Abstract
Purpose: To investigate the prevalence of occupational lower back pain (OLBP) among medical workers and identify the contributing factors. Methods: An electronic questionnaire was distributed to medical workers at Yuebei People’s Hospital to gather information on various factors, including gender, age, body mass index (BMI), length of employment, job role, education level, professional title, marital status, fertility status, frequency of night shift, weight lifting daily, duration of daily standing at work, frequency of bending, work-related stress, experience with low back protection training, and frequency of waist exercises. Univariate and multivariate logistic regression analyses were conducted to identify the factors associated with OLBP in medical workers. Results: Out of the 98 medical workers surveyed, 67 experienced OLBP (68.37%). The results of multivariate logistic regression analysis revealed that working for more than 5 years, holding a nursing position, and lacking training in low back protection were significant risk factors for developing OLBP in medical workers (all P<0.05). Conclusion: OLBP is a prevalent issue among medical workers, and various factors such as length of employment, job role, and training in low back protection can influence its occurrence.
Keywords: Medical workers, low back pain, investigation of the current status, multi-factor analysis
Introduction
In this fast-paced and ever-evolving society, low back pain (LBP) has emerged as a prevalent ailment that greatly affects individuals’ work and personal lives [1,2]. The World Health Organization recognizes LBP as a collection of syndromes wherein low back pain or sciatica are primary clinical manifestations. Research indicates that individuals have an 84% likelihood of experiencing LBP at some point in their lives, with the highest prevalence observed at ages of 40-69 years [3,4]. However, recent epidemiological studies suggest a growing trend of LBP among younger people [5,6]. Occupational low back pain (OLBP) characterized by pain between the 11th and 12th thoracic vertebrae and buttocks, as well as limited mobility resulting from work-related factors, significantly impacts an individual’s work performance and can even lead to work incapacity in severe cases. OLBP is particularly prevalent among medical professionals, office workers, farmers, and individuals engaged in occupations that entail prolonged periods of sitting, standing, or heavy lifting [7-9].
In recent years, there has been a surge in hospital visits due to improvement in medical services, patients’ self-care awareness and living standards. Amidst this influx, medical workers find themselves consistently occupied and under significant pressure, evident in the demanding nature of their responsibilities such as prolonged surgeries, patient transfers, and instrument lifting [10]. All these undoubtedly contribute to the occurrence of OLBP among medical staff to some extent. The impact of OLBP on the quality of life and work of medical professionals is profound, with far-reaching consequences extending to societal burdens [11,12]. Thus, it is imperative for both medical workers and healthcare institutions to prioritize addressing OLBP. It is crucial to investigate the current status of OLBP among medical workers and analyze the factors that influence its occurrence.
While there exist studies on OLBP among medical workers, previous studies have only focused on nursing workers, and few have included doctors, pharmacists, or other technicians [13]. Therefore, conducting a more comprehensive analysis of the current status of OLBP and its related influencing factors among medical workers would have theoretical value and significance. This study aims to address this gap by delving into the actual working conditions of medical workers affected by OLBP and by exploring strategies to mitigate its impact through an in-depth analysis of contributing factors.
Subjects and methods of research
Research subjects
This study collected data from medical staff at Yuebei People’s Hospital during September 2022 to September 2023 for the analysis. Inclusion criteria for research subjects were as follows: (1) Holding vocational qualification and being registered for practice; (2) Doctors, care workers, medical technicians, or pharmacists at the hospital; (3) No history of low back traumas. The exclusion criteria were as follows: (1) Experiencing low back pain due to menstruation or pregnancy; (2) Having low back pain caused by tumors, tuberculosis, or ankylosing spondylitis; (3) Being absent for study or vacation during the data collection period; (4) Being retired or re-employed after retirement. This study was approved by the Ethics Committee of Yuebei People’s Hospital.
Data collection
We utilized an electronic questionnaire for information surveying, comprising two parts: assessment of OLBP prevalence, and collection of general information. For the assessment of OLBP prevalence among medical workers, we employed the Oswestry Disability Index (ODI) questionnaire [14]. The ODI questionnaire evaluated various aspects of low back pain, including pain level, ability to perform daily activities, mobility, and engagement in social and sexual activities. Each dimension of the ODI questionnaire was scored on a 6-point scale, ranging from 0 (no pain) to 5 (extremely painful). The score was calculated as (actual score/50) × 100%. In this study, a score greater than 60 indicated the presence of OLBP, with higher scores indicating more severe low back pain. The Cronbach’s α of ODI was 0.78.
