Abstract
In recent years, dynamic musculoskeletal ultrasound (DMUS) technology has demonstrated great potential in the diagnosis and treatment of orthopedic diseases. As a non-invasive, real-time imaging technique, it provides a dynamic view of joints and soft tissues, offering crucial insight for evaluating muscle injuries and bone damage caused by motion. This article comprehensively reviews the latest research in the field of DMUS, discussing its significant roles in managing orthopedic diseases and enhancing clinical practice. The application of DMUS is wide-ranging, including but not limited to the diagnosis of tendon injuries, ligament tears, arthritis, and soft tissue diseases. Additionally, DMUS has significant value in monitoring treatment progress and evaluating post-operative recovery. Furthermore, we discuss the use of DMUS for improving the accuracy and effectiveness of orthopedic surgeries. DMUS can provide high-quality diagnostic and therapeutic services for patients without a need for expensive equipment or complex procedures. Despite its promising outlook in orthopedics, broader clinical adoption remains limited by factors such as the steep learning curve associated with its use, the demand for specialized skills in interpreting high-quality images, and the need for extensive clinical validation. Future research should focus on standardizing operational procedures, improving the automation of image analysis, and validating its application in different orthopedic diseases through clinical trials.
Keywords: Dynamic musculoskeletal ultrasound, orthopedic diseases, clinical application, treatment status
Introduction
Dynamic Musculoskeletal Ultrasound (DMUS) is a significant innovation in medical technology in the recent decades. It utilizes high-frequency sound waves that reflect off various tissues to produce real-time imaging of non-bony structures like soft tissues and joints [1]. Unlike traditional static ultrasound, DMUS provides real-time images of joints and soft tissues during movement, offering more precise information for diagnosis and treatment. The development of this technology has greatly enriched the diagnostic and therapeutic tools available to orthopedic physicians, particularly in the early detection and treatment planning of musculoskeletal injuries [2]. The principle of DMUS is based on the physical properties of ultrasound waves. When ultrasound waves pass through tissues of different densities, they generate reflected waves. By receiving and interpreting these reflected waves, tissue images can be constructed. Compared to Magnetic Resonance Imaging (MRI) and Computed tomography (CT) scans, DMUS has advantages such as lower cost, ease of operation, and no radiation exposure, making it particularly suitable for examinations involving infants, young children, and pregnant women, where safety and non-invasiveness are paramount [3-5].
Since its introduction in the 1980s, DMUS technology has undergone significant advancements and expanded its application from initial basic research to widespread clinical practice. This technology is not only used for diagnosing various soft tissue and joint diseases, such as tendinitis, synovitis, and joint effusion but also for guiding therapeutic procedures like joint injections and soft tissue aspirations [6]. With technological advancements, DMUS has become an essential adjunct tool for orthopedic surgeons, sports medicine specialists, and rehabilitation physicians. It offers exceptional insight into the structure and functional status of tendons, ligaments, muscles, nerves, and other soft tissues [7]. Particularly in the diagnosis and treatment of sports injuries, DMUS provides crucial visual information to aid in developing precise treatment plans. The recent years have seen significant improvements in DMUS image quality, driven by continuous upgrading of ultrasound equipment and advancements in image processing techniques. This not only enhances its accuracy in clinical diagnosis but also widens its application in orthopedic treatments [8]. For instance, by dynamically observing changes in musculoskeletal structures during specific movements, physicians can better understand the mechanisms of diseases and provide more personalized and effective treatment plans for patients. Despite the remarkable progress in the application of DMUS technology in orthopedics, its full potential is yet to be fully explored. Future research should further explore its application in different orthopedic diseases, optimize operational techniques, and improve image quality to better serve clinical diagnosis and treatment.
DMUS has become increasingly vital for the diagnosis and treatment of orthopedic diseases. As an advanced imaging technology, DMUS provides real-time and dynamic images of joints and soft tissues, which are crucial for understanding and treating musculoskeletal disorders [9]. With its non-invasive and high-resolution capabilities, DMUS has become an indispensable tool for orthopedic physicians, particularly in the evaluation of soft tissue injuries and diseases such as tendons, ligaments, muscles, and arthritis [10]. DMUS excels in diagnosing rotator cuff injuries, where real-time observations of shoulder joint movement enable accurate identification of tendon tears and inflammation, allowing for personalized treatment plans. Additionally, for knee joint diseases such as meniscus injuries and patellar chondromalacia, DMUS provides critical diagnostic information to assist physicians in assessing the extent of damage and formulating surgical plans. In the field of sports medicine, DMUS plays a significant role in the diagnosis and monitoring of common sports injuries such as Achilles tendinitis and plantar fasciitis. By dynamically observing the injured areas, physicians can assess tissue damage and monitor recovery progress, providing more precise rehabilitation guidance for athletes.
Dynamic musculoskeletal ultrasound technology, as an innovative imaging tool, has significantly impacted the diagnosis and treatment of orthopedic diseases over the past few decades. By providing dynamic and real-time images of joints and soft tissues, it significantly enhances physicians’ understanding and capabilities in managing musculoskeletal disorders [11]. From early detection of rotator cuff tears to precise assessment of meniscus injuries in the knee joint, and meticulous monitoring of sports injuries, DMUS has proven its unique value in improving diagnostic accuracy, optimizing treatment plans, and monitoring the rehabilitation process.
