Abstract
BACKGROUND
Subcutaneous administration of the monoclonal antibody L9LS protected adults against controlled Plasmodium falciparum infection in a phase 1 trial. Whether a monoclonal antibody administered subcutaneously can protect children from P. falciparum infection in a region where this organism is endemic is unclear.
METHODS
We conducted a phase 2 trial in Mali to assess the safety and efficacy of subcutaneous administration of L9LS in children 6 to 10 years of age over a 6-month malaria season. In part A of the trial, safety was assessed at three dose levels in adults, followed by assessment at two dose levels in children. In part B of the trial, children were randomly assigned, in a 1:1:1 ratio, to receive 150 mg of L9LS, 300 mg of L9LS, or placebo. The primary efficacy end point, assessed in a time-to-event analysis, was the first P. falciparum infection, as detected on blood smear performed at least every 2 weeks for 24 weeks. A secondary efficacy end point was the first episode of clinical malaria, as assessed in a time-to-event analysis.
RESULTS
No safety concerns were identified in the dose-escalation part of the trial (part A). In part B, 225 children underwent randomization, with 75 children assigned to each group. No safety concerns were identified in part B. P. falciparum infection occurred in 36 participants (48%) in the 150-mg group, in 30 (40%) in the 300-mg group, and in 61 (81%) in the placebo group. The efficacy of L9LS against P. falciparum infection, as compared with placebo, was 66% (adjusted confidence interval [95% CI], 45 to 79) with the 150-mg dose and 70% (adjusted 95% CI, 50 to 82) with the 300-mg dose (P<0.001 for both comparisons). Efficacy against clinical malaria was 67% (adjusted 95% CI, 39 to 82) with the 150-mg dose and 77% (adjusted 95% CI, 55 to 89) with the 300-mg dose (P<0.001 for both comparisons).
CONCLUSIONS
Subcutaneous administration of L9LS to children was protective against P. falciparum infection and clinical malaria over a period of 6 months.
PLASMODIUM FALCIPARUM causes more than 600,000 deaths from malaria annually, mostly among children in Africa.1 Despite the widespread use of mosquito-control measures, chemoprevention, and case management, little progress has been made in reducing malaria mortality in recent years,1 a trend that could worsen with increasing resistance to antimalarial drugs2,3 and insecticides.4 Thus, the development of new interventions to reduce malaria mortality is needed.
In 2021, the World Health Organization (WHO) recommended the RTS,S/AS01 vaccine for use in children5; four doses of the vaccine had 36% efficacy against malaria over a 4-year period among children 5 to 17 months of age.6 The WHO also recently endorsed the R21/Matrix-M vaccine for use in children.7 In locations where monthly seasonal malaria chemoprevention is the standard care during the 4-to-6-month malaria season, a three-dose regimen of the R21/Matrix-M vaccine had 75% efficacy over a 12-month period among children 5 to 36 months of age, and a booster after 12 months was necessary to maintain efficacy.8 When given seasonally, the RTS,S/AS01 and R21/Matrix-M vaccines have similar efficacy.9,10
The WHO also recommends malaria chemoprevention in high-risk populations, such as infants and young children, children with severe anemia after hospital discharge who are at risk for fatal malaria, and pregnant persons.1,11,12 Although malaria chemoprevention is safe and efficacious in children and pregnant persons,11–13 achieving a high level of coverage with regimens involving frequent administration is challenging.14 New drugs, including monoclonal antibodies, that prevent malaria for up to 6 months after the administration of a single dose may improve prevention coverage in these vulnerable populations.
In a phase 2 trial involving adults in Mali, an intravenous infusion of CIS43LS, a monoclonal antibody with an extended half-life that targets a conserved junctional epitope on the P. falciparum circumsporozoite protein (PfCSP), was administered at a dose of 10 mg per kilogram of body weight or 40 mg per kilogram. Over a 6-month malaria season, this monoclonal antibody provided protective efficacy against P. falciparum infection of 75.0% and 88.2% at the doses of 10 mg per kilogram and 40 mg per kilogram, respectively.15
These results were followed by the development of L9LS, a monoclonal antibody with an extended half-life that targets another highly conserved junctional PfCSP epitope that was more potent than CIS43LS in preclinical models.16 In a phase 1 trial, L9LS protected adults against controlled malaria infection, including in four of five adults who received L9LS at a dose of 5 mg per kilogram subcutaneously.17 Here, we report the results of a phase 2 trial that was conducted in Mali to assess the safety and efficacy of subcutaneous administration of L9LS against P. falciparum infection in healthy children 6 to 10 years of age over the 6-month malaria season.
METHODS
TRIAL OBJECTIVES, PARTICIPANTS, AND OVERSIGHT
We conducted this trial in Kalifabougou and Torodo, Mali, where P. falciparum is endemic and is transmitted from July through December.18 Eligible participants included healthy adults 18 to 55 years of age and healthy children 6 to 10 years of age. Details of the inclusion and exclusion criteria are provided in the Supplementary Appendix, available with the full text of this article at NEJM.org, and in the trial protocol, available at NEJM.org. Trial clinicians resided at both trial sites and were always available to attend to sick participants.
The trial was conducted in accordance with the Good Clinical Practice guidelines of the International Council for Harmonisation and with Malian regulations. The Food and Drug Administration reviewed the trial protocol in the investigational new drug application (number 160213). The trial was sponsored by the National Institute of Allergy and Infectious Diseases. The protocol and informed-consent forms were approved by the Faculté de Médecine et d’Odonto-Stomatologie and the Faculté de Pharmacie ethics committee at the University of Sciences, Techniques, and Technologies of Bamako, in Bamako, Mali, and by Malian regulatory authorities. Community permission was obtained,19 and written informed consent was obtained from all the adults and from all the parents or guardians of the children. A data and safety monitoring board reviewed the trial protocol and consent documents, reviewed adverse events, and conducted an interim safety review after the primary safety end points for part A of the trial were met and before part B began. The authors vouch for the accuracy and completeness of the data and for the fidelity of the trial to the protocol.