For the collection of general information, the following aspects were collected: gender, age, body mass index (BMI), years of employment, positions, education, title, marital status, fertility status, frequency of night shift, weight lifted per instance (>10 kg), daily standing hours at work (>5 h), frequency of bending (>10 times), working pressure, experience with low back protection training, and frequency of waist exercise.
Survey methods
Using our hospital’s staff information inquiry system, three trained investigators initially screened the research subjects who met the inclusion and exclusion criteria. They then contacted these individuals by telephone to inform them about the purpose and process of the study. Finally, an electronic questionnaire was distributed through WeChat to the medical workers who voluntarily participated in the study. A total of 120 questionnaires were distributed, out of which 111 were collected. Thirteen questionnaires were deemed invalid due to incomplete information or identical options and were excluded through manual screening. Ultimately, 98 valid questionnaires were obtained, resulting in a questionnaire recovery rate of 92.50% and an effective questionnaire rate of 88.29%.
Statistical analysis
The SPSS 25.0 statistics software was used for data analysis. The measured data were analyzed for normality. Those showing a normal distribution were expressed as mean ± standard deviation, and the t-test was used for group comparisons. Data not conforming to a normal distribution were expressed as median and interquartile range, and the rank sum test was used for group comparisons. Categorical data were expressed as frequency and percentage, and the comparison of groups was analyzed by chi-square test. Multivariate logistic regression analysis was used to explore the factors affecting the occurrence of OLBP in medical workers, and the specific influence of each factor on the occurrence of OLBP was determined according to the odds ratio (OR). P<0.05 was considered a statistical difference.
Result
Status of low back pain in medical workers
In this study, there were 59 male respondents and 39 female respondents, accounting for 60.2% and 39.8% respectively. In terms of job role, there were 31 medical workers (31.63%), 16 medico-technical workers (16.33%), and 51 nursing workers (52.04%). As for their professional titles, 37 held junior titles (37.76%), while 61 held intermediate or senior titles (62.24%). The details are listed in Table 1. Additionally, the ages of the respondents ranged from 20 to 42 years old, and the specific distribution is shown in Figure 1. BMI ranged from 22.32 to 26.87 kg/m2 (Figure 2). Among the 98 medical workers, 68.37% of them were experiencing OLBP (Figure 3).
Table 1.
General characteristics of respondents
| Characteristic | Number | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 59 | 60.20 |
| Female | 39 | 39.80 |
| Years of employment | ||
| >5 | 74 | 75.51 |
| ≤5 | 24 | 24.49 |
| Job role | ||
| Medical | 31 | 31.63 |
| Medical technology | 16 | 16.33 |
| Nursing | 51 | 52.04 |
| Education background | ||
| Bachelor’s degree or higher | 76 | 77.55 |
| Associate degree | 22 | 22.45 |
| Profession title | ||
| Intermediate or senior | 61 | 62.24 |
| Junior | 37 | 37.76 |
| Marital status | ||
| Married | 46 | 46.94 |
| Unmarried | 52 | 53.06 |
| Fertility status | ||
| Already had children | 36 | 36.73 |
| Haven’t had children | 62 | 63.27 |
| Frequency of night shifts (times/month) | ||
| >4 | 29 | 29.59 |
| ≤4 | 69 | 70.41 |
| Weight lifted daily >10 kg | ||
| Yes | 57 | 58.16 |
| No | 41 | 41.84 |
| Daily standing hours at work >5 h | ||
| Yes | 71 | 72.45 |
| No | 27 | 27.55 |
| Daily frequency of bending >10 | ||
| Yes | 86 | 87.76 |
| No | 12 | 12.24 |
| Working pressure | ||
| Very stressful | 63 | 64.29 |
| Moderately stressful or less stressful | 35 | 35.71 |
| Training in lower back protection | ||
| No | 44 | 44.90 |
| Yes | 54 | 55.10 |
| Frequency of waist exercises (times/month) | ||
| ≤4 | 23 | 23.47 |
| >4 | 75 | 76.53 |
Figure 1.
