Abstract
Background
The prone position has been seen to benefit patients experiencing acute respiratory distress syndrome. However, performing this position in pregnant patients has been difficult and raises safety concerns.
Objective
The current study aimed to test the use of a supportive pillow (Prone Pillow for Pregnant Patients or 4P) to address concerns regarding pregnant patients in prone position.
Methods
The study prospectively evaluated the use of the prone pillow for patient comfort and usability among healthcare workers with qualitative and quantitative measures.
Results
A total of three patients were recruited alongside 16 healthcare workers assisting pregnant patients to the prone position. Overall, awake pregnant patients found the pillow to be comfortable while healthcare workers perceived the pillow to be useful in improving quality of care among awake and intubated pregnant patients.
CONCLUSION
The 4P is a potentially useful and beneficial product in placing pregnant patients in the prone position during episodes of acute respiratory distress. However, due to the limited sample size, more clinical trials are needed to evaluate the impact of this innovation in improving patient and healthcare worker safety.
Keywords: prone positioning, prone pillow, COVID-19, ARDS
INTRODUCTION
The World Health Organization declared COVID-19 a pandemic on March 11, 20201 and there were over 45 million confirmed cases and over a million deaths due to COVID-19 worldwide in that year2. In comparison, COVID-19 cases in the Philippines rose with over 3,900,000 cases and more than 63,000 deaths in October of 2023.3 A major concern of physicians in managing patients diagnosed with COVID-19 is acute respiratory distress syndrome (ARDS). Several methods were seen to be viable in managing COVID-induced ARDS including intubation, low tidal volume, venous extra-corporeal membrane oxygenation (ECMO), high positive end expiratory pressure (PEEP), and prone positioning.4
The prone position has numerous benefits. A comparative study5 found that systolic blood pressure was found to decrease while on prone. This benefit extends to pregnant women as it has been seen to decrease respiratory rate and systolic blood pressure significantly with increased oxygen saturation in prone positioning compared to other positions.6 Physiologically, prone positioning reduces ventral-dorsal transpulmonary pressure difference,7 lung compression,8 and improves lung perfusion9.
Similar results were seen in COVID-19 patients, making prone positioning a feasible and effective method in improving blood oxygenation.10 Moreover, patients with COVID-19 reported increased comfort in prone positioning in combination with non-invasive ventilation such as high flow nasal oxygen therapy.11
The benefits of proning are even more important among pregnant patients experiencing COVID-induced ARDS which can have adverse effects on the developing fetus due to reduced oxygenation.12 Samanta, Samanta, Wig, and Baronia12 reported a case of severe ARDS in pregnancy with marked improvement in oxygenation with proning. They emphasized that proper precautions be observed when proning a patient in late pregnancy by providing support below the chest and iliac bone. Similarly, Tolcher, McKinney, Eppes, Muigai et al.13 highlighted that the physiologic changes and risks of pregnancy should be taken into account when proning pregnant patients experiencing severe respiratory distress. They noted that although the evidence is limited to case reports and expert experience, pregnant women may be safely placed in a prone position which will relieve both the diaphragmatic compression and aortocaval compression from the gravid uterus. They recommended padding above and below the gravid uterus.
However, the prone position may cause endotracheal obstruction and impaired mucus clearance among intubated patients.14 Additionally, patients in prolonged prone position were seen to have higher risk of pressure, facial, peripheral nerve injuries.14,15
If done correctly however, these risks can be minimized and pregnancy should not be a contraindication to this beneficial therapy. It is a low-cost, low harm intervention in pregnant patients experiencing COVID-induced ARDS. This has led to the development of an algorithm for prone position in awake and intubated pregnant patients.16
The Department of Medicine of the Philippine General Hospital (PGH) adopted a protocol for prone positioning of patients with moderate to severe SARS COVID-19. The indications for prone positioning include severe ARDS and refractory hypoxemia due to ARDS.17 The same protocol is used for pregnant patients. Centers worldwide have adapted various ways of providing prone positioning safely to these cases as a means of improving oxygenation.
Due to the engorged breasts and enlarged abdomen of pregnant patients, placing them on prone position may be uncomfortable without proper support. For intubated pregnant patients, placing them on prone position and inserting standard pillows on the shoulder, below the chest and belly is difficult. There is also a need to monitor uterine contractions and fetal heart tones, and proper positioning of the wires of the fetal electronic monitor is challenging. Unfortunately, there is no available pillow in the market that can accommodate these specifications.
