Abstract
BACKGROUND
The common cause of sodium nitrite poisoning has shifted from previous accidental intoxication by exposure or ingestion of contaminated water and food to recent alarming intentional intoxication as an employed method of suicide/exit. The subsequent formation of methemoglobin (MetHb) restricts oxygen transport and utilization in the body, resulting in functional hypoxia at the tissue level. In clinical practice, a mismatch of cyanotic appearance and oxygen partial pressure usually contributes to the identification of methemoglobinemia. Prompt recognition of characteristic mismatch and accurate diagnosis of sodium nitrite poisoning are prerequisites for the implementation of standardized systemic interventions.
CASE SUMMARY
A pregnant woman was admitted to the Department of Critical Care Medicine at the First Affiliated Hospital of Harbin Medical University due to consciousness disorders and drowsiness 2 h before admission. Subsequently, she developed vomiting and cyanotic skin. The woman underwent orotracheal intubation, invasive mechanical ventilation (IMV), and correction of internal environment disturbance in the ICU. Her premature infant was born with a higher-than-normal MetHb level of 3.3%, and received detoxification with methylene blue and vitamin C, supplemental vitamin K1, an infusion of fresh frozen plasma, as well as respiratory support via orotracheal intubation and IMV. On day 3 after admission, the puerpera regained consciousness, evacuated the IMV, and resumed enteral nutrition. She was then transferred to the maternity ward 24 h later. On day 7 after admission, the woman recovered and was discharged without any sequelae.
CONCLUSION
MetHb can cross through the placental barrier. Level of MetHb both reflects severity of the sodium nitrite poisoning and serves as feedback on therapeutic effectiveness.
Keywords: Sodium nitrite poisoning, Methemoglobinemia, Methemoglobin, Third trimester puerpera, Premature infant, Placental barrier, Methylene blue, Case report
Core Tip: This study is the first to present rare cases of acquired methemoglobinemia in pregnant women in the third trimester of pregnancy and in premature infants with high suspicion of sodium nitrite poisoning, revealing that methemoglobin (MetHb) can quickly cross the placental barrier. MetHb levels not only reflect the severity of sodium nitrite poisoning, but also serve as feedback on the effectiveness of treatment. However, fatal outcomes in patients with sodium nitrite poisoning are related to potential comorbidities of poor health at advanced age and worsening organ function, not just the poisoning itself, which requires greater attention from medical personnel.
INTRODUCTION
The common cause of sodium nitrite poisoning has shifted from previous accidental intoxication by exposure or ingestion of contaminated water and food to recent alarming intentional intoxication as an employed method of suicide/exit[1-4]. Online forums and social media have reported many cases of intentional poisoning by nitrites[5,6].
As a powerful oxidizing agent, sodium nitrite in excess of safe dose can restrict oxygen transport and utilization in the body through the formation of methemoglobin (MetHb) by oxidizing the ferrous iron (Fe2+) in normal hemoglobin to the ferric iron (Fe3+). This results in a mismatch of cyanotic appearance and oxygen partial pressure (PO2), and damage to oxygen-intensive vital organs[7,8]. Prompt recognition of characteristic mismatch and accurate diagnosis of sodium nitrite poisoning are prerequisites for the implementation of standardized systemic interventions. Furthermore, due to allosteric changes to hemoglobin molecules during oxidation, there is an increase in affinity between partially oxidized hemoglobin molecules and oxygen, triggering a left shift to the oxygen-hemoglobin dissociation curve, and resulting in a further impairment of oxygen delivery to the systemic tissue[9]. Additionally, oxidation of sodium nitrite can independently induce hemolysis, destroy oxygen carriers, and further deteriorate oxygen transport[10,11]. Nitric oxide (NO), as a metabolite of sodium nitrite, can also exert vasodilation in the peripheral blood vessels, leading to hypotension, which elicits further difficulties to oxygen transport[12,13].
The fatal consequences of patients with sodium nitrite poisoning can also be attributed to advanced age, poor health condition, underlying comorbidities, and deteriorating organ function[14]. However, there have been no clinical cases of MetHb crossing through the placental barrier to date. Herein, we present a rare case of acquired methemoglobinemia in a third trimester puerpera and her premature infant with sodium nitrite poisoning.
