Abstract
Sickle-cell Disease (SCD) is a major public health problem in Africa, and there are significant obstacles to its comprehensive management, particularly in terms of access to appropriate healthcare. This calls for inventive approaches to improve patients' prospects. Among the major challenges to be met are the primary and secondary prevention of certain serious complications associated with the disease, such as neurocognitive, motor and respiratory functional disorders. This perspective argues for the rapid creation of specific, cost-effective, technology-supported rehabilitation centres to advance SCD care, identify patients at high risk of stroke and implement tailored rehabilitation strategies. The TechnoRehabLab in Lubumbashi illustrates this shift in thinking by using cutting-edge technologies such as virtual reality (VR), serious games and mobile health to create a comprehensive and easily accessible rehabilitation framework. Diagnostic tools used to perform functional assessment can be used to identify cognitive, balance and walking deficits respectively. Transcranial Doppler enables early detection of sickle cell cerebral vasculopathy, making it possible to provide early and appropriate treatment. VR technology and serious games enable effective rehabilitation and cognitive stimulation, which is particularly advantageous for remote or community-based rehabilitation. In the context of African countries where there is a glaring disparity in access to digital resources, the TechnoRehabLab serves as a tangible example, demonstrating the flexibility and accessibility of technology-assisted rehabilitation. This perspective is an urgent call to governments, non-governmental organisations and the international community to allocate resources to the replication and expansion of similar facilities across Africa.
Keywords: sickle cell disorders, rehabilitation, technology-supported, rehabilomics, virtual reality, serious games
1. Introduction
Sickle cell disease (SCD) is associated with severe morbidity, particularly due to acute and chronic complications affecting several organs (1). Some of these complications are disabling, such as stroke and osteoarticular damage (2, 3), and increase the social and financial burden of the disease (4). It is estimated that 8.3% of patients with SCD will suffer a stroke at a young age (5). Ultimately, these patients suffer motor and cognitive sequelae leading to severe disability. SCD is also associated with aseptic necrosis of the femoral heads, leading to complications of the musculoskeletal system that may ultimately necessitate the fitting of prostheses (6). Improving this morbidity depends above all on preventive measures, the primum movens of which is early detection of the disease, which ensures appropriate treatment before the first complications arise. Prevention of infection and measures to promote a healthy lifestyle have improved the life expectancy of patients. These measures have been complemented by therapeutic advances, in particular the use of hydroxyurea, chronic transfusions with the possibility of oral iron chelation, and the use of erythrocytapheresis, bone marrow transplants and, more recently, gene therapy, although this is not yet available in current practice. Despite disparities in access to care, which tend to disadvantage certain social groups, particularly in the US (4), These therapeutic advances are widely available in developed and some emerging countries, but are not yet well implemented in Sub-Saharan Africa, where the majority of people with SCD live (7, 8). This is due to non-existent or unsuitable infrastructures, the fact that funding for health services is essentially dependent on direct out-of-pocket payments and external partners who have other priorities than SCD, and the inadequacy or non-existence of diagnostic services (9). However, over the last two decades there have been several initiatives that have led to an improvement in the provision of care for sickle cell patients. In Nigeria and Tanzania, haematopoietic stem cell transplantation units are operational to offer patients the possibility of curative treatment at an affordable cost to stem the burden of the disease, the cumulative cost of non-curative treatments of which is enormous in this context of scarce resources (10–12) and Ethiopia plans to have it by 2029 (13). These ambitious initiatives are certainly commendable, but they would not immediately apply to the largest number of sickle cell patients in Sub-Saharan Africa. The challenges remain enormous. And even in developed and emerging countries, not all sickle cell patients benefit from bone marrow transplantation. The most significant advances are to be found in the emergence of specialised centres or services in certain major cities in different countries. From Bamako to Dar-es-Salam, via Dakar, Brazzaville, Bangui, etc., the most significant advances are found in the emergence of specialised centres or services. These centres, together with the introduction of various university diplomas aimed at improving the knowledge and skills of healthcare professionals in the field of SCD, are vectors for improving the survival and quality of life of people with these patients (14). In the Democratic Republic of Congo, the first structure dedicated to SCD was created in 1974 within the National Research and Development Office. This structure was subsequently placed under the administrative supervision of the Institut de Recherche en Sciences de la Santé, whose mission is to provide services and training to find solutions to priority health problems, in particular SCD, malnutrition, malaria, and HIV/AIDS. It organizes the care of sickle cell patients at the Centre de Médecine Mixte et d'Anémie SS in Kinshasa and at the Centre de Référence de la Drépanocytose de Lubumbashi in its provincial branch. However, the diagnostic and therapeutic challenges to making a real impact on the course of SCD disease in Sub-Saharan Africa remain enormous.
Among the many challenges facing the Lubumbashi Sickle Cell Reference Center was identifying patients at risk of stroke and those with cognitive impairment. Additionally, there was a need to promptly establish rehabilitation services for individuals facing motor deficits post-stroke or aseptic necrosis of the femoral head, particularly after undergoing surgical drilling treatment. To address these challenges and enhance patient-centered care, the Institute forged a partnership with REVAL of Hasselt University, leading to the establishment of the TechnoRehabLab in Lubumbashi. This program outlines a north-south initiative aimed at enhancing services provided to SCD patients by implementing best practices that enhance care quality, mitigate treatment expenses, and ultimately improve patient well-being.
