Eli Lilly, Janssen, Roche; speaker honoraria from AstraZaneca, Biogen, Bristol Myers Squibb, Bromatech, Celgene, Genzyme, Horizon Therapeutics Italy, Merck Serono SpA, Novartis, Roche, Sanofi and Teva; research support from MS Society of Canada, Italian Ministry of Health, Italian Ministry of University and Research, and FISM.
EPO‐732
A combined neuromodulation protocol to enhance cognitive and lower limb rehabilitation in corticobasal degeneration
A. Hurtado‐Martínez 1; Y. González‐Zamorano2; A. Martínez‐Benito1; M. Moreno‐Verdú3; D. De Noreña4; F. Sánchez‐Cuesta1; J. Romero1
1Brain Injury and Movement Disorders Neurorehabilitation Group (GINDAT), Francisco de Vitoria University, Pozuelo de Alarcón, Spain; 2Cognitive Neuroscience, Pain, and Rehabilitation Research Group (NECODOR), Faculty of Health Sciences, Rey Juan Carlos University, Madrid, Spain; 3Brain, Action and Skill Laboratory (BAS‐Lab), Institute of Neuroscience (Cognition and Systems Division), UC Louvain, Woluwe‐Sain‐Laimbert, Belgium; 4Brain Damage Unit, Beata María Ana Hospital, Madrid, Spain
Background and Aims: Corticobasal Degeneration (CBD) is characterized by asymmetrical motor alterations and neuropsychological impairments. No effective therapy is known. Non‐invasive neuromodulation can modulate cortical activity in other diseases, improving motor performance (1). Motor imagery and action observation are known to improve motor control and gait in several neurological disorders (2). We describe the outcome of a personalized neuromodulation protocol on a 71‐year‐old female, diagnosed with CBD. A PET‐CT revealed right frontal hypoactivity. Although lower limb strength is normal, alien leg and apraxia rendered her wheelchair‐bound. The objective was to assess the effectiveness of a non‐invasive neuromodulation protocol—tDCS, Action Observation (AO), and Motor Imagery (MI)—for enhancing motor and cognitive performance.
Methods: 20 sessions of 20‐minute 2 mA anodal tDCS stimulation over right M1, combined with 30‐minute AO+MI (fig 1). Treatment was administered daily for 4 weeks. Training involved different movements each weekday (fig 2), with a gradual shift from AO to a more active approach as weeks progressed.
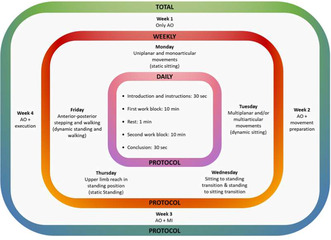
FIGURE 1 The four‐week intervention protocol based on graded progression. AO: Action Observation; MI: Motor Imagery; tDCS: Transcranial Direct Current Stimulation.
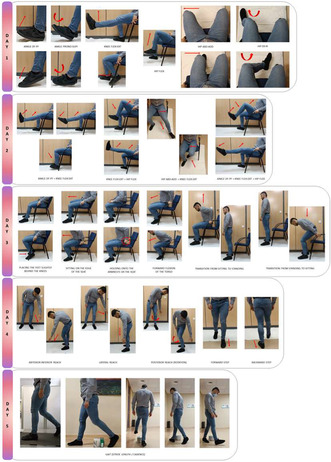
FIGURE 2 The weekly intervention protocol based on graded progression.
Results: Post‐treatment improvements were observed in balance (16 to 23), functional strength (5TSTS 83 to 53), and partially sustained postural control enhancements (5TSTS 83 to 67 in follow‐up). Persistent gains in set‐shifting, inhibitory control (TMT‐B), working memory (Inverse Digits), and attentional span (Direct Digits) were noted. Post‐treatment improvements in emotional well‐being and general health (SF‐36) weren't sustained. FES‐I scores remained stable post‐treatment but rose during follow‐up.

TABLE 1 Outcome measures pertaining to each domain evaluation. Score columns A to C correspond to each of the 3 evaluations: baseline, post‐intervention and follow‐up.
Conclusion: The combined tDCS+AO+MI protocol maintained or improved balance, motor control, attentional, mnesic, and executive functions in a CBD patient, highlighting the potential of this technology in CBD rehabilitation and treatment.
Disclosure: Nothing to disclose.
EPO‐733
Motivation and recovery: An analysis of reward sensitivity and motor learning after ischemic stroke
A. Oppermann 1; J. Maas1; J. Rogenz1; L. Opitz1; H. Am Ende2; H. Köhler3; A. Schmidt3; S. Brodoehl4; C. Klingner4; F. Wagner4
1IZKF Graduate Program Experimental Medicine, Jena University Hospital, Germany; 2Else Kröner Graduate School for Medical Students “JSAM”, Jena University Hospital, Jena; 3Biomagnetic Center, Jena University Hospital, Jena; 4Department of Neurology, Jena University Hospital, Jena
Background and Aims: Stroke is a major global cause of disability, posing challenges in neurological rehabilitation. Cerebral network reorganization and learning limitations are critical in this process. Despite the recognized importance of behavioral rehabilitation, the specific role of the brain's reward system in post‐stroke learning remains unclear. Hypothesis: Building on our prior findings (Wagner et al., 2023), we posit an intrinsic link between the reward system's functionality and motor learning abilities after a stroke. We propose parallel recovery processes for both, with a gap in understanding their timelines.
Methods: A cohort study of 20 stroke patients (mean age: 67, range: 55–80 years) evaluated at t 3–4 months post‐stroke. Motor learning and reward system functionality were assessed using the Monetary Incentive Delay (MID) task during MEG for connectivity analysis. A (VR) learning environment was used for five days to control fluctuations and to study motor learning consolidation.
Results: Patients displayed reduced reward sensitivity, needing greater incentives for improvement, and experienced learning deficits. These deficits correlated with altered connectivity patterns during the MID task, revealing stroke's impact on the reward system and behavior. Learning impairment closely linked to reward sensitivity, irrespective of lesion localization (Coherence Analyses ongoing).
Conclusion: By demonstrating the connection between stroke, reward sensitivity, and learning ability, this research contributes valuable knowledge to the field, suggesting why some stroke survivors continue to experience long‐term challenges despite rehabilitation. The findings underscore the necessity of assessing reward sensitivity in stroke patients to optimize rehabilitation protocols, thereby maximizing their recovery potential.
Disclosure: Nothing to disclose.
EPO‐734
The role of sleep in motor memory consolidation in subacute stroke patients: A pilot study
A. Antonioni 1; N. Cellini2; A. Ugolini1; A. Baroni1; G. Fregna1; N. Lamberti1; F. Manfredini1; P. Malerba3; S. Straudi1
1Department of Neuroscience and Rehabilitation, University of Ferrara, Ferrara, Italy; 2Department of General Psychology, University of Padua, Padua, Italy.; 3School of Medicine, The OhioState University, Columbus, Ohio
Background and Aims: Since sleep improves motor learning and stroke patients are frequently characterised by sleep disorders, it is essential to evaluate its contribution in memory consolidation in this context. While evidence already exists in chronic stroke, data are still scarce on the subacute phase during neurorehabilitation treatment. In order to characterise the role of sleep in subacute stroke, we evaluated: i) whether sleep promotes the consolidation of declarative and non‐declarative memory; ii) possible correlations between sleep and motor and cognitive performance.
Methods: Eight subacute stroke patients, on different days, underwent two experimental conditions each including two sessions of the Memory Similarity Task (MST) and two sessions of the Finger‐tapping Task (FTT). The two conditions, in randomised order, involved: (I) Day trial: patients were tested first at 8 am and, thereafter, at 8 pm, avoiding sleep during the day; II) Night trial: test times were reversed with a night's sleep between them. Moreover, sleep and biometric data were collected by means of a ©Fitbit device.
Results: Accuracy and recognition memory at MST showed a significant effect of session (p < 0.001). Furthermore, patients' recognition memory improved in the sleep condition rather than in wakefulness (p = 0.041). Similarly, FTT accuracy had a significant effect of session (p < 0.001). Moreover, an improvement in sleep‐related accuracy was observed (p = 0.025). The session‐by‐condition effect was not statistically significant in both tasks.
Conclusion: Sleep seems crucial in the consolidation of procedural memory also in the subacute stroke timeframe. Thus, sleep quality interventions are fundamental in promoting recovery from the earliest stroke stages.
Disclosure: The authors declare no conflicts of interest. This work was supported by the project MNESYS (PE0000006) – A Multiscale integrated approach to the study of the nervous system in health and disease (DN. 1553 11.10.2022).
EPO‐735
Gait rehabilitation of patients after stroke using the C‐Mill treadmill
P. Konecny 1; G. Krejstova2; K. Konečná3
1Clinical Rehabilitation Department of the Faculty of Physical Therapy and the Neurological Clinic of the Faculty of Medicine, Olomouc, Czechia; 2Centre for Medical Rehabilitation of the Hospital and Neurological Department of AGEL Prostějov, Czechia; 3Ordinace FBLR, Czechia
Background and Aims: Patients after stroke often have gait disturbances with asymmetry, slowing, discoordination of gait and increased risk of falling. Gait rehabilitation on the C‐Mill walking/treadmill is one way to improve gait parameters. Aim of the study: to test whether using the C‐Mill treadmill will improve walking parameters such as walking speed and gait quality.
Methods: 20 probands in subacute to chronic stage after stroke participated in the study. All patients had gait impairment but with the condition of walking without support. Patients were randomly divided into a control group (standard rehabilitation + 1 hour of C‐Mill walking per week) and an experimental group (standard rehabilitation + 5 hours of C‐Mill walking per week). Before starting therapy, medical history and clinical tests were taken and questionnaires were filled in for all patients. After a 3‐week hospitalization with intensive rehabilitation and C‐mill walking training, an exit examination was performed. Gait speed, subjective perception of gait quality, and self‐sufficiency were assessed.
Results: At baseline examination, patients in the experimental group showed clinically and statistically significant (p < 0.05) improvement compared to the control group. This was evident in all measured domains, i.e.: gait speed, subjective perception of gait quality and self‐sufficient.
Conclusion: the combination of complex rehabilitation (physiotherapy, mechanotherapy, physical therapy and gait training on the C‐Mill treadmill positively affects gait in patients in the subacute and chronic stage after stroke.
Disclosure: We have no conflicts of interest.
EPO‐736
Outcome measures to assess the efficacy of physical therapy in postural orthostatic tachycardia: A systematic review
H. Halbedl 1; N. Campese1; B. Calió1; G. Schönherr1; R. Granata1; J. Mitterhuber1; G. Göbel2; G. Wenning1; A. Fanciulli1
1Department of Neurology, Medical University of Innsbruck, Innsbruck, Austria; 2Department of Medical Statistics, Informatics and Health Economics, Medical University of Innsbruck, Innsbruck, Austria
Background and Aims: Physical therapy is recommended as first‐line treatment for individuals with POTS by expert consensus. There is a need to identify the evidence base of this treatment approach. Here we evaluated how primary (p) and secondary (s) outcome has been measured to date.
Methods: We systematically screened the databases PubMED, Cochrane and Web of Science combining the keywords: “Postural orthostatic tachycardia”, “physical therapy”, "exercise".
Results: We selected 17 studies and two study protocols. Change after exercising was measured by active standing test (primary np = 3, secondary ns = 10) or head‐up tilt test (np = 5, ns = 3), cardiopulmonary exercise tests (np = 3, ns = 8), pulse‐oximetry (np = 0, ns = 1), walking test (np = 0, ns = 1) or questionnaires (np = 1, ns = 13). Mean or highest heart rate response to exercise measured at different timepoints was a common outcome (np = 6, ns = 12). Further primary outcome measures were: time spend upright and steps per day (n = 1), number of individuals who fulfilled the POTS‐criteria (n = 2) or peak oxygen uptake (VO2max, VO2peak) (n = 3). Symptom severity improvement as secondary outcome was assessed with the Short Form Health Survey in three studies, Composite Autonomic Symptom Score −31 items (n = 2), Vanderbilt Orthostatic Symptom Score (n = 3), Malmö‐POTS‐questionnaire and Boston Autonomic Symptom Questionnaire (one study each). Health related quality of life was assessed with the EQ‐5D‐5L in two studies and with the SF‐36 in one.
Conclusion: Recent studies and ongoing trials adopt detailed outcome assessments, taking into account POTS clinical heterogeneity and focusing on meaningful changes of functional ability.
Disclosure: Nothing to disclose.
EPO‐737
Abstract withdrawn
EPO‐738
Role of supination, extension and abduction posture in upper limb spasticity prevention in acute stroke
V. Singh; A. Pathak; A. Kumar
Department of Neurology, Institute of Medical Science, Banaras Hindu University, Varanasi, India
Background and Aims: Post‐stroke spasticity is a common complication of stroke. The study evaluated the efficacy of a posture opposite to the typical spastic posture i.e. Supinated forearm, Extended fingers and elbow and Abducted and externally rotated shoulder (SEA) with wrist in neutral position (Figure 1) in acute stroke patients with flaccid weakness in prevention of development of spasticity.

Figure depicting the application of a splint keeping the flaccid upper limb of a patient in a SEA posture i.e. Supinated forearm, Extended fingers and elbow and Abducted and externally rotated shoulder (SEA) with wrist in neutral position.
Methods: Hemodynamically stable acute stroke patients between 18–80 years of age with flaccid upper limb weakness presenting within 72 hours were included. It was a prospective, single‐center, randomized, open‐label trial with blinded endpoint assessment.
Results: Of 170 acute stroke patients, 76 met the inclusion criteria. 38 patients randomized in each splint (Group 1) and control arm (Group 2). Ten patients lost to follow up. Of remaining 66 patients (34 in splint and 32 in control), the median age of patients was 55 years. Forty‐two (64%) patients were male. There was no significant difference in baseline demographic, clinical, radiological, and biochemical parameters between the two groups (Table 1). At 3 and 6 months, there was significant difference (p value < 0.05) in Modified Ashworth upper limb spasticity score at elbow, forearm (pronation and supination), wrist and fingers between the two groups. Barthel Index for Activities of Daily Living was also significantly better in group 1 at 3 and 6 months (Table 2). However, there was no difference in mRS score during follow up.

Comparison of baseline demographic, clinical, radiological and laboratory variables between the two groups.
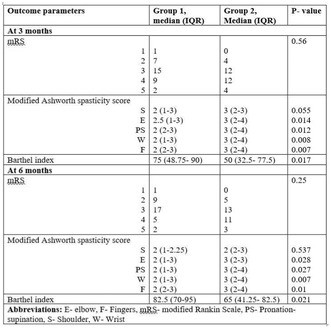
Comparison of outcome measures between the two groups at 3 and 6 months.
Conclusion: SEA posture if applied early in acute stroke patients is effective in reducing the grade of upper limb spasticity.
Disclosure: Nothing to disclose.
EPO‐739
Creating interactive virtual reality applications for social deficit remediation in children with neurological disorders
M. Saard1; A. Roštšinskaja 1; C. Kööp1; L. Uutsalu2; A. Kolk2
1Faculty of Medicine, University of Tartu, Tartu, Estonia; 2Department of Pediatrics and Neurology, Tartu University Hospital Children's Clinic, Tartu, Estonia
Background and Aims: The aim was to evaluate the suitability of SocialVR applications developed for pediatric neurorehabilitation with assessing anxiety levels during difficult social situations.
Methods: 33 children aged 6–15 yrs participated: 17 with neurological disorders (ND) and 16 healthy controls. Therapist observed scenarios on screen, selecting the avatar's according to child's skills. Headsets Oculus Rift or HTC Vive were used. 10 difficult social VR metaphors with 2 levels of complexity were created by authors (cafeteria, cinema, bullying, etc.). Social anxiety was assessed by heart rate (HR) changes in all children and with Spence Anxiety Questionnaire (SCAS) in 14 children.

FIGURE 1 Child with ND participating in a cafeteria metaphor during a social rehabilitation session.
Results: Applications of varying severity were suitable and indicated for developing social neurorehabilitation. Most challenging situations were “friend losing a phone” (average HR rise 9.1) and “ball in neighbor's garden” (HR rise 9). Therefore, metaphors requiring patients to console or apologize showed higher anxiety compared to the control group (HR 7.9 and 8.3, respectively). Examination of social attention showed lower abilities in finding details. By SCAS 8/9 ND patients reported elevated anxiety base levels in at least one domain; only 2 out of 5 controls reported some anxiety symptoms.
Conclusion: Artificial VR environments allow children to practice communication skills in socially and emotionally challenging but safe situations. SocialVR is a new promising pediatric neurorehabilitation tool to support prosocial learning and reduce social anxiety in children.
Disclosure: Authors declare no relevant or material financial interests that relate to research. The study was funded by Estonian Science Foundation PRG789.
EPO‐740
Effectiveness of shock wave therapy in the treatment of patients with neurological post‐COVID‐19 erectile dysfunction
M. Al‐Zamil 1; D. Zalozhnev2
1Department of Physiotherapy of Peoples' Friendship University of Russian Federation; 2Department of Restorative Medicine and Neurorehabilitation, Medical Dental Institute, Moscow, Russian Federation
Background and Aims: To study the effectiveness of shock wave therapy (SWT) in treatment of patients with neurological post COVID‐19 erectile dysfunction compared to sham SWT.
Methods: We observed 40 patients with neurological erectile dysfunction after suffering from COVID‐19. The patients were divided into 2 groups. In addition to standard drug therapy 20 patients underwent sham SWT (control group) and 20 patients received effective SWT (treatment group). Impairment of the pudendal nerve has been confirmed by clinical and neurophysiological examinations.
Results: The International Index of Erectile Function (IIEF) scores after SWT were 1.54 times higher than after sham SWT (p < 0.01). Sexual quality of life (QoL) became 1.52 times better after SWT compared to sham SWT (p < 0.01). In addition, SWT increased the effectiveness of PDE‐5 inhibitor drugs in improving erectile function by 2.54 times (p < 0.01).
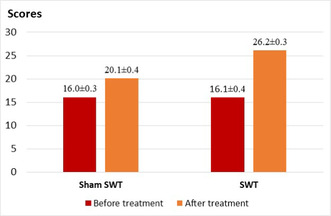
Dynamics of the international index of erectile function in the treatment of patients with erectile dysfunction after COVID‐19 in the control and treatment groups.
Conclusion: SWT therapy has proven effective in improving erections in patients with neurological post COVID‐19 erectile dysfunction. The high effectiveness of SWT is due to the activation of regenerative processes in tissues, improved blood circulation, increased excitability of nerve fibers, stimulation of neovascularization and normalization of NO levels in cavernous endothelial cells.
Disclosure: Nothing to disclose.
EPO‐741
Efficiency of low level laser therapy in improvement of fine movement skills after carpal tunnel decompression
M. Al‐Zamil 1; R. Kuliev2
1Department of Physiotherapy of Peoples' Friendship University of Russia, Moscow, Russian Federation; 2Department of Restorative Medicine and Neurorehabilitation, Medical Dental Institute, Moscow, Russian Federation
Background and Aims: To compare the effectiveness of low level laser therapy of median nerve in improvement of fine movement skills after carpal tunnel decompression surgery.
Methods: We observed 50 patients with residual fine movement skills impairment after Carpal Tunnel Decompression Surgery. 25 patients underwent sham laser therapy (control group) and 25 patients received low level laser therapy (treatment group). Fine movement skills were assessed in all patients using the Jebsen‐Taylor test before treatment, after treatment and after 3‐months of follow‐up period.
Results: After treatment: a significant improvement in Jebsen‐Taylor's test scores was found in treatment group after low level laser therapy, but not in control group. The total test execution time in treatment group decreased by 12% (t = 2.14, p‐value = 0.036). After 3 months of follow‐up period additional positive therapeutic response was found in reduction of the test duration in all subtests by 10.6% (t = 4.91, p‐value = 0.01).
Conclusion: Low‐level laser therapy for the median nerve has been shown to be very effective in improving residual fine motor skills after carpal tunnel decompression surgery. This is due to decreased fiber axonopathy and effective reinnervation, which improve coordinated sensorimotor control of the fingers.
Disclosure: Nothing to disclose.
EPO‐742
Efficacy and safety of modafinil/armodafinil for post‐traumatic hypersomnia: A systematic review and meta‐analysis
R. João 1; N. Pacheco2; M. Hidalgo3; Z. Bakir4; Y. Soares5; M. Oliveira6; J. Dantas7
1Neurology Department – Doutor José de Carvalho Florence Hospital, São José dos Campos, Brazil; 2Neurology Department – Harvard Medical School, Boston, USA; 3Internal Medicine Department – Santa Marcelina Medical School, São Paulo, Brazil; 4Internal Medicine Department – Sapienza University of Rome, Rome, Italy; 5Internal Medicine Department – Federal University of Paraíba, João Pessoa, Brazil; 6Internal Medicine Department – Federal University of Curitiba, Curitiba, Brazil; 7Internal Medicine Department – Federal University of Rio Grande do Norte, Natal, Brazil
Background and Aims: Traumatic Brain Injury (TBI) is a global health issue frequently related to chronic debilitating symptoms such as excessive daytime sleepiness (EDS). While the optimal management of EDS is still unclear, neurostimulants are often empirically employed. Thus, we aimed to perform a systematic review and meta‐analysis to assess the efficacy and safety of modafinil/armodafinil versus placebo on post‐TBI patients experiencing EDS.
Methods: We searched PubMed, Cochrane, Embase, Web of Science, and ClinicalTrials.Gov databases and identified studies comparing modafinil or armodafinil to placebo in post‐TBI patients experiencing EDS. A random‐effects model was used in all analyses.
Results: We included three randomized controlled trials involving 188 patients. The mean age was 34.11, and 61.9% were male. In patients treated with modafinil (dose range: 100–400 mg) or armodafinil (dose range: 150–250 mg), the mean Epworth Sleepiness Scale score was decreased in comparison to placebo (mean difference −1.70; 95% confidence interval [CI] −3.32 to −0.09; p = 0.04; Fig. 1). The risk of insomnia was higher in the modafinil/armodafinil group compared to placebo (risk ratio 3.73; 95% CI 1.11 to 12.54; p = 0.03). There was no difference between groups in the risk of other adverse events, such as nausea (p = 0.09), headache (p = 0.56), dizziness (p = 0.25), and nasopharyngitis (p = 0.67).
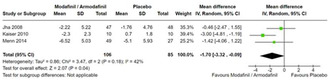
FIGURE 1 In patients with post‐traumatic hypersomnia, somnolence, as measured by the Epworth Sleepiness Scale, was significantly reduced in the modafinil/armodafinil when compared to placebo.
Conclusion: Treatment with modafinil or armodafinil was associated with a significant reduction in somnolence in post‐TBI patients when compared to placebo. However, this therapy also increased the risk of insomnia. Further research is warranted to optimize the risk‐benefit profile of these agents in this population.
Disclosure: Nothing to disclose.
EPO‐743
EEG evaluation of the influence of rTMS in the rehabilitation of patients with ischemic stroke
S. Bozhinov 1; P. Bozhinov2; P. Lambeva3
1Heart and Brain Center of Clinical Excellence, Pleven, Bulgaria; 2Medical University of Pleven; 3Medical Center Galileo, Pleven, Bulgaria
Background and Aims: Objective: To study the influence of rTMS on the state of the brain's bioelectric activity in patients with ischemic stroke in order to determine the prognostic parameters for better motor recovery and to develop an optimal therapeutic protocol.
Methods: For the period between January 2015 and September 2022, a total of 136 patients with ischemic stroke were included in the study. Patients were divided into three groups: In the first, 17 patients (12.5%) received 10 consecutive sessions of rTMS with LF stimulation in the unaffected hemisphere, in the second – 18 (13.2%) HF stimulation in the affected hemisphere, and in the third – 101 (74.3%) combined rTMS protocol in both hemispheres. EEG was performed in all patients before the start of the course and after the last session.
