Abstract
Background/Aims
Noncardiac chest pain (NCCP) of esophageal origin is a challenging clinical problem of diverse etiology that affects more than 80 million Americans yearly. We assess the prevalence and impact of psychological disorders on NCCP of esophageal origin, describe possible mechanisms associated with this condition, and review psychological therapy options.
Methods
Online search using PubMed and Medline from January 1, 1966, to April 30, 2023.
Results
Psychological disorders have been reported in up to 79% of patients with NCCP of esophageal origin. Several psychological disturbances have been identified with this condition, including depression, anxiety, panic disorder, phobias, and obsessive-compulsive and somatoform disorders. It is unclear whether the psychological disorders trigger the chest pain or vice versa. Multiple psychological mechanisms have been linked to chest pain and may contribute to its pathogenesis and severity. These mechanisms include cardiophobia, poor coping strategies, negative social problem solving, stress and perceived control, hypervigilance to cardiopulmonary sensations, altered pain perception, and alexithymia. Psychological therapies for NCCP of esophageal origin include cognitive behavioral therapy, hypnotherapy, physical and relaxation training, breathing retraining, and alternative medicine. Among the therapeutic options, cognitive behavioral therapy has been shown to be an effective treatment for NCCP of esophageal origin.
Conclusion
This review raises awareness about the high prevalence of psychological disorders in NCCP of esophageal origin and highlights the need for clinical trials and trained therapists to address the management of this taxing clinical problem.
Keywords: Chest pain, Functional gastrointestinal disorders, Psychiatric disorders
Introduction
Noncardiac chest pain (NCCP) of esophageal origin affects more than 80 million Americans yearly.1 Population-based studies indicate that it is not only ubiquitous in the United States but has also been reported in Australia and Asia, with prevalence rates ranging from 10% to 30%.2,3 NCCP accounts for recurrent visits to emergency departments and is an important cause of health care expenditure, poor quality of life, and disability.4 A study in 1989, estimated the health-care costs for NCCP at $315 million annually.5 It is likely these costs have escalated considerably in recent years. Indeed, a more recent European study calculated the cumulative annual cost of patients with NCCP at nearly €817 million (United States $893 million).6
NCCP is a challenging diagnosis to make. Chest pain is frequently indistinguishable from cardiac chest pain and other life-threatening conditions. Distinguishing esophageal chest pain from cardiac origin and serious conditions (eg, pulmonary embolism, dissecting thoracic aortic aneurysm, and pericarditis) is of paramount importance since these disorders may result in fatal consequences.7 The causes of NCCP are multifactorial. Psychological disorders have been reported in a high percentage of these patients; however, clinicians often lack sufficient awareness and training to recognize the role of psychological factors in these patients.8 Furthermore, there is a need for physicians and therapists to consider the high prevalence of psychological disorders in NCCP. The purpose of this study is to review the role of psychological factors in NCCP. We aim to provide a broader picture of the prevalence of psychological conditions in NCCP, the possible psychological mechanisms contributing to chest pain in these patients, and the psychological treatment options.
Methods
We performed an online search using PubMed, Medline from January 1, 1966, to April 30, 2023, using the following keywords: Noncardiac chest pain (NCCP), functional esophageal pain, atypical chest pain, psychology, psychological, panic disorder, anxiety, depression, somatoform, obsessive-compulsive disorder, cognitive behavioral therapy, hypnotherapy, relaxation, acupuncture, and Johrei. In addition, Boolean operators were employed to strengthen the combination of keywords.
Inclusion criteria involved articles written in English in the form of full text, including meta-analysis, systematic reviews, randomized controlled trials, reviews, cohort studies, case-control, and case series, all in adult populations. Articles concerning the pediatric population; articles not written in English; and articles concerning the terms cardiac chest pain, acute myocardial infarction, acute coronary syndrome, and acute cardiac chest pain were excluded. A manual search was also conducted to look for pertinent cross-references from existing searched articles.
Results
Of the 1464 articles found in our search, 60 met inclusion criteria.
Psychological Disorders in Patients With Noncardiac Chest Pain in Various Settings
Psychological disorders have been identified in patients with NCCP in various clinical settings. In the following section we highlight several studies describing the prevalence of psychological conditions in NCCP in diverse clinical scenarios.
Population studies
In a Swedish population study, 231 patients (127 men and 104 women) with NCCP had higher indices of depression and anxiety than 1069 controls.9 The study participants were well matched (age: men, 45.7 years, vs women, 47.7 years, P = not significant [NS]; marital status: single men, 24.0%, vs single women, 30.0%, P = NS; university education: men, 28.0%, vs women, 25.0%, P = NS). Specifically, depression was observed in 35.0% of men and 50.0% of women vs 18.0% and 28.0% respectively in controls. Similarly, anxiety was noted in 36.0% of the men and 47.0% of the women vs 19.0% and 30.0% of the control group.9 The study used several scales to determine depression and anxiety, including the Interview Schedule for Social Interaction, Zung Self-Rating Depression Scale, and Trait-Anxiety Inventory.
