Abstract
Objectives:
Open tibia fractures are associated with substantial morbidity and impact on quality of life. Despite increasing incidence in low-resource settings, most open tibia fracture research comes from high-resource settings. This study aimed to assess the impact of socioeconomic status on treatment modality and evaluate predictors of health-related quality of life following open tibia fractures in Ghana.
Design:
A single-center prospective observational study was conducted in Kumasi, Ghana, from May 2020 to April 2022. Adults with open tibial shaft fractures presenting within 2 weeks of injury were eligible. Demographics, comorbidities, socioeconomic factors, and hospital course were collected at enrollment. Follow-up was scheduled at 8, 12, 26, and 52 weeks. A telephone survey assessing reasons for loss to follow-up was initiated on enrollment completion.
Results:
A total of 180 patients were enrolled. Most patients were employed before injury (79.9%), had government insurance (67.2%), and were from rural areas (59.4%). Fracture classification was primarily Gustilo–Anderson type 3A (49.1%). No relationship between socioeconomic predictors and treatment modality was identified. The largest barriers to follow-up were preference for bonesetter treatment (63.1%), treatment cost (48.8%), and travel cost (29.8%). Of the lost to follow-up patients contacted, 67 (79.8%) reported receiving traditional bonesetter care. Reasons for seeking traditional bonesetter care included ease of access (83.6%), lower cost (77.6%), and familial influence (50.7%).
Conclusion:
No association was identified between socioeconomic predictors and choice of treatment. Bonesetter treatment plays a substantial role in the care of open tibia fractures in Ghana, largely because of ease of access and lower cost.
Key Words: open tibia fracture, quality of life, loss-to-follow-up
1. Introduction
Open tibia fractures are surgical emergencies associated with a high degree of morbidity, including infection (up to 40%), nonunion, and amputation.1–3 These fractures represent a large portion of orthopaedic morbidity in developing countries, particularly as injuries resulting from road traffic accidents continue to increase.4–8 Yet, despite the designation of open tibia fractures as a “bellwether” surgical procedure by the World Health Organization (WHO), most open fracture research comes from high-income countries.9 Therefore, the effects of these injuries and their optimal management strategies in resource-constrained environments are relatively unknown.
Open tibia fractures are costly injuries because of the expense of surgery and extended recovery. These injuries may lead to catastrophic health expenditures, either bankrupting individuals and families or preventing them from seeking care in the first place.10,11 In addition to the impact on patients and their families, open tibia fractures are also costly at the societal level because of lost work and productivity for patients and their caretakers.8,12 These effects are well documented in high-income countries; however, they are less well understood in resource-limited settings.
Open tibia fractures can also greatly affect quality of life. One study in the United States found that complications stemming from these injuries had a greater impact on quality of life than stroke, myocardial infarction, and end-stage arthritis.13 Similarly, a study in Tanzania demonstrated a reduction in health-related quality of life of up to 40% at 3 months after injury compared with those who did not experience an open fracture.14,15 In Ghana, as in other lower-middle income countries, these effects are further complicated by the requirement for upfront payment for health care services and limited resource availability, each of which may drive choice of treatment.16 Traditional bonesetters (TBS), a form of traditional medicine provider, also play a large role in the treatment of all types of fractures and bone-related injury in Ghana.17,18 Between 52% and 78% of fractures are seen by TBS in Ghana, largely because of trust, ease of access, and more affordable care.17,18 The level and type of care provided by TBS is relatively unknown because there is no formal training or accreditation for these providers.17,18
The objectives of this study were to 1) assess the effect of socioeconomic predictors on type of treatment and 2) evaluate predictors of health-related quality of life (HRQOL) after open tibia fracture in Kumasi, Ghana. We hypothesized that higher socioeconomic status would be associated with a higher likelihood of surgical management in general (and a higher rate of intramedullary nailing [IMN] in particular) and a decreased time between presentation and surgery. We also hypothesized that surgical management would be associated with increased HRQOL at one year. Owing to high loss-to-follow-up rates, an additional survey was distributed to study patients to determine reasons for discontinuation of care.
