Abstract
Background/Objectives: The forced social isolation implemented to prevent the spread of the COVID-19 virus was accompanied by a worsening of mental health, an increase in insomnia symptoms, and the emergence of ‘skin hunger’—an increased longing for personal touch. This study aimed to enhance our understanding of the interconnection between sleep, mental health, and the need for physical (NPC) and real-life social contact (NRL-SC). Methods: A total of 2827 adults participated in an online survey during the second COVID-19 lockdown. A Bayesian Gaussian copula graphical model (BGCGM) and a Bayesian-directed acyclic graph (DAG) were estimated, and mixed ANOVAs were carried out. Results: NPC with non-family members (t(2091) = 12.55, p < 0.001, d = 0.27) and relational lifestyle satisfaction (t(2089) = 13.62, p < 0.001, d = 0.30) were lower during the second lockdown than before the pandemic. In our BGCGM, there were weak positive edges between the need for PC and RL-SC on one hand and sleep and mental health on the other. Conclusions: During the second lockdown, people craved less physical contact with non-family members and were less satisfied with their relational lifestyle than before the pandemic. Individuals with a greater need for PC and RL-SC reported poorer mental health (i.e., worry, depression, and mental fatigue).
Keywords: sleep, mental health, touch, pandemic, lockdown, long COVID, social isolation
1. Introduction
The year 2020 was marked by the COVID-19 pandemic, which led governments to implement measures to curb its spread. In Belgium, the first lockdown commenced on March 10th, and social distancing measures were implemented such that individuals could interact with only one person with whom they did not reside. This was followed a few days later by closing schools and non-essential stores, prohibiting travel, and instating telework. In May and June, many measures were lifted, such as people were permitted to return to work, stores reopened, and travel was once again allowed. Social measures were lifted until July when everyone was allowed to see up to fifteen people per week. However, a few weeks later, social measures became stricter again, and eventually, on the 2nd of November, individuals were restricted to inviting only one person to their homes with whom they could have close contact. Those living alone could be in close contact with two people. Teleworking and remote learning were reinstated, non-essential stores had to close, and wearing a mask when leaving the house became mandatory [1]. Thus, a second lockdown was then introduced. Hale et al. [2] developed a stringency index, ranging from 0 to 100, indicating the strictness of the measures taken by a country’s government. During the first lockdown, Belgium soared to a stringency index of 81.48, and during the second lockdown, the stringency index peaked at 75.93.
This forced social isolation was accompanied by a worsening of mental health and an increase in insomnia symptoms [3,4,5]. Additionally, it gave rise to the phenomenon called “skin hunger” [6], characterized by an increased longing for interpersonal touch [7]. The latter has been associated with a lower experienced quality of life [8], increased mental health symptoms [9], and sleep disturbances [10] during the pandemic. One’s living situation has been related to the need for interpersonal physical contact, with those living alone reporting higher levels of touch deprivation than those cohabiting during the COVID-19 pandemic [7,10].
This study is one of a few that took place during the second COVID-19-related lockdown and, as far as we know, the first regarding touch and social contact. We aimed to enhance understanding of the interconnection between sleep, mental health, and the need for interpersonal physical (NPC) and real-life social contact (NRL-SC) with family and non-family members during the second COVID-19 lockdown (starting 2 November 2020) using Bayesian network analysis, a recent and innovative method.
Our first research question was to explore the relationships between NPC and NRL-SC with family and non-family members and mental health and sleep complaints during the second COVID-19 lockdown. We expected people with greater NPC and NRL-SC to have worse mental health and more sleep complaints. Our second research question was: what were the roles of age, sex, cohabitation, and satisfaction with relational lifestyle play in this relationship? We expected women to report more sleep complaints, worrying, and depressive feelings and for relational lifestyle satisfaction to be negatively related to mental health and sleep complaints. Finally, the third research question was: were NPC and NRL-SC with family and non-family members and relational lifestyle satisfaction different during the second lockdown than before the COVID-19 pandemic? We expected NPC with family members to increase and NPC with non-family members to decrease during the lockdown. This final research question had two subquestions: we wished to know whether there was an interaction effect for people living alone with (not) being in a romantic relationship. For the people cohabiting, we wished to know whether there was an interaction effect with whom they were cohabiting.
2. Materials and Methods
2.1. Participants
The participants of this study included 2827 adults with a mean age of 41.42 years (SD = 14.31 years). The minors who replied to the questionnaire were excluded from the analysis. Males (M = 43.87 years; SD = 14.55) were significantly older than females (M = 40.13 years, SD = 14.13) (t(2825) = 6.61, p ≤ 0.001, d = 0.27). Most participants in this study were female (n = 1923, 68.02%). See Table 1 for a breakdown of who the participants cohabitated with based on their age categories. This information was not provided by 67 participants. Of the people living alone, 360 were single, and 144 were in a relationship. Thirty-three participants did not provide this information.
Table 1.
Distribution of with whom the participants cohabitated based on their age categories.
| 18–24 Years | 25–44 Years | 45–64 Years | 65+ Years | Total | |
|---|---|---|---|---|---|
| Lives alone | 44 | 244 | 194 | 55 | 537 |
| Lives only with partner | 28 | 367 | 257 | 84 | 736 |
| Lives with partner and other family members (child, parent, …) | 22 | 407 | 345 | 5 | 779 |
| Lives with other family members (child, parent, …) | 314 | 201 | 125 | 3 | 643 |
| Lives with partner and non-family members (friend, housemate, …) | 5 | 8 | 2 | 0 | 15 |
| Lives with non-family members (friend, housemate, …) | 18 | 32 | 0 | 0 | 50 |
| Total | 431 | 1259 | 923 | 147 | 2760 |
2.2. Materials and Procedure
This study was approved by the Comité d’éthique hospitalier (hospital ethical committee) of the Brugmann Hospital (Brussels, Belgium; number: CE 2023/40). Informed consent of the participants was obtained. The survey was launched and sent out on 23 November 2020 in French and Dutch via hospital newsletters, regular media (newspapers and radio), and social media. Data were retrieved on 6 February 2021. Most respondents replied to the Dutch version (75.6%).
The survey consisted of 74 questions, of which only those pertinent to this study were reported. First, biographical data such as sex, age, and cohabitation status were collected. Additional details about their cohabitants were requested for those indicating cohabitation. Then, a set of questions were asked twice: once regarding their situation during the pre-pandemic period and once regarding the second lockdown of COVID-19 (winter 2020–2021). These questions included the Insomnia Severity Index (ISI). The ISI is a seven-item scale measuring the severity of difficulties initiating sleep (DIS), maintaining sleep (DMS), early morning awakenings (EMA), sleep dissatisfaction, interference of sleep difficulties with daytime functioning, noticeability of sleep problems by others and distress caused by the sleep difficulties. These items are answered on a five-point Likert scale (no problem to very severe problem) [11]. It is a reliable and validated questionnaire for the measurement of insomnia [12]. In our analysis, only the first four of the seven items were used to avoid having too many sleep-related items in the analyses. In addition to insomnia-related inquiries, information on participants’ satisfaction with their relational lifestyle (married, single, cohabiting, etc.) was assessed. We also explored the need for interpersonal physical contact (NPC) and real-life social contact (NRL-SC) with both family (including romantic partners) and non-family members, such as friends and colleagues. A specific distinction was made between NPC and NRL-SC to account for the nuanced circumstances during the pandemic because while it remained possible to engage in real-life social interactions, maintaining a certain distance was mandatory. This allowed for face-to-face meetings, distinct from virtual interactions such as video calls or social media connections, while still prohibiting physical touch. Additionally, participants were asked about their levels of worry, experiences of depressive feelings, and extent of mental fatigue as part of a comprehensive assessment of their mental health. Table A1, in Appendix A, contains the variable names with the question asked and the available answer options.
