Abstract
Background:
Drug checking is a harm reduction strategy that provides greater awareness and information about the drug supply to the community. While fentanyl test strips are low-cost and available in most parts of the U.S., community-based organizations are considering using more sophisticated technologies, such as Fourier-transform infrared (FTIR) spectroscopy to test drugs. FTIR can detect multiple substances in a non-destructive manner that can be rapidly communicated to the end user by a trained technician, however implementation costs in community-based settings have not been assessed.
Methods:
We conducted a costing analysis of a new pilot drug checking service that employed an FTIR spectrometer, fentanyl test strips and confirmatory testing in Rhode Island from January 2023-May 2023. We used microcosting methods to determine the overall cost during this period and cost per drug checked, reflecting realistic service capacity.
Results:
Among 101 drug samples that were voluntarily submitted and tested, 53% tested positive for fentanyl, 39% for cocaine, 9% for methamphetamine and 13% for xylazine, a powerful sedative. The total cost during this period was $71,044 and the cost per drug checked was $474, though sensitivity analyses indicated that the cost would rise to $78,058 - $83,058 or $544 - $593 for programs needing to pay for specialized training.
Conclusions:
These findings demonstrate feasibility and inform the resources needed to scale-up drug checking services to reduce overdose risk.
Keywords: Drug checking, harm reduction, substance use, test strips, infrared spectroscopy, cost analysis
1. INTRODUCTION
In 2021, the age-adjusted overdose mortality in Rhode Island was 41.7 deaths per 100,000 population, 29% higher than the age-adjusted national estimate of 32.4 deaths per 100,000 population (Centers for Disease Control and Prevention, 2023). Fentanyl, powerful non-opioid sedatives like xylazine, and adulterants more commonly found in stimulants such as levamisole, complicate efforts to effectively respond to rising drug-related morbidity and mortality. Traditionally, illicit drug testing was conducted exclusively by law enforcement forensic labs, without intent of informing people who use drugs (PWUD) to mitigate overdose risk. Drug checking is a harm reduction strategy that provides greater awareness and information about the drug supply to the community. Although event-based drug checking has occurred at music festivals in the U.S., the implementation of point-of-care drug checking programs targeting people with substance use disorder is a newer undertaking. Drug checking services involves the consensual collection and testing of drug samples, including drug residues in bags and capsules, to rapidly communicate results to end users (Carroll et al. 2022; Maghsoudi et al., 2022; Harper et al. 2017). Due to the reported interest in community-based drug checking among PWUD, point-of-care drug checking services were piloted in Rhode Island (Sherman et al., 2019).
Drug checking is a nascent, albeit burgeoning, public health intervention in the U.S. To date, it has been mostly limited to distribution of fentanyl test strips (FTS) and use of reagents at festivals and raves, which remain illegal in some states (Davis et al., 2019). Due to the pervasiveness of potent substances such as fentanyl and xylazine and other contaminants with harmful effects like levamisole found in drugs, community-based organizations are considering implementing drug checking services beyond fentanyl test strips by using more sophisticated devices like Fourier-transform infrared (FTIR) spectroscopy. A major advantage of FTIR over fentanyl test strips and reagents is its ability to identify multiple unknown substances and their relative presence in each sample. The testing process is non-destructive so the small amount of sample required for on-site testing can be returned (if permissible) or efficiently prepared for further off-site testing without the need for additional sample submission. As results are provided by a trained technician, there is limited subjectivity of interpreting results that would be required if self-administering test strips.
Understanding the implementational procedures, start-up costs, and recurrent costs is critical to program planning, resource allocation, and scale-up. Accordingly, the objective of this analysis was to estimate the costs of launching and sustaining a community-based drop-in drug checking service program after it was piloted in Pawtucket, Rhode Island. Prior to implementation, virtually no sample-level data were publicly available about the local drug market in this town, except for one public health drug surveillance project that had tested 13 samples from Pawtucket in a laboratory in 2022 (Collins et al., 2023).
