Abstract
Objective:
In this article we present preliminary findings from a research program designed to investigate the value of alliance-focused training (AFT), a supervision approach designed to enhance therapists’ ability to work constructively with negative therapeutic process.
Method:
In the context of a multiple baseline design, all therapists began treating their patients using cognitive therapy and then joined AFT supervision groups at either session 8 or 16 of a 30 session protocol. Study I investigated the impact of AFT on patient and therapist interpersonal process as assessed through the Structural Analysis of Social Behavior (SASB). Study 2 investigated the impact of AFT on therapists’ tendency to reflect on their relationships with their patients in an experientially grounded fashion, as assessed via the Experiencing Scale (EXP). Since one of the goals of AFT is to train therapists to use their own emerging feelings as important clues regarding what may be taking place in the therapeutic relationship, we hypothesized that they would show increased levels of EXP after undergoing AFT.
Results and Conclusion:
The results of both studies 1 and 2 were for the most part consistent with hypotheses. Implications and future research directions are discussed.
Keywords: alliance, psychotherapist training/supervision/development, process research, psychoanalytic/psychodynamic therapy
One of the most consistent findings emerging from psychotherapy research is that the quality of the therapeutic alliance is a robust predictor of outcome across a range of different treatments and that, conversely, weakened alliances are correlated with unilateral termination by the patient (e.g., Horvath, Del Re, Flückiger, & Symonds, 2011). In addition, there is now evidence that some therapists consistently have better alliances, along with better outcomes (see Baldwin, Wampold, & Imel, 2007; Wampold, 2001). There is also a growing body of evidence suggesting that therapists often respond to patient hostility with counter-hostility, and that this type of “negative process” is associated with poor outcome (Anderson, Knobloch-Fedders, Stiles, Ordonez, & Heckman, 2012; Binder & Strupp, 1997; Safran, Muran, Samstag, & Stevens, 2001).
The empirical focus on negative process emerged in tandem with the growing empirical interest in the therapeutic alliance. A key impetus was Hans Strupp’s efforts to make sense of the Vanderbilt I study’s finding that seasoned professional therapists were no more helpful to patients than a group of college professors who had received no clinical training (Strupp & Hadley, 1979). Strupp’s subsequent use of a series of research-informed case studies comparing good and bad outcome cases from the Vanderbilt I study led him to what was to become the central theme of his research career: the attempt to grapple with the problem of training therapists to work constructively with negative therapeutic process. As he said at the time, “In our study, we failed to encounter a single instance in which a difficult patient’s hostility and negativism were successfully confronted or resolved … therapists’ negative responses to difficult patients are far more common and far more intractable than has been generally recognized” (Strupp, 1980, p. 954).
In the last two decades, there has emerged a “second generation” of alliance research that integrates work on the alliance with attention to negative process by focusing on improving therapists’ abilities to repair ruptures in the alliance when they occur (see Eubanks-Carter, Muran, & Safran, 2010; Safran et al., 2001; Safran, Muran, & Eubanks-Carter, 2011, for reviews). A number of studies have evaluated the effectiveness of treatment interventions and training procedures designed specifically to improve therapists’ abilities to work constructively with weakened alliances and negative therapeutic process. In a recent meta-analysis, Safran et al. (2011) found a moderate and significant effect size for studies of this type when examining pre-post effect sizes. However, the average between-group effect size, though still significant, was relatively modest.
The lack of large differences between treatments targeting problems in the alliance should come as no surprise. One of the most common findings in psychotherapy research is the “therapeutic equivalence effect,” i.e., the failure to find that one form of treatment is consistently more effective than others (Luborsky et al., 2002; Wampold et al., 1997). Various hypotheses have been advanced to account for this effect. One is that group averages in randomized clinical trial studies can mask the fact that not all patients in a given treatment condition show equal benefit and that not all therapists are equally effective. The situation is further complicated by the fact that even if we were able to control for both patient and therapist variables, we would also need to take into account the patient-therapist interaction variable (i.e., factors unique to the specific therapeutic dyad). Another way of framing this issue is in terms of Stiles’ notion of therapeutic responsiveness (Stiles, Honos-Webb, & Surko, 1998): Therapists and patients are always influencing and responding to one another on an ongoing basis. Thus, every therapeutic dyad is unique, and their style of mutual responsiveness will vary at different points in time.
Although it is impossible to control for all of these variables at the same time, there are ways of controlling for more of them than we normally do. For example, both Strupp and colleagues (Bein et al., 2000; Henry, Strupp, Butler, Schacht, & Binder, 1993; Strupp, 1993) in the Vanderbilt II study and Crits-Christoph et al. (2006) evaluated the effectiveness of training programs designed specifically to improve therapists’ abilities to enhance the alliance and work constructively with negative therapeutic process. Both studies evaluated the therapeutic outcomes obtained by the same therapists with different cohorts of patients pre- and post-training. In this way, they were able to reduce the degree of variance attributable to individual therapists by holding the therapist variable constant. Although the results of Crits-Christoph et al.’s study were more promising than Strupp et al.’s, they were still somewhat equivocal. Moreover, it is important to bear in mind that both studies attempted to control for the therapist variable while failing to control for the patient variable. Thus one cannot, for example, rule out the possibility that the patients treated after training were in some ways more difficult to work with than the patients treated before training.
In a pilot study designed to test the effectiveness of an alliance-focused intervention with patients who were potential treatment failures, Safran, Muran, Samstag, and Winston (2005) attempted to reduce the degree of patient variance by including only patients with whom therapists had difficulty establishing a good therapeutic alliance in the first phase of the study. These challenging patients were reassigned to a different set of therapists working in either an alliance-focused modality or a control condition in the second phase of the study. Although the results of this study provided promising support for the alliance-focused treatment, the sample was too small to draw any definitive conclusions. Moreover, in contrast to the Vanderbilt II and Crits-Christoph et al. (2006) studies, Safran et al. (2005) focused on reducing patient variance, while neglecting to control for the therapist variable.
In this article, we present preliminary findings emerging from an ongoing research project currently under way at the Beth Israel Psychotherapy Research Program (see Muran, 2002, for background) designed to investigate the effectiveness of a training protocol to enhance therapists’ abilities to detect and work constructively with alliance ruptures and negative therapeutic process. The training protocol, which we will refer to as alliance-focused training (AFT), is based upon the principles of the alliance-focused treatment we have described elsewhere (e.g., Muran, Safran & Eubanks-Carter, 2010; Muran, Safran, Samstag, & Winston, 2005; Safran & Muran, 2000; Safran et al., 2005) and will discuss briefly below. This project was designed to control for variance attributable to patient, therapist, and patient-therapist interactional sources. In order to evaluate whether changes taking place after the implementation of AFT were attributable to AFT or to other factors (e.g., an improvement in therapist skill due to increased experience or greater familiarity with a specific patient), we employed a multiple baseline design. In this design, all therapists began treating a case with CBT while receiving CBT supervision, and then at predetermined points (at session 8 or at session 16) switched from CBT supervision to AFT. By introducing AFT at different time intervals, we were able to control for time or maturation effects. We were then able to evaluate whether theoretically predictable changes on a variety of dimensions occurred after the implementation of AFT. By testing for differences within, rather than between patient-therapist dyads, we were able to control for patient and therapist individual differences as well as differences specific to each dyad.
This project consisted of two phases. In the first phase therapists (who were primarily graduate students in clinical psychology) received 1 year of training in CBT and completed one 30-session CBT case while attending weekly CBT supervision sessions. Therapists were required to demonstrate adherence to the CBT protocol in order to enter the second phase of the study. In this phase, therapists began treating a second case with CBT, while continuing to attend CBT supervision. After either eight or 16 sessions of CBT (the timing was determined by random assignment), therapists were transferred from the CBT supervision group to an AFT supervision group, where they learned how to augment CBT with AFT principles while continuing to work with the same patient. Because all therapists in the second phase began AFT at some point (albeit at different time intervals), we did not necessarily expect to find differences in ultimate outcome between therapeutic dyads who switched to AFT at session 8 versus session 16. Our focus was thus on proximal outcome (including changes in theoretically relevant processes) rather than ultimate outcome. It may ultimately be the case that dyad-specific differences in proximal outcome prove to be predictive of ultimate outcome, but this question was not examined in the studies that follow. All data collected in the two studies described below came from an ongoing investigation designed to examine the impact of augmenting CBT with AFT training. Because of missing data the cases analyzed in the two studies were only partially overlapping.
Training Conditions
Cognitive-Behavioral Therapy (CBT: Turner & Muran, 1992; Turner, Muran, & Ochoa, 2004).
The cognitive-behavioral therapy condition is designed to treat patients presenting with anxious, fearful, and avoidant Cluster C personality disorders and with personality disorders “not otherwise specified” according to DSM-IV in a 30-session, one 45-minute session/week protocol. It is largely based on Beck, Freeman, and associates’ (1990) adaptation of cognitive therapy to the treatment of personality disorders, and incorporates Persons and Silberschatz’s (1988) case formulation approach. According to this treatment model, personality and behavior are understood as organized by underlying belief systems or schemas. The treatment process involves the application of various cognitive and behavioral strategies to reduce symptoms and change schemas, including in-session tasks (e.g., breathing retraining, applied relaxation, role-playing, exposure exercises, eliciting and testing automatic thoughts, cognitive restructuring, and rehearsal) and extra-session tasks in the form of homework assignments (e.g., self-monitoring with thought records, scheduling activities, in vivo exposure exercises, and behavioral experiments).