CASE PRESENTATION
Chief complaints
A puerpera, approximately 40-years-old, was admitted to the Department of Critical Care Medicine at the First Affiliated Hospital of Harbin Medical University due to consciousness disorder and drowsiness 2 h before admission.
History of present illness
Two hours before admission, the puerpera developed consciousness disorder and drowsiness, followed by vomiting and cyanotic skin.
History of past illness
The woman was 34 wk of gestation on admission, and began to feel fetal movement from week 20 of suppressio mensiun, which was active until then. There was no history of exposure to toxins, radiation, or pets in the first trimester, and no lightheadedness in the third trimester. There was also no history of comorbidities.
Personal and family history
The woman had no personal or family history and no exposure to any known toxins or drugs. Further investigation revealed that a small amount of sodium nitrite remained in a warehouse after pickling vegetables in the autumn, but the exact amount was unknown.
Physical examination
Physical examination of the puerpera on admission showed the following: temperature, 36.2 °C; heart rate, 104 bpm; respiratory rate, 28 bpm; blood pressure, 120/72 mmHg; blood oxygen saturation, 90%; needlepoint pupils; cyanosis on the lips; acral skin; respiratory distress; rough breath sound in both lungs; and Glasgow coma score, 9 points. An obstetric examination revealed the following: Abdominal shape in the third trimester with uterine height of 30 cm and abdominal circumference of 98 cm; fetal heart rate, 128 bpm; and no uterine contraction, vaginal bleeding, nor discharge. Blood drawn from the veins and arteries was noted to have a dark red appearance.
Physical examination of the premature infant after birth showed the following: Weight, 2550 g; height, 48 cm; heart rate, 130 bpm; blood pressure, 69/37 mmHg; no spontaneous breathing; cyanotic skin; weak breath sounds in both lungs after orotracheal intubation and invasive mechanical ventilation (IMV); three depressions sign; diminution of cardiac sounds; grade 2/6 systolic murmurs in the precardiac region; low muscle tone in the extremities; and a vanishing Moro reflex. Apgar scores at 1 min and 5 min after birth were 2 and 5 points, respectively.
Laboratory examinations
The laboratory parameters of the puerpera on admission and during hospitalization are displayed in Table 1. Arterial blood gas (ABG) analysis showed that carbon dioxide partial pressure (PCO2), PO2, potassium ion (K+), chloridion (Cl-), free calcium ion (Ca2+), lactic acid, and MetHb were 26.7 mmHg, 115 mmHg, 2.6 mmol/L, 111 mmol/L, 1.08 mmol/L, 4.2 mmol/L, and 28.8%, respectively. Sequential organ failure assessment score on admission was 4 points. No bromadiolone, fluoroacetic acid, or estazolam were detected in the blood of the puerpera.
Table 1.
Timeline of the disease course of the puerpera (December 14 to 20, 2021)
|
Parameter
|
Day 1
|
|
Day 2
|
Day 3
|
Day 4
|
Day 5
|
Day 6
|
Day 7
|
| Disease course | Hospitalization/ICU | Maternity ward | Hospital discharge | |||||
