Abstract
Background
Stretching has garnered significant attention in sports sciences, resulting in numerous studies. However, there is no comprehensive overview on investigation of stretching in healthy athletes.
Objectives
To perform a systematic scoping review with an evidence gap map of stretching studies in healthy athletes, identify current gaps in the literature, and provide stakeholders with priorities for future research.
Methods
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 and PRISMA-ScR guidelines were followed. We included studies comprising healthy athletes exposed to acute and/or chronic stretching interventions. Six databases were searched (CINAHL, EMBASE, PubMed, Scopus, SPORTDiscus, and Web of Science) until 1 January 2023. The relevant data were narratively synthesized; quantitative data summaries were provided for key data items. An evidence gap map was developed to offer an overview of the existing research and relevant gaps.
Results
Of ~ 220,000 screened records, we included 300 trials involving 7080 athletes [mostly males (~ 65% versus ~ 20% female, and ~ 15% unreported) under 36 years of age; tiers 2 and 3 of the Participant Classification Framework] across 43 sports. Sports requiring extreme range of motion (e.g., gymnastics) were underrepresented. Most trials assessed the acute effects of stretching, with chronic effects being scrutinized in less than 20% of trials. Chronic interventions averaged 7.4 ± 5.1 weeks and never exceeded 6 months. Most trials (~ 85%) implemented stretching within the warm-up, with other application timings (e.g., post-exercise) being under-researched. Most trials examined static active stretching (62.3%), followed by dynamic stretching (38.3%) and proprioceptive neuromuscular facilitation (PNF) stretching (12.0%), with scarce research on alternative methods (e.g., ballistic stretching). Comparators were mostly limited to passive controls, with ~ 25% of trials including active controls (e.g., strength training). The lower limbs were primarily targeted by interventions (~ 75%). Reporting of dose was heterogeneous in style (e.g., 10 repetitions versus 10 s for dynamic stretching) and completeness of information (i.e., with disparities in the comprehensiveness of the provided information). Most trials (~ 90%) reported performance-related outcomes (mainly strength/power and range of motion); sport-specific outcomes were collected in less than 15% of trials. Biomechanical, physiological, and neural/psychological outcomes were assessed sparsely and heterogeneously; only five trials investigated injury-related outcomes.
Conclusions
There is room for improvement, with many areas of research on stretching being underexplored and others currently too heterogeneous for reliable comparisons between studies. There is limited representation of elite-level athletes (~ 5% tier 4 and no tier 5) and underpowered sample sizes (≤ 20 participants). Research was biased toward adult male athletes of sports not requiring extreme ranges of motion, and mostly assessed the acute effects of static active stretching and dynamic stretching during the warm-up. Dose–response relationships remain largely underexplored. Outcomes were mostly limited to general performance testing. Injury prevention and other effects of stretching remain poorly investigated. These relevant research gaps should be prioritized by funding policies.
Registration
OSF project (https://osf.io/6auyj/) and registration (https://osf.io/gu8ya).
Supplementary Information
The online version contains supplementary material available at 10.1007/s40279-024-02002-7.
Key Points
| Research investigating stretching in healthy athletes is mostly limited to small-scale trials of adult, nonelite male athletes, assessing acute effects of static active stretching or dynamic stretching applied to the lower limbs during the warm-up, commonly compared with passive controls. |
| Outcomes have mostly been limited to general performance tests, with scarce information on the underlying mechanisms and on sport-specific performance data. Dose–response relationships were seldom explored. |
| Surprisingly, only five trials assessed injury data. Their results do not support a role for stretching in injury prevention, but further research is required on the topic. |
| Future research and funding policies should devote more effort toward investigating the gaps identified in this scoping review. |
Introduction
In the context of sports and physical exercise, stretching refers to a set of interventions focused primarily on improving joint flexibility or range of motion (ROM) [1–3]. The benefits of stretching on flexibility and ROM seem consensual in the scientific milieu [4–10] (i.e., large and mostly homogeneous body of research supporting this effect) and are integrated into internationally recognized guidelines for exercise prescription [1, 2]. The mechanisms mediating stretching effects on flexibility include structural (e.g., increased fascicle length), mechanical (e.g., decreased muscle stiffness), and sensorial/neural changes (e.g., improved stretch tolerance) [8, 10–14]. The most commonly used stretching methods are static (passive or active), dynamic, ballistic (a form of dynamic stretching where the velocity of limb motion is very high), and passive stretching coupled with isometric muscle actions, commonly termed proprioceptive neuromuscular facilitation (PNF) [1, 3]. These stretching modalities may operate through partially overlapping mechanisms and produce differentiated effects [3, 4, 8, 9, 15]. Stretching volume, intensity, and weekly frequency may have far-reaching impacts on the dose–response relationships [15].
Although stretching interventions conducted in athletes are commonly focused on improving ROM, arguments in favor of stretching also revolve around its value for injury prevention [4, 16–18], warm-up [4, 19, 20], and cool-down/recovery [21–23]. Nonetheless, the evidence for the overall effectivity of stretching in the aforementioned contexts is unclear and heterogeneous at best [5]. Furthermore, answering the question “Can I stretch?” does not answer the question “Must I stretch?” [5]: for the purposes of ROM gains, injury risk, warm-up, and cool-down, stretching can be performed but possibly does not need to be mandatory. Conceivable exceptions are a few selected sports with very specific demands (i.e., gymnastics), although targeted research on this topic is required. Aside from the lack of robust evidence favoring stretching, recent evidence suggests that alternative interventions, such as strength training or foam rolling, may offer similar ROM gains [5, 24–29]. However, such findings should not be used as an argument against stretching, as its applications are not limited to improving ROM (e.g., it may improve strength and muscle hypertrophy [30–32]), and other effects of stretching warrant greater research efforts.
Focusing overly on the acute effects of stretching when applied during the warm-up and/or the cool-down, as well as on the acute and/or chronic effects on ROM and injury risk, may systematically allocate more and more resources (human, financial, and time based) to the same areas of research, while risking neglecting or overlooking other opportunities for implementing stretching interventions focused on alternative outcome measures. For example, the acute nonlocal effects of stretching on ROM and strength [13, 14] are based on generalized mechanisms that may be harnessed when considering injury rehabilitation, as stretching the noninjured areas may generate effects on the injured areas. Stretching has also been shown to generate acute changes in the autonomic nervous system [33–35] and in the cardiovascular system [34, 36, 37]. Moreover, despite the existing research on the chronic effects of stretching focusing on muscle architecture, scarce research is available assessing the effects on nerves and other structures [38]. Athletic preparation may potentially benefit from extending the scope of research on stretching.
Within the traditionally analyzed topics, much research is focused on static stretching (active and passive), PNF (albeit only in a few select types of PNF), and dynamic stretching [4]. How, when, and why athletes could benefit from lesser-known stretching modalities such as global active stretching (SGA, from the original French expression) [39] and Gyrotonic stretching [40], among others, is largely unknown and warrants further exploration. How these interventions may be substantially changed by manipulating the set of provided instructions constitutes another emerging field of research [41]. It is also troublesome that a few purported applications of stretching have remained for decades despite the absence of research to sustain them, as is the case with stretching for the recovery from groin pain or injury in athletes [18]. Overall, valuable research opportunities and potentially relevant applications of stretching in sporting and athletic environments are possibly being wasted due to overemphasis on specific domains (e.g., ROM) and poor investment in relevant others (e.g., nonlocal neural effects).
Scoping reviews perform a systematic mapping of existing evidence and identify relevant gaps in the literature [42, 43]; their aim is not to provide pooled results or analytical comparisons, but to map the existing evidence [43]. Future research would benefit from clear guidance based on an evidence gap map (EGM) [44, 45], and scoping reviews provide a suitable and systematic approach to building such maps [43]. Fitting into the broad approach of most scoping reviews, EGMs graphically represent the body of evidence, conveying an intuitive visual interpretation of research efforts allocation (i.e., where the evidence is rich versus where it is scarce) [44–46]. Such data assist in developing policies and guidelines and exposes areas requiring further research [44–46]. Sports medicine-related reviews with EGMs have been published in recent years [47–49]. Therefore, a scoping review with EGM will provide a clearer picture of what are the research trends, as well as what is known and unknown (i.e., gaps in research) about stretching in athletes, which can inform future policies and funding.
A quick search in PubMed (using “stretching [Ti/Ab] AND sport* [Ti/Ab] OR exercise* [Ti/Ab]”) yielded 1611 records from inception to 2012 and 2177 records from 2013 to 2022, showing that more than half of all studies on the subject of stretching in healthy athletes have been published in the last ~ 10 years and highlighting the fast-growing pace of research on stretching. Therefore, our goal was to perform a systematic scoping review with EGM of stretching-related studies in healthy athletes to identify trends and gaps in the literature and inform stakeholders in priorities for future research.
Methods
This systematic scoping review with EGM followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 [50], the PRISMA extension for Scoping Reviews (PRISMA-ScR) [42], and the Cochrane guidelines [51] (e.g., search for errata before closing the final list of included studies).
Eligibility Criteria
Research articles published in peer-reviewed journals were considered, with no limitations imposed on publication date or language. Eligibility criteria were set based on the Participants, Intervention, Comparators, Outcomes and Study Design (PICOS) framework:
(P) Healthy athletes of any age, sex, or sport, with a competitive level corresponding to tier 2 (trained/developmental) or higher of the Participant Classification Framework (PCF; tiers 0 and 1 are not athletes, falling outside the scope of this review) [52], regardless of how the original studies have classified them. Studies with injured (e.g., studies on rehabilitation or return to sports) or disabled athletes (e.g., cerebral palsy) were excluded. Since the goal was to provide an overview of the research field and not provide meta-analytical summaries of data, no minimum number of participants per study was stipulated.
(I) Acute (single session or multiple sessions but with assessments of acute responses up to 72 h postintervention) or chronic (multiple sessions with assessment of pre- to post- differences) interventions exclusively using any form of stretching (e.g., static active or passive stretching, dynamic stretching, PNF, other), either single mode (e.g., static passive stretching only) or combined mode (e.g., static passive stretching combined with static active stretching). Multimodal interventions (e.g., stretching + foam rolling or stretching + strength training) were not considered. We chose not to predefine a minimum length for an intervention to be considered chronic (e.g., 4 weeks or 8 weeks), since these thresholds may vary depending on the specific outcome (i.e., some outcomes may experience faster adaptations than others) and on the characteristics and doses of the interventions. Moreover, these thresholds are largely arbitrary.
(C) Comparators were not compulsory (because we were not directly comparing the effectiveness or efficacy of stretching interventions). However, if available, these were considered and could include stretching interventions with different modalities, intensities and/or durations, nonstretching-based interventions, multimodal interventions (e.g., stretching + strength training), or passive controls.
(O) At least one of the following: acute or chronic physiological, biomechanical, psychological, performance-related outcomes/adaptations, and/or data on injury risk (from prevention-focused studies).
(S) All types of experimental and observational studies [single- or multi-arm, randomized (parallel, crossover, cluster, other) or nonrandomized], including case series and case studies.
Information Sources and Search Strategy
CINAHL, EMBASE, PubMed, Scopus, SPORTDiscus (via EBSCO), and Web of Science were searched on 15 July 2022, and again on 1 January 2023. As per the preregistered protocol, additional procedures (e.g., snowballing citation tracking, expert consultation) were not performed, due to the large number of included studies (> 300). A comprehensive reporting of information sources and of the search strategy is provided in the Electronic Supplementary Material (ESM Sects. 1.1 and 1.2.).
Selection Process
Three authors (JA, SRR, and AP) independently screened all retrieved records. A third author (RA) arbitrated in case of disagreements. Automated removal of duplicates was performed using EndNote 20.3 for Mac (Clarivate), but further manual removal of duplicates was required.
Data Collection Process
Eight authors (JA, SRR, FYN, AFS, LL, ZA, RC, AP) independently extracted data from the included studies. The coordinator author (JA) double-checked all assessments. After completion of data collection, four authors (RA, HS, RRC, FMC) reanalyzed 40 randomly selected studies (~ 13%) to further ensure proper data quality and completeness of data extraction. Data on competitive level were recoded by three authors (JA, SSR, and AP) using the PCF [52], but excluding tiers 0 and 1 participants: (i) tier 2: Trained/developmental; (ii) tier 3: Highly trained/national level; (iii) tier 4: Elite/international level; (iv) tier 5: World class. A fourth author (RA) arbitrated in case of disagreements.
Data Items and Management
Data were extracted within six domains: (i) participant-related information, (ii) intervention-related information, (iii) comparator-related information, (iv) outcome-related information, (v) study design, and (vi) context of interventions. Full details and explanations can be found in the ESM (Sect. 1.3). Given that stretching interventions were at the core of this work, we followed a mainstream, reader-friendly approach to the classification of stretching modalities [3]: (i) static stretching involving the lengthening of a muscle until a feeling of stretch or point of discomfort are reached, and keeping that position, with (passive) or without (active) assistance from an external force (e.g., a person or a machine); (ii) dynamic stretching involving controlled movements through the joint ROM; (iii) ballistic stretching as an extreme form of dynamic stretching performed at high speeds and with bouncing actions near or at the end-ROM; (iv) PNF stretching combining static stretching and isometric contractions in a cyclical pattern; and (v) other forms of stretching (e.g., SGA). A complete description of data management procedures, including further details regarding how stretching interventions were classified, is provided in the ESM (Sect. 1.4).
Data Synthesis Methods
A narrative synthesis was performed, accompanied by data summaries (number, percentage) for the previously defined data items. To provide an overview of the existing body and the corresponding gaps in research, an EGM was constructed to graphically represent the body of evidence and intuitively convey an overview of the existing evidence and the current research gaps [44–46]. In the EGM, the different circles have proportional sizes, reflecting the number of trials; however, this proportionality is only applied within each cell, and not between cells.
Results
Study Selection
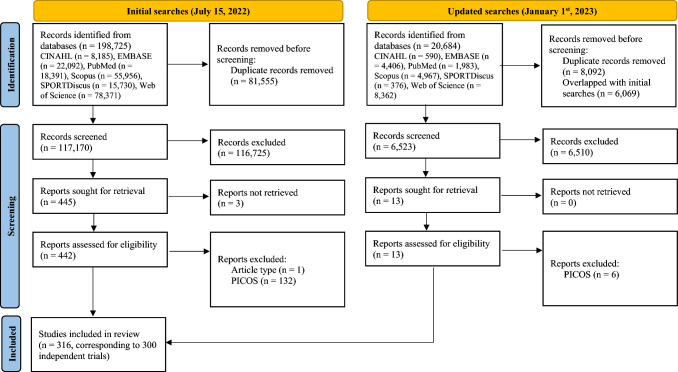
The initial and updated database searches resulted in ~ 220,000 records, of which 316 studies (corresponding to 300 independent trials) [39, 53–367] complied with eligibility criteria and were included in this scoping review (Fig. 1). This means that 300 independent trials gave origin to 316 publications, as some trial authors chose to report different outcomes in different publications (suggesting a high risk of bias for selective reporting, especially in the absence of a preregistered protocol). More detailed information on study selection is provided in the ESM (Sect. 2.1).
Fig. 1.
PRISMA 2020 flow diagram
Publication-Level Information
Publication Date and Study Design
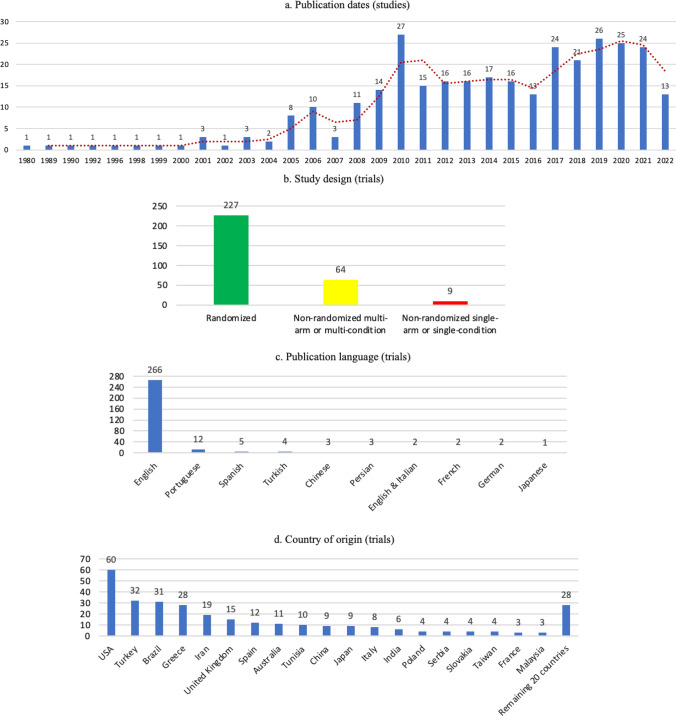
The 300 trials were published between 1980 and 2022 (ESM Sect. 2.2), resulting in 316 publications (i.e., some trial authors chose to report different outcomes from a single experiment in different publications). Date of publication was evenly distributed before or after 2015 (48.7% before 2015 and 51.3% from 2015 onwards; Fig. 2a), meaning that more than half of research was performed in the last 7 years (last search on 1 January 2023). Since 2008, research on the topic has steadily generated over ten publications each year. Most trials (n = 227, 75.7%) were randomized (Fig. 2b), followed by nonrandomized multi-arm/condition trials (k = 64, 21.3%), and a minority of nonrandomized single-arm/condition trials (k = 9, 3.0%).
Fig. 2.
Publication-level distributions
Publication Language and Geographical Location
English was the predominant language of publication (266 trials, 88.7%). Other languages each represented less than 5% of trials, and when combined represented 11.3% (Fig. 2c). Most trials were performed in Europe (k = 94, 31.3%), followed by North America (k = 63, 21.0%), Asia (k = 55, 18.3%), South America (k = 33, 11.0%), and Turkey (technically, belonging to both Europe and Asia; k = 32, 10.7%). Africa contributed with 11 trials (3.7%, of which 10 were from Tunisia), Oceania also delivered 11 trials (3.7%, all from Australia), while one research had unclear origin (either Europe or South America). Out of nearly 40 countries contributing with research, the USA produced the largest number of trials (k = 60, 20.0%), followed by Turkey (k = 32, 10.7%), Brazil (k = 31, 10.3%), Greece (k = 28, 9.3%), Iran (k = 19, 6.3%), and UK (k = 15, 5.0%) (Fig. 2d and e). More detailed information is available in the ESM (Sect. 2.2).
Funding and Competing Interests
A total of 102 studies included a funding statement, with 48 trials (16.0%) reporting not having funding and 54 trials (18.0%) reporting their funding sources; however, the majority of trials (k = 198, 66.0%) did not provide any (published) funding statement. A single trial (0.3%) reported having a conflict of interest, while 102 trials (34.0%) declared having no competing interests; again, the majority of trials (k = 197, 65.6%) failed to provide a published competing interests statement. Overall, 159 trials (53.0%) failed to report both funding and competing interests (Fig. 2f). Considering the 153 trials published from 2015 onward, the percentage of nonreported information on funding (51.6%) and competing interests (41.8%) is lower in comparison with the 147 trials published before 2015 (81.0% and 89.1%, respectively).
Participant-Related Characteristics
Sample Size and Sex
Across the 300 trials, a combined aggregate of 7080 athletes were involved, of which 6005 performed stretching and 1075 athletes only participated in nonstretching-related control groups. Trials averaged 23.3 ± 20.8 athletes per trial (median: 18), ranging from 5 [173] to 220 athletes [177]. A total of 282 trials (94.0%) had fewer than 51 athletes (more detailed information in ESM Sect. 2.2).
A total of 168 trials (56.0%) only included male athletes (n = 4035), 54 trials (18.0%) only included female athletes (n = 1079), and 36 trials (12.0%) included both male (n = 589) and female athletes (n = 378). In one study, there was a nonanalyzed participant, but it was unclear whether this individual was male or female, and this participant was therefore not considered here. In total, there were 4624 male (65.3%) and 1457 female athletes (20.6%). Two trials [124, 135] included male and female athletes (n = 48) but failed to report the number or percentage of each. Forty trials (13.3%) including 950 athletes did not report on sex. A summary of sample size and sex can be found in Sect. 3.7 (EGM).
Age
Most trials (k = 290, 96.7%) reported age, but not in an easily comparable manner, which precluded a simplified cross-study synthesis. The reasons for that and a more complete reporting can be found in the ESM (Sect. 2.2). Considering the 25 trials (8.3%) that provided ranges, age varied from to 8 [149, 338] to 36 [177] years. The narrowest range was 14–15 years of age [265] and the broadest range was 17–36 years [177]. Only four trials included athletes ≤ 12 years of age [86, 141, 149, 338], seven trials included athletes ≥ 30 years of age [105, 177, 218, 232, 311, 329, 358], and a single trial included athletes up to 36 years [177]. Age was reported in the form of mean ± SD in 264 trials (88.0%): at the lower end, a mean age of 9.6 ± 1.5 years was reported [55], while at the upper end the mean age was 35.7 ± 6.1 years [137].
Sports and Competitive Level
Most trials (k = 260 trials, 86.7%) were conducted within a single sport. Thirty-six trials (12.0%) included athletes from multiple sports, and four trials (1.3%) [81, 82, 108, 261] provided insufficient information to assess this item. The available information showed that at least 43 sports were represented (possibly more). Soccer was represented in 98 trials (26.2%), track and field in 41 (11.0%), volleyball in 32 (8.6%), basketball in 29 (7.8%), and artistic gymnastics in 19 (5.1%). All other sports were represented in less than 4% of trials each. More details are provided in the ESM (Sect. 2.2).
Regarding the competitive level (PCF), no trial was found including tier 5 athletes. Most trials (k = 175, 46.8%) included tier 2 athletes, followed by tier 3 (k = 95, 25.4%). Tier 4 (k = 18, 4.8%), mixed tiers 2 and 3 (k = 8, 2.1%), and mixed tiers 3 and 4 (k = 4, 1.1%) were less common. The few tier 4 trials were spread across several different sports (artistic gymnastics, Brazilian jiu-jitsu, fencing, handball, judo, kickboxing, rhythmic gymnastics, rowing, soccer, synchronized swimming, taekwondo, tennis, track and field, volleyball, wrestling), while the mixed tiers 3 and 4 trials included field hockey, futsal, and rhythmic gymnastics (one study reported multiple individual and team sports, but it was unclear which [117]). A visual summary of sport and competitive level can be found in Sect. 3.7 (EGM).
Context of Intervention
Fully detailed, context-level reporting of stretching interventions is provided in the ESM (Sect. 2.2), while summary data for key features (e.g., length of interventions) are provided in Sect. 3.7 (EGM).
Length of Interventions
Most trials focused on acute stretching effects (k = 244, 81.3%), while 51 trials (17.0%) assessed chronic effects (see ESM Sect. 2.2 for the remaining cases). Trials assessing chronic effects lasted between 1 and 21 weeks [90, 285, 312, 351], with an average of 7.4 ± 5.1 and a median of 6.0 [interquartile range (IQR) 4.0–10.5] weeks. Eleven trials, from 12 studies, (3.7%) failed to reach a minimum length of 4 weeks [78, 90, 154, 161, 211, 237, 285, 299, 300, 304, 329, 351] that would suffice to generate adaptations to stretching interventions in humans [368]. Trials lasting up to 8 weeks represented 13.0% of the publications (k = 39), and only six trials, from 10 studies, (2.0%) lasted ≥ 16 weeks [99, 188, 259, 265, 305–309, 312]. Additional information is available in the ESM (Sect. 2.2).
Number of Weekly Sessions and Total Number of Sessions in Chronic Trials
The number of weekly stretching sessions in chronic interventions varied from < 1 per week [188] to 14 weekly sessions [329], with an average of 3.4 ± 2.0 and a median of 3 (IQR 3.0–4.0). Thirty-three trials (67.3%) had less than 4 weekly sessions, 15 trials (27.2%) had between 4 and 7 sessions, and a single trial exceeded 7 weekly sessions [329]. Six of the 55 relevant trials (10.9%) did not report the number of weekly sessions [78, 105, 177, 211, 258, 304].
The total number of stretching sessions in trials assessing chronic effects ranged from 3 to 150 [90, 154, 237, 312, 351], with an average of 24.6 ± 24.1, a median of 19 (IQR 10.3–31.5), and was unreported and impossible to assess in three trials [105, 211, 304].