Training consisted of a weekly 90-minute group supervision format. It entailed teaching a cognitive-behavioral conceptualization of anxiety, depression, and personality, how to establish a case formulation and identify core schemas, and how to implement the two intervention phases: (1) symptom reduction and (2) schema change. Training also involved a didactic component, observation of videotapes of skilled cognitive therapists, feedback on videotapes of trainees’ therapy cases, and role-playing exercises. These role-playing exercises were used to help therapists develop basic skills such as agenda setting, eliciting automatic thoughts and abstracting underlying schemas, and the use of various cognitive and behavioral strategies for challenging cognitive distortions and dysfunctional attitudes.
CBT training began with a 4-month-long didactic seminar on CBT taught by a psychologist who has an extensive background as a CBT therapist, including a 1-year postdoctoral fellowship at the Beck Institute, and 15 years of clinical experience. She is a fellow of the Academy of Cognitive Therapy. Following the seminar, trainees were assigned to supervision groups ranging in size from six to eight participants. The majority of trainees participated in groups led by the same psychologist who had led the didactic seminar. Approximately 20% of trainees participated in group supervision led by a second psychologist, trained as a cognitive therapist, with 20 years of clinical experience.
Alliance-focused training (AFT: Muran et al., 2010; Safran & Muran, 2000; Safran, Muran, Stevens, & Rothman, 2008).
The principles of AFT derive from our ongoing research program on resolving therapeutic alliance ruptures (see Safran et al., 2001, 2011 for reviews) as well as contemporary developments in relational psychoanalysis (e.g., Aron, 1996; Benjamin, 1990; Bromberg, 1998; Goldfried, 1994; Harris, 2011; Mitchell, 1988; Pizer, 1998; Safran 2002, 2012; Safran & Muran, 2006a Stern, 1998). Safran and Muran’s (2000) Negotiating the therapeutic alliance: A relational treatment guide was used as a training manual. This was supplemented with the training DVD Resolving therapeutic impasses (Safran & Muran, 2006b). The training included introducing an array of strategies to resolve alliance ruptures from explaining the rationale of the treatment, clarifying misunderstandings, and changing a task or goal, to exploring core relational themes.
Some of the key features of AFT are as follows: (a) it assumes that alliance ruptures result from patients and therapists becoming unwittingly embedded in negative interpersonal cycles with one another (e.g., hostility and counter-hostility), (b) therapists are taught to recognize that all interventions are relational acts, (c) therapists are trained to monitor what is taking place in the therapeutic relationship on an ongoing basis, (d) therapists are taught to take responsibility for their own contributions to what is taking place in the therapeutic relationship and to recognize that they are often contributing in ways that they do not fully recognize, (e) therapists are taught to use their own emerging feelings as important clues regarding what may be taking place in the therapeutic relationship, and (f) an important emphasis is placed on training therapists to explore their own emerging experience in a non-defensive fashion. As indicated above, this type of self-exploration is considered crucial since therapists’ feelings are viewed as a potentially valuable source of information about what may be taking place in the therapeutic relationship. Moreover, to the extent that therapists have difficulty fully acknowledging their own experience, their actions will be motivated by dissociated feelings and they are more likely to remain embedded or locked into pernicious transference-countertransference enactments (Safran & Muran, 2000).
Training was conducted in a weekly 90-minute group supervision format, consisting of a didactic component, videotaped demonstrations, and experiential exercises. The didactic component involved readings and lectures provided by supervisors regarding the definition and identification of ruptures and various rupture resolution strategies, with particular emphasis on the principles of therapeutic metacommunication. Metacommunication (i.e., communicating about implicit relational communications) is a commonly used intervention (Kiesler, 1996; Safran & Muran, 2000). Therapists are trained to invite patients to collaborate with them in the process of exploring how both partners in the therapeutic relationship are contributing to recurring patterns that are playing out. Metacommunication may involve exploring links between what is taking place in the therapeutic relationship and other patterns in the patient’s life, but therapists are trained to bear in mind that interventions of this type (traditionally referred to as transference interpretations) are relational acts as well. Depending on what the patient feels this act means, and what motivates the therapist’s intervention, patients may or may not find a particular metacommunication helpful
Alliance-focused training emphasizes experiential learning and self-exploration. Therapists were trained to attend to and explore their own feelings as important sources of information about what is going on in the therapeutic relationship. Role-playing exercises are used in AFT in order to bring to life interactions moments in treatment trainees have described to the group or illustrated through video-recordings. The objective of the role-plays is not only to experiment with intervening in different ways, but also to provide trainees with the opportunity to explore their own feelings and internal conflicts as they emerge in the moment. These exercises are referred to as “awareness-oriented role-plays” (Muran et al., 2010; Safran & Muran, 2000; Safran et al., 2008). Supervisors monitor the role-plays carefully and intervene at critical moments to direct therapists’ attention to their inner experience, and to encourage them to put unarticulated feelings and intuitions into words. In some cases, this process deepens into an exploration of internal conflicts that play a role in the therapist’s contribution to the rupture. In other cases, the supervisor helps the trainee explore feelings emerging in the context of a role-play and then encourages him or her to verbalize these feeling in the role-play as part of a metacommunication process.
Supervision sessions also employed mindfulness training for the purpose of helping therapists refine their capacity to observe their own inner experience as well as the nature of their own contributions to interaction. All supervision sessions devoted some time to mindfulness training, and therapists were encouraged to develop an ongoing mindfulness practice on their own between training sessions. Metacommunication is conceptualized as a type of “mindfulness in action” (Safran & Muran, 2000). In other words, therapists are taught to view metacommunication as an extension of mindfulness practice in which the goal is to attend to what is happening in the here-and-now, both in the therapeutic relationship and in their own emerging internal experience, with an attitude of curiosity and nonjudgmental acceptance.
Unlike the CBT supervision condition, AFT supervision did not begin with a didactic course in AFT. Instead trainees were reassigned from their ongoing CBT supervision to an AFT training group when the design dictated that it was time for them to begin augmenting CBT with AFT training. AFT supervision groups ranged in size from four to eight participants. Each group was led by one of the two main developers of the AFT approach, with support in some of the groups from a more junior PhD psychologist, who had received 2 years of AFT training and supervision while on predoctoral internship and postdoctoral fellowship.
Augmenting CBT with AFT
Once therapists transitioned from CBT supervision into alliance-focused training, they were instructed to begin incorporating principles of AFT into their work with their patients in a fashion that felt appropriate for their particular case. The precise pace and extent to which they used specific AFT interventions (e.g., metacommunication, therapists’ exploration of their own contributions to enactments, in-depth exploration of patients’ emerging feelings in context of the therapeutic relationship) were worked out collaboratively with their supervisors. In some cases, where it became apparent that there were well-defined ruptures in the alliance, therapists were encouraged to begin collaboratively exploring these ruptures with their patients soon after transitioning to AFT. In other cases, where ruptures were more subtle or it was not clear that ruptures of any type were taking place, therapists were encouraged simply to begin the process of paying closer attention to their own feelings while interacting with their patients, and to reflect internally and during supervision on subtle patterns that may have been playing out in the therapeutic relationship.
In cases where patients appeared to be benefiting from the use of cognitive-behavioral interventions, therapists were encouraged to continue using these interventions, while at the same time becoming more mindful of distinctive relational patterns or subtle enactments that might be playing out between them and their patients in sessions. In other cases, where the use of CBT interventions appeared to be problematic, therapists were encouraged to modify their approach more dramatically—in some cases actually abandoning the use of cognitive-behavioral interventions in order to focus more intensively on the use of relational interventions.
Given the individually tailored nature of the shift to AFT and the fact that this transition was often gradual and more subtle in nature, therapists were not instructed to tell their patients that they were beginning a new form of treatment. They were, however, instructed to provide their patients with rationales for employing interventions they had not used up until that point (e.g., explicitly exploring what is going on in the here and now of the therapeutic relationship). This process of providing rationales when relevant was considered to be important for purposes of maintaining a therapeutic alliance.
Study 1
The aim of Study 1 was to evaluate whether the introduction of AFT would result in changes in patient and therapist interpersonal process that are predictable on theoretical grounds, and that have been established as predictive of ultimate outcome. To assess for differences between the CBT and AFT conditions in therapist and patient interpersonal process, we employed a simplified version of the Structural Analysis of Social Behavior (SASB; Benjamin, 1974) coding system (described below). The SASB is a circumplex model that allows interpersonal behaviors to be coded along three dimensions: Interpersonal focus (focus on other, focus on self in relation to the other, or focus on self in relationship to the self), affiliation (friendliness vs. hostility), and interdependence (differentiation vs. enmeshment). The SASB model allows predictions to be made about complementary behaviors that are likely to emerge in an interpersonal interaction (Benjamin, 1974, 1994). The simplified version of the SASB we employed enabled us to code videotapes of sessions as a whole, in terms of the octant versions of Surface 1 (Focus on Self in Relation to the Other) and Surface 2 (Focus on Other) of the SASB. Below we describe the differences in interpersonal process that we hypothesized would emerge between the CBT and AFT phases.
Hypotheses
Given the more directive nature of CBT relative to AFT, we hypothesized that therapists in AFT would display less evidence of friendly, controlling interpersonal processes (AFT therapists < Watching & Controlling and Nurturing & Protecting) than they did in CBT training. We also anticipated a complementary pattern of patients displaying less evidence of friendly, submissive interpersonal process (patients < Deferring & Submitting and < Trusting & Relying) in AFT than in CBT.
Because AFT tends to be more exploratory and process-oriented in nature than CBT, and because AFT places an emphasis on encouraging patients to explore any concerns they have about the therapy or therapeutic relationship and to express wishes or needs that they feel are not being met by the therapist, we hypothesized that therapists in AFT would be more empathic and understanding and more encouraging of patient autonomy than they were during CBT training. We hypothesized that this would be reflected in an increase in therapist empathic understanding in AFT (therapists > Affirming & Understanding). For patients, we hypothesized a corresponding shift in AFT toward a greater degree of patient self-exploration (AFT patients > Disclosing & Expressing), and more self-assertion in the context of the therapeutic relationship (AFT patients > Asserting & Separating) than in CBT training.
