Abstract
Objectives
To investigate the amount of Leisure-Time Physical Activity (LTPA) that people over 45 years with a spinal cord injury (SCI) performed and to determine the frequency, duration, intensity, and modality of LTPA performed.
Data Sources
We searched 5 major electronic databases (CINAHL, SCOPUS, EMBASE, MEDLINE, and PubMed) from inception to March 2023.
Study Selection
Cross-sectional, longitudinal studies and control arm of controlled trials that assessed LTPA in participants over 45 years old, with a SCI. We included 19 studies in the review and 11 in the meta-analysis.
Data Extraction
We followed the PRISMA checklist for Systematic Reviews. Two review authors independently assessed the risk of bias and extracted data on participants’ demographics, injury characteristics, and LTPA participation of the included studies. Risk of bias was assessed using the Joanne Briggs Institute critical appraisal tool for cross-sectional studies. Any conflicts were resolved by a third author.
Data Synthesis
We found considerable variability in LTPA participation in adults 45 years and older with SCI. An estimated 27%-64% of participants did not take part in any LTPA. A random effects meta-analysis model was completed for studies that reported total or moderate-to-heavy LTPA scores in minutes per week. Overall, participants (n=1675) engaged in 260 [205;329] (mean [95% CI]) mins/week of total LTPA. Those participating in moderate-heavy intensity LTPA (n=364) completed 173 [118; 255] (mean [95% CI]) mins/week. LTPA modalities included walking, wheeling, hand-cycling, basketball, and swimming, among others.
Conclusions
While many older adults with SCI seem to be meeting the recommended weekly physical activity volume, many still remain sedentary. There was significant variation in reporting of frequency, intensity, and duration of LTPA and reporting on modality was limited. Because of differences in reporting, it was challenging to compare results across studies. Data constraints prevented subgroup analysis of LTPA disparities between paraplegia and tetraplegia.
Keywords: Leisure-Time Physical Activity, Middle age, Older age, Rehabilitation, Spinal cord injury
Spinal cord injuries (SCI) often result in significant motor and sensory impairments, autonomic dysfunction, and severe mobility restrictions1 which increases the risk of developing secondary health conditions, such as cardiovascular diseases and metabolic syndrome.2, 3, 4, 5 Because of medical advances in the past few decades, more people are surviving after SCI and therefore, are aging with the condition.6, 7, 8 Aging with SCI brings greater risks for the development of metabolic and cardiovascular diseases when compared with the population aging without a SCI.9 In addition, people with SCI compared with non-injured people are 5% more likely to develop anxiety, 20% more likely to develop depression, and 15% more likely to develop psychological issues.10
Regular physical activity in middle/older-aged adults with SCI can improve mobility and quality of life.11 Middle- or older-aged adults with SCI have among the lowest levels of physical activity and energy expenditure compared with other disability groups12 due, in part, to the many biopsychosocial barriers preventing access exercise and physical activity.13 The Canadian Physical activity guidelines for people with SCI guidelines recommend that adults with a SCI should participate in at least 30 minutes of moderate-to-heavy aerobic exercise 2 times per week, and perform at least 3 sets of resistance training exercises for the major functioning muscle groups.14 Similarly, the World Health Organization (WHO) 2020 physical activity guidelines recommend that adults living with a disability perform at least 75-100 minutes of vigorous intensity exercise per week, or 150-300 minutes of moderate intensity aerobic exercise per week, and moderate-to-heavy strength training of major muscle groups 2 times per week.15 Approximately 47% of the people living with a SCI currently do not meet those reccomendations,16 particularly middle/older-aged adults.16, 17, 18 Common barriers to meet physical activity recommendations include reduced access to exercise facilities, pain, mobility restrictions, and need of assistance to exercise and self-care.19,20
Leisure-Time Physical Activity (LTPA) is recreational physical activity including walking, self-propelling a wheelchair, gardening, playing sport, attending the gym, or any other recreational exercise.21 LTPA is performed in people's spare time and presents as an opportunity to increase daily physical activity participation. Previous research has shown that older age is associated with lower LTPA participation in people with SCI,22,23 as is true with the general population.24 The Swedish Aging with Spinal Cord Injury Study (SASCIS) showed that older people living in the community frequently suffer from co-morbidities that could be prevented by regular exercise and physical activity.4,17,25 The SASCIS also revealed that older people with a SCI (>50 years and at least 10 years since injury) did not participate in the intensity or volume of physical activity required to achieve health benefits.4,17 Furthermore, it showed that age and wheelchair use were predictors of low levels of engagement in physical activity.17 This highlights the importance of embedding LTPA in daily lives of people with SCI as early as possible. There is a lot of research on participation in LTPA in the general SCI population, however, less is known about the participation and volume of LTPA in middle/older-aged adults with SCI.
This review aims to (1) investigate the amount of LTPA performed by middle/older-aged adults (≥45 years) with SCI and (2) determine the frequency, duration, intensity, and modality of LTPA performed by middle/older-aged adults with SCI.
Methods
This study is a systematic review with meta-analysis. The Cochrane Handbook recommendations26 and the Preferred Items for Systematic Reviews and Meta-Analysis (PRISMA) reporting guidelines27 were followed. The protocol for this review was prospectively registered with the International Prospective Register of Systematic Reviews (PROSPERO, Identifier CRD42022311618).
Literature search
The search was conducted in CINAHL, SCOPUS, PubMed, MEDLINE (Ovid), and EMBASE (Ovid) databases from inception of the databases to March 2023. We did not restrict our search by date or language. Conference abstracts and proceedings were excluded. Reference lists of included studies were also checked for potentially relevant studies. An information specialist was consulted to assist with developing the search strategy. The search strategy included synonyms for “leisure-time physical activity” and “spinal cord injury” (see appendix 1).
Study selection
We used Covidence software28 to perform title/abstract screening, full-text screening, and data extraction. Selection of studies was performed by 2 review authors (a combination of L.S., C.Q.O., E.R., and P.S.) independently. Any disagreements were discussed and if agreement could not be achieved, a third review author (A.V.) was consulted for a final decision.
Eligibility criteria
Study design
Cross-sectional studies, longitudinal studies, or randomized controlled trials where baseline data on LTPA participation were available.
Participants
We included data from individuals aged ≥45 years, based on multiple large longitudinal studies in the aging population that used the age of 45 as the threshold to define middle/older-aged people.29, 30, 31 Studies were included if participants had a SCI, were ≥45 years old and were community-dwelling, when data for participants ≥45 years were presented separately or when authors could provide separate data when contacted. Included participants had a SCI of any cause (traumatic or non-traumatic) and any severity of injury or level of injury as classified by the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) score. Studies including participants with multiple conditions were included if data from individuals with SCI were reported separately or if more than 75% of the sample contained individuals with SCI. When studies were unclear whether participants with SCI or aged ≥45 years were included or analyzed separately, we contacted the authors for additional data. Authors were contacted via email for data twice over a 3-week period. If authors were unresponsive, the study was excluded. Studies with individuals with SCI of all ages were excluded if the sample size of people aged ≥45 was less than 10 participants. Other excluded studies were animal studies, case control studies, and randomized controlled trials where the sample was composed solely of participants that were non-exercisers.
