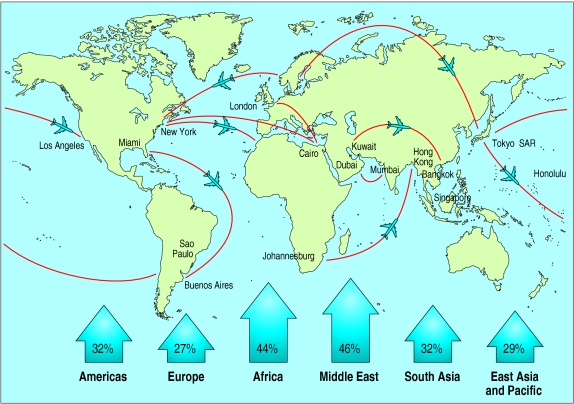
Travel medicine is an exciting interdisciplinary specialty that has developed rapidly in response to the needs of the travelling population worldwide. International arrivals worldwide by any form of transport were around 664 million in 2000 (fig 1), and the World Tourist Organisation has predicted an 80% increase in travel to long haul destinations between 1995 and 2010.1,2 Specialists in travel medicine consider diverse aspects of travel related health, including fitness to travel and the health risks of travelling in itself, as well as the implications of exposure to a variety of infectious diseases. This review highlights current topical issues in this evolving specialty.
Figure 1.
Percentage increase in international arrivals between 1993 and 19973
Sources and search criteria
This article is based on information from several sources, including a review of the literature obtained from the PubMed database, clinical experience, and textbooks on the subject of travel medicine.
The development of travel medicine as a distinct discipline
The development of travel medicine as a discipline is a recent advance in itself.4 This has been recognised in the United Kingdom by the Department of Health in its new strategy for combating infectious disease, which confirms the need for specialists in travel medicine.5
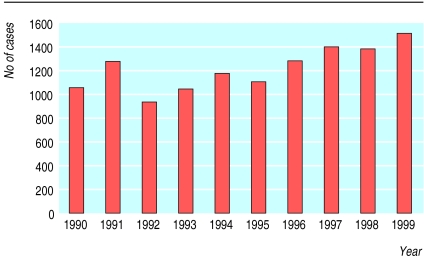
An important organisational development has been the establishment of dedicated specialist travel health clinics in teaching hospitals and primary care (in addition to clinics operated by independent commercial groups). These provide individual pretravel risk assessments (box B1) and should improve services for patients, many of whom seldom seek health advice before travel.6 The importance of providing services for patients is increasingly being recognised in relation to an increased incidence of travel related disease (box B2) and importation of infection (fig 2).7
Recent developments
Travel medicine is developing as a new specialty providing specialist travel services to meet the health needs of vastly increasing numbers of travellers
A pretravel risk assessment allows travel health related risk factors to be identified
The public health implications of the growing number of refugees and migrants from less developed to developed countries need to be fully assessed, and appropriate services need to be provided
Vector borne diseases, in particular malaria, remain an important health risk
The appropriate use of malaria standby treatment may become an option for experienced travellers
New combination vaccines that can be administered by an accelerated schedule are a welcome advance in combating infectious disease
Assessment of fitness to fly and awareness of the possible physiological and psychological impacts of air travel should be considered
Box 1.
Pretravel risk assessment
- Detailed itinerary:
- Countries and regions
- Urban, rural, or jungle
- Purpose of travel
- Mode of travel
- Type of accommodation
- Duration of stay and travel
- Consider:
- Special activities
- Special needs
- Special high risks
- Previous travel
- Available medical facilities
- Detailed medical history
- Concurrent medications
- Personal immunisation history
- Appropriate immunisations and malaria prophylaxis
Box 2.
Key travel related health problems
- Travellers' diarrhoea
- Malaria
- Respiratory tract infections
- Hepatitis A and B
- Skin infections
- Sexually transmitted infections
Figure 2.