The Philippine Obstetrical and Gynecological Society together with the Philippine Infectious Diseases Society for Obstetrics and Gynecology reported admissions of 948 COVID-19 pregnant patients in 20 institutions since March 2020.18 Four percent presented with moderate to severe COVID 19 infections with 19 patients requiring admission to the Intensive Care Unit. Approximately 7% were undelivered and admitted for medical management. Based on the census from the PGH Department of Obstetrics and Gynecology, 343 COVID-19 positive pregnant patients have been admitted since March 2020, 17 cases for medical management (5%), with one mortality.19
Recognizing the need for such a pillow, the investigators developed a customized pillow with cushioned recesses which conforms to the breast and abdomen. Anthropometric measurements were considered. For sanitation purposes, the pillow was manufactured to be disposable. The first Prone Pillow for Pregnant Patients (4P) prototype 1.0 was evaluated using the Noelle* Maternal and Neonatal Birthing Simulator and adjustments were made.
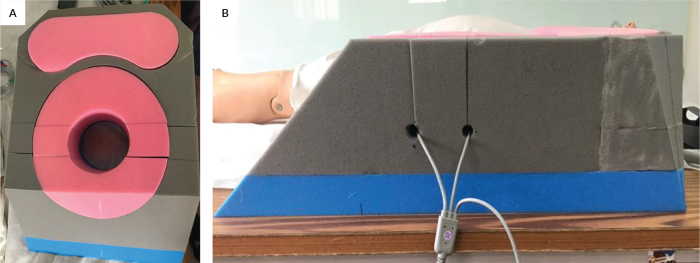
In the second prototype, modifications in both measurements and foam insert design were applied (Figure 1). The foam used were of different densities and varied in hardness. The bottom foam (blue) had the highest density and hardness to prevent it from being deformed. The inserts (pink) were of lighter density and hardness allowing them to conform to a variety of sizes of the breast and gravid uterus since patients may present in different age of gestations. The pillow was designed to provide the needed support on the chest, above and below the abdomen. Cord holes were modified into slits from the top of the pillow to accommodate the cords of the transducers used to monitor fetal heart tones and uterine contractions.
Figure 1.
4P 2.0 Prototype. (A) View from the top: pink dumbbell shape (top) for the breast and circular shape (bottom) for the abdomen which are removable; (B) Side View: shows the top foam using Permasoft gray and firmer bottom foam using Uratex blue and a support foam, Permasoft Pink; wires of the transducers to monitor uterine contractions and fetal heart tones are seen threaded thru the slits.
The second prototype 4P 2.0 underwent evaluation with a volunteer wearing a pregnant belly device with the abdomen approximately 24 weeks in size (Figure 2). This was followed by lying on prone position following the standard protocol. A face pillow was used to support the head.
Figure 2.
Awake volunteer using the 4P 2.0 Prototype.
The wires of the transducers for monitoring uterine contractions and fetal heart tones were threaded thru the slits of the pillow. The pillow was evaluated for comfort and any pressure points were noted. The volunteer found it comfortable and easy to lie prone on the pillow.
Volunteer using a pregnant belly device with the prone pillow and also a face pillow to support her head.
Prototype 4P 2.0 was then evaluated using the Noelle* Maternal and Neonatal Birthing simulator with the same protocol of turning intubated patients to the prone position done in PGH. The protocol uses a manual prone positioning method. Additional steps were added for the application of the transducers for uterine contraction and fetal heart tone monitoring. The corresponding recesses in the pillow were placed on top of the breast and abdomen. Similar to the step for awake patients, the wires of the transducers for monitoring uterine contractions and fetal heart tones were threaded thru the slits of the pillow (Figure 3). Five persons helped in turning Noelle* with one dedicated to the head for support and to keep the endotracheal tube in place. Once on prone, the pillow and the wires were noted to remain in place. The face pillow was used to support the head.
Figure 3.