TRIAL PRODUCT
L9LS is a human IgG1 monoclonal antibody that is produced in accordance with current Good Manufacturing Practices by means of cell-culture expression in a recombinant Chinese hamster ovary-cell line.16,17 Processes and analytic methods were developed at the Vaccine Production Program of the Vaccine Research Center and transferred to the Vaccine Clinical Materials Program (operated under contract with Leidos Biomedical Research) for production in accordance with current Good Manufacturing Practices. L9LS was put in vials in a buffered formulation at a concentration of 150 mg per milliliter.
TRIAL PROCEDURES
Age Deescalation and Dose-Escalation Trial (Part A)
For part A, we prespecified that 18 adults would be assigned in open-label fashion to receive L9LS at a dose of 300 mg or 600 mg, administered subcutaneously, or 20 mg per kilogram of body weight, administered intravenously; each group included 6 participants. Administration began in the lowest-dose group (the group receiving 300 mg subcutaneously), and once participants reached day 7 after the injection, administration began at the subsequent dose level if no safety concerns had arisen.
After the last adult participant in the highest dose group (the group receiving the dose intravenously) reached day 7 after the infusion, 18 children were randomly assigned (in a 1:1 ratio) to receive either 150 mg of L9LS or normal saline placebo, administered subcutaneously. If no safety concerns had arisen once all the participants in that group reached day 7 after the injection, an additional 18 children underwent randomization (in a 1:1 ratio) to receive 300 mg of L9LS or placebo, administered subcutaneously. In part A, stratification according to body weight was used to categorize all 36 children (26 to 30 kg, 20 to 25 kg, or 15 to 19 kg, with 12 participants in each stratum, as prespecified).
The participants and trial team members were unaware of the trial-group assignments; only the trial pharmacists were aware of the assignments. Details of the administration procedures are provided in the Supplementary Appendix. Adults were followed for safety on days 1, 3, 7, 14, 21, and 28 and then monthly through 28 weeks after administration, and children on days 1, 3, 7, 14, 21, and 28 and then every 2 weeks through 28 weeks after administration.
In both parts A and B of the trial, data on solicited local and systemic adverse events were recorded for 7 days after the administration of L9LS or placebo, and laboratory assessments were collected for 14 days. In both parts A and B, data on unsolicited adverse events, including serious adverse events, were collected for the duration of the trial. All the adverse events were followed through resolution, and causality was determined by trial clinicians. After the last pediatric participant in the highest dose group (the group receiving the 300-mg dose) reached day 7 of the safety follow-up, an interim safety evaluation was performed before enrollment began in part B.
Randomized, Placebo-Controlled Trial (Part B)
Children were randomly assigned (in a 1:1:1 ratio) by means of block randomization to receive 150 mg of L9LS, 300 mg of L9LS, or normal saline placebo. L9LS or placebo was administered subcutaneously. Randomization was stratified according to body weight (26 to 30 kg, 20 to 25 kg, or 15 to 19 kg, with 75 participants in each stratum). Only the trial pharmacists were aware of the group assignments. Participants received L9LS or placebo (day 0) and were followed up on days 1, 3, 7, 14, 21, and 28 and every 2 weeks thereafter through 24 weeks. Primary assessments included physical examination and the detection of P. falciparum by means of microscopic examination of blood smears (see the Supplementary Appendix).
The primary efficacy end point was P. falciparum blood-stage infection (regardless of the presence of symptoms) as detected by means of microscopic examination of thick blood-smear samples obtained at least every 2 weeks during scheduled trial visits and unscheduled illness visits. Blood smears were not read at the time that they were obtained unless signs or symptoms of malaria were present.
Clinical malaria (a secondary efficacy end point) was detected during scheduled and unscheduled visits. The first definition of clinical malaria (definition 1) was a body temperature of at least 37.5°C or a history of fever in the previous 24 hours and P. falciparum asexual parasitemia of more than 5000 parasites per cubic millimeter; the second definition of clinical malaria (definition 2) was an illness accompanied by any level of P. falciparum asexual parasitemia that resulted in the receipt of antimalarial treatment.
All the participants received a directly observed treatment course of artemether–lumefantrine 7 to 12 days before the administration of L9LS or placebo in order to clear possible P. falciparum infection so that the primary efficacy end point could be assessed. For the remainder of the trial, asymptomatic P. falciparum infections were not treated, in accordance with national guidelines in Mali. All the participants in whom symptomatic malaria developed received standard treatment.
STATISTICAL ANALYSIS
The intention-to-treat population was defined as all the participants who had undergone randomization. Primary efficacy analyses were conducted in the modified intention-to-treat population, which included all the participants who had undergone randomization and received L9LS or placebo. Primary efficacy analyses were based on the time to the first P. falciparum infection (primary efficacy end point) or clinical malaria episode (secondary efficacy end point). P values were based on the log-rank test for the comparison of each L9LS group with the placebo group. Protective efficacy was estimated by means of Cox proportional-hazards modeling that accounted for interval censoring. Efficacy in time-to-event analyses was calculated as (1 – hazard ratio) × 100, in which the hazard ratio was for infection or clinical malaria. The Holm method was applied separately to the primary and secondary efficacy end points to control for multiplicity in the comparison of each L9LS dose group with the placebo group, and the adjusted 95% confidence intervals are reported accordingly. Details about the statistical methods are provided in the Supplementary Appendix.
RESULTS
PARTICIPANTS
From March 18 to August 10, 2022, a total of 24 adults 18 to 55 years of age and 341 children 6 to 10 years of age were assessed for eligibility (Fig. 1 and Fig. S1 in the Supplementary Appendix). Five adults were excluded because they were not eligible, and the remaining 19 adults were enrolled in part A of the trial and received artemether–lumefantrine. A total of 73 children were excluded because they were not eligible (54), because they served as backups and were not needed (17), or for other reasons (2). The remaining 268 children were enrolled in part A or B.
Figure 1. Screening, Enrollment, Randomization, and Follow-up of Pediatric Participants.