An overview of dynamic musculoskeletal ultrasound technology
DMUS is a non-invasive, radiation-free diagnostic technique that allows real-time dynamic visualization of musculoskeletal diseases. In recent years, with advancements in ultrasound technology and continuous development of techniques, DMUS has gained widespread use for the diagnosis and treatment of orthopedic diseases [12].
The concept of DMUS was first introduced in the 1980s by M. van Holsbeeck, an American scholar, who pioneered the method of real-time ultrasound detection for the musculoskeletal system. Since then, DMUS has seen substantial technological evolution, establishing itself as a critical diagnostic tool in orthopedics [13]. A typical DMUS setup consists of an ultrasound transducer, main unit, and monitor. The transducer emits and receives ultrasound signals, while the main unit processes the signals to generate real-time dynamic ultrasound images, which are displayed on the monitor [14]. Additionally, the equipment includes various accessories such as transducers, scanning lines, and adjusters to meet the examination requirements for different body parts and pathologies. Since the 1980s, DMUS technology has undergone development from single scans to continuous scanning and from qualitative analysis to quantitative analysis [15]. In recent years, the emergence of high-resolution ultrasound transducers has significantly improved the resolution and frame rate capabilities of DMUS, enabling real-time dynamic observation of musculoskeletal diseases. Furthermore, the integration of Doppler ultrasound technology within DMUS allows for the detection of hemodynamic changes, adding crucial diagnostic value. The continuous development of ultrasound contrast imaging techniques, such as contrast-enhanced ultrasound and elastography, has further increased the diagnostic accuracy of DMUS [16].
The operational procedure of DMUS mainly includes patient preparation, probe selection and placement, scan parameter configuration, image acquisition, and analysis. First, the patient’s skin should be locally cleaned, and the probe selection should be based on the location and size of the patient’s lesion, ensuring proper contact between the probe and the skin. Next, the scan parameter should be adjusted according to the lesion characteristics and the performance of the ultrasound probe, such as frequency, dynamic range, and gain [17]. During image acquisition, it is essential to observe and record the dynamic changes of the lesion in real-time. In terms of image interpretation, physicians need to possess ultrasound image recognition skills, which they must integrate with combined clinical manifestations and other examination results to accurately diagnose and evaluate the disease. DMUS is highly valued for diagnosing and treating musculoskeletal diseases, thanks to its non-invasiveness, radiation-free nature, and real-time dynamic observation capabilities. DMUS not only allows real-time visualization of dynamic changes in lesions, providing clinicians with direct insight into the patient’s condition but also detects hemodynamic changes, assisting in the qualitative diagnosis of diseases. However, DMUS technology also has limitations, such as high operator dependency, requirements for probe placement and scan parameter configuration, and limited ability to detect lesions in certain specific areas. Therefore, in practical applications, physicians need to integrate patient conditions and other examination results for comprehensive judgment to improve diagnostic accuracy [18]. Although DMUS technology demonstrates high sensitivity and specificity in diagnosing soft tissue lesions, it is relatively less sensitive and specific in diagnosing skeletal lesions. Therefore, in practical applications, physicians need to choose the most effective examination method based on the patient’s condition [19].
Application of dynamic musculoskeletal ultrasound in orthopedic diseases
Tendon and ligament injuries are common orthopedic conditions, including rotator cuff tears, bicipital tendonitis, and ankle sprains. DMUS technology offers substantial diagnostic advantages for these conditions. For instance, rotator cuff tears, a common shoulder joint disease, present a challenge for traditional diagnostic methods like X-ray and MRI, which may not effectively reveal the dynamic structure and function of the cuff. In contrast, DMUS enables real-time visualization of dynamic changes in the rotator cuff, such as bursitis, tendonitis, and tears, providing clinicians with more intuitive information about the condition. Additionally, DMUS can assess the sliding movement of the long head of the biceps tendon, evaluating its function during shoulder joint movements [20]. Muscle injuries, including muscle tears and inflammation, are also prevalent in orthopedics. Traditional diagnostic methods like X-ray and MRI often fall short for effectively diagnosing conditions like quadriceps muscle injuries, a frequent issue of the knee joint. In contrast, DMUS allows real-time observation of dynamic changes in the quadriceps muscle, such as muscle tears and inflammation, providing clinicians with more intuitive information about the condition [21]. Furthermore, DMUS can assess muscle contraction function and tendon sliding, aiding in the diagnosis and evaluation of muscle injury severity.
Real-time DMUS is a cutting-edge technology that allows for the visualization of the movement and function of various structures, such as bones, muscles, and joints, during physical activities [22]. Knee joints are one of the most commonly involved joints in orthopedic diseases, and studies have shown that DMUS can effectively monitor the development of pathologic conditions of the knee joint, such as fluid accumulation, synovitis, meniscus injuries, and ligament injuries [23]. Furthermore, DMUS can dynamically observe the changes in articular cartilage, joint capsule, and ligaments during joint movement. In the diagnosis of anterior cruciate ligament (ACL) injuries, DMUS can clearly display the morphology, position, and continuity of the ligament, as well as the adhesion between the ligament and surrounding soft tissues, aiding in the localization, qualitative assessment, and staging of ACL injuries [24,25]. The shoulder joint, a ball-and-socket joint with a large range of motion, is susceptible to injury, and DMUS can visualize damage to structures like the shoulder joint capsule, labrum, and long head of the biceps tendon, as well as the stability of the glenohumeral joint [26].