2. METHODS AND MATERIALS
Formal planning and training for drug checking services commenced on July 31, 2022. The drug checking services were co-located within a community drop-in center, which provided free naloxone, sterile drug use equipment, FTS, and recovery support services to PWUD. The drug checking services program consisted of an FTIR spectrometer (Bruker, Billerica, MA, USA), which can detect a broad range of chemicals, as well as a lateral flow immunoassay FTS (Green et al, 2020). Testing was completed onsite within 15 minutes and FTIR and FTS results were shared directly with the sample submitter (Beaulieu et al., 2021). All samples were then sent to the Rhode Island Hospital Toxicology Laboratory for confirmatory testing (Quadrupole Time of Flight Mass Spectrometry).
The program operated 2 days per week for 2-3 hours daily from January 27, 2023, to May 4, 2023, and was promoted by word-of-mouth by the center’s staff and a peer outreach specialist who assisted with liaising and engaging with PWUD and sample collection. One research assistant and one FTIR technician completed all sample data entry, sample preparation, FTS immunoassay testing, and real-time result communication. Compiled on-site testing results and confirmatory laboratory testing results were available through the no-cost StreetCheck web application, which was developed by a separate team to standardize reporting for community-based drug checking services (see Table S1) (Collaborative OPR, 2023; StreetCheck, 2023). No personal or demographic data were collected. Each submitter was paid $5 per sample, and unique identifiers were generated for each sample submitted to maintain anonymity.
2.1. Costing procedures
We conducted an ingredients-based micro-costing study to estimate total service costs during the implementation period. We adopted a payer perspective and determined the costs of all inputs required to conduct drug checking, regardless of if they were paid or donated. The program manager reviewed financial records, itemized bills/receipts, and equipment catalogues to obtain unit prices for supplies. Equipment-related capital costs consisted of the FTIR machine as well as ancillary software and libraries (e.g., Bruker pharmaceutical libraries, the Science Working Group for the Analysis of Seized Drugs library, the British Columbia Centre on Substance Use library, and the TICTAC library), which contained infrared spectra of drugs, pharmaceuticals, and common adulterants. These spectra were compared to the sample spectra during the identification process. Purchasing the libraries represented a one-time cost, however yearly updates to the libraries could incur additional costs. We accounted for a 10% discount, which is available to academic and non-profit affiliated programs operating drug checking services, for bundling the purchase of the FTIR machine with the libraries. Personnel-related costs, such as salaries and fringe benefits, were obtained from expenditure reports. We converted all salaries to an hourly wage which was multiplied by the total number of hours that staff were involved with drug checking services during the evaluation period as recorded in shift logs. Due to the technical expertise required for conducting FTIR spectroscopy, we interviewed program staff to estimate the number of hours dedicated to receipt of technical assistance and troubleshooting (i.e., independent practice). This included time spent corresponding with technical consultants via email. Training costs also included attendance and travel to a two-day conference, ongoing remote supports, learning collaborative participation, and one-one-one technical assistance sessions hosted by the Massachusetts Drug Supply Data Stream (MADDS) at Brandeis University which were provided in-kind for this pilot project. Topics of the training included sample collection processes, instrument overview, sample accounting, FTIR spectroscopy training, and analyzing samples using FTIR (Collaborative OPR, 2023).
Normal output of drug checking services was not achieved until the end of the pilot period after most operational issues had been resolved. To estimate unit costs (i.e., the cost per drug checked), we distributed fixed (e.g., equipment) and recurrent (e.g., personnel) costs appropriately. For example, as the FTIR machine constituted a substantial start-up cost, we annualized the cost over its lifespan by applying straight line depreciation, assuming 50% salvage value after five years of useful life.