2. Materials and Methods
This study was approved by UCSF IRB (#19-28230) and the Committee for Human Research, Publication, and Ethics at Kwame Nkrumah University of Science and Technology in Kumasi, Ghana. We conducted a prospective observational study at a single large teaching hospital in Kumasi, Ghana. All adult patients with an acute open tibia fracture who presented to the emergency department in Kumasi, Ghana, during the period of enrollment from May 2020 through April 2021 were considered for inclusion. Inclusion criteria included age 18 years or older with an open tibial shaft fracture (OTA/AO type 42) who were willing and able to consent and comply with study follow-up. Exclusion criteria included proximal fractures (OTA/AO 41), distal tibia fractures (OTA/AO type 43), delayed presentation (>2 weeks), severe head injury (GCS <12 on presentation), major burns (>10% of body surface area), spinal cord injury, or a pathologic fracture.
Treatment was administered according to local standard of care and treating surgeon discretion; however, all patients received irrigation and debridement and basic wound care in the emergency department. Patients treated nonoperatively did not undergo a formal debridement in the operating room, rather received simple wound care (including regular dressing changes and close follow-up) and other requisite medical management during the course of their hospital stay as determined by the treating team. Treatment was not altered by participation in the study.
Demographics, medical history, socioeconomic factors (insurance status, education level, employment status and income, and household setting), and hospital treatment course were collected, and follow-up was scheduled at 2 weeks, 8 weeks, 3 months, 6 months, and 1 year after injury. To assess the impact of open tibia fracture treatment on HRQOL, the EQ5D survey was administered at hospital presentation and at each follow-up interval starting at 8 weeks. The EQ5D is a validated 5-question survey that is widely used for evaluating the HRQOL impact of various types of health problems.19 Patients were not compensated for any aspect of participation in the study, although fees for x-rays were paid by the study at the 6-month and 1-year follow-up visits. The sample size required for our primary end point of assessing differences in HRQOL at one year was estimated based on having approximately 10 patients for every 1 evaluated predictor for linear regression models.20,21 To study 20 potential predictors, our required sample size was 200 patients.
Owing to high loss-to-follow-up rates, a telephone lost-to-follow-up survey was created. Patients who did not complete the 1-year in-person follow-up visit were contacted by the phone numbers received during enrollment. Contact attempts were made up to 3 times for all eligible patients. This survey consisted of 3 questions evaluating why the patient did not attend their 1-year follow-up appointment, whether they were receiving care from a traditional bonesetter, and reasons for preferring bonesetter treatment.
All patients with complete EQ5D data at 1-year follow-up were included in our multiple logistic regression. This model was used to evaluate socioeconomic predictors' effects on mode of definitive treatment. Multiple linear regression was also used to evaluate these predictors' effects on time to presentation and time to definitive treatment. Covariates including sex, age, medical comorbidities, mechanism of injury, Gustilo–Anderson (GA) class, smoking status, alcohol consumption, HIV status, time to operation, income, and treatment modality (nail vs. other) were assessed for statistical significance through a one-way ANOVA. Variables with an alpha less than 0.2 were included in the multivariate linear regression model. Nonsignificant variables in the multivariate model were sequentially removed to optimize model fit.
3. Results
In total, 232 patients were screened, during enrollment of which 20 were excluded for OTA/AO type 41 fractures and 32 were excluded for OTA/AO type 43 fractures. 180 patients met inclusion criteria, most of whom were male (84%) with a mean age of 34.7 (SD 12.9) years. Most patients were previously employed in some capacity (79.9%), had government insurance (67.2%), and were from a rural household (59.4%) (Table 1). The plurality of open fractures were GA type 3a (49.1%), followed by type 3b (23.4%) and type 2 (20.6%). These fractures were primarily treated with external fixation (104, 57.8%), followed by nonoperative treatment (59, 32.8%) and IMN (12, 6.7%) (Table 2). Several other treatment modalities were seen in the study, including amputation (1, 0.6%), plate and screws (2, 1.1%), and casting under anesthesia (2, 1.1%); these were excluded from additional analysis because of their small sample sizes.