DMUS is also instrumental during treatment. For knee diseases, it helps monitor the absorption of joint fluid, the repair of articular cartilage, and the healing of the meniscus, thereby guiding the formulation of clinical treatment plans [27]. In the treatment of knee synovitis, DMUS can monitor the absorption of joint fluid in real-time, evaluate the effectiveness of treatment, and guide clinical medication and physical therapy. Similarly, during the treatment of shoulder diseases, DMUS aids in assessing the repair of the labrum, the sliding of the long head of the biceps tendon, and the stability of the glenohumeral joint, thereby guiding the development of clinical treatment plans.
In recent years, with successive upgrades of ultrasound equipment and continuous improvements in technology, DMUS has broadened its application for the diagnosis and treatment of orthopedic diseases, particularly excelling in areas such as soft tissue tumor detection [28]. Lipomas, the most common benign soft tissue tumors, frequently occur in the limb and trunk. DMUS is capable of clearly depicting the morphology, boundaries, internal echo characteristics, and the adherence of the tumor to surrounding tissues, aiding in the localization, characterization, and staging of lipomas. Additionally, hemangiomas, benign tumors caused by the abnormal proliferation of vascular endothelial cells, can be classified into types such as strawberry hemangiomas and cavernous hemangiomas. DMUS is able to display the blood flow signals of hemangiomas and delineate the tumor boundaries with surrounding tissues, aiding in both diagnosis and differential diagnosis [29,30]. Moreover, DMUS also finds application in malignant tumors, where sarcomas, originating from muscle tissues and frequently occurring in limbs and trunks, can be evaluated for their morphology, boundaries, and internal echo characteristics, as well as the adherence of the tumor to surrounding tissues, facilitating the localization, characterization, and staging of sarcomas [31]. The application of DMUS for the treatment of soft tissue tumors primarily includes preoperative assessment, postoperative evaluation, and monitoring of treatment efficacy. By observing real-time changes in tumor morphology, size, and position, as well as the adherence of the tumor to surrounding tissues, DMUS can provide essential information for developing clinical treatment plans. For lipomas, DMUS facilitates monitoring of tumor volume changes and evaluating treatment efficacy, guiding decisions for clinical medication and physical therapy. Furthermore, in the treatment of hemangiomas, DMUS tracks changes in tumor blood flow signals, assesses treatment efficacy, and supports surgical and medical decisions.
Moreover, studies have discovered that DMUS possesses unique advantages in the localization and quantitative assessment of fractures. Traditional imaging techniques, such as X-rays and CT scans, can provide qualitative information about fractures but lack the ability to directly observe the functional state of muscles and ligaments [32]. DMUS, however, can accurately assess the stability and healing status of the fracture site through real-time observation of the movement and deformation of musculoskeletal tissues. After fracture fixation surgery, DMUS assists physicians in observing the precise position of fixation screws or plates, identifying any issues including looseness or displacement, and guiding further treatment measures [33]. Additionally, DMUS can evaluate the extent of ligament and muscle injuries, which is crucial for the recovery of joint function related to fractures. Minimally invasive techniques, which are becoming increasingly common in orthopedic surgeries such as arthroscopic surgery and endoscopic soft tissue repair, require highly precise visual guidance due to the demanding nature of the surgical procedures [34]. DMUS offers real-time three-dimensional imaging, aiding surgeons in precisely locating and quantitatively assessing key structures during surgery, such as fracture fragments, patellar ligaments, and tendons. In arthroscopic chondroplasty, DMUS helps surgeons observe changes at the cartilage level and the effectiveness of the repair, allowing for timely adjustment to the surgical plan, thereby enhancing the success rate. Furthermore, DMUS plays a significant role in orthopedic rehabilitation. Assessing the recovery of muscle strength and functionality is crucial during the rehabilitation process, and DMUS enables real-time observation of muscle contraction and extension, aiding physicians in evaluating the recovery of a patient’s muscle strength and coordination. Specifically in the rehabilitation following anterior cruciate ligament reconstruction of the knee, DMUS assists rehabilitation therapists in quantitatively assessing the contraction of the patient’s thigh muscles, enabling timely adjustment to the rehabilitation plan to improve outcome.
In sports medicine, musculoskeletal injuries represent a common affliction among athletes [35]. Traditional imaging modalities like X-rays and CT scans are capable of providing static images of fractures but fail to capture the functional state of injured muscles. DMUS, on the other hand, enables the observation of muscle behavior during movement, offering real-time assessment of the extent of bone and muscle damage as well as monitoring the recovery process [36]. Specifically for diagnosing tendon ruptures, DMUS provides immediate morphologic and functional information of the injured tendon by observing changes in the tendon during motion, which helps precisely locate and evaluate the severity and healing of the rupture. Recent studies have demonstrated the effectiveness of DMUS in evaluating muscle strength impairment following Achilles tendon rupture and in guiding rehabilitation treatment. Furthermore, common athletic injuries such as muscle strains and tendinitis can also be monitored in real-time, aiding physicians in directing treatment [37-39]. In cases of Achilles tendinitis, DMUS can reveal the morphology and changes of the tendon during movement. By comparing dynamic images of injured and healthy tendons, physicians can clearly determine the presence and severity of the lesion. Additionally, DMUS allows for quantitative assessment of the mechanical properties of the affected tendon, such as its elastic modulus and strain rate, providing a basis for customized treatment plans.