Within-Season Timing
Most trials (k = 180, 60.0%) failed to report the within-season timing and provided insufficient information for the reviewers to infer this (e.g., by providing specific date ranges for data collection). Of the trials that reported this information, 70 (23.3%) were performed during the competitive season, 24 (8.0%) in the off-season and 22 (7.3%) in the pre-season. The remaining trials (k = 4, 1.2%) were either mixed (e.g., pre-season and competitive season) [125, 177, 365] or the authors reported the specific weeks of the season, but it was unclear whether that still represented the pre-season or was already in the competitive season (i.e., coded as unclear) [182].
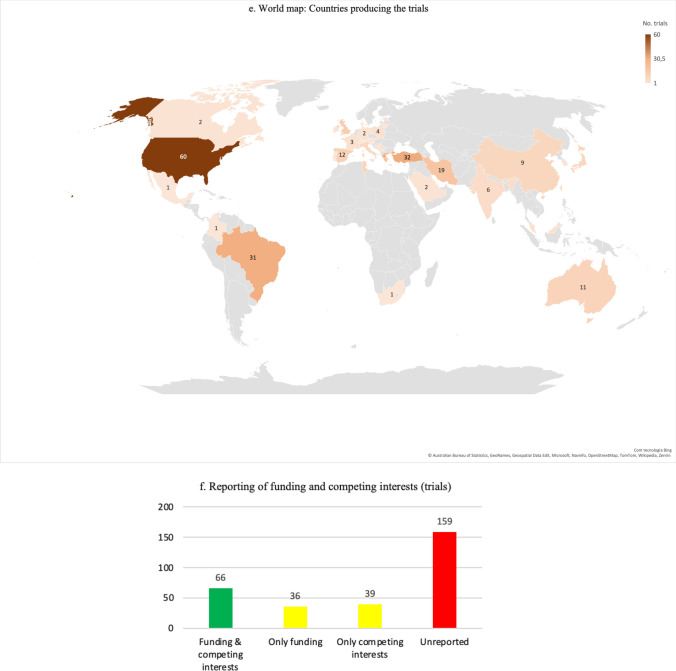
Within-Session Timing
Most trials (k = 252, 84.0%) implemented stretching as warm-up or within the context of a warm-up. Postexercise stretching was analyzed in isolation in 22 trials published in 26 studies (7.3%) [57, 99, 105, 111, 113, 115, 123, 139, 160, 177, 245, 259, 277, 278, 285–287, 294, 305–309, 336, 347, 357], in conjunction with warm-up (i.e., stretching in the warm-up and also postexercise) in two trials [124, 175], optionally in the warm-up or postexercise in one trial [150], and combined with independent sessions in another trial [87]. Trials studying the effects of postexercise stretching in athletes began to be published in 2003 and seem to be growing, albeit there is fluctuating interest in the topic (Fig. 3).
Fig. 3.
Time map of research on postexercise stretching
The remaining categories (e.g., inter-set, independent sessions, at night) combined were represented in only 13 trials (4.2%) (see ESM Sect. 2.2 for full details) [87, 95, 124, 150, 154, 175, 191, 247, 262, 268, 273, 312, 352]. Of note, all inter-set research with athletes was performed between 2009 and 2015 and limited to males [95, 247, 262, 352]. Additionally, the within-session timing of the stretching intervention was unclear or unreported in 13 trials (4.3%) [85, 90, 92, 106, 131, 141, 171, 188, 208, 235, 265, 274, 311].
Intervention-Level Information
The full details of intervention-level related features can be found in the ESM (Sect. 2.3) and a summary of key features is presented in Sect. 3.7 (EGM).
Stretching Interventions
Static active stretching was the most common modality (k = 187, 62.3%), followed by dynamic stretching (k = 115, 38.3%), and static passive stretching (k = 77, 25.7%). PNF was implemented in 36 trials [12.0%, mostly contract–relax (k = 22), with the remaining methods being represented in less than 4 trials each], ballistic stretching in 13 trials (4.3%), and static stretching (unclear if active or passive) in 6 trials (2.0%). The remaining stretching modalities (e.g., SGA) were applied in two or less studies each (see ESM Sect. 2.3 for further details).
Overall, 154 trials (51.3%) applied a single stretching modality (e.g., ballistic stretching [205], PNF [142]), 133 trials (44.3%) compared two or more stretching modalities (e.g., dynamic stretching versus static active stretching [61]), and 11 trials (3.7%) implemented a single combination of stretching modalities (e.g., dynamic stretching + static active stretching within the same intervention group [314]). Twelve trials (4.0%) had at least one group performing some stretching modality with superimposed vibration (e.g., static active stretching + vibration [235]) (k = 10, 3.3%), heat (k = 2, 0.6% [106, 176]), or ice (k = 1, 0.3% [106]); considering the eligibility criteria, these were classified as being comparators.
Twenty-two trials (7.3%) compared different doses within a given stretching modality (e.g., 1 versus 2 versus 3 sets of ballistic stretching [205]; 6 versus 12 versus 18 repetitions of dynamic stretching [121]; and 35 s repetitions versus 65 s repetitions of PNF contract–relax [142]). There were specific comparisons within dynamic stretching: three trials (1.0%) compared stationary dynamic stretching versus dynamic stretching while moving [97, 167, 168], and one trial (0.3%) compared dynamic stretching performed at self-paced versus self-paced with additional forces versus maximal speed [343]. Five trials (1.7%) compared continuous with intermittent static active or passive stretching [82, 103, 114, 147, 149]. A single trial (0.3%) included a comparison of static active stretching to differing intensity thresholds: less than to the point of discomfort versus to the point of discomfort [117]. Occasionally (k = 7, 2.3%), the order of the interventions (e.g., dynamic stretching + static active stretching versus static active stretching + dynamic stretching [322]) was compared [70, 77, 91, 117, 216, 315, 322]. Additional information is available in the ESM (Sect. 2.3).
Nonstretching Comparators
A total of 169 trials (56.3%) included a no-stretching control group (i.e., passive controls or no-stretching on contralateral limb), while 76 trials (25.3%) included ≥ 1 comparator groups involving nonstretching interventions (e.g., parallel squat [202], FIFA 11 + [79]), or stretching combined with additional interventions (e.g., dynamic stretching followed by vibration foam rolling [229]). Nonstretching-related comparators were highly heterogeneous, and most were underrepresented. Strength-based training (e.g., resistance training [255], plyometrics [283]; 25 trials, 8.3%) and multimodal exercise and/or warm-up programs (e.g., FIFA 11 + [79]; 20 trials, 6.7%) were the most common comparisons, followed by aerobic-based activities (e.g., cycling [247]; 13 trials, 4.3%). A more detailed explanation is available in the ESM (Sect. 2.3).
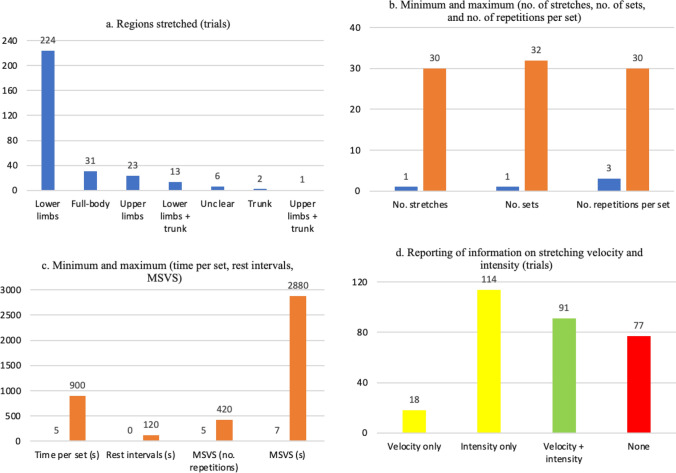
Anatomical Regions Stretched
Most trials (k = 224, 74.7%) focused on stretching the lower limbs (Fig. 4a). An additional 13 trials (4.3%) stretched the lower limbs and the trunk. The upper limbs were stretched in 23 trials (7.7%), while 31 trials (10.3%) stretched the full body. Full details are provided in the ESM (Sect. 2.3).
Fig. 4.
Summary of prescription of stretching interventions. For the stretching modalities, refer to Sect. 3.7 (EGM). *Only considering the trials that reported the relevant values. MSVS, minimum stretching volume per session
Number of Stretches Per Intervention
When reported, the number of stretching exercises per intervention (Fig. 4b) ranged from one in 54 trials (18.0%; e.g., [60, 89]) to 22 (single stretching modality [172]) or 30 (combined stretching modalities, e.g., dynamic stretching + static active stretching group [250]). We refrained from calculating pooled means and standard deviations, as there was considerable complexity that could result in miscalculations (a detailed explanation is provided in ESM Sect. 2.3).
Number of Sets
The number of sets was not always explicitly stated but, in most cases, it could be inferred from the description that a single set was performed (for exceptions, see ESM Sect. 2.3). When reported, the minimum number of sets was one (83 trials, 27.7%), while the maximum was 32 (high-volume group in [363]) (Fig. 4b). For purposes of making terminology more uniform across different stretching modalities, in cases such as static stretching, each repetition was deemed a set and we then reported time per repetition.
Four chronic trials [55, 287, 327, 336] (1.3%) had a progressive number of sets, i.e., the number of sets increased throughout the weeks (e.g., 2 sets in week 1 versus 5 sets in week 4 [336]). Fifteen trials from 16 studies (5.0%) compared different numbers of sets [75, 82, 98, 110, 178, 203–205, 249, 332, 340, 359–363] (e.g., 4 versus 8 versus 12 sets [98]), with difference between the minimum and the maximum number of sets ranging from twofold (e.g., 2 versus 4 sets [75]) to 16-fold (e.g., 1 versus 16 sets [362]). Trials comparing continuous versus intermittent static active or passive stretching [103, 114, 147, 149] also had groups performing a different number of sets (e.g., single, longer set for continuous stretching versus six smaller sets for intermittent stretching [147]). For other less common cases, see the ESM (Sect. 2.3).
Trials of multiple stretching interventions also presented relevant specificities regarding the number of sets. For example, in 30 trials (10.0%) the number of sets was not equated between the interventions (e.g., one set for static active stretching versus three sets for dynamic stretching [66]). The difference in number of sets ranged from a 133.3% increase (three sets for Mulligan stretching versus four sets for static passive stretching [90]) to a 500% increase (two sets for static passive stretching versus ten sets for dynamic stretching [146]). In a subset of trials, the difference in the number of sets was mostly between combined versus noncombined interventions, but the implementation could be the reverse. For example, one trial applied two sets for the static passive stretching and dynamic stretching interventions, but only one set for the combined dynamic + static passive stretching groups [77], possibly in an attempt to match training volume. Conversely, another trial implemented two sets of dynamic stretching, but a combined group performed three sets of static passive stretching in addition to the two sets of dynamic stretching [167], effectively increasing training volume.
Number of Repetitions or Time Per Set
For interventions reporting time, values ranged from 5 s (e.g., [178, 343]) to 900 s [39, 60] (Fig. 4c). In nine trials (3.0%) [81, 82, 142, 151, 180, 224, 340, 359, 360], different durations were compared (e.g., 5 s for the five-set group versus 30 s for the single-set group [359, 360] or 35 s for the low-volume group versus 65 s for the high-volume group [142]). This was obviously extended to the trials comparing continuous versus intermittent stretching [103, 114, 147, 149]. In some experiments, the duration could vary [237, 252, 259, 279, 280, 336, 367] (e.g., 19–30 s [336]), but without a rationale being provided and without an analysis of whether that varying duration had an impact on the results. Two trials [270, 327] implemented a progressively increasing duration (e.g., 45 s in the first 3 weeks versus 75 s in the last 6 weeks [270]).
For interventions reporting repetitions per set, values ranged from 3 (for the ballistic stretching group in [331]) to 30 (for the dynamic stretching groups in [330]) (Fig. 4b). One trial compared different volumes (6 versus 12 versus 18 repetitions) [121]. Five trials from seven studies (1.7%) presented a variable number of repetitions [237, 243, 279–281, 321, 337] (e.g., 3–10 repetitions for the dynamic stretching group [243]), but without a rationale behind it or any monitoring being implemented to assess the impact of such variation on the results. One trial implemented a progressive increase in the number of repetitions, starting with 15 and adding 5 repetitions every three sessions [258].
Trials of multiple stretching modalities could either report all modalities in time (e.g., 30 s for both dynamic and static active stretching [220, 221]) or report some modalities in time and others in repetitions (e.g., 10 repetitions for dynamic stretching, 90 s for static active stretching [314]). Accordingly, combined interventions could be reported in uniform units (e.g., 120 s of dynamic stretching + 300 s of static passive stretching [244]) or in nonuniform units (e.g., 30 s of ballistic stretching + 15 repetitions of dynamic stretching [219]). However, multiple reporting problems were identified and are detailed in the ESM (Sect. 2.3).
Rest Intervals
When reported (k = 187, 62.3%), it was not always clear whether the rest intervals were between exercises or between sets. Regardless, rest intervals ranged from 0 s (e.g., [105, 276]) to 120 s [57] (Fig. 4c). While most trials reporting rest intervals provided fixed values, some provided a narrow (e.g., 5–8 s [281]) or large (e.g., 45–60 s [93]) range of possible values. Some dynamic stretching trials reported recovery in terms of a walked distance (e.g., 20 m walking recovery [167]). It should be highlighted that some trials provided rest intervals that were longer than the duration of each set [56, 57, 184, 242, 249, 335, 342, 343, 351]. For example, one trial requested the athletes to perform 3 sets of 10 s repetitions of combined static active and passive stretching, but the rest between exercises lasted 30 s [184], i.e., the work to rest ratio was 1:3. Additional information is available in the ESM (Sect. 2.3).
Minimum Stretching Volume Per Session
There was insufficient information to assess minimum stretching volume per session in 32 trials (10.7%). For interventions reported in seconds, the minimum stretching volume per session ranged from 7 s of static passive stretching [218] to 2880 s of PNF (contract–relax) in the last 2 weeks of the intervention [327] (Fig. 4c). For those reported in number of repetitions, the minimum stretching volume per session was 5 repetitions [267] and the maximum was 420 [330] (Fig. 4c). As for other variables (e.g., age, number of stretches per intervention), we refrained from providing pooled means and standard deviations due to the mixed character of several trials, such as: (i) having different volume groups (e.g., low versus intermediate versus high volume groups, ranging from 100 to 300 repetitions [205], or 200 s in the smaller duration group versus 1200 s in the larger duration group [82]); (ii) presenting a dynamic, evolving volume across the trial (e.g., 60 repetitions during the first week sessions versus 160 repetitions in the last week sessions [258]); (iii) having mixed reporting (e.g., a combined group performing 70 repetitions of dynamic stretching + 810 s of static active stretching [314]); or (iv) having groups with sufficient versus insufficient information to assess this variable (e.g., 360 s for static active stretching but insufficient information regarding ballistic and dynamic stretching [174]).
Stretching Velocity and Intensity
Stretching velocity (e.g., 1 repetition every 2 s for dynamic stretching [79], slowly for static active stretching [114]) and intensity (e.g., to point of discomfort [81], maximum ROM while avoiding pain [141]) were unreported in 77 trials (23.3%), 114 trials (48.0%) reported stretching intensity but not stretching velocity, and 18 trials (6.0%) reported stretching velocity but not intensity. Overall, 91 trials (30.3%) reported both stretching velocity and intensity (Fig. 4d).
Reporting of stretching intensity presented considerable variation, making intertrial comparisons challenging; however, some common trends emerged. For the few cases where intensity was prescribed (or at least reported) for ballistic stretching, it varied from reaching the point of light discomfort (e.g., [181]), to maximum ROM while avoiding pain (e.g., [238]), to extreme ROM (e.g., [174]). Reporting of intensity for dynamic stretching commonly ranged from “through active ROM” (e.g., [97]) to maximum ROM (e.g., [122]), but other descriptions were provided as well (e.g., with slight pain [281], to point of discomfort [247], or from low to high intensity [255]). Static active and passive stretching, as well as PNF, were commonly reported as being performed to certain degrees of discomfort (e.g., to point of mild discomfort [75, 167, 182], to point of discomfort [61, 142, 216]), feeling a stretch (e.g., [154, 222, 285]), or to maximum ROM (e.g., [76, 90, 201]). Often, the request to achieve maximum ROM in static active and passive stretching was followed by qualifiers such as “while avoiding pain” (e.g., [141, 327, 364]). One trial assessed static active stretching to point of discomfort versus to ~ 90% of point of discomfort [117].
Reporting of stretching intensity was not always the same for different stretching modalities within a given trial. Three scenarios occurred: (i) some trials had comparable descriptions of intensity for all included stretching modalities (e.g., maximum ROM while avoiding pain for ballistic stretching, PNF, and static active stretching [238]); (ii) other trials had different descriptions for different stretching modalities (e.g., progressing from moderate to high intensity in dynamic stretching versus maximum ROM for static active stretching [76]); (iii) still other trials specified intensity for one stretching modality, but not for the others (e.g., to point before discomfort for static active stretching but unreported for dynamic stretching [232]). Thus, the requested intensity levels were not always equated (or even reported) between groups or conditions.
The reporting of stretching velocity varied depending on the stretching modality. For example, ballistic stretching was commonly prescribed at a rate of one repetition per second (e.g., [174, 181, 202]), but some descriptions were considerably vaguer (e.g., “in rapid fashion” [331] or “with velocity” [339]). Reporting of dynamic stretching velocity ranged from highly specific information (e.g., 1 repetition every 2 s [79]) to vaguer qualitative descriptions such as “slowly” [96] or “gently” [203], sometimes specifically stating the movements had to be performed without ballistic or abrupt movements [97] or without bouncing [121]. In some cases, there was a progression in velocity (e.g., five repetitions slowly, then ten repetitions quickly [129]). One trial compared dynamic stretching at self-selected speed versus at maximal speed [343].
Stretching velocity was rarely reported for PNF, static active stretching, and static passive stretching, presumably because these modalities tend to be performed at slow velocities by default (e.g., slow progression until reaching maximum ROM, followed by even slower progression to even greater ROM during the stretch). When it was reported, it was usually using the term “slowly” (e.g., [115, 267, 360]) or similar expressions such as “gently” [349] or “smoothly” [318]. A single trial, using static passive stretching, provided an objective measure of stretching velocity, set at 20 degrees per second [187].
Within-Trial Inconsistencies in Intervention Volume
There were considerable within-trial inconsistencies that may have compromised the interpretation of results (see ESM Sect. 2.3 for more details). An example emerges from trials that aimed to compare different interventions that were not volume equated (within reasonable limits). As an example, one trial compared 90 s of static active stretching to 20 min of moist heat pack application [176]. Another trial compared 150 s of static active stretching with 750 s of combined static active and dynamic stretching [232].
Outcome-Level Information
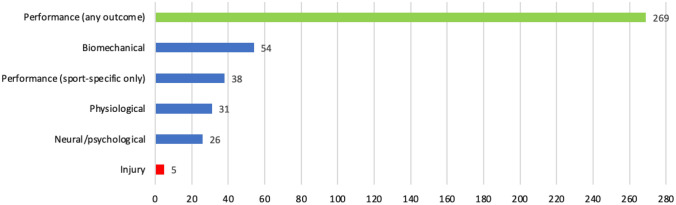
Overview of Outcome-Level Information
Complete details of outcome-level features can be found in the ESM (Sect. 2.4) and a summary of the most salient features in Sect. 3.7 of the manuscript (EGM). In summary, five outcome domains were considered: physiological, biomechanical, neural/psychological, performance related, and injury related. No trial assessed outcomes across more than three domains, e.g., physiological, biomechanical, and performance [169, 170]. Biomechanical outcomes were assessed in 54 trials (18.0%), physiological outcomes in 31 (10.3%), and neural/psychological in 26 trials (8.7%). Only five trials (1.7%) assessed injury-related outcomes [e.g., injury incidence, risk ratios (RR)] [87, 99, 105, 177, 312], none of which supported the purported preventive role of stretching. Considering the disparity between the widespread interest on the topic of stretching for injury prevention and the scarcity of studies on the subject (at least with athletes), we provide more in-depth information in the ESM (Sect. 2.5).
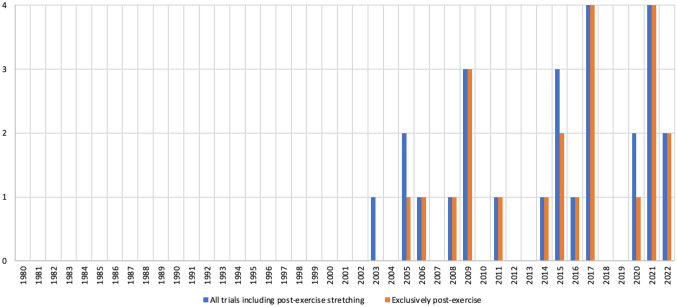
Most trials (k = 269, 89.7%) reported performance-related outcomes, mainly focusing on strength/power and ROM (49.7% and 41.0% of trials, respectively), followed by speed (20.3% of trials), and change of direction (COD; 12.3% of trials). All other performance-related outcomes (e.g., balance, endurance, proprioception) were assessed in fewer than 5% of trials. Importantly, sport-specific performance tests were applied in only 38 trials published in 43 studies (12.7%) across 17 sports (most commonly soccer, swimming, artistic gymnastics, and volleyball, in order). Figure 5 synthesizes the research trends for outcome domains.
Fig. 5.
Number of trials assessing each outcome domain
Main Outcomes Assessed Per Domain
Regarding physiological outcomes, blood lactate [115, 203–205, 247, 262, 271, 347, 367] and heart rate [169, 170, 174, 203–205, 208, 247, 248, 287, 315, 347, 349, 353, 354, 357] were the most commonly reported, but a diverse range of other outcomes were reported, such as core temperature [169, 170] and inflammation [60].
Biomechanical outcomes ranged from kinetic and/or kinematic analysis of sport-specific actions (e.g., [64, 206, 253]) to measures of muscle properties such as fascicle length and muscle thickness, among others (e.g., [122, 148, 270]). In this context, 22 trials (7.3%) assessed electromyographic activity, but only two focused on the upper limb [200, 215].
Neural/psychological outcomes including perceived pain [57, 99, 187, 251, 292, 304], soreness [139, 245, 277, 278, 286, 320, 324], and exertion [174, 203–205, 245, 248, 264, 287, 315, 349, 353] were the most commonly reported outcomes in this context, but other outcomes were considered as well (e.g., mood state [245, 347]).
Among performance outcomes, the strength/power-related outcomes (e.g., isokinetic knee flexion and extension [322], medicine ball throw [39]) dominated the research, having been assessed in 149 trials (49.7%). ROM (e.g., sit and reach [331], trunk lateral flexion [343]) was assessed in 123 trials (41.0%), followed by speed (e.g., 15 m sprint [275], curved 55 m sprint [200]) in 61 trials (20.3%). COD (e.g., Illinois Agility Test [63, 326]) was reported in 37 trials (12.3%), and balance (e.g., Star Excursion Balance Test [131, 154]) in 12 trials (4.0%) [53, 55, 65, 98, 120, 131, 154, 200, 252, 276, 289, 301]. Speed endurance (e.g., 6 × 20 m sprints [95]) was assessed in 11 trials published in 12 studies (3.7%) [75, 95, 97, 191, 203–205, 223, 231, 315, 351, 365]. Endurance (e.g., time to exhaustion in supramaximal cycling [247]) was reported in ten trials (3.3%) [137, 233, 247, 248, 342, 349, 352–354, 366]. Proprioception (e.g., knee joint position sense [266, 345]) was reported in six trials (2.0%) [119, 160, 266, 289, 296, 345]. Other outcomes (e.g., global coordination testing [174], functional independence measure score [304], strength endurance [187]) were usually assessed in only one to three trials and had no overall expression.
Sport-specific performance tests were applied in only 38 trials (12.7%) across 17 sports: archery [334], artistic gymnastics [53, 166, 209, 243, 313], badminton [229], baseball [190], Brazilian jiu-jitsu [115], handball [239, 258], fencing [331], ice hockey [288], judo [39], rhythmic gymnastics [145], rowing [286], soccer [67, 69, 174, 182, 189, 210, 252, 305–309], swimming [54, 134, 212, 228, 254, 271], table tennis [199], tennis [184, 238], track and field [283], and volleyball [114, 132, 279–281].