Results: The main trend of influence of rTMS on the brain activity is associated with a clear increase in the share of alpha rhythm, especially pronounced in the combined stimulation group. A correlation was observed between the increase in alpha activity in the affected hemisphere, recorded on EEG, and the motor performance of the patient, demonstrated by the decrease in the motor threshold over the course of treatment.
Conclusion: rTMS appears to be a promising therapeutic method to improve functional recovery in patients with ischemic stroke. The routine use of EEG is an invaluable technique for monitoring and optimizing the individual effect of each patient during the course of treatment.
Disclosure: Nothing to disclose.
EPO‐744
Longitudinal goal attainment following treatment with abobotulinumtoxinA in adults with lower limb spasticity
V. Inestam 1; J. Jacinto2; R. Zorowitz3; S. Ashford4; A. Grandoulier5; P. Maisonobe5; C. Hannes6; A. Esquenazi7
1Ipsen, Kista Sweden; 2Centro de Medicina de Reabilitaçãode Alcoitão, Serviço de Reabilitação de adultos 3, Estoril, Portugal; 3MedStar Health, Washington and Georgetown University School of Medicine, DC, USA; 4London North West University Healthcare NHS Trust, Regional Hyper‐acute Rehabilitation Unit, Northwick Park Hospital, London, UK; 5Ipsen, Boulogne‐Billancourt, France; 6Ipsen, Munich, Germany; 7MossRehab Jefferson Health, Elkins Park, PA, USA
Background and Aims: This prospective, observational study (NCT04050527) assessed the longitudinal attainment (over 16 months) of function‐related goals after one or more abobotulinumtoxinA injections for lower limb spasticity in the clinical setting.
Methods: Ambulatory adult patients with unilateral lower limb spasticity (able to take at least 5 steps with/without assistance) were treated with abobotulinumtoxinA in accordance with local prescribing guidelines to achieve individualized function‐related goals.
Results: At the population level, goal attainment was as expected over repeated cycles; mean cumulated GAS‐leg T score at 16 months (primary endpoint) was 48.2 [47.4, 48.9] (mean change from baseline of 9.9 [9.1, 10.7]). Patients who were injected with injection guidance at baseline were significantly more likely to attain their goals than those in whom no guidance was used (odds ratio: 2.63 [1.72, 4.0], p < 0.0001). Patients treated concomitantly for upper limb spasticity were also more likely to attain their goals than those only injected in the lower limb (odds ratio: 2.3 [1.3, 4.3], p = 0.005). Adverse events (AEs) were reported by 56 (13.5%) patients; most were mild‐moderate and considered unrelated to treatment. Six patients (1.4%) had an AE possibly/probably related to treatment.
Conclusion: This large, international study provides evidence for the benefit of repeated cycles of abobotulinumtoxinA in the lower limb in helping patients achieve meaningful goals, demonstrates the importance of appropriate injection guidance techniques and points to the benefit of treating the upper limb in combination with lower limb when clinically indicated. Treatment with abobotulinumtoxinA was generally well‐tolerated and safe; no new safety issues were identified.
Disclosure: Funded by Ipsen.
Movement disorders 7
EPO‐745
Movement disorders after basal ganglia ischemic lesions following mechanical thrombectomy: An emerging clinical entity
L. Rigon 1; D. Genovese2; V. Brunetti2; V. Guglielmi2; I. Scala1; S. Citro1; A. Cimmino1; A. Bentivoglio1; P. Calabresi1; C. Piano2; G. Della Marca1
1Dipartimento di Neuroscienze, Università Cattolica del Sacro Cuore, Rome, Italy; 2Dipartimento di neuroscienze, Organi di Senso e Torace, Fondazione Policlinico Universitario A. Gemelli IRCCS – UOC Neurologia, Rome, Italy
Background and Aims: Post‐stroke movement disorders (PMDs) following ischemic lesions of the basal ganglia (BG) are a known entity, but data regarding incidence are missing. Ischemic strokes secondary to proximal middle cerebral artery (MCA) occlusion treated with thrombectomy represent a model of selective damage of the BG. Aim of this study was to assess prevalence and features of movement disorders after selective BG ischemia in patients with successfully‐reperfused acute ischemic stroke.
Methods: We enrolled 64 consecutive subjects with acute ischemic stroke due to proximal MCA occlusion treated with thrombectomy. Patients were clinically evaluated by a movement disorders specialist for PMDs onset at baseline, after 6 and 12 months.
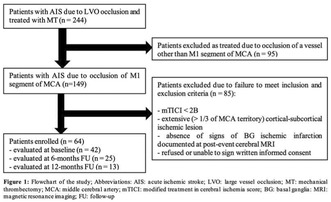
Flowchart of the study.
Results: None of the subjects showed an identifiable movement disorder in the subacute phase of the stroke. At 6‐ and 12‐months respectively 7/25 (28%) and 7/13 (53.8%) of evaluated patients developed PMDs. The clinical spectrum of PMDs encompassed parkinsonism, dystonia and chorea, either isolated or combined. In most patients, symptoms were contralateral to the lesion, although a subset of patients presented with bilateral involvement and prominent axial signs.

Prevalence and clinical subtype of post stroke movement disorders six (A) and twelve (B) months after the acute event.
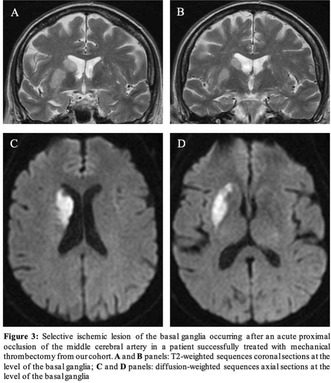
Selective ischemic lesion of the basal ganglia occurring after an acute proximal occlusion of the middle cerebral artery in a patient successfully treated with mechanical thrombectomy from our cohort.
Conclusion: PMDs are not uncommon in a long‐term follow‐up of successfully reperfused acute ischemic strokes. A prosecution of follow‐up in a multidisciplinary team is strongly advisable in patients with selective lesions of the BG after AIS, even if asymptomatic at discharge.
Disclosure: Nothing to disclose.
EPO‐746
Effect of a single session of transcranial pulse stimulation on tremor in Parkinson patients
P. Manganotti; M. LIccari; M. Catalan; P. Busan
Clinical Neurology, Department of Medical, Surgery and Health Services, University of Trieste, Italy
Background and Aims: Tremor is a common signs in movement disorders. Tremor itself is very sensitive to brain stimulation, from deep brain stimulation to Transcranial magnetic stimulation. Transcranial pulse stimulation (TPS) is a painless and non‐invasive new technique which produces a magnetic field by low frequency ultrasound. Aim of the study is to investigate possible long term changes on cortical activity after Transcranial Pulse Stimulation in motor cortex in patients with Parkinson and tremor.
Methods: TPS was delivered in 14 patients affected by PD tremor dominant, which was measured at the baseline (T0) after the TPS (T1) and after 24 hours (T2). The resting tremor was present in all patients with an average of 9–10 Hz/sec. The treatment protocol was 4 Hz, 0.20 mJ/mm2 by default. A single‐session of 1500 pulses were delivered to the subjects’ motor cortex (M1) of the contralateral to the most affected side of the tremor.
Results: We noted a reduction of tremore at T1 and T2 compared to baseline T0 in 13 patients, from 20% to 40% in amplitude, reaching a decrease of 57% in one case. In all the patients we noted a decrease in amplitude and duration of tremor at rest but not in frequency. No effect was note in placebo stimulation.
Conclusion: TPS as a new brain stimulation method induces a reduction of tremor for 24 hours without side effects documenting a significant physiological changes in these patients. TPS is a new techniques for brain stimulation effective on motor areas.
Disclosure: Nothing to disclose.
EPO‐747
Opicapone's real‐world experience in Spanish patients with Parkinson's disease: The OPTIMO study
M. Luquin 1; C. Martin2; I. Tegel3; C. Moreno3
1Clinica Universidad de Navarra; 2Evidenze Group; 3Bial Spain
Background and Aims: Opicapone (OPC), a third generation COMT inhibitor, has been shown to be generally well‐tolerated and efficacious in reducing off time in two pivotal trials in patients with Parkinson's disease (PD) and motor fluctuations (MF) (BIPARK‐I and ‐II). The OPTIMO study aims to confirm these data in the everyday practice by evaluating the clinical performance of opicapone in Spanish movement Disorders Units.
Methods: OPTIMO was an observational, retrospective, post‐authorization study in patients with PD conducted at outpatient consultations for movement disorders in 16 Spanish centers. The inclusion period lasted 12 months. Clinical data were collected before the start of treatment with OPC and between 3 and 7 months post‐treatment. Adverse effects were documented, with particular focus on monitoring the development of dyskinesias.
Results: 245 patients were enrolled (mean age, 67.7 years; mean time of PD evolution, 8.3 years; mean levodopa daily dose, 620.7 mg). Treatment with OPC reduced the percentage of patients with wearing‐off MF (98% vs. 61.6%), delayed‐on (p = 0.010), non‐on (p = 0.027) and non‐motor fluctuations (p = 0.010). The daily OFF‐time was significantly reduced (143 vs. 67.9 minutes). 74.2% of patients described clinical improvement in MF, which did not worsen dyskinesias in 64.6%. No significant increase in ON‐time with dyskinesias was observed. Only 8.6% of patients experienced OPC‐related adverse events.
Conclusion: These results confirm the findings of previous clinical trials, demonstrating that, in routine clinical practice, OPC significantly reduces motor and non‐motor fluctuations without a significant increase in severity of dyskinesias, along with a good tolerance profile.
Disclosure: Supported by BIAL Spain.
EPO‐748
Expanding phenotype of LRRK2 G2019S mutation: Case description of two sisters showing peculiar phenomenological traits
S. Cartella; S. Neri; G. Foti; G. Cartella
Movement Disorders Centre, Department of Neurology, Policlinico Madonna della Consolazione, Reggio Calabria, Italy
Background and Aims: LRRK2 is the most common risk gene for Parkinson's disease (PD). It presents with a milder course and a less common non‐motor involvement than idiopathic PD.
Methods: The aim of this report is to describe LRRK2 phenomenology. We describe two sisters, one presenting with cervical dystonia (CD) and the other one presenting with typical parkinsonian features, although showing prominent non‐motor fluctuations.
Results: A 80‐year old lady was referred to our outpatient clinic due a 2‐year history of head tremor. She showed cervical dystonia characterized by head tremor, inclination to the left side, left shoulder elevation, head rotation to the right, antecollis, retrocaput and limitation of range of motion. She had positive family history for Parkinson's disease (two of her mother's siblings, one of her father's and 5 of her own). Her sister was a 83‐year old lady, who had been diagnosed with Parkinson's disease 8 years previously. Her major complaints were related to her non‐motor fluctuations: her OFF phases were characterized by severe anxiety and pain. We run genetic testing for both patients and found the CD one to be a heterozygotic carrier of G2019S mutation and the PD sister to be a homozygotic carrier of the same mutation. We added safinamide and duloxetine to the treatment of the PD sister, with a major impact on non‐motor fluctuations and QoL, and decided to treat the CD sister with levodopa/carbidopa, with considerable clinical improvement.
Conclusion: Our data may contribute to expanding LRRK2 phenotype and providing insights on its clinical course and treatment.
Disclosure: Dr Cartella SM received speaking honoraria from Zambon and Bial Dr Cartella G received speaking honoraria from Abbvie.
EPO‐749
Proinflammatory IgG glycans correlate with putaminal damage in patients with parkinsonism
S. Matosa 1; A. Vuksan2; D. Snajder Mujkic3; J. Juric4; G. Lauc5; T. Gilman Kuric1; T. Mirosevic Zubonja1; Z. Popovic1; S. Juric1; J. Kragujevic1; A. Poturak6; S. Tomic1
1Department of Neurology, University Hospital Center Osijek, Osijek, Croatia; 2Faculty of Medicine, University of J. J. Strossmayer in Osijek, Osijek, Croatia; 3Clinical Institute for Nuclear Medicine and Radiation Protection, University Hospital Center Osijek, Osijek, Croatia; 4GlycanAge d.o.o., Osijek, Croatia; 5Genos Glycoscience Research Laboratory, Zagreb, Croatia; 6Department of Gastroenterology, University Hospital Center Osijek, Osijek, Croatia
Background and Aims: Objectives: To examine the correlation between dopaminergic denervation evaluated with DaTSPECT and the different types of IgG glycans distributed into mature, youth, and shields glycan groups. The glycan mature group provides proinflammatory, while glycan youth and shield groups provide antiinflammatory potential to IgG antibodies.
Methods: Study design: Cross‐sectional study with historical data Participants and methods: Data used in this study is part of another study that has been approved by the local ethical committee (R2‐3775/2022). Patients diagnosed and treated with Parkinson's disease or atypical parkinsonism were included. Blood samples for evaluating IgG glycan composition were analysed by Genos Glycoscience laboratory in Zagreb. Data on DaTSPECT were analysed from the computer system of the patient registry.
Results: Results: Fifteen patients (10 male, 5 female) were evaluated, 12 with Parkinson's disease and 3 with atypical parkinsonism. The median age was 60 (IQR 55–66), and the disease duration was 3 (IQR 1–4) years. A negative correlation was observed between the IgG glycan mature group, right putamen (Rho = −0.626; p = 0.013), and right putamen/caudate ratio (Rho = −0.703; p = 0.003). A positive correlation was seen between the IgG glycan youth group with right putamen (Rho = 0.627; p = 0.012) and right putamen/caudate ratio (Rho = 0.699; p = 0.004), while the IgG glycan shield group positively correlated with right putamen/caudate ratio (Rho = 0.725; p = 0.002). No significant correlation was observed between glycans, age, or disease duration.
Conclusion: Conclusion: Higher IgG glycan mature group values correlate with increased putaminal degeneration, while higher IgG glycan shield and youth values correlate with reduced putaminal degeneration.
Disclosure: Gordan Lauc is named as an inventor on the GlycanAge patent and serves as the founder and CEO of Genos Ltd.
EPO‐750
Sleep evaluation in functional neurological disorder – Preliminary data of a pilot study
J. Bühler1; N. Schwab1; F. Messmer1; S. Weber1; J. van der Meer2; S. Duss2; S. Aybek 3
1Psychosomatic Medicine, Department of Neurology, University Hospital, Inselspital, Bern, Switzerland; 2Sleep Wake Epilepsy Center, Department of Neurology, University Hospital, Inselspital, Bern, Switzerland; 3Faculté des Sciences et de Médecine, Université de Fribourg, Fribourg, Switzerland
Background and Aims: Functional neurological disorder (FND) is a common neuropsychiatric condition with high burden on patients and where self‐reports often deviate from objective measures. Despite frequent observations of patients suffering from sleep disturbances as a comorbidity, studies evaluating sleep in FND are scarce. We thus aim to describe objective sleep parameters and patients’ subjective perception of sleep in FND.
Methods: In a pilot study, FND patients and age‐ and sex‐matched healthy controls (HC) completed the Pittsburgh Sleep Quality Index (PSQI; subjective), whereas patients additionally underwent a 2‐week actigraphy measurement (objective). We describe subjective sleep quality in FND compared to HC. Furthermore, we report the FND cohort's objective sleep quality in terms of clinical relevance threshold and assess between‐measure accuracy.
Results: 26 FND patients (73% female, mean age = 38.4 y) and 26 HC (73% female, mean age = 36.5 y) were included. Patients reported significantly worse scores of subjective sleep including a higher PSQI total score (p < 0.001). Similarly, subjectively reported sleep latency (p = 0.014), time‐in‐bed (p = 0.032) and sleep efficiency (p = 0.009) significantly differed between FND and HC. Analysis of actigraphy as objective sleep quality measure revealed reduced sleep efficiency (<85%) in 73% of patients. Moreover, in the FND cohort, an incongruency between objective and subjective reports was observed regarding sleep latency (p = 0.005).
Conclusion: This pilot study depicts sleep disturbances in FND patients compared to a healthy cohort and in terms of clinically relevant thresholds. Furthermore, we identified inaccurate perception of one's own sleep onset among FND patients. Studies on larger sample sizes are required to disentangle the role of sleep in FND.
Disclosure: Nothing to disclose.
EPO‐751
Prevalence, pre‐existing conditions, and prior treatments among european adults diagnosed with Tardive dyskinesia
S. Reshef 1; M. Edwards2; M. Forrest Gordon3; N. Chaijale3; A. Kurzeja4; M. Driessen4; C. Correll5
1Teva Branded Pharmaceutical Products R&D, Inc., Parsippany, NJ, USA; 2King's College London, London, UK; 3Teva Branded Pharmaceutical Products R&D, Inc., West Chester, PA, USA; 4Teva Pharmaceuticals Europe B.V., Amsterdam, The Netherlands; 5The Zucker Hillside Hospital, Northwell Health, Glen Oaks, NY, USA
Background and Aims: Tardive dyskinesia (TD) is a hyperkinetic movement disorder mostly associated with chronic antipsychotic (AP) exposure. TD prevalence and associated risk factors in Europe are understudied. This study aimed to evaluate TD prevalence, pre‐existing conditions, and pre‐TD treatments in European adult populations.
Methods: A retrospective study of adults (≥18 years) from 6 European healthcare databases representing Belgium, France, Germany, Italy, Spain, and United Kingdom (UK) was conducted. The index event was first TD diagnosis within the study period (1 Jan 2016–31 Dec 2021). To adhere to regional reporting practices, patient numbers <10 for France and <5 for all others were masked.
Results: Cumulative adult TD prevalence was 1, 3, and 3 per 100,000 in France (<88 of 11,171,508), Germany (660 of 23,235,594), and UK (78 of 2,486,459), respectively. Italy (n = 1,829,406), Spain (n = 1,507,900), and Belgium (n = 712,035) had <5 adults with TD reported, which did not enable prevalence calculations. In ages 18–40 years in France (n = 4,148,423), Germany (n = 8,022,427), and UK (n = 1,221,030), TD prevalence was <0.24, 0.96, and 1.06 per 100,000. For ages ≥41 years in France (n = 7,023,085), Germany (n = 15,213,167), and UK (n = 1,265,429), TD prevalence was 1.14, 3.83, and 5.14 per 100,000. In Germany and UK, 22%–46% of patients with TD had diagnosed schizophrenia, 34%–48% had schizophrenia spectrum disorder, and <5%–34% had anxiety disorders; 40%–56% previously received atypical APs and 15%–42% had received typical APs.
Conclusion: TD prevalence was low and variable across European countries, suggesting limited awareness, underdiagnosis, and coding differences in European health settings.
Disclosure: This study was supported by funding from Teva Branded Pharmaceutical Products R&D, Inc. Mark J. Edwards and Christoph U. Correll have received fees and/or honoraria from Teva Pharmaceuticals. Shoshana Reshef, Mark Forrest Gordon, Nayla Chaijale, Anna Kurzeja, and Maurice T. Driessen are employees and/or stockholders of Teva Pharmaceuticals.
EPO‐752
Post hoc analysis of foot abnormalities in patients with Friedreich ataxia in the MOXIe trial
S. Boesch 1; P. Giunti2; S. Chimalapati3; W. Costello3; A. Goldsberry3; S. Rich3; C. Ruhl3; D. Lynch4
1Department of Neurology, Medical University Innsbruck, Innsbruck, Austria; 2Ataxia Centre, Department of Clinical and Movement Neurosciences, University College London, London, UK; 3Department of Research and Development, Biogen, Cambridge, USA; 4Departments of Pediatrics and Neurology, The Children's Hospital of Philadelphia, Philadelphia, USA
Background and Aims: The MOXIe trial (NCT02255435/EudraCT2015‐002762‐23) evaluated omaveloxolone in patients with Friedreich ataxia (FA); 20% were considered to have severe pes cavus, determined by a flashlight test, and not included in the full analysis set (FAS). This exploratory analysis compared foot angle abnormalities in the MOXIe severe pes cavus and FAS populations.
Methods: Weight‐bearing lateral foot radiographs were obtained and centrally read. Post hoc analyses assessed frequency and distribution of abnormalities in radiological angles indicative of pes cavus (calcaneal pitch >30°, talo‐first metatarsal angles >5°) in the FAS and severe pes cavus populations (Figure 1).
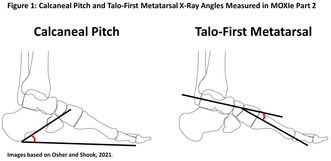
Results: Patients with severe pes cavus (n = 20) had similar baseline characteristics to FAS patients (n = 82); ~90% of patients were ambulatory in each group. Overall, 11% and 45% of FAS and severe pes cavus patients, respectively, had an abnormal calcaneal pitch, and 42.7% and 50% had abnormal talo‐first metatarsal angles (Table 1). Calcaneal pitch and talo‐first metatarsal angles were distributed across a range of values in both populations, though the pes cavus population had more severe angle abnormalities (Figure 2). In patients with severe pes cavus, mFARS results at Week 48 directionally favored omaveloxolone versus placebo; in the all‐randomized population, omaveloxolone demonstrated benefit over placebo. Safety profiles were similar between patients with versus without severe pes cavus.
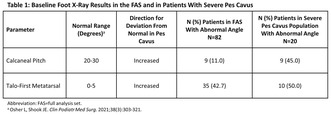
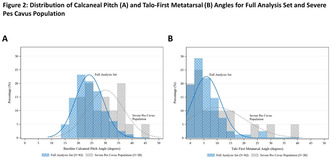
Conclusion: Patients with severe pes cavus were not phenotypically or clinically distinct from the FAS. Pes cavus appears as a continuum in patients with FA. Omaveloxolone was safe and demonstrated benefit over placebo across a full spectrum of foot deformities.
Disclosure: This study was funded by Reata Pharmaceuticals. Reata was acquired by Biogen in 2023. S Boesch has received fees for consultancy, advisory boards, and/or honoraria from AbbVie, Ipsen, Reata Pharmaceuticals, Merz Pharma, Stada Arzneimittel, and VICO Therapeutics. P Giunti has received grants and fees for advisory boards from Reata Pharmaceuticals, and fees for consultancy from VICO Therapeutics, Triplet Therapeutics, and PTC Therapeutics. S Chimalapati, W Costello, A Goldsberry, S Rich, and C Ruhl are employees of Biogen. D Lynch reports grants from FARA, the Muscular Dystrophy Association (MDA), the National Institutes of Health (NIH), Reata Pharmaceuticals, and Retrotope.
EPO‐753
Path to prevention therapeutics platform trial in stage 2B neuronal alpha‐synuclein disease: Study design and timeline
T. Simuni
Northwestern University, Chicago, USA
Background and Aims: To describe the study design and proposed timeline of the first interventional study in Neuronal α‐Synuclein Disease (NSD).
Methods: P2P is a perpetual platform trial with a single Master Protocol dictating the conduct of the trial and regimen specific subprotocols outlining intervention specific aspects for each arm. Qualified participants will be recruited from the PPMI participants, based on NSD Stage 2B criteria (see Table 1). The study's Multiple Primary Endpoints include 1) DAT imaging as measured by the rate of progression in the mean striatum Specific Binding Ratio (SBR) and 2) rate of progression in the MDS‐UPDRS part III score. Secondary endpoints include safety, tolerability and feasibility. The study will have an array of exploratory clinical (including digital) and biomarker measures. Participants will first be randomized in an equal manner among all of the regimen‐specific sub‐protocols for which they are eligible and then within the regimen to an active arm or placebo (N = 125 per arm) in a K:1 ratio with K the number of active interventions. Intervention duration will be at least 24 months. The study is 90% powered to detect a slowing in either primary endpoint for each regimen, assuming a 30% slowing in DAT and a 40% slowing in MDS‐UPDRS Part III.
Results: Interventions are being selected by a Therapeutic Evaluation Committee from >15 industry submitted applications. The study targets to start enrolment in the first 2 regimens in 2025.