Outcomes
The primary outcome was LTPA levels measured via self-reported diaries or valid questionnaires, such as the Physical Activity Scale for Individuals with Physical Disability (PASIPD), the Physical Activity Recall Assessment for People with Spinal Cord Injury (PARA-SCI), or the Leisure-Time Physical Activity Question for people with Spinal Cord Injuries (LTPAQ-SCI). Studies that used accelerometers or other questionnaires, and scales to assess physical activity participation, were also included. Secondary outcomes were intensity (recall assessments, Borg rating of perceived exertion scale or wearable monitors), duration, frequency, and modality of LTPA that could be measured using the above tools.
Data extraction
Two of the review authors (L.S./C.Q.O./P.S./E.R.) independently extracted data using a standardized data extraction form. The following information was extracted for each study: first author, year of publication, study design, aim, setting, duration of study (when applicable), sample size, mean age, injury characteristics (injury level, time since injury, paraplegia/tetraplegia, INSCSCI score, complete/incomplete injury), details of LTPA outcomes (eg, frequency, intensity, duration, and modality of LTPA) where available; and the proportion of participants engaging in LTPA. For studies with 2 reported time points, we used the longest time point post injury to better reflect the physical activity behaviors of people living in the community for longer. If studies reported being affected by COVID, we used pre-COVID measures only, as COVID may have affected the participant's ability to engage in LTPA.
Risk of bias assessment
The risk of bias of the included studies was assessed using the Joanna Briggs Institute (JBI) critical appraisal for cross-sectional studies32,33 (appendix 2). The JBI has 8 items and provided a score (Yes, No, Unclear) for each item. Item 7 was not applicable for this review because it assesses the validity and reliability of “outcomes”, and this review only assessed the exposure to LTPA and not LTPA as an outcome. The JBI recommends that each item is reported separately without providing a summed score.32 The JBI was used for longitudinal studies and clinical trials as only 1 cross-sectional time point was included in the review. Two review authors (L.S./C.Q.O./P.S./E.R.) independently conducted the risk of bias assessment. Any disagreements were discussed and if agreement could not be achieved, a third review author (A.V.) was consulted to make the final decision.
Synthesis methods
A meta-analysis was completed for all studies that reported total or moderate-to-heavy LTPA scores in minutes per week. Individual studies were pooled by outcome measure used and were combined in the meta-analysis. For studies that used the PASIPD tool, a separate meta-analysis was performed as this tool reports LTPA in metabolic equivalent of task (MET) hours per day and not minutes per week. PASIPD “total scores” and “recreation scores” were included in a separate meta-analysis, as total PASIPD scores encompass recreational, household, and occupational physical activities, which is more than only LTPA while the PASIPD “recreation scores” more closely align to our definition of LTPA. Data were obtained in text or requested from authors. Self-report tools that reported in minutes per day were converted to minutes per week for consistency in the meta-analysis.
The meta-analysis was completed in R34,a using the “meta” package. Inverse variance weights were performed on log transformed values from the systematic review and back-transformed after a random-effects meta-analysis. Results (mean, pooled means, and 95% CI) were displayed in a forest plot. Heterogeneity was assessed using the I2 and τ2 statistics.
Results
Study selection
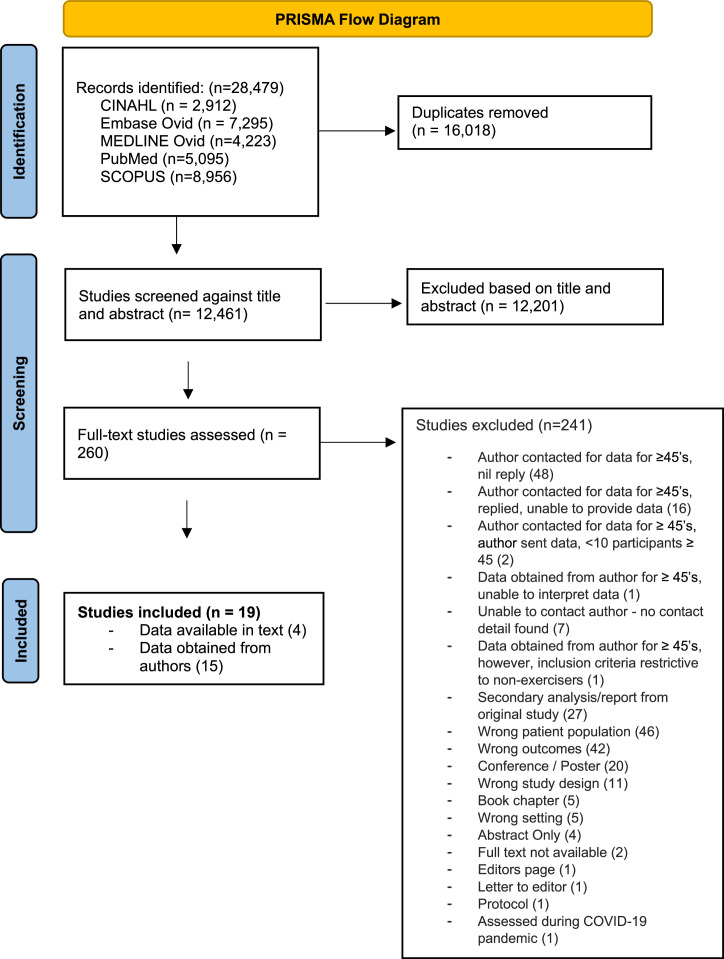
We screened 11,728 titles and abstracts of studies and assessed 117 full texts (fig 1). Once secondary reports from original studies were excluded,26 80 authors were contacted for data for participants ≥45years. Seventeen authors provided the requested data, however, the data for 2 studies were unclear and excluded. In total, 19 studies were included in this review, and 11 studies were included in the meta-analysis. From the 15 studies that include participants of all ages, the proportion participants aged ≥45 years old ranged from 18% to 85%. Only 4 studies provided data in the report for participants ≥45 years.
Fig 1.
PRISMA flow diagram.
Characteristics of included studies
Study design
Fifteen cross-sectional studies,4,16, 17, 18,23, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44 2 longitudinal,45,46 and 2 clinical trials were included.47,48 For the clinical trials, only baseline LTPA data were obtained. One longitudinal study (n=29, ≥45 years) reported levels of LTPA at 2 different data points, 6 months and 12 months post-hospital discharge,46 so the latest timepoint (12 months) was chosen. Another longitudinal study reported levels of LTPA at 2 different timepoints, pre-COVID and during COVID,45 so the pre-COVID timepoint was used. The studies were performed in Europe, Asia, South and North Americas (table 1). Only 2 studies came from low-income countries.37,41
Table 1.
