Abstract
Background: Maxillary sinus lift is a well-documented and accepted technique in the rehabilitation of the posterior maxilla. Schneiderian membrane perforation is the most common complication and may occur in between 7% and 56% of cases. Different materials and techniques have been described to achieve reparation of the perforation. The aim of this study was to establish whether the perforation of the Schneiderian membrane and its repair during maxillary sinus lift surgery results in a lower implant survival rate compared to those cases where the membrane has not been perforated. Materials and methods: A systematic review and meta-analysis of studies assessing the survival rate of implants placed in regenerated sinus using the lateral window approach, where the perforation of the Schneiderian membrane occur, was carried out. Statistical analysis was performed with Open Meta-Analyst, calculating the odds ratio of implants placed in perforated sinuses and non-perforated sinuses. Results: Ten articles were included in the qualitative analysis and seven articles in the quantitative analysis or meta-analysis. A total of 1224 maxillary sinus augmentation surgeries were performed without perforation of the Schneiderian membrane and 2725 implants were placed; 62 implants failed during the follow-up period with an overall survival rate of 97.7%. In 480 perforated sinuses, 1044 implants were placed, of which 30 failed; the overall survival rate was 97.1%. There were no significant differences between the implant survival rate of the implants in the two groups (OR = 0.78; CI = 0.49–2.23; p = 0.28 and I2 heterogeneity: 0%, p = 0.44). Conclusions: Schneiderian membrane perforation, as long as it is repaired, does not appear to negatively influence implant survival rate. Membrane perforation should not be considered a reason to abort the procedure or an absolute contraindication to implant placement.
Keywords: maxillary sinus membrane, sinus floor augmentation, dental implants, bone regeneration
1. Introduction
Implant rehabilitation of the posterior maxilla can be a challenge for the professional due to the pneumatization of the maxillary sinus or bone resorption after tooth loss [1]. The insufficient bone height can condition the correct placement of the implants; in these cases, it may be necessary to implement techniques that help us increase the bone availability, such as guided bone regeneration using resorbable and non-resorbable membranes, block graft, and bone distraction, among others [2,3], being that the sinus lift is one of the most-performed techniques [4].
Sinus lift is a well-documented and accepted technique in posterior maxilla rehabilitation and was introduced by Tatum H [5] and Boyne and James [6] in the 1980s. The open technique consists of preparing a window on the lateral aspect of the maxillary sinus and subsequently releasing and elevating the Schneiderian membrane, allowing the space between the membrane and the bone to be filled with graft material [7].
Schneiderian membrane perforation is the most frequent complication during a sinus lift and can occur in between 7% and 56% of cases [8,9,10,11,12]. There are various factors, both anatomical and technical, that influence the perforation, including the thickness of the membrane, previous sinus pathology, the presence of sinus septa, existing perforations, the design of the osteotomy, inadequate management of the membrane, and/or the surgeons experience [12,13,14,15]. Different techniques have been described to solve perforations, such as membrane suturing and the use of collagen membranes and fibrin glues, among others [11,13,16,17].
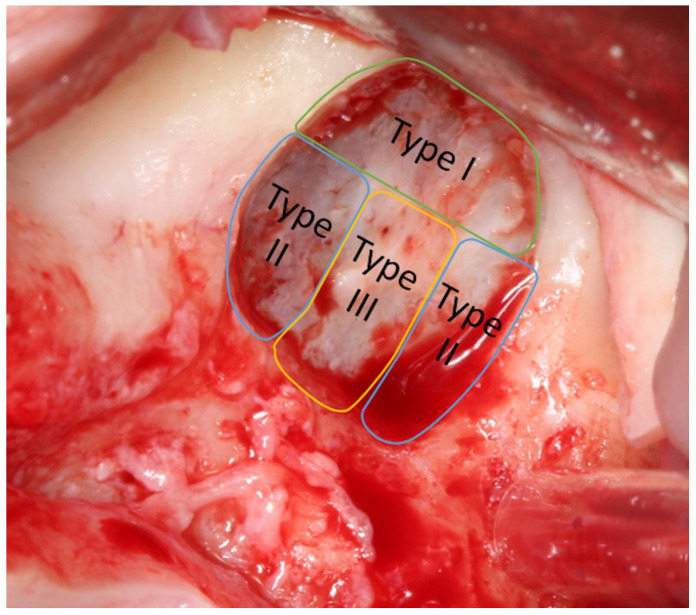
Fugazzotto and Vlassis [13] proposed a classification for perforations according to size and the difficulty of reparation. Class I perforations are those that occur in the upper part of the osteotomy; the separation of the membrane from the bone will eventually close due to membrane folding upon itself. Class II occurs close to the lateral or lower walls of the osteotomy and its treatment is more complex. Class III perforations are located right in the center of the osteotomy window and are frequently preexisting, either due to a previous traumatic dental extraction or an oroantral fistula, although they can occur during the preparation of the membrane as well; their clinical management is similar to those of class II (Figure 1).
Figure 1.
Diagram created by the authors to illustrate the classification of the perforations of the maxillary sinus membrane described by Fugazzotto and Vlassis [13].
The most frequent postoperative complications associated with sinus elevation that we can find are acute sinusitis, infection, and loss of graft material; the last of which, according to some studies, is greater in sinuses with perforated membranes. For this reason, some authors believe that there may be a relationship between perforation of the membrane during sinus lift and implant failure [8,16,18].
The aim of this systematic review and meta-analysis is to establish whether perforation of Schneiderian membrane and its repair during maxillary sinus lift results in a lower implant survival rate compared to sinus elevations where the membrane has not been perforated.
2. Materials and Methods
2.1. Data Sources and Search Criteria
The following review was written using PRISMA guidelines [19].
The PICO question that arises is: Does perforation of Schneiderian membrane cause an increased risk of implant failure? (P) Patient/Problem: perforation of Schneiderian membrane during sinus lift; (I) Intervention: Membrane repair; (C) Control: Sinus elevations without perforation of the membrane; (O) Result: decreased survival rate.
