Abstract
Obesity, primarily characterized by excessive fat accumulation, is a multifactorial chronic disease with an increasing global prevalence. Despite the well-documented epidemiology and significant advances in understanding its pathophysiology and clinical implications, the impact of sex is typically overlooked in obesity research. Worldwide, women have a higher likelihood to become obese compared to men. Although women are offered weight loss interventions more often and at earlier stages than men, they are more vulnerable to psychopathology. Men, on the other hand, are less likely to pursue weight loss intervention and are more susceptible to the metabolic implications of obesity. In this narrative review, we comprehensively explored sex- and gender-specific differences in the development of obesity, focusing on a variety of biological variables, such as body composition, fat distribution and energy partitioning, the impact of sex steroid hormones and gut microbiota diversity, chromosomal and genetic variables, and behavioural and sociocultural variables influencing obesity development in men and women. Sex differences in obesity-related comorbidities and varying effectiveness of different weight loss interventions are also extensively discussed.
Keywords: obesity, sex-related differences, gender-related differences, weight loss
1. Introduction
Obesity is defined as excessive fat accumulation that can have a negative impact on health [1]. Body mass index (BMI) is a commonly used parameter for obesity classification. Adults with a BMI greater or equal to 25 kg/m2 are considered overweight, and a BMI greater or equal to 30 kg/m2 is considered obese. Obesity has become an ongoing pandemic as its prevalence in adults has more than doubled since 1990 [1]. The global prevalence of overweight and obese in the year 2020 was estimated at 2603 million (38%) and 988 million (14%) people, respectively. The prevalence of obesity in males (14%) was lower than in females (18%). Sex-specific differences are evident in all regions of the world [2]. Data from 3663 population-based studies with 222 million participants from 197 countries covering more than 99% of the world’s population demonstrated that the global age-standardised prevalence of obesity has increased from 8.8% in 1990 to 18.5% in 2022 in women and from 4.8% in 1990 to 14.0% in 2022 in men [3]. The age-standardized prevalence of obesity in adults increased from 1990 to 2022 in 188 countries for women and in all except one country for men, leading to a more than 20% increase in 49 countries for women and 24 countries for men [3]. The largest increases in obesity in women were in some countries in sub-Saharan Africa. In men, obesity increased most in the USA, Brunei, and some countries in central Europe, Polynesia, and Micronesia. In some countries in the Caribbean, the Middle East, and north Africa, obesity increased in both sexes. The countries with the largest absolute numbers of adults with obesity in 2022 were the USA, China, and India [3]. In low-income countries, obesity is more common in urban areas among wealthier subjects, especially women. In high-income countries, both sexes are equally affected. However, there is a greater impact on groups of lower socioeconomic status [4]. The National Health and Nutrition Examination Survey (NHANES), conducted between 2017–2018, showed a higher prevalence of obesity in non-Hispanic black women than men, and no sex differences in other races. There were also significantly more women with severe obesity (BMI ≥ 40 kg/m2) [5].
World Obesity Atlas predicts obesity trends by the year 2035 by assessing published data from 1975 to 2016 [2]. In the future, the prevalence of obesity is forecasted to increase. An additional increase was evident after the COVID-19 pandemic in the years from 2020 to 2022 [2]. Restrictions of movement, troublesome access to medical care, and changes in diet and behaviour are few of the reasons for the worsening of obesity epidemics in that period [2]. According to predictions for the year 2035, prevalence will almost double. Projected numbers of overweight and obese are 4005 million (51%) and 1914 million (24%) people, respectively. Globally, obesity will still be more common in females (27%) than males (23%). Regionally, trends will be the same, except for European and the Western Pacific regions, where obesity in males will surpass obesity in females [2].
The epidemiology, pathophysiology, and clinical implications of obesity have been well documented [1,6]. Nevertheless, a neglected factor in earlier research is the impact of sex, as there has traditionally been a significant lack of female representation in pre-clinical and clinical research [7,8]. In 2016, with increasing awareness of the importance of this biological variable, the United States National Institutes of Health (NIH) accepted a policy requiring future researchers to include males and females in every experiment funded by the NIH, which has led to increasing reports of sex differences in a variety of research fields [8], including obesity. In this narrative review, we comprehensively summarize evidence of sex- and gender-specific differences in obesity pathogenesis, risk factors, and clinical implications. Table 1 summarises the main subsections and topic highlights.
Table 1.
Summary of variety of variables influencing sex and gender—specific differences in obesity.
| Variables Influencing Sex and Gender Dimorphism in Obesity | |
|---|---|
| Sex and Gender—Specific Differences underlying Obesity Pathology |
|
| Sex and Gender—Specific Risk Factors Influencing Obesity Pathology |
|
| Clinical Implications of Sex and Gender—Related Differences in Obesity |
|
2. Sex and Gender-Specific Differences Underlying Obesity Pathology
2.1. Differential Body Composition and Fat Distribution in Men and Women
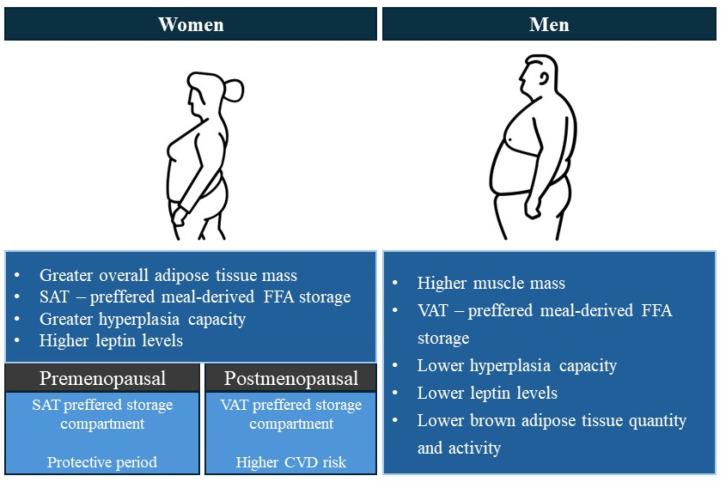
The main mechanism for obesity development is chronically increased energy intake and/or decreased energy expenditure [9]. The excess energy is stored in the adipose tissue with white adipose tissue (WAT) being the metabolic and endocrine organ that is the primary site of excess energy storage [9]. In times of positive energy balance WAT expands either by hypertrophy with an increase in cell size or by hyperplasia with an increase in cell number. The type of adipose tissue expansion differs depending on the depot and sex. Adipocyte hypertrophy is characteristic of the abdominal depot which is the main fat storage location in males, while adipocyte hyperplasia is more characteristic of the gluteofemoral depot which is the main fat storage location for females [10]. For the same BMI, the percentage of total adipose tissue in females is approximately 10% greater compared to males [11,12]. Although females have higher total body fat compared to males, males have higher visceral adipose tissue (VAT) [13]. The accumulation of fat derived from free fatty acids (FFA) and triglycerides is rate-limited by lipoprotein lipase (LPL) activity, which is higher in gluteal/subcutaneous fat depot in females and higher in the abdominal/visceral fat depot in males [14]. Therefore, females tend to store meal-derived FFA in the subcutaneous adipose tissue (SAT) in contrast to males, who preferably store meal-derived FFA in VAT [11,15]. Additionally, in premenopausal women, SAT has an increased ratio of alpha (α) 2 to beta (β) 1-2 adrenergic receptors, which leads to a decreased catecholamine—stimulated lipolysis compared to men and postmenopausal women. In premenopausal women, VAT has a reversed balance of adrenergic receptors, thus favouring lipolysis [16]. In times of positive energy balance, lower body SAT in females has a greater capacity for expansion by hyperplasia and is less responsive to catecholamine-stimulated lipolysis in contrast to the upper body fat [15]. Despite being a buffer for fat storage in periods of positive energy balance, increased gluteofemoral SAT has also been associated with a lower level of arterial calcifications and stiffness as well as improved lipid levels, implying atherosclerosis protection [17]. This sex-specific fat distribution is likely also connected to improved glucose metabolism and protection against diabetes development in premenopausal women, while preferential fat accumulation in the abdominal VAT in men is associated with an increased risk of metabolic disease [16]. A schematic highlighting the differential body composition and fat distribution in females and males is presented in Figure 1.
Figure 1.
Differential body composition and fat distribution in women and men.
On the other hand, brown adipose tissue (BAT) and the browning of white adipose tissue are crucial for energy expenditure functions [18]. Browning or beiging of adipocytes refers to the process by which WAT acquires characteristics similar to BAT, including increased mitochondrial content and the expression of uncoupling protein 1 (UCP1) [19]. Increasing BAT activation and browning of WAT can influence energy homeostasis and protect against obesity and obesity-related metabolic diseases [20]. BAT and the process of browning white adipocytes exhibit significant sexual dimorphism, potentially contributing to differences in obesity and metabolic disease risks between men and women. However, sex and gender differences in human thermogenic adipose tissue are still understudied. Studies have demonstrated that women generally have higher amounts of BAT and exhibit greater BAT activity through non-shivering thermogenesis compared to men [21,22,23]. This heightened activity is due to several factors, including hormonal influences and intrinsic cellular properties. Studies show that sex hormones regulate BAT activity in a sex-specific manner through direct and indirect mechanisms. Oestrogens induce a stimulatory effect on BAT activity, while androgens appear to have an inhibitory effect. The crosstalk between sex hormones and glucocorticoids adds to the mechanisms that control sexually dimorphic BAT activity [10,21]. In addition, women have more inducible beige adipocytes, within their subcutaneous fat depots compared to men. This is supported by evidence showing higher expression levels of genes related to mitochondrial function and thermogenesis in female adipocytes [24]. Furthermore, women display greater sensitivity to cold exposure, which enhances the browning process [24]. Studies have also suggested that oestradiol could regulate thermogenic adipose tissue at the central level via hypothalamic AMPK activation [25]. It is important to note that despite understanding the higher prevalence, mass, and activity of thermogenic adipose tissue and the initial clues of the physiological mechanisms behind these differences, the consequences for metabolic disease progression are still largely unknown beyond speculation [23].
Adipokines, such as leptin and adiponectin, secreted from adipose tissue also have a significant association in obesity pathogenesis and its metabolic complication [26].
Leptin is a peptide hormone and a well-known adipokine which interacts with leptin receptors in the hypothalamus and brainstem [27]. Leptin levels are in direct proportion to total fat content, and high levels inhibit food intake and increase lipolysis, thermogenesis, and energy expenditure [27]. Leptin levels have a higher correlation to SAT and thus are higher in females, and these differences seem to be more pronounced during puberty and decrease after menopause [10,27]. Since these sex-specific differences in adiposity appear at the onset of puberty and decrease after menopause in females or with declining testosterone in males, one can conclude that sex steroid hormones have a substantial impact on obesity development [10]. Adiponectin concentration is negatively connected to visceral adipose tissue content, and this finding is stronger in females compared to males [13]. This sexual dimorphism may be due to higher adiponectin mRNA expression in ectopic fat in females. A study by Christen et al. using MRI for quantification of abdominal SAT and VAT and measuring leptin and adiponectin levels showed that adiponectin levels are higher in females than in males, which is not completely explained by differences in VAT. On the other hand, leptin was also higher in females and was strongly related to total body fat [13]. Obesity is associated with higher leptin levels, lower adiponectin levels, and a higher leptin/adiponectin (L/A) ratio [28]. According to a study of 2258 children with overweight/obesity, girls with higher L/A ratios were more likely to have insulin resistance, glucose impairment, and dyslipidemia, while boys were more likely to have insulin resistance [28].