| WBC as × 109/L | 13.64 | 15.78 | 12.24 | 11.39 | 10.12 | 6.82 | 4.77 | |
| NEUT as % | 74.00 | 87.5 | 80.6 | 83.6 | 81.4 | 75.6 | 60.7 | |
| NEUT as × 109/L | 10.09 | 13.82 | 9.87 | 9.52 | 8.24 | 5.15 | 2.9 | |
| LYMPH as % | 18.80 | 6.2 | 11.1 | 8.8 | 12.5 | 15.2 | 25.6 | |
| HGB in g/L | 119.00 | 99.00 | 85.00 | 74.00 | 63.00 | 76.00 | 79.00 | |
| D-dimer in μg/mL | 2.49 | NP | 5.88 | 5.41 | 4.02 | NP | 2.15 | |
| TP in g/L | 73.84 | 56.70 | 54.50 | 50.40 | 50.60 | NP | 55.10 | |
| ALB in g/L | 38.63 | 33.10 | 31.57 | 28.81 | 30.60 | NP | 31.90 | |
| BUN in mmol/L | 1.88 | 2.33 | 2.95 | 5.3 | 5.36 | NP | 4.15 | |
| Cr in μmol/L | 30.16 | 32.60 | 43 | 55.6 | 34.50 | NP | 33.90 | |
| GLU in mmol/L | 30.16 | 7.7 | 6.1 | 5.8 | 4.0 | NP | 4.44 | |
| Mg2+ in mmol/L | 0.82 | 0.71 | NP | NP | NP | NP | 0.73 | |
| CRP in mg/L | 8.86 | 45.9 | 62.5 | 34.1 | 17.1 | |||
| PCT in ng/mL | 0.17 | 0.18 | 0.18 | 0.12 | 0.06 | 0.04 | ||
| Oxygen therapy | Nasal catheter oxygen therapy | IMV | HFNC | Nasal catheter oxygen therapy | ||||
| FiO2 | 5 L/min | 80% | 55% | 40% | 4 L/min | 3 L/min | 1 L/min | |
| PEEP in cmH2O | 10 | 5 | NP | NP | NP | NP | ||
| PO2 in mmHg | 115 | 200 | 146 | 196 | 185 | 157 | 101 | |
| OI in mmHg | 280.49 | 250 | 265.45 | 490 | 500 | 475.76 | 404 | |
| PCO2 in mmHg | 26.7 | 24.4 | 35 | 33 | 37.6 | 39.6 | 39.3 | |
| LAC in mmol/L | 4.2 | 1.2 | 1.4 | 0.6 | 0.6 | 0.7 | ||
| MetHb | 28.8% | 18.2% | 17.7% | 2.2% | 0.9% | 1% |
ALB: Albumin; BUN: Blood urea nitrogen; Cr: Creatinine; CRP: C-reactive protein; GLU: Glucose; HFNC: High-flow nasal cannula oxygen therapy; HGB: Hemoglobin; ICU: Intensive care unit; IMV: Invasive mechanical ventilation; LAC: Lactic acid; LYMPH: Lymphocyte; MetHb: Methemoglobin; NEUT: Neutrophil; NP: Not performed; OI: Oxygenation index; PCO2: Carbon dioxide partial pressure; PCT: Procalcitonin; PEEP: Positive end-expiratory pressure; PO2: Oxygen partial pressure; TP: Total protein; WBC: White blood cell.
The laboratory parameters of the premature infant after birth and during hospitalization are exhibited in Table 2. ABG analysis after orotracheal intubation and IMV showed that PCO2, PO2, K+, sodium ion (Na+), bicarbonate ion (HCO3-), base excess, and MetHb were 13.8 mmHg, 136 mmHg, 3.0 mmol/L, 183 mmol/L, 7.6 mmol/L, -18.0 mmol/L, and 3.3%, respectively.
Table 2.
Timeline of the disease course of the premature infant (December 14 to 19, 2021)
|
Parameter
|
Day 1
|
Day 2
|
Day 3
|
Day 5
|
Day 6
|
| Disease course | Neonatal ICU | Clinical death | |||
| WBC as × 109/L | 7.58 | 23.17 | 11.51 | 12.67 | |
| NEUT% | 53.80 | 64.90 | 64.50 | 80.00 | |
| NEUT as × 109/L | 4.08 | 15.06 | 7.42 | 10.14 | |
| LYMPH% | 36.80 | 19.70 | 15.60 | 12.1 | |
| HGB in g/L | 182.00 | 165.00 | 96.00 | 93.00 | |
| PLT as × 109/L | 223.00 | 294.00 | 168.00 | 108.00 | |
| PT in s | 71.90 | NP | 22.90 | NP | |
| PT as % | 10.00 | NP | 39.90 | NP | |
| INR | 6.16 | NP | 1.79 | NP | |
| FIB in g/L | 1.42 | NP | 0.69 | NP | |
| APTT in s | 41.30 | NP | 41.00 | NP | |
| TT in s | 14.80 | NP | 19.20 | NP | |