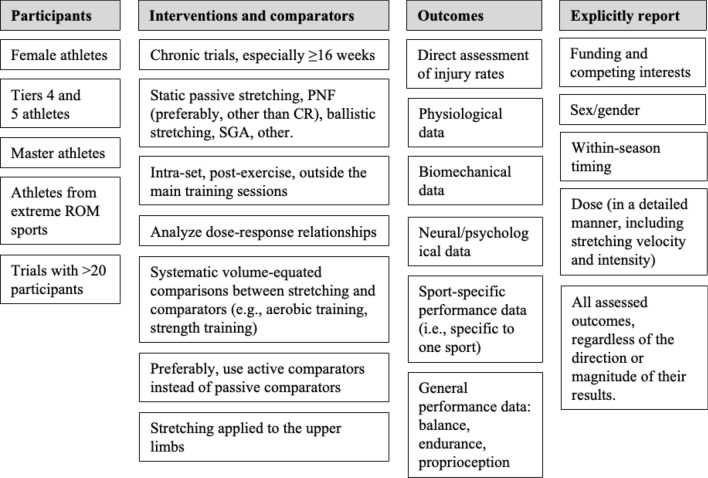
Evidence Gap Map
Figure 6 shows the EGM that synthesizes the patterns and gaps that were previously identified. Beyond visually conveying the information in a user-friendly manner, some data are shown with a slightly different perspective to avoid redundancy with the previously presented figures.
Fig. 6.
Evidence gap map of stretching research with healthy athletes
Inspection of the EGM reveals some key findings: (1) there was an over-abundance of trials with up to 20 participants, but very few large-scale (> 100 participants) trials; (2) most research was performed with male participants, and several trials failed to report on sex; (3) soccer dominated the research efforts, while sports such as artistic gymnastics and martial arts were severely underrepresented; (4) most athletes were tier 2, with scarce research with tier 4 athletes and none with tier 5 athletes; (5) most information derived from acute trials, while chronic trials were mostly ≤ 8 weeks in length and rarely surpassed 16 weeks; (6) trials mostly explored stretching interventions with 3 weekly sessions, with 12–23 total sessions, performed in the context of the warm-up part of the training session; (7) most trials did not report season timing; (8) static active stretching predominated the body of research and was mostly compared with nonstretching passive controls; (9) performance outcomes were very commonly assessed, while biomechanical, physiological, and neural/psychological assessments were less often performed; (10) within performance-related outcomes, trials mostly focused on strength/power and ROM; and (11) only scarce data were available regarding injuries.
Discussion
Stretching is implemented widespread in multiple sports and different contextual settings. Due to the high number of studies investigating the effects of stretching using different methodologies and protocols, an updated and reliable summary from direct comparisons between studies becomes cumbersome and often challenging. Aiming to guide and inform future research and funding policies, we systematically reviewed the existing literature to map the existing research and identify the trends and current gaps relating to stretching interventions in healthy athletes with a minimum competitive level of tier 2 or higher [52].
Are All Athletes the Same? Who is Being Studied?
Roughly 7000 athletes were included across the 300 trials, but the median of athletes per trial was 18, and 94.0% of trials had less than 50 athletes. This means that most trials were likely underpowered, and their results lack generalizability, a common problem within the sports science field [369–372]. Such a pattern would be expected if there was a predominance of trials of the most high-level athletes (i.e., tiers 4 and 5), as these populations are statistically small and challenging to enrol in research [52, 372] (being possibly concerned that experimental interventions may disrupt their training routines and, eventually, impair performance). Notwithstanding, there was a complete lack of stretching-related research with tier 5 athletes (a noticeable gap in itself), and research including tier 4 athletes (k = 22) represented only 7.3% of all trials. The field of elite sport research faces significant challenges arising from the limited availability of elite athletes as study participants. Longitudinal case studies, ensuring a large number of data points while upholding the fundamental principles that underlie successful clinical trials, could potentially be devised to investigate such high-level athletes [372]. Currently, most knowledge on stretching in athletes is likely limited to underpowered trials and involving nonelite athletes whose results should not be lightly transferred to elite athletes [372]. The results from our scoping review pertain only to the healthy athletic populations (i.e., tier 2 or higher [52]) and should not be extrapolated to other populations, including athletes in rehabilitation contexts.
Sex
Typical of sex imbalances in sports sciences publications [373–379], female athletes are underrepresented in the stretching literature (~ 20% versus ~ 65% of male athletes). The missing percentage refers to trials that failed to report sex, potentially meaning they were also male, considering societal biases. The observed disparity in sex representation also aligns with the broader imbalance in samples within the field of sport and exercise psychology [379] and extends to research authorship as well [380]. A discussion of the societal biases that may underlie this phenomenon is beyond the scope of our review, but we strongly support increasing research efforts in female athletes. To rectify this sex-based imbalance, it is crucial for funders, researchers, and journal editors to collaborate actively and diligently toward making significant advancements in addressing this issue.
Age
Age was reported very differently across trials, but a rough simplification highlights an age range from 8 to ~ 40 years, and mostly limited to athletes under 30 years of age. Therefore, it can be concluded that research on stretching is mostly focused on adolescents and young adults in their most physically active years and when organized sports participation and engagement in physical activity in general are most common [381, 382]. Notwithstanding, there has been increased participation in sports by older adults, with rising awareness of the specificity of the master athlete in the sports science literature [383–388]. Our scoping review showed that research on stretching in master athletes is largely lacking, and so how these older athletes respond to stretching interventions is currently unclear.
Sports
While at least 43 sports were represented (soccer being the most studied), there was a noticeable scarcity of trials performed in sports such as artistic or rhythmic gymnastics, or in martial arts. Stretching, as the most popular exercise modality for improving ROM [3, 4], might be more determinant for performance in some of these sports (e.g., gymnastics, martial arts), where extreme ROM is required [265, 314, 389]. As these types of sports are greatly underrepresented in the stretching literature (as our scoping review has shown), no strong conclusions can be made as to the role of stretching in these sports, and it is unclear whether findings from other sports (e.g., soccer, volleyball) can be extrapolated to gymnastics or martial arts [5]. Even in sports not requiring extreme ROM, there may be important differences in the typical ROMs presented [390], i.e., different sports will pose specific necessities and therefore stretching may play different roles.
Context Matters! In What Circumstances are Athletes Being Studied?
Over 80% of stretching research in athletic populations focused only on the acute effects. Knowledge about chronic effects of stretching in athletes derives from a much narrower body of research, and no trial lasted more than 21 weeks. Therefore, all knowledge concerning the chronic effects of stretching in athletes derives from trials lasting < 6 months. However, this is an overly optimistic scenario because trials assessing chronic effects lasted a median of 6 weeks, and only 2.0% of trials lasted ≥ 16 weeks. This seems a common limitation within research dealing with other training methods and concepts (e.g., plyometric training [374], periodization [391]). Furthermore, almost 70% of chronic trials implemented ≤ 3 weekly stretching sessions, which may be inferior to common practice in many sports (e.g., artistic gymnastics [392]), especially at higher levels of practice. Possibly, future terminological revisions should consider a category between acute and chronic (e.g., delayed effects?). As explained in Sect. 2, we avoided stipulating an arbitrary temporal threshold for what should be considered a chronic intervention. Regardless, we also feel that trials lasting 1 week or having only three sessions in total should probably not be considered chronic. In summary, there is still a huge knowledge gap about the chronic effects of stretching interventions in athletes, which may result from the extensive resources required and the challenges inherent in performing such longitudinal studies [393].
Season timing may influence the athletes’ fitness status at the time of testing [52, 394]. It may also impact the willingness of athletes to engage in experimental interventions; for example, weekly matches may result in time constraints and concerns about recovery [395, 396], which may influence the weekly contents and workload. Overall, 40% of stretching research with athletes reported the within-season timing. When reported, the competitive season was more common than the off-season and preseason combined. This seems similar to other research training methods (e.g., [397]). Future studies should more consistently report within-season timing.
Most trials (~ 85%) implemented stretching in the context of a warm-up (either in isolation or as a part of the warm-up), denoting a considerable imbalance in the literature and providing a very limited account of stretching effects when applied in other settings. For example, postexercise stretching represented only ~ 7% of all trials. Despite widespread use of [398–401], and support for post-exercise stretching [402, 403], it seems largely ineffective as a recovery method [21, 404], and there is little scientific scrutiny of its effects in athletes. Even less is known about other applications of stretching (e.g., inter-set, at night before falling asleep), representing a major gap in research.
All Stretching is Not the Same: What Stretching Modalities are Being Implemented?
According to the literature, static active, static passive, dynamic, ballistic, and PNF are the most commonly used stretching methods [1, 3]. Stretching research with healthy athletes is dominated by static active stretching, represented in > 60% of trials, followed by dynamic stretching (< 40% of trials). Of note, trials could implement multiple stretching modalities and doses. Static passive stretching and PNF (mostly limited to the contract–relax method) were analyzed in only ~ 25% and 12% of trials, respectively, and ballistic stretching represented less than 5% of trials. This means that further research is required to better understand the effects of static passive stretching, PNF, and ballistic stretching in athletes. It is possible that static passive stretching and PNF may play a more determinant role in performance in sports requiring extreme ROM (e.g., gymnastics, martial arts), and this literature gap may therefore differentially affect distinct sports.
Alternative stretching methods (e.g., SGA) are being largely neglected by research, which does not benefit scientific advances and fails to either support or recommend against their application. The effects of combining stretching with heat, cold, or vibration superimposed on the stretches are also largely unexplored. Finally, ~ 75% of the trials applied stretching to the lower limbs, with much less information being available concerning the trunk and the upper limbs. This is problematic, as the upper limbs and the trunk play a major role in several sports (e.g., handball, throwing-based track and field events, volleyball, and weightlifting, among others). The existing imbalance in the body of knowledge concerning the primary areas of intervention raises concerns about the potential generalization of evidence that is specifically researched. To mitigate this issue, it is crucial to foster a greater proportion of research in less explored domains and to incorporate an analysis of anatomical variability. Such an approach would shed light on the diverse mechanisms of adaptation and underscore the significance of considering case studies that reflect this variability.
Everything May be Superior to Nothing: What Comparisons are Being Performed?
Beyond comparisons between different stretching modalities and doses, more than half of the trials included a no-stretching control group that otherwise was subjected to the same procedures as the stretching groups. This is highly relevant to ascertain the effects of stretching compared with individuals who were maintained at rest (i.e., passive controls), and can be used to justify stretching. However, alternative interventions may show equal or superior efficacy or effectiveness (e.g., strength training versus stretching for small ROM improvements [24, 405]). Moreover, such relative effectiveness is likely to vary depending on the specific outcome being assessed and with potential varying adherence. Unfortunately, only ~ 25% of all trials included active, nonstretching-related comparators (e.g., FIFA 11 +), or stretching added to some other intervention not included in the stretching-only groups (e.g., stretching followed by vibration foam rolling). These trials were spread across more than 15 classes of comparators (e.g., foam rolling, aerobic training), and within each class there were considerable differences in the interventions. Moreover, these interventions were often not equated for volume. Therefore, systematic comparisons between stretching and alternative interventions are lacking, with some exceptions regarding strength training and multimodal exercise programs.
How Much? Is Dose-Response Being Scrutinized?
Volume, intensity, and weekly frequency may strongly influence the effects of stretching [15]. However, less than 8% of all trials compared different doses of stretching (usually, through manipulation of duration, number of repetitions and/or number of sets), and only one trial compared different intensity thresholds [117]. Overall, the number of stretches varied widely (1–22), occasionally even between two stretching groups within the same trial (e.g., [232]). The same was true for the number of sets (1–32), number of repetitions (3–30), time per set (5–900 s), rest intervals (0–120 s), and, consequently, in the minimum stretching volume per session (5–420 repetitions; 7–2880 s). Information concerning stretching velocity and intensity was reported very inconsistently across and within trials, and only less than ~ 33% of all trials provided sufficient information to assess both velocity and intensity. Although some protocol variability is required to search for the most suitable stretching protocol(s), there is also the need for replicability and reproducibility. Likewise, equalizing the volume between stretching methods is challenging but needed. Perhaps time under tension could be applied, but it is difficult to assess this variable in dynamic or ballistic stretching as the tension is not uniform during the course of the movement. More research is required to better understand how to properly equate training volume when comparing different stretching interventions.
As a result, there is a paucity of information pertaining to dose–response relationships in the context of implementing stretching protocols for athletes, despite the importance of understanding such relationships to more appropriately design and prescribe exercise interventions [406–410]. Relatedly, it is further imperative to incorporate the concept of individualization into training practices and consider the impact of human variability when addressing dose–response relationships [411–414]. However, our understanding of this individualized training approach remains limited, necessitating the establishment of new research avenues to explore this direction comprehensively.
Are We Looking for the Most Relevant Outcomes? What Has the Literature Assessed?
Physiological outcomes were assessed in only ~ 10% of trials, (most commonly, blood lactate and heart rate), and the same applies to neural and/or psychological outcomes (commonly perceived pain, perceived soreness, and perceived exertion). More information is available on how stretching affects biomechanical outcomes, but less than 20% of trials reported such outcomes. The limited reporting on physiological, neural/psychological, and biomechanical outcomes precludes a robust understanding of the mechanisms underlying changes in the commonly assessed performance outcomes, which affects knowledge on causal relationships and thus provides limited information regarding the optimization of training prescription [415].
Performance outcomes were reported in ~ 90% of trials. However, most reporting referred to strength/power and ROM, with less information available concerning speed and COD (~ 10 to 20% of trials). Outcomes reported in less than 5% of trials included balance, speed endurance, endurance, and proprioception, among others. The predominance of strength/power outcomes was expected, as these constructs are strongly associated with performance in athletes (e.g., [416–419]), while ROM is perhaps the most obvious outcome to check when implementing stretching interventions. What is surprising is the very limited exploration of how stretching affects other parameters such as balance, endurance, or proprioception. Furthermore, sport-specific performance tests were applied in < 15% of trials. Currently, most knowledge on performance-related effects of stretching derives from general tests (e.g., 20 m sprint, 1 RM strength tests, sit and reach) that are transversal but lack specificity, with much less being known about the effects of stretching on sport-specific performance.
A glaring gap is the lack of trials investigating the effects of stretching on injury prevention/injury risk reduction. We identified a lacklustre total of five trials (mostly chronic postexercise stretching interventions with male athletes) that assessed injury (i.e., that provided data on injury incidence, prevalence, or risk, instead of relying exclusively on surrogate measures of injury risk, such as strength). These trials failed to support the notion that stretching reduces injury risk and, despite being limited to athlete tiers 2 or higher, align well with the results of several reviews on the topic [4, 16, 17, 420–425]. Of note, not all reviews on the topic reach the same conclusions [426], and these reviews were not necessarily limited by the minimum PCF tier 2. This is perhaps the most striking gap in our knowledge, and probably should be the focus of ample research investment in the near future.
Additional opportunities for research with athletes (some of which have started being scrutinized in different populations) would include exploration of the effects of stretching on venous and lymphatic circulation [427, 428], nonlocal effects of stretching [13, 14], and the effect of previous knowledge/expectations on the efficacy of stretching interventions [429].
What Lies Ahead? Priorities for Future Research
Based on the most relevant gaps that were identified, Fig. 7 shows suggested research priorities. This summary provides opportunities for funders and researchers to focus on less researched areas of stretching, while potentially eliminating wasteful research on further investigating topics that are already well researched. We also propose that more funding is provided for the development of stretching-based research in African countries, as research on the topic performed in this continent is mostly limited to Tunisia. Additionally, any information concerning funding and competing interests should be mandatory, and all journals should define them as a prerequisite for publication. Finally, we highlight the need to implement efforts to avoid selective reporting of outcomes, which may bias not only the original research findings, but also future reviews on selected topics. Preregistration of experimental studies is highly advisable.
Fig. 7.
Research priorities regarding stretching interventions with athletes. CR contract–relax, PNF proprioceptive neuromuscular facilitation, ROM range of motion, SGA global active stretching (from the French original Stretching Global Actif)
Limitations
By focusing solely on athletes and establishing the PCF’s tier 2 as the minimum for inclusion, it is possible that other well-trained populations have been left out (e.g., regular gym goers engaging in noncompetitive CrossFit or bodybuilding, dancers). However, a threshold had to be established, and participation in competitions was deemed necessary to use the term “athlete.” Regardless, the sample of 316 published studies showed trends that would likely remain robust even if some extra trials had been considered. The exclusion of injured athletes precludes us from making any statements regarding the role of stretching in injury rehabilitation, while the exclusion of athletes with disabilities inhibits any statements concerning the status of stretching research in these populations. However, these specific populations were outside the scope we intended for our scoping review. Interpreting the results of the included trials should be moderated by knowledge that 66.0% did not provide a published funding statement (i.e., whether there was funding or not) and 65.6% did not provide a published statement pertaining competing interests.
Should We Reconsider the Terminology and Description of Stretching Exercises?
An additional limitation that may impact the findings deserves to be highlighted. Commonly, static stretching is deemed passive if an external agent (e.g., coach, teammate) applies the stretch to the athlete, and our scoping review followed that logic and terminology to facilitate an intuitive understanding for most readers. However, future discussions on the terminology should be considered, as in many of the so-called active stretching exercises the athletes used a part of their body to stretch another part, or they used external surfaces (e.g., walls). Therefore, those exercises would technically have a passive component. Moreover, in such cases, it was unclear whether the “self-passive” assistance was used from the beginning of the stretching until reaching the desired endpoint, or if it was used exclusively near or at the endpoint. It was further unclear how long each phase lasted, i.e., whether the stretching was mostly active with a slight passive component or the reverse. We encourage the scientific community to engage in a debate surrounding the terminology, and perhaps less commonly used taxonomy such as self-stretching [91] is appropriate. Within the concept of self-stretching, authors should carefully describe the details of each exercise, including an estimate of the role played by the active and passive phases (when applicable). The fact that so-called static active stretching may, in fact, include a considerable passive phase could impact the interpretation of findings from stretching studies.
Conclusions
There are noticeable gaps in stretching research in athletic populations, precluding a thorough knowledge of its effects. Some problems are common to most research in sports sciences (e.g., small samples; poor representation of females, master athletes, and tiers 4 and 5 athletes; lack of long-term chronic trials; scarce exploration of dose–response relationships), but there are additional relevant gaps. Most evident is the negligible number of trials assessing the effects of stretching on injury rates (and those that exist do not support a preventive effect). This refers specifically to trials containing explicit information to allow considering the participants as tier 2 or higher, and so may not be directly comparable to most reviews on the topic, which usually have broader eligibility criteria, including participants below tier 2. Therefore, the possibility of stretching reducing overall or specific (e.g., musculotendinous) injury risk in athletes (tier 2 or higher) requires more extensive research.
Furthermore, the outcomes assessed in the included trials have been largely limited to general performance tests, with reduced exploration of sport-specific performance tests and mechanistic assessments (e.g., biomechanical, physiological). Also relevant is the scarcity of trials with participants from sports demanding extreme ROM (e.g., gymnastics), and the underrepresentation of static passive stretching, PNF, and especially ballistic stretching.
Currently, most knowledge regarding applications of stretching with athletes derives from underpowered trials of nonelite athletes, assessing the acute effects of static active or dynamic stretching applied to the lower limbs compared with passive controls, and mostly performed in the context of a warm-up. This field of research seems to be limiting itself, focusing on a very narrow range of possibilities and therefore providing only a limited window for stretching and its potential effects in athletes. We advise a change in research priorities, policies, and funding, focusing future research on fulfiling the extensive existing gaps.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
None to report.
Authors contributions
JA, RA, RRC, and FMC were responsible for the initial drafting of the article. All authors were involved in the conception, design, and interpretation of data. All authors read and reviewed the manuscript critically for important intellectual content and approved the final version to be submitted. Specific contributions pertaining to data selection, extraction, and analysis are detailed in Sect. 2. All authors read and approved the final manuscript.
Funding
Open access funding provided by FCT|FCCN (b-on).
Declarations
Registration and protocol
The protocol was created (https://osf.io/6auyj/) and preregistered (https://osf.io/gu8ya) as an Open Science Framework (OSF) project and made public on 14 July 2022 (1 day before the initial database searches). We originally designed this scoping review as a living review. However, considering the amount of work involved (an extremely large number of records in the searches and a very large number of trials included in the review), our team is currently not able to guarantee future updates.
Funding
There was no financial or nonfinancial support for the review. The were no funders or sponsors of the review.
Conflict of interest
The authors have no competing interests.
Data availability
The data used to inform this review are fully disclosed either in the manuscript or in its Electronic Supplementary Material.
References
- 1.ACSM. ACSM’s Guidelines for Exercise Testing and Prescription. 10th ed. Wolters Kluwer; 2018.
- 2.Association AH: Guidelines and statements. 2020. https://professional.heart.org/en/guidelines-and-statements/guidelines-and-statements-search. Accessed 25/10/2020.