Because therapeutic metacommunication (which involves therapist self-disclosure) plays an important role in AFT, we predicted more evidence of therapist self-disclosure (therapists > Disclosing & Expressing) in AFT than in the CBT phase of training. Based on our prior work on rupture resolution (see Safran & Muran, 2000), we predicted that greater therapist self-disclosure would also contribute to the increase in patient self-disclosure (patients > Disclosing & Expressing) noted above.
Finally, since AFT emphasizes the importance of therapists reflecting on and making constructive use of their own countertransference rather than expressing it unconsciously through their actions, we hypothesized that they would display less hostile interpersonal process (therapists < Belittling & Blaming and < Ignoring & Neglecting) in AFT than in CBT. We also hypothesized that patients would show a complementary decrease in hostile interpersonal process (patients < Sulking & Scurrying and < Walling-off & Distancing) during AFT.
For purposes of clarity we have stated our hypotheses as a series of specific shifts in therapist interpersonal stance, each followed by a specific shift in patient interpersonal stance. It is important to bear in mind, however, that in reality we anticipated that any links between shifts in therapist and patient interpersonal stance would operate in a more holistic fashion. For example, we anticipated that patients in AFT would show increased levels of self-disclosure as a function of a number of shifts in therapist process, including decreased controlling process, increases in friendly autonomy-granting process, and increased levels of therapist self-disclosure.
Method
Therapy cases used in the present study were selected from the ongoing research project described above. All patients entered into the project study met criteria for an Axis II diagnosis of either Cluster C or PD-NOS. Consistent with the multiple baseline design described earlier, therapists began weekly AFT supervision at either session 8 or session 16 to control for a time effect (e.g., change resulting from therapists becoming more experienced, or developing more experience with the particular patient in the study, or changes which might be attributable to the stage of the treatment).
To analyze the study data and make use of the multiple baseline design, six sessions were coded for each dyad. Two sessions were selected from each of the following phases of treatment: the early phase (defined as sessions 6–8), mid-phase (defined as sessions 14–16), and late phase (defined as sessions 22–24) to allow for an analysis of both within-group differences (i.e., changes attributable to training modality), and between-group differences (i.e., change attributable to the time factor) The two sessions for each phase were selected within a range of three sessions to accommodate missing data (see Figure 1). In cases where three sessions were available, two were randomly selected.
Figure 1.
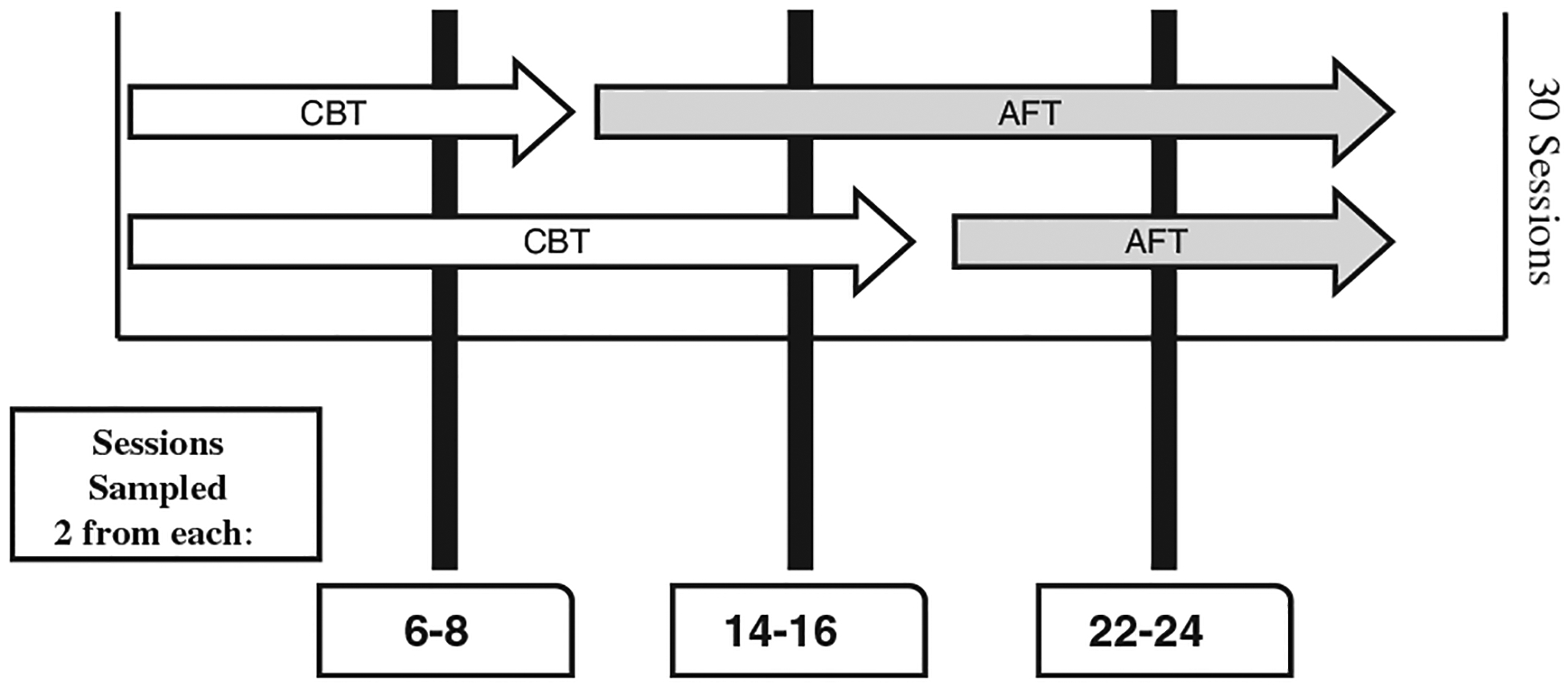
Study design, showing CBT and AFT (alliance-focused training) phases for the group that switched at session 8 (top row of arrows) and the group that switched at session 16 (bottom row of arrows).
Sample.
Twenty-two patients were selected for the study based on availability of video data. Of these patients, 12 were male and 10 female with a mean age of 45.13 (SD = 10.23). Seventeen patients included in the present study were White (77.3%), two African-American (9.1%), and three of Asian-Pacific Island descent (13.6%). Regarding primary Axis I diagnoses, 10 patients had a diagnosis of Major Depressive Disorder (45.5%), three met criteria for Dysthymia (13.6%), three met for Generalized Anxiety Disorder (13.6%), one Panic Disorder with Agoraphobia (4.5%), one Panic Disorder without Agoraphobia (4.5%), one Social Phobia (4.5%), and three had no Axis I diagnosis (13.6%). All patients in the study had a Cluster C or a PD-NOS diagnosis on Axis II. Nine patients (40.9%) met criteria for PD-NOS (two with Negativistic PD, one with Depressive PD), seven for Avoidant PD (31.8%), and six for Obsessive-Compulsive PD (27.2%).
Therapists were 22 externs, who were doctoral candidates in clinical psychology. These therapists received 20 weeks of CBT didactic training before completing a 30-session CBT therapy case to assess treatment modality competency and adherence. Therapists received weekly CBT group supervision throughout treatment. Upon case completion, they were assigned a second case beginning in CBT, and switching to AFT at either session 8 or session 16 (11 in each condition). Eighteen of the therapists were female (82%) and four were male (18%), with a mean age of 29.55 (SD = 3.42). Eighteen of the therapists were White (82%), two Hispanic (9%), and two of Asian-Pacific Island descent (9%).
Measures.
The SASB is typically used to code process at the level of thought units (i.e., portions of speech corresponding to one complete thought). An important advantage of this procedure is that it allows for a fine-grained analysis of turn-by-turn shifts in interpersonal process. This coding process is, however, relatively labor intensive and, consequently, researchers often restrict themselves to coding samples of process presumed to be representative (e.g., 15–30 minutes of the third session [Henry, Schacht, & Strupp, 1986]). For the present study, we reasoned that global ratings of entire sessions would be a meaningful and adequate unit of analysis. This rendered SASB coding less labor intensive, thus allowing us to code more sessions of potential interest, including multiple sessions per dyad, and to code entire sessions rather than samples of sessions. We thus traded off the potential value of a more fine-grained analysis for the gain of being able to increase the degree of representativeness of the material coded.
Using a working group of 10 graduate student coders, a number of videotapes of psychotherapy sessions were viewed, and the team gradually refined its sense of how best to code these videotapes at a global level. Ultimately the decision was made to code using the octant level of the SASB for both Surface 1 (Focus on Self) and Surface 2 (Focus on Other).
This resulted in 16 possible codes or dimensions that coders were instructed to rate on a 5-point scale borrowed from Baranackie and Crits-Christoph’s (1992) QUAINT methodology, with 1 meaning not present and 5 meaning very present. Both patients and therapists were rated on each of these 16 dimensions, thus resulting in a total of 32 codes (16 for patients and 16 for therapists). Therapy sessions were broken into 5-minute intervals which served as the units of coding. Ratings for each of the 5-minute intervals were then averaged to provide a total of 32 SASB dimension ratings for each session coded. Reliability was calculated at the session level. Approximately 15 weeks of coding training were required to attain inter-rater reliability.
Data analysis.
After the 15-week training period, inter-rater reliability on therapy sessions that were not included in this study was assessed using intraclass correlation coefficients (ICCs; two-way random effects model with absolute agreement on single measures). Groups were judged to be reliable after attaining ICC scores above .70 for each SASB item for five consecutive codings. Following this, pairs of raters independently coded the sessions included in this study. Mean scores of pairs were retained if the two raters were reliable with each other (ICC > .70). One session in the present study’s data set received an ICC below .70 (.67). This session was coded by a third coder, and the two most reliable scores were retained for the session’s composite SASB scores. The present study’s average ICC score for all sessions included was .78.