A bibliographic research was carried out on the Medline/Pubmed, Scopus and Web of Science platforms on May 2024 using the MeSH term “Sinus floor Augmentation” associated with Boolean operators AND and OR, combined with the following keywords: (“Schneiderian membrane” OR “Maxillary Sinus Membrane” OR “Sinus Augmentation” OR “Sinus Lift” OR “Sinus Floor Elevation”) AND (“Perforation Repair” OR “Schneiderian membrane perforation” OR “maxillary sinus membrane perforation”) AND (“Implant survival”).
2.2. Inclusion and Exclusion Criteria
Inclusion and exclusion criteria were compiled to ensure methodological consistency across all studies being included in the meta-analysis and to address potential study-level bias.
The search was limited to articles in English. The inclusion criteria were prospective and retrospective in vivo human studies. Only those articles where sinus elevation was performed using the lateral window technique with the placement of graft material were included. The sample had to include sinus elevations where perforation of the Schneiderian membrane occurred, and the repair technique used was described. Studies with a follow-up period of at least 6 months after prosthesis placement were included. Randomized and non-randomized clinical trials, cohort studies, case-control studies, and case series were accepted. Bibliographic reviews, systematic reviews and meta-analysis, clinical trials in animal models, and reports of clinical cases were excluded. Studies in which no graft material was used after sinus lift, that included elevation using the transcrestal technique, or that were associated with other bone regeneration techniques in the sample were considered not to meet the inclusion criteria, as were studies that did not specify the number of lost implants or the type of bone graft material that was used.
2.3. Data Extraction
All titles were analyzed to rule out irrelevant, repeated, animal model, or in vitro studies. The abstracts were then analyzed to assess the basic characteristics of the study. The publications that remained after abstract analysis were subjected to a full text study and chosen according to the inclusion and exclusion criteria.
The information extracted from the articles was: authors, year of publication, study design, number of patients included, graft material used in sinus lift, number of sinus lifts, number of sinuses with membrane perforation, material used for membrane repair, incidence of membrane perforation, number of implants placed, and number of failed implants.
2.4. Risk of Bias
To assess any potential risk of bias, the authors critically appraised each study by the Newcastle–Ottawa Scale. It was developed to assess the quality of nonrandomized studies. A ‘star system’ has been developed in which a study is judged on three broad perspectives: the selection of the study groups; the comparability of the groups; and the ascertainment of either the exposure or the outcome of interest for case-control or cohort studies, respectively [20].
2.5. Variables Studied and Statistical Analysis
The only variable studied was the survival rate of implants placed in sinuses where Schneiderian membrane perforation occurred compared to non-perforated membranes. The implants included in the study were those implants that remained present and functional during the follow-up period.
The data meta-analysis was performed with the Review Manager 5.4 to analyze the difference between implant survival rates in sinuses with perforated membranes and sinuses without perforation. The study group consisted of the sinuses where there was perforation of the Schneiderian membrane, while the control group consisted of the sinuses where there was no perforation. The analysis method used was the binary random effect and the odds ratio was calculated with a 95% confidence interval. The forest plot was made to graphically represent the results. The level of significance was established with p < 0.05. Heterogeneity among studies was considered statistically significant for a p-value < 0.05 and was interpreted as recommended by the Cochrane Handbook: 0–40% was considered unimportant, 30–60% as moderate heterogeneity, 50–90% as substantial heterogeneity, and 75–100% as considerable heterogeneity.
To evaluate the outcome between 1-stage and 2-stage implants performed in perforated membranes or in non-perforated, a subgroup analysis has been done.
3. Results
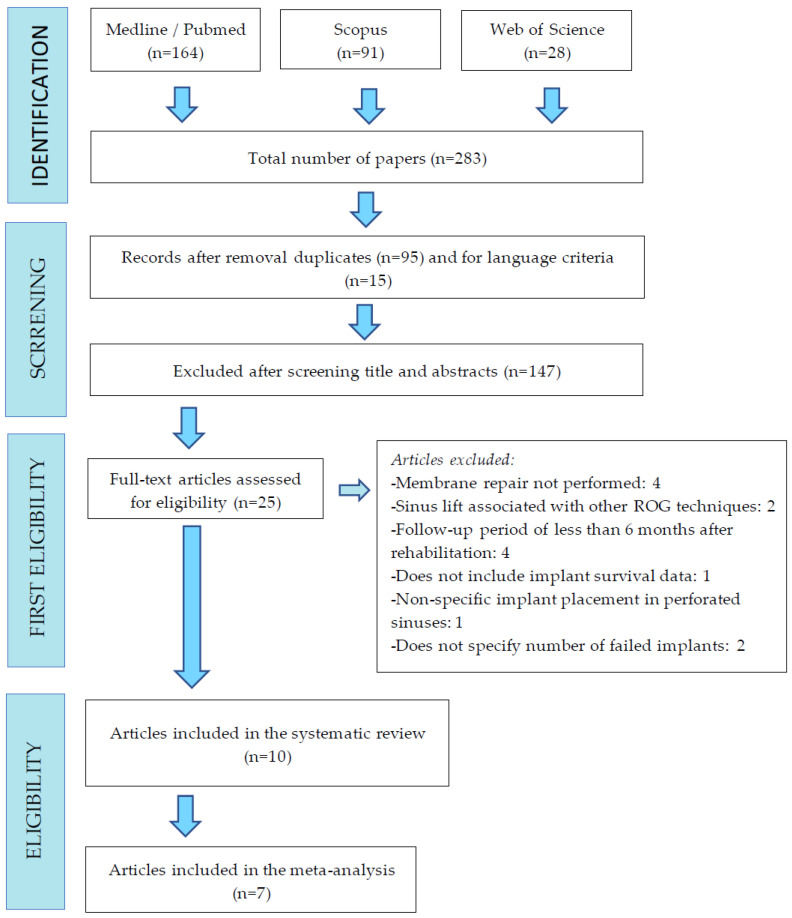
A total of 283 titles were obtained after the bibliographic research of Medline/Pubmed; in addition, 91 titles were obtained from Scopus and, finally, 28 from Web of Science. Fifteen articles were discarded because they were not written in English; 95 titles were duplicated. In the first screening of titles and abstracts, 26 articles were chosen for full-text reading. Of these 26 articles, 15 were discarded according to the inclusion and exclusion criteria. Finally, after reading the full text, 10 articles were selected to be analyzed (Figure 2).