Cardiology clinics
In a prospective study of 229 patients with NCCP attending a cardiology clinic, psychological disorders were noted in 75.0% of the patients.10 These patients exhibited lifetime diagnoses of anxiety (55.0%), mood disorders (44.0%), major depressive disorder (41.0%), social phobia (25.0%), and panic disorder (22.0%).10 According to Fleet and Beitman,11 among the different psychological comorbidities, panic disorder is one of the best described in association with NCCP. The most commonly reported physical causes of persistent chest pain in patients with normal coronary arteries included: microvascular angina, esophageal motility disorders, gastroesophageal reflux disease, mitral valve prolapse, and abnormal visceral nociception. Panic disorder has been found in some series as frequent as 30.0% and as high as 70.0% in patients suffering chest pain with normal coronary arteries.12 In another study of patients attending a cardiology clinic, the prevalence of psychological disorders in patients with NCCP was evaluated in 70 patients using a structured clinical interview for Diagnostic Statistical Manual of Mental Disorders-IV. The investigators noted a heterogeneous group of disorders: panic disorder (47.1%), depressive disorder (21.4%), generalized anxiety disorder (5.7%), anxiety disorder unspecified (5.7%), obsessive compulsive disorder (5.7%), and undifferentiated somatoform disorder (2.9%). As many as 13.0% of the patients had 2 psychological diagnoses simultaneously.13
Patients undergoing coronary artery angiography
In a study of 99 patients with suspected cardiac pain who underwent coronary angiography, the patients had psychological testing within 24 hours after angiography.14 Nearly two-thirds of patients with normal or near-normal coronary arteries had psychological disorders in comparison with 23.0% of those with significant coronary artery disease (CAD). The 26 men with insignificant CAD had higher scores of neuroticisms and extroversion than the 41 with important coronary occlusions.14 In a similar study of 74 patients, a psychological diagnosis was established in 79.0% of those with NCCP versus 26.0% of those without evidence of CAD.15 When comparing patients with NCCP to those with CAD, those without CAD had more panic disorder (43.0% vs 6.5%), major depression (36.0% vs 4.0%), and 2 or more phobias (36.0% vs 15.0%). Patients with NCCP were also younger and more commonly female than patients with CAD.15
Patients discharged from hospital with noncardiac chest pain
The Hospital Anxiety and Depression Scale (HADS) is a diagnostic tool to evaluate anxiety and depression in hospitalized patients and outpatients. The questionnaire consists of 14 items, 7 for depression and 7 for anxiety. In one study, patients who were discharged from the hospital with a diagnosis of NCCP and a HADS score of 8 or higher were compared with patients with a score less than 8 (control group).16 After answering the questionnaire, both groups underwent psychological evaluation. Panic disorder or depressive episodes occurred in up to 73.3% of patients with NCCP and a HADS score of 8 or higher compared with 3.9% in the control group (P < 0.001).16
Patients in the emergency department
Most studies comparing patients with NCCP to those with CAD describe a higher prevalence of psychological disorders in the NCCP groups.13,15 Eken et al17 evaluated the prevalence of depression and anxiety in patients with cardiac chest pain compared to those with NCCP presenting to an emergency department using the HADS. The reported cardiac diagnoses were stable angina, unstable angina, and acute myocardial infarction; most of the patients were diagnosed with NCCP (59.9%). They found that patients with NCCP had similar levels of anxiety, depression, and quality of life compared to those with cardiac chest pain, but worse levels than healthy controls.17 Factors associated with worse psychological outcomes include younger age, female sex, previous psychiatric history, and panic disorder.18 It is possible that psychological disorders in the emergency department are high in all patients with undifferentiated chest pain until further evaluations are completed.
Noncardiac chest pain in non-Western countries
In a study from India, 54 male inpatients in a cardiology general ward were divided into 2 groups: 1 with CAD and 1 with NCCP.19 A blinded psychological interview was conducted with the help of a structured interview schedule. Sixty-eight percent in the NCCP group and 27.0% in the CAD group had a psychological disorder, such as panic or major depression.19
In summary, most published research in diverse clinical scenarios, including developing nations, shows a high prevalence of psychological disorders in patients with NCCP. The prevalence rates range from 35.0% to 79.0%,9,15 and the psychological conditions associated with NCCP include panic disorder, anxiety, depression, somatoform conditions, social phobia, and obsessive-compulsive traits.
Possible Psychological Mechanisms
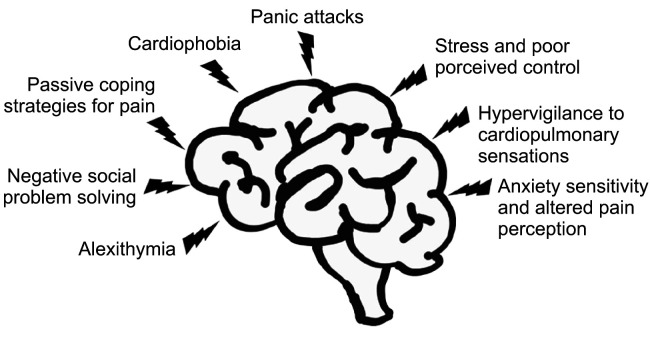
The high prevalence of psychological disorders among patients with NCCP suggests that these conditions must play either an etiologic role or contribute to perpetuating the disease. This high prevalence also raises the question as to why patients with NCCP suffer from psychological conditions. While the causes remain unclear, several studies have proposed explanations of the interrelation between NCCP and various psychological conditions, including cardiophobia,20 panic attacks,21,22 passive coping strategies for pain,23,24 negative social problem solving,25,26 hypervigilance to cardiopulmonary sensations,27 stress and poor perceived control,28,29 alexithymia and anxiety sensitivity,30,31 and altered pain perception (Table 1 and Figure).32-34
Table 1.