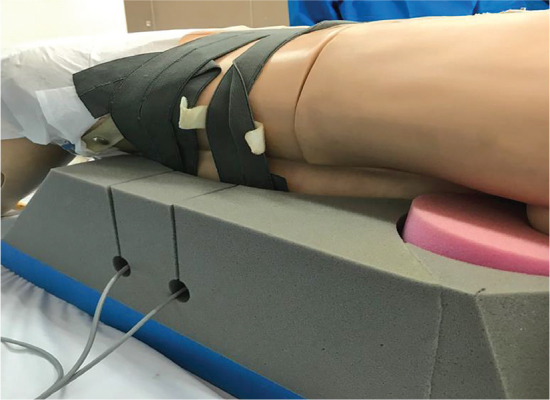
Noelle* Maternal Care Patient simulator using the 4P 2.0 Prototype.
The current study aimed to describe the experience of pregnant COVID patients on the use of the pillow in terms of ease in breathing and comfort/discomfort while on pronation.
METHODS
The study prospectively evaluated the use of the prone pillow for patient comfort and usability with the 4P 2.0 prototype. Questionnaires were given to ascertain patient comfort. Usability was measured by the healthcare workers’ report of ease in assisting awake and sedated or intubated patients to the prone position and in monitoring the aforementioned specific parameters. Quantitative and qualitative data were used to evaluate study outcomes.
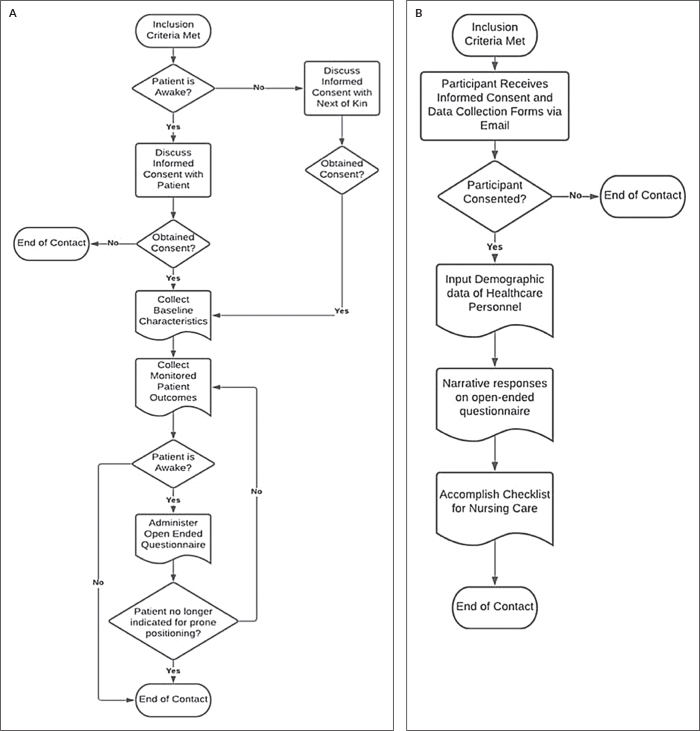
The study participants for this study consisted of COVID-19 confirmed pregnant patients at any age of gestation, and with a medical indication for the prone position: two (2) awake patients and one (1) intubated patient admitted in the PGH in 2021. Informed consent from the awake patients were taken. For the intubated patient, informed consent was obtained from her next of kin. The figures below show the recruitment protocol for pregnant patients who tested positive for SARS-COV-2 infection (Figure 4A) and healthcare workers (Figure 4B).
Figure 4.
Recruitment protocol for pregnant patients who tested positive for SARS-CoV-2 infection (A) and healthcare workers (B).
Pregnant patients participating in the study were hospitalized in the PGH. Indications for prone positioning were severe ARDS and refractory hypoxemia due to ARDS. Consecutive patients were enrolled in the study.
Healthcare personnel assisting pregnant patients with COVID-19 to the prone position included medical doctors, nurses, midwives, and institutional workers. They were trained on the use of the pillow through a simulation workshop and followed a specific protocol. The simulation training workshop will be published in a separate article.
Informed consent were collected prior to participation in the study. In the event that the patient cannot give her consent, the nearest of kin were requested to provide consent on behalf of the patient. Patients, next of kin, and healthcare workers who refused to give their consent were not included in the study. The protocol was approved by the UPM-REB (2020-0796-01) and was registered in the Philippine Health Research Registry: PHRR: 220104-004201. The study was conducted from April 2021 and was completed within the same year. It received partial support through a faculty grant from the PGH and UP SIBOL.