We hypothesized that any differences between CBT and AFT in interpersonal process would be evident regardless of whether AFT was implemented at session 8 or 16. In other words, we hypothesized that any differences in interpersonal process would be attributable specifically to training modality rather than the number of sessions that had taken place in the treatment. Moreover, we did not anticipate any training modality × time interval (8 or 16) interaction. In other words, we did not anticipate that shifts in interpersonal process would be moderated by time interval. To control for non-independence of observations, a Generalized Estimating Equations (GEE) analysis and repeated measures design was utilized for each item of the SASB.
Because of the large number of SASB items and the associated concerns about incurring Type I error, 17 items with minimal variance were not included in the analysis. These items largely corresponded to “Focus on Self” items for therapists, and “Focus on Other” items for patients. This is not surprising—due to the nature of the therapeutic relationship, the “Focus on Self” surface is rarely coded for therapist, and the “Focus on Other” surface is rarely coded for patients (Henry et al., 1986, 1993). In addition there were a few codes that were rarely used because of their extreme degree of intensity with respect to the affiliation dimension (e.g., therapist codes of attacking & rejecting or ignoring & neglecting). This left a total of 15 items for analysis (see Table I for descriptive data).
Table I.
Patient and therapist mean SASB scores across the entire treatment.
| SASB item | Therapist Mean (SD) | Patient Mean (SD) |
|---|---|---|
| Surface 1: Focus on Other | ||
| Freeing & Forgetting | 1.00 (.00)i | 1.00 (.00)i |
| Affirming & Understanding | 2.67 (.77) | 1.00 (.00)i |
| Loving & Approaching | 1.07 (.13) | 1.00 (.00)i |
| Nurturing & Protecting | 2.18 (.84) | 1.00 (.00)i |
| Watching & Controlling | 1.23 (.37) | 1.02 (.07) |
| Belittling & Blaming | 1.02 (.06) | 1.05 (.18) |
| Attacking & Rejecting | 1.00 (.00)i | 1.00 (.00)i |
| Ignoring & Neglecting | 1.00 (.00)i | 1.00 (.00)i |
| Surface 2: Focus on Self | ||
| Asserting & Separating | 1.02 (.03) | 1.28 (.50) |
| Disclosing & Expressing | 1.31 (.38) | 2.93 (.80) |
| Joyfully Connecting | 1.00 (.00)i | 1.20 (.16) |
| Trusting & Relying | 1.00 (.00)i | 1.65 (.67) |
| Deferring & Submitting | 1.00 (.00)i | 1.20 (.34) |
| Sulking & Scurrying | 1.00 (.00)i | 1.12 (.21) |
| Protesting & Recoiling | 1.00 (.00)i | 1.00 (.00)i |
| Walling off & Distancing | 1.00 (.00)i | 1.20 (.41) |
Not included in analyses because of lack of variance.
Results
Several significant shifts in both therapist and patient interpersonal process emerged after CBT was augmented with AFT (see Tables II and III for statistical results). All significant differences in therapist interpersonal process (except for Disclosing & Expressing) emerged on the “other” or “transitive” surface of the SASB (Surface 2). All significant differences in patient interpersonal process emerged on the “self-focused” or “intransitive” surface of the SASB (Surface 1).
Table II.
Analysis of changes in therapist SASB scores from CBT to AFT phases.
| 95% Wald CI (grand mean) | ||||||
|---|---|---|---|---|---|---|
| SASB item | Significant model effect | Wald x2 | CBT mean | AFT mean | Lower | Upper |
| Affirming & Understanding | Training condition | 169.29** | 2.12 | 3.23 | 2.54 | 2.81 |
| Nurturing & Protecting | Training condition | 106.34** | 2.78 | 1.59 | 2.04 | 2.31 |
| Watching & Controlling | Training condition | 47.88** | 1.48 | 1.02 | 1.17 | 1.32 |
| Disclosing & Expressing | Training condition | 39.35** | 1.09 | 1.51 | 1.24 | 1.36 |
| Asserting & Separating | N/A | 1.10 | 1.01 | 1.00 | 0.09 | 1.00 |
| Loving & Approaching | N/A | 1.97 | 1.04 | 1.08 | 1.03 | 1.08 |
| Belittling & Blaming | N/A | 2.90 | 1.03 | 1.00 | 0.99 | 1.03 |
Note. No significant findings had interaction effects.
p ≤ .05.
p ≤ .01.
Table III.
Analysis of changes in patient SASB scores from CBT to AFT phases.
| SASB item | Significant model effect | Wald x2 | CBT mean | AFT mean | Lower | Upper | |
|---|---|---|---|---|---|---|---|
| Disclosing & Expressing | Training Condition | 149.91** | 2.27 | 3.52 | 2.78 | 3.01 | |
| Trusting & Relying | Training Condition | 51.96** | 2.07 | 1.21 | 1.52 | 1.76 | |
| Deferring & Submitting | Training Condition | 33.60** | 1.33 | 1.01 | 1.11 | 1.22 | |
| Sulking & Scurrying | Training Condition | 21.22** | 1.20 | 1.02 | 1.07 | 1.15 | |
| Walling Off & Distancing | Training Condition | 4.16* | 1.29 | 1.04 | 1.05 | 1.28 | |
| Joyfully Connecting | N/A | 0.29 | 1.07 | 1.08 | 1.04 | 1.10 | |
| Belittling & Blaming | N/A | 0.53 | 1.08 | 1.04 | 1.01 | 1.12 | |
| Watching & Controlling | N/A | 1.96 | 1.02 | 1.00 | 0.99 | 1.03 | |
| 95% Wald CI | |||||||
| SASB Item | Significant Model Effect | Wald x2 | Time of AFT | Modality | Mean | Lower | Upper |
| Asserting & Separating | Interaction (Condition × Time of Implementation) | 4.46* | 8 | CBT | 1.17 | 0.99 | 1.36 |
| AFT | 1.38 | 1.13 | 1.63 | ||||
| 16 | CBT | 1.04 | .99 | 1.09 | |||
| AFT | 1.63 | 1.29 | 1.95 | ||||
Note. No significant findings but Asserting & Separating had interaction effects.
p ≤ .05.
p ≤ .01.
Consistent with hypothesis 1, therapists in AFT showed significantly less evidence of both Watching & Controlling (Cluster 5, Surface 2) and Nurturing & Protecting (Cluster 4, Surface 2) interpersonal process than they did in CBT training. Complementing this shift in therapist interpersonal process, patients in AFT showed significantly less evidence of Deferring & Submitting process (Cluster 5, Surface 1) than they did in CBT. Further, patients in AFT displayed significantly less evidence of Trusting & Relying (Cluster 4, Surface 1) process than they did in CBT.
Consistent with hypothesis 2, therapists in AFT showed more evidence of Affirming & Understanding (Cluster 2, Surface 2) process than they did in CBT training. Also, consistent with hypothesis 2, patients in AFT showed more evidence of Disclosing & Expressing (Cluster 2, Surface 2) process than they did in CBT. In addition, patients in AFT showed more evidence of self-assertion, i.e. Asserting & Separating (Cluster 1, Surface 1) than they did in CBT.
Consistent with hypothesis 3, therapists in AFT showed more evidence of Disclosing & Expressing (Cluster 2, Surface 1) process than they did in CBT training. As noted above, patients in AFT also demonstrated an increase in Disclosing & Expressing process.
Our findings did not support the first part of hypothesis 4: Therapists in AFT did not show less evidence of the hostile interpersonal processes of Belittling &Blaming (Cluster 6, Surface 2) or Ignoring & Neglecting (Cluster 8, Surface 2) than they did in CBT training. Consistent with the second part of hypothesis 4, however, patients in AFT did show decreases in hostile interpersonal processes of both Walling off & Distancing (Cluster 8, Surface 1) and Sulking & Scurrying (Cluster 6, Surface 1).
Consistent with our hypotheses, the majority of significant differences between training modalities in both therapist and patient interpersonal processes emerged regardless of time of implementation of AFT (session 8 or session 16). Moreover, there were for the most part no training modality × time interactions. The one exception was Asserting & Separating (Cluster 1, Surface 1). Here we found that patients whose therapists switched to AFT in session 8 displayed significantly more evidence of Asserting & Separating process than patients whose therapists switched to AFT in session 16.
Discussion
The majority of the findings were consistent with our hypotheses. Although we have summarized our results sequentially in a fashion that corresponds to our hypotheses, it may be useful at this point to discuss their implications as a whole (see Figures 2 & 3). Therapists in AFT were less likely to display controlling interpersonal process than they were during CBT training. They showed less evidence of both Watching & Controlling process (controlling interpersonal process that is neutral with respect to the affiliation dimension) and less evidence of Nurturing & Protecting process (controlling process that is friendly in nature). Therapists in the AFT phases were also more Affirming & Understanding (a friendly autonomy-granting behavior) than they were in CBT training. Finally, therapists in AFT tended to self-disclose (Disclosing & Expressing) more than they did in CBT training.
Figure 2.