- 3.Behm DG. The science and physiology of flexibility and stretching. Implications and applications in sport performance and health. Oxon: Routledge; 2019. [Google Scholar]
- 4.Behm DG, Blazevich AJ, Kay AD, McHugh M. Acute effects of muscle stretching on physical performance, range of motion, and injury incidence in healthy active individuals: a systematic review. Appl Physiol Nutr Metab. 2016;41(1):1–11. doi: 10.1139/apnm-2015-0235. [DOI] [PubMed] [Google Scholar]
- 5.Afonso J, Olivares-Jabalera J, Andrade R. Time to move from mandatory stretching? We need to differentiate “can i?” From “do i have to?”. Front Physiol. 2021;12:714166. doi: 10.3389/fphys.2021.714166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fukaya T, Matsuo S, Iwata M, Yamanaka E, Tsuchida W, Asai Y, Suzuki S. Acute and chronic effects of static stretching at 100% versus 120% intensity on flexibility. Eur J Appl Physiol. 2021;121(2):513–523. doi: 10.1007/s00421-020-04539-7. [DOI] [PubMed] [Google Scholar]
- 7.de Baranda PS, Ayala F. Chronic flexibility improvement after 12 week of stretching program utilizing the ACSM recommendations: hamstring flexibility. Int J Sports Med. 2010;31(6):389–396. doi: 10.1055/s-0030-1249082. [DOI] [PubMed] [Google Scholar]
- 8.Konrad A, Stafilidis S, Tilp M. Effects of acute static, ballistic, and PNF stretching exercise on the muscle and tendon tissue properties. Scand J Med Sci Sports. 2017;27(10):1070–1080. doi: 10.1111/sms.12725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Medeiros DM, Martini TF. Chronic effect of different types of stretching on ankle dorsiflexion range of motion: systematic review and meta-analysis. Foot. 2018;34:28–35. doi: 10.1016/j.foot.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 10.Freitas SR, Mendes B, Le Sant G, Andrade RJ, Nordez A, Milanovic Z. Can chronic stretching change the muscle-tendon mechanical properties? A review. Scand J Med Sci Sports. 2018;28(3):794–806. doi: 10.1111/sms.12957. [DOI] [PubMed] [Google Scholar]
- 11.Guissard N, Duchateau J. Effect of static stretch training on neural and mechanical properties of the human plantar-flexor muscles. Muscle Nerve. 2004;29(2):248–255. doi: 10.1002/mus.10549. [DOI] [PubMed] [Google Scholar]
- 12.Blazevich AJ, Cannavan D, Waugh CM, Miller SC, Thorlund JB, Aagaard P, Kay AD. Range of motion, neuromechanical, and architectural adaptations to plantar flexor stretch training in humans. J Appl Physiol. 2014;117(5):452–462. doi: 10.1152/japplphysiol.00204.2014. [DOI] [PubMed] [Google Scholar]
- 13.Behm DG, Alizadeh S, Anvar SH, Drury B, Granacher U, Moran J. Non-local acute passive stretching effects on range of motion in healthy adults: a systematic review with meta-analysis. Sports Med. 2021;51(5):945–959. doi: 10.1007/s40279-020-01422-5. [DOI] [PubMed] [Google Scholar]
- 14.Behm DG, Alizadeh S, Drury B, Granacher U, Moran J. Non-local acute stretching effects on strength performance in healthy young adults. Eur J Appl Physiol. 2021;121(6):1517–1529. doi: 10.1007/s00421-021-04657-w. [DOI] [PubMed] [Google Scholar]
- 15.Thomas E, Bianco A, Paoli A, Palma A. The relation between stretching typology and stretching duration: the effects on range of motion. Int J Sports Med. 2018;39(4):243–254. doi: 10.1055/s-0044-101146. [DOI] [PubMed] [Google Scholar]
- 16.Small K, Mc Naughton L, Matthews M. A systematic review into the efficacy of static stretching as part of a warm-up for the prevention of exercise-related injury. Res Sports Med. 2008;16(3):213–231. doi: 10.1080/15438620802310784. [DOI] [PubMed] [Google Scholar]
- 17.Lewis J. A systematic literature review of the relationship between stretching and athletic injury prevention. Orthop Nurs. 2014;33(6):312–320. doi: 10.1097/nor.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 18.Afonso J, Claudino JG, Fonseca H, Moreira-Gonçalves D, Ferreira V, Almeida JM, et al. Stretching for recovery from groin pain or injury in athletes: a critical and systematic review. J Funct Morphol Kinesiol. 2021;6(3):73. doi: 10.3390/jfmk6030073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaabene H, Behm DG, Negra Y, Granacher U. Acute effects of static stretching on muscle strength and power: an attempt to clarify previous caveats. Front Physiol. 2019;10:1468. doi: 10.3389/fphys.2019.01468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blazevich AJ, Gill ND, Kvorning T, Kay AD, Goh AG, Hilton B, et al. No effect of muscle stretching within a full, dynamic warm-up on athletic performance. Med Sci Sports Exerc. 2018;50(6):1258–1266. doi: 10.1249/mss.0000000000001539. [DOI] [PubMed] [Google Scholar]
- 21.Afonso J, Clemente FM, Nakamura FY, Morouço P, Sarmento H, Inman RA, Ramirez-Campillo R. The effectiveness of post-exercise stretching in short-term and delayed recovery of strength, range of motion and delayed onset muscle soreness: a systematic review and meta-analysis of randomized controlled trials. Front Physiol. 2021;12:677581. doi: 10.3389/fphys.2021.677581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Hooren B, Peake JM. Do we need a cool-down after exercise? A narrative review of the psychophysiological effects and the effects on performance, injuries and the long-term adaptive response. Sports Med. 2018;48(7):1575–1595. doi: 10.1007/s40279-018-0916-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herbert RD, de Noronha M, Kamper SJ. Stretching to prevent or reduce muscle soreness after exercise. Cochrane Database Syst Rev. 2011;7:Cd004577. doi: 10.1002/14651858.CD004577.pub3. [DOI] [PubMed] [Google Scholar]
- 24.Afonso J, Ramirez-Campillo R, Moscão J, Rocha T, Zacca R, Martins A, et al. Strength training versus stretching for improving range of motion: a systematic review and meta-analysis. Healthcare. 2021;9(4):427. doi: 10.3390/healthcare9040427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saraiva AR, Reis VM, Costa PB, Bentes CM, Costa ESGV, Novaes JS. Chronic effects of different resistance training exercise orders on flexibility in elite judo athletes. J Hum Kinet. 2014;40:129–137. doi: 10.2478/hukin-2014-0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nuzzo JL. The case for retiring flexibility as a major component of physical fitness. Sports Med. 2020;50(5):853–870. doi: 10.1007/s40279-019-01248-w. [DOI] [PubMed] [Google Scholar]
- 27.Konrad A, Nakamura M, Tilp M, Donti O, Behm DG. Foam rolling training effects on range of motion: a systematic review and meta-analysis. Sports Med. 2022;52(10):2523–2535. doi: 10.1007/s40279-022-01699-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Konrad A, Nakamura M, Paternoster FK, Tilp M, Behm DG. A comparison of a single bout of stretching or foam rolling on range of motion in healthy adults. Eur J Appl Physiol. 2022;122(7):1545–1557. doi: 10.1007/s00421-022-04927-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilke J, Müller AL, Giesche F, Power G, Ahmedi H, Behm DG. Acute effects of foam rolling on range of motion in healthy adults: a systematic review with multilevel meta-analysis. Sports Med. 2020;50(2):387–402. doi: 10.1007/s40279-019-01205-7. [DOI] [PubMed] [Google Scholar]
- 30.Warneke K, Zech A, Wagner CM, Konrad A, Nakamura M, Keiner M, et al. Sex differences in stretch-induced hypertrophy, maximal strength and flexibility gains. Front Physiol. 2022;13:1078301. doi: 10.3389/fphys.2022.1078301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Warneke K, Konrad A, Keiner M, Zech A, Nakamura M, Hillebrecht M, Behm DG. Using daily stretching to counteract performance decreases as a result of reduced physical activity-a controlled trial. Int J Environ Res Public Health. 2022 doi: 10.3390/ijerph192315571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Warneke K, Lohmann LH, Keiner M, Wagner CM, Schmidt T, Wirth K, et al. Using long-duration static stretch training to counteract strength and flexibility deficits in moderately trained participants. Int J Environ Res Public Health. 2022 doi: 10.3390/ijerph192013254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cui J, Blaha C, Moradkhan R, Gray KS, Sinoway LI. Muscle sympathetic nerve activity responses to dynamic passive muscle stretch in humans. J Physiol. 2006;576(Pt 2):625–634. doi: 10.1113/jphysiol.2006.116640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Costa e Silva G, Costa PB, da Conceição RR, Pimenta L, de Almeida RL, Sato MA. Acute effects of different static stretching exercises orders on cardiovascular and autonomic responses. Sci Rep. 2019;9(1):15738. doi: 10.1038/s41598-019-52055-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Inami T, Shimizu T, Baba R, Nakagaki A. Acute changes in autonomic nerve activity during passive static stretching. Am J Sports Sci Med. 2014;2(4):166–170. doi: 10.12691/ajssm-2-4-9. [DOI] [Google Scholar]
- 36.Thomas E, Bellafiore M, Gentile A, Paoli A, Palma A, Bianco A. Cardiovascular responses to muscle stretching: a systematic review and meta-analysis. Int J Sports Med. 2021;42(6):481–493. doi: 10.1055/a-1312-7131. [DOI] [PubMed] [Google Scholar]
- 37.Kato M, Nihei Green F, Hotta K, Tsukamoto T, Kurita Y, Kubo A, Takagi H. The efficacy of stretching exercises on arterial stiffness in middle-aged and older adults: a meta-analysis of randomized and non-randomized controlled trials. Int J Environ Res Public Health. 2020;17(16):5643. doi: 10.3390/ijerph17165643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Andrade RJ, Freitas SR, Hug F, Sant GL, Lacourpaille L, Gross R, et al. Chronic effects of muscle and nerve-directed stretching on tissue mechanics. J Appl Physiol. 2020;129(5):1011–1023. doi: 10.1152/japplphysiol.00239.2019. [DOI] [PubMed] [Google Scholar]
- 39.Almeida Júnior H, De Souza RF, Aidar FJ, Da Silva AG, Regi RP, Bastos AA. Global Active stretching (SGA®) practice for judo practitioners' physical performance enhancement. Int J Exerc Sci. 2018;11(6):364–374. doi: 10.70252/YWBV9174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Seo HR, Kim TH. The effects of Gyrotonic expansion system exercise and trunk stability exercise on muscle activity and lumbar stability for the subjects with chronic low back pain. J Exerc Rehabil. 2019;15(1):129–133. doi: 10.12965/jer.1836512.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Radaelli R, Freitas J, Almeida N, Vaz JR, Freitas SR. Which stretching instruction should be given to assess joint maximal range of motion? J Bodyw Mov Ther. 2022;31:45–50. doi: 10.1016/j.jbmt.2022.04.010. [DOI] [PubMed] [Google Scholar]
- 42.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 43.Peters MDJ, Godfrey C, McInerney P, Khalil H, Larsen P, Marnie C, et al. Best practice guidance and reporting items for the development of scoping review protocols. JBI Evid Synth. 2022;20(4):953–968. doi: 10.11124/jbies-21-00242. [DOI] [PubMed] [Google Scholar]
- 44.Schuller-Martínez B, Meza N, Pérez-Bracchiglione J, Franco JVA, Loezar C, Madrid E. Graphical representation of the body of the evidence: the essentials for understanding the evidence gap map approach. Medwave. 2021;21(3):e8164. doi: 10.5867/medwave.2021.03.8164. [DOI] [PubMed] [Google Scholar]
- 45.Snilstveit B, Vojtkova M, Bhavsar A, Stevenson J, Gaarder M. Evidence & Gap Maps: a tool for promoting evidence informed policy and strategic research agendas. J Clin Epidemiol. 2016;79:120–129. doi: 10.1016/j.jclinepi.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 46.Miake-Lye IM, Hempel S, Shanman R, Shekelle PG. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst Rev. 2016;5:28. doi: 10.1186/s13643-016-0204-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tayfur A, Haque A, Salles JI, Malliaras P, Screen H, Morrissey D. Are landing patterns in jumping athletes associated with patellar tendinopathy? A systematic review with evidence gap map and meta-analysis. Sports Med. 2022;52(1):123–137. doi: 10.1007/s40279-021-01550-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Budarick AR, Moyer RF. Linking physical activity with clinical, functional, and structural outcomes: an evidence map using the Osteoarthritis Initiative. Clin Rheumatol. 2022;41(4):965–975. doi: 10.1007/s10067-021-05995-y. [DOI] [PubMed] [Google Scholar]
- 49.Alsaleh SA, Murphy NA, Miller SC, Morrissey D, Lack SD. Local neuromuscular characteristics associated with patellofemoral pain: a systematic review and meta-analysis. Clin Biomech. 2021;90:105509. doi: 10.1016/j.clinbiomech.2021.105509. [DOI] [PubMed] [Google Scholar]
- 50.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch V. Cochrane handbook for systematic reviews of interventions. 2. Chichester: Wiley; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McKay AKA, Stellingwerff T, Smith ES, Martin DT, Mujika I, Goosey-Tolfrey VL, et al. Defining training and performance caliber: a participant classification framework. Int J Sports Physiol Perform. 2022;17(2):317–331. doi: 10.1123/ijspp.2021-0451. [DOI] [PubMed] [Google Scholar]
- 53.Abadi FA, Avandi SM, Aminian-Far A. Acute effect of different warm up protocols on static and dynamic balance indices and balance the vault in skilled female gymnast. Koomesh. 2015;17(1):99–110. [Google Scholar]
- 54.Agopyan A, Bozdogan FS, Tekin D, Yetgin MK, Guler CG. Acute effects of static stretching exercises on short-distance flutter kicking time in child swimmers. Int J Perform Anal Sport. 2012;12(3):484–497. doi: 10.1080/24748668.2012.11868613. [DOI] [Google Scholar]
- 55.Ahmadabadi F, Avandi SM, Aminian-Far A. Correlation between sway parameters of center of pressure in static and dynamic balance indices with eyes closed after four weeks static warm up in skilled gymnast athletes. Koomesh. 2017;19(1):102–112. [Google Scholar]
- 56.Akarsu M, Kurhan CO, İlbak İ, Altuntop R, Gönç M, Stojanović S, Purenovic-Ivanović T. Acute effects of self-myofascial release through foam roller and static stretching methods on vertical jump performance of taekwondo players. J Pharm Negat Results. 2022;13:1630–1634. doi: 10.47750/pnr.2022.13.S06.215. [DOI] [Google Scholar]
- 57.Akehurst H, Grice JE, Angioi M, Morrissey D, Migliorini F, Maffulli N. Whole-body vibration decreases delayed onset muscle soreness following eccentric exercise in elite hockey players: a randomised controlled trial. J Orthop Surg Res. 2021;16(1):589. doi: 10.1186/s13018-021-02760-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Alipasali F, Papadopoulou SD, Gissis I, Komsis G, Komsis S, Kyranoudis A, et al. The effect of static and dynamic stretching exercises on sprint ability of recreational male volleyball players. Int J Environ Res Public Health. 2019;16(16):2835. doi: 10.3390/ijerph16162835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Alipasali F, Papadopoulou SD, Kyranoudis AE, Gisis I. The effect of static and dynamic stretching exercises on the jumping ability of recreational male volleyball players. J Phys Educ Sport. 2022;22(4):1026–1032. doi: 10.7752/jpes.2022.04130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Almeida Júnior H, Bastos AA, Martins FJA, De Souza RF, Martins COD, Da Silva AG, et al. Effect of the global active stretching (SGA®) for restoring the normal values of thermal asymmetry. J Phys Educ Sport. 2019;19:1453–1459. doi: 10.7752/jpes.2019.s4211. [DOI] [Google Scholar]
- 61.Alp M. Acute effects of static and dynamic stretching exercises on isokinetic strength of hip flexion-extension in male handball players. Prog Nutr. 2020;22(1):161–166. doi: 10.23751/pn.v22i1.9209. [DOI] [Google Scholar]
- 62.Alp M, Catikkas F, Kurt C. Acute effects of static and dynamic stretching exercises on lower extremity isokinetic strength in taekwondo athletes. Isokinet Exerc Sci. 2018;26(4):307–311. doi: 10.3233/ies-183159. [DOI] [Google Scholar]
- 63.Amir Vazini T, Parnow A. Level of functional capacities following soccer-specific warm-up methods among elite collegiate soccer players. J Sports Med Phys Fit. 2017;57(5):537–542. doi: 10.23736/s0022-4707.16.06236-8. [DOI] [PubMed] [Google Scholar]
- 64.Amiri-Khorasani M. Kinematics analysis: the acute effect of different stretching methods on dynamic range of motion of lower extremity joints during soccer instep kicking. Int J Perform Anal Sport. 2013;13(1):190–199. doi: 10.1080/24748668.2013.11868641. [DOI] [Google Scholar]
- 65.Amiri-Khorasani M. Acute effects of different stretching methods on static and dynamic balance in female football players. Int J Ther Rehabil. 2015;22(2):68–73. doi: 10.12968/ijtr.2015.22.2.68. [DOI] [Google Scholar]
- 66.Amiri-Khorasani M, Ferdinands RED. The acute effect of stretching on the kinematics of instep kicking in soccer. Sports Technol. 2014;7(1–2):69–78. doi: 10.1080/19346182.2014.893348. [DOI] [Google Scholar]
- 67.Amiri-Khorasani M, Kellis E. Static vs. dynamic acute stretching effect on quadriceps muscle activity during soccer instep kicking. J Hum Kinet. 2013;39(1):37–47. doi: 10.2478/hukin-2013-0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Amiri-Khorasani M, Sotoodeh V. The acute effects of combined static and dynamic stretch protocols on fitness performances in soccer players. J Sports Med Phys Fit. 2013;53(5):559–565. [PubMed] [Google Scholar]
- 69.Amiri-Khorasani M, Abu Osman NA, Yusof A. Electromyography assessments of the vastus medialis muscle during soccer instep kicking between dynamic and static stretching. J Hum Kinet. 2010;24:35–41. doi: 10.2478/v10078-010-0017-2. [DOI] [Google Scholar]
- 70.Amiri-Khorasani M, Calleja-Gonzalez J, Mogharabi-Manzari M. Acute effect of different combined stretching methods on acceleration and speed in soccer players. J Hum Kinet. 2016;50(1):179–186. doi: 10.1515/hukin-2015-0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Amiri-Khorasani M, Abu Osman NA, Yusof A. Acute effect of static and dynamic stretching on hip dynamic range of motion during instep kicking in professional soccer players. J Strength Cond Res. 2011;25(6):1647–1652. doi: 10.1519/JSC.0b013e3181db9f41. [DOI] [PubMed] [Google Scholar]
- 72.Amiri-Khorasani M, Mohammadkazemi R, Sarafrazi S, Riyahi-Malayeri S, Sotoodeh V. Kinematics analyses related to stretch-shortening cycle during soccer instep kicking after different acute stretching. J Strength Cond Res. 2012;26(11):3010–3017. doi: 10.1519/JSC.0b013e3182443442. [DOI] [PubMed] [Google Scholar]
- 73.Amiri-Khorasani M, Sahebozamani M, Tabrizi KG, Yusof AB. Acute effect of different stretching methods on Illinois Agility Test in soccer players. J Strength Cond Res. 2010;24(10):2698–2704. doi: 10.1519/JSC.0b013e3181bf049c. [DOI] [PubMed] [Google Scholar]
- 74.Andre MJ, Fry AC, McLellan E, Weiss LW, Moore CM. Acute effects of static stretching on bench press power and velocity in adolescent male athletes. Int J Sports Sci Coach. 2014;9(5):1145–1152. doi: 10.1260/1747-9541.9.5.1145. [DOI] [Google Scholar]
- 75.Andrejić O, Tošić S, Knežević O. Acute effects of low- and high-volume stretching on fitness performance in young basketball players. Serb J Sports Sci. 2012;1:11–16. [Google Scholar]
- 76.Annino G, Ruscello B, Lebone P, Palapalazzo F, Lombardo M, Paduapadua E, et al. Acute effects of static and dynamic stretching on jump performance after 15 min of reconditioning shooting phase in basketball players. J Sports Med Phys Fit. 2017;57(4):330–337. doi: 10.23736/s0022-4707.16.06143-0. [DOI] [PubMed] [Google Scholar]
- 77.Ari Y. Effects of different stretching methods on speed, jump, flexibility and upper extremity performance in wrestlers. Kinesiol Slov. 2021;27(1):162–176. doi: 10.52165/kinsi.27.1.162-176. [DOI] [Google Scholar]
- 78.Arihiro H, Miku O, Katsuaki S, Norikazu YAO, Kanae I, Hideyuki K. Pilates exercise improves hip joint flexion mobility in rugby players. Adv Exerc Sports Physiol. 2018;24(3):45–49. [Google Scholar]
- 79.Avaz MA, Saghebjoo M, Zardast M, Ilbeigi S. Acute effects of proprioception, massage and dynamic stretching warm up protocols on serum CK and LDH activity levels after one session of plyometric training in male volleyball players. Koomesh. 2016;17(2):393–402. [Google Scholar]
- 80.Avedesian JM, Judge LW, Wang H, Dickin DC. The biomechanical effect of warm-up stretching strategies on landing mechanics in female volleyball athletes. Sports Biomech. 2020;19(5):587–600. doi: 10.1080/14763141.2018.1503322. [DOI] [PubMed] [Google Scholar]
- 81.Avloniti A, Chatzinikolaou A, Fatouros IG, Avloniti C, Protopapa M, Draganidis D, et al. The acute effects of static stretching on speed and agility performance depend on stretch duration and conditioning level. J Strength Cond Res. 2016;30(10):2767–2773. doi: 10.1519/jsc.0000000000000568. [DOI] [PubMed] [Google Scholar]
- 82.Avloniti A, Chatzinikolaou A, Fatouros IG, Protopapa M, Athanailidis I, Avloniti C, et al. The effects of static stretching on speed and agility: one or multiple repetition protocols? Eur J Sport Sci. 2016;16(4):402–408. doi: 10.1080/17461391.2015.1028467. [DOI] [PubMed] [Google Scholar]
- 83.Ayala F, De Baranda PS. Acute effect of stretching on sprint in honour division soccer players. RICYDE. 2010;6(18):1–12. doi: 10.11138/mltj/2018.8.1.037. [DOI] [Google Scholar]
- 84.De Baranda PS, Ayala F. Efecto agudo del estiramiento sobre la agilidad y coordinación de movimientos rápidos en jugadores de fútbol de División de Honor [The Acute effect of stretching on the agility and coordination in fast movements of first division football players] Kronos. 2010;9(17):21–28. [Google Scholar]
- 85.Ayala F, De Baranda PS, De Ste CM. Effect of active stretch on hip flexion range of motion in female professional futsal players. J Sports Med Phys Fit. 2010;50(4):428–435. [PubMed] [Google Scholar]
- 86.Aydoǧ ST, Hazir M, Hasçelik Z, Çaǧlar A, Özdoǧan M. The effect of stretching exercise on maximum peak torque. J Rheumatol Med Rehabil. 2000;11(4):278–281. [Google Scholar]
- 87.Azuma N, Someya F. Injury prevention effects of stretching exercise intervention by physical therapists in male high school soccer players. Scand J Med Sci Sports. 2020;30(11):2178–2192. doi: 10.1111/sms.13777. [DOI] [PubMed] [Google Scholar]
- 88.Babbar S, Zutshi K, Munjal J. Acute effect of a dynamic and static stretching exercise bout during warm up on power in soccer players. Indian J Physiother Occup Ther. 2011;5(2):141–143. [Google Scholar]
- 89.Balci A, Unuvar E, Akinoglu B, Kocahan T. The effect of different neural mobilization exercises on hamstring flexibility and functional flexibility in wrestlers. J Exerc Rehabil. 2020;16(6):503–509. doi: 10.12965/jer.2040700.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bali S, Guru K. Comparative effect of static stretching and mulligan stretching on hip adductor flexibility in footballers: a two group trial. JK Sci. 2020;22(2):96–100. [Google Scholar]
- 91.Barbosa GM, Dantas GAF, Pinheiro SM, Rego JTP, Oliveira TLC, Silva KKF, et al. Acute effects of stretching and/or warm-up on neuromuscular performance of volleyball athletes: a randomized cross-over clinical trial. Sport Sci Health. 2020;16(1):85–92. doi: 10.1007/s11332-019-00576-8. [DOI] [Google Scholar]
- 92.Baumgart C, Gokeler A, Donath L, Hoppe MW, Freiwald J. Effects of static stretching and playing soccer on knee laxity. Clin J Sport Med. 2015;25(6):541–545. doi: 10.1097/jsm.0000000000000174. [DOI] [PubMed] [Google Scholar]
- 93.Bazett-Jones DM, Gibson MH, McBride JM. Sprint and vertical jump performances are not affected by six weeks of static hamstring stretching. J Strength Cond Res. 2008;22(1):25–31. doi: 10.1519/JSC.0b013e31815f99a4. [DOI] [PubMed] [Google Scholar]
- 94.Bazett-Jones DM, Winchester JB, McBride JM. Effect of potentiation and stretching on maximal force, rate of force development, and range of motion. J Strength Cond Res. 2005;19(2):421–426. doi: 10.1519/14193.1. [DOI] [PubMed] [Google Scholar]
- 95.Beckett JRJ, Schneiker KT, Wallman KE, Dawson BT, Guelfi KJ. Effects of static stretching on repeated sprint and change of direction performance. Med Sci Sports Exerc. 2009;41(2):444–450. doi: 10.1249/MSS.0b013e3181867b95. [DOI] [PubMed] [Google Scholar]
- 96.Behara B, Jacobson BH. Acute effects of deep tissue foam rolling and dynamic stretching on muscular strength, power, and flexibility in division i linemen. J Strength Cond Res. 2017;31(4):888–892. doi: 10.1519/jsc.0000000000001051. [DOI] [PubMed] [Google Scholar]
- 97.Belkhiria-Turki L, Chaouachi A, Turki O, Chtourou H, Chtara M, Chamari K, et al. Eight weeks of dynamic stretching during warm-ups improves jump power but not repeated or single sprint performance. Eur J Sport Sci. 2014;14(1):19–27. doi: 10.1080/17461391.2012.726651. [DOI] [PubMed] [Google Scholar]
- 98.Belkhiria-Turki L, Chaouachi A, Turki O, Hammami R, Chtara M, Amri M, et al. Greater volumes of static and dynamic stretching within a warm-up do not impair star excursion balance performance. J Sports Med Phys Fit. 2014;54(3):279–288. [PubMed] [Google Scholar]
- 99.Bello M, Mesiano Maifrino LB, Gama EF, de Souza RR. Rhythmic stabilization versus conventional passive stretching to prevent injuries in indoor soccer athletes: a controlled clinical trial. J Bodyw Mov Ther. 2011;15(3):380–383. doi: 10.1016/j.jbmt.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 100.Ben Maaouia G, Nassib S, Negra Y, Chammari K, Souissi N. Agility performance variation from morning to evening: dynamic stretching warm-up impacts performance and its diurnal amplitude. Biol Rhythm Res. 2020;51(4):509–521. doi: 10.1080/09291016.2018.1537553. [DOI] [Google Scholar]
- 101.Bingul BM, Son M, Aydin M, Gelen E, Cinel Y, Bulgan C. The effects of static and dynamic stretching on agility performance. J Phys Educ Sports Sci. 2014;8(1):43–48. [Google Scholar]
- 102.Bishop D, Middleton G. Effects of static stretching following a dynamic warm-up on speed, agility and power. J Hum Sport Exerc. 2013;8(2 Suppl):391–400. doi: 10.4100/jhse.2012.82.07. [DOI] [Google Scholar]
- 103.Bogdanis GC, Donti O, Tsolakis C, Smilios I, Bishop DJ. Intermittent but not continuous static stretching improves subsequent vertical jump performance in flexibility-trained athletes. J Strength Cond Res. 2019;33(1):203–210. doi: 10.1519/jsc.0000000000001870. [DOI] [PubMed] [Google Scholar]
- 104.Boudenot A, Jaffre C, Portier H. Comparaison de quatre méthodes d'échauffement sur la performance lors du Wingate test [Comparing four warm-up procedures on Wingate test performance] Kinesitherapie. 2014;14(146):34–38. doi: 10.1016/j.kine.2013.10.017. [DOI] [Google Scholar]