The survey questionnaire was conducted among awake patients and consisted of three parts: six open-ended questions gathering their insights on comfort of the pillow, an adapted patient comfort questionnaire20,21 and a verbal rating scale22 for pain. Patients shared their level of comfort (0 meaning uncomfortable and 4 perfectly comfortable) and pain (with 0 meaning no pain and 4 with very severe pain) in the following six areas: neck, shoulder, chest, waist, hip, and thigh. Filipino translation was available. Awake patients were asked to answer the survey after they lie on prone position using the 4P 2.0 prototype. Intervals of prone positioning were determined through the recommendations of their attending physician. Clinical parameters were monitored and recorded before prone positioning, immediately after prone positioning, hourly intervals while on prone, and after placing the patient on supine position.
A separate questionnaire was given to the healthcare personnel assisting patients to lay prone. The questionnaire was divided into three parts to assess their experience while using the prototype 4P 2.0. The first part contained six open-ended questions aimed at gathering their insights on the usability of the pillow. The second part was a checklist for Nursing care23 and Patient Adverse Events based on prevalence studies of medical device-related pressure injuries.24
Descriptive statistics and measures of central tendency were used as statistical treatment for the included areas in the survey. Answers to the surveys were transcribed by a research assistant. Data were coded according to common responses of participants and the findings were synthesized.
RESULTS
A total of six patients were invited to participate in the study, only one of whom was intubated. One patient withdrew from the study upon having difficulty going into prone position while two recruited awake patients deteriorated and expired before feedback was obtained. Patient 3 was initially intubated however feedback was obtained when her condition improved. Three patients, all multigravids, were included. Two patients were placed on prone position while awake and the third patient was intubated and placed on prone position. All three patients had similar body mass index with the age of gestation from 25 to 30 weeks. Table 1 summarizes the baseline demographics of patients who were included in the study.
Table 1.
Patient Demographics
| Patient 1 (Awake) | Patient 2 (Awake) | Patient 3 (Intubated) | |
|---|---|---|---|
| Age (years) | 31 | 39 | 38 |
| Obstetric score | Gravida 2 Para 1 (1001) | Gravida 3 Para 1 (1011) | Gravida 4 Para 3 (3003) |
| BMI (kg/m 2 ) | 28.4 | 27 | 26.7 |
| Age of gestation (weeks) | 29 1/7 | 25 6/7 | 30 |
| Fundic height (cm) | 26 | 25 | 23 |
| Estimated fetal weight (kg) | 1.2 - 1.4 | 0.6 - 0.8 | 1.2 - 1.4 |
| Co-morbidity | Diabetes, Anemia | None | None |
| Number of times placed in prone position | 2 | 1 | 1 |
| Total duration (hours) | 2 (over 2 days) | 1-2 | 3 |
| PaO2:FiO2 ratio | 187 | 74 | 93 |
There were 15 healthcare workers who assisted the patients to lie on prone position. Participants included 12 medical officers (8 obstetricians, 2 pulmonologists, and 2 anesthesiologists), two nurses, and one midwife. One medical officer assisted an awake and an intubated patient. There were 16 answered questionnaires in all. The participants had an average age of 32.94 (SD ± 7.48), 12 of whom were female, and 10 of them having no previous experience in assisting patients to go on prone position. Half of the participant healthcare workers assisted intubated pregnant patients.
Patient Experience and Outcomes
Awake pregnant patients were asked about their experience while using the pillow. Although Patient 3 was recruited as an intubated patient, feedback was obtained when the patient was extubated. Recruited patients were only able to use the pillow for an hour or less before their primary physician discontinued proning. Patients 1 and 3 noted greater ease in breathing while using the pillow on prone position (“mas maginhawa”) while Patient 2 felt discomfort due to persistent cough. Patients 1 and 2 reported some discomfort due to the warmth of the pillow as well as some pressure on their abdomen while lying down on prone. Patient 3 felt discomfort on her knees and feet due to lack of support. Patient 1 expressed her concerns about her baby while on prone while Patient 2 worried about suffocation.