Some organokines, such as chemerin and betatrophin, have a role in glucose and lipid metabolism [29,30]. Chemerin acting through CMKLR1 is adipokine, the expression of which is influenced by metabolic status [29]. Chemerin levels correlate with BMI and waist-to-hip ratio and increase during development of impaired glucose tolerance or diabetes. Animal studies show that chemerin levels are increased in male compared to female rats at the pre-pubertal stage, and chemerin expression was attenuated in ovariectomized female rats but enhanced in orchiectomized male rats [29]. Its receptor, CMKLR1, on the other hand, showed no difference in its expression after gonadectomy but was markedly influenced by nutritional status, as its levels markedly decreased with high fat diet (HFD) [29]. Betatrophin acts as a hepatokine involved in triglyceride hepatic metabolism [30]. Betatrophin levels have a strong correlation with atherogenic lipoprotein subfraction. Betatrophin levels are higher in all subjects with type 2 diabetes or obesity and in females, but not in males, indicating a possible influence of oestrogen on betatrophin-mediated lipoprotein metabolism [30].
2.2. Differential Energy Expenditure in Men and Women
Daily energy expenditure is comprised of three components: activity-induced energy expenditure, diet-induced expenditure, and resting energy expenditure. Resting energy expenditure is determined by body size and composition and is the main component of the total energy expenditure [31]. Diet-induced energy expenditure for a mixed diet results in 10% of daily energy expenditure [32]. Physical activity-induced energy expenditure is defined by body size and movement and it is the most variable component of daily energy expenditure [33]. Activity-induced energy expenditure changes during different life stages as it increases from 20% at age 1 to around 35% at age 18 and decreases after age 50 [33]. The largest changes in body composition occur during adolescent growth, emphasizing the importance of physical activity from a young age. Physical activity is a determinant of peak fat-free mass, which is essential for preventing sarcopenic obesity later in life [31].
Data on 4240 individuals, out of which 1870 were twin pairs, explored the transition period from adolescence to young adulthood and showed that physical inactivity during adolescence significantly increased the risk of obesity in adulthood, especially central obesity [34]. In a monozygotic twin substudy, co-twins with obesity in adulthood were found to be less physically active in adolescence, and discordant monozygotic twins showed that obesity development was independent of genetic effects. Additionally physical activity also declined after developing obesity [34]. With increasing age, there is a decrease in physical activity levels, decrease in fat-free mass, and an increase in fat mass [33]. For males, changes in body composition during exercise training are highly related to initial fat mass, as subjects with higher initial fat mass lose more fat than leaner subjects. This was not seen in females [33]. Combining aerobic training with resistance exercises has been linked to decreased visceral fat in males and subcutaneous leg fat in females [35]. While physical activity intensity has been linked to fat loss in both sexes, physical activity duration has been linked to fat loss in males only [36].
There are clear sex differences in energy partitioning between males and females. In times of increased energy requirements, females oxidize a greater proportion of FFA, while males have a higher preference for using carbohydrates, thus increasing glycogen utilization. Postprandially or in resting conditions, females—in contrast to males—oxidize less FFA and tend to store FFA in adipose tissue [15,37]. Estradiol is responsible for reducing resting/postprandial lipid utilization by suppressing hepatic lipid oxidation while promoting skeletal muscle fatty acid oxidation during exercise and in postmenopausal females, overall lipid utilization is decreased [38]. Despite relying on lipid utilization during exercise, females are less likely to have a reduction in fat mass in resting conditions [15]. The strategy of lipid utilization during periods of prolonged exercise or food shortage provides females with a higher ability to spare protein mass which is a clear survival advantage. However, during times of food abundance, this survival advantage becomes a predisposition for obesity development [15].
2.3. Sex-Specific Roles of Sex Steroid Hormones
2.3.1. Lessons from Animal Models
Oestrogen acts on the central nervous system, particularly on the hypothalamus, which regulates body weight homeostasis and energy balance by controlling food intake and energy expenditure [38]. By activating oestrogen receptor (ER)α, prominently expressed on pro-opiomelanocortin (POMC) neurons within the arcuate nucleus, oestrogen modulates and suppresses food intake. Additionally by activating ERα in neurons of the ventromedial hypothalamus oestrogen also stimulates physical activity and thermogenesis and regulates fat distribution [38]. In adipose tissue, oestrogens can act on oestrogen receptors alpha (ERα) or oestrogen receptors beta (ERβ). Animal studies demonstrated that the distribution of these receptors is particularly important for oestrogen’s ability to modulate its effects on fat distribution [16,39,40]. ERα knockout mice had increased adiposity and visceral fat accumulation [40]. In ovariectomized mice [39], oestrogen substitution reduced visceral fat mass in wild-type and ERβ knockout mice, but not in ERα knockout mice, which indicates that the lipolytic effects of oestrogens are primarily mediated by ERα. The ERβ knockout mice had a greater reduction in visceral fat mass, which can suggest that ERβ activation may oppose oestrogen’s lipolytic effects mediated by ERα activation [16,39,41]. Males have a relative lack of ERα in the visceral depot, which can explain the preferential storage of fat in the visceral compartment [16,40]. Animal studies showed that despite female mice having a lesser propensity to obesity development when exposed to HFD than their male counterparts, the natural protective effect from HFD-induced obesity diminishes after ovariectomy, a type of surgical menopause [42]. Some also hypothesized that follicle-stimulating hormone (FSH) may also play a role in menopause-induced obesity, as blocking FSH interaction with its receptor by an administration of FSH antibodies protected both male and female mice against HFD-induced obesity by inducing the browning of WAT, thermogenesis, and increasing energy expenditure [43].
Testosterone is an androgen receptor (AR) agonist. AR distribution and expression are higher in VAT compared to SAT [44]. Testosterone can act on the AR or can also be converted to dihydrotestosterone (DHT) or oestradiol by 5α-reductase and aromatase, respectively. Dihydrotestosterone is a more potent androgen that cannot be aromatized to oestradiol [45]. A recent study by Sebo and Rodeheffer assessed the effect of testosterone deficiency and the individual contributions of testosterone, oestradiol, and dihydrotestosterone to body composition, total adiposity, and fat distribution by using mouse models with castration-induced hypogonadism that were fed a standard or HFD [45]. Hypogonadal mice gained more fat mass and less lean mass compared to controls on both diets, with the rate of fat gain being more pronounced in the HFD group, indicating that hypogonadism accelerates obesity development when dietary fat intake is high. Hypogonadism altered body composition but not fat distribution [45]. To evaluate the individual-specific contributions of different hormones on body composition and fat distribution, the castrated hypogonadal mice on HFD underwent hormone replacement therapy either with testosterone, oestradiol or DHT, and the gonadally intact mice were treated with aromatase inhibitors [45]. Testosterone replacement successfully reduced HFD-induced fat expansion in both visceral and subcutaneous depots. Oestradiol replacement only modestly reduced HFD-induced fat expansion in the visceral depot with no significant effect on subcutaneous fat, while DHT replacement had reduction only in subcutaneous fat with no significant reduction in total fat mass compared to controls. These findings suggest that testosterone replacement has an anti-obesogenic effect in a hypogonadal state [45]. The gonadally intact mice treated with aromatase inhibitors gained more fat, with a preferential increase in visceral fat accumulation compared to controls [45]. Since aromatase inhibitor therapy leads to a decrease in testosterone conversion to oestradiol, this gain in fat mass also implies that the anti-obesogenic effect of testosterone in males may be at least partly mediated by its conversion to oestradiol [45].
Testosterone also appears to be important for metabolic programming [46,47]. Studies on animal models showed that testosterone exposure and neonatal androgenization in female mice led to an increase in WAT with adipocyte hypertrophy, a decreased insulin-dependent lipogenesis, hypoadiponectinemia, and a decrease of the intensity of POMC neuronal projections within the arcuate nucleus. These changes led to increased food intake and hyperleptinemia with reduced ability to up-regulate POMC expression [46,47,48].
2.3.2. Insights from Human Physiology
Over the last 15 years, new insights into the links between sex steroid hormones and diet, eating behaviour, neuroendocrine control of energy homeostasis, and obesity have greatly expanded our knowledge of sex-specific human physiology of obesity. In premenopausal females, there is a higher ERα protein content in the abdominal than the gluteal depot, and ERβ protein is higher in the gluteal than the abdominal depot [49]. This higher ERα/β ratio in the visceral depot limits adipose fat accumulation, and a lower ERα/β ratio in the gluteal fat leads to preferential fat accumulation and storage in that depot [16]. Additionally, oestradiol also upregulates the number of the anti-lipolytic α-2a adrenergic receptors in SAT but not in VAT, leading to a diminished epinephrine-mediated lipolytic effect in SAT, which additionally shifts fat accumulation from VAT to SAT [50].
Given the complex relationship of these hormones in the etiopathogenesis of obesity, alterations in sex hormones are associated with various changes in body composition, fat distribution, and metabolic diseases. While all females gain SAT over time, with the decrease in oestrogen throughout menopause, energy expenditure and fat oxidation in females also decrease, which eventually leads to an increase in total body fat as well as VAT [51]. Thus, menopause, evident from a decrease in oestradiol levels and an increase in FSH, triggers a relative shift in adipose tissue accumulation, specifically from SAT to VAT accumulation, and this finding is partially reversed by oestrogen hormone replacement therapy [52]. Low oestrogen levels in menopause or premature ovarian insufficiency are also connected to increased risk of diabetes development [53], and hormonal replacement therapy seems to reduce this risk and improve glucose homeostasis [54,55].
There is a bidirectional relationship between obesity and testosterone. In a sex-specific, two-sample Mendelian randomization analysis, Loh et al. provided evidence of this bidirectional interplay by showing that in females, high bioavailable testosterone can be both a cause as well as consequence of obesity, while in males higher bioavailable testosterone was associated with lower hip circumference and lower fasting glucose and obesity was linked to lower bioavailable testosterone and higher oestradiol [56]. Subjects with prostate cancer treated with androgen deprivation therapy, on the other hand, have increased visceral abdominal fat and subcutaneous fat and a decrease in lean mass as a consequence of testosterone deficiency [57]. Age-related testosterone decline is also associated with a change in body composition, leading to an increase in fat mass and decrease in fat-free mass [58]. The effects of acute testosterone deficiency were studied by Santosa et al. in a prospective randomized trial, in which they found that acute testosterone withdrawal resulted in a greater meal-derived FFA storage in SAT by increasing LPL and acyl coenzyme A synthetase activity. Therefore, testosterone in males may have a tonic role in femoral fat storage by supressing LPL activity [59].
Conversely, obesity can also induce hypogonadism. While obesity-related secondary hypogonadism is a well-known condition in males, there is evidence suggesting the existence of obesity-related secondary hypogonadism in females as well [60]. Male obesity-related hypogonadism is characterized by higher conversion of testosterone to oestradiol in adipocytes, which then exerts negative feedback on gonadotropin-releasing hormone (GnRH) secretion. This, in turn, leads to a decreased production of luteinizing hormone (LH) and FSH and therefore impaired testicular testosterone production [60,61]. Female-obesity-related hypogonadism is characterized by increased endogenous LH clearance and/or reduced pituitary response to GnRH. This results in reduced LH levels as well as LH pulse amplitudes, which in turn impairs ovarian function [60]. As opposed to low testosterone levels in male-obesity-induced hypogonadism, females with obesity may have increased androgen production regardless of the presence of PCOS, which further reduces LH levels and predisposes them to metabolic dysfunction [60]. High androgen levels in females, like in polycystic ovary syndrome (PCOS), promote insulin resistance and alterations in glucose tolerance [62].