2. SCD rehabilitation dynamics in Africa
The complexities associated with tackling SCD in the African environment manifest as an intricate and varied task. The burden of SCD is worsened throughout the continent due to a combination of variables, such as inadequate availability of rehabilitative services, scarcity of resources, and the lack of specific therapies. But there is also a lack of guidelines and recommendations about the need of rehabilitation services for patients with SCD in the official recommendation of the Lancet Haematology Commission (15). Rehabilitation, physiotherapy, or physical medicine were hardly mentioned in this report. This omission is of particular concern, especially when considering the recent focus of WHO on global rehabilitation services and the prioritized management of disabilities within the health-care domain. This effort is highlighted in the establishment of the World Rehabilitation Alliance, aimed at addressing the escalating global need for comprehensive rehabilitation solutions (16). Unfortunately, this crucial component is notably absent from the Commission's recommendations despite its significance for patients (17).
The urgent necessity for efficient rehabilitation interventions is further emphasized by the increased occurrence of stroke among patients dealing with SCD, intensifying the need for a reevaluated and all-encompassing healthcare approach (18).
The lack of access to rehabilitation treatments in numerous African countries is evident (16), resulting in a significant gap between the requirements of individuals with SCD and the existing healthcare infrastructure (19). The limited availability of resources exacerbates the difficulties, leading to a healthcare environment that is not well prepared to meet the complex requirements presented by SCD (20). Without specific interventions, individuals with SCD are left to navigate a complicated healthcare system that often lacks the necessary specialist support to meet their distinct needs (21).
The high frequency of stroke among individuals with SCD creates an emergency situation, requiring the rapid deployment of appropriate interventions, including early rehabilitation (17, 18). Conventional methods of rehabilitation struggle with obstacles caused by a significant scarcity of healthcare specialists who specialize in SCD care. Furthermore, deficiencies in healthcare infrastructure, worsened by financial limitations, additionally impede the provision of prompt and specific rehabilitation services (22). The current paradigms need a thorough reassessment to tackle these systemic barriers and establish a more comprehensive, flexible, and patient-centered care approach (23).
The necessity for a comprehensive approach is clear, one that not only tackles the urgent medical requirements but also recognizes the socioeconomic issues that underlie the difficulties connected with SCD in Africa (24). In order to improve the treatment of these patients in Africa's healthcare system, it is important to carefully analyze the current obstacles and develop novel solutions. This will help create a more fair and effective approach to SCD management within the complex and highly underfinanced African healthcare environment.
3. The TechnoRehabLab
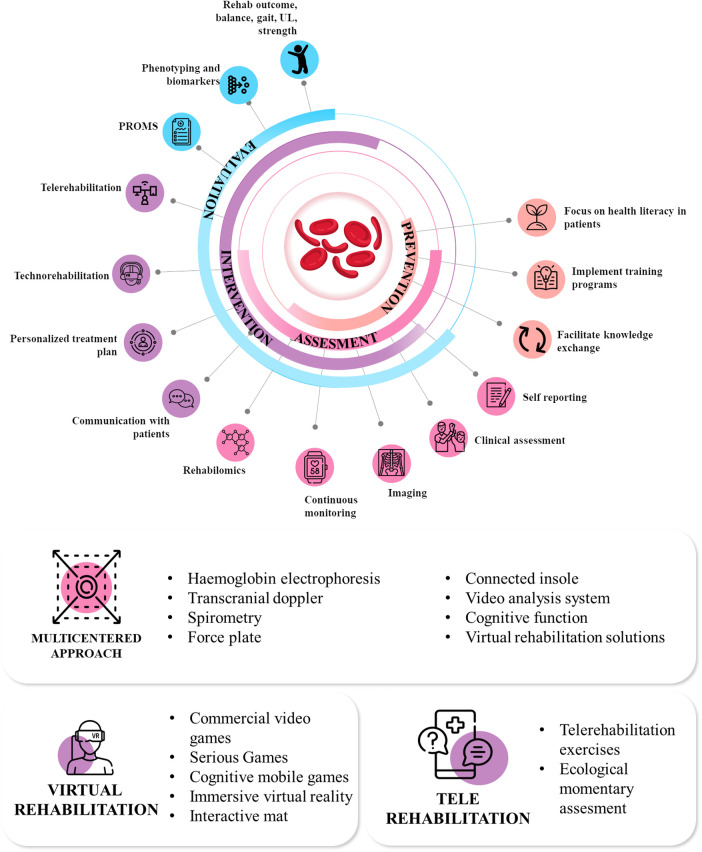
The TechnoRehabLab in Lubumbashi is at the forefront of scientific innovation and practical application, addressing the significant issues associated with managing SCD in the African environment. This advanced facility, opened in November 2023, goes beyond traditional limits, combining technology and rehabilitation approaches to create a comprehensive framework for managing both cognitive and motor impairments of SCD. The TechnoRehabLab combines modern tools such as virtual reality (VR) and mobile technology to provide cost-effective and accessible rehabilitation services to SCD patients. Being highly patients-centred (25) and goal-oriented (26), these services are specifically designed to meet the individual needs of each patient. The technologies and services can be summarized into three key main components, complete list and descriptions of the technologies and service available are presented in Table 1 and summarized in Figure 1.
Table 1.