Patients were also asked to rate their comfort and pain on different areas of the body. Overall, results were mixed on the levels of pain and comfort they felt throughout the process (supine, prone initial, prone after several hours, and post-prone). Patient 1 experienced pain (3 out of 4, 4 most severe) on her chest on supine, prone, and post-prone position. There was no pain noted on any other area. Patient 2 noted discomfort on the neck (1-2 over 4) during prone positioning and this was relieved after proning. She experienced pain (2-3 over 4) on all areas on the supine and prone positions but was comfortable post-proning (no pain, 4 out of 4 in comfort). Patient 3 experienced pain (3 out of 4) on the thighs in the prone position. No data was available prior to and after prone positioning for Patient 3. Figures 5 and 6 show the pregnant patients using the 4P 2.0 prototype.
Figure 5.

Awake pregnant patient using the 4P 2.0 Prototype. Actual patient using the prone pillow and a face pillow to support her body and head. Wires of the transducers for monitoring are seen.
Figure 6.

Intubated pregnant patient using the 4P 2.0 Prototype. Actual patient using the prone pillow and a face pillow to support her body and head. Wires of the transducers for monitoring are seen. This patient was intubated.
Patients’ clinical parameters were also collated among intubated and awake pregnant patients. In all three patients, respiratory rate, oxygen saturation (SpO2), and ROX index improved while on prone position. The ROX index has been used as a predictor of the need to intubate in patients while receiving high flow nasal cannula oxygen therapy. ROX index was not computed for Patient 3 as she was already intubated. No adverse events such as pressure sores were reported by their attending physicians while using the 4P 2.0 prototype. Table 2 shows the respiratory rate, oxygen saturation, HNFO FiO2, and available ROX index of each patient before, during, and after prone positioning.
Table 2.
Summary of Patient Clinical Parameters Before, During and After Prone Positioning
| Patient 1 | Patient 2 | Patient 3 (Intubated) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Before | During | After | Before | During | After | Before | During | After | |
| Respiratory Rate | 30 | 26 | 30 | 32.5 | 29 | 22 | 32.5 | 27.5 | 30 |
| Oxygen Saturation | 94 | 96 | 95 | 88 | 97 | 98 | 92.5 | 96 | 94 |
| HNFO FiO2 | 90 | 90 | 90 | 100 | - | - | 95 | 95 | 95 |
| ROX Index | 3.48 | 4.1 | 3.52 | 2.71 | - | - | - | - | - |
Respiratory Rate is reported as average breaths per minute
Oxygen saturation or SpO2
HNFO FIO2: high flow nasal cannula oxygen fraction of inspired oxygen
ROX index is computed as (SpO2/FiO2)/RR
Patient 1 was discharged well, undelivered at 32 1/7 weeks after 21 days in the hospital. Patient 2 underwent emergency classical cesarean section for non-reassuring fetal status. She died on her 19th hospital day and her baby succumbed to neonatal pneumonia and prematurity on the 22nd day of life. Patient 3 was intubated when the prone pillow was used and was extubated afterwards. However, she rapidly deteriorated on her third hospital day and underwent perimortem cesarean section. Her baby died of respiratory distress syndrome and pneumonia on the 15th day of life.
Healthcare Worker Experience
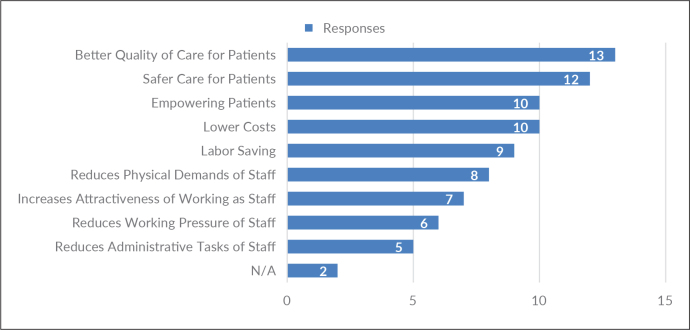
To evaluate the usability of the 4P Prone 2.0 prototype, healthcare workers were asked to answer a questionnaire to describe their experience using the pillow, as well as a checklist on perceived advantages in adapting technologies for nursing care.23 Figure 7 summarizes the responses of healthcare workers in the checklist.
Figure 7.
Checklist for nursing care responses.