2.3. Statistical Analysis
We estimated a Bayesian Gaussian copula graphical model (BGCGM) and a Bayesian-directed acyclic graph (DAG). A BGCGM is an undirected Bayesian network for mixed data because we included both binary and continuous variables in the network. The nodes represent variables, and the edges show conditional dependence between two variables. The advantage of using Bayesian networks over frequentists is obtaining evidence supporting the inclusion or exclusion of edges. This implies that one can ascertain whether an edge is absent in the network because of genuine conditional independence between two variables or simply because there is insufficient evidence to support the claim of conditional dependence. Edges were included if their Bayes Factor was at least 1, but only those with a factor of at least 10 have strong evidence for inclusion. No prior distribution was used to estimate this network. We used the R package easybgm [13].
For the DAG, arrows pointing to sex and age were blacklisted since these variables cannot be directly influenced by others. This is the only prior distribution that was included in this network. The Hill-Climbing algorithm, a score-based method, was employed to select the optimal network model based on goodness-of-fit measures [14]. We bootstrapped 10,000 samples and applied 50 different random restarts and 100 perturbations to circumvent getting stuck at a local maximum. A network was estimated for each of the 10,000 bootstrapped samples. The final network structure was constructed by averaging the 10,000 estimated networks. The thickness of the arrows represents Bayesian Information Criterion (BIC) values, indicating the significance of an arrow in the network. Variables with lower BIC values make a more substantial contribution to the network structure. Arrows are visible only if the directional probability, the likelihood that an arrow points in a particular direction, exceeds 0.5. All network analyses were performed using R studio version 4.2.2, and the DAG was plotted using R studio version 4.1.2. We used the packages bnlearn [14] and Rgraphviz [15].
T-tests and mixed ANOVAs were performed using SPSS version 28. Data were normally distributed. We estimated Cohen’s d effect sizes and used the cut-offs as proposed by Cohen [16]: d = 0.20 as a small effect, d = 0.50 as a medium effect, and d = 0.80 as a large effect. For the ANOVAs, we estimated partial etas squared and used the cut-offs as proposed by Cohen [16]: ηp2 = 0.0099 as a small effect, ηp2 = 0.0588 as a medium effect, and ηp2 = 0.1379 as a large effect. In all analyses, missing data were handled using pairwise deletion.
3. Results
3.1. Network Analysis
3.1.1. BGCGM
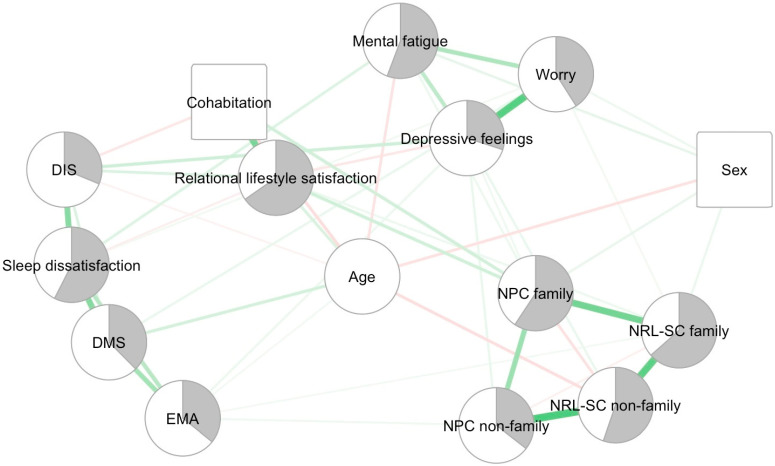
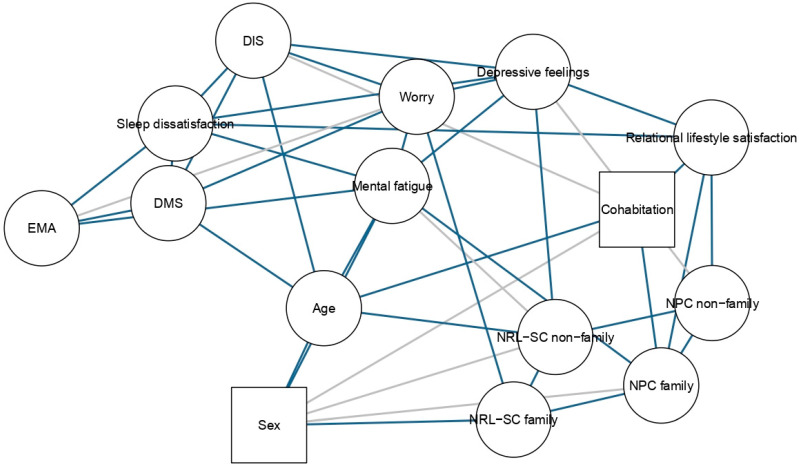
The BGCGM can be seen in Figure 1. The strongest edges in our network are NPC non-family–NRL-SC non-family (0.40), worry–depressive feelings (0.36), NRL-SC family–NRL-SC non-family (0.36), DMS–sleep dissatisfaction (0.35), NPC family–NRL-SC family (0.32), cohabitation–relational lifestyle satisfaction (0.31) and DIS–sleep dissatisfaction (0.30). A table with the edge weights can be consulted in Appendix A, Table A2. Figure A1 and Figure A2 in Appendix A represent the edge evidence plots. All of the edges in the BGCGM have a Bayes Factor of at least 10, indicating strong evidence for inclusion. Several edges have an infinite Bayes Factor.
Figure 1.
Bayesian Gaussian Copula Graphical Model. Note: Circles represent continuous variables and square binary variables. The grey area in the nodes represents the mean scores on a scale from 1 to 5, a mean score of 3 being represented by half of the node shaded in grey. For relational lifestyle satisfaction, the scale was from 1 to 4. This grey area was not computed for the demographic variables. The weight of the edges is represented by their thickness and color saturation. Positive connections are green, and negative connections are red. An edge between two continuous variables (circles) represents a partial correlation. An edge between two binary variables (squares) or between a binary and a continuous variable represents a regression coefficient. NPC family = need for physical contact with family members; NPC non-family = need for physical contact with non-family members; NRL-SC family = need for real-life social contact with family members; NRL-SC non-family = need for real-life social contact with non-family members; DIS = difficulties initiating sleep; DMS = difficulties maintaining sleep; EMA = early morning awakenings.