Summary table of participants ≥45 years old
| Author, Year, and Study Design | Country | Number of Participants | Number of Participants ≥45 years | Age (Mean years ± SD) | Paraplegia/Tetraplegia (%) | Complete/Incomplete (%) | Time Since Injury (Mean years ± SD) | ISNCSCI Classification (%) |
|---|---|---|---|---|---|---|---|---|
| Blauwet, 2013 Cross-sectional study |
United States | 149 | 104 | 55.11±5.69 | 47.12/52.88 | N/R | 22.39±12.35 | A - 50.96 B – 0 C – 8.65 D – 42 |
| Connell, 2023 Cross-sectional study |
Canada | 98 | 18 | 56.06±6.58 | 55.56/44.44 | N/R | N/R | N/R |
| de Groot, 2016 Cross-sectional study |
Netherlands | 223 | 157 | 53.78±6.07 | 46.5/52.2 /1.3* | 66.7/33.3 | 28.61±8.08 | A –66.7 B – 12.8 C – 8.3 D – 12.2 0.6* |
| de Oliveira, 2016 Clinical trial |
Australia | 64 | 39 | 57±8.63 | 53.85/46.14 | 35.90/64.10 | 14.00±14.01 | N/R |
| Eitivipart, 2021 Cross-sectional study |
Thailand | 200 | 44 | 51.49±5.91 | 63.64/36.36 | 70.45/29.55 | 22.50±15.49 | A – 50.96 B – 0 C – 8.65 D – 40.38 |
| Hansen, 2021 Cross-sectional study |
Denmark | 181 MWCUs | 69 SCI | 58±8.17 | 70/20/10* | 46/51/3* | N/R | N/R |
| Jorgensen, 2017 Cross-sectional study |
Sweden | 119 | 119 | 63.5±8.7 | N/R | N/R | N/R | Tetraplegia AIS A–C: 18 Paraplegia AIS A–C: 33 All AIS D: 50 |
| Koutrakis, 2019 Cross-sectional study |
United States | 174 | 174 | 57±12.4 | N/R | N/R | N/R | Cervical motor complete & ISNCSCI C: 23; Other motor complete & ISNCSCI C: 37.4 All ISNCSCI D: 39.7 |
| Lundstrom, 2017 Cross-sectional study |
Sweden | 73 | 73 | 63.7±9.4 | N/R | N/R | 36.3±9.2 | A – 56.2 B – 6.9 C – 16.4 D – 20.5 |
| Marco-Ahullo, 2021 Longitudinal study |
Spain | 20 | 13 | 52.15±6.61 | 100/0 | N/R | 19.69±10.5 | N/R |
| Matsuda, 2020 Cross-sectional study |
United States | 1812 (total), 414 (SCI) | 305 (SCI) | 59.85±9.35 | 50/50 | 41/52/7* | 21.1±21.02 | N/R |
| Myers, 2012 Clinical trial |
United States | 26 | 26 | 56.92±5.74 | N/R | 23.8±12.3 | Tetraplegia, ISNCSCI A & B - 34.6 Tetraplegia, ISNCSCI C – 0 Paraplegia, ISNCSCI A & B – 30.8 Paraplegia, ISNCSCI C – 15.4 ISNCSCI D – 19.2 |
|
| Neto, 2021 Cross-sectional study |
Brazil | 108 | 23 | 53.4±7.33 | 100/0 | 100/0 | 15.60±16.04 | N/R |
| Postma, 2020 Longitudinal study |
Netherlands | 38 | 29 | 59±9.87 | 48.6/51.4 | 0/100 | N/R | A – 0 B – 0 C – 5.4 D – 94.6 |
| Rauch, 2014 Cross-sectional study |
Switzerland | 505 | 336 | 56.37±9.04 | 72.67/26.43/0.90* | 46.85/52.55/2.10* | 21.97±12.19 | N/R |
| Rauch, 2016 Cross-sectional study |
Switzerland | 485 | 277 (>51 y/o) |
* Mean age for whole sample 52.9±14.8 |
Whole sample: C para: 32.9 IC para: 35 C tetra: 11.4 IC tetra: 20.7 |
Whole sample: 17.3±12.9 | N/R | |
| Rocchi, 2017 Cross-sectional study |
Canada | 73 | 55 | 58.44±7.77 | 63/37 | N/R | 22.58±13.84 | A – 42.60 B – 11.10 C – 18.50 D – 25.90 E – 1.90 |
| Santino, 2021 Cross-sectional study |
Canada | 170 | 144 | 63.53±10.27 | 46.9/53.1 | N/R | 24.43±10.27 | A – 41.00 B – 9.70 C – 4.20 D – 37.50 7.6* |
| Watson, 2022 Cross-sectional study |
Australia | 1579 | 1281 | 62.67±10.09 | 57.8/35.8/6* | 30.1/63.5/6.4* | 18.67±14.76 | N/R |
Abbreviations: C, complete; IC, incomplete, N/R, not reported; MWCU, Manual Wheelchair User.
Unknown/missing data.
Participants
Overall, 1987 participants aged over 45 years were included in this review. The injury characteristics are described in table 1. The sample sizes of participants ranged from 13 to 336. The mean age range of participants was from 51.5 to 63.5 years. The mean time since injury ranged from 16 to 36 years. The proportion of participants with paraplegia ranged from 47% to 100%, and 0% to 53% for tetraplegia.
Risk of bias
Of the 19 included studies, 84% and 94% of studies met questions 1 (Were the criteria for inclusion in the sample clearly defined?) and 2 (Were the study subjects and the setting described in detail?), respectively. Sixty three percent and 74% of studies met question 3 (Was the exposure measured in a valid and reliable way?) and 4 (Were objective, standard criteria used for measurement of the condition?), respectively. Fifty percent to 56% of studies met questions 5, 6, and 8 (Were confounding factors identified? Were strategies to deal with confounding factors stated? Was appropriate statistical analysis used?) (table 2).
Table 2.
Risk of bias assessment
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 |
|---|---|---|---|---|---|---|---|---|
| Blauwet, 2013 | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | N/A | U |
| Connell, 2023 | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | N/A | ✓ |
| de Groot, 2016 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ |
| de Oliveira, 2016 | ✓ | ✓ | ✓ | ✓ | N/A | N/A | N/A | N/A |
| Eitivipart, 2021 | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | N/A | ✗ |
| Hansen, 2021 | ✗ | ✓ | ✗ | ✗ | U | ✓ | N/A | ✓ |
| Jorgensen, 2017 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ |
| Koutrakis, 2019 | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | N/A | ✓ |
| Lundstrom, 2017 | ✓ | ✓ | ✓ | ✓ | N/A | N/A | N/A | ✓ |
| Marco-Ahullo, 2021 | ✗ | ✗ | ✓ | ✓ | ✗ | ✗ | N/A | ✗ |
| Matsuda, 2020 | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | N/A | ✓ |
| Myers, 2012 | ✓ | ✓ | ✓ | ✓ | N/A | N/A | N/A | N/A |
| Neto, 2021 | ✓ | ✓ | ✗ | ✓ | ✗ | ✗ | N/A | ✗ |
| Postma, 2020 | ✓ | ✓ | ✓ | ✓ | U | U | N/A | ✗ |
| Rauch, 2014 | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | N/A | ✓ |
| Rauch, 2016 | ✗ | ✓ | ✓ | ✓ | U | U | N/A | U |
| Rocchi, 2017 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ |
| Santino, 2021 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ |
| Watson, 2022 | ✓ | ✓ | ✗ | ✗ | ✗ | U | N/A | U |
NOTE. Q1. Were the criteria for inclusion in the sample clearly defined? Q2. Were the study subjects and the setting described in detail? Q3. Was the exposure measured in a valid and reliable way? Q4. Were objective, standard criteria used for measurement of the condition? Q5. Were confounding factors identified? Q6. Were strategies to deal with confounding factors stated? Q7. Were the outcomes measured in a valid and reliable way? Q8. Was appropriate statistical analysis used?