Description of the technology available in the center.
| Category | Technology | Description | Aim |
|---|---|---|---|
| Virtual rehabilitation | Commercial video games | Commercial video games such as Nintendo Wii, alone or in combination with the Balance Board, the Microsoft Xbox Kinect and the Nintendo Switch has been successfully tested and integrated in the rehabilitation program to increase both motor and cognitive functions (27). |
|
| Serious games | Serious games are video games that have been specifically developed for rehabilitation purposes. They are adapted to the specificity of the rehabilitation process and can be easily configured to each and every patients (28). |
|
|
| Cognitive mobile games | Brain training exercises have been increasingly assimilated into computerized training paradigms, spanning across various platforms including personal computers, gaming consoles, and, more recently, smartphones and tablets (29). This evolution in delivery mechanisms has widened the accessibility and utilization of cognitive training interventions, facilitating their integration into daily routines and enabling a broader demographic to engage in structured cognitive enhancement programs. |
|
|
| Immersive virtual reality | Virtual Reality (VR) is characterized as a sophisticated human-computer interface, facilitating users’ exploration, interaction, and immersion in environments simulating real-world objects and events. This immersive experience is enriched by real-time feedback and augmented sensory inputs, providing users with comprehensive insights into their performance. VR technology encompasses a diverse array of hardware configurations, including computers, mobile device screens, and head-mounted displays, which collectively enable patients to engage in repetitive, intensive, and goal-oriented practice across various levels of immersion within virtual environments (30). |
|
|
| Interactive mat | The interactive mat is a pressure-sensitive rehabilitation mat equipped with sensors. It offers a variety of exercises aimed at improving balance, coordination, muscular strength, and mobility. All exercises can be tailored to the individual needs of patients (31). |
|
|
| Telerehabilitation | Telerehabilitation exercises | Telerehabilitation presents a novel approach to delivering rehabilitation services, offering patients the opportunity to engage in exercises more conveniently from the comfort of their homes. Leveraging information and communication technologies, telerehabilitation fosters seamless communication between healthcare professionals and patients, even when they are in remote locations. This innovative approach not only enhances accessibility to rehabilitation services but also empowers patients to perform exercises with greater ease and consistency, promoting improved outcomes and overall well-being (32). |
|
| Ecological momentary assessment | SEMA (Smartphone Ecological Momentary Assessment) emerges as a solution tailored for the intensive longitudinal evaluation of pain, fatigue, motivation, and other pertinent factors in SCD patients (33). This method allows researchers and clinicians to gain real-time insights into the fluctuating experiences and challenges faced by children with SCD, facilitating tailored interventions and improving overall care strategies. |
|
|
| Multidimensional assessment unit | Transcranial doppler | Transcranial Doppler (TCD) is a rapid and non-invasive diagnostic technique that can provide real-time measurements of the relative changes in cerebral blood velocity (CBV). Therefore, TCD is a useful tool in the diagnosis and treatment of clinical cerebrovascular diseases (CVDs). Specifically, TCD could be applied to evaluate occlusive CVD, assess collateral circulation in patients with ischemic stroke, and monitor cerebral vascular occlusion before and after thrombolysis as well as cerebral vasospasm (VSP) and microembolization signals after aneurysmal subarachnoid hemorrhage (SAH). Moreover, TCD could predict short-term stroke and transient cerebral ischemia in patients with anterior circulation occlusion treated with endovascular therapy and in patients with anterior circulation vascular occlusion (34). |
|
| Haemoglobin electrophoresis | The utilization of a haemoglobin electrophoresis reader presents an invaluable asset in the swift and accurate identification as well as quantification of various haemoglobin types, including but not limited to, Hb A (normal), Hb S (sickle cell), Hb F (fetal), and Hb A2/C/E. This advanced diagnostic tool enables clinicians to promptly discern and measure the relative concentrations of these haemoglobin variants, facilitating comprehensive assessments crucial for precise diagnosis and tailored treatment strategies, particularly in the context of hemoglobinopathies such as sickle cell disease (35). |
|
|
| Spirometry | Spirometry is classically used to diagnose airway diseases in patients with SCD. This is crucial tool given that compromised pulmonary function stands as a primary contributor to the morbidity and mortality rates observed in pediatric SCD cases. By utilizing spirometry, clinicians can effectively evaluate respiratory function, aiding in the early detection and management of respiratory complications (36). |
|
|
| Force plate | Evaluation of both static and dynamic balance under different conditions (i.e., eyes open, closed, stable or unstable surfaces) (37), to monitor the evolution of the patients and offers personalized-rehabilitation exercises. The force plate also has a rehabilitation component offering serious games to improve biofeedback. |
|
|
| Connected insole | Gait analysis is a powerful technique for capturing human locomotion and accurately measure numerous related factors. The ability of this equipment to offer comprehensive insights on gait has made it an essential instrument in both clinical and scientific environments (38). |
|
|
| Video analysis system | The development and evolution of video based analysis (marker less system) supported by artificial intelligence allow to perform simple yet validated functional assessment of the patients (39). |
|
|
| Cognitive function | Fully automated and quantitative evaluation of various cognitive functions such as inspection time, reaction time, impulse control, short term memory, and executive function using tablets (40). The added value of this system is that the evaluations are not impacted by educational level of culture. |
|
|
| Virtual rehabilitation solutions | One of the salient aspects of the new technologies used to support the rehabilitation process is that a lot of data can be collected to monitor the evolution of the patients and to provide them direct feedback. Serious games can be used to assess both motor (41, 42) and cognitive (43) functions. |
|
Figure 1.