2.2. Sensitivity analysis
Our program benefited from a strong partnership between a community-based harm reduction organization and an academic research institution. As a result, the in-kind training costs could underestimate the actual cost for community-based organizations without readily available access to technical expertise in FTIR spectroscopy. Thus, we gathered estimates from coauthors providing technical assistance services and received input from key informants indicating that harm reduction organizations should budget $10,000 - $15,000 for training-related costs that would likely be incurred within the first three months of operation (personal communication with Remedy Alliance, 2023). These costs incorporated effort and travel for direct service FTIR technicians and trainers. While no- or low-cost training and technical assistance may be provided through some funders such as the U.S. Centers for Disease Control and Prevention, if sites do not receive such funding, specialized training could be an important and potentially costly additional component to consider. In a sensitivity analysis, we replaced our estimated training costs with those assuming purchase of these start-up training services.
3. RESULTS
The pilot study team analyzed 101 residual drug samples, among which, 53% tested positive for fentanyl, 39% for cocaine, 9% for methamphetamine and 13% for xylazine (Figure 1). No adverse events to submitters or staff occurred during the operation or delivery of results to submitters in this intervention.
Figure 1.
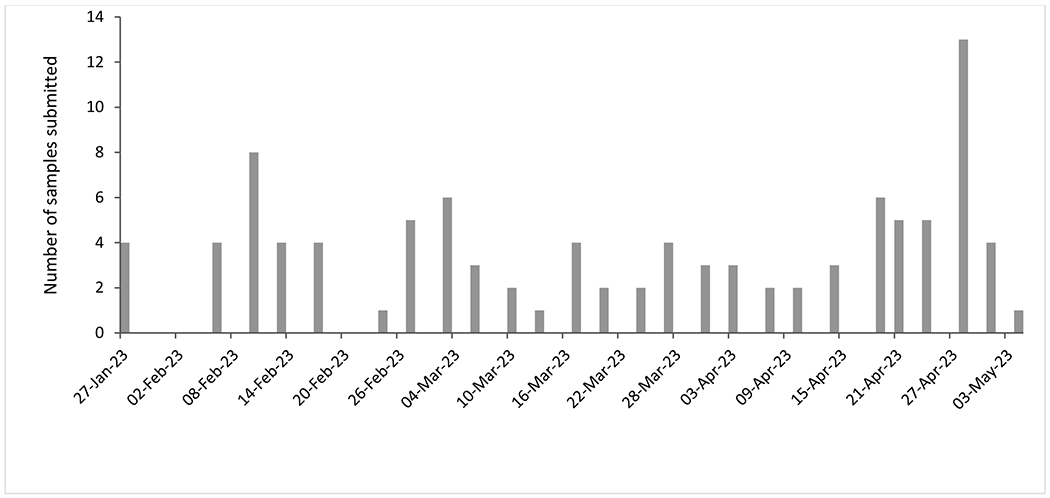
Frequency of drug checking over the evaluation period (January 27, 2023 – May 4, 2023). Note: The program operated only twice per week.
The total cost of establishing and operating the service over nine months (with over three months of drug checking) was $71,044, with approximately 54% attributed to the FTIR machine, software, libraries, and technical training (Table 1). Approximately 16% of the total cost was attributed to personnel, which consisted of a program director, FTIR technician (who held a bachelor’s degree in a scientific field), research assistant, outreach worker, and administrative assistant. Four percent (4%) of the cost was attributed to training, which involved approximately 80 hours of technical assistance, in-person training, and independent practice.
Table 1.