Figure 2.
Flowchart illustrating the search strategy and selection process.
Of the articles included in the qualitative analysis (n = 10), five were retrospective observational studies classified as cohort studies [10,18,21,22,23], two were case-control studies [24,25], two were case series [26,27] and one was a clinical trial [28] (Table 1). Only seven articles were included in the quantitative analysis or meta-analysis [10,21,22,23,24,25,28].
Table 1.
Summary of the 10 articles reviewed. CM = Collagen Membrane. CTG = Connective Tissue Graft. FG = Fibrin glue. PRF = Platelet rich fibrin. * Autologous cortical bone obtained from the lateral window, symphysis block, or mandibular retromolar space.
| Author, Year | Type of Study | Graft Material | Schneiderian Membrane Repair | Follow-Up |
|---|---|---|---|---|
| Shlomi et al., 2004 [10] | Cohort study | Autologous | Lambone® demineralized human cortical bone | 24 months |
| Autologous + xenograft (Bio-Oss®) | ||||
| Hernández-Alfaro et al., 2007 [18] | Cohort study | Autologous + xenograft (Bio-Oss®) | Suture with Vicryl® | 6 months |
| CM (Bio-Gide®) | ||||
| Autologous block | Human cortical bone * | |||
| Bichat fat ball graft | ||||
| Oh and Kraut 2011 [21] | Cohort study | Alloplastic (hydroxyapatite + calcium carbonate Proosteon®) | Oxidized cellulose (Surgicel®) | 12 months |
| CM (Ace Surgical®) | ||||
| Gehrke et al., 2012 [26] | Case series | Alloplastic (hydroxyapatite NanoBone®) | CTG from palate | 12 months |
| Cha et al., 2012 [28] | Clinical trial | Xenograft (Bio-Oss®) | CM (Bio-Gide®) + FG (Greenplast®) | 36–98 months |
| Froum et al., 2013 [22] | Cohort study | Xenograft Bio-Oss®) | CM (Bio-Gide®/CollaTape®) | 6–32 months |
| Alloplastic (BoneCeramic®) | ||||
| Allograft (Puros®) | ||||
| Kim et al., 2016 [27] | Case series | Autologous | CM (Rapiderm®, Ossguide®, CollaTape®, Bio-Gide®) + fibrin | 6–60 months |
| Xenograft (Bio-Oss®) | ||||
| Allograft (Ora-Graft®) | ||||
| Alloplastic (Novosis®) | ||||
| Autologous + xenograft/Allograft | ||||
| Öncü and Kaymaz. 2017 [24] | Case Control | Xenograft (Apatos®) | PRF membrane | 6–12 months |
| De Almeida-Ferreira et al., 2017 [23] | Cohort study | Xenograft (Bio-Oss®) | Suture with Vicryl | 24 months |
| CM (CollaCote®) | ||||
| Krennmair et al., 2022 [25] | Case Control | Autologous + xenograft (Bio-Oss®) |
CM (Bio-Gide®) | 12 months |
In all studies, the surgical technique used was the sinus lift with a lateral window and graft material was used to fill the sinus. Five studies used only one type of biomaterial [21,23,24,26,28] and five used between two and four different types of biomaterials [10,18,22,25,27]. In four of them, autologous bone mixed with xenograft or allograft was used [10,18,25,27]. The most widely used was xenograft [10,18,22,23,24,25,27,28], followed by alloplastic graft [21,22,26,27], autologous bone with or without combining with xenograft or allograft [10,18,25,27], and lastly, allograft [22,27]. In the cases where there was perforation of the Schneiderian membrane (635 sinuses), seven of the studies performed repair with collagen membranes [18,21,22,23,25,27,28] and two of them were associated with fibrin glues [27,28]. Demineralized human cortical bone [10], suture of the membrane with vicryl [18,23], pedicled Bichat fat ball graft [18], block graft [18], oxidized cellulose [21], palatal connective tissue graft [26], and Platelet-rich fibrin membranes (PRF) [24] were also used for repair. The mean follow-up of the patients was 25.15 months (range 6–98 months).
The total number of patients included was 1666; a total of 2229 sinus lifts were performed, and 5052 implants were placed (range between 18 and 1588 implants). The sample size regarding implant placement in articles is heterogeneous. In two articles, fewer than 50 implants were placed [24,26]; in another two, fewer than 100 implants were placed [22,27]; in three, more than 200 but fewer than 500 were placed [10,21,28]; and in two, more than 1000 were placed [18,24] (Table 2).
Table 2.
Incidence of Schneiderian membrane perforation, postoperative measurements, implant placement, and complications. Pat = Patients. Imp = Implants. PSM = Perforation of Schneiderian Membrane. NE = Not Specified. ATB = Antibiotic. NSAIDs = Non-steroidal analgesics. CLH = Chlorhexidine.