| D-dimer in μg/mL | 1.69 | NP | 5.13 | NP | |
| TP in g/L | 44.55 | NP | 42.20 | NP | |
| ALB in g/L | 26.83 | NP | 31.10 | NP | |
| AST in U/L | 49.18 | NP | 165.30 | NP | |
| ALT in U/L | 20.64 | NP | 55.10 | NP | |
| BUN in mmol/L | 2.84 | NP | 12.20 | NP | |
| Cr in μmol/L | 46.05 | NP | 64.5 | NP | |
| CK in U/L | 150.12 | NP | 1313.75 | NP | |
| GLU in mmol/L | 2.87 | 4.64 | 7.76 | 6.35 | 4.48 |
| Ca2+ in mmol/L | 2.14 | NP | 1.75 | NP | |
| Oxygen therapy | IMV | IMV | IMV | IMV | |
| FiO2 | 80% | 60% | 60% | 45% | 40% |
| PEEP in cmH2O | 6 | 5 | 5 | 4 | 4 |
| PO2 in mmHg | 136 | 83.8 | 267 | 81 | 119 |
| OI in mmHg | 170 | 140 | 445 | 180 | 297.5 |
| PCO2 in mmHg | 13.8 | 30.8 | 29.5 | 42 | 38 |
| MetHb | 3.3% | 2% | NP | 2% | |
| pH | 7.351 | 7.312 | 7.212 | 7.26 | 7.35 |
| Lactates | NP | 1.5 | 8.5 | NP | |
| Bicarbonate | 7.5 | 15.5 | 11.8 | 23.8 | 21.6 |
ALB: Albumin; ALT: Alanine transaminase; APTT: Activated partial thromboplastin time; AST: Aspartate transaminase; BUN: Blood urea nitrogen; CK: Creatine kinase; Cr: Creatinine; CRP: C-reactive protein; FIB: Fibrinogen; GLU: Glucose; HGB: Hemoglobin; ICU: Intensive care unit; IMV: Invasive mechanical ventilation; INR: International normalized ratio; LYMPH: Lymphocyte; MetHb: Methemoglobin; NEUT: Neutrophil; NP: Not performed; OI: Oxygenation index; PCO2: Carbon dioxide partial pressure; PCT: Procalcitonin; PEEP: Positive end-expiratory pressure; PLT: Platelet; PO2: Oxygen partial pressure; PT: Prothrombin time; TP: Total protein; TT: Thrombin time; WBC: White blood cell.
Imaging examinations
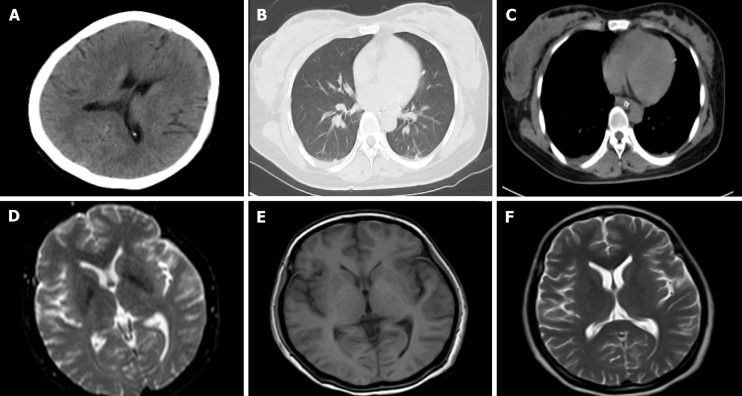
Brain computed tomography (CT), magnetic resonance imaging, and diffusion-weighted imaging of the puerpera were unremarkable, whereas a lung CT indicated small shadows with blurred borders in the lower lobes of both lungs and a small amount of pleural effusion on both sides, as shown in Figure 1. A chest X-ray of the premature infant showed no abnormalities. Abdominal, cranial, and cardiac ultrasound revealed bloating and flatulence in the intestines, a small amount of peritoneal effusion, minimal hemorrhage at the choroid plexus of the left lateral ventricle, patent ductus arteriosus, decreased left cardiac systolic function, and a small amount of tricuspid regurgitation and pericardial effusion.
Figure 1.
Cranial computed tomography, magnetic resonance, and diffusion-weighted imaging. A: Brain computed tomography of the puerpera on December 14, 2021; B and C: Lung computed tomography on December 14, 2021; D: Diffusion-weighted imaging on December 15, 2021; E and F: Magnetic resonance imaging on December 15, 2021.
FINAL DIAGNOSIS
Combined with on-site evidence, acute episodes, clinical manifestations and signs, laboratory parameters, and imaging findings, the puerpera and her premature infant were highly suspected of acquired methemoglobinemia induced by sodium nitrite poisoning. However, the possibility of mixed poisoning with other toxins or drugs could not be ruled out, as the well-defined process and specific cause of exposure or ingestion remain unknown.