3.1.2. DAG
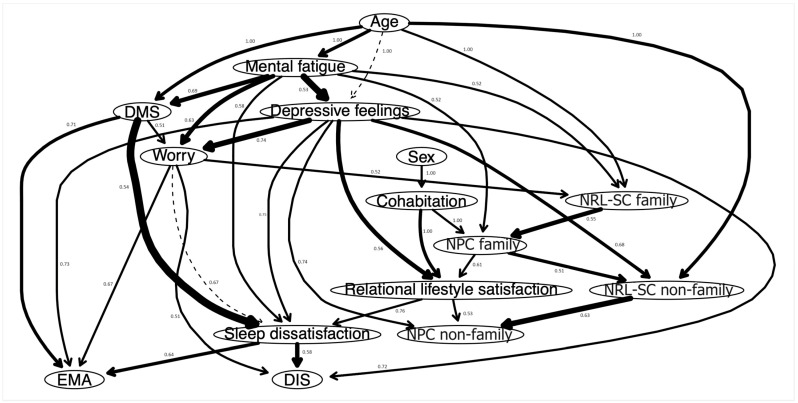
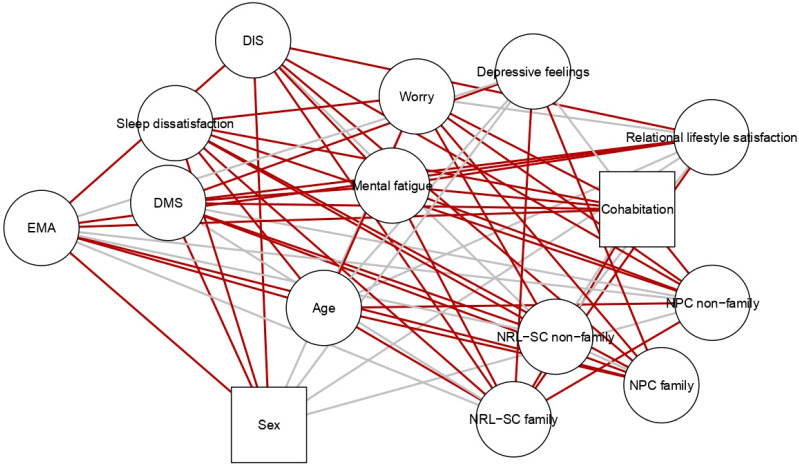
The DAG can be seen in Figure 2. The most important arrows to the network structure are DMS–sleep dissatisfaction (BIC: −408.58), mental fatigue–depressive feelings (BIC: −389.66), NRL-SC non-family–NPC non-family (BIC: −354.91), depressive feelings–worry (BIC: −289.18), sleep dissatisfaction–DIS (BIC: −271.69), NRL-SC family–NPC family (BIC: −269.74).
Figure 2.
Bayesian-Directed Acyclic Graph. Note: The thickness of an arrow indicates its importance to the overall network model fit. The numbers indicate the likelihood of a given direction. NPC family = need for physical contact with family members; NPC non-family = need for physical contact with non-family members; NRL-SC family = need for real-life social contact with family members; NRL-SC non-family = need for real-life social contact with non-family members; DIS = difficulties initiating sleep; DMS = difficulties maintaining sleep; EMA = early morning awakenings.
Since we blacklisted arrows going to sex and age, those leaving sex and age obviously have a directional probability of 1. Sex and age are parent nodes, but this could be artificial due to the blacklisting. Cohabitation is the only other variable with departing arrows whose directional probability is 1. Other arrows with strong directional probabilities are relational lifestyle satisfaction to sleep dissatisfaction (0.76), depressive feelings to sleep dissatisfaction (0.75), depressive feelings to worry (0.74), depressive feelings to NPC non-family (0.74), depressive feelings to EMA (0.73), depressive feelings to DIS (0.72) and DMS to EMA (0.71). EMA, DIS, and NPC non-family are child nodes. A table with all the strengths, BIC values, and directional probabilities of the visible arrows can be consulted in Appendix A, Table A3.
3.2. Pre- vs. Peri-Lockdown
The reported NPC non-family members and relational lifestyle satisfaction were lower during the second lockdown than before the pandemic. These differences, however, exhibited a small effect size. The reported NRL-SC with family members was higher during the lockdown, but the effect size was negligible. See Table 2 for the results of all t-tests.
Table 2.
t-test results.
| Pre-Lockdown (M, SD) |
Peri-Lockdown (M, SD) |
t(df) | p | d | |
|---|---|---|---|---|---|
| NPC family | 3.37 (0.93) | 3.39 (1.00) | −0.83 (2094) | 0.41 | −0.02 |
| NPC non-family | 2.70 (1.10) | 2.43 (1.19) | 12.55 (2091) | <0.001 | 0.27 |
| NRL-SC family | 3.43 (0.98) | 3.55 (1.05) | −6.45 (2092) | <0.001 | −0.14 |
| NRL-SC non-family | 3.24 (0.99) | 3.23 (1.12) | 0.81 (2090) | 0.21 | 0.02 |
| Relational lifestyle satisfaction | 3.18 (0.74) | 2.98 (0.85) | 13.82 (2089) | <0.001 | 0.30 |
Note: Response scale going from 1 to 5, except for relational lifestyle satisfaction going from 1 to 4. Bold indicates significance.
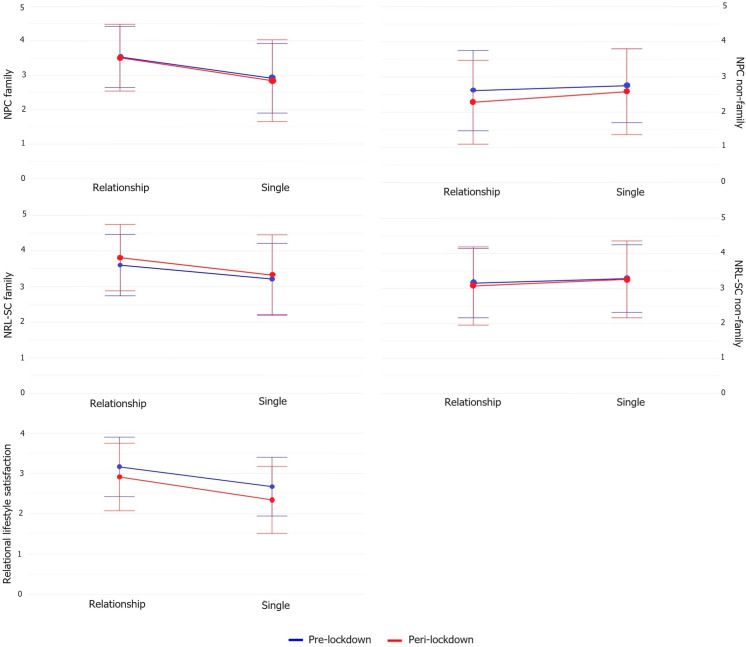
3.2.1. People Living Alone
As apparent from Table 3, no significant interactions were found between pre- vs. peri-lockdown and being in a romantic relationship or not when living alone. Significant main effects of being in a relationship were found for NPC family, NRL-SC family, and relational lifestyle satisfaction. As can be seen in Figure 3, singles showed a lower NPC and NRL-SC with family members compared with those in a relationship. Additionally, those in a relationship (albeit long-distance) were more satisfied with their current relational lifestyle than singles.