Cases of falciparum malaria in the United Kingdom, 1990-95
The International Society of Travel Medicine and the British Travel Health Association (UK) provide information and support to health professionals who are offering travel advisory services to patients. Information from the International Society of Travel Medicine is available on the internet and includes a comprehensive and international listing of travel medicine specialists and travel health clinics. Guidelines and information relating to the discipline of travel medicine are also available from the World Health Organization, the Department of Health, and the Centers for Disease Control and Prevention, as well as from the recently formed European Travel Health Advisory Board (see additional educational resources).8
Training in the discipline is available both nationally and internationally through certification, diploma, or masters degrees (see bmj.com). A new initiative from the International Society of Travel Medicine includes a certificate in travel medicine that encompasses a body of knowledge in travel medicine developed by an international group of travel medicine physicians.
Refugees and migrants
International migration, usually from poor countries to rich countries, is a worldwide phenomenon. Estimates put the number of migrants worldwide in 1990 in excess of 120 million, with an annual growth rate of 1.9%.9 Net international migration contributed to 45% of the population growth in the developed world and almost 88% of the population growth in Europe in 1990-5. The number of refugees worldwide, including asylum seekers, in 2001 totalled 19.8 million.10 Trafficking in migrants has become a lucrative illegal market.
The migration process has important health implications. Migrants often have a higher rate than other travellers of conditions such as tuberculosis, hepatitis B and C, schistosomiasis, malaria, and sexually transmitted infections (including syphilis and HIV). They also have a higher rate of non-infectious conditions such as diabetes, cardiovascular disease, malignant diseases, asthma, respiratory diseases linked to smoking, occupational diseases, and injuries, as well as psychological disorders.11 Stress related health problems are exacerbated by changes in lifestyle, food habits, culture, and religious life. As the number of refugees and migrants grows, medical providers and travel medicine physicians need to understand and respond to the wide range of health problems they have.
Vector borne disease
Up to 8 in 1000 travellers in developed countries become infected with malaria, resulting in more than 10 000 cases of malaria being imported into Europe each year (fig 2).12,13 Other vector borne diseases, such as dengue and yellow fever, are also increasingly important.14
Since December 2001, following the report of six deaths possibly associated with the administration of yellow fever vaccine in elderly travellers, health professionals have expressed concern about the use of yellow fever vaccine.15–17 Millions of doses of vaccine have been administered over many years, however, with a minimum risk of morbidity or mortality, and experts agree that the benefits of yellow fever vaccination outweigh the risks.
Malaria remains the single most important disease hazard facing travellers. Adherence to antimalarial chemoprophylaxis, in addition to adopting measures to avoid being bitten, is essential. Chloroquine resistant falciparum malaria is an increasing problem in Central and South America, South East Asia, Oceania, and sub-Saharan Africa.18 Recommended prophylaxis for chloroquine resistant areas, to be discussed with the individual traveller, include mefloquine, doxycycline, and atovaquone plus proguanil (Malarone). Chloroquine continues to be recommended as prophylaxis for malaria in areas where there is no chloroquine resistance.
It is advisable for people taking mefloquine for the first time to start three weeks before departure so that if they experience side effects such as anxiety or nightmares alternative prophylactic drugs can be considered. Alternatives include Malarone one tablet daily, doxycycline 100 mg daily, dapsone plus pyrimethamine (Maloprim) one tablet weekly or chloroquine and proguanil. Malarone consists of 250 mg atovaquone and 100 mg proguanil and is of particular value for people travelling to chloroquine resistant areas.19 Prophylaxis should be started one day before entry into an endemic area and continued for seven days after leaving it.
Guidance on antimalarial chemoprophylaxis has recently been issued by the Advisory Committee on Malaria Prevention for UK Travellers (box B3). Malarone, doxycycline, and mefloquine are recommended in chloroquine resistant areas. Mefloquine is recommended for travel of longer than two weeks' duration to West, Central, and East Africa and specific areas of South East Asia. Chloroquine and proguanil are recommended for travel to other areas.20
Box 3.