In a prospective study, Huang et al. demonstrated sex differences in the association of maternal androgen levels with the development of metabolic syndrome in the offspring later in life [63]. By following sons and daughters for up to 50 years after birth they concluded that although sons had significantly worse cardiometabolic profiles compared to daughters, higher prenatal levels of androgens in the mothers were associated with an increased metabolic syndrome incidence in the daughters but not in sons, further confirming the effect of perinatal androgen exposure on metabolism programming [63]. To conclude, masculinized energy metabolism in daughters born to mothers with higher levels of androgens seems to be a predisposition to visceral adiposity and insulin resistance later in life.
Another example of the implication of sex steroid hormones in body composition, fat distribution, and obesity development is seen with gender-affirming hormone therapy (GAHT) [64,65]. Here transgender women are usually treated with oestrogens and anti-androgens, while transgender men are treated with testosterone [64]. A study with a baseline obesity prevalence of 25% in the transfeminine group and 39% in the transmasculine group found that even though obesity rates increased in both groups during hormone therapy, specifically within 2–4 months in the transmasculine group and after 22 months in the transfeminine group, the rates of obesity and weight gain were higher in the transmasculine group (with testosterone being the most likely reason) [64]. A recent review analysed 20 studies focusing on body composition changes in transgender individuals receiving GAHT. Oestrogen therapy in transgender women was associated with a decrease in lean mass and waist-to-hip ratio and an increase in fat mass and BMI, while testosterone therapy in transgender man was associated with an increase in lean mass, increase in BMI and waist-to-hip ratio with a tendency to gain visceral adiposity and lose subcutaneous adiposity [65], again confirming the impact of sex hormones on fat distribution and body composition.
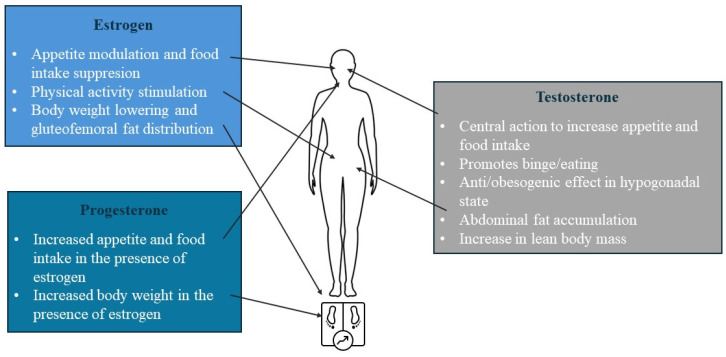
In addition to their importance in regulating fat distribution, sex hormones are also involved in appetite regulation, as oestrogen decreases appetite and food intake in women, while progestine, progesterone in the presence of oestrogen, and testosterone increase appetite and food intake [66]. This is evident from the varying caloric intake across the menstrual cycle. Increasing oestrogen levels cause a progressive decrease in eating during the follicular [67] and the 4-day periovulatory phase, when estradiol is at its highest levels, which is not seen in anovulatory women [68,69]. Additionally, resting energy expenditure fluctuates during the menstrual cycle, reaching its lowest point during the early follicular phase and increases to approximately 50–100 kcal/day more in the luteal phase [67]. The effect of sex steroid hormones on appetite is summarised in Figure 2.
Figure 2.
Summarised effect of sex steroid hormones on appetite.
2.4. Sex Difference in Obesity-Related Genetic Susceptibility
It is well known that around 40–70% of BMI variability can be attributed to genetic factors, and studies have identified around 900 genetic loci associated with BMI, which explains only 6% of the population variance in adult BMI [70]. Some studies additionally confirmed sexual dimorphism in the genetic loci for some anthropometric traits with a stronger effect in females than in males [71,72].
Sex chromosomes are an additional important factor for sex dimorphism in obesity. This has been proven by the development and use of the four-core genotype (FCG) mouse model, a model that separates the contributions of gonads and sex chromosomes to obesity development [73]. Through production of XX and XY mice with ovaries and XX and XY mice with testes and analysis of all four genotypes, one can differentiate whether a specific trait is influenced by chromosomal sex (XX or XY) or gonadal sex (ovaries or testes) [73]. Chen et al. gonadectomized the FCG mice to diminish the hormonal effects on adiposity and showed that gonadectomized XX-carrying mice, regardless of the gonadal type before gonadectomy, had worse HFD-induced obesity outcomes with greater food intake, increased adiposity, and accelerated weight gain and also developed fatty liver, hyperleptinemia, hyperinsulinemia, and hyperlipidemia [74]. When studying different chromosomal combinations, such as XO and XXY, the negative effects of a HFD on obesity development were more pronounced by increasing the number of X chromosomes and not by the absence of the Y chromosome, confirming the importance of the X chromosome on obesity development and its sexual dimorphism [74]. In another study, the group identified a positive relationship between Kdm5c gene expression and adiposity [75]. Kdm5c is an X chromosome gene, which influences gene expression involved in extracellular matrix reorganization, which is crucial for adipose tissue expansion. Kdm5c expression in females is higher, likely because of X chromosome inactivation escape and experimental reduction of Kdm5c dosage in XX females to a level usually present in XY males leads to reduced adipose tissue expansion [75].
Genome-wide association studies (GWAS) also showed that there is strong sexual dimorphism in the genetic regulation of WAT. Bernabeu et al. investigated the effect of sex on genetic architecture by analysing 530 complex traits in 450,000 individuals in the UK Biobank [76]. When considering the autosomal genome, they found that the trait with the largest number of sex-dimorphic single nucleotide polymorphisms (SNPs) was the waist-to-hip circumference ratio, with a total of 2421 sex-dimorphic SNPs, representing 100 unique loci [76]. Kilpeläinen et al. identified a locus near the IRS1 gene that was associated with reduced body fat percentage, more specifically with less SAT compared to VAT in males but not in females, and this was also linked to an unfavourable lipide profile, insulin resistance, decreased levels of adiponectin, and increased risk for diabetes and coronary artery disease [77]. In another recent study, Kaisinger et al. undertook an exome-wide association study by using data from 419,692 UK Biobank participants and identified genes for which rare heterozygous loss-of-function is associated with an increased BMI in females (DIDO1, PTPRG, and SLC12A5) and in males (SLTM), with effect sizes up to 8 kg/m2 [70]. A common limiting factor of these studies is that the analysis is restricted to individuals of European ancestry.
2.5. Sex-Related Differences in Gut Microbiota
The gut microbiome has a vital role in digestion, metabolism, and nutrient absorption. Additionally, it has other critical functions, such as preserving the intestinal immune system response and tolerance, as well as stimulating and regulating hormone synthesis [78]. Dysbiosis can be defined as a decrease in gut microbiota compositional variety and/or functional diversity. Although it is not known whether dysbiosis is the cause or the consequence of a certain disease, it is well known that significant changes in the gut microbiota were noticed in people with obesity. One of the most researched parameters since its discovery in 2005 is the Firmicutes:Bacteroidates (F:B) ratio [78]. Animal and human studies showed an increase in the F:B ratio, which is associated with a greater capacity to extract energy from the diet, in obesity [79,80,81] and a decrease in the F:B ratio with weight loss [79], although this hypothesis has been challenged by underpowered studies. Gut microbiota composition and diversity are also affected by sex. An observational study that compared microbiota diversity in males and females with high sex hormone levels to those with low sex hormone levels showed that high sex steroid hormone levels are associated with greater microbiota diversity in both sexes, and females with higher oestrogen levels had a higher abundance of Bacteroidetes and lower levels of Firmicutes phyla compared to those with low oestrogen levels [82]. Qin et al. showed that female mice on HFD showed slower weight gain as well as slower increase in F:B ratio compared to male mice fed the same diet, once again showing that females are more resistant to diet-inducing obesity [83]. He et al. also showed that there are gut microbiota sex differences as a response to probiotic strain Lactobacillus reuteri, with a positive effect on immune response, an increase in the abundance of phylum Bacteroidates, and a decrease in Firmicutes phyla seen in females and not in males [84]. Firmicutes phyla are the main producers of butyrate, which is an anti-inflammatory metabolite. The higher prevalence of Firmicutes phyla in males with obesity can lead to an increased generation of butyrate, which may suppress the immune response [9]. Bacteroidetes phyla—which are more prevalent in females with obesity, on the other hand—are gram-negative bacteria containing lipopolysaccharides (LPS) in the membrane, which are associated with a more robust immune response [9]. A stronger immune response may be the reason that delays the development of obesity-related metabolic diseases in females [9].
Additionally, the gut microbiota is involved in sex steroid metabolism [85,86,87]. Oestrogen metabolism occurs mainly in the liver through a two-stage reaction by hydroxylation and conjugation, and conjugated oestrogens are later excreted in the bile and passed into the intestine in conjugated form. Here, gut microbial beta-glucuronidase plays a vital role in regulating physiological oestrogen metabolism, as this enzyme deconjugates oestrogens in the intestine. These oestrogens regain biological activity and can be reabsorbed [85]. This reabsorption of deconjugated oestrogens in the blood and the liver is called enterohepatic recycling of oestrogens, a process which is important for maintaining sex hormone homeostasis. Increased beta-glucuronidase activity is inversely correlated with faecal oestrogens [87], and by increasing the production and activity of beta-glucuronidase there is an increase in enterohepatic circulation of biologically active oestrogens [85]. Gut microbiota, by having a role in the deconjugation of DHT and testosterone, may be an important regulator of intestinal androgen metabolism as well [86]. A study showed that mice with normal microbiota composition had remarkably increased free levels of the most potent androgen, DHT, while mice lacking gut microbiota had substantially lower levels of free DHT [86]. This finding was also tested in human physiology, as young men also had substantially increased faecal free DHT levels and the group proposed that diet changes affecting gut microbiota composition or probiotic use might modulate intestinal androgen metabolism [86].
3. Sex and Gender—Specific Risk Factors Influencing Overweight/Obesity Pathology
3.1. Behavioural Neuroadaptive Food Intake Preferences
Obesity is associated with structural and functional changes in the brains reward system [88,89]. Palatable food consumption activates the mesolimbic dopaminergic pathway, inducing rewarding effects. Repeated activation of this pathway by palatable food consumption in obesity leads to neuroadaptation in its downstream inhibitory cortico-striatal circuits, which leads to compulsive behaviour and loss of control in food intake [89,90,91]. Although this neuroadaptation is shared in both sexes, females are more susceptible to obesity-induced neural adaptations in the reward regions than males [88]. Based on a systematic review of functional neuroimaging studies, females showed greater neural responses in striatal/limbic system and frontal/cortical system in response to food cues and may be more sensitive to visual food cues, although this conclusion was made based on a limited number of studies with small sample sizes [88,92]. Furthermore, studies show that females compared to males experience stronger tonic and trait food cravings overall [93,94,95] and may be less successful in regulating and suppressing cue-induced food cravings [96,97].
There appear to be gender differences in food preferences and eating behaviours between males and females [98,99,100,101,102]. A cross-sectional study in 21 European countries showed that females have greater consumption of fruits and vegetables compared to males [98,99]. A study examining comfort food preferences across gender showed that females were more likely to prefer sweet tastes and snack-based comfort food, such as candy or chocolate, while males were more likely to choose meal-based comfort food, like pizza or pasta [100]. Another cross-sectional study by Lombardo et al. looking at gender differences in taste and food habits in 2021 subjects showed that females preferred more whole grain foods, cereals, and vegetables, while males preferred more eggs, meats, and processed meat. While males ate faster and skipped breakfast more often, females were more likely to eat uncontrollably, even when not hungry [101]. Feraco et al. used an online survey to examine gender differences in food preferences and eating habits in 2198 subjects and also confirmed that males are more likely to prefer red and processed meat, while females aligned with healthier food choices and were more likely to choose vegetables, whole grains, tofu, and dark chocolate. Males also ate faster and dined out, while females more frequently ate without hunger [102].