Potential Psychological Factors Involved in the Pathogenesis of Noncardiac Chest Pain
| Factor | Description |
|---|---|
| Cardiophobia | Recurrent pain with multiple other cardiac symptoms, mainly focused on the chest, without evidence of structural pathology |
| Panic attacks | Sudden episodes of intense fear that trigger severe physical reactions and the psychological distress derived from those attacks when there is no real danger or apparent cause |
| Passive coping strategies for pain | Conscious personal effort to change cognitive or behavioral reactions to different situations to solve internal or external problems and minimize stress |
| Negative social problem solving | Failure to identify different problems or stressful situations of daily living, involving the capacity to react, adapt, and deal with the situation |
| Hypervigilance to cardiopulmonary sensations | Increased awareness of internal body sensations |
| Stress and poor perceived control | Patterns of psychological adjustment under stress |
| Alexithymia | A deficit in the processing and regulation of emotions, making them difficult to verbalize or identify |
| Anxiety sensitivity | |
| Altered pain perception | Enhanced perception to visceral stimulation |
Figure.
Psychological mechanisms involved in the etiology of noncardiac chest pain of esophageal origin.
Psychological Therapies
The management of NCCP with psychological disorders is challenging. Those with obvious depression, anxiety, panic disorders, and somatization should be referred to a psychologist or psychiatrist. For the remaining patients, there are several treatment techniques that may be employed by a trained therapist, including cognitive behavioral therapy (CBT), hypnotherapy, relaxation training, metaphor therapy, and breathing retraining.
Cognitive behavioral therapy
CBT is a technique where a systematized approach is used to change malfunctioning cognitive patterns to improve behavior responses. During CBT, patients work with a therapist in various structured sessions aimed at learning about negative or inaccurate thinking and how to improve faulty behaviors. CBT is one of the most investigated psychological interventions for patients with NCCP (Table 2).35-40
Table 2.
Randomized Controlled Trials of Cognitive Behavioral Therapy for Noncardiac Chest Pain
| Author, year | No. of pts | No. of sessions | Results |
|---|---|---|---|
| Klimes et al, 199035 | 35 | 7.2 (average) | Significant reductions in chest pain, limitations of daily life, distress and psychological morbidity in CBT group after 4-6–month follow-up. After trial, control group patients were treated with CBT with similar symptom reduction. |
| Mayou et al, 199736 | 37 |
12 (average) Two groups: (1) outpatient investigation only, (2) admitted for coronary angiography with normal results |
Notable reduction in frequency, severity, and associated distress of symptoms and increase in social activities and quality of life maintained at 6 months in the CBT group. |
| van Peski-Oosterbaan et al, 199937 | 72 |
4-12 12-month follow-up |
Reduction of frequency and intensity of chest pain in 48% of patients in the CBT group vs 13% of the control group. |
| Jonsbu et al, 201138 | 40 |
3 First CBT for NCCP to include exposure to physical activity as part of treatment |
Improvement in fear of bodily sensations, avoidance of physical activity, and depression in CBT group. |
| van Beek et al, 201339 | 113 |
6 (45 min each) 24-week follow-up |
Significant reduction in anxiety and depressive symptoms after CBT in patients diagnosed with panic or depressive disorders who presented to a cardiac emergency unit with NCCP. |
| Mourad et al, 202240 | 109 |
5 (1 per week) 3-month follow-up |
iCBT showed long-term improvement on cardiac anxiety, health-related quality of life, and NCCP frequency vs psychoeducation alone. No difference at 5 weeks, but better outcomes with iCBT at the end of follow-up. |
CBT, cognitive behavioral therapy; iCBT, internet-delivered cognitive behavioral therapy; NCCP, noncardiac chest pain of esophageal origin; pts, patients.