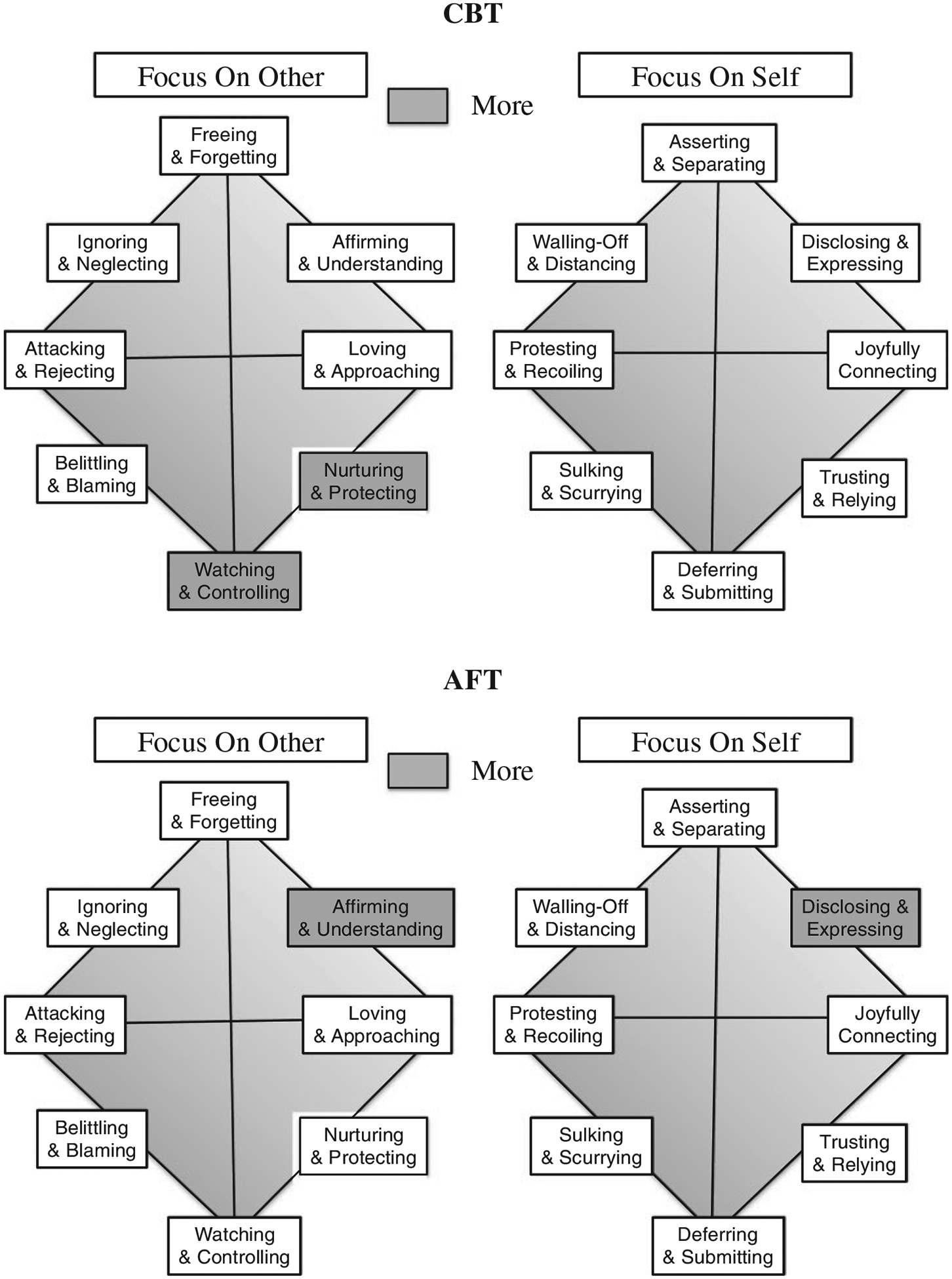
Therapist results on the Focus on Other and Focus on Self surfaces of the SASB. Shaded items in the top two figures were rated significantly higher in the CBT phase relative to the AFT phase of treatment. Shaded items in the bottom two figures were rated significantly higher in AFT than CBT.
Figure 3.
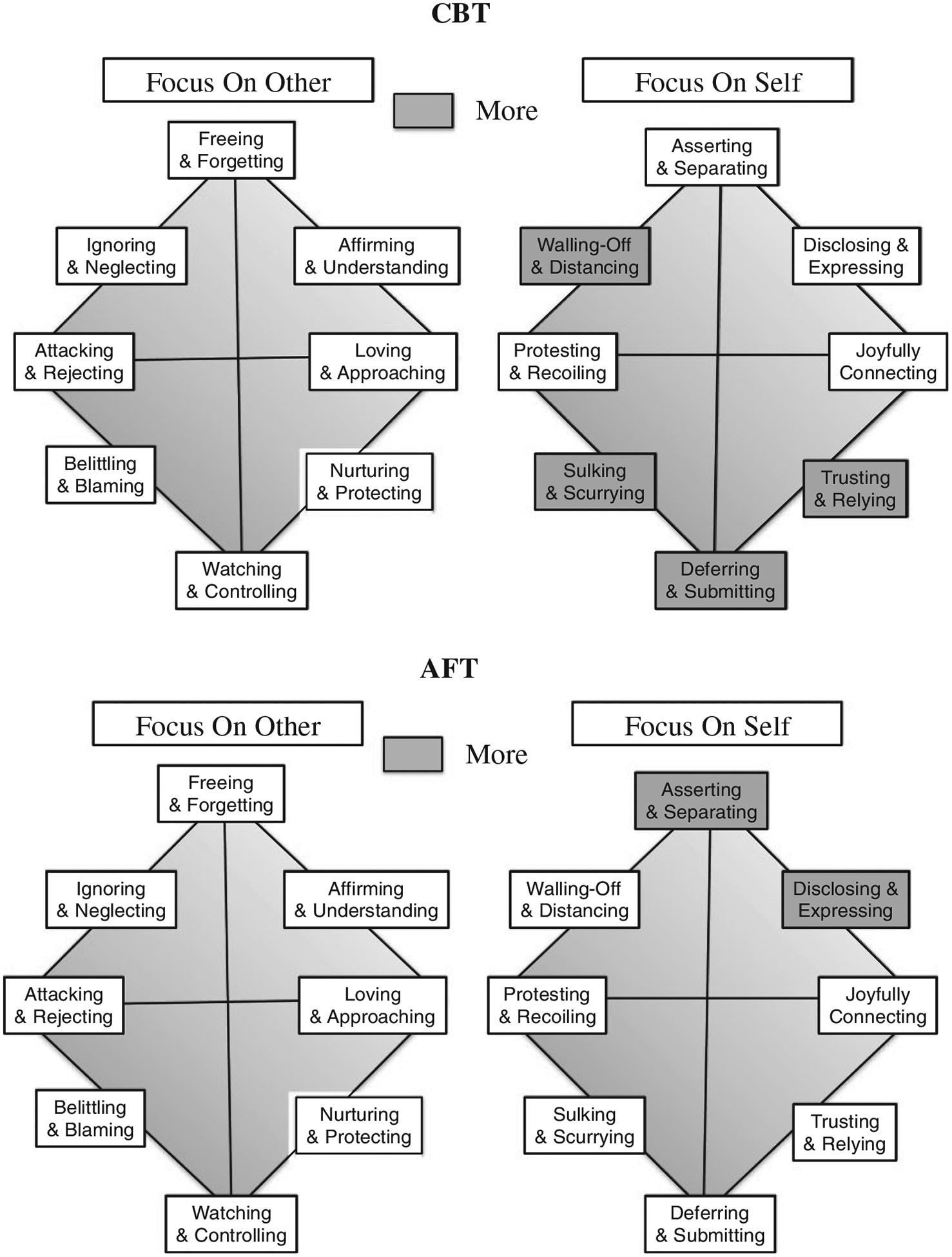
Patient results on the Focus on Other and Focus on Self surfaces of the SASB. Shaded items in the top two figures were rated significantly higher in the CBT phase relative to the AFT phase of treatment. Shaded items in the bottom two figures were rated significantly higher in AFT than CBT.
Patients in the AFT phases tended to display complementary shifts in interpersonal process. First, they displayed less submissive interpersonal process, both (1) less friendly-submissive process (Trusting & Relying) and (2) less submissive process that is neutral with respect to affiliation (Deferring & Submitting). They also displayed more interpersonal process of a self-disclosing nature. Finally, consistent with therapists’ shift towards a less controlling and more autonomy-encouraging stance, patients in AFT displayed an increase in Asserting & Separating interpersonal process.
It is worth noting that some previous studies (e.g., Henry et al., 1986; Henry, Schacht, & Strupp, 1990) found that patient interpersonal process that is coded as Asserting & Separating on the SASB was associated with poor outcome. In this particular context, however patient movement in the direction of greater self-assertion is consistent with the goals of AFT. There are two reasons for this: First, facilitating patient self-assertion in relationship to the therapist is considered to be an important component of the rupture resolution process (Safran & Muran, 1996, 2000). Especially in the context of alliance ruptures, it is considered important for patients to have the experience of telling their therapists what they want from them and from the treatment, rather than hiding their feelings and concerns for fear of alienating their therapists. Second, it is important to bear in mind that the patients in this study were primarily cluster C patients, who tend to present with problems with excessive compliance, deference, and avoidance. For this particular subgroup of patients, movement in the direction of increased self-assertion is likely to be a desirable outcome of therapy.
The finding that this difference was even more pronounced when AFT commenced at the earlier time interval (session 8), while not anticipated, is also not surprising. It stands to reason that the process of being able to assert oneself in relationship to the therapist may take more time, especially with this population. A possible explanation is that, while therapists may be able to change their interpersonal stance in a direction that encourages greater patient self-assertion after as few as 14 sessions of AFT (i.e., when AFT begins at session 16), and while patients may be able to begin to shift their stances in corresponding fashion, additional time may help to strengthen or facilitate patients’ ability to assert themselves.