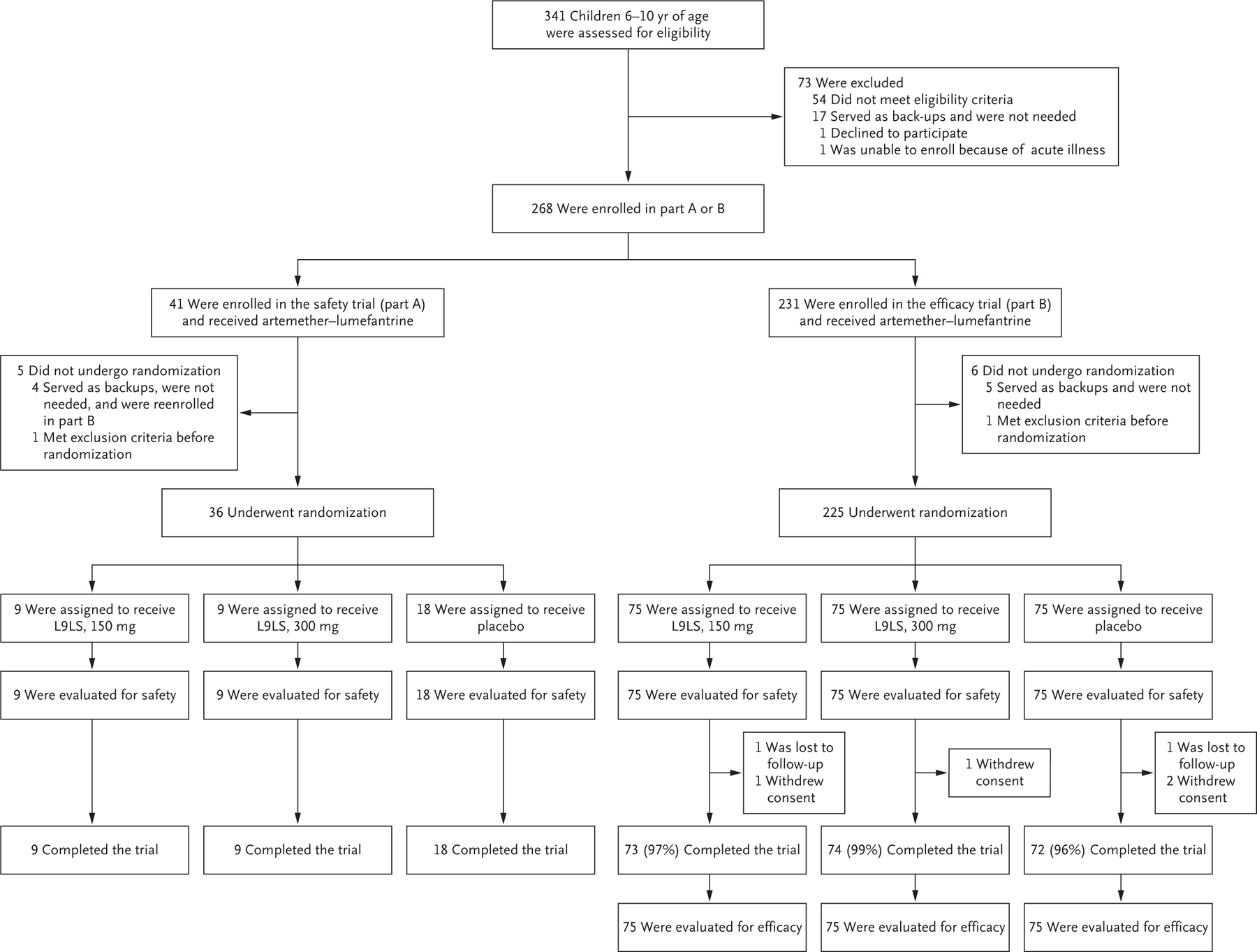
For pediatric participants, the trial was conducted in two parts. Part A was a double-blind, randomized, placebo-controlled, dose-escalation trial that was conducted before the malaria season to evaluate the safety and side-effect profile of the monoclonal antibody L9LS. Part B was a double-blind, randomized, placebo-controlled trial to assess the safety and efficacy of L9LS. A total of 268 participants were enrolled. Of the 41 participants who were initially enrolled in part A, 4 served as backups and were not needed but were reenrolled in part B. In part A, 36 participants underwent randomization between May 3 and May 17, 2022, and received a single subcutaneous injection of placebo or L9LS in one of two dose-escalation groups: 18 participants received placebo, 9 received 150 mg of L9LS, and 9 received 300 mg of L9LS. In part B, 225 participants underwent randomization between July 18 and August 15, 2022, and received a single subcutaneous injection of placebo or L9LS, with 75 participants in each group, before the peak of the malaria season. The final trial visits for part B occurred after the malaria season, on January 31, 2023. As prespecified in the protocol, the efficacy analysis was based on the modified intention-to-treat data set, which included all the participants who had undergone randomization and received L9LS or placebo, including those who withdrew or were lost to follow-up. In parts A and B of the trial, artemether–lumefantrine was given to all the participants as a standard, directly observed treatment course at enrollment, 7 to 12 days before the administration of L9LS or placebo, to clear any possible Plasmodium falciparum blood-stage infection.
In the adult phase of part A of the trial, 1 of the 19 enrolled participants did not proceed to L9LS administration because the prespecified sample size of 18 had been reached. Between March 30 and April 23, 2022, a total of 18 adults received L9LS in the three dose-escalation groups: 300 mg administered subcutaneously, 600 mg administered subcutaneously, or 20 mg per kilogram administered intravenously, with 6 participants in each group. The characteristics of these participants at baseline are shown in Table S1. All 18 adult participants completed trial visits through day 196.
In the pediatric phase of part A, 5 of the 41 enrolled participants did not undergo randomization because they were backups and not needed (4) or because exclusion criteria were met before randomization (1). Between May 3 and May 17, 2022, a total of 36 children underwent randomization and received placebo or L9LS, administered subcutaneously, in one of two dose-escalation groups: 9 received 150 mg of L9LS, 9 received 300 mg of L9LS, and 18 received placebo. The characteristics of these participants at baseline are shown in Table S2. All 36 pediatric participants completed trial visits through day 196.
In part B of the trial, 231 children were enrolled and received artemether–lumefantrine. Six participants did not undergo randomization because they were backups and not needed (5) or because exclusion criteria were met before randomization (1). Between July 18 and August 15, 2022, a total of 225 participants underwent randomization and received 150 mg of L9LS, 300 mg of L9LS, or placebo, with 75 participants in each group. The final trial visits for part B occurred on January 31, 2023. All 225 participants were included in the safety analysis. A total of 219 participants (97%) completed follow-up through the last trial visit. The characteristics of the participants at baseline were similar across the trial groups (Table 1).
Table 1.