The different objectives, level of intervention and technologies available at the center.
3.1. Virtual rehabilitation
The use of new and affordable technologies goes beyond the scope of simple functional rehabilitation; it also introduces a paradigm shift by including an element of cognitive stimulation (44). Current modalities of rehabilitation include both supervised and unsupervised exercises, but advances in technology are opening new horizons in this field such as Virtual Reality (VR), Augmented Reality (AR), gamification, and telerehabilitation (45). This forward-thinking strategy encourages the highest possible level of patient engagement inside the comforting environment of their own homes. The selection of various technologies has been based on our expertise in technology-supported rehabilitation, as well as on different criteria including financial considerations, language support, offline usability, and geographical accessibility for telerehabilitation applications (46).
The TechnoRehabLab accommodates a wide range of rehabilitation requirements through the utilization of a variety of applications. These technologies improve patient compliance and successfully solve issues that are inherent to conventional rehabilitation paradigms (47).
3.2. Telerehabilitation services
Recognizing the existing digital divide, the TechnoRehabLab makes strategic advantage of the widespread use of mobile devices that are within a reasonable price range in Lubumbashi. Mobile health (mHealth) refers to the integration of mobile devices, including mobile phones and patients monitoring devices, into medical and public health practice. This approaches leverages the fundamental capabilities of mobile phones, encompassing short messaging system, as well as advanced technologies (3G, 4G and 5G), global positioning system and Bluetooth (48).
The seamless implementation of at-home training programs is made possible by these apps, which serve as an accessible way of providing telerehabilitation, guarantying the continuity of the care (49). This is especially beneficial for families that do not have access to long-term rehabilitation clinics.
3.3. Multidimensional assessment unit
For the purpose of facilitating the early detection of cerebral vasculopathy (50), the TechnoRehabLab makes use of cutting-edge diagnostic technologies such as transcranial doppler (TCD) (51). In the process of identifying patients who are at an increased risk of having a stroke, this evaluation plays a crucial role in prevention (52).
These diagnostic findings serve therefore as the basis for implementation of early intervention techniques, which may include continuous transfusion programs and therapy with hydroxyurea (53). It is important to note that these measurements are precisely adjusted to the personalized needs of patients, which represents a substantial change from the standard treatments that are designed to be universally applicable and highlights the significance of precision medicine in the management of SCD given the scarcity of resources. Not only does the incorporation of technology at each and every stage guarantee prompt interventions (54), but it also guarantees a more nuanced and individualized treatment trajectory for persons who are attempting to deal with the many issues that are posed by SCD (55).
4. Challenges and opportunities
The TechnoRehabLab, at the intersection of technology and rehabilitation, grapples with unique challenges and promising opportunities to increase both the quality and quantity of rehabilitation services in regions with limited human and financial resources.
4.1. Challenges
The limited accessibility of rehabilitation therapies presents a major obstacle in the management of SCD in Africa (56). This inadequacy worsens the already significant burden of SCD on individuals affected by it (57). The facility established in Lubumbashi has been assigned the critical mission of addressing and resolving this pervasive problem. The organization's mandate extends beyond conventional rehabilitation approaches, requiring innovative measures to effectively tackle the accessibility obstacles encountered by those coping with SCD. Important efforts also need to be done in order to monitor the efficacy of such intervention and to define local evidences supporting this. Therefore in parallel with the clinical training of the personal we are also forming them to research principles in order to collect high quality data and determine which interventions are the most suited for these patients in this particular context.
The center faces a substantial obstacle as a result of the scarcity of financial and infrastructural resources (19). The insufficient resources provide a substantial barrier to the efficient operation and potential growth of the TechnoRehabLab and the development of other centers. The Lab's mission is to address these resource limits, which is an important objective. Efficient strategic planning and innovative solutions are necessary to acquire the necessary resources, guaranteeing the uninterrupted provision of high-quality rehabilitation services. The TechnoRehabLab was established as a commissioned entity within a North-South collaboration. The funds were used towards acquiring necessary equipment and covering operational expenses, so guaranteeing patients unrestricted access to assessment and rehabilitation services without charge. Securing adequate funding is a significant obstacle in ensuring the long-term sustainability of this specialized center and preserving access to its services (58). There are requirements that must be fulfilled in terms of equipment to enhance the technological infrastructure for conventional rehabilitation, as well as in terms of accessibility to healthcare. The last point is particularly significant, as user fees serve as the primary means of funding healthcare in the Democratic Republic of Congo. This hinders the ability of underprivileged patients to receive high-quality healthcare since there is an imbalance in the allocation of resources, resulting in unequal access to care for everyone (59). The primary problem lies in acquiring the necessary resources to fully fund the operational expenses of the center. Currently the center is integrated whithin the Institut de Recherche en Sciences de la Santé, which also manages the Centre de Référence de la Drépanocytose de Lubumbashi. However, it is located in premises that have been generously provided by a partnering hospital.
In order to ensure the long-term viability of its operations, the organization needs a dedicated physical facility that is both feasible and well-suited to fully maximize the services it can provide to patients. This area should provide the necessary conditions for the installation of all essential utilities and guarantee uninterrupted access to electricity and the internet for the daily functioning of the facility. The lab also requires a diverse array of medical supplies and equipment in order to enhance its technical infrastructure and uphold the standard of care and effectiveness offered to patients (see Table 1). Having motivated and trained personnel is crucial for the functioning of the system. This necessitates continuous investment in the remuneration and training of healthcare professional (60). To ensure the long-term sustainability of this project, contact and regular discussions with the local Ministry of Health are underway to integrate these services into the universal health coverage for these patients.