Klimes et al35 evaluated the effects of CBT in 35 patients with NCCP referred by general practitioners or cardiologists (patients had persistent symptoms despite reassurance for at least 3 months). The participants were randomly allocated to a CBT group or an assessment-only control group. The average number of sessions was 7.2. They found significant reductions in chest pain, limitations of daily life, autonomic symptoms, distress, and psychological morbidity in the CBT group compared to controls.35
Mayou et al36 examined the effects of CBT in patients with NCCP during a period of 6 months. CBT was aimed at offering an alternative, noncardiac explanation of symptoms. During a maximum of 12 sessions, patients were taught how to cope with symptoms using behavioral methods and examine the problems that may be perpetuating the symptoms, including stress or anxiety caused by work, relationships, or family difficulties. Thirty-seven patients were included in the trial, 20 in the CBT group and 17 in the control group. CBT was successful in reducing frequency, severity, and associated distress of symptoms, improving mental state, changing thoughts about the causes of symptoms, and increasing social activities and quality of life. These improvements were maintained for up to 6 months in the CBT group.36
van Peski-Oosterbaan et al37 evaluated the frequency and intensity of chest pain at 6 and 12 months in 72 patients with NCCP (31 assigned to CBT and 33 to usual care). Fifteen of 31 patients (48.4%) in the CBT group were pain free at 12-month follow-up compared with 4 of 33 patients (12.1%) in the control group (P = 0.002).37
Jonsbu et al38 studied the effects of a 3-session manualized CBT intervention with normal care for patients with NCCP or benign palpitations in a randomized controlled trial. Forty patients were enrolled (21 in the intervention group and 19 in the control group). The first session focused on physical symptoms, the second session exposed patients to physical activity on a treadmill, and the third session concentrated on avoidance of behavior and patients’ interpretations of their symptoms. The patients were followed for 12 months. The authors found significant improvement in the CBT group regarding fear of bodily sensations, avoidance of physical activity, and depression.38
van Beek et al39 investigated the effects of a brief CBT intervention in patients who presented to a cardiac emergency unit with NCCP, were diagnosed with panic or depressive disorder using the Mini International Neuropsychiatric Interview, and had HADS scores of 8 or higher. A CBT group (n = 60) given 6 sessions of 45 minutes each was compared to a control group (n = 53) only receiving reassurance from the cardiologist that the symptoms were not caused by cardiac disease (did not receive psychotherapy, CBT, or antidepressants). After 24 weeks of follow-up, they found that CBT was superior to no treatment, reducing disease severity assessed with a clinical global inventory (P < 0.001). Overall, data suggest that CBT improves chest pain parameters and may also improve anxiety and depressive symptoms.39
A more recent study investigated the effects of internet-delivered CBT (iCBT) and psychoeducation on cardiac anxiety (evaluated by a Cardiac Anxiety Questionnaire score ≥ 24) and patient-reported outcomes (fear of bodily sensations, depressive symptoms, health-related quality of life, and chest pain frequency) in patients with NCCP.40 Patients were randomized to either iCBT for 5 weeks (n = 54) or psychoeducation (n = 55) and were followed for 3 months. The authors found improvement with both therapies, with no significant differences between the iCBT and psychoeducation groups in the short term. However, 36.0% of the patients in the iCBT group reported improvement on cardiac anxiety (Cohen d = 0.31), with a positive reliable change in score (≥ 11 points on the Cardiac Anxiety Questionnaire) compared to 27.0% in the psychoeducation group. There was also significant within-group analysis improvement in cardiac anxiety (P = 0.040) at 3-month follow-up in the iCBT group. The authors concluded that iCBT tends to have better long-term effects on cardiac anxiety, health-related quality of life, and NCCP frequency than psychoeducation.40
Hypnotherapy
Hypnosis is an induced mental process where the central nervous system is silenced and a hypervigilant, hypersuggestive state emerges with the potential to induce changes in physical, emotional, and behavioral patterns.41 Hypnotherapy has been used in multiple clinical scenarios and has been shown to be effective in depressive disorders,42 anxiety and stress-related disorders,43 irritable bowel syndrome,44 and multiple pain syndromes including fibromyalgia,45 osteoarthritis-related pain,46 sickle cell disease–associated pain,47 and chronic pain.48
Jones et al49 addressed the efficacy of hypnotherapy in a group of 28 patients with NCCP. Patients were randomized to receive either 12 sessions of hypnotherapy or supportive therapy plus placebo medication over a 17-week period. More patients (80.0%) in the hypnotherapy group experienced a global improvement in pain (P = 0.008) associated with a significantly greater reduction in pain intensity (P = 0.046), compared to 23.0% in the control group.49 The same authors published a 2-year follow-up report of the same cohort after stopping treatment.50 Patients who received hypnotherapy had further improvement, with 93.0% classified as responders compared to 23.0% in the control group (P = 0.001).50 While the results of this approach appear promising, studies with larger sample sizes are needed to confirm these observations.
Relaxation training and metaphor therapy
Relaxation training is a technique where attention is focused on calming or relaxing thoughts to increase body awareness. Metaphor therapy is a type of psychotherapy that explores patient’s perception about aspects of life, irrational beliefs, and personal meaning, where the patient’s beliefs about their medical condition are challenged. Metaphoric stories are created for the patient to symbolically express their feelings about their medical conditions to improve symptoms and feelings of hopelessness.51
A randomized controlled trial investigated the use of relaxation training versus metaphor therapy in patients with NCCP.52 Thirty-three patients divided into 3 groups: relaxation training (n = 13), metaphor therapy (n = 10), and control (n = 10). Patients were followed for 4 weeks. The authors found that the patients in the relaxation training group showed more improvement in symptoms compared to the control and metaphor therapy groups, and the metaphor therapy group did not show significant improvement.52 However, this was a small study performed for a short time. Another study investigating the effects of metaphor therapy in depression, anxiety, stress, and pain discomfort in patients with NCCP found no significant benefit.53 Larger clinical trials are needed to determine if these techniques are of benefit in NCCP.
Breathing retraining
Respiratory biofeedback–assisted therapy has been studied in panic disorder. The rationale is that sustained hypocapnia resulting from hyperventilation is a key mechanism in the production and maintenance of panic.54 DeGuire et al55 performed a randomized controlled trial of 37 patients with NCCP classified into 4 groups: (1) guided breathing retraining and physiologic monitoring of diaphragmatic breathing and end-tidal CO2, (2) guided breathing retraining and physiologic monitoring of diaphragmatic breathing, (3) guided breathing retraining, and (4) no treatment (control group). Regardless of the type of breathing retraining, the number of symptomatic days decreased after treatment.55
The same authors published a 3-year follow-up study involving a cohort of 10 patients from their original group.56 Their results indicated that breathing retraining had lasting effects on respiratory parameters measured and the patients continued to report a decrease in the frequency of chest pain.56 Larger randomized trials are needed to confirm these findings.