Characteristics of the Participants at Baseline in the Efficacy Trial (Part B).*
| Characteristic | L9LS, 150 mg (N = 75) |
L9LS, 300 mg (N = 75) |
Placebo (N = 75) |
|---|---|---|---|
| Median age (range) — yr | 8 (6–10) | 8 (6–10) | 7 (6–10) |
| Sex — no. (%) | |||
| Female | 31 (41) | 33 (44) | 36 (48) |
| Male | 44 (59) | 42 (56) | 39 (52) |
| Median weight (range) — kg | 24 (16–30) | 22 (16–30) | 23 (15–30) |
| Site — no. (%) | |||
| Kalifabougou | 56 (75) | 49 (65) | 52 (69) |
| Torodo | 19 (25) | 26 (35) | 23 (31) |
| Any plasmodium species detected on blood-smear examination at enrollment — no. (%) | 14 (19) | 13 (17) | 12 (16) |
| Plasmodium falciparum | 12 (16) | 13 (17) | 12 (16) |
| P. malariae | 2 (3) | 0 | 0 |
| P. ovale | 0 | 0 | 0 |
| Median interval between administration of artemether–lumefantrine and L9LS or placebo (range) — days | 7 (7–12) | 7 (6–10) | 7 (7–12) |
| Hemoglobin genotype — no. (%) | |||
| Hemoglobin AA | 57 (76) | 62 (83) | 64 (85) |
| Hemoglobin AS | 11 (15) | 7 (9) | 6 (8) |
| Hemoglobin AC | 6 (8) | 6 (8) | 5 (7) |
| Hemoglobin CC | 1 (1) | 0 | 0 |
| Hemoglobin SC | 0 | 0 | 0 |
For pediatric participants, the trial was conducted in two parts. Part B was a double-blind, randomized, placebo-controlled trial to assess the safety and efficacy of the monoclonal antibody L9LS.
At enrollment, P. falciparum was detected by means of blood smear in 12 participants (16%) in the 150-mg group, in 13 (17%) in the 300-mg group, and in 12 (16%) in the placebo group (Table 1). All the participants had negative blood smears on the day that L9LS or placebo was administered. The representativeness of the trial participants is described in Table S8.
SAFETY
Among the adult participants in part A, three of six (50%) who received 300 mg of L9LS and one of six (17%) who received 600 mg of L9LS had mild, transient swelling at the injection site. No other solicited adverse events were observed within 7 days after the administration of L9LS (Table S3). During the 28-week study period, no serious adverse events were reported, and all the unsolicited adverse events that occurred were of grade 1 or 2 and resolved without intervention (Table S5).
Among the pediatric participants in part A, no solicited local or systemic reactogenicity events were noted within 7 days after the administration of L9LS (Table S4). No serious adverse events were observed during the 28-week trial period, and all the unsolicited adverse events that occurred were of grade 1 or 2, except for one instance of grade 4 leukocytosis that occurred in one participant 19 days after the receipt of 150 mg of L9LS (Table S6); this event resolved without intervention and was considered to be unrelated to L9LS in blinded investigations. This participant had no notable symptoms or findings on physical examination, and other laboratory and radiographic studies were unremarkable.
In part B, solicited local and systemic adverse events within 7 days after the administration of L9LS or placebo were uncommon, were mild to moderate in severity, were similar in frequency across the trial groups, and resolved without intervention (Table 2). During the 24-week trial, 108 unsolicited adverse events of grade 1 and 701 unsolicited adverse events of grade 2 were observed (Table S7), and no serious adverse events occurred.
Table 2.
Solicited Maximum Local and Systemic Reactogenicity Events within 7 Days after Administration of L9LS or Placebo in the Efficacy Trial (Part B).*
| Symptom and Severity† | L9LS, 150 mg (N = 75) |
L9LS, 300 mg (N = 75) |
Placebo (N = 75) |
|---|---|---|---|
| number of participants (percent) | |||
| Local reactogenicity events ‡ | |||
| Pain | |||
| None | 74 (99) | 75 (100) | 74 (99) |
| Mild | 1 (1) | 0 | 1 (1) |
| Pruritus | |||
| None | 75 (100) | 75 (100) | 74 (99) |
| Mild | 0 | 0 | 1 (1) |
| Swelling | |||
| None | 74 (99) | 72 (96) | 75 (100) |
| Mild | 1 (1) | 3 (4) | 0 |
| Any local symptom | |||
| None | 73 (97) | 72 (96) | 73 (97) |
| Mild | 2 (3) | 3 (4) | 2 (3) |
| Systemic reactogenicity events § | |||
| Fever | |||
| None | 72 (96) | 75 (100) | 74 (99) |
| Mild | 1 (1) | 0 | 1 (1) |
| Moderate | 2 (3) | 0 | 0 |
| Headache | |||
| None | 73 (97) | 74 (99) | 74 (99) |
| Mild | 0 | 0 | 1 (1) |
| Moderate | 2 (3) | 1 (1) | 0 |
| Chills | |||
| None | 75 (100) | 74 (99) | 75 (100) |
| Mild | 0 | 1 (1) | 0 |
| Any systemic symptom | |||
| None | 70 (93) | 73 (97) | 73 (97) |
| Mild | 1 (1) | 1 (1) | 2 (3) |
| Moderate | 4 (5) | 1 (1) | 0 |
For participants who reported multiple episodes of a given event, the event type was counted once per participant at the maximum severity. Percentages may not total 100 because of rounding.
No severe (grade 3) or life-threatening (grade 4) solicited local or systemic reactogenicity events were reported within 7 days after the administration of L9LS in the efficacy trial (part B).
No participant reported local symptoms of tenderness, redness, or bruising.
No participant reported systemic symptoms of malaise, muscle aches, nausea, or joint pain.
EFFICACY
In the efficacy trial (part B), among the 225 participants who were included in the modified intention-to-treat population (which was equal to the intention-to-treat population), P. falciparum infection with an onset between week 1 and week 24 after administration occurred in 36 participants (48%) who received the 150-mg dose of L9LS, in 30 (40%) who received the 300-mg dose of L9LS, and in 61 (81%) who received placebo. In the efficacy analysis that was based on the time to the first P. falciparum infection over the 24-week trial period, the efficacy of the 150-mg dose of L9LS as compared with placebo was 66% (adjusted 95% confidence interval [CI], 45 to 79; P<0.001), and the efficacy of the 300-mg dose of L9LS as compared with placebo was 70% (adjusted 95% CI, 50 to 82; P<0.001) (Fig. 2).