4.2. Opportunities
In the context of managing SCD, the newly developed center plays a crucial role in providing a unique chance to create a comprehensive framework that surpasses conventional methods. By using technology, the lab establishes itself as an essential link in the chain of providing appropriate care for a complete solution that effectively addresses the complex problems associated with SCD.
Another really important aspect is the development of local research expertise in the center. It is indeed of the utmost importance to develop local evidences supporting local interventions. The disparity between the quantity of scientific and clinical researchers in low- and middle-income countries (LMICs) and their significant burden of diseases like sickle cell disease is compounded by the emigration of a substantial portion—up to 70%—of scientists seeking education and employment opportunities abroad (61). However, it's notable that while new technology-supported interventions have been validated primarily in high-income countries (HICs), it remains crucial for clinicians and researchers in LMICs to conduct studies to ascertain the applicability of these findings to their contexts. It is imperative that studies are conducted to assess the viability and effectiveness of these new interventions in LMIC settings. Only through such research can the clinical utility of these interventions be established, thereby paving the way for their reimbursement and widespread implementation (62).
The success of this center makes it a viable model that can be replicated in many places throughout Africa. The lab's exemplary status has the potential to influence not only Lubumbashi but also other regions throughout the continent by encouraging the creation of similar services aimed at resolving the difficulties associated with the management of neurocognitive and motor complications associated with SCD, but these facilities can also be used to provide (neuro)rehabilitation services to other highly prevalent pathologies such as for example stroke (63) and cerebral palsy (64). These can be services operating independently or integrated into the operation of centers dedicated to the management of SCD.
Furthermore, the use of technology in the TechnoRehabLab creates opportunities for groundbreaking rehabilitation methods. By employing, amongst other, VR and mHealth, the lab can provide solutions that are both innovative and patient-centric while still being cost-effective. This strategy is specifically designed to address the distinct situations and difficulties encountered by those coping with SCD. Although the lab faces substantial challenges presented here above, strategic initiatives, collaborative endeavors, and resolute dedication to patient-centered treatment have the potential to convert these obstacles into favorable circumstances. The pressing need for action involves harnessing the potential of technology-supported rehabilitation to transform patients' management in Africa.
This project is an important symbol of constructive progress, mandating the establishment of an effective health financing system that ensures individuals with SCD can access the appropriate care they need without being burdened by excessive costs. This initiative encourages governments, non-governmental organizations (NGOs), and the international community to allocate resources and actively support programs that can have significant and far-reaching impacts. In our case, a consortium of public and private partners is in action. It relies on the institutional and technical support of the Provincial Ministry of Health, which is involved in providing premises for the definitive establishment of the center and in supporting advocacy for the search for funding. The scientific and administrative managers of the Health Research Institute do their utmost to ensure that the project benefits from all the administrative facilities necessary for its optimal functioning and the improvement of the remuneration conditions of the staff assigned to this service. The entire civil society in the fight against SCD in the region is mobilized to support the center in its acceptance in the community and in its efforts to mobilize local and international resources.
5. Conclusion
The TechnoRehabLab in Lubumbashi serves as a clear example of how technology-based rehabilitation can effectively transform the way SCD is managed in limited-resourced environment. Immediate effort is necessary to duplicate and expand such projects throughout the African continent, initiating a significant change in healthcare delivery. It is crucial for governments, NGOs, and the international community to make significant investments in the establishment of economically feasible rehabilitation institutions that utilize technology. This investment is designed to guarantee fair and equal access to high-quality care for those dealing with SCD. At this time, it is necessary to take decisive action as we work towards a future where technology enables effective management of SCD, reduces the impact of stroke, and improves the quality of life for many people throughout the continent.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This work was supported by the VLIR-UOS through the Short Initiative Program (328-SI2022-77969).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
