Abstract:
PURPOSE:
The purpose of the study was to study the relationship between the timing of pars plana vitrectomy (PPV) with corrected distance visual acuity (CDVA) in cases of nucleus drop during phacoemulsification.
METHODS:
This retrospective analysis included 83 patients, who underwent PPV for nucleus or nuclear fragment drop from July 2017 to November 2019. Timing of PPV (≤2 weeks and >2 weeks) after the primary cataract surgery was noted. The primary endpoint was CDVA at 1 month, which was compared with the time of PPV. Visual outcome was assessed as good if CDVA was better than or equal to 20/40 and poor if CDVA was worse than 20/40. Mode of management along with type of secondary intraocular lens (IOL) implanted was also evaluated.
RESULTS:
Out of the 83 cases (55 males and 28 females) in which vitrectomy for nucleus drop was performed, 36 cases were operated within 2 weeks and 47 were operated between 2 weeks and 1 month. In cases which were operated within 2 weeks, CDVA of 20/20–20/40 was achieved in 33 cases. For those who were operated on after 2 weeks, CDVA of 20/20–20/40 was achieved in 43 cases. The difference in visual outcome in both the groups was statistically nonsignificant (Fisher’s exact t-test, P = 0.97). In 64 (77%) cases, adequate sulcus was present, in which foldable 3-piece IOL was placed in 29 (35%) cases.
CONCLUSION:
Timing of intervention has no bearing on the final visual outcome after vitrectomy in cases of nucleus drop during phacoemulsification. The continuity of the capsulorrhexis and the availability of capsular support determines the type of placement of the lens. A foldable lens can be placed in the sulcus if continuous capsulorrhexis is present.
Keywords: Pars plana vitrectomy, phacoemulsification, visual outcome
Introduction
Phacoemulsification is the procedure of choice for cataract surgery. Posterior dislocation of the lens in toto or its fragments into the vitreous is a serious intraoperative complication.[1] The reported incidence of this is between 0.4% and 4%.[2] The continuity of capsulorhexis and adequacy of capsular support determines the type of intraocular lens (IOL) to be implanted after pars plana vitrectomy (PPV).
The presence of lens fragments can incite complications such as uveitis, cystoid macular edema, and retinal detachment, thereby affecting the visual outcome after PPV.[1] PPV has been the procedure of choice to minimize these complications. The timing of PPV still remains a matter of debate. Many studies suggest early vitrectomy; however, presence of corneal edema or inflammation may preclude early PPV and requires medical management followed by PPV. At times, availability of vitreo-retina setup or surgeon may also lead to a delay in the procedure.
This study was designed to find out the effect of timing of PPV on corrected distance visual acuity (CDVA) in cases of nucleus drop during phacoemulsification.
Methods
In a retrospective longitudinal study, a total of 83 nucleus drop cases were included from July 2017 to November 2019. The study protocol was approved by the ethics committee of the institute. Written informed consent was obtained from all the patients, and the tenets of the Declaration of Helsinki were followed. The medical records of all the patients who had this complication in-house or referred from other centers were evaluated. A complete detailed evaluation was done, with regard to the following parameters:
Time of vitreo-retinal intervention for nucleus removal – within 2 weeks or after 2 weeks
Continuity of capsulorrhexis (continuous curvilinear capsulorrhexis, two-third regular, and completely irregular)
Adequacy of capsular support (<50% or >50%)
Type of secondary IOL implantation (in the sulcus – foldable or polymethyl methacrylate (PMMA), scleral fixated IOL (SFIOL), or anterior chamber IOL (ACIOL)
CDVA at 1 month postoperatively – the visual acuity was measured using the Snellen visual acuity chart and then converted to logarithm of minimum angle of resolution LogMAR for statistical purposes. Visual outcome was assessed as good if CDVA was better than or equal to 20/40 and poor if CDVA was <20/40.
Any case with retinal detachment at the time of presentation or any preoperative macular pathology was excluded from the study, as they would have affected the final visual outcome.
Surgical technique
To begin with, a thorough anterior vitrectomy was performed to clear the anterior chamber of any vitreous or any lens matter. This was followed by three ports 23 gauge PPV. Posterior core vitrectomy was done to clear the nuclear fragment from the surrounding vitreous. Preservative-free triamcinolone was used for visualization of the vitreous in some cases. Posterior vitreous detachment was induced whenever absent, to reduce the risk of postoperative retinal tears.
Once the vitrectomy was complete and all the three ports were cleared of vitreous, the lens material was emulsified with the help of 23 gauge fragmentome. The perfluorocarbon liquid was used to float the lens away from the retina to protect the macula from fragmentome while manipulating the lens matter.