Figure 2. Efficacy against P. falciparum Infection.
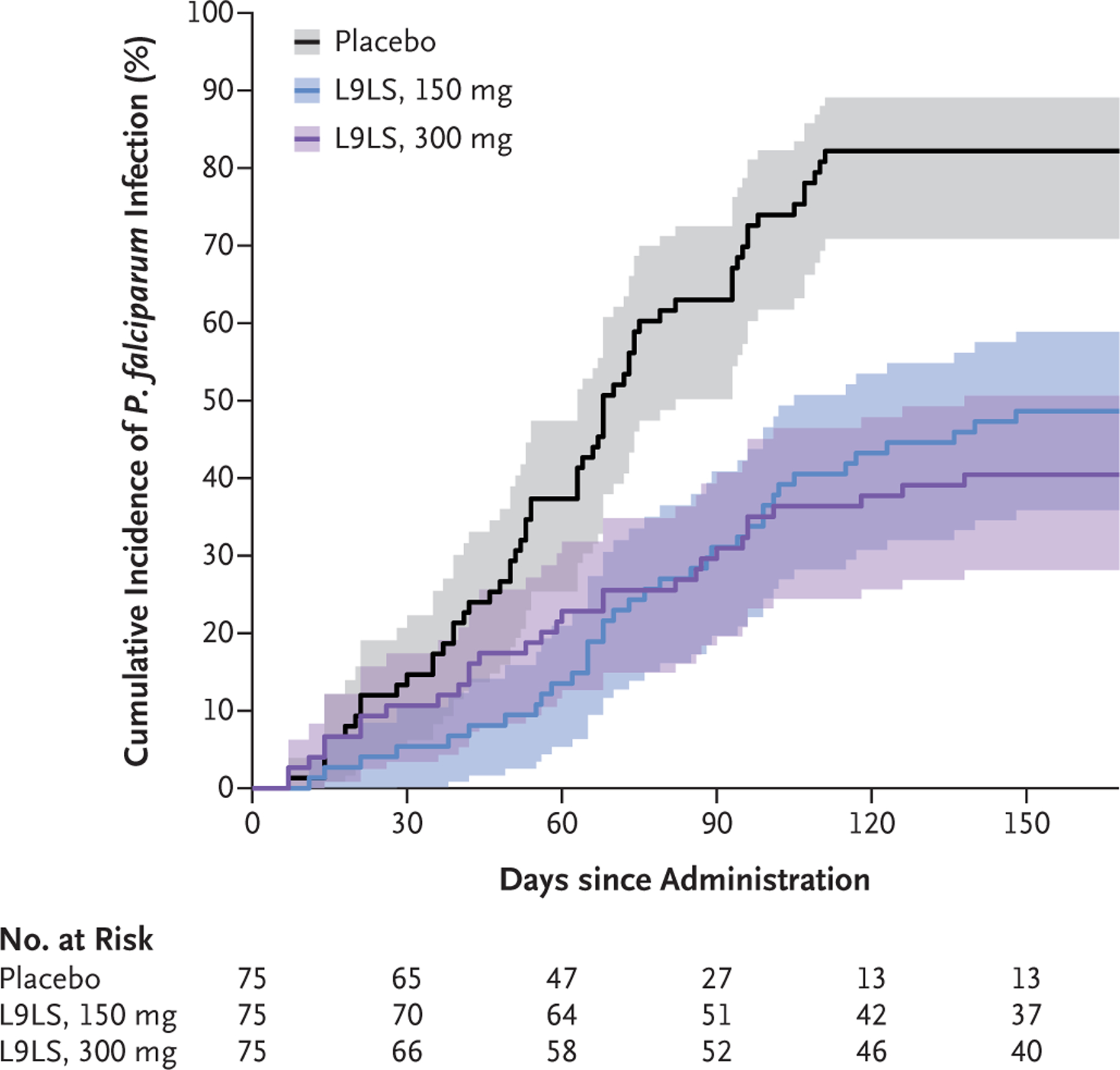
Shown is the cumulative incidence of the first P. falciparum blood-stage infection during a 6-month malaria season (regardless of the presence of symptoms) after a single subcutaneous injection of 150 mg of L9LS, 300 mg of L9LS, or placebo. P. falciparum infections were detected by means of microscopic examination of thick blood-smear samples obtained during scheduled trial visits and unscheduled visits due to illness. Samples for blood smears were obtained before the administration of L9LS or placebo on day 0 and then on days 3, 7, 14, 21, and 28 and every 2 weeks thereafter, for a total of 24 weeks. Only blood-smear samples that were obtained between week 1 and week 24 were included in the efficacy analysis. Shaded areas indicate 95% confidence intervals.
Clinical malaria (definition 1) with an onset between week 1 and week 24 after administration occurred in 21 participants (28%) who received the 150-mg dose of L9LS, in 14 (19%) who received the 300-mg dose of L9LS, and in 44 (59%) who received placebo. In the efficacy analysis that was based on the time to the first episode of clinical malaria over the 24-week trial period, the efficacy of the 150-mg dose of L9LS as compared with placebo was 67% (adjusted 95% CI, 39 to 82; P<0.001), and the efficacy of the 300-mg dose of L9LS as compared with placebo was 77% (adjusted 95% CI, 55 to 89; P<0.001) (Fig. 3).
Figure 3. Efficacy against Clinical Malaria.