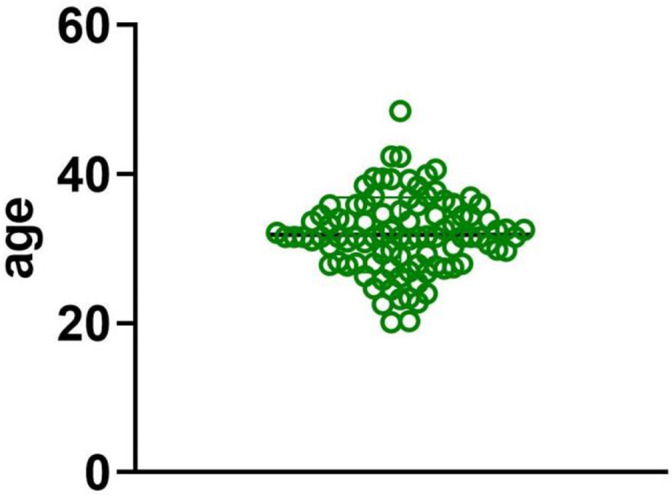
Age distribution of respondents.
Figure 2.
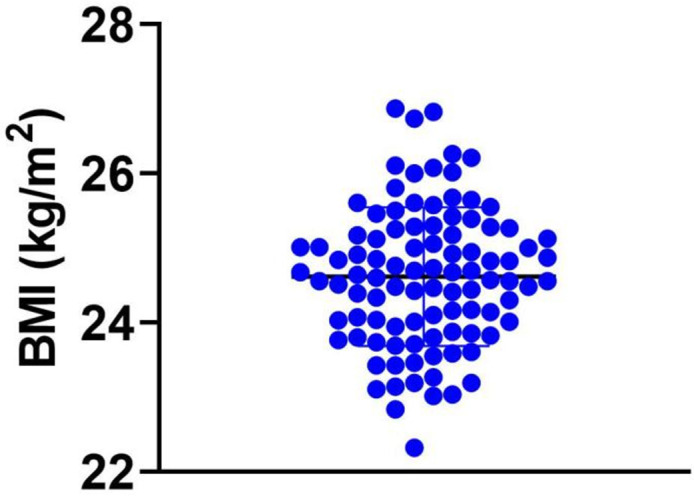
BMI distribution of respondents.
Figure 3.
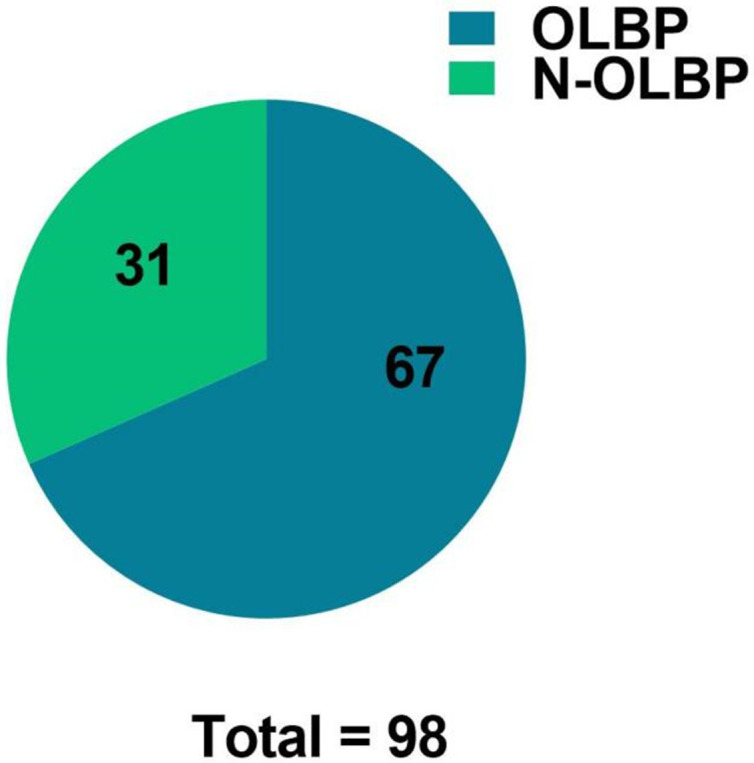
Prevalence of OLBP in respondents.