- 105.Bouthin B, Edouard P. Les étirements sont-ils un facteur préventif des lésions de l’appareil locomoteur ? Étude pilote prospective dans une population de footballeurs amateurs [Is stretching a good strategy to prevent musculo-skeletal injuries? A prospective pilot study on football amateur players] J Traumatol du Sport. 2015;32(1):22–28. doi: 10.1016/j.jts.2015.01.001. [DOI] [Google Scholar]
- 106.Brodowicz GR, Welsh R, Wallis J. Comparison of stretching with ice, stretching with heat, or stretching alone on hamstring flexibility. J Athl Train. 1996;31(4):324–327. [PMC free article] [PubMed] [Google Scholar]
- 107.Burkett LN, Phillips WT, Ziuraitis J. The best warm-up for the vertical jump in college-age athletic men. J Strength Cond Res. 2005;19(3):673–676. doi: 10.1519/15204.1. [DOI] [PubMed] [Google Scholar]
- 108.Burkett LN, Ziuraitis J, Phillips WT. The effect of four different warm-ups on the maximum vertical jump test scores for female college athletes. Women Sport Phys Act J. 2001;10(2):83–93. doi: 10.1123/wspaj.10.2.83. [DOI] [Google Scholar]
- 109.Buttifant D, Hrysomallis C. Effect of various practical warm-up protocols on acute lower-body power. J Strength Cond Res. 2015;29(3):656–660. doi: 10.1519/jsc.0000000000000690. [DOI] [PubMed] [Google Scholar]
- 110.Caliskan E, Akkoc O, Bayramoglu Z, Gozubuyuk OB, Kural D, Azamat S, Adaletli I. Effects of static stretching duration on muscle stiffness and blood flow in the rectus femoris in adolescents. Med Ultrason. 2019;21(2):136–143. doi: 10.11152/mu-1859. [DOI] [PubMed] [Google Scholar]
- 111.Caplan N, Rogers R, Parr MK, Hayes PR. The effect of proprioceptive neuromuscular facilitation and static stretch training on running mechanics. J Strength Cond Res. 2009;23(4):1175–1180. doi: 10.1519/JSC.0b013e318199d6f6. [DOI] [PubMed] [Google Scholar]
- 112.Carvalho FLP, Carvalho MC, Simão R, Gomes TM, Costa PB, Neto LB, et al. Acute effects of a warm-up including active, passive, and dynamic stretching on vertical jump performance. J Strength Cond Res. 2012;26(9):2447–2452. doi: 10.1519/JSC.0b013e31823f2b36. [DOI] [PubMed] [Google Scholar]
- 113.Carvalho FLP, Rayol Prati JEL, Alencar Carvalho MCG, Dantas EHM. Efectos agudos del estiramiento estático y de la facilitación neuromuscular proprioceptiva en el desempeño del salto vertical de tenistas adolescentes [Acute effects of static stretching and proprioceptive neuromuscular facilitation on the performance of vertical jump in adolescent tennis players] Fit Perform J Online. 2009;8(4):264–268. doi: 10.3900/fpj.8.4.264.e. [DOI] [Google Scholar]
- 114.Celik A. Acute effects of cyclic versus static stretching on shoulder flexibility, strength, and spike speed in volleyball players. Turk J Phys Med Rehabil. 2017;63(2):124–132. doi: 10.5606/tftrd.2017.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.César EP, Junior CSR, Francisco RN. Effects of 2 intersection strategies for physical recovery in jiu-jitsu athletes. Int J Sports Physiol Perform. 2021;16(4):585–590. doi: 10.1123/ijspp.2019-0701. [DOI] [PubMed] [Google Scholar]
- 116.Cetin O, Isik O, Yasar MN. The acute effects of a dynamic warm-up including hip mobility exercises on sprint, agility and vertical jump performance. Eur J Hum Mov. 2020 doi: 10.21134/eurjhm.2020.45.6. [DOI] [Google Scholar]
- 117.Chaouachi A, Castagna C, Chtara M, Brughelli M, Turki O, Galy O, et al. Effect of warm-ups involving static or dynamic stretching on agility, sprinting, and jumping performance in trained individuals. J Strength Cond Res. 2010;24(8):2001–2011. doi: 10.1519/JSC.0b013e3181aeb181. [DOI] [PubMed] [Google Scholar]
- 118.Chaouachi A, Padulo J, Kasmi S, Ben Othmen A, Chatra M, Behm DG. Unilateral static and dynamic hamstrings stretching increases contralateral hip flexion range of motion. Clin Physiol Funct Imaging. 2017;37(1):23–29. doi: 10.1111/cpf.12263. [DOI] [PubMed] [Google Scholar]
- 119.Chatzopoulos D, Doganis G, Lykesas G, Koutlianos N, Galazoulas C, Bassa E. Effects of static and dynamic stretching on force sense, dynamic flexibility and reaction time of children. Open Sports Sci J. 2019;12(1):22–27. doi: 10.2174/1875399X01912010022. [DOI] [Google Scholar]
- 120.Chatzopoulos D, Galazoulas C, Patikas D, Kotzamanidis C. Acute effects of static and dynamic stretching on balance, agility, reaction time and movement time. J Sports Sci Med. 2014;13(2):403–409. [PMC free article] [PubMed] [Google Scholar]
- 121.Chatzopoulos D, Kapodistria L, Doganis G, Messaritakis V, Lykesas G. Effects of varying volumes of dynamic stretching on active range of motion, reaction time, and movement time in female soccer players. J Exerc Physiol Online. 2019;22(5):147–156. [Google Scholar]
- 122.Chen CH, Ye X, Wang YT, Chen YS, Tseng WC. Differential effects of different warm-up protocols on repeated sprints-induced muscle damage. J Strength Cond Res. 2019;32(11):3276–3284. doi: 10.1519/JSC.0000000000002310. [DOI] [PubMed] [Google Scholar]
- 123.Chen YL, Tsai FM, Hsu WC, Yang CJ, Yei TY. Exploring shank circumference by stretching after training among volleyball players. Int J Environ Res Public Health. 2021;18(16):8849. doi: 10.3390/ijerph18168849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chinnavan E, Gopaladhas S, Kaikondan P. Effectiveness of pilates training in improving hamstring flexibility of football players. Bangladesh J Med Sci. 2015;14(3):265–269. doi: 10.3329/bjms.v14i3.16322. [DOI] [Google Scholar]
- 125.Christensen B, Nordstrom BJ. The effects of proprioceptive neuromuscular facilitation and dynamic stretching techniques on vertical jump performance. J Strength Cond Res. 2008;22(6):1826–1831. doi: 10.1519/JSC.0b013e31817ae316. [DOI] [PubMed] [Google Scholar]
- 126.Christensen B, Bond CW, Napoli R, Lopez K, Miller J, Hackney KJ. The effect of static stretching, mini-band warm-ups, medicine-ball warm-ups, and a light jogging warm-up on common athletic ability tests. Int J Exerc Sci. 2020;13(4):298–311. doi: 10.70252/OVNN5227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Chtourou H, Aloui A, Hammouda O, Chaouachi A, Chamari K, Souissi N. Effect of static and dynamic stretching on the diurnal variations of jump performance in soccer players. PLoS ONE. 2013;8(8):e70534. doi: 10.1371/journal.pone.0070534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Church JB, Wiggins MS, Moode FM, Crist R. Effect of warm-up and flexibility treatments on vertical jump performance. J Strength Cond Res. 2001;15(3):332–336. [PubMed] [Google Scholar]
- 129.Colak S. Effects of dynamic stretches on isokinetic hamstring and quadriceps femoris muscle strength in elite female soccer players. S Afr J Res Sport Phys Ed Recreat. 2012;34(2):15–25. [Google Scholar]
- 130.Coons JM, Gould CE, Kim JK, Farley RS, Caputo JL. Dynamic stretching is effective as static stretching at increasing flexibility. J Hum Sport Exerc. 2017;12(4):1153–1161. doi: 10.14198/jhse.2017.124.02. [DOI] [Google Scholar]
- 131.Correia JDB, Martins GA, da Silva LG, Silveira EM, Steffens T, Pietta-Dias C, Cadore EL. Comparação dos efeitos agudos dos métodos FNP e estabilização (FIFA 11+) no equilíbrio dinâmico de atletas de futebol universitário [Comparison of the acute effects of the PNF and stabilization methods (FIFA 11+) on the dynamic balance of university football athletes] Rev Bras Futsal Futeb. 2021;13(53):234–243. [Google Scholar]
- 132.Cwirlej-Sozanska AB, Wójcik O, Wójcik J, Mól M, Kolasa T. The influence of static stretching of specific lower limb muscle groups on the jump height parameter of volleyball players aged 16–17: a pilot study. Adv Rehabil. 2021 doi: 10.5114/AREH.2021.102315. [DOI] [Google Scholar]
- 133.da Silva FF, de Souza RA, do Couto CLB, Magalhães RF, Kawatake JP. Efeitos agudos do alongamento estático no rendimento de testes funcionais em atletas de voleibol e futebol [Acute effects of static stretching on functional performance tests on volleyball and soccer athletes]. Rev Terapia Manual. 2011;9(42):138–42.
- 134.Dalamitros AA, Vagios A, Toubekis AG, Tsalis G, Clemente-Suarez VJ, Manou V. The effect of two additional dry-land active warm-up protocols on the 50-m front-crawl swimming performance. Hum Mov. 2018;19(3):75–81. doi: 10.5114/hm.2018.76082. [DOI] [Google Scholar]
- 135.Dallas G, Smirniotou A, Tsiganos G, Tsopani D, Di Cagno A, Tsolakis CH. Acute effect of different stretching methods on flexibility and jumping performance in competitive artistic gymnasts. J Sports Med Phys Fit. 2014;54(6):683–690. [PubMed] [Google Scholar]
- 136.Dalrymple KJ, Davis SE, Dwyer GB, Moir GL. Effect of static and dynamic stretching on vertical jump performance in collegiate women volleyball players. J Strength Cond Res. 2010;24(1):149–155. doi: 10.1519/JSC.0b013e3181b29614. [DOI] [PubMed] [Google Scholar]
- 137.Damasceno MV, Duarte M, Pasqua LA, Lima-Silva AE, MacIntosh BR, Bertuzzi R. Static stretching alters neuromuscular function and pacing strategy, but not performance during a 3-km running time-trial. PLoS ONE. 2014;9(6):e99238. doi: 10.1371/journal.pone.0099238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Darcadia CAF, Silva MJ, de Souza RA, de Carvalho WRG, da Silva FF. Efeitos agudos do alongamento estático no rendimento de testes funcionais em atletas de futebol [Acute effects of static stretching on functional performance tests on soccer athletes] Rev Terapia Manual. 2011;9(45):503–507. [Google Scholar]
- 139.Dawson B, Gow S, Modra S, Bishop D, Stewart C. Effects of immediate post-game recovery procedures on muscle soreness, power and flexibility levels over the next 48 hours. J Sci Med Sport. 2005;8(2):210–221. doi: 10.1016/S1440-2440(05)80012-X. [DOI] [PubMed] [Google Scholar]
- 140.de Almeida Leme JAC, Barberi RA, Curiacos KJ, Rogatto PV. Stretch influence on pre-competitive stress on juvenile soccer players. Motricidade. 2008;4(3):57–60. doi: 10.6063/motricidade.271. [DOI] [Google Scholar]
- 141.de Castro JV, Machado KC, Scaramussa K, Gomes JLE. Incidence of decreased hip range of motion in youth soccer players and response to a stretching program: a randomized clinical trial. J Sport Rehabil. 2013;22(2):100–107. doi: 10.1123/jsr.22.2.100. [DOI] [PubMed] [Google Scholar]
- 142.De Oliveira Júnior JD, De Lima Pinto JCB, De Caldas HR, De Barros ACM, Da Silva Santos TR, Mortatti AL. The acute effect of proprioceptive neuromuscular facilitation in explosive force and jump resistance of basketball players. J Phys Educ Sport. 2018;18(2):632–636. doi: 10.7752/jpes.2018.02092. [DOI] [Google Scholar]
- 143.de Oliveira FCL, Pinto Lopes Rama LM. Alongamento estático ativo no desempenho em provas de potência e velocidade. Braz J Biomot. 2013;7(2):128–38.
- 144.de Rezende FN, da Mota GR, Lopes CR, da Silva BVC, Simim MAM, Marocolo M. Specific warm-up exercise is the best for vertical countermovement jump in young volleyball players. Motriz. 2016;22(4):299–303. doi: 10.1590/S1980-6574201600040013. [DOI] [Google Scholar]
- 145.Di Cagno A, Baldari C, Battaglia C, Gallotta MC, Videira M, Piazza M, Guidetti L. Preexercise static stretching effect on leaping performance in elite rhythmic gymnasts. J Strength Cond Res. 2010;24(8):1995–2000. doi: 10.1519/JSC.0b013e3181e34811. [DOI] [PubMed] [Google Scholar]
- 146.Di Cagno A, Calcagno G, Buonsenso A, Iuliano E, Innocenti G, Piazza M, Fiorilli G. Effects of static and dynamic stretching on upper limb explosive, isometric and endurance strength, in male volleyball players. Ital J Anat Embryol. 2019;124(1):113–121. doi: 10.13128/IJAE-25475. [DOI] [Google Scholar]
- 147.Donti O, Gaspari V, Papia K, Panidi I, Donti A, Bogdanis GC. Acute effects of intermittent and continuous static stretching on hip flexion angle in athletes with varying flexibility training background. Sports (Basel). 2020;8(3):28. doi: 10.3390/sports8030028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Donti O, Panidis I, Terzis G, Bogdanis GC. Gastrocnemius medialis architectural properties at rest and during stretching in female athletes with different flexibility training background. Sports (Basel). 2019;7(2):39. doi: 10.3390/sports7020039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Donti O, Papia K, Toubekis A, Donti A, Sands WA, Bogdanis GC. Flexibility training in preadolescent female athletes: acute and long-term effects of intermittent and continuous static stretching. J Sports Sci. 2018;36(13):1453–1460. doi: 10.1080/02640414.2017.1397309. [DOI] [PubMed] [Google Scholar]
- 150.Drews S, Goltz C. Lässt sich durch Querdehnung ein größerer Gewinn an Beweglichkeit erzielen als durch Längsdehnung? Randomisierte kontrollierte Studie am Beispiel der Hüftgelenkadduktoren von Fußballspielern und deren Beweglichkeit in die Abduktion [Can transversal stretching yield higher mobility than longitudinal stretching?] Manuelle Ther. 2005;9(2):59–64. doi: 10.1055/s-2005-858183. [DOI] [Google Scholar]
- 151.Ebadi LA, Cetin E. Duration dependent effect of static stretching on quadriceps and hamstring muscle force. Sports (Basel). 2018;6(1):24. doi: 10.3390/sports6010024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Egan AD, Cramer JT, Massey LL, Marek SM. Acute effects of static stretching on peak torque and mean power output in National Collegiate Athletic Association division I women's basketball players. J Strength Cond Res. 2006;20(4):778–782. doi: 10.1519/R-18575.1. [DOI] [PubMed] [Google Scholar]
- 153.Eken Ö, Bayer R. Acute effects of proprioceptive neuromuscular facilitation stretching, massage and combine protocols on flexibility, vertical jump and hand grip strength performance in kickboxers. Pedagogy Phys Cult Sports. 2022;26(1):4–12. doi: 10.15561/26649837.2022.0101. [DOI] [Google Scholar]
- 154.Espi-Lopez GV, Lopez-Martinez S, Ingles M, Serra-Ano P, Aguilar-Rodriguez M. Effect of manual therapy versus proprioceptive neuromuscular facilitation in dynamic balance, mobility and flexibility in field hockey players. A randomized controlled trial. Phys Ther Sport. 2018;32:173–179. doi: 10.1016/j.ptsp.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 155.Evetovich TK, Cain RM, Hinnerichs KR, Engebretsen BJ, Conley DS. Interpreting normalized and nonnormalized data after acute static stretching in athletes and nonathletes. J Strength Cond Res. 2010;24(8):1988–1994. doi: 10.1519/JSC.0b013e3181e3132a. [DOI] [PubMed] [Google Scholar]
- 156.Faigenbaum AD, Kang J, McFarland J, Bloom JM, Magnatta J, Ratamess NA, Hoffman JR. Acute effects of different warm-up protocols on anaerobic performance in teenage athletes. Pediatr Exerc Sci. 2006;18(1):64–75. doi: 10.1123/pes.18.1.64. [DOI] [Google Scholar]
- 157.Faigenbaum AD, McFarland JE, Kelly NA, Ratamess NA, Kang J, Hoffman JR. Influence of recovery time on warm-up effects in male adolescent athletes. Pediatr Exerc Sci. 2010;22(2):266–277. doi: 10.1123/pes.22.2.266. [DOI] [PubMed] [Google Scholar]
- 158.Faigenbaum AD, McFarland JE, Schwerdtman JA, Ratamess NA, Kang J, Hoffman JR. Dynamic warm-up protocols, with and without a weighted vest, and fitness performance in high school female athletes. J Athl Train. 2006;41(4):357–363. [PMC free article] [PubMed] [Google Scholar]
- 159.Famisis K. Acute effect of static and dynamic stretching exercise on sprint and flexibility of amateur soccer players. Phys Train. 2015:1–12.
- 160.Farshidi B, Daneshjoo A, Sahebozamani M, Konrad A. Effects of static and PNF stretching on joint position sense and range of motion after a fatigue protocol in professional male soccer players. Med Sport (Roma). 2022;75(2):206–17. 10.23736/S0025-7826.22.04148-5.
- 161.Fattahi-Bafghi A, Amiri-Khorasani M. Sustaining effect of different stretching methods on power and agility after warm-up exercise in soccer players. World Appl Sci J. 2013;21(4):520–525. doi: 10.5829/idosi.wasj.2013.21.4.2242. [DOI] [Google Scholar]
- 162.Favero JP, Midgley AW, Bentley DJ. Effects of an acute bout of static stretching on 40 m sprint performance: influence of baseline flexibility. Res Sports Med. 2009;17(1):50–60. doi: 10.1080/15438620802678529. [DOI] [PubMed] [Google Scholar]
- 163.Feitosa Junior JVA, Solon Junior LJF, da Silva Neto LV. Alongamento estático não reduz a força de preensão manual isométrica máxima em lutadores Brasileiros de Jiu-Jitsu [Static stretching does not reduce the maximum isometric handgrip strength in Brazilian Jiu-Jitsu fighters] Rev Bras Prescrição Fisiol Exerc. 2019;13(86):1021–1025. [Google Scholar]
- 164.Fernandes IA, Kawchuk G, Bhambhani Y, Gomes PSC. Does vibration counteract the static stretch-induced deficit on muscle force development? J Sci Med Sport. 2013;16(5):472–476. doi: 10.1016/j.jsams.2012.11.886. [DOI] [PubMed] [Google Scholar]
- 165.Ferreira VD, Muller BC, Achour A. Efeito agudo de exercícios de alongamento estático e dinâmico na impulsão vertical de jogadores de futebol [Acute effects of static versus dynamic stretching on the vertical jump performance of soccer players] Motriz. 2013;19(2):450–459. doi: 10.1590/S1980-65742013000200022. [DOI] [Google Scholar]
- 166.Ferri-Caruana A, Roig-Ballester N, Romagnoli M. Effect of dynamic range of motion and static stretching techniques on flexibility, strength and jump performance in female gymnasts. Sci Gymnast J. 2020;12(1):87–100. doi: 10.52165/sgj.12.1.87-100. [DOI] [Google Scholar]
- 167.Fletcher IM, Anness R. The acute effects of combined static and dynamic stretch protocols on fifty-meter sprint performance in track-and-field athletes. J Strength Cond Res. 2007;21(3):784–787. doi: 10.1519/R-19475.1. [DOI] [PubMed] [Google Scholar]
- 168.Fletcher IM, Jones B. The effect of different warm-up stretch protocols on 20 meter sprint performance in trained rugby union players. J Strength Cond Res. 2004;18(4):885–888. doi: 10.1519/14493.1. [DOI] [PubMed] [Google Scholar]
- 169.Fletcher IM, Monte-Colombo MM. An investigation into the effects of different warm-up modalities on specific motor skills related to soccer performance. J Strength Cond Res. 2010;24(8):2096–2101. doi: 10.1519/JSC.0b013e3181e312db. [DOI] [PubMed] [Google Scholar]
- 170.Fletcher IM, Monte-Colombo MM. An investigation into the possible physiological mechanisms associated with changes in performance related to acute responses to different preactivity stretch modalities. Appl Physiol Nutr Metab. 2010;35(1):27–34. doi: 10.1139/h09-125. [DOI] [PubMed] [Google Scholar]
- 171.Forte D, Ferrara F, Altavilla G. Relationship between types of stretching and jumping in volleyball. J Phys Educ Sport. 2019;19:1859–1862. doi: 10.7752/jpes.2019.s5275. [DOI] [Google Scholar]
- 172.Frantz TL, Ruiz MD. Effects of dynamic warm-up on lower body explosiveness among collegiate baseball players. J Strength Cond Res. 2011;25(11):2985–2990. doi: 10.1519/JSC.0b013e31820f509b. [DOI] [PubMed] [Google Scholar]
- 173.Fredericson M, White JJ, MacMahon JM, Andriacchi TP. Quantitative analysis of the relative effectiveness of 3 iliotibial band stretches. Arch Phys Med Rehabil. 2002;83(5):589–592. doi: 10.1053/apmr.2002.31606. [DOI] [PubMed] [Google Scholar]
- 174.Frikha M, Derbel MS, Chaari N, Gharbi A, Chamari K. Acute effect of stretching modalities on global coordination and kicking accuracy in 12–13 year-old soccer players. Hum Mov Sci. 2017;54:63–72. doi: 10.1016/j.humov.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 175.Funk DC, Swank AM, Mikla BM, Fagan TA, Farr BK. Impact of prior exercise on hamstring flexibility: a comparison of proprioceptive neuromuscular facilitation and static stretching. J Strength Cond Res. 2003;17(3):489–492. doi: 10.1519/1533-4287(2003)017<0489:iopeoh>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 176.Funk DC, Swank AM, Adams KJ, Treolo D. Efficacy of moist heat pack application over static stretching on hamstring flexibility. J Strength Cond Res. 2001;15(1):123–126. [PubMed] [Google Scholar]
- 177.Gabbe BJ, Branson R, Bennell KL. A pilot randomised controlled trial of eccentric exercise to prevent hamstring injuries in community-level Australian Football. J Sci Med Sport. 2006;9(1–2):103–109. doi: 10.1016/j.jsams.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 178.Galazoulas C. Effects of static stretching duration on isokinetic peak torque in basketball players in semi-professional male basketball players. J Phys Educ Sport. 2016;16:1058–1063. doi: 10.7752/jpes.2016.s2168. [DOI] [Google Scholar]
- 179.Galazoulas C. Acute effects of static and dynamic stretching on the sprint and countermovement jump of basketball players. J Phys Educ Sport. 2017;17(1):219–223. doi: 10.7752/jpes.2017.01033. [DOI] [Google Scholar]
- 180.Galetin N, Cvetković M, Ujsasi D, Čokorilo N, Andrašić S, Lazarević M. Effects of static stretching of various durations on the vertical jump among female volleyball players. FU Phys Educ Sport. 2017;15(1):207–217. doi: 10.22190/FUPES1701207G. [DOI] [Google Scholar]
- 181.Gao ZX, Song Y, Yu PM, Zhang Y, Li SD. Acute effects of different stretching techniques on lower limb kinematics, kinetics and muscle activities during vertical jump. J Biomim Biomater Biomed Eng. 2019;40:1–15. doi: 10.4028/www.scientific.net/JBBBE.40.1. [DOI] [Google Scholar]
- 182.Gelen E. Acute effects of different warm-up methods on sprint, slalom dribbling, and penalty kick performance in soccer players. J Strength Cond Res. 2010;24(4):950–956. doi: 10.1519/JSC.0b013e3181cb703f. [DOI] [PubMed] [Google Scholar]
- 183.Gelen E, Bakici D, Yasar MN, Turgut A. Does static stretching compromise jump performance in diurnal variation? Eur J Hum Mov. 2021;47:23–31. doi: 10.21134/eurjhm.2021.47.3. [DOI] [Google Scholar]
- 184.Gelen E, Dede M, Bingul BM, Bulgan C, Aydin M. Acute effects of static stretching, dynamic exercises, and high volume upper extremity plyometric activity on tennis serve performance. J Sports Sci Med. 2012;11(4):600–605. [PMC free article] [PubMed] [Google Scholar]
- 185.Gergley JC. Acute effects of passive static stretching during warm-up on driver clubhead speed, distance, accuracy, and consistent ball contact in young male competitive golfers. J Strength Cond Res. 2009;23(3):863–867. doi: 10.1519/JSC.0b013e3181a00c67. [DOI] [PubMed] [Google Scholar]
- 186.Gergley JC. Latent effect of passive static stretching on driver clubhead speed, distance, accuracy, and consistent ball contact in young male competitive golfers. J Strength Cond Res. 2010;24(12):3326–3333. doi: 10.1519/JSC.0b013e3181e725e4. [DOI] [PubMed] [Google Scholar]
- 187.Ghasemi M, Bagheri H, Olyaei G, Talebian S, Shadmehr A, Jalaei S, Kalantari KK. Effects of cyclic static stretch on fatigue recovery of triceps surae in female basketball players. Biol Sport. 2013;30(2):97–102. doi: 10.5604/20831862.1044224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Gonçalves DL, Pavão TS, Dohnert MB. Efeitos agudos e crônicos de um programa de alongamento estático e dinâmico no rendimento em jovens atletas do futebol [Acute and chronic effects of a static and dynamic stretching program in the performance of young soccer athletes] Rev Bras Med Esporte. 2013;19(4):241–246. doi: 10.1590/s1517-86922013000400003. [DOI] [Google Scholar]
- 189.Gürses VV, Akgül MŞ. Futbolcularin isinmada uyguladiklari farkli germe yöntemlerinin dikey siçrama, sürat ve çeviklik performansina akut etkisi [Acute effects of different stretching methods during warm-up on vertical jump, speed and agility of soccer players performance] J Phys Educ Sports Sci. 2019;17(1):178–186. doi: 10.33689/spormetre.520033. [DOI] [Google Scholar]
- 190.Haag SJ, Wright GA, Gillette CM, Greany JF. Effects of acute static stretching of the throwing shoulder on pitching performance of National Collegiate Athletic Association division III baseball players. J Strength Cond Res. 2010;24(2):452–457. doi: 10.1519/JSC.0b013e3181c06d9c. [DOI] [PubMed] [Google Scholar]
- 191.Haddad M, Dridi A, Chtara M, Chaouachi A, Wong DP, Behm D, Chamari K. Static stretching can impair explosive performance for at least 24 hours. J Strength Cond Res. 2014;28(1):140–146. doi: 10.1519/JSC.0b013e3182964836. [DOI] [PubMed] [Google Scholar]
- 192.Haddad M, Prince MS, Zarrouk N, Tabben M, Behm DG, Chamari K. Dynamic stretching alone can impair slower velocity isokinetic performance of young male handball players for at least 24 hours. PLoS ONE. 2019;14(1):e0210318. doi: 10.1371/journal.pone.0210318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Han G, Lee M, Cho B. Effects of dynamic stretch training on lower extremity power performance of young sprinters. J Phys Ther Sci. 2011;23(3):401–404. doi: 10.1589/jpts.23.401. [DOI] [Google Scholar]
- 194.Heisey CF, Kingsley JD. Effects of static stretching on squat performance in division I female athletes. Int J Exerc Sci. 2016;9(3):359–367. doi: 10.70252/FISD4148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Herman SL, Smith DT. Four-week dynamic stretching warm-up intervention elicits longer-term performance benefits. J Strength Cond Res. 2008;22(4):1286–1297. doi: 10.1519/JSC.0b013e318173da50. [DOI] [PubMed] [Google Scholar]
- 196.Higuchi T, Nakao Y, Tanaka Y, Sadakiyo M, Hamada K, Yokoyama S. Acute effects of doorway stretch on the glenohumeral rotational range of motion and scapular position in high-school baseball players. JSES Int. 2021;5(6):972–977. doi: 10.1016/j.jseint.2021.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Holt BW, Lambourne K. The impact of different warm-up protocols on vertical jump performance in male collegiate athletes. J Strength Cond Res. 2008;22(1):226–229. doi: 10.1519/JSC.0b013e31815f9d6a. [DOI] [PubMed] [Google Scholar]
- 198.Hough PA, Ross EZ, Howatson G. Effects of dynamic and static stretching on vertical jump performance and electromyographic activity. J Strength Cond Res. 2009;23(2):507–512. doi: 10.1519/JSC.0b013e31818cc65d. [DOI] [PubMed] [Google Scholar]
- 199.Hsu FY, Tsai KL, Lee CL, Chang WD, Chang NJ. Effects of dynamic stretching combined with static stretching, foam rolling, or vibration rolling as a warm-up exercise on athletic performance in elite table tennis players. J Sport Rehabil. 2021;30(2):198–205. doi: 10.1123/jsr.2019-0442. [DOI] [PubMed] [Google Scholar]
- 200.Huang S, Zhang HJ, Wang X, Lee WCC, Lam WK. Acute effects of soleus stretching on ankle flexibility, dynamic balance and speed performances in soccer players. Biology (Basel). 2022;11(3):374. doi: 10.3390/biology11030374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Huang Y, Zhu X-n. 男子跆拳道运动员下肢肌肉最大肌力肌电电压受PNF牵拉训练影响的研究 [Research on the effects of PNF stretching on strength and EMG parameters in taekwondo male players]. J Beijing Sport University. 2011;34(10):56–68.
