Abstract
Heart failure (HF) is a growing epidemic, affecting millions of people worldwide, and is a major cause of mortality, morbidity, and impaired quality of life. Traditional cardiac rehabilitation is a valuable approach to the physical and quality-of-life recovery of patients with cardiovascular disease. The innovative approach of remote monitoring through telemedicine offers a solution based on modern technologies, enabling continuous collection of health data outside the hospital environment. Remote monitoring devices present challenges that could adversely affect patient adherence, resulting in the risk of dropout. By applying a cognitive-behavioral model, we aim to identify the antecedents of dropout behavior among patients adhering to traditional cardiac rehabilitation programs and remote monitoring in order to improve the latter. Our study was conducted from October 2023 to January 2024. In the first stage, we used data from literature consultation. Subsequently, data were collected from the direct experience of 49 health workers related to both remote monitoring and traditional treatment, recruited from the authors’ workplace. Results indicate that patients with cardiovascular disease tend to abandon remote monitoring programs more frequently than traditional cardiac rehabilitation therapies. It is critical to design approaches that take these barriers into account to improve adherence and patient satisfaction. This analysis identified specific antecedents to address, helping to improve current monitoring models. This is crucial to promote care continuity and to achieve self-management by patients in the future.
Keywords: cardiac rehabilitation, remote monitoring, drop-out, cognitive behavioral analysis
1. Introduction
1.1. Heart Failure: A Growing Global Epidemic
Heart failure (HF) is a growing global epidemic affecting more than 37.7 million people worldwide [1] and it represents a major cause of mortality, morbidity, hospitalization, and poor quality of life. Heart failure is defined as a clinical syndrome characterized by the inability of the heart to pump blood through the body at a rate adequate for its needs, or to do so only at the cost of high filling pressures because of functional or organic abnormalities [2].
1.2. Promoting Recovery in Heart Failure Treatment: Key Role of Remote Monitoring
Cardiac rehabilitation (CR) is a key component of HF treatment as it aims to improve quality of life and reduce hospitalizations through education, exercise, stress management, and lifestyle modification [3]. Both in-person rehabilitation and remote monitoring aim to promote patient recovery [4]. Remote monitoring of heart failure patients through telemedicine is an approach that takes advantage of modern technologies to receive health care and continuously collect data on sick individuals outside the hospital setting [5]. This approach has led to a reduction in hospital admissions and length of stay because it allows for early intervention in case of changes in the patient’s health status [6]. In addition, it can be accompanied by psychological support services that help patients manage the stress and anxiety related to their medical condition [7]. In the elderly and their caregivers, remote monitoring increases peace of mind and reduces disease-related distress and anxiety related to physical distance from the hospital. Patients are actively involved through access to real-time data via apps or online platforms; this allows for more informed and responsible participation in their own well-being [8]. Four types of data can be monitored: (I) symptoms, e.g., shortness of breath and fatigue; (II) behaviors or events, e.g., medication compliance and physical activity; (III) biological data acquired noninvasively through external devices, e.g., body weight, blood pressure, heart rate, and ECG; (IV) biological data acquired invasively through implantable devices, e.g., intracardiac blood pressure [9]. The data provided by remote monitoring can promote patient empowerment by actively involving the patient in managing their health and making them more aware of the factors that influence their condition.
1.3. Addressing Limitations and Preventing Abandonment of Remote Monitoring
Despite the progress and benefits of monitoring from the literature, limitations emerge that could be enhanced. Asynchronous contact, such as through email, could negatively affect the quality of patient-clinician interaction as decreased empathy and loss of meaningful nonverbal information. This can lead to feelings of loneliness, especially for those who find comfort and support in medical appointments. Remote monitoring devices may have a complex interface that is difficult for the elderly to understand, which could generate frustration and constant calls for help to caregivers. Patients with physical limitations may find it difficult to use remote monitoring dis-positive devices, especially if these are not designed with their specific needs in mind. For example, those with visual impairment may have difficulty viewing the screen and may require constant assistance from a caregiver. In addition, there may be problems with the Internet in rural areas, where the high-speed connection may be limited, subject to interruptions, or totally absent. These difficulties could prompt patients to drop out of the monitoring program. Finally, if patients do not perceive the importance of remote monitoring to their well-being or if they are not sufficiently motivated to take care of their health, they may be less inclined to continue participating.
Therefore, it is essential to design approaches that consider aspects that result in dropout behaviors to avoid discontinuation and improve patient satisfaction. The effectiveness of remote monitoring for heart failure patients could be increased through cognitive behavioral analysis.
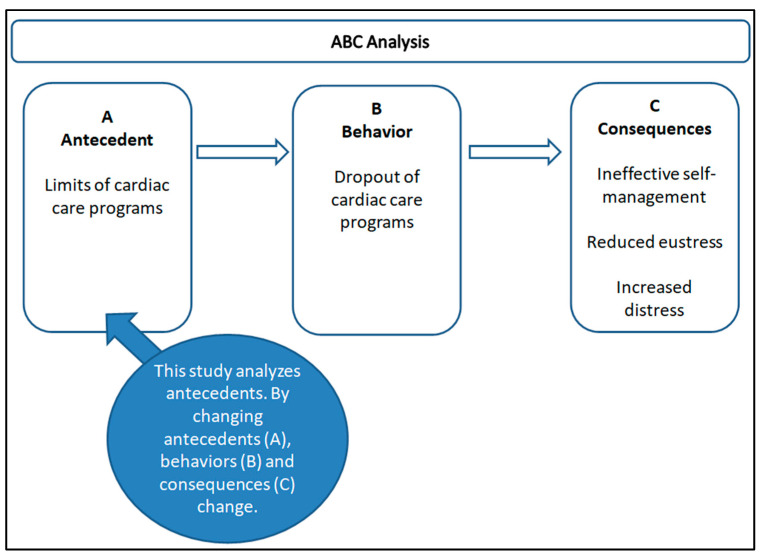
1.4. Cognitive Behavioral Analysis: Antecedents, Consequences and Function of Behavior
Cognitive behavioral theories tend to be linear, explaining why behavior may occur by considering a number of predictors and how these might influence the likelihood of a behavior [10]. One must look at what comes before, that is the antecedents (A), and what comes after, that is the consequence (C); such analysis can explain the function of the behavior (B). The analysis of antecedents allows one to identify the motivations that increase and decrease the occurrence of a behavior [11]. Therefore, if a certain behavior occurs frequently after a specific event, that event can be considered a significant antecedent. Similarly, observing the consequences of the behavior helps to understand how they influence its repetition: if a behavior produces a positive consequence, it is more likely to be repeated. This in-depth understanding of antecedent factors and consequences is essential for developing effective intervention strategies.