After the removal of the nucleus, IOL was implanted. In cases where there was a continuous curvilinear capsulorrhexis and ≥50% capsular support, a foldable 3-piece lens was placed in the sulcus, and in cases where two-third rhexis was intact and ≥50% posterior capsular support was present, a PMMA lens was placed in the sulcus. In cases with <50% capsular support with completely irregular capsulorrhexis, SFIOL/ACIOL was placed.
Patients with corneal edema and inflammation were put on topical or systemic medication followed by vitreo-retinal intervention once the media were clear.
Results
A total of 83 cases (55 males and 28 females) were analyzed. The age group of all patients ranged between 50 and 84 years as illustrated in Figure 1.
Figure 1.
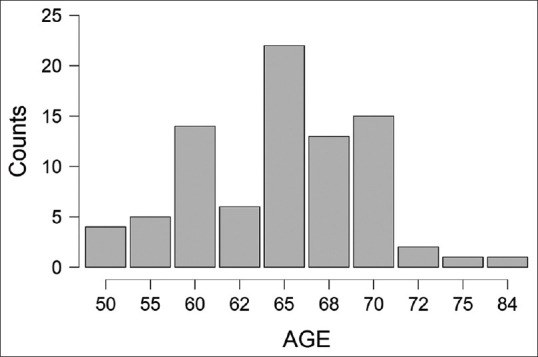
Age distribution
Out of the 83 cases in which vitrectomy for nucleus drop was performed, 36 cases were operated within 2 weeks and 47 were operated between 2 weeks and 1 month time.
The timing of the intervention was compared with CDVA at 1 month postoperatively. Table 1 shows the number of patients who attained good or poor CDVA at 1 month postoperatively with different timing of intervention.
Table 1.
Comparison between timing of intervention and corrected distance visual acuity at 1 month postoperatively
| Timing of intervention (weeks) | Total number of cases | CDVA 20/20 to 20/40 | CDVA <20/40 |
|---|---|---|---|
| <2 | 36 | 33 | 3 |
| >2 | 47 | 43 | 4 |
CDVA: Corrected distance visual acuity
Fisher’s exact t-test was applied, and it was statistically nonsignificant with P value being 0.97.
The IOL was implanted after PPV in the same sitting in 62 cases and as a secondary procedure in 21 cases.
In 64 cases, adequate sulcus was present, in which foldable 3-piece IOL was placed in 29 cases and nonfoldable PMMA lens was placed in 35 cases. In the remaining 19 cases with inadequate sulcus, SFIOL was placed in five cases, and ACIOL was placed in 14 cases.
In the late vitrectomy Group, two cases had retinal tears which were lasered peroperatively. In the same Group, one patient had choroidal detachment which was treated with systemic steroids postoperatively and one patient had hypotonous maculopathy postoperatively, for which the patient was put on systemic steroids and topical cycloplegic.
The statistical analysis was performed with -JASP is a software for statistics. It is not a physical product. JASP version 0.12.20, University of Amsterdam, the Netherlands.
Discussion
Nucleus drop during phacoemulsification is a common complication, especially during the learning curve of trainee surgeons.
With the advent of modern-day minimally invasive vitrectomy surgery, the visual outcome in such cases is reasonably good with early rehabilitation. There is no consensus on the timing of PPV. Some studies suggest that early intervention within 1 week is beneficial as compared to delayed intervention after 1 week in terms of good visual outcome.[3] On the contrary, further studies suggest that delaying PPV can lead to softening of nuclear material, posterior vitreous detachment, and better control of IOP and inflammation before surgery, thereby facilitating the procedure.[4] Salehi et al.[3] concluded in their study on 60 cases that early vitrectomy within 1 week was associated with a less pronounced inflammatory response, less IOP rise, and lesser chances of retinal detachment.
At times, there is a delay in PPV for removal of the dropped nucleus, due to nonavailability of V-R setup or the surgeon. In such cases, retained lens fragments can cause complications such as uveitis, cystoid macular edema, and retinal detachment, thereby affecting the visual outcome after PPV.[1] Furthermore, at times, improper management of PC rent during primary surgery may lead to increased postoperative inflammation, edema, or increased IOP hampering visualization, which may preclude early PPV.
In the present study, out of the 83 cases in which vitrectomy for nucleus drop was performed, 36 cases were operated on within 2 weeks and 47 were operated on after 2 weeks. The delay in PPV was either due to increased inflammation, raised IOP, or corneal edema or nonavailability of vitreo-retinal surgeon. The timing of the intervention was compared with CDVA at 1 month postoperatively. At 1 month follow-up, CDVA of 20/20–20/40 was achieved in 33 cases in those operated in <2 weeks and in 43 cases in those operated after 2 weeks. The difference in visual outcome in both the groups was statistically nonsignificant (P = 0.97).