- 202.Ide BN, Moreira A, Schoenfeld BJ, Lodo L, Santos AR, Barbosa WP, et al. Acute effect of different warm-up interventions on neuromuscular performance of recreational soccer players. Rev Bras Ciência Mov. 2017;25(3):34–43. doi: 10.31501/rbcm.v25i3.7053. [DOI] [Google Scholar]
- 203.Ishak A, Ahmad H, Mohamed NI, Rosman NA. The effects of different volumes of dynamic stretching on 20-m repeated sprint ability performance. J Fundam Appl Sci. 2017;9:1041–1049. doi: 10.4314/jfas.v9i6s.76. [DOI] [Google Scholar]
- 204.Ishak A, Ahmad H, Wong FY, Rejeb A, Hashim HA, Pullinger SA. Two sets of dynamic stretching of the lower body musculature improves linear repeated-sprint performance in team-sports. Asian J Sports Med. 2019 doi: 10.5812/asjsm.91775. [DOI] [Google Scholar]
- 205.Ishak A, Priestley J, Malik ZA, Osman N, Txi MRS, Rosman N, Ping FWC. Acute effect of different sets of ballistic stretching protocol on repeated sprint performance among football players. Eur J Mol Clin Med. 2020;7(2):5896–5903. [Google Scholar]
- 206.Jang HS, Kim D, Park J. Immediate effects of different types of stretching exercises on badminton jump smash. J Sports Med Phys Fit. 2018;58(7–8):1014–1020. doi: 10.23736/s0022-4707.17.06989-4. [DOI] [PubMed] [Google Scholar]
- 207.Jemni M, Mkaouer B, Marina M, Asllani A, Sands WA. Acute static vibration-induced stretching enhanced muscle viscoelasticity but did not affect maximal voluntary contractions in footballers. J Strength Cond Res. 2014;28(11):3105–3114. doi: 10.1519/jsc.0000000000000404. [DOI] [PubMed] [Google Scholar]
- 208.Jing L, Yang G. Effects of two kinds of stretch training on lower limb kinetics and energy absorption pattern during cushioning period. Chin J Appl Mech. 2021;38(6):2432–2440. doi: 10.11776/cjam.38.06.D040. [DOI] [Google Scholar]
- 209.Johnson AW, Warcup CN, Seeley MK, Eggett D, Feland JB. The acute effects of stretching with vibration on dynamic flexibility in young female gymnasts. J Sports Med Phys Fit. 2019;59(2):210–216. doi: 10.23736/s0022-4707.18.08290-7. [DOI] [PubMed] [Google Scholar]
- 210.Jordan JB, Korgaokar AD, Farley RS, Caputo JL. Acute effects of static and proprioceptive neuromuscular facilitation stretching on agility performance in elite youth soccer players. Int J Exerc Sci. 2012;5(2):97–105. [Google Scholar]
- 211.Junqueira C, Rudnick CT, Facci LM. Stretching Global Ativo comparado aos alongamentos convencionais em atletas de basquetebol [Active global stretching compared to conventional stretching in basketball athletes] Rev Terapia Manual. 2011;9(45):612–618. [Google Scholar]
- 212.Kafkas A, Eken Ö, Kurt C, Kafkas ME. The effects of different stretching and warm-up exercise protocols on 50-meter swimming performance in sub-elite women swimmers. Isokinet Exerc Sci. 2019;27(4):289–297. doi: 10.3233/ies-193141. [DOI] [Google Scholar]
- 213.Karloh M, dos Santos RP, Kraeski MH, Matias TS, Frutuoso AS. Alongamento estático versus conceito Mulligan—efeitos crônicos no treino de flexibilidade em ginastas [Static stretch versus Mulligan concept—long-term effects in gymnast's flexibility] Rev Bras Cineantropometria Desempenho Hum. 2010;12(3):202–208. doi: 10.5007/1980-0037.2010v12n3p202. [DOI] [Google Scholar]
- 214.Karloh M, dos Santos RP, Kraeski MH, Matias TS, Kraeski D, de Menezes FS. Alongamento estático versus conceito Mulligan: aplicações no treino de flexibilidade em ginastas [Static stretch versus Mulligan concept: flexibility training in gymnasts] Fisioter Mov. 2010;23(4):523–533. doi: 10.1590/S0103-51502010000400003. [DOI] [Google Scholar]
- 215.Kazemi O, Letafatkar A, Marchetti PH. Effect of stretching protocols on glenohumeral-joint muscle activation in elite table tennis players. Int J Sports Physiol Perform. 2021;16(1):110–116. doi: 10.1123/ijspp.2019-0768. [DOI] [PubMed] [Google Scholar]
- 216.Kilit B, Arslan E, Soylu Y. Effects of different stretching methods on speed and agility performance in young tennis players. Sci Sports. 2019;34(5):313–320. doi: 10.1016/j.scispo.2018.10.016. [DOI] [Google Scholar]
- 217.Konrad A, Tilp M, Stöcker F, Mehmeti L, Mahnič N, Seiberl W, et al. Quadriceps or triceps surae proprioceptive neuromuscular facilitation stretching with post-stretching dynamic activities does not induce acute changes in running economy. Front Physiol. 2022;13:981108. doi: 10.3389/fphys.2022.981108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Kornberg C, Ther GDM, McCarthy T. The effect of neural stretching technique on sympathetic outflow to the lower limbs. J Orthop Sports Phys Ther. 1992;16(6):269–274. doi: 10.2519/jospt.1992.16.6.269. [DOI] [PubMed] [Google Scholar]
- 219.Krčmár M, Šimonek J, Polačková B. Impact of different warm-up modalities on the height of countermovement vertical jump and its practical applicability. J Phys Educ Sport. 2016;16(2):481–488. doi: 10.7752/jpes.2016.02074. [DOI] [Google Scholar]
- 220.Kruse NT, Barr MW, Gilders RM, Kushnick MR, Rana SR. Using a practical approach for determining the most effective stretching strategy in female college division I volleyball players. J Strength Cond Res. 2013;27(11):3060–3067. doi: 10.1519/JSC.0b013e31828bf2b6. [DOI] [PubMed] [Google Scholar]
- 221.Kruse NT, Barr MW, Gilders RM, Kushnick MR, Rana SR. Effect of different stretching strategies on the kinetics of vertical jumping in female volleyball athletes. J Sport Health Sci. 2015;4(4):364–370. doi: 10.1016/j.jshs.2014.06.003. [DOI] [Google Scholar]
- 222.Kurt C. Alternative to traditional stretching methods for flexibility enhancement in well-trained combat athletes: local vibration versus whole-body vibration. Biol Sport. 2015;32(3):225–233. doi: 10.5604/20831862.1150305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Kurt C, Firtin I. Comparison of the acute effects of static and dynamic stretching exercises on flexibility, agility and anaerobic performance in professional football players. Turk J Phys Med Rehabil. 2016;62(3):206–213. doi: 10.5606/tftrd.2016.32698. [DOI] [Google Scholar]
- 224.Kurtdere I, Kurt C, Nebioglu IO. Acute static stretching with different volumes improves hamstring flexibility but not reactive strength index and leg stiffness in well-trained judo athletes. J Hum Sport Exerc. 2021;16(4):760–771. doi: 10.14198/jhse.2021.164.03. [DOI] [Google Scholar]
- 225.Kyranoudis Α, Arsenis S, Ispyrlidis I, Chatzinikolaou A, Gourgoulis V, Kyranoudis E, Metaxas T. The acute effects of combined foam rolling and static stretching program on hip flexion and jumping ability in soccer players. J Phys Educ Sport. 2019;19(2):1164–1172. doi: 10.7752/jpes.2019.02169. [DOI] [Google Scholar]
- 226.Kyranoudis Α, Nikolaidis V, Ispirlidis I, Galazoulas C, Alipasali F, Famisis K. Acute effect of specific warm-up exercises on sprint performance after static and dynamic stretching in amateur soccer players. J Phys Educ Sport. 2018;18(2):825–830. doi: 10.7752/jpes.2018.02122. [DOI] [Google Scholar]
- 227.Laudner KG, Sipes RC, Wilson JT. The acute effects of sleeper stretches on shoulder range of motion. J Athl Train. 2008;43(4):359–363. doi: 10.4085/1062-6050-43.4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Li B, Bai X, Zhu Y. Study on the effect of PNF method on the flexibility and strength quality of stretching muscles of shoulder joints of swimmers. MCB Mol Cell Biomech. 2021;18(2):99–105. doi: 10.32604/MCB.2021.014748. [DOI] [Google Scholar]
- 229.Lin WC, Lee CL, Chang NJ. Acute effects of dynamic stretching followed by vibration foam rolling on sports performance of badminton athletes. J Sports Sci Med. 2020;19(2):420–428. [PMC free article] [PubMed] [Google Scholar]
- 230.Little T, Williams AG. Effects of differential stretching protocols during warm-ups on high-speed motor capacities in professional soccer players. J Strength Cond Res. 2006;20(1):203–207. doi: 10.1519/R-16944.1. [DOI] [PubMed] [Google Scholar]
- 231.Lotfi N, Mohamadi S, Mirzaei-Takmil M. Effects of stretching before intense exercise training on hematologic and cellular injury indices. Pedagog Psychol Med Biol Probl Phys Train Sports. 2018;22(6):301–305. doi: 10.15561/18189172.2018.0604. [DOI] [Google Scholar]
- 232.Loughran M, Glasgow P, Bleakley C, McVeigh J. The effects of a combined static-dynamic stretching protocol on athletic performance in elite Gaelic footballers: a randomised controlled crossover trial. Phys Ther Sport. 2017;25:47–54. doi: 10.1016/j.ptsp.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 233.Lowery RP, Joy JM, Brown LE, de Souza EO, Wistocki DR, Davis GS, et al. Effects of static stretching on 1-mile uphill run performance. J Strength Cond Res. 2014;28(1):161–167. doi: 10.1519/JSC.0b013e3182956461. [DOI] [PubMed] [Google Scholar]
- 234.Makaruk H, Makaruk B, Sacewicz T. The effects of static stretching and isometric strength on hamstring strength and flexibility asymmetry. Pol J Sport Tour. 2010;17(3):153–156. [Google Scholar]
- 235.Manzi V, Iellamo F, Alashram AR, D'Onofrio R, Padua E, Casasco M, Annino G. Effects of three different stretching protocols on hamstring muscle flexibility in professional soccer players: a randomized study. J Sports Med Phys Fit. 2020;60(7):999–1004. doi: 10.23736/s0022-4707.20.10562-0. [DOI] [PubMed] [Google Scholar]
- 236.Mariscal SL, Garcia VS, Fernandez-Garcia JC, de Villarreal ES. Acute effects of ballistic vs. passive static stretching involved in a prematch warm-up on vertical jump and linear sprint performance in soccer players. J Strength Cond Res. 2021;35(1):147–153. doi: 10.1519/jsc.0000000000002477. [DOI] [PubMed] [Google Scholar]
- 237.Martin P, Pavol P, Zuzana P, Martina T, Juraji M. Effectiveness of static and dynamic stretching prior to speed and speed-strength load. J Phys Educ Sport. 2014;14(4):455–458. doi: 10.7752/jpes.2014.04069. [DOI] [Google Scholar]
- 238.Martinez-Chicote R, Brizuela G, Perez-Soriano P, Llana-Belloch S. Acute effect of 3 stretching techniques in sideward movements in tennis. Eur J Hum Mov. 2016;36:48–56. [Google Scholar]
- 239.Mascarin NC, Vancini RL, Lira CAB, Andrade MS. Stretch-induced reductions in throwing performance are attenuated by warm-up before exercise. J Strength Cond Res. 2015;29(5):1393–1398. doi: 10.1519/jsc.0000000000000752. [DOI] [PubMed] [Google Scholar]
- 240.McNeal JR, Sands WA. Acute static stretching reduces lower extremity power in trained children. Pediatr Exerc Sci. 2003;15(2):139–145. doi: 10.1123/pes.15.2.139. [DOI] [Google Scholar]
- 241.McNeal JR, Edgerly S, Sands WA, Kawaguchi J. Acute effects of vibration-assisted stretching are more evident in the non-dominant limb. Eur J Sport Sci. 2011;11(1):45–50. doi: 10.1080/17461391003774642. [DOI] [Google Scholar]
- 242.Meerits T, Bacchieri S, Pääsuke M, Ereline J, Cicchella A, Gapeyeva H. Acute effect of static and dynamic stretching on tone and elasticity of hamstring muscles and on vertical jump performance in track-and-field athletes. Acta Kinesiol Univ Tartu. 2014;20:48–59. doi: 10.12697/akut.2014.20.05. [DOI] [Google Scholar]
- 243.Melocchi I, Filipas L, Lovecchio N, De Nardi M, La Torre A, Codella R. Effects of different stretching methods on vertical jump ability and range of motion in young female artistic gymnastics athletes. J Sports Med Phys Fit. 2021;61(4):527–533. doi: 10.23736/s0022-4707.20.11386-0. [DOI] [PubMed] [Google Scholar]
- 244.Mendez-Sanchez R, Alburquerque-Sendin F, Fernandez-de-las-Penas C, Barbero-Iglesias FJ, Sanchez-Sanchez C, Calvo-Arenillas JI, Huijbregts P. Immediate effects of adding a sciatic nerve slider technique on lumbar and lower quadrant mobility in soccer players: a pilot study. J Altern Complement Med. 2010;16(6):669–675. doi: 10.1089/acm.2009.0403. [DOI] [PubMed] [Google Scholar]
- 245.Merrigan JJ, Tynan MN, Oliver JM, Jagim AR, Jones MT. Effect of post-exercise whole body vibration with stretching on mood state, fatigue, and soreness in collegiate swimmers. Sports (Basel). 2017;5(1):7. doi: 10.3390/sports5010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Mikolajec K, Waskiewicz Z, Maszczyk A, Bacik B, Kurek P, Zajac A. Effects of stretching and strength exercises on speed and power abilities in male basketball players. Isokinet Exerc Sci. 2012;20(1):61–69. doi: 10.3233/ies-2012-0442. [DOI] [Google Scholar]
- 247.Miladi I, Temfemo A, Mandengue SH, Ahmaidi S. Effect of recovery mode on exercise time to exhaustion, cardiorespiratory responses, and blood lactate after prior, intermittent supramaximal exercise. J Strength Cond Res. 2011;25(1):205–210. doi: 10.1519/JSC.0b013e3181af5152. [DOI] [PubMed] [Google Scholar]
- 248.Mojock CD, Kim JS, Eccles DW, Panton LB. The effects of static stretching on running economy and endurance performance in female distance runners during treadmill running. J Strength Cond Res. 2011;25(8):2170–2176. doi: 10.1519/JSC.0b013e3181e859db. [DOI] [PubMed] [Google Scholar]
- 249.Molacek ZD, Conley DS, Evetovich TK, Hinnerichs KR. Effects of low- and high-volume stretching on bench press performance in collegiate football players. J Strength Cond Res. 2010;24(3):711–716. doi: 10.1519/JSC.0b013e3181c7c242. [DOI] [PubMed] [Google Scholar]
- 250.Montalvo S, Dorgo S. The effect of different stretching protocols on vertical jump measures in college age gymnasts. J Sports Med Phys Fit. 2019;59(12):1956–1962. doi: 10.23736/s0022-4707.19.09561-6. [DOI] [PubMed] [Google Scholar]
- 251.Moore MA, Hutton RS. Electromyographic investigation of muscle stretching techniques. Med Sci Sports Exerc. 1980;12(5):322–329. doi: 10.1249/00005768-198025000-00004. [DOI] [PubMed] [Google Scholar]
- 252.Mor A, Yurtseven R, Mor H, Acar K. 11–12 yaş grubu futbolcularda farkli isinma protokollerinin bazi performans parametrelerine etkisi [The effects of different warm-up protocols on some performance parameters in 11–12 age group football players]. J Phys Educ Sports Sci. 2021;19(4):72–83. 10.33689/spormetre.907920.