Malaria chemoprophylaxis by continent (depending on season and area visited)
- North Africa and Middle East—chloroquine alone or chloroquine plus proguanil
- Sub-Saharan Africa—mefloquine, doxycycline, or atovaquone plus proguanil
- South Asia—chloroquine plus proguanil
- South East Asia—mefloquine, doxycycline, or atovaquone plus proguanil (Indonesia and forests of Malaysia and Sarawak—chloroquine plus proguanil)
- Oceania—mefloquine, doxycycline, or atovaquone plus proguanil
- Latin America—mefloquine, doxycycline, or atovaquone plus proguanil
- Caribbean—chloroquine plus proguanil or chloroquine alone
- Chloroquine—two tablets taken weekly starting a week before travel to endemic area and continuing for four weeks after leaving malarious area
- Proguanil—one tablet daily starting a week before travel to endemic area and continuing for four weeks after leaving malarious area
- Doxycycline—one tablet daily starting one day before travel to endemic area and continuing for four weeks after leaving malarious area
- Atovaquone plus proguanil (Malarone)—one tablet daily starting one day before travel to endemic area and continuing for seven days after leaving malarious area
- Mefloquine—one tablet weekly starting trial dose three weeks before departure if appropriate and continuing for four weeks after leaving malarious area
Standby treatment in defined circumstances may become of increasing value to travellers. Standby treatment consists of a course of antimalarial drugs that travellers to malaria endemic areas can use for self treatment if they are unable to gain access to medical advice within 24 hours of becoming unwell. The treatment kits are supplied with written instructions, and travellers must seek medical advice as soon as possible. Recently licensed agents indicated for use as standby treatment include Malarone and Riamet, which is a new fixed dose antimalarial drug containing 20 mg artemether and 120 mg lumefantrine.21
Prevention of infectious disease
The prevention of infectious disease in travellers continues to receive substantial consideration, as an appreciable number of such diseases are now considered to be “vaccine preventable.”22 Vaccines usually recommended for general travel include tetanus, poliomyelitis, and hepatitis A. As destinations become more diverse, with people increasingly travelling outside Europe, additions to this list include typhoid, hepatitis B, diphtheria, and rabies (box B4). Mandatory vaccines, for which certification is often necessary, include yellow fever and meningoccocal meningitis, as appropriate to the destination. Travellers at high risk, such as those with chronic medical problems, would benefit from vaccination against diseases such as influenza, whose seasonal prevalence differs in temperate and tropical climates, as well as pneumococcal vaccine and hepatitis B vaccine.
Additional educational resources
Bradley DJ, Bannister B. Guidelines for malaria prevention in travellers from the United Kingdom for 2001. Commun Dis Public Health 2001;4:84-101
Department of Health. Health information for overseas travel 2001. London: Department of Health, 2001
World Health Organization. International travel and health 2002. Geneva: WHO, 2002
Zuckerman JN, ed. The principles and practice of travel medicine. Chichester: John Wiley & Sons, 2001
Websites
Foreign and Commonwealth Office—general travel health and safety advice (www.fco.gov.uk/travel/)
World Health Organization, International Travel and Health—vaccination requirements and health (www.who.int/ith/) and disease outbreak reports (www.who.int/disease-outbreak-news/)
Centers for Disease Control and Prevention—US health information for international travel (www.cdc.gov/travel)
International Society of Travel Medicine—information resource for both travel medicine practitioners and travellers (www.istm.org)
NHS resource for healthcare professionals advising travellers about how to avoid illness when travelling abroad—www.travax.scot.nhs.uk
Fit for Travel—public access website provided by the NHS, which gives travel health information for people travelling abroad from the UK (www.fitfortravel.scot.nhs.uk)
Medical care before, during, and after air travel—www.britishairways.com/health
BMJ archive
Mortimer P. Yellow fever vaccine. BMJ 2002;324:439
Goodwin T. In-flight medical emergencies: an overview. BMJ 2000;321:1338-41
Webster G, Barnes E, Dusheiko G, Franklin I. Protecting travellers from hepatitis A. BMJ 2001;322:1194-5
Box 4.