As previously stated, although these changes have been described separately for simplicity, in actuality they occurred in a more holistic fashion. This type of process can be illustrated with the following clinical example. In one session in the CBT phase, the patient expressed difficulty with the previous session’s homework assignment and apprehension about therapy tasks. The therapist adopted a friendly yet dominant stance, and explained the rationale for the homework and therapy tasks, indicating how they would help alleviate the patient’s symptoms. The therapist’s stance was coded as Nurturing & Protecting. The patient, who loudly sighed and expressed both doubts and anxiety with therapy tasks, ultimately complied. The patient’s reluctant submission was captured through a code of Sulking & Scurrying.
In contrast, during the AFT phase, when the patient experienced a similar apprehension about therapy tasks, the therapist metacommunicated the following: “I’m getting the sense that this feels really difficult. Almost like I’m asking you to face what you fear the most.” This utterance, coded as therapist Disclosing & Expressing, was not dominating of the other as in the previous example. The patient did not submit or display self-focused hostility as in the previous example, but rather disclosed her experience in a friendly and autonomous way, which was coded as Disclosing & Expressing: “Yeah… I don’t know… it is like, I can hold onto the fact that I know that it’ll be helpful, but it really is tough for me.”
Finally, while we did not find that therapists in the CBT phases were more likely to display hostile interpersonal process than they did in AFT, we did find more evidence of hostile patient interpersonal process in CBT phases. However, it is possible that the therapist dominance seen in CBT (as in the clinical example above) represents a subtle form of hostility that is difficult to detect using the SASB, which requires that codes be made purely based on observable behavior. It was not uncommon for therapists in the AFT phases to retrospectively report in supervision groups that they had been experiencing subtle feelings of frustration and irritation towards their patients during CBT phases of treatment that they had not discussed extensively with their CBT supervisors. It is possible that such feelings had been leaking out in the form of subtle nonverbal manifestations of hostility which were sensed at some level by their patients, thus contributing to their tendency towards hostility (albeit of a self-focused or intransitive nature).
It is worth noting that these patients did not show the type of other-focused hostility (Belittling & Blaming, Attacking & Rejecting, Ignoring & Rejecting that has been found to be associated with poor outcome (e.g., Henry et al., 1986, 1990). However, both Walling Off & Distancing and Sulking & Scurrying acts are still forms of hostile patient interpersonal process that are associated with poor outcome (Henry et al., 1986, 1990). In this respect, it is important to bear in mind that the distinction between hostility coded on the self-focused versus the other-focused surfaces of the SASB is not one of intensity, but rather one of directionality. In other words, hostile interpersonal behavior coded on the other-focus surface is directed at the therapist, whereas hostility on the self-focused surface of the SASB tends to be less direct (examples will be given in the final discussion). Another way of looking at it is that this self-focused form of hostility is more likely to manifest as what we have termed a withdrawal rupture, in which the patient moves away from the therapist, than a confrontation rupture, in which the patient moves against the therapist. Again, this is not surprising given this particular population of patients.
Study 2
Our aim in study 2 was to explore whether AFT had any impact on therapists’ tendency to engage in the type of experientially grounded self-reflection about their relationships with their patients that AFT attempts to promote. It has been theorized that therapists who have difficulty becoming aware of their own negative countertransference feelings may inadvertently engage in hostile or complex communications outside their awareness and, as a consequence, perpetuate a vicious circle of hostility and counterhostility (Safran & Muran, 2000). In addition, a failure to fully attend to one’s own countertransference feelings can play an important role in keeping therapists embedded in negative transference/countertransference enactments (Safran & Muran, 2000; Safran & Reading, 2008).
As previously indicated, an important component of AFT involves training therapists to attend to their own internal experience and to accept it in a nonjudgmental fashion. This study examined the impact of AFT on therapists’ capacity for experientially grounded reflection and awareness. We hypothesized that AFT would enhance therapists’ capacity to explore and make constructive use of their own affectively grounded experience with their patients. Using interview data collected at time intervals that capitalized on the multiple baseline design, we tested the hypothesis that therapists would demonstrate an increase in their tendency to engage in experientially grounded reflection about their relationships with their patients after undergoing AFT, regardless of whether they began the training after session 8 (in which case they received AFT for 22 sessions) or session 16 (in which case they received AFT for 14 sessions).
This dimension of therapists’ reflective style was assessed with the use of a semi-structured interview designed to probe for therapists’ tendency to reflect on their own internal experience when responding to questions about their relationships with the patients they were treating in the study. This interview, known as the Therapist Relationship Interview (TRI; Safran & Muran, 2007) was then coded with the Experiencing Scale (EXP; Klein, Mathieu, Gendlin, & Kiesler, 1969). Although the EXP Scale is typically used for the purposes of coding patient material in therapy sessions, we reasoned that it could serve as a meaningful measure of the relevant therapist processes in the current context. Furthermore, in a previous study using the same measures, we found that higher levels of therapist EXP on the TRI were associated with an increased proportion of resolved to unresolved alliance ruptures over the course of treatment (Kazariants, 2011).
Method
Therapist Relationship Interviews (TRIs) were conducted with all therapists before the switch from CBT to AFT, and at the end of treatment. Specifically, therapists who switched from CBT to AFT after session 8 were interviewed at session 8, and therapists who switched from CBT to AFT after session 16 were interviewed at session 16. All therapists were also administered the TRI at termination. The aim of this design was to enable us to evaluate whether increases in EXP were attributable specifically to AFT rather than maturation effects. Increases in therapists’ capacity for experientially grounded reflection were not expected to be contingent on the amount of time spent in AFT.
Sample.
Due to missing TRI data for many of the cases used in Study 1 (at either termination, or at session eight or 16), only 10 of the cases from that study could be included in the present study. These 10 cases were augmented with an additional 13 cases from the larger ongoing study that had complete TRI data. The resulting sample included 13 cases that switched from CBT supervision to AFT at session 8, and 10 cases that switched at session 16. The sample included 11 men and 12 women patients (N = 23) ranging from 23 to 67 years of age (M = 48.35, SD = 13.77). Most patients identified as White (78.3%), and one as African American (4.3%), while others did not specify (17.4%). The majority of the patients met criteria for an Axis I diagnosis (78.3%), with seven meeting for major depression (30%), two for generalized anxiety disorder (8.7%), one for dysthymia (4.3%), one panic disorder with agoraphobia (4.3%), four for past episode of major depression (17%), and one eating disorder in full remission (4.3%). The remaining patients (21.7%) were not given an Axis I diagnosis. All patients in this study had a Cluster C or PD-NOS diagnosis on Axis II. Seven met for Avoidant PD (30%), eight met for Obsessive Compulsive PD (35%), and eight for Personality Disorder not otherwise specified (35%, with one Depressive PD). Therapists were 22 clinical psychology externs and one psychiatry resident. Eight of the therapists were male (34.8%) and 15 female (65.2%), and they ranged in age from 26 to 39 (M = 29.22, SD = 3.37). Most therapists identified as White (87%), two therapists identified as Hispanic/Latino (8.7%), and one as Asian or Pacific Islander (4.3%).
Measures.
The Therapist Relationship Interview (TRI; Safran & Muran, 2007) is a semi-structured interview designed to probe for therapists’ memories, thoughts, and reflections about a specific patient they have been treating. It consists of nine open-ended questions and a number of follow-up questions asking about the therapist’s experience of his or her relationship with the patient. Administration time is 45–60 minutes. The objective of the TRI is to elicit a sample of therapists’ verbal account of their experiences, which can then be coded for quality and style of reflection. For example, therapists are asked to choose five adjectives that reflect how they feel about the patient and to then elaborate on each adjective. Additional questions ask therapists whether there is anything about this specific patient that they find puzzling. Considerable attention in the TRI is given to moments of tension in the therapeutic relationship, and to negative process. Examples of relevant questions include: “Did you experience any moments of conflict, disagreement, misunderstanding, or tension in your relationship with your patient; or a particular time when you felt rejected, attacked, or criticized by your patient?” “Can you describe a specific time that happened?” “When did this occur? What did you do? How did your patient respond? What was your understanding of the cause? What was your initial feeling or experience of it?” “Have you ever felt your patient would end therapy?” and “Have you ever felt criticized, rejected or attacked by your patient?”
The questions in the TRI are open-ended; they give therapists the freedom to respond in a fashion that is as personal, emotionally distant, or factual as they wish. Each TRI was videotaped and administered by the program’s research assistants, who were instructed to closely follow the protocol with minimal use of personal judgment. TRIs were administered by trained interviewers twice: Once at the point of the switch from CBT into AFT (either session 8 or 16), in order to assess the impact of CBT on their tendency to reflect on the work with their patients in an experientially grounded fashion, and a second time at the end of treatment (session 30), to determine whether their tendency to reflect on the therapeutic relationship increased after undergoing AFT.
The Experiencing Scale (EXP; Klein, Mathieu-Coughlan, & Kiesler, 1986) is an observer rated coding system that assesses the extent to which an individual makes sense of events by reflecting on internal experience. EXP measures the level to which one attends to feelings as they emerge and integrates these feelings into a personally involved appraisal of external events. EXP assesses the quality of an individual’s verbalizations along a 7-point scale. On the lower end of the scale, the person’s narratives focus on the description of other people or events in which they themselves are not personally involved. At the higher end of the EXP scale, the speaker struggles to elaborate on his or her implicit, felt sense of what is going on in a given event. The quality of the narrative is described in a personally involved fashion with attention placed on feelings in order to expand the speaker’s understanding of the personal meaning of the event. Coders give an EXP rating for each of the interviewee’s speech turns. For this study, the mode and the peak EXP ratings for each interview were entered into the analyses.