Risk of bias assessed using the Joanna Briggs Institute critical appraisal checklist for analytical cross-sectional studies.
Abbreviations: ✓, yes; ✗, no; U, unclear; N/A, not applicable.
Exposure
The outcomes used to measure the exposure (LTPA participation) are outlined in table 3. Four studies used the PASIPD, 2 studies used the LTPAQ-SCI, 1 study used the Godin Leisure-Time Exercise Questionnaire, 3 studies used the PARA-SCI, 1 study used the Participation Survey of Mobility Limited People version 3 (PARTS/M-v3) outcome measure (where we extracted the “active recreation” data), 5 studies used non-validated self-report measures, and 1 study used an accelerometer to measure time spent on LTPA.
Table 3.
LTPA participation for participants ≥45 years
| Author, Year, and Study Design | Outcome Measure | LTPA Participation (Mean ± SD Unless Stated Otherwise) | Mod-heavy LTPA Participation (Mean ± SD Unless Stated Otherwise) | Participation in Sports (%) | LTPA Modality | Participation in NO LTPA (%) |
|---|---|---|---|---|---|---|
| Blauwet, 2013 Cross-sectional study |
Nil validated OCM Participants asked: “Do you participate in any organized sports?” and to list the type of sport. |
N/R | N/R | 20.2 | Basketball, bowling, tennis, racquetball, fishing, swimming, canoeing, skiing, road racing, coach football, curling, sailing, golf, rowing, hand cycling, hunting, martial arts, rowing, wheelchair softball | N/R |
| Connell, 2023 Cross-sectional study |
PARA-SCI (mins/week) | 283±596 | 91±113 | N/R | N/R | N/R |
| de Groot, 2016 Cross-sectional study |
PASIPD (MET h/week) | 16.7±17.1 | N/R | N/R | N/R | N/R |
| de Oliveira, 2016 Clinical trial |
PARA-SCI (mins/day) | Mild LTPA 10±26 Moderate LTPA 14±26 Heavy LTPA 21±53 Total LTPA score: 45±54 |
Moderate LTPA 14±26 Heavy LTPA 21±53 Total moderate-heavy LTPA: 36±51 |
N/R | N/R | 27 |
| Eitivipart, 2021 Cross-sectional study |
Thai PARA-SCI (mins/day) (mins/week) Engaging in Strengthening Exercise or Aerobic Exercise >20 min: |
Mild LTPA 4±18 Moderate LTPA 12±25 Heavy LTPA 6±13 Total LTPA: 158±251 61.4% do not engaging in strengthening Exercise and Aerobic Exercise 18.2% engage in strengthening exercise only 13.6% engage in aerobic exercise only 6.8% engage in both strength and aerobic exercise |
Moderate LTPA 12± 25 Heavy LTPA 6±13 Total moderate-to-heavy LTPA: 127±215 |
N/R | N/R | Total LTPA: Age 46-60: 50 Age 61-75: 64 Moderate-to-heavy LTPA: Age 46-60: 50 Age 61-75: 56 |
| Hansen 2021 Cross-sectional study |
Self-reported PAL on a 10-point scale (1=not being physically active at all; 10=extremely physically active)† | Low PAL n=19 (27.5%) Medium PAL n=37 (53.6%) High PAL n=13 (18.8%) Mean: 5.8±2.0 |
N/R | N/R | N/R | N/R |
| Jorgensen, 2017 Cross-sectional study |
PARA-SCI (mins/week) | 243±291 | 158±246 | N/R | N/R | 29 |
| Koutrakis, 2019 Cross-sectional study |
Self-report (no validated questionnaire) (mins/week) | 360±324 | N/R | N/R | N/R | N/R |
| Lundstrom, 2017 Cross-sectional study |
PARTS/M-v3 Participation in “Active recreation” |
N/R | N/R | 58% for participants with TSI 20-30 years 23% for participants with TSI of 36-55 years |
N/R | N/R |
| Marco-Ahullo, 2021 Longitudinal study |
PASIPD (MET h/week) | Total: 21.5±12.3 Recreation: 15.5±11.8 |
N/R | N/R | N/R | N/R |
| Matsuda, 2020 Cross-sectional study |
GLTEQ – modified* (Total Activity Score) | Leisure score: Mild days/week: 3±2.8 Mod days/week: 2±2.5 Strong days/week: 1±1.7 Weekly leisure score: 25 |
Moderate-to-Strong leisure score: 19 | N/R | N/R | N/R |
| Myers, 2012 Clinical trial |
PASIPD (MET h/week) | 13.9±10.0 | N/R | N/R | N/R | N/R |
| Neto, 2021 Cross-sectional study |
Nil validated OCM. PAL was estimated based on hours of participation in sports and exercises. 1=sedentary (0 hours per week), 2=moderately active (1-3 hours per week), 3=active (3-6 hours per week), and 4=very active/athlete (more than 6 hours per week). |
1 n=3 (13.04%) 2 n=14 (60.87%) 3 n=4 (17.39%) 4 n=2 (69%) |
N/R | N/R | N/R | N/R |
| Postma, 2020 Longitudinal study |
Accelerometer (mins/week) | 718±345 | N/R | N/R | Walking, running, cycling, wheeling | N/R |
| Rauch, 2014 Cross-sectional study |
Nil validated outcome measure. “Sport” was not defined more precisely than “more than 30 minutes”. 1=daily; 2=several × per week; 3=once per week; 4=several × per month; 5=less |
N/R | N/R | 1 n=29 (8.63%) 2 n=98 (29.17%) 3 n=71 (21.13%) 4 n=17 (5.06%) 5 n=121 (36.01%) |
N/R | N/R |
| Rauch, 2016 Cross-sectional study |
PASIPD (MET h/week) – modified (items 3-6) | Recreation only: Age 51-70: 8.4 (mean); 6 (2.3, 11.3) Age 71 & older: 6.9 (mean), 4.5 (1.5, 10.5) |
Recreation only: Age 51-70: 4.3 (mean), 2.2 (0.0; 6.0) Age 71 and older: 3.1 (mean), 1.5 (0.0; 5.3) |
N/R | N/R | N/R |
| Rocchi, 2017 Cross-sectional study |
LTPAQ-SCI (days, mins) | Aerobic mild days: 1.1±2.2 Aerobic mild mins: 23±69 Aerobic moderate days: 1.1±1.8 Aerobic moderate mins: 23±64 Aerobic heavy days: 0.7±1.7 Aerobic heavy mins: 7±20 Resistance mild days: 0.4±1.3 Resistance mild mins: 13±46 Resistance moderate days: 0.57±1.19 Resistance moderate mins: 14±31 Resistance heavy days: 0.24±1.06 Resistance heavy mins: 2±6 |
Aerobic moderate days: 1.1±1.8 Aerobic moderate mins: 23±64 Aerobic heavy days: 0.7±1.7 Aerobic heavy mins: 7±20 Resistance moderate days: 0.6±1.2 Resistance moderate mins: 14±31 Resistance heavy days: 0.2±1.1 Resistance heavy mins: 2±6 |
N/R | N/R | N/R |
| Santino, 2021 Cross-sectional study |
LTPAQ-SCI (mins/week) | N/R | 268±41 | N/R | N/R | N/R |
| Watson, 2022 Cross-sectional study |
PASIPD – modified (mins/week) | 225±431 | N/R | N/R | N/R | N/R |
Abbreviations: ADL, Activity of Daily Living; GLTEQ, Godin Leisure-Time Exercise Questionnaire; Mod-heavy, moderate to heavy; N/R, not reported; PAL, Physical Activity Level; PARTS/M-v3, Participation Survey of Mobility Limited People version 3; TSI, time since injury.