Vaccines for travellers
- Poliomyelitis
- Tetanus
- Childhood immunisations (in date)
- Recommended for travel outside northwest Europe, North America, Australia, and New Zealand:
- Diphtheria (travellers in close contact with the indigenous population)
- Hepatitis A
- Hepatitis B
- Typhoid
- Influenza (travellers with underlying medical problems)
- Japanese encephalitis (travel for more than four weeks in rural area)
- Meningoccocal meningitis (travellers in close contact with the indigenous population)
- Pneumococcus (travellers with underlying medical problems)
- Rabies (rural travel and travel more than 24 hours away from medical help)
- Tick borne encephalitis (travel to forested areas of Eastern Europe)
- Meningoccocal meningitis (travel to Saudi Arabia for purposes of a pilgrimage)
- Yellow fever (travel to parts of sub-Saharan Africa and parts of Central and South America)
Hepatitis B vaccine should also be considered for a wider range of travellers, including those who may travel to areas endemic for hepatitis B, may be exposed by virtue of their sexual practices, or may be exposed to unscreened or inadequately screened blood or blood products or inadequately sterilised medical and surgical equipment.23
People are increasingly travelling at short notice, and the ability to provide good levels of protection within a period of four weeks is an important development. Newer combination vaccines, such as hepatitis A plus typhoid and hepatitis A plus B, provide dual protection by a single injection (box B5). This increases uptake and convenience (particularly for people with a fear of needles) and by using only one site makes another injection site available when time is short and multiple immunisations need to be considered. Rapid schedules of vaccination include monovalent hepatitis B vaccine, which can be administered according to three different schedules, and combined hepatitis A and B vaccine, which can be administered as a primary course within three weeks.24
Box 5.
Rapid schedules of vaccination
- Hepatitis B (Engerix B)—days 0, 7, and 21; booster at 12 months
- Hepatitis A and B (Twinrix)—days 0, 7, and 21; booster at 12 months
- Hepatitis A and B (Twinrix)
- Hepatitis A and typhoid (Hepatyrix; ViATIM)
- Diphtheria and tetanus (DT, d, Td)
Other recent developments include the introduction of a quadrivalent meningoccocal meningitis vaccine to protect against the W135 strain, which has been associated with several outbreaks of disease in Saudi Arabia as well as in parts of sub-Saharan Africa.25 Other new vaccines licensed in the United States include a vaccine against varicella.26
As part of the expanded programme on immunisation, under the auspices of the WHO, worldwide eradication of poliomyelitis remains a goal. The report of outbreaks of vaccine associated poliomyelitis in countries where wild poliovirus has been eliminated is, however, of concern.27 In view of this, it would seem prudent for those travellers at particular risk—for example, those in contact with the local population, such as aid workers—to maintain levels of protection against poliomyelitis.
Aviation medicine
Health practitioners need to be aware of the health effects of reduced atmospheric pressure, transmeridian travel (causing jetlag), and motion sickness and to consider passengers' fitness to travel by air. Guidelines for medical clearance, in-flight medical emergencies, and aircraft emergency medical equipment have been reviewed.28
The risk of transmission of respiratory diseases in association with air travel should also be considered. No case of active tuberculosis as a result of exposure during travel by air has yet been identified, but transmission of Mycobacterium tuberculosis may occur during flights of more than eight hours, as the risk of infection is related to the proximity and duration of exposure to the source patient.29
Considerable attention has been given to travel related deep vein thrombosis.30,31 The estimated risk of developing deep vein thrombosis after a long distance flight is between 0.1 and 0.4 per thousand of the general population.32 Methods of preventing deep vein thrombosis, including identification of travellers with predisposing risk factors,32 are important. All passengers, regardless of their risk, should move around in their seats and in the aircraft cabin as much as possible during the journey. Drinks containing alcohol or caffeine should be avoided before and during the flight, and water or soft drinks should be taken to reduce the effects of dehydration. Exercising the calf muscles every half hour while seated by spending a few minutes flexing and rotating the ankles is also recommended to reduce the effects of stasis.