The coders consisted of 10 Master’s level psychology graduate students who attended weekly didactic trainings over 1 year led by one of the co-authors. Experiencing ratings have been shown to be equivalent whether determined by audio recordings or printed transcriptions (Mathieu-Coughlan & Klein, 1984). Consistent with the guidelines contained in Klein et al’s. (1969) training manual, coders were trained until they reached reliability (ICC > .70) with the gold standard audio recordings across 20 segments. Once reliability was achieved using the gold standard as provided by the manual, coders then rated transcripts of TRIs that were not included in this study until the coders reached an ICC of .70 (two-way random effects model with consistency agreement on average measures) three times in a row. At that point, coders began coding the study data. Five coders independently coded each interview, and their ratings were averaged to form the mode and peak scores for each case.
Results
We used a mixed-design ANOVA in which the within-groups factor represented changes in therapists’ EXP levels on the TRI following AFT (regardless of whether they began AFT after sessions 8 or 16), and the between-groups factor represented time interval (i.e., whether AFT began after session 8 or 16). The means and standard deviations are presented in Table IV. Consistent with our hypothesis, we found a significant main effect for training modality on both mode and peak EXP scores. Mode EXP scores were significantly higher for therapists administered TRIs after AFT phases of training than after CBT phases of training, regardless of whether AFT began after session 8 or 16, F(1,21) = 5.015, p = .036. The same finding emerged for EXP peak scores for TRI interviews after the AFT phase compared to peak EXP scores after the CBT phase, F(1,21) = 4.613, p = .044. As predicted, there were no significant main effects for time interval on either EXP mode (F(1,21) = .008, p = .93) or peak (F(1,21) = 1.832, p = .19), and no training modality by time interval interaction on either EXP mode (F(1,21) = 1.73, p = .203) or peak (F(1,21) = .018, p = .895). Results were consistent with the hypothesis that after receiving AFT, therapists would demonstrate a greater tendency during TRI interviews to reflect on their relationships with their patients in a personally involved, experientially grounded fashion than they did after receiving CBT training. The absence of a significant main effect for time interval (session 8 or 16) on EXP mode or peak suggests that therapists’ increase in EXP was not likely to be simply a function of (1) receiving more supervision of any type or (2) working with and becoming familiar with a specific patient. The absence of a significant interaction between training modality and time interval for either mode or peak EXP suggests that therapists who switched at session 8 and received 22 sessions of AFT did not have significantly higher mode or peak EXP scores at termination than therapists who switched at session 16 and received only 14 sessions of AFT.
Table IV.
Mean EXP mode and peak scores (standard deviations)
| EXP mode | EXP peak | |||
|---|---|---|---|---|
| Condition | Interview 1 (post CBT) | Interview 2 (post AFT) | Interview 1 (post CBT) | Interview 2 (post AFT) |
| Switch at 8 (n = 13) | 2.18 (.27) | 2.50 (.34) | 3.30 (.41) | 3.53 (.58) |
| Switch at 16 (n = 10) | 2.28 (.35) | 2.37 (.44) | 3.08 (.40) | 3.35 (.38) |
| Total (N = 23) | 2.22 (.31) | 2.44 (.39) | 3.20 (.41) | 3.45 (.50) |
Discussion
This study investigated the impact of alliance-focused training on therapists’ tendency to reflect on their relationships with their patients in a personally involved and experientially grounded fashion. We hypothesized that following alliance-focused training, therapists would be more likely to respond to an interview protocol designed to probe for their reflections about their therapeutic relationships with higher levels of EXP than they would following CBT training (and before commencing AFT). Results were consistent with our hypotheses. After receiving AFT therapists were more inclined to explore and share their own personal feelings and reactions to their patients with interviewers than they were following CBT training. In other words, they showed a greater tendency to reflect on their relationships with their patients in a fashion that made reference to their own felt experience in an attempt to make sense of these relationships.
For example, during the Therapist Relationship Interview (TRI) administered at the end of the CBT phase, when one therapist in this sample was asked, “Is there anything that puzzles you or that you find challenging in your work with your patient?” she gave the following response: “… it’s been hard to pin down what she [the patient] wants to get out of the entire endeavor. It’s clear that she was in a great deal of pain when she came in, and she would like for that pain to be eased, but she has had real difficulty conceptualizing what she wants to be happening.” The therapist’s response was coded as level two on the EXP scale because personal feelings, thoughts and reflections were not referred to directly, but the beginning of a personal perspective on therapeutic events was beginning to emerge.
During the second TRI, which occurred after AFT, the same therapist responded to the question above by explicitly disclosing her own inner thoughts and feelings, “I guess initially I felt that it was hard to create a comfortable place for Susan (a pseudonym for the patient) to share and disclose with me and I guess I felt a little hesitant to force disclosure … I guess I felt like it was hard to be flexible and I felt that Susan needed a lot of flexibility on my part. I also felt like there were times in our work together when I had no idea what was going to happen when Susan came in ….” After AFT the therapist’s remarks were coded at level four on the EXP scale: The “quality of involvement or ‘set’ shifts to the speaker’s attention to the subjective felt flow of experience as referent, rather than events or abstractions” (Klein et al., 1969, p. 23).
The absence of significant main effects for time interval suggests that our findings are not likely to be solely attributable to maturation effects. The absence of a significant interaction between training modality and time interval suggests that receiving an additional eight sessions of AFT did not have an incremental effect on therapists’ tendency towards experientially grounded reflection over and above the first 8 sessions of AFT. Although the interaction between training interval and time interval was not significant, a graphical representation of the interaction does suggest a trend towards higher EXP levels for those therapists who received more alliance-focused training, and it is possible that a larger sample with more statistical power would have yielded a significant interaction. Certain features of the design also precluded our exploration of other types of training modality × time interactions. For example, the absence of a pure CBT training modality with TRI interviews administered at sessions 8, 16 and at termination makes it impossible to examine whether therapist EXP levels on the TRI increase over time as a result of CBT training in and of itself. To summarize, the present study provides preliminary evidence that alliance-focused training has the capacity to enhance a style of therapist reflection hypothesized to be advantageous in the context of therapeutic interactions that are vulnerable to negative therapeutic process or potentially problematic transference-countertransference enactments, and that has been found to be related to the process of alliance rupture resolution (Kazariants, 2011).
General Discussion and Conclusion
Taken together, the findings of studies 1 and 2 provide intriguing preliminary evidence regarding the potential of alliance-focused training to have a positive impact on both in-session interpersonal process, and on therapists’ capacity to reflect on the therapeutic relationship in a fashion that incorporates their own felt experience. One possible methodological limitation worth considering is the question of whether SASB and EXP coders were able to distinguish between therapeutic modalities (and the TRIs associated with them) and if so whether this might have biased their coding. While we cannot rule out the possibility that they were able to distinguish between CBT versus AFT material, they were blind to study hypotheses.
A second question concerns the degree of variability in the ways therapists implemented the AFT aspects of treatment. Given the fact that supervisors worked collaboratively with trainees to tailor the timing and degree of implementation of AFT-related interventions, our general sense is that there was considerable variability in this respect. While the finding of modality-specific differences in SASB codes provide us with a global picture of how therapists intervened during AFT phases relative to CBT phases, a more detailed picture of the various ways that therapists blended CBT and AFT interventions will need to be obtained through the examination of treatment adherence ratings that assess the extent to which different therapists incorporated various blends of CBT and AFT interventions into their treatments.
And finally, further research will be essential to evaluate whether differences in SASB and EXP ratings are related to ultimate outcome. As we indicated earlier, since all patients received some combination of CBT and AFT, we did not expect to find between-group differences in treatment outcome. It will, however, be critical to examine whether differences in treatment process are meaningfully related to one another and predictive of treatment outcome. At the present time, we continue to enter more patients and therapists into the larger, ongoing research project, and will be in the position to examine these questions in the future.
Funding
The research was supported by a grant from the National Institute for Mental Health [MH071768] (Principal Investigator: J. Christopher Muran).
References
- Anderson T, Knobloch-Fedders LM, Stiles WB, Ordonez T, & Heckman BD (2012). The power of subtle hostility in psychotherapy: A speech acts analysis. Psychotherapy Research, 22, 348–362. doi: 10.1080/10503307.2012.658097 [DOI] [PubMed] [Google Scholar]
- Aron L (1996). A meeting of minds: Mutuality in psychoanalysis. Hillsdale, NJ: Analytic Press. [Google Scholar]
- Baldwin SA, Wampold BE, & Imel ZE (2007). Untangling the alliance-outcome correlation: Exploring the relative importance of therapist and patient variability in the alliance. Journal of Consulting and Clinical Psychology, 75, 842–852. doi: 10.1037/0022-006X.75.6.842 [DOI] [PubMed] [Google Scholar]
- Baranackie K, & Crits-Cristoph P (1992). The Quantitative Assessment of Interpersonal Themes (QUAINT) Rater Manual. Unpublished manuscript.