Table 3.
Mixed ANOVA results for people not cohabiting.
| Main Effect of Being in a Relationship | Interaction Effect of Being in a Relationship and Time | |||||
|---|---|---|---|---|---|---|
| F(df) | p | ηp 2 | F(df) | p | ηp 2 | |
| NPC family | 36.10 (1372) | <0.001 | 0.09 | 0.26 (1372) | 0.61 | 0.001 |
| NPC non-family | 3.45 (1373) | 0.06 | 0.01 | 1.90 (1373) | 0.17 | 0.005 |
| NRL-SC family | 18.59 (1373) | <0.001 | 0.05 | 0.80 (1373) | 0.37 | 0.002 |
| NRL-SC non-family | 2.24 (1373) | 0.14 | 0.01 | 0.28 (1373) | 0.60 | 0.001 |
| Relational lifestyle satisfaction | 44.98 (1370) | <0.001 | 0.11 | 1.26 (1371) | 0.26 | 0.003 |
Note: Bold indicates significance.
Figure 3.
Interaction effects for people not cohabiting.
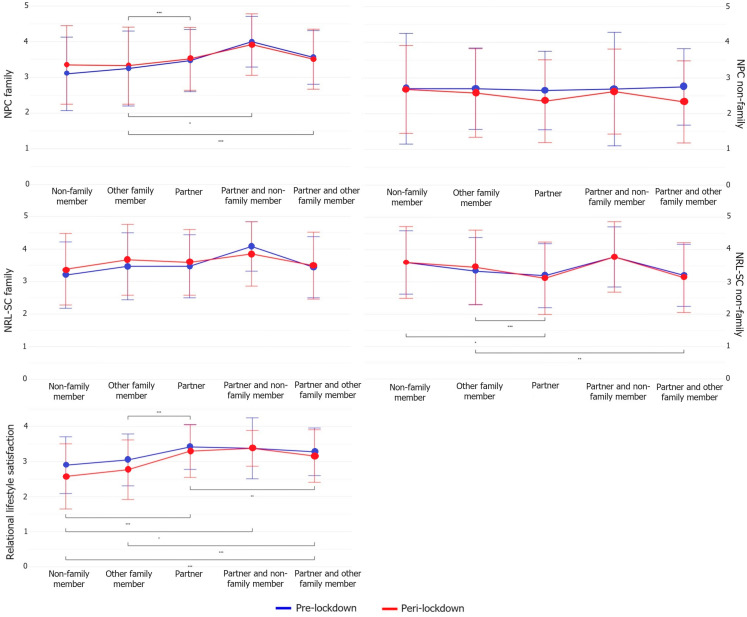
3.2.2. People Cohabiting
These data presented in Table 4 and Figure 4 indicate significant main effects and interactions among cohabiting individuals. Specifically, those residing with their partners, or with both their partners and other family members, reported a reduced NPC with non-family members during the lockdown. This pattern was not observed in other groups. Furthermore, individuals living with their partners or other family members experienced an increased NRL-SC with family members during the lockdown, a trend that did not appear in the other groups. Despite a notable interaction effect, changes in the NPC with family and NRL-SC with non-family were consistent across groups over time. Among those cohabiting with their partner and non-family members, relational lifestyle satisfaction levels remained stable before and during the lockdown. In contrast, the other groups reported a decrease in relational lifestyle satisfaction during the lockdown.
Table 4.
Mixed ANOVA results for people cohabiting.
| Main Effect Cohabiting | Interaction Effect Cohabiting and Time | |||||
|---|---|---|---|---|---|---|
| F(df) | p | ηp2 | F(df) | p | ηp2 | |
| NPC family | 8.33 (4, 1709) | <0.001 | 0.02 | 3.67 (4, 1709) | 0.01 | 0.01 |
| NPC non-family | 1.39 (4, 1705) | 0.24 | 0.003 | 7.04 (4, 1705) | <0.001 | 0.02 |
| NRL-SC family | 2.25 (4, 1707) | 0.06 | 0.01 | 2.72 (4, 1707) | 0.03 | 0.01 |
| NRL-SC non-family | 7.63 (4, 1704) | <0.001 | 0.02 | 3.30 (4, 1704) | 0.01 | 0.01 |
| Relational lifestyle satisfaction | 36.07 (4, 1707) | <0.001 | 0.08 | 6.31 (4, 1707) | <0.001 | 0.02 |
Note: Bold indicates significance.
Figure 4.
Interaction effects for people cohabiting. Note: * p < 0.05, ** p < 0.01, *** p < 0.001.
4. Discussion
The aim of this study was to explore the interconnection between sleep, mental health, and the need for interpersonal physical and real-life social contact with family and non-family during the second COVID-19 lockdown compared with before, using a Bayesian network analysis.
4.1. Network Analysis
Unsurprisingly, people with a greater skin hunger also reported a greater need to see those people in real life (meaning not through a screen). Since physical contact inherently involves seeing someone in real life, a greater need for physical contact logically corresponds to a greater need for real-life social contact. Furthermore, those expressing a greater need for physical and real-life social contact with non-family members also tend to express this need more greatly with family members. This suggests an overall greater requirement for physical and real-life social contact with family than with non-family members. Individuals who express those needs with non-family members tend to have a higher need for physical and real-life social contact with family members, hinting at a general inclination toward increased need for physical and social contact.
Individuals who experience worry are more likely to report difficulties in maintaining sleep, feelings of depression, and mental fatigue. Worrying emerges thus as an important symptom in night-time awakenings, depressive feelings, and mental fatigue and establishes itself as a transdiagnostic factor in the depression–insomnia relationship [17]. Furthermore, people who report worrying, experiencing night-time awakenings, or feeling depressed are more likely to report feeling mentally tired. This means that mental fatigue likely operates as a transdiagnostic factor in the anxiety–depression–insomnia relationship.
Individuals with a greater need for physical and real-life social contact reported poorer mental health (i.e., worry, depression, and mental fatigue), confirming our hypothesis and earlier findings on the importance of interpersonal touch interactions for the quality of life during COVID-19 [8]. Consequently, this means that having a particularly high need for physical and real-life social contact might be a sign of bad mental health. In contrast, people with mental health struggles will not necessarily have a need for touch or social contact. This might be due to their attachment style or negative attitudes towards others and physical contact [9].