3.2. Sociocultural Role Modelling and Gender-Different Psychological Influence during Development
As proposed according to the gender intensification hypothesis in 1983 by Hill and Lynch [103], as adolescents develop physically and emotionally, they tend to align themselves closely with the stereotypes associated with their gender. The main stereotype in males is mesomorphism, and that in females is physical attractiveness, which in Western societies is closely linked to thinness [104]. With the increase in adiposity following puberty, the discrepancy between the actual and ideal body is increased, creating a period of vulnerability for girls to body dissatisfaction [104] as well as for the development of eating disordered behaviours, such as binge-eating disorder or night-eating syndrome [105,106].
Females generally experience greater levels of body dissatisfaction in comparison to males, likely due to more significant societal pressure and pressure from friends and family to adhere to cultural standards, being more influenced by social media to follow appearance ideals and face a higher amount of criticism on their physical appearance from both male and female peers compared to male individuals [104,107,108]. A recent study by Dougherty et al. examined the relationship between interpersonal stress and shape/weight concerns in a group of boys and girls with overweight/obesity using ecological momentary assessment [109]. Interpersonal stress was connected to shape/weight concerns in girls with overweight/obesity but was not related to shape/weight concerns in boys with overweight/obesity. Additionally, girls who experienced higher feelings of loneliness, social rejection, and a desire for more friends had higher levels of shape/weight concerns as well [109].
Obesity is strongly associated with a wide range of psychological and mental disorders, from low self-esteem and body image disturbance to depression, eating disorders, and low quality of life [110]. The connection between obesity and depression seems to be bidirectional, as some studies show that antidepressant use increases the risk of obesity, while others indicate that obesity is often the cause of depression. Depression is more common in females with obesity than males [111,112]. Eating-disordered behaviours, such as binge-eating disorder and night-eating syndrome, are also commonly found in people with obesity. Female sex can be a risk factor, as these disorders are more common in females [110,113]. Obesity also has an impact on quality of life separately from depression and low self-esteem, including impacts on education opportunities, income, and relationships. Even here, we can find gender differences, as female gender was associated with a lower chance to complete an advanced educational program, lower household income, and lower likelihood to get married [110].
In summary, although food preferences and eating behaviours may vary between males and females, females are more susceptible to obesity-induced neural adaptations and less successful in managing food cravings. Furthermore, females generally experience greater body dissatisfaction—often due to societal pressure, social media influence, and criticism from peers—as well as more eating-disordered behaviour and depression.
4. Clinical Implications of Sex-Related Differences in Obesity
4.1. Differential Sex and Gender Risks of Obesity-Related Comorbidities
Obesity has also sex-specific differences in related comorbidities. Even though obesity is more prevalent in females, females may be protected from obesity-associated metabolic implications [114,115]. Studies on animal models showed that male rodents compared to females exhibit an earlier onset of obesity, a higher degree of obesity, and have a greater prevalence of accompanying risk factors such as hyperglycaemia, hyperinsulinemia, and hypertension when subjected to an HFD [9,114,115]. Obesity is an important risk factor for diabetes development [116] and according to a meta-analysis by Guh et al. diabetes incidence rate ratios are higher in females than males [117]. On the other hand, there is also a sex difference in the time of diabetes development in people with obesity, as studies show that females are diagnosed with diabetes mellitus at a later age and have a higher BMI at diagnosis compared to males [118,119,120]. These differences are likely due to the impact of sex steroid hormones on body composition, fat distribution, and energy metabolism and are attenuated with increased age and menopause [121]. The major proposed underlying mechanism of obesity-induced hypertension is the activation of the sympathetic nervous system, however, obesity seems to increase sympathetic nerve activity (SNA) in males but not in females [122]. A potential explanation might be in the different central actions of insulin and possibly leptin in patients with obesity [122]. Specifically, insulin increases SNA similarly in lean males and females, while this sympathoexcitatory response to insulin is amplified in males with obesity, it is abolished in females with obesity [123]. In addition angiotensinogen expression and secretion is greater in visceral adipocytes, and studies show that VAT also has greater SNA compared to SAT adding to the development of sex differences [124]. Waist circumference and BMI are also strongly associated with obstructive sleep apnoea (OSA). In a cross-sectional study including 14,3326 females and 22,896 males, OSA was diagnosed in 6.4% of females and 13.8% of males. OSA prevalence increased with increasing BMI, and among individuals with morbid obesity (BMI ≥ 40 kg/m2), OSA was present in 50% of males compared to 30% of females [125].
Evidence from epidemiological studies shows that obesity is not only associated with an increased risk of cancer but also an increased risk of recurrence and cancer-related mortality in several malignancies [126]. According to the report from the International Agency for Research on Cancer Working Group on Body Fatness in 2016, there is sufficient evidence for an association between obesity and cancer risk in 13 cancers, such as postmenopausal breast cancer, endometrial cancer, ovarian cancer, colorectal cancer, oesophageal cancer, stomach cancer, pancreatic cancer, cancer of the gallbladder, liver cancer, kidney cancer, meningioma, multiple myeloma, and thyroid cancer [126]. Similar findings were found in an umbrella review by Kyrgiou et al. [127]. There is a sex variation in the relative risk of cancer development. When looking at the total number of obesity-related cancers, females had a higher number of obesity-related cancer cases [126]. The higher overall incidence among females is likely due to the contribution of endometrial, ovarian, and postmenopausal breast cancer, and obesity-related cancers that concern both sexes show a higher incidence in males [128].
To summarise, all of this shows that while males may be more at risk for the development of the metabolic implications of obesity, females are more at risk for the psychological implications of obesity. While obesity-related cancer seems to be more prevalent in females, this is mostly due to gynaecological malignancies, and when looking at cancers that concern both sexes, there is a higher incidence in males.
4.2. Gender-Differential Effectiveness of Weight Loss Interventions
4.2.1. Non-Pharmacological Interventions
There seem to be gender differences in treatment-seeking, with females being more likely to pursue a lifestyle weight loss intervention [121] as well as more likely to be offered a weight loss intervention [129]. A study analysing differences in healthcare professional counselling of individuals with overweight and obesity found that females were more likely to receive physician counselling to control/lose weight, reduce fat/calorie intake, and increase physical activity compared to males [129]. This could be the result of healthcare providers perceiving females as being more receptive than males or because females visit healthcare providers more often, thus having a greater chance to develop a trusting relationship and comfort in discussing sensitive subjects such as weight loss. On the other hand, while females were more likely to adopt recommendations to increase physical activity, there were no significant gender differences in reported efforts to control/lose weight or reduce fat/calorie intake, meaning that both genders were similarly susceptible to behavioural change if offered proper counselling [129].
Regarding diet success, a recent meta-analysis of sex differences in weight loss on a low-carbohydrate diet (LCD) showed that while most included studies did not report a significant difference in weight loss on a LCD, some of them had a numerical difference, with a greater absolute weight loss in males over females [130]. When a significant sex difference was reported, all but one included study showed that males lost more weight on LCD compared to females [130], which has also been a conclusion in previous analyses on sex differences in weight loss intervention effectiveness [131].
4.2.2. Pharmacological Interventions
At the moment there are six medications for non-syndromic obesity: orlistat, naltrexone/bupropion, liraglutide, semaglutide, and tirzepatide—which are all approved by the Food and Drug Administration (FDA) and European Medical Agency (EMA)—and phentermine/topiramate, which is only approved by the FDA [132]. An analysis of 26,522 patients who were prescribed antiobesogenic medications between 2015 and 2016 revealed that pharmacotherapy was more often prescribed to females. Specifically, 85.5% of naltrexone/bupropion, 82.2% of phentermine/topiramate, and 72.4% of liraglutide prescriptions were given to females [133]. Furthermore, when looking at the demographics of the randomized patients, the majority of studies on the efficacy of antiobesogenic medications have involved a larger cohort of female participants, leading to the underrepresentation of males [132]. The STEP clinical program examining semaglutide efficacy in treating obesity showed clear female predominance, with STEP 1 including 74.1% of females [134], STEP 3 including 81% of females [135], STEP 4 including 79% [136], and STEP 5 including 77.6% of females [137]. STEP 2 recruiting people with obesity and diabetes was more gender-balanced, including 49% of male participants [138]. The latest SURMOUNT program evaluating the efficacy of the GIP/GLP1-RA tirzepatide included a greater proportion of males (30–49%) compared to other trials, likely due to capping female enrolment at 70% [139].
This female predominance and male underrepresentation are particularly important since some studies show sex-specific differences in pharmacotherapy efficacy. A study conducting exposure–response analysis using liraglutide for obesity treatment showed a clear positive relationship between liraglutide exposure and weight loss [140]. Females also had a 32% higher drug exposure than males of similar body weight and achieved greater weight loss at any given exposure compared to males [140]. They also found that the exposure–weight loss response did not plateau in males receiving liraglutide at a dose of 3 mg, possibly suggesting that additional weight loss may be achieved by using doses above 3 mg, which has not been clinically tested [140]. Subgroup analyses of the STEP program also showed a greater weight reduction in females compared to males. Possible reasons could be exposure differences, as females may have a lower mean body weights, leading to higher exposure to GLP1-RA, different feeding behaviour regulation due to the impact of sex hormones, slower gastric emptying in premenopausal females, and higher frequency of gastrointestinal side effects in females [141]. Preregistration clinical trials of the combination naltrexone/bupropion and phentermine/topiramate also showed a tendency of higher weight loss in females than males [142].
To conclude, females are more likely to be offered a weight loss intervention, including pharmacotherapy which is evident by the male underrepresentation in most registration trials of anti-obesogenic medication as well as the lower prescription of obesity pharmacotherapy in males. Studies on pharmacotherapy show a tendency for greater efficacy in females and more research is needed to examine whether there is a need for sex-tailored dosing of pharmacotherapy.
4.2.3. Bariatric Surgery
There seems to be gender disparity in bariatric surgery utilization among eligible patients, with females comprising over 80% of patients and males being underrepresented in most bariatric surgery studies [143]. This can be a consequence of gender-based differences in perception of body weight impacting motivation to pursue surgical treatment as well as possible gender bias in patient selection by the physicians [143]. A study examining patients’ motivation for seeking surgical treatment showed that when the primary motivation for surgical treatment was appearance and embarrassment, the subjects were far more likely female, younger, and with a lower presenting BMI. When the primary motivation was stated as a medical condition and health concern, the subjects were more likely to be male, older, and with fewer depression symptoms and better mental health [144]. Another study by Kochkodan et al. looked at the sex and gender differences in preoperative characteristics, postoperative complications, and comorbidity resolution in patients undergoing bariatric surgery [145]. Out of the total 61,708 patients, 78% were female and 22% were male. While both females and males benefited from surgical treatment, preoperatively, males had significantly more risk factors, a higher BMI and comorbidity burden, and postoperatively had increased surgical complications, less weight loss, and less comorbidity resolution [145]. Females, on the other hand, continued to express lower body image and lower psychological well-being scores, leading to lower postoperative satisfaction despite having lower preoperative BMI, having lost more body weight, and having greater comorbidity resolution postoperatively, showing again that body image perception has a higher impact in females, who may perceive obesity differently than males [145]. This shows that there is a gender inequality in the offering of bariatric surgery to males, and when offered, it is performed at a later stage of the disease. Although females have better surgical outcomes, there is a need for increased attention to the psychological effect of surgery, as they may benefit from psychological treatment pre- and postoperatively.
While many have implied that there is a beneficial effect of bariatric surgery and weight loss on cancer risk [128,146,147,148], one study also implied that bariatric surgery may be more effective in lowering cancer risk in females in contrast to males [149], although this has been limited by the relatively short mean time of follow-up and the smaller sample size of male participants [146,149].