TABLE 1.
Patient Demographics
| Nonoperative (n = 61) | Operative (n = 119) | P | |
| Age: mean ± SD | 32.7 ± 12.1 | 36.1 ± 13.4 | 0.09 |
| Male: n (%) | 53 (86.9) | 99 (83.2) | 0.67 |
| Rural residence: n (%) | 32 (52.4) | 75 (63.0) | 0.23 |
| Education | |||
| None | 9 (14.8) | 14 (11.8) | 0.85 |
| K-12 | 48 (78.7) | 97 (81.5) | |
| University | 4 (3.3) | 8 (6.7) | |
| Gustilo–Anderson: n (%) | <0.01 | ||
| Type 1 | 8 (13.1) | 1 (0.8) | |
| Type 2 | 26 (42.6) | 10 (8.4) | |
| Type 3A | 21 (34.4) | 65 (54.6) | |
| Type 3B | 1 (1.6) | 40 (33.6) | |
| Type 3C | 0 (0.0) | 3 (2.5) | |
| Insurance status: n (%) | 0.59 | ||
| Private | 0 (0.0) | 2 (1.7) | |
| Government | 41 (67.2) | 80 (67.2) | |
| Uninsured | 20 (32.8) | 37 (31.1) | |
| Employment: n (%) | 0.93 | ||
| Formal | 44 (72.1) | 87 (73.1) | |
| Informal | 4 (6.6) | 9 (7.6) | |
| None | 13 (21.3) | 23 (19.3) | |
| Work hours/week: mean ± SD, cedis | 43.3 ± 15.9 | 46.9 ± 14.1 | 0.19 |
| Earnings/week: mean ± SD, cedis | 399.2 ± 748 | 429.2 ± 591 | 0.82 |
All statistical tests were conducted using the χ2 test for categorical variables and the Student t-test for continuous variables.
TABLE 2.
Method of Treatment
| Treatment | N (%) |
| Nonoperative | 59 (32.8) |
| Operative with cast or splint | 2 (1.1) |
| External fixation | 104 (57.8) |
| IMN | 12 (6.7) |
| Plate and screw fixation | 2 (1.1) |
| Amputation | 1 (0.6) |
There was no significant association between the socioeconomic predictors (insurance status, household setting, or income) and treatment categorized either as operative versus nonoperative or IMN versus other. Fractures treated operatively were generally more severe with higher Gustilo–Anderson grades than those treated nonoperatively (Table 1). Having a college degree was associated with an approximately 48-hour increase in the total time from the time of injury to hospital presentation (48.1 hours, 95% CI 4.2–91.9); however, no other predictors were found to be associated (Table 3). There were no significant socioeconomic predictors for differences in the total amount of time from hospital presentation to definitive operative treatment (Table 3).
TABLE 3.