| Author, Year | N.° Pat. | N.° sinus | N.° Imp | N.° PSM | Perforation Incidence (%) |
Postoperative Care | Implant Placement | Postoperative Complications | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Shlomi et al., 2004 [10] | 63 | 73 | 253 | 20 | 28% | NE | Simultaneous | NE | ||
| 2 phases 4–6 months | ||||||||||
| Hernández-Alfaro et al., 2007 [18] | 338 | 474 | 1166 | 104 | 21.9% | ATB/7 days NSAID |
Simultaneous | NE | ||
| Oh and Kraut 2011 [21] | 128 | 175 | 438 | 60 | 34% | NE | Simultaneous | 4 sinusitis | ||
| 2 phases 8 months | ||||||||||
| Gehrke et al., 2012 [26] | 10 | 10 | 18 | 10 | NE | ATB/7 days NSAID |
2 phases 6 months |
No complications | ||
| Cha et al., 2012 [28] | 161 | 217 | 462 | 35 | 16.1% | ATB/5 days NSAID/5 days Corticosteroids CLH 0.2% |
Simultaneous | NE | ||
| Froum et al., 2013 [22] | 23 | 40 | 80 | 15 | 37% | ATB/7–10 days CLH 0.12% |
2 phases 6–9 months |
NE | ||
| Kim et al., 2016 [27] | 41 | 41 | 99 | 41 | NE | ATB/3 days | Simultaneous | 8 sinusitis | ||
| 2 phases 4–6 months |
6 local infections | |||||||||
| 10 rhinorrheas | ||||||||||
| Öncü and Kaymaz. 2017 [24] | 16 | 20 | 35 | 10 | NE | ATB/14 days NSAID/14 days CLH 0.12% |
2 phases 6–8 months |
NE | ||
| de Almeida-Ferreira et al., 2017 [23] | 531 | 745 | 1588 | 237 | 31.8% | ATB/10 days NSAID CLH 0.12% |
Simultaneous | NE | ||
| 2 phases 6–10 months | ||||||||||
| Krennmair et al., 2022 [25] | 355 | 434 | 913 | 103 | 23.80% | NSAID, CLH, ATB/8 days, decongestant spray | Simultaneous | Sinusitis | ||
| 10 | 4 | |||||||||
| 2 phases | NE | Graft necrosis | ||||||||
| 7 | 1 | |||||||||
| Total | 1666 | 2229 | 5052 | 635 | ||||||
| Media | 29.42% | |||||||||
Schneiderian membrane perforation occurred in 635 sinuses (Range: 10–237) and the mean incidence of perforation was 29.42% (Table 2). Postoperative care was not specified in two articles [10,21]; in the remaining eight, all included antibiotic treatment, six of them were associated with non-steroidal anti-inflammatories [18,23,24,25,26,28], five with rinses with chlorhexidine 0.12–0.2% [22,23,24,25,28], and one with corticosteroids [28]. In all studies, postoperative care was the same for perforated and non-perforated sinus.
The placement of the implants was carried out simultaneously with the sinus lift or in two phases. In two articles, all the implants were placed during the same surgical procedure [18,28], and in three, they were placed during a surgery carried out between 6 and 9 months after sinus elevation [22,24,26]. In the remaining five articles [10,21,23,25,27], the implants were placed simultaneously or during a second surgery, depending on the height of the residual bone crest. Among the postoperative complications described are sinusitis [21,25,27], infection of the surgical wound [27], rhinorrhea [27], and graft necrosis [25]. Six articles did not specify whether or not there were postoperative complications [10,18,22,23,24,28], and in one of them, there were none [26] (Table 2).
The Newcastle–Ottawa scale [20] allowed to classify the case-control and cohort studies included in the systematic review as follows: two studies [18,22] scored 7 points and four studies [10,21,23,25] scored 6 points, so could be considered as low risk of bias; and one study [24] scored five points (Table 3).
Table 3.
Quality assessment of included studies using the Newcastle–Ottawa scale.
| Case-Control | Selection | Comparability | Exposure | Score (0–9) |
|---|---|---|---|---|
| Öncü and Kaymaz [24] | ★★★ | ★ | ★ | 5 |
| Krennmair et al. [25] | ★★★ | ★ | ★★ | 6 |
| Cohort Studies | Selection | Comparability | Outcome | Score (0–9) |
| De Almeida-Ferreira et al. [23] | ★★★ | ★ | ★★ | 6 |
| Oh et al. [21] | ★★★ | ★ | ★★ | 6 |
| Hernández-Alfaro et al. [18] | ★★★★ | ★ | ★★ | 7 |
| Froum et al. [22] | ★★★★ | ★ | ★★ | 7 |
| Shlomi et al. [10] | ★★★ | ★ | ★★ | 6 |
Three articles were discarded for the meta-analysis: The study carried out by Hernández-Alfaro et al. [18] was discarded for not specifying the data of the control group, and the studies by Gehrke et al. [26] and Kim et al. [27] were discarded because there was no control group.
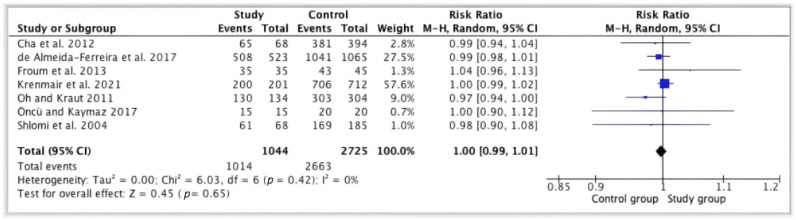
In total, 1224 sinus elevations were performed without perforation of the Schneiderian membrane, and 2725 implants were placed, of which 62 failed during the follow-up period, obtaining an overall survival rate of 97.7%. In 480 elevations where the membrane was perforated, 1044 implants were placed, of which 30 failed in the follow-up period, with an overall survival rate of 97%. There were no significant differences between the implant survival rates of the two groups (RR = 1.00; CI = 0.99, 1.01; p = 0.65); I2 heterogeneity was 0% (p = 0.42) (Figure 3).
Figure 3.
Forest plot; survival of implants in perforated versus non-perforated sinuses [10,21,22,23,24,25,28].
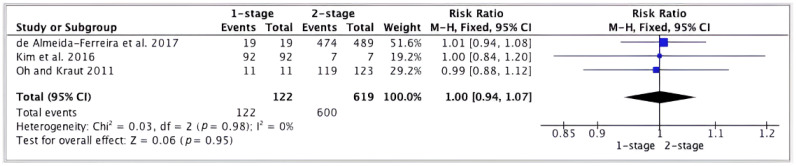
Regarding the evaluation of the outcome between one-stage and two-stage implants. A forest plot was made to represent the difference between the results of one-stage vs. two-stage implants performed in perforated membrane cases. Three articles [21,23,27] were chosen because, in their studies, the data of one-stage and two-stage were provided. The results were not statistically significant (RR = 1.00; CI = 0.94, 1.07; p = 0.95); I2 heterogeneity was 0% (p = 0.98) (Figure 4).