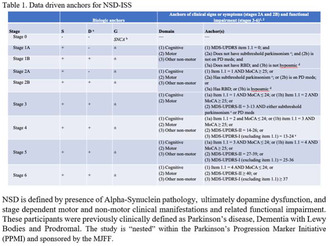
Conclusion: We report the design of the first platform interventional study targeting NSD Stage 2B population.
Disclosure: In the last 12 months Tanya Simuni, MD has served as a consultant for AskBio, Amneal, Blue Rock Therapeutics, Critical Path for Parkinson's Consortium (CPP), Denali, General Electric, Kyowa, Neuroderm/ MTPA, Prevail/ Lilly, Roche, Sanofi, Sinopia, Takeda and Vanqua Bio. Dr. Simuni served on the ad board for AskBio, Amneal, Biohaven, Denali, GAIN, General Electric, Kyowa, MJFF, Neuron23, Parkinson Study Group, Prevail/ Lilly, and Roche. Dr. Simuni has served as a member of the scientific advisory board of Koneksa, Neuroderm/ MTPA, Sanofi and UCB. Dr. Simuni has received research funding from Amneal, Biogen, Neuroderm, Prevail, Roche, UCB and is an investigator for NINDS, MJFF, Parkinson's Foundation (Other authors disclosures to be updated if accepted).
EPO‐754
A closer look at eye movements in cervical dystonia
T. Gilman Kuric 1; Z. Popovic1; A. Sadikov2; V. Groznik2; D. Georgiev3; A. Gerbasi4; S. Juric1; S. Matosa1; T. Mirosevic Zubonja1; S. Tomic1
1Department of Neurology, Osijek University Hospital Centre, Osijek, Croatia; 2University of Ljubljana, Faculty of Computer and Information Science, Ljubljana, Slovenia; 3Department of Neurology, University Medical Centre Ljubljana, Ljubljana, Slovenia; 4Department of Electrical, Computer and Biomedical Engineering, University of Pavia, Pavia, Italy
Background and Aims: In the last few decades cervical dystonia (CD) has come under attention of experts in the field of movement disorders. The studies of its complex pathophysiology propose a disorganization within the motor cortex‐basal ganglia‐cerebellum axis i.e. network. For some time now, eye movements can serve as a good model for researching the motility of patients and thereby expand the knowledge about cervical dystonia.
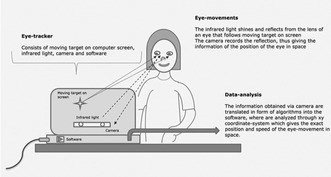
FIGURE 1 Representation of eye movements’ analysis using an eye‐tracker, original scheme.
Methods: 30 cervical dystonia patients and 30 matched healthy controls performed eye‐movement examination including smooth‐eye movements, prosaccade, antisaccade and memory saccade tasks on an eye tracker to assess automatic visual response.
Results: Cervical dystonia patients expressed poorer fixation (p = 0.02) and target following (p = 0.04) of smooth eye‐movements on vertical axis, diminished maximum speed of prosaccades (p = 0.03) which are of significant latency (p = 0.02), more directional errors in the antisaccade task (p = 0.04) and poorer execution of memory saccades testing (p = 0.002). There were no changes in smooth eye‐movements horizontally compared with healthy controls.
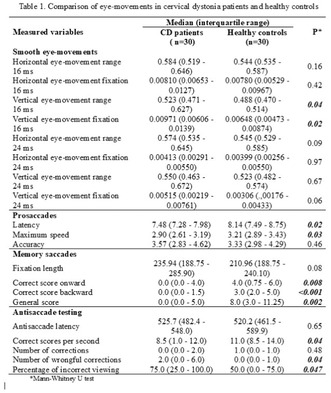
Conclusion: Based on the obtained results and known anatomic connections, we assume a more significant pathophysiology of the interstitial nucleus of Cajal in CD patients than was previously known, considering altered vertical but not horizontal smooth‐pursuit. Also, we suggest changes of saccadic inhibitory control in patients with CD at multiple levels, including dorsolateral prefrontal cortex and frontal eye fields and their projections to the superior colliculus, suggesting alterations of corticobasal networking.
Disclosure: Nothing to disclose.
EPO‐755
Pisa syndrome and botulinum toxin injection in paraspinal muscle ipsilateral to the bending site
T. Lombardo; V. Cenacchi; G. Bellavita; V. Tommasini; M. Catalan; L. Antonutti; M. Liccari; P. Manganotti
Clinical Unit of Neurology, Department of Medical Sciences, University Hospital and Health Services of Trieste, University of Trieste, Trieste, Italy
Background and Aims: The aim of this study was to evaluate the clinical and electromyographical effects of Botulinum toxin injections in patients with Parkinson's disease (PD) suffering from Pisa syndrome (PS).
Methods: We recruited 16 PD patients with PS from the Movement Disorders Unit of Trieste (Italy). Each patient was evaluated at baseline, 1 and 3 months after BoNT injection, which was ipsilateral to the bending site regardless of EMG activation. We recorded demographic, PD‐ and PS‐related clinical variables, including PDQ‐8 and PGIC scales, and back pain evaluation (VAS scale). Muscular hypo‐ and hyperactivity patterns were assessed using superficial EMG recording. Lateral bending angle of the spine was calculated on the planar view photographs as the angle between the vertical axis and a line connecting the fulcrum of the bent spine with the C7 spinous process.
Results: Sixteen outpatients showed an initial reduction in bending degrees followed by a reversion (6.5 ± 3, 5 ± 1.5, 6.7 ± 6 degrees at baseline, 1 and 3 months respectively), a substantial stability in PDQ‐8 scores, and a reduction in back pain. Accordingly to 91 and 100% of the patients, at 1 and 3 months respectively, their condition globally improved (PGIC scores ≥3). Qualitative EMG signal analysis showed an almost uniform improvement in paraspinal muscles activation.
Conclusion: Our study shows an efficacy in bending angle reduction after 1 month from the treatment with a reversion after 3 months, and a subjective clinical improvement. This may indicate a benefit deriving from ipsilateral injection regardless of EMG activity.
Disclosure: Nothing to disclose.
EPO‐756
Selection of candidates for treatment with deep brain stimulation among patients with focal and segmental dystonia
V. Markovic; A. Tomic; M. Jecmenica Lukic; N. Kresojevic; I. Petrovic; N. Dragasevic; M. Svetel
Movement Disorders Department, Neurology Clinic, Medical Faculty, Belgrade, Serbia
Background and Aims: Focal and segmental dystonia are commonly successfully treated with the application of botulinum toxin; however, a proportion of patients remains challenging. GPi deep brain stimulation (DBS) is successfully used in some of these patients, but their frequency and characteristics are still unknown.
Methods: We included 150 consecutive patients in cross‐sectional study at the Neurology Clinic, Belgrade. A semi‐structured survey was used to collect demographic and clinical data, relevant clinical scales to assess dystonia severity (BFMD) and psychiatric symptoms (HAMD; HAMA; Apathy scale). Current criteria were used to diagnose functional dystonia.
Results: Overall, patients were satisfied with the therapy: 74 (49.3%) felt better than 75%, and an additional 43 (28.7%) were 50% better compared to the period before starting botulinum toxin therapy. 33 (22%) respondents had an unsatisfactory therapeutic response (lower than 50%). These patients showed significantly worse scores regarding: BFMD, HAMD and HAMA. We further analyzed these patients found that 9 (6%) had purely functional dystonia, while further 9 (6%) were too old or had significant comorbities to be considered for DBS, thus leaving 15 (10%) potential candidates to be considered for DBS referral which showed no difference regarding duration and severity of the disease nor psychiatric symptoms severity, but they were significantly younger.
Conclusion: About 10% of the subjects with focal or segmental dystonia at the tertiary botulinum toxin center can be considered for DBS referral. Special precaution should be made to exclude patients with functional symptoms.
Disclosure: Nothing to disclose.
EPO‐757
Phenotypic heterogeneity of genetic forms of dystonia
V. Cukic 1; A. Tomic2; A. Tuzinac3; M. Svetel2; I. Petrovic2; M. Jecmenica Lukic2; V. Markovic2; N. Dragasevic Miskovic2; N. Cerovac4; V. Kostic5
1Neurology Department, General Hospital Pancevo, Pancevo, Serbia; 2Neurology Clinic, University Clinical Center of Serbia, Belgrade, Serbia; 3School of Medicine, University of Belgrade, Belgrade, Serbia; 4Clinic of Neurology and Psychiatry for Children and Adolescents, Belgrade, Serbia; 5Serbian Academy of Science and Arts, Belgrade, Serbia
Background and Aims: Dystonia is a movement disorder characterized by continuous or intermittent muscle contraction that causes abnormal positions of body parts. It represents a clinically and genetically very heterogeneous disease. More than 200 genes have been identified that are associated with different, mostly generalized forms of early‐onset/infantile dystonia. The aim of this work is to describe the clinical characteristics and patterns of progression of different genetic forms of dystonia.
Methods: Carriers of DYT‐TOR1A, DYT‐THAP6 (isolated AD dystonia), DYT‐GCH1 and DYT‐SCGE (combined AD dystonia) mutations were included in the study. The data were obtained from the Registry of the Laboratory for Genetics, as well as from medical records. The assessment of the clinical picture was performed for each patient as typical or atypical based on the analysis of demographic data and phenotype analysis, which included data on initial presentation, progression and distribution of dystonia, presence of tremors, presence of other involuntary movements. Statistical processing included standard methods.
Results: Disease progression and dystonia spreading to unaffected regions occurred in all examined groups, according to specific patterns within the groups. There was no difference in the distribution of dystonia by region in DYT‐TOR1A and DYT‐THAP1 carriers. Additionally, atypical clinical presentation was described in all groups.
Conclusion: Our results indicate that two‐thirds of patients with genetic forms of dystonia experience disease progression, while one‐third of patients have signs of atypical manifestations. An adequate assessment of the clinical picture and recognition of the potential genetic basis of the disease significantly improves diagnostic and therapeutic strategies.
Disclosure: Nothing to disclose.
EPO‐758
Autosomal recessive spastic ataxia of Charlevoix‐Saguenay (ARSACS) with novel mutation in SACS gene
Y. Seçil 1; A. Subaşioğlu2; S. Gündoğan1; Ş. Arici1
1İzmir Katip Celebi University Ataturk Education and Research Hospital Neurology Department; 2İzmir Katip Celebi University Ataturk Education and Research Hospital Medical Genetics Department
Background and Aims: Autosomal recessive spastic ataxia of Charlevoix‐Saguenay (ARSACS) is a rare disease with cerebellar ataxia, peripheral neuropathy and pyramidal signs. It is caused by homozygous mutations in the SACS gene (1). It was first reported in the population of French descent in the Charlevoix Saguenay region of Quebec, Canada in 1978 (2). Over 200 pathogenic mutations have been described outside of Quebec (3, 4). ARSACS patients are not limited to a particular ethnic group (3, 4, 5). We present a patient with novel homozygous mutation in the SACS gene from Turkey.
Methods: Forty years old male, born of consanguineous marriage, presented with progressive ataxia and recurrent falls from 20 years of age. He has two cousins suffering from the similar symptoms. Neurological examination revealed ataxia, dysarthria, spasticity, walking difficulty, pes cavus deformity and polyneuropathy. Brain MRI scans show linear T2 and fluid attenuated inversion‐recovery (FLAIR) hypointensities in the pons.
Results: Patient was diagnosed of Charlevoix Saguenay ataxia syndrome. Clinical exome sequencing revealed a homozygous frameshift mutation on exon 10 of SACS gene (NM_014363.6). The mutation, c.7720dup, p.Arg2574LysfsTer4 resulting in a stop codon and premature truncation of the protein.
Conclusion: This mutation is a novel variant that has not been published in the literature until now. According to the ACMG guidelines, as it causes the premature truncation, it can cause damaging effect. We present here a rare case of Charlevoix Saguenay ataxia that occurred secondary to a novel mutation in SACS gene from Türkiye.
Disclosure: There is no disclosure.
Neuropathies
EPO‐759
3 Cases of canvas in a Spanish third level hospital
A. Zahonero Ferriz; R. Vilar Ventura; H. Benetó Andrés; A. Monclús Blecua; M. Fortanet García; C. Vilar Fabra
Servicio Neurología, Hospital General Universitario de Castellón
Background and Aims: CANVAS (cerebellar ataxia, neuropathy and vestibular areflexia syndrome) is a recently genetically diagnosed disease that is caused by abnormal expansion in RFC1 gene. It typically presents in middle age with a combination of neuropathy, ataxia, vestibular disease and dry cough. Typical findings are: pure sensory axonal neuropathy and bilateral vestibular areflexia.
Methods: 3 cases of CANVAS confirmed with genetic study treated in our center.
Results: We present 3 patients with a mean age at onset of symptoms of 50.6 years. None of them had a family history of neurological disease or consanguinity. The average delay time from the onset of symptoms to the first evaluation was 4.6 years, with the reason for consultation being sensory alteration in two of them and walking instability in one of them. 67% had a history of cough years before presentation. 67% developed cerebellar symptoms during follow‐up. In complementary tests, 100% had pure sensory axonal polyneuropathy and only one showed bilateral vestibular areflexia. The delay time until the genetic study was 4 years from the first visit. All 3 had homozygous expansion for AAGGG in the RFC1 gene with a number of expansions between 400–2000.
Conclusion: CANVAS syndrome is a relatively recent entity and it is interesting to know the forms of presentation when it comes to properly identifying patients. Our case series presents concordant and discordant data with respect to other series described, which is explained by the variability of presentation and evolution of these patients, which makes the diagnosis of suspected onset difficult.
Disclosure: Nothing to disclose.
EPO‐760
Longitudinal follow‐up of neuropathy symptoms, neuropathy signs and gait in older adults from good aging in Skåne study
A. Siennicki‐Lantz; S. Elmståhl
Division of Geriatric Medicine; Department of Clinical Sciences, Malmö; Lund University, Sweden
Background and Aims: We aimed to study an extent of neuropathy symptoms and their association with clinical signs of neuropathy and gait speed during 3–6 years follow‐up.
Methods: Older adults (n = 2805, females 55%, mean age 71.5 ± 10.0 ys.) answered on questionnaire Neuropathy Scale Score (NSS), modified for self‐assessment (max score18). At survey‐2, 399 who reached at least 80 ys, were re‐examined after mean 3.4 ys (age 85.6 ± 4.1) with NSS, Gait Speed and Utah Early Neuropathy Scale (UENS). After further 3 ys, all were invited to survey‐3: 211 from the survey‐2 and the rest of the baseline cohort, totally 1598 at mean age 74.1 ± 7.3 ys (figure below).
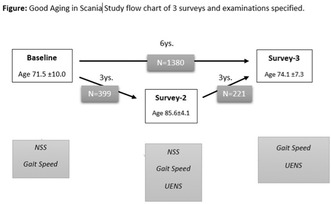
Results: At baseline, median NSS was 0p (0–13; iQR = 1; 41.4% had ≥1p) and was associated with decreased Gait Speed (<1 m/s in 8.5%) (OR = 1.40; 95% CI 1.27–1.54; p < 0.00001). At survey‐2, NSS (median 1.0; 0–11; iQR = 3; 68.2% had ≥1p) was associated with higher risk of neuropathy (UENS ≥7p) (OR = 1.36; 95% CI 1.21–1.53; p < 0.00001) and Gait Speed < 1 m/s (OR = 1.54; 95% CI 1.31–1.81; p < 0.00001). Difference in NSS between survey‐2 and baseline (mean = 1 ± 1.86; range: −4–8) was associated with higher risk of neuropathy (OR = 1.38; 95% CI 1.21–1.57; p < 0.00001) and Gait Speed < 1 m/s (OR = 1.49; 95% CI 1.25–1.77; p < 0.00001). NSS at the baseline was also associated with higher risk of neuropathy in 1598 subjects at survey‐3 (OR = 1.23; 95% CI 1.12–1.34; p = 0.00001) and gait speed < 1 m/s (OR = 1.50; 95% CI 1.30–1.72; p < 0.00001). In 218 oldest old, NSS time‐difference between survey‐2 and baseline (mean 0.7; p ± 1.66; range: −4–7) was associated with neuropathy in survey‐3 (OR = 1.61; 95% CI 1.24–2.01; p = 0.0002).
Conclusion: in general population of older adults, self‐assessed Neuropathy Scale Score and it's time change was sensitive for future clinical signs of neuropathy and decreasing gait speed.
Disclosure: The Good Aging in Skåne (GÅS‐SNAC) project, was supported by the Swedish Ministry of Health and Social Affairs, the county Region Skåne, the Medical Faculty at Lund University, and the Swedish Research Council (grant number 2013‐8604, 2017‐01613, 2021‐01437).
EPO‐761
A new method to objectify the degree of spontaneous activity seen during electromyography study of denervated muscles
A. Sreij; R. Sawaya
American University of Beirut Medical Center
Background and Aims: The degree of spontaneous activity seen during electromyographic analysis of denervated muscles is conventionally defined by the electrophysiologist performing the procedure subjectively as mild, moderate, or severe. Discrepancy between physicians analyzing the quantity of spontaneous activity is not uncommon. The aim of this study is to create an EMG signal parameter capable of objectifying the degree of denervation activity of a given muscle through software analysis rather than subjective evaluation.
Methods: We analyzed the amount of spontaneous activity during the routine electromyographic study of patients referred for testing. We recorded the subjective evaluation of the quantity of spontaneous activity reported by the electrophysiologist. At the same time, we collected a 4 seconds epoch of that same activity. This epoch was incorporated in the electromyographic signal parameter analysis supplied by the manufacturers of the apparatus. The spontaneous activity was evaluated for the peak‐to‐peak value, root‐mean‐square, mean absolute value, and turns/second. We then correlated statistically the physician evaluation with the four parameters.
Sample of EMG signal parameters recorded at time base: 200 ms and sensitivity: 50 uV/division.
Results: The findings of the study confirm that the best objective electromyographic signal parameter reflecting the subjective evaluation of the experienced electrophysiologist was turns/second analysis of the epoch studied. The other three parameters did not correlate with the subjective evaluation.
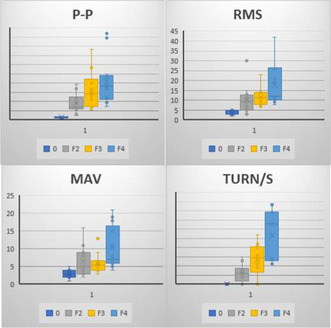
The data collected for peak‐to‐peak value (P‐P) uV, root‐mean‐square (RMS) uV, mean absolute value (MAV) uV, and turns/second through the software incorporated in the EMG machine from the manufacturer.
Conclusion: The turns/second electromyographic parameter seems to be the best electromyographic signal analysis reflecting the subjective opinion of the experienced electrophysiologist in defining the degree of denervation in a given muscle.
Disclosure: The authors have no conflict of interest and they did not receive any funding for this work.
EPO‐762
Small fiber dysfunction in chronic myeloid leukemia
A. Akkan Suzan 1; T. Gurer2; A. Eskazan2; A. Gunduz1
1Department of Neurology and Clinical Neurophysiology, Istanbul University‐Cerrahpasa, Faculty of Medicine, Istanbul, Turkey; 2Department of Internal Medicine, Division of Hematology, Istanbul University‐Cerrahpasa, Faculty of Medicine, Istanbul, Turkey
Background and Aims: In this study, we evaluated the frequency of small fiber dysfunction and the contribution of sympathetic skin response (SSR) in understanding small fiber function in patients with chronic myeloid leukemia (CML).
Methods: We evaluated all patients with CML who were receiving tyrosine kinase inhibitors (TKIs) and complained of neuropathic pain using a modified Toronto clinical neuropathy score (mTNS) and performed sensory and motor conduction studies. Based on clinical and nerve conduction studies, patients with large fiber neuropathy were excluded. In the remaining patients, we evaluated palmar and plantar SSRs and compared them with the findings of 13 healthy individuals.
Results: There were 18 patients with suspected small fiber dysfunction. The mean amplitude of the palmar and plantar SSR were lower in the patient group than those in the control group (p = 0.199 and p < 0.001, respectively). Comparing patients with CML and healthy individuals, ROC curve analysis showed the area under the curve was 0.64 for palmar and 0.94 for plantar SSR. If the plantar SSR amplitude cut‐off value was 114 μV, sensitivity, and specificity were 67.1% and 50%, respectively. However, comparing patients with or without small fiber dysfunction, the area under the curve was low, and no cut‐off value distinguished these groups.
Conclusion: Here, we report that dysfunction of small fibers can occur during CML and the use of TKIs. Plantar SSR is a nonspecific method that may be used in screening. The awareness of small fiber dysfunction and evaluation with nerve conduction studies, including SSRs in suspected patients are essential.
Disclosure: Nothing to disclose.
EPO‐763
Unveiling subclinical autonomic dysfunction in coeliac disease
O. Akan1; B. Kılboz 1; B. Yaralıoğlu1; Y. Gökden2
1Department of Neurology, University of Health Sciences, Prof. Dr. Cemil Tascioglu City Hospital, Istanbul, Turkey; 2Department of Gastroenterology, University of Health Sciences, Prof. Dr. Cemil Tascioglu City Hospital, Istanbul, Turkey
Background and Aims: Celiac disease (CD) patients can exhibit dysautonomia. Early detection can be crucial for timely intervention and managing complications such as syncope. This study aims to identify subclinical autonomic changes in CD patients using heart rate variability and sympathetic skin response tests, compared to healthy controls.
Methods: Serial CD patients from our gastroenterology outpatient clinic and matched controls underwent testing for sympathetic skin response and heart rate variability (including standing up and valsalva 30:15 ratio, and R‐R interval ratios during normal and deep breathing) using the Natus Dantec Keypoint Focus device. Statistical analysis in R 4.3.2 included Welch's t‐test and Mann‐Whitney U test for means, Shapiro‐Wilk test for normality, and descriptive statistics.
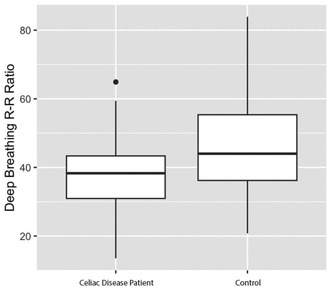
Deep breathing R‐R interval ratios.
Results: The study included 38 CD patients (mean age 31.81 years, 33 females) and 30 controls (mean age 30 years, 20 females). CD patients had a mean disease duration of 5.26 years. IgA transglutaminase antibodies were positive in 15 patients, indicating lack of response to gluten‐free diet. CD patients showed significantly lower deep breathing and valsalva R‐R interval ratios compared to controls (p = 0.0065‐d = 0.706 & p = 0.0011‐d = 0.40). Median nerve proximal and distal CMAP amplitudes were significantly lower in IgA positive CD patients (p = 0.0092‐d = 0.83 & p = 0.0065‐d = 0.706).
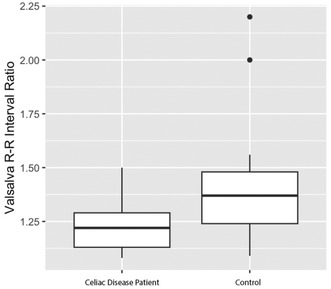
Valsalva R‐R interval ratios.
Conclusion: CD patients exhibit lower valsalva and deep breathing R‐R interval ratios, suggesting subclinical autonomic dysfunction. Additionally, higher median nerve CMAP amplitudes correlate with diet unresponsiveness in CD patients. These findings underscore the need for further research and clinical monitoring.
Disclosure: Nothing to disclose.