Multiple Linear Regression Coefficients Examining the Influence of Socioeconomic Factors on the Total Time From Injury to Hospital Presentation and the Total Time From Hospital Presentation to Operative Management
| Total Time to Hospital (h) | Coefficient (95% Confidence Interval) | P |
| Insurance type | ||
| None | Ref | — |
| Private insurance | 354.7 (278.1 to 431.3) | <0.001 |
| Public insurance | 8.1 (−11.5 to 27.8) | 0.42 |
| Education | ||
| None | Ref | — |
| Primary/secondary education | 11.4 (−16.8 to 39.7) | 0.43 |
| College education | 48.1 (4.2 to 91.9) | 0.03 |
| Income (per 10 USD) | 0.07 (−1.7 to 1.8) | 0.93 |
| Rural house | −17.9 (−36.9 to 1.1) | 0.07 |
| GA classification | ||
| Type 1 | Ref | |
| Type 2 | 25.4 (−20.7 to 71.6) | 0.28 |
| Type 3A | 30.6 (−12.3 to 73.5) | 0.16 |
| Type 3B | 22.3 (−22.4 to 67.1) | 0.33 |
| Type 3C | 15.7 (−59.2 to 90.5) | 0.68 |
| Total Time to OR (d) | Coefficient (95% Confidence Interval) | P |
| Insurance type | ||
| None | Ref | — |
| Private insurance | 1.79 (−7.1 to 10.7) | 0.69 |
| Public insurance | 1.27 (−1.5 to 4) | 0.36 |
| Education | ||
| None | Ref | — |
| Primary/secondary education | 0.13 (−3.9 to 4.2) | 0.94 |
| College education | 5.03 (−0.9 to 11) | 0.1 |
| Income (per 10 USD) | −0.03 (−0.3 to 0.2) | 0.79 |
| Rural house | −2.1 (−4.8 to 0.5) | 0.11 |
| GA classification | ||
| Type 1 | Ref | — |
| Type 2 | 4.9 (−8.2 to 18.1) | 0.47 |
| Type 3A | 5.1 (−7.3 to 17.6) | 0.42 |
| Type 3B | 5.5 (−7 to 18.2) | 0.39 |
| Type 3C | 12.2 (−2.2 to 26.6) | 0.1 |
1-year follow-up was completed for 116 (64.0%) patients, of which 102 (87.9%) were completed by telephone. Complete follow-up at all time points is presented in Table 4. No significant differences were noted regarding demographics or treatment characteristics between those who completed 1-year follow-up and those who did not. The 3 main treatment groups (IMN, external fixation, and nonoperative) demonstrated similar HRQOL over the initial follow-up periods. Patients treated with IMN had a higher mean EQ5D score at the 6-month and 1-year follow-ups (Fig. 1). In a univariate analysis, treatment modality (nail vs. other), sex, medical comorbidity, income, and GA class met criteria for inclusion in our model. Of those, only treatment with IMN (P = 0.045) was statistically significant. Our multivariate model demonstrated that higher baseline income was associated with lower HRQOL at one year (−0.008, 95% CI −0.01 to −0.0007) (Table 5).
TABLE 4.
Patient Follow-Up at Each Time Point
| In-Person | Telephone | Percentage of Enrolled (n = 180) | |
| 2-week follow-up | 119 | 47 | 166 (92.2%) |
| 8-week follow-up | 98 | 65 | 163 (90.6%) |
| 3-month follow-up | 75 | 86 | 161 (89.4%) |
| 6-month follow-up | 35 | 119 | 154 (85.5%) |
| 1-year follow-up | 14 | 102 | 116 (64.4%) |
Figure 1.
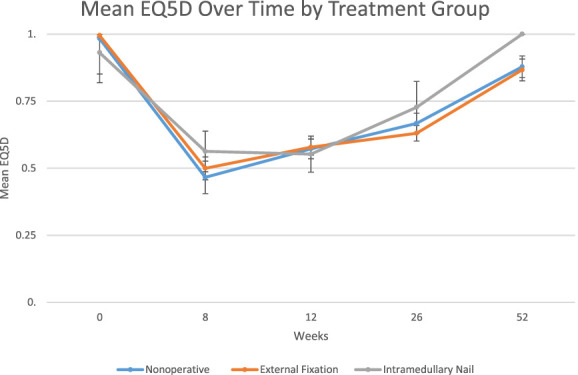
Plot representing the mean EQ5D score and 95% confidence interval for the 3 treatment groups, nonoperative, external fixation, and intramedullary nail, at 8, 12, 26, and 52 weeks.
TABLE 5.