- Beck AT, Freeman AM, & Associates. (1990). Cognitive therapy of personality disorders. New York: Guilford Press. [Google Scholar]
- Bein E, Anderson T, Strupp H, Henry WP, Schacht TE, Binder J, & Butler S (2000). The effects of training in Time-Limited Dynamic Psychotherapy: Changes in therapeutic outcome. Psychotherapy Research, 10, 119–132. doi: 10.1080/713663669 [DOI] [PubMed] [Google Scholar]
- Benjamin J (1990). An outline of intersubjectivity: The development of recognition. Psychoanalytic Psychology 7 (Suppl.), 33–46. doi: 10.1037/h0085258 [DOI] [Google Scholar]
- Benjamin LS (1974). Structural analysis of social behavior. Psychological Review, 81, 392–425. doi: 10.1037/h0037024 [DOI] [Google Scholar]
- Benjamin LS (1994). SASB: A bridge between personality theory and clinical psychology. Psychological Inquiry, 5, 273–316. doi: 10.1207/s15327965pli0504_1 [DOI] [Google Scholar]
- Binder JL, & Strupp HH (1997). “Negative process”: A recurrently discovered and underestimated facet of therapeutic process and outcome in the individual psychotherapy of adults. Clinical Psychology: Science and Practice, 4, 121–139. doi: 10.1111/j.1468-2850.1997.tb00105.x [DOI] [Google Scholar]
- Bromberg P (1998). Standing in the spaces: Essays on clinical process, trauma, and dissociation. Hillsdale, NJ: Analytic Press. [Google Scholar]
- Crits-Christoph P,Gibbons MBC,Crits-Christoph K, Narducci J,Schamberger M, & Gallop R (2006). Can therapists be trained to improve their alliances? A preliminary study of alliance-fostering psychotherapy. Psychotherapy Research, 16, 268–281. doi: 10.1080/10503300500268557 [DOI] [Google Scholar]
- Eubanks-Carter C, Muran JC, & Safran JD (2010). Alliance ruptures and resolution. In Muran JC & Barber JP (Eds.), The therapeutic alliance: An evidence-based approach to practice and training (pp. 74–94). New York, NY: Guilford Press. [Google Scholar]
- Goldfried MR (1994). Considerations in developing a core assessment battery. In Strupp HH, Horowitz LM, & Lambert MJ (Eds.), Measuring patient changes (pp. 99–116). Washington DC: American Psychological Association. [Google Scholar]
- Harris AE (2011). The relational tradition: Landscape and canon. Journal of the American Psychoanalytic Association, 59, 701–735. doi: 10.1177/0003065111416655 [DOI] [PubMed] [Google Scholar]
- Henry WP, Schacht TE, & Strupp HH (1986). Structural analysis of social behavior: Application to a study of interpersonal process in differential psychotherapeutic outcome. Journal of Counseling and Clinical Psychology, 54, 27–31. doi: 10.1037/0022-006X.54.1.27 [DOI] [PubMed] [Google Scholar]
- Henry WP, Schacht TE, & Strupp HH (1990). Patient and therapist introject, interpersonal process, and differential psychotherapy outcome. Journal of Consulting and Clinical Psychology, 58, 768–77. doi: 10.1037/0022-006X.58.6.768 [DOI] [PubMed] [Google Scholar]
- Henry WP, Strupp HH, Butler SF, Schacht TE, & Binder JL (1993). Effects of training in time-limited dynamic psychotherapy: Changes in therapist behavior. Journal of Consulting and Clinical Psychology, 61, 434–440. doi: 10.1037/0022-006X.61.3.434 [DOI] [PubMed] [Google Scholar]
- Horvath AO, Del Re AC, Flückiger C, & Symonds D (2011). Alliance in individual psychotherapy. Psychotherapy, 48, 9–16. doi: 10.1037/a0022186 [DOI] [PubMed] [Google Scholar]
- Kazariants G (2011). The relationship between therapist capacity for experientially grounded reflection on the therapeutic relationship and alliance rupture resolution. ProQuest, UMI Dissertation Publishing. [Google Scholar]
- Kiesler DJ (1996). Contemporary interpersonal theory and research: Personality, psychopathology and psychotherapy. New York: John Wiley & Sons. [Google Scholar]
- Klein MH, Mathieu PL, Gendlin ET, & Kiesler DJ (1969). The experiencing scale: A research and training manual. Madison: University of Wisconsin Extension Bureau of Audio-visual Instruction. [Google Scholar]
- Klein MH, Mathieu-Coughlan P, & Kiesler DJ (1986). The Experiencing Scales. In Pinsof WP & Greenberg LS (Eds.), The psychotherapeutic process: A research handbook (pp. 21–71). New York, NY: Guilford Press. [Google Scholar]
- Luborsky L, Rosenthal R, Diguer L, Andrusyna TP, Berman JS, Levitt JT, Seligman DA, & Krause ED (2002). The Dodo bird verdict is alive and well - mostly. Clinical Psychology: Science and Practice, 9, 2–12. doi: 10.1093/clipsy/9.1.2 [DOI] [Google Scholar]
- Mathieu-Coughlan P, & Klein MH (1984). Experiential psychotherapy: Key events in client-therapist interaction. In Rice LN & Greenberg LS, (Eds.), Patterns of change. New York: Guilford Press. [Google Scholar]
- Mitchell SA (1988). Relational concepts in psychoanalysis. Cambridge, MA: Harvard University Press. [Google Scholar]
- Muran JC (2002). A relational approach to understanding change: Plurality and contextualism in a psychotherapy research program. Psychotherapy Research, 12, 113–138. [Google Scholar]
- Muran JC, Safran JD, & Eubanks-Carter C (2010). Developing therapist abilities to negotiate alliance rupture. In Muran JC & Barber JP (Eds), The therapeutic alliance: An evidence-based guide to practice (pp. 320–340). New York: Guilford Press. [Google Scholar]
- Muran JC, Safran JD, Samstag L, & Winston A (2005). Evaluating an alliance-focused treatment for personality disorders. Psychotherapy, 42, 512–531. doi: 10.1037/0033-3204.42.4.532 [DOI] [Google Scholar]
- Persons JB, & Silberschatz G (1998). Are results of randomized controlled trials useful to psychotherapists? Journal of Consulting and Clinical Psychology, 66, 126–135. doi: 10.1037/0022-006X.66.1.126 [DOI] [PubMed] [Google Scholar]
- Pizer SA (1998). Building bridges: The negotiation of paradox in psychoanalysis. Hillsdale, NJ: Analytic Press. [Google Scholar]
- Safran JD (2002). Brief relational psychoanalytic treatment. Psychoanalytic Dialogues, 12, 171–195. doi: 10.1080/10481881209348661 [DOI] [Google Scholar]
- Safran JD (2012). Psychoanalysis and psychoanalytic therapies. Washington DC: American Psychological Association. [Google Scholar]
- Safran JD, & Muran JC (1996). The resolution of ruptures in the therapeutic alliance. Journal of Consulting and Clinical Psychology, 64, 447–458. doi: 10.1037/0022-006X.64.3.447 [DOI] [PubMed] [Google Scholar]
- Safran JD, & Muran JC (2000). Negotiating the therapeutic alliance: A relational treatment guide. New York: Guilford Press. [Google Scholar]
- Safran JD, & Muran JC (2006a). Has the concept of the alliance outlived its usefulness? Psychotherapy, 43, 286–291. doi: 10.1037/0033-3204.43.3.286 [DOI] [PubMed] [Google Scholar]
- Safran JD, & Muran JC (2006b). Resolving therapeutic impasses. CustomFlix. http://www.amazon.com. [Google Scholar]
- Safran JD, & Muran JC (2007). Therapist Relational Interview: Administration manual. Unpublished manuscript.
- Safran JD, & Reading R (2008). Mindfulness, metacommunication and and affect regulation in psychoanalytic treatment. In Hick S & Bien T (Eds.), Mindfulness and the therapeutic relationship (pp. 112–140). New York, NY: Guilford. [Google Scholar]
- Safran JD, Muran JC, Samstag L, & Stevens C (2001). Repairing therapeutic alliance ruptures. Psychotherapy, 38, 406–412. doi: 10.1037/0033-3204.38.4.406 [DOI] [Google Scholar]
- Safran JD, Muran JC, Samstag LW, & Winston A (2005). Evaluating an alliance focused treatment for potential treatment failures. Psychotherapy, 42, 512–531. [Google Scholar]
- Safran JD, Muran JC, & Eubanks-Carter C (2011). Repairing alliance ruptures. Psychotherapy, 48, 80–87. doi: 10.1037/a0022140 [DOI] [PubMed] [Google Scholar]
- Safran JD, Muran JC, Stevens C, & Rothman M (2008). A relational approach to supervision: Addressing ruptures in the alliance. In Falender CA & Shafranske EP (Eds.), Casebook for clinical supervision: A competency-based approach (pp. 137–157). Washington DC: APA Books. [Google Scholar]
- Stern DB (1998). Unformulated experience: From dissociation to imagination in psychoanalysis. Hillsdale, NJ: Analytic Press. [Google Scholar]
- Stiles WB, Honos-Webb L, & Surko M (1998). Responsiveness in psychotherapy. Clinical Psychology: Science and Practice, 5, 439–458. doi: 10.1111/j.1468-2850.1998.tb00166.x [DOI] [Google Scholar]
- Strupp H (1980). Success and failure in time-limited psychotherapy. Archives of General Psychiatry, 37, 947–954. doi: 10.1001/archpsyc.1980.01780210105011 [DOI] [PubMed] [Google Scholar]
- Strupp H (1993). The Vanderbilt psychotherapy studies: synopsis. Journal of Consulting and Clinical Psychology, 61, 431–433. doi: 10.1037/0022-006X.61.3.431 [DOI] [PubMed] [Google Scholar]
- Strupp HH, & Hadley SW (1979). Specific vs. nonspecific factors in psychotherapy: Controlled study of outcome. Archives of General Psychiatry, 36, 1125–1136. doi: 10.1001/archpsyc.1979.01780100095009 [DOI] [PubMed] [Google Scholar]
- Turner AE, & Muran JC (1992). Cognitive-behavioral therapy for personality disorders: A treatment manual. San Diego, CA: Social & Behavioral Documents. [Google Scholar]
- Turner AE, Muran JC, & Ochoa E (2004). Cognitive-behavioral therapy for personality disorders: A treatment manual (Updated Version). New York: Beth Israel Medical Center. [Google Scholar]
- Wampold BE (2001). The great psychotherapy debate: Model, methods, and findings. Mahwah, NJ: Lawrence Erlbaum. [Google Scholar]
- Wampold B, Mondin GW, Moody M, Stich F, Benson K, & Ahn H (1997). Psychological Bulletin, 122, 203–215. doi: 10.1037/0033-2909.122.3.203 [DOI] [Google Scholar]