PB: Conceptualization, Writing – original draft, Writing – review & editing. SN: Investigation, Writing – original draft, Writing – review & editing. JP: Conceptualization, Writing – original draft, Writing – review & editing. BB: Conceptualization, Funding acquisition, Project administration, Resources, Writing – original draft, Writing – review & editing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Farooq S, Testai FD. Neurologic complications of sickle cell disease. Curr Neurol Neurosci Rep. (2019) 19:17. 10.1007/s11910-019-0932-0 [DOI] [PubMed] [Google Scholar]
- 2.Colombatti R, Birkegård C, Medici M. Global epidemiology of sickle cell disease: a systematic literature review. HemaSphere. (2022) 6:2085–6. 10.1097/01.HS9.0000851688.00394.f4 [DOI] [Google Scholar]
- 3.Habibi A, Arlet J-B, Stankovic K, Gellen-Dautremer J, Ribeil J-A, Bartolucci P, et al. Recommandations françaises de prise en charge de la drépanocytose de l’adulte: actualisation 2015. Rev Méd Interne. (2015) 36:5S3–84. 10.1016/S0248-8663(15)60002-9 [DOI] [PubMed] [Google Scholar]
- 4.Lee L, Smith-Whitley K, Banks S, Puckrein G. Reducing health care disparities in sickle cell disease: a review. Public Health Rep. (2019) 134:599–607. 10.1177/0033354919881438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ware RE, De Montalembert M, Tshilolo L, Abboud MR. Sickle cell disease. Lancet. (2017) 390:311–23. 10.1016/S0140-6736(17)30193-9 [DOI] [PubMed] [Google Scholar]
- 6.Grosse SD, Odame I, Atrash HK, Amendah DD, Piel FB, Williams TN. Sickle cell disease in Africa: a neglected cause of early childhood mortality. Am J Prev Med. (2011) 41:S398–405. 10.1016/j.amepre.2011.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.GBD 2021 Sickle Cell Disease Collaborators. Global, regional, and national prevalence and mortality burden of sickle cell disease, 2000–2021: a systematic analysis from the global burden of disease study 2021. Lancet Haematol. (2023) 10:e585–99. 10.1016/S2352-3026(23)00118-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Piel FB, Hay SI, Gupta S, Weatherall DJ, Williams TN. Global burden of sickle cell anaemia in children under five, 2010–2050: modelling based on demographics, excess mortality, and interventions. PLoS Med. (2013) 10:e1001484. 10.1371/journal.pmed.1001484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ifeagwu SC, Yang JC, Parkes-Ratanshi R, Brayne C. Health financing for universal health coverage in Sub-Saharan Africa: a systematic review. Glob Health Res Policy. (2021) 6:8. 10.1186/s41256-021-00190-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mtenga J, Orf K, Zheng J, Chamba C, Chuwa H, Luoga F, et al. Haematopoietic stem cell transplantation in Tanzania. Br J Haematol. (2021) 192:17–21. 10.1111/bjh.17106 [DOI] [PubMed] [Google Scholar]
- 11.Isgro A, Paciaroni K, Gaziev J, Sodani P, Gallucci C, Marziali M, et al. Haematopoietic stem cell transplantation in Nigerian sickle cell anaemia children patients. Niger Med J. (2015) 56:175. 10.4103/0300-1652.160355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.John TD, Namazzi R, Chirande L, Tubman VN. Global perspectives on cellular therapy for children with sickle cell disease. Curr Opin Hematol. (2022) 29:275. 10.1097/MOH.0000000000000738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mekonnen S, Farris H. Why and how should Ethiopia establish a stem cell transplant service? A review article. BTT. (2023) 17:33–40. 10.2147/BTT.S401289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diallo DA. La drépanocytose en afrique: problématique, stratégies pour une amélioration de la survie et de la qualité de vie du drépanocytaire. Bull Acad Nat Méd. (2008) 192:1361–73. 10.1016/S0001-4079(19)32686-X [DOI] [PubMed] [Google Scholar]
- 15.The Sickle Cell Disease Commissioners. The lancet haematology commission on sickle cell disease: key recommendations. Lancet Haematol. (2023) 10:e564–7. 10.1016/S2352-3026(23)00154-0 [DOI] [PubMed] [Google Scholar]
- 16.Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the global burden of disease study 2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2021) 396:2006–17. 10.1016/S0140-6736(20)32340-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bonnechère B. Sickle cell disease strategies and priorities. Lancet Haematol. (2023) 10:e793–4. 10.1016/S2352-3026(23)00266-1 [DOI] [PubMed] [Google Scholar]
- 18.Boma PM, Panda J, Ngoy Mande JP, Bonnechère B. Rehabilitation: a key service, yet highly underused, in the management of young patients with sickle cell disease after stroke in DR of Congo. Front Neurol. (2023) 14:1104101. 10.3389/fneur.2023.1104101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amarachukwu CN, Okoronkwo IL, Nweke MC, Ukwuoma MK. Economic burden and catastrophic cost among people living with sickle cell disease, attending a tertiary health institution in south-east zone, Nigeria. PLoS One. (2022) 17:e0272491. 10.1371/journal.pone.0272491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WHO. Fact Sheets: Rehabilitation. (2020). Available online at: https://www.who.int/news-room/fact-sheets/detail/rehabilitation (Accessed January 09, 2024).
- 21.WHO. The World Rehabilitation Alliance. Available online at: https://www.who.int/initiatives/world-rehabilitation-alliance (Accessed January 09, 2024).