To summarize, DMUS represents a non-invasive and real-time imaging technology with a broad application spectrum in sports medicine. Its use in diagnosing, treating, and guiding surgery for musculoskeletal injuries furnishes physicians with accurate and immediate information that enhances the diagnosis and treatment of orthopedic diseases.
Technological innovations and clinical practice
In the current landscape of medical technology, there is significant poten tial for advancement in DMUS devices and techniques. The resolution of these devices on the market today is somewhat limited, compromising the clarity with which finer structures are visualized [40,41]. Furthermore, due to the inherent requirement for high imaging speed and frame rate in DMUS, existing equipment requires further refinement of these aspects. These limitations affect the accuracy and reliability of DMUS in clinical application [42]. Recent years have witnessed significant interest in high-frequency ultrasound technology for the assessment of fine structures [43]. Studies have demonstrated that high-frequency ultrasound can clearly delineate various structures of the meniscus in the knee joints of healthy volunteers, providing a new radiologic basis for diagnosing meniscal injury. Additionally, this technology is effective in assessing fine structures such as joint cartilage and ligaments, facilitating early diagnosis and treatment of orthopedic diseases [44].
Elastography, a novel ultrasound technique developed in recent years, assesses tissue elasticity by measuring its elastic modulus. In musculoskeletal diseases, elastography has been used to evaluate the elasticity changes in soft tissues, muscles, and ligaments. For instance, research using elastography to study the muscle elasticity changes in patients with long head biceps tendinitis revealed a significant decrease in muscle elasticity around the tendon, suggesting the potential of elastography for diagnosing and treating musculoskeletal diseases [45].
Additionally, three-dimensional imaging technology has garnered significant attention in musculoskeletal ultrasound. Evaluations of hip joints in patients with avascular necrosis of the femoral head using this technology have clearly identified the extent and location of the necrosis, providing a critical basis for treatment. Moreover, when combined with quantitative analysis methods, three-dimensional imaging technology allows for precise measurement and assessment of musculoskeletal diseases. Research employing this technology for quantitative analysis of knee joint cartilage in patients with cartilage injuries has demonstrated a significant reduction in cartilage thickness, offering a new radiologic basis for the treatment of these injuries.
Furthermore, with the advancement of artificial intelligence (AI) technology, many studies have focused on the application of AI for recognizing and analyzing musculoskeletal ultrasound images [46]. Research utilizing Convolutional Neural Networks (CNN) for the automatic recognition and analysis of musculoskeletal ultrasound images has shown that CNNs can accurately identify musculoskeletal diseases and perform quantitative analyses. In addition, the use of deep learning technologies for automatic segmentation and analysis of musculoskeletal ultrasound images has provided new tools for the diagnosis and treatment of musculoskeletal diseases [47].
In summary, the application and therapeutic relevance of DMUS in orthopedic diseases has garnered widespread attention. With the continual development of new technologies such as high-frequency ultrasound, elastography, three-dimensional imaging, and AI, the role of DMUS in the diagnosis and treatment of orthopedic diseases is growing. Therefore, future efforts should focus on further research and promotion of DMUS technology, to enhance awareness of itsapplication among clinicians. This advancement will offer a more precise and effective means for diagnosing and treating orthopedic disease.
Clinical treatment and rehabilitation monitoring
DMUS enables the real-time observation of dynamic changes at surgical sites, offering a robust tool for monitoring surgical outcome [48]. In the context of knee replacement surgery, DMUS enables the observation of post-operative synovial fluid production and absorption, as well as the healing process of joint surfaces. This information is crucial for assessing the effectiveness of the surgical treatment and for the timely detection and management of complications [49,50]. DMUS can also be employed to evaluate the outcomes of non-surgical treatments, such as physical and pharmacologic therapies. For instance, the evaluation of muscle elasticity changes in patients with long head biceps tendinitis after physical therapy using DMUS revealed significant improvement in muscle elasticity after a period of treatment [51]. Additionally, DMUS can monitor changes in the affected areas during drug therapy, providing a basis for adjusting pharmacologic treatment [52]. In the rehabilitation process, DMUS facilitates dynamic assessment of a patient’s condition, offering personalized rehabilitation guidance based on the assessment results [53]. For patients with fractures, DMUS allows observation of the healing process at the fracture site and the recovery of surrounding soft tissues. Utilizing the feedback from DMUS results, a tailored rehabilitation plan can be developed for the patient to promote fracture healing and recovery through functional exercises [54].
In summary, DMUS holds significant value in clinical treatment and rehabilitation monitoring. By providing real-time observation of the dynamic changes in diseased areas, DMUS technology offers robust support for the assessment of clinical treatment outcomes and the rehabilitation process. However, in practical application, it is essential to integrate DMUS technology with other imaging modalities to enhance the accuracy and reliability of assessments. As DMUS technology continues to evolve, its application for clinical treatment and rehabilitation monitoring is expected to become increasingly widespread.
Challenges, opportunities, and future directions
Despite the significant potential of DMUS technology in diagnosing and treating orthopedic diseases, its widespread application still faces several challenges. Concurrently, advancements in science and technology present new opportunities for the development of DMUS.