GTLEQ-modified - Physical activity was measured by participants reporting the number of days they spent doing more than 15 minutes of physical activity during their free time, over a 7-day period (1 week), in each of 3 categories (strenuous, moderate, and mild). Their modified version asked participants the “number of days” spent in various exercise activities. The total activity score (LSI) is then calculated by multiplying the frequency score (number of days in each category) by metabolic equivalents for each respective category (3=mild, 5=moderate, 9=strenuous). individuals reporting moderate-to-strenuous LSI ≥ 24 are classified as active, whereas individuals reporting moderate-to-strenuous LSI ≤ 23 are classified as insufficiently active.
PAL scores ranged from 1 to 10 and were stratified for descriptive purposes as follows: 1-4=low PAL; 5-7=moderate, PAL; and 8-10=high PAL.
LTPA participation
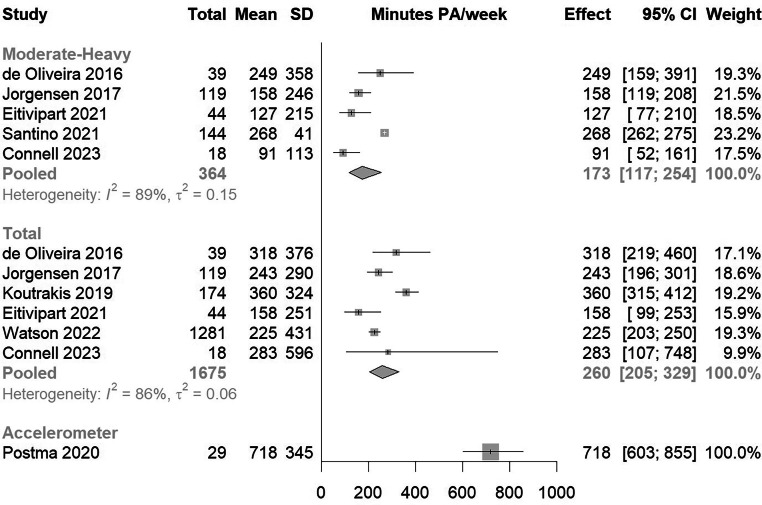
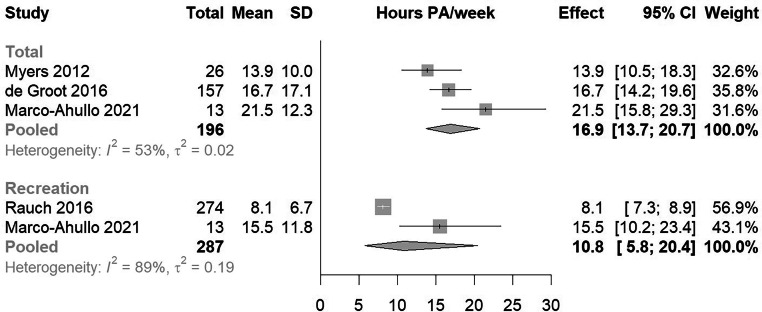
Three studies (n=202) reported that 27%-64% of their participants did not participate in any LTPA at all (table 3). Seven studies (n=1704) found that participants engaged between 243 and 718 mins/week in LTPA (table 3). Six studies (n=419) reported on participation in moderate-heavy LTPA and found that the participants completed between 157 and 268 mins/week (table 3). LTPA participation using self-reported measures (in mins/week) (fig 2) showed a mean [95% confidence interval] of 260 [205; 329] mins/week, which included light, moderate, and heavy LTPA. LTPA participation using the PASIPD (fig 3), measured in MET hours/week, was 16.9 [13.7; 20.7] MET hours/week, inclusive of activities of daily living and 10.8 [5.8; 20.4] MET hours/week excluding activities of daily living.
Fig 2.
Meta-analysis of physical activity participation using self-reported measures (mins/week). Abbreviation: SD, standard deviation. CI, confidence interval, PA, physical activity.
Fig 3.
Meta-analysis of physical activity participation using the PASIPD (MET hours/week). Abbreviation: SD, standard deviation. CI, confidence interval, PA, physical activity.
Frequency, duration, intensity, and modality of LTPA
Eight studies (n=1001) provided levels of participation in moderate-heavy intensity LTPA. Moderate-to-heavy intensity of self-reported LTPA (5 studies included in the meta-analysis) was 173 [118; 255] mins/week (fig 2). LTPA duration and frequency was represented as minutes per day, minutes per week, hours per week, or MET hours/week, depending on the tool used (table 3). Only 2 studies (n=133) provided the modality of LTPA, which included walking, using a wheelchair, hand-cycling, basketball, swimming, and other leisure activities/sports (table 3). Three studies (n=513) reported that between 20% and 58% of individuals participated in sports on a weekly basis (table 3).
Discussion
An estimated 27%-64% of middle/older-aged adults participated in no LTPA.17,37,48 The average weekly participation in moderate-to-heavy LTPA (173 mins/week) suggested that many individuals aged 45 and over could be meeting the WHO recommendations for aerobic physical activity to prevent cardiovascular diseases. On average, people participated in a satisfactory amount of “total LTPA” (including light, moderate, and heavy intensities) with an average of 260 mins/week. There was substantial variation in LTPA participation as shown by the large standard deviations in the included studies. This indicates that while some people might participate in large amounts of LTPA, others are engaging in very little or no LTPA. Those participating in LTPA engaged in a variety of modalities including wheeling, hand-cycling, walking, basketball, swimming among others, although “modality and frequency” of LTPA was not frequently reported.