The prophylactic use of aspirin, and in some cases subcutaneous heparin, to prevent deep vein thrombosis is under discussion. Under the auspices of the WHO, studies are planned to evaluate the risk of deep vein thrombosis associated with travelling by air. The aims of the research programme are to determine the frequency and cause of travellers' thrombosis through epidemiological studies, to identify who is at greatest risk through pathophysiological studies, and to undertake clinical studies that will focus on the effectiveness of possible preventive strategies.33
Supplementary Material
Figure.
PETER MACDIARMID/REX
The increase in air travel has led to increases in the incidence of travel related disease and the importation of infection
Footnotes
Competing interests: JNZ has been reimbursed by several manufacturers of vaccines and antimalarial prophylaxis for attending conferences and running educational programmes and has received unrestricted educational grants. JNZ is also a consultant in travel medicine to British Airways travel clinics.
Details of courses in travel medicine appear on bmj.com
References
- 1.World Tourist Organisation. Tourism highlights. Madrid: World Tourist Organisation; 1998. [Google Scholar]
- 2.World Tourist Organisation. World Tourism Organisation statistics service. Madrid: World Tourist Organisation; 2000. [Google Scholar]
- 3.Lederberg J. Emerging infectious diseases from the global to the local perspective. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 4.Mardh PA. What is travel medicine? Content, current position, tools and tasks. J Travel Med. 2002;9:34–47. [PubMed] [Google Scholar]
- 5.Department of Health. Getting ahead of the curve—a strategy for combating infectious diseases in the United Kingdom. London: Department of Health; 2002. [Google Scholar]
- 6.Stringer C, Chiodini J, Zuckerman JN. Travel health risk assessment. Nursing Standard. 2002;16(39):49–54. doi: 10.7748/ns2002.06.16.39.49.c3212. [DOI] [PubMed] [Google Scholar]
- 7.Travellers Omnibus Survey. London: Ipsos RSL; 1999. [Google Scholar]
- 8.Zuckerman JN. Reflections and reactions: shaping travel health and medicine for the future. Lancet Infect Dis. 2001;1:296–297. doi: 10.1016/S1473-3099(01)00142-6. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. The world health report. Geneva: WHO; 1998. [Google Scholar]
- 10. United Nations High Commissioners for Refugees. Statistical reports. www.unhcr.ch/statistics (accessed 17 July 2002).