Younger individuals reported experiencing fewer night-time awakenings, more mental fatigue, and a greater need to see non-family in real life compared with older individuals. Non-family members, which encompass friends, are more likely to be considered best friends by individuals under 26 years old. Past this age, people tend to designate their partner or a relative as their best friend [18]. Consequently, younger individuals are more inclined to express a greater need for real-life social contact with non-family members.
It is worth noting that despite women being more at risk of suffering from depression, anxiety [19], and insomnia [20], the partial correlations between these variables and sex were small or not present in the network. Moreover, sex was either not or weakly associated with the need for interpersonal touch and social contact.
Despite not blacklisting arrows towards the variable cohabitation in the DAG, all arrows identified (even those not included in the network because of insufficient strength) all had a directional probability of 1 when departing from the cohabitation variable. This implies that in 100% of the cases, cohabitation was solely dependent on sex: people who lived alone were more likely to be men.
People who were more satisfied with their relational lifestyle and who had a greater need for interpersonal touch with family members were more likely to cohabit. The correlation between cohabiting and relational lifestyle satisfaction was one of the strongest in our network. Even though we did not measure relationship satisfaction, previous research by Tai et al. [21] found that couples without intentions of living together report lower relationship satisfaction compared with married couples or couples with intentions of marrying or living together.
Our hypothesis of a negative relationship between relational lifestyle satisfaction, on the one hand, and mental health and sleep complaints, on the other hand, was confirmed by our results. People who were satisfied with their sleep were more satisfied with their relational lifestyle. On the other hand, people who are satisfied with their relational lifestyle are not necessarily satisfied with their sleep. This suggests that being dissatisfied with one’s relational lifestyle might be one of the many factors that impair sleep.
People who were satisfied with their relational lifestyle felt less depressed, tended to cohabitate, and had a greater need for interpersonal touch with family members. Being in a satisfying romantic relationship has been linked with better mental health than being single [22].
4.2. Pre- vs. Peri-Lockdown
The need for physical contact with non-family members was lower during the second lockdown compared with before in those cohabiting with their partner and in those cohabiting with their partner and other family members. This contradicts earlier findings of a higher longing for touch linked with the duration of COVID-19 regulations [7]. However, our results can partially align with the results of von Mohr et al. [9] during the first wave of the pandemic, who found that the longer people experienced social distancing, the less they craved physical contact with friends and colleagues, but the more they craved intimate touch (i.e., a kiss, hug, caress from partner or close family). However, contrary to our hypothesis, we did not find a noticeable increase in the need for physical contact with family members during the lockdown compared with before.
Note that our study encompassed data gathered during the second lockdown and not the first lockdown, as in the study by von Mohr et al. [9]. In that regard, another possible explanation might be that having already experienced a lockdown and a loosening of social distancing measures before may have caused the subsequent second lockdown to install a sense of habituation and acceptance of the ongoing abnormal and uncontrollable social circumstances [23], which is reflected in a lower need for interpersonal touch with non-family members. We know that touch deprivation in the long term can lead to a desensitization to interpersonal affective touch [24]. The question then is where the craving [25] for physical contact ends and transits to a sense of habituation and what the mediating factors in that process are. We lack data from the first lockdown to obtain a better picture of this.
However, regarding the need to see family members in real life, this increased in those cohabiting with their partner or with other family members during the lockdown, compared with before. Additionally, those cohabiting with their partner reported a lower need to see non-family members in real life overall compared with those cohabiting with others and non-family members, which can be linked with a decreased need for physical contact with non-family members.
Regarding the need for physical contact with family and the need for real-life social contact with non-family, the groups did not differ in their change over time despite a significant interaction effect. This could be due to the small sample size of the group living with non-family members and the group living with their partner and non-family members. The power might thus be high enough to detect the interaction effect but not to detect the effect of time inside these small groups.
Overall, we found that those living alone who were in a relationship showed a higher need for physical contact and real-life social contact with family members than singles. Similarly, those cohabiting with their partner, or with their partner and other or non-family members, also reported an overall significantly higher need for interpersonal touch with family members compared with those cohabiting with others than their partner. A possible explanation could be that those in a relationship received intimate touch on a regular basis from their partner, causing them to enjoy interpersonal touch from familiar people more [26] and thus seek more physical contact with them [27].
During the second lockdown, people reported lower satisfaction with their relational lifestyle compared with before the lockdown. A study has shown that with regard to life satisfaction (response scale: 0 = “worst possible life”; 10 = “best possible life”), during the lockdowns, singles’ life satisfaction decreased as they had to spend more time alone. In contrast, married couples’ life satisfaction increased as more time was spent with their partner [28]. Relatedly, we found in our study that in those living alone, relational lifestyle satisfaction was higher overall when being in a romantic relationship compared with when being single. In those cohabiting with their partner, or with their partner and other family members or non-family members, this satisfaction was also higher compared with those cohabiting with others than their partner. This is possibly related to previous findings that being in a fulfilling romantic relationship could buffer against COVID-19-related mental health risks [29,30].
Additionally, we found that those cohabiting with their partners and non-family members were the only ones not decreasing relational lifestyle satisfaction before versus during the lockdown. However, the sample size of this group was very small, which could have confounded these results.
4.3. Strengths and Limitations
To find significant differences in the t-tests with a Cohen’s d of at least 0.20 and a power of 0.90, we needed a sample size of at least 265. To find significant differences in the repeated measures ANOVA with an ηp2 of at least 0.01 and a power of 0.90, we needed a sample size of at least 218 of those non-cohabitating and of at least 305 of those cohabitating. Our sample size was thus large enough. Our study is one of the few that took place during the second COVID-19-related lockdown. By making the questionnaire available in both French and Dutch, we were able to obtain a sample that is more representative of the Belgian population. This approach ensured inclusivity and minimized potential language-related biases that might have arisen if the questionnaire had been accessible in only one language.
It is important to note that the arrows in the DAG indicate directional dependence rather than causal relationships. Directional dependence means that in the relationship x -> y, the presence of the node y more strongly implies the presence of the node x than vice versa [31]. The interpretation of the results regarding the people living with their partner and non-family members was limited due to the small sample size of this subgroup. Furthermore, these pre-lockdown data were collected retrospectively, which led to a potential recall bias. However, as mentioned, these data are part of a larger study wherein we collected data during the first and the second lockdowns. Both questionnaires had many questions in common, including the questions about sleep and mental health, which were used in this study. While we did not collect mail addresses, it is possible that some people replied to both questionnaires. During both lockdowns, participants were asked to recall their pre-pandemic sleep and mental health retrospectively. During the first lockdown, participants were prompted to reflect on a situation that occurred approximately a month prior, a timeframe commonly utilized in questionnaires. During the second lockdown, participants were recalling a situation that occurred more than six months earlier. Despite this temporal discrepancy, our previous analyses indicated that the results regarding pre-pandemic sleep and mental health collected during the second lockdown closely mirrored those obtained during the first lockdown [32]. Consequently, we believe that any potential recall bias was minimal.