5. Challenges and Future Directions
Even though great progress has been achieved in the understanding of the impact of sex in obesity pathophysiology, past obesity research has often been gender-neutral or with female underrepresentation and recent clinical registration trials of anti-obesity medications show male underrepresentation. A sex-specific analysis is often missing. Given the emerging trend toward personalized medicine and patient-tailored approach, considering the implication of sex and gender on different stages of obesity development is crucial in optimizing both its prevention and treatment effectiveness. Further obesity research is also needed on the full spectrum of gender identities to ensure awareness, inclusiveness, and reflectiveness of the diverse needs of the population.
6. Conclusions
There is a clear sexual dimorphism in obesity prevalence, which can be explained by differences in obesity pathophysiology, including fat distribution, energy metabolism, and gut microbiota diversity, as well as the impact of chromosomes and genetic predisposition. Additionally, sex and gender differences in risk factors contribute to weight gain disparities. Obesity-induced comorbidities also show sexual dimorphism, with males more susceptible to the metabolic consequences and females more vulnerable to psychopathology. Regular obesity screening is mandatory for both sexes since studies show that obesity in males is often recognized and treated at a later stage, when obesity-related comorbidities are well developed. Understanding the factors that predict body dissatisfaction and psychological challenges is crucial for developing effective prevention programs. Further research on sex and gender-related differences across different treatment modalities is needed to ensure optimized and personalized obesity management.
Author Contributions
Conceptualization, A.K., R.H. and M.J.; investigation, A.K., R.H., A.J. and M.J.; writing—original draft preparation, A.K., R.H., M.R., A.J. and M.J.; writing—review and editing, A.K., R.H., M.R., A.J. and M.J.; supervision, A.J. and M.J. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.World Health Organisation Global Health Observatory (GHO) Data: Overweight and Obesity. [(accessed on 25 May 2024)];2022 Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 2.Lostein T., Jackson-Leach R., Powis J., Brinsden H., Gray M. World Obesity Federation, World Obesity Atlas 2023. [(accessed on 25 May 2024)]. Available online: https://www.worldobesity.org/resources/resource-library/world-obesity-atlas-2023.
- 3.Phelps N.H., Singleton R.K., Zhou B., Heap R.A., Mishra A., Bennett J.E., Paciorek C.J., Lhoste V.P., Carrillo-Larco R.M., Stevens G.A., et al. Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet. 2024;403:1027–1050. doi: 10.1016/S0140-6736(23)02750-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swinburn B.A., Sacks G., Hall K.D., McPherson K., Finegood D.T., Moodie M.L., Gortmaker S.L. The global obesity pandemic: Shaped by global drivers and local environments. Lancet. 2011;378:804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 5.Hales C.M., Carroll M.D., Fryar C.D., Ogden C.L. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018. NCHS Data Brief, No. 360. [(accessed on 25 May 2024)]; Available online: https://www.cdc.gov/nchs/data/databriefs/db360-h.pdf. [PubMed]
- 6.Lin X., Li H. Obesity: Epidemiology, Pathophysiology, and Therapeutics. Front. Endocrinol. 2021;12:706978. doi: 10.3389/fendo.2021.706978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allegra S., Chiara F., Di Grazia D., Gaspari M., De Francia S. Evaluation of Sex Differences in Preclinical Pharmacology Research: How Far Is Left to Go? Pharmaceuticals. 2023;16:786. doi: 10.3390/ph16060786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia-Sifuentes Y., Maney D.L. Reporting and misreporting of sex differences in the biological sciences. eLife. 2021;10:e70817. doi: 10.7554/eLife.70817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brettle H., Tran V., Drummond G.R., Franks A.E., Petrovski S., Vinh A., Jelinic M. Sex hormones, intestinal inflammation, and the gut microbiome: Major influencers of the sexual dimorphisms in obesity. Front. Immunol. 2022;13:971048. doi: 10.3389/fimmu.2022.971048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gavin K.M., Bessesen D.H. Sex Differences in Adipose Tissue Function. Endocrinol. Metab. Clin. N. Am. 2020;49:215–228. doi: 10.1016/j.ecl.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karastergiou K., Smith S.R., Greenberg A.S., Fried S.K. Sex differences in human adipose tissues—The biology of pear shape. Biol. Sex Differ. 2012;3:13. doi: 10.1186/2042-6410-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jackson A., Stanforth P., Gagnon J., Rankinen T., Leon A., Rao D., Skinner J., Bouchard C., Wilmore J. The effect of sex, age and race on estimating percentage body fat from body mass index: The Heritage Family Study. Int. J. Obes. 2002;26:789–796. doi: 10.1038/sj.ijo.0802006. [DOI] [PubMed] [Google Scholar]
- 13.Christen T., Trompet S., Noordam R., Van Klinken J.B., Van Dijk K.W., Lamb H.J., Cobbaert C.M., Den Heijer M., Jazet I.M., Jukema J.W., et al. Sex differences in body fat distribution are related to sex differences in serum leptin and adiponectin. Peptides. 2018;107:25–31. doi: 10.1016/j.peptides.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 14.Arner P., Lithell H., Wahrenberg H., Brönnegard M. Expression of lipoprotein lipase in different human subcutaneous adipose tissue regions. J. Lipid Res. 1991;32:423–429. doi: 10.1016/S0022-2275(20)42065-6. [DOI] [PubMed] [Google Scholar]
- 15.Mauvais-Jarvis F. Sex differences in energy metabolism: Natural selection, mechanisms and consequences. Nat. Rev. Nephrol. 2024;20:56–69. doi: 10.1038/s41581-023-00781-2. [DOI] [PubMed] [Google Scholar]
- 16.Palmer B.F., Clegg D.J. The sexual dimorphism of obesity. Mol. Cell. Endocrinol. 2015;402:113–119. doi: 10.1016/j.mce.2014.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manolopoulos K.N., Karpe F., Frayn K.N. Gluteofemoral body fat as a determinant of metabolic health. Int. J. Obes. 2010;34:949–959. doi: 10.1038/ijo.2009.286. [DOI] [PubMed] [Google Scholar]
- 18.Liu X., Zhang Z., Song Y., Xie H., Dong M. An update on brown adipose tissue and obesity intervention: Function, regulation and therapeutic implications. Front. Endocrinol. 2023;13:1065263. doi: 10.3389/fendo.2022.1065263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schirinzi V., Poli C., Berteotti C., Leone A. Browning of Adipocytes: A Potential Therapeutic Approach to Obesity. Nutrients. 2023;15:2229. doi: 10.3390/nu15092229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh R., Barrios A., Dirakvand G., Pervin S. Human Brown Adipose Tissue and Metabolic Health: Potential for Therapeutic Avenues. Cells. 2021;10:3030. doi: 10.3390/cells10113030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaikaew K., Grefhorst A., Visser J.A. Sex Differences in Brown Adipose Tissue Function: Sex Hormones, Glucocorticoids, and Their Crosstalk. Front. Endocrinol. 2021;12:652444. doi: 10.3389/fendo.2021.652444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoffman J.M., Valencak T.G. Sex differences and aging: Is there a role of brown adipose tissue? Mol. Cell. Endocrinol. 2021;531:111310. doi: 10.1016/j.mce.2021.111310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keuper M., Jastroch M. The good and the BAT of metabolic sex differences in thermogenic human adipose tissue. Mol. Cell. Endocrinol. 2021;533:111337. doi: 10.1016/j.mce.2021.111337. [DOI] [PubMed] [Google Scholar]
- 24.Lee M.-J., Fried S.K. Sex-dependent Depot Differences in Adipose Tissue Development and Function; Role of Sex Steroids. J. Obes. Metab. Syndr. 2017;26:172–180. doi: 10.7570/jomes.2017.26.3.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martínez de Morentin P.B., González-García I., Martins L., Lage R., Fernández-Mallo D., Martínez-Sánchez N., Ruíz-Pino F., Liu J., Morgan D.A., Pinilla L., et al. Estradiol Regulates Brown Adipose Tissue Thermogenesis via Hypothalamic AMPK. Cell Metab. 2014;20:41–53. doi: 10.1016/j.cmet.2014.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Oliveira Dos Santos A.R., de Oliveira Zanuso B., Miola V.F.B., Barbalho S.M., Santos Bueno P.C., Flato U.A.P., Detregiachi C.R.P., Buchaim D.V., Buchaim R.L., Tofano R.J., et al. Adipokines, Myokines, and Hepatokines: Crosstalk and Metabolic Repercussions. Int. J. Mol. Sci. 2021;22:2639. doi: 10.3390/ijms22052639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shi H., Clegg D.J. Sex differences in the regulation of body weight. Physiol. Behav. 2009;97:199–204. doi: 10.1016/j.physbeh.2009.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Frithioff-Bøjsøe C., Lund M.A.V., Lausten-Thomsen U., Hedley P.L., Pedersen O., Christiansen M., Baker J.L., Hansen T., Holm J.-C. Leptin, adiponectin, and their ratio as markers of insulin resistance and cardiometabolic risk in childhood obesity. Pediatr. Diabetes. 2020;21:194–202. doi: 10.1111/pedi.12964. [DOI] [PubMed] [Google Scholar]
- 29.Sanchez-Rebordelo E., Cunarro J., Perez-Sieira S., Seoane L., Diéguez C., Nogueiras R., Tovar S. Regulation of Chemerin and CMKLR1 Expression by Nutritional Status, Postnatal Development, and Gender. Int. J. Mol. Sci. 2018;19:2905. doi: 10.3390/ijms19102905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lőrincz H., Csiha S., Ratku B., Somodi S., Sztanek F., Seres I., Paragh G., Harangi M. Gender-Dependent Associations between Serum Betatrophin Levels and Lipoprotein Subfractions in Diabetic and Nondiabetic Obese Patients. Int. J. Mol. Sci. 2023;24:16504. doi: 10.3390/ijms242216504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Westerterp K.R. Changes in physical activity over the lifespan: Impact on body composition and sarcopenic obesity. Obes. Rev. 2018;19:8–13. doi: 10.1111/obr.12781. [DOI] [PubMed] [Google Scholar]
- 32.Westerterp K.R. Diet induced thermogenesis. Nutr. Metab. 2004;1:5. doi: 10.1186/1743-7075-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Westerterp K.R. Physical activity and physical activity induced energy expenditure in humans: Measurement, determinants, and effects. Front. Physiol. 2013;4:90. doi: 10.3389/fphys.2013.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pietiläinen K.H., Kaprio J., Borg P., Plasqui G., Yki-Järvinen H., Kujala U.M., Rose R.J., Westerterp K.R., Rissanen A. Physical inactivity and obesity: A vicious circle. Obes. Silver Spring Md. 2008;16:409–414. doi: 10.1038/oby.2007.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sanal E., Ardic F., Kirac S. Effects of aerobic or combined aerobic resistance exercise on body composition in overweight and obese adults: Gender differences. A randomized intervention study. Eur. J. Phys. Rehabil. Med. 2013;49:1–11. [PubMed] [Google Scholar]