1.5. Aims
The objective of our study is to identify behavioral antecedents on which to base more effective models. Initially, this was conducted with a literature consult and successively by administering questionnaires to health care providers who participated in remote monitoring and traditional treatment.
2. Materials and Methods
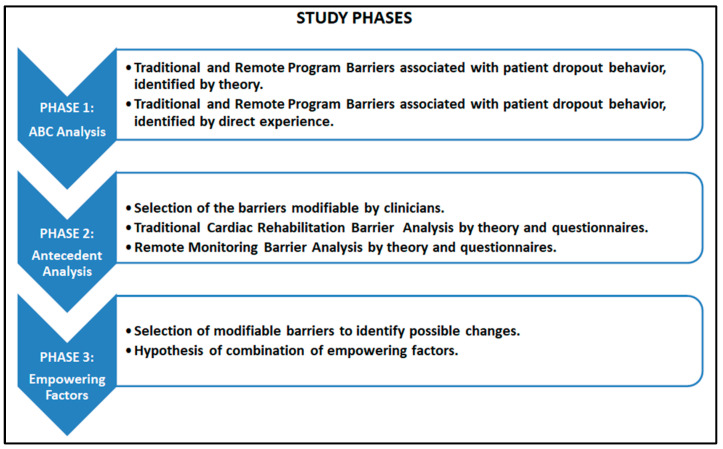
From October 2023 to January 2024, our research was conducted. In the present study, data from the literature and data from the direct experience of 49 health workers recruited at the authors’ workplace were used. See Figure 1 for a detailed description of the three phases of the study.
Figure 1.
Study phases.
2.1. Phase 1: ABC Analysis
We examined the scientific literature, consulting meta-analysis studies and systematic reviews in major databases such as PubMed and Cochrane, to analyze the participation of patients with heart failure and other cardiovascular diseases in rehabilitation and remote monitoring programs. Studies have identified possible causes of patients’ abandonment behavior. In addition, studies have assessed the factors that motivate patients to participate in traditional rehabilitation and remote monitoring. We collected professionals’ opinions through two specially prepared semi-structured online questionnaires ad hoc on the motivating and demotivating factors for patients’ participation in the relevant pathways expressed in the reviews analyzed [4,12]. One questionnaire was aimed at professionals with experience in traditional rehabilitation (doctors, nurses, and rehabilitators) and one questionnaire was aimed at professionals with experience in remote monitoring programs (doctors, nurses, rehabilitation, and telemedicine operators). Both questionnaires were completed anonymously and included a demographic section and a section of multiple-choice questions (ten multiple-choice questions for each questionnaire) with a Likert 0 to 5 scale on the strengths and weaknesses of the treatments analyzed. Finally, both questionnaires included two open-ended questions on the motivating and demotivating factors found in the patients. This analysis served to identify behavioral antecedents on which to build more effective models. The behavioral ABC concept analyzed is summarized in Figure 2.
Figure 2.
ABC Analysis.
2.2. Phase 2: Behavioral Antecedents
After the analyses in phase 1, we identified the behavioral antecedents of heart failure patients adhering to remote monitoring and conventional treatment. In particular, we selected modifiable barriers that can be manipulated by the clinicians.
2.3. Phase 3: Empowering Elements
Based on the previous steps, we hypothesized possible changes to be made and combined them with existing strengths to propose enhancing elements for monitoring programs.
3. Results
Below are the results of the literature consultation and those that emerged from the questionnaires on the direct experience of the 49 health workers involved.
3.1. Results of the Literature Consultation
Recent literature reviews and meta-analyses [4,12] show that the dropout rate for traditional cardiac rehabilitation ranges from 12% to 56%. In comparison, the dropout rate for remote monitoring shows even greater variability, ranging from 9% to 78% (see Table 1).
Table 1.
Literature consultation on dropout rates on traditional cardiology rehabilitation and remote monitoring.