Figure 4.
Forest plot; survival of implants in perforated sinuses of one-stage vs. two-stage implants [21,23,27].
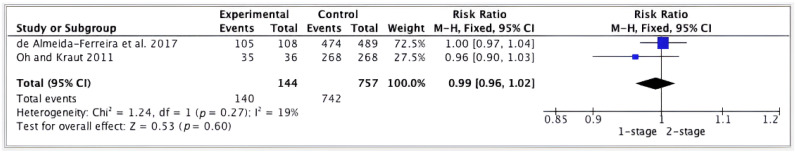
Focusing on the evaluation of the outcome between one-stage vs. two-stage implants in non-perforated sinus membranes, a forest plot was performed to represent the difference in these results. Two studies [21,23] provided data between one-stage and two-stage implants in non-perforated sinuses. The results were not statistically significant (RR = 0.99; CI = 0.96, 1.02; p = 0.60) and I2 heterogeneity was 19% (p = 0.27) (Figure 5).
Figure 5.
Forest plot; survival of implants in non-perforated sinuses of one-stage vs. two-stage implants [21,23].
4. Discussion
Lateral sinus window elevation is a well-known and predictable technique for implant rehabilitation of the atrophic maxilla [18,22,26]. As we already remarked, the most common intraoperative complication is Schneiderian membrane perforation, with an incidence between 16% and 56% [8,11,13,15,18,28]. In this review, results were found within this range, with a perforation rate of 29.42%. Different factors have been related to an increased risk of perforation. Ardekian et al. [29] found that 85% of the perforations occurred in patients with 3 mm residual alveolar ridges vs 25% in patients with 6 mm ridges. The presence of sinus septa is found amongst 13% and 35.3% of the sinuses [30]. Septed sinuses add difficulty to surgical management of the procedure since they increase the risk of perforation; it is advisable to adapt the osteotomy and divide it into smaller sections [18]. Other factors such as the design of the window, the size of the window, the presence of mucous retention cysts, and the skills and experience of the surgeon also play a fundamental role in the appearance of complications [12,13,15].
Some authors consider that the presence of perforations in the sinus membrane signifies a contraindication to continue the procedure [8,31,32]. However, in this review it was observed that there are techniques to repair or cover the membrane perforation without having to abort the procedure, with an overall implant survival rate (ISR) of 97.1% in sinuses with perforated and repaired membranes.
In this review, the complication of Schneiderian membrane perforation was found in 635 cases and was treated using different techniques and materials for its repair. Despite that the gold standard technique for the management of perforations is not described in the literature, most of the authors reviewed used collagen membranes [18,21,22,23,27,28]. Other less common alternative materials and techniques have also been described, and according to this review, have also proven to be effective. The absorbable suture [18,23] 25 and oxidized cellulose (Surgicel®) [12,21] are very frequently used and easily accessible materials, which can be useful in some cases. The average thickness of the Schneiderian membrane (1.32 ± 0.87 mm) should be taken into account [33] when considering closing the perforation with suturing, since it is a difficult procedure and requires high precision from the professional.
Techniques such as block grafts [18], connective tissue [26], the use of the Bichat fat ball [18,34], or the membranes of Platelet Rich Fibrin (PRF) [24,35,36] could have a better biocompatibility due to their autologous origin. These techniques are subjected to the biological availability of the tissue, instruments and equipment, in addition to the skills of the surgeon.
Other techniques reported in the literature include demineralized human cortical bone (Lambone® Pacific Coast Tissue Bank, Los Angeles, CA, USA) [10], fibrin glue (Greenplast® Green cross, Gyeonggi-do, Republic of Korea) [28,37], autologous periosteum grafts [38] and amniotic membranes (Amnion-Chorion barriers, BioXclude®, Snoasis Medical, Denver, CO, USA) [39].
In a study conducted by Hernández-Alfaro et al. [18], with a sample of 474 sinus elevations and the placement of 1166 implants, the perforations were classified according to size and the sample was divided into three groups. Of 104 perforations, those smaller than 5 mm were the most frequent, followed by perforations between 5–10 mm and, finally, those greater than 10 mm. The implant survival rate was 97.14%, 91.89%, and 74.14%, respectively. With these results, the authors concluded that the larger the perforation, the lower the implant survival rate. The data from this review lead to the conclusion that small perforations do not significantly influence the outcome of implant treatment.
In the study carried out by de Almeida-Ferreira et al. [23] with the placement of 1588 implants in 745 sinuses, the global ISR of implants placed in sinuses with perforated membranes was 97.1% and in sinuses with non-perforated membranes it was 97.7%. Within the group of perforated membranes, the perforations were divided similarly to the study by Hernández-Alfaro et al. [18]; in this study, a survival rate of 95.3% was obtained for large perforations, 97.3% for medium perforations, and 97.7% for small perforations. The ISR differences between the three groups were not statistically significant, and in the case of small perforations, it was exactly the same as in sinuses with non-perforated membranes. Schwartz-Arad et al. [9] found no relationship between membrane perforation and the presence of postoperative complications with the success of the implants. As long as the perforation of the membrane is properly treated, it will not influence the success of the implants [29]. Despite finding that the survival rate of implants in non-perforated sinus is higher than in perforated sinus, at 97.7% vs. 97,1% respectively, the difference between the two groups is not statistically significant.
Even though the difference in the inclusion criteria that allowed us to include more studies, our results confirm those reported by Diaz-Olivares et al. [40] in their systematic review and meta-analysis, where the ISR among perforated membranes was 97.71%, vs. 98.88% in the non-perforated group.