Systematic Review of Psychological Interventions
A Cochrane systematic review of the literature by Kisely et al57 was performed to evaluate psychological intervention in NCCP. Seventeen randomized control trials including 1006 patients with NCCP were evaluated. The psychological techniques used for the treatment of NCCP were heterogeneous and included CBT, relaxation therapy, hyperventilation control, hypnotherapy, and other psychotherapy or counselling, with standard care, attention placebo, waiting list, or no intervention as the control conditions. The authors found a modest to moderate benefit for psychological interventions, particularly CBT, which was largely restricted to the first 3 months after treatment, with a random-effects relative risk = 0.70 (95% CI, 0.53 to 0.92). Hypnotherapy was considered a possible alternative, but the evidence for other interventions was less clear. The authors concluded that more randomized controlled trials with longer follow-up periods (at least 12 months) are needed.57
Other Nontraditional Therapies
Although acupuncture has been shown to be effective in many clinical pain scenarios,58 it has not been studied in NCCP and may be a potential target of investigation in these patients. A survey administered to 235 patients with NCCP with a 69.0% return rate indicated that 42.0% would consider acupuncture.59
Johrei is a Japanese ritual consisting of spiritual purification and transmission of healing energy. In a randomized controlled trial, Gasiorowska et al60 compared the effects of Johrei (21 patients) to a waiting-list control group (18 patients). After 18 sessions, there was a significant posttreatment reduction in symptom intensity in the Johrei group (20.28 vs 7.00, P = 0.0023) compared to the control group (23.06 vs 20.69, P = NS).60
Noncardiac Chest Pain and Persistent Physical Symptoms
Flóvenz et al61 studied patients with NCCP as a persistent physical symptom (PPS) in an attempt to better classify and identify patients with NCCP who may benefit from psychological interventions. They found that approximately 30.0% of patients with NCCP met criteria for PPS; these patients were more likely to have more symptoms of anxiety and depression, to be inactive or unable to work, and had a higher number of other PPS. They suggested these patients were more likely to respond to psychological therapies such as CBT.
Summary
NCCP represents a global health care burden affecting 80 million people in the US each year. There is ample information regarding the diverse causes of NCCP; however, the role of psychological disorders has not been systematically described. We performed a comprehensive search using PubMed to identify the relevant literature linking psychological disorders to NCCP. Between 35.0% and 79.0% of patients with NCCP suffer from psychological disorders. These psychological disorders are heterogeneous and include depression, anxiety, panic disorder, somatization, and obsessive-compulsive disorder. It is unclear why psychological disorders are so common in NCCP. Several mechanisms have been proposed related to the pathogenesis of chest pain in NCCP. Whether the psychological disorders trigger the chest pain or vice versa is not known. A series of therapeutic modalities have been used to treat patients with NCCP and psychological disorders. CBT is the better studied technique, and the results of the investigations suggest a beneficial role in NCCP. However, further studies are required to examine the optimal therapeutic strategies needed for the effective treatment of NCCP with psychological disorders.
Footnotes
Financial support: None.
Conflicts of interest: None.
Author contributions: Sami R Achem supervised the project; Fernando Gonzalez-Ibarra and Sami R Achem contributed to conceptualization, contributed to the visualization, and wrote the original draft; Fernando Gonzalez-Ibarra curated the data, set the methodology, and performed the investigation; and Mauricio Cruz-Ruiz, Joel Murillo Llanes, Sami R Achem, and Ronnie Fass critically reviewed and edited the manuscript.