EPO‐764
Motor unit number estimation (MUNE) test as assessment tool for motor impairment in Charcot Marie tooth disease
C. Bravi 1; E. Merico2; V. Montano1; D. Viola1; E. Schirinzi1; G. Siciliano1
1Department of Neuroscience, Neurological Clinic, Santa Chiara Hospital, University of Pisa, Italy; 2Cardinal Giovanni Panico Hospital, Tricase, Lecce
Background and Aims: Charcot‐Marie‐Tooth Disease (CMT) represents the most common form of hereditary neuropathy, often burdened by a significant motor impairment. Several clinical validated scales are used to evaluate the degree of disability and to estimate the progression of the disease. The aim of our study has been to evaluate the correlation between electromyography estimation of the residual motor units (MUNE), in targeted muscles, and data obtained by an extensive clinimetric assessment, in different CMT subtypes.
Methods: 29 CMT patients (11 males and 18 females, median age 52,45‐SD = 13,90, median disease duration 28,93 years ‐SD = 17,11) were recruited, including CMT1, CMT2 and HNPP subtypes. For all patients MUNE calculation and clinimetric evaluation by means of CMTNSv2 and CMT‐FOM scales were done.
Results: In CMT2 patients, statistically significant correlations were found between CMT‐FOM sub‐items scores (right/left dorsiflexion, left/right plantar flexion and “4 Stair Descend), CMTNSv2 total score and MUNE values (on Tibialis Anterior muscle). In CMT1 patients, statistically significant correlation between Tibial MUNE value and “4 Stair Climb” sub item score was observed; in HNPP patient no correlations were observed.
Conclusion: MUNE has proven useful for quantifying denervation, highlighting a direct correlation with clinimetric evaluation, in most severe forms of CMT. In less disabling forms, such as HNPP, MUNE appears to be less useful, due to the absent of clear correlations with the result obtained on the clinimetric scales. In future studies MUNE should be considered a surrogate laboratory marker to monitor disease course, also in a clinical trial setting.
Disclosure: Nothing to disclose.
EPO‐765
Neurophysiological outcomes of Rituximab responsive inflammatory neuropathies
D. Viola; V. Montano; C. Bravi; E. Schirinzi; G. Siciliano
Department of Clinical And Experimental Medicine, University of Pisa, Pisa, Italy
Background and Aims: Rituximab (RTX) significantly improves the clinical outcome of selected cases of inflammatory polyneuropathies (IPN) resistant to standard treatments. Here we present the preliminary data of a retrospective study we are conducting at the Neurological Unit of Pisa University Hospital, aiming to characterize the neurophysiological effects of RTX on IPN.
Methods: The following data are collected: a) diagnosis of IPN; b) clinical, laboratory and demographical data; c) Inflammatory Neuropathy Cause and Treatment (INCAT) Disability Score before and after (6 months) RTX treatment; d) electrophysiological data before and after (6 months) RTX treatment. Electroneurography (ENG) parameters measured are: conduction velocity (CV), distal latency (DL) and amplitude (Am).
Results: Eight IPN patients (38% males; mean age 62.6 and SD 10.7 years) were included. Remarkable improvements were observed in in the whole group, with the mean CV and Am increased by 23% and 26% respectively, and DL reduced by 26%. Only two patients did not show a significant response to RTX, with no or limited changes observed after the treatment. Whole group INCAT was significantly lower post RTX treatment (p = 0.042).
Conclusion: The longer disease duration of the two non‐responder patients (10 and 7 years) compared to the other subjects (3 years) might partially explain their poorer clinical and ENG outcome. This ENG‐based study of RTX‐treated IPN patients may aid in identifying individuals most likely to benefit from the therapy and refining optimal treatment timelines.
Disclosure: Nothing to disclose.
EPO‐766
Quantitative sudomotor axonal reflex test in patients with chemotherapy induced polyneuropathy
K. Shin; J. Eun
Department of Neurology, Haeundae‐Paik Hospital, Inje University
Background and Aims: Chemotherapy induced polyneuropathy (CIPN) is one of the common neurological complications that can occur in patients undergoing cancer treatment. While research on risk factors for CIPN has been conducted, there is limited research specifically focused on small fiber neuropathy (SFN). In this study we conducted quantitative sudomotor axon reflex test to evaluate SFN in CIPN patients. Then, we aimed to identify predictors of SFN by analyzing independent variables.
Methods: This is a retrospective observational study conducted at a single institution. Clinical and electrophysiological variables between groups with SFN and without SFN (non‐SFN) were analyzed using t‐tests, Mann‐Whitney tests, and chi‐square tests. Logistic regression analysis was performed for variables that showed significant differences.
Results: A total of 102 patients with CIPN included in the study. Among them, 25 patients had SFN and 77 patients did not. When comparing the two groups, significant differences were observed in age (p = 0.0422), gender (p = 0.0221), history of diabetes (p = 0.0791), and history of radiation therapy (p = 0.0035). On the other hand, variables such as duration of cancer, duration of chemotherapy, type of chemotherapy agents, and number of chemotherapy agents did not show significant differences. Quality of Life Questionnaire – Chemotherapy Induced Peripheral Neuropathy (QLQ‐CIPN20) and the results of the nerve conduction study also did not show significant differences. In logistic regression analysis, the only significant predictor was the history of radiation therapy.
Conclusion: Older age, male, history of diabetes mellitus, and having not been treated with radiation therapy is related with SFN in CIPN patients. Among them, radiation therapy was the most significant factor.
Disclosure: There is no conflict of interest.
EPO‐767
Exploring etiologies and diagnostic precision in hypoglossal neuropathy cases
H. El Mouhajir Mohamed 1; C. Rodríguez Sánchez1; C. Moñino Riquelme2; G. Torres Sanchez1; L. Garcia‐Blanco3; A. Juanatey1
1Neurology Service, Hospital Universitario Juan Ramón Jiménez, Huelva, Spain; 2Rehabilitation Service, Hospital Universitario Juan Ramón Jiménez, Huelva, Spain; 3Neurology Service, Complexo Hospitalario Universitario de Ourense, Spain
Background and Aims: Isolated neuropathy of the hypoglossal nerve is a rare cranial neuropathy, typically arising as a secondary condition linked to lesions in one of its five nerve segments (nuclei, cisternal segment, hypoglossal canal, extracranial portion, and tongue segment).
Methods: This study presents a multicentric series involving consecutive patients seeking medical attention for unilateral tongue paralysis. Comprehensive otorhinolaryngological examinations and craniocervical MRI scans were conducted. In cases where these assessments yielded negative results, electromyography was subsequently performed.
Results: The study comprised six patients (4 female, aged 57–84), with all cases detailed in Table 1. Notably, two patients exhibited hypoglossal nerve compression—Pt1 due to synovial cyst in the atlanto‐occipital joint, and Pt5 with a clival bone lesion linked to multiple myeloma. Pt2, despite a negative MRI, displayed electromyogram indications of bulbar amyotrophic lateral sclerosis (ALS), and she progressed to bilateral tongue paralysis within a month and full bulbar involvement within 3 months. Pt3 presented with hypoglossal compression at the carotid artery, a unique manifestation of carotid extracranial dissection. Pt4, experiencing idiopathic XII neuropathy, fully recovered within a month. Finally, Pt6 showed a vascular vertebral artery loop at the cisternal nerve portion and was ultimately diagnosed with microvascular XII neuropathy due to multiple vascular risk factors. He demonstrated clinical stability after a thorough examination and several months of follow‐up.
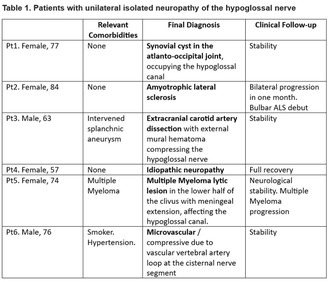
TABLE 1 Patients with unilateral isolated neuropathy of the hypoglossal nerve.
Conclusion: While hypoglossal neuropathy is uncommon, clinicians should remain vigilant for potential secondary etiologies. In instances where routine MRI testing proves inconclusive, electromyography and diligent follow‐up play pivotal roles in ensuring an accurate diagnosis.
Disclosure: Nothing to disclose.
EPO‐768
Neurofilament light chain as a universal biomarker in neuropathies
I. Glāzere 1; K. Ivanova1; D. Pretkalniņa1; T. Čupāne2; M. Roddate1; V. Ķēniņa1
1Riga Stradinš University, Rīga, Latva; 2Children's Clinical University Hospital, Rīga, Latvia
Background and Aims: Neurofilaments, specifically their light chains (NfL), are released following neuroaxonal injuries. Charcot–Marie–Tooth disease (CMT) is a hereditary neuropathy with no effective treatments or sensitive markers available for clinical use. Chronic autoimmune neuropathies arise from an immune response against peripheral nervous system antigens. NfL levels have potential as biomarkers for both conditions, and this study seeks to assess and compare NfL levels to aid in clinical differentiation and improve patient care.
Methods: In this study, a total of 44 Charcot–Marie–Tooth disease (CMT) patients, 34 individuals with chronic autoimmune neuropathy, and 44 control subjects were included. Plasma neurofilament light chain (NfL) concentrations were quantified using the Single molecule array (Simoa) NfL assay. CMT diagnoses relied on genetic testing, while diagnoses for CIDP and MMN followed the European Federation of Neurological Societies/Peripheral Nerve Society (EFNS/PNS) criteria.
Results: Sex and age distribution did not significantly differ among the groups. Both CMT and autoimmune neuropathy patients exhibited significantly higher NfL levels than controls (p < 0.05). Importantly, there was no significant difference in NfL levels between the two patient groups (p = 0.22).
Conclusion: Our study confirms elevated NfL levels in CMT, CAN, and SS neuropathy patients compared to controls. Remarkably, despite the distinct nature of these neuropathies, NfL levels did not significantly differ among the patient groups. These findings underscore the potential of NfL as a universal biomarker and warrant further exploration in neuropathology research.
Disclosure: This research has been developed with financing from the Latvian Science Council, Project Discovering biomarkers of disease progression and variability in Charcot‐Marie‐Tooth neuropathy, No lzp‐2021/1‐0327.
EPO‐769
Abstract withdrawn
EPO‐770
Temporal kinetics of sensorimotor and autonomic recovery in Guillain Barre syndrome
R. Mahajan; J. Kalita
Department of Neurology, Sanjay Gandhi Post graduate Institute of Medical Sciences, Lucknow, India
Background and Aims: Guillain‐Barré syndrome (GBS) is characterized by rapidly progressive quadriparesis with or without sensory or autonomic dysfunction. There is paucity of information regarding recovery pattern in GBS. We evaluate the temporal kinetics of recovery and its pattern among demyelinating (AIDP) and axonal (AMAN) forms.
Methods: Patients with GBS diagnosed on clinical, laboratory and neurophysiological criteria, were included and disabilities were evaluated on Hughes score. Motor, sensory, cranial nerve and autonomic recovery days were recorded and compared among AIDP and AMAN at 3 months. Early recovery was defined as an improvement ≥2 Hughes grades within 4 weeks of symptom onset and late recovery as improvement beyond 4 weeks.
Results: 42 patients were analyzed. Median age was 31 years and 26.2% were females. Autonomic dysfunction recovered in all and at the earliest with median of 12 days (5–69); followed by bulbar weakness and facial weakness with median of 15 days (2–81) & 19 days (4–86) respectively. Sensory function improved over a median period of 20 days (5–66). Motor recovery occurred in 17 (40.5%) patients with median of 65 days (20–90). Dysautonomia occurred more frequently in AIDP (68% vs 10%; p = 0.03) than AMAN. Recovery patterns were comparable in AIDP and AMAN. 20 (47.6%) patients had early recovery and proportion of patients in demyelinating vs axonal were similar.
Conclusion: The neurological recovery in GBS occurred first in autonomic followed by bulbar, facial, sensory, and motor functions. The recovery is comparable between AMAN and AIDP.
Disclosure: Nothing to disclosure.
EPO‐771
A 15‐year retrospective analysis of Guillain Barre syndrome in the adult population of the Maltese Islands
M. Bonello; A. Ferriggi; F. Gauci; H. Schembri; G. Vella
Neurosciences Department, Mater Dei Hospital, Malta
Background and Aims: Guillain Barre Syndrome (GBS) has a worldwide overall incidence rate of 1–2 cases per 100,000 people per year 1. It typically presents with ascending lower limb weakness, associated with hypo/areflexia. Most patient require hospitalization and active treatment with IVIg of Plasma Exchange. The aim of the study is to retrospectively analyze the adult cohort of patients who were admitted with GBS in the Maltese Islands.
Methods: Data were retrospectively collected from National Registries and discharge summaries. Demographic details, infectious screens, lumbar puncture results, nerve conduction study results, treatment regimens and outcomes were collected.
Results: A total of 100 patients were diagnosed with GBS; M = 68. The median age was 53 years. The average length of inpatient acute hospital care was 22.1 days (±32.4SD) (Chart 1). 60% had a previous infection documented. All patients underwent lumbar puncture, most of which happened within 48 hours of admission. 55% of patients had albuminocytological dissociation, with a protein level of >500 mg/L) (Chart 2). 72% were discharged home, 24% needed rehab, 2% passed away during their inpatient stay and 2% required admission to a long‐term facility.
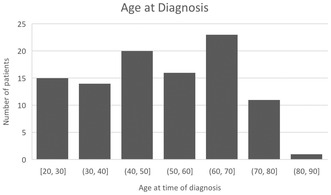
Age distribution of our local cohort.
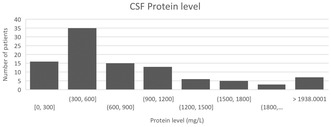
CSF protein levels.
Conclusion: The Maltese population has a similar incidence rate of GBS with a relatively low mortality. Clinical correlation between CSF protein level, presence of positive serum anti‐gangliosides and length of hospital stay, and long‐term outcomes is being sought.
Disclosure: Nothing to disclose.
EPO‐772
Charcot‐Marie‐tooth type 2P in a Spanish family with the novel variant in the LRSAM1 gene: p.Gln698_Gln701del
N. Rabaneda‐Lombarte 1; J. Alonso‐Pérez2; S. Díaz‐González2; A. Menéndez‐Albarracín1; B. Yugueros‐Baena1; A. González‐Manero3; A. Castellano‐Vicente4; C. Gómez‐López de San Román5; C. Casasnovas‐Pons6; A. Martínez‐Piñeiro1; S. Figueroa‐Bonaparte1
1Departamento de Neurociencias, Hospital Universitari Germans Trias i Pujol, Badalona; 2Unidad Enfermedades Neuromuscular, Servicio de Neurología, Hospital Universitario Nuestra Señora de Candelaria, Fundación Canaria Instituto de Investigación Sanitaria de Canarias (FIISC), Tenerife; 3Servicio de Neurología, Hospital General La Mancha‐Centro, Alcázar de San Juan; 4Servicio de Neurología, Hospital de Valdepeñas, Ciudad Real; 5Servicio de Neurología, Hospital General de Segovia, Segovia; 6Servicio de Neurología, Hospital de Bellvitge, L’Hospitalet de Llobregat
Background and Aims: Charcot‐Marie‐Tooth disease (CMT) is the most common hereditary neuropathy. The CMT2 subtype is typically caused by mutations in MFN2 and GDAP1; other genes such as LRSAM1 are exceptional. LRSAM1 mutations specifically cause CMT2‐P, characterized by progressive sensory‐motor neuropathy. Twelve mutations in LRSAM1 causing CMT2‐P have been documented, but each one has been reported only in a single individual or family. Here, we present a Spanish family with dominant CMT2‐P associated with a novel mutation in LRSAM1 recently identified in a single study in French families.
Methods: Analysis of clinical, electrophysiological, and laboratory findings of patients diagnosed with CMT2‐P and carriers of the c.2093_2104del mutation in LRSAM1 gene.
Results: Eight patients within a single family were identified, with onset spanning 23–52 years. Pes cavus were the onset symptom in 5 patients. Currently, they exhibit distal weakness in upper limbs (1 patient), lower limbs (3 patients), or both (3 patients). Bilateral atrophy of hand interossei muscles and short extensor muscle of toes was observed. Achilles areflexia was evident in all patients, with patellar areflexia in 5. Seven experienced lower limbs hypoesthesia, and 3 neuropathic pain. A sensory predominant axonal polyneuropathy was observed in all patients, with a motor component in 5. Exome sequencing revealed the heterozygous pathogenic variant c.2093_2104del (p.Gln698_Gln701del) in the LRSAM1 gene.
Conclusion: This study reports for the first time a Spanish family afflicted by the p.Gln698_Gln701del variant in the LRSAM1 gene causing CMT2‐P. The presence of pes cavus and axonal sensory polyneuropathy are characteristic features of this disease.
Disclosure: None.
EPO‐773
Clinical outcomes, disease course, and QoL in patients with multifocal motor neuropathy: iMMersioN, study in progress
S. Peric 1; L. Querol2; S. Altamimi3; I. Van de Walle4; E. Persson4; I. Van Hoomissen4; G. Szmyd4; M. Vujcic4; M. Hamwright4; O. Van de Steen4; C. Arvin‐Bérod4; J. A. Allen5
1University of Belgrade, Faculty of Medicine, Neurology Clinic, University Clinical Center of Serbia, Belgrade, Serbia; 2Hospital de la Santa Creu i Sant Pau, Neuromuscular Disorders Unit, Barcelona, Spain; 3The Neurology Group, Pomona, CA, USA; 4argenx, Ghent, Belgium; 5University of Minnesota, Department of Neurology, Minneapolis, MN, USA
Background and Aims: Multifocal motor neuropathy (MMN) is a rare, peripheral, immune‐mediated, chronic neuropathy resulting from motor nerve conduction block due to IgM auto‐antibodies leading to axonal degeneration and progressive disabling asymmetric limb weakness with absence of sensory loss. Data on patient experience and clinical management of MMN are limited to small cohorts and retrospective analyses. There is a need to further understand MMN diagnosis, disease course and management and to characterise the healthcare resource use of patients with MMN.
Methods: iMMersioN (NCT05988073), a global, prospective, longitudinal study, will enrol approximately 150 participants. No investigational medicinal product will be administered. Participants will be observed as they receive standard of care treatments. Site visits will coincide with regular MMN treatment visits and will occur approximately every 3 months, and participants will be followed for up to 24 months. In certain countries, optional blood samples may be collected from participants.
Results: The objectives of the iMMersioN study are: to characterise MMN participant profiles, assess disease management and disease course, including outcomes measures such as MMN‐RODS, MMRC‐10, and adjusted INCAT, estimate the economic burden and impact of MMN on quality of life, and collect data on relevant disease biomarkers such as autoantibody titers against gangliosides, components of the complement cascade, and a marker of neurological degeneration. The first participant was enrolled on 29 November 2023.
Conclusion: iMMersioN is an ongoing global, prospective, longitudinal study to examine clinical outcomes, disease course, resource utilization and health‐related quality of life in adult patients with MMN.
Disclosure: SP received lecture honoraria from argenx, Viatris, Pfizer, Teva Actavis, Berlin‐Chemie Menarini, Mylan, Wörwag, ADOC, Remedica and Salveo; research grants from argenx, Kedrion Biopharma and Octapharma; consultant fees from argenx, Dianthus Therapeutics and Mylan; and travel grants from Octapharma, Kedrion Biopharma, Teva Actavis, Sanofi Genzyme, Pfizer, Roche, ADOC, Wörwag, Medis, and Berlin‐Chemie Menarini; and reports no other conflicts of interest outside or related to this work. LQ received research grants from Instituto de Salud Carlos III – Ministry of Economy and Innovation (Spain), CIBERER, Fundació La Marató, GBS/CIDP Foundation International, UCB and Grifols; speaker or expert testimony honoraria from CSL Behring, Novartis, Sanofi Genzyme, Merck, Annexon, Alnylam, Biogen, Janssen, Lundbeck, argenx, UCB, LFB, Avilar Therapeutics, Octapharma and Roche; serves at Clinical Trial Steering Committee for Sanofi Genzyme; and was Principal Investigator for UCB's CIDP01 trial. SA nothing to disclose. IVW, EP, IVH, MH, CA‐B are employees of argenx. OVS works as a consultant for argenx. GS, MV work as consultants for argenx and PPD. JA has received consulting honoraria from argenx, Alexion, Akcea, CSL Behring, Johnson & Johnson, Grifols, Takeda, and Sanofi.
MS and related disorders 7
EPO‐774
Abstract withdrawn
EPO‐775
Nocturnal melatonin ingestion alleviated dynamic postural imbalance and muscle weakness in multiple sclerosis
S. Jallouli1; S. Sakka 2; M. Damak2; S. Ghroubi1; I. Ben Dhia1; A. Yahia1; C. Mhiri2; M. Elleuch1; O. Hammouda3
1Research Laboratory of Evaluation and Management of Musculoskeletal System Pathologies, LR20ES09, University of Sfax, Sfax Tunisia; 2Laboratory of Neurogenetics, Parkinson's Disease and Cerebrovascular Disease (LR12SP19), Habib Bourguiba University Hospital, University of Sfax, Sfax, Tunisia; 3Interdisciplinary Laboratory in Neurosciences, Physiology and Psychology: Physical Activity, Health and Learning (LINP2), UFR STAPS, UPL, Paris Nanterre University, Nanterre, France
Background and Aims: Endogenous melatonin (MEL) deficiency in patients with multiple sclerosis (PwMS) was linked to pain and fatigue that induce postural imbalance and muscle weakness. Exogenous MEL has been shown to present anti‐fatigue and analgesic effects. Despite this association between physical and perceptual disorders, no study has examined the acute effect of MEL intake on dynamic postural stability and muscle strength in PwMS. This study aimed to investigate the effect of nocturnal MEL ingestion on dynamic postural control and leg muscle strength the following morning in PwMS.
Methods: Fourteen PwMS (28.36 ± 6.81 years) were assessed before and after nocturnal ingestion of 6‐mg MEL or placebo (PLA). A force platform was used to evaluate dynamic postural balance in the frontal and sagittal planes. Leg muscles strength (5‐sit to stand test (5‐STST)), fatigue (Hooper index), nociceptive pain (visual analogue scale (VAS)), and neuropathic pain neuropathic pain 4 questions (DN4)) were also evaluated.
Results: MEL decreased posturographic parameters compared with PLA [frontal plane: center of pressure (CoP) path length (CoPL): 7.56% (p = 0.02), mean CoP velocity: 11.1%, (p = 0.00003); sagittal plane: only CoPL: 9.1% (p = 0.005)]. MEL reduced duration of 5‐STST, and scores of VAS and DN4 compared with PLA (8.19% (p = 0.008), 84.44% (p = 0.04) and 37.69% (p = 0.023), respectively). Compared with PLA, MEL alleviated fatigue (42.29% (p = 0.044)) and enhanced sleep quality (30.2% (p = 0.012)).
Conclusion: A single dose of MEL enhanced dynamic postural stability and lower‐extremity muscle strength probably through alleviating pain, fatigue, and sleep disorders in PwMS.
Disclosure: Nothing to disclose.
EPO‐776
Incidence of relapses after meningococcal vaccination in clinical trials of eculizumab and ravulizumab in AQP4+ NMOSD
S. Fam 1; K. Allen2; B. Parks3
1Global Medical Affairs, Alexion, AstraZeneca Rare Disease, Boston, MA, USA; 2Biostatistics, Alexion, AstraZeneca Rare Disease, Boston, MA, USA; 3Clinical Development, Alexion, AstraZeneca Rare Disease, Boston, MA, USA
Background and Aims: Ravulizumab and eculizumab are complement C5 inhibitors (C5ITs) approved for anti‐aquaporin‐4 antibody‐positive (AQP4+) neuromyelitis optica spectrum disorder (NMOSD). Because C5ITs are associated with increased Neisseria meningitidis infection risk, patients are generally advised to be vaccinated ≥2 weeks before receiving C5ITs; however, vaccination may further activate the complement pathway. Patients with complement‐mediated diseases, including NMOSD, may experience increased signs and symptoms of their underlying disease when vaccinated before C5IT initiation. We report on relapses occurring within 4 weeks of meningococcal vaccination administered before initiating C5IT in patients screened in CHAMPION‐NMOSD (NCT04201262) and enrolled in PREVENT (NCT01892345).