This study omitted the measurement of certain concepts such as relationship satisfaction, loneliness, current touch exposure, and longing for touch, leaving gaps in our understanding. Additionally, the broader concept of relational lifestyle satisfaction poses challenges in accurately gauging how individuals interpret it. The interpretation of the results regarding NPC and NRL-SC is limited by not knowing whether that need was fulfilled. It is possible that some people who were not cohabitating with a partner actually had one. However, people cohabiting were not asked whether they were in a relationship. Finally, we lack data from the first lockdown, which limits interpretations.
4.4. Implications and Suggestions for Further Research
This paper gives a first impression of the relationship between physical and real-life social contact, mental health, and sleep by means of a network analysis. More research is needed in this field to understand the nature of these relationships better. Note that we obtained data before and during the second lockdown in Belgium but not post-lockdown. Research on post-lockdown effects is valuable in investigating whether the effects found can be recovered in a given time frame. It would also be interesting to investigate possible causal relationships between these variables through temporal networks.
5. Conclusions
During the second lockdown, individuals with greater NPC and NRL-SC reported poorer mental health (i.e., worry, depression, and mental fatigue). Younger individuals reported experiencing fewer DMS, more mental fatigue, and a greater NRL-SC with non-family compared with older individuals. Sex was either not or weakly associated with the other variables in our networks despite the well-documented greater prevalence of anxiety, depression, and insomnia among women. Additionally, sleep satisfaction was linked with a higher relational lifestyle satisfaction. Individuals satisfied with their relational lifestyle reported lower levels of depressive feelings and a greater NPC with family members.
NPC with non-family members and relational lifestyle satisfaction was lower during the second lockdown compared with before the pandemic. Overall, individuals in a romantic relationship who are living alone or cohabiting with their partner reported a higher NPC with family members (which includes the partner) and relational lifestyle satisfaction.
Acknowledgments
Since most of the authors do not have English as a mother tongue, we used a Large Language Model (LLM) to correct grammar and spelling mistakes and to reformulate certain sentences to make them more readable. The code necessary for making Figure 3 and Figure 4 was controlled by the ChatGPT code interpreter.
Appendix A
Table A1.
Items and answer options.
| Variable Name | Item | Answer Options |
|---|---|---|
| Cohabitation | I live alone/I do not live alone | |
| Relational lifestyle satisfaction | Since the second lockdown, I am … about my current relational lifestyle (married, in a romantic relationship, …). | Very unsatisfied/unsatisfied/satisfied/very satisfied |
| Need for physical contact with family | Since the second/before (the) lockdown, I need(ed) physical contact or hugs with my family and/or partner. | Not at all/slightly/moderately/a lot/extremely |
| Need for real-life social contact with family | Since the second/before (the) lockdown, I need(ed) to see my family and/or partner outside of virtual contacts (video calls, social media, …). | Not at all/slightly/moderately/a lot/extremely |
| Need for physical contact with non-family | Since the second/before (the) lockdown, I need(ed) physical contact or hugs with non-family members (friends, colleagues, …). | Not at all/slightly/moderately/a lot/extremely |
| Need for real-life social contact with non-family | Since the second/before (the) lockdown, I need(ed) to see non-family members (friends, colleagues, …) outside of virtual contacts (video calls, social media, …). | Not at all/slightly/moderately/a lot/extremely |
| DIS | Difficulty falling asleep | None/mild/moderate/severe/very severe |
| DMS | Difficulty staying asleep | None/mild/moderate/severe/very severe |
| EMA | Problem waking up too early in the morning | None/mild/moderate/severe/very severe |
| Sleep dissatisfaction | How satisfied/dissatisfied are you with your current sleep pattern? | Very satisfied/satisfied/neutral/dissatisfied/very dissatisfied |
| Mental fatigue | Since/before the lockdown, I need(ed) to get some mental rest | Not at all/slightly/moderately/a lot/extremely |
| Worry | Since/before the lockdown, I feel/felt worried | Not at all/slightly/moderately/a lot/extremely |
| Depressive feelings | Since/before the lockdown, I feel/felt depressed | Not at all/slightly/moderately/a lot/extremely |
Table A2.
Edge weights of the BGCGM.
| X1 | X2 | X3 | X4 | X5 | X6 | X7 | X8 | X9 | X10 | X11 | X12 | X13 | X14 | X15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| X1 | |||||||||||||||
| X2 | −0.134 | ||||||||||||||
| X3 | 0.042 | −0.130 | |||||||||||||
| X4 | 0.014 | 0.010 | 0.308 | ||||||||||||
| X5 | 0.044 | −0.000 | 0.146 | 0.092 | |||||||||||
| X6 | −0.015 | −0.000 | −0.000 | −0.128 | 0.210 | ||||||||||
| X7 | 0.104 | −0.002 | 0.000 | 0.000 | 0.320 | −0.001 | |||||||||
| X8 | −0.068 | −0.016 | −0.005 | −0.007 | −0.024 | 0.397 | 0.356 | ||||||||
| X9 | 0.002 | −0.054 | −0.065 | 0.000 | 0.000 | 0.000 | 0.000 | 0.006 | |||||||
| X10 | 0.000 | 0.166 | 0.000 | 0.000 | 0.000 | 0.003 | −0.004 | 0.000 | 0.114 | ||||||
| X11 | −0.003 | 0.002 | 0.000 | −0.002 | 0.000 | 0.007 | 0.003 | 0.004 | 0.000 | 0.220 | |||||
| X12 | −0.000 | 0.000 | 0.000 | −0.071 | 0.000 | 0.000 | 0.000 | −0.000 | 0.297 | 0.346 | 0.219 | ||||
| X13 | 0.090 | −0.143 | 0.000 | −0.000 | 0.083 | 0.000 | 0.000 | 0.032 | 0.000 | 0.002 | 0.068 | 0.146 | |||
| X14 | 0.013 | −0.000 | 0.000 | 0.003 | 0.000 | 0.000 | 0.080 | 0.000 | 0.074 | 0.118 | 0.054 | −0.000 | 0.273 | ||
| X15 | −0.001 | −0.019 | −0.003 | −0.186 | 0.000 | 0.056 | 0.000 | 0.069 | 0.107 | 0.000 | 0.014 | 0.065 | 0.217 | 0.359 |
Note: X1 = sex; X2 = age; X3 = cohabitation; X4 = relational lifestyle satisfaction; X5 = need for physical contact with family; X6 = need for physical contact with non-family; X7 = need for real-life social contact with family; X8 = need for real-life social contact with non-family; X9 = difficulties initiating sleep; X10 = difficulties maintaining sleep; X11 = early morning awakenings; X12 = sleep dissatisfaction; X13 = mental fatigue; X14 = worry; X15 = depressive feelings.
Figure A1.
Evidence plot for present edges. Note: Blue represents edges for which there is evidence of presence (BF > 10). Grey represents edges for which there is not enough evidence to include them (1 < BF < 10). NPC family = need for physical contact with family members; NPC non-family = need for physical contact with non-family members; NRL-SC family = need for real-life social contact with family members; NRL-SC non-family = need for real-life social contact with non-family members; DIS = difficulties initiating sleep; DMS = difficulties maintaining sleep; EMA = early morning awakenings.