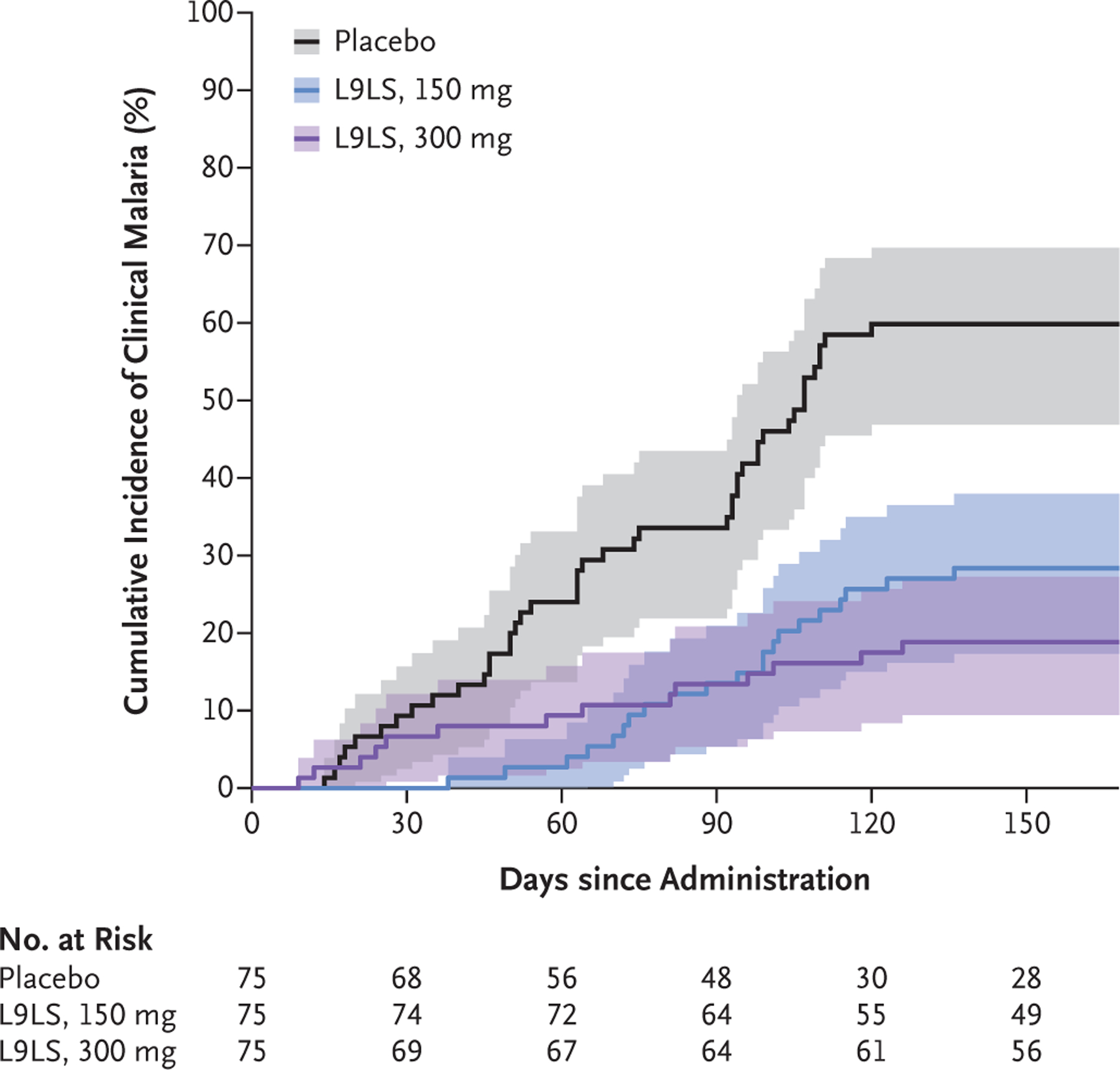
Shown is the cumulative incidence of the first clinical malaria episode due to P. falciparum infection during a 6-month malaria season after a single subcutaneous injection of 150 mg of L9LS, 300 mg of L9LS, or placebo. The prespecified definition of clinical malaria that was used in this analysis was an illness accompanied by a measured axillary temperature of at least 37.5°C or a history of fever (subjective or objective) in the previous 24 hours and P. falciparum asexual parasitemia of more than 5000 parasites per cubic millimeter as detected on microscopic examination of thick blood smears (definition 1). Episodes of clinical malaria were detected during scheduled trial visits and unscheduled visits due to illness. Only clinical malaria episodes that occurred between week 1 and week 24 were included in the efficacy analysis. Shaded areas indicate 95% confidence intervals.
The risks of infection and clinical malaria were similar in the 300-mg L9LS group and the placebo group during the first 28 days of the trial (Figs. 2 and 3). A post hoc analysis of the pharmacokinetics of L9LS through trial day 28 suggested that reduced L9LS bioavailability was not responsible for early infections in the 300-mg group (Fig. S2). A post hoc genotype analysis of P. falciparum infections through trial day 28 suggested that recrudescent infection after the administration of artemether–lumefantrine at enrollment had occurred in some participants (Fig. S3). Infection was detected at enrollment by means of quantitative reverse-transcriptase–dose of L9LS, in 29 (39%) who received the 300-mg dose of L9LS, and in 27 (36%) who received placebo. Among 22 participants who had infection detected by means of blood smear between day 7 and day 28, infection was also detected by means of qRT-PCR assay at enrollment in 4 of 4 participants (100%) in the 150-mg group, in 5 of 8 (62%) in the 300-mg group, and in 7 of 10 (70%) in the placebo group.
Results of prespecified secondary efficacy analyses that were based on time-to-event analyses of efficacy against clinical malaria (definition 2) are shown in Figure S6. The proportion of participants who had at least one P. falciparum infection or clinical malaria episode is discussed in the Supplementary Appendix. Exploratory analyses of body weight–based dose levels and efficacy are shown in Figures S7 through S11. Post hoc analyses of the cumulative incidence of malaria are shown in Figures S12 and S13, and the efficacy of L9LS over time is shown in Tables S9 and S10.
DISCUSSION
We found that a single subcutaneous dose of L9LS provided protective efficacy of up to 70% against P. falciparum infection and of up to 77% against clinical malaria in children 6 to 10 years of age over a 6-month malaria season, during which 81% of the participants in the placebo group became infected with P. falciparum and 59% had clinical malaria. The scale-up of malaria chemoprevention in children younger than 6 years of age has been associated with a higher incidence of malaria among school-age children,20 which is possibly due to delayed acquisition of immunity.21 Vaccination of young children with the RTS,S/AS01 or R21/Matrix-M vaccine could further shift the burden of malaria to older children.22 Moreover, school-age children are a major reservoir of asymptomatic infection23 and transmission to mosquitoes.24 Given that chemoprevention is not widely used in school-age children and that they are not eligible for the RTS,S/AS01 or R21/Matrix-M vaccines, the data from our trial support the administration of a single dose of L9LS in school-age children before the malaria season as an approach toward possibly reducing the disease burden in this accessible population.