References
- 1.Pitts SR, Niska RW, Xu J, Burt CW. National hospital ambulatory medical care survey: 2006 emergency department summary. Natl Health Stat Report. 2008:1–38. doi: 10.3886/icpsr28321.v1. [DOI] [PubMed] [Google Scholar]
- 2.Eslick GD, Talley NJ. Non-cardiac chest pain: squeezing the life out of the Australian healthcare system? Med J Aust. 2000;173:233–234. doi: 10.5694/j.1326-5377.2000.tb125626.x. [DOI] [PubMed] [Google Scholar]
- 3.Wong WM, Lam KF, Cheng C, et al. Population based study of noncardiac chest pain in southern Chinese: prevalence, psychosocial factors and health care utilization. World J Gastroenterol. 2004;10:707–712. doi: 10.3748/wjg.v10.i5.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fass R, Achem SR. Noncardiac chest pain: epidemiology, natural course and pathogenesis. J Neurogastroenterol Motil. 2011;17:110–123. doi: 10.5056/jnm.2011.17.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richter JE, Bradley LA, Castell DO. Esophageal chest pain: current controversies in pathogenesis, diagnosis, and therapy. Ann Intern Med. 1989;110:66–78. doi: 10.7326/0003-4819-110-1-66. [DOI] [PubMed] [Google Scholar]
- 6.Mourad G, Alwin J, Strömberg A, Jaarsma T. Societal costs of non-cardiac chest pain compared with ischemic heart disease--a longitudinal study. BMC Health Serv Res. 2013;13:403. doi: 10.1186/1472-6963-13-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fass R, Achem SR. Noncardiac chest pain: diagnostic evaluation. Dis Esophagus. 2012;25:89–101. doi: 10.1111/j.1442-2050.2011.01225.x. [DOI] [PubMed] [Google Scholar]
- 8.Ho KY, Kang JY, Yeo B, Ng WL. Non-cardiac, non-oesophageal chest pain: the relevance of psychological factors. Gut. 1998;43:105–110. doi: 10.1136/gut.43.1.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fagring AJ, Kjellgren KI, Rosengren A, Lissner L, Manhem K, Welin C. Depression, anxiety, stress, social interaction and health-related quality of life in men and women with unexplained chest pain. BMC Public Health. 2008;8:165. doi: 10.1186/1471-2458-8-165.07df97676b274a6a9dcfd9db70ccb3a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White KS, Raffa SD, Jakle KR, et al. Morbidity of DSM-IV Axis I disorders in patients with noncardiac chest pain: psychiatric morbidity linked with increased pain and health care utilization. J Consult Clin Psychol. 2008;76:422–430. doi: 10.1037/0022-006X.76.3.422. [DOI] [PubMed] [Google Scholar]
- 11.Fleet RP, Beitman BD. Unexplained chest pain: when is it panic disorder? Clin Cardiol. 1997;20:187–194. doi: 10.1002/clc.4960200303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beitman BD, Mukerji V, Lamberti JW, et al. Panic disorder in patients with chest pain and angiographically normal coronary arteries. Am J Cardiol. 1989;63:1399–1403. doi: 10.1016/0002-9149(89)91056-4. [DOI] [PubMed] [Google Scholar]
- 13.Hocaoglu C, Gulec MY, Durmus I. Psychiatric comorbidity in patients with chest pain without a cardiac etiology. Isr J Psychiatry Relat Sci. 2008;45:49–54. [PubMed] [Google Scholar]
- 14.Bass C, Wade C. Chest pain with normal coronary arteries: a comparative study of psychiatric and social morbidity. Psychol Med. 1984;14:51–61. doi: 10.1017/S003329170000307X. [DOI] [PubMed] [Google Scholar]
- 15.Katon W, Hall ML, Russo J, et al. Chest pain: relationship of psychiatric illness to coronary arteriographic results. Am J Med. 1988;84:1–9. doi: 10.1016/0002-9343(88)90001-0. [DOI] [PubMed] [Google Scholar]
- 16.Kuijpers PM, Denollet J, Lousberg R, Wellens HJ, Crijns H, Honig A. Validity of the hospital anxiety and depression scale for use with patients with noncardiac chest pain. Psychosomatics. 2003;44:329–335. doi: 10.1176/appi.psy.44.4.329. [DOI] [PubMed] [Google Scholar]
- 17.Eken C, Oktay C, Bacanli A, et al. Anxiety and depressive disorders in patients presenting with chest pain to the emergency department: a comparison between cardiac and non-cardiac origin. J Emerg Med. 2010;39:144–150. doi: 10.1016/j.jemermed.2007.11.087. [DOI] [PubMed] [Google Scholar]
- 18.Webster R, Norman P, Goodacre S, Thompson A. The prevalence and correlates of psychological outcomes in patients with acute non-cardiac chest pain: a systematic review. Emerg Med J. 2012;29:267–273. doi: 10.1136/emermed-2011-200526. [DOI] [PubMed] [Google Scholar]
- 19.Alexander PJ, Prabhu SG, Krishnamoorthy ES, Halkatti PC. Mental disorders in patients with noncardiac chest pain. Acta Psychiatr Scand. 1994;89:291–293. doi: 10.1111/j.1600-0447.1994.tb01517.x. [DOI] [PubMed] [Google Scholar]
- 20.Zvolensky MJ, Feldner MT, Eifert GH, Vujanovic AA, Solomon SE. Cardiophobia: a critical analysis. Transcult Psychiatry. 2008;45:230–252. doi: 10.1177/1363461508089766. [DOI] [PubMed] [Google Scholar]
- 21.Beitman BD, Basha I, Flaker G, DeRosear L, Mukerji V, Lamberti J. Non-fearful panic disorder: panic attacks without fear. Behav Res Ther. 1987;25:487–492. doi: 10.1016/0005-7967(87)90056-8. [DOI] [PubMed] [Google Scholar]