- 36.Aadland E., Jepsen R., Andersen J.R., Anderssen S.A. Differences in fat loss in response to physical activity among severely obese men and women. J. Rehabil. Med. 2014;46:363–369. doi: 10.2340/16501977-1786. [DOI] [PubMed] [Google Scholar]
- 37.Power M.L., Schulkin J. Sex differences in fat storage, fat metabolism, and the health risks from obesity: Possible evolutionary origins. Br. J. Nutr. 2008;99:931–940. doi: 10.1017/S0007114507853347. [DOI] [PubMed] [Google Scholar]
- 38.Mauvais-Jarvis F., Clegg D.J., Hevener A.L. The Role of Estrogens in Control of Energy Balance and Glucose Homeostasis. Endocr. Rev. 2013;34:309–338. doi: 10.1210/er.2012-1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lindberg M., Weihua Z., Andersson N., Moverare S., Gao H., Vidal O., Erlandsson M., Windahl S., Andersson G., Lubahn D., et al. Estrogen receptor specificity for the effects of estrogen in ovariectomized mice. J. Endocrinol. 2002;174:167–178. doi: 10.1677/joe.0.1740167. [DOI] [PubMed] [Google Scholar]
- 40.Davis K.E., Neinast M.D., Sun K., Skiles W.M., Bills J.D., Zehr J.A., Zeve D., Hahner L.D., Cox D.W., Gent L.M., et al. The sexually dimorphic role of adipose and adipocyte estrogen receptors in modulating adipose tissue expansion, inflammation, and fibrosis. Mol. Metab. 2013;2:227–242. doi: 10.1016/j.molmet.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Naaz A., Zakroczymski M., Heine P., Taylor J., Saunders P., Lubahn D., Cooke P.S. Effect of Ovariectomy on Adipose Tissue of Mice in the Absence of Estrogen Receptor Alpha (ERα): A Potential Role for Estrogen Receptor Beta (ERβ) Horm. Metab. Res. 2002;34:758–763. doi: 10.1055/s-2002-38259. [DOI] [PubMed] [Google Scholar]
- 42.Hong J., Stubbins R.E., Smith R.R., Harvey A.E., Núñez N.P. Differential susceptibility to obesity between male, female and ovariectomized female mice. Nutr. J. 2009;8:11. doi: 10.1186/1475-2891-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu P., Ji Y., Yuen T., Rendina-Ruedy E., DeMambro V.E., Dhawan S., Abu-Amer W., Izadmehr S., Zhou B., Shin A.C., et al. Blocking FSH induces thermogenic adipose tissue and reduces body fat. Nature. 2017;546:107–112. doi: 10.1038/nature22342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O’Reilly M.W., House P.J., Tomlinson J.W. Understanding androgen action in adipose tissue. J. Steroid Biochem. Mol. Biol. 2014;143:277–284. doi: 10.1016/j.jsbmb.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 45.Sebo Z.L., Rodeheffer M.S. Testosterone metabolites differentially regulate obesogenesis and fat distribution. Mol. Metab. 2021;44:101141. doi: 10.1016/j.molmet.2020.101141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nohara K., Zhang Y., Waraich R.S., Laque A., Tiano J.P., Tong J., Münzberg H., Mauvais-Jarvis F. Early-Life Exposure to Testosterone Programs the Hypothalamic Melanocortin System. Endocrinology. 2011;152:1661–1669. doi: 10.1210/en.2010-1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nohara K., Waraich R.S., Liu S., Ferron M., Waget A., Meyers M.S., Karsenty G., Burcelin R., Mauvais-Jarvis F. Developmental androgen excess programs sympathetic tone and adipose tissue dysfunction and predisposes to a cardiometabolic syndrome in female mice. Am. J. Physiol.-Endocrinol. Metab. 2013;304:E1321–E1330. doi: 10.1152/ajpendo.00620.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mauvais-Jarvis F. Developmental androgenization programs metabolic dysfunction in adult mice: Clinical implications. Adipocyte. 2014;3:151–154. doi: 10.4161/adip.27746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gavin K.M., Cooper E.E., Hickner R.C. Estrogen receptor protein content is different in abdominal than gluteal subcutaneous adipose tissue of overweight-to-obese premenopausal women. Metabolism. 2013;62:1180–1188. doi: 10.1016/j.metabol.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 50.Pedersen S.B., Kristensen K., Hermann P.A., Katzenellenbogen J.A., Richelsen B. Estrogen controls lipolysis by up-regulating alpha2A-adrenergic receptors directly in human adipose tissue through the estrogen receptor alpha. Implications for the female fat distribution. J. Clin. Endocrinol. Metab. 2004;89:1869–1878. doi: 10.1210/jc.2003-031327. [DOI] [PubMed] [Google Scholar]
- 51.Lovejoy J.C., Champagne C.M., de Jonge L., Xie H., Smith S.R. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int. J. Obes. 2008;32:949–958. doi: 10.1038/ijo.2008.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bernasochi G.B., Bell J.R., Simpson E.R., Delbridge L.M.D., Boon W.C. Impact of estrogens on the regulation of white, beige, and brown adipose tissue depots. In: Prakash Y.S., editor. Comprehensive Physiology. Wiley; Hoboken, NJ, USA: 2019. pp. 457–475. [DOI] [PubMed] [Google Scholar]
- 53.Anagnostis P., Christou K., Artzouchaltzi A.-M., Gkekas N.K., Kosmidou N., Siolos P., Paschou S.A., Potoupnis M., Kenanidis E., Tsiridis E., et al. Early menopause and premature ovarian insufficiency are associated with increased risk of type 2 diabetes: A systematic review and meta-analysis. Eur. J. Endocrinol. 2019;180:41–50. doi: 10.1530/EJE-18-0602. [DOI] [PubMed] [Google Scholar]
- 54.Kanaya A.M., Herrington D., Vittinghoff E., Lin F., Grady D., Bittner V., Cauley J.A., Barrett-Connor E. Heart and Estrogen/progestin Replacement Study Glycemic effects of postmenopausal hormone therapy: The Heart and Estrogen/progestin Replacement Study. A randomized, double-blind, placebo-controlled trial. Ann. Intern. Med. 2003;138:1–9. doi: 10.7326/0003-4819-138-1-200301070-00005. [DOI] [PubMed] [Google Scholar]
- 55.Margolis K.L., Bonds D.E., Rodabough R.J., Tinker L., Phillips L.S., Allen C., Bassford T., Burke G., Torrens J., Howard B.V., et al. Effect of oestrogen plus progestin on the incidence of diabetes in postmenopausal women: Results from the Women’s Health Initiative Hormone Trial. Diabetologia. 2004;47:1175–1187. doi: 10.1007/s00125-004-1448-x. [DOI] [PubMed] [Google Scholar]
- 56.Loh N.Y., Humphreys E., Karpe F., Tomlinson J.W., Noordam R., Christodoulides C. Sex hormones, adiposity, and metabolic traits in men and women: A Mendelian randomisation study. Eur. J. Endocrinol. 2022;186:407–416. doi: 10.1530/EJE-21-0703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hamilton E.J., Gianatti E., Strauss B.J., Wentworth J., Lim-Joon D., Bolton D., Zajac J.D., Grossmann M. Increase in visceral and subcutaneous abdominal fat in men with prostate cancer treated with androgen deprivation therapy. Clin. Endocrinol. 2011;74:377–383. doi: 10.1111/j.1365-2265.2010.03942.x. [DOI] [PubMed] [Google Scholar]
- 58.Stanworth R.D., Jones T.H. Testosterone for the aging male; current evidence and recommended practice. Clin. Interv. Aging. 2008;3:25–44. doi: 10.2147/cia.s190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Santosa S., Bush N.C., Jensen M.D. Acute Testosterone Deficiency Alters Adipose Tissue Fatty Acid Storage. J. Clin. Endocrinol. Metab. 2017;102:3056–3064. doi: 10.1210/jc.2017-00757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eng P.C., Phylactou M., Qayum A., Woods C., Lee H., Aziz S., Moore B., Miras A.D., Comninos A.N., Tan T., et al. Obesity-Related Hypogonadism in Women. Endocr. Rev. 2024;45:171–189. doi: 10.1210/endrev/bnad027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kelly D.M., Jones T.H. Testosterone and obesity. Obes. Rev. 2015;16:581–606. doi: 10.1111/obr.12282. [DOI] [PubMed] [Google Scholar]
- 62.Tramunt B., Smati S., Grandgeorge N., Lenfant F., Arnal J.-F., Montagner A., Gourdy P. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia. 2020;63:453–461. doi: 10.1007/s00125-019-05040-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Huang G., Cherkerzian S., Loucks E.B., Buka S.L., Handa R.J., Lasley B.L., Bhasin S., Goldstein J.M. Sex Differences in the Prenatal Programming of Adult Metabolic Syndrome by Maternal Androgens. J. Clin. Endocrinol. Metab. 2018;103:3945–3953. doi: 10.1210/jc.2018-01243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kyinn M., Banks K., Leemaqz S.Y., Sarkodie E., Goldstein D., Irwig M.S. Weight gain and obesity rates in transgender and gender-diverse adults before and during hormone therapy. Int. J. Obes. 2021;45:2562–2569. doi: 10.1038/s41366-021-00935-x. [DOI] [PubMed] [Google Scholar]
- 65.Ford K., Huggins E., Sheean P. Characterising body composition and bone health in transgender individuals receiving gender-affirming hormone therapy. J. Hum. Nutr. Diet. 2022;35:1105–1114. doi: 10.1111/jhn.13027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hirschberg A.L. Sex hormones, appetite and eating behaviour in women. Maturitas. 2012;71:248–256. doi: 10.1016/j.maturitas.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 67.Leeners B., Geary N., Tobler P.N., Asarian L. Ovarian hormones and obesity. Hum. Reprod. Update. 2017;23:300–321. doi: 10.1093/humupd/dmw045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Barr S.I., Janelle K.C., Prior J.C. Energy intakes are higher during the luteal phase of ovulatory menstrual cycles. Am. J. Clin. Nutr. 1995;61:39–43. doi: 10.1093/ajcn/61.1.39. [DOI] [PubMed] [Google Scholar]
- 69.Davidsen L., Vistisen B., Astrup A. Impact of the menstrual cycle on determinants of energy balance: A putative role in weight loss attempts. Int. J. Obes. 2007;31:1777–1785. doi: 10.1038/sj.ijo.0803699. [DOI] [PubMed] [Google Scholar]
- 70.Kaisinger L.R., Kentistou K.A., Stankovic S., Gardner E.J., Day F.R., Zhao Y., Mörseburg A., Carnie C.J., Zagnoli-Vieira G., Puddu F., et al. Large-scale exome sequence analysis identifies sex- and age-specific determinants of obesity. Cell Genom. 2023;3:100362. doi: 10.1016/j.xgen.2023.100362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Heid I.M., Jackson A.U., Randall J.C., Winkler T.W., Qi L., Steinthorsdottir V., Thorleifsson G., Zillikens M.C., Speliotes E.K., Mägi R., et al. Meta-analysis identifies 13 new loci associated with waist-hip ratio and reveals sexual dimorphism in the genetic basis of fat distribution. Nat. Genet. 2010;42:949–960. doi: 10.1038/ng.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Randall J.C., Winkler T.W., Kutalik Z., Berndt S.I., Jackson A.U., Monda K.L., Kilpeläinen T.O., Esko T., Mägi R., Li S., et al. Sex-stratified Genome-wide Association Studies Including 270,000 Individuals Show Sexual Dimorphism in Genetic Loci for Anthropometric Traits. PLoS Genet. 2013;9:e1003500. doi: 10.1371/journal.pgen.1003500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mauvais-Jarvis F., Arnold A.P., Reue K. A Guide for the Design of Pre-clinical Studies on Sex Differences in Metabolism. Cell Metab. 2017;25:1216–1230. doi: 10.1016/j.cmet.2017.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen X., McClusky R., Chen J., Beaven S.W., Tontonoz P., Arnold A.P., Reue K. The Number of X Chromosomes Causes Sex Differences in Adiposity in Mice. PLoS Genet. 2012;8:e1002709. doi: 10.1371/journal.pgen.1002709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Link J.C., Wiese C.B., Chen X., Avetisyan R., Ronquillo E., Ma F., Guo X., Yao J., Allison M., Chen Y.-D.I., et al. X chromosome dosage of histone demethylase KDM5C determines sex differences in adiposity. J. Clin. Investig. 2020;130:5688–5702. doi: 10.1172/JCI140223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bernabeu E., Canela-Xandri O., Rawlik K., Talenti A., Prendergast J., Tenesa A. Sex differences in genetic architecture in the UK Biobank. Nat. Genet. 2021;53:1283–1289. doi: 10.1038/s41588-021-00912-0. [DOI] [PubMed] [Google Scholar]