The top responses of the participants indicate that the 4P 2.0 prototype provides better quality of care for patients, safer care for patients, empowers patients, and lowers cost of care by reducing the need for invasive ventilation. They stated that it is labor saving as such it saves effort and time, and reduces the physical demands on the staff.
Assisting Awake Patients
Healthcare workers assisting patients in prone positioning generally found the process easier when using the 4P 2.0 prototype especially when assisting awake pregnant patients. Almost all participants found the pillow to be useful even for intubated patients. Participants also reported that they were mostly confident in the process of assisting patients, however, there were some hesitations if they were the only one to assist. More participants who assisted awake pregnant patients perceived the prone pillow to be advantageous in saving labor and lowering the cost of care.
Despite the advantages of using the 4P 2.0 prototype in assisting awake pregnant patients, participants expressed concerns and challenges in monitoring their patient while on prone position. Particularly, participants reported difficulty in monitoring blood pressure, oxygen saturation, and fetal heart tones. There were also some concerns on not being able to see the expression of the patient’s face while they were on prone especially when they were dyspneic.
Assisting Intubated Patients
When the healthcare workers were assisting an intubated patient in prone positioning, participants noted the need for several personnel to assist the patient despite the use of the 4P Prone Pillow. All participants perceived the pillow to be useful in prone positioning of pregnant patients as well as in their monitoring and accommodation of ventilation equipment.
Similar to those assisting awake pregnant patients, healthcare workers assisting intubated patients had concerns on their ability to monitor the patient while on prone particularly with the electronic fetal monitor transducer. However, a unique concern expressed by those assisting intubated patients involved the possible inadvertent removal of the endotracheal tube or self-extubation. There were also concerns on the pillow’s reusability and or disinfection protocol. Some improvements were suggested that can be incorporated into future iterations of the pillow.
DISCUSSION
Patient outcomes observed in the study are similar to those of previous research8-17 wherein lying down on prone position improves oxygenation, and lowers heart and respiratory rates. Although the evidence is limited, initial reports show better maternal and neonatal outcomes after prone positioning. No adverse events were also reported throughout the use of the 4P 2.0 prototype despite pressure ulcers being a common adverse effect of prone positioning.15 Other adverse effects of long-term use14,15,25,26 were also not observed as patients only stayed in the prone position for one hour at a time.
The results of the study noted some improvement in patient comfort while on prone with the use of the 4P 2.0 prototype. It is difficult to compare the experience from proning with the use of ordinary pillows versus the use of the 4P 2.0 prototype due to the patients’ condition. Overall, awake pregnant patients reported that the pillow or the prone position helped them breathe better, despite some discomfort in the chest and abdominal areas due to the warmth of the pillow while lying on prone.
Healthcare workers assisting awake and intubated pregnant patients noted the pillow to be useful in increasing quality of care and patient safety across the two types of patients. They noted that the use of the 4P 2.0 prototype required less patient assistance and physical demands from the staff. It is beneficial to decrease the number of personnel needed to position a patient to prone not only due to staffing concerns but to decrease the exposure risk to COVID-19. The decrease in demands from the staff will also lessen possible physical injury from strains. Thus, the use of the 4P 2.0 prototype improves safety of both patient and healthcare worker. This is especially useful in low resource settings where manual methods of prone positioning are performed and lift equipment is not available.
It is recommended to check the transducers for monitoring of fetal heart tones and uterine contractions after prone positioning since these may be displaced. Additional support below the knee may be included in the future. The pillow must be properly disposed after use and should be disposed as infectious waste. It is also recommended that each hospital create prone-positioning teams who can evaluate patient eligibility and safely assist patients to the prone position either awake or intubated. The team must undergo standardized interprofessional simulation-based training for prone positioning. The use of the 4P may be included in future training workshops as part of capacity building.
CONCLUSION
The current study described the 4P prototype 2.0 and its perceived comfort among patients and usability among healthcare workers assisting them to the prone position. The 4P prototype 2.0 shows potential for better and safer patient and healthcare worker safety as shown by their positive feedback with the use of the pillow.
It is recommended for future iterations of the 4P 2.0 prototype and the prone positioning protocol to address concerns on the stability of the monitoring equipment especially for fetal heart tones, as well as the prevention of the inadvertent removal of the endotracheal tube. It would also be useful to investigate the comfort and usability of the 4P prototype 2.0 in non-pregnant patients with similar concerns such as those with abdominal obesity and patients with non-COVID-19-related ARDS. As this study has a limited number of participants, it is also recommended for the study to be scaled up to a clinical trial to determine effectiveness in improving patient and healthcare worker safety.