- 11.Carballo M, Divino JJ, Zeric D. Migration and health in the European Union. Trop Med Int Health. 1998;3:936–944. doi: 10.1046/j.1365-3156.1998.00337.x. [DOI] [PubMed] [Google Scholar]
- 12.Steffen R, DuPont HL. Manual of travel medicine and health. Hamilton, Canada: BC Decker; 1999. Overview of health risks in travellers; pp. 43–49. [Google Scholar]
- 13.World Health Organization. International travel and health: vaccination requirements and health advice. Geneva: WHO; 2001. [Google Scholar]
- 14.Heymann D, Rodier GR. Hot spots in a wired world: WHO surveillance of emerging and re-emerging infectious diseases. Lancet Infect Dis. 2001;1:345–353. doi: 10.1016/S1473-3099(01)00148-7. [DOI] [PubMed] [Google Scholar]
- 15.Martin M, Tsai TF, Cropp B, Chang G-JJ, Holmes DA, Tseng J, et al. Fever and multisystem organ failure associated with 17D-204 yellow fever vaccination: a report of four cases. Lancet. 2001;358:98–104. doi: 10.1016/s0140-6736(01)05327-2. [DOI] [PubMed] [Google Scholar]
- 16.Chan RC, Penney DJ, Little D, Carter IW, Roberts JA, Rawlinson WD. Hepatitis and death following vaccination with 17D-204 yellow fever vaccine. Lancet. 2001;358:121–126. doi: 10.1016/S0140-6736(01)05341-7. [DOI] [PubMed] [Google Scholar]
- 17.Mortimer P. Yellow fever vaccine. BMJ. 2002;324:439. doi: 10.1136/bmj.324.7335.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization 2000(b) WHO Expert Committee on Malaria (20th report). Geneva: WHO; 2000. :i-v,1-74. (WHO Technical Report Series 892.) [Google Scholar]
- 19.Nosten F. Prophylactic effect of Malarone against malaria: all good news? Lancet. 2000;356:864–865. doi: 10.1016/S0140-6736(00)03250-5. [DOI] [PubMed] [Google Scholar]
- 20.Bradley DJ, Bannister B. Guidelines for malaria prevention in travellers from the United Kingdom for 2001. Commun Dis Public Health. 2001;4:84–101. [PubMed] [Google Scholar]
- 21.Schlagenhauf P, Steffen R. Standby treatment of malaria in travellers: a review. J Trop Med Hyg. 1994;97:151–160. [PubMed] [Google Scholar]
- 22.Zuckerman JN. Principles and practice of travel medicine. Chichester: John Wiley & Sons; 2001. Vaccine-preventable disease; pp. 165–185. [Google Scholar]
- 23.Zuckerman JN, Steffen R. Risks of hepatitis B in travellers as compared to immunisation status. J Travel Med. 2000;7:170–174. doi: 10.2310/7060.2000.00054. [DOI] [PubMed] [Google Scholar]
- 24. Zuckerman JN, Dietrich M, Nothdurft HD, Knotloch J, Kern P, Vollmar J, et al. Rapid protection against hepatitis A and hepatitis B following accelerated schedule of combined hepatitis A/B vaccine [abstract]. Tenth International Symposium on Viral Hepatitis and Liver Disease, Atlanta, USA, 9-13 April 2000:No 012.
- 25.Meningococcal disease serogroup W135. WER. 2001;19:141–142. [PubMed] [Google Scholar]
- 26.Varicella, measles, mumps, rubella vaccine. Interim recommendations from the Advisory Committee on Immunisation Practices. MMWR Morb Mortal Wkly Rep. 2002;51:190–197. [PubMed] [Google Scholar]
- 27.Progress toward global eradication of poliomyelitis, 2001. MMWR Morb Mortal Wkly Rep. 2002;51:253–256. [PubMed] [Google Scholar]
- 28.Dowdall N. “Is there a doctor on the aircraft?” Top 10 in-flight medical emergencies. BMJ. 2000;321:1336–1337. doi: 10.1136/bmj.321.7272.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization. Tuberculosis and air travel. Geneva: WHO; 2001. [Google Scholar]
- 30.Geroulakos G. The risk of venous thromboembolism from air travel. BMJ. 2001;322:188. doi: 10.1136/bmj.322.7280.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scurr JH, Machin SJ, Bailey-King S, Mackie IJ, McDonald S, Smith PD. Frequency and prevention of symptomless deep vein thrombosis in long-haul flights: a randomised trial. Lancet. 2001;357:1485–1489. doi: 10.1016/S0140-6736(00)04645-6. [DOI] [PubMed] [Google Scholar]
- 32.House of Lords. Select Committee on Science and Technology, fifth report. London: Stationery Office; 2000. [Google Scholar]
- 33.WHO study of venous thrombosis and air travel. Weekly Epidemiological Record. 2002;77:197–199. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.