TREATMENT
The puerpera underwent orotracheal intubation, IMV, gastric lavage with warm saline, catharsis with magnesium sulfate, detoxification with methylene blue (methylthioninium chloride), and high-dose vitamin C (10 g/d), appropriate hydration, and correction of internal environment disorder in the intensive care unit, followed by lower uterine cesarean section to terminate the pregnancy and hemoperfusion (HP). The premature infant was born with a higher-than-normal MetHb level of 3.3%, and also received detoxification with methylene blue and vitamin C, supplement of vitamin K1, infusion of fresh frozen plasma, as well as respiratory support via orotracheal intubation and IMV. On day 3 after admission, the puerpera regained consciousness, was withdrawn from IMV, and resumed enteral nutrition. She was transferred to the maternity ward 24 h later. However, the condition of her premature infant continued to deteriorate, with gastrointestinal and airway bleeding and refractory bloating.
OUTCOME AND FOLLOW-UP
On day 6 after admission, treatment of the premature infant was stopped and clinical death occurred subsequently. On the 7th d after admission, the puerpera recovered and was discharged without any sequelae.
DISCUSSION
At present, sodium nitrite is widely used as a food preservative, coloring, and antimicrobial agent because of its anti-corrosive properties; however, due to the enzymatic action of MetHb reductase in the body, dietary exposure to trace amounts is considered harmless[15]. It is extremely difficult to control sodium nitrite at the source due to its widespread application and easy access without restrictions, not to mention black markets and unregulated online sales[16,17].
Hemoglobin is an oxygen-carrying metalloprotein in the blood, while MetHb is the oxidized form of hemoglobin with a normal level less than 1% in a physiologic state. As a chemical asphyxiant, sodium nitrite in toxic doses can cause a significant reduction in oxygen-carrying capacity of the blood and induce functional hypoxia at the tissue level by forming high levels of MetHb, and its clinical symptoms, signs, oxygen-carrying capacity of the blood, disease severity, as well as clinical prognosis are all dose-dependent[10,14]. In clinical practice, a mismatch of cyanotic appearance and PO2 may be a hallmark of methemoglobinemia and, therefore, a useful bedside clue for diagnosis, with characteristic cyanosis becoming more pronounced with the increase in MetHb levels. The lack of knowledge of this characteristic cyanotic-type picture may make sodium nitrite poisoning unidentifiable or delay diagnosis in clinical settings. Therefore, clinical identification of methemoglobinemia should be strengthened from a technical and conscious perspective.
In Heilongjiang province, the most northeast province in China, where our patient lives, the weather is cold for close to half the year. Therefore, it has been her custom for a long time to pickle vegetables with sodium nitrite in the autumn, putting her in contact with it intentionally or unintentionally. The textbook sign of a mismatch of cyanotic appearance and PO2 on admission strongly suggested the presence of methemoglobinemia. More importantly, no other toxins or drugs known to cause methemoglobinemia were found in the warehouse. Qualitative or quantitative toxicological analysis of a wide range of samples from the puerpera, as convincing evidence, will make the diagnosis of sodium nitrite poisoning more rigorous[18]. However, unfortunately these toxicological analyses are unavailable in our institution. Combined with on-site evidence, acute episodes, clinical manifestations and signs, laboratory parameters, and imaging findings, the puerpera and her premature infant were highly suspected of acquired methemoglobinemia induced by sodium nitrite poisoning. However, the possibility of mixed poisoning with other toxins or drugs could not be ruled out, as the well-defined process and specific cause of exposure or ingestion remain unknown.
The premature infant was born with a higher-than-normal MetHb level of 3.3%, suggesting that MetHb can quickly cross through the placental barrier. As MetHb levels continued to improve, the clinical prognosis of the puerpera and her premature infant were quite different, reaffirming that the prognosis was related to poor health condition and deteriorating organ function, not just poisoning itself. Gastrointestinal and airway bleeding and refractory bloating may be the main culprits for disease deterioration of the premature infant, while sodium nitrite poisoning may be the final death blow. Therefore, in the rescue and treatment process of patients with sodium nitrite poisoning, in addition to monitoring MetHb levels that reflect the severity of poisoning and therapeutic effectiveness, attention should be paid to other clinical indicators closely related to fatal consequences. Furthermore, infants and children are particular susceptible to sodium nitrite poisoning and tend to worsen for a variety of reasons[19]. Due to the large individual variability of patients with sodium nitrite poisoning, it is sometimes unreliable to use estimated lethal dose and MetHb levels as the sole prognostic criterion in clinical practice[9,20,21].