- 22.Akinyemi RO, Ovbiagele B, Adeniji OA, Sarfo FS, Abd-Allah F, Adoukonou T, et al. Stroke in Africa: profile, progress, prospects and priorities. Nat Rev Neurol. (2021) 17:634–56. 10.1038/s41582-021-00542-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Louw Q, Dizon J, van Niekerk S-M, Ernstzen D, Grimmer K. Contextualised evidence-based rehabilitation recommendations to optimise function in African people with stroke. In: Louw Q, editor. Collaborative Capacity Development to Complement Stroke Rehabilitation in Africa. Human Functioning, Technology and Health. Cape Town (ZA): AOSIS; (2020). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK574240/ (Accessed August 17, 2023) [PubMed] [Google Scholar]
- 24.Ezenwa MO, Dennis-Antwi JA, Dallas CM, Amarachukwu C, Ezema CI, Yao Y, et al. The crisis of sickle cell disease in Africa from insights into primary prevention in Ghana and Nigeria: notes from the field. J Immigr Minor Health. (2021) 23:871–8. 10.1007/s10903-021-01186-8 [DOI] [PubMed] [Google Scholar]
- 25.Crawford L, Maxwell J, Colquhoun H, Kingsnorth S, Fehlings D, Zarshenas S, et al. Facilitators and barriers to patient-centred goal-setting in rehabilitation: a scoping review. Clin Rehabil. (2022) 36:1694–704. 10.1177/02692155221121006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verschure PFMJ, Páscoa Dos Santos F, Sharma V. Redefining stroke rehabilitation: mobilizing the embodied goal-oriented brain. Curr Opin Neurobiol. (2023) 83:102807. 10.1016/j.conb.2023.102807 [DOI] [PubMed] [Google Scholar]
- 27.Bonnechère B, Jansen B, Omelina L, Van Sint Jan S. The use of commercial video games in rehabilitation: a systematic review. Int J Rehabil Res. (2016) 39:277–90. 10.1097/MRR.0000000000000190 [DOI] [PubMed] [Google Scholar]
- 28.Kushnir A, Kachmar O, Bonnechère B. STASISM: a versatile serious gaming multi-sensor platform for personalized telerehabilitation and telemonitoring. Sensors. (2024) 24:351. 10.3390/s24020351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sagary R, Malim NHAH, Abdullah NL, Mohamad WNAW, Ahmad AL. Impact of Mobile games-aided neurorehabilitation: a systematic literature review. Malays J Med Sci. (2023) 30:29–44. 10.21315/mjms2023.30.6.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bargeri S, Scalea S, Agosta F, Banfi G, Corbetta D, Filippi M, et al. Effectiveness and safety of virtual reality rehabilitation after stroke: an overview of systematic reviews. EClinicalMedicine. (2023) 64:102220. 10.1016/j.eclinm.2023.102220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peng H-T, Tien C-W, Lin P-S, Peng H-Y, Song C-Y. Novel mat exergaming to improve the physical performance, cognitive function, and dual-task walking and decrease the fall risk of community-dwelling older adults. Front Psychol. (2020) 11:1620. 10.3389/fpsyg.2020.01620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laver KE, Adey-Wakeling Z, Crotty M, Lannin NA, George S, Sherrington C. Telerehabilitation services for stroke. Cochrane Database Syst Rev. (2020) 1:CD010255. 10.1002/14651858.CD010255.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jonassaint CR, Parchuri E, O’Brien JA, Lalama CM, Lin J, Badawy SM, et al. Mental health, pain and likelihood of opioid misuse among adults with sickle cell disease. Br J Haematol. (2024) 204(3):1029–38. 10.1111/bjh.19243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wan Y, Teng X, Li S, Yang Y. Application of transcranial Doppler in cerebrovascular diseases. Front Aging Neurosci. (2022) 14:1035086. https://www.frontiersin.org/articles/10.3389/fnagi.2022.1035086 (accessed February 12, 2024) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pecker LH, Lanzkron S. Sickle cell disease. Ann Intern Med. (2021) 174:ITC1–16. 10.7326/AITC202101190 [DOI] [PubMed] [Google Scholar]
- 36.Mondal P, Yirinec A, Midya V, Sankoorikal B-J, Smink G, Khokhar A, et al. Diagnostic value of spirometry vs impulse oscillometry: a comparative study in children with sickle cell disease. Pediatr Pulmonol. (2019) 54:1422–30. 10.1002/ppul.24382 [DOI] [PubMed] [Google Scholar]
- 37.Silva PO, Ferreira AS, Lima CMA, Guimarães FS, Lopes AJ. Balance control is impaired in adults with sickle cell anaemia. Somatosens Mot Res. (2018) 35:109–18. 10.1080/08990220.2018.1481829 [DOI] [PubMed] [Google Scholar]
- 38.Loukovitis A, Ziagkas E, Zekakos DX, Petrelis A, Grouios G. Test-Retest reliability of PODOSmart® gait analysis insoles. Sensors (Basel). (2021) 21:7532. 10.3390/s21227532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hellsten T, Karlsson J, Shamsuzzaman M, Pulkkis G. The potential of computer vision-based marker-less human motion analysis for rehabilitation. Rehabil Process Outcome. (2021) 10:11795727211022330. 10.1177/11795727211022330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.VanRavenhorst-Bell HA, Muzeau MA, Luinstra L, Goering J, Amick RZ. Accuracy of the SWAY mobile cognitive assessment application. Int J Sports Phys Ther. (2021) 16:991–1000. 10.26603/001c.24924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bonnechère B, Sholukha V, Omelina L, Van Vooren M, Jansen B, Van Sint Jan S. Suitability of functional evaluation embedded in serious game rehabilitation exercises to assess motor development across lifespan. Gait Posture. (2017) 57:35–9. 10.1016/j.gaitpost.2017.05.025 [DOI] [PubMed] [Google Scholar]
- 42.Bonnechère B, Jansen B, Haack I, Omelina L, Feipel V, Van Sint Jan S, et al. Automated functional upper limb evaluation of patients with Friedreich ataxia using serious games rehabilitation exercises. J Neuroeng Rehabil. (2018) 15:87. 10.1186/s12984-018-0430-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bonnechère B. Evaluation of processing speed of different cognitive functions across the life span using cognitive Mobile games. Games Health J. (2022) 11:132–40. 10.1089/g4h.2021.0144 [DOI] [PubMed] [Google Scholar]
- 44.Zhang X, Xu F, Shi H, Liu R, Wan X. Effects of dual-task training on gait and balance in stroke patients: a meta-analysis. Clin Rehabil. (2022) 36:1186–98. 10.1177/02692155221097033 [DOI] [PubMed] [Google Scholar]
- 45.Berton A, Longo UG, Candela V, Fioravanti S, Giannone L, Arcangeli V, et al. Virtual reality, augmented reality, gamification, and telerehabilitation: psychological impact on orthopedic patients’ rehabilitation. J Clin Med. (2020) 9:E2567. 10.3390/jcm9082567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mitchaï PM, Mapinduzi J, Verbrugghe J, Michiels S, Janssens L, Kossi O, et al. Mobile technologies for rehabilitation in non-specific spinal disorders: a systematic review of the efficacy and potential for implementation in low- and middle-income countries. Eur Spine J. (2023) 32:4077–100. 10.1007/s00586-023-07964-2 [DOI] [PubMed] [Google Scholar]
- 47.Bonnechère B, Van Vooren M, Jansen B, Van Sint JS, Rahmoun M, Fourtassi M. Patients’ acceptance of the use of serious games in physical rehabilitation in Morocco. Games Health J. (2017) 6:290–4. 10.1089/g4h.2017.0008 [DOI] [PubMed] [Google Scholar]
- 48.WHO. mHealth: New Horizons for Health Through Mobile Technologies. Global Observatory for eHealth Series. (2011). Available online at: https://www.who.int/goe/publications/goe_mhealth_web.pdf (Accessed February 02, 2024).