The considerable variability in the amount of weekly LTPA observed is consistent with previous research among people with SCI.17,37,49 Comparative analysis of LTPA participation between middle/older-aged adults with SCI and the general (non-SCI) aging population (≥45 years) in 2 countries showed notable differences. The SASCIS study found that 29% of individuals with SCI aged ≥45 years were sedentary, meaning that they engaged in no LTPA.17 In a different study, from Thailand, 50% of the individuals with SCI aged 46-60 years did not participate in any LTPA, and the proportion increased to 64% among those aged 61-75 years.37 A Canadian study, including individuals with SCI of all ages, showed that on average people participated in 55 mins/day of LTPA, which could be interpreted as very active, however, while some people with SCI were engaging in considerable amounts of LTPA, most were doing much less (median of 33 mins/day).49 In comparison, in Sweden, 18% of the non-disabled population (>65 years) are sedentary,50 and in Australia 4.2% of men and 4.1% of women aged 65-74 years are sedentary, increasing to 13.2% (men) and 20.5% (women) once aged over 85 years.51 Given this, there is a large difference in LTPA in people with and without SCI. This disparity highlights the concerningly high prevalence of sedentary behavior and the need for targeted interventions to promote LTPA among middle/older-aged adults ≥45 years with SCI.
We found a large variation in the outcome measures used to assess LTPA in the SCI population, which made direct comparisons across all studies difficult. Some studies used the PASIPD and reported measurements in MET hours per week, while others used the PARA-SCI or the LTPAQ-SCI, reporting in minutes per day or week. These differences posed a challenge to the data synthesis and comparisons between studies. When data were obtained from authors, it often only included total PASIPD scores, which included a combination of recreational, household, and occupational physical activities. Consequently, the reported total PASIPD score in MET h/week appears disproportionally high as total score comprises of “occupation, activities of daily living and recreation”, hence the inclusion of “recreation score” alone when available. One study included in this review used accelerometer data to assess LTPA participation and excluded sedentary behaviors such as minor maneuvering of a wheelchair, but still captured all physical activities including activities of daily living.46 The inconsistency in reporting of the included studies could be related to the lack of initiatives to implement a core outcome set of measures of physical activity participation. There have been some core outcome set initiatives, with 1 recommending the use of the PARA-SCI,52 but no final consensus has been made.52,53 The International Spinal Cord Injury Society has no recommended core outcome sets including LTPA.54,55 As there are a lot of different measures for LTPA, it is problematic for comparisons and generalization of findings, as shown in this review.
Strengths and limitations
This is the first review that investigates LTPA in middle/older-aged adults with SCI. Extensive efforts were made to contact 80 authors for specific information related to individuals ≥45 years and above. Only 4 studies reported on middle/older-aged adults as a separate group. Many studies screened for this review did not publish LTPA data on different age groups, despite occasionally establishing correlations between LTPA and age. Fifteen authors responded with relevant data. Some authors of studies with large data sets on LTPA were unresponsive to our inquiries and data from these studies were excluded from this review. Inclusion of these data could have changed overall conclusions or increased the certainty of these. Limitations arise from reliance on authors’ data, often lacking raw LTPA levels for different injury levels, providing only percentages of paraplegia and tetraplegia. Varying reporting practices across studies further hindered assessing LTPA differences between these groups, constraining subgroup analysis depth. For 1 study,18 we could not combine data points (provided by the author) to produce a total LTPA score, leading to its exclusion from the meta-analysis. One study46 reported significantly higher levels of LTPA, likely attributed to the use of an accelerometer. Another study discussed that a major limitation of their study was the large amount of missing LTPA data, and the authors noted the presence of (unrealistic) extreme values.23 Only 3 studies37,18,43 reported strength-specific physical activity, despite WHO physical activity guidelines and the Canadian SCI-specific physical activity guidelines outlining both aerobic and strength requirements15 to achieve health benefits. Unfortunately, the use of the JBI for risk of bias does not assess dealing with missing data, or management of data so these were not accounted in our risk of bias assessment. Finally, this review included predominantly (89%) high income earning countries, with only 2 low-income countries included.37,41 Taken together, these limitations could affect the comprehensiveness and generalizability of our findings.
Clinical implications and future research
There is a significant variation in the weekly time spent doing LTPA. Some people with SCI ≥45 years seem to meet the recommended physical activity guidelines, but concerningly, some are participating in little to no LTPA at all. This means middle/older-aged adults with SCI are at an increased risk of developing cardiometabolic diseases and increased disability. Embedding LTPA early on post injury is crucial in maintaining LTPA participation,23 and providing support to those people aging with SCI with the correct resources (as early as possible) to access LTPA to live a healthy and fulfilled life is necessary.
Future research should report LTPA data on different age groups, or make all data freely available, so that strategies to embed LTPA to middle/older-aged people with SCI can be targeted correctly. Future research should attempt to use a common validated and reliable outcome measure, consistent across studies. Consensus should be drawn about the appropriate tool used, which should be able to measure against the WHO physical activity guidelines and SCI-specific guidelines. Furthermore, future studies should focus on identifying those at risk of not participating in LTPA post-SCI in middle/older-age and on the determinants of LTPA participation. Policy initiatives to increased LTPA uptake could include increasing government funding, improving community access, and promoting enjoyable LTPA. Supporting physical activity initiatives in those aging reduces the risk of losing mobility and independence and will ultimately reduce associated health costs and hospitalizations associated with declines in health and disability.
Conclusions
There is considerable variability in LTPA participation among middle/older-aged adults with SCI. Because of differences in reporting, it was challenging to combine and compare results across studies. Limitations in data availability and varied reporting practices restricted subgroup analysis, particularly in assessing LTPA disparities between those with paraplegia vs tetraplegia. While some middle/older-aged adults with SCI seem to be meeting recommended weekly aerobic physical activity guidelines and likely achieving the health benefits, there are still some participating in little to no LTPA. Therefore, strategies to increase LTPA participation and intensity for aerobic and strength activities in middle/older-aged adults with SCI are necessary. Because of the significant variation in the outcome measures used to report LTPA, initiatives to implement core outcome sets in physical activity research in SCI are needed.
Suppliers
-
a.
R version 4.21, R Core Team
Acknowledgment
The authors would like to acknowledge the support of Ms Ana Shah Hosseani (Education and Research Services Librarian, University of Technology Sydney) for her assistance in developing the search strategy and all authors who provided additional requested data.
Footnotes
Disclosure: There is no conflict of interest for this review.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.arrct.2024.100335.