Total and unit cost (USD) of drug checking program in Rhode Island operating from January 27, 2023 – May 4, 2023 (N=101 drugs submitted for checking)
| Total cost (USD) | Cost per drug checked (USD)* | |
|---|---|---|
| Personnel | ||
| Program director (16 hours) | 756 | 7 |
| FTIR technician (128 hours) | 3,317 | 33 |
| Research assistant (96 hours) | 2,488 | 25 |
| Peer outreach worker (119 hours) | 3,570 | 35 |
| Front desk staff (48 hours) | 1,058 | 10 |
| Sub-total (% of total) | 11,188 (16%) | 111 (23%) |
| Non-personnel recurrent | ||
| Supplies** | 461 | 4 |
| Office space (50 ft2 or 4.65 m2) | 1,600 | 16 |
| Sub-total (% of total) | 2,061 (3%) | 20 (4%) |
| Equipment and other start-up | ||
| FTIR machine | 23,391 | 9 |
| FTIR spectral analysis software | 2,349 | 23 |
| FTIR libraries | 9,839 | 97 |
| Designated FTIR laptop | 1,724 | 1 |
| Library update | 20 | |
| Tablets | 1,289 | 3 |
| Office and lab. equip*** | 563 | 6 |
| Incentive | 505 | 5 |
| Confirmatory testing | 15,150 | 150 |
| Sub-total (% of total) | 54,809 (77%) | 314 (66%) |
| Training | ||
| Technical training (66 hours) | 2,167 | 21 |
| Troubleshooting (14 hours) | 630 | 7 |
| Mileage to attend in-person training | 189 | 2 |
| Sub-total (% of total) | 2,986 (4%) | 30 (6%) |
| Total | 71,044 **** | 474 **** |
assuming realistic service capacity and incorporating depreciation for equipment
supplies include: small mylar or plastic bags, tissue wipes, disposal bags, plastic cups, nitrile gloves, small scoops, disposable surgical masks, dental bibs, fentanyl test strip, aluminum foil, isopropyl alcohol, distilled water, syringes without needles, microtubes, medium bags, labels, business cards
office-related equipment include: dispensing bottles, goggles/glasses, safe/lock, despite lock bag, supply box, pencil box, graduated cylinder, dental tools, mortar and pestle, tweezers, surge protector
may not sum to total due to rounding
The cost per drug checked was $474, including confirmatory testing ($150 per sample). However, in real-world implementation, possibly 10%-25% of samples may need to be checked for ongoing quality assurance, which would result in a range from $339 -$361 per drug checked after the establishment of the program. Lastly, in sensitivity analyses which incorporated estimated at-cost training supports ($10,000 - $15,000), the total cost of the program over this period would increase to $78,058 - $83,058 and a cost per drug checked ranging from $544 - $593.
4. DISCUSSION
To our knowledge, this is the first empirical costing analysis of a community-based drug checking program in the U.S. Findings from this evaluation indicate that drug checking using FTIR was feasible, and frequently utilized by PWUD, with relatively low cost. Indeed, consistent access to drug checking is important therefore substantial investment will be needed to ensure this a viable and useful service for many PWUD who might be using drugs daily. Nonetheless, more research is needed to determine the effectiveness (e.g., change in behaviors after using the drug checking program that mitigate overdose risk) and cost-effectiveness of the program to determine its value-for-money and inform evidence-based decision-making for policymakers.
Illicit drug markets often evolve faster than the public health response needed to mitigate consequent harms. Drug checking represents a critical harm reduction tool for promoting safer consumption practices and reducing drug-related morbidity and mortality. Further, drug checking services can inform near real-time surveillance of the illicit drug supply which can be rapidly disseminated to enhance community awareness. While the unit cost of fentanyl test strips and reagents are substantially less using FTIR, major advantages of FTIR over fentanyl test strips and reagents are its ability to adapt to the evolving drug market, identify multiple substances in a sample as well as their relative presence, non-destructive method, and involvement of a trained technician. Prior studies have shown that PWUD modify consumption behaviors after receiving an undesirable result, and this is even more relevant for those who do not intend to use opioids but unwittingly learn that fentanyl or other substances that can increase overdose risk are in their sample (The Network for Public Health Law, 2023;
This study has several limitations. First, as data collection for personnel effort involved in pre-intervention training occurred after the program had been piloted, there could be some imprecision with these costs. For this reason, we conducted sensitivity analysis with higher training costs to estimate the overall cost per drug analyzed. Second, given the retrospective nature of data collection, we could not obtain client-level costs, such as out-of-pocket expenses related to travel, missed time from work, and other costs that would not be accounted from a payer perspective. Third, this evaluation was conducted within the context of a pilot study and the cost per drug checked could be lower once the program reaches full maturity.