Promotion of DMUS technology encounters challenges related to technical standardization and operational training. Given the relatively recent advent of DMUS, the absence of uniform technical standards and procedural guidelines has resulted in considerable variability in its application across different healthcare facilities and among physicians, impacting the effectiveness of diagnoses and treatments [55,56]. To address this issue, it is crucial to enhance the standardization of DMUS technology by establishing uniform technical standards and operational protocols, coupled with extensive training and dissemination efforts. With scientific and technological progress, the performance and accessibility of DMUS equipment have significantly improved. The market now offers devices with high-resolution and high-speed imaging capabilities, meeting the clinical demand for detailed structural observations. Moreover, as the technology matures, the cost of DMUS equipment is gradually decreasing, making it more affordable for a broader range of medical institutions and patients [57].
DMUS technology retains immense developmental potential for the diagnosis and treatment of orthopedic diseases. Researchers are encouraged to further investigate the use of DMUS for the early diagnosis and treatment of orthopedic conditions to enhance patient recovery rates and quality of life. Additionally, by integrating advanced technologies such as artificial intelligence and big data, researchers can develop novel DMUS analysis methods to increase the accuracy and efficiency of diagnoses and treatments. Moreover, the application of DMUS for rehabilitation monitoring should be explored to foster a more scientific and personalized rehabilitation process for patients.
Conclusion
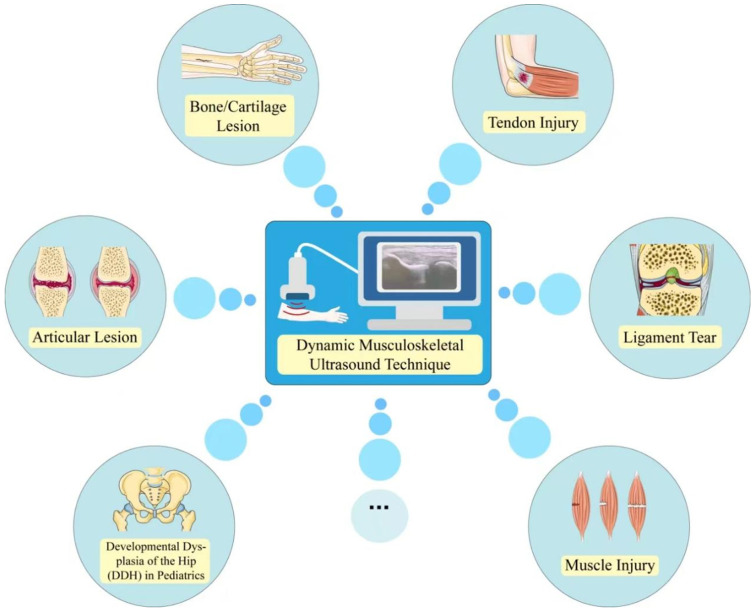
Dynamic musculoskeletal ultrasound technology (DMUS), characterized by its non-invasive nature, absence of radiation, and user-friendly operation, is a novel approach to the diagnosis and treatment of orthopedic conditions. Currently, this technology has demonstrated effective outcomes in diagnosing and treating orthopedic ailments such as fractures, arthritis, and musculoskeletal tumors. Moreover, its application for rehabilitation monitoring has attracted significant attention, contributing to a more scientific and personalized rehabilitation process for patients (Figure 1). Nonetheless, the clinical application of DMUS technology still faces challenges including the standardization of techniques, operator training, equipment performance, and accessibility. To maximize the benefits of this technology, it is crucial to enhance technical standardization, establish unified clinical guidelines, and promote widespread training and dissemination. Additionally, advancements in science and technology have notably improved the performance and accessibility of DMUS devices, promising to increase their prevalence in clinical settings. The technology is undergoing further development for the diagnosis and treatment of orthopedic diseases. Researchers are encouraged to explore its application in for early diagnosis and treatment of orthopedic conditions, aiming to improve patient recovery rates and quality of life. Furthermore, the integration of cutting-edge technologies such as artificial intelligence and big data can lead to the development of new DMUS analysis methods, further enhancing the accuracy and efficiency of diagnosis and treatment. The application of DMUS in rehabilitation monitoring also warrants further investigation to foster a more scientific and personalized recovery process.
Figure 1.
Current status of the application of dynamic musculoskeletal ultrasound in orthopedic diseases.
In conclusion, DMUS technology holds great promise for orthopedic disease diagnosis and treatment. Overcoming hurdles associated with technique standardization and operator training, and improving equipment functionality and accessibility, along with the continuous exploration of new avenues for research and technological breakthroughs, will make DMUS technology an increasingly accurate and efficient tool.
Disclosure of conflict of interest
None.