Multiple Linear Regression Coefficients Examining Predictors of EQ5D Score at 1 Year From Injury
| Coefficient (95% CI) | P | |
| Intramedullary nail (IMN) | 0.14 (−0.006 to 0.28) | 0.065 |
| Female sex | −0.09 (−0.17 to 0.00002) | 0.054 |
| Income (per 10 USD) | −0.008 (−0.01 to −0.0007) | 0.029 |
| Medical comorbidity* | −0.03 (−0.27 to 0.2) | 0.78 |
| GA classification | ||
| Type 2 | −0.03 (−0.2 to 0.13) | 0.72 |
| Type 3A | −0.08 (−0.24 to 0.09) | 0.36 |
| Type 3B | −0.12 (−0.29 to 0.04) | 0.14 |
| Type 3C | −0.1 (−0.33 to 0.14) | 0.42 |
Medical comorbidities included diabetes mellitus, heart disease, lung disease, kidney disease, history of stroke, and/or tuberculosis.
Of the 168 patients who did not attend a 1-year follow-up in person, 84 (50%) were reached by phone to complete the loss-to-follow-up survey. The largest barriers to follow-up were a preference for bonesetter treatment (63.1%), cost of treatment (48.8%), and travel cost (29.8%) (Table 6). 67 patients (79.8%) indicated that they had received or were receiving traditional bonesetter care during the follow-up period. The most often cited reasons indicated for preferring bonesetter care were ease of access (83.6%), lower cost (77.6%), and familial influence (50.7%) (Table 6).
TABLE 6.
Loss-to-Follow-up Survey Results
| Barriers to 1-Year Follow-up | Yes (%) (n = 84) |
| Prefer bonesetter treatment | 53 (63.1) |
| Cost of treatment | 41 (48.8) |
| Travel cost | 25 (29.8) |
| Travel distance | 10 (11.9) |
| Work responsibility | 6 (7.1) |
| Family responsibility | 2 (2.4) |
| COVID-19 concerns | 2 (2.4) |
| Feeling better | 2 (2.4) |
| Hospital debt | 1 (1.2) |
| Other medical problems | 0 (0) |
| None of the above | 11 (13.1) |
| Reason for Preferring Traditional Bonesetters From Those Receiving Care From Them | Yes (%) (n = 67) |
| Easier to access | 56 (83.6) |
| Lower cost | 52 (77.6) |
| Family influence | 34 (50.7) |
| Cultural influence | 26 (38.8) |
| Existing/future hospital bills | 11 (16.4) |
| Fear of amputation | 9 (13.4) |
| Spiritual reasons | 6 (9) |
| Mistrust of hospitals | 2 (3) |
| Referred by hospital providers | 0 (0) |
4. Discussion
We did not find any relationship between socioeconomic predictors and treatment modality for open tibia fractures. Patients who were treated with an intramedullary nail had a higher HRQOL at 1 year when compared with other treatment modalities, although this effect did not remain significant in our multivariate model. In addition, cost of treatment and preference for traditional bonesetter care greatly reduced in-person patient follow-up, which could have affected our ability to detect meaningful differences.
Contrary to our expected finding, socioeconomic status was not found to influence the treatment of open tibia fractures in our study in Ghana. This is also contrary to findings by O'Hara et al16 in Uganda, which demonstrated an association between socioeconomic factors and treatment modality. Our finding of an improved HRQOL with IMN is consistent with previous literature suggesting that stabilizing lower extremity injuries in a delayed or ineffective manner can lead to lower HRQOL.22 However, another study conducted in Tanzania found that while IMN was associated with earlier improvements in HRQOL compared with external fixation, this effect dissipated by the 1-year follow-up.23
Bonesetter treatment seems to play a significant role in the care of open tibia fractures in Ghana, largely because of ease of access and lower cost compared with care from a trained orthopaedic surgeon. Little is known about the type of care provided by these providers, but in general, they rely on traditional methods of splinting, bandaging, and applying poultices for wound care.17,24 These findings are important to consider when conducting future studies of orthopaedic care in the region because they will need to address access and cost of care if they are to be successful in promoting patient retention and maximizing long-term follow-up. More importantly, these data suggest the need for additional trained orthopaedic surgeons to meet demand for care, particularly in more rural regions. There may be opportunities for partnership with traditional bonesetters to ensure appropriate triage and care of more complex injuries.