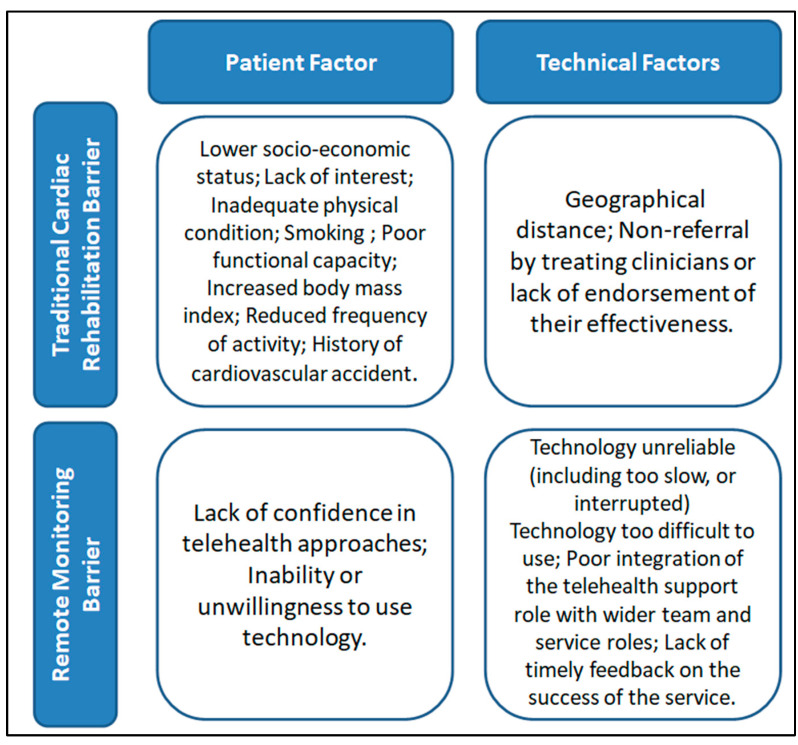
From the literature analysis, a higher dropout rate has emerged in remote monitoring programs compared to traditional rehabilitation. The reasons for dropout in both analyzed pathways were attributed to patient-related characteristics, as well as technical and logistical features (Figure 3). In addition, for traditional cardiac rehabilitation, patient-related causes were prevalent, while for remote monitoring programs, causes related to technical problems were prevalent.
Figure 3.
Results of the literature consultation. In traditional rehabilitation, patient-related barriers prevail. In remote monitoring, technology-related barriers prevail.
3.2. Results from the Analysis of Professionals’ Direct Experience
We reviewed a total of 49 responses from health care providers: 28 with experience in traditional care and 21 with experience in remote monitoring. For a detailed description of socio-demographic characteristics, see Table 2.
Table 2.
Socio demographic characteristics.
| Socio-Demographic Variables | Traditional Cardiac Rehabilitation | Remote Monitoring Program |
|---|---|---|
| Male | 13 | 8 |
| Female | 15 | 13 |
| Age ≤ 30 years | 2 | 2 |
| Age 31–50 years | 23 | 16 |
| Age ≥ 50 years | 3 | 3 |
| Work seniority 0–10 years | 10 | 5 |
| Work seniority 11–20 years | 13 | 13 |
| Work seniority 21–30 years | 4 | 3 |
| Work seniority > 30 years | 1 | / |
| Bachelor’s Degree | 8 | 3 |
| Master’s Degree | 13 | 13 |
| Postgraduate Degree | 7 | 5 |
3.3. Traditional Cardiac Rehabilitation
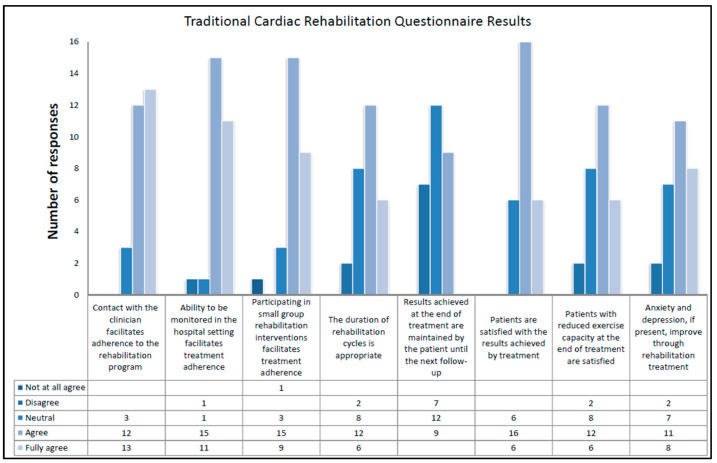
The results of traditional cardiac rehabilitation align with findings from the literature. In particular, professionals believe that the facilitating elements include the following: contact with the clinician (89%), in-hospital monitoring (92%), rehabilitation in small groups (86%), and satisfaction with the outcomes achieved through traditional treatment (79%). Experts hold contrasting opinions on the facilitating role of the duration of rehabilitation cycles, the maintenance of results until the next follow-up, and patient satisfaction with reduced exercise capacity. Professionals are also divided on the effectiveness of traditional rehabilitation in improving anxiety and depression. Specifically, 7% strongly disagree on the improvement of anxiety and depression, 68% assert that physical rehabilitation has a positive impact, and the remaining 25% remain neutral on this matter. For a detailed description, see Figure 4
Figure 4.
Results of questionnaires on traditional cardiac rehabilitation for each question.
Each professional who participated in the study answered two open-ended questions about the motivating and demotivating aspects for the patient who wants to undertake traditional rehabilitation. For a detailed description of the responses, see Table 3.
Table 3.
Responses to open-ended questions on the motivating and demotivating aspects of traditional rehabilitation.