Management of sodium nitrite poisoning focuses on aggressive decontamination, organ function support, and detoxification[22]. Among these factors, organ function support refers to maintaining airway patency, receiving different forms of oxygen therapy as soon as possible to improve functional hypoxia, and appropriate hydration and/or infusion of vasopressors to antagonize potent peripheral vascular dilation of NO. During detoxification, methylene blue, as a specific antidote, facilitates the conversion of Fe3+ in MetHb back to Fe2+ in normal hemoglobin via nicotinamide adenine dinucleotide phosphate-dependent MetHb reductase, thereby restoring the oxygen-carrying capacity of the blood and increasing tissue oxygenation[23]. Moreover, methylene blue can be utilized as an adjunctive therapy to reverse widespread vasodilation and reduce vasopressor requirements without compromising blood pressure via inhibiting NO synthase[24,25]. Once sodium nitrite poisoning is considered, methylene blue should be administered promptly, with high initial doses for massive exposure or ingestion, and repeated if necessary unless clearly contraindicated[26,27]. High-dose vitamin C, as a potent antioxidant and reducing agent, can be an effective alternative in the management of severe methemoglobinemia without side effects, especially in the absence of methylene blue or with clear contraindications for its application[28]. HP has been well established as the first-line therapy for the removal of a variety of toxins and drugs, especially for those with high albumin binding rates, through a mainly adsorption-based mechanism[29]. Three consecutive sessions of HP played a significant role in the removal of toxins or drugs, improvement of methemoglobinemia and functional hypoxia, and recovery of consciousness in this puerpera.
CONCLUSION
This study is the first to present a rare case of acquired methemoglobinemia in a third trimester puerpera and her premature infant with sodium nitrite poisoning, revealing that MetHb can quickly cross through the placental barrier. In clinical practice, a mismatch of cyanotic appearance and PO2 may be a hallmark of methemoglobinemia and thus a useful bedside clue for diagnosis. MetHb levels should be routinely monitored in patients with clinically suspected sodium nitrite poisoning, which can not only reflect the severity of poisoning, but also feedback treatment effects. However, the fatal consequences of patients with sodium nitrite poisoning are related to advanced age, poor health condition, underlying comorbidities, and deteriorating organ function, rather than just poisoning itself. Once sodium nitrite poisoning is considered, methylene blue should be administered promptly, with high initial doses for massive exposure or ingestion, and repeated if necessary unless clearly contraindicated. This should be administered by intramuscular or intraspinal injection, as subcutaneous injection may produce a local necrotic abscess. Intraspinal injection may cause permanent organic damage to the central nervous system.
Footnotes
Informed consent statement: The authors extend their gratitude to all those who provided valuable assistance, guidance, and support for this article.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade C, Grade C
Novelty: Grade B, Grade B
Creativity or Innovation: Grade B, Grade B
Scientific Significance: Grade B, Grade C
P-Reviewer: Juneja D, India S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Zhang YL
Contributor Information
Dong-Sheng Fei, Department of Critical Care Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China.
Yang Gao, Department of Critical Care Medicine, The Sixth Affiliated Hospital of Harbin Medical University, Harbin 150027, Heilongjiang Province, China.
Xue-Jiao Bao, Department of Critical Care Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China.
Yu-Jia Tang, Department of Critical Care Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China.
Yi-Lu Lin, Department of Critical Care Medicine, The Sixth Affiliated Hospital of Harbin Medical University, Harbin 150027, Heilongjiang Province, China.
Jia-Xi Xu, Department of Critical Care Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China.
Jia-Ning Zhang, Department of Critical Care Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China.
Bo-Wen Liu, Department of Critical Care Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China.
Kai Kang, Department of Critical Care Medicine, The First Affiliated Hospital of Harbin Medical University, Harbin 150001, Heilongjiang Province, China. janekk1021@126.com.