This study was limited by patient loss to follow-up, which limited the ability to make inferences related to predictors of HRQOL at 1 year. This also limited our ability to evaluate for outcomes of treatment including infections and reoperations. In addition, we were unable to assess functional and radiographic outcomes because of poor in-person follow-up and low rates of radiographic evaluation.
Nevertheless, this study remains one of the largest investigations of open tibia fractures conducted in Ghana to date. Our findings indicate a possible long-term improved effectiveness of intramedullary nails, suggesting that efforts should be made to make intramedullary nails cheaper and more widely available in the region. Additional studies are required to better understand the cost effectiveness of intramedullary nailing and the role of traditional bonesetter care in Ghana.
ACKNOWLEDGMENTS
The authors thank the many health care providers at Komfo Anokye Teaching Hospital (KATH) for their support and effort in the completion of this project, particularly the clinical research assistants at KATH for the efforts in data collection and follow-up. The authors also thank the UCSF Department of Orthopaedic Surgery, UCSF Clinical & Translational Science Institute, AO Trauma North America, and the AO Alliance for their generous support.
Footnotes
The study was supported with funding from the UCSF department of Orthopaedic Surgery, UCSF Clinical & Translational Science Institute, AO Trauma North America, and the AO Alliance.
The authors have no conflict of interest to report.
Contributor Information
Vincent Ativor, Email: vincentativor@yahoo.com.
Dominic Konadu-Yeboah, Email: domiyk@yahoo.com.
Kelsey Brown, Email: kelsey_brown@brown.edu.
Patricia Rodarte, Email: patricia_rodarte@brown.edu.
Ralph Kumah, Email: raphael.kumah@gmail.com.
Ralph Quartey, Email: raphaelquartey4@gmail.com.
Dominic Awariyah, Email: ddrawariyah@hotmail.co.uk.
Peter Konadu, Email: peterkonadu60@yahoo.de.
Paa Kwesi Baidoo, Email: Pakvandal@gmail.com.
Kanu Okike, Email: kanuokike@gmail.com.
Saam Morshed, Email: saam.morshed@ucsf.edu.
David Shearer, Email: david.shearer@ucsf.edu.
Heather Roberts, Email: hjroberts@gmail.com.
References
- 1.Barei DP, Nork SE, Mills WJ, et al. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma. 2004;18:649–657. [DOI] [PubMed] [Google Scholar]
- 2.Harris AM, Althausen PL, Kellam J, et al. Lower Extremity Assessment Project LEAP Study Group. Complications following limb-threatening lower extremity trauma. J Orthop Trauma. 2009;23:1–6. [DOI] [PubMed] [Google Scholar]
- 3.Kohlprath R, Assal M, Uçkay I, et al. [b]Fractures[/b] ouvertes de la diaphyse tibiale chez l’adulte: prise en charge chirurgicale et complications. Rev Med Suisse. 2011;7:2482–2488. [PubMed] [Google Scholar]
- 4.Chagomerana MB, Tomlinson J, Young S, et al. High morbidity and mortality after lower extremity injuries in Malawi: a prospective cohort study of 905 patients. Int J Surg. 2017;39:23–29. [DOI] [PubMed] [Google Scholar]
- 5.Cordero DM, Miclau TA, Paul AV, et al. The global burden of musculoskeletal injury in low and lower-middle income countries: a systematic literature review. OTA Int. 2020;3:e062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elliott IS, Groen RS, Kamara TB, et al. The burden of musculoskeletal disease in Sierra Leone. Clin Orthop Relat Res. 2015;473:380–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joshipura M, Gosselin RA. Surgical burden of musculoskeletal conditions in low- and middle-income countries. World J Surg. 2020;44:1026–1032. [DOI] [PubMed] [Google Scholar]