- 253.Moran KA, McGrath T, Marshall BM, Wallace ES. Dynamic stretching and golf swing performance. Int J Sports Med. 2009;30(2):113–118. doi: 10.1055/s-0028-1103303. [DOI] [PubMed] [Google Scholar]
- 254.Moran MP, Whitehead JR, Guggenheimer JD, Brinkert RH. The effects of static stretching warm-up versus dynamic warm-up on sprint swim performance. J Swim Res. 2014;22(1):1–9. [Google Scholar]
- 255.Moreno-Perez V, Hernandez-Davo JL, Nakamura F, Lopez-Samanes A, Jimenez-Reyes P, Fernandez-Fernandez J, Behm DG. Post-activation performance enhancement of dynamic stretching and heavy load warm-up strategies in elite tennis players. J Back Musculoskelet Rehabil. 2021;34(3):413–423. doi: 10.3233/bmr-191710. [DOI] [PubMed] [Google Scholar]
- 256.Needham RA, Morse CI, Degens H. The acute effect of different warm-up protocols on anaerobic performance in elite youth soccer players. J Strength Cond Res. 2009;23(9):1614–1620. doi: 10.1519/JSC.0b013e3181b1f3ef. [DOI] [PubMed] [Google Scholar]
- 257.Nelson AG, Driscoll NM, Landin DK, Young MA, Schexnayder IC. Acute effects of passive muscle stretching on sprint performance. J Sports Sci. 2005;23(5):449–454. doi: 10.1080/02640410410001730205. [DOI] [PubMed] [Google Scholar]
- 258.Nobre TL, Rocha LY, Ramos CC, Mazuchi F, Carbone PO, Madureira D, et al. The use of proprioceptive neuromuscular facilitation for increasing throwing performance. Rev Bras Med Esporte. 2020;26(4):332–336. doi: 10.1590/1517-869220202604185184. [DOI] [Google Scholar]
- 259.Notarnicola A, Perroni F, Campese A, Maccagnano G, Monno A, Moretti B, Tafuri S. Flexibility responses to different stretching methods in young elite basketball players. Muscles Ligaments Tendons J. 2017;7(4):582–589. doi: 10.11138/mltj/2017.7.4.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Nuri L, Ghotbi N, Faghihzadeh S. Acute effects of static stretching, active warm up, or passive warm up on flexibility of the plantar flexor muscles of Iranian professional female taekwondo athletes. J Musculoskelet Pain. 2013;21(3):263–268. doi: 10.3109/10582452.2013.827771. [DOI] [Google Scholar]
- 261.O'Sullivan K, Murray E, Sainsbury D. The effect of warm-up, static stretching and dynamic stretching on hamstring flexibility in previously injured subjects. BMC Musculoskelet Disord. 2009 doi: 10.1186/1471-2474-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Ohshita T, Mitsuzono R. Influence of different stretching on range of motion and running economy in long distance runners. Jpn J Phys Fit Sports Med. 2009;58(3):395–404. doi: 10.7600/jspfsm.58.395. [DOI] [Google Scholar]
- 263.Olivares-Arancibia J, Solis-Urra P, Rodriguez-Rodriguez F, Santos-Lozano A, Sanchez-Martinez J, Martin-Hernandez J, et al. A single bout of whole-body vibration improves hamstring flexibility in university athletes: a randomized controlled trial. J Hum Sport Exerc. 2018;13(4):776–788. doi: 10.14198/jhse.2018.134.06. [DOI] [Google Scholar]
- 264.Oliveira LP, Vieira LHP, Aquino R, Manechini JPV, Santiago PRP, Puggina EF. Acute effects of active, ballistic, passive, and proprioceptive neuromuscular facilitation stretching on sprint and vertical jump performance in trained young soccer players. J Strength Cond Res. 2018;32(8):2199–2208. doi: 10.1519/jsc.0000000000002298. [DOI] [PubMed] [Google Scholar]
- 265.OñaTacan EJ, Chamorro Werz DN, Chávez CE. Insistencia pasiva dinámica y contracción maximal: influencia en la flexibilidad del split en kárate [Dynamic passive insistence and maximal contraction: flexibility influence on the karate split] Podium. 2021;16(2):524–534. [Google Scholar]
- 266.Oskouei ST, Abazari R, Kahjoogh MA, Goljaryan S, Zohrabi S. The effect of static stretching of agonist and antagonist muscles on knee joint position sense. Int J Ther Rehabil. 2021 doi: 10.12968/ijtr.2020.0043. [DOI] [Google Scholar]
- 267.Osternig LR, Robertson RN, Troxel RK, Hansen P. Differential responses to proprioceptive neuromuscular facilitation (PNF) stretch techniques. Med Sci Sports Exerc. 1990;22(1):106–111. doi: 10.1249/00005768-199002000-00017. [DOI] [PubMed] [Google Scholar]
- 268.Oyama S, Goerger CP, Goerger BM, Lephart SM, Joseph BM. Effects of non-assisted posterior shoulder stretches on shoulder range of motion among collegiate baseball pitchers. Athlet Train Sports Health Care J Pract Clin. 2010;2(4):163–170. doi: 10.3928/19425864-20100524-01. [DOI] [Google Scholar]
- 269.Pagaduan JC, Pojskic H, Uzicanin E, Babajic F. Effect of various warm-up protocols on jump performance in college football players. J Hum Kinet. 2012;35:127–132. doi: 10.2478/v10078-012-0086-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Panidi I, Bogdanis GC, Terzis G, Donti A, Konrad A, Gaspari V, Donti O. Muscle architectural and functional adaptations following 12-weeks of stretching in adolescent female athletes. Front Physiol. 2021;12:701338. doi: 10.3389/fphys.2021.701338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Papadimitriou K, Loupos D, Tsalis G, Manou B. Effects of proprioceptive neuromuscular facilitation (PNF) on swimmers leg mobility and performance. J Phys Educ Sport. 2017;17(2):663–668. doi: 10.7752/jpes.2017.02099. [DOI] [Google Scholar]
- 272.Papia K, Bogdanis GC, Toubekis A, Donti A, Donti O. Acute effects of prolonged static stretching on jumping performance and range of motion in young female gymnasts. Sci Gymnast J. 2018;10(2):217–226. [Google Scholar]
- 273.Pellegrini A, Tonino P, Salazar D, Hendrix K, Parel I, Cutti A, et al. Can posterior capsular stretching rehabilitation protocol change scapula kinematics in asymptomatic baseball pitchers? Musculoskelet Surg. 2016;100:39–43. doi: 10.1007/s12306-016-0416-1. [DOI] [PubMed] [Google Scholar]
- 274.Penichet-Tomas A, Pueo B, Abad-Lopez M, Jimenez-Olmedo JM. Acute comparative effect of foam rolling and static stretching on range of motion in rowers. Sustainability. 2021 doi: 10.3390/su13073631. [DOI] [Google Scholar]
- 275.Pojskic H, Pagaduan JC, Babajic F, Uzicanin E, Muratovic M, Tomljanovic M. Acute effects of prolonged intermittent low-intensity isometric warm-up schemes on jump, sprint, and agility performance in collegiate soccer players. Biol Sport. 2015;32(2):129–134. doi: 10.5604/20831862.1140427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Polat SC, Cetin E, Yarim I, Bulgay C, Cicioglu HI. Effect of ballistic warm-up on isokinetic strength, balance, agility, flexibility and speed in elite freestyle wrestlers. Sport Mont. 2018;16(3):85–89. doi: 10.26773/smj.181015. [DOI] [Google Scholar]
- 277.Pooley S, Spendiff O, Allen M, Moir HJ. Static stretching does not enhance recovery in elite youth soccer players. BMJ Open Sport Exerc Med. 2017 doi: 10.1136/bmjsem-2016-000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Pooley S, Spendiff O, Allen M, Moir HJ. Comparative efficacy of active recovery and cold water immersion as post-match recovery interventions in elite youth soccer. J Sports Sci. 2020;38(11–12):1423–1431. doi: 10.1080/02640414.2019.1660448. [DOI] [PubMed] [Google Scholar]
- 279.Popelka J, Pivovarniček P. Comparison of the effects of static and dynamic stretching on the force-velocity capabilities of young volleyball players. J Phys Educ Sport. 2018;18(4):2314–2318. doi: 10.7752/jpes.2018.04349. [DOI] [Google Scholar]
- 280.Popelka J, Beťák B, Pivovarniček P. In which indicators can the difference between effectivity of static and dynamic stretching of young volleyball players be noticed? Sport Sci. 2020;14(1):21–26. [Google Scholar]
- 281.Popelka J, Pivovarniček P. The effect comparison of foam rolling and dynamic stretching on performance in motion tests by young volleyball players: a pilot study. Phys Act Rev. 2022;10(2):140–149. doi: 10.16926/par.2022.10.28. [DOI] [Google Scholar]
- 282.Portilla-Dorado E, Villaquiran-Hurtado A, Molano-Tobar N. Potencia del salto en jugadores de fútbol sala después de la utilización del rodillo de espuma y la facilitación neuromuscular propioceptiva en la musculatura isquiosural [Jump power in futsal players after foam roller use and proprioceptive neuromuscular facilitation in the ischiosural muscles]. Revista de la Academia Colombiana de Ciencias Exactas, Fisicas y Naturales. 2019;43(167):165–76. 10.18257/raccefyn.846.
- 283.Racil G, Jlid MC, Bouzid MS, Sioud R, Khalifa R, Amri M, et al. Effects of flexibility combined with plyometric exercises vs. isolated plyometric or flexibility mode in adolescent male hurdlers. J Sports Med Phys Fit. 2020;60(1):45–52. doi: 10.23736/s0022-4707.19.09906-7. [DOI] [PubMed] [Google Scholar]
- 284.Reis EDS, Pereira GB, de Sousa NMF, Tibana RA, Silva MF, Araujo M, et al. Acute effects of proprioceptive neuromuscular facilitation and static stretching on maximal voluntary contraction and muscle electromyographical activity in indoor soccer players. Clin Physiol Funct Imaging. 2013;33(6):418–422. doi: 10.1111/cpf.12047. [DOI] [PubMed] [Google Scholar]
- 285.Reuther KE, Larsen R, Kuhn PD, Kelly JD, Thomas SJ. Sleeper stretch accelerates recovery of glenohumeral internal rotation after pitching. J Shoulder Elbow Surg. 2016;25(12):1925–1929. doi: 10.1016/j.jse.2016.07.075. [DOI] [PubMed] [Google Scholar]
- 286.Robey E, Dawson B, Goodman C, Beilby J. Effect of postexercise recovery procedures following strenuous stair-climb running. Res Sports Med. 2009;17(4):245–259. doi: 10.1080/15438620902901276. [DOI] [PubMed] [Google Scholar]
- 287.Rodriguez-Marroyo JA, Gonzalez B, Foster C, Carballo-Leyenda AB, Villa JG. Effect of the cooldown type on session rating of perceived exertion. Int J Sports Physiol Perform. 2021;16(4):573–577. doi: 10.1123/ijspp.2020-0225. [DOI] [PubMed] [Google Scholar]
- 288.Rogan S, Blasimann A, Steiger M, Torre A, Radlinger L. Acute effects of fast dynamic stretching on rate of force development in ice hockey players: a pilot study. Sportverletzung-Sportschaden. 2012;26(4):207–11. 10.1055/s-0032-1325416. [DOI] [PubMed]
- 289.Romero-Franco N, Parraga-Montilla JA, Molina-Flores EM, Jimenez-Reyes P. Effects of combining running and practical duration stretching on proprioceptive skills of national sprinters. J Strength Cond Res. 2020;34(4):1158–1165. doi: 10.1519/jsc.0000000000002620. [DOI] [PubMed] [Google Scholar]
- 290.Sekir U, Arabaci R, Akova B. Acute effects of static stretching on peak and end-range hamstring-to-quadriceps functional ratios. World J Orthop. 2015;6(9):719–726. doi: 10.5312/wjo.v6.i9.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Sagiroglu I, Kurt C, Pekunlu E, Ozsu I. Residual effects of static stretching and self-myofascial-release exercises on flexibility and lower body explosive strength in well-trained combat athletes. Isokinet Exerc Sci. 2017;25(2):135–141. doi: 10.3233/ies-160656. [DOI] [Google Scholar]
- 292.Sampaio-Jorge F, Rangel LFC, Mota HR, Morales AP, Costa L, Coelho GMO, Ribeiro BG. Acute effects of passive stretching on muscle power performance. J Exerc Physiol Online. 2014;17(6):81–89. [Google Scholar]
- 293.Sánchez-Sánchez J, Rodríguez-Fernández A, Villa-Vicente G, Petisco-Rodríguez C, Ramírez-Campillo R, Gonzalo-Skok O. Efecto de un calentamiento con estiramientos estáticos y dinámicos sobre el salto horizontal y la capacidad para repetir esprint con cambio de dirección [Effect of warm-up with static and dynamic stretching on the horizontal jump and repeated sprint ability with changes of direction] RICYDE. 2017;13(47):26–38. doi: 10.5232/ricyde2017.04702. [DOI] [Google Scholar]
- 294.Sands WA, McNeal JR, Stone MH, Kimmel WL, Haff GG, Jemni M. The effect of vibration on active and passive range of motion in elite female synchronized swimmers. Eur J Sport Sci. 2008;8(4):217–223. doi: 10.1080/17461390802116682. [DOI] [Google Scholar]
- 295.Sands WA, McNeal JR, Stone MH, Russell EM, Jemni M. Flexibility enhancement with vibration: acute and long-term. Med Sci Sports Exerc. 2006;38(4):720–725. doi: 10.1249/01.mss.0000210204.10200.dc. [DOI] [PubMed] [Google Scholar]
- 296.Satkunskiene D, Ardekani MMZ, Khair RM, Kutraite G, Venckuniene K, Snieckus A, Kamandulis S. Warm-up and hamstring stiffness, stress-relaxation, flexibility and knee proprioception in young soccer players. J Athl Train. 2022;57(5):485–493. doi: 10.4085/1062-6050-0416.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Sauers E, August A, Snyder A. Fauls stretching routine produces acute gains in throwing shoulder mobility in collegiate baseball players. J Sport Rehabil. 2007;16(1):28–40. doi: 10.1123/jsr.16.1.28. [DOI] [PubMed] [Google Scholar]
- 298.Sayers AL, Farley RS, Fuller DK, Jubenville CB, Caputo JL. The effect of static stretching on phases of sprint performance in elite soccer players. J Strength Cond Res. 2008;22(5):1416–1421. doi: 10.1519/JSC.0b013e318181a450. [DOI] [PubMed] [Google Scholar]
- 299.Schmitt GD, Pelham TW, Holt LE. Changes in flexibility of elite female soccer players resulting from a flexibility program or combined flexibility and strength program: a pilot study. Clin Kinesiol. 1998;52(3):64–67. [Google Scholar]
- 300.Schmitt GD, Pelham TW, Holt LE. A comparison of selected protocols during proprioceptive neuromuscular facilitation stretching. Clin Kinesiol. 1999;53(1):16–21. [Google Scholar]
- 301.Seçer E, Kaya DO. Comparison of immediate effects of foam rolling and dynamic stretching to only dynamic stretching on flexibility, balance, and agility in male soccer players. J Sport Rehabil. 2022;31(1):10–16. doi: 10.1123/jsr.2021-0017. [DOI] [PubMed] [Google Scholar]
- 302.Sekir U, Arabaci R, Akova B, Kadagan SM. Acute effects of static and dynamic stretching on leg flexor and extensor isokinetic strength in elite women athletes. Scand J Med Sci Sports. 2010;20(2):268–281. doi: 10.1111/j.1600-0838.2009.00923.x. [DOI] [PubMed] [Google Scholar]
- 303.Sekir U, Arabaci R, Akova B. Acute effects of dynamic stretching on peak and end-range functional hamstring/quadriceps strength ratios. Turk Klin J Med Sci. 2010;30(1):164–173. doi: 10.5336/medsci.2008-8752. [DOI] [Google Scholar]
- 304.Selkar SP, Ramteke GJ, Dongare AK. Effect of eccentric muscle training to reduce severity of delayed onset muscle soreness in athletic subjects. Eur J Gen Med. 2009;6(4):213–7. 10.29333/ejgm/82672.
- 305.Sermaxhaj S, Arifi F, Bahtiri A. The effect of static stretching in agility and isokinetic force at football players. Sport Mont. 2017;15(3):29–33. 10.26773/smj.2017.10.005.
- 306.Sermaxhaj S, Arifi F, Bahtiri A, Alaj I. The impact of recuperation with static stretching in flexibility and agility with and without ball of young soccer players. Acta Kinesiol. 2017;11(Suppl 1):33–38. [Google Scholar]
- 307.Sermaxhaj S, Popovic S, Bjelica D, Gardasevic J, Arifi F. Effect of recuperation with static stretching in isokinetic force of young football players. J Phys Educ Sport. 2017;17(3):1948–1953. doi: 10.7752/jpes.2017.03191. [DOI] [Google Scholar]
- 308.Sermaxhaj S, Arifi F, Iber A, Bahtiri A, Havolli J, Sermaxhaj S. The effect of static stretching in agility and isokinetic force at football players. Sport Mont. 2018;16(2):45–49. doi: 10.26773/smj.180608. [DOI] [Google Scholar]
- 309.Sermaxhaj S, Arifi F, Havolli J, Luta F, Isufi I. The effect of physical exercise according to a programme for the development of flexibility in the motor abilities of young football players. Sport Mont. 2021;19(1):25–29. doi: 10.26773/SMJ.210209. [DOI] [Google Scholar]
- 310.Sheard PW, Paine TJ. Optimal contraction intensity during proprioceptive neuromuscular facilitation for maximal increase of range of motion. J Strength Cond Res. 2010;24(2):416–421. doi: 10.1519/JSC.0b013e3181c50a0d. [DOI] [PubMed] [Google Scholar]
- 311.Shekadar M, Ganesh MSP, Mitra M. The immediate effects of sleeper stretch versus cross-body stretch on shoulder range of motion in volleyball players. Indian J Physiother Occup Ther. 2016;10(4):26–31. doi: 10.5958/0973-5674.2016.00114.3. [DOI] [Google Scholar]
- 312.Shitara H, Tajika T, Kuboi T, Ichinose T, Sasaki T, Hamano N, et al. Shoulder stretching versus shoulder muscle strength training for the prevention of baseball-related arm injuries: a randomized, active-controlled, open-label, non-inferiority study. Sci Rep. 2022;12(1):22118. doi: 10.1038/s41598-022-26682-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Siatras T, Papadopoulos G, Mameletzi D, Gerodimos V, Kellis S. Static and dynamic acute stretching effect on gymnasts' speed in vaulting. Pediatr Exerc Sci. 2003;15(4):383–391. doi: 10.1123/pes.15.4.383. [DOI] [Google Scholar]
- 314.Silva GF, Almeida AR, Rodrigues SA, Szmuchrowski LA, da Silva RAD, Drummond MDM. The acute effect of a sport-specific stretching routine on the performance of vertical jumps in rhythmic gymnasts. J Exerc Physiol Online. 2018;21(2):30–39. [Google Scholar]
- 315.Sim AY, Dawson BT, Guelfi KJ, Wallman KE, Young WB. Effects of static stretching in warm-up on repeated sprint performance. J Strength Cond Res. 2009;23(7):2155–2162. doi: 10.1519/JSC.0b013e3181b438f3. [DOI] [PubMed] [Google Scholar]
- 316.Skarabot J, Beardsley C, Stirn I. Comparing the effects of self-myofascial release with static stretching on ankle range-of-motion in adolescent athletes. Int J Sports Phys Ther. 2015;10(2):203–212. [PMC free article] [PubMed] [Google Scholar]
- 317.Solon Júnior LJF, Neto LVD. Efeito do alongamento estático e da corrida submáxima no desempenho do salto contramovimento e sprint em jogadores universitários de voleibol [Effect of static stretching and submaximal running on countermovement jump performance and sprint on college volleyball players] Retos. 2021;39:325–329. doi: 10.47197/retos.v0i39.79344. [DOI] [Google Scholar]
- 318.Song Y, Zhao XX, Finnie KP, Shao SR. Biomechanical analysis of vertical jump performance in well-trained young group before and after passive static stretching of knee flexors muscles. J Biomim Biomater Biomed Eng. 2018;36:24–33. doi: 10.4028/www.scientific.net/JBBBE.36.24. [DOI] [Google Scholar]
- 319.Stevanovic VB, Jelic MB, Milanovic SD, Filipovic SR, Mikic MJ, Stojanovic MDM. Sport-specific warm-up attenuates static stretching-induced negative effects on vertical jump but not neuromuscular excitability in basketball players. J Sports Sci Med. 2019;18(2):282–289. [PMC free article] [PubMed] [Google Scholar]
- 320.Stewart M, Adams R, Alonso A, Van Koesveld B, Campbell S. Warm-up or stretch as preparation for sprint performance? J Sci Med Sport. 2007;10(6):403–410. doi: 10.1016/j.jsams.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 321.Stojanovic MD, Mikic M, Vucetic V, Belegisanin B, Karac A, Bianco A, Drid P. Acute effects of static and dynamic stretching on vertical jump performance in adolescent basketball players. Gazz Med Ital. 2022;181(6):417–424. doi: 10.23736/S0393-3660.20.04575-1. [DOI] [Google Scholar]
- 322.Su RH, Wei C, Hsu MC. Effects of Different stretching strategies on soccer players' power, speed, and muscle strength performance. Rev de Cercet si Interv Soc. 2019;66:328–341. doi: 10.33788/rcis.66.19. [DOI] [Google Scholar]
- 323.Sudhakar S, Padmasheela V. To investigate the effects of different warm- up protocols in vertical jump performance in male collegiate volleyball players. Int J Sports Sci Fit. 2012;2(1):142–153. [Google Scholar]
- 324.Taber CB, Colter RJ, Davis JJ, Seweje PA, Wilson DP, Foster JZ, Merrigan JJ. The effects of body tempering on force production, flexibility and muscle soreness in collegiate football athletes. J Funct Morphol Kinesiol. 2022 doi: 10.3390/JFMK7010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Takeuchi K, Tsukuda F. Comparison of the effects of static stretching on range of motion and jump height between quadriceps, hamstrings and triceps surae in collegiate basketball players. BMJ Open Sport Exerc Med. 2019 doi: 10.1136/bmjsem-2019-000631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Taleb-Beydokhti I, Haghshenas R. Static versus dynamic stretching: chronic and acute effects on agility performance in male athletes. Int J Appl Exerc Physiol. 2015;4(1):1–8. [Google Scholar]
- 327.Tammam AH, Hashem EM. Individual and combined effects of PNF stretching and plyometric training on muscular power and flexibility for volleyball players. Amazonia Investiga. 2020;9(36):73–82. doi: 10.34069/ai/2020.36.12.6. [DOI] [Google Scholar]
- 328.Taylor KL, Sheppard JM, Lee H, Plummer N. Negative effect of static stretching restored when combined with a sport specific warm-up component. J Sci Med Sport. 2009;12(6):657–661. doi: 10.1016/j.jsams.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 329.Toft E, Espersen GT, Kålund S, Sinkjær T, Hornemann BC. Passive tension of the ankle before and after stretching. Am J Sports Med. 1989;17(4):489–494. doi: 10.1177/036354658901700407. [DOI] [PubMed] [Google Scholar]
- 330.Torres EM, Kraemer WJ, Vingren JL, Volek JS, Hatfield DL, Spiering BA, et al. Effects of stretching on upper-body muscular performance. J Strength Cond Res. 2008;22(4):1279–1285. doi: 10.1519/JSC.0b013e31816eb501. [DOI] [PubMed] [Google Scholar]
- 331.Tsolakis C, Douvis A, Tsigganos G, Zacharogiannis E, Smirniotou A. Acute effects of stretching on flexibility, power and sport specific performance in fencers. J Hum Kinet. 2010;26:105–114. doi: 10.2478/v10078-010-0054-x. [DOI] [Google Scholar]
- 332.Turki O, Chaouachi A, Behm DG, Chtara H, Chtara M, Bishop D, et al. The effect of warm-ups incorporating different volumes of dynamic stretching on 10-and 20-m sprint performance in highly trained male athletes. J Strength Cond Res. 2012;26(1):63–72. doi: 10.1519/JSC.0b013e31821ef846. [DOI] [PubMed] [Google Scholar]
- 333.Turki O, Dhahbi W, Padulo J, Khalifa R, Ridene S, Alamri K, et al. Warm-up with dynamic stretching: positive effects on match-measured change of direction performance in young elite volleyball players. Int J Sports Physiol Perform. 2020;15(4):528–533. doi: 10.1123/ijspp.2019-0117. [DOI] [PubMed] [Google Scholar]
- 334.Turna B, Bayazit B, Eryucel ME, Yildiz M, Karademir MB. Acute effect of dynamic and static stretching exercises on targeting performance in archery. Prog Nutr. 2021 doi: 10.23751/pn.v23iS1.11385. [DOI] [Google Scholar]
- 335.Unick J, Kieffer HS, Cheesman W, Feeney A. The acute effects of static and ballistic stretching on vertical jump performance in trained women. J Strength Cond Res. 2005;19(1):206–212. doi: 10.1519/R-14843.1. [DOI] [PubMed] [Google Scholar]
- 336.Valdivia JED, Moreno PJF, Gonzalez JB, Pineda LTB, Valencia RTM, Gomez EG. Efectos de un programa de flexibilidad en el desarrollo de la fuerza muscular en jugadoras de futbol femenil [Effects of a program of stretching in the development of muscular strength in women's soccer players]. Educacion Fisica y Ciencia. 2015;17(2).
- 337.Van Gelder LH, Bartz SD. The effect of acute stretching on agility performance. J Strength Cond Res. 2011;25(11):3014–3021. doi: 10.1519/JSC.0b013e318212e42b. [DOI] [PubMed] [Google Scholar]
- 338.Van Zyl C, De Beer R, Bassett SH. The immediate effect of vibration therapy on flexibility in female junior elite gymnasts. Afr J Phys Health Educ Recreat Dance. 2011 doi: 10.4314/ajpherd.v17i3.68069. [DOI] [Google Scholar]
- 339.Vasconcellos F, Salles PGCM, Cardozo GP, Achour Junior A, Mello DB, Dantas EHM. Efeitos do flexionamento dinâmico agudo no impulsão vertical de jogadores de futebol. Fit Perform J Online. 2010;9(1):5–9. doi: 10.3900/fpj.9.1.5.p. [DOI] [Google Scholar]
- 340.Vasconcellos F, Massaferri R, Reis M, Carnevale D, Salles PG, Brito J. Could the deleterious effect of stretching only influence soccer players with better performance in the vertical jump? Hum Mov. 2018;19(5 Special Issue):23–8. 10.5114/hm.2018.79736.