References
- 1.Lee C, Jang EJ, Yum H, Choi YS, Hong J. Unintentional mass sodium nitrite poisoning with a fatality. Clin Toxicol (Phila) 2017;55:678–679. doi: 10.1080/15563650.2017.1303142. [DOI] [PubMed] [Google Scholar]
- 2.Jiranantakan T, Olson KR, Tsutaoka B, Smollin CG. Methemoglobinemia from frozen-dried mudfish contaminated with sodium nitrite. Clin Toxicol (Phila) 2016;54:892. doi: 10.1080/15563650.2016.1201677. [DOI] [PubMed] [Google Scholar]
- 3.McCann SD, Kennedy JM, Tweet MS, Bryant SM. Sodium Nitrite Ingestion: an Emerging Trend in Suicide Attempts Shared via Online Communities. J Emerg Med. 2021;60:409–412. doi: 10.1016/j.jemermed.2020.10.021. [DOI] [PubMed] [Google Scholar]
- 4.Theobald JL, Spoelhof R, Pallasch EM, Mycyk MB. The Beef Jerky Blues: Methemoglobinemia From Home Cured Meat. Pediatr Emerg Care. 2018;34:e122–e123. doi: 10.1097/PEC.0000000000000917. [DOI] [PubMed] [Google Scholar]
- 5.Vodovar D, Tournoud C, Boltz P, Paradis C, Puskarczyk E. Severe intentional sodium nitrite poisoning is also being seen in France. Clin Toxicol (Phila) 2022;60:272–274. doi: 10.1080/15563650.2021.1919695. [DOI] [PubMed] [Google Scholar]
- 6.Pires KD, Hart K, Tomassoni AJ. Internet-assisted suicide by nitrite poisoning - a case report and increase in reported intentional nitrite/nitrate exposures in U.S. Poison Center data. Clin Toxicol (Phila) 2022;60:271–272. doi: 10.1080/15563650.2021.1926474. [DOI] [PubMed] [Google Scholar]
- 7.Hwang C, Yeon SH, Jung J, Na JY. An autopsy case of sodium nitrite-induced methemoglobinemia with various post-mortem analyses. Forensic Sci Med Pathol. 2021;17:475–480. doi: 10.1007/s12024-021-00378-w. [DOI] [PubMed] [Google Scholar]
- 8.Maric P, Ali SS, Heron LG, Rosenfeld D, Greenwood M. Methaemoglobinaemia following ingestion of a commonly available food additive. Med J Aust. 2008;188:156–158. doi: 10.5694/j.1326-5377.2008.tb01559.x. [DOI] [PubMed] [Google Scholar]
- 9.Durão C, Pedrosa F, Dinis-Oliveira RJ. A fatal case by a suicide kit containing sodium nitrite ordered on the internet. J Forensic Leg Med. 2020;73:101989. doi: 10.1016/j.jflm.2020.101989. [DOI] [PubMed] [Google Scholar]
- 10.Durão C, Pedrosa F, Dinis-Oliveira RJ. Another suicide by sodium nitrite and multiple drugs: an alarming trend for "exit"? Forensic Sci Med Pathol. 2021;17:362–366. doi: 10.1007/s12024-020-00340-2. [DOI] [PubMed] [Google Scholar]
- 11.Mudan A, Repplinger D, Lebin J, Lewis J, Vohra R, Smollin C. Severe Methemoglobinemia and Death From Intentional Sodium Nitrite Ingestions. J Emerg Med. 2020;59:e85–e88. doi: 10.1016/j.jemermed.2020.06.031. [DOI] [PubMed] [Google Scholar]
- 12.Neth MR, Love JS, Horowitz BZ, Shertz MD, Sahni R, Daya MR. Fatal Sodium Nitrite Poisoning: Key Considerations for Prehospital Providers. Prehosp Emerg Care. 2021;25:844–850. doi: 10.1080/10903127.2020.1838009. [DOI] [PubMed] [Google Scholar]
- 13.Bailey JC, Feelisch M, Horowitz JD, Frenneaux MP, Madhani M. Pharmacology and therapeutic role of inorganic nitrite and nitrate in vasodilatation. Pharmacol Ther. 2014;144:303–320. doi: 10.1016/j.pharmthera.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 14.Cvetković D, Živković V, Lukić V, Nikolić S. Sodium nitrite food poisoning in one family. Forensic Sci Med Pathol. 2019;15:102–105. doi: 10.1007/s12024-018-0036-1. [DOI] [PubMed] [Google Scholar]