- 77.Kilpeläinen T.O., Zillikens M.C., Stančákova A., Finucane F.M., Ried J.S., Langenberg C., Zhang W., Beckmann J.S., Luan J., Vandenput L., et al. Genetic variation near IRS1 associates with reduced adiposity and an impaired metabolic profile. Nat. Genet. 2011;43:753–760. doi: 10.1038/ng.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ley R.E., Bäckhed F., Turnbaugh P., Lozupone C.A., Knight R.D., Gordon J.I. Obesity alters gut microbial ecology. Proc. Natl. Acad. Sci. USA. 2005;102:11070–11075. doi: 10.1073/pnas.0504978102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ley R.E., Turnbaugh P.J., Klein S., Gordon J.I. Human gut microbes associated with obesity. Nature. 2006;444:1022–1023. doi: 10.1038/4441022a. [DOI] [PubMed] [Google Scholar]
- 80.Koliada A., Syzenko G., Moseiko V., Budovska L., Puchkov K., Perederiy V., Gavalko Y., Dorofeyev A., Romanenko M., Tkach S., et al. Association between body mass index and Firmicutes/Bacteroidetes ratio in an adult Ukrainian population. BMC Microbiol. 2017;17:120. doi: 10.1186/s12866-017-1027-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Palmas V., Pisanu S., Madau V., Casula E., Deledda A., Cusano R., Uva P., Vascellari S., Loviselli A., Manzin A., et al. Gut microbiota markers associated with obesity and overweight in Italian adults. Sci. Rep. 2021;11:5532. doi: 10.1038/s41598-021-84928-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shin J.-H., Park Y.-H., Sim M., Kim S.-A., Joung H., Shin D.-M. Serum level of sex steroid hormone is associated with diversity and profiles of human gut microbiome. Res. Microbiol. 2019;170:192–201. doi: 10.1016/j.resmic.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 83.Qin Y., Roberts J.D., Grimm S.A., Lih F.B., Deterding L.J., Li R., Chrysovergis K., Wade P.A. An obesity-associated gut microbiome reprograms the intestinal epigenome and leads to altered colonic gene expression. Genome Biol. 2018;19:7. doi: 10.1186/s13059-018-1389-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.He J., Wang W., Wu Z., Pan D., Guo Y., Cai Z., Lian L. Effect of Lactobacillus reuteri on intestinal microbiota and immune parameters: Involvement of sex differences. J. Funct. Foods. 2019;53:36–43. doi: 10.1016/j.jff.2018.12.010. [DOI] [Google Scholar]
- 85.Hu S., Ding Q., Zhang W., Kang M., Ma J., Zhao L. Gut microbial beta-glucuronidase: A vital regulator in female estrogen metabolism. Gut Microbes. 2023;15:2236749. doi: 10.1080/19490976.2023.2236749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Colldén H., Landin A., Wallenius V., Elebring E., Fändriks L., Nilsson M.E., Ryberg H., Poutanen M., Sjögren K., Vandenput L., et al. The gut microbiota is a major regulator of androgen metabolism in intestinal contents. Am. J. Physiol. Endocrinol. Metab. 2019;317:E1182–E1192. doi: 10.1152/ajpendo.00338.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Flores R., Shi J., Fuhrman B., Xu X., Veenstra T.D., Gail M.H., Gajer P., Ravel J., Goedert J.J. Fecal microbial determinants of fecal and systemic estrogens and estrogen metabolites: A cross-sectional study. J. Transl. Med. 2012;10:253. doi: 10.1186/1479-5876-10-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kroll D.S., Feldman D.E., Biesecker C.L., McPherson K.L., Manza P., Joseph P.V., Volkow N.D., Wang G.-J. Neuroimaging of Sex/Gender Differences in Obesity: A Review of Structure, Function, and Neurotransmission. Nutrients. 2020;12:1942. doi: 10.3390/nu12071942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stice E., Spoor S., Bohon C., Small D.M. Relation between obesity and blunted striatal response to food is moderated by TaqIA A1 allele. Science. 2008;322:449–452. doi: 10.1126/science.1161550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Horstmann A., Busse F.P., Mathar D., Müller K., Lepsien J., Schlögl H., Kabisch S., Kratzsch J., Neumann J., Stumvoll M., et al. Obesity-Related Differences between Women and Men in Brain Structure and Goal-Directed Behavior. Front. Hum. Neurosci. 2011;5:58. doi: 10.3389/fnhum.2011.00058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Volkow N.D., Wang G.-J., Telang F., Fowler J.S., Thanos P.K., Logan J., Alexoff D., Ding Y.-S., Wong C., Ma Y., et al. Low dopamine striatal D2 receptors are associated with prefrontal metabolism in obese subjects: Possible contributing factors. NeuroImage. 2008;42:1537–1543. doi: 10.1016/j.neuroimage.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chao A.M., Loughead J., Bakizada Z.M., Hopkins C.M., Geliebter A., Gur R.C., Wadden T.A. Sex/gender differences in neural correlates of food stimuli: A systematic review of functional neuroimaging studies. Obes. Rev. 2017;18:687–699. doi: 10.1111/obr.12527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lafay L., Thomas F., Mennen L., Charles M.A., Eschwege E., Borys J.M., Basdevant A., Fleurbaix Laventie Ville Santé Study Group Gender differences in the relation between food cravings and mood in an adult community: Results from the fleurbaix laventie ville santé study. Int. J. Eat. Disord. 2001;29:195–204. doi: 10.1002/1098-108X(200103)29:2<195::AID-EAT1009>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 94.Cepeda-Benito A., Fernandez M.C., Moreno S. Relationship of gender and eating disorder symptoms to reported cravings for food: Construct validation of state and trait craving questionnaires in Spanish. Appetite. 2003;40:47–54. doi: 10.1016/S0195-6663(02)00145-9. [DOI] [PubMed] [Google Scholar]
- 95.Imperatori C., Innamorati M., Tamburello S., Continisio M., Contardi A., Tamburello A., Fabbricatore M. Gender differences in food craving among overweight and obese patients attending low energy diet therapy: A matched case-control study. Eat. Weight Disord. EWD. 2013;18:297–303. doi: 10.1007/s40519-013-0054-7. [DOI] [PubMed] [Google Scholar]
- 96.Hallam J., Boswell R.G., DeVito E.E., Kober H. Gender-related Differences in Food Craving and Obesity. Yale J. Biol. Med. 2016;89:161–173. [PMC free article] [PubMed] [Google Scholar]
- 97.Wang G.-J., Volkow N.D., Telang F., Jayne M., Ma Y., Pradhan K., Zhu W., Wong C.T., Thanos P.K., Geliebter A., et al. Evidence of gender differences in the ability to inhibit brain activation elicited by food stimulation. Proc. Natl. Acad. Sci. USA. 2009;106:1249–1254. doi: 10.1073/pnas.0807423106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Stea T.H., Nordheim O., Bere E., Stornes P., Eikemo T.A. Fruit and vegetable consumption in Europe according to gender, educational attainment and regional affiliation—A cross-sectional study in 21 European countries. PLoS ONE. 2020;15:e0232521. doi: 10.1371/journal.pone.0232521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Emanuel A.S., McCully S.N., Gallagher K.M., Updegraff J.A. Theory of Planned Behavior explains gender difference in fruit and vegetable consumption. Appetite. 2012;59:693–697. doi: 10.1016/j.appet.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wansink B., Cheney M., Chan N. Exploring comfort food preferences across age and gender1. Physiol. Behav. 2003;79:739–747. doi: 10.1016/S0031-9384(03)00203-8. [DOI] [PubMed] [Google Scholar]
- 101.Lombardo M., Aulisa G., Padua E., Annino G., Iellamo F., Pratesi A., Caprio M., Bellia A. Gender differences in taste and foods habits. Nutr. Food Sci. 2019;50:229–239. doi: 10.1108/NFS-04-2019-0132. [DOI] [Google Scholar]
- 102.Feraco A., Armani A., Amoah I., Guseva E., Camajani E., Gorini S., Strollo R., Padua E., Caprio M., Lombardo M. Assessing gender differences in food preferences and physical activity: A population-based survey. Front. Nutr. 2024;11:1348456. doi: 10.3389/fnut.2024.1348456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hill J.P., Lynch M.E. The Intensification of Gender-Related Role Expectations during Early Adolescence. In: Brooks-Gunn J., Petersen A.C., editors. Girls at Puberty. Springer; Boston, MA, USA: 1983. pp. 201–228. [DOI] [Google Scholar]
- 104.Bearman S.K., Presnell K., Martinez E., Stice E. The Skinny on Body Dissatisfaction: A Longitudinal Study of Adolescent Girls and Boys. J. Youth Adolesc. 2006;35:217–229. doi: 10.1007/s10964-005-9010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.McCuen-Wurst C., Ruggieri M., Allison K.C. Disordered eating and obesity: Associations between binge-eating disorder, night-eating syndrome, and weight-related comorbidities. Ann. N. Y. Acad. Sci. 2018;1411:96–105. doi: 10.1111/nyas.13467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Keel P.K., Fulkerson J.A., Leon G.R. Disordered Eating Precursors in Pre- and Early Adolescent Girls and Boys. J. Youth Adolesc. 1997;26:203–216. doi: 10.1023/A:1024504615742. [DOI] [Google Scholar]
- 107.Ata R.N., Ludden A.B., Lally M.M. The Effects of Gender and Family, Friend, and Media Influences on Eating Behaviors and Body Image During Adolescence. J. Youth Adolesc. 2007;36:1024–1037. doi: 10.1007/s10964-006-9159-x. [DOI] [Google Scholar]
- 108.Taylor N.L. “Guys, She’s Humongous!”: Gender and Weight-Based Teasing in Adolescence. J. Adolesc. Res. 2011;26:178–199. doi: 10.1177/0743558410371128. [DOI] [Google Scholar]
- 109.Dougherty E.N., Goldschmidt A.B., Johnson N.K., Badillo K., Engel S.G., Haedt-Matt A.A. Gender differences in the relation between interpersonal stress and momentary shape and weight concerns in youth with overweight/obesity. Body Image. 2022;40:249–255. doi: 10.1016/j.bodyim.2022.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chu D.-T., Minh Nguyet N.T., Nga V.T., Thai Lien N.V., Vo D.D., Lien N., Nhu Ngoc V.T., Son L.H., Le D.-H., Nga V.B., et al. An update on obesity: Mental consequences and psychological interventions. Diabetes Metab. Syndr. Clin. Res. Rev. 2019;13:155–160. doi: 10.1016/j.dsx.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 111.Herva A., Laitinen J., Miettunen J., Veijola J., Karvonen J.T., Läksy K., Joukamaa M. Obesity and depression: Results from the longitudinal Northern Finland 1966 Birth Cohort Study. Int. J. Obes. 2006;30:520–527. doi: 10.1038/sj.ijo.0803174. [DOI] [PubMed] [Google Scholar]