Acknowledgments
The authors would like to thank Ms. Jael C. Gonzales for her services as research assistant, Dr. Koleen Pasamba for her assistance in data collection in the COVID-19 ward, Mr. Carlos Diego A. Rozul for his technical writing services, and Mr. Dindo Medina of Multiflex RNC Philippines, Inc. (MRPI) for fabricating the prototypes.
Statement of Authorship
All authors certified fulfillment of ICMJE authorship criteria.
Author Disclosure
All authors declared no conflicts of interest.
REFERENCES
- 1.Cucinotta D, Vanelli M. WHO Declares COVID-19 a pandemic. Acta Biomed. 2020. Mar 19;91(1):157-60. doi: 10.23750/abm.v91i1.9397. PMID: 32191675; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CoronaTracker [Internet]. October 31, 2022. [cited 2022 Oct 21]. Available from: https://www.coronatracker.com/analytics
- 3.Department of Health . COVID-19 Tracker [Internet]. October 31, 2020. [cited 2022 Oct 21]. Available from: https://www.doh.gov.ph/covid19tracker.
- 4.Fan E, Beitler JR, Brochard L, Calfee CS, Ferguson ND, Slutsky AS, et al. COVID-19-associated acute respiratory distress syndrome: is a different approach to management warranted? Lancet Respir Med. 2020. Aug;8(8):816-21. doi: 10.1016/S2213-2600(20)30304-0. PMID: 32645311; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meftahi N, Bervis S, Taghizadeh S, Ghafarinejad F. The effect of lying in prone position on blood pressure and heart rate with and without massage. J Rehab Sci Res. 2014;1(2):40-3. [Google Scholar]
- 6.Oliveira C, Lopes MAB, Rodrigues AS, Zugaib M, Francisco RPV. Influence of the prone position on a stretcher for pregnant women on maternal and fetal hemodynamic parameters and comfort in pregnancy. Clinics (Sao Paulo). 2017. Jun;72(6):325-32. doi: 10.6061/clinics/2017(06)01. PMID: 28658431; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Douglas WW, Rehder K, Beynen FM, Sessler AD, Marsh HM. Improved oxygenation in patients with acute respiratory failure: the prone position. Am Rev Respir Dis. 1977. Apr;115(4):559-66. doi: 10.1164/arrd.1977.115.4.559. PMID: 322557. [DOI] [PubMed] [Google Scholar]
- 8.Pelosi P, Tubiolo D, Mascheroni D, Vicardi P, Crotti S, Valenza F, et al. Effects of the prone position on respiratory mechanics and gas exchange during acute lung injury. Am J Respir Crit Care Med. 1998. Feb;157(2):387-93. doi: 10.1164/ajrccm.157.2.97-04023. PMID: 9476848. [DOI] [PubMed] [Google Scholar]
- 9.Nyrén S, Radell P, Lindahl SGE, Mure M, Peterson J, Larsson SA, et al. Lung ventilation and perfusion in prone and supine postures with reference to anesthetized and mechanically ventilated healthy volunteers. Anesthesiology. 2010. Mar;112(3):682-7. doi: 10.1097/ALN.0b013e3181cf40c8. PMID: 20179506. [DOI] [PubMed] [Google Scholar]
- 10.Coppo A, Bellani G, Winterton D, Di Pierro M, Soria A, Faverio P, et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med. 2020. Aug;8(8):765-74. doi: 10.1016/S2213-2600(20)30268-X. PMID: 32569585; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu Q, Wang T, Qin X, Jie Y, Zha L, Lu W. Early awake prone position combined with high-flow nasal oxygen therapy in severe COVID-19: a case series. Crit Care. 2020. May 24;24(1):250. doi: 10.1186/s13054-020-02991-7. PMID: 32448330; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Samanta S, Samanta S, Wig J, Baronia AK. How safe is the prone position in acute respiratory distress syndrome at late pregnancy? Am J Emerg Med. 2014. Jun;32(6):687.e1-3. doi: 10.1016/j.ajem.2013.12.021. PMID: 24412021. [DOI] [PubMed] [Google Scholar]