- 22.Huffman JC, Pollack MH, Stern TA. Panic disorder and chest pain: mechanisms, morbidity, and management. Prim Care Companion J Clin Psychiatry. 2002;4:54–62. doi: 10.4088/PCC.v04n0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Husser D, Bollmann A, Kühne C, Molling J, Klein HU. Evaluation of noncardiac chest pain: diagnostic approach, coping strategies and quality of life. Eur J Pain. 2006;10:51–55. doi: 10.1016/j.ejpain.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 24.Vitaliano PP, Katon W, Maiuro RD, Russo J. Coping in chest pain patients with and without psychiatric disorders. J Consult Clin Psychol. 1989;57:338–343. doi: 10.1037/0022-006X.57.3.338. [DOI] [PubMed] [Google Scholar]
- 25.Nezu AM, Nezu CM, Jain D. Social problem solving as a mediator of the stress-pain relationship among individuals with noncardiac chest pain. Health Psychol. 2008;27:829–832. doi: 10.1037/0278-6133.27.6.829. [DOI] [PubMed] [Google Scholar]
- 26.Nezu AM, Nezu CM, Jain D, et al. Social problem solving and noncardiac chest pain. Psychosom Med. 2007;69:944–951. doi: 10.1097/PSY.0b013e31815a995a. [DOI] [PubMed] [Google Scholar]
- 27.White KS, Craft JM, Gervino EV. Anxiety and hypervigilance to cardiopulmonary sensations in non-cardiac chest pain patients with and without psychiatric disorders. Behav Res Ther. 2010;48:394–401. doi: 10.1016/j.brat.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aikens JE, Zvolensky MJ, Eifert GH. Differential fear of cardiopulmonary sensations in emergency room noncardiac chest pain patients. J Behav Med. 2001;24:155–167. doi: 10.1023/A:1010710614626. [DOI] [PubMed] [Google Scholar]
- 29.Rosenbaum DL, White KS, Gervino EV. The impact of perceived stress and perceived control on anxiety and mood disorders in noncardiac chest pain. J Health Psychol. 2012;17:1183–1192. doi: 10.1177/1359105311433906. [DOI] [PubMed] [Google Scholar]
- 30.Spitzer C, Siebel-Jurges U, Barnow S, Grabe HJ, Freyberger HJ. Alexithymia and interpersonal problems. Psychother Psychosom. 2005;74:240–246. doi: 10.1159/000085148. [DOI] [PubMed] [Google Scholar]
- 31.White KS, McDonnell CJ, Gervino EV. Alexithymia and anxiety sensitivity in patients with non-cardiac chest pain. J Behav Ther Exp Psychiatry. 2011;42:432–439. doi: 10.1016/j.jbtep.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hollerbach S, Bulat R, May A, et al. Abnormal cerebral processing of oesophageal stimuli in patients with noncardiac chest pain (NCCP) Neurogastroenterol Motil. 2000;12:555–565. doi: 10.1046/j.1365-2982.2000.00230.x. [DOI] [PubMed] [Google Scholar]
- 33.Mehta AJ, De Caestecker JS, Camm AJ, Northfield TC. Sensitization to painful distention and abnormal sensory perception in the esophagus. Gastroenterology. 1995;108:311–319. doi: 10.1016/0016-5085(95)90055-1. [DOI] [PubMed] [Google Scholar]
- 34.Orlando RC. Esophageal perception and noncardiac chest pain. Gastroenterol Clin North Am. 2004;33:25–33. doi: 10.1016/S0889-8553(03)00133-X. [DOI] [PubMed] [Google Scholar]
- 35.Klimes I, Mayou RA, Pearce MJ, Coles L, Fagg JR. Psychological treatment for atypical non-cardiac chest pain: a controlled evaluation. Psychol Med. 1990;20:605–611. doi: 10.1017/S0033291700017116. [DOI] [PubMed] [Google Scholar]
- 36.Mayou RA, Bryant BM, Sanders D, Bass C, Klimes I, Forfar C. A controlled trial of cognitive behavioural therapy for non-cardiac chest pain. Psychol Med. 1997;27:1021–1031. doi: 10.1017/S0033291797005254. [DOI] [PubMed] [Google Scholar]
- 37.van Peski-Oosterbaan AS, Spinhoven P, van Rood Y, van der Does JW, Bruschke AV, Rooijmans HG. Cognitive-behavioral therapy for noncardiac chest pain: a randomized trial. Am J Med. 1999;106:424–429. doi: 10.1016/S0002-9343(99)00049-2. [DOI] [PubMed] [Google Scholar]
- 38.Jonsbu E, Dammen T, Morken G, Moum T, Martinsen EW. Short-term cognitive behavioral therapy for non-cardiac chest pain and benign palpitations: a randomized controlled trial. J Psychosom Res. 2011;70:117–123. doi: 10.1016/j.jpsychores.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 39.van Beek MH, Oude Voshaar RC, Beek AM, et al. A brief cognitive-behavioral intervention for treating depression and panic disorder in patients with noncardiac chest pain: a 24-week randomized controlled trial. Depress Anxiety. 2013;30:670–678. doi: 10.1002/da.22106. [DOI] [PubMed] [Google Scholar]
- 40.Mourad G, Eriksson-Liebon M, Karlström P, Johansson P. The effect of internet-delivered cognitive behavioral therapy versus psychoeducation only on psychological distress in patients with noncardiac chest pain: randomized controlled trial. J Med Internet Res. 2022;24:e31674. doi: 10.2196/31674.0eafe3bd09bb46edb0cd3352408410db [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jiang H, White MP, Greicius MD, Waelde LC, Spiegel D. Brain activity and functional connectivity associated with hypnosis. Cereb Cortex. 2017;27:4083–4093. doi: 10.1093/cercor/bhw220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shih M, Yang YH, Koo M. A meta-analysis of hypnosis in the treatment of depressive symptoms: a brief communication. Int J Clin Exp Hypn. 2009;57:431–442. doi: 10.1080/00207140903099039. [DOI] [PubMed] [Google Scholar]