References
- 1.Wang L, Zhao W, Xing Y, Sun T, Chen X. Research progress of dynamic musculoskeletal ultrasound image processing. Zhongguo Yi Liao Qi Xie Za Zhi. 2019;43:32–36. doi: 10.3969/j.issn.1671-7104.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Bright JM, Fields KB, Draper R. Ultrasound diagnosis of calf injuries. Sports Health. 2017;9:352–355. doi: 10.1177/1941738117696019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sikdar S, Wei Q, Cortes N. Dynamic ultrasound imaging applications to quantify musculoskeletal function. Exerc Sport Sci Rev. 2014;42:126–135. doi: 10.1249/JES.0000000000000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chauvin NA, Khwaja A. Musculoskeletal imaging in neonates: use of ultrasound. Pediatr Radiol. 2022;52:765–776. doi: 10.1007/s00247-021-05152-2. [DOI] [PubMed] [Google Scholar]
- 5.Jacobson JA. Musculoskeletal ultrasound and MRI: which do I choose? Semin Musculoskelet Radiol. 2005;9:135–149. doi: 10.1055/s-2005-872339. [DOI] [PubMed] [Google Scholar]
- 6.Caldwell AS, Elangovan SM, Jacobson JA. Dynamic musculoskeletal ultrasound: slipping rib, muscle hernia, snapping hip, and peroneal tendon pathology. Pediatr Radiol. 2023;53:1553–1561. doi: 10.1007/s00247-023-05700-y. [DOI] [PubMed] [Google Scholar]
- 7.Pesquer L, Guillo S, Poussange N, Pele E, Meyer P, Dallaudière B. Dynamic ultrasound of peroneal tendon instability. Br J Radiol. 2016;89:20150958. doi: 10.1259/bjr.20150958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kara M, Özçakar L, De Muynck M, Tok F, Vanderstraeten G. Musculoskeletal ultrasound for peripheral nerve lesions. Eur J Phys Rehabil Med. 2012;48:665–674. quiz 708. [PubMed] [Google Scholar]
- 9.Karnik AS, Karnik A, Joshi A. Ultrasound examination of pediatric musculoskeletal diseases and neonatal spine. Indian J Pediatr. 2016;83:565–577. doi: 10.1007/s12098-015-1957-2. [DOI] [PubMed] [Google Scholar]
- 10.Lee KS, Rosas HG, Craig JG. Musculoskeletal ultrasound: elbow imaging and procedures. Semin Musculoskelet Radiol. 2010;14:449–460. doi: 10.1055/s-0030-1263260. [DOI] [PubMed] [Google Scholar]
- 11.Löfstedt T, Ahnlund O, Peolsson M, Trygg J. Dynamic ultrasound imaging--a multivariate approach for the analysis and comparison of time-dependent musculoskeletal movements. BMC Med Imaging. 2012;12:29. doi: 10.1186/1471-2342-12-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neubauer R, Recker F, Bauer CJ, Brossart P, Schäfer VS. The current situation of musculoskeletal ultrasound education: a systematic literature review. Ultrasound Med Biol. 2023;49:1363–1374. doi: 10.1016/j.ultrasmedbio.2023.02.008. [DOI] [PubMed] [Google Scholar]
- 13.van Holsbeeck M, Introcaso JH. Musculoskeletal ultrasonography. Radiol Clin North Am. 1992;30:907–925. [PubMed] [Google Scholar]
- 14.Flores DV, Bohyn C, Murray TÉ, Murphy DT, Cresswell M. Dynamic US of musculoskeletal disorders: a pictorial review with emphasis on techniques. Radiographics. 2023;43:e220130. doi: 10.1148/rg.220130. [DOI] [PubMed] [Google Scholar]
- 15.Forney MC, Delzell PB. Musculoskeletal ultrasonography basics. Cleve Clin J Med. 2018;85:283–300. doi: 10.3949/ccjm.85a.17014. [DOI] [PubMed] [Google Scholar]
- 16.Pirri C, Pirri N, Stecco C, Macchi V, Porzionato A, De Caro R, Özçakar L. ‘Ultrasound examination’ of the musculoskeletal system: bibliometric/visualized analyses on the terminology (change) Tomography. 2023;9:352–361. doi: 10.3390/tomography9010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eranki A, Cortes N, Ferenček ZG, Sikdar S. A novel application of musculoskeletal ultrasound imaging. J Vis Exp. 2013:e50595. doi: 10.3791/50595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Markowski AM, Watkins MK, Maitland ME, Manske RC, Podoll KR, Hayward LM. Exploring the integration of diagnostic musculoskeletal ultrasound imaging into clinical practice by physical therapists. Physiother Theory Pract. 2024;40:544–555. doi: 10.1080/09593985.2022.2135979. [DOI] [PubMed] [Google Scholar]
- 19.Innes S, Jackson J. Musculoskeletal ultrasound imaging - integration with the biopsychosocial model. Musculoskelet Sci Pract. 2019;44:102067. doi: 10.1016/j.msksp.2019.102067. [DOI] [PubMed] [Google Scholar]
- 20.Draghi F, Bortolotto C, Draghi AG, Gitto S. Intrasheath instability of the peroneal tendons: dynamic ultrasound imaging. J Ultrasound Med. 2018;37:2753–2758. doi: 10.1002/jum.14633. [DOI] [PubMed] [Google Scholar]