| Indicate from Your Experience the Aspect That Most Motivates the Patient to Treatment. | Indicate from Your Experience the Aspect That Does Not Motivate the Patient to Treatment. |
|---|---|
| 1. Physical and mental recovery | 1. Logistical difficulties |
| 2. Participation in groups | 2. Depression |
| 3. Functional recovery, empathy of carers, the expectation of a better quality of life. | 3. Initial mistrust, socio-cultural barriers, resistance to lifestyle change, logistical difficulties in reaching the venue. |
| 4. Physical recovery, contact with the clinician, participation in groups | 4. Logistical difficulties, anxiety, depression |
| 5. Hospitality and professionalism | 5. Lack of information on the rehabilitation treatment to be carried out |
| 6. Physical recovery, contact with the clinician, participation in groups | 6. Logistical difficulties, anxiety, stress, depression |
| 7. Physical recovery, mood | 7. Anxiety, motivation |
| 8. Participation in groups | 8. Anxiety |
| 9. Direct contact with clinical staff | 9. Difficulties in reaching the facility, especially if physically distant |
| 10. Contact with the clinician | 10. Logistical difficulties |
| 11. Direct contact with the reference team | 11. Logistical difficulties in reaching the venue |
| 12. Physical recovery and psychological support | 12. Discouragement and lack of organization in rehabilitation activities |
| 13. Participation in small groups increases motivation and adherence | 13. Improving the organization |
| 14. / | 14. / |
| 15. Physical recovery | 15. Logistical difficulties |
| 16. Contact with the clinician | 16. Logistical difficulties |
| 17. Physical recovery | 17. Stress |
| 18. Contact with the clinician | 18. Stress |
| 19. Recovery of physical performance, rehabilitation activity in groups | 19. Still being busy with work and not reconciling with rehabilitation schedules. |
| 20. Contact with the reference team, participation in groups, physical recovery as far as possible | 20. Remoteness and difficulty in reaching the venue |
| 21. Therapeutic interaction, positive psychological attitude | 21. Depression |
| 22. Contact with the clinician | 22. Depression |
| 23. Physical recovery | 23. Depression |
| 24. Contact with the clinician | 24. Logistical difficulties |
| 25. Contact with the clinician | 25. Depression |
| 26. The pre-injury lifestyle | 26. Review |
| 27. Physical recovery | 27. Commitment required |
| 28. The perception of being taken care of and being looked after | 28. Lack of confidence in clinical treatment |
Experienced professionals in the field say the most motivating aspects of continuing traditional cardiac rehabilitation treatments are related to physical recovery (46%), participation in small groups (25%), psychological support (18%), and direct contact with referring physicians (39%). In contrast, demotivating aspects relate to logistical difficulties such as distance from the rehabilitation site (36%), the presence of anxiety and depression (43%), and aspects related to the organization of the service (14%).
3.4. Remote Monitoring Programs
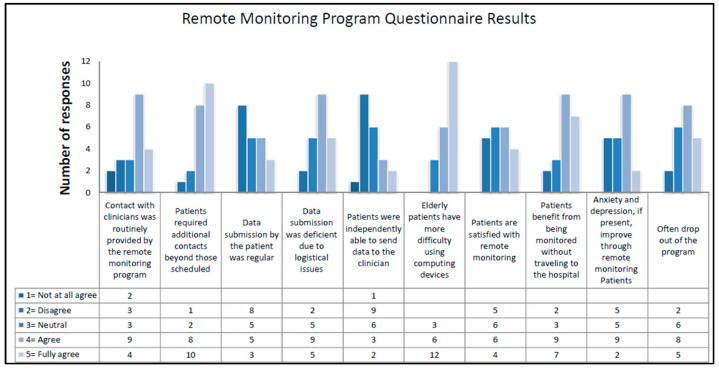
In this case, the results of remote monitoring programs align with those found in the literature analysis. It has been observed that remote monitoring programs involve routine contacts with clinicians (62%), although many professionals report that patients required additional contacts (86%). Overall, 66% of operators state that data submission was lacking due to logistical reasons, and patients were unable to independently send data collected by the device (48%), especially elderly patients (86%). A facilitating factor for participation in remote programs is the benefit of being monitored without having to visit the hospital. However, 61% affirm that dropout is frequent. Finally, 52% state that, if present, anxiety and depression improve with remote monitoring. Opinions on patient satisfaction with remote monitoring are favorable for 48%, neutral for 29%, and unfavorable for 23% (Figure 5).
Figure 5.
Results of questionnaires on remote monitoring programs for each question.
Each professional who participated in the study answered two open-ended questions about the motivating and demotivating aspects of remote monitoring for the patient. For a detailed description of the responses, see Table 4.
Table 4.
Responses to open-ended questions on the motivating and demotivating aspects of remote monitoring programs.
| Indicate from Your Experience the Aspect That Most Motivates the Patient to Remote Monitoring. | Indicate from Your Experience the Aspect That Does Not Motivate the Patient to Remote Monitoring. |
|---|---|
| 1. Having the peace of mind that it is monitored by a professional | 1. The complexity of the equipment |
| 2. Contact with the clinician | 2. Difficulties in handling equipment |
| 3. None | 3. Technical and logistical difficulties |
| 4. Difficulties in moving, potential convenience of the instrument, contact with the referring clinician. | 4. Excessively high number of instruments, network issues, intermittent contact with the clinician. |
| 5. Contact with the clinician | 5. Anxiety, stress, depression |
| 6. Contact with the clinician | 6. Anxiety, depression |
| 7. Contact with the clinician | 7. Anxiety |
| 8. The especially older patient prefers contact with the clinician | 8. Some patients cannot handle devices |
| 9. The possibility of being followed by clinicians without the need to travel to the facility | 9. The ‘duty’ to send parameters at set times, or at least punctual slots |
| 10. Contact with the clinician | 10. Stress |
| 11. Monitoring makes the patient feel calmer because they know they are constantly being monitored. 24-h monitoring also makes family members feel more relaxed. | 11. Complex applications that make it difficult to use, especially for elderly patients. Connection problems. |
| 12. Not feeling alone | 12. The thought of being abandoned by the clinician |
| 13. Ease with which the clinician can reach the patient | 13. Facial contact cannot be replaced with remote |
| 14. / | 14. / |
| 15. Contact with the clinician | 15. Stress |
| 16. The reduction of anxiety because they are constantly monitored | 16. Difficulties in using platforms |
| 17. Functional alternative | 17. Stress |
| 18. Contact with the clinician | 18. The obligation to send |
| 19. Knowing that there is continuous monitoring of their health status | 19. Equipment too complicated to send data |
| 20. Logistical difficulties, contact with referring clinicians if foreseen | 20. Connection difficulties, asynchronous and untimely communication |
| 21. Equity of access | 21. Technological difficulties |
Experienced professionals in the field say that the most motivating aspects of continuing remote monitoring programs are related to contact with physicians where provided (33%), reduction of anxiety due to continuous monitoring (29%), and reduction of geographic distances that promotes equity of access to care (14%). In contrast, demotivating aspects include the complexity of equipment and the process of sending data to the physician (57%), lack of contact with physicians (14%), and the presence of anxiety, depression, and stress (29%).