Methods: Patients analyzed included those with vaccination data who were screened in CHAMPION‐NMOSD, irrespective of screening outcome, and those randomised to placebo or eculizumab in PREVENT (vaccination data unavailable for screen failures). Outcomes were relapses occurring within 4 weeks of last meningococcal vaccination and before study drug initiation.
Results: In CHAMPION‐NMOSD (N = 71), 1 enrolled patient was excluded from this analysis because of vaccination before AQP4+ confirmation. Among remaining patients (57 enrolled; 13 screen failures), 2/70 (2.9%) patients experienced a relapse; both were screen failures. In PREVENT, 3.1% (3/96) of eculizumab and 10.6% (5/47) of placebo patients had a relapse.
Conclusion: This retrospective analysis indicates a low relapse incidence (2.9%–3.1%) within 4 weeks of meningococcal vaccinations before C5IT initiation and up to 10.6% for those randomised to placebo. Available information precludes determination as to whether relapses observed are attributable to meningococcal vaccination or inherent relapse risk among patients with AQP4+ NMOSD.
Disclosure: All authors are employees of Alexion, AstraZeneca Rare Disease and hold stock options in AstraZeneca. This study was funded by Alexion, AstraZeneca Rare Disease. Medical writing and editorial support were provided by James Banigan, PhD, CMPP, and Melissa Austin of Apollo Medical Communications (Guilford, CT), part of Helios Global Group, with funding from Alexion, AstraZeneca Rare Disease.
EPO‐777
MS‐STAT2 (UCL cohort) baseline analysis: ABILHAND and nine‐hole peg test in secondary progressive multiple sclerosis
S. Apap Mangion 1; C. Wade1; T. Williams1; N. John2; A. Calvi1; A. Bianchi1; F. Dr Angelis1; A. Doshi1; S. Wright1; M. Shatila1; M. Braisher1; J. Blackstone3; R. Farrell1; J. Chataway1
1Queen Square Multiple Sclerosis Centre, Department of Neuroinflammation, UCL Queen Square Institute of Neurology, Faculty of Brain Sciences, University College London, London, UK; 2Monash University, Department of Medicine, School of Clinical Sciences, Clayton, Australia; 3Comprehensive Clinical Trials Unit, Institute of Clinical Trials and Methodology, University College London, London, UK
Background and Aims: Upper limb (UL) dysfunction affecting 80% of people with MS is associated with reduced independence and quality of life. The Nine‐Hole Peg Test (9HPT) is an important progressive MS clinical trial measure, ABILHAND is a 23‐item patient reported outcome measure (PROM) covering UL function, shown to correlate variably with the 9HPT depending on the trial mean/median EDSS. Given the ease with which PROMs can be collected, it is important to assess their potential to predict trial relevant clinically reported measures.
Methods: Blinded ABILHAND total scores were calculated, logits calculated using rehab‐scales.org, and analysis with reciprocal 9HPT performed using Spearman's correlation and linear regression.
Results: ABILHAND data from 232 trial participants (female n = 177, male n = 54), median EDSS of 6.0 (4.0 to 6.5) was analysed. The mean dominant hand 9HPT was 34.1 s, and non‐dominant was 34.4 s. Correlation between ABILHAND total score and reciprocal 9HPT was moderate (rho −0.53). There was not a significant change when subgrouping into low/high EDSS groups; or scoring only the easy/difficult ABILHAND items. ABILHAND total scores accounted for variance of: 18% of the 9HPT dominant hand, 27% of the non‐dominant hand, and 27.8% of the combined result.
Conclusion: ABILHAND has moderate negative correlation with 9HPT. The discrepancy in hand variance accountability may reflect the implied practical bimanual functionality assessed in the ABILHAND items, and relatively reduced functional reserve of the non‐dominant hand. However ultimately the variance was similar when 9HPT results were combined. Longitudinal information will be available late 2024/early 2025 to explore this relationship in more detail.
Disclosure: In the last 3 years, JC has received support from the Health Technology Assessment (HTA) Programme (National Institute for Health Research, NIHR), the UK MS Society, the US National MS Society and the Rosetrees Trust. He is supported in part by the NIHR University College London Hospitals (UCLH) Biomedical Research Centre, London, UK. He has been a local principal investigator for a trial in MS funded by MS Canada. A local principal investigator for commercial trials funded by: Ionis and Roche; and has taken part in advisory boards/consultancy for Biogen, Janssen, Lucid, Merck, NervGen, Novartis and Roche. The other authors have no disclosures related to this work.
EPO‐778
Autologous hematopoietic stem cell transplantation (AHSCT) in relapsing multiple sclerosis (RMS): A real‐world study
S. Malucchi 1; F. Sperli1; R. Bottero1; M. Lo Re1; D. Quartana1; A. Oggero1; M. De Gobbi2; A. Bertolotto3; M. Malentacchi1; A. di Sapio1
1Department of Neurology and CRESM, University Hospital San Luigi Gonzaga, Orbassano (Italy); 2Department of Clinical and Biological Sciences, University Hospital San Luigi Gonzaga, Orbassano, Italy; 3NICO‐Neuroscience Institute Cavalieri Ottolenghi, Orbassano, Italy; Koelliker Hospital, C.so Galileo Ferraris, Turin, Italy
Background and Aims: In recent years treating MS patients early and efficaciously has become prevalent. Literature data agree that a better treatment response occurs when therapy starts in the early phase. The use of AHSCT in MS evolved, passing from a “rescue therapy” in patients who failed all the available DMTs, to an earlier use. No guidelines exist about its correct placement in drugs sequencing; due to its safety profile, AHSCT is usually reserved to patients with hyperaggressive onset or poor responder to highly efficacious therapies. Aim of the study: to describe a series of 24 RMS patients who received AHSCT in our Center.
Methods: 24 RMS patients underwent AHSCT between 2001 and 2023; 23 had a relapsing remitting course, 1 had a relapsing progressive course. Two out of 24 had an aggressive onset. Clinical and demographic characteristics are presented in table 1. 15 patients received BEAM+AGT as conditioning regimen, 1 received BEAM without ATG; 1 patient received only BEAM and subsequently underwent a second AHSCT.
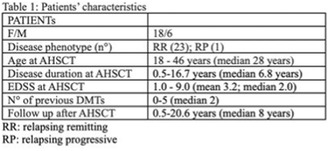
Results: Median EDSS changed from 2.0 at the time of AHSTC to 1.5 at the last follow up visit. 62.5% patients were in NEDA‐3 status at the last visit. Limiting the analysis to patients who received BEAM+AGT as conditioning regimen, 82.3% was in NEDA‐3 status at the end of follow up. No major adverse event occurred.
Conclusion: AHSCT represents a highly efficacious treatment in patients with aggressive disease course. Careful selection and both hematological and neurological evaluation should be performed in order to better define risks and benefits.
Disclosure: SM received speaker honoraria from Biogen, Merck, Sanofi, Novartis, Roche. FS received honaria for talking from Novartis. RB received compensation from Novartis, Sanofi, reimbursement from Bristol Myers, Janssen. MLR received compensation from Novartis and Merck. DQ received compensation from Merck and Novartis and reimbursement from Merck, Roche, Novartis and Biogen. AO has nothing to disclose. MDG has nothing to disclose. AB served on the scientific advisory board of Almirall, Bayer, Biogen, Genzyme; received speaker honoraria from Biogen, Novartis, Sanofi, grant support from Almiral, Biogen, Associazione San Luigi Gonzaga ONLUS, Fondazione per la Ricerca Biomedica ONLUS, Mylan, Novartis and the Italian Multiple sclerosis Society. MM received compensation from Alexion and Novartis. ADS received honoraria from Biogen, Novartis, Roche, sanofi, Merck, Alexion and Sandoz and has been reimbursed by Merck, Biogen, Sanofi, Novartis and Roche for attending conferences.
EPO‐779
The remyelinating potential of non‐invasive neuromodulation and its effects on cognition
T. Scheinok 1; J. Van Schependom1; D. De Bundel2
1AIMS Lab, Center for Neurosciences, UZ Brussel, Vrije Universiteit Brussel, Brussel, Belgium; 2Laboratory of Pharmaceutical Chemistry, Drug Analysis and Drug Information (FASC), Vrije Universiteit Brussel (VUB), Brussels, Belgium
Background and Aims: Previous preclinical studies have revealed that neuronal activity can enhance remyelination and that different patterns of neuronal activity can be sensed by oligodendrocytes. These techniques, however, are not translatable to people with MS due to their invasive nature. In that regard, we intend to investigate the potential of tACS at different frequencies in the cuprizone model.
Methods: Eight‐week‐old mice receive a cuprizone diet for six weeks enabling demyelination whereafter the mice are reverted to a normal diet allowing partial remyelination. During the withdrawal phase, mice receive either tACS at one, five or 10 Hz or sham stimulation for a week. Readouts include cognitive tests such as the novel object location task and the y‐maze as well as immunohistochemistry.
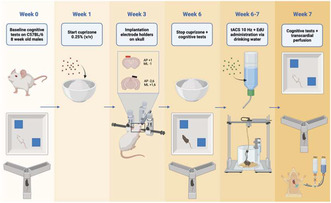
Overview of the project.
Results: Preliminary results indicate that one week of tACS at 10 Hz leads to improved cognition as demonstrated by improvements in the discrimination index during the novel object location task (p = 0.0064). The improvements were not associated with enhanced remyelination in the corpus callosum (p = 0.1207). However, the number of mature oligodendrocytes colocalizing EdU was increased in the corpus callosum after one week of tACS 10 Hz compared to sham stimulation (p = 0.0301).
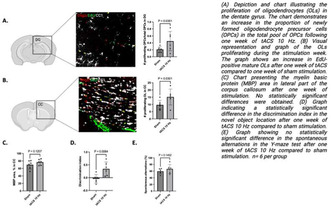
Summary of the results.
Conclusion: One week of tACS at 10Hz during the withdrawal phase of cuprizone leads to improved spatial working memory. While we do not show increased remyelination, we do report an acceleration of maturation of OLs within the OLs proliferating in the corpus callosum. Future experiments will confirm whether these findings can be confirmed and whether different stimulation frequencies might be more effective in remyelination.
Disclosure: Thomas Scheinok received a travel grant from Merck of 250 euros for the EAN congress in 2022. Other authors have nothing to disclose.
EPO‐780
Effectiveness of telemedicine neurologic examination in real‐life settings
T. Gündüz 1; S. Taşdelen1; B. Karaman2; N. Yüceyar2; M. Atmaca3; N. Bülbül3; N. Çınar4; T. Okluoğlu5; A. Aksoy Gündoğdu6; B. Demiryürek7; G. Uncu8; Z. Özözen Ayaz8; İ. Güngör Doğan9; S. Demir9; D. Öz10; D. Özbabalık Adapınar11; P. Kutluay İşeri12; G. Yener13; G. Demir14; E. Kocasoy Orhan1; N. Şirin İnan1; S. Şen15; S. Bünül16; K. Alpay14; Turkey Telenueology Study Group1
1Neurology Department, Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey; 2Neurology Department, Faculty of Medicine, Ege University, İzmir, Turkey; 3Neurology Department, Health Sciences University, Sultan 2. Abdul Hamid Khan Education and Research Hospital, İstanbul, Turkey; 4Neurology Department, Faculty of Medicine, Maltepe University, İstanbul, Turkey; 5Neurology Department, Health Sciences University, Istanbul Training and Research Hospital, Istanbul, Turkey; 6Neurology Department, Faculty of Medicine, Tekirdağ Namık Kemal University, Tekirdağ, Turkey; 7Neurology Department, Kocaeli Medicalpark Hospital, Kocaeli, Turkey; 8Neurology Department, Eskişehir City Hospital, Eskişehir, Turkey; 9Neurology Department, Health Sciences University, Sancaktepe Sehit Prof Dr Ilhan Varank Training and Research Hospital, İstanbul, Turkey; 1010 Neurology Department, Faculty of Medicine, Dokuz Eylul University, İzmir, Turkey; 11Neurology Department, Faculty of Medicine, İstanbul Atlas University, İstanbul, Turkey; 12Neurology Department, Faculty of Medicine, İstanbul Yeni Yüzyıl University, İstanbul, Turkey; 13Neurology Department, Faculty of Medicine, İzmir Economy University, İzmir, Turkey; 14Neurology Department, Faculty of Medicine, Bezmialem Vakıf University, İstanbul, Turkey; 15Neurology Department, Faculty of Medicine, Samsun Ondokuz Mayıs University, Samsun, Turkey; 16Neurology Department, Faculty of Medicine, Kocaeli University, Kocaeli, Turkey
Background and Aims: The importance of telemedicine applications in neurology practice has been widely recognized during the COVID‐19 period, although there is no clear scientific evidence about the feasibility of general neurological examinations performed with telemedicine. In this study, we aimed to determine the effectiveness of telemedicine neurologic examination (TNE) in real‐life conditions and in various disease groups.
Methods: In this multicenter, prospective, and cross‐sectional study, patients with various neurological diagnoses were first evaluated face‐to‐face. These patients were then evaluated by a randomly assigned physician via TNE in terms of 42 different components performed with video conferencing tools used by the public in daily life. These components were scored as categorical variables. Fleiss‐Kappa analysis was used for interrater agreement.
Results: The study included 93 patients 64 of whom were female. Among all, 39 patients had demyelinating diseases, 15 headaches, 9 movement disorders, 6 dementia, 8 neuromuscular diseases, 6 epilepsy, 5 strokes, and 4 other neurological disorders. During the in‐person examination, 17.2–50.5 percent of the patient population had abnormal neurological findings in four different domains. The telemedicine exam had almost perfect interrater agreement in 4 domains (Kappa > 0.8), substantial agreement in 16 domains (Kappa = 0.6–0.8), moderate agreement in 10 domains (Kappa = 0.4–0.6), and slight agreement in 8 domains (Kappa = 0.2–0.4). Although a rather heterogeneous distribution was observed in all neurological examination domains, the best performance was observed in cranial nerve examinations, paresis testing, and cerebellar system examinations.
Conclusion: Our study provides scientific evidence that many components of the neurological examination can be effectively implemented with telemedicine.
Disclosure: Nothing to disclose.
EPO‐781
Conversational agent engagement patterns among individuals with MS: A retrospective analysis of the mHealth application
S. Demir1; S. Colakoglu2; Z. Polat2; M. Durmus2; E. Sezgin3; M. Tutuncu 4
1University of Health Science, Sancaktepe Sehit Prof.Dr.Ilhan Varank Training and Research Hospital, Department of Neurology, Istanbul, Turkey; 2Albert Heath Ltd, Clinical Development & Research; 3Abigail Wexner Research Institute at Nationwide Children's Hospital, Columbus, OH, USA; The Ohio State University College of Medicine, Columbus, OH, USA; 4Istanbul University – Cerrahpasa, Department of Neurology, Istanbul, Turkey
Background and Aims: This study analyzes the engagement patterns of MS‐diagnosed individuals with "Albert MS+" a mHealth application tailored for MS self‐management and remote monitoring, with conversational agent (CA) support.
Methods: We retrospectively analyzed the data based on the intent classification during conversations with CA such as accessing health information, recording clinical parameters, treatment‐related queries, small talk, and fallbacks.
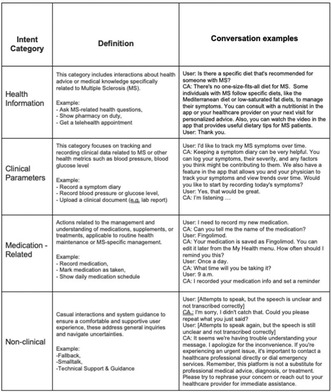
Categories of intents created by the patients using the app.
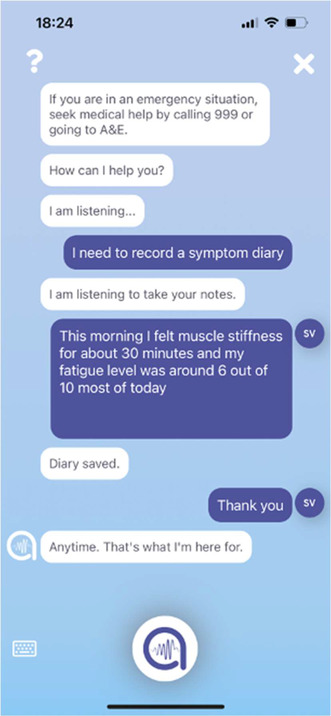
An example of a clinical parameter recorded by a patient via conversational agent.
Results: A total of 263 individuals diagnosed with MS for up to 20 years were enrolled to use Albert. Out of these, 125 participants interacted with the CA 1196 times between 2022 and 2023. The demographic profile showed an average age of 36.3 years with a predominance of females (72.57%) and a high educational background, as 69.6% are university graduates. The average duration since diagnosis was 7.5 years. Health Information accounted for 50.8% of total interactions. Within this category, the specific queries around MS, telehealth, and pharmacy information represent significant areas of user engagement indicating a high demand for accessible health‐related information. Clinical parameters and medication‐related topics together made up 13.7% of interactions. Smalltalk constituted 14.5% of the interactions. Fallbacks comprised 16.1% of interactions, this highlights opportunities for improving the agent's understanding and response accuracy.
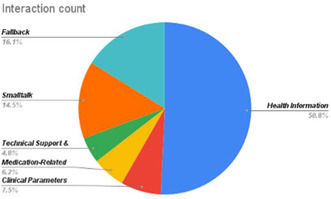
The distribution of intent categories.
Conclusion: The analysis underscores the conversational agent's role in providing health information, and supporting self‐management and indicates a potential to enhance user experience by improving its response capabilities.
Disclosure: Nothing to disclose.
EPO‐782
Prognostic biomarkers of silent progression in multiple sclerosis (MS): Report from an Italian cohort
V. Gasparini 1; M. Jaafar1; T. Carandini2; L. Ghezzi3; F. Certo1; M. De Riz2; C. Fenoglio3; F. Triulzi2; D. Galimberti3; A. Pietroboni2
1University of Milan, Milan, Italy; 2Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milan, Italy; 3Department of Biomedical, Surgical and Dental Sciences, Dino Ferrari Center, University of Milan, Milan, Italy
Background and Aims: Silent progression is a central topic in MS, with a lack of prognostic indicators. This study aims to discern radiological and biochemical markers to identify silent progressors from relapsing‐remitting MS (RR‐MS).
Methods: A total of 42 untreated RR‐MS subjects were enrolled. Twenty‐two out of 42 were identified as silent progressors (SiPr) (Cree et al., 2019). Each patient underwent a 3‐Tesla Magnetic Resonance Imaging (MRI) at diagnosis. Serum levels of neurofilaments light chains (Nfl) and Glial Fibrillary Acidic Protein (GFAP) were assessed on 29 subjects. Comparison between groups were analyzed using Student t‐tests or the non‐parametric Mann‐Whitney test. Univariate and multivariate linear regression analysis were performed to assess association between different neuroradiological quantitative data and being SiPr.
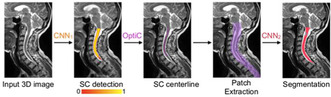
We used Spinal Cord Toolbox (SCT) software to acquire cervical spinal cord volumes at C2‐C3 from T1‐weighted MRI images. SCT created a 3D mask, and convolutional neural networks (CNN) facilitated spinal cord segmentation.
Results: At the univariate analysis lesion load, count of cortical and spinal lesions, choroid plexus volume, and cervical spinal cord volume resulted predictors of silent progression. However, at the multivariate analysis, only the number of spinal cord lesions was a significant predictor of silent progression. No significant differences in Nfl and GFAP levels were noted across groups.

Univariate analysis of radiological characteristics among non‐SiPr and SiPr. OR: odds ratio; CI: confidence intervals; NchP: normalized choroidal plexus volume.
Conclusion: The study highlights spinal cord lesions as key predictors of silent progression in MS. SiPr presented a more enlarged choroidal plexus compared to non‐SiPr patients, suggesting a chronic inflammatory state and an impairment of periventricular remyelination. Identifying RR‐MS patients with worse prognosis and faster progression from onset could enable targeted therapeutic interventions for improved outcomes.
Disclosure: Nothing to disclose.
EPO‐783
Cognitive and neuropsychological features among patients with multiple sclerosis and epilepsy
V. Pozzilli 1; C. Tortorella2; L. Prosperini2; S. Ruggieri2; S. Haggiag2; C. Gasperini2; A. Cruciani1; F. Capone1; V. Di Lazzaro1; L. Celani1; G. Evangelista3; G. De Luca3; S. Cipollone3; V. Tomassini3; F. Dono3
1Department of Neurology, Neurophysiology and Neurobiology, University Campus Bio‐Medico, Rome, Italy; 2Department of Neurosciences, San Camillo‐Forlanini Hospital, Rome Italy; 3Institute for Advanced Biomedical Technologies (ITAB) and Department of Neurosciences, Imaging and Clinical Sciences, University G. d'Annunzio of Chieti‐Pescara, Chieti, Italy; MS Centre, SS. Annunziata University Hospital, Chieti, Italy
Background and Aims: Epilepsy is 2–3 fold more common in patients affected by multiple sclerosis (pwMS) compared to the general population. Currently it is not elucidated whether patients with MS and epilepsy (MS+E) exhibit distinct cognitive and neuropsychological features compared to MS patients.
Methods: Our study aimed to assess the cognitive and neuropsychological impact of epilepsy on MS. Data including clinical features of MS, epilepsy, and medications were collected. Neuropsychological tests including the brief cognitive assessment for MS (BICAMS), the general anxiety disorder‐7, beck's depression inventory and symptom checklist‐90 for psychiatric morbidity were administered.
Results: kkThirty‐three MS+E patients and 33 MS controls matched for age, sex and MS duration were included. MS+E individuals showed lower processing speed (p < 0.01) and visuospatial memory scores (p = 0.03). Seizure onset timing influenced seizure freedom, as in those who manifested their first seizure within 1 year of MS onset had higher seizure freedom rates (p = 0.03). Slowing and/or epileptic activity in at least one EEG were associated with elevated psychological distress. In MS+E patients, higher levels of psychological distress were associated to lower verbal learning test abilities (p = 0.04). Compared to the general population, MS+E patients yielded higher scores in somatization, depression, anxiety, phobia, paranoid ideation, and psychoticism (p < 0.001), with phobia deviating the most from normative values.
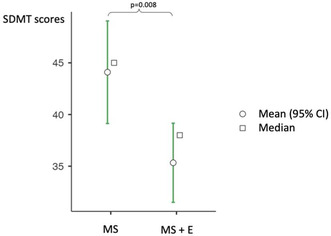
Symbol digit modalities test (SDMT) scores in patients with MS + E (epilepsy) compared to MS.
Conclusion: Epilepsy in MS is associated to worse cognition and psychological morbidity, particularly phobia. This suggests a need for comprehensive patient care, possibly addressing the neuropsychological aspect. Larger studies are needed to confirm such findings.
Disclosure: Nothing to disclose.
EPO‐784
Assessing spatio‐temporal pattern of thalamic damage in multiple sclerosis patients
V. Penati 1; E. Portaccio1; A. Caporali1; M. Betti1; C. Ballerini1; C. Fabbiani2; R. Bonacchi3; E. Fainardi2; E. De Meo1; M. Amato1
1Department of Neurofarba, University of Florence, Florence, Italy; 2Neuroradiology Department, Careggi, Florence, Italy; 3Neuroradiology Department, Vita‐Salute San Raffaele University, San Raffaele Hospital, Milan, Italy
Background and Aims: Thalamic atrophy is one of the earliest changes occurring during multiple sclerosis. Several pathogenetic mechanisms underlying thalamic damage have been hypothesized including Wallerian degeneration from white matter lesions (WM) and cerebrospinal fluid (CSF)‐immunocytotoxic factors mediated damage. We aim to identify long‐term trajectories of thalamic nuclei damage and the contribution of its progression in determining clinical disability and cognitive impairment.