Al-Moraissi et al. [41], in their systematic review, observed a greater survival rate, with statistical significance, between the perforated membranes group (89.65%) and the non-perforated membranes group (97.51%). Nevertheless, it should be highlighted that the present systematic review only included the results of procedures using the lateral window approach, while the previous authors included both the lateral and crestal approaches.
Many authors hypothesize that the lower survival rate of implants in perforated sinuses is due to the displacement of biomaterial particles that can trigger an acute or chronic sinusitis, producing a reabsorption of the graft and compromising the prognosis of implants [16,18,42]. Amongst the complications of the procedure sinusitis, infection of the wound, rhinorrhea, and graft necrosis were described. In the study conducted by Krennmair et al. [25] a higher incidence of sinusitis was found in perforated membranes, similar to the results reported from Oh and Kraut [21].
Concerning the survival rate of one-stage or two-stage implants in perforated or intact Scheneridan membrane, non-statistically significant differences were found. The literature found similar survival rates for implants placed in one-stage or two-stage [23]. Hence, immediate and sinus lifting in one-stage could provide us benefits like the reduction of the number of surgeries or a decrease in the treatment time [28].
Regardless of the fact that sinus elevation is a highly predictable procedure [43] and the most used biomaterial for its elevation has been beta tricalcium phosphate [44], regarding the placement of implants in regenerated sinuses, i.e., simultaneously vs. delayed, it is still controversial. If the residual ridge is greater than 5 mm, implant stability is generally achieved [18]. However, if it is less than 5 mm, it can be considered insufficient mechanical support, advising a delayed placement [45]. Cha et al. [28] did not find statistically significant differences in the success rate of implants placed in residual alveolar ridges of >5 mm (97.33%) vs. <5 mm (95.50%) (p = 0.3135). In reference to this issue, some authors defend that the regenerative result of sinus lift is compromised by perforation of the membrane and, therefore, the simultaneous placement of implants should not be performed [10]. Other authors consider that perforation of the membrane should not be considered a contraindication for simultaneous implant placement [18].
If we focus on the quality of regenerated bone, Testori et al. [46] obtained between 22% and 26% of vital bone in sinuses with perforated membranes, using collagen membranes that allowed the containment of the graft. Similar results were obtained by Froum et al. [22] when conducting a histological and histomorphometric study, with a higher percentage of vital bone formed in sinuses with perforated membranes (26.3 ± 6.3%) than in sinuses with non-perforated membranes (19.1 ± 13.7%). A possible explanation for these results could be that the membrane placed between the Schneiderian membrane and the graft acts as a barrier, preventing soft tissue migration, or it performs better containment and immobilization of the graft material, facilitating revascularization [22].
The limitations of this study were the non-inclusion of other variables, such as the design and treatment of the implant surface, the type of graft material, the surgical skills of the surgeon, and the patient’s habits, which may influence the survival rate of the implants.
5. Conclusions
Schneiderian membrane perforation is a common complication in sinus elevations and can occur in up to 30.5% of cases. There are different materials and techniques that allow the membrane to be repaired and the perforation to be covered successfully. Schneiderian membrane perforation, as long as it is repaired, does not appear to negatively influence the implant survival rate. Considering the above points, membrane perforation should not be considered a reason to abort the procedure nor as an absolute contraindication to implant placement.
Author Contributions
Conceptualization, J.L.-L. and V.S.-D.F.; methodology, S.E.-M. and B.G.-N.; software, L.M.-G. and J.L.-L.; formal analysis, all authors; investigation, J.L.-L. and V.S.-D.F.; writing—original draft preparation, J.L.-L. and V.S.-D.F.; writing—review and editing, all authors; visualization, J.L.-L.; supervision, J.L.-L. and S.E.-M.; project administration, J.L.-L. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
The authors can provide details of the research upon request by letter commenting on their needs.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Mohan N., Wolf J., Dym H. Maxillary Sinus Augmentation. Dent. Clin. N. Am. 2015;59:375–388. doi: 10.1016/j.cden.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Polis-Yanes C., Cadenas-Sebastián C., Gual-Vaqués P., Ayuso-Montero R., Marí-Roig A., López-López L. Guided bone regeneration of an atrophic maxilla using heterologous cortical lamina. Case Rep. Dent. 2019;2019:5216362. doi: 10.1155/2019/5216362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arcas-Sanabre A.J., Gutierrez-Santamaria J., López-López J., Ayuso-Montero R., Velasco-Ortega E. Horizontal augmentation of the maxillary alveolar ridge to change the prosthetic profile: Clinical and radiological results of a retrospective study. J. Stomatol. Oral Maxillofac. Surg. 2020;121:25–29. doi: 10.1016/j.jormas.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Chiapasco M., Zaniboni Z. Methods to Treat the Edentulous Posterior Maxilla: Implants with Sinus Grafting. J. Oral Maxillofac. Surg. 2009;67:867–871. doi: 10.1016/j.joms.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 5.Tatum H.J. Maxillary and sinus implant reconstructions. Dent. Clin. N. Am. 1986;30:207–229. doi: 10.1016/S0011-8532(22)02107-3. [DOI] [PubMed] [Google Scholar]