3.5. Proposal for Enhancement Elements
Based on the results obtained from remote monitoring and traditional treatment, we have identified factors on which the clinician can intervene through cognitive-behavioral analysis. The analysis is detailed in Table 5.
Table 5.
Behavioral antecedents and proposed improvement.
| Type of Intervention | Antecedent | Modifiable Exclusively by Clinicians | How to Change |
|---|---|---|---|
| Traditional Cardiac Rehabilitation | Non-referral by treating clinicians | Yes | Training in effective patient communication; Avoiding clinician turnover. |
| Lack of endorsement of clinicians effectiveness | Yes | Training in effective patient communication | |
| Lower socio-economic status | No | / | |
| Lack of interest | Yes | Implement health education and psychoeducation pathways | |
| Inadequate physical condition | No | / | |
| Geographical distance | No | / | |
| Smoking | No | / | |
| Poor functional capacity | No | / | |
| Increased body mass index | No | / | |
| History of cardiovascular accident | No | / | |
| Reduced frequency of activity | No | / | |
| Remote Heart Failure Monitoring | Lack of confidence in telehealth approaches | Yes | Training on methods and purpose of programs before recruitment |
| Preference for direct contact with clinician | Yes | Implement synchronous contacts with a team of referring clinicians | |
| Inability or unwillingness to use technology | Yes | Define simple and intuitive usability | |
| Technology unreliable (including too slow, or interrupted) | Yes | Verify network reliability through periodic testing | |
| Technology too difficult to use (user interface design, accessibility features, complexity of procedures, integration with other devices) | Yes | Define simple and intuitive usability | |
| Poor integration of the telehealth support role with wider team and service roles | Yes | Implement synchronous contacts with a team of referring clinicians | |
| Lack of timely feedback on the success of the service | Yes | Introduce immediate visual feedback to confirm correct data submission |
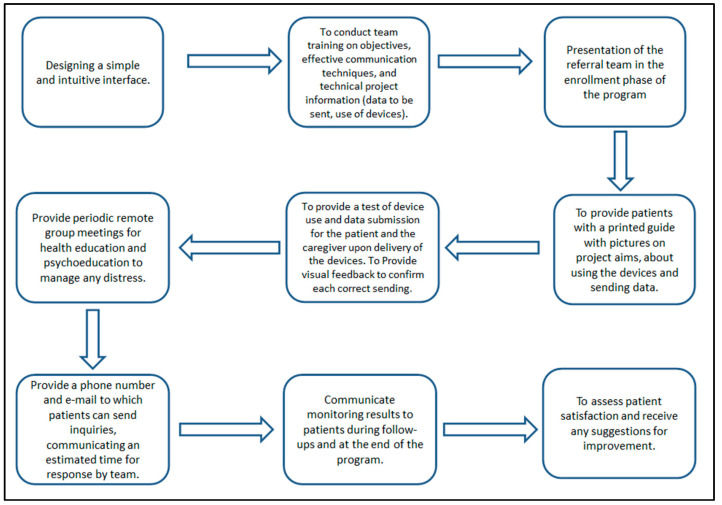
3.6. Identification and Implementation of Strategies for Improvement
This assessment allowed for the identification of reinforcing elements to address weaknesses and the inclusion of new elements deemed effective. For a detailed description of the reinforcing elements, see Figure 6.
Figure 6.
Elements of remote program enhancement.
4. Discussion
Our study analyzed the antecedents of the dropout behavior for two types of interventions. We examined the reasons for dropout in traditional cardiac rehabilitation programs to evaluate what motivates patients to complete the course. We also explored the reasons for dropout in remote monitoring programs to understand what leads patients to abandon the course. This examination allowed us to identify antecedents for intervention, enhancing current monitoring models.
The results highlight that patients with heart failure and other cardiovascular conditions are more likely to abandon remote monitoring programs compared to traditional cardiac rehabilitation treatments [13,14].
4.1. Traditional Cardiology Rehabilitation and Remote Monitoring
Traditional cardiology rehabilitation is characterized by direct and regular contact between patients and clinicians, establishing a solid bond of trust. During these personal interactions, patients benefit from immediate emotional support, instant feedback on their condition, and comprehensive assessment of their physical condition [3,7]. This type of approach encourages active patient involvement in the treatment process and promotes greater adherence to the rehabilitation program [4].
Remote monitoring represents an innovative mode of care that allows the physician to monitor the patient’s health status remotely, exploiting the potential of telemedicine. This approach offers numerous advantages, such as the ability to collect real-time data and detect changes in the patient’s vital parameters early [5,7]. It also offers greater flexibility and convenience for the patient, reducing the need for frequent hospital or outpatient visits. This means reduced costs associated with travel to follow-up appointments [9]. The use of remote monitoring allows health services to expand the scope of cardiac rehabilitation services without increasing the workload of health care personnel or the use of resources [8]. This can help improve the accessibility and coverage of rehabilitation services, ensuring that more patients can benefit from quality care, regardless of their geographic location or willingness to travel to the hospital.
The integration of traditional approaches and remote monitoring could optimise patient outcomes by combining the personal relationship of traditional rehabilitation with the convenience of telemedicine. This balance allows for personalised attention during face-to-face interactions and constant remote monitoring.