Figure A2.
Evidence plot for absent edges. Note: Red represents edges for which there is evidence of absence (BF < 0.1). Grey represents edges for which there is inconclusive evidence to exclude them (0.1 < BF < 1). NPC family = need for physical contact with family members; NPC non-family = need for physical contact with non-family members; NRL-SC family = need for real-life social contact with family members; NRL-SC non-family = need for real-life social contact with non-family members; DIS = difficulties initiating sleep; DMS = difficulties maintaining sleep; EMA = early morning awakenings.
Table A3.
Strength, BIC values, and directional probabilities.
| From | To | Strength | BIC Value | Directional Probability |
|---|---|---|---|---|
| Sex | Cohabitation | 0.55 | −0.39 | 1.00 |
| Age | NRL-SC family | 0.68 | −24.41 | 1.00 |
| Age | NRL-SC non-family | 1.00 | −44.87 | 1.00 |
| Age | DMS | 1.00 | −47.65 | 1.00 |
| Age | Mental fatigue | 1.00 | −59.93 | 1.00 |
| Age | Depressive feelings | 0.55 | 2.47 | 1.00 |
| Cohabitation | Relational lifestyle satisfaction | 1.00 | −72.44 | 1.00 |
| Cohabitation | NPC family | 1.00 | −33.56 | 1.00 |
| Relational lifestyle satisfaction | NPC non-family | 0.99 | −6.09 | 0.53 |
| Relational lifestyle satisfaction | Sleep dissatisfaction | 0.94 | −6.31 | 0.76 |
| NPC family | Relational lifestyle satisfaction | 1.00 | −28.28 | 0.61 |
| NPC family | NRL-SC non-family | 0.56 | −49.29 | 0.51 |
| NRL-SC family | NPC family | 1.00 | −269.74 | 0.55 |
| NRL-SC non-family | NPC non-family | 1.00 | −354.91 | 0.63 |
| DMS | EMA | 1.00 | −95.65 | 0.71 |
| DMS | Sleep dissatisfaction | 1.00 | −408.58 | 0.54 |
| DMS | Worry | 0.99 | −28.36 | 0.51 |
| Sleep dissatisfaction | DIS | 1.00 | −271.69 | 0.58 |
| Sleep dissatisfaction | EMA | 1.00 | −66.32 | 0.64 |
| Mental fatigue | NPC family | 0.89 | −7.36 | 0.52 |
| Mental fatigue | NRL-SC family | 0.52 | −11.43 | 0.52 |
| Mental fatigue | DMS | 0.59 | −169.51 | 0.69 |
| Mental fatigue | Sleep dissatisfaction | 1.00 | −32.25 | 0.58 |
| Mental fatigue | Worry | 1.00 | −113.70 | 0.63 |
| Mental fatigue | Depressive feelings | 1.00 | −389.66 | 0.53 |
| Worry | NRL-SC family | 0.88 | −11.68 | 0.52 |
| Worry | DIS | 0.55 | −1.19 | 0.51 |
| Worry | EMA | 0.61 | −0.18 | 0.67 |
| Worry | Sleep dissatisfaction | 0.53 | 0.58 | 0.67 |
| Depressive feelings | Relational lifestyle satisfaction | 1.00 | −164.29 | 0.56 |
| Depressive feelings | NPC non-family | 0.88 | −9.09 | 0.74 |
| Depressive feelings | NRL-SC non-family | 0.88 | −61.01 | 0.68 |
| Depressive feelings | DIS | 1.00 | −22.76 | 0.72 |
| Depressive feelings | EMA | 0.77 | −1.83 | 0.73 |
| Depressive feelings | Sleep dissatisfaction | 0.64 | −3.25 | 0.75 |
| Depressive feelings | Worry | 1.00 | −289.18 | 0.74 |
Note: NPC family = need for physical contact with family members; NPC non-family = need for physical contact with non-family members; NRL-SC family = need for real-life social contact with family members; NRL-SC non-family = need for real-life social contact with non-family members; DIS = difficulties initiating sleep; DMS = difficulties maintaining sleep; EMA = early morning awakenings.
Author Contributions
Conceptualization, A.R., M.V.P. and O.M.; Data curation, A.R.; Formal analysis, A.R. and L.S.; Funding acquisition, A.R. and L.S.; Investigation, A.R. and O.M.; Methodology, A.R., M.V.P. and O.M.; Project administration, A.R., M.V.P. and O.M.; Resources, A.R. and O.M.; Software, A.R.; Supervision, M.V.P., F.M. and O.M.; Validation, A.R.; Visualization, A.R.; Writing—original draft, A.R. and L.S.; Writing—review and editing, A.R., L.S., F.M. and O.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Comité d’éthique Hospitalier (hospital ethical committee) of the Brugmann Hospital (Brussels, Belgium; reference: CE 2023/40, approved on 14 February 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The dataset analyzed during the current study is available at the Open Science Framework, https://osf.io/tv2dw/, accessed on 2 February 2024.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
A.R. (11N8923N) and L.S. (11M0123N) are funded by the Fonds Wetenschappelijk Onderzoek (FWO, Belgium).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Belga 1 Jaar Corona—Een Chronologisch Overzicht. [(accessed on 28 June 2024)]. Available online: https://www.despecialist.eu/nl/nieuws/1-jaar-corona-een-chronologisch-overzicht.html.