- 21.Sahr ME, Endo Y, Sink EL, Miller TT. Dynamic ultrasound assessment of hip instability and anterior and posterior hip impingement. Skeletal Radiol. 2023;52:1385–1393. doi: 10.1007/s00256-022-04264-6. [DOI] [PubMed] [Google Scholar]
- 22.Mezian K, Ricci V, Güvener O, Jačisko J, Novotný T, Kara M, Chang KV, Naňka O, Pirri C, Stecco C, Dughbaj M, Jain NB, Özçakar L. EURO-MUSCULUS/USPRM dynamic ultrasound protocols for (Adult) hip. Am J Phys Med Rehabil. 2022;101:e162–e168. doi: 10.1097/PHM.0000000000002061. [DOI] [PubMed] [Google Scholar]
- 23.Özçakar L, Ricci V, Mezian K, Pirri C. A new and dedicated video gallery: EURO-MUSCULUS/USPRM protocols for dynamic ultrasound examination of the joints. Am J Phys Med Rehabil. 2022;101:201–202. doi: 10.1097/PHM.0000000000001956. [DOI] [PubMed] [Google Scholar]
- 24.Wu WT, Onishi K, Mezian K, Naňka O, Wang B, Su DC, Ricci V, Chang KV, Özçakar L. Ultrasound imaging of the posterior lateral corner of the knee: a pictorial review of anatomy and pathologies. Insights Imaging. 2024;15:39. doi: 10.1186/s13244-024-01606-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pirri C, Stecco C, Güvener O, Mezian K, Ricci V, Jačisko J, Novotný T, Kara M, Chang KV, Dughbaj M, Jain NB, Özçakar L. EURO-MUSCULUS/USPRM dynamic ultrasound protocols for knee. Am J Phys Med Rehabil. 2023;102:e67–e72. doi: 10.1097/PHM.0000000000002173. [DOI] [PubMed] [Google Scholar]
- 26.Ricci V, Chang KV, Güvener O, Mezian K, Kara M, Leblebicioğlu G, Stecco C, Pirri C, Ata AM, Dughbaj M, Jain NB, Özçakar L. EURO-MUSCULUS/USPRM dynamic ultrasound protocols for shoulder. Am J Phys Med Rehabil. 2022;101:e29–e36. doi: 10.1097/PHM.0000000000001833. [DOI] [PubMed] [Google Scholar]
- 27.De Muynck M, Parlevliet T, De Cock K, Vanden Bossche L, Vanderstraeten G, Özçakar L. Musculoskeletal ultrasound for interventional physiatry. Eur J Phys Rehabil Med. 2012;48:675–87. [PubMed] [Google Scholar]
- 28.Gross JS, Yaeger A, Tchelepi H, Matcuk GR Jr. Ultrasound fusion: applications in musculoskeletal imaging. Life (Basel) 2023;13:1278. doi: 10.3390/life13061278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Navarro SM, Matcuk GR, Patel DB, Skalski M, White EA, Tomasian A, Schein AJ. Musculoskeletal imaging findings of hematologic malignancies. Radiographics. 2017;37:881–900. doi: 10.1148/rg.2017160133. [DOI] [PubMed] [Google Scholar]
- 30.Tannenbaum MF, Noda S, Cohen S, Rissmiller JG, Golja AM, Schwartz DM. Imaging musculoskeletal manifestations of pediatric hematologic malignancies. AJR Am J Roentgenol. 2020;214:455–464. doi: 10.2214/AJR.19.21833. [DOI] [PubMed] [Google Scholar]
- 31.Howe BM, Broski SM, Littrell LA, Pepin KM, Wenger DE. Quantitative musculoskeletal tumor imaging. Semin Musculoskelet Radiol. 2020;24:428–440. doi: 10.1055/s-0040-1708825. [DOI] [PubMed] [Google Scholar]
- 32.Gitto S, Messina C, Mauri G, Aliprandi A, Sardanelli F, Sconfienza LM. Dynamic high-resolution ultrasound of intrinsic and extrinsic ligaments of the wrist: how to make it simple. Eur J Radiol. 2017;87:20–35. doi: 10.1016/j.ejrad.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 33.Pai DR, Thapa M. Musculoskeletal ultrasound of the upper extremity in children. Pediatr Radiol. 2013;43(Suppl 1):S48–S54. doi: 10.1007/s00247-012-2600-2. [DOI] [PubMed] [Google Scholar]
- 34.Nazarian LN. Musculoskeletal ultrasound: applications in the hip. J Dance Med Sci. 2011;15:173–176. [PubMed] [Google Scholar]
- 35.Torriani M, Kattapuram SV. Musculoskeletal ultrasound: an alternative imaging modality for sports-related injuries. Top Magn Reson Imaging. 2003;14:103–111. doi: 10.1097/00002142-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Robotti G, Draghi F, Bortolotto C, Canepa MG. Ultrasound of sports injuries of the musculoskeletal system: gender differences. J Ultrasound. 2020;23:279–285. doi: 10.1007/s40477-020-00438-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meyer NB, Jacobson JA, Kalia V, Kim SM. Musculoskeletal ultrasound: athletic injuries of the lower extremity. Ultrasonography. 2018;37:175–189. doi: 10.14366/usg.18013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centurion AJ, Youmans H, Zeini IM. Use of musculoskeletal ultrasound and regenerative therapies in soccer. Am J Orthop (Belle Mead NJ) 2018;47 doi: 10.12788/ajo.2018.0093. [DOI] [PubMed] [Google Scholar]
- 39.Bailowitz Z, Visco CJ, Christen K, Ahmad CS. Diagnostic musculoskeletal ultrasound for the acute evaluation and management of soccer players. Curr Sports Med Rep. 2021;20:525–530. doi: 10.1249/JSR.0000000000000890. [DOI] [PubMed] [Google Scholar]