- 8.Mock C, Cherian MN. The global burden of musculoskeletal injuries: challenges and solutions. Clin Orthop Relat Res. 2008;466:2306–2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O'Neill KM, Greenberg SLM, Cherian M, et al. Bellwether procedures for monitoring and planning essential surgical care in low- and middle-income countries: caesarean delivery, laparotomy, and treatment of open fractures. World J Surg. 2016;40:2611–2619. [DOI] [PubMed] [Google Scholar]
- 10.Holler JT, MacKechnie MC, Albright PD, et al. The impact of inadequate soft-tissue coverage following severe open tibia fractures in Tanzania. Plast Reconstr Surg Glob Open. 2020;8:e3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meara JG, Leather AJM, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–624. [DOI] [PubMed] [Google Scholar]
- 12.Beveridge M, Howard A. The burden of orthopaedic disease in developing countries. J Bone Joint Surg Am. 2004;86:1819–1822. [DOI] [PubMed] [Google Scholar]
- 13.Brinker MR, Hanus BD, Sen M, et al. The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am. 2013;95:2170–2176. [DOI] [PubMed] [Google Scholar]
- 14.Albright PD, Ali SH, Jackson H, et al. Delays to surgery and coronal malalignment are associated with reoperation after open tibia fractures in Tanzania. Clin Orthop Relat Res. 2020;478:1825–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haonga BT, Areu MMM, Challa ST, et al. Early treatment of open diaphyseal tibia fracture with intramedullary nail versus external fixator in Tanzania: cost effectiveness analysis using preliminary data from Muhimbili Orthopaedic Institute. SICOT-J. 2019;5:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Hara NN, Mugarura R, Potter J, et al. The socioeconomic implications of isolated tibial and femoral fractures from road traffic injuries in Uganda. J Bone Joint Surg Am. 2018;100:e43. [DOI] [PubMed] [Google Scholar]
- 17.Nwachukwu BU, Okwesili IC, Harris MB, et al. Traditional bonesetters and contemporary orthopaedic fracture care in a developing nation: historical aspects, contemporary status and future directions. Open Orthop J. 2011;5:20–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yempabe T, Edusei A, Donkor P, et al. Factors affecting utilization of traditional bonesetters in the Northern Region of Ghana. Afr J Emerg Med. 2021;11:105–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stolk E, Ludwig K, Rand K, et al. Overview, update, and lessons learned from the international EQ-5D-5L valuation work: version 2 of the EQ-5D-5L valuation protocol. Value Health. 2019;22:23–30. [DOI] [PubMed] [Google Scholar]
- 20.Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–1379. [DOI] [PubMed] [Google Scholar]
- 21.Schemitsch EH, Bhandari M, Guyatt G, et al. Study to Prospectively Evaluate Reamed Intramedullary Nails in Patients with Tibial Fractures SPRINT Investigators. Prognostic factors for predicting outcomes after intramedullary nailing of the tibia. J Bone Joint Surg Am. 2012;94:1786–1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sprague S, Petrisor BA, Jeray KJ, et al. Factors associated with health-related quality of life in patients with open fractures. J Orthop Trauma. 2018;32:e5–e11. [DOI] [PubMed] [Google Scholar]
- 23.Haonga BT, Liu M, Albright P, et al. Intramedullary nailing versus external fixation in the treatment of open tibial fractures in Tanzania: results of a randomized clinical trial. J Bone Joint Surg Am. 2020;102:896–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Omololu AB, Ogunlade SO, Gopaldasani VK. The practice of traditional bonesetting: training algorithm. Clin Orthop Relat Res. 2008;466:2392–2398. [DOI] [PMC free article] [PubMed] [Google Scholar]