4.2. Determinants of Abandonment of Traditional Cardiac Rehabilitation and Remote Monitoring
Reasons for dropout in traditional cardiac rehabilitation are predominantly linked to patient-related factors [15] that clinicians cannot easily intervene in, such as age, socioeconomic status, and geographic distance, or can intervene minimally, such as reduced physical exercise capacity, resistance to lifestyle changes, and low interest [16,17,18]. An element that can be more readily addressed to reduce dropout in traditional cardiac rehabilitation is the establishment of a dedicated team [19], limiting excessive turnover of healthcare providers. Reasons for dropout in remote monitoring programs are mostly related to organizational and logistical factors that clinicians can modify, along with low patient motivation [4]. These factors include difficulties in technology use, especially among elderly patients, connectivity issues, and limited contact with designated clinicians [20,21]. Special attention should be given to scheduling contacts with clinicians. Even in Boriani et al.’s study [22], comparing exclusively outpatient monitoring with remote monitoring, the number of unscheduled visits for patients monitored remotely was four times higher than those in the standard monitoring group [23]. Participation in small groups can promote adherence to traditional cardiac rehabilitation treatments and can also be an effective coping strategy for patients with heart failure. The group allows patients to share their experiences and feelings with individuals facing similar challenges. This can reduce the sense of isolation and promote treatment adherence. Therefore, introducing periodic group meetings could influence the patient’s ability to engage in remote monitoring programs.
4.3. Application of Functional Behavioral Assessment to Reduce Patient Abandonment
Functional Behavioral Assessment (FBA) includes a descriptive process that identifies the role of antecedent variables before the behavior and the consequences that follow the analyzed problem behavior [24]. Improving the scheduling of monitoring programs reduces patient dropout. FBA techniques include various assessment tools, including interviews. A problem behavior can be improved by intervening in the antecedents or consequences that maintain it [10]. The cognitive behavioral approach is a methodology that combines the principles of cognitive and behavioral psychology to understand and modify dysfunctional behaviors. This approach has become an increasingly valuable tool used in a variety of clinical and organizational settings because behavioral analysis enables the planning of health services and interventions that improve the quality of care and effectiveness of treatment. In our study, it was found that, in traditional cardiac rehabilitation, the factors that can be changed solely by the physician are: lack of referral from treating physicians, lack of approval of physician effectiveness, and lack of interest. These factors can be modified through: training on effective communication with the patient, reduction of physician turnover, and implementation of health education and psychoeducation pathways. In remote monitoring, factors that can be modified solely by the physician include: lack of confidence in telemedicine approaches, preference for direct contact with the physician, inability or reluctance to use technology, unreliable technology, technology too difficult to use, and poor integration of the telemedicine support role with the broader team and service roles. These elements can be changed through: training on the methods and purposes of the programs prior to recruitment, implementing synchronous contact with a team of referring physicians, developing simple and intuitive usability, verifying the reliability of the network through periodic testing, and introducing immediate visual feedback to confirm correct data submission.
4.4. Limitations and Strengths
To our knowledge, our study is the first to propose enhancement elements for remote monitoring programs based on the limitations identified in the literature and the direct experience of healthcare professionals.
The main limitation of our study is not collecting the direct perspective of patients, which would undoubtedly be valuable to identify key issues. Potential errors and variability in health care providers’ responses are also a limitation. Providers may not be fully aware of all the difficulties faced by patients or may misinterpret the causes of their dropout. Through analysis of patients’ experiences and perceptions, it would be possible to identify specific factors contributing to the difficulty of adhering to monitoring programs. These factors could include technical problems, lack of adequate support, difficulty understanding instructions, or lack of motivation. Understanding the personal challenges and motivations underlying dropout behavior would provide important information for improving patient compliance and the effectiveness of remote monitoring programs in cardiac rehabilitation. Another limitation is the absence of the perspective of caregivers. These people, often family members or close acquaintances of patients, play a crucial role in the process of care and assistance. Their perspective provides a more comprehensive view of the challenges faced by patients, whether in traditional cardiac rehabilitation or remote monitoring. They accompany patients in their daily experiences, supporting them with difficulties such as technical problems and closely observing their progress and needs that are not always expressed directly.
Additionally, an analysis comparing traditional cardiac rehabilitation and remote monitoring has the inherent limitation of comparing different types of treatments, although physical activity is often monitored remotely as well [25,26]. These two approaches are the most widely used to support patients with heart failure and other cardiovascular conditions in recovering daily life activities [4]. In both remote monitoring and traditional treatment of cardiovascular disease, the goal is to provide patients with the tools and support they need to effectively manage their condition. In this way, it is possible to reduce distress (negative stress) [27] and increase eustress (positive stress) in patients. In remote monitoring, patients can experience a feeling of safety and well-being through regular monitoring of their vital parameters. In traditional treatment, patients are engaged in structured physical exercises and group therapy sessions that can help improve mood and reduce stress. In this way, reduced discomfort and increased eustress promote the patient’s overall well-being [28]. Cardiovascular diseases are a major social and economic problem [29] and remain the diseases with the highest mortality and morbidity rates [30].
4.5. Future Perspectives
Future perspectives on heart failure and other cardiovascular conditions management are moving towards patient self-management [21]. Self-management would allow patients to be independent in monitoring symptoms, understanding the need for medication readjustment, and discerning when to consult a physician [31]. However, achieving the ultimate goal of self-management requires guiding the patient to understand their clinical condition and the changes that occur over time. Following patients with standardized therapeutic and care pathways using traditional, remote, or integrated approaches can facilitate the achievement of self-management.
5. Conclusions
Traditional cardiac rehabilitation represents a historically valid approach in the recovery of physical capabilities and quality of life for patients with heart failure and other cardiovascular conditions. This treatment has the advantage of direct contact with clinicians and is well-tolerated by patients, with a lower treatment dropout rate compared to remote monitoring. Remote monitoring programs have developed more recently and offer the advantage of monitoring patients while overcoming logistical barriers such as geographic limitations. However, remote monitoring programs experience a higher dropout rate due to technical difficulties in using the equipment and the absence or intermittence of contact with clinicians. Implementing remote programs and preventing patient dropout is crucial because they serve as a valuable guide to steer patients towards self-management of the disease.