- 112.Pratt L.A., Brody D.J. Depression and Obesity in the U.S. Adult Household Population, 2005–2010. Centers for Disease Control and Prevention; Atlanta, GA, USA: 2014. [Google Scholar]
- 113.De França G.V.A., Gigante D.P., Olinto M.T.A. Binge eating in adults: Prevalence and association with obesity, poor self-rated health status and body dissatisfaction. Public Health Nutr. 2014;17:932–938. doi: 10.1017/S1368980013000591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Yang Y., Smith D.L., Keating K.D., Allison D.B., Nagy T.R. Variations in body weight, food intake and body composition after long-term high-fat diet feeding in C57BL/6J mice: Variations in Diet-Induced Obese C57BL/6J Mice. Obesity. 2014;22:2147–2155. doi: 10.1002/oby.20811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hwang L., Wang C., Li T., Chang S., Lin L., Chen C., Chen C., Liang K., Ho I., Yang W., et al. Sex Differences in High-fat Diet-induced Obesity, Metabolic Alterations and Learning, and Synaptic Plasticity Deficits in Mice. Obesity. 2010;18:463–469. doi: 10.1038/oby.2009.273. [DOI] [PubMed] [Google Scholar]
- 116.Narayan K.M.V., Boyle J.P., Thompson T.J., Gregg E.W., Williamson D.F. Effect of BMI on Lifetime Risk for Diabetes in the U.S. Diabetes Care. 2007;30:1562–1566. doi: 10.2337/dc06-2544. [DOI] [PubMed] [Google Scholar]
- 117.Guh D.P., Zhang W., Bansback N., Amarsi Z., Birmingham C.L., Anis A.H. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health. 2009;9:88. doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Logue J., Walker J.J., Colhoun H.M., Leese G.P., Lindsay R.S., McKnight J.A., Morris A.D., Pearson D.W., Petrie J.R., Philip S., et al. Do men develop type 2 diabetes at lower body mass indices than women? Diabetologia. 2011;54:3003–3006. doi: 10.1007/s00125-011-2313-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Paul S., Thomas G., Majeed A., Khunti K., Klein K. Women develop type 2 diabetes at a higher body mass index than men. Diabetologia. 2012;55:1556–1557. doi: 10.1007/s00125-012-2496-2. [DOI] [PubMed] [Google Scholar]
- 120.Kwon S.K. Women Are Diagnosed with Type 2 Diabetes at Higher Body Mass Indices and Older Ages than Men: Korea National Health and Nutrition Examination Survey 2007–2010. Diabetes Metab. J. 2014;38:74. doi: 10.4093/dmj.2014.38.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cooper A.J., Gupta S.R., Moustafa A.F., Chao A.M. Sex/Gender Differences in Obesity Prevalence, Comorbidities, and Treatment. Curr. Obes. Rep. 2021;10:458–466. doi: 10.1007/s13679-021-00453-x. [DOI] [PubMed] [Google Scholar]
- 122.Shi Z., Wong J., Brooks V.L. Obesity: Sex and sympathetics. Biol. Sex Differ. 2020;11:10. doi: 10.1186/s13293-020-00286-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Shi Z., Cassaglia P.A., Pelletier N.E., Brooks V.L. Sex differences in the sympathoexcitatory response to insulin in obese rats: Role of neuropeptide Y. J. Physiol. 2019;597:1757–1775. doi: 10.1113/JP277517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Alvarez G.E., Ballard T.P., Beske S.D., Davy K.P. Subcutaneous obesity is not associated with sympathetic neural activation. Am. J. Physiol.-Heart Circ. Physiol. 2004;287:H414–H418. doi: 10.1152/ajpheart.01046.2003. [DOI] [PubMed] [Google Scholar]
- 125.Huang T., Lin B.M., Markt S.C., Stampfer M.J., Laden F., Hu F.B., Tworoger S.S., Redline S. Sex differences in the associations of obstructive sleep apnoea with epidemiological factors. Eur. Respir. J. 2018;51:1702421. doi: 10.1183/13993003.02421-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sung H., Siegel R.L., Torre L.A., Pearson-Stuttard J., Islami F., Fedewa S.A., Goding Sauer A., Shuval K., Gapstur S.M., Jacobs E.J., et al. Global patterns in excess body weight and the associated cancer burden. CA. Cancer J. Clin. 2019;69:88–112. doi: 10.3322/caac.21499. [DOI] [PubMed] [Google Scholar]
- 127.Kyrgiou M., Kalliala I., Markozannes G., Gunter M.J., Paraskevaidis E., Gabra H., Martin-Hirsch P., Tsilidis K.K. Adiposity and cancer at major anatomical sites: Umbrella review of the literature. BMJ. 2017;356:j477. doi: 10.1136/bmj.j477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Argyrakopoulou G., Dalamaga M., Spyrou N., Kokkinos A. Gender Differences in Obesity-Related Cancers. Curr. Obes. Rep. 2021;10:100–115. doi: 10.1007/s13679-021-00426-0. [DOI] [PubMed] [Google Scholar]
- 129.Greaney M.L., Cohen S.A., Xu F., Ward-Ritacco C.L., Riebe D. Healthcare provider counselling for weight management behaviours among adults with overweight or obesity: A cross-sectional analysis of National Health and Nutrition Examination Survey, 2011–2018. BMJ Open. 2020;10:e039295. doi: 10.1136/bmjopen-2020-039295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Susanto A., Burk J., Hocking S., Markovic T., Gill T. Differences in weight loss outcomes for males and females on a low-carbohydrate diet: A systematic review. Obes. Res. Clin. Pract. 2022;16:447–456. doi: 10.1016/j.orcp.2022.09.006. [DOI] [PubMed] [Google Scholar]
- 131.Williams R.L., Wood L.G., Collins C.E., Callister R. Effectiveness of weight loss interventions—Is there a difference between men and women: A systematic review. Obes. Rev. 2015;16:171–186. doi: 10.1111/obr.12241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Chakhtoura M., Haber R., Ghezzawi M., Rhayem C., Tcheroyan R., Mantzoros C.S. Pharmacotherapy of obesity: An update on the available medications and drugs under investigation. eClinicalMedicine. 2023;58:101882. doi: 10.1016/j.eclinm.2023.101882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Ganguly R., Tian Y., Kong S.X., Hersloev M., Hobbs T., Smolarz B.G., Ramasamy A., Haase C.L., Weng W. Persistence of newer anti-obesity medications in a real-world setting. Diabetes Res. Clin. Pract. 2018;143:348–356. doi: 10.1016/j.diabres.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 134.Wilding J.P.H., Batterham R.L., Calanna S., Davies M., Van Gaal L.F., Lingvay I., McGowan B.M., Rosenstock J., Tran M.T.D., Wadden T.A., et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N. Engl. J. Med. 2021;384:989–1002. doi: 10.1056/NEJMoa2032183. [DOI] [PubMed] [Google Scholar]
- 135.Wadden T.A., Bailey T.S., Billings L.K., Davies M., Frias J.P., Koroleva A., Lingvay I., O’Neil P.M., Rubino D.M., Skovgaard D., et al. Effect of Subcutaneous Semaglutide vs Placebo as an Adjunct to Intensive Behavioral Therapy on Body Weight in Adults With Overweight or Obesity: The STEP 3 Randomized Clinical Trial. JAMA. 2021;325:1403. doi: 10.1001/jama.2021.1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Rubino D., Abrahamsson N., Davies M., Hesse D., Greenway F.L., Jensen C., Lingvay I., Mosenzon O., Rosenstock J., Rubio M.A., et al. Effect of Continued Weekly Subcutaneous Semaglutide vs Placebo on Weight Loss Maintenance in Adults With Overweight or Obesity: The STEP 4 Randomized Clinical Trial. JAMA. 2021;325:1414. doi: 10.1001/jama.2021.3224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Garvey W.T., Batterham R.L., Bhatta M., Buscemi S., Christensen L.N., Frias J.P., Jódar E., Kandler K., Rigas G., Wadden T.A., et al. Two-year effects of semaglutide in adults with overweight or obesity: The STEP 5 trial. Nat. Med. 2022;28:2083–2091. doi: 10.1038/s41591-022-02026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Davies M., Færch L., Jeppesen O.K., Pakseresht A., Pedersen S.D., Perreault L., Rosenstock J., Shimomura I., Viljoen A., Wadden T.A., et al. Semaglutide 2·4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): A randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. Lancet. 2021;397:971–984. doi: 10.1016/S0140-6736(21)00213-0. [DOI] [PubMed] [Google Scholar]
- 139.Le Roux C.W., Zhang S., Aronne L.J., Kushner R.F., Chao A.M., Machineni S., Dunn J., Chigutsa F.B., Ahmad N.N., Bunck M.C. Tirzepatide for the treatment of obesity: Rationale and design of the SURMOUNT clinical development program. Obesity. 2023;31:96–110. doi: 10.1002/oby.23612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Wilding J.P.H., Overgaard R.V., Jacobsen L.V., Jensen C.B., le Roux C.W. Exposure-response analyses of liraglutide 3.0 mg for weight management. Diabetes Obes. Metab. 2016;18:491–499. doi: 10.1111/dom.12639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Jensterle M., Rizzo M., Janež A. Semaglutide in Obesity: Unmet Needs in Men. Diabetes Ther. 2023;14:461–465. doi: 10.1007/s13300-022-01360-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Cataldi M., Muscogiuri G., Savastano S., Barrea L., Guida B., Taglialatela M., Colao A. Gender-related issues in the pharmacology of new anti-obesity drugs. Obes. Rev. 2019;20:375–384. doi: 10.1111/obr.12805. [DOI] [PubMed] [Google Scholar]
- 143.Aly S., Hachey K., Pernar L.I.M. Gender disparities in weight loss surgery. Mini-Invasive Surg. 2020;4:21. doi: 10.20517/2574-1225.2019.57. [DOI] [Google Scholar]
- 144.Libeton M., Dixon J.B., Laurie C., O’Brien P.E. Patient Motivation for Bariatric Surgery: Characteristics and Impact on Outcomes. Obes. Surg. 2004;14:392–398. doi: 10.1381/096089204322917936. [DOI] [PubMed] [Google Scholar]
- 145.Kochkodan J., Telem D.A., Ghaferi A.A. Physiologic and psychological gender differences in bariatric surgery. Surg. Endosc. 2018;32:1382–1388. doi: 10.1007/s00464-017-5819-z. [DOI] [PubMed] [Google Scholar]
- 146.Avgerinos K.I., Spyrou N., Mantzoros C.S., Dalamaga M. Obesity and cancer risk: Emerging biological mechanisms and perspectives. Metabolism. 2019;92:121–135. doi: 10.1016/j.metabol.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 147.Zhou X., Yu J., Li L., Gloy V.L., Nordmann A., Tiboni M., Li Y., Sun X. Effects of Bariatric Surgery on Mortality, Cardiovascular Events, and Cancer Outcomes in Obese Patients: Systematic Review and Meta-analysis. Obes. Surg. 2016;26:2590–2601. doi: 10.1007/s11695-016-2144-x. [DOI] [PubMed] [Google Scholar]
- 148.Casagrande D.S., Rosa D.D., Umpierre D., Sarmento R.A., Rodrigues C.G., Schaan B.D. Incidence of Cancer Following Bariatric Surgery: Systematic Review and Meta-analysis. Obes. Surg. 2014;24:1499–1509. doi: 10.1007/s11695-014-1276-0. [DOI] [PubMed] [Google Scholar]
- 149.Sjöström L., Gummesson A., Sjöström C.D., Narbro K., Peltonen M., Wedel H., Bengtsson C., Bouchard C., Carlsson B., Dahlgren S., et al. Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish Obese Subjects Study): A prospective, controlled intervention trial. Lancet Oncol. 2009;10:653–662. doi: 10.1016/S1470-2045(09)70159-7. [DOI] [PubMed] [Google Scholar]