Univariate analysis of the occurrence of OLBP in medical workers
Results from univariate analysis showed that factors such as BMI, years of employment, job role, frequency of night shift, daily standing hours at work, and training in low back protection were significantly different between medical workers with and without OLBP (Table 2).
Table 2.
Univariate analysis of the occurrence of OLBP in medical workers
| Factor | OLBP Group (n = 67) | N-OLBP Group (n = 31) | χ2/t | P |
|---|---|---|---|---|
| Gender | 3.016 | 0.082 | ||
| Male | 38 (64.41) | 21 (35.59) | ||
| Female | 29 (74.36) | 10 (25.64) | ||
| Age (years old) | 31.56±5.16 | 32.17±5.73 | 0.460 | 0.646 |
| BMI (kg/m2) | 24.83±0.97 | 24.16±0.63 | 2.969 | 0.004 |
| Years of employment | 10.478 | 0.001 | ||
| >5 | 57 (77.03) | 17 (22.97) | ||
| ≤5 | 10 (41.46) | 14 (58.33) | ||
| Job role | 10.590 | 0.005 | ||
| Medical | 15 (48.39) | 16 (51.61) | ||
| Medical technology | 10 (62.50) | 6 (37.50) | ||
| Nursing | 42 (82.35) | 9 (17.65) | ||
| Education background | 1.040 | 0.308 | ||
| Bachelor’s degree or higher level | 50 (65.79) | 26 (34.21) | ||
| Associate degree | 17 (77.27) | 5 (22.73) | ||
| Profession title | 2.181 | 0.140 | ||
| Intermediate or senior | 45 (73.77) | 16 (26.23) | ||
| Junior | 22 (59.46) | 15 (40.54) | ||
| Marital status | 0.456 | 0.500 | ||
| Married | 33 (71.74) | 13 (28.26) | ||
| Unmarried | 34 (65.38) | 18 (34.62) | ||
| Fertility status | 2.330 | 0.127 | ||
| Already had children | 28 (77.78) | 8 (22.22) | ||
| Haven’t had children | 39 (62.90) | 23 (37.10) | ||
| Frequency of night shift (times/month) | 3.944 | 0.047 | ||
| >4 | 24 (82.76) | 5 (17.24) | ||
| ≤4 | 43 (62.32) | 26 (37.68) | ||
| Weight lifted daily >10 kg | 1.064 | 0.302 | ||
| Yes | 41 (71.93) | 16 (28.07) | ||
| No | 26 (63.41) | 15 (36.59) | ||
| Daily standing hours at work >5 h | 4.700 | 0.030 | ||
| Yes | 53 (74.65) | 18 (25.35) | ||
| No | 14 (51.85) | 13 (48.15) | ||
| Daily frequency of bending >10 | 0.637 | 0.425 | ||
| Yes | 60 (69.77) | 26 (30.23) | ||
| No | 7 (58.33) | 5 (41.67) | ||
| Working pressure | 0.764 | 0.382 | ||
| Very stressful | 45 (71.43) | 18 (28.57) | ||
| Moderately stressful or less stressful | 22 (62.86) | 13 (37.14) | ||
| Training in lower back protection | 4.614 | 0.032 | ||
| No | 35 (79.55) | 9 (20.45) | ||
| Yes | 32 (59.26) | 22 (40.74) | ||
| Frequency of waist exercises (times/month) | 1.360 | 0.243 | ||
| ≤4 | 18 (78.26) | 5 (21.74) | ||
| >4 | 49 (65.33) | 26 (34.67) |
Multivariate analysis
The indicators with significant differences in the univariate analysis were used as independent variables, while the occurrence of OLBP among medical workers was used as the dependent variable. A multivariate logistic regression analysis was conducted, with the assignment of each variable shown in Table 3. The Results indicated that employment for over 5 years, holding a nursing position and lack of training in low back protection were risk factors for OLBP in medical workers (all P<0.05, see Table 4).
Table 3.