Author Contributions
Conceptualization: M.P. and F.C.; methodology: M.P., F.C. and I.C.; resources: P.B., A.D. and P.D.; validation: F.C., A.B. and M.G.; investigation: F.M.G. and G.M.; writing—original draft preparation: I.C. and M.P.; writing—review and editing: I.C. and A.A.; supervision: F.C.; data curation: M.P. and I.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Datasets are available to download on request. Requests should be directed to the corresponding author: Francesco Corallo, francesco.corallo@irccsme.it.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding Statement
This study was funded by the Italian Ministry of Health, Italian Health Operational Plan (Cohesion and Development Fund 2014–2020), trajectory 2 “eHealth, advanced diagnostics, medical devices, and mini-invasiveness”, under the project title “Sistema di Monitoraggio ed Analisi basato su intelligenza aRTificiale per pazienti affetti da scompenso CARdiaco cronico con dispositivi medici miniinvasivi e indossabili Evoluti-SMART CARE” (Project Code: T2-AN-10)—CUP I43C22000300001.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Darvishzadehdaledari S., Harrison A., Gholami F., Azadnia A. Examining the effectiveness of home-based cardiac rehabilitation programs for heart failure patients with reduced ejection fraction: A critical review. BMC Cardiovasc. Disord. 2023;23:593. doi: 10.1186/s12872-023-03640-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McDonagh T.A., Metra M., Adamo M., Gardner R.S., Baumbach A., Böhm M., Burri H., Butler J., Čelutkienė J., Chioncel O., et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2021;42:3599–3726. doi: 10.1016/j.rec.2022.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Lundgren K.M., Langlo K.A.R., Salvesen Ø., Zanaboni P., Cittanti E., Mo R., Ellingsen Ø., Dalen H., Aksetøy I.A. Feasibility of telerehabilitation for heart failure patients inaccessible for outpatient rehabilitation. ESC Heart Fail. 2023;10:2406–2417. doi: 10.1002/ehf2.14405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hannan A.L., Harders M.P., Hing W., Climstein M., Coombes J.S., Furness J. Impact of wearable physical activity monitoring devices with exercise prescription or advice in the maintenance phase of cardiac rehabilitation: Systematic review and meta-analysis. BMC Sports Sci. Med. Rehabil. 2019;11:14. doi: 10.1186/s13102-019-0126-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guzman-Clark J., Farmer M.M., Wakefield B.J., Viernes B., Yefimova M., Lee M.L., Hahn T.J. Why patients stop using their home telehealth technologies over time: Predictors of discontinuation in Veterans with heart failure. Nurs. Outlook. 2021;69:159–166. doi: 10.1016/j.outlook.2020.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dierckx R., Pellicori P., Cleland J.G.F., Clark A.L. Telemonitoring in heart failure: Big Brother watching over you. Heart Fail. Rev. 2015;20:107–116. doi: 10.1007/s10741-014-9449-4. [DOI] [PubMed] [Google Scholar]
- 7.Piotrowicz E., Mierzyńska A., Jaworska I., Opolski G., Banach M., Zaręba W., Kowalik I., Pencina M., Orzechowski P., Szalewska D., et al. Relationship between physical capacity and depression in heart failure patients undergoing hybrid comprehensive telerehabilitation vs. usual care: Subanalysis from the TELEREH-HF Randomized Clinical Trial. Eur. J. Cardiovasc. Nurs. 2022;21:568–577. doi: 10.1093/eurjcn/zvab125. [DOI] [PubMed] [Google Scholar]
- 8.Kitsiou S., Paré G., Jaana M. Effects of home telemonitoring interventions on patients with chronic heart failure: An overview of systematic reviews. J. Med. Internet Res. 2015;17:e63. doi: 10.2196/jmir.4174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abraham W.T., Perl L. Implantable hemodynamic monitoring for heart failure patients. J. Am. Coll. Cardiol. 2017;70:389–398. doi: 10.1016/j.jacc.2017.05.052. [DOI] [PubMed] [Google Scholar]
- 10.Badgett N., Falcomata T.S. A comparison of methodologies of brief functional analysis. Dev. Neurorehabilit. 2015;18:224–233. doi: 10.3109/17518423.2013.792298. [DOI] [PubMed] [Google Scholar]
- 11.Davis R., Campbell R., Hildon Z., Hobbs L., Michie S. Theories of behaviour and behaviour change across the social and behavioural sciences: A scoping review. Health Psychol. Rev. 2015;9:323–344. doi: 10.1080/17437199.2014.941722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turk-Adawi K.I., Grace S.L. Narrative review comparing the benefits of and participation in cardiac rehabilitation in high-, middle- and low-income countries. Heart Lung Circ. 2015;24:510–520. doi: 10.1016/j.hlc.2014.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duscha B.D., Piner L.W., Patel M.P., Craig K.P., Brady M., McGarrah R.W., 3rd, Chen C., Kraus W.E. Effects of a 12-week mHealth program on peak VO2 and physical activity patterns after completing cardiac rehabilitation: A randomized controlled trial. Am. Heart J. 2018;199:105–114. doi: 10.1016/j.ahj.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Skobel E., Knackstedt C., Martinez-Romero A., Salvi D., Vera-Munoz C., Napp A., Luprano J., Bover R., Glöggler S., Bjarnason-Wehrens B., et al. Internet-based training of coronary artery patients: The Heart Cycle Trial. Heart Vessels. 2017;32:408–418. doi: 10.1007/s00380-016-0897-8. [DOI] [PubMed] [Google Scholar]