Methods: A cohort of 108 MS patients underwent annual 3T MRI scans (3DT1‐ and T2‐weighted images) and clinical/cognitive assessments for up to 8 years from disease onset. Thalamic nuclei segmentation was performed using Freesurfer 7.2.0. Growth models by alternating conditional expectation evaluated long‐term thalamic volume changes. Linear regression models determined the relationship between thalamic damage progression and clinical disability and cognitive decline.
Results: Bilateral thalamic nuclei adjacent to CSF exhibited a slower, steady volume loss, while those near white matter demonstrated rapid progression. Using growth models, we identified a relative progression index (γ), reflecting shared variance in thalamic nuclei volumes. Significant correlations were found between γ and clinical disability, information processing speed, and executive functions.
Conclusion: The study confirms heterogenous pathogenetic mechanisms in thalamic damage: Wallerian degeneration due to macroscopic white matter damage and CSF‐cytotoxic mediated damage. The identified index (γ) effectively links thalamic damage to cognitive impairment and clinical disability, suggesting its potential as a biomarker for disease monitoring and aiding in treatment strategy identification.
Disclosure: Nothing to disclose.
EPO‐785
Carotid intima media thickness, neutrophil to lymphocyte ratio, and platelet to lymphocyte ratio in multiple sclerosis
N. Eissazade1; S. Eghdami2; E. Alizadeh Najmi3; D. Hemmati1; Z. Mirzaasgari 3
1Student Research Committee, School of Medicine, Iran University of Medical Sciences, Tehran, Iran; 2Cellular and Molecular Research Center, Iran University of Medical Sciences, Tehran, Iran; 3Department of Neurology, Firoozgar Hospital, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
Background and Aims: Limited evidence suggests that carotid intima‐media thickness (cIMT) and neutrophil‐to‐lymphocyte ratio (NLR) increase in patients with MS. Furthermore, platelet‐to‐lymphocyte ratio (PLR) can increase in neuroinflammatory and autoimmune diseases, and it is better interpreted when measured along with other biomarkers, such as NLR. We aimed to assess cIMT, NLR, and PLR levels and their possible correlation in patients with MS.
Methods: We included 110 patients and 110 healthy controls in this case‐control study. All participants underwent complete history taking, and general and neurological examination. Expanded Disability Status Scale was used to assess disability. cIMT was measured with B‐mode ultrasound images, 10 mm before the bifurcation of the common carotid artery.
Results: NLR, PLR, and cIMT were significantly increased in patients with MS, compared to healthy controls (p < 0.001). Among patients with MS, higher cIMT (p < 0.001) was significantly associated with older age (p < 0.001), higher BMI (p < 0.001), higher EDSS scores (p = 0.005), older age of disease onset (p < 0.001) and SPMS type (p = 0.003). Further linear regression analysis revealed that cIMT was marginally associated with higher NLR values (p = 0.055). After controlling for confounding factors, cIMT was significantly associated with NLR (p = 0.047), and not with PLR (p = 0.2). The cut‐off value of mean cIMT (sensitivity: 84%; specificity: 49%) for discriminating mild‐to‐moderate and severe disability was calculated as 0.5.
Conclusion: Higher cIMT levels are significantly associated with higher NLR levels. cIMT could be used as a simple, rapid, and cost‐effective inflammatory marker for MS disability. Further multi‐center studies with larger sample sizes are needed to validate the findings of this study.
Disclosure: Nothing to disclose.
Neuro‐ophthalmology/neuro‐otology
EPO‐786
A case series of five fulminant idiopathic intracranial hypertension (IIH) patients at a tertiary care hospital
S. Mandal; S. Biswas
Bangur Institute of Neurosciences, IPGME&R and SSKM Hospital, Kolkata, India
Background and Aims: Fulminant IIH, presents with abrupt symptom onset and signs of intracranial hypertension, progressing to rapid vision decline within four weeks.
Methods: This case series evaluates clinical, ophthalmological, and radiological features in five non‐obese female patients aged 28–40 years.
Results: Comprehensive evaluation of these patients, revealed symptoms like acute migranous headache, nausea, diplopia and transient visual obscurations (TVO's). Progression to near‐total blindness occurred swiftly within 14 days, with one patient experiencing this within 48 hours. Uniform grade 4 papilledema was observed, including two cases with associated peripapillary hemorrhages. The CSF opening pressure ranged from 35 to 45 cm of H2O. Optical coherence tomography (OCT) illustrated increased retinal nerve fiber layer (RNFL) thickness. MRI findings aligned with IIH, coupled with evidence of transverse sinus stenosis. Optic nerve sheath diameter (ONSD) measured by MRI exceeded 6mm in all cases. Four patients underwent medical management with acetazolamide and temporary CSF drainage for ongoing rapid visual loss. One patient underwent delayed optic nerve sheath fenestration after conservative management. Notable improvements in headache, nausea, and TVO's with subjective visual function improvement. Visual fields remained severely altered.
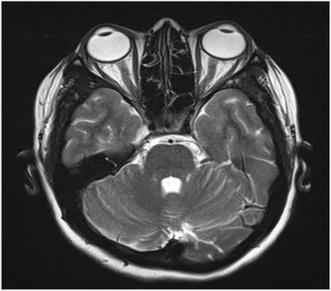
MRI consistent with IIH.
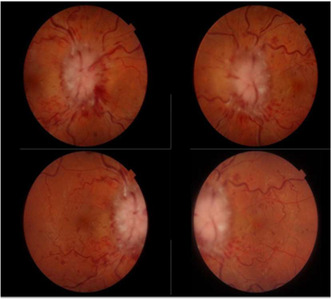
Papilledema with peripapillary hemorrhage.

Conclusion: Fulminant IIH, characterized by distinctive traits, is not universally linked to obesity. Acute symptoms, near‐total blindness, grade 4 papilledema, significantly elevated CSF opening pressure, and raised ONSD can help initiate swift identification and management thereby preventing potential permanent visual loss. Immediate medical therapy with temporary CSF drainage is vital in cases of anticipated intervention delay.
Disclosure: Nothing to disclose.
EPO‐787
Clinical and multimodal imaging findings in traumatic optic neuropathy
S. Kamoun1; M. Rekik1; K. Moalla2; A. Jallouli1; M. Damak2; C. Mhiri 1; A. Trigui1
1Ophthalmology Department, Habib Bourguiba Hospital, Sfax, Tunisia; 2Neurology Department, Habib Bourguiba Hospital, Sfax, Tunisia
Background and Aims: Traumatic optic neuropathy (TON) is a grave complication of cranio‐orbital injury, causing visual involvement. The severity may range from simple contusion to complete avulsion of the optic nerve. We review clinical presentation and multimodal imaging findings in TON.
Methods: Retrospective review of patients with the diagnosis of TON. Clinical records of patients treated in ophthalmology department of Habib Bourguiba Hospital were collected.
Results: Our study included 8 patients with an average age of 22,2 years comprising 7 males and 1 female. All patients complained of sudden vision loss following blunt ocular trauma. Neurological examination was normal in all patients. The TON was unilateral in all cases. Visual acuity was limited to counting fingers in all cases with an afferent pupillary defect. Fundus examination showed signs of partial optic nerve avulsion in two patients, was normal in others. Optical coherence tomography showed a disruption of optic nerve axons in two patients diagnosed with optic nerve avulsion and was normal in 6 cases. Orbital scan revealed orbital fractures in two patients with a bony fragment adjacent to the optic nerve in one case. Six patients received high‐dose corticosteroid. Improvement of visual acuity was achieved in one case.
Conclusion: The diagnosis of TON is clinical, based on visual acuity impairment with the afferent pupillary defect. Optical coherence tomography reveal the disruption of optic nerve axons at the scleral rim in optic nerve avulsion. There is no consensus in the management of TON and visual recovery is uncertain.
Disclosure: Nothing to disclose.
EPO‐788
The condition of vestibular and auditory function in patients with established endolymphatic hydropsis
A. Poddubnyy 1; I. Maryenko2; N. Greben1; S. Likhachev2; A. Kleban2; A. Smolyak1; V. Lisotskaya1
1The State Institution “Republican Scientific and Practical Centre of Otorhinolaryngology”, Minsk, Belarus; 2The State Institution “Republican Scientific and Practical Center of Neurology and Neurosurgery”, Minsk, Belarus
Background and Aims: One of the causes of recurrent cochleovestibular syndrome is endolymphatic hydrops (EH) in Meniere's disease (MD). The study was to assess vestibular and auditory function in patients with a fixed EH according to MRI data.
Methods: 32 patients with MD were examined (оf the criteria of the Barany Society, 2015) 21 women and 11 men, average age 53.22 ± 12.6 years). 2 groups were identified: definite MD (DMD), n = 17 and probable MD (PMD), n = 15. Tonal threshold audiometry (TTA), vestibulometry with functional tests (de Klein's test, hyperventilation, Valsalva, Dix‐Hallpike, McClure‐Pagnini) with registration of spontaneous (SN) and provocative nystagmus (PN), brain MRI and inner ear (IE) with delayed intravenous or transtympanal by contrast.
Results: The TTA data the average value of the hearing threshold on the affected side in the DMD group – 47.08 ± 23.18 dB, in the PMD group – 36.31 ± 22.25 dB, (p > 0.05). SN was registered in 2 (12%) of 17 and PN in 9 (53%) patients with DMD. In the PMD group SN was not registered, in 5 (35%) PN was registered on the lesion side. Significant vestibular hyporeflexia on the hearing loss side was detected in 100% patients with DMD and PMD. In the PMD group brain MRI and IE did not reveal MR signs of EH. In the DMD group MRI revealed EH in 8 (47%) of 17 patients (p < 0.05) on the affected side it corresponded (100%) to the detected hearing loss and vestibular hyporeflexia.
Conclusion: The results obtained make it possible to objectify the EG during subcompensation, which is confirmed by MRI diagnostics.
Disclosure: Nothing to disclose.
EPO‐789
Clinical and evolutionary characteristics of optic neuritis inaugurating multiple sclerosis: About 38 Algerian patients
S. Bourokba 1; F. Boulaneb Bediar2; N. Toubal1
1Department of Neurology, CHU Annaba, Algeria; 2Department of Ophthalmology, CHU Annaba, Algeria
Background and Aims: Optic neuritis (ON) is a frequent clinical presentation in multiple sclerosis (MS), which may be inaugural or occur during the course of the disease, and is considered in the literature to be a factor with a good prognosis. We describe the clinical and evolutionary characteristics of optic neuritis in 38 Algerian patients.
Methods: Prospective longitudinal descriptive and analytical study over a 3‐year period in the neurology department of the CHU annaba Algeria, involving patients over 15 years of age presenting with inaugural ON alone or associated with other neurological signs.
Results: Out of 79 patients, 38 were diagnosed with clinically defined MS according to the 2017 McDonald criteria; sex ratio F/M = 4.42, mean age 29.39 ± 10.61 years; ON was acute in 86. 8%, unilateral in 84.21%, painful in 81.57%, Uhthoff's phenomenon was present in only 6 patients, distance visual acuity was <1/10th in 31.81%, fundus appearance was normal in 68.18%, neurological examination revealed multifocal CNS involvement in 55.28%, orbital MRI was performed in only 11 patients, with ON found in 8; brain MRI met Barkhoff criteria in 68.42%, with active lesions in 6 patients; spinal cord MRI was pathological in over half of cases, dominated by cervical myelitis; symptomatic treatment based on high doses of corticosteroid was initiated in 76.3%, with a good response in the majority of cases.
Conclusion: This study enabled us to assess the characteristics of ON inaugurating MS in an Algerian population; Is ON in MS really a good prognostic factor?
Disclosure: Nothing to disclose.
EPO‐790
An exceptionally uncommon stroke syndrome: A case of cortical deafness
C. Örken; O. Çelik; S. Dirkeç; C. Bolcu Emir
Neurology Department, Prof Dr Cemil Taşcıoğlu Education and Research Hospital, İstanbul, Turkey
Background and Aims: Cortical deafness is an extremely rare condition that arises from bilateral cortical lesions in the primary auditory cortex. Its main clinical manifestation is a sudden bilateral hearing loss. Diagnosis is challenging due to its rarity and similarity to other language and communication disorders, such as Wernicke's aphasia, auditory agnosia, or pure word deafness.
Methods: Case report.
Results: We present a 33‐year‐old female with an acute onset of complete bilateral hearing loss. The hearing loss was attributed to a subacute cortical infarction at the level of the superior and transverse temporal gyri on the left, and an older cortical infarction at a similar location on the right. The etiology of these recurrent cardioembolic infarcts was her mechanical heart valve.
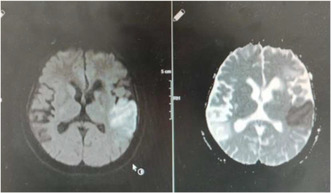
Initial diffusion MR.
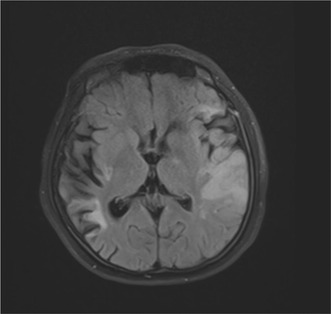
MRI, 3 months.
Conclusion: Both the peripheral and central auditory pathways must be intact for proper hearing. Auditory signals from each ear are evaluated bilaterally in the cerebral cortex. Therefore, for a complete hearing loss, there must be damage to both auditory cortices, the Heschl's gyri. As a result, stroke‐induced deafness is an exceptionally uncommon situation that should be kept in mind in a patient presenting with acute bilateral hearing loss to treat appropriately and to prevent permanent disability.
Disclosure: Nothing to disclose.
EPO‐791
“Complete external ophthalmoplegia” as an adverse reaction to Adalimumab
C. Nieva Sánchez; A. García Díaz; A. Freixa Cruz; L. Perez Girona; E. Ruiz Fernández
Neurology Department, Arnau de Vilanova University Hospital, Lleida, Spain
Background and Aims: "Complete external ophthalmoplegia" refers to the inability of the eyes to move conjugately in all gaze positions. It is caused by damage to the brainstem conjugate gaze control nuclei.
Methods: A 51‐year‐old male, treated with Adalimumab for primary uveitis suffered sudden horizontal binocular diplopía two weeks after Adalimumab administration, which was firstly orientated as microangiopathic IIIpc palsy. He was found two weeks later with a sudden worsening with a complete external ophthalmoplegia. The patient was admitted to the neurology department for study.
Results: In 2017, a magnetic resonance imaging (MRI) conducted in context of the uveitis, revealed a subcortical small hyperintense lesion. A follow‐up MRI one week after the initial clinical presentation identified a small hyperintense lesion located parasagittally in the dorsal tegmentum of the pons. Another MRI during admission (15 days later) demonstrates an increase in size of the lesion, showing diffusion restriction. The cerebrospinal fluid (CSF) exhibited mild pleocytosis. Rest of the ancillary tests were normal. The patient received high‐dose methylprednisolone for five days, showing favorable evolution of symptoms. Due to suspicion of adverse drug reaction, Adalimumab was discontinued. Subsequent follow‐up MRI shows an inflammatory activity regression.
Conclusion: We report a case of an adverse reaction to Adalimumab consisting of brainstem inflammation with complete external ophthalmoplegia. Anti‐TNF‐alpha therapy is not indicated in patients with central demyelinating diseases. Our patient had a previous suspicious lesion so that may not have been the best option.
Disclosure: No conflicts of interest.
EPO‐792
Abstract withdrawn
EPO‐793
Vestibular perceptual thresholds in patients with persistent postural perceptual dizziness
H. Rust 1; J. Allum2; K. Roushan3; C. Stieger2; B. Seemungal4; F. Honegger1
1Department of Neurology, Vestibular Neurology Unit, University Hospital Basel, Switzerland; 2ORL Department, Division of Neuro‐Otology, University Hospital Basel, Switzerland; 3ORL Private Pracitce, Liestal, Switzerland; 4Centre for Vestibular Neurology, Imperial College London, UK
Background and Aims: Persistent postural perceptual dizziness (PPPD) is a common functional disorder. It is characterized by a chronic sensation of dizziness which is exacerbated by upright posture. PPPD usually evolves as a consequence of a vestibular or other illness. With standard vestibular testing being usually normal in those patients with PPPD we studied whether there are changes in vestibular perception.
Methods: 12 patients with PPPD were assessed, 10 males, 2 females (mean age 60 years). The diagnosis of PPPD was established according to the criteria of the Bárány Society from 2017. 23 healthy controls were assessed, 11 males, 12 females (mean age 42.3 years). Vestibular perceptual thresholds were determined for yaw‐plane rotations with randomly presented half cosine stimuli. Patients were assessed for handedness, Dizziness Handicap Inventory (DHI), Ten‐item personality inventory (TIPI) and Hospital Anxiety and Depression scale (HADS).
Results: Vestibular perceptual thresholds in PPPD patients did not significantly differ from those of normal controls. There was no correlation between age and elevated thresholds. The number of trials needed to determine the respective threshold was not related to lower threshold values. Handedness was not correlated with direction errors when indicating motion perception. There was no correlation between DHI values and high or low thresholds.
Conclusion: Patients with PPPD did not differ from normal controls regarding vestibular perceptual threshold values for yaw‐plane rotations. There was no correlation between age and threshold value.
Disclosure: Nothing to disclose.
EPO‐794
Neurological aspect of peripapillary retinal nerve fiber layer changes analysis in idiopathic intracranial hypertension
M. Janani 1; B. Shalbafan2; H. Lanjanian3; H. Sajjadi4
1Student Research Committee, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 2Cellular and Molecular Endocrine Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 3Cellular and Molecular Endocrine Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran; 4Ophthalmic Research Center, Research Institute for Ophthalmology and Vision Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Background and Aims: Papilledema is a biomarker of the elevated intracranial pressure (ICP), observable in fundoscopy. Optic Coherence Tomography (OCT) is a superior method that provides valuable real‐time information about retinal nerve fiber layers (RNFL) and uneven RNFL distribution and thickness, with more density in the temporal circumpapillary bundle (Figure‐1). This allows us to observe sequential changes even before the formation of overt papilledema and diagnose Idiopathic Intracranial Hypertension (IIH) in its early stages.

Methods: In this study, we have enrolled 4 patients whose OCTs were suggestive of elevated ICP based on Sajjadi et al 2017 patterns. Their investigation included: ICP measurement by lumbar puncture (LP), circumpapillary RNFL thickness assessment in temporal, superior, nasal and inferior (TSNI) quarters (Figure‐1) and Brain Magnetic Resonance Imaging (MRI). As normal people and patients with overt papilledema can be diagnosed definitely, they have been excluded from our study.
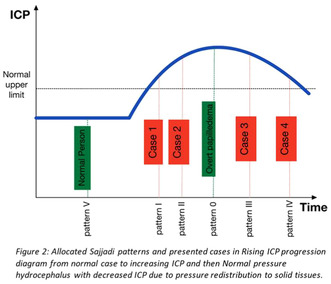
Results: As demonstrated in table‐1 Despite all cases having elevated ICP, case 2 and 3 had RNFL thicknesses were in the normal chart and case 1 had minimal elevation in RNFL thickness and surprisingly case 4 had generalized depression.
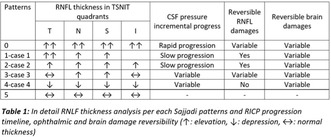
Conclusion: As demonstrated in table‐1 Despite all cases having elevated ICP, case 2 and 3 had RNFL thicknesses were in the normal chart and case 1 had minimal elevation in RNFL thickness and surprisingly case 4 had generalized depression.
Disclosure: Nothing to disclose.
EPO‐795
The diagnostic potential of mesosystolic notch in transcranial Doppler for reversible cerebral vasoconstriction syndrome
V. Chavignier1; A. Lecluse2; S. Godard2; S. Henni1; J. Fortrat 3
1Service de Médecine Vasculaire, CHU Angers, Angers, France; 2Service de Neurologie, CHU Angers, Angers, France; 3Univ Angers, Inserm, CNRS, Équipe CARME, SFR ICAT, Angers, France
Background and Aims: Reversible Cerebral Vasoconstriction Syndrome (RCVS) poses diagnostic challenges due to its manifestation through severe headaches and dynamic vascular abnormalities, with confirmation typically requiring invasive procedures like arteriography, computed tomography angiography (CTA), or magnetic resonance angiography (MRA). The centripetal evolution of vasospasm and the absence of specific clinical criteria hinder early detection.
Methods: In our center, we systematically employed transcranial Doppler (TCD) in suspected RCVS cases, obtaining crucial information on velocity, Lindegard index, and flow turbulences. To assess TCD's diagnostic potential, we conducted a one‐year survey of all TCD examinations, with a specific focus on suspected RCVS cases. A total of 191 TCD examinations were performed, including 38 on 23 patients with suspected RCVS.
Results: Within the cohort, a distinctive TCD flow pattern was identified in four cases, characterized by a mesosystolic notch reaching the baseline or elevating the pulsatility index, notably within seven days of headache onset in three patients. Despite subnormal arteriography results in two cases, only two out of the four patients received a confirmed RCVS diagnosis. TCD, however, normalized during follow‐up in all four cases.
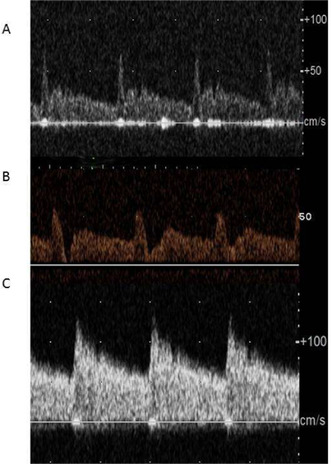
Illustrations depicting deep mesosystolic notches in two patients diagnosed with reversible cerebral vasoconstriction syndrome (A and B), contrasted with a typical cerebral artery flow pattern observed in a normal case (C).
Conclusion: This study highlights the potential diagnostic significance of a mesosystolic notch on TCD in RCVS, offering a non‐invasive and easily repeatable criterion for early detection and follow‐up monitoring. Although not universally conclusive, the presence of a mesosystolic notch on TCD may serve as a pathological finding associated with RCVS, providing valuable insights for early diagnosis and supporting clinical decision‐making to prevent exacerbation of conditions when observed.
Disclosure: Nothing to disclose.
EPO‐796
Analgesia‐related dizziness
M. Villar‐Martinez; P. Amarasena; R. Wilcha; P. Goadsby
Wolfson Sensory Pain and Regeneration Centre (SpaRC), Institute of Psychiatry, Psychology and Neuroscience, King's College London, UK
Background and Aims: Dizziness and vertigo are frequent symptoms reported in migraine during spontaneous and triggered attacks. Medication‐Overuse Headache is a type of secondary headache that could be attributed to frequent use of analgesia in patients with an underlying headache. Our impression is patients with vestibular symptoms of unknown cause may have a migrainous biology and potentially frequent use of painkillers. Our aim was to study the relationship between analgesia and vertigo in a migraine cohort.
Methods: This study is part of the prospective cohort questionnaire‐based IMPARTS at King's College Hospital. We did a cross‐sectional analysis from February‐September 2023. We used SPSS 28 and generalised linear models including linear and binomial (normal and logit functions, respectively), adjusted for normality as appropriate. Presence of vertigo or total score in the Situational Vertigo Questionnaire were dependent variables. Presence of triptans, NSAIDs, opioids, paracetamol and medication overuse were selected as predictors.
Results: The consumption of paracetamol was a predictor for a higher score of vertigo in patients that describe dizziness (n = 96, β = 0.56, p = 0.045). The remaining painkillers and the presence of overuse, and none the predictors for the presence of dizziness, were significant. Medication overuse had a slightly higher percentage in the group that reported dizziness (24% vs 20%, NS).