- 341.Veevo M, Ereline J, Riso E-M, Gapeyeva H, Pääsuke M. The acute effects of warm-up, static and dynamic stretching exercises on biceps brachii muscle function in female basketball players. Acta Kinesiol Univ Tartu. 2012;18:39–46. doi: 10.12697/akut.2012.18.05. [DOI] [Google Scholar]
- 342.Velasque R, Paulucio D, Alvarenga RL, Santos CG, Serpa TK, Machado M, et al. Could static stretching decrease anaerobic power in young soccer players? Med Sport (Roma). 2020;73(2):210–219. doi: 10.23736/s0025-7826.20.03629-7. [DOI] [Google Scholar]
- 343.Walker MA, Li Y, Samson CO, Simpson KJ, Foutz T, Brown CN. Differences in trunk range of motion for various flexibility protocol types, particularly in quarterbacks wearing rib protectors. Sports Orthop Traumatol. 2021;37(1):41–50. doi: 10.1016/j.orthtr.2020.11.001. [DOI] [Google Scholar]
- 344.Wallmann HW, Gillis CB, Martinez NJ. The effects of different stretching techniques of the quadriceps muscles on agility performance in female collegiate soccer athletes: a pilot study. N Am J Sports Phys Ther. 2008;3(1):41–47. [PMC free article] [PubMed] [Google Scholar]
- 345.Walsh GS. Effect of static and dynamic muscle stretching as part of warm up procedures on knee joint proprioception and strength. Hum Mov Sci. 2017;55:189–195. doi: 10.1016/j.humov.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 346.Werstein KM, Lund RJ. The effects of two stretching protocols on the reactive strength index in female soccer and rugby players. J Strength Cond Res. 2012;26(6):1564–1567. doi: 10.1519/JSC.0b013e318231ac09. [DOI] [PubMed] [Google Scholar]
- 347.West AD, Cooke MB, LaBounty PM, Byars AG, Greenwood M. Effects of G-trainer, cycle ergometry, and stretching on physiological and psychological recovery from endurance exercise. J Strength Cond Res. 2014;28(12):3453–3461. doi: 10.1519/jsc.0000000000000577. [DOI] [PubMed] [Google Scholar]
- 348.Williams JG, Laudner KG, McLoda T. The acute effects of two passive stretch maneuvers on pectoralis minor length and scapular kinematics among collegiate swimmers. Int J Sports Phys Ther. 2013;8(1):25–33. [PMC free article] [PubMed] [Google Scholar]
- 349.Wilson JM, Hornbuckle LM, Kim JS, Ugrinowitsch C, Lee SR, Zourdos MC, et al. Effects of static stretching on energy cost and running endurance performance. J Strength Cond Res. 2010;24(9):2274–2279. doi: 10.1519/JSC.0b013e3181b22ad6. [DOI] [PubMed] [Google Scholar]
- 350.Winchester JB, Nelson AG, Landin D, Young MA, Schexnayder IC. Static stretching impairs sprint performance in collegiate track and field athletes. J Strength Cond Res. 2008;22(1):13–18. doi: 10.1519/JSC.0b013e31815ef202. [DOI] [PubMed] [Google Scholar]
- 351.Wong PL, Lau PWC, Mao DW, Wu YY, Behm DG, Wisloff U. Three days of static stretching within a warm-up does not affect repeated-sprint ability in youth soccer players. J Strength Cond Res. 2011;25(3):838–845. doi: 10.1519/JSC.0b013e3181cc2266. [DOI] [PubMed] [Google Scholar]
- 352.Yamaguchi T, Takizawa K, Shibata K. Acute effect of dynamic stretching on endurance running performance in well-trained male runners. J Strength Cond Res. 2015;29(11):3045–3052. doi: 10.1519/jsc.0000000000000969. [DOI] [PubMed] [Google Scholar]
- 353.Yamaguchi T, Takizawa K, Shibata K, Tomabechi N, Samukawa M, Yamanaka M. Effect of general warm-up plus dynamic stretching on endurance running performance in well-trained male runners. Res Q Exerc Sport. 2019;90(4):527–533. doi: 10.1080/02701367.2019.1630700. [DOI] [PubMed] [Google Scholar]
- 354.Yamaguchi T, Takizawa K, Shibata K, Tomabechi N, Samukawa M, Yamanaka M. Acute effect of dynamic stretching or running on endurance running performance in well-trained male runners. Gazz Med Ital. 2020;179(1–2):13–19. doi: 10.23736/s0393-3660.18.03987-6. [DOI] [Google Scholar]
- 355.Yaşli BÇ, Müniroğlu RS. Futbolcularda 8 haftalik statik germe antrenmanlarinin siçrama performansina etkileri [The effects of 8 weeks static stretching traning on jumping in soccer players] J Phys Educ Sports Sci. 2019;17(4):134–142. doi: 10.33689/spormetre.562545. [DOI] [Google Scholar]
- 356.Yildiz M. An acute bout of self-myofascial release increases flexibility without a concomitant deficit in muscle performance in football players. Int J Physiother. 2018;5(3):92–97. doi: 10.15621/ijphy/2018/v5i3/173932. [DOI] [Google Scholar]
- 357.Yıldırım Y, Arabacı R, Güngör AK, Görgülü R. The effects of dynamic and static stretching exercises performed to elite wrestlers after high intensity exercise on heart rate variability. Sci Sports. 2022 doi: 10.1016/j.scispo.2022.03.008. [DOI] [Google Scholar]
- 358.Young W, Clothier P, Otago L, Bruce L, Liddell D. Acute effects of static stretching on hip flexor and quadriceps flexibility, range of motion and foot speed in kicking a football. J Sci Med Sport. 2004;7(1):23–31. doi: 10.1016/s1440-2440(04)80040-9. [DOI] [PubMed] [Google Scholar]
- 359.Zakas A, Galazoulas C, Zakas N, Vamvakoudis E, Vergou A. The effect of stretching duration on flexibility during warming up in adolescent soccer players. Phys Train. 2005:2.
- 360.Zakas A. The effect of stretching duration on the lower-extremity flexibility of adolescent soccer players. J Bodyw Mov Ther. 2005;9(3):220–225. doi: 10.1016/j.jbmt.2004.07.002. [DOI] [Google Scholar]
- 361.Zakas A, Doganis G, Galazoulas C, Vamvakoudis E. Effect of acute static stretching duration on isokinetic peak torque in pubescent soccer players. Pediatr Exerc Sci. 2006;18(2):252–261. doi: 10.1123/pes.18.2.252. [DOI] [Google Scholar]
- 362.Zakas A, Doganis G, Papakonstandinou V, Sentelidis T, Vamvakoudis E. Acute effects of static stretching duration on isokinetic peak torque production of soccer players. J Bodyw Mov Ther. 2006;10(2):89–95. doi: 10.1016/j.jbmt.2005.04.007. [DOI] [Google Scholar]
- 363.Zakas A, Galazoulas C, Doganis G, Zakas N. Effect of two acute static stretching durations of the rectus femoris muscle on quadriceps isokinetic peak torque in professional soccer players. Isokinet Exerc Sci. 2006;14(4):357–362. doi: 10.3233/ies-2006-0249. [DOI] [Google Scholar]
- 364.Zakas A, Grammatikopoulou MG, Zakas N, Zahariadis P, Vamvakoudis E. The effect of active warm-up and stretching on the flexibility of adolescent soccer players. J Sports Med Phys Fit. 2006;46(1):57–61. [PubMed] [Google Scholar]
- 365.Zmijewski P, Lipinska P, Czajkowska A, Mroz A, Kapuscinski P, Mazurek K. Acute effects of a static vs. a dynamic stretching warm-up on repeated-sprint performance in female handball players. J Hum Kinet. 2020;72(1):161–172. doi: 10.2478/hukin-2019-0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Zourdos MC, Wilson JM, Sommer BA, Lee SR, Park YM, Henning PC, et al. Effects of dynamic stretching on energy cost and running endurance performance in trained male runners. J Strength Cond Res. 2012;26(2):335–341. doi: 10.1519/JSC.0b013e318225bbae. [DOI] [PubMed] [Google Scholar]
- 367.孙勇. 不同恢复手段对青年男子篮球运动员高强度间歇训练时运动能力和能量代谢的影响 [Effects of distinct recovery methods on exercise performance and energy metabolism in high intensity interval training of young male basketball athletes]. J Shenyang Sport Univ. 2017;36(4):106–12.
- 368.Nakamura M, Ikezoe T, Takeno Y, Ichihashi N. Effects of a 4-week static stretch training program on passive stiffness of human gastrocnemius muscle-tendon unit in vivo. Eur J Appl Physiol. 2012;112(7):2749–2755. doi: 10.1007/s00421-011-2250-3. [DOI] [PubMed] [Google Scholar]
- 369.Abt G, Boreham C, Davison G, Jackson R, Nevill A, Wallace E, Williams M. Power, precision, and sample size estimation in sport and exercise science research. J Sports Sci. 2020;38(17):1933–1935. doi: 10.1080/02640414.2020.1776002. [DOI] [PubMed] [Google Scholar]
- 370.Speed HD, Andersen MB. What exercise and sport scientists don't understand. J Sci Med Sport. 2000;3(1):84–92. doi: 10.1016/s1440-2440(00)80051-1. [DOI] [PubMed] [Google Scholar]
- 371.Sainani K, Chamari K. Wish list for improving the quality of statistics in sport science. Int J Sports Physiol Perform. 2022;17(5):673–674. doi: 10.1123/ijspp.2022-0023. [DOI] [PubMed] [Google Scholar]
- 372.Skorski S, Hecksteden A. Coping with the “small sample–small relevant effects” dilemma in elite sport research. Int J Sports Physiol Perform. 2021;16(11):1559–1560. doi: 10.1123/ijspp.2021-0467. [DOI] [PubMed] [Google Scholar]
- 373.Ramirez-Campillo R, Thapa RK, Afonso J, Perez-Castilla A, Bishop C, Byrne PJ, Granacher U. Effects of plyometric jump training on the reactive strength index in healthy individuals across the lifespan: a systematic review with meta-analysis. Sports Med. 2023;53(5):1029–1053. doi: 10.1007/s40279-023-01825-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Ramirez-Campillo R, Moran J, Chaabene H, Granacher U, Behm DG, García-Hermoso A, Izquierdo M. Methodological characteristics and future directions for plyometric jump training research: a scoping review update. Scand J Med Sci Sports. 2020;30(6):983–997. doi: 10.1111/sms.13633. [DOI] [PubMed] [Google Scholar]
- 375.Patel R, Kemp CL, Hafejee M, Peckham N, Jain V, McCann GP, Pallikadavath S. The underrepresentation of females in studies assessing the impact of high-dose exercise on cardiovascular outcomes: a scoping review. Sports Med Open. 2021;7(1):30. doi: 10.1186/s40798-021-00320-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Afonso J, Olivares-Jabalera J, Fernandes RJ, Clemente FM, Rocha-Rodrigues S, Claudino JG, et al. Effectiveness of conservative interventions after acute hamstrings injuries in athletes: a living systematic review. Sports Med. 2023;53(3):615–635. doi: 10.1007/s40279-022-01783-z. [DOI] [PubMed] [Google Scholar]
- 377.Cowley ES, Olenick AA, McNulty KL, Ross EZ. “Invisible sportswomen”: the sex data gap in sport and exercise science research. Women Sport Phys Act J. 2021;29(2):146–151. doi: 10.1123/wspaj.2021-0028. [DOI] [Google Scholar]
- 378.Kristian T, Laura K, Thomas B, Julie Sandell J, Michael Skovdal R, Heidi K, Karen K. ‘More Walk and Less Talk’: changing gender bias in sports medicine. Br J Sports Med. 2020;54(23):1380. doi: 10.1136/bjsports-2020-102966. [DOI] [PubMed] [Google Scholar]
- 379.Walton CC, Gwyther K, Gao CX, Purcell R, Rice SM. Evidence of gender imbalance across samples in sport and exercise psychology. Int Rev Sport Exerc Psychol. 2022 doi: 10.1080/1750984X.2022.2150981. [DOI] [Google Scholar]
- 380.Sallie MC, Joanne LK, Clare LA, Jane ST, Ebonie Kendra R, Andrea MB, et al. Sport and exercise medicine/physiotherapy publishing has a gender/sex equity problem: we need action now! Br J Sports Med. 2023;57(7):401. 10.1136/bjsports-2022-106055.
- 381.Eime RM, Harvey JT, Charity MJ, Casey MM, Westerbeek H, Payne WR. Age profiles of sport participants. BMC Sports Sci Med Rehabil. 2016;8(1):6. doi: 10.1186/s13102-016-0031-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Organization WH. Global status report on physical activity 2022. Geneva: World Health Organization; 2022. [Google Scholar]
- 383.Huebner M, Ma W. Health challenges and acute sports injuries restrict weightlifting training of older athletes. BMJ Open Sport Exerc Med. 2022;8(2):e001372. doi: 10.1136/bmjsem-2022-001372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Huebner M, Meltzer D, Ma W, Arrow H. The Masters athlete in Olympic weightlifting: training, lifestyle, health challenges, and gender differences. PLoS ONE. 2020;15(12):e0243652. doi: 10.1371/journal.pone.0243652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.McKendry J, Breen L, Shad BJ, Greig CA. Muscle morphology and performance in master athletes: a systematic review and meta-analyses. Ageing Res Rev. 2018;45:62–82. doi: 10.1016/j.arr.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 386.Sousa CV, Silva Aguiar S, Deus LA, Barbosa LP, Dos Santos PA, Neves RVP, et al. Faster and healthier: relationship between telomere and performance in master athletes. Int J Sports Med. 2020;41(5):339–344. doi: 10.1055/a-1088-5279. [DOI] [PubMed] [Google Scholar]
- 387.Tso J, Kim JH. Master endurance athletes and cardiovascular controversies. Curr Sports Med Rep. 2020;19(3):113–118. doi: 10.1249/jsr.0000000000000695. [DOI] [PubMed] [Google Scholar]
- 388.Zambolin F, McPhee JS, Duro-Ocana P, Ganse B, Bagley L, Faisal A. The association of elevated blood pressure during ischaemic exercise with sport performance in master athletes with and without morbidity. Eur J Appl Physiol. 2022;122(1):211–221. doi: 10.1007/s00421-021-04828-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Donti O, Konrad A, Panidi I, Dinas PC, Bogdanis GC. Is there a “window of opportunity” for flexibility development in youth? A systematic review with meta-analysis. Sports Med Open. 2022;8(1):88. doi: 10.1186/s40798-022-00476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Martínez-Silván D, Johnson A. Lower limb flexibility characteristics in youth athletics. Differences among events and age groups in highly trained adolescent athletes. Apunts Sports Med. 2020;55(207):89–95. doi: 10.1016/j.apunsm.2020.05.003. [DOI] [Google Scholar]
- 391.Afonso J, Nikolaidis PT, Sousa P, Mesquita I. Is empirical research on periodization trustworthy? A comprehensive review of conceptual and methodological issues. J Sports Sci Med. 2017;16(1):27–34. [PMC free article] [PubMed] [Google Scholar]
- 392.Schärer C, Tacchelli L, Göpfert B, Gross M, Lüthy F, Taube W, Hübner K. Specific eccentric-isokinetic cluster training improves static strength elements on rings for elite gymnasts. Int J Environ Res Public Health. 2019 doi: 10.3390/ijerph16224571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Afonso J, Reurink G, Clemente FM, Ramirez-Campillo R, Pizzari T, Andrade R. Revisiting the hamstring injury prevention and rehabilitation literature: filling the gaps! Br J Sports Med. 2023. 10.1136/bjsports-2023-106878. [DOI] [PubMed]
- 394.Heck K, Zeppieri G, Bruner M, Moser M, Farmer KW, Pozzi F. Preseason upper extremity range of motion and strength in relation to in-season injuries in NCAA division I gymnasts. Orthop J Sports Med. 2021;9(1):2325967120977090. doi: 10.1177/2325967120977090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Howle K, Waterson A, Duffield R. Recovery profiles following single and multiple matches per week in professional football. Eur J Sport Sci. 2019;19(10):1303–1311. doi: 10.1080/17461391.2019.1601260. [DOI] [PubMed] [Google Scholar]
- 396.Noor D, McCall A, Jones M, Duncan C, Ehrmann F, Meyer T, Duffield R. Perceived load, fatigue and recovery responses during congested and non-congested micro-cycles in international football tournaments. J Sci Med Sport. 2021;24(12):1278–1283. doi: 10.1016/j.jsams.2021.07.001. [DOI] [PubMed] [Google Scholar]
- 397.Ramirez-Campillo R, Moran J, Oliver JL, Pedley JS, Lloyd RS, Granacher U. Programming plyometric-jump training in soccer: a review. Sports (Basel). 2022 doi: 10.3390/sports10060094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Querido SM, Brito J, Figueiredo P, Carnide F, Vaz JR, Freitas SR. Postmatch recovery practices carried out in professional football: a survey of 56 Portuguese professional football teams. Int J Sports Physiol Perform. 2022;17(5):748–754. doi: 10.1123/ijspp.2021-0343. [DOI] [PubMed] [Google Scholar]
- 399.Judge LW, Avedesian JM, Bellar DM, Hoover DL, Craig BW, Langley J, et al. Pre- and post-activity stretching practices of collegiate soccer coaches in the United State. Int J Exerc Sci. 2020;13(6):260–272. doi: 10.70252/PDCB3344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Spence AJ, Helms ER, McGuigan MR. Stretching practices of international powerlifting federation unequipped powerlifters. J Strength Cond Res. 2022;36(12):3456–3461. doi: 10.1519/jsc.0000000000003800. [DOI] [PubMed] [Google Scholar]
- 401.Babault N, Rodot G, Champelovier M, Cometti C. A survey on stretching practices in women and men from various sports or physical activity programs. Int J Environ Res Public Health. 2021 doi: 10.3390/ijerph18083928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Bompa TO, Buzzichelli CA. Periodization: Theory and Methodology of Training. 6. Champaign, IL: Human Kinetics; 2019. [Google Scholar]
- 403.American College of Sports Medicine. ACSM’s exercise testing and prescription. 1st ed. Wolters Kluwer; 2018.
- 404.Querido SM, Radaelli R, Brito J, Vaz JR, Freitas SR. Analysis of recovery methods' efficacy applied up to 72 hours postmatch in professional football: a systematic review with graded recommendations. Int J Sports Physiol Perform. 2022;17(9):1326–1342. doi: 10.1123/ijspp.2022-0038. [DOI] [PubMed] [Google Scholar]
- 405.Alizadeh S, Daneshjoo A, Zahiri A, Anvar SH, Goudini R, Hicks JP, et al. Resistance training induces improvements in range of motion: a systematic review and meta-analysis. Sports Med. 2023;53(3):707–722. doi: 10.1007/s40279-022-01804-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Herold F, Müller P, Gronwald T, Müller NG. Dose–response matters!—a perspective on the exercise prescription in exercise–cognition research. Front Physiol. 2019 doi: 10.3389/fpsyg.2019.02338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Slimani M, Paravlic A, Granacher U. A meta-analysis to determine strength training related dose-response relationships for lower-limb muscle power development in young athletes. Front Physiol. 2018;9:1155. doi: 10.3389/fphys.2018.01155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Galloway M, Marsden DL, Callister R, Erickson KI, Nilsson M, English C. What is the dose-response relationship between exercise and cardiorespiratory fitness after stroke? A systematic review. Phys Ther. 2019;99(7):821–832. doi: 10.1093/ptj/pzz038. [DOI] [PubMed] [Google Scholar]
- 409.Lee I-M. Dose-response relation between physical activity and fitnesseven a little is good; more is better. JAMA. 2007;297(19):2137–2139. doi: 10.1001/jama.297.19.2137. [DOI] [PubMed] [Google Scholar]
- 410.Lauersen JB, Andersen TE, Andersen LB. Strength training as superior, dose-dependent and safe prevention of acute and overuse sports injuries: a systematic review, qualitative analysis and meta-analysis. Br J Sports Med. 2018;52(24):1557–1563. doi: 10.1136/bjsports-2018-099078. [DOI] [PubMed] [Google Scholar]
- 411.Pickering C, Kiely J. Do non-responders to exercise exist-and if so, what should we do about them? Sports Med. 2019;49(1):1–7. doi: 10.1007/s40279-018-01041-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Pickering C, Kiely J. The development of a personalised training framework: implementation of emerging technologies for performance. J Funct Morphol Kinesiol. 2019;4(2):25. doi: 10.3390/jfmk4020025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Gronwald T, Törpel A, Herold F, Budde H. Perspective of dose and response for individualized physical exercise and training prescription. J Funct Morphol Kinesiol. 2020 doi: 10.3390/jfmk5030048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Wackerhage H, Schoenfeld BJ. Personalized, evidence-informed training plans and exercise prescriptions for performance, fitness and health. Sports Med. 2021;51(9):1805–1813. doi: 10.1007/s40279-021-01495-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Impellizzeri FM, Shrier I, McLaren SJ, Coutts AJ, McCall A, Slattery K, et al. Understanding training load as exposure and dose. Sports Med. 2023 doi: 10.1007/s40279-023-01833-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Loturco I, Nakamura FY, Artioli GG, Kobal R, Kitamura K, Cal Abad CC, et al. Strength and power qualities are highly associated with punching impact in elite amateur boxers. J Strength Cond Res. 2016;30(1):109–116. doi: 10.1519/jsc.0000000000001075. [DOI] [PubMed] [Google Scholar]
- 417.Suchomel TJ, Nimphius S, Stone MH. The importance of muscular strength in athletic performance. Sports Med. 2016;46(10):1419–1449. doi: 10.1007/s40279-016-0486-0. [DOI] [PubMed] [Google Scholar]
- 418.Styles WJ, Matthews MJ, Comfort P. Effects of strength training on squat and sprint performance in soccer players. J Strength Cond Res. 2016;30(6):1534–1539. doi: 10.1519/jsc.0000000000001243. [DOI] [PubMed] [Google Scholar]
- 419.Lum D, Barbosa TM. Brief review: effects of isometric strength training on strength and dynamic performance. Int J Sports Med. 2019;40(6):363–375. doi: 10.1055/a-0863-4539. [DOI] [PubMed] [Google Scholar]
- 420.Herbert R, Gabriel M. Effects of stretching before and after exercising on muscle soreness and risk of injury: systematic review. BMJ. 2002;325(7362):468. doi: 10.1136/bmj.325.7362.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Weldon SM, Hill RH. The efficacy of stretching for prevention of exercise-related injury: a systematic review of the literature. Man Ther. 2003;8(3):141–150. doi: 10.1016/s1356-689x(03)00010-9. [DOI] [PubMed] [Google Scholar]
- 422.Thacker SB, Gilchrist J, Stroup DF, Kimsey CD., Jr The impact of stretching on sports injury risk: a systematic review of the literature. Med Sci Sports Exerc. 2004;36(3):371–378. doi: 10.1249/01.mss.0000117134.83018.f7. [DOI] [PubMed] [Google Scholar]
- 423.Lauersen JB, Bertelsen DM, Andersen LB. The effectiveness of exercise interventions to prevent sports injuries: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2014;48(11):871–877. doi: 10.1136/bjsports-2013-092538. [DOI] [PubMed] [Google Scholar]
- 424.Leppänen M, Aaltonen S, Parkkari J, Heinonen A, Kujala UM. Interventions to prevent sports related injuries: a systematic review and meta-analysis of randomised controlled trials. Sports Med. 2014;44(4):473–486. doi: 10.1007/s40279-013-0136-8. [DOI] [PubMed] [Google Scholar]
- 425.Dijksma I, Arslan IG, van Etten-Jamaludin FS, Elbers RG, Lucas C, Stuiver MM. Exercise programs to reduce the risk of musculoskeletal injuries in military personnel: a systematic review and meta-analysis. PM&R. 2020;12(10):1028–1037. doi: 10.1002/pmrj.12360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Behm DG, Kay AD, Trajano GS, Alizadeh S, Blazevich AJ. Effects of stretching on injury risk reduction and balance. J Clin Exerc Physiol. 2021;10(3):106–116. doi: 10.31189/2165-6193-10.3.106. [DOI] [Google Scholar]
- 427.Menegatti E, Mandini S, Pagani A, Mandini B, Zerbini V, Piva T, et al. The effect of active stretching training in patients with chronic venous insufficiency monitored by raster-stereography. Sensors (Basel). 2022 doi: 10.3390/s22218509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Hwang WT, Jeong YJ, Kim SY, Jeong YG. Effects of proprioceptive neuromuscular facilitation stretching and deep-breathing exercises on upper extremity lymphedema in stroke patients. J Phys Ther Sci. 2016;28(12):3276–3278. doi: 10.1589/jpts.28.3276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.Janes WC, Snow BB, Watkins CE, Noseworthy EA, Reid JC, Behm DG. Effect of participants' static stretching knowledge or deception on the responses to prolonged stretching. Appl Physiol Nutr Metab. 2016;41(10):1052–1056. doi: 10.1139/apnm-2016-0241. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used to inform this review are fully disclosed either in the manuscript or in its Electronic Supplementary Material.