Appendix. Supplementary materials
References
- 1.Ahuja CS, Wilson JR, Nori S, et al. Traumatic spinal cord injury. Nat Rev Dis Primers. 2017;3:17018. doi: 10.1038/nrdp.2017.18. [DOI] [PubMed] [Google Scholar]
- 2.Charlifue SW, Weitzenkamp D, Whiteneck GG. Longitudinal outcomes in spinal cord injury: aging, secondary conditions, and well-being. Arch Phys Med Rehabil. 1999;80:1429–1434. doi: 10.1016/s0003-9993(99)90254-x. [DOI] [PubMed] [Google Scholar]
- 3.Myers J, Lee M, Kiratli J. Cardiovascular disease in spinal cord injury: an overview of prevalence, risk, evaluation, and management. Am J Phys Med Rehabil. 2007;86:142–152. doi: 10.1097/PHM.0b013e31802f0247. [DOI] [PubMed] [Google Scholar]
- 4.Lundstrom U, Wahman K, Seiger A, Gray DB, Isaksson G, Lilja M. Participation in activities and secondary health complications among persons aging with traumatic spinal cord injury. Spinal Cord. 2017;55:367–372. doi: 10.1038/sc.2016.153. [DOI] [PubMed] [Google Scholar]
- 5.Montesinos-Magraner L, Serra-Ano P, Garcia-Masso X, Ramirez-Garceran L, Gonzalez LM, Gonzalez-Viejo MA. Comorbidity and physical activity in people with paraplegia: a descriptive cross-sectional study. Spinal Cord. 2018;56:52–56. doi: 10.1038/sc.2017.90. [DOI] [PubMed] [Google Scholar]
- 6.Aarabi B, Albrecht JS, Simard JM, et al. Trends in demographics and markers of injury severity in traumatic cervical spinal cord injury. J Neurotrauma. 2020;38:756–764. doi: 10.1089/neu.2020.7415. [DOI] [PubMed] [Google Scholar]
- 7.Buchholz AC, McGillivray CF, Pencharz PB. Physical activity levels are low in free-living adults with chronic paraplegia. Obes Res. 2003;11:563–570. doi: 10.1038/oby.2003.79. [DOI] [PubMed] [Google Scholar]
- 8.Kocina P. Body composition of spinal cord injured adults. Sports Med. 1997;23:48–60. doi: 10.2165/00007256-199723010-00005. [DOI] [PubMed] [Google Scholar]
- 9.Buchholz AC, Ginis KAM, Bray SR, et al. Greater daily leisure time physical activity is associated with lower chronic disease risk in adults with spinal cord injury. Appl Physiol Nutr Metab. 2009;34:640–647. doi: 10.1139/H09-050. [DOI] [PubMed] [Google Scholar]
- 10.Sweis R, Biller J. Systemic complications of spinal cord injury. Curr Neurol Neurosci Rep. 2017;17:8. doi: 10.1007/s11910-017-0715-4. [DOI] [PubMed] [Google Scholar]
- 11.Tomasone JR, Wesch NN, Ginis KAM, Noreau L. Spinal cord injury, physical activity, and quality of life: a systematic review. Kinesiol Rev. 2013;2:113–129. [Google Scholar]
- 12.van den Berg-Emons RJP, Bussmann JBP, Stam HJMDP. Accelerometry-based activity spectrum in persons with chronic physical conditions. Arch Phys Med Rehabil. 2010;91:1856–1861. doi: 10.1016/j.apmr.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 13.Kroll T, Kratz A, Kehn M, et al. Perceived exercise self-efficacy as a predictor of exercise behavior in individuals aging with spinal cord injury. Am J Phys Med Rehabil. 2012;91 doi: 10.1097/PHM.0b013e31825a12cd. [DOI] [PubMed] [Google Scholar]
- 14.Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56:308–321. doi: 10.1038/s41393-017-0017-3. [DOI] [PubMed] [Google Scholar]
- 15.Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rauch A, Hinrichs T, Oberhauser C, Cieza A, SwiSCI Study Group Do people with spinal cord injury meet the WHO recommendations on physical activity? Int J Public Health. 2016;61:17–27. doi: 10.1007/s00038-015-0724-5. [DOI] [PubMed] [Google Scholar]
- 17.Jorgensen S, Ginis KAM, Lexell J. Leisure time physical activity among older adults with long-term spinal cord injury. Spinal Cord. 2017;55:848–856. doi: 10.1038/sc.2017.26. [DOI] [PubMed] [Google Scholar]
- 18.Rocchi M, Routhier F, Latimer-Cheung AE, Ginis KAM, Noreau L, Sweet SN. Are adults with spinal cord injury meeting the spinal cord injury-specific physical activity guidelines? A look at a sample from a Canadian province. Spinal Cord. 2017;55:454–459. doi: 10.1038/sc.2016.181. [DOI] [PubMed] [Google Scholar]
- 19.Vissers M, van den Berg-Emons R, Sluis T, Bergen M, Stam H, Bussmann H. Barriers to and facilitators of everyday physical activity in persons with a spinal cord injury after discharge from the rehabilitation centre. J Rehabil Med. 2008;40:461–467. doi: 10.2340/16501977-0191. [DOI] [PubMed] [Google Scholar]
- 20.Roberton T, Bucks R, Skinner T, Allison G, Dunlop S. Barriers to physical activity in individuals with spinal cord injury: a Western Australian Study. Aust J Rehabil Counsel. 2011;17:74–88. [Google Scholar]
- 21.Bouchard C, Shephard RJ, Brubaker PH. Physical activity, fitness, and health: Consensus Statement. Med Sci Sports Exerc. 1994;26:119. [Google Scholar]
- 22.Martin Ginis KA, Latimer AE, Arbour-Nicitopoulos KP, et al. Leisure time physical activity in a population-based sample of people with spinal cord injury Part I: demographic and injury-related correlates. Arch Phys Med Rehabil. 2010;91:722–728. doi: 10.1016/j.apmr.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 23.Watson PK, Arora M, Middleton JW, et al. Leisure-time physical activity in people with spinal cord injury—predictors of exercise guideline adherence. Int J Public Health. 2022;67 doi: 10.3389/ijph.2022.1605235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Milanović Z, Pantelić S, Trajković N, Sporiš G, Kostić R, James N. Age-related decrease in physical activity and functional fitness among elderly men and women. Clin Interv Aging. 2013;8:549–556. doi: 10.2147/CIA.S44112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jörgensen S, Iwarsson S, Lexell J. Secondary health conditions, activity limitations, and life satisfaction in older adults with long-term spinal cord injury. PM R. 2017;9:356–366. doi: 10.1016/j.pmrj.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 26.Higgins JPT, Thomas J, Chandler J, et al. 2nd edition. Wiley-Blackwell; Hoboken, NJ: 2019. Cochrane handbook for systematic reviews of interventions. [Google Scholar]
- 27.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at: www.covidence.org. Accessed February 20, 2023.