- 15.Hickey TBM, MacNeil JA, Hansmeyer C, Pickup MJ. Fatal methemoglobinemia: A case series highlighting a new trend in intentional sodium nitrite or sodium nitrate ingestion as a method of suicide. Forensic Sci Int. 2021;326:110907. doi: 10.1016/j.forsciint.2021.110907. [DOI] [PubMed] [Google Scholar]
- 16.Dinis-Oliveira RJ, Durão C. Commentary on: Dean DE, Looman KB, Topmiller RG. Fatal methemoglobinemia in three suicidal sodium nitrite poisonings. J Forensic Sci. doi: 10.1111/1556-4029.14689. Epub 2021 Feb 17. J Forensic Sci. 2021;66:1589–1590. doi: 10.1111/1556-4029.14723. [DOI] [PubMed] [Google Scholar]
- 17.Bottei EM, Houselog GJ. Letter to the editor: Dramatic increase in deaths from nitrate/nitrite self-poisonings reported to poison control centers since June 2020. Clin Toxicol (Phila) 2022;60:139–140. doi: 10.1080/15563650.2021.1930031. [DOI] [PubMed] [Google Scholar]
- 18.Tomsia M, Głaz M, Nowicka J, Szczepański M. Sodium nitrite detection in costal cartilage and vitreous humor - Case report of fatal poisoning with sodium nitrite. J Forensic Leg Med. 2021;81:102186. doi: 10.1016/j.jflm.2021.102186. [DOI] [PubMed] [Google Scholar]
- 19.Rino PB, Scolnik D, Fustiñana A, Mitelpunkt A, Glatstein M. Ascorbic acid for the treatment of methemoglobinemia: the experience of a large tertiary care pediatric hospital. Am J Ther. 2014;21:240–243. doi: 10.1097/MJT.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 20.Kanji R, Schneider HJ, Pontin M. Brown-Colored Buccal Mucosa Associated with Methemoglobinemia. Cyanosis Appears Different in Varying Ethnic Groups. J Emerg Med. 2017;52:e209–e211. doi: 10.1016/j.jemermed.2016.11.033. [DOI] [PubMed] [Google Scholar]
- 21.Dean DE, Looman KB, Topmiller RG. Fatal methemoglobinemia in three suicidal sodium nitrite poisonings. J Forensic Sci. 2021;66:1570–1576. doi: 10.1111/1556-4029.14689. [DOI] [PubMed] [Google Scholar]
- 22.Harvey M, Cave G, Chanwai G. Fatal methaemoglobinaemia induced by self-poisoning with sodium nitrite. Emerg Med Australas. 2010;22:463–465. doi: 10.1111/j.1742-6723.2010.01335.x. [DOI] [PubMed] [Google Scholar]
- 23.Umbreit J. Methemoglobin--it's not just blue: a concise review. Am J Hematol. 2007;82:134–144. doi: 10.1002/ajh.20738. [DOI] [PubMed] [Google Scholar]
- 24.Buckley MS, Barletta JF, Smithburger PL, Radosevich JJ, Kane-Gill SL. Catecholamine Vasopressor Support Sparing Strategies in Vasodilatory Shock. Pharmacotherapy. 2019;39:382–398. doi: 10.1002/phar.2199. [DOI] [PubMed] [Google Scholar]
- 25.Jang DH, Nelson LS, Hoffman RS. Methylene blue for distributive shock: a potential new use of an old antidote. J Med Toxicol. 2013;9:242–249. doi: 10.1007/s13181-013-0298-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lefevre T, Nuzzo A, Mégarbane B. Poppers-induced Life-Threatening Methemoglobinemia. Am J Respir Crit Care Med. 2018;198:e137–e138. doi: 10.1164/rccm.201806-1044IM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCann SD, Tweet MS, Wahl MS. Rising incidence and high mortality in intentional sodium nitrite exposures reported to US poison centers. Clin Toxicol (Phila) 2021;59:1264–1269. doi: 10.1080/15563650.2021.1905162. [DOI] [PubMed] [Google Scholar]
- 28.Dhibar DP, Sahu KK, Jain S, Kumari S, Varma SC. Methemoglobinemia in a Case of Paint Thinner Intoxication, Treated Successfully with Vitamin C. J Emerg Med. 2018;54:221–224. doi: 10.1016/j.jemermed.2017.10.035. [DOI] [PubMed] [Google Scholar]
- 29.Ronco C, Bellomo R. Hemoperfusion: technical aspects and state of the art. Crit Care. 2022;26:135. doi: 10.1186/s13054-022-04009-w. [DOI] [PMC free article] [PubMed] [Google Scholar]