Conclusion: The consumption of analgesia, specifically that of paracetamol, may be related with the presence of more vertiginous symptoms in those patients that report dizziness in spontaneous attacks. More power is needed to determine if those symptoms are due to “Medication‐Overuse Dizziness”.
Disclosure: Nothing to disclose.
EPO‐797
Extrapulmonary tuberculosis presenting as diplopia in an immunocompetent patient
M. Domine 1; P. Boned Fustel2; N. Blanco Sanromán1; M. Coronel Coronel1; M. Bort Martí2; L. García Fernández2
1Neurology Department, Hospital de la Santa Creu i Sant Pau, Barcelona, Spain; 2Ophtalmology Department, Hospital Universitario i Politècnic La Fe, Valencia, Spain
Background and Aims: Extrapulmonary tuberculosis, accounting for 10–15% of cases, can manifest in various forms, including central nervous system involvement. While meningitis is the more common presentation, it is essential to consider tuberculoma in the differential diagnosis of cerebral masses, particularly in immunocompetent individuals.
Methods: We report an 18‐year‐old woman with no significant medical history, presenting to the emergency department with a two‐week history of binocular diplopia. Physical examination revealed left sixth cranial nerve paralysis.
Results: Blood analysis and cranial CT scan yielded no significant findings. Brain MRI identified a 1.8 cm oval lesion in the left bulbar region extending into the pons, accompanied by extensive vasogenic edema. Cerebrospinal fluid analysis showed no biochemical, cytological, or microbiological abnormalities. PET‐CT revealed lesions with heightened glucose metabolism in the bulb and axillary regions. Ultrasound‐guided fine‐needle aspiration of lymphadenopathy demonstrated histiocytic groups on a necrotic background with cellular debris, indicative of necrotic granuloma. PCR on the sample tested positive for Mycobacterium Tuberculosis, and Quantiferon was also positive. Upon further inquiry, relatives reported a history of tuberculosis during pregnancy. One year of quadruple anti‐tuberculous therapy led to symptom remission and lesion resolution.
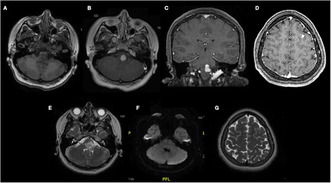
Focal lesion with oval morphology, measuring 1.8 cm, located in the bulbar region with extension towards a hypointense protuberance in T1‐weighted sequence (A). The lesion homogeneously enhances in T2‐weighted sequences (B, C), with extensive perilesional.

Whole‐body FDG‐F18 PET‐CT revealing a lesion in the brainstem with increased glycolytic metabolism and hypermetabolic supraclavicular right lymph nodes. Additionally, smaller nodes with metabolism are observed in the high right paratracheal region.
A. Cytological staining with Giemsa reveals a cluster of cells with broad cytoplasm and oval‐shaped nuclei, suggestive of histiocytes. B. Papanicolaou‐stained cytology displays a cluster of histiocytes on a necrotic background, indicative of a necrotic gr.
Conclusion: This case highlights the atypical presentation of extrapulmonary tuberculosis in an immunocompetent patient, emphasizing the importance of considering infectious etiologies in the differential diagnosis of neurological manifestations and brain masses. Early detection and treatment are critical in mitigating the associated high morbidity and mortality.
Disclosure: Nothing to disclose.
EPO‐798
The influence of virtual reality on the optokinetic nystagmus parameters in patients with stroke
A. Kramarenko; I. Maryenko; S. Likhachev
Republican Research and Clinical Center of Neurology and Neurosurgery, Minsk, Belarus
Background and Aims: Using virtual reality (VR) in patients with stroke rehabilitation is a promising way for motor and oculomotor function recovery. Pathophysiological similarity of motor disorders after stroke and oculomotor phenomena makes it possible to use the oculomotor function assessment as a non‐invasive method for rehabilitation effectiveness evaluation. We aimed to assess the dynamics of optokinetic nystagmus (OKN) under the influence of VR training.
Methods: We examined oculomotor function in 23 patients, using electronystagmography, to explore vertical and horizontal OKN. We registered OKN twice in every patient: before the first training in VR, and after the last one. OKN fast and slow phase amplitude and velocity were measured and analyzed before and after training.
Results: There was a noticeable decrease in asymmetry coefficient (CA) for all horizontal OKN phases characteristics (p = 0.06). CA of fast phase amplitude before starting VR training was 11%, at the end of the course – 5%. CA of OKN slow phase amplitude decreased from 32% to 5% (p < 0.05). CA of OKN slow phase velocity decreased from 23% to 7%, p < 0.05. Also, we discovered absent vertical optokinetic nystagmus (OKN) in 18/23 (78%) patients before training. In 6 patients out of 18 (33%) restoration of the vertical OKN was detected after VR training course.
Conclusion: OKN abnormalities in stroke are common. OKN registration may be used to assess the effectiveness of VR in rehabilitation. Vertical OKN restoration and eye movement asymmetry decrease after VR training demonstrates significant restorative potential of VR for oculomotor functions in patients with stroke.
Disclosure: Nothing to disclose.
EPO‐799
Effect of duration and severity of migraine on ocular structures
Y. Walha1; M. Rekik1; K. Moalla2; S. Kammoun1; A. Trigui1; M. Damak 2; C. Mhiri2
1Ophthalmology Department, Habib Bourguiba Hospital, Sfax, Tunisia; 2Neurology Department, Habib Bourguiba Hospital, Sfax, Tunisia
Background and Aims: Migraine is a complex neurovascular disorder. The pathophysiology of the disease suggests that duration and severity lead to more ocular changes. We investigate the effect of duration and severity of migraine on macular thickness using optical coherence tomography (OCT).
Methods: A cross‐sectional case‐control study conducted at the Habib Bourguiba University Hospital in Sfax. This study included migraine patients and control subjects. Mean macular thickness measurements (MMT) was performed by OCT. Years of evolution were recorded. Severity was assessed using the MIDAS (Migraine Disability Assessment Scale) and MIGSEV (migraine severity scale) scores.
Results: One hundred and twenty eyes from 60 patients (60 eyes in the migraine without aura (MWoA) group and 60 eyes in the migraine with aura (MWA group) were included. Control group included 30 age and gender matched healthy participants (60 eyes). The mean duration of migraine was 12.27 ± 5.88 years. According to the MIGSEV score, migraine was considered of intermediate severity in 43.3% and 50% of MWoA and MWA patients respectively. According to the MIDAS score, migraine caused moderate disability (Grade III) in 43.3% and 26.7% of MWoA and MWA patients respectively. OCT revealed a significant reduction in both groups compared to the control group. Prolonged disease duration was not associated with decreased MT. The severity was the determinant factor of MMT.
Conclusion: Migraine has strong effect on the macular structures. The duration of the disease does not affect the MMT, while the severity has a stronger effect on MMT.
Disclosure: Nothing to disclose.
EPO‐800
The impact of the frequency and the duration of migraine attacks on macular thickness
Y. Walha1; K. Moalla2; M. Rekik1; S. Kammoun1; A. Trigui1; M. Damak 2; C. Mhiri2
1Ophthalmology Department, Habib Bourguiba Hospital, Sfax, Tunisia; 2Neurology Department, Habib Bourguiba Hospital, Sfax, Tunisia
Background and Aims: Migraine episodically leads to the activation and sensitization of the trigeminovascular system leading to vasoconstriction not only of cerebral blood vessels but also of retinal blood vessels. We investigate the frequency and the duration of migraine attacks on macular thickness (MT) using optical coherence tomography (OCT).
Methods: This study aimed to compare MT, measured using OCT, among patients diagnosed with migraine with aura (MWA) and migraine without aura (MWoA), compared to healthy controls. The mean MT (MMT) and pericentral quadrants was measured conforming to the segmentation of the Early Treatment Diabetic Retinopathy Study.
Results: One hundred and twenty eyes from 60 patients (60 eyes in the MWoA group and 60 eyes in the MWA group) were included. The control group consisted of 30 age‐ and gender‐matched healthy participants (60 eyes). The frequency of attacks was between one and four per month in 66.7% of MWoA and 56.7% of MWA. The frequency of attacks was between 4 and 12 hours in 50% and 76.7% of MWoA and MWA respectively. The frequency of attacks was correlated with the MMT, superior parafoveal thickness, and superior, nasal and inferior perifoveal thickness in both groups, while the attack duration does not affect the MMT.
Conclusion: Migraine patients with and without aura are prone to have damages in MT. In our study, the thinning of MT is significantly influenced by the duration of migraine attacks than their duration.
Disclosure: Nothing to disclose.
Muscle and neuromuscular junction disorder 4
EPO‐801
Assessment of sympathetic sudomotor function in myotonic dystrophy type 1 with electrochemical skin conductance
M. Schön; I. Castro; J. Castro; M. De Carvalho; M. Oliveira Santos
Serviço de Neurologia, Departamento de Neurociências e de Saúde Mental, Hospital de Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Lisbon, Portugal
Background and Aims: Myotonic dystrophy type 1 (MD1) is an autosomal dominant disease caused by an expansion of CTG repeats. One of the most controversial manifestations consist of its potential autonomic involvement. The electrochemical skin conductance (ESC) is a non‐invasive neurophysiologic technique, which has been considered a reliable tool in the assessment of small‐fibre neuropathy caused by diabetes mellitus, hereditary ATTR amyloidosis, Fabry disease, and amyotrophic lateral sclerosis.
Methods: ESC measurements were prospectively investigated in 18 consecutive MD1 patients (8 males, 44%) with a median age of 46 years (1st–3rd IQR, 37–55), that were compared with a group of 24 age and sex‐matched healthy subjects as controls. Their nerve conduction studies were normal and none of the individuals had a previous history of diabetes or was taking any anticholinergic medication.
Results: ESC values from MD1 patients did not differ from controls: hands [74 μS (1st–3rd IQR, 67–78) vs 79 μS (1st–3rd IQR, 67–85, p = 0.27)] and feet [81 μS (1st–3rd IQR, 77–85) vs 81 μS (1st–3rd IQR, 78–85, p = 0.87]. No significant correlation was found between hands and feet ECS measurements and the disease duration or number of CTG repeats, as well as between feet ESC and anterior tibialis weakness (p > 0.05).
Conclusion: This innovative technique does not confirm the potential involvement of cholinergic unmyelinated postganglionic sympathetic C fibres in patients with DM1. An altered function of the target organ due to smooth muscle compromise seems to be a possible explanation for those manifestations rather than the primary involvement of the autonomic nervous system.
Disclosure: Nothing to disclose.
EPO‐802
Identification of novel plasma biomarkers for myasthenia gravis prognostication
M. Li 1; M. Petersson1; F. Piehl2; S. Brauner2
1Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden; 2Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden & Department of Neurology, Karolinska University Hospital, Stockholm, Sweden
Background and Aims: Myasthenia Gravis (MG) is an antibody‐mediated neurological disease characterized by potentially life‐threatening muscular fatigability. Currently, there are no established prognostic biomarkers predicting outcomes, and the understanding of the underlying immunopathogenesis is limited.
Methods: Plasma from 60 newly diagnosed MG patients and 51 age‐ and sex‐matched healthy controls (HCs) were assayed on the Olink EXPLORE 1536 panel, measuring 1460 pre‐selected soluble proteins. Protein expression was calculated as relative NPX values, and corrected for age, sex, and sample handling. Groupwise expression differences were calculated using post‐hoc ANOVA test. Prognostic power was determined using survival analyses investigating time to remission (defined as quantitative MG score, QMG, ≤2 and no rescue treatment within 3 months).
Results: Baseline characteristics of patients were: Average age 59.5 years (SD 18.6), 36.7% females, 88.3% AChR+, QMG 5.9 (SD 4.4) and 86.7% were untreated. Significant differences between MG patients and HC were observed in nine proteins, with the strongest association observed for oligodendrocyte myelin glycoprotein (OMG; adj. p < 0.0001), which aside the nervous system also is expressed in leukocytes. Four of the nine proteins were associated to the STAT1/3 pathway. Altered expression of proteins linked to T‐cell activation and migration were significantly associated with earlier remission within one year from sampling, including increased CCL27 and ITGAV expression, and decreased CLEC4D expression (all adj. p = 0.033).
Conclusion: We observed plasma proteins differentially expressed between new‐onset MG and matched HC. Additionally, we identified proteins linked to T‐cell activation and migration as potential biomarkers of medium‐term disease remission.
Disclosure: SB has received in non‐restricted research grants from UCB Pharma and Janssen, not related to this study. FP has received research grants from Janssen, Merck KGaA and UCB, and fees for serving on DMC in clinical trials with Chugai, Lundbeck and Roche, and preparation of expert witness statement for Novartis.
EPO‐803
Sensitivity to change and meaningful change thresholds of the quick motor function test (QMFT) in Pompe disease
N. van der Beek 1; A. Sjöström‐Bujacz2; C. Daskalopoulou3; D. Papageorgiou3; K. An Haack4; V. Gallego5; P. DasMahapatra5; N. Thibault5; A. Zaher6; N. Armstrong5; M. Kruijshaar1; A. van der Ploeg1
1Erasmus MC University Medical Center, Center for Lysosomal and Metabolic Diseases, Rotterdam, The Netherlands; 2IQVIA, Solna, Sweden; 3IQVIA, Athens, Greece; 4Sanofi, Chilly‐Mazarin, France; 5Sanofi, Cambridge, MA, USA; 6Sanofi, ON, Canada
Background and Aims: QMFT is a 16‐item validated scale for assessing motor function in Pompe disease. Objectives were to determine whether QMFT was sensitive to changes in patient's status and inform on meaningful change thresholds (MCTs) for within‐patient change.
Methods: Using blinded, pooled data from COMET (NCT02782741) study of late‐onset Pompe disease (LOPD), sensitivity to change was examined from baseline to Week 49. Mean QMFT total score was investigated among those who improved, worsened, and remained unchanged based on other collected and theoretically related clinical outcomes assessments (COAs) via Kruskal‐Wallis analysis. Spearman correlations of changes between QMFT and COAs were also examined. CMT for within‐patient change was estimated via anchor approaches, based on anchors with appropriate correlations (>0.371 corresponding to d = 0.8), and distribution approaches (0.5 standard deviation [SD] and standard error of measurement [SEM] to estimate a lower bound; minimal detectable change [MDC] for upper bound).
Results: Sensitivity to change was indicated, due to the expected pattern between changes in QMFT and most COAs (Table 1) and high correlations between QMFT and the COAs (Table 2). Summary statistics for change scores for improvement ranged from mean/median of 3.0–8.0 points (Table 3). Distribution results were 0.5 SD = 5.16 points; SEM = 3.94 points; and MDC = 10.92 points. Considering the above, the within‐patient MCT for improvement ranged from 5.16 to 10.92 points.
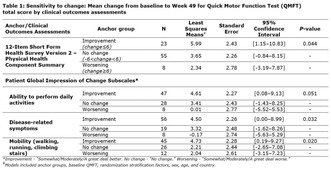

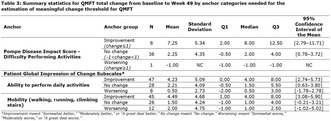
Conclusion: QMFT appeared sensitive to change in ambulatory LOPD patients. MCTs for within‐person improvement can be used to interpret change in this population. However, further investigation is needed among more patients across the spectrum of disease severity.
Disclosure: The study was funded by Sanofi. Nadine van der Beek has received consulting fees, speaking fees, and fees for attending meetings and advisory boards by Sanofi. Nicole Armstrong, Kristina An Haack, Víctor Gallego, Pronabesh DasMahapatra, Nathan Thibault, and Atef Zaher are employees of Sanofi and may own Sanofi stock. Aleksandra Sjöström‐Bujacz, Christina Daskalopoulou and Dimitrios‐Paraskevas Papageorgiou are employees of IQVIA and serve as consultants to Sanofi. Michelle Kruijshaar declares no conflicts of interest. Ans van der Ploeg received funding for research, clinical trials, and advisory fees from Sanofi‐Genzyme, Amicus Therapeutics, BioMarin, Ultragenyx, Sarepta, Audentes, and Spark Therapeutics working on enzyme replacement therapy or next‐generation therapies in the field of Pompe disease, other lysosomal storage diseases, or neuro‐muscular disorders, under agreements with the Erasmus MC University Medical Center and the relevant industry.
EPO‐804
Efficacy, safety, and factors predicting response in Rituximab therapy for generalised myasthenia gravis
N. Thambirajah; G. Logou; S. Sumaria; R. Howard; D. Kullmann; J. Spillane
National Hospital for Neurology and Neurosurgery, Queen Square, London, UK
Background and Aims: Rituximab (RTX) is an anti CD20 monoclonal antibody approved for use in refractory generalised Myasthenia Gravis (gMG). We aimed to assess the efficacy, safety, and factors predicting response in RTX therapy for gMG.
Methods: A retrospective observational study was conducted at our centre. Case notes of patients with gMG treated with rituximab from 2019 to 2023 were analysed. Positive outcomes were recorded if, at six months a) a reduction of at least 2 points in MG Activities of Daily Living (ADL) or 3 points in MG composite scale occurred, or b) if at one year – treatment escalation was not required, or c) if either prednisolone or intravenous immunoglobulin were weaned.
Results: Of the 32 patients included in the study, 26 (81.2%) were female and 6 were male. Eighteen (56.2%) were acetylcholine receptor antibody positive (AchR) and thirteen were muscle‐specific kinase (MuSK) antibody positive. Mean age at start of treatment was 46.8 years (range 25–76) and mean disease duration was 13.2 (±10) (range 1 to 47). Patients had previously received an average of 4 immunosuppressive agents (range 1–7). Twenty (62.5%) patients responded to RTX. 76.9% (10/13) of the MuSK positive group responded compared to 50% (9/18) of the AchR positive cohort. Age and thymectomy were unrelated to outcomes while time to treatment of less than 10 years was correlated to positive outcome. A multi‐morbid patient died of COVID‐19 two months after treatment.
Conclusion: Rituximab is effective in MuSK gMG but variably effective in AchR gMG.
Disclosure: 1. Nothing to disclose 2. Has received travel support from UCB and been on an advisory board for Alexion 3. Nothing to disclose 4. Nothing to disclose 5. Nothing to disclose 6. Has received speakers fees and travel support from Argenx and served on an advisory board for UCB.
EPO‐805
Abstract withdrawn
EPO‐806
Patient characteristics and exacerbations in incident myasthenia gravis: Analysis of US commercial insurance claims data
P. Mina‐Osorio 1; J. Arackal2; J. Wang3; J. Schwinn1; B. Venker3; L. Miller‐Wilson1
1Immunovant, Inc., New York, NY, USA; 2University of Health Sciences & Pharmacy, St. Louis, MO, USA; 3Roivant Sciences, Ltd., New York, NY, USA
Background and Aims: The incident myasthenia gravis (MG) population in the United States (US) is not well‐characterized. Many patients experience exacerbations despite the use of conventional immunosuppressive treatments; however, this has not been studied in detail.
Methods: This retrospective analysis used Inovalon claims data to estimate the incidence of MG among adults aged ≥18 years in the US for 2019. Patient characteristics, treatment utilization patterns, and exacerbation frequency were assessed in the incident population.
Results: We identified 1,372 incident patients with MG, corresponding to a raw incidence rate of 4.9 per 100,000 persons, and an adjusted incidence of 5.2 per 100,000 after extrapolating to the US population. More than half (56.9%) of the patients were women, and the median age for women (58 years) was lower than for men (62 years). Hypertension was the most common comorbidity, occurring in 50.4% of patients. Among 920 patients who received medication, 773 (84.0%) received acetylcholinesterase inhibitors. Among 1,204 incident patients with ≥1 year of continuous follow‐up, 387 (32.1%) experienced exacerbations, with the majority experiencing ≥3 exacerbations. Median (interquartile range [IQR]) time to first exacerbation was 7 (60) days, and in patients with >1 exacerbation, the median (IQR) time from the first to subsequent exacerbation was 25 (42) days.
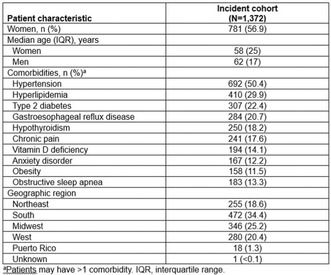
TABLE 1 Demographics and baseline characteristics of the incident population.
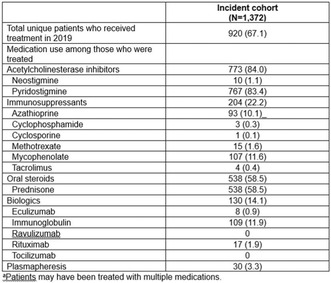
TABLE 2 Treatment utilization in the incident population.
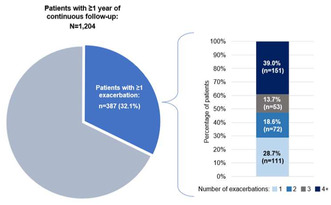
FIGURE 1 Number of MG exacerbations in incident patients with ≥1 year of follow‐up.
Conclusion: The estimated incidence of MG among adults in the US was 5.2 per 100,000 persons. Approximately one‐third of patients experienced exacerbations within a year, with >50% of those patients having ≥3 exacerbations. These findings highlight the unmet need for targeted therapies that provide sustained symptom control.
Disclosure: This analysis was funded by Immunovant, Inc. PMO is an employee of Immunovant, Inc. JA has nothing to disclose. JW is an employee of Roivant Sciences, Ltd. BV is an employee of Roivant Sciences, Ltd. JS is an employee of Immunovant, Inc. LAMW is an employee of Immunovant, Inc.
EPO‐807
Characterisation of patients with myasthenia gravis in France: A cluster analysis of patients from the SPOON study
S. Sacconi1; G. Solé2; A. Crochard3; J. Bertocchio4; A. Archer5; P. Boulanger6; P. Villy 3; A. Richard3; J. Camdessanché7
1Système nerveux périphérique et muscle, CHU de Nice, Université Côte d'Azur, NICE, France; 2Service de Neurologie et Maladies Neuromusculaires, CHU de Bordeaux, Centre de Référence des Maladies Neuromusculaires AOC, Hôpital Pellegrin, BORDEAUX, France; 3UCB Pharma, Colombes, France; 4SKEZI, Annecy, France; 5AFM Telethon Groupe d’intérêt Myasthénies, EVRY, France; 6AMIS (Association des Myasthéniques Isolés et Solidaires), La Chapelle En Serval, France; 7Service de Neurologie, Centre de Référence des Maladies Neuromusculaires PACA‐Réunion‐Rhône Alpes, CHU de Saint‐Étienne, Hôpital Nord, Saint‐Étienne, France
Background and Aims: The SPOON study was an online patient survey about living with myasthenia gravis (MG). The present analysis aimed to identify potential patient subgroups with different disease characteristics and experiences, and to document their aspirations about living with MG.
Methods: Cluster analysis was performed using ascending hierarchical clustering. The characteristics of each cluster were described. Differences in characteristics between clusters were tested using the χ2 or Student's t‐test as appropriate.
Results: The cluster analysis included 255 participants. Three clusters were identified, which accounted for 52.5% of the inertia in the sample (Figure 1). Characteristics of the clusters are described in Table 1. Cluster 1 (n = 83; 32.5%), mostly comprising women (86%) diagnosed at an older age than cluster 3, appears to be the one most affected by MG, with 78% of the patients with current symptom exacerbation and a heavier burden of disease. Cluster 2 (n = 44; 17.3%) mostly comprises men diagnosed later in life with a lower disease burden. Cluster 3 is the largest cluster (n = 128; 50.2%) and is principally women (94%) diagnosed at a younger age than cluster 1, with stable disease (96.9% without current symptom exacerbation), a moderate disease burden and relatively low psychological burden. Aspirations about living with MG are similar across clusters: for all clusters, the main aspiration is to be more physically active (Figure 2).