- 2.Hale T., Angrist N., Goldszmidt R., Kira B., Petherick A., Phillips T., Webster S., Cameron-Blake E., Hallas L., Majumdar S., et al. A Global Panel Database of Pandemic Policies (Oxford COVID-19 Government Response Tracker) Nat. Hum. Behav. 2021;5:529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- 3.Alimoradi Z., Broström A., Tsang H.W.H., Griffiths M.D., Haghayegh S., Ohayon M.M., Lin C.-Y., Pakpour A.H. Sleep Problems during COVID-19 Pandemic and Its’ Association to Psychological Distress: A Systematic Review and Meta-Analysis. eClinicalMedicine. 2021;36:100916. doi: 10.1016/j.eclinm.2021.100916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roland A., Colomb C., Noël S., Putilov A., Oginska H., Delwiche B., Benkirane O., Windal M., Vanlaer N., Briganti G., et al. Prevalence of Insomnia and Sleep Habits during the First and Second Wave of COVID-19 in Belgium. Psychol. Belg. 2023;63:18–29. doi: 10.5334/pb.1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of Mental Health Problems during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. J. Affect. Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Durkin J., Jackson D., Usher K. Touch in Times of COVID-19: Touch Hunger Hurts. J. Clin. Nurs. 2021;30:e4–e5. doi: 10.1111/jocn.15488. [DOI] [PubMed] [Google Scholar]
- 7.Meijer L.L., Hasenack B., Kamps J.C.C., Mahon A., Titone G., Dijkerman H.C., Keizer A. Affective Touch Perception and Longing for Touch during the COVID-19 Pandemic. Sci. Rep. 2022;12:3887. doi: 10.1038/s41598-022-07213-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hasenack B., Meijer L.L., Kamps J.C.C., Mahon A., Titone G., Dijkerman H.C., Keizer A. Longing for Touch and Quality of Life during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2023;20:3855. doi: 10.3390/ijerph20053855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.von Mohr M., Kirsch L.P., Fotopoulou A. Social Touch Deprivation during COVID-19: Effects on Psychological Wellbeing and Craving Interpersonal Touch. R. Soc. Open Sci. 2021;8:210287. doi: 10.1098/rsos.210287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Field T., Poling S., Mines S., Bendell D., Veazey C. Touch Deprivation and Exercise during the COVID-19 Lockdown April 2020. Med. Res. Arch. 2020;8 doi: 10.18103/mra.v8i8.2204. [DOI] [Google Scholar]
- 11.Morin C.M. Insomnia: Psychological Assessment and Management. Guilford Press; New York, NY, USA: 1993. [Google Scholar]
- 12.Bastien C. Validation of the Insomnia Severity Index as an Outcome Measure for Insomnia Research. Sleep. Med. 2001;2:297–307. doi: 10.1016/S1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 13.Huth K.B.S., de Ron J., Goudriaan A.E., Luigjes J., Mohammadi R., van Holst R.J., Wagenmakers E.-J., Marsman M. Bayesian Analysis of Cross-Sectional Networks: A Tutorial in R and JASP. Adv. Methods Pract. Psychol. Sci. 2023;6 doi: 10.1177/25152459231193334. [DOI] [Google Scholar]
- 14.Scutari M. Learning Bayesian Networks with the Bnlearn R Package. J. Stat. Softw. 2010;35:1–22. doi: 10.18637/jss.v035.i03. [DOI] [Google Scholar]
- 15.Gentry J., Gentleman R., Huber W. How to Plot a Graph Using Rgraphviz. [(accessed on 28 June 2024)]. Available online: http://www.bioconductor.org/packages/release/bioc/vignettes/Rgraphviz/inst/doc/
- 16.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Lawrence Erlbaum; Hillsdale, NJ, USA: 1988. [Google Scholar]
- 17.Wallsten D., Norell A., Anniko M., Eriksson O., Lamourín V., Halldin I., Kindbom T., Hesser H., Watkins E., Tillfors M. Treatment of Worry and Comorbid Symptoms within Depression, Anxiety, and Insomnia with a Group-Based Rumination-Focused Cognitive-Behaviour Therapy in a Primary Health Care Setting: A Randomised Controlled Trial. Front. Psychol. 2023;14:1196945. doi: 10.3389/fpsyg.2023.1196945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pahl R., Pevalin D.J. Between Family and Friends: A Longitudinal Study of Friendship Choice. Br. J. Sociol. 2005;56:433–450. doi: 10.1111/j.1468-4446.2005.00076.x. [DOI] [PubMed] [Google Scholar]
- 19.Altemus M., Sarvaiya N., Neill Epperson C. Sex Differences in Anxiety and Depression Clinical Perspectives. Front. Neuroendocrinol. 2014;35:320–330. doi: 10.1016/j.yfrne.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang B., Wing Y.-K. Sex Differences in Insomnia: A Meta-Analysis. Sleep. 2006;29:85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]
- 21.Tai T., Baxter J., Hewitt B. Do Co-Residence and Intentions Make a Difference? Relationship Satisfaction in Married, Cohabiting, and Living Apart Together Couples in Four Countries. Demogr. Res. 2014;31:71–104. doi: 10.4054/DemRes.2014.31.3. [DOI] [Google Scholar]
- 22.Leach L.S., Butterworth P., Olesen S.C., Mackinnon A. Relationship Quality and Levels of Depression and Anxiety in a Large Population-Based Survey. Soc. Psychiatry Psychiatr. Epidemiol. 2013;48:417–425. doi: 10.1007/s00127-012-0559-9. [DOI] [PubMed] [Google Scholar]
- 23.Maier S.F., Seligman M.E. Learned Helplessness: Theory and Evidence. J. Exp. Psychol. Gen. 1976;105:3–46. doi: 10.1037/0096-3445.105.1.3. [DOI] [Google Scholar]
- 24.Devine S.L., Walker S.C., Makdani A., Stockton E.R., McFarquhar M.J., McGlone F.P., Trotter P.D. Childhood Adversity and Affective Touch Perception: A Comparison of United Kingdom Care Leavers and Non-Care Leavers. Front. Psychol. 2020;11:557171. doi: 10.3389/fpsyg.2020.557171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Franken I., Wiers R. Motivational Processes in Addiction: The Role of Craving, Salience and Attention. Tijdschr. Psychiatr. 2013;55:833–840. [PubMed] [Google Scholar]
- 26.Sailer U., Ackerley R. Exposure Shapes the Perception of Affective Touch. Dev. Cogn. Neurosci. 2019;35:109–114. doi: 10.1016/j.dcn.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walker S.C., McGlone F.P. The Social Brain: Neurobiological Basis of Affiliative Behaviours and Psychological Well-Being. Neuropeptides. 2013;47:379–393. doi: 10.1016/j.npep.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 28.Hamermesh D.S. Life Satisfaction, Loneliness and Togetherness, with an Application to Covid-19 Lock-Downs. Rev. Econ. Househ. 2020;18:983–1000. doi: 10.1007/s11150-020-09495-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Balzarini R.N., Muise A., Zoppolat G., Di Bartolomeo A., Rodrigues D.L., Alonso-Ferres M., Urganci B., Debrot A., Bock Pichayayothin N., Dharma C., et al. Love in the Time of COVID: Perceived Partner Responsiveness Buffers People from Lower Relationship Quality Associated with COVID-Related Stressors. Soc. Psychol. Personal. Sci. 2023;14:342–355. doi: 10.1177/19485506221094437. [DOI] [Google Scholar]
- 30.Pieh C., O’Rourke T., Budimir S., Probst T. Relationship Quality and Mental Health during COVID-19 Lockdown. PLoS ONE. 2020;15:e0238906. doi: 10.1371/journal.pone.0238906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McNally R.J., Robinaugh D.J., Deckersbach T., Sylvia L.G., Nierenberg A.A. Estimating the symptom structure of bipolar disorder via network analysis: Energy dysregulation as a central symptom. J. Psychopathol. Clin. Sci. 2022;131:86. doi: 10.1037/abn0000715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roland A., Windal M., Briganti G., Kornreich C., Mairesse O. Intensity and Network Structure of Insomnia Symptoms and the Role of Mental Health during the First Two Waves of the COVID-19 Pandemic. Nat. Sci. Sleep. 2023;15:1003–1017. doi: 10.2147/NSS.S432944. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset analyzed during the current study is available at the Open Science Framework, https://osf.io/tv2dw/, accessed on 2 February 2024.