- 6.Boyne P.J., James R.A. Grafting of the maxillary sinus floor with autogenous marrow and bone. J. Oral Surg. 1980;38:613–616. [PubMed] [Google Scholar]
- 7.Stern A., Green J. Sinus Lift Procedures: An Overview of Current Techniques. Dent. Clin. N. Am. 2012;56:219–233. doi: 10.1016/j.cden.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Khoury F. Augmentation of the sinus floor with mandibular bone block and simultaneous implantation: A 6-year clinical investigation. Int. J. Oral Maxillofac. Implant. 1999;14:557–564. [PubMed] [Google Scholar]
- 9.Schwartz-Arad D., Herzberg R., Dolev E. The Prevalence of Surgical Complications of the Sinus Graft Procedure and Their Impact on Implant Survival. J. Periodontol. 2004;75:511–516. doi: 10.1902/jop.2004.75.4.511. [DOI] [PubMed] [Google Scholar]
- 10.Shlomi B., Horowitz I., Kahn A., Dobriyan A., Chaushu G. The effect of sinus membrane perforation and repair with Lambone on the outcome of maxillary sinus floor augmentation: A radiographic assessment. Int. J. Oral Maxillofac. Implant. 2004;19:559–562. [PubMed] [Google Scholar]
- 11.Pikos M.A. Maxillary sinus membrane repair: Update on technique for large and complete perforations. Implant. Dent. 2008;17:24–31. doi: 10.1097/ID.0b013e318166d934. [DOI] [PubMed] [Google Scholar]
- 12.Nolan P.J., Freeman K., Kraut R.A. Correlation between schneiderian membrane perforation and sinus lift graft outcome: A retrospective evaluation of 359 augmented sinus. J. Oral Max Surg. 2014;72:47–52. doi: 10.1016/j.joms.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 13.Fugazzotto P.A., Vlassis J.A. Simplified Classification and Repair System for Sinus Membrane Perforations. J. Periodontol. 2003;74:1534–1541. doi: 10.1902/jop.2003.74.10.1534. [DOI] [PubMed] [Google Scholar]
- 14.Schwarz L., Schiebel V., Hof M., Ulm C., Watzek G., Pommer B. Risk Factors of Membrane Perforation and Postoperative Complications in Sinus Floor Elevation Surgery: Review of 407 Augmentation Procedures. J. Oral Max Sur. 2015;73:1275–1282. doi: 10.1016/j.joms.2015.01.039. [DOI] [PubMed] [Google Scholar]
- 15.Wen S.C., Lin Y.H., Yang Y.C., Wang H.L. The influence of sinus membrane thickness upon membrane perforation during transcrestal sinus lift procedure. Clin. Oral Implant. Res. 2015;26:1158–1164. doi: 10.1111/clr.12429. [DOI] [PubMed] [Google Scholar]
- 16.Proussaefs P., Lozada J., Kim J., Rohrer M.D. Repair of the perforated sinus membrane with a resorbable collagen membrane: A human study. Int. J. Oral Maxillofac. Implant. 2004;19:413–420. [PubMed] [Google Scholar]
- 17.Massei G., Romano F., Aimetti M. An Innovative Technique to Manage Sinus Membrane Perforations: Report of Two Cases. Int. J. Periodontics Restor. Dent. 2015;35:373–379. doi: 10.11607/prd.2195. [DOI] [PubMed] [Google Scholar]
- 18.Hernández-Alfaro F., Torradeflot M.M., Marti C. Prevalence and management of Schneiderian membrane perforations during sinus-lift procedures. Clin. Oral Implant. Res. 2008;19:91–98. doi: 10.1111/j.1600-0501.2007.01372.x. [DOI] [PubMed] [Google Scholar]
- 19.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 21.Oh E., Kraut R.A. Effect of sinus membrane perforation on dental implant integration: A retrospective study on 128 patients. Implant. Dent. 2011;20:13–19. doi: 10.1097/ID.0b013e3182061a73. [DOI] [PubMed] [Google Scholar]
- 22.Froum S.J., Khouly I., Favero G., Cho S.C. Effect of Maxillary Sinus Membrane Perforation on Vital Bone Formation and Implant Survival: A Retrospective Study. J. Periodontol. 2013;84:1094–1099. doi: 10.1902/jop.2012.120458. [DOI] [PubMed] [Google Scholar]
- 23.de Almeida-Ferreira C.E., Martinelli C.B., Novaes A.B., Pignaton T.B., Guignone C.C., Gonçalves-de Almeida A.L., Saba-Chujfi E. Effect of Maxillary Sinus Membrane Perforation on Implant Survival Rate: A Retrospective Study. Int. J. Oral Maxillofac. Implant. 2017;32:401–407. doi: 10.11607/jomi.4419. [DOI] [PubMed] [Google Scholar]
- 24.Öncü E., Kaymaz E. Assessment of the effectiveness of platelet rich fibrin in the treatment of Schneiderian membrane perforation. Clin. Implant. Dent. Relat. Res. 2017;19:1009–1014. doi: 10.1111/cid.12528. [DOI] [PubMed] [Google Scholar]
- 25.Krennmair S., Weinländer M., Forstner T., Malek M., Krennmair G., Postl L. The influence of different forms of sinus membrane perforation on the prevalence of postoperative complications in lateral window sinus floor elevation: A retrospective study. Clin. Implant. Dent. Relat. Res. 2022;24:13–23. doi: 10.1111/cid.13056. [DOI] [PubMed] [Google Scholar]
- 26.Gehrke S.A., Taschieri S., Del Fabbro M., Corbella S. Repair of a perforated sinus membrane with a subepithelial palatal conjunctive flap: Technique report and evaluation. Int. J. Dent. 2012;2012:489762. doi: 10.1155/2012/489762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim G.S., Lee J.W., Chong J.H., Han J.J., Jung S., Kook M.S., Park H.J., Ryu S.Y., Oh H.K. Evaluation of clinical outcomes of implants placed into the maxillary sinus with a perforated sinus membrane: A retrospective study. Maxillofac. Plast. Reconstr. Surg. 2016;38:50. doi: 10.1186/s40902-016-0097-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cha H., Kim A., Nowzari H., Chang H.S., Ahn K.M. Simultaneous Sinus Lift and Implant Installation: Prospective Study of Consecutive Two Hundred Seventeen Sinus Lift and Four Hundred Sixty-Two Implants. Clin. Implant. Dent. Relat. Res. 2014;16:337–347. doi: 10.1111/cid.12012. [DOI] [PubMed] [Google Scholar]