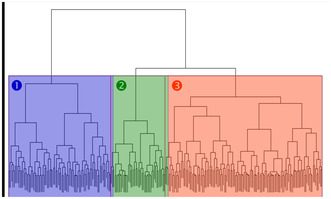
FIGURE 1 Cluster dendrogram obtained after hierarchical ascending classification.
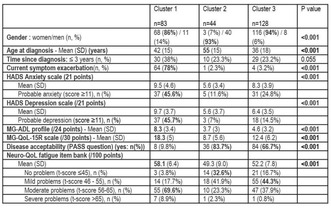
TABLE 1 Characteristics of the clusters.

FIGURE 2 Domains and dimensions of patients’ aspiration with respect to MG.
Conclusion: Three clusters were identified defined by gender and disease stage. Regardless of cluster, patients’ aspirations were similar, centered on physical activity.
Disclosure: This study was funded by UCB Pharma. A Crochard, P‐E Villy and A Richard are employees of UCB Pharma. Other authors declare no conflict of interest.
EPO‐808
Long‐term safety and efficacy of subcutaneous efgartigimod PH20: Interim results of the ADAPT‐SC+ trial
J. De Bleecker 1; J. Howard Jr2; Y. Li3; T. Vu4; D. Korobko5; S. Steeland6; B. Van Hoorick6; J. Podhorna6; M. Hodari6; K. Utsugisawa7; F. Sacca8; H. Wiendl9; R. Mantegazza10; E. Cortés‐Vicente11; ADAPT‐SC Study Group12
1Department of Neurology, Ghent University Hospital, Ghent, Belgium; 2Department of Neurology, The University of North Carolina, Chapel Hill, North Carolina, USA; 3Cleveland Clinic, Cleveland, Ohio, USA; 4Department of Neurology, University of South Florida Morsani College of Medicine, Tampa, Florida, USA; 5State Budgetary Healthcare Institution of Novosibirsk Region “State Novosibirsk Regional Clinical Hospital,” Novosibirsk, Russian Federation; 6argenx, Ghent, Belgium; 7Department of Neurology, Hanamaki General Hospital, Hanamaki, Japan; 8GENESIS Department, Federico II University of Naples, Naples, Italy; 9Department of Neurology, University of Münster, Münster, Germany; 10Department of Neuroimmunology and Neuromuscular Diseases, Fondazione Istituto Neurologico Carlo Besta, Milan, Italy; 11Neuromuscular Diseases Unit, Department of Neurology, Hospital de la Santa Creu i Sant Pau, Barcelona, Spain; 12Biomedical Research Institute Sant Pau, Barcelona, Spain
Background and Aims: Efgartigimod, a human IgG1 antibody Fc‐fragment, reduces IgG levels through neonatal Fc receptor blockade. In the ADAPT‐SC study, subcutaneous (SC) efgartigimod PH20 (coformulated with recombinant human hyaluronidase PH20) was shown to be noninferior in total immunoglobulin G reduction compared with intravenous (IV) efgartigimod. Participants completing ADAPT‐SC or enrolled in ADAPT+ were eligible for the ongoing ADAPT‐SC+ open‐label extension, which sought to evaluate long‐term safety, tolerability, and efficacy of efgartigimod PH20 SC in participants with gMG.
Methods: Efgartigimod PH20 SC 1000 mg was administered in cycles of 4 once‐weekly injections. Subsequent cycles were initiated ≥28 days from the last dose based on clinical evaluation. MG‐ADL score assessed clinical efficacy.
Results: Through December 2022, 179 participants received ≥1 dose of efgartigimod PH20 SC, with a mean (SD) treatment and follow‐up time of 395 (116) days, resulting in 193 participant‐years of follow‐up. Treatment‐emergent adverse events (TEAEs) were predominantly mild/moderate. The most frequent TEAEs (Table 1) were injection site erythema (29.1%), COVID‐19 (22.3%), and headache (20.1%). TEAEs, serious TEAEs, and infections did not increase with subsequent cycles through Cycle 9 (Figure 1). Improvement from cycle baseline (mean [SE] improvement at Week 4) was observed in Cycle 1 in MG‐ADL total score (−4.0 [0.24]) with consistent and repeatable improvements seen through Cycle 9 (Figure 2), and the number of participants achieving minimal symptom expression (MSE) at any time in each cycle ranged from 35.5% to 43.5%.
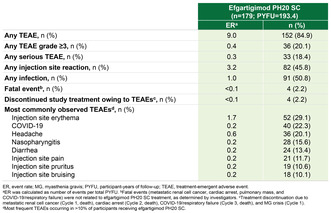
TABLE 1 Summary of TEAEs.
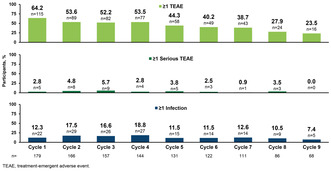
FIGURE 1 TEAEs by Cycle.
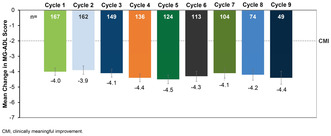
FIGURE 2 Mean Change in MG‐ADL From Study Baseline at Week 4.
Conclusion: Treatment with multiple cycles of efgartigimod PH20 SC was well tolerated and efficacious, consistent with efgartigimod IV in ADAPT/ADAPT+.
Disclosure: Multiple relationships financial and non‐financial nature for authors JLDB, JFH, YL, TV, DK, SS, BVH, JP, MH, KU, FS, HW, RM, and ECV stated at point of presentation.
EPO‐809
BCMA‐targeted CAR T cell therapy in the management of refractory myasthenia gravis
M. Qu 1; X. Rong1; Y. Zhao1; X. Sun1; M. Lv1; Y. zhou2; G. Tang2; M. Liu1
1Department of Neurology, Affiliated Hospital of Qingdao University; 2Danlo Med., Co., Ltd
Background and Aims: Chimeric antigen receptor (CAR) T cell therapy shown promise in treating hematologic malignancies and autoimmune diseases. This study reports an ongoing Investigator‐initiated trial (IIT) involving B‐cell maturation antigen (BCMA)‐targeted CAR T therapy for refractory myasthenia gravis (MG) patients with anti‐acetylcholine receptor (AChR) antibodies positive.
Methods: The study enrolled seven patients (3 females and 4 males) with a median quantitative myasthenia gravis score (QMGS) of 15 (range: 11–27), a median age of 50 years (range: 24–64), and a median disease duration of 4 years (range: 1.25–11). After lymphodepletion, autologous BCMA‐targeting CAR T cells were administered as a single infusion at doses ranging from 1.7 × 105/kg to 10 × 105/kg.
Results: The results showed all patients developed grade 1 or 2 Cytokine Release Syndrome (CRS), and no neurotoxicity syndrome was observed. The most common adverse events of grade 3 or higher were hematologic toxicity. One patient was infected with the COVID‐19 virus but recovered rapidly after supportive therapies. The expansion of CAR T cells in vivo was associated with clinical symptom improvement and normalization of laboratory parameters, including serum anti‐AChR IgG. MG syndromes remission was achieved in all seven patients after 3 months, and the median QMGS decreased to 5 (range: 0–11) from 15 at baseline (range: 11–27). During a median follow‐up of 4 months (range: 3–10 months), drug‐free remission was maintained after CAR T cell administration.
Conclusion: In conclusion, the study demonstrated that BCMA‐targeted CAR T therapy is a safe and effective treatment for refractory MG.
Disclosure: Nothing to disclose.
EPO‐810
Late‐onset Pompe disease: Patient journeys from symptom onset to diagnosis
R. Martínez Marín 1; A. Doerr2; R. Gould2; J. Heuterman3; P. Rajasekhar4
1Neurology Service, Hospital Universitario La Paz, Madrid, Spain; 2Fulcrum Research Group, Waltham, MA, USA; 3Global Medical Affairs, Sanofi, Amsterdam, The Netherlands; 4Global Rare Diseases Strategy & Operations, Sanofi, Cambridge, MA, USA
Background and Aims: Pompe disease is a rare neuromuscular disorder caused by deficiency of acid alpha‐glucosidase, leading to lysosomal glycogen accumulation and consequential progressive muscle weakness, respiratory dysfunction, and functional disabilities. Pompe disease has a broad clinical spectrum in terms of affected body systems, symptom onset age, and progression rate. We aim to describe the path from symptoms onset to diagnosis in late‐onset Pompe disease (LOPD) to gain a better understanding of the diagnostic journey.
Methods: Data about demographic, clinical pre‐diagnosis symptoms, and diagnostic experience were collected by independent researchers during a 30‐minute pre‐interview survey and 60‐minute telephone interview with patients or their caregivers.
Results: 56 patients with Pompe disease were interviewed; 51 had LOPD. Main demographic/clinical characteristics are given in Table 1. Frequencies of pre‐diagnosis symptoms are summarised in Figure 1; the most frequent was lower limb weakness (86% [44/51] patients). Patients with earlier symptoms in life received a quicker diagnosis than older ones; 75% (9/12) aged 1–9 years were diagnosed within 2 years of symptoms versus 36% (14/39) aged ≥10 years. Most patients (66% [33/51]) were referred by healthcare professionals to neuromuscular specialists/neurologists with a final diagnosis made mainly by neuromuscular specialists (39% [20/51]) and neurologists (31% [16/51]) often as part of a team of physicians (Figure 2). Key tests leading to diagnosis: muscle biopsy (n = 18), genetic testing (n = 12), blood panel (n = 8), dry blood spots (n = 5), liver biopsy (n = 1). Around one‐third of patients were misdiagnosed before Pompe disease was confirmed.

TABLE 1 Demographic and clinical characteristics of patients with LOPD.
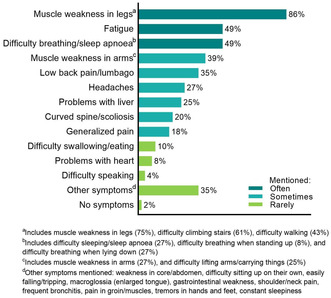
FIGURE 1 Frequency of pre‐diagnosis symptoms of Pompe disease mentioned by patients at interview.
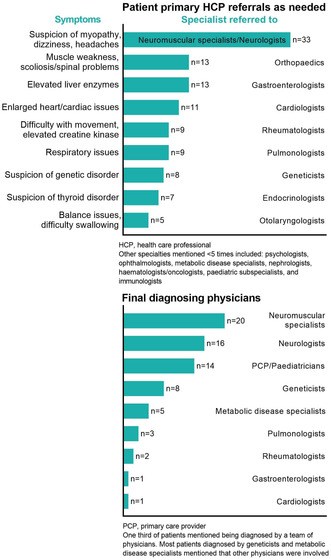
FIGURE 2 Diagnosis referrals in patients with LOPD and final diagnosing physicians.
Conclusion: These findings underline the need to raise worldwide awareness of Pompe disease symptoms and improve diagnostic pathways.
Disclosure: Funding: Sanofi Rafael Jenaro Martínez Marín has received travel expenses from Sanofi. Andrew Doerr and Rebecca Gould are employees of Fulcrum Research Group, which was contracted by Sanofi to conduct the research for this study. Jennifer Heuterman and Pamela Rajasekhar are employees of Sanofi and hold stock/stock options in Sanofi.
EPO‐811
Near fiber segment jitter in the diagnosis of myasthenia gravis
R. Mandeville 1; J. Luk1; O. Garnes‐Camarena2; D. Stashuk3
1Beth Israel Deaconess Medical Center, Boston, MA, USA; 2Jimenez Diaz Foundation University Hospital, Madrid, Spain; 3Systems Desing Engineering, University of Waterloo, Ontario, Canada
Background and Aims: Near fiber EMG (NFEMG) focuses on the activity of muscle fibers close to the electrode, can be applied to routinely acquired needle EMG, and offers the ability to semi‐automatically assess neuromuscular junction stability in a conceptually similar manner to single fiber EMG (SFEMG).
Methods: NFEMG was blindly applied to SFEMG recordings of 50 patients tested at BIDMC in the prior 18 months. In those without myopathy or neuropathy, we performed 10‐fold cross validation using two E‐Ref‐based NFEMG jitter value thresholds to establish the performance of several different criteria for classifying patients as MG or non‐MG, compared to clinical diagnosis, in each of the 10 testing sets as well as the full cohort.
Results: 12 of 50 patients were diagnosed clinically as MG after SFEMG testing (3 diagnosed as myopathy, 1 as neuropathy). Of those without myopathy or neuropathy, the sensitivity for detecting MG using NFEMG was 100% while the specificity ranged from 89% to 95% (mean of 90%). When testing on the whole cohort, sensitivity and specificity were 100% and 94%.
Conclusion: NFEMG performs well in diagnosing MG. Due to the ease of application to routine EMG and the minimal need for training, NFEMG may represent an effective screen prior to referring for SFEMG or as a viable alternative diagnostic test when SFEMG is not available, potentially addressing a significant global healthcare disparity.
Disclosure: Nothing to disclose.
EPO‐812
Natural history of distal and myofibrillar myopathies assessed by clinical and technological outcome measures (Dista‐Myo)
S. Bortolani 1; A. Vicino2; M. Gambella3; L. Villa3; M. Rabuffetti4; A. Marzegan4; V. Trombetta1; M. Cheli2; A. Parrotta3; E. Rolle5; E. Torchia6; B. Ravera6; M. Monforte1; J. Hogrel7; E. Ricci6; T. Mongini5; S. Sacconi3; L. Maggi2; G. Tasca8
1UOC di Neurologia, Fondazione Policlinico Universitario “A. Gemelli” IRCCS, Roma, Italy; 2Neuroimmunology and Neuromuscular Diseases Unit, Foundation IRCCS Neurological Institute Carlo Besta, Milano, Italy; 3Department Centre de référence des maladies Neuromusculaires, Centre Hospitalier Universitaire (CHU) de Nice, France; 4IRCCS Fondazione Don Carlo Gnocchi, Milan, Italy; 5Department of Neurosciences “Rita Levi Montalcini”, University of Torino, Torino, Italy; 6Università Cattolica del Sacro Cuore, Rome, Italy; 7Institut de Myologie, GH Pitié‐Salpêtrière, Paris, France; 8John Walton Muscular Dystrophy Research Centre, Newcastle University and Newcastle Hospitals NHS Foundation Trusts, Newcastle Upon Tyne, UK
Background and Aims: Dista‐Myo is an international multicentre longitudinal study that integrates validated motor function scales with novel technological tools for gait and strength assessment in patients with distal (DM) and myofibrillar myopathies (MFM). The study aims to gather natural history data and build a new toolbox for the evaluation of these disorders.
Methods: Patients were assessed by Motor Function Measure (MFM‐32), timed tests and dexterity tests as functional outcome measures; technological outcome measures included Myotools for muscle strength evaluation, and wireless insoles for gait analysis.
Results: Forty‐seven patients were assessed at baseline. Ninety‐six% showed reduced MFM‐32 scores, while 65% underperformed on 6MWT. Most patients presented impaired distal muscle strength (80% at ankle dorsiflexion, 92% at ankle plantar‐flexion, 50% at grip and pinch level). Metrics extracted from gait analysis significantly differed between patients and controls and correlated with distal muscle strength and functional scores. Preliminary analysis of the changes at 12 months showed a mild but significant decrease in MFM‐32 scores and MyoTools strength values compared to baseline, with a moderate responsiveness.
Conclusion: Baseline results showed heterogeneous impairment in the global motor function in our cohort of patients with DM and MFM. Distal muscle weakness and gait ability were efficiently captured by the combination of functional and digital outcome measures. MyoTools are promising digital tools able to define the extent of weakness even in severely affected patients and to capture changes in longitudinal studies.
Disclosure: This work has been funded by AFM Telethon (Grant to GT #23493).
EPO‐813
Assessing the suitability of the Neuro‐QoL fatigue to evaluate fatigue in patients living with myasthenia gravis
S. Pease; K. Scippa
Janssen Global Services, LLC
Background and Aims: Generalized myasthenia gravis (gMG) is a rare, chronic, autoantibody‐mediated neuromuscular disease characterized by fatigable muscle weakness. The objectives of this research were to identify an appropriate patient‐reported outcome (PRO) measure to assess fatigue in patients living with gMG and to conduct patient interviews to evaluate the content validity of the measure.
Methods: A literature review identified the Neuro‐QoL Fatigue as a suitable candidate PRO to assess fatigue in gMG. Twenty‐three interviews were conducted with adults living with gMG. All participants were recruited from the United States via research partners following IRB approval. Each interview explored the symptoms and impacts of gMG on participants’ daily lives. The last 8 interviews included debriefing of the Neuro‐QoL Fatigue to determine its appropriateness for use in gMG. Interviews were recorded and transcribed verbatim, and data were thematically analyzed.
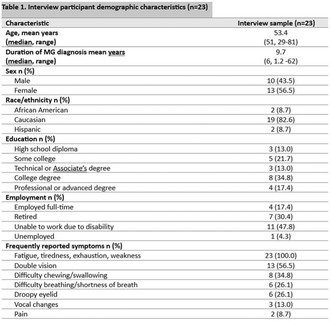
MG Research Participant Characteristics.
Results: All participants reported experiencing fatigue as part of their experience with gMG and that fatigue impacted their ability to carry out daily life activities and participation limitations. Among those asked to provide bothersome ratings, 80% (n = 12 of 15) reported that fatigue was their most bothersome symptom. The debriefing exercise demonstrated that nearly all participants interpreted the Neuro‐QoL Fatigue instructions, items, and recall period as intended.
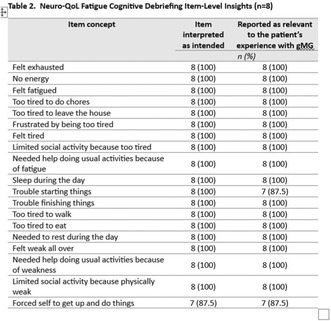
Cognitive Debriefing Item‐Level Insights.
Conclusion: Fatigue is a bothersome symptom of gMG that limits patients’ abilities to participate in daily life. The interview insights support the content validity of the Neuro‐QoL Fatigue in gMG patients. Future research will focus on evaluating the psychometric properties of the Neuro‐QoL Fatigue in the gMG population.
Disclosure: Sheryl Pease and Kayla Scippa are employees of Janssen Global Services, LLC This study was sponsored by Janssen Global Services, LLC.
EPO‐814
Very late onset myasthenia gravis with an unexpected high titer of AChR Abs: A new serological subtype?
E. Strataki; S. Bellos; L. Lymperopoulos; V. Zouvelou
1st Neurology Department, National and Kapodistrian University of Athens, Greece, Eginitio Hospital, ERN EURO‐MND
Background and Aims: Very late onset myasthenia gravis (VLOMG) (onset ≥65 years) is typically associated with low titers of acetylcholine receptor antibodies (AChR Abs), consistent with the age‐related thymic atrophy. This study investigates the occurrence and characteristics of VLOMG patients with high levels of AChR Abs at diagnosis.
Methods: We performed a registry‐based search for VLOMG patients with longitudinal follow‐up between 2008–2023. Clinical data were collected through our MG‐database.
Results: Of 69 VLOMG patients we identified 11 (15.9%) with a titer of AChR Abs ≥100 nM/L (radioimmunoprecipitation assay), 9 male and 2 female, with age at onset ranging from 65 to 85 years (mean: 75.2). AChR Abs titers ranged from 116 to 433 nM/L (mean: 217). There was no association with thymoma. All patients had generalized MG with prominent bulbar involvement. Two patients required intensive care unit monitoring. Plasmapheresis and/or intravenous immunoglobulin were necessitated in 9/11 patients. All patients were treated with prednisolone with prompt clinical response, while one received rituximab for refractory bulbar symptoms. The majority received concomitant non‐steroidal immunosuppression. At the last follow‐up, 9/11 patients had achieved a post‐intervention status of minimal manifestations or better.
Conclusion: Patients in this serological subgroup present clinical and therapeutic characteristics of typical VLOMG patients. However, the unexpected high titer of AChR Abs raises concern about residual thymic lymphoid follicles, a possible but rare finding in LOMG. This could not be confirmed, as none of our patients underwent thymectomy. Another plausible explanation could be the presence of autoantibodies targeting multiple AChR subunits. The latter warrants additional analysis of Abs subunit specificity.
Disclosure: Nothing to disclose.
EPO‐815
Long term follow up of late‐onset Pompe disease (LOPD) treated with alglucosidase alfa: The Italian experience
T. Mongini 1; O. Musumeci2; S. Ravaglia3; L. Ruggiero4; A. Fiumara5; R. Barone5; S. Servidei6; G. Siciliano7; G. Ricci7; L. Maggi8; M. Filosto9; G. D'Angelo10; G. Comi11; P. Tonin12; L. Verriello13; A. Barp14; E. Pegoraro15; A. Toscano2
1Department of Neurosciences, University of Torino, Torino, Italy; 2Unit of Neurology and Neuromuscular Disorders, Department of Clinical and Experimental Medicine, University of Messina, Italy; 3IRCCS Mondino Foundation, Pavia, Italy; 4Department of Neurosciences and Reproductive and Odontostomatological Sciences, University of Naples “Federico II”, Naples, Italy; 5Department of Clinical and Experimental Medicine, University of Catania, Catania, Italy; 6Unit of Neurophysiopathology, Institute of Neurology, University Cattolica del Sacro Cuore, Rome, Italy; 7Department of Clinical and Experimental Medicine, Neurological Clinic, University of Pisa, Pisa, Italy; 8Neurology IV‐Neuroimmunology and Neuromuscular Diseases Unit, Istituto Neurologico “Carlo Besta”, Milan, Italy; 9Department of Clinical and Experimental Sciences, University of Brescia, ASST Spedali Civili; NeMO‐Brescia Clinical Center for Neuromuscular Diseases, Brescia, Italy; 10Department of Scientific Institute E. Medea, Bosisio Parini, Italy; 11Neuromuscular and Rare Diseases Unit, Department of Neuroscience, Ospedale Maggiore Policlinico, Milan, Italy; 12Section of Clinical Neurology, Department of Neurosciences, Biomedicine and Movement Sciences, University of Verona, Verona, Italy; 13Neurology Unit, Department of Neurosciences, University Hospital Santa Maria della Misericordia, Udine, Italy; 14NeuroMuscular Omnicentre (NeMO) Trento, Villa Rosa Hospital, Pergine Valsugana, Italy; 15Department of Neurosciences, University of Padua, Padua, Italy
Background and Aims: Pompe Disease is due to deficiency of the lysosomal enzyme acid alfa‐glucosidase (GAA), with large phenotypic variability. An enzymatic replacement therapy (ERT) has been available since 2006, with different individual responses. Considering the new emerging therapies, it is important to collect information on large patients’ cohorts to define subgroups with homogeneous characteristics and their prognostic factors.
Methods: Fifteen Neuromuscular Centers, afferent to the Italian Myology Association (AIM), collected data from 90 LOPD patients (1–72 y, median 47) ERT‐treated for 10 years; for 39 of them, data at 15 years were available.
Results: At baseline, 6MWT results were wide‐ranging (60–814 m); 13/79 patients needed ventilatory support. FVC% values paralleled 6MWT results, with few exceptions. After 10 y, 6/77 patients had lost ambulation, and additional 3/30 after 15 years. Baseline 6MWT was <250 m in 8/9 of them. After 15 y, 9/27 patients were still stable, whereas 18 patients had worsened (66.6%). Age at start of therapy <18 y was a positive factor (85% stable after 15 y, against 7.31% treated aging >40 y). Five/32 patients (15.6%) with an initial FVC >80% started NIV after 10 y, compared to 21/34 (61.76%) with an initial FVC <80%. After 15 y, 16/39 patients (41.02%) were still ventilator‐free.
Conclusion: Our results confirm the large variability of clinical course and ERT responses in LOPD patients, with about 30% patients stable after 15 years (most of them with an early‐stage start of therapy), and a variable type and degree of decline in the others. A careful individual evaluation is requested in every patient when discussing the switch to alternative therapies.
Disclosure: Nothing to disclose.