- 13.Tolcher MC, McKinney JR, Eppes CS, Muigai D, Shamshirsaz A, Guntupalli KK, et al. Prone positioning for pregnant women with hypoxemia due to Coronavirus Disease 2019 (COVID-19). Obstet Gynecol. 2020. Aug;136(2):259-61. doi: 10.1097/AOG.0000000000004012. PMID: 32516274. [DOI] [PubMed] [Google Scholar]
- 14.Le MQ, Rosales R, Shapiro LT, Huang LY. The down side of prone positioning: the case of a Coronavirus 2019 survivor. Am J Physl Med Rehabil. 2020. Oct;99(10):870-872. doi: 10.1097/PHM.0000000000001530. PMID: 32657818; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moore Z, Patton D, Avsar P, McEvoy NL, Curley G, Budri A, et al. Prevention of pressure ulcers among individuals cared for in the prone position: lessons for the COVID-19 emergency. J Wound Care. 2020. Jun 2;29(6):312-20. doi: 10.12968/jowc.2020.29.6.312. PMID: 32530776. [DOI] [PubMed] [Google Scholar]
- 16.Oxford-Horrey C, Savage M, Prabhu M, Abramovitz S, Griffin K, LaFond E, et al. Putting it all together: clinical considerations in the care of critically ill obstetric patients with COVID-19. Am J Perinatol. 2020. Aug;37(10):1044-51. doi: 10.1055/s-0040-1713121. PMID: 32575140; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al.; PROSEVA Study Group . Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013. Jun 6;368(23):2159-68. doi: 10.1056/NEJMoa1214103. PMID: 23688302. [DOI] [PubMed] [Google Scholar]
- 18.Mesa E. Philippine Data: POGS-PIDSOG COVID Registry in Pregnancy. Paper presented at: Philippine Obstetrical and Gynecological Society Pre-Conference Webinar. Manila, Philippines. 2020 October 28. [Google Scholar]
- 19.Bravo S. COVID-19 Census of the Department of Obstetrics and Gynecology, Philippine General Hospital as of October 2020.
- 20.Erfanian P, Hagino CC, Guerriero RC. A preliminary study assessing adverse effects of a semi-customized cervical pillow on asymptomatic adults. J Can Chiropr Assoc. 1998. Sep;42(3):156-62. PMCID: . [PMC free article] [PubMed] [Google Scholar]
- 21.Gordon SJ, Grimmer-Somers K, Trott P. Pillow use: the behaviour of cervical pain, sleep quality and pillow comfort in side sleepers. Man Ther. 2009. Dec;14(6):671-8. doi: 10.1016/j.math.2009.02.006. PMID: 19427257. [DOI] [PubMed] [Google Scholar]
- 22.The British Pain Society . Outcome Measures [Internet]. 2019. January [cited 2020 Oct 31]. Available from: https://www.britishpainsociety.org/static/uploads/resources/files/Outcome_Measures_January_2019.pdf
- 23.de Veer AJE, Fleuren MAH, Bekkema N, Francke AL. Successful implementation of new technologies in nursing care: a questionnaire survey of nurse-users. BMC Med Inform Decis Mak. 2011. Oct 27;11:67. doi: 10.1186/1472-6947-11-67. PMID: 22032728; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kayser SA, VanGilder CA, Ayello EA, Lachenbruch C. Prevalence and analysis of medical device-related pressure injuries: Results from the International Pressure Ulcer Prevalence Survey. Adv Skin Wound Care. 2018. Jun;31(6):276-85. doi: 10.1097/01.ASW.0000532475.11971.aa. PMID: 29782417; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martel T, Orgill DP. Medical device-related pressure injuries during the COVID-19 pandemic. J Wound Ostomy Continence Nurs. 2020. Sep/Oct;47(5):430-4. doi: 10.1097/WON.0000000000000689. PMID: 32868735; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simpson AI, Vaghela KR, Brown H, Adams K, Sinisi M, Fox M, et al. Reducing the risk and impact of brachial plexus injury sustained from prone positioning - a clinical commentary. J Intensive Care Med. 2020. Dec;35(12):1576-82. doi: 10.1177/0885066620954787. PMID: 32959717. [DOI] [PubMed] [Google Scholar]