- 29.Ardekian L., Oved-Peleg E., Mactei E.E., Peled M. The clinical significance of sinus membrane perforation during augmentation of the maxillary sinus. J. Oral Max Sur. 2006;64:277–282. doi: 10.1016/j.joms.2005.10.031. [DOI] [PubMed] [Google Scholar]
- 30.Maestre-Ferrín L., Galán-Gil S., Rubio-Serrano M., Peñarrocha-Diago M., Peñarrocha-Oltra D. Maxillary sinus septa: A systematic review. Med. Oral Patol. Oral Cir. Bucal. 2010;15:10–13. doi: 10.4317/medoral.15.e383. [DOI] [PubMed] [Google Scholar]
- 31.Aimetti M., Romagnoli R., Ricci G., Massei G. Maxillary Sinus Elevation: The Effect of Macrolacerations and Microlacerations of the Sinus Membrane as Determined by Endoscopy. Int. J. Periodontics Restor. Dent. 2001;21:581–589. [PubMed] [Google Scholar]
- 32.Karabuda C., Arısan V., Hakan Ö. Effects of Sinus Membrane Perforations on the Success of Dental Implants Placed in the Augmented Sinus. J. Periodontol. 2006;77:1991–1997. doi: 10.1902/jop.2006.060102. [DOI] [PubMed] [Google Scholar]
- 33.Yin Y.H., Yang Y.C., Wen S.C., Wang H.L. The influence of sinus membrane thickness upon membrane perforation during lateral window sinus augmentation. Clin. Oral Implant. Res. 2016;27:612–617. doi: 10.1111/clr.12646. [DOI] [PubMed] [Google Scholar]
- 34.Kim Y.K., Hwang V.W., Yun P.Y. Closure of large perforation of sinus membrane using pedicled buccal fat pad graft: A case report. Int. J. Oral Maxillofac. Implant. 2008;23:1139–1142. [PubMed] [Google Scholar]
- 35.Baykul T., Yındık Y. Maxillary sinus perforation with presence of an antral pseudocyst, repaired with platelet rich fibrin. Ann. Maxillofac. Surg. 2014;4:205–207. doi: 10.4103/2231-0746.147144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pinto G.D.D.S., Pigossi S.C., Pessoa T., Nícoli L.G., Araújo R.F.S.B., Marcantonio C., Marcantonio E., Jr. Successful Use of Leukocyte Platelet-Rich Fibrin in the Healing of Sinus Membrane Perforation: A Case Report. Implant. Dent. 2018;27:375–380. doi: 10.1097/ID.0000000000000731. [DOI] [PubMed] [Google Scholar]
- 37.Shin H.I., Sohn D.S. A method of sealing perforated sinus membrane and histologic finding of bone substitutes: A case report. Implant. Dent. 2005;14:328–335. doi: 10.1097/01.id.0000188465.93052.cd. [DOI] [PubMed] [Google Scholar]
- 38.de Oliveira H.A.A.B., de Moraes R.P.F.P., Limirio H.J.O., Dechichi P. Repair of a perforated sinus membrane with an autogenous periosteal graft: A study in 24 patients. Br. J. Oral Maxillofac. Surg. 2018;56:299–303. doi: 10.1016/j.bjoms.2017.12.020. [DOI] [PubMed] [Google Scholar]
- 39.Holtzclaw D. Maxillary Sinus Membrane Repair with Amnion–Chorion Barriers: A Retrospective Case Series. J. Periodontol. 2015;86:936–940. doi: 10.1902/jop.2015.140087c. [DOI] [PubMed] [Google Scholar]
- 40.Díaz-Olivares L.A., Cortés-Bretón Brinkmann J., Martínez-Rodríguez N., Martínez-González J.M., López-Quiles J., Leco-Berrocal I., Meniz-García C. Management of Schneiderian membrane perforations during maxillary sinus floor augmentation with lateral approach in relation to subsequent implant survival rates: A systematic review and meta-analysis. Int. J. Implant. Dent. 2021;7:91. doi: 10.1186/s40729-021-00346-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Al-Moraissi E., Elsharkawy A., Abotaleb B., Alkebsi K., Al-Motwakel H. Does intraoperative perforation of Schneiderian membrane during sinus lift surgery causes an increased the risk of implants failure?: A systematic review and meta regression analysis. Clin. Implant. Dent. Relat. Res. 2018;20:882–889. doi: 10.1111/cid.12660. [DOI] [PubMed] [Google Scholar]
- 42.Nkenke E., Schlegel A., Schultze-Mosgau S., Neukam F.W., Wiltfang J. The endoscopically controlled osteotome sinus floor elevation: A preliminary prospective study. Int. J. Oral Maxillofac. Implant. 2000;17:557–566. [PubMed] [Google Scholar]
- 43.Velasco-Ortega E., Sierra-Baztan A., Jiménez-Guerra A., España-López A., Ortiz-Garcia I., Núñez-Márquez E., Moreno-Muñoz J., Rondón-Romero J.L., López-López J., Monsalve-Gui L. Long-Term Clinical Study of Implants Placed in Maxillary Sinus Floor Augmentation Using Beta-Tricalcium Phosphate. Int. J. Environ. Res. Public Health. 2021;18:9975. doi: 10.3390/ijerph18199975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Velasco-Ortega E., Valente N.A., Iezzi G., Petrini M., Derchi G., Barone A. Maxillary sinus augmentation with three different biomaterials: Histological, histomorphometric, clinical, and patient-reported outcomes from a randomized controlled trial. Clin. Implant. Dent. Relat. Res. 2021;23:86–95. doi: 10.1111/cid.12964. [DOI] [PubMed] [Google Scholar]
- 45.Peleg M., Mazor Z., Garg A.K. Augmentation grafting of the maxillary sinus and simultaneous implant placement in patients with 3 to 5 mm of residual alveolar bone height. Int. J. Oral Maxillofac. Implant. 1999;14:549–556. [PubMed] [Google Scholar]
- 46.Testori T., Wallace S.S., Del Fabbro M., Taschieri S., Trisi P., Capelli M., Weinstein R.L. Repair of large sinus membrane perforations using stabilized collagen barrier membranes: Surgical techniques with histologic and radiographic evidence of success. Int. J. Periodontics Restor. Dent. 2008;28:9–17. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors can provide details of the research upon request by letter commenting on their needs.