- 40.Wu WT, Chang KV, Hsu YC, Hsu PC, Ricci V, Özçakar L. Artifacts in musculoskeletal ultrasonography: from physics to clinics. Diagnostics (Basel) 2020;10:645. doi: 10.3390/diagnostics10090645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Taljanovic MS, Melville DM, Scalcione LR, Gimber LH, Lorenz EJ, Witte RS. Artifacts in musculoskeletal ultrasonography. Semin Musculoskelet Radiol. 2014;18:3–11. doi: 10.1055/s-0034-1365830. [DOI] [PubMed] [Google Scholar]
- 42.Motamedi D, Bauer AH, Patel R, Morgan TA. Problem solved: integral applications of musculoskeletal ultrasound. J Ultrasound Med. 2021;40:1693–1704. doi: 10.1002/jum.15551. [DOI] [PubMed] [Google Scholar]
- 43.Albano D, Aringhieri G, Messina C, De Flaviis L, Sconfienza LM. High-frequency and ultra-high frequency ultrasound: musculoskeletal imaging up to 70 MHz. Semin Musculoskelet Radiol. 2020;24:125–134. doi: 10.1055/s-0039-3401042. [DOI] [PubMed] [Google Scholar]
- 44.Jabbar SI, Aladi AQ, Day C, Chadwick E. A new method of contrast enhancement of musculoskeletal ultrasound imaging based on fuzzy inference technique. Biomed Phys Eng Express. 2021;7 doi: 10.1088/2057-1976/ac0dce. [DOI] [PubMed] [Google Scholar]
- 45.Corazza A, Orlandi D, Fabbro E, Ferrero G, Messina C, Sartoris R, Perugin Bernardi S, Arcidiacono A, Silvestri E, Sconfienza LM. Dynamic high-resolution ultrasound of the shoulder: how we do it. Eur J Radiol. 2015;84:266–277. doi: 10.1016/j.ejrad.2014.11.007. [DOI] [PubMed] [Google Scholar]
- 46.Dinescu SC, Stoica D, Bita CE, Nicoara AI, Cirstei M, Staiculesc MA, Vreju F. Applications of artificial intelligence in musculoskeletal ultrasound: narrative review. Front Med (Lausanne) 2023;10:1286085. doi: 10.3389/fmed.2023.1286085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shin Y, Yang J, Lee YH, Kim S. Artificial intelligence in musculoskeletal ultrasound imaging. Ultrasonography. 2021;40:30–44. doi: 10.14366/usg.20080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Apard T. Ultrasonography for the orthopaedic surgeon. Orthop Traumatol Surg Res. 2019;105:S7–S14. doi: 10.1016/j.otsr.2018.04.027. [DOI] [PubMed] [Google Scholar]
- 49.Liu X, Chen Z, Gao Y, Zhang J, Jin Z. High tibial osteotomy: review of techniques and biomechanics. J Healthc Eng. 2019;2019:8363128. doi: 10.1155/2019/8363128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Soliman SB, Davis JJ, Muh SJ, Vohra ST, Patel A, van Holsbeeck MT. Ultrasound evaluations and guided procedures of the painful joint arthroplasty. Skeletal Radiol. 2022;51:2105–2120. doi: 10.1007/s00256-022-04080-y. [DOI] [PubMed] [Google Scholar]
- 51.Jopowicz R, Jopowicz M, Czarnocki Ł, Deszczyński JM, Deszczyński J. Current uses of ultrasound imaging in musculoskeletal rehabilitation. Ortop Traumatol Rehabil. 2017;19:503–511. doi: 10.5604/01.3001.0010.7036. [DOI] [PubMed] [Google Scholar]
- 52.Ozçakar L, Tok F, De Muynck M, Vanderstraeten G. Musculoskeletal ultrasonography in physical and rehabilitation medicine. J Rehabil Med. 2012;44:310–318. doi: 10.2340/16501977-0959. [DOI] [PubMed] [Google Scholar]
- 53.Qiu M, Wu Q, Tao J, Song Z, Yuan X, Li J. Application and thinking of musculoskeletal ultrasound in diagnosis and treatment of musculoskeletal diseases with acupuncture and moxibustion. Zhongguo Zhen Jiu. 2023;44:39–42. doi: 10.13703/j.0255-2930.20230630-k0004. [DOI] [PubMed] [Google Scholar]
- 54.Strakowski JA, Visco CJ. Diagnostic and therapeutic musculoskeletal ultrasound applications of the shoulder. Muscle Nerve. 2019;60:1–6. doi: 10.1002/mus.26505. [DOI] [PubMed] [Google Scholar]
- 55.Ricci V, Güvener O, Chang KV, Wu WT, Mezian K, Kara M, Leblebicioğlu G, Pirri C, Ata AM, Dughbaj M, Jain NB, Stecco C, Özçakar L. EURO-MUSCULUS/USPRM dynamic ultrasound protocols for elbow. Am J Phys Med Rehabil. 2022;101:e83–e92. doi: 10.1097/PHM.0000000000001915. [DOI] [PubMed] [Google Scholar]
- 56.Karnik AS, Karnik A, Joshi A. Ultrasound examination of pediatric musculoskeletal diseases and neonatal spine. Indian J Pediatr. 2016;83:565–77. doi: 10.1007/s12098-015-1957-2. [DOI] [PubMed] [Google Scholar]
- 57.Nguyen S, Lu X, Ma Y, Du J, Chang EY, von Drygalski A. Musculoskeletal ultrasound for intra-articular bleed detection: a highly sensitive imaging modality compared with conventional magnetic resonance imaging. J Thromb Haemost. 2018;16:490–499. doi: 10.1111/jth.13930. [DOI] [PMC free article] [PubMed] [Google Scholar]