Assignment of each variable
| Variable | Assignment |
|---|---|
| Dependent variables | |
| Occurrence of OLBP | 1 = “OLBP”, 0 = “No OLBP” |
| Independent variables | |
| BMI | Actual value entered |
| Years of employment | 1 = “>5 years”, 0 = “≤5 years” |
| Position | 1 = “nursing”, 0 = “medical or medical technology” |
| Frequency of night shift | 1 = “>4 times/month”, 0 = “≤4 times/month” |
| Standing hours at work | 1 = “>5 h/d”, 0 = “≤5 h/d” |
| Training in low back protection | 1 = “No”, 0 = “Yes” |
Table 4.
Multivariate analysis
| Variable | B | SE | Wald χ2 | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| BMI | 0.050 | 0.026 | 3.648 | 0.056 | 1.051 | 0.999-1.106 |
| Years of employment >5 | 0.118 | 0.021 | 32.893 | 0.000 | 1.125 | 1.081-1.171 |
| Nursing position | 1.387 | 0.460 | 9.090 | 0.003 | 4.001 | 1.625-9.855 |
| Frequency of night shift >4 times/month | 0.280 | 0.474 | 0.350 | 0.554 | 1.324 | 0.523-3.352 |
| Standing hours at work >5 h/d | 0.530 | 0.469 | 1.277 | 0.258 | 1.699 | 0.678-4.258 |
| Without training in low back protection | 1.687 | 0.499 | 11.448 | 0.001 | 5.404 | 2.034-14.358 |
| Constant | -30.457 | 4.731 | 41.446 | 0.000 | - | - |
Discussion
Occupational low back pain (OLBP) is a significant health concern for medical workers. In a specialized survey conducted by Alshahrani [15], it was shown that over 74% of nursing workers experienced some level of low back pain (LBP). Alshahran called for relevant departments to develop policies for intervention. Yokota [16] conducted a large sample study and found that the prevalence of OLBP among nursing workers was 64.6%, with most cases being acute OLBP, significantly affecting their work quality. Gilchrist [17] investigated the prevalence of LBP among 569 nursing workers and found that 84.7% of respondents experienced LBP. In our study, 98 medical workers from our hospital participated in the questionnaire, revealing that 68.37% of medical workers reported experiencing OLBP. This percentage was slightly higher than Yokota’s survey results but lower than the results of Alshahrani and Gilchrist. Despite variations in results, our study underscores the persistent high prevalence of OLBP among medical workers. This suggests that both medical workers and hospital administrators should pay more attention to this issue. Discrepancies in findings may be attributed to factors such as the grade and type of hospital, as well as racial differences among the study subjects.
Following multivariate analysis, this study concluded that the occurrence of OLBP among medical workers is influenced by their job role, years of employment and participation in training. Nursing workers were found to have the highest risk of OLBP, followed by medico-technical workers. Nursing roles entail a wide range of duties, including manual patient handling, assisting with daily patient care, performing medical procedures like venous transfusion, collecting arteriovenous blood samples, suctioning sputum, and other activities that involve frequent bending, which increases the risk of OLBP in nursing staffs compared to workers in other positions [18-20]. Medical workers with more than 5 years of experience are four times more likely to develop OLBP than those with less than five years of experience. Long-term and repetitive lifting of heavy objects can lead to chronic musculoskeletal injuries. The risk of OLBP in medical workers increases with the number of years of employment [21,22]. Lack of training and experience in dealing with low back pain is a risk factor for the development of OLBP in medical workers. Due to their heavy workload, most medical workers experience varying degrees of low back pain. Without appropriate intervention, this pain is likely to progress to OLBP. Adequate training enables medical workers to effectively address muscle spasms and improve low back muscle function, thus reducing the prevalence of OLBP [23-26]. To enhance the awareness of self-protection against OLBP among medical workers, relevant management departments should implement standardized, systematic, and targeted OLBP protection courses as part of school education, pre-job training and continuing education.
Limitations and prospects
It is important to note that the duration of OLBP was not analyzed in this study, which is a limitation of retrospective studies. The duration of OLBP may have an impact on pain severity, dysfunction, treatment outcome, and its effect on work. Future studies should consider including the duration of OLBP as a variable to comprehensively assess contributing factors and offer more precise recommendations for prevention and treatment in clinical settings.
The sample size of this study was small, and it was conducted at a single center. Future research endeavors should aim to collaborate with multiple institutions to conduct large-sample, multi-center randomized studies. This will help identify more relevant factors that influence the occurrence of OLBP among medical workers. Additionally, some of the observation indicators in this study were subjective, suggesting the need for introducing diagnostic and treatment equipment to provide more scientific and objective observation indicators. Furthermore, relevant follow-up should be conducted based on evidence-based medicine, in subsequent studies.