- 29.Up Study Collaborators Cohort profile: the 45 and up study. Int J Epidemiol. 2008;37:941–947. doi: 10.1093/ije/dym184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perianayagam A, Bloom D, Lee J, et al. Cohort profile: The Longitudinal Ageing Study in India (LASI) Int J Epidemiol. 2022;51:e167–e176. doi: 10.1093/ije/dyab266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raina PS, Wolfson C, Kirkland SA, et al. The Canadian Longitudinal Study on Aging (CLSA) Canad J Aging. 2009;28:221–229. doi: 10.1017/S0714980809990055. [DOI] [PubMed] [Google Scholar]
- 32.Joanna Briggs Critical Appraisal Tool - Checklist for Analytical Cross Sectional Studies. Available at: https://jbi.global/critical-appraisal-tools. Accessed March 20, 2023.
- 33.Ma L-L, Wang Y-Y, Yang Z-H, Huang D, Weng H, Zeng X-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. 2020;7:7. doi: 10.1186/s40779-020-00238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2023. A Language and Environment for Statistical Computing.https://www.R-project.org/ Available at: Accessed March 26, 2023. [Google Scholar]
- 35.Blauwet C, Sudhakar S, Doherty AL, Garshick E, Zafonte R, Morse LR. Participation in organized sports is positively associated with employment in adults with spinal cord injury. Am J Phys Med Rehabil. 2013;92:393–401. doi: 10.1097/PHM.0b013e3182876a5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Groot S, Adriaansen JJ, Tepper M, Snoek GJ, van der Woude LHV, Post MWM. Metabolic syndrome in people with a long-standing spinal cord injury: associations with physical activity and capacity. Appl Physiol Nutr Metab. 2016;41:1190–1196. doi: 10.1139/apnm-2016-0269. [DOI] [PubMed] [Google Scholar]
- 37.Eitivipart AC, Arora M, Quel de Oliveira C, Heard R, Middleton JW, Davis GM. Assessing physical activity and health-related quality of life in individuals with spinal cord injury: a national survey in Thailand. Disabil Rehabil. 2022;44:7048–7058. doi: 10.1080/09638288.2021.1979665. [DOI] [PubMed] [Google Scholar]
- 38.Hansen RK, Larsen RG, Laessoe U, Samani A, Cowan RE. Physical activity barriers in Danish manual wheelchair users: a cross-sectional study. Arch Phys Med Rehabil. 2021;102:687–693. doi: 10.1016/j.apmr.2020.09.384. [DOI] [PubMed] [Google Scholar]
- 39.Koutrakis NE, Goldstein RL, Walia P, et al. Vitamin D, diet, and lifestyle in a chronic SCI population. Spinal Cord. 2019;57:117–127. doi: 10.1038/s41393-018-0148-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matsuda PN, Eagen T, Hreha KP, Finlayson ML, Molton IR. Relationship between fear of falling and physical activity in people aging with a disability. PM R. 2020;12:454–461. doi: 10.1002/pmrj.12289. [DOI] [PubMed] [Google Scholar]
- 41.Neto FR, Dorneles JR, Carneiro Leão Veloso JH, Gonçalves CW, Gomes Costa RR. Peak torque prediction using handgrip and strength predictors in men and women with motor complete spinal cord injury. Top Spinal Cord Inj Rehabil. 2021;27:49–59. doi: 10.46292/sci20-00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rauch A, Fekete C, Oberhauser C, Marti A, Cieza A. Participation in sport in persons with spinal cord injury in Switzerland. Spinal Cord. 2014;52:706–711. doi: 10.1038/sc.2014.102. [DOI] [PubMed] [Google Scholar]
- 43.Santino N, Larocca V, Hitzig SL, Guilcher SJT, Craven BC, Bassett-Gunter RL. Physical activity and life satisfaction among individuals with spinal cord injury: exploring loneliness as a possible mediator. J Spinal Cord Med. 2022;45:173–179. doi: 10.1080/10790268.2020.1754651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.EM Connell, JV Olthuis, Mental health and physical activity in SCI: Is anxiety sensitivity important?, Rehab. Psychol, 68 (2), 2023, 174–183. [DOI] [PubMed]
- 45.Marco-Ahulló A, Montesinos-Magraner L, González L-M, Morales J, Bernabéu-García JA, García-Massó X. Impact of COVID-19 on the self-reported physical activity of people with complete thoracic spinal cord injury full-time manual wheelchair users. J Spinal Cord Med. 2022;45:755–759. doi: 10.1080/10790268.2020.1857490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Postma K, Bussmann JBJ, van Diemen T, et al. Physical activity and sedentary behavior from discharge to 1 year after inpatient rehabilitation in ambulatory people with spinal cord injury: a longitudinal cohort study. Arch Phys Med Rehabil. 2020;101:2061–2070. doi: 10.1016/j.apmr.2020.06.027. [DOI] [PubMed] [Google Scholar]
- 47.Myers J, Gopalan R, Shahoumian T, Kiratli J. Effects of customized risk reduction program on cardiovascular risk in males with spinal cord injury. J Rehabil Res Dev. 2012;49:1355–1364. doi: 10.1682/jrrd.2011.11.0215. [DOI] [PubMed] [Google Scholar]
- 48.de Oliveira BIR, Howie EK, Dunlop SA, Galea MP, McManus A, Allison GT. SCIPA Com: outcomes from the spinal cord injury and physical activity in the community intervention. Spinal Cord. 2016;54:855–860. doi: 10.1038/sc.2015.235. [DOI] [PubMed] [Google Scholar]
- 49.Ginis KAM, Arbour-Nicitopoulos KP, Latimer AE, et al. Leisure time physical activity in a population-based sample of people with spinal cord injury Part II: activity types, intensities, and durations. Arch Phys Med Rehabil. 2010;91:729–733. doi: 10.1016/j.apmr.2009.12.028. [DOI] [PubMed] [Google Scholar]
- 50.The Public Health Agency of Sweden Public Health reporting and statistics. The national public health survey “Health on equal terms”. Available at: http://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/statistikdatabaseroch-visualisering/nationella-folkhalsoenkaten/levnadsvanor/fysisk-aktivitet/. Accessed August 23, 2023.
- 51.Bauman A, Lee K, Ding D, Phongsavan P. Physical activity research in the first 15 years of the “45 and Up” cohort study: a narrative review and citation analysis. Public Health Res Pract. 2022;32 doi: 10.17061/phrp3242234. [DOI] [PubMed] [Google Scholar]
- 52.Kahn JH, Tappan R, Newman CP, et al. Outcome measure recommendations from the spinal cord injury EDGE Task Force. Phys Ther. 2016;96:1832–1842. doi: 10.2522/ptj.20150453. [DOI] [PubMed] [Google Scholar]
- 53.Ramdharry G, Buscemi V, Boaz A, et al. Proposing a core outcome set for physical activity and exercise interventions in people with rare neurological conditions. Front Rehabil Sci. 2021;2 doi: 10.3389/fresc.2021.705474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Post MW, Charlifue S, Biering-Sørensen F, et al. Development of the International Spinal Cord Injury Activities and Participation Basic Data Set. Spinal Cord. 2016;54:530–534. doi: 10.1038/sc.2015.188. [DOI] [PubMed] [Google Scholar]
- 55.International Spinal Cord Injury Society. Available at: https://www.iscos.org.uk/. Accessed August 23, 2023.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.