Our estimates are consistent with the unit cost of forensic laboratory testing used in prosecution of drug-related offenses (approximately $450 inclusive of personnel-related costs in Baltimore City) (Rouhani, 2023). Given that drug checking services could be an important component of overdose risk reduction, providing these services, which are likely affordable, could be useful for policymakers, government agencies and foundations for appropriating funding to implement and scale-up.
Supplementary Material
References
- Beaulieu T, Wood E, Tobias S, et al. I s expected substance type associated with timing of drug checking service utilization?: A cross-sectional study. Harm Reduction Journal 2021; 18: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll JJ, Mackin S, Schmidt C, McKenzie M, Green TC. The Bronze Age of drug checking: barriers and facilitators to implementing advanced drug checking amidst police violence and COVID-19. Harm reduction journal 2022; 19(1): 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- QuickStats: Age-Adjusted Drug Overdose Death Rates, by State — National Vital Statistics System, United States, 2021. MMWR Morb Mortal Wkly Rep 2023;72:293. DOI: 10.15585/mmwr.mm7211a7. (accessed 16 October 2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collaborative OPR. StreetCheck: Community Drug Checking App. 2023. https://heller.brandeis.edu/opioid-policy/community-resources/street-check/index.html.
- Collins AB, Wightman RS, Macon EC, Guan Y, Shihipar A, Krieger M, Elmaleh R, Smith MC, Morales A, Badea A. Comprehensive testing and rapid dissemination of local drug supply surveillance data in Rhode Island. International Journal of Drug Policy. 2023. Aug 1;118:104118. [DOI] [PubMed] [Google Scholar]
- Davis CS, Carr DH, Samuels EA. Paraphernalia laws, criminalizing possession and distribution of items used to consume illicit drugs, and injection-related harm. American Journal of Public Health. 2019. Nov;109(11):1564–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green TC, Park JN, Gilbert M, McKenzie M, Struth E, Lucas R, Clarke W, Sherman SG. An assessment of the limits of detection, sensitivity and specificity of three devices for public health-based drug checking of fentanyl in street-acquired samples. International Journal of Drug Policy. 2020. Mar 1;77:102661. [DOI] [PubMed] [Google Scholar]
- Harper L, Powell J, Pijl EM. An overview of forensic drug testing methods and their suitability for harm reduction point-of-care services. Harm reduction journal 2017; 14(1): 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maghsoudi N, Tanguay J, Scarfone K, et al. Drug checking services for people who use drugs: a systematic review. Addiction 2022; 117(3): 532–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Personal Communication with Remedy Alliance. August 3, 2023. [Google Scholar]
- Rouhani S, Tomko C, Silberzahn B, Sherman SG, Cepeda J. Estimating economic costs of prosecuting simple drug possession in Baltimore City. 2023. https://americanhealth.jhu.edu/sites/default/files/estimating-economic-costs-prosecuting-simple-drug-possession-baltimore-city-april-2023.pdf (accessed 1 August 2023).
- Sherman SG, Morales KB, Park JN, McKenzie M, Marshall BD, Green TC. Acceptability of implementing community-based drug checking services for people who use drugs in three United States cities: Baltimore, Boston and Providence. International Journal of Drug Policy 2019; 68: 46–53. [DOI] [PubMed] [Google Scholar]
- StreetCheck. 2023. www.streetcheck.org (accessed 25 July 2023).
- The Network for Public Health Law. Legality of Drug Checking Equipment in the United States 2022. https://www.networkforphl.org/wp-content/uploads/2023/01/Legality-of-Drug-Checking-Equipment-in-the-United-States-August-2022-Update.pdf (accessed 26 June 2023).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