Conclusion
We investigated the current status of OLBP among medical workers in our hospital. We found that the prevalence of OLBP among medical workers in our hospital is relatively high, underscoring the importance for both medical staff and hospital administrators to recognize and address this issue. After further analysis of the factors that contribute to OLBP in medical workers, we concluded that the occurrence of OLBP is influenced by various factors, including years of employment, job role, and relevant training. Therefore, there is a pressing need for comprehensive preventive measures targeting individual characteristics, job role, occupational exposure, and environmental management within hospitals.
Disclosure of conflict of interest
None.
References
- 1.Gerding T, Syck M, Daniel D, Naylor J, Kotowski SE, Gillespie GL, Freeman AM, Huston TR, Davis KG. An assessment of ergonomic issues in the home offices of university employees sent home due to the COVID-19 pandemic. Work. 2021;68:981–992. doi: 10.3233/WOR-205294. [DOI] [PubMed] [Google Scholar]
- 2.Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J, Pransky G, Sieper J, Smeets RJ, Underwood M Lancet Low Back Pain Series Working Group. What low back pain is and why we need to pay attention. Lancet. 2018;391:2356–2367. doi: 10.1016/S0140-6736(18)30480-X. [DOI] [PubMed] [Google Scholar]
- 3.Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM, Koes BW, Peul W, Turner JA, Maher CG Lancet Low Back Pain Series Working Group. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391:2368–2383. doi: 10.1016/S0140-6736(18)30489-6. [DOI] [PubMed] [Google Scholar]
- 4.Bento TPF, Genebra CVDS, Maciel NM, Cornelio GP, Simeao SFAP, Vitta A. Low back pain and some associated factors: is there any difference between genders? Braz J Phys Ther. 2020;24:79–87. doi: 10.1016/j.bjpt.2019.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fatoye F, Gebrye T, Odeyemi I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol Int. 2019;39:619–626. doi: 10.1007/s00296-019-04273-0. [DOI] [PubMed] [Google Scholar]
- 6.Hayden JA, Wilson MN, Riley RD, Iles R, Pincus T, Ogilvie R. Individual recovery expectations and prognosis of outcomes in non-specific low back pain: prognostic factor review. Cochrane Database Syst Rev. 2019;2019:CD011284. doi: 10.1002/14651858.CD011284.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aleku M, Nelson K, Abio A, Lowery Wilson M, Lule H. Lower back pain as an occupational hazard among Ugandan health workers. Front Public Health. 2021;9:761765. doi: 10.3389/fpubh.2021.761765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bontrup C, Taylor WR, Fliesser M, Visscher R, Green T, Wippert PM, Zemp R. Low back pain and its relationship with sitting behaviour among sedentary office workers. Appl Ergon. 2019;81:102894. doi: 10.1016/j.apergo.2019.102894. [DOI] [PubMed] [Google Scholar]
- 9.Malinska M, Bugajska J, Bartuzi P. Occupational and non-occupational risk factors for neck and lower back pain among computer workers: a cross-sectional study. Int J Occup Saf Ergon. 2021;27:1108–1115. doi: 10.1080/10803548.2021.1899650. [DOI] [PubMed] [Google Scholar]
- 10.Souza NVDO, Carvalho EC, Soares SSS, Varella TCMYML, Pereira SRM, Andrade KBS. Nursing work in the COVID-19 pandemic and repercussions for workers’ mental health. Rev Gaucha Enferm. 2021;42:e20200225. doi: 10.1590/1983-1447.2021.20200225. [DOI] [PubMed] [Google Scholar]
- 11.Van Hoof W, O’Sullivan K, O’Keeffe M, Verschueren S, O’Sullivan P, Dankaerts W. The efficacy of interventions for low back pain in nurses: a systematic review. Int J Nurs Stud. 2018;77:222–231. doi: 10.1016/j.ijnurstu.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 12.Celik S, Celik K, Dirimese E, Tasdemir N, Arik T, Buyukkara I. Determination of pain in musculoskeletal system reported by office workers and the pain risk factors. Int J Occup Med Environ Health. 2018;31:91–111. doi: 10.13075/ijomeh.1896.00901. [DOI] [PubMed] [Google Scholar]