- 49.Bonnechère B, Kossi O, Mapinduzi J, Panda J, Rintala A, Guidetti S, et al. Mobile health solutions: an opportunity for rehabilitation in low- and middle income countries? Front Public Health. (2022) 10:1072322. 10.3389/fpubh.2022.1072322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Boma P, Kaponda A, Panda J, Bonnechere B. Enhancing the management of pediatric sickle cell disease by integrating functional evaluation to mitigate the burden of vaso-occlusive crises. J Vasc Dis. (2024) 105:102828. 10.1016/j.bcmd.2024.102828 [DOI] [Google Scholar]
- 51.Crow A. Transcranial Doppler in children with sickle cell disease: five years of screening experience. Australas J Ultrasound Med. (2020) 23:39–46. 10.1002/ajum.12192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.DeBaun MR, Jordan LC, King AA, Schatz J, Vichinsky E, Fox CK, et al. American society of hematology 2020 guidelines for sickle cell disease: prevention, diagnosis, and treatment of cerebrovascular disease in children and adults. Blood Adv. (2020) 4:1554–88. 10.1182/bloodadvances.2019001142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rankine-Mullings AE, Nevitt SJ. Hydroxyurea (hydroxycarbamide) for sickle cell disease. Cochrane Database Syst Rev. (2022) 9:CD002202. 10.1002/14651858.CD002202.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bonnechère B, Timmermans A, Michiels S. Current technology developments can improve the quality of research and level of evidence for rehabilitation interventions: a narrative review. Sensors (Basel). (2023) 23:875. 10.3390/s23020875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brandow AM, Liem RI. Advances in the diagnosis and treatment of sickle cell disease. J Hematol Oncol. (2022) 15:20. 10.1186/s13045-022-01237-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kpadonou GT, Fiossi-Kpadonou E, Alagnidé E, Bagre F, Rahimy MC. Problems of rehabilitation in patients with sickle cell disease in Cotonou, Benin. Med Trop (Mars). (2011) 71:558–61. [PubMed] [Google Scholar]
- 57.Merlet AN, Chatel B, Hourdé C, Ravelojaona M, Bendahan D, Féasson L, et al. How sickle cell disease impairs skeletal muscle function: implications in daily life. Med Sci Sports Exerc. (2019) 51:4–11. 10.1249/MSS.0000000000001757 [DOI] [PubMed] [Google Scholar]
- 58.Mayhew SH, Doherty J, Pitayarangsarit S. Developing health systems research capacities through north-south partnership: an evaluation of collaboration with South Africa and Thailand. Health Res Policy Syst. (2008) 6:8. 10.1186/1478-4505-6-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Norheim OF. Ethical priority setting for universal health coverage: challenges in deciding upon fair distribution of health services. BMC Med. (2016) 14:75. 10.1186/s12916-016-0624-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bonnechère B, Kossi O, Adoukonou T, Coninx K, Spooren A, Feys P. Improving public health through the development of local scientific capacity and training in rehabilitation in LMICs: a proof-of-concept of collaborative efforts in Parakou, Benin. Front Public Health. (2022) 10:952727. 10.3389/fpubh.2022.952727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pillai G, Chibale K, Constable EC, Keller AN, Gutierrez MM, Mirza F, et al. The next generation scientist program: capacity-building for future scientific leaders in low- and middle-income countries. BMC Med Educ. (2018) 18:233. 10.1186/s12909-018-1331-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Essén A, Stern AD, Haase CB, Car J, Greaves F, Paparova D, et al. Health app policy: international comparison of nine countries’ approaches. NPJ Digit Med. (2022) 5:31. 10.1038/s41746-022-00573-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Okekunle AP, Jones S, Adeniji O, Watkins C, Hackett M, Di Tanna GL, et al. Stroke in Africa: a systematic review and meta-analysis of the incidence and case-fatality rates. Int J Stroke. (2023) 18:634–44. 10.1177/17474930221147164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Donald KA, Kakooza AM, Wammanda RD, Mallewa M, Samia P, Babakir H, et al. Pediatric cerebral palsy in Africa: where are we? J Child Neurol. (2015) 30:963–71. 10.1177/0883073814549245 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.