The type of cataract to be operated determines the possibility of this complication. Hard cataracts, irregular or extended anterior capsulorrhexis, or extension of radial tears further add to the possibility.[5] Another type of cataract prone to such complications is the posterior polar cataract.[6] The posterior capsule may give way during hydrodissection, leading to a breach in the capsule and a drop of the nucleus. Therefore, such cases should be taken up under the supervision of an experienced surgeon.
Surgical intervention was done in all cases with dropped nucleus. The nuclear material was removed using standard three-port 23 gauze PPV. Previous studies have reported a final visual outcome of ≥20/40 after PPV for dropped nucleus in 44%–71.3% of patients.[7,8] In our study, 91.5% of cases had a good vision (≥20/40) at 1-month follow-up.
Appropriate management of the posterior capsular rent and good anterior vitrectomy are key to a quiet eye postoperatively which can then be managed by PPV.
It is also important to choose the appropriate IOL to be placed in the sulcus in case of a PCR. An intact continuous anterior capsulorrhexis allows for optic capture which ensures better stability and lesser chances of decentration in future. Furthermore, thin and long haptic length, 14 mm or more allows for a more stable fit in the sulcus with less chances of movement. Furthermore, the type of material of lens acrylic or silicon is also important. Acrylic lenses are more slippery, whereas silicon lenses tend to stick to the remaining posterior capsule making it more stable. However, at the same time, these cases may require vitrectomy with silicon oil later which make acrylic again a better choice. PMMA lenses can also be used in case of PCR and can be placed in the sulcus. They are more rigid and therefore tend to remain stable over time. Being nonfoldable, they require a larger incision for placement in the eye.[9]
Conclusion
Nucleus drop during phacoemulsification can be managed with a reasonably good visual outcome by PPV. The timing of intervention has no bearing on the final visual outcome. Eyes with increased inflammation and corneal edema can be managed medically and then taken up for vitrectomy. In cases with continuous curvilinear capsulorrhexis and >50% posterior capsular support, foldable three-piece IOL can be implanted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Monshizadeh R, Samiy N, Haimovici R. Management of retained intravitreal lens fragments after cataract surgery. Surv Ophthalmol. 1999;43:397–404. doi: 10.1016/s0039-6257(99)00022-3. [DOI] [PubMed] [Google Scholar]
- 2.Aasuri MK, Kompella VB, Majji AB. Risk factors for and management of dropped nucleus during phacoemulsification. J Cataract Refract Surg. 2001;27:1428–32. doi: 10.1016/s0886-3350(01)00784-2. [DOI] [PubMed] [Google Scholar]
- 3.Salehi A, Razmju H, Beni AN, Beni ZN. Visual outcome of early and late pars plana vitrectomy in patients with dropped nucleus during phacoemulsification. J Res Med Sci. 2011;16:1422–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Ross WH. Management of dislocated lens fragments after phacoemulsification surgery. Can J Ophthalmol. 1996;31:234–40. [PubMed] [Google Scholar]
- 5.Ergun ŞB, Kocamış Sİ, Çakmak HB, Çağıl N. The evaluation of the risk factors for capsular complications in phacoemulsification. Int Ophthalmol. 2018;38:1851–61. doi: 10.1007/s10792-017-0667-3. [DOI] [PubMed] [Google Scholar]
- 6.Osher RH, Yu BC, Koch DD. Posterior polar cataracts: A predisposition to intraoperative posterior capsular rupture. J Cataract Refract Surg. 1990;16:157–62. doi: 10.1016/s0886-3350(13)80724-9. [DOI] [PubMed] [Google Scholar]
- 7.Hansson LJ, Larsson J. Vitrectomy for retained lens fragments in the vitreous after phacoemulsification. J Cataract Refract Surg. 2002;28:1007–11. doi: 10.1016/s0886-3350(01)01223-8. [DOI] [PubMed] [Google Scholar]
- 8.Al-Khaier A, Wong D, Lois N, Cota N, Yang YC, Groenewald C. Determinants of visual outcome after pars plana vitrectomy for posteriorly dislocated lens fragments in phacoemulsification. J Cataract Refract Surg. 2001;27:1199–206. doi: 10.1016/s0886-3350(01)00750-7. [DOI] [PubMed] [Google Scholar]
- 9.Chang DF, Masket S, Miller KM, Braga-Mele R, Little BC, Mamalis N, et al. Complications of sulcus placement of single-piece acrylic intraocular lenses: Recommendations for backup IOL implantation following posterior capsule rupture. J Cataract Refract Surg. 2009;35:1445–58. doi: 10.1016/j.jcrs.2009.04.027. [DOI] [PubMed] [Google Scholar]