- 13.Yoshimoto T, Oka H, Ochiai H, Ishikawa S, Kokaze A, Muranaga S, Matsudaira K. Presenteeism and associated factors among nursing personnel with low back pain: a cross-sectional study. J Pain Res. 2020;13:2979–2986. doi: 10.2147/JPR.S269529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee CP, Fu TS, Liu CY, Hung CI. Psychometric evaluation of the Oswestry disability index in patients with chronic low back pain: factor and Mokken analyses. Health Qual Life Outcomes. 2017;15:192. doi: 10.1186/s12955-017-0768-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alshahrani A. Prevalence of low back pain among nursing staff in Najran, Saudi Arabia: a cross-sectional study. Med Sci (Basel) 2020;8:45. doi: 10.3390/medsci8040045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yokota J, Fukutani N, Nin K, Yamanaka H, Yasuda M, Tashiro Y, Matsushita T, Suzuki Y, Yokota I, Teramukai S, Aoyama T. Association of low back pain with presenteeism in hospital nursing staff. J Occup Health. 2019;61:219–226. doi: 10.1002/1348-9585.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gilchrist A, Pokorna A. Prevalence of musculoskeletal low back pain among registered nurses: results of an online survey. J Clin Nurs. 2021;30:1675–1683. doi: 10.1111/jocn.15722. [DOI] [PubMed] [Google Scholar]
- 18.Citko A, Gorski S, Marcinowicz L, Gorska A. Sedentary lifestyle and nonspecific low back pain in medical personnel in north-east poland. Biomed Res Int. 2018;2018:1965807. doi: 10.1155/2018/1965807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yoshimoto T, Oka H, Ishikawa S, Kokaze A, Muranaga S, Matsudaira K. Factors associated with disabling low back pain among nursing personnel at a medical centre in Japan: a comparative cross-sectional survey. BMJ Open. 2019;9:e032297. doi: 10.1136/bmjopen-2019-032297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kazemi SS, Tavafian SS, Hiller CE, Hidarnia A, Montazeri A. The effectiveness of social media and in-person interventions for low back pain conditions in nursing personnel (SMILE) Nurs Open. 2021;8:1220–1231. doi: 10.1002/nop2.738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin YP, Su YH, Chin SF, Chou YC, Chia WT. Light-emitting diode photobiomodulation therapy for non-specific low back pain in working nurses: a single-center, double-blind, prospective, randomized controlled trial. Medicine (Baltimore) 2020;99:e21611. doi: 10.1097/MD.0000000000021611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skela-Savic B, Pesjak K, Hvalic-Touzery S. Low back pain among nurses in Slovenian hospitals: cross-sectional study. Int Nurs Rev. 2017;64:544–551. doi: 10.1111/inr.12376. [DOI] [PubMed] [Google Scholar]
- 23.Mijena GF, Geda B, Dheresa M, Fage SG. Low back pain among nurses working at public hospitals in Eastern Ethiopia. J Pain Res. 2020;13:1349–1357. doi: 10.2147/JPR.S255254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.d’Ettorre G, Vullo A, Pellicani V, Ceccarelli G. Acute low back pain among registered nurses. Organizational implications for practice management. Ann Ig. 2018;30:482–489. doi: 10.7416/ai.2018.2248. [DOI] [PubMed] [Google Scholar]
- 25.Latina R, Petruzzo A, Vignally P, Cattaruzza MS, Vetri Buratti C, Mitello L, Giannarelli D, D’Angelo D. The prevalence of musculoskeletal disorders and low back pain among Italian nurses: an observational study. Acta Biomed. 2020;91:e2020003. doi: 10.23750/abm.v91i12-S.10306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Dillen LR, Lanier VM, Steger-May K, Wallendorf M, Norton BJ, Civello JM, Czuppon SL, Francois SJ, Roles K, Lang CE. Effect of motor skill training in functional activities vs strength and flexibility exercise on function in people with chronic low back pain: a randomized clinical trial. JAMA Neurol. 2021;78:385–395. doi: 10.1001/jamaneurol.2020.4821. [DOI] [PMC free article] [PubMed] [Google Scholar]