The risks of P. falciparum infection and clinical malaria were similar in the 300-mg L9LS group and the placebo group in the early weeks of the trial. We hypothesize that new sporozoite infections were possible before L9LS reached the maximum serum concentration approximately 7 days after administration, which resulted in infections that were detectable on blood smear 7 to 21 days later. The higher incidence of early infections in the 300-mg group than in the 150-mg group may be related to the higher prevalence of baseline submicroscopic infection in the 300-mg group, given that submicroscopic infection is a marker of higher reinfection risk and a cause of recrudescent infections in some persons.25 Future trials may assess the efficacy of administration of L9LS with an antimalarial drug to mitigate the risk of preexisting and early infections, particularly in areas with high transmission.
The results of this trial support the development of antimalarial monoclonal antibodies in other high-risk populations for whom the WHO recommends chemoprevention, including infants and young children, children with severe anemia after hospital discharge, and pregnant persons.1,11,12 L9LS could complement or replace chemoprevention in order to improve coverage in these populations. A phase 2 trial in Kenya involving children 5 months to 5 years of age is assessing the efficacy of subcutaneous administration of L9LS against perennial transmission (ClinicalTrials.gov number, NCT05400655), and a phase 2 trial in Mali is evaluating the efficacy of subcutaneous administration of L9LS in women of childbearing potential (NCT05816330), ahead of trials in pregnancy.
The use of antimalarial monoclonal antibodies needs to be considered in the context of deployment of the RTS,S/AS01 and R21/Matrix-M vaccines. A recent trial showed that seasonal malaria chemoprevention plus an annual booster of RTS,S/AS01 through 5 years of age (after the initial three-dose vaccine series is started at 5 to 17 months of age) led to a lower risk of malaria than either intervention alone.9,10 Given that seasonal malaria chemoprevention involves at least four monthly treatment courses each year, the strategy of combining seasonal malaria chemoprevention with an annual booster of vaccine would necessitate more than 20 health care contacts through 5 years of age. Therefore, comparison of this strategy with a single annual dose of L9LS, which would necessitate only five health care contacts through 5 years of age, may be of interest.
This trial provides evidence to support the continued development of monoclonal antibodies as an additional tool to reduce malaria morbidity and mortality.
Supplementary Material
Acknowledgments
(Funded by the National Institute of Allergy and Infectious Diseases; ClinicalTrials.gov number, NCT05304611.)
Supported by the Division of Intramural Research and the Vaccine Research Center, National Institute of Allergy and Infectious Diseases, National Institutes of Health.
We thank the trial participants and their families in Kalifabougou and Torodo, Mali, for their contributions and commitment to malaria research.
APPENDIX
The authors’ full names and academic degrees are as follows: Kassoum Kayentao, M.D., Ph.D., M.P.H., Aissata Ongoiba, M.D., M.P.H., Anne C. Preston, R.N., Sara A. Healy, M.D., M.P.H., Zonghui Hu, Ph.D., Jeff Skinner, M.S., Safiatou Doumbo, M.D., Ph.D., Jing Wang, M.S., Hamidou Cisse, Pharm.D., Didier Doumtabe, Pharm.D., Abdrahamane Traore, M.D., Hamadi Traore, M.D., Adama Djiguiba, M.D., Shanping Li, M.S., Mary E. Peterson, B.S., Shinyi Telscher, Pharm.D., Azza H. Idris, M.D., Ph.D., William C. Adams, Ph.D., Adrian B. McDermott, Ph.D., Sandeep Narpala, M.S., Bob C. Lin, B.S., Leonid Serebryannyy, Ph.D., Somia P. Hickman, Ph.D., Andrew J. McDougal, Ph.D., Sandra Vazquez, M.S., Matthew Reiber, M.S., Judy A. Stein, M.B.A., Jason G. Gall, Ph.D., Kevin Carlton, M.S., Philipp Schwabl, Ph.D., Siriman Traore, M.S., Mamadou Keita, Pharm.D., Amatigué Zéguimé, Pharm.D., Adama Ouattara, Pharm.D., M’Bouye Doucoure, M.S., Amagana Dolo, Pharm.D., Sean C. Murphy, M.D., Ph.D., Daniel E. Neafsey, Ph.D., Silvia Portugal, Ph.D., Abdoulaye Djimdé, Pharm.D., Ph.D., Boubacar Traore, Pharm.D., Ph.D., Robert A. Seder, M.D., and Peter D. Crompton, M.D., M.P.H.
Footnotes
A list of the contributors in the Mali Malaria mAb Trial Team is provided in the Supplementary Appendix, available at NEJM.org.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
A data sharing statement provided by the authors is available with the full text of this article at NEJM.org.
Contributor Information
K. Kayentao, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
A. Ongoiba, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
A.C. Preston, Malaria Infection Biology and Immunity Section, Laboratory of Immunogenetics, Division of Intramural Research, Maryland
S.A. Healy, Malaria Infection Biology and Immunity Section, Laboratory of Immunogenetics, Division of Intramural Research, Maryland
Z. Hu, Biostatistics Research Branch, Division of Clinical Research, Maryland
J. Skinner, Malaria Infection Biology and Immunity Section, Laboratory of Immunogenetics, Division of Intramural Research, Maryland
S. Doumbo, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
J. Wang, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, and the Clinical Monitoring Research Program Directorate, Frederick National Laboratory for Cancer Research, Frederick, Maryland
H. Cisse, Malaria Infection Biology and Immunity Section, Laboratory of Immunogenetics, Division of Intramural Research, Maryland
D. Doumtabe, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
A. Traore, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
H. Traore, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
A. Djiguiba, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
S. Li, Malaria Infection Biology and Immunity Section, Laboratory of Immunogenetics, Division of Intramural Research, Maryland
M.E. Peterson, Malaria Infection Biology and Immunity Section, Laboratory of Immunogenetics, Division of Intramural Research, Maryland
S. Telscher, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
A.H. Idris, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
W.C. Adams, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
A.B. McDermott, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
S. Narpala, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
B.C. Lin, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
L. Serebryannyy, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
S.P. Hickman, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
A.J. McDougal, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
S. Vazquez, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
M. Reiber, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
J.A. Stein, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
J.G. Gall, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
K. Carlton, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
P. Schwabl, Department of Immunology and Infectious Diseases, Harvard T.H. Chan School of Public Health, Boston
S. Traore, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
M. Keita, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
A. Zéguimé, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
A. Ouattara, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
M’B. Doucoure, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
A. Dolo, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
S.C. Murphy, Malaria Molecular Diagnostic Laboratory, Department of Laboratory Medicine and Pathology, and the Center for Emerging and Re-emerging Infectious Diseases, University of Washington, Seattle
D.E. Neafsey, Department of Immunology and Infectious Diseases, Harvard T.H. Chan School of Public Health, Boston
S. Portugal, Max Planck Institute for Infection Biology, Berlin
A. Djimdé, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
B. Traore, Malaria Research and Training Center, Mali International Center of Excellence in Research, University of Sciences, Techniques, and Technologies of Bamako, Bamako, Mali
R.A. Seder, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rockville, the Vaccine Research Center, Maryland
P.D. Crompton, Malaria Infection Biology and Immunity Section, Laboratory of Immunogenetics, Division of Intramural Research, Maryland
References
- 1.World Health Organization. World malaria report 2023 (https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2023).