- 43.Hammond DC. Hypnosis in the treatment of anxiety- and stress-related disorders. Expert Rev Neurother. 2010;10:263–273. doi: 10.1586/ern.09.140. [DOI] [PubMed] [Google Scholar]
- 44.Whorwell PJ. Hypnotherapy for irritable bowel syndrome: the response of colonic and noncolonic symptoms. J Psychosom Res. 2008;64:621–623. doi: 10.1016/j.jpsychores.2008.02.022. [DOI] [PubMed] [Google Scholar]
- 45.Bernardy K, Füber N, Klose P, Häuser W. Efficacy of hypnosis/guided imagery in fibromyalgia syndrome--a systematic review and meta-analysis of controlled trials. BMC Musculoskelet Disord. 2011;12:133. doi: 10.1186/1471-2474-12-133.cb7aca33e7c548578c1791b887013349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gay MC, Philippot P, Luminet O. Differential effectiveness of psychological interventions for reducing osteoarthritis pain: a comparison of Erikson [correction of Erickson] hypnosis and Jacobson relaxation. Eur J Pain. 2002;6:1–16. doi: 10.1053/eujp.2001.0263. [DOI] [PubMed] [Google Scholar]
- 47.Dinges DF, Whitehouse WG, Orne EC, et al. Self-hypnosis training as an adjunctive treatment in the management of pain associated with sickle cell disease. Int J Clin Exp Hypn. 1997;45:417–432. doi: 10.1080/00207149708416141. [DOI] [PubMed] [Google Scholar]
- 48.Elkins G, Jensen MP, Patterson DR. Hypnotherapy for the management of chronic pain. Int J Clin Exp Hypn. 2007;55:275–287. doi: 10.1080/00207140701338621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jones H, Cooper P, Miller V, Brooks N, Whorwell PJ. Treatment of non-cardiac chest pain: a controlled trial of hypnotherapy. Gut. 2006;55:1403–1408. doi: 10.1136/gut.2005.086694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miller V, Jones H, Whorwell PJ. Hypnotherapy for non-cardiac chest pain: long-term follow-up. Gut. 2007;56:1643. doi: 10.1136/gut.2007.132621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Landau MJ. Using metaphor to find meaning in life. Rev Gen Psychol. 2018;22:62–72. doi: 10.1037/gpr0000105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bahremand M, Moradi G, Saeidi M, Mohammadi S, Komasi S. Reducing irrational beliefs and pain severity in patients suffering from non-cardiac chest pain (NCCP): a comparison of relaxation training and metaphor therapy. Korean J Pain. 2015;28:88–95. doi: 10.3344/kjp.2015.28.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bahremand M, Saeidi M, Komasi S. How effective is the use of metaphor therapy on reducing psychological symptoms and pain discomfort in patients with non-cardiac chest pain: a randomized, controlled trial. J Cardiothorac Med. 2016;4:444–449.6731aa9570d44bac98a4e849a97f83e9 [Google Scholar]
- 54.Meuret AE, Wilhelm FH, Roth WT. Respiratory feedback for treating panic disorder. J Clin Psychol. 2004;60:197–207. doi: 10.1002/jclp.10245. [DOI] [PubMed] [Google Scholar]
- 55.DeGuire S, Gevirtz R, Kawahara Y, Maguire W. Hyperventilation syndrome and the assessment of treatment for functional cardiac symptoms. Am J Cardiol. 1992;70:673–677. doi: 10.1016/0002-9149(92)90211-G. [DOI] [PubMed] [Google Scholar]
- 56.DeGuire S, Gevirtz R, Hawkinson D, Dixon K. Breathing retraining: a three-year follow-up study of treatment for hyperventilation syndrome and associated functional cardiac symptoms. Biofeedback Self Regul. 1996;21:191–198. doi: 10.1007/BF02284695. [DOI] [PubMed] [Google Scholar]
- 57.Kisely SR, Campbell LA, Yelland MJ, Paydar A. Psychological interventions for symptomatic management of non-specific chest pain in patients with normal coronary anatomy. Cochrane Database Syst Rev. 2015;2015:CD004101. doi: 10.1002/14651858.CD004101.pub5. [DOI] [PubMed] [Google Scholar]
- 58.Lee MS, Ernst E. Acupuncture for pain: an overview of cochrane reviews. Chin J Integr Med. 2011;17:187–189. doi: 10.1007/s11655-011-0665-7. [DOI] [PubMed] [Google Scholar]
- 59.Macpherson H, Dumville JC. Acupuncture as a potential treatment for non-cardiac chest pain--a survey. Acupunct Med. 2007;25:18–21. doi: 10.1136/aim.25.1-2.18. [DOI] [PubMed] [Google Scholar]
- 60.Gasiorowska A, Navarro-Rodriguez T, Dickman R, et al. Clinical trial: the effect of Johrei on symptoms of patients with functional chest pain. Aliment Pharmacol Ther. 2009;29:126–134. doi: 10.1111/j.1365-2036.2008.03859.x. [DOI] [PubMed] [Google Scholar]
- 61.Flóvenz SÓ, Salkovskis P, Svansdóttir E, Karlsson HD, Andersen K, Sigurðsson JF. Non-cardiac chest pain as a persistent physical symptom: psychological distress and workability. Int J Environ Res Public Health. 2023;20:2521. doi: 10.3390/ijerph20032521. [DOI] [PMC free article] [PubMed] [Google Scholar]