- 15.Resurrección D.M., Moreno-Peral P., Gómez-Herranz M., Rubio-Valera M., Pastor L., de Almeida J.M.C., Motrico E. Factors associated with non-participation in and dropout from cardiac rehabilitation programmes: A systematic review of prospective cohort studies. Eur. J. Cardiovasc. Nurs. 2019;18:38–47. doi: 10.1177/1474515118783157. [DOI] [PubMed] [Google Scholar]
- 16.Suaya J.A., Shepard D.S., Normand S.-L.T., Ades P.A., Prottas J., Stason W.B. Use of Cardiac Rehabilitation by Medicare Beneficiaries After Myocardial Infarction or Coronary Bypass Surgery. Circulation. 2007;116:1653–1662. doi: 10.1161/circulationaha.107.701466. [DOI] [PubMed] [Google Scholar]
- 17.Oosenbrug E., Marinho R.P., Zhang J., Marzolini S., Colella T.J., Pakosh M., Grace S.L. Sex Differences in Cardiac Rehabilitation Adherence: A Meta-analysis. Can. J. Cardiol. 2016;32:1316–1324. doi: 10.1016/j.cjca.2016.01.036. [DOI] [PubMed] [Google Scholar]
- 18.Ruano-Ravina A., Pena-Gil C., Abu-Assi E., Raposeiras S., van ‘t Hof A., Meindersma E., Prescott E.I.B., González-Juanatey J.R. Participation and adherence to cardiac rehabilitation programs. A systematic review. Int. J. Cardiol. 2016;223:436–443. doi: 10.1016/j.ijcard.2016.08.120. [DOI] [PubMed] [Google Scholar]
- 19.Dalal H.M., Doherty P., Taylor R.S. Cardiac rehabilitation. BMJ. 2015;351:h5000. doi: 10.1136/bmj.h5000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Purcell R., McInnes S., Halcomb E.J. Telemonitoring can assist in managing cardiovascular disease in primary care: A systematic review of systematic reviews. BMC Fam. Pract. 2014;15:43. doi: 10.1186/1471-2296-15-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenhalgh T., A’court C., Shaw S. Understanding heart failure; explaining telehealth—A hermeneutic systematic review. BMC Cardiovasc. Disord. 2017;17:156. doi: 10.1186/s12872-017-0594-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boriani G., Da Costa A., Quesada A., Ricci R.P., Favale S., Boscolo G., Clementy N., Amori V., Stefano L.M.d.S., Burri H., et al. Effects of remote monitoring on clinical outcomes and use of healthcare resources in heart failure patients with biventricular defibrillators: Results of the MORE-CARE multicentre randomized controlled trial. Eur. J. Heart Fail. 2017;19:416–425. doi: 10.1002/ejhf.626. [DOI] [PubMed] [Google Scholar]
- 23.Yamashita R., Sato S., Sakai Y., Tamari K., Nozuhara A., Kanazawa T., Tsuzuku S., Yamanouchi Y., Hanatani S., Nakamura T., et al. Effects of small community walking intervention on physical activity, well-being, and social capital among older patients with cardiovascular disease in the maintenance phase: A randomized controlled trial. J. Phys. Ther. Sci. 2024;36:128–135. doi: 10.1589/jpts.36.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Edelson S.M. Understanding challenging behaviors in autism spectrum disorder: A multi-component, interdisciplinary model. J. Pers. Med. 2022;12:1127. doi: 10.3390/jpm12071127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li J., Yang P., Fu D., Ye X., Zhang L., Chen G., Yang Y., Luo H., Chen L., Shao M., et al. Effects of home-based cardiac exercise rehabilitation with remote electrocardiogram monitoring in patients with chronic heart failure: A study protocol for a randomised controlled trial. BMJ Open. 2019;9:e023923. doi: 10.1136/bmjopen-2018-023923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Senarath S., Fernie G., Fekr A.R. Influential Factors in Remote Monitoring of Heart Failure Patients: A Review of the Literature and Direction for Future Research. Sensors. 2021;21:3575. doi: 10.3390/s21113575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garcia M., Moazzami K., Almuwaqqat Z., Young A., Okoh A., Shah A.J., Sullivan S., Lewis T.T., Elon L., Ko Y.-A., et al. Psychological distress and the risk of adverse cardiovascular outcomes in patients with coronaryheart disease. JACC Adv. 2024;3:100794. doi: 10.1016/j.jacadv.2023.100794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen J., Dobron A., Esterson A., Fuchs L., Glassberg E., Hoppenstein D., Kalandarev-Wilson R., Netzer I., Nissan M., Ovsiovich R.S., et al. A randomized, controlled, blinded evaluation of augmenting point-of-care ultrasound and remote telementored ultrasound in inexperienced operators. Isr. Med. Assoc. J. IMAJ. 2022;24:596–601. [PubMed] [Google Scholar]
- 29.Stamenic D., Fitzgerald A.P., Gajewska K.A., O’Neill K.N., Bermingham M., Cronin J., Lynch B.M., O’Brien S.M., McHugh S.M., Buckley C.M., et al. Health care utilization and the associated costs attributable to cardiovascular disease in Ireland: A cross-sectional study. Eur. Heart J. Qual. Care Clin. Outcomes. 2024:qcae014. doi: 10.1093/ehjqcco/qcae014. [DOI] [PubMed] [Google Scholar]
- 30.Martin S.S., Aday A.W., Almarzooq Z.I., Anderson C.A., Arora P., Avery C.L., Baker-Smith C.M., Gibbs B.B., Beaton A.Z., Boehme A.K., et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation. 2024;149:e347–e913. doi: 10.1161/cir.0000000000001209. [DOI] [PubMed] [Google Scholar]
- 31.Yu D.S.F., Lee T.F.D., Kwong A.N., Thompson D.R., Woo J. Living with chronic heart failure: A review of qualitative studies of older people. J. Adv. Nurs. 2008;61:474–483. doi: 10.1111/j.1365-2648.2007.04553.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Datasets are available to download on request. Requests should be directed to the corresponding author: Francesco Corallo, francesco.corallo@irccsme.it.