- 2.Conrad MD, Asua V, Garg S, et al. Evolution of partial resistance to artemisinins in malaria parasites in Uganda. N Engl J Med 2023;389:722–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mihreteab S, Platon L, Berhane A, et al. Increasing prevalence of artemisinin-resistant HRP2-negative malaria in Eritrea. N Engl J Med 2023;389:1191–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hancock PA, Hendriks CJM, Tangena J-A, et al. Mapping trends in insecticide resistance phenotypes in African malaria vectors. PLoS Biol 2020;18(6):e3000633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malaria vaccine: WHO position paper — March 2022. Wkly Epidemiol Rec 2022;97: 61–80 (https://iris.who.int/bitstream/handle/10665/352332/WER9709-eng-fre.pdf). [Google Scholar]
- 6.RTS S Clinical Trials Partnership. Efficacy and safety of RTS,S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet 2015; 386:31–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO recommends R21/Matrix-M vaccine for malaria prevention in updated advice on immunization. Geneva: World Health Organization, October 2, 2023 (https://www.who.int/news/item/02-10-2023-who-recommends-r21-matrix-m-vaccine-for-malaria-prevention-in-updated-advice-on-immunization). [Google Scholar]
- 8.Datoo MS, Dicko A, Tinto H, et al. Safety and efficacy of malaria vaccine candidate R21/Matrix-M in African children: a multicentre, double-blind, randomised, phase 3 trial. Lancet 2024;403: 533–44. [DOI] [PubMed] [Google Scholar]
- 9.Chandramohan D, Zongo I, Sagara I, et al. Seasonal malaria vaccination with or without seasonal malaria chemoprevention. N Engl J Med 2021;385:1005–17. [DOI] [PubMed] [Google Scholar]
- 10.Dicko A, Ouedraogo J-B, Zongo I, et al. Seasonal vaccination with RTS,S/AS01E vaccine with or without seasonal malaria chemoprevention in children up to the age of 5 years in Burkina Faso and Mali: a double-blind, randomised, controlled, phase 3 trial. Lancet Infect Dis 2024;24: 75–86. [DOI] [PubMed] [Google Scholar]
- 11.Kwambai TK, Dhabangi A, Idro R, et al. Malaria chemoprevention in the postdischarge management of severe anemia. N Engl J Med 2020;383:2242–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Desai M, Hill J, Fernandes S, et al. Prevention of malaria in pregnancy. Lancet Infect Dis 2018;18(4):e119–e132. [DOI] [PubMed] [Google Scholar]
- 13.Meremikwu MM, Donegan S, Sinclair D, Esu E, Oringanje C. Intermittent preventive treatment for malaria in children living in areas with seasonal transmission. Cochrane Database Syst Rev 2012; 2012:CD003756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.ACCESS-SMC Partnership. Effectiveness of seasonal malaria chemoprevention at scale in west and central Africa: an observational study. Lancet 2020;396: 1829–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kayentao K, Ongoiba A, Preston AC, et al. Safety and efficacy of a monoclonal antibody against malaria in Mali. N Engl J Med 2022;387:1833–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang LT, Pereira LS, Flores-Garcia Y, et al. A potent anti-malarial human monoclonal antibody targets circumsporozoite protein minor repeats and neutralizes sporozoites in the liver. Immunity 2020;53(4): 733–744.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu RL, Idris AH, Berkowitz NM, et al. Low-dose subcutaneous or intravenous monoclonal antibody to prevent malaria. N Engl J Med 2022;387:397–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan J, Cho H, Pholcharee T, et al. Functional human IgA targets a conserved site on malaria sporozoites. Sci Transl Med 2021;13(599):eabg2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diallo DA, Doumbo OK, Plowe CV, Wellems TE, Emanuel EJ, Hurst SA. Community permission for medical research in developing countries. Clin Infect Dis 2005;41:255–9. [DOI] [PubMed] [Google Scholar]
- 20.Coulibaly D, Guindo B, Niangaly A, et al. A decline and age shift in malaria incidence in rural Mali following implementation of seasonal malaria chemoprevention and indoor residual spraying. Am J Trop Med Hyg 2021;104:1342–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenwood B, Zongo I, Dicko A, Chandramohan D, Snow RW, Ockenhouse C. Resurgent and delayed malaria. Malar J 2022;21:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olotu A, Fegan G, Wambua J, et al. Seven-year efficacy of RTS,S/AS01 malaria vaccine among young African children. N Engl J Med 2016;374:2519–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Portugal S, Tran TM, Ongoiba A, et al. Treatment of chronic asymptomatic Plasmodium falciparum infection does not increase the risk of clinical malaria upon reinfection. Clin Infect Dis 2017;64:645–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andolina C, Rek JC, Briggs J, et al. Sources of persistent malaria transmission in a setting with effective malaria control in eastern Uganda: a longitudinal, observational cohort study. Lancet Infect Dis 2021;21:1568–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mumtaz R, Okell LC, Challenger JD. Asymptomatic recrudescence after artemether-lumefantrine treatment for uncomplicated falciparum malaria: a systematic review and meta-analysis. Malar J 2020;19:453. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


